Document
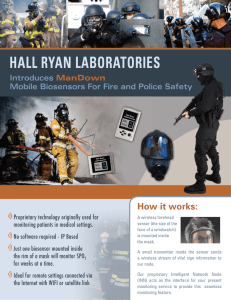
advertisement

Introduction to Biomedical Engineering Biomedical sensors Kung-Bin Sung 5/21/2007 1 Outline • Chapter 9: Biomedical sensors – Biopotential measurements – Physical measurements – Chemical measurements • Blood gases and pH sensors – Biosensors • • • Affinity biosensors: enzymatic and antibodybased Direct and indirect detection Fiber optic biosensors 2 Introduction • • • • Transducer is a device that converts energy from one form to another In sensors, a transducer converts an observed change into a measurable signal Integrated with other parts to “read” out the signal (electrically, optically, chemically) Some are used in vivo to perform continuous, invasive or non-invasive monitoring of critical physiological variables – • pressure, flow, concentration of gas Some are used in vitro to help clinicians in various diagnostic procedures – electrolytes, enzymes, metabolites in blood 3 Introduction • • • • in vivo: inside a living body (human or animal) ex vivo: outside the living body in vitro: in a test tube in situ: right in the place where reactions happen (could be in the cells, tissue, test tube, etc.) 4 Physical measurements • Displacement – – – – • • Inductive Resistive Capacitive Ultrasonic Air flow Temperature 5 Displacement transducers Linear Variable Differential Transformer (LVDT) The primary coil P is excited by an AC current The induced potentials at the 2 secondary coils are canceled due to the opposite polarities When the core moves toward one coil, the induced potential in the coil increases and the voltage in the other coil decreases Induced voltage ∝ Displacement 6 Displacement transducers Potentiometer: resistance is proportional to position If the current through the resistor is constant, the displacement (linear or angular) will be proportional to ∆VO = I∆R 7 Displacement transducers Strain gauge: measures a small change in the length of an object as a result of an applied force l R=ρ A Resistance of a conductive materiel with length l and cross-sectional area A. ρ is a constant (resistivity) The fractional change in length of an object is called strain ∆l S= l Now consider a metal wire as a strain gauge l Original Stretched l+∆l l + ∆l l ∆l ∆R = ρ −ρ ≈2 R Al /(l + ∆l ) A l The gauge factor G G= ∆R / R =2 ∆l / l For silicon strain gauges, G > 100 (much more sensitive than metal) 8 Displacement transducers Strain gauge examples Bonded to a semiflexible backing material Unbonded configuration for measuring blood pressure The change in resistance is quite small ⇒ amplifiers Strain gauges are very sensitive to temperature ⇒ temperature compensation 9 Displacement transducers Capacitive: change in distance between two parallel plates (an insulating material sandwiched in the middle) results in a change in capacitance A: area A d: distance between two conductors C = ε 0ε r d where ε0 is the permittivity of vacuum = 8.85×10-12 F/m εr is dielectric constant of the insulating material 10 Displacement transducers Piezoelectric transducer: certain crystal (such as quartz) generates a small electric potential when it is mechanically strained. The charge Q induced at surface is proportional to the applied force F Q = kF (k is a constant and specific to the material) Then the voltage across the crystal is V= Q C Not used for measuring DC (static) displacement due to internal leakage resistance that dissipates the surface charge The inverse reaction can also happen ⇒ apply an voltage across the crystal, and the crystal expands or contracts In fact, piezoelectric transducers are often used to generate high frequency vibrations such as ultrasonic pulse transducers and resonant oscillators 11 Air flow Fleish pneumotachometer Flow rate ∝ ∆P Pressure is measured at both sides of the resistive screen The screen obstruction provides some resistance to the air flow and therefore generates pressure drop across the screen 12 Blood flow Apply a uniform magnetic field B across blood vessel r r r F = q (v × B ) If velocity of blood flow is v, F is force experienced by charged particles in blood This force causes movement of charges ⇒ distribution of charges generates an electric field E F (blood flows into the screen) B E r V E= d d: diameter of blood vessel For charged particles, there is a second force qE, at equilibrium: V qvB = qE = q d V ⇒v= Bd 13 Temperature transducer - thermocouple Thermocouple: two different metal wires welded together Seebeck (1821) effect: - Thermal to electrical - An electromotive force (emf) exists across the junction and is temperature dependent Nickel If we use two such junctions, one is at a known temperature and the other is at the sample I ∝ (T1 − T2 ) when the temperature difference is small 14 Temperature transducer - thermocouple The reference is typically in ice bath ⇒ 0°C Thermocouples: - very rapid response - stable over wide range of temperatures (up to hundreds or even 1000) - can be made quite small ⇒ in 30 gauge needle (outside diameter = 0.3mm) - disadvantage: need a reference (ice bath) 15 Temperature transducer – thermistor Thermistor: semiconductor; the resistance is a function of temperature β (1 / T −1 / T0 ) RT = R0 e where R0 is the resistance at a reference temperature, T0, and RT is the resistance at temperature T. β is a material-specific constant. Both temperatures are expressed in degrees K Common shapes of thermistors The size and mass of a thermistor probe must be small to produce a rapid response to temperature variations 16 Temperature transducer – thermistor Thermistors: - have high sensitivity (<<1°C) - range is not as great as thermocouples (-50°C – 100°C), but suitable for biological/physiological measurements - need calibration (R vs. temperature curve) - can also be made very small 17 Cardiac output measured by thermodilution Catheter with multiple ports - Inject cold saline into the right atrium (intravenous catheter) - Measure temperature at the pulmonary artery over time - Conservation of energy: The total heat content of the injected saline will be T Vi ∆Ti ρ i ci = ρ b cb ∫ flow ⋅ ∆Tb (t )dt 0 Average blood flow (m3/s) ρ: density (kg/m3) c: specific heat capacity (J/kgK) Vi: injection volume T: temperature 18 Chemical measurements Important analytes and their normal ranges in blood, which indicate the physiological status of the body: gas pressure and related parameters, electrolytes, and metabolites 19 Electrochemical cells as sensors - Typically used for measurements of ion or gas-molecule concentrations - The sensor consists of two electrodes and an ionic conductive material called an electrolyte - Operation of electrochemical sensors is based on reactions and their equilibrium at the electrode surfaces (interface between electronic and ionic conductors) 20 Blood oxygen measurement Measuring arterial blood gases pO2: in operating room and intensive care unit to monitor respiratory and circulatory condition of a patient Clark electrode: measures partial pressure of O2 bias voltage ~0.7 V O 2 + 2H 2 O + 4e − ↔ 4OH − Measured current ∝ concentration of O2 Ag ↔ Ag + + e − Ag + + Cl − ↔ AgCl ↓ 21 Transcutaneous pO2 measurement The skin is heated to 43°C to increase local blood flow and enhance diffusion of O2 through the skin Mostly used on newborn babies in the ICU because their skin is thinner 22 Blood oxygenation Oxygen saturation (% of oxygenated hemoglobin) can be measured and used to represent blood oxygenation Relationship between arterial blood oxygen saturation and partial pressure of O2 mm Hg Note different curves at different pH values 23 Oxygen saturation Saturation of O2 SO2 [ HbO 2 ] = × 100% [Hb] + [HbO 2 ] Oximetry: (color) measures light absorbance at one wavelength where there is a large difference between Hb and HbO2 and at another wavelength (or more wavelengths) SO 2 = x + y Absorbance A(λ1 ) A(λ2 ) A: absorbance x and y are constants depending on optical properties of blood 24 Oxygen saturation Pulse oximetry: use the pulsatile (AC) component to extract oxygen saturation information and the non-pulsatile (DC) signal as a reference for normalization Change in arterial blood volume associated with periodic contraction of the heart 25 pH measurements Membrane permeable to H+ is located at the tip of the active electrode The potential across the membrane (Nernst equation) V = 0.059 ⋅ log10 [H + ] + K K is a constant pH = − log10 [H + ] V ion-selective membrane The glass membrane is highly selective to H+ 26 pCO2 measurements For pCO2 measurement H 2 O + CO 2 ↔ H 2 CO 3 ↔ H + + HCO 3 [CO 2 ] = a(PCO 2 ) − a is a constant It can be shown that − pH = log[HCO3 ] − logk − log a − log PCO 2 Linear relationship over range of 10-90 mmHg 27 Biosensor – introduction • Biosensor: is a sensor using a living component or a product of a living thing for measurement or indication. Generally a biosensor consists of two parts – – A biological recognition element (enzyme, antibody, receptor) to provide selectivity to sense the target of interest (referred to as the analyte) A supporting element which also acts as a transducer to convert the biochemical reaction into “signal” that can be read out 28 Biosensor – introduction “Receptor” provides selective molecular recognition For example: enzymes, antibodies, receptors, nucleic acids, polypeptides, etc. Transducer types in biosensors: calorimetric, electrochemical, optical, etc. 29 Enzymatic biosensors Enzymes are catalysts for biochemical reactions; large macromolecules consisting mostly of protein, and usually containing a prosthetic group (metals) Substrate: the target molecule of an enzymatic reaction S+E ES E+P S: substrate; E: enzyme; ES: enzyme-substrate complex; P: product Reaction rate vs. substrate concentration at constant enzyme concentration 30 Enzymatic biosensors • Advantages – Highly selective – Enzymes are catalytic, thus improving the sensitivity – Fairly fast • Disadvantages – Expensive: cost of extraction, isolation and purification – Activity loss when enzymes are immobilized – Enzymes tend to be deactivated after a relatively short period of time 31 Enzymatic biosensors - In an enzymatic biosensor, the enzyme is immobilized as the “receptor” - Enzymes are specific to their substrates which can be the analyte Example: glucose sensors glucuse oxidase Glucose + O 2 + H 2 O ←⎯ ⎯ ⎯⎯→ gluconic acid + H 2 O 2 Measures the amount of O2 consumption permeable to O2 only Glucose O2 32 Enzymatic biosensors Alternatively, the reaction product hydrogen peroxide can also be measured through reduction of H2O2 H 2 O 2 → 2H + + O 2 + 2e − Use a Clark-type electrochemical cell similar to the one for measuring O2, but at a positive bias voltage of 0.65V Problems: 1. The reduction/oxidation potentials are fairly high ⇒ other materials will interfere 2. The concentration of O2 needs to be kept constant, which is difficult since O2 is involved in the reactions 33 Electron mediators in enzymatic biosensors In the membrane: S + O 2 ⎯oxidase ⎯⎯→ P + H 2 O 2 At the anode: H 2 O 2 → 2H + + O 2 + 2e − Oxygen is consumed and later regenerated, therefore it only serves to transfer electron ⇒ can be replaced by a mediator Example: multi-cycle chemical electrochemical reaction chain for detecting glucose (ox) (red) (ox) GO: glucose oxidase M: mediator 34 Immunosensors Immunosensors: based on highly specific antigen-antibody reactions Antibody: works against the foreign body Immunoglobin: globular proteins that participate in the immune response Structure of antibody The Fc end of an antibody can bind to other immune cells and the binding activate these immune cells 35 Immunosensors Detection of the reaction (binding/association) can be either direct or indirect (labeled) Direct detection: the binding of the analyte (antigen) to the “receptor” (antibody) is detected directly through the presence of the analyte However, most are indirect due to lack of signal from the analyte itself 36 Immunosensors Indirect detection: signal is provided by an exogenous reporter competitive sandwich 37 Immunosensors The interaction between antigen and antibody can be expressed as ka A+ B kb AB A: free antigen; B: free antibody ka: association rate constant; kb: dissociation rate constant At equilibrium, the affinity constant (or association constant) KA = ka [AB] = k d [A][B ] (units M-1) And the dissociation constant k d [A][B ] = KD = [AB] ka (units M) 38 Immunosensors Antigen-antibody interactions are reversible and the interaction halflife is determined by the magnitude of the kinetic rate constant Dissociation rate constant kd and half-life of an antigen-antibody binding complex Kinetic rate constants of antigen-antibody interactions can be obtained with biosensors based on surface plasmon resonance 39 Immunosensors The surface density of antigen molecules bound to the sensor vs. the bulk concentration of antigen K: binding constant of the antibody-antigen interaction Γmax: maximum surface density of antigen molecules 40 Indirect detection • Radioimmunoassay (RIA) – – – • ELISA (Enzyme-Linked Immunosorbent Assay) – – • The labels are radioactive isotopes (for example 131I) Highly sensitive and specific but inconvenient and expensive Less popular now due to safety issues Enzymes are used for labeling and signal is provided by the reaction product Simple in terms of procedure and equipment Fluorescent immunoassay – Labeled with fluorescent dyes 41 ELISA detection antibody secondary detection antibody substrate and product analyte Capture antibody Typically colorimetric measurement (absorbance at certain wavelength ∝ analyte concentration) 42 Direct detection – Surface plasmon resonance A surface plasma wave (SPW) is an electromagnetic wave (due to charge density oscillation) which propagates along the boundary between a dielectric (e.g. glass) and a metal Magnetic field parallel to the interface n1 The magnitude of the surface plasmon wave decreases exponentially into both dielectric and metal media Electric field is parallel to the plane of incidence 43 SPR biosensors A surface plasmon wave can be excited optically: when the propagation constant β of the incident light and the SPW are equal in magnitude and direction for the wavelength This corresponds to a certain angle of incident light at a fixed wavelength ⇒ the reflected light reaches its minimum reflectivity Incident light with various angles Binding induced change in propagation constant of SPW is proportional to the refractive index change in the sample ⇒ the angle of incident light also changes 44 SPR biosensors Different parameters are measured in SPR biosensors to indicate the refractive index change in the sample (due to binding) Using monochromatic light Angle of incident light Using fixed incident and reflection angles Wavelength of incident light 45 SPR biosensors The kinetics of binding events can be monitored continuously sensorgram BSA: bovine serum albumin, used to non-specific binding Analyte: SEB (staphylococcal enterotoxin B) a-SEB: antibody against SEB ⇒ sandwich binding 46 SPR biosensors • • • • • Direct detection ⇒ no need for labeling High sensitivity Fast ⇒ real-time monitoring Used with sample in liquid ⇒ important for biological samples Relatively simple device, which makes multichannel parallel detection easier ⇒ high throughput 47 SPR commercialization - BIACORE BIACORE optical system: light from different angle of reflection is imaged onto different position of a photo-detector array 2D photo-detector array Multiple flow-cells ⇒ simultaneous detection of reflection intensity 48 BIACORE products 49 BIACORE features • • • • • Specificity: different molecules interact with a single partner immobilized on a sensor surface Kinetics: rates of complex formation (ka) and dissociation (kb) Affinity: the level of binding at equilibrium (KD, KA) Concentration: can be determined for purified molecules or for molecules in complex mixtures such as serum (needs a calibration curve) Multiple interactions during complex formation 50 Fiber optic based biosensors Optical fibers are flexible and compact which are important features for applications that need miniaturization such as in vivo measurements 51 Optical fiber Typically made of glass SiO2, and consisting of a core and a cladding layer Transmits light through the core (total internal reflection) Diameter can be very small ~µm ⇒ very flexible The angle of light rays that go into the fiber core and can be accepted (transmitted) by the fiber is dependent on the core and cladding materials Incident angle of light rays going into a fiber must be less than θ θ θt NA of an optical fiber = sinθ = n2 n1 n1 − n2 2 2 52 Optical fiber sensor – examples • Sensing area along side of an optical fiber Total internal reflection inside the fiber • Sensing area located at distal end surface of an optical fiber 53 Optical fiber sensor – examples A fiber optic (imaging) bundle is used for detecting multiple analytes simultaneously - Each latex sphere can specifically binds to one analyte - The analytes can be fluorescently labeled - Use of reference channels could increase the reliability of detection (e.g. spheres without recognition element still bind to some analyte molecules non-specifically, so the measured fluorescence from the reference spheres is considered “background” and should be subtracted) 54 Trends in biomedical sensors Centralized laboratory Point of care Patients’ home in vitro Single test in vivo Multiple tests in a single run Key technologies for miniaturization of biomedical sensors and realization of biochips: microfluidics, semiconductor fabrication processes, microelectromechanical systems (MEMS) Equally important are: the development of more stable and effective biomolecules used for recognition; search for new target analytes that are of diagnostic and/or biological significance 55 Biochips • • • • Miniaturized and highly integrated Provide analytical or diagnostic function Substrates can be glass, silicon, polymer, plastic, etc Desired features: high sensitivity and specificity, high speed, small size, small sample requirement, multi-channel and parallel analyzing, reliable, cost-effective 56 References • • • Medical Instrumentation: Application and Design, edited by John G. Webster Chemical sensors and biosensors, by Brian R. Eggins Sensors in Biomedical Applications: Fundamentals, Technology & Applications, by Gábor Harsányi – • • Ch7: Biosensors Information about glucose meters http://www.diabetesmonitor.com/meters.htm#fc nim Biomolecular sensors, edited by Electra Gizeli & Christopher R. Lowe 57