Cardiac Auscultation - ANIMAL CARE FOUNDATION
advertisement
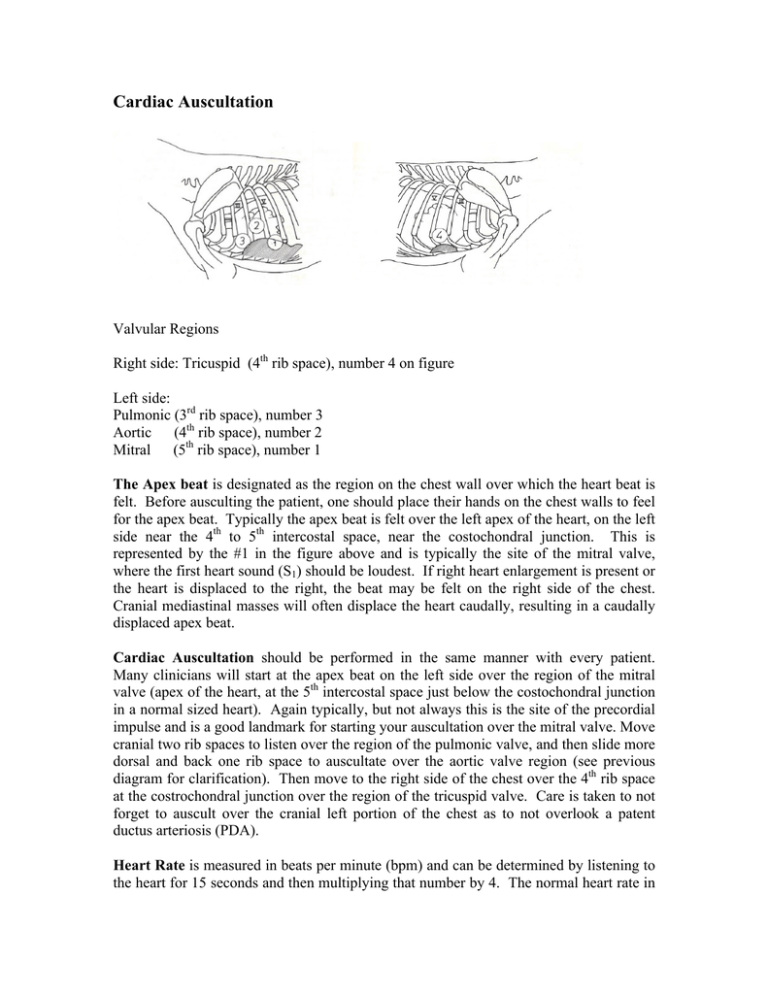
Cardiac Auscultation Valvular Regions Right side: Tricuspid (4th rib space), number 4 on figure Left side: Pulmonic (3rd rib space), number 3 Aortic (4th rib space), number 2 Mitral (5th rib space), number 1 The Apex beat is designated as the region on the chest wall over which the heart beat is felt. Before ausculting the patient, one should place their hands on the chest walls to feel for the apex beat. Typically the apex beat is felt over the left apex of the heart, on the left side near the 4th to 5th intercostal space, near the costochondral junction. This is represented by the #1 in the figure above and is typically the site of the mitral valve, where the first heart sound (S1) should be loudest. If right heart enlargement is present or the heart is displaced to the right, the beat may be felt on the right side of the chest. Cranial mediastinal masses will often displace the heart caudally, resulting in a caudally displaced apex beat. Cardiac Auscultation should be performed in the same manner with every patient. Many clinicians will start at the apex beat on the left side over the region of the mitral valve (apex of the heart, at the 5th intercostal space just below the costochondral junction in a normal sized heart). Again typically, but not always this is the site of the precordial impulse and is a good landmark for starting your auscultation over the mitral valve. Move cranial two rib spaces to listen over the region of the pulmonic valve, and then slide more dorsal and back one rib space to auscultate over the aortic valve region (see previous diagram for clarification). Then move to the right side of the chest over the 4th rib space at the costrochondral junction over the region of the tricuspid valve. Care is taken to not forget to auscult over the cranial left portion of the chest as to not overlook a patent ductus arteriosis (PDA). Heart Rate is measured in beats per minute (bpm) and can be determined by listening to the heart for 15 seconds and then multiplying that number by 4. The normal heart rate in adult dogs ranges from approximately 60 to 160 with rates in puppies as high as 200, and the normal rate in adult cats ranges from 120 to 240 beats per minute. Slower than normal heart rates are termed bradycardia and faster than normal rates are termed tachycardia. Remember to palpate the femoral pulse while ausculting heart rate to assess for pulse deficits. Heart Rhythm can be characterized as either a normal sinus rhythm (NSR), normal respiratory sinus arrhythmia (NRSA) or as an arrhythmia. Electrocardiography (ECG) is often necessary to confirm the nature of the arrhythmia. • Normal Respiratory Sinus Arrhythmia is a phenomenon where heart rate is slowly altered by changes in autonomic nervous tone associated with breathing patterns. Higher vagal (parasympathetic) tone during expiration can cause the heart rate to slow during this phase of the respiratory cycle. The heart rate will increase during inspiration as parasympathetic tone decreases. This is common in dogs, but it is rarely seen in cats in the clinic environment. • Arrhythmias can be characterized by abnormal fast rates (tachyarrhythmia), slow rates (bradyarrhythmia), or extra heart beats (extra-systoles – premature contractions). Arrhythmias can be characterized further by their rhythm. They are often categorized as being irregular or chaotic, sustained (>30 seconds) or paroxysmal (short bursts). • Extra-systoles are just that, extra contractions or heart beats. They are often distinguished by the pause created after the extra beat, rather than the extra beats themselves. To some, this phenomenon sounds like a person tripping, followed by taking a brief moment to regain their stride. They may present randomly or in patterns. • Atrial fibrillation is typically a very rapid, irregularly irregular rhythm and is often described as the chaotic sound heard when tennis shoes are placed in the dryer. Atrial fibrillation is common in dogs with an extremely enlarged left atrium as seen in some dogs with dilated cardiomyopathy (DCM). Any abnormality in heart rate or rhythm detected during cardiac auscultation is a clear indication to perform electrocardiography to determine the precise nature of the arrhythmia. Heart sounds can be characterized as normal, muffled, gallop sounds, clicks, split sounds or murmurs. If applicable, the sounds should be described in regards to their location heard and timing in the cardiac cycle (systole, diastole or both). Normal heart sounds in dogs and cats are systolic in nature and represented by S1 and S2 described by many as “lub-dub”. The first heart sound (S1) represents closure of the AV valves (mitral and tricuspid). S1 is loudest over the mitral valve area, and is louder, longer and lower pitched than the second heart sound, S2. S2 represents closure of the pulmonic and aortic semilunar valves and is heard loudest by moving the stethoscope cranially from the area of the mitral valve auscultation toward the heart base on the left side. S2 is shorter and higher pitched than S1. In the dog and cat (in contrast to the horse), it is abnormal to hear the third and forth heart sounds (S3 and S4) which are diastolic in nature. The presence of S3 or S4 is recognized when a gallop sound is heard during auscultation. Gallop Sounds sound like a horse galloping and are associated with diastolic dysfunction in dogs and cats (see below). Gallop sounds are audible sounds associated with ventricular filling and do not represent a rhythm abnormality. They can often be heard in cats with hypertrophic cardiomyopathy (HCM) or dogs with dilated cardiomyopathy (DCM). Gallop sounds are low frequency sounds accentuated by the bell of the stethoscope. These sounds occur during early (S3) and late (S4) diastolic filling and again are not heard in normal dogs and cats. Their presence indicates ventricular rigidity (decreased compliance), which commonly occurs with cardiomyopathy. Muffled heart sounds may represent pleural or pericardial effusion. If you can not clearly hear the heart sounds, consider additional diagnostic testing to rule out these conditions. Systolic clicks may also be heard. Systolic clicks are often high frequency sounds occurring in mid to late systole associated with valvular prolapse of the atrioventricular valves (mitral or tricuspid) and can be noted in early degenerative valve disease. Split heart sounds occur with asynchronous closure of either the atrioventricular or semilunar valves. This can be normal or a pathologic process. A split S1 may be due to electrical disturbances or stenotic AV valves. A split S2 can be appreciated with pulmonary hypertension and therefore can be seen with heartworm disease. Murmurs: Murmurs are created by turbulent blood flow through a narrowed orifice in the heart. They can be due to regurgitant blood flow across an insufficient valve or due to aberrant blood flow through septal defects. The key to murmurs is to be able to properly characterize them and know how to categorize them (differential list). Murmurs are characterized most importantly by their timing in the cardiac cycle (systole, diastole or both) and point of maximum intensity (PMI- or loudest location). They are also characterized by their grade (1 out of 6 to 6 out of 6) and shape. Timing: Murmurs can occur in systole, diastole, both (to and fro), or be continuous. Moreover, some may be only present during a focal time of the cardiac cycle (i.e. early, mid or late). ♦ Systolic murmurs occur in systole between S1 and S2 o holosystolic refers to murmurs that begin with S1 and end just prior to S2 allowing S2 to be heard o pansystolic refers to murmurs that continue throughout the entire systolic cycle obliterating the S2 sound ♦ Diastolic murmurs are extremely uncommon in small animals and occur during the diastolic phase of the cardiac cycle, usually begin during S2 masking this sound. ♦ Continuous murmur refers to a murmur that extends through systole and diastole without any pauses. They are also termed machinery murmurs. ♦ To and Fro murmurs are heard in systole and diastole but the systolic and diastolic phases are created by two different abnormalities such as subaortic stenosis and aortic insufficiency. There are short pauses between each phase. They have a sound that resembles sawing wood. Location or Point of Maximum Intensity (PMI) refers to the area over the heart where the murmur is heard loudest and may be characterized as left or right, apical or basilar, and parasternal (cats). Additionally, the murmur should be localized to a specific valve area if possible (see above diagram). PMI - Examples -Left Apical *mitral regurgitation *subaortic stenosis -Left Basilar *pulmonic stenosis *subarotic stenosis -Left Cranial *left-to-right patent ductus arteriosus -Right Sided *left-to-right ventricular septal defect *tricuspid regurgitation Shape of the murmur refers to its shape as it would be diagramed on a phonocardiogram. Some murmurs start loud and fade (decrescendo), some increase and then fall (diamond), and some remain stable in intensity (plateau) (see diagram below). Grading is based on the intensity or loudness of the murmur Grade 1/6: Grade 2/6: Grade 3/6: Grade 4/6: Grade 5/6: Grade 6/6: Softest murmur audible in a quiet room after minutes of listening Soft but readily heard Easily heard, focal Loud, but not accompanied by a palpable thrill, radiates Loud and accompanied by a palpable thrill Can be heard without a stethoscope by listening close to the thorax or with stethoscope lifted off thoracic wall A thrill is a vibration that can be palpated with the palm of your hand over the region of the murmur (PMI) which feels like a cell phone or pager vibration. Note: The grading system is somewhat subjective and will vary between individuals and stethoscope type. Also, murmur intensity is not necessarily related to severity of heart disease. Regurgitant or murmurs of valvular insufficiency occur across incompetent valves. Atrioventricular valvular regurgitant murmurs (mitral and tricuspid) occur during systole and are typically plateau in shape. Aortic and pulmonic valvular insufficiency occurs during early diastole and is typically decrescendo in shape. The PMI for each murmur would be located over each individual valve location. Murmurs created secondary to turbulent blood flow through a narrowed outflow tract. Examples of a fixed outflow tract obstruction include pulmonic and (sub)aortic stenosis. These murmurs occur during systole and are typically diamond shaped. Aberrant blood flow across shunts can also create audible murmurs. ♦ Patent ductus arteriosus (PDA - left to right) results in a continuous murmur, usually with a thrill with a PMI high over the left cranial thorax. ♦ Ventricular septal defect (VSD – left to right) will result in a right sided murmur varying in intensity and shape depending on its size (plateau to diamond). In certain circumstances (i.e. pulmonary hypertension) PDAs and VSDs can reverse their direction from a left to right to a right to left shunts. If this occurs, the PDA murmur no longer is audible. In its place a split S2 sound can usually be heard. Auscultation of the lower airways is another critical component of the cardiac evaluation. Patients, once again, should be relaxed in a standing position. They can not be panting. The thorax should be systematically ausculted. Pulmonary and pleural space disease can be primary or secondary to cardiac or systemic disease. Although auscultation of the chest and lower airways is not particularly sensitive or specific, it can provide important information. Thoracic radiographs are typically recommended to help correlate physical examination findings. When listening to the lungs it is important to note 1) the area(s) in which you detect abnormalities (i.e. cranial, caudal, ventral, dorsal, left, right lung fields), 2) the abnormalities noted (i.e. inspiratory crackles, expiratory wheezes, muffled or decreased respiratory sounds, increased bronchovesicular sounds) and 3) the phase(s) of the respiratory cycle in which they are found (i.e. inspiratory versus expiratory). Crackles represent inspiratory sounds heard at the level of the alveoli and can be present with primary pulmonary disease as well as pulmonary edema secondary to left sided congestive heart failure. In fact, crackles are more commonly noted with primary pulmonary disease and may not always be heard in patients with left sided congestive heart failure (with pulmonary edema). For example, in chronic bronchitis, some of the smaller airways are collapsed, especially during the earlier phase of inspiration, then suddenly open with a crackling sound as inspiration progresses. Again, radiographs and other physical examination findings can play a large role in differentiating between primary pulmonary disease and a patient in left sided congestive heart failure. . Wheezes (which may be further classified as high-pitched and low-pitched) are continuous musical or whistling sounds generated by air passing through narrowed airways (e.g., intrathoracic tracheal collapse). Wheezes that arise from intrathoracic disorders are usually more pronounced during expiration. Muffled breath sounds may occur with conditions such as pleural effusions. With a pleural effusion, careful auscultation of your patient in the standing position will frequently reveal normal breath sounds in the dorsal lung fields, and muffled or even absent breath sounds in the ventral lung fields