Current Pathway for Pre Operative Assessment for Surgeries Off
advertisement

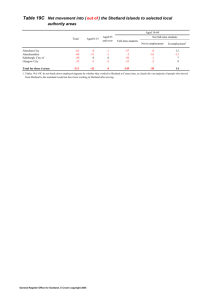
NHS Board NHS Shetland Contact Linda Halcrow Email linda.halcrow@nhs.net Title Current Pathway for Pre-Operative Assessment for Surgeries Off Island (Orthopaedic) Category Whole System Patient Flow Background/ context The NHS Board’s corporate objectives are to provide quality, effective and safe services, delivered in the most appropriate setting for the patient. Several NHS Shetland pathways were identified as potentially having challenges and variation within them with pre-operative assessment for off island procedures being identified as one of the priorities. It was therefore this pathway that was chosen as a project to identify the current state so the challenges could be identified from within it. Problem The main problem was that the staff members working within this pathway were voicing confusion and finding it stressful working within the current system. Initial conversations with staff members revealed variation, duplication and ambiguity and it was decided to map the current state so the problem could be identified and future recommendations suggested. Aim The aim over a four month period was to identify the current pathway for patients and their clinical information for preassessment for planned hip and knee joint replacements off island. This would take into account both the staff and patient experience. By the end of the four months, the current pathway would be identified and shared with the staff members (on Shetland, Elgin and Aberdeen) involved. On island, Shetland staff members will be aware of their own and each other’s roles within the current system and future recommendations will be made. Action taken Initially a project initiation document, contract, charter and driver diagram were drawn up. Then, interviews were held with staff members involved in the current system (10 members of staff on island) and telephone/email conversations with staff members off island (five in Elgin, six in Woodend) and the current system was drawn up as a process map. This map was sense checked with all staff members to ensure it was accurate. Data was collected to find out how many patients went through the system. Patient stories were collected using emotional touch points. Following collection of this information, a facilitated discussion was held on Shetland with the NHS Shetland staff members involved. During this session staff members measured their understanding of each other’s roles at the beginning and end of the session on a scale 1-10 (1 being they do not understand the role at all, 10 being full understanding of the role). The beginning of the day saw scores varying from 1-10, the end showing variation of 8-10. This session also allowed future recommendations to be set. During the project, there were several risks identified that were resolved. Procedural errors were highlighted where staff were unaware around policy sharing and this was addressed immediately. There was also ambiguity of words on documents being shared with across NHS Boards which was highlighted and changed. It was highlighted that there was variation in how patient information was being sent to the mainland (posted recorded delivery and scanned and emailed) and this was streamlined to be the same system for all hospitals. Results Attached at the end of the report are three figures which show the pathways for Shetland, Elgin and Aberdeen as they currently stand. This work benefits patients as staff are now aware of the current process they follow so can better inform them of their journey which leads to less confusion. Staff members appear happier in their work and have a clearer understanding of their role and each other’s, thus enhancing working relationships. This work has raised the profile of NHS Shetland within mainland NHS Boards, organisationally staff are compliant with policies within the pathway and variation has been reduced thus reducing associated costs. Efficiency savings and productive gains Productivity has been improved because staff are now fully aware of the system they work within, they are able to provide the same service within existing budget but are able to inform the patients better around their journey. Costs have been lowered by scanning and emailing pre assessment pack to the mainland rather than sending recorded delivery which has led to a more efficient and cost effective means of producing the same results with less input. The future recommendations this project has identified will further add to the efficiency and productive gains by further reducing variation and streamlining the system to ensure faster throughput of patients. Sustainability A local working orthopaedic group has been established on island to take forward to recommendations from this project. All key stakeholders have been identified and invited. This will ensure regular and effective communication links are maintained between key staff members, which will also ensure sustainability of the current changes. Lessons learned The main lesson learned from this work was the time it took to extract the information from all stakeholders and the complexity of working across NHS Boards. It highlighted the importance of having a clear working pathway which everyone is aware of and understands. Challenging assumptions was another learning point, as often these assumptions are not factual and can further lead to confusion. The local orthopaedic working group will take forward the recommendations which have been identified by completing this work. Others looking to map similar pathways could use this as a means of demonstrating the benefits of this type of analysis – without mapping these pathways, it would have been impossible to find where the variation and ambiguity was and therefore, how to find solutions. Figure 1 – Shetland pathway Figure 2 – Elgin Pathway The Pathway for Patients and Their Clinical Information For Planned Hip/Knee Replacements – Elgin Receives letter from Shetland orthopaedic secretary regarding patient All patients out with waiting time guarantee – phone patient and offer operation elsewhere sooner Patient wishes to be seen elsewhere – Amanda informs her supervisor Patient details added to CWTT spreadsheet and sent to CWTT on Friday. Details sent to CWTT: patient name, CHI, waiting list details and highlight it is a Shetland Mr Anderson patient. Patient requests Dr Gray, Elgin. Receives POA pack via e-mail from Shetland PFB Team (Hannah) Receives POA pack and checks everything there Receives POA pack from Shetland PFB Team (Hannah) Orthopaedic secretary will print POA pack and give to nurse If patient rejected elsewhere or wish to come back to CWTT email back with POA If anything missing contact Shetland POA nurses Pack passed to anaesthetist for reviewing POA pack. Patient passed or failed. Letter sent to patient with date and details of travel Key: Orthopaedic Secretary – BLACK Medical Secretary Supervisor/Trainer – GREY Pre assessment Nurse – RED Anaesthetist – BROWN Other - GREEN Notes and POA pack arranged for admission Patient admitted day before surgery. Checked in by ward staff. Abbreviations: CWTT – Central Waiting Times Team POA – Pre operative assessment PFB – Patient Focussed Booking Surgery CWTT Figure 3 – Aberdeen Pathway