Abstract final draft
advertisement

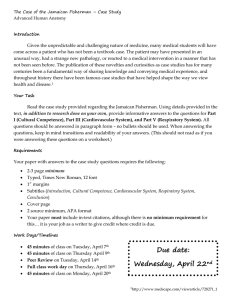
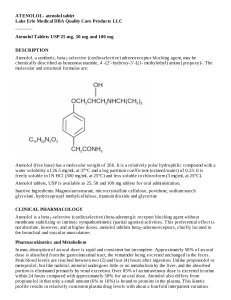
Comparison of acute effects of beta-adrenoceptor antagonists on cardiovascular and respiratory function Abstract: Background and Purpose: Beta-Adrenergic receptor antagonists β-blockers have been considered a cornerstone therapeutic drug class used to treat cardiovascular conditions such as hypertension and heart disease for decades. However, despite well-established cardiovascular and antihypertensive benefits, poor receptor selectivity of some β-blockers may precipitate adverse respiratory effects. The purpose of this study was to determine the acute effects of two B-adrenoceptor antagonists with variable specificity on cardiovascular system and respiratory function. Subjects and Methods: A placebo-controlled double-blind randomised 3-hour trial was performed to investigate effects of atenolol (β1-selective) and pindolol (non-selective βblocker with intrinsic sympathomimetic activity) at equipotent doses (100 mg and 10 mg for atenolol and pindolol respectively). Recruitment of subjects was done on a voluntary participation basis. Groups A and B contained 8 and 9 randomly selected subjects respectively, and Group C contained 6 randomly selected subjects. Group P contained 10 subjects who opted out with and were excluded from treatment considerations of their asthma, diabetes, heart failure, depression, or drug interactions. Group P subjects received a placebo. Group A subjects were treated with pindolol (10 mg (>60 kg) or 5 mg (<60 mg)), Group B was assigned atenolol (100 mg (>60 kg) or 50 mg (<60)), and Group C subjects received a matching placebo. Cardiovascular function was assessed every 15 mins from baseline (for 150 mins inclusive). These tests were resting heart rate (bpm), systolic blood pressure (mmHg), diastolic blood pressure (mmHg) (indirect measurements), and facial temperature (°C). Heart rate (bpm) and perceived fatigue (scale of 1-5) after exercise was measured at each 30 min interval of the trial (beginning at 30 mins from baseline). Respiratory function was measured throughout the trial (every 15 mins from baseline) represented by subjects’ peak expiratory flow (L/min). End point was chosen to be when a subject feels faint and the study was terminated for that individual. Results: Treatment with cardioselective beta-adrenergic antagonist atenolol was associated with a significant decrease in resting heart rate (bpm) (11% from baseline), and the same effects were seen to a much lesser extent with non-selective pindolol (4% decrease) due to the drug’s inherent ISA. After exercise however cardiovascular impairment was more pronounced, as pindolol was seen to reduce HR by 22% and atenolol caused a 16% decrease from baseline. SBP was reduced more by pindolol than atenolol (16% reduction vs 14% and DBP was decreased more by atenolol (13% vs 12% decrease). PEF remained constant in the constant in the group treated with atenolol (0.3% decrease at 135 min), but treatment with pindolol caused a 2% decrease in PEF due to its relatively large affinity for β2 receptors at the dose used. Conclusion: Nevertheless, upon comparison of B1 selective atenolol and non-selective ISA pindolol, it was determined that respiratory function was not significantly impacted by either drugs and would but further studies with a larger sample size might clarify findings and determine the safety for COPD or asthma sufferers. Furthermore, our study suggests atenolol impacted cardiovascular greater without causing side effects and had the most advantageous effects. Keywords: Hypertension, Asthma, Heart disease, Beta-blocker, Intrinsic Sympathomimetic Activity.