African American Physicians and Organized Medicine, 1846-1910
advertisement
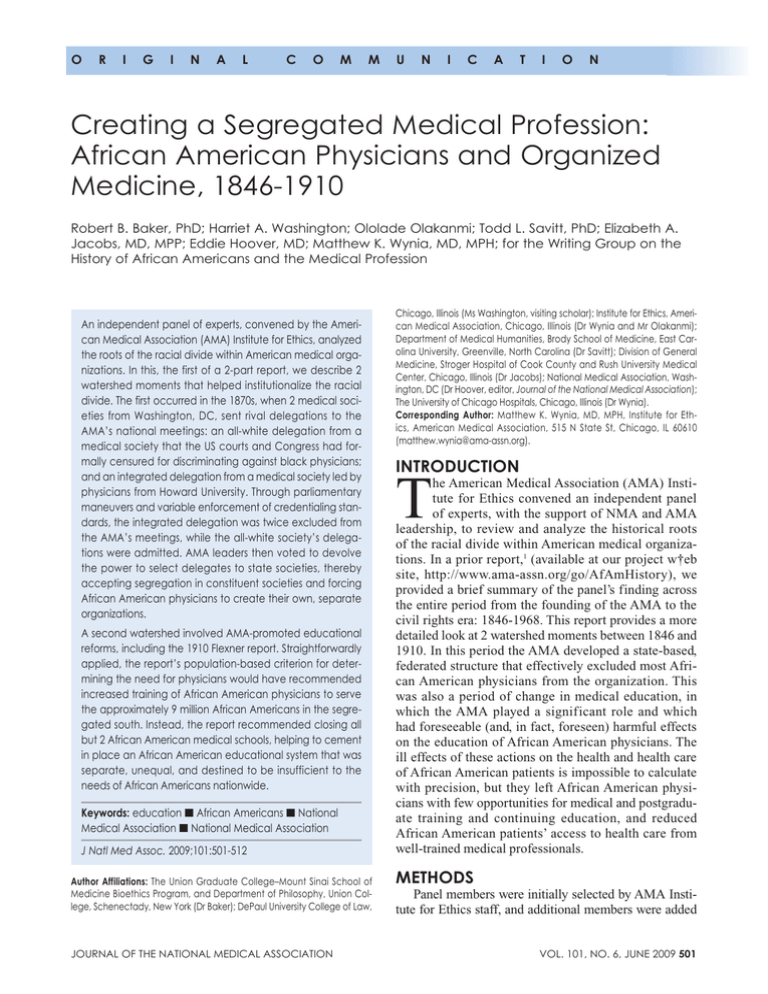
o r i g i n a l c o m m u n i c a t i o n Creating a Segregated Medical Profession: African American Physicians and Organized Medicine, 1846-1910 Robert B. Baker, PhD; Harriet A. Washington; Ololade Olakanmi; Todd L. Savitt, PhD; Elizabeth A. Jacobs, MD, MPP; Eddie Hoover, MD; Matthew K. Wynia, MD, MPH; for the Writing Group on the History of African Americans and the Medical Profession An independent panel of experts, convened by the American Medical Association (AMA) Institute for Ethics, analyzed the roots of the racial divide within American medical organizations. In this, the first of a 2-part report, we describe 2 watershed moments that helped institutionalize the racial divide. The first occurred in the 1870s, when 2 medical societies from Washington, DC, sent rival delegations to the AMA’s national meetings: an all-white delegation from a medical society that the US courts and Congress had formally censured for discriminating against black physicians; and an integrated delegation from a medical society led by physicians from Howard University. Through parliamentary maneuvers and variable enforcement of credentialing standards, the integrated delegation was twice excluded from the AMA’s meetings, while the all-white society’s delegations were admitted. AMA leaders then voted to devolve the power to select delegates to state societies, thereby accepting segregation in constituent societies and forcing African American physicians to create their own, separate organizations. A second watershed involved AMA-promoted educational reforms, including the 1910 Flexner report. Straightforwardly applied, the report’s population-based criterion for determining the need for physicians would have recommended increased training of African American physicians to serve the approximately 9 million African Americans in the segregated south. Instead, the report recommended closing all but 2 African American medical schools, helping to cement in place an African American educational system that was separate, unequal, and destined to be insufficient to the needs of African Americans nationwide. Keywords: education n African Americans n National Medical Association n National Medical Association J Natl Med Assoc. 2009;101:501-512 Author Affiliations: The Union Graduate College–Mount Sinai School of Medicine Bioethics Program, and Department of Philosophy, Union College, Schenectady, New York (Dr Baker); DePaul University College of Law, JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION Chicago, Illinois (Ms Washington, visiting scholar); Institute for Ethics, American Medical Association, Chicago, Illinois (Dr Wynia and Mr Olakanmi); Department of Medical Humanities, Brody School of Medicine, East Carolina University, Greenville, North Carolina (Dr Savitt); Division of General Medicine, Stroger Hospital of Cook County and Rush University Medical Center, Chicago, Illinois (Dr Jacobs); National Medical Association, Washington, DC (Dr Hoover, editor, Journal of the National Medical Association); The University of Chicago Hospitals, Chicago, Illinois (Dr Wynia). Corresponding Author: Matthew K. Wynia, MD, MPH, Institute for Ethics, American Medical Association, 515 N State St, Chicago, IL 60610 (matthew.wynia@ama-assn.org). Introduction T he American Medical Association (AMA) Institute for Ethics convened an independent panel of experts, with the support of NMA and AMA leadership, to review and analyze the historical roots of the racial divide within American medical organizations. In a prior report,1 (available at our project w†eb site, http://www.ama-assn.org/go/AfAmHistory), we provided a brief summary of the panel’s finding across the entire period from the founding of the AMA to the civil rights era: 1846-1968. This report provides a more detailed look at 2 watershed moments between 1846 and 1910. In this period the AMA developed a state-based, federated structure that effectively excluded most African American physicians from the organization. This was also a period of change in medical education, in which the AMA played a significant role and which had foreseeable (and, in fact, foreseen) harmful effects on the education of African American physicians. The ill effects of these actions on the health and health care of African American patients is impossible to calculate with precision, but they left African American physicians with few opportunities for medical and postgraduate training and continuing education, and reduced African American patients’ access to health care from well-trained medical professionals. Methods Panel members were initially selected by AMA Institute for Ethics staff, and additional members were added VOL. 101, NO. 6, JUNE 2009 501 African Americans and Organized Medicine by the panel. The panel was convened with the support of NMA and AMA leadership, and both were asked to provide comments on drafts. However, AMA and NMA leadership were not asked to approve the members of the panel or the contents of manuscripts prior to submission. For source materials, the panel examined primarily AMA, NMA, and newspaper archives, the latter via online databases (http://www.accessible.com, http://bsc. chadwyck.com, and http://www.proquest.com). In addition, we searched Medline using keywords race, segregation integration, and the MesH heading prejudice. A number of books were especially useful and are listed in a bibliography at the project Web site (http://www .ama-assn.org/go/AfAmHistory). Early in its work process, the panel decided to avoid making moral judgments about the intent and motivations of actors in this history. Primary sources about motivation are scant to nonexistent and, insofar as motivations are discernible, they appear mixed or obscured, perhaps even to the actors themselves. The results of decisions, by contrast, are clearer, and so this is where the panel elected to focus its attention. Some broader social historical context is provided both here and in supplemental materials available on the project Web site; however, space constraints and the limits of our project preclude a full explication of the many sociopolitical factors that may have been reflected in the historical episodes we describe. Creating a United Society in a Divided Nation Today, membership in medical societies is largely voluntary, and many physicians choose not to join. But this was not always the case. Between 1846 and 1910, medical societies were the crucibles in which the organized profession of medicine was formed.2 They were where one met and developed relationships with professional colleagues—people one could call upon for a second opinion or to assist in surgery. They were also a forum in which to present papers and learn the latest techniques and treatments. Beyond these direct educational functions, hospital admitting privileges came to be closely linked to medical society membership, along with advanced training opportunities. Moreover, medical society membership was sometimes linked to state licensing and regulatory bodies, and to one’s ability to obtain the bank loans necessary to establish a practice and to purchase newly important scientific equipment, such as stethoscopes and microscopes. In sum, between 1846 and 1910 exclusion from these societies came to mean professional isolation, heightened barriers to adequate training, limitations on professional skills and contacts, and severe constraints on sources of income.2-9 The AMA was conceived as a confederation of US medical societies, colleges, and institutions—the majority being state and local societies—with the avowed pur502 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION poses of creating a “uniform and elevated standard…for the degree of MD;” providing a common code of medical ethics; and promoting the profession’s “interests,” “honor,” “respectability,” “knowledge,” and “usefulness.” 2(xxvi) The idea of a single, unified, national medical society, however, ran against the strong tide of pre–Civil War regional divisions over the question of slavery. In slave states, most African Americans were property,10 and physicians owned African American slaves and/or made a living through the patronage of slaveholding plantations.10-12 Racism was present in the North as well and assumptions about the mental inferiority of African Americans were prevalent in the North and South alike.6(242) African Americans, like James McCune Smith (1813-1865) of New York, were forced to travel abroad for medical education after being rebuffed from American schools on the grounds of race.13 (Smith book) Three African American students (Daniel Liang, Isaac Snowden and Martin Delaney) were initially admitted into Harvard in 1850, but were expelled when a group of 27 white students protested.14 Within medicine, scientific racism, which inculcated the belief that blacks were physiologically different from whites in ways that justified enslavement, was common in the United States and Europe, with many prominent US physicians at its vanguard.3,12,15,16 For example, the AMA’s Committee on Medical Sciences reported in 1850 that, “The Negro brain is nine cubic inches less than the Teutonic [i.e., white].”17 Nevertheless, some physicians directly challenged these theories. For example, Philadelphian John Bell (1796-1872), an ardent abolitionist and chair of the committee that drafted the AMA’s original Code of Medical Ethics in 1847, re-published a synopsis of a remarkable paper by one of the few European proponents of egalitarianism, the “Great Physiologist of Heidelberg” Friedrich Tiedemann, in his Eclectic Journal of Medicine, in which Tiedemann found “no perceptible difference [between] the brain of the Negro and that of the European.”18 Tiedemann had also noted that, after taking account of body size, he had proven, “by measuring the cavity of the skull in Negroes and the men of the Caucasian, Mongolian, American, and Malayan races, that the brain of the Negro is as large as that of the European,” a finding that directly contradicted widely held beliefs of the time. 19 Moreover, some Northern medical schools and medical societies were successful in opening their doors to African Americans. Rush Medical School (Illinois) awarded the first American MD degree to an African American, David Jones Peck (1826/1827-?) in 1847.20 And in 1854, the Massachusetts Medical Society (MMS) accepted into membership John Van Surly DeGrasse (1825-1868), who was probably the first African American member of any state medical society.21 In 1846, when a national conference on medical education closed by recommending the formation of a national medical society, the AMA, to address the issues VOL. 101, NO. 6, JUNE 2009 African Americans and Organized Medicine of medical and pre-medical education on an on-going basis it also mandated that this society have a national code of medical ethics. Written by Bell and Isaac Hayes (1796-1879) and a small committee, this code was adopted by the full AMA at its founding meeting in 1847. The code made no mention of race,2(xxvi-xxvii, 324-34) but espoused ideals of equal treatment on the basis of scientific qualifications alone. It noted that, “A regular medical education furnishes the only presumptive evidence of professional ability and acquirements, and ought to be the only acknowledged right of an individual to the exercise and honours of his profession” and that “no one can be considered as a regular practitioner, or fit associate in consultation, whose practice is based on exclusive dogma, to the rejection of the accumulated experience of the profession, and of the aids furnished by anatomy, physiology, pathology, and organic chemistry.”2(329) The exclusion clause was specifically directed against socalled “irregulars,” like homeopaths, who subscribed to alternative theories of sickness and therapeutics that the AMA members deemed unscientific, and who, at the time, successfully competed with regular practitioners in the medical marketplace. The AMA code and other regulations focused on medical practice and conduct and no mention of race is found in AMA records of the time, therefore it is unknown whether any African American physicians sought to serve as AMA delegates in the organization’s very early years. It is also uncertain whether any African Americans served as delegates to an AMA meeting in this era, though this seems unlikely. Rather, given the way future events unfolded, it seems likely that to have included African Americans would have raised the ire of many physicians who, despite the language of the Code, saw the AMA as both a scientific fraternity and an exclusive social gathering. Unity Through Exclusion Pivotal events that would set the role of African Americans in organized American medicine unfolded at a series of meetings in the 1870s. To appreciate these events, one needs to recognize that this was a period of reconciliation and reform in America, during which the entire nation was searching for union even as it debated the status of newly freed slaves. Presidents Abraham Lincoln (1809-1865) and Andrew Johnson (1808-1875) favored a moderate, conciliatory approach to Reconstruction policy, with the goal of quickly reuniting the country.22 By 1870, every secessionist Southern state had been readmitted to the Union. Yet, they were readmitted to a new nation in which radical Republicans had ratified the 13th, 14th, and 15th Amendments – granting certain civil and political rights to newly emancipated slaves. These rights, however, were immediately sabo- Table 1. American Medical Association Meeting Locations and Presidents in the Years Surrounding the US Civil War Were Balanced Between Northern and Southern Statesa Year Preliminary convention 1846 1847 1848 1849 1850 1851 1852 1853 1854 1855 1856 1857 1858 1859 1860 1861 1862 1863 1864 1865 1866 1867 1868 1869 1870 a Meeting Location NY PA MD MA OH SC VA NY MO PA MI TN DC KY CT Meeting deferred due to Civil War Meeting deferred due to Civil War IL NY MA MD OH DC LA DC AMA President (State) J. Knight (CT) N. Chapman (PA) A.H. Stevens (NY) J.C. Warren (MA) R.D. Mussey (OH) J. Moultrie (SC) B.R. Wellford (VA) J. Knight (CT) C.A. Pope (MO) G.B. Wood (PA) Z. Pitcher (MI) P.F. Eve (TN) H. Lindsly (DC) H. Miller (KY) E. Ives (CT) A. March (NY) N.S. Davis (IL) N.S. Davis (IL) D.H. Storer (MA) H.F. Askew (DE) S.D. Gross (PA) W.O.Baldwin (AL) G. Mendenhall (OH) Southern states: those with a history of slave holding and trading through the time of the Civil War are bold. JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION VOL. 101, NO. 6, JUNE 2009 503 African Americans and Organized Medicine taged by repressive legislation. As early as November 1865 punitive Black Codes were being passed in southern states, restricting African Americans’ activity and movements, often requiring them to remain on plantations, sometimes even as indentured servants.22(199-201),23 These codes, in turn, raised the ire of many northern abolitionists, who thought (correctly) that they were an attempt to maintain a society that was “as near to slavery as possible.”22(199) The AMA, meanwhile, carefully maintained a pattern of North-South balance in locating national meetings and electing presidents both before and after the Civil War—presumably in an attempt to maintain professional unity despite rising regional tensions (Table 1). Following the war, as early as 1868 the AMA meeting included delegations from six Southern states24; and by 1869, the annual meeting was held in New Orleans with William Baldwin (1818-1886) of Alabama as president. “Eight years ago we were separated by civil war … [that] engendered the bitterest feeling in every other national organization,” Baldwin observed. “[I]t has been left to the [AMA] to teach … charity and forgiveness.” 25(pp56-60), a The AMA’s plan to maintain professional unity was soon tested, however, when three black physicians— Alexander Thomas Augusta (1825-1890), Charles Burleigh Purvis (1842-1929), and Alpheus W. Tucker (unknown dates)—sought recognition as delegates from the District of Columbia’s new, racially-integrated National Medical Society of the District of Columbia (NMS; not to be confused with the NMA, founded in 1895) at the AMA’s 1870 meeting in Washington, DC (Figure 1).26,27 The NMS had been formed in reaction to racial exclusion on the part of the Medical Society of the District of Columbia (MSDC).27 After their initial exclu- sion, these African American physicians appealed to congress, which had direct authority over the District of Columbia, for redress. In 1869 a congressional investigation found that the MSDC had indeed refused to admit these same three, otherwise-qualified black physicians, “solely on account of color.”29(p2550) However, congress provided no remedy, so these physicians founded an integrated society: the NMS. Since at this time the AMA was a confederation of municipal, county, and state medical societies, medical hospitals, and other medical institutions, any medical institution of “regular” physicians that abided by the AMA Code of Ethics could send delegates to the national AMA meeting. When the AMA held its 25th meeting in Washington DC in 1870, both the NMS and the MSDC sent delegates —the all-white MSDC urged massive attendance by white physicians in an attempt to stack a potential vote against admission of the integrated NMS delegation.28 Both the MSDC and the NMS filed ethics complaints against each other. The MSDC challenged the inclusion of the NMS delegation, which comprised not only the 3 black physicians but a number of sympathetic white physicians as well,291 on the grounds that the NMS “was formed in contempt of,” and “[had] attempted, through legislative influence, to break down,” the MSDC.26(p173-174) In other words, the MSDC opposed the NMS because NMS members had petitioned Congress to address racial discrimination within the MSDC. The NMS, in turn, charged the MSDC with licensing “irregular” practitioners. Quite independently, dissident members of another society, the Massachusetts Medical Society had also charged their own society with accepting “irregulars,” specifically homeopaths, into membership. 30(pp26,53-54),31 Figure 1. Alexander T. Augusta (1825-1890) and Charles B. Purvis (1842-1929) Three African American physicians were denied entrance into the Medical Society of the District of Columbia in 1869 and the annual convention of the American Medical Association in 1870: Alexander Thomas Augusta (left), Charles Burleigh Purvis (right), and Alpheus W. Tucker (not pictured). In: Alexander T. Augusta. Arlington National Cemetery Web site. http://www.arlingtoncemetery.net/ataugust. htm. Accessed January 28, 2008.; and Morais H. The History of the Negro in Medicine. 1st ed. New York, NY: Association for the Study of Negro Life and History and Publishers Co Inc; 1967:52. a See also, Blight, D. Race and Reunion: The Civil War in American Memory. Cambridge MA: Belknap Press of Harvard University; 2002. 504 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION VOL. 101, NO. 6, JUNE 2009 African Americans and Organized Medicine Homeopaths, as noted earlier, were characterized by the AMA Code of Ethics as practicing “an exclusive dogma to the rejection of the accumulated experience of the profession” and their exclusion was considered a defining issue for the AMA.9(114-115),19(99-100),32(174) Since all of these cases involved allegations that a society had violated the Code of Ethics, all three were referred to the AMA’s Committee on Ethics. Following protracted deliberation – lasting almost the entire duration of one meeting, possibly stalling to avoid making a controversial decision until just before the meeting adjourned26 – the Committee found that the charge that the MSDC granted licenses to irregulars was “not of a nature to require the action of the [AMA]” because it was a matter for Congress to address, and recommended inclusion of the MSDC’s all-white delegation.30(p54) The Committee also urged recognition of the delegates from Massachusetts, even though the charge that their society accepted irregulars as members was “fully proved” and “plainly in violation of the Code of Ethics”30(p29) — observing that the charges should have been first lodged locally. Therefore, the Massachusetts society was instructed to expel any irregulars from membership before the next AMA meeting, which they did.31 With respect to the integrated NMS, however, the Committee was divided, 2 to 3. Two of the AMA’s founders led the ensuing debate: AMA vice-president Alfred Stillé (1813-1900), speaking for the Committee’s minority, recommended recognition of the NMS delegation.30(pp5556) Nathan Smith Davis (1817-1904), whom the AMA had twice elected as its president during the Civil War (Table 1) and would later laud as its “father,”29(p603),33 spoke for the Committee’s majority and urged exclusion of all NMS members, including all of the white members who supported the integrated society30(pp53-55) When the issue was put to a roll call vote (in which the 36 delegates from the MSDC, but no NMS members, were allowed to vote), the minority report was tabled (114 to 82) and the majority report adopted. As a result, the integrated NMS delegation was excluded. 30(pp56-58) Following the vote, a written clarification of the Davis committee’s recommendations was requested. The next day, before Davis’ clarification was presented, two Massachusetts delegates who had supported the inclusion of the NMS delegates, the anti-abortionist Horatio R. Storer (1830-1922) and colleague John L. Sullivan (sometimes referred to as O’Sullivan, unknown dates) expressly raised the issue of race. Sullivan proposed that the AMA adopt the policy that “no distinction of race or color shall exclude from the Association persons claiming admission and duly accredited thereto.”30(p65) According to the New York Times this proposal was submitted amid, a storm of hisses, which compelled him [Sullivan] to stop. Cries of ‘Go on; go on!’ were heard, and he said he would do so when the serpents became JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION quiet. He then finished reading [the proposal], and was allowed to speak five minutes.34 But AMA vice-president Lewis A. Sayre (18201900) of New York proposed – and the delegates voted to approve – that action on Sullivan’s proposal be postponed so that Davis could present the written report clarifying the Committee’s reasoning for not admitting delegates from the NMS. Davis’ clarification stated that “if the medical department of Howard University had chosen to send any delegates who are not members of [the NMS] there is nothing whatever in [this] report to prevent them from being received [as delegates].” As to the NMS and its members, they were in violation of various by-laws of the MSDC, and, they had used unfair and dishonorable means to procure the destruction of the [MSDC] by inducing congress to abrogate their charter. Each and all of these charges were…fully proved. Therefore if we have any regard for the laws of the land, or the ethics of our medical organizations, the undersigned could not come to any other conclusion.30(pp65-66) Sullivan’s proposal that no distinction of race or color shall exclude someone from the AMA was then voted upon. It lost by a vote of 106 to 60. Storer then proposed what can only be seen as an effort to save face: a resolution stating that Davis, having distinctly stated and proved that the consideration of race and color has had nothing whatsoever to do with the decision of the question of the Washington delegates, and inasmuch as charges have been made in open session to-day attaching the stigma of dishonor to parties implicated…therefore the report of the majority of the Committee on Ethics be declared, as to all intents and purposes, unanimously adopted. According to the minutes, however, Davis never mentioned race or color. He merely stated that nothing in the report excluded the faculty of the Howard medical department (many of whom were white). One southern medical journal, in an editorial favoring exclusion of the NMS, called this resolution “a kind of placebo—an effort to pore [sic] oil on troubled waters, even at the hazard of strict interpretation of truth.”28(p201) In any event, Storer’s motion passed, 112 to 34.30(pp66-67) The AMA thus excluded an integrated medical society through selective enforcement of membership standards. At the same meeting it allowed leniency to 2 allwhite delegations that had clearly breached scientific credentialing standards specified in its code of ethics by admitting “irregulars” and then stringently applied stanVOL. 101, NO. 6, JUNE 2009 505 African Americans and Organized Medicine dards of collegial behavior to a delegation with black members—and, immediately thereafter, declined to adopt a policy of nondiscrimination, and finished the meeting by officially absolving itself of the charge of racism. The AMA’s decision to provide itself instant absolution is evidence of, if not guilt, at least recognition that the decision had the effect of racial discrimination, which some physicians found condemnable. Indeed, an unnamed white commentator, reflecting on the decision, wrote in 1870: “I doubt whether, in the last 50 years, a national scientific body has convened anywhere that would have excluded a competent scientist on the ground of color.”26(p178) He noted further that it was contrary to the “ethics” and “avowed purpose” of the AMA “to propose tests for membership totally irrelevant to capacity or character.”26(pp172,176) But, despite this, the AMA had put up “new barriers to entrance”26(p177) and, in doing so, “unharnessed itself from its code of ethics.”2(p180) And “the profession as well as the laity know…[that the AMA’s action] was aimed at the exclusion of the colored physician,” yet it had to be “made to appear that they were not excluded on the ground of color…[because the act was] somewhat monstrous, and would need plausible excuse before others.”26(pp172,175) (The entire text of this remarkable 1870 commentary is available at our project Web site.) Despite Davis’ public statement that nothing whatsoever in the 1870 report of the Committee on Ethics would prevent members of the Howard faculty from being “received” as AMA delegates, when members of the Howard faculty applied to be received as delegates in 1872, Davis argued that the Howard faculty members could not be received “on account of want of good standing on the part of those institutions, as indicated by the action of this Association at its annual meetings in 1870.”35(p53) Davis further alleged that Howard faculty should be excluded because the institution admitted women to its faculty and because it allowed members to practice without a license from the MSDC (which still refused to admit or license black physicians). Davis strove to appear impartial in adducing “evidence” favoring exclusion, but at one point he misrepresented an 1871 vote of 83 to 26 to postpone discussion when the hour grew late as a lopsided vote against admitting institutions with women. In fact, the 1871 vote to exclude institutions admitting women was quite close: 45 against admission vs 41 in favor.36 Dr Robert Reyburn (1833-1909) rose to defend the Howard delegation in 1872. He observed that the MSDC’s licensing practices had been struck down “by the local courts [as discriminatory]; and being considered unconstitutional, could not be enforced.” 35(p55) Reyburn admitted that “Howard University…received all who applied for medical education, without distinction of color or of sex….[in the belief that] every human being should be allowed the right to the highest developb ment that God has made him capable of.”35(p55) Dr Samuel C. Busey (1828-1901) of the MSDC responded. Acknowledging the truth of Reyburn’s claims, Busey proclaimed that the MSDC “had not attempted to maintain its [licensing] authority through the local courts” after a judge had declared its procedures unconstitutional, because The members of the profession in the District of Columbia, standing upon its honor and dignity appeal neither to the courts nor legislative bodies, but to their peers—to this body, which was the only competent arbiter and tribunal to determine questions of medical honor, or ethics, and professional decorum.35(p55)b After this exchange, the AMA members voted to accept Davis’ report, including the recommendation to exclude the Howard faculty delegates, “by a very large majority.”35(p59) As we noted in the methodology section, the focus of this paper is on the effects of actions, not the intentions of actors. Nonetheless, one can summarize that Davis reneged on his public statement not to use the 1870 report against future Howard delegations and misrepresented a prior decision in seeking evidence to support exclusion. For its part, the assembled AMA more than once voted to seat the all-white MSDC but not the integrated NMS or Howard delegations, even though a court had found the MSDC’s licensure practices discriminatory and unconstitutional and the organization had licensed irregular practitioners. Finally, the minutes of the 1872 meeting also state that the ultimate grounds given for denying admission to the integrated Howard delegation in 1872 was that the school admitted women students and faculty—a curious linkage of race and gender. In the end, although the AMA never adopted Jim Crow–like regulations formally excluding women or blacks from attending national meetings, after repeated attempts of integrated delegations and those from institutions admitting women to be recognized at AMA national meetings between 1870-1872, the racial and gender composition of the AMA remained unchanged— uniformly white and male—and the AMA’s national scientific and social meeting was, in consequence, an exclusive white man’s club. Leaving Racial Segregation to the States In 1873, Davis offered a proposal to put an end to seemingly interminable squabbles over seating delegations: delegations would henceforth be restricted to state and local medical societies—and state societies, not the national AMA convention, would determine which local societies should be officially recognized by the AMA.37 Minutes House Delegates 25th Annual meeting AMA, 1872, p. 55 506 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION VOL. 101, NO. 6, JUNE 2009 African Americans and Organized Medicine Davis’ proposal, adopted in 187438, conceivably had various motivations but, regardless of intent, it was a dramatic shift of power to the state societies, functionally transforming the AMA into a state society-based federation. The effects of this transformation were clear: because many AMA-affiliated medical societies, and all of those in the south, where the vast majority of blacks lived, openly practiced racial exclusion, the AMA’s new structure effectively excluded most black physicians from the AMA. In the late 1800s, an increasing number of northern societies elected to admit women, which ushered some into AMA membership. In 1876, the Illinois delegation to the national AMA convention included Sarah Hackett Stevenson (1841-1909), the AMA’s first woman member.39(p16) She was admitted into the AMA’s national meeting by that year’s president, James Marion Sims (1813-1883), with the statement that if any woman [in] the medical profession makes such a reputation…as to be sent as a delegate… we are bound to receive her. And if any colored man should rise to the dignity of representing a [society] we must receive him as such.39(p93) Note again the curious link between admitting a member of another gender and admitting a member of another race. Note further that the statement implies that there had been no black AMA delegates prior to 1876. Before 1888 the AMA was a confederacy, and thus there were no individual members of the AMA as such, only delegates to the national AMA convention and members of organizations that belonged to the AMA. A change in the bylaws in 1888 made all members of constituent state societies “de facto permanent [AMA] members.”40(pp477-478),41 Since some northern state societies had African American members at the time, the AMA probably gained its first African American members in 1888. racial exclusiveness”51 and included white members. The AMA similarly “boasted itself as exclusive only of the false in science and character”26 and, after 1888, had a few northern black members. Among the NMA’s founders was at least 1 African American AMA member, Daniel Hale Williams (1856-1931, Figure 2), an 1883 graduate of the Chicago Medical College (now Northwestern University).49,52-54 But formal exclusionary policies at the national level were not needed to maintain near-total segregation, given the role of the state and local societies. In actuality, the segregation of organized medicine at the turn of the century was nearly complete—the AMA was almost entirely white; the NMA, mostly black. Segregated and Unequal Education The AMA was conceived as an organization to reform American medical education. At its founding meeting in 1846, the AMA had established a Committee on Medical Education (renamed the Council on Medical Education, CME, in 1904). The CME reported annually to the AMA national convention,55 and the policies and initiatives it recommended would significantly impact African Americans’ access to medical education. Only a handful of African Americans graduated from northern medical schools during the antebellum period. Others, rebuffed by US schools, earned MDs abroad. Among these early African American physicians were James McCune Smith (1813-1865), perhaps the first African American to earn an MD and practice in the United States, who graduated from the University of Glasgow in 1832,13 and Alexander Augusta, who was the first African American to serve as a surgeon in the Union Army (and one of the NMS members rejected from serving as an AMA delegate in 1870), who earned an MD from Trinity Medical College in Toronto in 1856.56 Figure 2. Daniel Hale Williams (1856-1931) African American Physician Organizations In the south, African American physicians responded to their exclusion from AMA-affiliated medical societies by founding their own local and state societies. The Medico-Chirurgical Society of the District of Columbia was founded in 1884;42-45 the Lone Star State Medical, Dental, and Pharmaceutical Association of Texas in 1886;46 the Old North State Medical Society of North Carolina in 1887;47 and the North Jersey National Medical Association in 1895.48 None of these societies could send delegations to AMA meetings. In 1895, feeling the need for a national organization to support black physicians, leading African American physicians formed the NMA.3(pp392, 400-402),45,49,50 Notably, neither the NMA nor the AMA has ever had any explicit, race-based membership criteria at the national level. The NMA was “conceived in no spirit of JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION A renowned surgeon, Williams was the first African American member of the American College of Surgeons, 1913. He cofounded the NMA in 1895 and served as its first vice president. AMA records indicate that Williams was an AMA member as early as 1906.49 VOL. 101, NO. 6, JUNE 2009 507 African Americans and Organized Medicine Following the war, southern medical schools continued to refuse black students. The few northern schools that accepted African Americans generally did so in ones and twos.6(pp302-321),45 In reaction, some of the missionary groups that founded colleges in the Reconstruction South (schools that today are called historically black colleges and universities) also established medical schools. For example, Meharry Medical College (Tennessee) was founded in 1876 and Leonard Medical School (North Carolina) was founded in 1882.57(p1416) Howard University was founded by a group of citizens and an act of Congress, and its medical school opened in 1868 (Figure 3).58-60 Starting in the late 1880s, a few black physicians established independent medical schools as well. These schools were small and struggling (Table 2). By 1890, 25 years after the Civil War ended, there were only 909 black physicians in the entire United States, although the census recorded nearly 7.5 million African Americans.61 By 1907, the CME tracked state medical board licensure failure rates by medical school and had established a grading system to assess school quality. African American schools (8 existed in 1907) fared badly. Their licensure failure rates were over 20% and the AMA rating system routinely placed them in the bottom third of the 135 US medical schools examined.57 Moreover, since all the African American schools lacked financial resources, rising educational standards and increasing pressure for reform created a crisis for these schools. The crisis deepened after the CME asked the Carnegie Foundation for the Advancement of Teaching to sponsor an on-site survey of all American and Canadian medical schools in 1908. The foundation commissioned Abraham Flexner (1866-1955), an educator from Kentucky, to head the study. Flexner was charged with reviewing every medical school in North America. He visited each school, usually accompanied by the secretary of the CME.55(pp10-11) Flexner’s 1910 report to the foundation, Medical Education in the United States and Canada,62 commonly known as the “Flexner report,” is often credited with reforming American medical education.63 In truth, it was part of an ongoing and complicated evolution, but the report’s finding were especially effective—and scathing.63-65 Approximately 90% of all schools had inadequate admissions standards (for example, only 16 medical schools required a bachelor’s degree from their applicants), most medical schools lacked trained faculty, their curricular offerings were inadequate, and they failed to provide adequate laboratories and clinical experience in hospitals. The report’s recommendations for the reform of American medical education were predicated on a basic finding of enormous over-production of uneducated and ill trained medical practitioners…in absolute disregard of the public welfare.…Taking the United States as a whole, physicians are four or five times [more] numerous in proportion to the population [than needed].”62(x) Assessing the need for medical schools in a given state in terms of the number of physicians required to serve that state’s population, Flexner recommended closing weak schools so that resources could be focused on stronger schools. Flexner abandoned his population-based standard, however, when assessing the need for African American medical schools to serve the 9.8 million African Americans living in the United States in 1910.66 Given segregation, a population-based assessment would have supported a substantial increase in the number of African Figure 3. Few Medical Schools Open to African American Students First class of Leonard Medical School at Shaw University, Raleigh, North Carolina circa 1886 (left). The Howard University medical faculty, Washington, DC, 1869-1870 (right). Left to right: Alexander T. Augusta, Silas L. Loomis (Dean), Gideon S. Palmer, Major General Oliver O. Howard (President), Robert Reyburn, Joseph Taber Johnson (secretary), Charles B. Purvis, and Phineas H. Strong.40(p42) In: Virtual Museum of African American Medical History in North Carolina. Old North State Medical Society Web site. http://www. oldnorthstatemedicalsociety.org/virtualMuseum/Main%20-%20ONSMS%20Virtual%20Museum.html. Accessed January 28, 2008. 508 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION VOL. 101, NO. 6, JUNE 2009 African Americans and Organized Medicine American physicians. To accomplish this, Flexner could have recommended several strategies: integrating African Americans into white medical schools (as he recommended the coeducation of women physicians), creating segregated branches at high-quality white schools, providing resources to improve poor-performing African American schools, or increasing enrollment at existing high-quality African American schools. Flexner recommended none of these. Instead, arguing that African Americans needed “good schools rather than many schools,” he recommended the closure of all but 2 of the 7 African American medical schools operating in 1910— Howard and Meharry—without recommending any mechanism to increase the total output of black physicians. Flexner, thereby, left black patients in the segregated south—where, at the time, more than 90% of the black population resided67—with even fewer sources of African American physicians. Flexner seemed to appreciate that he was applying a double standard in assessing the need for African American physicians. He addressed the issue by observing that, while the “practice of the negro doctor will be limited to his own race,” the “medical care of the negro race will never be wholly left to negro physicians.”62(p180) Flexner, thus, suggested that the medical care of African Americans would, ultimately, be entrusted to white physicians. But by parity of reasoning—and as was true under segregation—it follows that white physicians in the Jim Crow south would primarily serve their people, leaving black populations medically underserved, caught in a racially segregated system that was both separate and destined to remain unequal under Flexner’s recommendations. Further cementing the unequal status of African American medical education, Flexner recommended that “negro doctors” be educated not as surgeons or other specialists but primarily as “sanitarians,” to “humbly and devotedly” teach hygienic principles to “their people.”62(p180) The Flexner report was initiated at the request of the AMA and was meant to buttress the work of the CME.55(pp10,5859),68-72 The AMA embraced Flexner’s recommendations wholeheartedly and in annual evaluations of medical schools in the Journal of the American Medical Association, the CME kept up the pressure for reform. By 1923, 51 of the 131 (40%) US medical colleges operating in 1910 had closed. Amongst these were 5 of the 7 (71%) African American medical colleges; only Howard and Meharry remained open (Table 2). Both struggled for survival.57,72 In the decade following the report, the General Education Board (GEB)—the Rockefeller family’s philanthropic foundation—and the Carnegie Foundation, both advised by Flexner, donated large sums of money to establish new medical schools and to reform existing schools. Flexner did not, however, immediately recommend adequate increases in funding for Howard and Meharry to help them meet the new education standards.57 Meanwhile, the CME continued to give Howard and Meharry low ratings each year, keeping them in constant jeopardy. Toward the end of the decade Flexner became an important supporter of Meharry in particular and, after funding white schools first, the Carnegie Foundation and GEB eventually provided substantial funding to Meharry.57 Table 2. Black Medical Colleges, 1868-1923 Year Year Opened Discontinued Name City Howard University Medical Dept Lincoln University Medical Dept Straight University Medical Dept Washington, DC 1868 Oxford, PA 1870 New Orleans 1873 ---1874 1874 Meharry Medical College Leonard Medical School of Shaw University Louisville National Medical College Flint Medical College of New Orleans University Hannibal Medical College Knoxville College Medical Dept Chattanooga National Medical College State University Medical Dept Nashville Raleigh 1876 1882 ---1918 None Presbyterian (local) American Missionary Association Methodist Episcopal Baptist Louisville New Orleans 1888 1889 1912 1911 Independent Methodist Episcopal Memphis Knoxville Chattanooga Louisville 1889 1895 1899 1899 Knoxville Medical College University of West Tennessee College of Medicine & Surgery Medico-Chirurgical & Theological College of Christ’s Inst. Knoxville Jackson Memphis Baltimore 1900 1900 1907 1900 1896 1900 1904 1903 merged with LNMC 1910 1907 1923 1908? Independent Presbyterian Independent Colored Baptist (Kentucky) Independent Independent JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION Religious Affiliation Independent VOL. 101, NO. 6, JUNE 2009 509 African Americans and Organized Medicine Discussion In the United States, organized medicine emerged from a society deeply divided over slavery, but largely accepting of racial inequities. Throughout this period, racism was pervasive, and pseudoscientific theories of racial inferiority were common. Hospitals, training programs, and many medical and nonmedical organizations, in addition to the AMA, accepted or enforced racial segregation. Yet, one might have expected the AMA to lead the way in integration, since its code of ethics and formal membership policies specifically valorized only science, education, and character and made no mention of race. Indeed, when AMA actions effectively broke from this ideal—in refusing to admit the NMS delegation in 1870—it felt the need to claim it was doing so for nonracial reasons, the decision was contentious, and it was criticized for turning on its own code of ethics. Instead of standing for its stated ideals, however, the AMA adopted policies that countenanced medical segregation and racism. As AMA President Baldwin observed in 1869, the AMA had, indeed, taught postwar “charity and forgiveness,” but reconciliation was on white southern terms—on the terms offered by the MSDC, which was practicing discrimination that courts had ruled unconstitutional—and came at the expense of the civil rights of blacks. Moreover, early in Reconstruction, more than 20 years before the Plessy v Ferguson US Supreme Court case endorsed legalized segregation,73 the AMA modeled a states’ rights solution to maintaining national professional unity by allowing outright professional segregation and racial exclusion at the state and local level. Then, in pursuing a quality improvement agenda that promoted the closure of most African American medical schools, the AMA effectively helped to deprive many African American patients of access to well-trained African American physicians. For the medical profession, as for the nation as a whole, this postwar path to reconciliation ultimately created a false unity, a partial unity that included only white physicians. Professional unity based on allowing racial exclusion would prove to be unteneble, yet profoundly damaging, in the decades to come. Acknowledgments The authors are indebted to the following individuals for their support of this project: John C. Nelson, MD, MPH, past president, AMA; Sandra L. Gadson, MD, past president, NMA; Ronald M. Davis, MD, past president, AMA; Phyllis R. Kopriva, director, Special Groups, AMA; and Arthur B. Elster, MD, former director, Medicine and Public Health, AMA. We also extend our thanks to Laura L. Carroll, MA, MLIS, archivist, Emory University, and former archivist, AMA; and Andrea Bainbridge, archivist, AMA, for their assistance in locating primary source data and other records at the AMA. 510 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION For their helpful comments on previous drafts of this paper, the Writing Group thanks John S. Haller Jr, PhD, vice president for academic affairs, Southern Illinois University, Carbondale; Douglas M. Haynes, PhD, associate professor of history, University of California, Irvine; Darlene Clark Hine, PhD, board of trustees professor of African American studies, and professor of history, Northwestern University; Kenneth M. Ludmerer, MD, professor of medicine, Washington University; Katya Gibel Mevorach, PhD, associate professor of anthropology and American studies, Grinnell College; Susan M. Reverby, PhD, MA, Marion Butler McLean Professor of Women’s Studies, Wellesley College; David Barton Smith, PhD, research professor, Center for Health Equality and Department of Health Management and Policy, Drexel University School of Public Health, and professor emeritus, Department of Risk, Insurance, and Health Care Management, Fox School of Business, Temple University; and Karen Kruse Thomas, PhD, associate director, Reichelt Oral History Program, Florida State University, and adjunct assistant professor of History, University of Florida. The Writing Group on the History of African Americans and the Medical Profession includes Robert Baker, PhD, The Union Graduate College-Mount Sinai School of Medicine Bioethics Program, and Department of Philosophy, Union College; Janice Blanchard, MD, George Washington University School of Medicine, Department of Emergency Medicine; L. Ebony Boulware, MD, MPH, Johns Hopkins Medical Institutions, Welch Center for Prevention, Epidemiology, and Clinical Research; Clarence Braddock, MD, MPH, Stanford Center for Biomedical Ethics; Giselle Corbie-Smith, MD, MSc, Department of Social Medicine, University of North Carolina at Chapel Hill; LaVera Crawley, MD MPH, Stanford University Center for Biomedical Ethics; Eddie Hoover, MD, editor, Journal of the National Medical Association; Elizabeth Jacobs, MD, MPP, Cook County Hospital & Rush Medical College; Thomas A. LaVeist, PhD, Johns Hopkins Bloomberg School of Public Health, Department of Health Policy and Management; Randall Maxey, MD, PhD, past president, NMA; Charles Mills, PhD, University of Illinois at Chicago; Kathryn L. Moseley, MD, University of Michigan Medical School; Todd L. Savitt, PhD, Department of Medical Humanities, Brody School of Medicine, East Carolina University; Harriet A. Washington, visiting scholar, DePaul University College of Law; David R. Williams, PhD, Institute for Social Research, University of Michigan. References 1. Baker RB, Washington HA, Olakanmi O, et al. African American physicians and organized medicine, 1846-1968: Origins of a racial divide. JAMA. 2008; 300(3):306-314. 2. Baker R, Caplan A, Emanuel L, Latham S, eds. The American Medical Ethics Revolution: How the AMA’s Code of Ethics Has Transformed Physicians’ Relationships to Patients, Professionals, and Society. Baltimore, MD: The Johns Hopkins University Press; 1999. VOL. 101, NO. 6, JUNE 2009 African Americans and Organized Medicine 3. Hyde DR, Wolff P, Gross A, Hoffman EL. The American Medical Association: power, purpose, and politics in organized medicine. Yale Law J. 1954;63(7):937-1022. 4. Garceau O. The Political Life of the American Medical Association. Cambridge, MA: Harvard University Press; 1941. 5. Starr P. The Social Transformation of American Medicine. New York, NY: Basic Books Inc; 1982. 6. Byrd WM, Clayton LA. An American Health Dilemma: A medical history of African Americans and the problem of race; beginnings to 1900. New York, NY: Routledge; 2000. 7. Kessel RA. Price discrimination in medicine. J Law Econ. 1958;1(1):20-53. 8. Shryock RH. Medical Licensing in America, 1650-1965. Baltimore, MD: The Johns Hopkins Press; 1967. 9. Fishbein M. The American Medical Association, 1847 to 1947. Philadelphia, PA: WB Saunders; 1947. 10. Savitt T. Medicine and Slavery: The Diseases and Health Care of Blacks in Antebellum Virginia. Urbana: University of Illinois Press; 1978. 11. Washington HA. Medical Apartheid: The dark history of medical experimentation on black Americans from Colonial time to the present. New York: Doubleday; 2006. 12. Fisher W. Physicians and slavery in the antebellum Southern Medical Journal. J Hist Medicine Allied Sci. 1968;23(1):36-49 (??145–152). 13. Smith JM. The Writings of James McCune Smith: Black Intellectual and Abolitionist. Stauffer J, ed. New York, NY: Oxford University Press; 2006. 14. Nercessian N. Against all Odds. Cambridge, MA: Harvard University Press. 15. Dain B. A Hideous Monster of the Mind: American Race Theory in the Early Republic. Cambridge, MA: Harvard University Press; 2002. 16. Stanton W. The Leopard’s Spots: Scientific Attitudes Toward Race in America, 1815-1859. Chicago, IL: The University of Chicago Press; 1960. 17. The transactions of the American Medical Association; May 7-10, 1850; p57. Cincinnati, OH. http://www.nmt.com/ama_ndls. Accessed January 28, 2008. 18. Tiedemann F. On the brain of the Negro, compared with that of the European and the orangutan by Fredrick Tiedmann, MD [read before the Royal Society].In: Bell J, ed. The Eclectic J Med. Vol 1. Philadelphia, PA. Haswell, Barrington and Haswell; 1837:301. 19. Gould SJ. The great physiologist of Heidelberg. Natural History. July 1999. Available at: http://findarticles.com/p/articles/mi_m1134/is_6_108/ ai_55127879. Accessed September 26, 2008. 20. David Jones Peck, MD. Rush University Medical Center Archives Web site. http://www.lib.rush.edu/archives/DJP_pathfinders.html. Accessed September 26, 2008. 21. DeGrasse-Howard papers: 1776-1976. The Massachusetts Historical Society Web site. http://www.masshist.org/findingaids/doc.cfm?fa=fa015 3#bioghistfa0153. Accessed September 25, 2008. 22. Foner E. Reconstruction: America’s Unfinished Revolution, 1863-1877. 1st Perennial Classics ed. New York, NY: HarperCollins Publishers; 2002. 23. Mississippi Black Codes. Passed in November 1865. Available at: http://chnm. gmu.edu/courses/122/recon/code.html. Accessed September 29, 2008. 24. The transactions of the American Medical Association; May 5-8, 1868; Washington, DC. http://www.nmt.com/ama_ndls. Accessed January 28, 2008. 25. The transactions of the American Medical Association; May 4-7, 1869; New Orleans, LA. http://www.nmt.com/ama_ndls. Accessed January 28, 2008. 26. Unnknown author. Nat Med J. 1870/1871;1:168-180. 27. Nickens HW. A case of professional exclusion in 1870: the formation of the first black medical society. JAMA. 1985;253(17):2549-2552. 28. Haynes DM. A Question of Taste: The racial and sexual politics in the making of the American Medical Association, 1847-1900 (unpublished manuscript). 29. Reyburn RR, Stephenson JG, Augusta AT, et al. A plea for racial equality. The New Era (Washington). January 27, 1870. In: Morais H. The History of the Negro in Medicine. 1st ed. New York, NY: Association for the Study of Negro Life and History and Publishers Co Inc; 1967:215-216. 30. The transactions of the American Medical Association; May 3-6, 1870; Washington, DC. http://www.nmt.com/ama_ndls. Accessed January 28, 2008. JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION 31. Burrage WL. A History of the Massachusetts Medical Society with Brief Biographies of the Founders and Chief Officers, 1781-1922. Boston, MA: Massachusetts Medical Society; 1923:129. 32. Haynes D. Policing the social boundaries of the American Medical Association, 1847-70. J Hist Med Allied Sci. 2005;60(2):170-195. 33. AMA’s founder. American Medical Association Web site. http://www. ama-assn.org/ama/pub/category/print/12981.html. Updated September 4, 2007. Accessed January 28, 2008. 34. The Doctors. The question of color. NY Times. May 7, 1870. Available at: http://query.nytimes.com/gst/abstract.html?res=9F00E5D9153BE63BBC4F5 3DFB366838B669FDE. Accessed September 29, 2008. 35. The transactions of the American Medical Association; May 7-10, 1872; Philadelphia, PA. http://www.nmt.com/ama_ndls. Accessed January 28, 2008. 36. The transactions of the American Medical Association; DATES, 1871 (p.41); San Franscisco, CA. http://www.nmt.com/ama_ndls. Accessed January 27, 2009. 37. The transactions of the American Medical Association; May 6-9, 1873; St. Louis, MO:44. http://www.nmt.com/ama_ndls. Accessed January 28, 2008. 38. The transactions of the American Medical Association; June 2-5, 1874; Detroit, MI:33. http://www.nmt.com/ama_ndls. Accessed January 28, 2008. 39. The transactions of the American Medical Association, June 6-9, 1876; Philadelphia, PA. http://www.nmt.com/ama_ndls. Accessed January 28, 2008. 40. Blasingame FJL. Digest of Official Actions, 1846-1958. Chicago, IL: American Medical Association Press; 1959:477-478. 41. The transactions of the American Medical Association; May 8-11, 1888; Cincinnati, OH:693-694. http://www.nmt.com/ama_ndls. Accessed January 28, 2008. 42. Cobb WM. The black American in medicine. J Natl Med Assoc. 1981;73:1185-1244. 43. Cobb MW. The First Negro Medical Society. Washington, DC: The Associated Publishers; 1939. 44. Gallman B. From Africa to South Carolina: a brief review of the contributions of Africans and African-Americans to medicine. J S C Med Assoc. 1988;84(5):249-255. 45. Morais H. The History of the Negro in Medicine. 1st ed. New York, NY: Association for the Study of Negro Life and History and Publishers Co Inc; 1967. 46. The Lone Star State Medical, Dental, and Pharmaceutical Association. The Handbook of Texas Web site. http://www.tsha.utexas.edu/handbook/ online/articles/LL/sal1.html Accessed September 5, 2007. 47. Old North State Medical Society Virtual Museum Web site. www.oldnorthstatemedicalsociety.org/virtualMuseum/Main%20-%20ONSMS%20Virt ual%20Museum.html. Accessed June 6, 2007. 48. North Jersey National Medical Association Records Web site. http:// www.umdnj.edu/librweb/speccoll/NoJNatMedAssn.html. Updated June 3, 2001. Accessed June 6, 2007. 49. About the NMA. National Medical Association Web site. http://www. nmanet.org/index.php/nma_sub/history. Accessed September 15, 2007. 50. Wright CH. The National Medical Association Demands Equal Opportunity: Nothing More, Nothing Less. Southfield, MI: Charro Book Co; 1995:29-39. 51. Roman CV. Historical manifesto. National Medical Association Web site. http://www.nmanet.org/index.php/nma_sub/introduction. Accessed August 21, 2007. 52. American Medical Directory. 1st ed. Chicago, IL: American Medical Association Press; 1906. 53. Deaths. JAMA. 1931;97(10):721. 54. Daniel Hale Williams. Northwestern University Archives Web site. http:// www.library.northwestern.edu/archives/exhibits/alumni/williams.html. Accessed September 18, 2007. 55. Johnson V. A History of the Council on Medical Education and Hospitals of the American Medical Association. Philadelphia, PA: WB Saunders; 1947. 56. Johnston P. Dr. Alexander Augusta: breaking down the barriers for black doctors. Can Med Assoc J. 1993;149:1322-3. 57. Savitt T. Abraham Flexner and the black medical schools. J Natl Med Assoc. 2006;98:1415-1424. VOL. 101, NO. 6, JUNE 2009 511 African Americans and Organized Medicine 58. Holmes DOW. Fifty years of Howard University: Part I. J Negro Hist. 1918;3(2):128-138. 59. Holmes DOW. Fifty years of Howard University: Part II. J Negro Hist. 1918;3(4):368-380. 60. Lloyd SM Jr. A short history of the Howard University College of Medicine. Howard University College of Medicine Web site. http://www.med. howard.edu/nuHoward/history.html. Updated May, 2006. Accessed April 24, 2007. 61. Callis HA. The need and training of negro physicians. J Negro Educ. 1935;4(1):32-41. 62. Flexner A. Medical Education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching. Available at: http://www.carnegiefoundation.org/files/elibrary/flexner_ report.pdf. Accessed September 29, 2008. 63. Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education 100 years after the Flexner report. N Eng J Med. 2006;355(13):13391344. 64. Ludmerer K. Learning to Heal: The Development of American Medical Education. New York, NY: Basic Books; 1985. 65. King LS. Medicine in the USA: historical vignettes XX: the Flexner report of 1910. JAMA. 1984;251(8):1079-1086. 66. We, the American blacks. United States Census Bureau Web site. http:// www.census.gov/apsd/wepeople/we-1.pdf. Updated September, 1993. Accessed January 28, 2008. 67. Lemann N. Promised Land: The Great Black Migration and How It Changed America. New York, NY: Knopf; 1991. 68. Editorial. The influence of the Carnegie Foundation on medical education. JAMA 1909;53(7):559-560. 69. Bevan AD. Cooperation in medical education and medical service: functions of the medical profession, of the university and of the public. JAMA. 1928;90(15):1173-1177. 70. Medicine pays tribute to Dr. Flexner. American Medical Association News. October 5, 1959. 71. Martini CJM. An estimable legacy. JAMA. 1990;264(7):795-797. 72. Medical education in the United States. JAMA. 1923;81(7):553. 73. Plessy v Ferguson, 163 US 537, 538 (1896). FindLaw Web site. http:// caselaw.lp.findlaw.com/scripts/printer_friendly.pl?page=us/163/537.html. Accessed January 31, 2008. n We Welcome Your Comments The Journal of the National Medical Association welcomes your Letters to the Editor about articles that appear in the JNMA or issues relevant to minority healthcare. Address correspondence to EditorJNMA@nmanet.org. 512 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION VOL. 101, NO. 6, JUNE 2009