Unit 4 Anki
advertisement
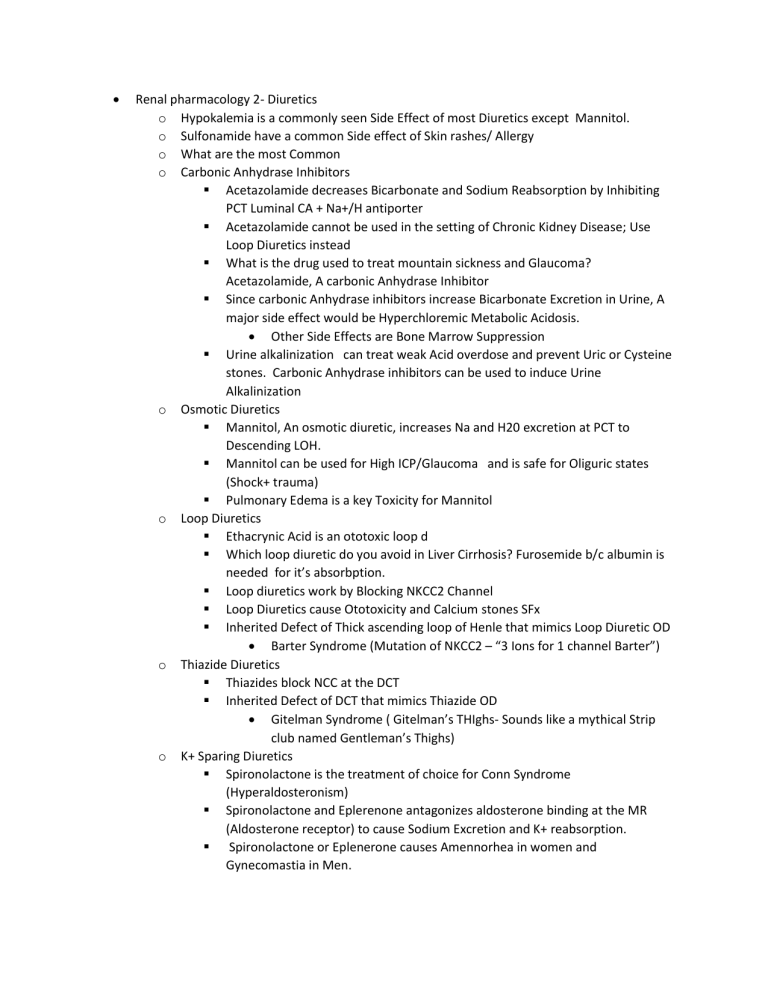
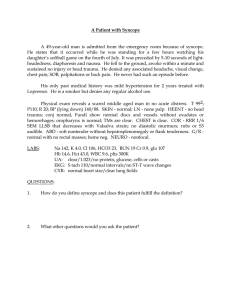
Renal pharmacology 2- Diuretics o Hypokalemia is a commonly seen Side Effect of most Diuretics except Mannitol. o Sulfonamide have a common Side effect of Skin rashes/ Allergy o What are the most Common o Carbonic Anhydrase Inhibitors Acetazolamide decreases Bicarbonate and Sodium Reabsorption by Inhibiting PCT Luminal CA + Na+/H antiporter Acetazolamide cannot be used in the setting of Chronic Kidney Disease; Use Loop Diuretics instead What is the drug used to treat mountain sickness and Glaucoma? Acetazolamide, A carbonic Anhydrase Inhibitor Since carbonic Anhydrase inhibitors increase Bicarbonate Excretion in Urine, A major side effect would be Hyperchloremic Metabolic Acidosis. Other Side Effects are Bone Marrow Suppression Urine alkalinization can treat weak Acid overdose and prevent Uric or Cysteine stones. Carbonic Anhydrase inhibitors can be used to induce Urine Alkalinization o Osmotic Diuretics Mannitol, An osmotic diuretic, increases Na and H20 excretion at PCT to Descending LOH. Mannitol can be used for High ICP/Glaucoma and is safe for Oliguric states (Shock+ trauma) Pulmonary Edema is a key Toxicity for Mannitol o Loop Diuretics Ethacrynic Acid is an ototoxic loop d Which loop diuretic do you avoid in Liver Cirrhosis? Furosemide b/c albumin is needed for it’s absorbption. Loop diuretics work by Blocking NKCC2 Channel Loop Diuretics cause Ototoxicity and Calcium stones SFx Inherited Defect of Thick ascending loop of Henle that mimics Loop Diuretic OD Barter Syndrome (Mutation of NKCC2 – “3 Ions for 1 channel Barter”) o Thiazide Diuretics Thiazides block NCC at the DCT Inherited Defect of DCT that mimics Thiazide OD Gitelman Syndrome ( Gitelman’s THIghs- Sounds like a mythical Strip club named Gentleman’s Thighs) o K+ Sparing Diuretics Spironolactone is the treatment of choice for Conn Syndrome (Hyperaldosteronism) Spironolactone and Eplerenone antagonizes aldosterone binding at the MR (Aldosterone receptor) to cause Sodium Excretion and K+ reabsorption. Spironolactone or Eplenerone causes Amennorhea in women and Gynecomastia in Men. o Amiloride and Trimaterene loop diuretics work directly on Epithelial Na intake channels at CCT Triad of Hypertension, Hypokalemia, and Metabolic alkalosis caused by activated ENaC at the Collecting tubules. What Syndrome? Liddle Syndrome or Pseudo-hyperaldosteronism (Aldosterone binds MR causing Na Reabsorption and K wasting Liddle Syndrome is Tx’ed with Amiloride or triamterene K- Sparing diuretics are given with Loop or Thiazide diuretics to prevent Hypokalemia ADH antagonists Conivaptan-IV / Tolvaptan are used to treat SIADH. Conivaptan/Tolvaptan MOA? Block ADH Receptor V2 Central Diabetes Insipidus is treated by Aquaporin-2 agonists (Desmopressin/Vasopressin). Nephrogenic Diabetes Insipidus treated with Thiazides Mycobacteria o Zieh Nielsen Acid fast organisms retain Carbolfuchsin. Carbolfuchsin, Alcohol, and then methylene Blue counter stain. o M. Tuberculosis is Acid Fast Positive, Uniquely forms Cords , and is Pathogenic in Guinea Pigs. o What is the Cytokine necessary to coordinate a CMI response for TB latency)? TNF alpha. Can be blocked by Remicade causing TB reactivation o Pulmonary TB or ghon complex consists of a Hilar Lymph Node granuloma and Lobar Granuloma. o How does TB establish Extrapulmonary foci? Hematogenous Spread in Naïve Macrophages o What is the Preferred method for culture samples in pediatric TB? Gastric Aspirates o PPD and IGRA (Interferon Gamma release Assay) detect a previous CMI response to TB. o TB therapy requires Directly Observed multidrug Therapy with RIPE (Rifampin, Isoniazid , pyrazinamide and Ethambutol) o Isoniazid Blocks Mycolic Acid Synthesis with Side effect of Hepatitis. o Ethambutol blocks Synthesis of TB cell wall with Side effect of Optic Neuritis. o Previous BCG vaccination or exposure can cause a false Positive TST. o A CMI response is required to clear leprosy. What are the specific types of CMI responses that result in Leprosy? Strong TH1 response leads to Tuberculoid. Th2 antibody production leads to Lepromatous. o Lepromatous leprosy will test Lepromatin PPD Negative and Show Anti- Glycoplid1 antibodies. Tuberculoid will test Lepromatin PPD Positive and LMIT positive (Lymphocyte Migration Inhibition Test) . o M. Leprae is treated with Dapsone and Rifampin for 2 or more years. o Erythema Nodosum rxn to M. Leprae treatment can be treated with thaliodimide o o Atypical Mycobacteria are environmental, Not Lethal in Guinea Pigs, and test negative for TST. Four groups of Atypical Mycobacteria are : Photochromogens produce pigment in light. Scotochromogens produce pigment in dark or light. Non-Chromogens produce no pigment, and Rapidly growing Mycobacteria. Bacterial Pneumonia 2 o How does legionella Infect and survive Inside Alveolar Macrophages? Type IV Secretion System(Alters endosome) And Protease to escape endosome. o What are the risk factors for Legionnaires disease? Older, Immunosuppressed, Smoker/Drinker o Legionella is Diagnosed with a Urine Antigen Test or Special Culture Media (Buffered Charcoal Yeast agar) o Compared to other causes of Atypical Pneumonia, Legionnaire’s pneumonia includes GI and Renal involvement. o Legionella Pneumonia and Mycoplasma Pneumonia are treated with Respiratory fluoroquinolones ( Levofloxacin and Moxifloxacin). o What is the Typical Presentation of Q Fever/ Coxiella Burnetti zoonosis by aerosolization? presents with Pneumonia and Hepatitis. o What is the treatment for Coxiella Burnettii Atypical Pneumonia ? Doxycyline or Flouroquinolones o Name the Bacteria that lacks a peptidoglycan cell wall, Has a cholesterol based Plasma membrane and Causes atypical/ walking Pneumonia? Mycoplasma Pneumoniae o 2 key Virulence factors for Mycoplasma Pneumonia are : Adhesin for Binding to Respiratory cells; CARDS Exotoxin that causes Ciliostasis o A key serological finding of Mycoplasma Walking Pneumonia is High Cold Agglutinin Titers that causes Anemia o A wild young seemingly healthy patient presents with a mild pneumonia and alarming patchy infiltrates on chest X-ray would increase suspicion for Mycoplasma Walking Pneumonia CAD Pharmacotherapy o STEMIs are seen with complete Coronary Artery occlusion causing epicardial and endocardial ischemia. o NSTEMIs are seen w/ partial coronary occlusion leading to endocardial ischemia. o Acute management of STEMIs mainly involves Reperfusion therapy with PCI angioplasty or Fibrinolytics ( tPA-Alteplase) if unavailable. o Fibrinolytics are contraindicated with recent surgery or Stroke, Brain Tumor, or Past history of Intracranial Bleeding o Heparin is used for Chronic management after Fibrinolytics in STEMI. Used separately in NSTEMI. o o o o o Heparin dosing is determined by aPTT or Anti-Xa Assay . Unfractionated Heparin is administered more often than LMWH. Bleeding and Heparin Induced Thrombocytopenia are key side effects of Heparin Use. What are other therapeutic approaches for Acute management of STEMI? MONA (Morphine, Oxygen, Nitrates, and Aspirin) Define Chest Jaw or Arm Discomfort that worsens with stress or exertion and Improves with Nitroglycerin. Angina Adjuvant therapy for ACS ( MI or Unstable Angina) includes : beta blockers to reduce Myocardial O2 demand ACE Inhibitors or ARB to reduce mortality and Aneurysm formation/ wall remodeling Statins to lower cholesterol Levels o All of the following are contraindications of Beta Blocker Use in acute MI Hypotension, Bradycardia, Asthma, Heart Block, Hypertension o Unstable Angina and NSTEMI are treated with Heparin ( to prevent clot formation) and Antiplatelet agents. o Antiplatelet agents used in NSTEMI are ADP receptor Blockers and Direct GP2/3a blockers o Name 2 Irreversible ADP receptor ( P2Y12) blockers that block platelet aggregation Clopidrogrel 1st line antiplatelet agent and Prasugrel ( More powerful; Increased bleeding risk ) o Name the Anitplatelet that is Safe only in patients < 75 YO weighing over 60 Kg without a history of Stroke or TIA Prasugrel o Ticagrelor is a reversible ADP receptor Blocker that is dosed twice daily o Abciximab, Eptifibatide and tirofiban are examples of direct Gp IIb/IIIa receptor blockers ( Prevents Platelet Aggregation) Syncope Evaluation and Management o Transient and complete loss of consciousness with loss of postural tone Syncope o Syncope occurs when there is decreased cerebral perfusion o 3 etiologies of Syncope : Neural/Reflex, Orthostatic Hypotension, and Cardiac. o A premonition, then drop in blood pressure followed by Bradycardia indicates Neural Syncope caused by loss of Sympathetic tone o A Drop in BP followed by Tachycardia indicates Orthostatic Hypotension Decreased peripheral Vasoconstriction triggered by DAAD( Drugs, Autonomic Dysfn, Alcohol and Dehydration) o Describe the presentation of Cardiac Syncope Sudden Drop attack due to Arrhythmia and Structural Heart disease o Syncope after sudden noise or extreme emotion indicates Cardiac Syncope ( Long QTSyndrome) o o o Long QT shows low Magnesium. Treated by Administering IV Magnesium Tilt table testing is used to confirm Neural/Vasovagal syncope. Cardiac Syncope is Confirmed with cardiac event monitors How are neural and orthostatic Hypotension Syncope managed? Primarily lifestyle Modifications to avoid triggers and dehydration. Stockings for counterpressure Alpha agonists (Midodrine) Bradycardic Cardiac Syncope is treated with Pacemaker implantation while Tachyarrhythmic cardiac syncope is treated with AICD (Defibrillation)