ASH NEWS AND REPORTS®
May/june 2014 Volume 11 Issue 3
Newly Redesigned ASH Website Offers Improved Search
Capability and Access to Most-Viewed Content
If you have visited the ASH website in the past few weeks
you may have noticed some significant changes. A new
site design was launched on April 4 as part of a multiyear effort to upgrade the Society’s technology platforms.
ASH President Linda J. Burns, MD, explained, “The ASH
leadership felt the time had come to invest in a strategy
that will better serve the Society’s membership by bringing
ASH’s digital offerings in closer alignment with member
needs.” These offerings include not only the Society’s
website, but also mobile apps, e-books, and other forms of
electronic communication.
The first step in the process entailed months of research
to better understand why ASH’s key audiences visit the
website, the specific tasks they are trying to accomplish,
and how successful they are. “By using software to track
where users tend to click most often throughout ASH’s
website, we learned that many of the navigational headings
designed to help users find information quickly were not
being utilized,” said Michael Mersky, ASH’s Web Manager.
“So we employed a number of user testing exercises to
find out what terms our users would choose to name and
(Cont. on page 6)
D I F F U S I O N
Features
A Hereditary Bleeding Disorder Reveals a New Cog in the Coagulation Mechanism
4
Vincent LM, Tran S, Livaja R, et al. Coagulation factor VA2440G causes east Texas bleeding disorder via TFPIα. J Clin Invest.
2013;123:3777-3787.
Ask the Hematologist –
Dr. Janet Abrahm discusses
her approach to the management of
chemotherapy-induced peripheral
neuropathy.
7
Update on the 2013
ASH Choosing Wisely
Initiative – Dr. Lisa Hicks reviews
the ASH Choosing Wisely initiative and
summarizes the ongoing aims of the
ASH Choosing Wisely Task Force.
14
My Journey in
Hematology – Dr. John
Adamson recounts highlights of his
remarkable career that has taken him on
a circuitous journey from California to
Oxford and back again.
DEPARTMENTS
2president’s column
3News and Reports
7The Hematologist Advocate
W
hat is the differential diagnosis in a 35-year-old male
with a lifelong history of easy bruising, epistaxis, and
prolongation of both the prothrombin time (PT) and the
activated partial thromboplastin time (APTT)? So began
the evaluation by Dr. Shao-Qing Kuang et al. in the laboratory of Dr.
Dianna Milewicz at the University of Texas Health Science Center in
Houston, Texas.1 The family history revealed an autosomal bleeding
disorder in an east Texas kindred consisting of 46 family members
spanning four generations. Surprisingly, coagulation factor assays
for fibrinogen and factors II, V, VII, VIII, IX, X, XI, and XII were normal.
Linkage analysis demonstrated that the factor V (FV) gene (F5)
mapped to the disease interval. Sequencing of the F5 gene revealed
an A2440G mutation in exon 13 at position 2440, predicting a
S756G mutation in the B domain of FV. However, because FV levels
were normal, the mutation was considered an unlikely cause of the
bleeding diathesis.
The cause of this mysterious bleeding disorder remained unknown for
more than another decade until it was elucidated by Dr. Lisa Vincent
and colleagues from the laboratories of Dr. Milewicz in Houston and
Dr. Björn Dahlbäck of Lund University Hospital in Malmö, Sweden.
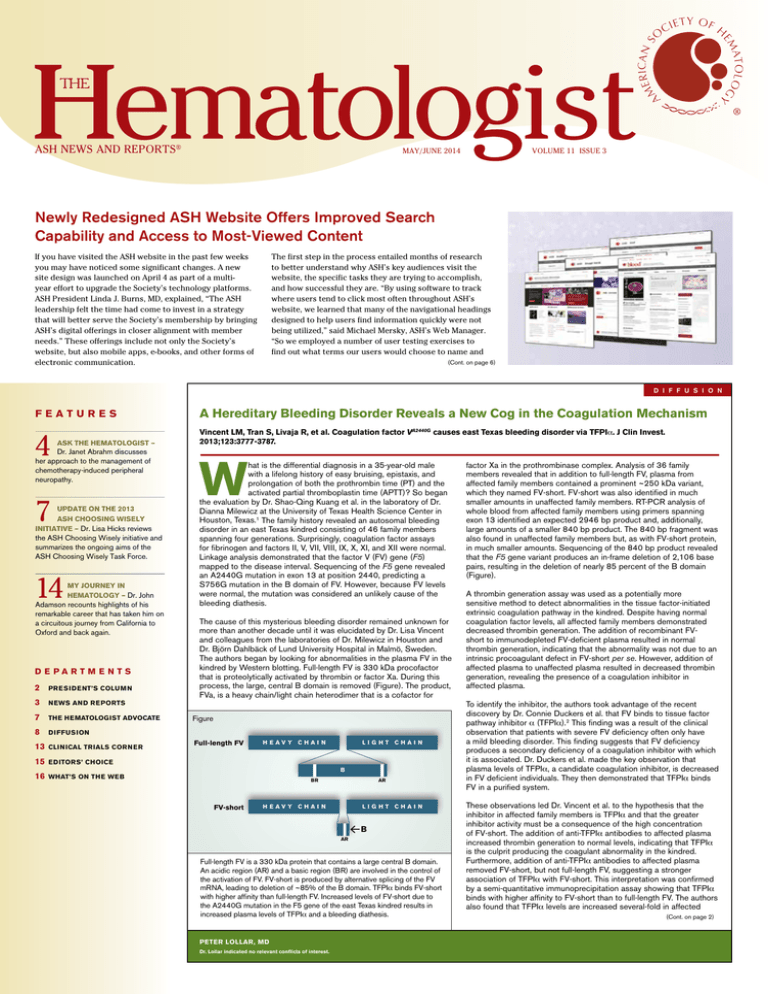
The authors began by looking for abnormalities in the plasma FV in the
kindred by Western blotting. Full-length FV is 330 kDa procofactor
that is proteolytically activated by thrombin or factor Xa. During this
process, the large, central B domain is removed (Figure). The product,
FVa, is a heavy chain/light chain heterodimer that is a cofactor for
Figure
8Diffusion
13Clinical Trials Corner
Full-length FV
HEAVY C HAIN
LIGHT C HAIN
15EDITORS’ CHOICE
B
16WHAT’S ON THE WEB
BR
FV-short
AR
HEAVY C HAIN
LIGHT C HAIN
B
AR
Full-length FV is a 330 kDa protein that contains a large central B domain.
An acidic region (AR) and a basic region (BR) are involved in the control of
the activation of FV. FV-short is produced by alternative splicing of the FV
mRNA, leading to deletion of ~85% of the B domain. TFPIα binds FV-short
with higher affinity than full-length FV. Increased levels of FV-short due to
the A2440G mutation in the F5 gene of the east Texas kindred results in
increased plasma levels of TFPIα and a bleeding diathesis.
peter lollar, MD
Dr. Lollar indicated no relevant conflicts of interest.
factor Xa in the prothrombinase complex. Analysis of 36 family
members revealed that in addition to full-length FV, plasma from
affected family members contained a prominent ~250 kDa variant,
which they named FV-short. FV-short was also identified in much
smaller amounts in unaffected family members. RT-PCR analysis of
whole blood from affected family members using primers spanning
exon 13 identified an expected 2946 bp product and, additionally,
large amounts of a smaller 840 bp product. The 840 bp fragment was
also found in unaffected family members but, as with FV-short protein,
in much smaller amounts. Sequencing of the 840 bp product revealed
that the F5 gene variant produces an in-frame deletion of 2,106 base
pairs, resulting in the deletion of nearly 85 percent of the B domain
(Figure).
A thrombin generation assay was used as a potentially more
sensitive method to detect abnormalities in the tissue factor-initiated
extrinsic coagulation pathway in the kindred. Despite having normal
coagulation factor levels, all affected family members demonstrated
decreased thrombin generation. The addition of recombinant FVshort to immunodepleted FV-deficient plasma resulted in normal
thrombin generation, indicating that the abnormality was not due to an
intrinsic procoagulant defect in FV-short per se. However, addition of
affected plasma to unaffected plasma resulted in decreased thrombin
generation, revealing the presence of a coagulation inhibitor in
affected plasma.
To identify the inhibitor, the authors took advantage of the recent
discovery by Dr. Connie Duckers et al. that FV binds to tissue factor
pathway inhibitor α (TFPIα).2 This finding was a result of the clinical
observation that patients with severe FV deficiency often only have
a mild bleeding disorder. This finding suggests that FV deficiency
produces a secondary deficiency of a coagulation inhibitor with which
it is associated. Dr. Duckers et al. made the key observation that
plasma levels of TFPIα, a candidate coagulation inhibitor, is decreased
in FV deficient individuals. They then demonstrated that TFPIα binds
FV in a purified system.
These observations led Dr. Vincent et al. to the hypothesis that the
inhibitor in affected family members is TFPIα and that the greater
inhibitor activity must be a consequence of the high concentration
of FV-short. The addition of anti-TFPIα antibodies to affected plasma
increased thrombin generation to normal levels, indicating that TFPIα
is the culprit producing the coagulant abnormality in the kindred.
Furthermore, addition of anti-TFPIα antibodies to affected plasma
removed FV-short, but not full-length FV, suggesting a stronger
association of TFPIα with FV-short. This interpretation was confirmed
by a semi-quantitative immunoprecipitation assay showing that TFPIα
binds with higher affinity to FV-short than to full-length FV. The authors
also found that TFPIα levels are increased several-fold in affected
(Cont. on page 2)
President’s Column
Hematologist
THE
AS H N e w s a n d R e p o rt s ®
I SSN 1 5 5 1 - 8 7 7 9
Training the Next Generation
Editor-in-Chief:
A
Charles Parker, MD
University of Utah
Salt Lake City, UT
I’m proud of the Society’s long history of partnering with medical educators in hematology to advance scholarship in our
subspecialty by tackling head-on the challenges we’ve all had to face. From practical approaches such as training guidelines, to
advocating for evidence-based medical education, to creation of tools for educators, to awarding of grants to trainees, ASH has stood
by those of us on the front lines of our medical schools and teaching hospitals. Several new initiatives aim to continue this tradition:
Pamela S. Becker, MD, PhD
University of Washington
Seattle, WA
s a fellowship program director for the past 18 years, I marvel at the changes that have been introduced into the training
environment. From managing mandated reductions in duty hours of fellows to documentation of competency measures,
it seems those of us in the educational space have not had a moment’s rest!
1. As has been reported in this publication, in ASH NewsLink, and on the ASH website, the Committee on Training, chaired by Gary
Schiller, MD, is interested in developing an ASH Medical Educators Institute. This program, modeled on ASH’s Clinical Research
Training Institute, will provide guidance to dedicated hematology educators who are aiming both to improve individual teaching
skills and to enhance learning opportunities at their home institution. The committee and I would be interested in your thoughts
on crafting this program and count on your enthusiastic volunteerism in making this new initiative a success.
2. A working group, organized by the Committee on Training and led by Elaine Muchmore, MD, is in the process of developing
milestones for fellows in hematology training programs. Creation of these milestones is a critical element necessary to meet the
requirements of the Accreditation Council for Graduate Medical Education’s Next Accreditation System (ACGME NAS). For those
of you who have yet to hear of this sweeping new program, NAS began phase implementation in July 2013 and represents the
culmination of a multi-year process of restructuring ACGME’s accreditation system based on educational outcomes in clinical
competency.
3. The Teaching Cases Subcommittee, which has responsibility for developing and maintaining the ever-popular medical student
cases on the ASH website, has been diligently developing new cases and researching new approaches to make the cases more
interactive and engaging. This program is strongly supported by the Society as evidence by its prominent place on the agenda of
the upcoming ASH Executive Committee meeting.
4. Last spring, the Society launched the Fundamentals for Hematology Fellows Program that provides a bundle of ASH resources
to fellows in hematology-related training programs. This initiative has exceeded our expectations by adding more than 1,000
additional fellows to our Associate member category. The program not only provides a connection from ASH to the trainee, but
also makes participants eligible for ASH programs such as the Clinical Research Training Institute.
These new efforts join a panoply of continuing programs, including the Research Training Award for Fellows, annual meeting events
such as the Hematology Course Directors’ Workshop, and services such as the Hematology In-Service Examination, designed to
address hematology training from the perspective of the learner, the educator, and the training environment. I hope every educator
in hematology knows about these programs and uses them to their best advantage. Please contact training@hematology.org with any
questions about ASH’s educational programs.
Our goal at ASH is to enthusiastically support medical educators in hematology and, together with this dedicated group, to continue
improving training in our subspecialty by developing new initiatives and sustaining ongoing programs that focus on the needs of
faculty and fellows.
Contributing Editors:
Theresa Coetzer, PhD
University of the Witwatersrand
Johannesburg, South Africa
Adam Cuker, MD, MS
University of Pennsylvania
Philadelphia, PA
David Garcia, MD
University of Washington
Seattle, WA
Jason Gotlib, MD, MS
Stanford Cancer Center
Stanford, CA
Peter Johnson, MD
Southampton General Hospital
Southampton, United Kingdom
Mark J. Koury, MD
Vanderbilt University
Nashville, TN
Peter Kurre, MD
Oregon Health & Science University
Portland, OR
Ann LaCasce, MD, MSc
Dana-Farber Cancer Institute
Boston, MA
Pete Lollar, MD
Emory Children’s Center
Atlanta, GA
Charles T. Quinn, MD, MS
Cincinnati Children’s Hospital
Medical Center
Cincinnati, OH
Gregory M. Vercellotti, MD
University of Minnesota
Minneapolis, MN
Linda J. Burns, MD
Managing Editor
Karen Learner
Editorial Assistant
Tiffany Reid, MA
Graphic Designer
A Hereditary Bleeding Disorder Reveals a New Cog in the
Coagulation Mechanism
D I F F U S I O N
The authors speculated that the normal levels of FV and other
coagulation factors in affected plasmas are due to the strong
procoagulant stimulus in coagulation assays (tissue factor in the PT
and activated partial thromboplastin in the APTT). Accordingly, the
rapid production of high concentrations of Factor VIIa and Factor
Xa would overwhelm TFPIα, even when its concentration is elevated
in affected plasmas. In contrast, thrombin generation assays were
performed in diluted plasma and at low concentrations of tissue factor,
leading to more sensitive detection of a coagulant defect due to
elevated levels of TFPIα.
The role of the large B domain in FV function has been enigmatic.
Recently, Dr. Mettine H.A. Bos and Dr. Rodney M. Camire
demonstrated that the B domain serves to maintain FV in an inactive,
procofactor state.3 A basic region and an acidic region in the B domain
have been identified that are necessary for this function (Figure).
Interestingly, the basic region is not present in FV-short (Figure), which
has implications for FV and TFPIα structure and function that remain to
be investigated.
2
American Society of Hematology
2021 L Street, NW, Suite 900
Washington, DC 20036
klearner@hematology.org
(Cont. from page 1)
plasmas compared with unaffected plasmas. They proposed that
free, 40 kDa TFPIα is cleared by kidneys, and that this clearance is
prevented when TFPIα is bound in a high-molecular-weight complex
with FV or FV-short. Thus, the increased association of TFPIα with FVshort leads to higher plasma levels.
grayHouse design
An A2440G mutation in exon 13 of the F5 gene results in increased
usage of an alternative splice-donor site, leading to production of
a previously undetected protein, FV-short. Alternative splicing and
expression of FV-short also occurs in the absence of the mutation,
albeit to a lesser extent. TFPIα binds to full-length FV and FV-short,
but with higher affinity to the latter. The association of TFPIα with
FV-short reduces the clearance of TFPIα by preventing renal filtration.
The resulting increase in TFPIα produces a bleeding diathesis due to
an increased inhibition of Factor VIIa and Factor Xa. The results of this
study have identified an important new mechanisms underlying FV and
TFPIα biology in the regulation of coagulation.
1. Kuang S, Hasham S, Phillips MD, et al. Characterization of a novel
autosomal dominant bleeding disorder in a large kindred from east
Texas. Blood. 2001;97:1549-1554.
2. Duckers C, Simioni P, Spiezia L, et al. Low plasma levels of
tissue factor pathway inhibitor in patients with congenital factor V
deficiency. Blood. 2008;112:3615-3623.
©2014 by the American Society of Hematology.
All materials contained in this newsletter are
protected by copyright laws and may not be
used, reproduced, or otherwise exploited in
any manner without the express prior written
permission of The Hematologist: ASH News and
Reports. Any third-party materials communicated
to The Hematologist become its copyrighted
property and may be used, reproduced, or
otherwise exploited by The Hematologist.
Contributing authors have declared any
financial interest in a product or in potentially
competing products, regardless of the dollar
amount. Any such financial interest is noted at
the bottom of the article.
Dr. Parker has no relevant conflicts of interest
to disclose.
3. Bos MH and Camire RM. A bipartite autoinhibitory region within
the B-domain suppresses function in factor V. J Biol Chem.
2012;287:26342-26351.
The Hematologist:
ASH News and Reports
n e ws
and
r e p or t s
Register to Attend the New ASH Meeting on
Lymphoma Biology
August 10-13, 2014
The Broadmoor, Colorado Springs, Colorado
Get a comprehensive update on the most recent discoveries in lymphoma
biology and interact with world-class experts in the field. During this three-day
forum, keynote speaker Klaus Rajewsky,
MD, will discuss immune regulation and
cancer, and attendees will hear about
the most recent progress in basic and
translational lymphoma research, share
their findings with colleagues, and
exchange ideas with experts on how to
move the field forward.
Klaus Rajewsky, MD
What to Expect
• Informal setting with networking opportunities to share ideas and establish
collaborations
• Presentations by invited experts on topics including:
• B-cell receptor signaling
• Germinal center biology
• Epigenetics of lymphoma
• Immune evasion
• Lymphoma genetics
• Metabolism
• T-cell lymphoma
• Panel discussions
• Oral presentations of the top-rated abstracts
• Poster sessions and interactive workshops
For more information about the meeting and to register, go to www.hematology.
org/Lymphoma-Biology.
2014 ASH Annual Meeting
and Exposition
December 6-9
Moscone Center, San Francisco, CA
The American Society of Hematology (ASH) invites you
to save the date for the 56th ASH Annual Meeting in
San Francisco, CA. As the premier hematology event,
this meeting will provide attendees with an invaluable
educational experience and the opportunity to:
• Review more than 3,000 scientific abstracts.
• Interact with the global community of more than 20,000
hematology professionals from every subspecialty.
• A
ttend the Education and Scientific Program sessions
that feature lectures by leaders in the field.
• D
evelop collaborations with clinical and basic
investigators who share your research interests.
• S
hare the experience with friends and colleagues in a
collegial, stimulating atmosphere in one of America’s
great cities.
Key Dates
Abstract submission site opensJune 5
Advance member registration & housingJuly 24
ASH and ASCO
Present New Seminar
on Hematology for
the Oncologist
ASH is partnering with the American
Society of Clinical Oncology (ASCO)
to present a Hematology for the
Oncologist symposium, May 2930, 2014, in Chicago, IL, as part
of ASCO’s Pre-Annual Meeting
Seminars. Lectures will focus on
hematologic issues that medical
oncologists commonly encounter in a
consultative practice. Experts in the
field will discuss clinical aspects of
bleeding and clotting disorders, novel
oral anticoagulants, iron replacement
therapy, and other benign hematology
topics. Question-and-answer periods
will be incorporated into the sessions
to encourage discussion and ensure
maximum interaction between faculty
and participants.
To learn more about the symposium,
go to http://am.asco.org/
hematology-oncologist-seminar.
Advance registration for non-membersAugust 13
The Hematologist:
ASH News and Reports
3
ASH does not recommend or endorse any specific tests, physicians, products, procedures, or opinions, and disclaims any representation, warranty, or guaranty as to the same.
Reliance on any information provided in this article is solely at your own risk.
Ask the Hematologist
janet l. abrahm, md
Professor of Medicine, Harvard Medical School; Division of Adult Palliative Care, Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute
The Case
The patient is a 54-year-old woman with IgA lambda multiple myeloma, receiving
dexamethasone, lenalidomide, and bortezomib therapy. She was healthy before her
diagnosis but had mild hypercalcemia and mild renal insufficiency at diagnosis, both of
which have resolved with treatment.
She is about to begin her third treatment cycle, but reports painful (pain score of
7/10) numbness and paresthesias in her fingers and feet. The former problem causes
clumsiness when using her touch-screen tablet and phone because she cannot accurately
feel her fingers touch the screens, and she needs the light on at night because she cannot
reliably feel when her feet touch the floor. Her Zubrod (ECOG) performance status is 1.
She had similar, but less severe, symptoms at the beginning of her last chemotherapy
cycle, but she did not mention them to anyone for fear that treatment would be delayed
or discontinued.
NCI-CTC for Neuropathy
Peripheral Sensory Neuropathy
Grade 1: Asymptomatic or loss of deep tendon reflexes or paresthesia
Grade 2: Moderate symptoms limiting instrumental activities of daily living (ADL)
Grade 3: Severe symptoms limiting self-care ADL
Grade 4: Life-threatening consequences; urgent intervention indicated
Grade 5: Death
Peripheral Motor Neuropathy
Grade 1: Asymptomatic clinical or diagnostic observations only; intervention not
indicated
Grade 2: Moderate symptoms limiting instrumental ADL
Grade 3: Severe symptoms limiting self-care ADL; assistive device indicated
During her exam, she was anxious, alert, and oriented. She denied both spine pain and
bowel or bladder incontinence. Her exam was unremarkable except for the neurologic
examination. She had impaired proprioception, decreased vibration and light touch in her
hands to the wrists and feet to the ankles, 4/5 hand grip and finger strength bilaterally,
and 4/5 ankle strength. Her ankle deep tendon reflexes (DTRs) were absent (flaccid).
Laboratory studies showed normal potassium, BUN, creatinine, glucose, calcium, and
magnesium. B12 concentration and thyroid function studies were normal. Her paraprotein
concentration showed a continuing decrease in response to treatment.
The Question
What is your approach to assessment and management of patients with chemotherapyinduced peripheral neuropathy?
My Response
Presentation/Physical Findings
The patient’s presentation is typical of chemotherapy-induced peripheral neuropathy
(CIPN) that is characterized by tingling (71%), numbness (58%), and paresthesias or
dysesthesias (45%), or spontaneous burning, cramping, or aching pain (40%) that is
usually symmetric, begins peripherally and progresses proximally.1 Patients often report
allodynia (i.e., pain from something that is usually not painful, like cold temperatures or
the touch of clothing), or hyperalgesia (i.e., experiencing more pain than usual from a
mildly painful stimulus).
The mechanisms of axonal nerve injury vary by agent and include damage to
mitochondria (bortezomib, platinum compounds, vincristine, paclitaxel), glial cells
and macrophages (bortezomib, oxaliplatin, vincristine, paclitaxel), vasa vasorum
(thalidomide, paclitaxel), endoplasmic reticulum (bortezomib), or microtubules
(bortezomib, taxanes, and vinca alkaloids).2,3
CIPN induced by vinca alkaloids causes numbness, not pain, and loss of DTRs,
proprioception, and motor impairment, such as foot drop.2 Patients receiving
thalidomide, bortezomib, or platinum have a mainly sensory neuropathy, which may
include loss of vibration, proprioception, and DTRs.2 Taxanes cause both a sensory
neuropathy and proximal weakness.2 Only CIPN induced by thalidomide is irreversible.
Evaluation
In a patient whose CIPN appears only after chemotherapy, the evaluation should include
laboratory testing for B12 deficiency, hypothyroidism, hypocalcemia, hypomagnesemia,
and hyperglycemia (Figure 1). Because patients with leptomeningeal carcinomatosis or
spinal cord compression can present with these symptoms, an MRI of the spine with
contrast is recommended for patients with back pain. If the test is negative, an MRI of the
brachial or lumbosacral plexus, depending on the location of the symptoms and clinical
suspicion, may be warranted.
Diagnosis of CIPN is clinical, and nerve conduction studies, EMGs, and skin biopsies are
not needed for diagnosis or management. Chemotherapy doses are generally adjusted for
patients with grade 3 or greater neuropathy based on NCI common terminology criteria
(CTC) for adverse events.
4
Grade 4: Life-threatening consequences; urgent intervention indicated
Grade 5: Death
The patient under discussion had grade 2 sensory neuropathy by these criteria, which
underestimated her disability and functional losses. The NCI-CTC are not as sensitive to
patient-reported symptoms or functional loss as are some other scoring systems, but no
consensus has yet been reached on a standard for grading neurotoxicity.4,5 Quality-of-life
scales may be more relevant (e.g., the CIPN 20 or FACT/GOG-Ntx).6
Treatment
Dose reduction or drug discontinuation is the only specific therapy for most CIPNs;
patients may tolerate higher doses of bortezomib if the drug is given by a subcutaneous
injection rather than by IV infusion. Symptomatic therapies for CIPN are limited (Figure
1). Of the adjuvant agents effective for patients with neuropathic pain, only duloxetine
(30-60 mg/day) has clearly shown efficacy for the CIPN induced by taxanes and platinum.7
Despite the lack of proven efficacy of other agents in CIPN, insurance companies usually
require that patients first fail a trial of gabapentin or pregabalin before authorizing
duloxetine. Occupational therapy or physical therapy is recommended for patients with
≥ grade 2 sensory or motor toxicity to improve function and quality of life. Patients should
also be assessed for depression, which often accompanies uncontrolled chronic pain.8
While vitamin E, vitamin B6, magnesium, calcium, acetyl-L-carnitine, glutamine,
glutathione, n-acetyl cysteine, omega-3 fatty acids, alpha lipoic acid, and cannabinoids
each have shown efficacy in non-randomized, non-placebo-controlled trials, none can be
recommended yet as standard therapy.1, 2, 9
Amitriptyline does not prevent or ameliorate chemotherapy-induced neuropathy from
vinca alkaloids, platins, or taxanes.1 Venlafaxine, gabapentin, the N-methyl-d-aspartate
(NMDA) receptor antagonist dextromethorphan, the oral anesthetics memantine and
mexiletine, and low-dose continuous capsaicin treatment are also ineffective.2
Opioids are recommended for CIPN patients with severe pain.10 Patients will usually
require a long-acting agent to provide basal pain relief (e.g., sustained-release morphine
or a fentanyl patch) and short-acting opioids for breakthroughs. Methadone (Figure
2) is particularly helpful for basal pain relief. Methadone includes d- and l-isomers
that act as opioid-receptor agonists and NMDA receptor antagonists.11 Because NMDA
antagonizes the activity of the opiate receptors, blocking NMDA receptors enhances the
analgesic effect of externally administered opioids. Methadone also inhibits the reuptake
of serotonin and norepinephrine; therefore, it functions as a serotonin-norepinephrine
reuptake inhibitor (SNRI).
Methadone is usually given orally bid to tid. Dose adjustment is needed for hepatic
failure but not for renal failure. The steady state is not reached until 72 hours after the
initial dose or after a dose increase. Therefore, short-acting opioids should be used to
control symptoms in the interim. If pain level falls to ≤ 3 within the first 24 to 48 hours of
initiating methadone, reduce the dose by half immediately to avoid excessive sedation
and respiratory depression that may otherwise occur in the next 24 hours. This delay in
reaching steady-state plasma levels, along with potential cardiac toxicity (prolongation
of the rate corrected QT [QTc] interval) and its interactions with inducers and inhibitors
of the cytochrome P450 system, CYP1A2, CYP3A4, and CYP2D6 make using methadone
safely somewhat complex. Palliative care specialists can be helpful in managing initiation
or adjustment of methadone doses or for consulting on patients with seemingly refractory
pain syndromes.
The Hematologist:
ASH News and Reports
t h e
p rac t icing
h e ma t ologis t
Evidence-Based Algorithm for Evaluation and Symptomatic Treatment of Patients with CIPN
Figure 1
Figure 2
First, exclude spinal or leptomeningeal metastases and plexopathies and correct vitamin or hormone
abnormalities, if present. For patients who have NCI-CTC grade ≥ 3 CIPN, follow standard
protocol guidelines for dose adjustments of anti-neoplastic agents. Use duloxetine for patients with
unacceptable pain levels who are receiving either platinum or taxanes. For refractory pain, add an
opioid. If standard opioids are not effective, or if they cause excessive sedation, myoclonus, or other
side effects, consider using methadone as the “basal” opioid, and use the standard opioids for
breakthrough pain.
*Despite the lack of proven efficacy, insurance companies may require that patients first fail a trial of gabapentin or
prebabalin before authorizing duloxetine.
Patients who, at baseline, have a prolonged QTc interval, or who need high doses of
methadone, have developed cardiac arrhythmias (torsades de pointes; polymorphic
ventricular tachycardia). Fatalities have been reported but were associated with doses
of > 600 mg per day. Common drugs used in hematology patients that also prolong the
QTc include the quinolone antibiotics (especially levofloxacin), typical and atypical
antipsychotics (such as haloperidol and olanzapine), selective serotonin reuptake
inhibitors (SSRIs) (but not SNRIs), and metoclopramide.
Methadone’s drug interactions are listed on websites including www.drugs.com or www.
qtdrug.org. Fluconazole, voriconazole, fluoxetine, and fluvoxamine raise methadone
levels. SSRIs may raise methadone levels in CYP2D6 rapid metabolizers but SNRIs
(e.g., venlafaxine) do not. Additionally, grapefruit juice and acute alcohol ingestion can
increase methadone levels. Drug levels of desipramine (or other tricyclic antidepressants)
and zidovudine increase when methadone is added. Antiretrovirals, phenobarbital,
carbamazepine, phenytoin, rifampin, somatostatin, spironolactone, and risperidone lower
the levels of methadone and have precipitated withdrawal symptoms.
1. Finnerup NB, Sindrup SH, Jensen TS. Management of painful neuropathies. Handb Clin Neurol.
2013;115:279-290.
2. Ferrier J, Pereira V, Busserolles J, et al. Emerging trends in understanding chemotherapy-induced
peripheral neuropathy. Curr Pain Headache Rep. 2013;17:364-372.
3. Diezi M, Buclin T, Kuntzer T. Toxic and drug-induced peripheral neuropathies: updates on causes,
mechanisms and management. Curr Opin Neurol 2013;26:481-488.
4.Alberti P, Rossi E, Cornblath DR, et al. Physician-assessed and patient-reported outcome measures
in chemotherapy-induced sensory peripheral neurotoxicity: two sides of the same coin. Ann Oncol.
2014;25:257-264.
5. Driessen CML, de Kleine-Bolt KME, Vingerhoets AJJM, et al. Assessing the impact of chemotherapyinduced peripheral neurotoxicity on the quality of life of cancer patients. Support Care Cancer.
2012;20:877-881.
6. Grisold W, Cavaletti G, Windebank AJ. Peripheral neuropathies from chemotherapeutics and targeted
agents: diagnosis, treatment, and prevention. Neuro Oncol. 2012;14:iv45-iv54.
7.Smith EML, Pang H, Cirrincione C, et al. Effect of duloxetine on pain, function, and quality of life
among patients with chemotherapy-induced painful peripheral neuropathy: a randomized clinical
trial. JAMA. 2013;309:1359-1367.
8. Glover J, Dibble SL, Dodd MJ, et al. Mood states of oncology outpatients: does pain make a
difference? J Pain Symptom Manage. 1995;10:120-128.
9.Schloss JM, Colosimo M, Airey C, et al. Nutraceuticals and chemotherapy induced peripheral
neuropathy (CIPN): a systematic review. Clin Nutr. 2013;32:888-893.
10. Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacologic management of
neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85:S3-S14.
Conclusion
The patient continued therapy, but bortezomib delivery was switched from IV infusion to
SQ injection. Her pain symptoms fell to tolerable levels on 2 mg tid of methadone such that
she was able to work, and her functional level was further enhanced by participation in an
occupational therapy program.
CIPN can be a disabling complication of chemotherapy. Patient education that encourages
reporting relevant symptoms, chemotherapy dose adjustment, occupational therapy, physical
therapy, and symptomatic therapy using duloxetine and opioids, including methadone, can
often help patients maintain or regain function and minimize pain and disability.
The Hematologist:
To safely prescribe methadone, monitor the QTc. If the QTc is prolonged, correct contributing
metabolic abnormalities or discontinue agents that can prolong the QTc. If the patient requires
concomitant therapy with a CYP3A4 competitor (such as voriconazole), use lower doses of
methadone. See text for other agents that require adjustments of methadone doses. Increase
methadone doses no more than every 72 hours.
ASH News and Reports
11. Rhondali W, Tremellat F, Ledoux M, et al. Methadone rotation for cancer patients with refractory
pain in a palliative care unit: an observational study. J Pall Med 2013;16:1382-1387.
Dr. Abrahm receives royalties from her book, A Physician’s Guide to Pain and Symptom
Management in Cancer Patients, 2nd edition, 2005, from Johns Hopkins University
Press. She is the paid section editor for UpToDate on the topic of pain in palliative care
patients. She also receives expense reimbursement and honoraria from Knowledge to
Practice for her lectures on palliative care.
5
Newly Redesigned ASH Website
(Cont. from page 1)
categorize various pieces of Web content, and we used those findings to develop a more
intuitive navigational scheme.”
meantime, please visit Hematology.org to explore the new design. We encourage you to share
your feedback by emailing webmaster@hematology.org.
Along with the upcoming Blood website redesign, more changes will be introduced
in the coming months, as standalone sites such as the ASH Academy, an eLearning
platform for hematologists, are brought into alignment with the look and feel of the
new website. In addition, both the functionality of the ASH Store and the account
management section of the ASH website will be enhanced throughout 2014. In the
ASH staff will continue to engage in ongoing user testing to refine the website user
experience. ASH members who are interested in being part of this process are encouraged
to email webmaster@hematology.org to sign up for the Website Users Group. Members of
this informal group will be invited to act as beta testers and to provide feedback prior to the
rollout of new website features.
Top 5 Website Changes You Should Know About:
Website Organized Around Most-Accessed Resources –
The site has been reorganized to showcase the content that
is most popular with users. This content includes Blood,
educational resources such as clinical practice guidelines,
and information about ASH’s upcoming meetings, which are
now front and center.
Enhanced Viewing
of The Hematologist
Online – Readers will
now be able to quickly
get to their favorite
sections and view
collections of articles
written by specific
authors.
➔
➔
Improved Search – Not only has ASH invested in a state-of-the-art search engine that
provides far superior results compared with the previous search function, but users are
now able to search across all ASH websites without leaving Hematology.org. In addition,
users will see suggestions for related searches when the item they search for is not found.
Responsive Design –
The new website
design adjusts
automatically for
optimal viewing from
smartphones and
tablet devices.
Consistent Navigation –
Later in 2014, all
auxiliary ASH websites
will have a consistent
navigational structure
for a more unified
experience across sites.
6
The Hematologist:
ASH News and Reports
T H E
H E M A T O L O G I S T
A D V O C A TE
HEADLINES FROM
Washington
Congress Moves Forward with FY 2015 Budget Process
I
n early March, President Obama kicked off the fiscal year (FY) budget and appropriations
process with the release of his FY 2015 budget proposal. While noting that “biomedical
research contributes to improving the health of the American people,” the President’s
proposed budget seeks $30.2 billion for the National Institutes of Health (NIH), a slight
increase over the amount provided for NIH in the final FY 2014 budget passed by Congress
in January. The proposed budget requests small increases in funding for all of the Institutes
of interest to hematology, including NHLBI, NCI, and NIDDK and estimates that this proposed
increase in funding “would support about 650 additional new grants” NIH-wide.
It is important to remember that the President’s nonbinding budget proposal merely sets
forth the Administration’s priorities and is just one step in a lengthy federal budget process.
Announced a month later than expected, and after the House and Senate had already
established FY 2015 spending blueprints, the President’s budget begins a new round of
congressional negotiations on annual spending bills. Obama Administration representatives
have begun to testify before Congress on the President’s proposals, and the House and
Senate Appropriations Committees are in the midst of drafting legislation establishing actual
federal spending levels for FY 2015.
As the FY 2015 budget process continues, lawmakers need to understand the impact that
unpredictable funding and potential funding cuts will have on research programs, and they
should be encouraged to acknowledge the value of biomedical research by maintaining the
nation’s investment in NIH. Visit the ASH Advocacy Center (www.hematology.org/Advocacy)
to read the latest news on NIH funding and to send a message in support of research funding
to your elected officials.
ASH Committee on Government Affairs Takes to Capitol Hill
to Discuss Research Funding
I
n April, while Congress was beginning the FY 2015 budget process in earnest, the ASH
Committee on Government Affairs conducted a Hill Day to discuss with congressional
offices the importance of biomedical research and the need to protect NIH from funding cuts.
These meetings with Congress are an important component of ASH’s advocacy efforts,
providing an opportunity for Members of Congress and their staff to gain insight into issues
of concern to hematologists. However, the Society needs the help of all members to bring
issues important to the future of hematology to the attention of the U.S. Congress and other
governmental agencies.
ASH strongly encourages members to let the Government Relations, Practice, and Scientific
Affairs staff know when you are in Washington, DC, and available to meet with your
congressional delegation. ASH staff can assist by arranging appointments so that your voice
is heard in the halls of Congress. You can also participate in the Society’s advocacy efforts
by visiting the ASH Advocacy Center and by joining the ASH Grassroots Network. Contact
ASH Legislative Advocacy Manager Tracy Roades at troades@hematology.org, or visit www.
hematology.org/Advocacy for additional information on ASH’s advocacy efforts.
ASH Provides Hematologists with Resources to Prepare for
ICD-10 Conversion
O
n October 1, 2015, all health-care business transactions in the United States must convert
from the use of the ninth version of the International Classification of Disease (ICD-9) to
the 10th version (ICD-10). This change entails a complete restructuring of the diagnosis codes
used by hematologists every day. The transition will take place on a single day, so there will
not be any time to try the new diagnosis codes. ASH will be helping members to prepare for
this transition, primarily by giving examples of the changes in hematology diagnosis coding.
Twice a month, a new disease category will be released, comparing the ICD-10 codes with
the ICD-9 codes. This review will provide clinicians with real examples so that they can
understand the effect of the changes on their individual practices. Visit www.hematology.
org/ICD10 to learn more about the ASH resources. If you have any questions about the
implementation of ICD-10 or ASH’s resources, please contact Brian Whitman, ASH’s Senior
Manager for Policy and Practice, at bwhitman@hematology.org or 202-776-0544.
General Accountability Office Releases Report on Drug
Shortages
I
n February, the General Accountability Office (GAO) issued a report titled, “Drug Shortages:
Public Health Threat Continues, Despite Efforts to Help Ensure Product Availability,” which
was called for in the Food and Drug Administration Safety and Innovation Act (FDASIA) of
2012. The report points to the combination of production lapses due to quality concerns
and constrained manufacturing capacity as being the main cause of the large number of
drug shortages experienced by the hematology community over the last several years.
Encouragingly, the report states that the FDA has made progress over the past two years
in preventing shortages by improving its recognition of and responsiveness to impending
supply chain disruptions. GAO recommends that FDA further strengthen internal controls
over data gathering that can alert the agency to a potential drug shortage and conduct
periodic analyses to systematically assess drug shortage information so as to proactively
identify drug shortage risk factors. Visit ASH’s drug shortage information page (www.
hematology.org/DrugShortages) to access information about current hematologic drug
shortages and to learn about ASH’s advocacy efforts and resources for physicians dealing
with shortages.
Update on the 2013 ASH Choosing Wisely Initiative
Lisa K. Hicks, MD, MSc
Staff Hematologist, St. Michael’s Hospital; Assistant Professor, University of Toronto; Chair of the Choosing Wisely Task Force
Choosing Wisely is an initiative led by
the ABIM Foundation in partnership with
professional societies across the country
(www.choosingwisely.org). This medical
stewardship campaign aims to encourage
physicians and patients to question the necessity of
common medical tests and treatments. ASH released its
first Choosing Wisely list at the ASH annual meeting in
December 2013, and the full list and methodology that
was used to develop the recommendations are available
at www.hematology.org/choosingwisely. In brief, the ASH
Choosing Wisely campaign suggests the following: 1) use
the minimum number of red blood cell transfusion units
to treat symptoms of anemia or to return a patient to a
safe hemoglobin range (7 to 8 g/dl in stable, non-cardiac
inpatients); 2) do not perform thrombophilia testing in
patients with a provoked venous thromboembolic event
(VTE); 3) do not use inferior vena cava (IVC) filters in the
routine management of patients with a VTE; 4) do not use
plasma to reverse the activity of vitamin K antagonists in
non-emergency situations; and 5) limit CT surveillance
for aggressive lymphoma in asymptomatic patients in
complete remission.
The Hematologist:
ASH News and Reports
After the release of the ASH Choosing Wisely List, the ASH
Choosing Wisely Task Force was inundated with feedback
from ASH members. The vast majority of feedback was
positive and two major themes emerged. First, many
members told us they want tools that will aid them in
sharing the ASH Choosing Wisely message with their home
institutions through teaching and continuing education
sessions. In an effort to meet this request, ASH has
developed a public-access Choosing Wisely slide deck. The
slide deck summarizes the list, identifies the underlying
evidence, and describes the methodology used to generate
each of the ASH Choosing Wisely recommendations. The
slide deck is available at www.hematology.org/choosingwisely.
We encourage all members to use it, and pass it on. ASH is
also developing a Choosing Wisely pocket guide that will be
available on the same Web page.
In addition to requests for tools to help disseminate the
Choosing Wisely message, the Task Force received numerous
emails suggesting that ASH produce a second Choosing
Wisely list. In collaboration with the ABIM Foundation, ASH
has already started working on a second list. Similar to the
first ASH list, the second will be evidence-based and will
prioritize tests and treatments that have limited benefit but
a recognized risk of harm; the Task Force is aiming to release
the second list at the annual meeting in December.
The Choosing Wisely Campaign has a formal partnership
with Consumer Reports and other consumer groups to both
facilitate outreach to patients and direct dissemination to
consumers. ASH has been working with Consumer Reports
to produce an article geared toward patients, focusing on
ASH’s recommendation to avoid routine use of IVC filters.
We anticipate that this resource will be available in mid 2014.
It will be posted on both the ASH Choosing Wisely landing
page, (www.hematology.org/choosingwisely) and at www.
consumerreports.org.
The future challenges for the ASH Choosing Wisely Task
Force are effective implementation and measurement of
outcomes of the recommendations. How can we encourage
the implementation of Choosing Wisely recommendations, and
how can we determine if Choosing Wisely recommendations
are leading to beneficial changes in patient care? These two
related objectives are likely to be the most exacting aspects of
this project. As yet, we on the ASH Choosing Wisely Task Force
don’t have the answers to these questions, but we look forward
to updating ASH membership as we tackle these issues.
7
Time to Retire the Old IMiD Mechanism of Action Slide
Lu G, Middleton RE, Sun H, et al. The myeloma drug lenalidomide promotes cereblon-dependent destruction of Ikaros proteins. Science. 2014;343:305-309.
Krönke J, Udeshi ND, Narla A, et al. Lenalidomide causes selective degradation of IKZF1 and IKZF3 in multiple myeloma cells. Science. 2014;343:301-305.
[Editor’s note: Data published in this paper were presented in abstract form by Dr. Krönke at the Late-Breaking Abstract Session during the 2013 ASH annual meeting in New Orleans.]
T
he publication of thalidomide’s remarkable and unanticipated anti-myeloma activity in
Dr. Lu and colleagues showed the importance of modulating expression of IKZF1 and
19991 heralded the anti-cancer successes of its more potent analogs, lenalidomide
IKZF3 in cell lines, demonstrating that cytotoxicity was observed only in cells in which
and pomalidomide, over this past decade. The reemergence of these therapeutics,
IKFZ1 and IKFZ3 expression was inhibited by lenalidomide. Additionally, both groups
known as immunomodulatory drugs (IMiDs), as effective treatment for myeloma
demonstrate that knockdown of either of these two targets is sufficient to induce
and other hematologic malignancies is a bookend to thalidomide’s tragic beginnings, which
cytotoxicity. Notably, Dr. Lu and colleagues observed resistance to lenalidomide-induced
are inexorably linked to phocomelic infants born to women who took the drug to mitigate
cytotoxicity in a number of myeloma cell lines. This unresponsiveness appears to be the
emesis gravidarum. How thalidomide’s teratogenicity interdigitates with its biologic activity
result of low-level expression of cereblon by the resistant cells, supporting the concept
in various malignancies has been a focus of intense
that the cytotoxic effects of lenalidomide are
investigation for more than 20 years. Early illustrations
cereblon-dependent through its action on
Figure 1
Host Microenvironment
depicting the mechanism of action of thalidomide
expression of IKFZ1 and IKZF3 (Figure 2).
IL-6
and lenalidomide highlighted autocrine and paracrine
IGF-1
NF-kB
VEGF
interactions between myeloma cells and stromal cells
A number of other purported mechanisms
SDF-1a
of the surrounding marrow microenvironment. An array
for lenalidomide’s activity in multiple
Inhibition of
bFGF
VCAM-1
MM cell adhesion
of imaginative artistic techniques were used to propose
myeloma have been reported, including
ICAM-1
Inhibition
to BMSC
TNGa
D of cytokine
mechanisms of action that involve anti-angiogenic and
down-regulation of expression of interferon
VEGF
C
immunomodulatory pathways, induction of oxidative
regulatory factor 4 (IRF4) and up-regulation
circuits
TGF-b
stress, and modulation of cytokines, including downof expression of interleukin-2 (IL-2). The
regulation of tumor necrosis factor-α and up-regulation
authors of both papers tied the decrease in
Thal/ImiDs
of interleukin-2, which stimulates T-cell production
IRF4 to the decrease of IKZF1 and IKZF3
Inhibition of
(Figure 1).
induced by lenalidomide, while Dr. Krönke et
BFGF
angiogenesis in
al. demonstrated a marked decrease in IKZF1
VEGF
BM milieu
The first major breakthrough in understanding the
and IKZF3 protein levels in T cells treated
B
mechanism of action of thalidomide and its derivatives
with lenalidomide that was accompanied by a
IL-2, IFNγ
Enhanced host
occurred when thalidomide was shown to bind to
coincident increase in IL-2 expression. Based
immune response
cereblon, a critical component of an E3 ubiquitin ligase
on these observations, it appears that these
Apoptosis
E
complex (Figure 2).2 This report tied the teratogenic
previously reported effects of lenalidomide
(growth arrest)
effects of thalidomide to inhibition of ubiquitination
(IRF4 down-regulation and IL-2 up-regulation)
T cells
MM cell
and toxic accumulation of proteins that led to cell
are downstream effects of a lenalidomideA
death. In the current reports published in Science,
induced decrease in IKZF1 and IKZF3
Reprinted with permission © 2014 American Society of Clinical Oncology. All rights reserved.
two independent groups have identified targets of
(Figure 2).
Richardson, P et al: Immunomodulatory analogs of thalidomide: an emerging new therapy in
lenalidomide that account for its therapeutic effect
myeloma. J Clin Oncol. Vol. 22 (16), 2004:3212-3214.
in multiple myeloma. Dr. Gang Lu and colleagues
Selective inhibition of transcription factors,
from the laboratory of Dr. William Kaelin, Dana-Farber
molecules otherwise considered undruggable,
Cancer Institute, Boston, MA, and Dr. Jan Krönke and
represents a novel therapeutic paradigm that
Figure 2
colleagues from the laboratory of Dr. Benjamin Ebert,
has emerged from the story of the relationship
Brigham and Women’s Hospital, Boston, MA, report
between IMiDs, cereblon, and IKZF1/IKZF3.
that treatment with lenalidomide, and other agents in
Data derived from these studies also provide
this class, through interaction with cereblon, do not
a foundation for exploiting these interactions
inhibit, but rather selectively enhance the ubiquitination
to design new therapeutics and to develop
and degradation of Ikaros (IKZF1) and Aiolos (IKZF3),
strategies for overcoming resistance to IMiDs.
two members of the Ikaros family of zinc finger
However, important issues remain unexplained.
transcription factors important in B-cell development.
The finding that the activity of IMiDs relies on
This finding was confirmed through two orthogonal
targeting transcription factors for proteasomal
screening approaches.
degradation seems incongruous with the highly
effective clinical response observed when IMiDs
In the work by Dr. Lu et al., 15,483 different genes were
are combined with proteasomal inhibitors in the
cloned into plasmids containing both firefly and renilla
treatment of patients with myeloma. This paradox,
luciferase and transfected into mammalian cells in order
and the contrasting roles of Ikaros transcription
to identify genes whose expression was affected by
factors in different disease contexts (e.g., as tumor
lenalidomide. By comparing the signal from these two
suppressors in acute lymphocytic leukemia, and
luciferases, the investigators were able to detect which
as anti-neoplastic targets in myeloma), require
of the 15,483 genes were transcribed into proteins
better understanding. Further, while several
and how levels of these proteins were affected by
mechanisms of action have been proposed to
lenalidomide. Expression of both IKZF1 and IKZF3
account for the therapeutic activity of lenalidomide
decreased in the presence of lenalidomide. These
in the treatment of del (5q) MDS, it is unclear
findings were subsequently validated in two myeloma
whether targeted ubiquitination and destruction of
cell lines, MM1S and L363.
specific transcription factors underlies the efficacy
of lenalidomide in this disease.
Using a different approach, Dr. Krönke et al. analyzed
the proteome and ubiquitinome of MM1S cells after
1. Singhal S, Mehta J, Desikan R, et al. Antitumor
treatment with lenalidomide. By using stable isotope
activity of thalidomide in refractory multiple
Immune modulators and myleoma. The small-molecule drugs thalidomide,
labeling of amino acids in cell culture (SILAC) and
myeloma. New Engl J Med. 1999;341:1565lenalidomide, and pomalidomide bind to the protein cereblon (CRBN), which
mass spectroscopy, the authors identified a significant
1571.
activates the enzymatic activity of the CRBN E3 ubiquitin ligase complex.
lenalidomide-induced decrease in both IKZF1 and
The transcription factors Ikaros (IKZF1) and Aiolos (IKZF3) are modified with
2. Ito T, Ando H, Suzuki T, et al. Identification of
IKZF3. The authors then went on to show that treatment
ubiquitin (Ub) molecules, targeting them for proteolysis. This alters the function
a primary target of thalidomide teratogenicity.
with lenalidomide produced a decrease in protein (but
of T cells and B cells, with a toxic outcome for multiple myeloma cells.
Science. 2010; 327:1345-1350.
not mRNA) levels of IKZF1 and IKZF3 in cells lines and
From Stewart KA. How thalidomide works against cancer. Science. 2014;343:256-257.
in primary patient samples.
Reprinted with permission from AAAS.
David Kurtz, MD, and Jason Gotlib, MD, MS
Dr. Kurtz and Dr. Gotlib indicated no relevant conflicts of interest.
8
The Hematologist:
ASH News and Reports
Unlocking the Mysteries of AITL
Odejide O, Weigert O, Lane AA, et al. A targeted mutational landscape of angioimmunoblastic T cell lymphoma. Blood. 2014;123:1293-1296.
T
hough angioimmunoblastic T-cell lymphoma (AITL) is a rare disease, it is one of
the more common subtypes of peripheral T-cell lymphoma in the Western world.
Patients typically present with advanced-stage disease and systemic symptoms, and
associated autoimmune manifestations of the disease are common. Histologically,
AITL is characterized by a proliferation of malignant T cells in a mixed background of
polyclonal plasma cells, eosinophils, histiocytes, and B cells, often harboring the EpsteinBarr virus (EBV), in an expanded network of follicular dendritic cells with increased numbers
of high endothelial venules. The pathogenesis of the disease is poorly understood and
recurrent genetic abnormalities have not been systematically characterized. Using targeted
exon capture and next-generation sequencing, Dr. Oreofe Odejide and colleagues in the
laboratory of Dr. David Weinstock at Dana-Farber Cancer Institute in Boston examined a
panel of 219 genes that were identified as mutated in other hematologic malignancies and
correlated the findings with demographic and clinical data in 85 cases of AITL (Figure).
AITL_ID
TET2
DNMT3A
IDH2
EP300
TP53
PCLO
STAT3
ARID1B
APC
DST
CREBBP
JAK2
Age
IPI
ECOG_PS
B_Symptoms
LDH_Elevation
1. Yoo HY, Sung MK, Lee SH, et al. A recurrent inactivating mutation in RHOA
GTPase in angioimmunoblastic T cell lymphoma. Nat Genet. 2014. Epub ahead of
print.
2. Sakata-Yanagimoto M, Enami T, Yoshida K, et al. Somatic RHOA mutation in
angioimmunoblastic T cell lymphoma. Nat Genet. 2014;46:171-175.
1
80
94
98
105
112
117
118
4
20
22
28
36
65
68
69
70
74
76
78
81
83
84
91
92
93
104
111
59
66
87
89
97
99
103
5
7
19
21
33
35
37
39
41
42
52
53
55
56
60
61
67
72
73
77
79
82
85
95
102
106
107
113
115
116
101
109
11
23
26
27
34
38
40
43
51
57
58
88
90
96
100
108
110
114
The median overall survival for patients was 18 months and was significantly inferior in
patients over the age of 70. Mutations were identified in the coding regions of 80 genes, 34
of which were altered in two or more cases. The genetic changes did not differ according to
the presence of EBV. Mutations in TET2 were present in 65 patients (76%), and 43 of 65
harbored two or three mutations in that gene. Twenty-eight patients (33%) had alterations
in DNMT3A, all of which were seen in the presence of mutant TET2, and 17 patients
(20%) had changes in IDH2, of which 15 also harbored TET2 mutations (Figure). Notably,
alterations in TET2 and DNMT3A, which function as epigenetic modifiers of DNA, and in
IDH2, a mitochondrial enzyme that when mutated produces the presumed oncometabolite
2-hydroxygluterate, are commonly found in myeloid neoplasms, and in contrast to many
other lymphoid malignancies, alterations in TP53 were identified in only four cases. Given
recent evidence suggesting that mutations in TET2 or DNMT3A may be derived from CD34+
progenitor cells, the investigators examined cellular subsets from a peripheral blood stem
cell collection from a patient with AITL in remission whose tumor cells had been shown to
harbor a TET2 mutation. That mutation was identified only in the lineage-negative CD34-/
CD38+ fraction of cells and not in the patient’s CD34+ positive cells or in cells with an
immunophenotype similar to that of the patient’s AITL cells. The authors used the same
experimental design to characterize the origin of the mutant cells in a patient with histology
that overlapped AITL and peripheral T-cell lymphoma. In contrast to the prior case in which
the mutation arose in a lineage-negative subpopulation, mutations in this case were acquired
within lineage-committed progenitors. Additional investigation is needed to understand the
origins of AITL.
The prognosis of AITL is poor. The optimal management of the disease has not been
well defined, and outcomes following anthracycline-based chemotherapy are dismal.
Although a small minority of patients will achieve long-term disease control following
stem cell transplantation, the vast majority of patients die of progressive disease. The
work of Dr. Odejide and colleagues, identifying recurrent and overlapping mutations
in TET2, DNMT3A, and IDH2, as well as recent reports demonstrating frequent
alternations in RHOA, a small GTPase that regulates diverse biologic processes,1,2
raise the exciting possibility of novel therapeutic approaches in this disease. Studying
drugs that work through epigenetic control over transcription, as well as investigating
the efficacy of inhibitors of IDH2, may provide critically needed advances in the
management of AITL.
Key
Age < 70 yrs
Age >= 70 yrs
IPI 1-2
IPI 3-5
ECOG PS 0-1
ECOG PS 2-3
no B Symptoms
B Symptoms
No LDH Elevation
LDH Elevation
Unknown
Distribution of mutations in 85 cases of AITL. Common mutations and demographic and clinical factors across the cohort are shown. Each column represents a single patient. IPI = International
Prognostic Index; ECOG PS = European Cooperative Oncology Group Performance Status.
From Odejide O, Weigert O, Lane AA, et al. A targeted mutational landscape of angioimmunoblastic T cell lymphoma. Blood. 2014;123:1293-1296.
Ann LaCasce, MD, MSc
Dr. LaCasce indicated no relevant conflicts of interest.
The Hematologist:
ASH News and Reports
9
The Fate of Hematopoietic Nuclei: Major Roles for Lamins Before
and After Marrow Release
JAK-STAT Signaling Goes Bad in
Primary Mediastinal Lymphoma
Shin J, Spinler KR, Swift J, et al. Lamins regulate cell trafficking and lineage maturation of adult human
hematopoietic cells. Proc Natl Acad Sci USA. 2013;110:18892-18897.
Gunawardana J, Chan FC, Telenius A, et al. Nat Genet.
2014;46:329-335.
M
arrow hematopoietic cells comprise a semi-solid tissue that differentiates into various mature cell types
that then populate the peripheral blood, a fluid tissue. The transition from marrow to blood requires
that the mature blood cells acquire viscoelastic properties that allow them to pass through apertures
as small as three microns as they traverse capillaries and narrow fenestrations in the marrow vascular
endothelium, in the splenic red pulp, and in lymph nodes. Now, in an elegant series of experiments, Dr. Jae-Won Shin
and colleagues in Dr. Dennis Discher’s laboratory at the University of Pennsylvania demonstrate that, depending upon
hematopoietic lineage, expression of nuclear lamins play differing roles in determining both the fate of hematopoietic
progenitor cells and the viscoelastic properties of mature nucleated blood cells.
The two most common A-type lamins, lamin-A and lamin-C, are alternatively spliced products of one gene, while
the two B-type lamins, B1 and B2, are products of separate genes. The lamin proteins form a mesh-like network,
the nuclear lamina, which is located between and interacting with the inner membrane of the nuclear envelope and
the peripheral heterochromatin of the nucleus.1 Nuclear lamins are also associated with nuclear scaffold proteins
such as actin, with chromatin modifying proteins, and with transcription factors.1 These interactions can influence
gene expression, nuclear shape, and nuclear deformability. Mutant A-type lamins are associated with myopathies,
neuropathies, and progeria. In murine models, germ-line mutations in B-type lamins result in death early in
embryogenesis, while mutant membrane receptors for B-type lamins are associated with progressive lymphopenia. 2
In humans, mutations in B-type lamin receptors cause the hyposegmentation of neutrophils that characterizes the
Pelger–Huet anomaly.3
Dr. Shin and colleagues used mass spectrometry-calibrated intracellular flow cytometry to determine amounts and
ratios of A-type and B-type lamins in normal human marrow and in nucleated blood cells. Using data from such
analyses, the investigators developed a method for distinguishing early-stage hematopoietic cells from their mature
progeny by plotting the content of A-type and B-type lamins versus the ratio of A-type:B-type lamins (Figure). In other
experiments, they perturbed expression of lamins in hematopoietic progenitors using specific interfering RNAs or
retinoic acid, which inhibits type-A lamin expression. They also tested nuclear deformability and chemotactic factorinduced cellular migration through three micron pores to simulate transit across capillary endothelium.
Megakaryocytes contained the most total lamins, which increased with increasing ploidy, whereas the erythroid
cells had the highest A-type:B-type lamin ratio, which increased with differentiation. The high lamin content of
megakaryocytes and the nuclear rigidity associated with the high lamin A:lamin B ratio in erythroblasts make these
marrow cell types least likely to migrate through the marrow vascular endothelium as they are the lineages that
produce anucleate blood cells through proplatelet formation in the case of megakaryocytes and undergo nuclear
extrusion prior to entering the circulation in the case of erythroblasts. Altered expression of A-type and B-type lamins
also affected the differentiation of myeloid progenitor cells such that increased lamin-A expression and/or decreased
lamin-B expression enhanced erythroid progenitor development but decreased granulocyte-monocyte progenitor
growth. Lamin-A overexpression was also associated
with increased megakaryocytic differentiation, while
Figure
decreased lamin-A expression inhibited erythroid progenitor
differentiation and enhanced granulocyte-monocyte
progenitor development. With decreased lamin-A:lamin-B
ratios compared with erythroid nuclei and decreased lamin
amounts compared with megakaryocytic nuclei, lymphocytic
and myeloid nuclei had greater nuclear deformability,
consistent with circulation of the mature nucleated cells
in blood. During differentiation, the lamin-A:lamin-B ratio
increased in granulocytic-monocytic cells, but their total
lamin content decreased. Mature granulocytes-monocytes as
well as lymphocytes readily migrated through three micron
pores and softening their nuclei by decreasing the lamin-A to
lamin-B ratio increased the migration rate.
Log-log plot of intensity of nuclear lamins A + B
versus ratio of lamin-A:lamin-B in human bone
marrow and peripheral blood cells based on
mean fluorescence intensity of A-type lamins and
B-type lamins as quantified by mass spectrometrycalibrated intracellular flow cytometry. The dashed
line demarcates cells residing in bone marrow
(BM) in upper gray area and cells circulating
in the peripheral blood (PB) in lower pink area.
Abbreviations: CD34+,CD38-, cell population enriched
in hematopoietic stem cells; CD34+,CD38+, cell
population enriched in multipotent hematopoietic
progenitors with limited proliferative capacity; MSC,
mesenchymal stromal cells; MkP, megakaryocyte
progenitors; MK, megakaryocytes; ProEry,
proerythroblasts; lateEry, late-stage erythroblasts;
BM-G and BM-M, bone marrow granulocytic
and monocytic cells; PB GM, peripheral blood
granulocytes and monocytes; T, T-lymphocytes; B,
B-lymphocytes; RBC, erythrocytes; Plt, platelets.
Shin J et al. Lamins regulate cell trafficking and lineage
maturation of adult human hematopoietic cells. PNAS.
2013;110:18893.
10
Dr. Shin and colleagues demonstrated a role for nuclear
lamins both in differentiation of marrow hematopoietic cells
and in the nuclear flexibility required by mature nucleated
blood cells to enter and remain in circulation. These
results suggest that increased nuclear rigidity contributes
both to the loss of circulating lymphocytes in lamin-B
receptor-deficient mice2 and to the impaired chemotactic
migration associated with the Pelger–Huet anomaly that is
a consequence of mutant lamin B receptors in humans.4
The findings also suggest mechanisms that could account
for the leukostasis observed in acute leukemias with high
numbers of circulating blasts. The hypothesis in this case is
that nuclei of the leukemic blast are more rigid than nuclei
of normal mature granulocytic-monocyctic cells. Further,
the high nuclear rigidity of circulating erythroblasts may
contribute to the development of microvascular occlusions
that complicate sickle cell anemia.
1. Zwerger M, Medalia O. Histochem Cell Biol.
2013;140:3-12.
2. Verhagen AM, de Graaf CA, Baldwin TM, et al. J
Immunol. 2012;188:122-34.
P
rimary mediastinal B-cell lymphoma (PMBL) is
distinct from other diffuse large B-cell types in its
epidemiology, biology, and clinical course. Arising
in the thymus, it is thought to originate in medullary
B cells. It is characterized by a relatively increased incidence
among young women, early local invasion, and a generally
favorable prognosis after chemoimmunotherapy, often
followed by consolidation radiotherapy. Failure of the initial
therapy is uncommon, but it is often rapid when it does
occur and extremely difficult to salvage. Gene-expression
profiling has demonstrated strong similarities to nodular
sclerosing Hodgkin lymphoma (HL), although no common
underlying mutational events have previously been identified
in more than a small number of cases. The pathogenesis
of PMBL remains unclear, and for this reason, there is
continuing investigation of its molecular characteristics. Led
by Dr. Randy D. Gascoyne and Dr. Christian Steidl at the
British Columbia Cancer Agency in Vancouver, Canada, this
study has used whole-genome sequencing as the starting
point for the identification of a previously unsuspected
mutation target that is altered in a significant number of
cases of both PMBL and HL.
Initial whole-genome sequencing of material from two cases
of PMBL, to a read depth of 60x and 52x, respectively,
identified mutations in two negative regulators of the
JAK-STAT signaling pathway, SOCS1 and PTPN1, in both
cases. Subsequent sequencing of the whole transcriptome
in another five cases and three PMBL cell lines revealed a
high frequency of alterations in several regulators of the JAKSTAT pathway, with SOCS1 and PTPN1 being the most
commonly affected. Next, the authors sequenced all 10
exons of PTPN1 in another 70 cases of PMBL and found a
total of 18 variants in 17 out of 77 cases and an additional
two variants in one of the three cell lines. Due to the
possible overlapping biology with HL, they also sequenced
PTPN1 in 30 cases and nine cell lines, finding another 12
variants among these. In clinical cases, the mutation rate
of PTPN1 was 22 percent in PMBL and 20 percent in HL.
Analysis of the PTP1B protein by immunohistochemistry
suggested that the mutations generally resulted in reduced
or completely absent expression, depending on the exact
location and type of sequence variant.
Investigating the functional consequences of these
mutations showed that they impaired the phosphatase
function of PTP1B, with higher levels of phospho-STAT6
seen in a reporter assay, suggesting constitutive upregulation of the signaling pathway through loss of
inhibition. This hypothesis was supported by knock-down
experiments using short-hairpin RNA to target PTPN1
transcripts in a wild-type HL cell line, which led to increased
phosphorylation in several members of the JAK-STAT
pathway and alterations in the gene-expression profile
showing up-regulation of many STAT targets. Among these
were oncogenes, including BCL-6, MYC, and JUN, and
members of the gene family of ATP-binding cassette (ABC)
transmembrane transporters, which are associated with
resistance to chemotherapy.
The evidence for de-regulation in the JAK-STAT pathway
in PMBL is mounting steadily, and this study shows
another way in which this pathologic process can come
about. It has previously been difficult to identify a common
pathogenetic pathway in PMBL, a disease with highly
variable cytogenetic findings and few common alterations
at the chromosomal level. However, the convergence
of many different abnormalities seems to center on the
JAK-STAT pathway and suggests a novel approach to
treatment. The finding that some of the downstream targets
of the mutations are mediators of drug resistance is also
interesting, and larger studies are now needed to determine
whether PTPN1 mutations convey an increased risk of
primary treatment failure.
3. Gravemann S, Schnipper N, Meyer H, et al. Nucleus.
2010;1:179-89.
4. C
unningham JM, Patnaik MM, Hammerschmidt DE, et al.
Am J Hematol. 2009;84:116-119.
mark koury, md
peter johnson, MD
Dr. Koury indicated no relevant conflicts of interest.
Dr. Johnson indicated no relevant conflicts of interest.
The Hematologist:
ASH News and Reports
Clots, Pumps, and Stockings – Do We Need to
Update the Lower Extremity Dress Code?
Genome Forensics Reveal Origins and the
Mechanism that Drives t(12;21) Childhood B-ALL
Kahn SR, Shapiro S, Wells PS, et al. Lancet. 2013. Epub ahead of print.
Papaemmanuil E, Rapado I, Li Y, et al. RAG-mediated recombination is the
predominant driver of oncogenic rearrangement in ETV6-RUNX1 acute
lymphoblastic leukemia. Nat Genet. 2014;46:116-125.
CLOTS (Clots in Legs Or sTockings after Stroke) Trials Collaboration,
Dennis M, Sandercock P, et al. Lancet. 2013;382:516-524.
E
lastic compression stockings (ECSs) and intermittent pneumatic
compression (IPC) devices have been used in a variety of medical
settings, usually with the goal of restoring or maintaining normal venous
return from the legs. Two recent publications provide important evidence
about the effectiveness of these modalities in two different settings.
The first study was a double-blinded, randomized, controlled trial of graduated
ECSs (30 to 40 mm Hg at the ankle) versus placebo stockings (< 5 mm Hg
compression at the ankle). The trial was designed to test the hypothesis that
ECSs reduce the risk of post-thrombotic syndrome (PTS), a chronic complication
of arm or leg deep-vein thrombosis (DVT). At 24 different North American
centers, the “SOX” investigators enrolled 806 patients (mean age 55 years;
60% men) with a first, proximal leg DVT. Patients were included only if they
1) had a life expectancy > 6 months, 2) did not receive up-front thrombolytic
therapy, and 3) had no contraindication to compression stockings. One year after
randomization, the proportion of patients with PTS (as defined by validated, prespecified scoring systems) was 14 percent in the ECS arm and 13 percent in
the “placebo stockings” arm. Similarly, overall quality of life (as measured by the
SF-36 questionnaire) was not statistically different between the two groups.
The second study was an unblinded, primary, VTE prevention trial, involving 2,876
patients (mean age 75 years, 52% women) from 105 hospitals in the United
Kingdom who were both hospitalized for acute stroke (ischemic or hemorrhagic)
and immobile. Patients in the CLOTS 3 trial were randomly assigned to receive
either bilateral thigh-length IPC (n=1438) or no IPC (n=1438). Individuals with
subarachnoid hemorrhage or leg problems (e.g., skin ulcers or severe edema)
were excluded. Sequential compression was continued in the intervention group
for 30 days or until the patient became independently mobile, was discharged,
declined further use, or had adverse effects. All outcomes were evaluated 30
days after enrollment. The primary outcome (symptomatic or asymptomatic
proximal DVT) occurred less commonly in the group assigned to IPC (9.6% vs.
14%; p=0.001). Symptomatic DVT, a key secondary endpoint, also occurred
less frequently in the intervention group (4.6% vs. 6.3%; p=0.045). The rate of
pulmonary embolism was not statistically different between the groups, but the
numeric trend favored IPC (2.0% vs. 2.4%; p=0.453). IPC increased skin breaks
(3.1% vs 1.4%, p=0.002). A strong, but statistically non-significant, trend toward
lower 30-day mortality favored the IPC group (22% vs. 25%, p=0.057).
Much can be learned from these two important prospective trials. The SOX trial
is probably practice-changing. Until now, VTE experts have recommended that
most patients with proximal leg DVT wear ECSs (30 - 40 mm Hg at the ankles)
because two previous studies1,2 had indicated that ECS use could decrease the
risk of PTS by 50 percent. However, neither of these often cited studies was
blinded. The PTS score, which is the key outcome measure of all these trials,
depends heavily on subjective assessments by both clinicians and patients; thus
the possibility of bias in unblinded comparisons is significant. By using “placebo”
stockings in the comparator arm, the SOX investigators eliminated this kind of
bias and found no benefit from ECSs. More evidence is needed about how we
might reduce the risk of PTS before it occurs. While ECSs may still be worth
trying as a palliative measure in the 10 to 15 percent of patients who develop
moderate to severe PTS, the SOX trial suggests we will need to look beyond
ECSs if we hope to prevent PTS in the first place.
The CLOTS-3 trial is by far the largest and most rigorously designed study that
shows that IPC devices can substantially reduce the risk of VTE in a non-surgical
population of hospitalized patients. Hematologists are often asked to comment
on the risks and benefits of VTE prevention. For some populations (e.g., patients
admitted for acute leukemia or hematopoietic cell transplantation), pharmacologic
modalities not only are costly but also probably carry a non-trivial risk of bleeding.
The CLOTS-3 study, along with a recent meta-analysis,3 provides high-quality
evidence that IPC, when properly applied, can provide substantial protection
against VTE.
A
t times, some of the most fundamental issues in human biology have appeared
inaccessible to direct experimental investigation and have consequently been
relegated to study using model systems. The origin of childhood precursor-B
cell acute lymphocytic leukemia (B-ALL) was included in that group until the
discovery 15 years ago of the prenatal origin of the t(12;21) translocation that generates
the ETV6-RUNX1 (formerly TEL-AML1) fusion gene found in 25 percent of childhood
ALL. In a succession of studies using blood samples from twin pairs, neonatal blood
spots from archived Guthrie cards, and stored cord blood units, investigators showed
that the ETV6-RUNX1 fusion gene developed in utero at an astounding frequency of
one percent.1 Clearly, 1 percent of children do not develop B-ALL. Thus, events acting in
concert with t(12;21) are necessary for leukemogenesis.
During the Ham-Wasserman Lecture at the 2009 ASH annual meeting, Professor Mel
Greaves, who had pioneered work in this area, made a compelling case for incorporating
Darwinian evolutionary principles into a conceptual framework for understanding ALL
leukemogenesis.1 But at the time, the genetic events underlying clonal evolution of
ETV6-RUNX1 expressing cells were speculative. Was the process merely stochastic,
or was it connected mechanistically to t(12;21)? The expanding use of genome-scale
technology over the past several years only added to the confusion by identifying many
seemingly random genetic abnormalities. Now, the current study, led by Prof. Greaves
from the Institute for Cancer Research in London and by Professor Peter Campbell from
the University of Cambridge, Cambridge, UK, reports identification of the mechanism that
underlies clonal expansion in B-ALL expressing ETV6-RUNX1.
In their detailed genetic analyses, Dr. Papaemmanuil and colleagues studied samples
from 57 ETV6-RUNX1 positive ALL patients. Using both exome and low-coverage
whole-genome sequencing, they found an average of 11 somatically acquired structural
variations per case, mostly deletions, with half being highly recurrent. Notably, deletions
mostly affected genes involved in B-cell differentiation. When the authors analyzed the
nucleotide sequence of the structural variants, they observed a striking frequency of
recombination signal sequence (RSS) motifs spanning breakpoint junctions. This finding
suggested that recombination-activating endonucleases (RAG)-1 and -2 were involved
in creation of the structural variants. RAG-1 and -2 are essential components of the
process involved in generating antibody and T-cell receptor diversity through mediation of
VDJ gene recombination. This process involves DNA cleavage and the addition of nontemplate nucleotide bases, which incidentally leaves a genomic fingerprint of RAG activity.
The authors found that 40 percent of the analyzed structural variants had RAG recognition
sequence (RSS) motifs and that 70 percent had inserted non-template sequence. Two
other intriguing findings were the unexpectedly high incidence of structural variants that
localized within promoter and enhancer regions, many of them coinciding with RSS
motifs, and identification of mutations in two previously unrecognized tumor suppressor
genes, ATF7IP and MGA. Interpreted as a whole, the mutational pattern suggests
successive inactivation of genes that would otherwise promote differentiation, stalling
the ETV-RUNX1 expressing cells in a stage of early B-lineage differentiation. Sustained
high RAG activity would then drive clonal evolution, converting a pre-leukemic cell into a
malignant clone.
This rigorous study provides a detailed genetic fingerprint of ETV6-RUNX1 B-ALL,
revealing RAG-mediated deletions as the driver of leukemogenesis. The contribution of
this process to leukemogenesis in other subtypes of ALL will be the subject of future
studies. The hope in understanding leukemic evolution is, of course, the possibility of
translation of that understanding into development of effective treatment. Knowing the
mechanisms at work, and the genomic fingerprints that signal progression to full-blown
disease versus regression, might not only allow for development of targeted therapy, but
perhaps suggest an approach to preemptive intervention. This study is also noteworthy
for identification of novel immunosuppressor genes and for the interwoven use of existing
databases with innovative bioinformatics. The authors’ genome forensics focused on
t(12;21) ALL, but their experimental design strategies may help gain insight into other
pediatric and adult malignancies.
1. Greaves M. Darwin and evolutionary tales in leukemia. Hematology Am Soc Hematol
Educ Program. 2009;2009:3-12.
1. Prandoni P, Lensing AWA, Prins MH, et al. Below-knee elastic compression
stockings to prevent the post-thrombotic syndrome: a randomized, controlled
trial. Ann Intern Med. 2004;141:249-256.
2. Brandjes DPM, Büller HR, Heijboer H, et al. Randomised trial of effect of
compression stockings in patients with symptomatic proximal-vein thrombosis.
Lancet. 1997;349:759-762.
3. Ho KM, Tan JA. Stratified meta-analysis of intermittent pneumatic
compression of the lower limbs to prevent venous thromboembolism in
hospitalized patients. Circulation. 2013;128:1003-1020.
david garcia, MD
Kelsie J. Storm, MD, and Peter Kurre, MD
Dr. Garcia indicated no relevant conflicts of interest.
Dr. Storm and Dr. Kurre indicated no relevant conflicts of interest.
The Hematologist:
ASH News and Reports
11
Lessons From the Liver: Rebalanced
Hemostasis in Immune Thrombocytopenia
Another Reason to Eat More Apples and Whole
Grain: How Inflammation and Hematopoiesis are
Affected by Dietary Fiber and GI Microbes
Kim WH, Park JB, Jung CW, et al. Rebalanced hemostasis in patients
with idiopathic thrombocytopenic purpura. Platelets. 2014. Epub
ahead of print.
Trumpette A, Gollwitzer ES, Yadava K, et al. Gut microbiota metabolism of
dietary fiber influences allergic airway disease and hematopoiesis. Nat Med.
2014;20:159-166.
C
O
ommon laboratory tests of the hemostatic system, such as the
platelet count, activated partial thromboplastin time (aPTT), and
prothrombin time (PT), are often abnormal in patients with liver
disease. If interpreted in isolation, these laboratory abnormalities
appear to indicate a tendency for the patient to bleed. Consequently,
clinicians often transfuse blood products in an attempt to normalize these
laboratory abnormalities, especially before invasive procedures. In recent
years, there has been an increasing understanding of a “rebalancing” of
the hemostatic system in liver disease, whereby hemostatic changes that
promote bleeding can be counterbalanced by hemostatic changes that
promote thrombosis.1 Thus, the platelet count, aPTT, and PT, although
commonly ordered, fail to reflect the globally rebalanced hemostasis of liver
disease, which can lead to unnecessary and possibly harmful treatments.
Indeed, preoperative “correction” of these laboratory abnormalities does not
necessarily reduce bleeding and may actually promote it.
Immune thrombocytopenia (ITP) is another disorder in which a laboratory
abnormality (i.e., the platelet count) does not accurately predict the risk of
bleeding, especially for the individual patient. A singular focus on the platelet
count in ITP can cause a clinician to make the treatment for ITP worse than
the disease itself, especially for childhood ITP. Such unnecessary therapy
and resulting iatrogenic morbidity has been called “medical nemesis.”2 To
decrease medical nemesis in ITP, it is important to begin to understand why
some patients do not bleed despite severe thrombocytopenia and why severe
hemorrhage can occur despite treatment to raise the platelet count. One
possible explanation could be that there are hemostatic differences beyond
the platelet count that predispose to severe bleeding.
Dr. Won Ho Kim and colleagues from Sungkyunkwan University School
of Medicine, Seoul, Republic of Korea, sought evidence for a rebalancing
of hemostasis in ITP, similar to that proposed for liver disease, which
could explain the frequent disconnect between the platelet count and the
occurrence of bleeding. They built upon prior observations that a global
assessment of hemostasis (thromboelastography) might predict bleeding
in ITP3 and that the reported decrease in von Willebrand factor (vWF)
cleaving protease activity in ITP4 could conceivably mitigate the effects of
thrombocytopenia. Dr. Kim and colleagues measured vWF antigen levels
and performed rotational thromboelastography in 20 adults with ITP and
followed them for six months for the occurrence of bleeding. The mean
vWF antigen level was 163 percent (S.D. 80%), and eight patients (40%)
had elevated vWF antigen levels (218%, S.D. 104%) when adjusted for
their blood group type. Thromboelastography parameters were within the
normal range for most patients. A subgroup analysis compared patients
with normal versus elevated vWF. Those with elevated vWF were older
and had longer duration of ITP. The clot formation time (CFT) was shorter,
and the α-angle was larger in those with elevated vWF. The CFT and
α-angle are sensitive to platelet number and function and fibrinogen level
and polymerization. So, higher vWF levels were associated with better
thromboelastography values compared with lower vWF values despite a
similar platelet count. Severe bleeding did not occur in any patient, but four
patients had minor bleeding (3 in the normal vWF group).
The study by Dr. Kim and colleagues was small and many aspects of the
hemostatic system were not measured, but they did document evidence
for “rebalanced hemostasis” in ITP. The main finding was an association
between high vWF antigen levels (in 8/20 patients) and improved
thromboelastographic measurements that might account for a decreased
tendency toward bleeding. Although these results are intriguing, they
cannot yet tenably inform clinical practice. Hopefully, further research can
more completely explain why some patients with ITP bleed and some do
not. Possible explanations include the effects of the autoantibody on platelet
function and a rebalance of hemostasis analogous to that of liver disease.
Whatever the answers, we clearly need better laboratory assessments to
understand the global hemostatic consequences of ITP, which would also
help to reduce medical nemesis in this challenging disease.
To examine the role that dietary fiber plays in modulating AAI, mice were fed a standard
diet containing 4 percent fiber or a low-fiber diet containing 0.3 percent fiber and exposed
to house dust mites. Compared with mice fed the low fiber diet, mice fed the higher-fiber
diet had less lung eosinophil and lymphocyte infiltration, reduced production of cytokines
IL-4, IL-5, IL-13, IL17A, lower levels of IgE, and IgG1 antibodies against the dust mite.
Mice fed a high-fiber diet had less severe AAI in response to methacholine, and lung DCs
were less activated as shown by lower expression of CD40, CD80, PDL-1, and PDL-2.
Complementary studies confirmed these findings in mice that were fed a diet supplemented
with the fermentable fiber pectin (a substance enriched in apples).
Dietary fiber changed the gut and lung microbiota by enhancing bacterial diversity, especially
in the proportion of bacteroidaceae and bifidobacteriaceae, both potent fermenters of
fiber into SFCAs. Both serum and cecal acetate and propionate levels were higher in the
high-fiber fed animals. To show that increased SCFAs mediate the protective effect of fiber
against inflammation, mice were fed acetate or propionate. One day after mice were given
an intranasal house mite challenge, inflammation was similar in control- and propionatefed animals, but after two to four days, eosinophils and cytokine levels in the lung were
reduced in SCFAs-treated mice. This protective effect was dependent on G-protein coupled
receptor 41 (also called free fatty acid receptor 3). There was impaired TH2 differentiation
and decreased dendritic cell (DC) activation in SCFAs-treated mice four days after the
challenge. Other experiments showed that propionate enhanced hematopoiesis, increasing
both common DCs and macrophage DCs in the bone marrow.
This study demonstrates the impact that dietary fermentable fibers have on the intestinal
microbiome, allergic/immune reactions, and bone marrow function. More than 40 years ago,
studies in germ-free or completely decontaminated mice showed that the absence or elimination
of the intestinal microflora prevented the development of delayed-type acute graft-versus-host
disease (GVHD) in mismatched bone marrow transplant models, putatively because of the
experimentally induced absence of gastrointestinal anaerobic bacteria in these animals.2-4
Recently, interest in gut microbes and GVHD has re-emerged.5-7 Antibiotics, diet,
immunosuppressive agents, radiation, and chemotherapy treatment alter the intestinal
microbial milieu and influence the barrier functions of the bowel, and the effects on GVHD
of interventions ranging from gut bacterial decontamination, to protective environments, to
the addition of certain bacteria into the gut are the subjects of ongoing investigation. Prof.
Burkitt’s hypothesis has proven prescient, and continued study of the relationship between
dietary fiber intake, the intestinal microbiome, systemic immuno/inflammatory processes,
and bone marrow function is warranted to further explore the wide spectrum of associated
disease pathophysiology and to identify new therapeutic targets.
1. Burkitt DP, Walker AR, and Painter NS. Effect of dietary fibre on stools and the transittimes, and its role in the causation of disease. Lancet. 1972;2:1409-1412.
2. Jones JM, Wilson R, Bealmear PM. Mortality and gross pathology of secondary disease
in germfree mouse radiation chimeras. Radiat Res. 1971;45;577-588.
1. Lisman T, Porte RJ. Rebalanced hemostasis in patients with
liver disease: evidence and clinical consequences. Blood.
2010;116:878-885.
3. van Bekkum DW, Roodenburg J, Heidt PJ, et al. Mitigation of secondary disease of
allogeneic mouse radiation chimeras by modification of the intestinal microflora. J Natl
Cancer Inst. 1974;52:401-404.
2. Lilleyman J. Medical nemesis and childhood ITP. Br J Haematol.
2003;123:586-589.
4. Beelen DW, Haralambie E, Brandt H, et al. Evidence that sustained growth suppression
of intestinal anaerobic bacteria reduces the risk of acute graft-versus-host disease after
sibling marrow transplantation. Blood.1992;80:2668-2676.
3. Gunduz E, Akay OM, Bal C, et al. Can thrombelastography be a new
tool to assess bleeding risk in patients with idiopathic thrombocytopenic
purpura? Platelets. 2011;22:516-520.
4. Moore JC, Hayward CPM, Warkentin TE, et al. Decreased von
Willebrand factor protease activity associated with thrombocytopenic
disorders. Blood. 2001;98:1842-1846.
12
ne day, sometime in the 1970s, when I was a medical student attending
Medicine Grand Rounds, I remember hearing Professor Denis Burkitt extol the
wonders of dietary fiber, arguing persuasively that, compared with Westerners,
Africans experience a lower incidence of diseases ranging from colon cancer
to hemorrhoids because their diet is relatively fiber-rich. The mechanisms that accounted
for the beneficial effects of high dietary fiber were unclear at the time, and the simple
concept of more rapid stool transit time was invoked to explain the difference. 1 Subsequent
investigation, however, has uncovered an intricate relationship between dietary fiber, the
microbes in our gut, and both intestinal and systemic immuno/inflammatory processes.
Dietary fibers are complex carbohydrates that can be fermented by certain species of
gut bacteria, leading to production of bioactive products including short-chain fatty acids
(SCFAs). SCFAs serve as an energy source for certain bacteria, but they also provide
fuel for intestinal epithelial cells. Available evidence suggests that their effects are exerted
through a surprisingly diverse range of mechanisms including engagement of G-protein
coupled receptors and inhibition of histone deacetylase activity. And SCFAs such as
acetate, propionate, and butyrate are not confined to the gut, being disseminated diffusely
after entering the circulatory system and thereby becoming available to participate in
systemic processes. Now, from Dr. Aurélien Trompette and colleagues at the University of
Lausanne, in Lausanne, Switzerland, we learn how generation of SCFAs by gut microbiota
metabolism both ameliorates allergic airway inflammation (AAI) and drives hematopoiesis.
5. Rezvani AR and Storb RF. Prevention of graft-vs.-host disease. Expert Opin
Pharmacother. 2012;13:1737–1750.
6. Jenq RR, Ubeda C, Taur Y, et al. Regulation of intestinal inflammation by microbiota
following allogeneic bone marrow transplantation. J Exp Med. 2012;209:903-911.
7. Bryson JS, Brandon JA, Jennings CD, et al. A gut feeling about murine syngeneic GVHD.
Chimerism. 2011;2:58-60.
charles T. Quinn, MD, ms
Gregory M. Vercellotti, MD
Dr. Quinn indicated no relevant conflicts of interest.
Dr. Vercellotti indicated no relevant conflicts of interest.
The Hematologist:
ASH News and Reports
Clinical Trials Corner
Not Just for GIST: A New FLT3
Inhibitor Active in Kinase Domain
Mutated AML
Study Title: A Phase II Study of Crenolanib in
Relapsed/Refractory Acute Myeloid Leukemia Patients
With FLT3 Activating Mutations
Clinical Trials.gov Identifier: NCT01657682
Coordinator: Arog Pharmaceuticals LLC
Participating Center: MD Anderson Cancer Center
Accrual Goal: 41
Rationale: AML patients with FLT3 internal tandem
duplications (ITD) have a poor prognosis. Several FLT3
TKIs have been studied in clinical trials, and the results
have been disappointing to date because of lack of efficacy
and treatment-related toxicity (Serve H et al. J Clin Oncol.
2013;31:3110-3118). Crenolanib was initially found to have
activity against the imatinib-resistant PDGFRA-mutant
kinases that drive gastrointestinal stromal tumors (GIST)
(Heinrich MC at al. Clin Cancer Res. 2012;18:4375-4384). In
addition, it is not only a potent inhibitor of FLT-ITD, but it
is also active against FLT3 with gain-of-function mutations
in the tyrosine kinase domain (TKD), including D835H/Y.
Comment: About 30 percent of AML patients have FLT3-
ITD mutations, and another 8 percent have FLT3-TKD
mutations. Studies of sorafenib, one of the early TKIs tried
in AML patients with FLT3-ITD, did not show appreciable
benefit despite early reduction in blasts (Serve H et al.
J Clin Oncol. 2013;31:3110-3118). This ultimate lack of
efficacy was explained by near uniform development
of drug resistance, by 72 days on average, attributed to
emergence of a clone with the D835 mutation in the kinase
domain of FLT3 (Man CH et al. Blood. 2012;119:5133-5143).
Subsequent trials were conducted with midostaurin (Stone
RM et al. Leukemia. 2012;26:2061-2068) and quizartinib
(Cortes JE et al. J Clin Oncol. 2013;31:3681-3687). The
latter is believed to be one of the most active clinical
agents. However, these drugs are not active against
ASH News and Reports
– Pamela S. Becker, MD, PhD
Dr. Becker indicated no relevant conflicts of interest.
Study Design: This is a phase II study of a new Fmslike tyrosine kinase 3 (FLT3) inhibitor (crenolanib) in
relapsed or refractory acute myeloid leukemia (AML). The
study includes two cohorts: one with relapsed/refractory
AML without prior FLT3 tyrosine kinase inhibitor (TKI)
treatment, and one with relapsed/refractory AML with
prior FLT3 TKI treatment. The primary endpoints are
response rate after the first 28-day cycle and at best
response and safety. There is a stopping rule that will be
applied if there is more than a 95 percent chance that the
toxicity rate exceeds 30 percent, with toxicity defined as
a grade 4 or greater non-hematologic adverse event. The
secondary endpoints are duration of clinical response and
progression-free and overall survival. Pharmacodynamic
markers, including phospho-FLT3, will be assayed in blood
and marrow blast samples, and pharmacokinetic studies
will be performed to determine the relationship of drug
concentration to response and toxicity. Patients in each
cohort receive the same dose of crenolanib besylate (200
mg/m2/day) divided into three daily doses, preferably
every eight hours, taken orally at least 30 minutes before
or after a meal. Concurrent hydroxyurea (maximum 5g
total daily dose for 14 days) is permitted during the first 28
days of study therapy.
The Hematologist:
cells with FLT3-TKD activating mutations. A recent
publication showed efficacy of crenolanib in laboratory
studies of drug-resistant FLT-TKD-mutated leukemia cells
(Zimmerman EI et al. Blood. 2013;122:3607-3615). The
current clinical trial will assess the efficacy of crenolanib
in two groups of patients: those without prior treatment
with TKIs and those who developed resistance after TKI
therapy. The two-cohort design should provide data
about whether the activity against FLT3-TKD mutants
observed in pre-clinical studies translates to the clinic and
whether use of the inhibitor in naïve patients prevents
development of drug resistance.
Rivaroxaban for the Treatment of HIT:
Hit or Miss?
Study Title: Rivaroxaban for Treatment of Patients
with Suspected or Confirmed Heparin-Induced
Thrombocytopenia
ClinicalTrials.gov Identifier: NCT01598168
Sponsor and Collaborator: McMaster University
Participating Centers: 7 medical centers in Canada
Accrual Goal: 200
Study Design: This is a prospective, multicenter, singlearm cohort study (Linkins LA et al. J Thromb Thrombolysis.
2014. Epub ahead of print). The target population is adult
patients with an intermediate or high clinical probability
(4T score ≥ 4) of heparin-induced thrombocytopenia
(HIT). Patients with mechanical heart valves, severe renal
insufficiency (CrCl <30 mL/min), or moderate or severe
hepatic disease (Child-Pugh B and C) are excluded. All
enrolled subjects are initially given 15 mg of rivaroxaban
twice daily while awaiting the results of HIT laboratory
testing. If laboratory testing is negative, rivaroxaban
is discontinued. In patients who test positive for HIT,
rivaroxaban is continued for 30 days. The dose is changed
to 20 mg daily after 21 days in patients with thrombosis,
and, in patients without thrombosis, the dose is changed
at the time of platelet count recovery (defined as platelet
count ≥ 150 x 109/L or recovery to platelet count at the
time heparin was initiated). The primary outcome is new
symptomatic venous or arterial thromboembolism at day
30. Secondary endpoints include major bleeding and time
to platelet count recovery. In addition to local testing,
serum from all subjects will be analyzed for platelet
activating antibodies in a central laboratory (McMaster
Platelet Immunology Laboratory) using a serotonin
release assay (SRA).
Rationale: Drugs licensed for the treatment of HIT (e.g.,
argatroban, danaparoid, lepirudin) are associated with
important drawbacks, including parenteral administration,
need for intensive laboratory monitoring, limited
availability (in the case of danaparoid and lepirudin),
high cost, and incomplete efficacy. These agents decrease
thromboembolism by 50 to 65 percent but do not reduce
HIT-associated amputation or mortality. Transitioning
from argatroban to warfarin is challenging because of
the effect of argatroban on the INR and added length of
hospital stay.
Rivaroxaban, a direct inhibitor of free and clot-bound
factor Xa, is a promising agent for the management of
HIT that may overcome some of these limitations. It is
administered orally as a fixed dose, is less costly than
parenteral agents, does not require routine laboratory
monitoring, does not cross-react with HIT antibodies in
vitro (Walenga JM et al. Br J Haematol. 2008;143:92-99),
and has an established efficacy and safety profile in the
management of other thromboembolic disorders.
Comment: There is an urgent need for novel therapeutics
in HIT that improve upon the efficacy, safety, convenience,
and cost-effectiveness of existing options. Whether one
or more of the target-specific oral anticoagulants will
be able to fill this niche is unproven. This study will
provide valuable preliminary information but, due to two
important limitations in its design, will not definitively
address the role of rivaroxaban in the management of HIT.
First, the study lacks a control group against which
rivaroxaban may be compared. Ideally, patients would
have been allocated to receive either rivaroxaban or
an active comparator (e.g., argatroban). However,
randomized controlled trials have proven difficult to
conduct in HIT; only two such trials have been published.
A trial of danaparoid versus dextran 70 was completed
in the 1990s prior to the advent of approved agents
(Chong BH et al. Thromb Haemost. 2001;86:1170-1175).
A more recent trial of desirudin versus argatroban was
terminated early due to poor accrual after only 16 subjects
had enrolled (Boyce SW et al. Am J Ther. 2011;18:1422). Comparisons between the rivaroxaban cohort and
the pivotal single-arm studies that led to approval of
argatroban and lepirudin are unlikely to be meaningful
because of differences in patient population, outcome
assessment, and adjunctive care.
Second, it is likely that the majority of patients enrolled
in the study will not have serologically confirmed HIT.
In a recent meta-analysis, HIT was corroborated using
a specific washed platelet assay (e.g., SRA) in only 23
percent of patients with suspected HIT and a 4T score ≥ 4
(Cuker A et al. Blood. 2012;120:4160-4167). Thus, it can be
anticipated that 50 or fewer of the 200 subjects enrolled
in the study will have “true” serologic HIT. Whether this
number will be sufficient for meaningful assessment
of rivaroxaban for the treatment of HIT remains to be
determined.
The aforementioned limitations notwithstanding,
this study represents an important step forward in
the investigation of HIT. It places renewed focus on a
potentially devastating orphan disease with limited
treatment options and no new FDA-approved therapies
since argatroban received licensure 14 years ago. Despite
lack of a control arm, the quality of evidence obtained
from this study will undoubtedly exceed that derived
from retrospective analyses cited to support off-label
use of fondaparinux and bivalirudin for HIT. If results
are promising, this study should pave the way for an
international, randomized, controlled trial to definitely
address the role of rivaroxaban for treatment of HIT.
– Adam Cuker, MD, MS
Dr. Cuker indicated no relevant conflicts of interest.
13
P r o f i l e s
in
H e m a t o l o g y
Hematology as a Journey
John W. Adamson, MD
Clinical Professor of Medicine, Hematology/Oncology, University of California, San Diego
Awed by the physician who removed my tonsils (probably unnecessarily), I have wanted to be a
doctor since the age of three. Not that there weren’t doubts along the way, as years later as a student
at the University of California, Berkeley, I envisioned the road (medical school, internship, residency)
that I would have to travel to reach that goal. For a time, I considered following my father’s lead, but
he, a high school English teacher, straightened me out. “Don’t be stupid!” he said. “Being a teacher
is fine, but you can teach at whatever you do.” Of course, he was right, and in the end, I had it both
ways, as I became a physician/teacher.
When it came time to apply to medical school in 1958, there
were the usual options for someone growing up in California:
Stanford, the University of California, San Francisco, the
University of Southern California, and the newly minted
University of California, Los Angeles (UCLA). For whatever
reason (likely intuitive), I chose UCLA. This decision led to
my first airplane ride when I moved from Berkeley to Los
Angeles. The experience at UCLA was eye-opening. Most of
the lectures were given by young faculty who were deeply
invested in their own research, so, predictably, part of the
class complained about the emphasis on science and the
others enjoyed the newness of it all.
As for internships, I didn’t apply very widely, and there
wasn’t anything like today’s computerized system that
“matches” applicants with a particular training program.
Fortuitously, I wound up in Seattle at the University
of Washington where I found myself among a group of
remarkable biomedical researchers including Earl Davie,
Clem Finch, and the nephrologist Belding Scribner, who was
pioneering hemodialysis as an approach to treating kidney
failure. Toward the end of my second year of residency
in 1964, I was asked if I would be interested in becoming
a hematology fellow. I don’t know why, but someone had
given my name to Clem, who was head of the Division of
Hematology at the time, and he approached me personally.
After some thought, I accepted the invitation and “shorttracked,” entering fellowship after two years as a resident.
I reasoned that if I didn’t like hematology, I would complete
my third year of internal medicine training and go into
practice.
Fellowship programs were so much less formulaic then. I
spent most of the first two years (1964-1966) in the lab and
fell in love with it. I was assigned to help develop a new
assay for the elusive erythropoietic stimulating factor (i.e.,
erythropoietin or Epo), and I plunged in. We started with
samples from normal subjects and then moved to patient
samples. The bioassay wasn’t sensitive enough to reliably
measure Epo activity in normal serum, so we had to
concentrate urine to detect a signal. These experiments led
to the discovery that Epo levels were consistently low in
patients with polycythemia vera, and we went on to use the
assay to analyze Epo levels in a number of polycythemic
states.
Things were going smoothly until 1967, when it became clear
that I was going to be drafted into the military. Coming to
my support, Clem called friends at the National Institutes of
Health (NIH) who informed him that there was an unexpected
opening in hematology in the Clinical Pathology Department.
I literally flew out that night, interviewed the next day, and,
thankfully, was offered the opportunity to apply for the
position. When I returned to Seattle, I found waiting for me
a draft notice stating that I was to report to the Presidio of
San Francisco on July 5. Now it was a race to see what would
come first: the offer of a commission in the Public Health
Service or July 5 and the Army. I was going somewhere, but
I just didn’t know where. Mercifully, the offer to join the
commissioned corps arrived about a week before July 5, and
I was off to Bethesda, Maryland.
NIH was the center of biomedical research at that time, and a
second postdoctoral experience there was a watershed event
in my career. It was at NIH that I learned the basics of cell
culture and the physical separation of cells, tools that made
14
feasible the study of subpopulations of hematopoietic cells.
And through the team of James Till and Ernie McCulloch
at the Ontario Cancer Institute (OCI) in Toronto, I was
exposed to novel concepts in the new world of experimental
hematology, as Till and McCulloch had made seminal
observations about the nature and function of stem cells
and about clonality and clonal evolution. Ernie was very
supportive, and I had the opportunity to visit the OCI on
several occasions at a time when colony-forming assays
were being developed.
When my time at NIH was up, Bob Petersdorf, chair of
Medicine at Washington, offered me the opportunity to
return, and I joined the faculty in 1969. I now had new tools
to apply to the lines of investigation that had been started
earlier. My work in the lab in Seattle linked two areas:
the clonal nature of the myeloproliferative neoplasms (in
collaboration with Phil Fialkow) and the potential value of
Epo as a therapeutic agent (in collaboration with my close
friend, Joe Eschbach). These two areas, along with ongoing
studies of iron physiology led by Clem, dominated the
next 20 years of my academic life in Seattle. Bev Mitchell
joined the lab early on and became a good friend. It was an
exciting time.
Joe and I had developed a large animal model of renal failure
and convincingly demonstrated that plasma that was rich
in Epo could reverse the accompanying anemia. As a result,
scientists from Amgen, then a small startup company,
contacted us to see if their recombinant human Epo would
work in our animal model. We never got there! Rather, we
quickly initiated the first clinical trials of Epo, in which we
assessed response in transfusion-dependent patients on
dialysis; it was amazing to see something work so well!
To extend our work on clonal disorders, we developed a
model of G-6-PD heterozygosity in the cat – a model that
Jan Abkowitz, then a fellow and currently ASH’s immediate
past president – exploited brilliantly. Ken Kaushansky,
also a fellow at the time, introduced molecular biology to
the division in studies of hematopoietic growth factors,
their receptors, and their biology. Ken’s work in this area
culminated in his cloning and expression of the gene that
encodes thrombopoietin (Tpo), Epo’s little sister.
My years in Seattle were interrupted by another important
event — a year on sabbatical with (now) Sir David Weatherall
at Oxford. The Weatherall lab was studying the regulation
of globin chain synthesis in an attempt to better understand
the pathophysiology of hemoglobinopathies. While I
probably disappointed David in how little I accomplished,
living abroad and watching really good minds in action in a
resource-restricted environment was revelatory. Through
that experience, I made many friends and adopted a view of
the world that I don’t believe I would have had it not been
for the experience of living outside of the United States. I also
came to like football, as it’s defined on the rest of the planet.
In 1989, I accepted a new challenge, moving to New York City
and the New York Blood Center with a goal of expanding
the research programs there. Fortunately, a very talented
husband-and-wife team of scientists, Anna Rita and Giovanni
Migliaccio, accompanied me, and they sustained and grew
the laboratory by encouraging and supporting the work of
visiting fellows and scientists. New York was a challenge, but
very exciting.
In 1998, I was recruited to the Blood Research Institute of
the BloodCenter of Wisconsin in Milwaukee, which Dick
Aster had led for many years. The Institute was home to a
group of extremely bright scientists including Dick, Peter
Newman, Bob Montgomery, and Hardy Weiler. My time at
the BloodCenter provided one of the best experiences of my
life, and with the support of the scientists and the Institute’s
Board, we were able to recruit a number of
outstanding young investigators who have
gone on to success in their own right.
The final move, in 2007, completed the circle,
bringing me back to California and to the
University of California, San Diego (UCSD),
where I rejoined Ken Kaushansky. At that
time, Ken was chair of the Department of
Medicine and (with some irony) my ultimate
boss. The move to UCSD was in support of
my wife’s career, and she now heads the
Center for Hemophilia and Thrombosis here.
With Sandy Shattil’s support, I try to do
what I can to remind people (especially the
fellows) that there is such a thing as benign
hematology and that the study of blood
should be a passion, not a pothole on the
road to board certification.
As I look back, I don’t have enough fingers
and toes to count all the good things that
have happened to me, starting with Clem,
my most influential mentor. Through
hematology, I have had the opportunity to
meet countless people brighter than me and
to work with outstanding fellows and young
scientists both here and abroad. And ASH
became, and remains, an enormous part of
my life.
Hematology has been a marvelous journey,
and I count myself most fortunate to have
been able to make the trip.
The Hematologist:
ASH News and Reports
EDITORS’
CHOICE ››
Thoughts From a
Former Protégé
F e b r u a r y 2 7, 2 0 1 4
Kenneth Kaushansky, MD
Senior Vice President for Health Sciences, Dean School of
Medicine, Stony Brook University
In 1996, Hilary Clinton penned the book It
Takes a Village to Raise a Child, based on an
ancient African parable. I have often hijacked
that title to claim, “It takes a village to raise
a physician-scientist.” While I do believe that
most successful physician-scientists can name
multiple mentors, there is almost always, as
John puts it, a “most important mentor.” Most
scholarly articles on mentorship list at least six
roles a successful mentor fills: teacher, sponsor,
advisor, agent, role model, and confidante. Most
would also agree that the successful mentor
does not have the role of cloning oneself, but
rather, he/she should be an astute enough
listener to help the protégé pursue their own
dreams – a seventh role. There is little doubt
that John Adamson is my most important
mentor, as he was able to fulfill each of these
roles. It is no wonder that he was the 2013
recipient of the ASH Mentor Award.
John taught me how to pen a scientific paper.
When he revised and then handed back to me
my very first scientific manuscript, I noticed
it weighed about twice what it had when I
handed it to him a few days earlier: the weight
difference, of course, being that of the red ink.
“Not bad for an author for whom English is a
second language,” he quipped. But the weight
of the red ink became less and less as time
went on, as I learned not only science from John,
but also how to communicate science. One of
the critical junctures in my career came when I
proudly pronounced that, despite not knowing
which end of the pipette to use, I wanted to
become a hematologic molecular biologist.
John was a terrific sponsor; he made sure I had
ample protected time for research, suggesting
that purifying hematopoietic growth factors
would help achieve my career goals and
introducing me to another mentor, Earl Davie,
who greatly enhanced my scientific toolbox.
John has served as a primary advisor and
academic confidante throughout my career,
epitomizing the principle that mentorship does
not end when the student leaves the lab. John
was also a terrific agent. Shortly after we cloned
human GM-CSF, John was invited to present his
work on erythropoietin at a Gordon Research
Conference (GRC). He suggested to the
meeting organizers that I present in his place. It
was my very first GRC. And John epitomizes the
quintessential role model, constantly exuding
scientific integrity, service to one’s community,
and excellence in clinical care, educational
endeavors, and scholarship.
The Hematologist:
ASH News and Reports
JAK2. These observations suggest that CALR-mutated
essential thrombocythemia is a distinct entity with a
more indolent natural history.
Dr. Bob Löwenberg (Editor-in-Chief) and Dr. Nancy
Berliner (Deputy Editor-in-Chief) have combined efforts
to identify some of the most outstanding Blood articles
that have appeared either in print or online during the
two-month interval between issues of The Hematologist.
The citations are annotated to provide readers both with
a concise description of the thrust of the article and an
explanation of why the paper is particularly important.
The goal is to underscore the remarkable research that is
published in Blood and to highlight the exciting progress
that is being made in the field.
March 13, 2014
Sparkenbaugh EM, Chantrathammachart P, Mickelson
J, et al. Differential contribution of FXa and thrombin to
vascular inflammation in a mouse model of sickle cell
disease. Blood. 2014;123:1747-1756.
Both vascular inflammation and activation of coagulation
contribute to the pathogenesis of sickle cell disease. In this
study, Sparkenbaugh and colleagues used a mouse model
of sickle cell disease (SCD) to demonstrate that inhibition
of Factor Xa with rivaroxaban and inhibition of thrombin
with dabigatran decrease lung neutrophil infiltration, and
that rivaroxaban, but not dabigatran, decreases IL-6 levels.
These observations could translate into development
of novel therapies aimed at ameliorating the clinical
manifestations of SCD. Hunter ZR, Xu L, Yang G, et al. The genomic landscape
of Waldenstöm’s macroglobulinemia is characterized by
highly recurring MYD88 and WHIM-like CXCR4 mutations,
and small somatic deletions associated with B-cell
lymphomagenesis. Blood. 2014;123:1637-1646.
Hunter and colleagues report a major advance in
our understanding of the genetic underpinnings of
Waldenström’s macroglobulinemia (WM). They performed
whole-genome sequencing on samples from 30 WM
patients and subsequently validated findings of copy
number alterations and somatic mutations in CXCR4
in expansion cohorts of 147 and 30 WM patients. The
most striking findings were the identification of somatic
mutations in MYD88 in 90 percent of patients (including
the L256P activating mutation), in CXCR4 in 27 percent,
and in ARID1A in 17 percent. Notably, the somatic CXCR4
mutations identified in this study included those observed
in patients with the warts, hyogammaglobulinemia,
infection and myelokathexis (WHIM) syndrome that had
previously been reported only in the germ line. These
findings, in addition to other recurring mutations identified
in this study, contribute to a more complete understanding
of the pathogenesis of WM. March 6, 2014
Rumi E, Pietra D, Ferretti V, et al. JAK2 or CALR mutation
status defines subtypes of essential thrombocythemia
with substantially different clinical course and outcomes.
Blood. 2014;123:1544-1551.
Rotunno G, Mannarelli C, Guglielmelli P, et al. Impact
of calreticulin mutations on clinical and hematological
phenotype and outcome in essential thrombocythemia.
Blood. 2014;123:1552-1555.
Recently, recurrent somatic calreticulin (CALR) insertion/
deletion mutations were discovered in the majority of
patients with essential thrombocythemia and primary
myelofibrosis in which neither JAK2 nor MPL was
somatically mutated. In two independent studies, Rumi
et al. and Rotunno et al. demonstrated that essential
thrombocythemia patients with CALR mutations exhibit
lower leukocyte and hemoglobin values, higher platelet
counts, and a lower thrombosis risk as compared with
patients with essential thrombocytosis with mutant
Shim YK, Rachel JM, Ghia P, et al. Monoclonal B-cell
lymphocytosis in healthy blood donors: an unexpectedly
common finding. Blood. 2014;123:1319-1326.
The prevalence of monoclonal B-cell lymphocytosis
(MBL) in the general population ranges from <1 percent
to 18 percent depending upon the detection method
and population tested. Although a precursor to chronic
lymphocytic leukemia, few people with MBL go on
to develop clinically significant disease. In this Blood
article, Shim and colleagues report the surprising
observation that 7.1 percent of healthy blood donors
have MBL. Most patients had “low-count” MBL (< 500
cells/L), but a small number had clinical MBL (> 500
cells/L). Although the risk of engraftment of these
premalignant cells is low, the current findings raise
questions about the need to screen for MBL in donated
blood. At the very least, retrospective study of the
outcomes of transfusion of MBL-containing units is
warranted.
Fe b r uary 20, 2014
Benveniste P, Serra P, Dervovic D, et al. Notch signals
are required for in vitro but not in vivo maintenance
of human hematopoietic stem cells and delay the
appearance of multipotent progenitors. Blood.
2014;123:1167-1177.
In murine model systems, Notch appears to be a pivotal
signaling molecule that promotes the maintenance
of “stemness” and expansion of self-renewing HSCs.
And human CD34+ cells expand in vitro in response to
Notch signals. In the current study, Benveniste and
colleagues address whether Notch directly affects all
hematopoietic stem cells (HSCs) and whether this
role is relevant in vivo. The results clarify essential
effects of Notch signaling on human HSC maintenance
and expansion, and reconcile discrepancies in the
literature about the role of Notch signaling in HSC
homeostasis. Their findings support the concept that
Notch signals maintain human HSCs in vitro that have
hematopoietic-reconstituting capacity in vivo and
delay the appearance of two newly described early
progenitor cells.
Fe b r uary 13, 2014
Aguilar R, Magallon-Tejada A, Achtman AH, et al.
Molecular evidence for the localization of Plasmodium
falciparum immature gametocytes in the bone marrow.
Blood. 2014;123:959-966.
Success in eradicating malaria hinges in part on the
ability to prevent transmission of the parasite from
the infected host back to the mosquito. In this article,
Aguilar and colleagues reveal how complex an issue
that may be. They present the first study based
on quantitative polymerase chain reaction-based
molecular analysis that delineates the characteristics
of bone marrow and peripheral blood reservoirs of the
parasite. They demonstrate that malarial sexual stages
mature in the bone marrow and that hematologic
manifestations (severe anemia and dyserythropoiesis)
correlate with higher prevalence of mature
gametocytes in the marrow. More important perhaps
is the observation that mature, infectious gametocytes
predominate in the peripheral blood, and that many
asymptomatic anemic children harbor unexpectedly
large numbers of circulating gametocytes. Such
studies that define quantitatively and qualitatively the
host-parasite relationship are a critical first step in
developing strategies aimed at eradicating the malaria
reservoir in humans.
15
wha t ’ s
on
t h e
MARK YOUR C ALENDAR
w e b
As technology and the Web have evolved, so too have ASH’s
online offerings. Now you can download ASH apps for your
smartphone or tablet, follow ASH on Twitter (www.twitter.com/
ASH_hematology), find ASH videos on YouTube (www.youtube.
com/user/ASHWebmaster), and visit ASH on Facebook at
www.facebook.com/AmericanSocietyofHematology.
ASH Seeks Volunteers for
Website Users Group
San Francisco, CA, December 6-9
May
1
Scholar Awards letter of intent due
Washington, DC www.hematology.org/awards
2Application deadline for the ASH Visitor Training Program
Washington, DC
www.hematology.org/awards
14-17American Society of Pediatric Hematology/Oncology Annual Meeting
Chicago, IL www.aspho.org
21-24 American Society of Gene & Cell Therapy Annual Meeting
Washington, DC www.asgct.org
29-30Hematology for the Oncologist Seminar
Chicago, IL
www.asco.org
30-American Society of Clinical Oncology Annual Meeting
June 3Chicago, IL As was mentioned in the cover story, a new site design
was launched on April 4, as part of a multi-year effort to
upgrade the Society’s technology platforms. ASH staff will
be engaging in ongoing user testing to refine the website
user experience. ASH members who are interested in being
part of this process are encouraged to email webmaster@
hematology.org to sign up for the Website Users Group.
Members of this informal group will be invited to act as
beta testers and to provide feedback prior to the rollout of
new website features.
www.asco.org
June
1
Application deadline for ASH Bridge Grant
Washington, DC www.hematology.org/awards
5ASH annual meeting abstract submission site opens
San Francisco, CA
www.hematology.org/meetings
5Scholar Awards application available*
Washington, DC
www.hematology.org/awards
12-1519th Congress of European Hematology Association
Milan, Italy www.ehaweb.org
July
2Nomination deadline for the 2015 ASH Honorific Awards
Washington, DC
www.hematology.org/awards
24Members-only registration and housing opens for 2014 ASH Annual
Meeting and Exposition
San Francisco, CA
www.hematology.org/meetings
August
1
ASH Active and International Membership application deadline
Washington, DC
www.hematology.org/membership
1
Application deadline for Translational Research Training in Hematology
Washington, DC
www.hematology.org/awards
1
Application deadline for Scholar Awards
Read The Hematologist online at
Washington, DC
www.hematology.org/awards
www.hematology.org/thehematologist,
5Deadline to submit abstracts for the ASH annual meeting
and catch up on the latest news in
San Francisco, CA
the field of hematology right on your
10-13ASH Meeting on Lymphoma Biology
desktop, mobile phone, or tablet.
Colorado Springs, CO
www.hematology.org/meetings
www.hematology.org/meetings
*In order to submit an application for the Scholar Awards, you must have submitted a letter of intent by May 1, 2014.
For additional meetings dates, go to www.hematology.org/Meetings/Non-ASH.aspx.