Exercise of the week nephro

Summary of the case
Madam P, a 60-year-old Indian lady with underlying diabetes mellitus type 2, hypertension and chronic kidney disease (CKD) presented to the Emergency Department complained of worsening shortness of breath 3 days prior to admission. She was apparently well until she had breathlessness for the past 3 days which worsening and associated with orthopnea and paroxysmal nocturnal dyspnea (PND). She also had productive cough with one teaspoon amount of whitish sputum. It was associated with left leg swelling only since her right leg undergone below knee amputation and had to sleep with 3 pillows since the onset of shortness of breath. Otherwise, she had no history of heart disease, no reduce effort tolerance, no pink frothy sputum, no fever, no chills and rigor, no haemoptysis, no history bed bound. Thirty years ago, she was diagnosed with hypertension and diabetes mellitus type 2 at Hospital Kuala
Lumpur (HKL). She had proper follow up at Hospital Ampang and compliant to the medications. No eyes follow up was done. She also complained of gloves and stocking distribution loss of sensation and blurred visions. Furthermore, 6 years ago she was diagnosed with chronic kidney disease stage 5. And having proper follow up at HKL and her last follow up on September 2017. She has restriction of fluid 500 mL but not compliance to it and refused to have haemodialysis. No remarkable past medical history, past surgical history and no known food and drug allergy. For her family history, her parents died of old age. No familial malignancy history and similar problem ever happened to her family members before.
She is a housewife and live with her daughter. She never smokes, never drinks alcohol, and non-drug abuser.
Her vital signs were recorded as follows; blood pressure was normal 131/69mmHg, normal pulse rate 78 beats per minute, she was tachypneic with respiratory rate 23 breaths per minute and febrile with 37.0 degree celsius. Her SpO2 was normal (99%) and she was hyperglycemic
(DXT 10.6 mmol/l). On examination, fine crepitation can be heard at the lower zone of the right lung. No other significant findings were found on general and systemic examinations.
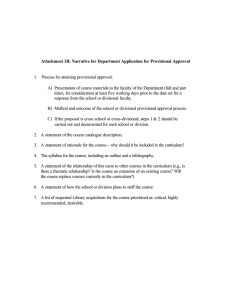
Instruction
1. Identify the chief complain?
2. What is the opening statement? Does it appropriate
3. Does the HOPI contain all of the following :
1. details of the provisional diagnosis?- all positive relevants
2. Risk factors of provisional diagnosis
3. Complications of the provisional diagnosis?
4. Rule out the differential diagnoses (negative relevants, can you guess the differential from the above history?)
5. Any chronic illness? Does in answer the: when? How? What treatment & compliance? Control? Complications?
4. In the physical examination, what features are missing?
5. What is the provisional diagnosis?
6. What is the 4 differential diagnoses?
7. List the appropriate investigations and reason
8. Principle of management