Oligomeric α-Synuclein as PD Biomarker
advertisement
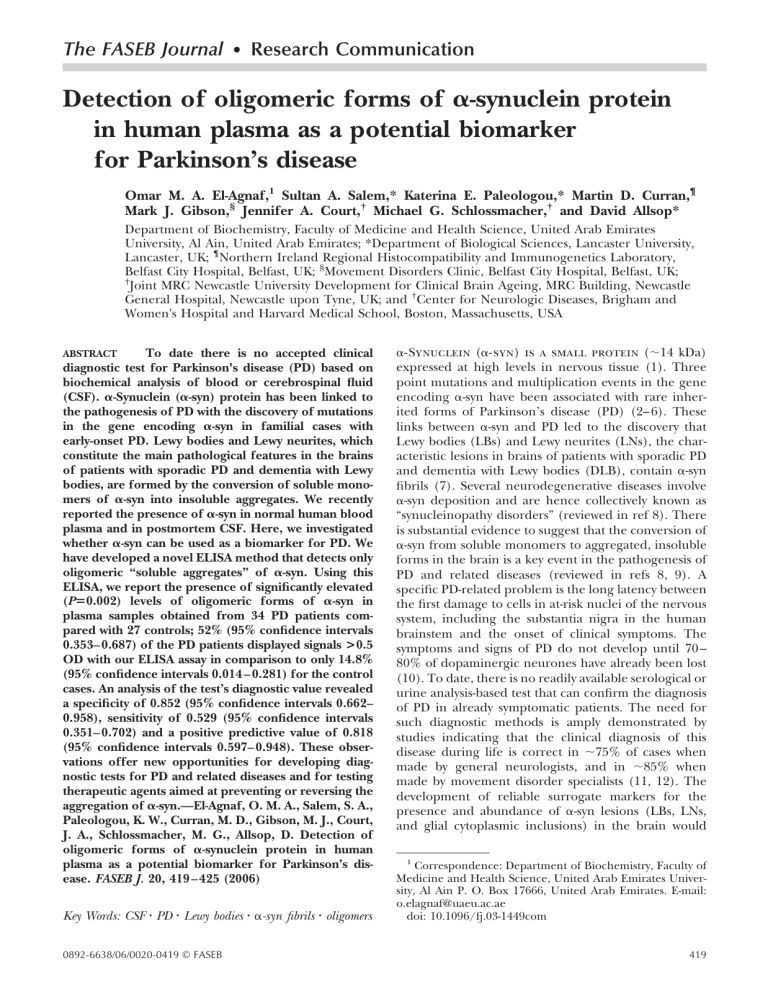
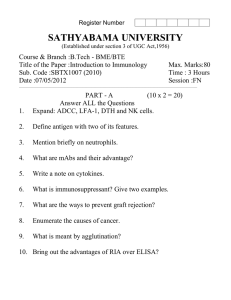
The FASEB Journal • Research Communication Detection of oligomeric forms of ␣-synuclein protein in human plasma as a potential biomarker for Parkinson’s disease Omar M. A. El-Agnaf,1 Sultan A. Salem,* Katerina E. Paleologou,* Martin D. Curran,¶ Mark J. Gibson,§ Jennifer A. Court,† Michael G. Schlossmacher,† and David Allsop* Department of Biochemistry, Faculty of Medicine and Health Science, United Arab Emirates University, Al Ain, United Arab Emirates; *Department of Biological Sciences, Lancaster University, Lancaster, UK; ¶Northern Ireland Regional Histocompatibility and Immunogenetics Laboratory, Belfast City Hospital, Belfast, UK; §Movement Disorders Clinic, Belfast City Hospital, Belfast, UK; † Joint MRC Newcastle University Development for Clinical Brain Ageing, MRC Building, Newcastle General Hospital, Newcastle upon Tyne, UK; and †Center for Neurologic Diseases, Brigham and Women's Hospital and Harvard Medical School, Boston, Massachusetts, USA To date there is no accepted clinical diagnostic test for Parkinson's disease (PD) based on biochemical analysis of blood or cerebrospinal fluid (CSF). ␣-Synuclein (␣-syn) protein has been linked to the pathogenesis of PD with the discovery of mutations in the gene encoding ␣-syn in familial cases with early-onset PD. Lewy bodies and Lewy neurites, which constitute the main pathological features in the brains of patients with sporadic PD and dementia with Lewy bodies, are formed by the conversion of soluble monomers of ␣-syn into insoluble aggregates. We recently reported the presence of ␣-syn in normal human blood plasma and in postmortem CSF. Here, we investigated whether ␣-syn can be used as a biomarker for PD. We have developed a novel ELISA method that detects only oligomeric “soluble aggregates” of ␣-syn. Using this ELISA, we report the presence of significantly elevated (Pⴝ0.002) levels of oligomeric forms of ␣-syn in plasma samples obtained from 34 PD patients compared with 27 controls; 52% (95% confidence intervals 0.353– 0.687) of the PD patients displayed signals >0.5 OD with our ELISA assay in comparison to only 14.8% (95% confidence intervals 0.014 – 0.281) for the control cases. An analysis of the test’s diagnostic value revealed a specificity of 0.852 (95% confidence intervals 0.662– 0.958), sensitivity of 0.529 (95% confidence intervals 0.351– 0.702) and a positive predictive value of 0.818 (95% confidence intervals 0.597– 0.948). These observations offer new opportunities for developing diagnostic tests for PD and related diseases and for testing therapeutic agents aimed at preventing or reversing the aggregation of ␣-syn.—El-Agnaf, O. M. A., Salem, S. A., Paleologou, K. W., Curran, M. D., Gibson, M. J., Court, J. A., Schlossmacher, M. G., Allsop, D. Detection of oligomeric forms of ␣-synuclein protein in human plasma as a potential biomarker for Parkinson’s disease. FASEB J. 20, 419 – 425 (2006) ABSTRACT Key Words: CSF 䡠 PD 䡠 Lewy bodies 䡠 ␣-syn fibrils 䡠 oligomers 0892-6638/06/0020-0419 © FASEB ␣-Synuclein (␣-syn) is a small protein (⬃14 kDa) expressed at high levels in nervous tissue (1). Three point mutations and multiplication events in the gene encoding ␣-syn have been associated with rare inherited forms of Parkinson’s disease (PD) (2– 6). These links between ␣-syn and PD led to the discovery that Lewy bodies (LBs) and Lewy neurites (LNs), the characteristic lesions in brains of patients with sporadic PD and dementia with Lewy bodies (DLB), contain ␣-syn fibrils (7). Several neurodegenerative diseases involve ␣-syn deposition and are hence collectively known as “synucleinopathy disorders” (reviewed in ref 8). There is substantial evidence to suggest that the conversion of ␣-syn from soluble monomers to aggregated, insoluble forms in the brain is a key event in the pathogenesis of PD and related diseases (reviewed in refs 8, 9). A specific PD-related problem is the long latency between the first damage to cells in at-risk nuclei of the nervous system, including the substantia nigra in the human brainstem and the onset of clinical symptoms. The symptoms and signs of PD do not develop until 70 – 80% of dopaminergic neurones have already been lost (10). To date, there is no readily available serological or urine analysis-based test that can confirm the diagnosis of PD in already symptomatic patients. The need for such diagnostic methods is amply demonstrated by studies indicating that the clinical diagnosis of this disease during life is correct in ⬃75% of cases when made by general neurologists, and in ⬃85% when made by movement disorder specialists (11, 12). The development of reliable surrogate markers for the presence and abundance of ␣-syn lesions (LBs, LNs, and glial cytoplasmic inclusions) in the brain would 1 Correspondence: Department of Biochemistry, Faculty of Medicine and Health Science, United Arab Emirates University, Al Ain P. O. Box 17666, United Arab Emirates. E-mail: o.elagnaf@uaeu.ac.ae doi: 10.1096/fj.03-1449com 419 naturally facilitate a more streamlined work-up during the early care of movement disorder patients, and allow for the biologically guided evaluation of future drug trials aimed at neuroprotection in the synucleinopathies. incubated with 100 L/well of ExtrAvidin-Alkaline phosphatase (Sigma) diluted 3:5000 in blocking buffer and incubated for 1 h at 37°C. The wells were then washed 4 times with PBST, before adding the enzyme substrate Yellow “pNPP” (Sigma) (100 L/well) and leaving the color to develop for 30 min at room temperature. Absorbance values at 405 nm were determined. PATIENTS AND METHODS Cerebrospinal fluid samples Preparation of ␣-syn Recombinant ␣-syn was expressed in Escherichia coli and purified as described previously (1, 13). Preparation of aged solutions of ␣-syn Purified samples of ␣-syn in sterilized phosphate-buffered saline (137 mM phosphate buffer, 150 mM NaCl, pH 7.4) (PBS), in parafilm-sealed, 1.5 mL Eppendorf tubes were incubated at 37°C for 4 days in an Eppendorf Thermomixer with continuous mixing (1000 rpm). Samples were collected at various time points and stored at – 80°C until tested by the ELISA. Antibodies The antibody used for the ELISA to detect ␣-syn oligomers was 211 mouse monoclonal antibody (mAb) (Santa Cruz Biotechnology, Santa Cruz, CA, USA), which recognizes amino acid residues 121-125 of human ␣-syn This mAb did not react with recombinant -synuclein or ␥-synuclein on Western blots. Some plasma samples were depleted of ␣-syn prior to analysis in the ELISA. This was achieved by prior treatment with magnetic dynabeads coupled to antibody LB509 (a mouse monoclonal antibody to ␣-syn residues 115-12, from Zymed Laboratories, San Francisco, CA, USA) or to antibody FL-140 (a rabbit polyclonal antibody raised against full-length ␣-syn, from Santa Cruz Biotechnology), as described (14). Preparation of the biotinylated antibody Sulfo-NHS-LC-Biotin (Pierce, Rockford, IL, USA) (200 g) was reacted with the antibody to be biotinylated (1 mL at 200 g/mL) in PBS, then placed on ice for 2 h. The mixture was desalted on Bio-Spin-6 columns (BIO-RAD, UK) to remove excess uncoupled biotin. The biotinylated antibodies were stored at 4°C until used. An ELISA to measure ␣-syn oligomers An ELISA plate was coated by overnight incubation with 1 g/mL of nonbiotinylated mAb 211 (100 L/well), in 200 mM NaHCO3 (Sigma, St. Louis, MO, USA), pH 9.6, containing 0.02% (w/v) sodium azide at 4°C, washed 4 times with PBST (PBS containing 0.05% Tween 20), and incubated with 200 L/well of blocking buffer (PBS containing 2.5% gelatin and 0.05% Tween 20) for 2 h at 37°C. The plate was washed 4 times with PBST, and 100 L of the samples to be tested were added to each well (fresh or aged ␣-syn solutions were diluted to 500 nM in PBS; cerebrospinal fluid (CSF) samples were diluted 1:1 with PBS, whereas plasma samples were used neat). The plate was incubated at 37°C for 2 h. After washing 4 times with PBST, 100 L of biotinylated mAb 211 diluted to 1 g/mL in blocking buffer was added, and incubated at 37°C for 2 h. The wells were washed 4 times with PBST and 420 Vol. 20 March 2006 Postmortem CSF samples were obtained from the London Neurodegenerative Diseases Brain Bank (Department of Neuropathology, Institute of Psychiatry, King’s College, UK), Queen Square Brain Bank for Neurological Disorders (Department of Molecular Pathogenesis, Institute of Neurology, University College London, UK), and The Newcastle Brain Tissue Resource (Joint MRC Newcastle University Development for Clinical Brain Ageing, MRC Building, Newcastle General Hospital, Westgate Road, Newcastle upon Tyne, UK). The samples were stored at – 80°C before analysis. Repeat freeze/thaw cycles were avoided. Plasma samples Blood samples were obtained from 34 clinically diagnosed PD patients (50% female, 50% male, age range 54 – 82 years, mean age 65.4) attending an outpatients’ clinic in the Neurology Department of Belfast City Hospital. For each case, the diagnosis of idiopathic PD was made by a consultant neurologist (M.J.G.), based on the UK Parkinson's Disease Society Brain Bank criteria for idiopathic Parkinson's disease (15). The diagnosis was made on the basis of a progressive history and more than two of the cardinal signs of PD being present (resting tremor, bradykinesia, rigidity, postural instability). In addition, there was an absence of any features, suggesting an alternative cause for parkinsonism. All subjects had been followed up in a Movement Disorders Clinic for at least 2 years. Ethical Committee approval was obtained and written consent given by all subjects. Age-matched control samples were obtained from the Haematology Department at Blackpool Victoria Hospital (50% female, 50% male, age range 55– 85 years, mean age 68.0). The control samples were from individuals suffering from disorders such as cancer, heart disease, stroke, diabetes, and chronic renal failure. For statistical analysis, the controls were not individually matched with each PD case. Ethical Committee approval was also obtained for these control samples. Blood (10 mL) was collected in plastic tubes containing either sodium citrate or potassiumEDTA from all subjects, and plasma was separated by centrifuging the blood at 3000 rpm at 4°C for 20 min. Plasma was collected in 0.5 mL plastic tubes and stored frozen at – 80°C. The samples were thawed at room temperature directly before analysis. Size exclusion chromatography Sephadex G-75 superfine gel (Amersham Pharmacia Biotech, Uppsala, Sweden) was packed into a 44 cm long and 1 cm internal diameter column. CSF or plasma samples were cleared by centrifugation (3000 rpm or 20 min), then 0.5 mL loaded onto the column and eluted with 50 mM ammonium acetate (pH 7.4) at a flow rate of 0.25 mL/min. Absorbance of the eluted material was monitored at 215 nm. Fractions of 1 mL were collected, concentrated to 300 L by centrifugation under vacuum, and analyzed by the ELISA for the presence of ␣-syn oligomers. The FASEB Journal EL-AGNAF ET AL. Statistical analysis Fisher’s exact probability tests were performed to assess whether the frequency differences observed between the levels of ␣-syn oligomers found in the cohort of PD subjects and the age-matched control group were statistically significant using the computer package “StatsDirect” (www. statsdirect.com). It was not possible to individually match the disease/control samples. Three arbitrary cutoff points were chosen (0.2, 0.3, and 0.5 OD absorbance at 405 nm) to discern the threshold of positive correlation between the clinical working diagnosis of PD and the signal obtained for the ELISA of plasma results, with cases above this point deemed to possess high levels of ␣-syn oligomers. RESULTS We recently reported the detection of ␣-syn in human plasma, postmortem CSF, and conditioned medium of neuronal cell cultures by immunoprecipitation followed by sodium dodecyl sulfate PAGE (SDS-PAGE) and Western blot methods (14). In this previous work, we found considerable overlap in the amount of monomeric ␣-syn detected in CSF and plasma samples from normal individuals and those from patients with PD and DLB. However, this work involved immunocapture of ␣-syn on magnetic dynabeads, followed by elution from the beads and separation by SDS-PAGE. This protocol thereby involves denaturing the proteins with heating and strong detergent (SDS), which could result in disassociation of any oligomeric forms of ␣-syn that we hypothesized to be present in vivo (16). Therefore, we developed a specific and sensitive novel ELISA method that uses a nondenaturing approach designed to recognize only the oligomeric species of human ␣-syn. Here, we have refined this method to detect oligomeric forms of ␣-syn in human CSF and plasma. The ELISA is based on a conventional sandwich system with capture of ␣-syn by highly specific anti-␣-syn monoclonal antibody (mAb) 211, followed by detection with a biotinylated form of the same mAb (Fig. 1A). The biotinylated mAb is subsequently detected with ExtrAvidin-Alkaline phosphatase, followed by a colorimetric enzyme substrate. Monomeric ␣-syn cannot give a signal in this assay because the capture mAb occupies the only antibody binding site available on the protein, but in the case of oligomeric forms of ␣-syn, multiple mAb binding sites are available, permitting both capture and detection (Fig. 1A). Recently, we successfully developed a similar ELISA for the detection of oligomeric A peptide, associated with Alzheimer’s disease (AD) (17). First, we studied the time-dependent oligomerization of recombinant ␣-syn using this novel ELISA and found that freshly dissolved ␣-syn (715 ng/well in a 96-well plate assay) gave a signal of 0.01 optical density (OD) units, whereas ␣-syn that had been allowed to aggregate at 37°C for 4 days in PBS at pH 7.4 gave a signal of 2.3 OD (Fig. 1B). Detection of a large signal in the ELISA correlated with the presence of soluble aggregates or “oligomeric” forms of ␣-syn (Fig. 1B, C). Solutions of OLIGOMERIC ␣-SYNUCLEIN AS BIOMARKER Figure 1. Oligomerization of ␣-syn measured by the ELISA. A) Principle of ELISA for oligomeric ␣-synuclein. B) Characterization of the ELISA. Solutions of ␣-syn in PBS at 50 M, 10 M, and 5 M were incubated at 37°C, diluted to 0.5 M, and transferred to a microtiter plate already coated with immobilized mAb 211. Additional epitopes formed by oligomerization of ␣-syn during the preincubation step were measured by the subsequent binding of biotinylated mAb 211. Data shown are representative of 5 independent experiments, from 3 different preparations of ␣-syn. Measurements were taken in triplicate, and the results show the mean ⫾ standard deviation for each point. C) Effect of the concentration of ␣-syn oligomers on the ELISA response. A solution of ␣-syn in PBS at 50 M was incubated for 4 days at 37°C, diluted to 1000 – 0.1 nM in PBS, and transferred to a microtiter plate coated with immobilized mAb 211. Assays were performed in triplicate; mean ⫾ standard deviations are shown. The mid-range of the assay for ␣-syn incubated for 4 days was 500 nM of the starting concentration of the fresh sample. At 500 nM, the within-assay variance was 5.3%. A day-to-day variance of 4.9% at 500 nM was found in 5 assays calibrated with standard solutions of 50 M ␣-syn incubated in PBS for 4 days, diluted to 0.5 M in PBS, divided into aliquots, and stored at – 80°C. 421 ␣-syn showed a gradual increase in the formation of oligomers as the concentrations and time of preincubation were increased (Fig. 1B). The ELISA gave a poor signal when ␣-syn was predominantly in the form of mature fibrils or “insoluble aggregates,” as revealed by a thioflavin-T binding assay and by electron microscopy (data not shown). We estimated the lower limit of detection of recombinant protein by the ELISA was ⬃14.3 ng/well, based on the starting concentration of the fresh ␣-syn sample (Fig. 1C). We investigated whether our ELISA could detect any ␣-syn oligomers in postmortem CSF samples at the time of autopsy from patients with PD and related disorders (based on clinical diagnosis and postmortem histopathology). Two of the three PD samples tested, and two of the eight DLB samples tested, gave a high signal (0.2–2.0 OD units), whereas very low signals (⬍0.1 OD) were obtained from 40 controls, including 26 nonneurological disease controls, 11 cases of AD, and 3 cases of motor neurone disease (data not shown). Given these results, which suggested the presence of soluble oligomers of ␣-syn in the extracellular space, we used the ELISA to test for the presence of soluble ␣-syn oligomers in a larger number of samples of peripheral plasma from PD cases and controls. We screened the plasma samples and observed that 18 of 34 (52%) PD samples gave a relatively high signal in the ELISA (⬎0.5 OD), whereas only 4 of 27 (14.8%) control samples gave a similar signal (Fig. 2). Overall the results generated a statistically significant difference between the PD and control samples (P⫽0.002), suggesting that the concentration of oligomeric ␣-syn is increased dramatically in PD plasma. This difference is further exaggerated (P⫽0.0003) if one extends the analysis to cases displaying levels above 0.3 OD, with 22 PD cases (64%) and 5 control samples (18%). A similar level of statistical significance is also achieved with a cutoff of 0.2 OD (P⫽0.0003) with 26 PD cases (76%) and 8 control cases (29%). Similar results were obtained whether plasma was collected in citrate or in EDTA tubes. When the reliability of the test is assessed by determining the established measurements of specificity (proportion of individuals without the disease who are correctly iden- tified by the test) and sensitivity (proportion of individuals with the disease who are correctly identified by the test) for these data, it is clear the test has significant diagnostic promise. Its specificity of 0.852 is relatively high, while the sensitivity of 0.529 is moderate for the selected cutoff of ⬎0.5 OD. This is again reflected in the positive and negative predictive values for the test, 0.818 (95% confidence intervals 0.597– 0.948) and 0.589 (95% confidence intervals 0.421– 0.744), respectively. However, a reduction of the cutoff of 0.5 OD units (which reflects an arbitrary decision by us to segregate the data) to 0.3 OD units improves the sensitivity to 0.647 (95% confidence intervals 0.465– 0.802) and only slightly compromises the specificity i.e., 0.814 (95% confidence intervals 0.619 – 0.937). A further drop in the cutoff to 0.2 OD units reduces the specificity further (0.7037, 95%CI 0.498 – 0.862) and again increases the sensitivity (0.765, 95%CI 0.588 – 0.892). While a sensitivity and specificity that are both as close to 1 as possible is ideal, in practice (as displayed here), sensitivity is gained at the expense of specificity and vice versa. To avoid making a false positive diagnosis a high specificity would be favored. This, together with the fact that the likelihood ratios for the 0.5 and 0.3 OD units cutoff points are similar, 3.57 (95% confidence intervals 1.50 –9.33) and 3.49 (95% confidence intervals 1.65– 8.14), respectively, and higher than the 0.2 OD cutoff of 2.58 (95% confidence intervals 1.49 – 4.93), makes either a good choice as a cutoff value for the test in its current form. When plasma samples were first immunoprecipitated with anti-␣-syn antibodies LB509, FL-140, or syn-1 coupled to magnetic beads (or to protein G Sepharose beads in the case of syn-1) (14), then tested by the ELISA, only traces of signals could be detected above background when compared with non-␣-syn-directed, “negative control IgG”-mediated capturing, suggesting that immunodepletion removed the antigen from the initial sample (data not shown). These data further demonstrated the specificity of the ELISA and show, for example, that the signal generated was not due to nonspecific binding of the biotinylated antibody to other proteins in our specimens. Figure 2. Detection of ␣-syn oligomers in human plasma. Plasma samples from Parkinson’s disease (PD) and control patients (C) (100 L) were analyzed by the ELISA for oligomeric ␣-syn. Data shown are representative of at least 4 independent experiments. The assays were performed in triplicate; mean ⫾ standard deviations are shown. 422 Vol. 20 March 2006 The FASEB Journal EL-AGNAF ET AL. To confirm that our ELISA detects only soluble oligomers and not monomeric forms of ␣-syn in our CSF and plasma specimens, we used size exclusion chromatography (SEC) to determine the molecular weight (MW) of the immunoreactive protein (Fig. 3). Recently, Sephadex G75 columns have been used successfully to detect soluble oligomers of ␣-syn in extracts from PD and DLB brains (18). The Sephadex G75 column used in our study gave a linear elution profile for a set of protein standards with MWs of 8 to 67 kDa, similar to those in the previous report (18). Postmortem CSF and plasma samples from those PD patients that gave a robust signal in the ELISA revealed immunoreactive material with an elution peak in SEC fractions corresponding to MWs of 55–70 kDa. Much of the immunoreactive material was eluted at the void volume, which indicated a MW of ⬎70 kDa (Fig. 3A, C). These SEC fractionation results are consistent with the detection of ␣-syn oligomers, since the protein material detected by the ELISA has a MW much greater than that of the monomeric form of ␣-syn. As expected, no significant immunoreactivity was detected in SEC fractions from control samples with low signals in the ELISA (Fig. 3B, D). Experiments are in progress in our laboratory to further characterize and analyze the structure and nature of the oligomeric species of ␣-syn and to discern any modifications of ␣-syn detected by the ELISA (i.e., nitrated, phosphorylated, dimers, or trimers, etc.). This information will be useful in order to improve both the sensitivity and selectivity for ␣-syn protein species in our future ELISA variants. DISCUSSION Our recent studies have shown that neuronal cells in culture constitutively secrete ␣-syn into the culture medium and that ␣-syn is normally present in CSF and peripheral plasma (14). There is some evidence that certain toxic metabolites, including the A peptide implicated in the pathogenesis of AD, can be cleared from the brain by drainage from the interstitial fluid into the CSF, then into the blood plasma (19). Further support for this idea has come from studies with a transgenic mouse model of AD, where peripheral administration of a monoclonal antibody to A was found to induce a rapid increase in plasma A, and the magnitude of this increase was highly correlated with amyloid burden in the hippocampus and cortex (20, 21). These results demonstrated that A can efflux from the brain into the plasma pool, and therefore, a similar mechanism could operate for ␣-syn. At present, it is unclear whether this “effluxed” A is an oligomeric form of the peptide. Nevertheless, the opposite may be true as well, where a principally peripheral source of ␣-syn derived from either corpuscular elements of whole blood (22) or peripheral organs, (e.g., liver) is responsible for detection of ␣-syn in plasma. The possibility of a peripheral source is particularly relevant in light of the very low OLIGOMERIC ␣-SYNUCLEIN AS BIOMARKER Figure 3. Size exclusion chromatographic analysis of ␣-syn oligomers in CSF and plasma. 0.5 mL of plasma from a PD patient (A) and a control (B), and CSF from a PD patient (C), and a control (D) were fractionated on a Sephadex G75 SEC column. Fractions (F ) of 1 mL were collected, concentrated to 300 L, and analyzed by the ELISA for the presence of ␣-syn oligomers. Peak fractions for the molecular weight (MW) standards are indicated. These were bovine serum albumin (67 kDa), ovalbumin (43 kDa), chymotrypsinogen A (25 kDa), myoglobin (18 kDa), and ubiquitin (8 kDa). The void volume corresponds to MW ⬎ 70 kDa. Freshly dissolved and preaggregated (aged) recombinant ␣-syn (ra-syn) were also tested in the ELISA. levels of total ␣-syn reactivity that are detectable in human CSF from living persons when compared with brain and plasma ␣-syn steady states (M. G. Schlossmacher et al., unpublished observation; El-Agnaf et al., 423 unpublished results). Likewise, future cell biological research will have to address the mechanism by which ␣-syn protein (and oligomers thereof) can be found in the extracellular space under physiological conditions (14), since no alternative splice variant has been published so far that would direct the nascent ␣-syn protein into and through the secretory pathway, and no such transcript of the SNCA gene could be found in an extensive investigation of primate brain specimens (M. G. Schlossmacher, unpublished data). There is some evidence for the existence of oligomeric forms of A and of the prion protein (PrP) that is associated with transmissible spongiform encephalopathies (TSEs) in CSF from patients with AD and the TSEs, respectively, but not in controls (23, 24). These various studies, together with mounting evidence for soluble oligomers being the pathogenetic species that drive neurodegeneration and neuronal cell death (25–31), led us to hypothesize that detection of soluble oligomers of ␣-syn in biological fluids could have potential use as a biomarker for PD and related diseases (16). Therefore, we developed a simple and novel ELISA method that specifically recognizes only oligomeric species of ␣-syn. We used this method to probe for oligomeric forms of ␣-syn in human CSF and in plasma. Based on our preliminary results, the ELISA was able to detect ␣-syn oligomers in postmortem CSF from some PD and DLB patients, but only a very low signal was obtained from all control samples tested. These data suggested a higher amount of ␣-syn oligomer production in PD patients either in vivo or during postmortem autolysis. Regrettably, at the writing of this report, no leftover CSF specimens were available from living PD patients to address this question. These promising results led us to carry out an extensive study of the more accessible peripheral blood plasma. We found there was a highly statistically significant difference between PD samples and controls, with most of the PD samples giving high signals, whereas only a few control samples gave a high signal. Our control samples consisted of a random selection of blood samples from a single hematology laboratory. The variation in signal from both PD and control subjects in this first cohort could be related to a number of different factors, including (but not limited to) differential blood cell count numbers, total plasma protein concentration, total ␣-syn content, ␣-syn turnover by degradation in the extracellular space, comorbidities, medication, and, last but not least, postphlebotomy processing time. If ␣-syn oligomerization occurs before the death of nigral neurons in PD, then our ELISA could potentially provide a diagnostic tool for the detection of oligomers in the early stages of the disease. This could lead to earlier detection and neuroprotective treatment intervention for high-risk subjects in the future. More extensive clinical studies are required to confirm and extend our results and to validate the ELISA as a potential diagnostic test for disease state. In fact, we recently began enrolment of subjects in a prospective, 424 Vol. 20 March 2006 case control study of 300 persons to be conducted over 2 years to monitor their oligomeric and total ␣-syn load in peripheral plasma. It will be interesting to determine whether there is any correlation between detection of ␣-syn oligomers and the severity and/or the stage of the disease and/or the rate of its progression. Studies performed on blood samples from familial PD cases will be useful to further validate the ELISA as an early diagnostic method (32). We also recognize that any medication, including dopaminergic replacement therapy, taken by previously diagnosed PD patients could influence the ELISA results (33). Studies of newly diagnosed patients who are not yet taking any medication (de novo) will indicate whether drugs have any confounding effect. The ELISA can also be used for high-throughput screening for modulators of ␣-syn oligomerization as potential novel drugs for PD and related disorders during preclinical validation studies prior to their evaluation in rodent or nonhuman primate models of PD (34). Moreover, the principle of our ELISA could be applied for the development of similar sensitive diagnostic tests for the presence of other forms of oligomeric protein aggregates, such as those found in AD (A) and the TSEs (PrP). We are grateful for support from Michael J. Fox Foundation (to O.M.E-A. and M.G.S.) and The Alzheimer’s Research Trust (to D.A. and S.A.S.). We thank The London Neurodegenerative Diseases Brain Bank (Department of Neuropathology, Institute of Psychiatry, King’s College, UK), The Queen’s Square Brain Bank for Neurological Disorders (Department of Molecular Pathogenesis, Institute of Neurology, University College London, UK) for the human postmortem CSF samples. REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. Jakes, R., Spillantini, M. G., and Goedert, M. (1994) Identification of two distinct synucleins from human brain. FEBS Lett. 345, 27–32 Polymeropoulos, M. H., Lavedan, C., Leroy, E., Ide, S. E., Dehejia, A., Dutra, A., Pike, B., Root, H., Rubenstein, J., Boyer, R., et al. (1997) Mutation in the ␣-synuclein gene identified in families with Parkinson’s disease. Science 276, 2045–2047 Kruger, R., Kuhn, W., Muller, T., Woitalla, D., Graeber, M., Kosel, S., Przuntek, H., Epplen, J. T., Schols, L., and Riess, O. (1998) Ala30Pro mutation in the gene encoding ␣-synuclein in Parkinson’s disease. Nature Gen. 18, 106 –108 Zarranz, J. J., Alegre, J., Gomez-Esteban, J. C., Lezcano, E., Ros, R., Ampuero, I., Vidal, L., Hoenicka, J., Rodriguez, O., Atares, B., et al. (2004) The new mutation, E46K, of ␣-synuclein causes Parkinson and Lewy body dementia. Ann. Neurol. 55, 164 –173 Singleton, A. B., Farrer, M., Johnson, J., Singleton, A., Hague, S., Kachergus, J., Hulihan, M., Peuralinna, T., Dutra, A., Nussbaum, R., et al. (2003) ␣-Synuclein locus triplication causes Parkinson's disease. Science 302, 841 Chartier-Harlin, M. C., Kachergus, J., Roumier, C., Mouroux, V., Douay, X., Lincoln, S., Levecque, C., Larvor, L., Andrieux, J., Hulihan, M., et al. (2004) ␣-Synuclein locus duplication as a cause of familial Parkinson's disease. Lancet 364, 1167–1169 Spillantini, M. G., Crowther, R. A., Jakes, R., Hasegawa, M., and Goedert, M. (1998) Alpha-Synuclein in filamentous inclusions of Lewy bodies from Parkinson's disease and dementia with Lewy bodies. Proc. Natl. Acad. Sci. USA 95, 6469 – 6473 Cookson, M. R. (2005) The biochemistry of Parkinson's disease. Annu. Rev. Biochem. 74, 29 –52 The FASEB Journal EL-AGNAF ET AL. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. Martin, F. L., Williamson, S. J., Paleologou, K. E., Allsop, D., and El-Agnaf, O. M. A. (2004) Alpha-synuclein and the pathogenesis of Parkinson's disease. Protein Pept. Lett. 11, 229 –237 Schapira, A. H. V. (1999) Science, medicine, and the future Parkinson's disease. Br. Med. J. 318, 311–314 Lang, A. E., and Lozano, A. M. (1998) Parkinson’s disease—first of two parts. N. Engl. J. Med. 339, 1130 –1143 Lang, A. E., and Lozano, A. M. (1998) Parkinson’s disease— second of two parts. N. Engl. J. Med. 339, 1144 –1153 El-Agnaf, O. M. A., Jakes, R., Curran, M. D., and Wallace, A. (1998) Effects of the mutations Ala30 to Pro and Ala53 to Thr on the physical and morphological properties of ␣-synuclein protein implicated in Parkinson’s disease. FEBS Lett. 440, 67–70 El-Agnaf, O. M. A., Salem, S. A., Paleologou, K. E., Cooper, L. J., Fullwood, N. J., Gibson, M. J., Curran, M. D., Court, J. A., Mann, D. M. A., Ikeda, S. I., et al. (2003) ␣-Synuclein implicated in Parkinson’s disease is present in extracellular biological fluids, including human plasma. FASEB J. 17, 1945–1947 Gibb, W. R., and Lees, A. J. (1988) The relevance of the Lewy body to the pathogenesis of Parkinson's disease. J. Neurol. Neurosurg. Psychiatry 51, 745–752 El-Agnaf, O. M. A., Walsh, D. M., and Allsop, D. (2003) Soluble oligomers for the diagnosis of neurodegenerative diseases. Lancet Neurol. 2, 461– 462 El-Agnaf, O. M. A., Mahil, D. S., Patel, B. P., and Austen, B. A. (2000) Oligomerization and toxicity of -amyloid-42 implicated in Alzheimer's disease. Biochem. Biophys. Res. Commun. 237, 1003–1007 Sharon, R., Bar-Joseph, I., Frosch, M. P., Walsh, D. M., Hamilton, J. A., and Selkoe, D. J. (2003) The formation of highly soluble oligomers of ␣-synuclein is regulated by fatty acids and enhanced in Parkinson's disease. Neuron 37, 583–595 Silverberg, G. D., Mayo, M., Saul, T., Rubenstein, E., and McGuire, D. (2003) Alzheimer’s disease, normal pressure hydrocephalus, and senescent changes in CSF circulatory physiology: a hypothesis. Lancet Neurol. 2, 506 –511 DeMattos, R. B., Bales, K. R., Parsadanian, M., O'Dell, M. A., Foss, E. M., Paul, S. M., and Holtzman, D. M. (2002) Plaqueassociated disruption of CSF and plasma amyloid-beta (A) equilibrium in a mouse model of Alzheimer's disease. J. Neurochem. 81, 229 –236 DeMattos, R. B., Bales, K. R., Cummins, D. J., Paul, S. M., and Holtzman, D. M. (2002) Brain to plasma amyloid-beta efflux: a measure of brain amyloid burden in a mouse model of Alzheimer's disease. Science 295, 2264 –2267 Li, Q. X., Campbell, B. C., McLean, C. A., Thyagarajan, D., Gai, W. P., Kapsa, R. M., Beyreuther, K., Masters, C. L., and Culvenor, J. G. (2002) Platelet ␣- and ␥-synucleins in Parkinson's disease and normal control subjects. J. Alzheimers Dis. 4, 309 –315 Pitschke, M., Prior, R., Haupt, M., and Riesner, D. (1998) Detection of single amyloid beta-protein aggregates in the cerebrospinal fluid of Alzheimer's patients by fluorescence correlation spectroscopy. Nat. Med. 4, 832– 834 Bieschke, J., Giese, A., Schulz-Schaeffer, W., Zerr, I., Poser, S., Eigen, M., and Kretzschmar, H. (2000) Ultrasensitive detection OLIGOMERIC ␣-SYNUCLEIN AS BIOMARKER 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. of pathological prion protein aggregates by dual-color scanning for intensely fluorescent targets. Proc. Natl. Acad. Sci. USA 97, 5468 –5473 Conway, K. A., Lee, S. J., Rochet, J. C., Ding, T. T., Williamson, R. E., and Lansbury, P. T., Jr. (2000) Acceleration of oligomerization, not fibrillization, is a shared property of both alphasynuclein mutations linked to early-onset Parkinson's disease: implications for pathogenesis and therapy. Proc. Natl. Acad. Sci. USA 97, 571–576 Bucciantini, M., Giannoni, E., Chiti, F., Baroni, F., Formigli, L., Zurdo, J., Taddei, N., Ramponi, G., Dobson, C. M., and Stefani, M. (2002) Inherent toxicity of aggregates implies a common mechanism for protein misfolding diseases. Nature (London) 416, 507–511 Walsh, D. M., Klyubin, I., Fadeeva, J. V., Cullen, W. K., Anwyl, R., Wolfe, M. S., Rowan, M. J., and Selkoe, D. J. (2002) Naturally secreted oligomers of amyloid beta protein potently inhibit hippocampal long-term potentiation in vivo. Nature (London) 416, 535–539 El-Agnaf, O. M. A., Nagala, S., Patel, B. P., and Austen, B. M. (2001) Nonfibrillar oligomeric species of the amyloid ABri peptide, implicated in familial British dementia, are more potent at inducing apoptotic cell death than protofibrils or mature fibrils. J. Mol. Biol. 310, 157–168 Masliah, E., Rockenstein, E., Veinbergs, I., Mallory, M., Hashimoto, M., Takeda, A., Sagara, Y., Sisk, A., and Mucke, L. (2000) Dopaminergic loss and inclusion body formation in ␣-synuclein mice: implications for neurodegenerative disorders. Science 287, 1265–1269 Kayed, R., Head, E., Thompson, J. L., McIntire, T. M., Milton, S. C., Cotman, C. W., and Glabe, C. G. (2003) Common structure of soluble amyloid oligomers implies common mechanism of pathogenesis. Science 5618, 486 – 489 Lashuel, H. A., Hartley, D., Petre, B. M., Walz, T., and Lansbury, P. T., Jr. (2002) Neurodegenerative disease: amyloid pores from pathogenic mutations. Nature (London) 418, 291 Miller, D. W., Hague, S. M., Clarimon, J., Baptista, M., GwinnHardy, K., Cookson, M. R. and Singleton, A. B. (2004) Alphasynuclein in blood and brain from familial Parkinson disease with SNCA locus triplication. Neurology 62, 1835–1838 Conway, K. A., Rochet, J. C., Bieganski, R. M., and Lansbury, P. T., Jr. (2001) Kinetic stabilization of the alpha-synuclein protofibril by a dopamine-alpha-synuclein adduct. Science 294, 1346 –1349 El-Agnaf, O. M. A., Paleologou, K. E., Greer, B., Abogrein, A. M., King, J. E., Salem, S. A., Fullwood, N. J., Benson, F. E., Hewitt, R., Ford, K. J., et al. (2004) A strategy for designing inhibitors of ␣-synuclein aggregation and toxicity as a novel treatment for Parkinson's disease and related disorders. FASEB J. 18, 1315– 1317 Received for publication September 1, 2005. Accepted for publication November 10, 2005. 425