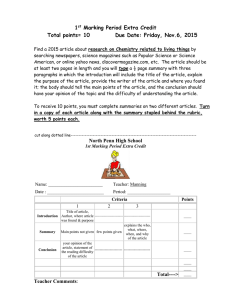
Guide to surgical site marking
advertisement

H'() 5*
GUIDE TO SURGICAL
SITE MARKING
HIGH 5s
“Performance of Correct
Procedure at Correct Body Site:
Correct Site Surgery”
ENGLISH EDITION
O OCTOBER 2012
GUIDE TO SURGICAL SITE MARKING
2
GUIDE TO SURGICAL SITE MARKING
CAUTION
This guide to marking forms part of the interna'onal High 5s project. High 5s was ini'ated by the WHO in 2007 to improve
the safety of healthcare in rela'on to some of the major pa'ent safety problems, and in par'cular by preven'ng wrong
site and wrong procedure surgery.
Marking the surgical site appears to be a key step in the preven'on of site errors; it is one of the three elements of standard opera'ng protocol* “Preven'ng wrong site, wrong procedure surgery”. The two other key steps are preopera've
checks* and the checks during the 'me out (the pause before the incision)*. Marking on its own is not a preven/on strategy and does not replace the need for preopera/ve and /me-out checks.
Every surgical team that wishes to ins'tute marking can make use of the basic principles of marking presented in this
guide.
A two-page "Quick reference surgical site marking» is also available. Contact: contact@ceppral-sante.fr
* All words followed by “*” are listed in the glossary on p. 22.
Preface
GUIDE TO SURGICAL SITE MARKING
3
“
Alas! How easily things go wrong!” wrote George Macdonald in Phantasies. Indeed, no surgeon means to operate on
the wrong pa'ent or the wrong side of the body or to remove the wrong organ or perform the wrong procedure. But
it happens. The best available evidence puts the number of wrong-site surgery cases at 1-2 per 100,000 procedures—
a disturbingly high number for an event that most agree should never happen. Clearly, competence and good
inten/on on the part of the surgeon are not sufficient to prevent these occurrences. As with most undesirable consequences,
periopera've processes that have been carefully designed to prevent such events.
The Correct Site Surgery Standard Opera'ng Protocol (SOP), which is being implemented in select hospitals interna'onally as
part of the WHO’s High 5s: Ac'on on Pa'ent Safety ini'a've, focuses on standardizing the preopera've processes for the
purpose of reducing the risk of wrong site surgery. Based on over 15 years of research on the incidence, causes and solu'ons
for this vexing problem, it establishes procedural requirements for three components of the process for preparing pa'ents for
surgery: the preopera've verifica'on check list; surgical site marking; and the final “'me-out” verifica'on. Of the three
components, the one that has proven most difficult to standardize is the site marking process.
The SOP provides guidance on what to do with respect to site marking (as well as the other preopera've processes). This Guide
Marquage provides the detailed informa'on on how to do it, which hospitals will need to effec'vely implement the SOP. In the
pages that follow, you will find specific instruc'on on the 'ming, loca'on, method and other aspects of site marking, and
addi'onal detail on how to handle site marking in certain special situa'ons. Par'cular aKen'on is paid to the role of the pa'ent
and family in the process and the overall approach is that of a team ac'vity. The instruc'ons are further enhanced with specific
examples of correct and incorrect site marking, complete with photographs of real pa'ents.
The guidance provided here is en'rely consistent with the requirements of the High 5s SOP as well as the Universal Protocol
and the WHO’s Safe Surgery Checklist. Applicable French law is cited and, in the final pages, answers are provided to the most
frequently asked ques'ons about surgical site marking. A valuable reference, indeed; this is must reading for surgeons, surgical
nurses and technicians, and any others who par'cipate in the process of preparing pa'ents for surgery.
Dr Rick Croteau,
Joint Commission Interna/onal
GUIDE TO SURGICAL SITE MARKING
preven'on requires an ac've effort, not just by the surgeon, but by the en're surgical team, func'oning within opera've and
Preface
Guide to surgical site marking
Th e H au t e Au t or it é d e San t é is h e a vi ly in vo l v e d in p ro m oti n g ch an g es in sa fe ty p ra ct ic e s an d
cu lt u r e wi th in or gan i s ation s, in con n e ct ion wi th p h y s ic ian c ert if i c ation an d ac cr ed i tat io n
p roc ed u r e s. Th e H A S “ s u rg ica l sa f ety ” ch ec kl i st h as th u s b e co m e a p ri ority p ra ct ic e in t eg rat e d
in to th e c e rti f ica tio n p roc ed u re fo r h e alt h ca r e or gan i sat ion s sin c e 2 01 0 an d h a s n o w b e en
d ep loy ed a cro s s al l op er atin g ro o m s.
4
GUIDE TO SURGICAL S IT E MARK ING
Th e H au t e Au t or it é d e San t é, in p a rtn er sh ip w i th CE PP R AL ( Coo rd in ati on p ou r l’ E va lu at ion d e s
Prat iq u e s Pr of e s s ion n el le s en san t é en Rh ôn e - Alp e s) , h a s b ee n in vo l v ed in th e WH O H i gh 5 s
“Ac tion on P ati en t Sa f ety ” p r oj ec t s in c e 2 00 9. T h e p re v en t ion o f wr on g si te an d wr on g
p roc ed u r e err or s in su r ge ry i s a “ Stan d ard Op e ratin g Pro toc ol”, a sta n d ard i s ed or gan i s ati on al
so lu t ion or p ra cti c e i mp le m en t ed an d e va lu a ted b y a r ou n d f if ty h os p it a ls wor ld wid e, in clu d in g
n in e Fr en ch h ea lth c ar e organ i sat ion s . Sa f eg u ar d s a re in c orp o rat ed in t o th e p ath way fo llo w ed
b y th e in p at i en t p rio r t o su rg er y v ia t h e st an d ard i sa tio n o f th e p r e su r gi cal ch ec k, su r gi cal s it e
ma rkin g an d “ti m e ou t” s te p s , d o cu me n t ed in th e for m o f a H igh 5 s ch e ckl i st wh ic h
in co rp o rat e s th e H A S ch ec kl is t.
Th e i m p l e me n tat ion of ma rki n g b y th e Fr en ch t ea m s rai s ed or gan is ati on al an d te ch n ica l
q u e st ion s a s w el l a s p r ob l e m s of a cu ltu r al a n d eth ic al n at u r e an d re lat in g t o m ed ic o -l eg a l
liab il ity . Th i s ch al le n g in g p ra ct ic e ap p li ed in ar o u n d t en ar ea s of sp e ci ali sa tion con v in ced th e
p ro fe s s ion a l s i n v ol v ed i n th e p ro j ect . Af te r t w o y e ar s o f i mp l e m en ta t ion an d e valu ati on , an d
mid - wa y th r ou gh th e H i gh 5 s p roj e ct, 20, 00 0 p ati en t s h a v e b en e fit ed f ro m s u r gi cal ma rk in g in
Fran c e w ith a h i gh l e v el of co mp li an c e with t h e ma r kin g p ro c ed u r e an d ex c el len t ac c ep tan c e b y
p ati en t s .
Mark in g i s p ot en t ial ly a ke y f ac tor in th e d e v el op men t o f p rac ti c es a n d in i mp ro v in g p at ie n t
sa f ety i f v i ew ed i n th e l i gh t o f th e 4 mi ll ion s u r g ica l p ro ce d u r e s p e rf or m ed e ach y ear in F ran c e.
Th is p ra cti c e i s s et to gr ow in th e p r e su r gi ca l p e riod fo r b oth i n p at ie n t s an d ou tp a ti en t s . It wi ll
b e su p p or te d b y th e V 20 14 c e rti f ica tio n of or gan i sa t ion s th ro u gh th e r e co gn it ion of
ou t stan d in g p ra ct ic e s.
Th is H i gh 5 s gu id e to su r gi ca l mar kin g, p rod u ce d b y CE P PR AL a n d H AS in coo p e rat ion w it h
h ea lth car e or gan i sat ion s, h a s b en e fi t ed fr o m th e ex p e rt op i n ion o f th e Jo in t C om m i s sio n
In t ern a tion al. I t is a m ajor c on tr ib u t ion to wa r d s t h e in c orp o rat ion o f go od ma rki n g p ra ct ic e
in to th e rou tin e a ct i vit y of th e t ea m s in vol v ed in su r gi ca l p at i en t ma n ag e men t a s op p o s ed to
ju s t th o s e te a ms in vo l v e d in H igh 5 s .
Pr Je an - Lu c H ar o u sse au ,
Ch a ir m an o f th e B o ar d
Hau te Au to r it é d e S an t é
Summary
GUIDE TO SURGICAL SITE MARKING
5
Introduc/on ..................................................................................................... ........6
2.
Marking procedure in the High 5s project .................................................................. 7
2.1. Involvement of pa'ent and family ............................................................................ 7
2.2. The marking process .................................................................................................. 8
2.3. Excep'ons to marking ............................................................................................. 10
2.4. Special cases ............................................................................................................ 11
2.5. Traceability and verifica'on of marking .................................................................. 12
2.6. Illustrated marking ................................................................................................... 15
3.
Team ques/ons ..................................................................................................... 18
4.
Case reports ........................................................................................................... 19
5.
Sources ................................................................................................................. 20
Annex : Glossary ............................................................................................................. 22
GUIDE TO SURGICAL SITE MARKING
1.
1
Introduc/on
GUIDE TO SURGICAL SITE MARKING
6
H
igh 5s was ini'ated by the WHO in 2007 to improve the safety of healthcare in rela'on to some of the major
pa'ent safety problems. The Haute Autorité de Santé, with the support of the Ministry of Health, commiKed itself
in 2009 to “Preven'ng wrong site, wrong procedure surgery” and “Assuring medica'on accuracy at transi'on of
care” and to providing the coordina'on for France.
A lack of preven've strategies during the pre-opera've period is the most common causes of wrong site surgery. Surgical site
marking is one of the cri'cal control points contribu'ng to safe surgery and a key step in the preven'on of wrong site surgery.
It is one of the components of the High5s standardised solu'on: “Performance of Correct Procedure at Correct Body Site:
Correct Site Surgery”.
GUIDE TO SURGICAL SITE MARKING
This solu'on was implemented by many hospitals in France in collabora'on with CEPPRAL for the 5 years of the project within
the framework of their par'cipa'on in the interna'onal collabora've project “High 5s: Ac'on on Pa'ent Safety”.
Marking the surgical site has confronted the teams at the hospitals with difficul'es with implementa'on that have led to them
reviewing their previous marking prac'ce (when this was done).
The objec've of this marking guide, created by CEPPRAL and HAS, with the support of the Joint Commission and in
collabora'on with the hospitals, is to assist hospitals in the implementa'on of the marking procedure according to the
requirements of High 5s and to respond to their ques'ons, in par'cular with respect to medico-legal responsibility.
It is also a tool for medico-surgical and nursing team professionals who wish to improve and harmonise their marking
prac'ces.
THE FIELD OF APPLICATION OF
THE HIGH 5S OPERATING
PROTOCOL
The High 5s opera'ng protocol
applies to all procedures carried
out in the surgical unit of the
hospital with the excep'on of
those carried out in outpa'ent
facili'es2.
MARKING THE SURGICAL SITE: :
A KEY STEP IN THE PREVENTION OF WRONG SITE SURGERY
A lack of preven've strategies during the pre-opera've period is the most common
cause of wrong site surgery.
In the Netherlands, de Vries et al1 reported, on the basis of insurance data, that there
were 294 complaints between 2004 and 2005. Wrong person, site or side errors were
ranked 3rd, represen'ng 16% of complaints (34 cases). In 12% of cases, the main
contribu'ng factor was the lack of or incorrect use of a marking procedure. Three
quarters of these errors could have been prevented by the appropriate applica'on of
a marking procedure. In France, SHAM, which insures 80% of public health care
organisa'ons and 25% of private hospitals, puts between 2007 and 2010 the number
of “confirmed” wrong side, site or person errors at 16 per year.
1
de Vries et al (Preven'on of Surgical Malprac'ce Claims by a Surgical Safety Checklist – de Vries, Annals of surgery – Jan 2011)
2
Except endoscopy and catheterisa'on rooms, labour wards and wards essen'ally dedicated to outpa'ent treatment.
2
Marking procedure
in the High 5s project
GUIDE TO SURGICAL SITE MARKING
7
2.1 IHIJKILMLHN JO PQN'LHN QHR OQM'KS
T
he surgeon is responsible for discussing marking with the pa'ent and has the duty of informing the pa'ent of the
benefits of marking which helps to make surgery safe.
INFORMATION PROVIDED VERBALLY BY THE SURGEON, WRITTEN INFORMATION ON THE CHECKLIST HANDED TO THE
PATIENT
The hospitals chose to explain the purpose and importance of the checklist to the pa'ent in a consulta'on se_ng. The
checklist is kept by the hospitals in the pa'ent’s medical file.
One hospital chose to involve the pa'ent by designa'ng him/her as the checklist holder and asking him/her to bring the
checklist along to all pre-opera've consulta'ons* and on the day of admission for the opera'on. WriKen pa'ent informa'on
was provided on the first page of the checklist.
The pa'ent must also be informed that the marking should remain visible despite the pre-opera've shower.
The pa/ent
Apart from where this is not possible because of the pa'ent’s condi'on (e.g.
confused pa'ent, etc.), marking should be carried out with the ac've involvement of the pa'ent, who should be awake and conscious.
Children
The parents of children should be involved in the marking process.
Adults with disabili/es or who are unable to communicate
Family members should be given the opportunity to be involved in the marking process.
3
In the date of December 2nd, 2011
The pa/ent may refuse marking,
but cases of refusal are rare.
Since January 2011, no pa/ent
(out of 8,547 checklists ini/ated3)
has refused marking.
Nevertheless, a procedure must
be compiled for cases where a
pa/ent refuses marking.
GUIDE TO SURGICAL SITE MARKING
Par'cipa'on of the pa'ent and his/her family help to reinforce the effec'veness of the marking process and should be
encouraged.
2.2 T)L MQWX'H( PWJYL**
When to mark ?
Marking is carried out before pa/ent transfer to theatre and ideally before seda've pre-medica'on on a pa'ent who is awake
8
and conscious.
How to mark ?
Marking is carried out a`er all the available informa'on concerning the pa'ent’s iden'ty, the procedure and the surgical site/
intended side (provided by the pa'ent, medical file, notes, imaging, consent, etc.) has been checked and cross-referenced.
Who marks ?
The site should preferably be marked by the surgeon who will be performing the opera'on.
The person who marks the site is iden'fied in the medical file (preferably in the pre-opera've verifica'on checklist*).
GUIDE TO SURGICAL SITE MARKING
Delega'on to a doctor or nurse is possible if this person is involved in the opera'on or is directly involved in the pa'ent
prepara'on process.
The organisa'on must specify the minimum qualifica'ons (for example: doctor, charge nurse) and the role (pa'ent
prepara'on or par'cipa'on in the surgical procedure) of the person to whom responsibility for marking may be delegated.
A doctor who, in isola'on, delegated certain ac'vi'es for which he/she alone is legally responsible to a paramedical
professional would be criminally liable.
And if the pa/ent refuses marking?
The pa'ent always has the right to refuse. This situa'on should be handled the same way as for any other refusal by a pa'ent
offered care, treatment or services. The organiza'on's responsibility is to provide the pa'ent with informa'on to understand
why site marking is appropriate and desirable, and the implica'ons of refusing the site marking. Then the pa'ent can make an
informed decision. The SOP does not require that the procedure be cancelled because the pa'ent refuses site marking. The
preopera've verifica'on check list has a place to document this situa'on. Organiza'on policy should describe the related
procedural and other documenta'on requirements.
Roles and responsibili/es of health professionals in the applica/on, maintenance and monitoring
of the marking procedure
Management: The management of the organisa'on is responsible for ensuring that a marking procedure, included in the preopera've verifica'on process, is in place in the organisa'on.
Heads of discipline: The heads of each discipline are responsible for ensuring that the surgeons in their discipline mark their
pa'ents in accordance with the procedure in force within their organisa'on.
Surgeon: The surgeon (or the person delegated to carry out marking) is responsible for marking the surgical site on his/her
pa'ent’s body prior to any interven'on and to carry out the marking in accordance with the procedure in force within their
organisa'on.
If the pa'ent refuses marking, the surgeon must apply the procedures in force within the organisa'on for these situa'ons.
Checklist coordinator in 'me out*: The checklist coordinator is responsible for ensuring that each pa'ent has been marked before
9
transfer to theatre.
correct surgical site has been marked before the start of the interven'on.
2—MARKING
PROCEDURE
Theatre team: The team present in the opera'ng room is responsible for conduc'ng final 'me out* and for ensuring that the
C)QWQYNLW'*N'Y* JO YJWWLYN MQWX'H(
Marking is carried out at the intended site of the incision or as near as possible to the intended site. Unless clinically necessary, no
other point should be marked besides the surgical site.
The mark must not be ambiguous. Crosses may not be used because they might be interpreted as “do not operate here”.
In general terms, the type of mark is determined specifically in accordance with the wishes of each organisa'on on the basis of a
formalised and harmonised marking procedure (same marking symbol for all professionals and all surgical disciplines).
This may be the ini'als of the surgeon, for example, or a line represen'ng the intended incision :
YES
A. B
#####
Fig. 1 : Examples of marking
The mark must be made with a skin marker that is sufficiently permanent to remain visible a`er prepara'on of the pa'ent (skin
prepara'on and applica'on of theatre drapes).
Which sites to mark?
Surgical site marking applies, as a minimum, to all cases of incision or percutaneous interven'on involving laterality* (i.e. a single
limb or one of a pair of organs), mul/ple structures or surfaces* (flexor/extensor, lesions, fingers, toes) or levels* (spine,
vertebra).
An organisa'on may decide to mark all pa'ents to prevent wrong person, wrong site errors.
The simple visceral organs (uterus, intes'ne, stomach, heart, bladder, appendix etc.) are not marked.
GUIDE TO SURGICAL SITE MARKING
The purpose of marking is to iden'fy clearly the site of incision or inser'on.
2.3 E[YLPN'JH* NJ MQWX'H(
I
10
n certain situa'ons, described below, marking must not be carried out for technical or anatomical reasons.
An alterna've method may be used to iden'fy the correct site visually. For example, a unique temporary bracelet may
be placed on the side where the interven'on is to be carried out.
The bracelet must indicate the pa'ent’s name, provide a second iden'fier, and indicate the intended procedure and the site.
The use of a bracelet on its own is not recommended as the first line method because of the risk of loss and errors in
reposi'oning.
Life-threatening emergencies
Life-threatening emergencies in which the 'me required for marking creates an addi'onal risk to the pa'ent are exempt from
marking. The risks and benefits must be assessed by the surgeon who decides whether or not to mark his/her pa'ent.
Premature infants
GUIDE TO SURGICAL SITE MARKING
Marking may cause a permanent taKoo. An alterna've method may be used.
Dental surgery
Because there is no prac'cal or reliable method for directly marking a tooth for intended extrac'on, dental surgery is exempt
from surgical site marking. As this type of surgery involves “mul'ple structures”, however, an alterna've method must be
used:
- Review of the dental records, the medical history, laboratory tests, dental charts and x-rays. The number(s) of
the teeth involved in the opera'on must be indicated or the surgical site marked on the chart or x-ray to be incorporated
into the pa'ent’s medical file.
- Verifica'on that x-rays are oriented correctly and visual iden'fica'on of the correct teeth or 'ssues
Simultaneous bilateral surgery
Opinions differ on the subject. Some people prefer to mark both eyes because, in the absence of any marking, there is a risk of
both eyes being operated on when only one was intended.
Endoscopy
All purely endoscopic procedures without a planned invasive interven'on are exempt from marking. Sites for which the
access point is not predetermined, as in cardiac catheterisa'on and other minimally invasive procedures, are considered
exempt.
Wounds or lesions
Site marking is not required in the case of obvious wounds or lesions if this wound or lesion is the site of the intended
procedure. However, if there are mul'ple wounds but only some of them must be treated, these sites must then be marked.
Cases in which the laterality must be confirmed a`er examina'on under anaesthesia or inves'ga'on.
2.4 SPLY'QK YQ*L*
Spinal surgery
Marking is usually carried out in two stages. First, the general area/level of the spine (cervical, thoracic or lumbar) must be
marked on the skin before the opera'on. Then, special intra-opera've radiographic techniques are used to mark the exact
level of the spine.
For the intended treatment of a lateralised internal organ, whether via a percutaneous approach or a natural orifice, the mark
must be made at or near the inser'on site with an arrow indica'ng the side to be reached.
2—MARKING
PROCEDURE
Laparoscopy/minimally invasive surgical procedures
11
Treatment of the breast in cases of lumpectomy
One hospital has incorporated a supplementary control, in addi'on to harpoon marking, into its procedure in the form of site
marking with an arrow in the department.
Ophthalmology
Betadine® may be used as a means of marking instead of a marker. For dark skins, an alterna've is proposed in the form of
adhesive tape applied to the eyelid on the side of the intended procedure in addi'on to the fi_ng of a wrist band on the side
of the intended procedure on which the following should be specified: Surname, first name, date of birth of the pa'ent,
intended procedure, surgical site and side. Adhesive tape alone or wrist bands alone must not be used as a means of site
marking.
ENT surgery
Tonsillectomy, adenoidectomy and laryngectomy are cases in which marking is technically impossible. Exemp'on from
marking applies.
Fingers or toes
All fingers/toes requiring surgery must be marked individually with specifica'on of the digit(s) requiring surgery.
Ovaries
If the opera'on involves both ovaries, marking is not required.
Thyroid
If the opera'on involves the whole organ, marking is not required.
GUIDE TO SURGICAL SITE MARKING
An alterna've to marking with a marker has been accepted by the Joint Commission: Non-palpable masses are marked using
ultrasound guidance in Radiology. A metal marker aKached to a wire is inserted up to the loca'on of the tumour. The wire is
clearly visible and aKached to the skin with an adhesive dressing. This is the standard method widely used by surgeons in the
United States.
2.5 TWQYLQ^'K'NS QHR ILW'O'YQN'JH JO MQWX'H(
Traceability of marking on the High 5s checklist*
Except in the case of refusal by the pa'ent, marking or non-marking should be documented on the High 5s checklist, in the pull
-out intended for this purpose (Fig. 2).
12
If marking has been carried out and was done correctly:
The “YES” box next to the ques'on “does the marking of the site sa'sfy the requirements of correct marking?” must be
checked. This is box “D”.
If marking has been carried out but was not done correctly:
The “NO” box next to the ques'on “does the marking of the site sa'sfy the requirements of correct marking?” must be
checked. The features of correct marking that were not respected must be circled in the list shown on the pull-out.
If the procedure does not fall within the criteria for High 5s marking, or if the procedure is exempt from marking or marking
is not possible:
Traceability and management of discrepancies
If a discrepancy* is observed, that is to say, marking was not carried out or marking does not correspond to the requirements
of correct marking and the interven'on is cancelled: this is documented in box “E”. If the interven'on is carried out despite
this discrepancy, this informa'on must be entered in the appropriate box. However, all members of the team must be warned
of this decision before the start of the interven'on.
SITE MARKING
Site marking is required if :
-> Laterality such as extremities; paired organs, specific surface such as flexor or extensor, specific level such as for spine
surgery, specific digit or lesion
Is site marking required or possible ?
OUI
YES
→
NO
YES
F
Exempt cases :
- Life-threatening emergencies
- Premature infants
- Cases in which site marking is
not technically feasible
↓
Is it properly marked?
D
NO
E
Patient refuses site mark
(appropriate procedure
followed)
If site marking is not properly marked, decision :
ACTOR
GUIDE TO SURGICAL SITE MARKING
Box “F” is checked.
Case cancelled (unreconciled discrepancy)
Case advanced with unresolved discrepancy
Specifications for properly marking the site
(If "No" is checked above, please circle all items in this list that are not met)
1. Marking is done by the person who will do the procedure or by
a qualified designee (MD or RN participating in procedure or
6. The mark is unambiguous ("X" is not used for site marking)
prep.)
2. The mark is made before patient is moved to procedure site
7. The mark is made using a "permanent" skin marker
3. Patient is aware and involved in site marking, if possible
8. The method of marking is consistent with hospital policy
4. The mark is made at or near the intended incision site
9. For midline access to lateral site, mark indicates correct
side
5. Non-operative sites are not marked
Name of the person who marked the surgical site :
Figure 2 : Checklist pull-out for marking
Iden/fica/on of the person who carried out the marking
In each case where marking is required, the person who marked the site is iden'fied in the medical records and preferably in
the designated place in the High 5s checklist (Fig. 2).
Verifica/on of marking
13
2—MARKING
PROCEDURE
The final verifica'on of marking is carried out in the course of the pause ('me out) before the incision (Fig. 3). When
prompted by the checklist coordinator, all members of the team present in the opera'ng theatre confirm verbally that the
site of surgery has been correctly iden'fied with reference to the marking and all the available informa'on (medical records
etc.).
PRIOR TO SKIN INCISION
Final Time out
YES
NO
If "No," circle non-compliant items in shaded
area below.
Specifications for properly conducting the final Time Out
- "Time out" occurs immediately prior to incision
- Active communication by all team members
- "Time out" is initiated by designated coordinator
- Activities (other than essential for safety) are suspended
- All operative team members participate in the "time out"
No discrepancy
ACTOR
Final "Time out" verifies the following :
Discrepancy noted
Not applicable
If discrepancies are noted below, please circle the
specific item that is missing or incorrect in the list to the
left.
• Correct patient identity (x2)
• Correct procedure (matches consent & other info)
• Correct site of surgery by visualizing site mark
• Correct patient position for intended procedure and site
• Images correctly labelled and properly displayed
• Correct implants/special equipment available
Final "time out" summary
Complete time out. (All elements listed above are checked)
One or more discrepancies noted in final "time out"
Management of discrepancies
All discrepancies reconciled
Case cancelled because of one or more unreconciled discrepancies
Case advanced with one or more unresolved discrepancies
G
H
I
J
Figure 3 : Checklist pull-out for the 'me out
Discrepancies rela'ng to marking to be reported during the 'me out:
The “NO” box next to the ques'on “does the marking of the site sa'sfy the requirements of correct marking?” is “NO” (Fig. 4),
—> a discrepancy must be recorded during the 'me out: box H is checked (Fig. 5).
GUIDE TO SURGICAL SITE MARKING
Was the final "time out" procedure conducted properly ?
SITE MARKING
Site marking is required if :
-> Laterality such as extremities; paired organs, specific surface such as flexor or extensor, specific level such as for spine
surgery, specific digit or lesion
Is site marking required or possible ?
OUI
YES
14
→
NO
YES
F
Exempt cases :
- Life-threatening emergencies
- Premature infants
- Cases in which site marking is
not technically feasible
↓
Is it properly marked?
D
NO
E
Patient refuses site mark
(appropriate procedure
followed)
ACTOR
If site marking is not properly marked, decision :
Case cancelled (unreconciled discrepancy)
Case advanced with unresolved discrepancy
Specifications for properly marking the site
GUIDE TO SURGICAL SITE MARKING
(If "No" is checked above, please circle all items in this list that are not met)
1. Marking is done by the person who will do the procedure or by
a qualified designee (MD or RN participating in procedure or
6. The mark is unambiguous ("X" is not used for site marking)
prep.)
2. The mark is made before patient is moved to procedure site
7. The mark is made using a "permanent" skin marker
3. Patient is aware and involved in site marking, if possible
8. The method of marking is consistent with hospital policy
4. The mark is made at or near the intended incision site
9. For midline access to lateral site, mark indicates correct
side
5. Non-operative sites are not marked
Name of the person who marked the surgical site :
Figure 4 : Example of the traceability of a discrepancy in the case of incorrect marking
PRIOR TO SKIN INCISION
Final Time out
Was the final "time out" procedure conducted properly ?
YES
If "No," circle non-compliant items in shaded
area below.
NO
Specifications for properly conducting the final Time Out
- "Time out" occurs immediately prior to incision
- Active communication by all team members
- "Time out" is initiated by designated coordinator
- Activities (other than essential for safety) are suspended
- All operative team members participate in the "time out"
No discrepancy
ACTOR
Final "Time out" verifies the following :
• Correct patient identity (x2)
• Correct procedure (matches consent & other info)
• Correct site of surgery by visualizing site mark
• Correct patient position for intended procedure and site
• Images correctly labelled and properly displayed
• Correct implants/special equipment available
Discrepancy noted
Not applicable
If discrepancies are noted below, please circle the
specific item that is missing or incorrect in the list to the
left.
Final "time out" summary
Complete time out. (All elements listed above are checked)
One or more discrepancies noted in final "time out"
Management of discrepancies
All discrepancies reconciled
Case cancelled because of one or more unreconciled discrepancies
Case advanced with one or more unresolved discrepancies
Figure 5 : Example of comple'on of the checklist in case of incorrect marking and resolu'on
of the discrepancy during the 'me out
G
H
I
J
- If marking was carried out and is correct, but is not visible during the 'me out (e.g.: field too small),
—> a discrepancy must be recorded during the 'me out: box H is checked (Fig. 6).
PRIOR TO SKIN INCISION
Final Time out
Was the final "time out" procedure conducted properly ?
YES
If "No," circle non-compliant items in shaded
area below.
NO
Specifications for properly conducting the final Time Out
15
- "Time out" occurs immediately prior to incision
- Active communication by all team members
- "Time out" is initiated by designated coordinator
- Activities (other than essential for safety) are suspended
No discrepancy
ACTOR
Final "Time out" verifies the following :
Not applicable
If discrepancies are noted below, please circle the
specific item that is missing or incorrect in the list to the
left.
Final "time out" summary
Complete time out. (All elements listed above are checked)
One or more discrepancies noted in final "time out"
Management of discrepancies
All discrepancies reconciled
Case cancelled because of one or more unreconciled discrepancies
Case advanced with one or more unresolved discrepancies
G
H
I
J
Figure 6 : Example of comple'on of the checklist in a case where the marking is not visible during the 'me out
The discrepancy may be resolved if all the professionals confirm orally their agreement to the site of surgery. The management
of discrepancies must be traceable on the checklist.
2.6 IKK`*NWQNLR MQWX'H(
Orthopaedics
Figure 7: Total prosthesis of knee
Figure 8: Arthroscopy
GUIDE TO SURGICAL SITE MARKING
• Correct patient identity (x2)
• Correct procedure (matches consent & other info)
• Correct site of surgery by visualizing site mark
• Correct patient position for intended procedure and site
• Images correctly labelled and properly displayed
• Correct implants/special equipment available
Discrepancy noted
2—MARKING
PROCEDURE
- All operative team members participate in the "time out"
16
Figure 10: Prosthesis of hip
Figure 9: Prosthesis of knee
GUIDE TO SURGICAL SITE MARKING
Thoracic surgery
Figure 11: Thoracic surgery
Gynecology
Figure 12: Loca'on under radiographic control for breast
Figure 13: Marking in gynecology
17
2—MARKING
PROCEDURE
Figure 15: Marking in gynecology
Figure 14: Marking in gynecology
GUIDE TO SURGICAL SITE MARKING
Neurosurgery
Figure 16: Rachis srugery
Figure 17: Intra-cranial surgery
Ophtalmology
A
B
C
D
Figure 18 : Tradi'onal marking for an intra-eye surgery ( A ) hidden by the hat ( B ). Proposal of marking on the cheek and
the forehead ( C ) always visible even if the hat hides the marking on the forehead ( D ).
3
Team ques/ons
GUIDE TO SURGICAL SITE MARKING
18
W)QN NJ RJ 'H QH LMLW(LHYS?
In the case of life-threatening emergencies in which the 'me required for marking would lead to an addi'onal risk to the pa'ent, marking is not required. The risk-benefit balance must be evaluated by the surgeon who makes the decision to mark or
not to mark the pa'ent.
W)QN 'O N)L PQN'LHN WLO`*L* *'NL MQWX'H(?
GUIDE TO SURGICAL SITE MARKING
The pa'ent always has the right to refuse. This situa'on should be handled the same way as for any other refusal by a pa'ent
offered care, treatment or services. The organiza'on's responsibility is to provide the pa'ent with informa'on to understand
why site marking is appropriate and desirable, and the implica'ons of refusing the site marking. Then the pa'ent can make an
informed decision. The SOP does not require that the procedure be cancelled because the pa'ent refuses site marking. The
preopera've verifica'on check list has a place to document this situa'on. Organiza'on policy should describe the related
procedural and other documenta'on requirements.
DLKL(QN'JH JO MQWX'H( NJ Q H`W*L JW P)S*'Y'QH R'WLYNKS 'HIJKILR 'H N)L PQN'LHN’* JPLWQN'JH, QHR MLR'YJ-KL(QK WL*PJH*'^'K'N'L*
High 5s defines precise rules and requirements for marking regarding the person who carries out the marking: ideally the
surgeon performing the opera'on. If this is not possible, a professional directly involved in pa'ent prepara'on or in the
opera'on can carry out this marking. This is then a case of regulated delega'on, Approved during a first review of the protocol
which ini'ally s'pulated that marking must be carried out by the surgeon performing the opera'on.
I* MQWX'H( YQWW'LR J`N JH N)L JPLWQN'H( NQ^KL YJWWLYN?
Marking must be carried out before the pa'ent is posi'oned because it is also used to check that the pa'ent is posi'oned
correctly (the marking is visible, so the pa'ent is posi'oned correctly). If carried out a`er posi'oning, marking loses its point.
If marking is carried out in the opera'ng room but before the pa'ent is on the opera'ng table, this is acceptable (correct
marking) even if it is not ideal.
However, if marking is carried out on the opera'ng table, this is clearly a contraven'on of the recommenda'on: “Marking is
carried out before the pa'ent is transferred to the place of surgery”. In these cases, the “Incorrect marking” item on the
checklist must be checked. Indeed, the indicators used in High 5s do not dis'nguish between marking carried out on the correct
side and marking carried out correctly. The indicator collected, in those cases where marking is required, covers “marking
carried out on the correct side and carried out correctly” (see 2.5).
AWL QKK *'MPKL JW(QH* L[LMPN OWJM MQWX'H(?
Marking is required if the intended interven'on involves only one side of an lateralised organ or one of a pair of organs, even if
the other side is checked visually during the interven'on. For organs such as ovaries or the thyroid, the lesions iden'fied by
imaging are not always iden'fied by visual inspec'on or palpa'on. It is thus important to be sure that the correct side is being
operated on. For certain gynaecological interven'ons, it is technically difficult or impossible to mark the site, and alterna've
methods of site iden'fica'on can be used, as described in the protocol (e.g. iden'fica'on wrist band specifying the pa'ent’s
iden'ty, the site/side and the procedure, see 2.3).
In the case of the ovaries, if the opera'on involves both organs, marking is not required. In the case of the thyroid, if the
opera'on involves the whole organ, marking is not required (see 2.4).
W)QN '* N)L P`WPJ*L JO N)L “CJWWLYN *`W('YQK *'NL b'N) I'*`QK'*QN'JH JO N)L MQWX'H(” 'NLM 'H N'ML J`N?
This is a cross-check of the marking carried out by the en're theatre team.
4
Case reports
GUIDE TO SURGICAL SITE MARKING
19
T
he importance of marking which is :
- systema/c
- clear
- always acempted before the pa/ent is transferred to theatre
The pa'ent is scheduled for right hip replacement surgery. Marking has been carried out the day before by the surgeon.
The opera'on is scheduled for midday, the 'me when the nurses change shi`.
Before transfer to theatre, the nurse checks the pa'ent’s iden'ty and medical file and aKaches the iden'fica'on wrist
band to the pa'ent’s wrist.
In theatre, the porter posi'ons the pa'ent for an opera'on on the le` side.
The theatre nurse asks the pa'ent to confirm his/her iden'ty, the site, the side to be operated on (right side) and
posi'ons the pa'ent in accordance with the arrangements in place.
The x-ray and the surgeon’s documents are displayed with the correct surgical site.
The nurse then has to leave the room. She is replaced by a second nurse who does not usually work with surgeons who
carry out marking, so she con'nues se_ng up and prepares the pa'ent’s skin.
The theatre nurse prepares the instrumenta'on for a le` hip replacement, s'll in accordance with the pa'ent’s posi'on.
The surgeon enters the opera'ng room, looks at the x-ray and determines the size of the prosthesis to be used.
When the opera'on starts, a 3rd nurse ini'ates 'me out. She checks the medical file and the pa'ent’s posi'on, no'ces
the anomaly and stops the interven'on which was about to start.
LEON BERARD CENTRE
A pa'ent is scheduled to undergo local anaesthesia in rela'on to his back.
The anaesthe'st is aided by a porter who supports the pa'ent by holding him so that he faces him. He thus sees the
marking performed correctly.
At induc'on of anaesthesia, the porter stops the anaesthe'st who, because he could not see the marking, was about to
perform anaesthesia on the wrong side.
GUIDE TO SURGICAL SITE MARKING
CAMBRESIS CLINIC
5
Sources
GUIDE TO SURGICAL SITE MARKING
20
OW(QH'*QN'JH*
GUIDE TO SURGICAL SITE MARKING
Joseph Ducuing Hospital (Toulouse),
Léon Bérard Centre (Lyon),
Bourg en Bresse Hospital,
Chambéry Hospital,
St Joseph-St Luc Hospital (Lyon),
Nice University Hospital,
Cambrésis Clinic,
Cornouaille Quimper Hospital.
B'^K'J(WQP)S
- Betz L., Ferguson L., Wibbens C., McCahill C. Memorial Hospital & Health System. Surgical Site Verifica'on and Time Out – Pre
-procedural Pa'ent Safety SITE VERIFICATION; LATERALITY; and TIME OUT PROCESSES. February 2004.
- East Kent Hospitals NHS Trust; Guidelines for Pre-opera've Site Marking Preven'ng Wrong Site Procedures. Issued January
2006.
- HAS, Recommanda'on en collabora'on avec l’ONDPS ; Déléga'on, transferts, nouveaux mé'ers… Comment favoriser des
formes nouvelles de coopéra'on entre professionnels de santé ? [Delega'on, transfers, new techniques: How can we encourage new modes of coopera'on between healthcare professionals?] 2008.
- Ludwick S.; Surgical Safety: Addressing the JCAHO Goals for Reducing Wrong-site, Wrong-pa'ent, Wrong-procedure Events.
Advances in Pa'ent Safety: Vol. 3. Available at: hKp://www.ahrq.gov/downloads/pub/advances/vol3/Ludwick.pdf
- Mokashi A., Stead R E., Subramaniam S. Preopera've site marking. Br J Ophthalmol 2009;93:275–276.
- Southampton University Hospitals NHS Trust, Correct Site Marking : Policy, May 2007, Version 1.0.
- Strongwater S. ; Director and CEO ; Stony Brook University Medical Center. Policy and Procedure for Opera've Site/Side
Marking and Verifica'on Stony Brook University Medical Center Ambulatory Surgery Center. 2006.
- Surgical site marking policy and protocol Version 1. Issued: 23.07.2010
JJ'HN YJMM'**'JH, `H'ILW*QK PWJNJYJK
- Joint Commission Perspec'ves, October 2009, Volume 29, Issue 10. Available at: hKp://www.med.uc.edu/Libraries/
GME_Forms/Perspec'ves_Oct09_1.sflb.ashx
- Joint Commission. Facts about the Universal Protocol. Available at: hKp://www.jointcommission.org/assets/1/18/
Universal%20Protocol%201%204%20111.PDF
- Joint Commission (JC) Guidelines. Guidelines for Implementa/on of the Universal Protocol for the Preven/on of Wrong
Site, Wrong Procedure and Wrong Person Surgery.
21
Available at: hcp://www.ahrq.gov/downloads/pub/advances/vol3/Ludwick.pdf
5—SOURCES
GUIDE TO SURGICAL SITE MARKING
Glossary
GUIDE TO SURGICAL SITE MARKING
22
Checklist
A checklist is a control list based on all the essen'al elements of safe surgical care. It is a simple and prac'cal tool. Every
surgical team can use it to check that the measures that have been shown to be beneficial for pa'ents have been
implemented in an 'mely and effec've manner.
GUIDE TO SURGICAL SITE MARKING
Discrepancy
A discrepancy corresponds to three possible cases:
1/ During verifica'on, the informa'on is not consistent, or the informa'on is missing (“A discrepancy is noted” box is
checked)
2/ The verifica'on is not included in the checklist (no box checked): “blank” line
3/ The process has not been performed properly (for marking and for 'me out: the NO boxes have been checked for
the ques'ons: “Does the site marking sa'sfy the requirements for correct marking?” and/or “Has the 'me out prior to
incision been carried out correctly?”
Except on the advice of the surgeon, who can decide to con'nue the process with a discrepancy (if he/she deems it to be
preferable, in the interest of the pa'ent, to operate despite the discrepancy), as a general rule, aKempts should be made to
correct a discrepancy as soon as one is no'ced.
Depending on the type of discrepancy, correc'ng the discrepancy will involve the following:
1/ In the case of a discrepancy observed in the informa'on rela'ng to the pa'ent’s iden'ty, the site or the procedure, the
professional must seek the truth and correct the document containing the error
2/ When a step has not been tracked in real 'me: the professional who notes this type of discrepancy carries out the
verifica'on if possible
3) When the process (marking or 'me out) has not been carried out properly, the step is started again in compliance with the
High 5s implementa'on rules
Laterality
The term “laterality” refers to a side of the body, i.e. the le` or right side.
Level
In spinal surgery, a level corresponds to a vertebra.
Standard Operang Protocol (SOP)
The Standard Opera'ng Protocol (SOP) rela'ng to the surgical site relates specifically to a par'cular type of surgical
complica'on: wrong person, wrong side or site, wrong procedure. The objec've of this standard protocol is to prevent
surgical site or procedure errors in all pa'ents in hospital for surgery, by implemen'ng and evalua'ng three complementary
steps during the preopera've period:
. a systema'c preopera've verifica'on process
. marking of the surgical site
. final verifica'on during the 'me out
Time out (or pause for briefing before incision)
Time out corresponds to the pause for briefing which takes place just before incision. The purpose of 'me out is to carry
out a final check regarding the correctness of the pa'ent’s iden'ty, the procedure, the site, the pa'ent’s posi'on and, if
applicable, the implants and special equipment required by means of ac've communica'on between all the surgical team
members present in theatre. The interven'on should not start un'l any anomalies have been resolved.
Specifica'ons for properly marking the site
23
The pre-opera've checks consist of a process of informa'on collec'on and verifica'on at each step of the pa'ent’s journey,
from the decision to operate through to the pause for briefing before incision (“'me out”). These checks are based on a pre
-opera've checklist which is unique to each pa'ent, completed in real 'me by the various individuals involved throughout
the pa'ent’s journey from the decision to operate up to the 'me of incision. This con'nuous collec'on of informa'on in
the form of “check boxes” relates to the pa'ent’s iden'ty, the surgical procedure, the side to be operated on and, if
applicable, the intended implant.
The purpose of these checks is to reduce the risks of wrong pa'ent and wrong procedure by ensuring that all the necessary
documents and diagnos'c inves'ga'ons are available before the start of the interven'on and that they have been
reviewed and correctly iden'fied. Any missing informa'on or anomaly must be inves'gated and any anomaly resolved
before the start of the interven'on.
H'() 5* PWJdLYN
Ini'ated by the WHO in 2006, the purpose of the “High 5s Project” is to improve the safety of
healthcare in rela'on to 5 major pa'ent safety problems: concentrated injectable medicines,
medica'on accuracy at transi'on of care, the preven'on of wrong site and wrong procedure errors in
surgery, communica'on errors during transfer of pa'ents and the fight against healthcare-associated
infec'ons. So far, the first three protocols are opera'onal.
GUIDE TO SURGICAL SITE MARKING
Pre-opera/ve checks
GLOSSARY
Marking is done by the person who will do the procedure or by a qualified designee (MD or RN par'cipa'ng in procedure or
prep.)
The mark is made before pa'ent is moved to procedure site. Pa'ent is aware and involved in site marking, if possible.
The mark is made at or near the intended incision site. Non-opera've sites are not marked.
The mark is unambiguous (« X » is not used for site marking).
The mark is made using a « permanent » skin marker.
The method of marking is consistent with hospital policy.
For midline access to lateral site, mark indicates correct side.
H'() 5*
Almnopqrstrurnvw
We would like to express our gra'tude to Dr. Rick Croteau of the Joint Commission Interna'onal for his exper'se and support
which were invaluable in the crea'on of this guide.
A`N)JW*: Lead Technical Agency
C. Chabloz (CEPPRAL coordinator), K. Fanget (CEPPRAL project assistant), B. Fort (CEPPRAL public health resident), M. Leclercq
(CEPPRAL project assistant)
A. Broyart (HAS project manager), C. Bruneau (HAS scien'fic consultant)
CJHNW'^`NJW*:
- Dr P. Papin (orthopedic surgeon, HAS project manager)
- Hospitals involved:
Joseph Ducuing Hospital (Toulouse): M. Mar'n (healthcare execu've), C. Pribilski (healthcare execu've – surgical unit), S.
Fristch (visceral surgeon), J. Rémi (orthopaedic surgeon), G. Giordano (orthopaedic surgeon), E. Labeyrie (gynaecological
surgeon), T. Charasson (gynaecological surgeon), M. Fabre (general healthcare coordinator, head of project)
Léon Bérard Centre (Lyon): M. Rivoire (visceral surgeon), I. Philip (quality director), V. Aloy (quality technician)
CH de Bourg en Bresse: H. Arnould (surgeon), F. Saussac (surgeon), C. Rigaud (healthcare execu've), C. Ravet (theatre nurse),
G. Nevoret (surgery nurse), S. Mouchet (nurse anaesthe'st)
Chambéry Hospital: C. Deyrolle (gynaecological surgeon), D. Beaudouin (physician specialising in the evalua'on of the quality
of care and medical risks), I. Benoit (healthcare execu've – gynaecology), A. Gambier (healthcare execu've – surgical unit), C.
Giraud (nurse anaesthe'st)
St Joseph-St Luc Hospital (Lyon): F. Weppe (orthopaedic surgeon), F. Normand (ophthalmologist), G. Delorme (healthcare
execu've – surgical unit), N. Chappaz (theatre nurse), J. Leynon (risk and safety manager)
Nice University Hospital: M. Lonjon (neurosurgeon), H. Bermond (healthcare execu've)
Cambrésis clinic (Cambrai): Drs Gaffuri, Audebert, Joveniaux, Henry, Au'ssier (orthopaedic surgeons), Dr Aissani
(ophthalmologist), Dr Hubaut (vascular), Dr Dessirier (angiologist), Dr ThuroKe (visceral), J.Gaffuri (director), J.Midavaine
(surgical unit manager), C. Avit (CIO and hygiene execu've), F. Pouillaude (quality trainee)
Cornouaille Hospital (Quimper): V. Capitaine (state registered nurse, short-stay surgery coordinator), Dr V. Deslandes
(obstetric gynaecology), Dr V. Devisme (manager of the medical anaesthesia unit), M. Dumou'er (quality-risk manager), P.
Fabre (healthcare execu've – surgical unit), M. Floc’h (healthcare execu've – short-stay surgery and day surgery unit), Dr C.
Foucher-Malecki (obstetric gynaecology), P. Gau'er (healthcare manager – urology, head and neck), Dr P. Germain (obstetric
gynaecology, head of the mother and baby unit), E. Grannec (theatre nurse), L. Grelet (director of healthcare/general
healthcare coordinator), Dr D. Hasle (head of the medical ophthalmology unit), M. H. Irvoas (theatre nurse), Dr M. Jacquot
(head of the medical obstetric gynaecology unit), F. Le Corre (healthcare execu've – obstetric gynaecology), A. Le Failler
(senior healthcare execu've – surgery), M. Le Floc’h (senior healthcare execu've – mother and baby unit), Dr G. Rolland-Jacob
(healthcare risk management), B. Salaun (state registered nurse, short-stay surgery coordinator), Dr N. Wong Chi Man
(obstetric gynaecology)
GUIDE TO SURGICAL SITE MARKING
English edi/on of october 2012
A two-page "Quick reference surgical site marking»
is also available.
Contact: contact@ceppral-sante.fr
HIGH 5s
Performance of Correct Procedure at Correct Body Site:
Correct Site Surgery