53 In Vivo Models of Skin Irritation
advertisement

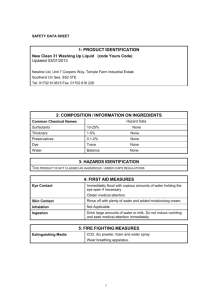
489 53 In Vivo Models of Skin Irritation F. Anthony Simion 53.2 Contents 53.1 53.2 53.3 Introduction . . . 489 Theoretical Models of Irritation . . . 489 The Initial Effects of Surfactants on the Skin . . . 490 53.3.1 Sensory Irritation . . . 490 53.3.2 Squamometry . . . 491 53.3.3 Superhydration of the Stratum Corneum . . . 492 53.4 The Role of Skin Condition on the Irritant Response . . . 492 53.5 Models for Assessing Skin Irritation . . . 493 53.5.1 Closed Patch Testing for Assessing Hazard . . . 493 53.5.2 Exaggerated Usage Tests . . . 494 53.5.2.1 Exaggerated Wash Tests . . . 494 53.5.2.2 Use Testing . . . 495 53.6 Models for Measuring the Moisturizing Potential of Cleansers . . . 496 53.6.1 Testing on Dry Skin . . . 496 53.6.2 Measuring the Clinical Effects of Moisturizing Cleansers on the Skin . . . 496 53.7 Bioengineering Measurements of Skin Condition . . . 498 References . . . 498 53.1 Theoretical Models of Irritation Theoretical, in vitro and in vivo models have been developed to assess many discreet forms of irritation, and some will be discussed below. As they all affect the same substrate, the skin, they frequently have characteristics in common. There are two theoretical models that help us better understand how the skin reacts to a variety of irritants. The trauma model of irritation proposed by Malten suggests that visible irritation occurs when the intensity of the insult exceeds a threshold [1]. A single large insult (a), or a series of small ones (b), that cumulatively exceed the threshold, can cause this (Fig. 1). As the skin repairs itself, the intensity is reduced, eventually falling below the threshold, and the clinical signs disappear. Introduction Irritation is the response of skin to noxious chemicals, trauma, or other insults from the environment. The response can take many forms, both visible and sensory, but by definition is unpleasant to the person experiencing it. The mechanisms by which different forms of irritation are produced can vary greatly. To develop optimal strategies to prevent or ameliorate the different forms of irritation being experienced, understanding what is happening and the factors that enhance or reduce the irritation is needed. This is best achieved by examining each form of irritation separately in a model system, where that type of irritation is the primary type induced. Fig. 1. Theory of traumiterative irritation One key implication from this model is that the skin can respond before clinical signs are apparent. This is the basis of the “invisible dermatoses” proposed by Kligman [2]. He demonstrated that the skin might be damaged at the histological level, even though nothing is visible at the surface. For instance, in photobiology, half the minimal dose of UV required to produce erythema (1/2 MED) will cause cell death in the epidermis, i.e., produce “sunburn” cells. Another 490 F. Anthony Simion example is patching the skin with 0.5% sodium lauryl sulfate (SLS) for 24 h. In many subjects, erythema was not observed, nor were there any histological changes apparent in hematoxylin-eosin stained sections. However, thin sections showed a great deal of epidermal damage, with swollen keratinocytes and edematous intercellular spaces. This also explains why damaged or compromised skin is more responsive. It already has a significant but subclinical level of damage, thus requiring a smaller insult to produce a visible sign that impact skin in good condition. Freeman and Maibach showed a greatly elevated TEWL response to a second SLS patch, applied to the same site as a first patch one week before, even though the TEWL rate had apparently returned to baseline in the intervening time [3]. Another implication of this model is that different forms of irritation have different thresholds. Therefore, a mild insult may produced only a few, mild forms of irritation, whereas with a greater insult, the threshold for more forms of irritation is surpassed, so they too are expressed. The second model relates skin strata to the type and degree of irritation (Fig. 2). Each strata produces irritation that is characteristic of that level: for instance, the stratum corneum and the upper epidermis can reduce sensory irritation and dryness. Erythema, which involves increased blood flow, requires dermal involvement. If the stratum corneum is damaged, then the irritants can penetrate to lower strata and produce a more intense irritation than is expected. This is the basis of the enhanced response of compromised skin. 53.3 The Initial Effects of Surfactants on the Skin Surfactants and other irritants initially interact with the stratum corneum. Thus, in normal skin it is the stratum corneum and the structures within the upper epidermis that initially respond to chemical irritants. These responses can take several different forms, including: • • • Sensory irritation Damage to the surface corneocytes Superhydration of the stratum corneum However, as the exposure to the irritant becomes more exaggerated, such as increased intensity, is prolonged, or the stratum corneum barrier is damaged, the lower skin structures will become involved, and other signs of irritation will appear. 53.3.1 Sensory Irritation Exposure to many chemicals or products can produce unwanted sensations such as the feelings of dryness, stinging, itching, or skin burning, even in the absence of visible signs of irritation. Epidemiological studies have indicated that half of the adverse reactions caused by personal care products fall into this category [4]. There are many different mechanisms by which such sensations are produced. Some personal care products such as sunscreens and lactic acid-containing lotions were shown to cause a facial stinging )RUQRUPDOVNLQ Method Skin Strata Affected Observable Instrumental Sensory %ULHI:DVK 1RUPDOZDVKHV 6XUIDFH 1R &RQGXFWDQFH ([DJJHUDWHG:DVK 6KRUWZDVKVHFV /HDYHODWKHURQVNLQ 5HSHDWXSWR[DGD\IRU VHYHUDOGD\V 3URORQJHG:DVK /RQJHUZDVKPLQXWH ,PPHGLDWHULQVH 5HSHDWXSWR[DGD\IRU VHYHUDOGD\V 6WUDWXP&RUQHXP 'U\QHVV &RQGXFWDQFH 6WLFN\WDSHVWDLQ" ,PDJHDQDO\VLV" 3KRWRJUDSK\ )HHOVVRIW )HHOVWLJKW )HHOVGU\ )HHOVGU\ /RRNVGU\ ,WFKHV 7R'HUPLV (U\WKHPD 'U\QHVV" 7(:/ &RORULPHWHU /DVHU'RSSOHU &RQGXFWDQFH &ORVHG3DWFK7HVW 2FFOXVLYHSDWFKLQJRQ UHVSRQVLYHVXEMHFWVIRU KUV Increased Treatment Intensity Fig. 2. The type of skin response to cleansers is a function of treatment intensity )HHOVGU\ 6WLQJV /RRNV5HG 53 In Vivo Models of Skin Irritation in a responsive subpopulation of consumers. Placing a 10% lactic acid solution on the face can identify these individuals while they are sweating [5]. The responsiveness of panelists can be increased by facial washing with soap and decreased by repeated applications of a good moisturizer. This suggests that the skin of lactic acid stingers is somewhat damaged, although the mechanism by which stinging is produced is not well understood. Exposure to capsicin, the hot component in Chili peppers, can reduce a burning sensation. Green and his colleagues have been able to measure this phenomenon using a labeled magnitude scale and have shown that although there is a large person-to-person variation in response, there is good reproducibility of the measurements within individuals [6]. The relative sensitivities to other chemical irritants such as lactic acid (stinging) and ethanol may be different in different individuals. The mechanisms by which these sensory irritations are produced are unclear. There appear to be several sensory mediators such as histamine and substance P. Indeed, intradermal injections of histamine can induce itching in many subjects [7]. As the unmyelinated C fibers appear to play an important role in the detection of chemical irritancy via the sensations of itching and stinging, it is likely that histamine stimulates them. These fibers also can detect heat and cold. It has been hypothesized that stimulation of a few fibers results in the perception of itching. As more of the fibers are stimulated, the signal is interpreted as stinging. The response of the C fiber can be blocked. Maibach and his colleagues have shown that a variety of anti-irritants such as menthol and anesthetics can modify the ability of the C fibers to detect heat and cold, itching and stinging [8]. Sensory irritation can frequently be detected before clinical signs can be observed. Simion et al. showed that in an exaggerated forearm wash test panelists could detect differences between soap and a milder synthetic detergent bar before a trained observer could differentiate the products [9]. This is consistent with the results of the epidemiological study by DeGroot et al., which reported that many people experience sensory irritation in the absence of visible signs, and discontinue use of that product before visible irritation appears. 53.3.2 things happen as a result. Firstly the corneocyte sheet begins to break into smaller sheets and individual cells. These cells will take up hydrophilic stains more readily than undamaged corneocytes. Both processes can be assessed. Whether sheets of corneocytes are present can be determined by visual inspection under a light microscope. Dye uptake is readily quantified by colorimetric assessment. This is the basis of both squamometry and corneosurfometry. The latter is the in vitro approach where the corneocytes are harvested first using a sticky tape and then exposed to surfactants. Squamometry involves treating the skin first and then harvesting the corneocytes with sticky tape and dyeing them. Periard, Paye, and their colleagues have used squamometry to assess the effects of cleansing products on the conditions that resemble normal usage. Paye and Cartiaux showed that the daily usage of the of dishwashing liquids combined with a 5-min soak for 4 consecutive days at normal usage concentrations (0.25%) gave the same line-up for skin damage as the highly exaggerated Frosch and Kligman soap chamber test (occlusive patching for 24 h with a 2.25% solution of the dishwashing liquid, followed by 6-h occlusive patches on the next 4 consecutive days [10]. Periard et al. have extended this methodology beyond surfactant-induced irritation. They showed squamometry was extremely sensitive in its ability to detect the effects of a fabric softener in reducing the degree of skin surface damage caused by repeated rubbing with wet towels. In this it was more discriminating than an observer, TEWL, or capacitance [11]. Squamometry can also be used to assess moisturizer efficacy. The effective moisturizers can stimulate the desquamation of damaged surface corneocytes. This results in the reduced dye uptake as measured by a lower C * value (Fig. 3). Polyol-based moisturizers are more effective than those without polyols at reducing C* and enhancing skin conductance. This suggests that the polyol-containing moisturizers are more effective at removing damaged aggregates of corneocytes otherwise known as dry skin scales or flakes. Squamometry Any short-term exposure of the skin surface to surfactants can damage the surface corneocytes. Two Fig. 3. After Lotion Treatment No Product Treatment 491 492 F. Anthony Simion 53.3.3 Superhydration of the Stratum Corneum Short-term (minutes) exposure of the stratum corneum to aqueous solutions of anionic surfactants causes it to swell. Wilhelm et al. showed that this swelling is related to the primary irritation potential of the surfactant [12]. When examined in an ex vivo model, Rhein et al. speculated swelling occured when the hydrophobic tails of the surfactants bound to the stratum corneum [13]. The negatively charged head groups would then repel each other. This would have two effects – firstly it will enable the small hydrophilic molecules such as the natural moisturizing factors (nmfs) to leach out, resulting in the skin’s reduced ability to hold moisture. Secondly the bound surfactants are not readily desorbed. As they remain in the upper stratum corneum, they damage the skin for example donator. Imokawa and his colleagues have proposed that surfactant binding to the skin is a major cause of skin roughness and perceived tightness [14, 15]. It should be noted that nonionic and cationic surfactants do not cause the stratum corneum to swell; yet cationic surfactants can be just as irritating as their anionic analogs. 53.4 The Role of Skin Condition on the Irritant Response The condition of the skin is a crucial factor on the type and intensity of the response to a set insult. Firstly, it must be realized that skin on different parts of the body will react with different intensities to the same stimulus. Cua et al. showed that the thigh was the most responsive anatomical site to SLS exposure, whereas the palms were least responsive. TEWL was found to be a more sensitive measure of irritation than visual scoring [16]. The basis for these differences in responsiveness is unclear. They may be related to the ease at which molecules can diffuse through the stratum corneum. Rougier et al. showed that there was a correlation between the skin’s permeability to water exiting and the absorption of hydrophobic molecules such as benzoic acid, acetyl salicylic acid, and caffeine [17]. The correlation coefficient (R) ranged from 0.92 down to 0.72. This may be a function of corneocyte size. The idea that the skin’s permeability to irritants is related to its responsiveness is not only intuitively reasonable but is supported by experimental data, especially for ionic irritants. 1. Predamaging the stratum corneum by immersing the skin in dilute surfactant solutions increases the erythema induced by subsequent patching with SLS [18]. 2. Predamaging the skin by physically abrading the stratum corneum with a needle significantly decreases the threshold concentration of Triton X-100, formalin, or nickel ions required to elicit irritation. This scarification procedure has much less effect on the skin’s responsiveness to hydrophobic irritants such as lauric or benzoic acids [19]. 3. Panelists who had a stronger than average vasodilation response due to the percutaneous penetration of methyl nicotinate also had a stronger irritant response to SLS [20]. 4. Skin responds more strongly in the winter to patching with SLS than in the summer [21]. The basal level of transepidermal water loss is higher in the winter, indicating the stratum corneum barrier is more permeable, i.e., damaged. 5. Agner showed that patients with atopic dermatitis, where the stratum corneum barrier is compromised (basal TEWL rate is higher), show a stronger TEWL response to SLS-induced irritation than nonatopic controls [22]. 6. Pinnagoda et al. extended Agner’s observation to a nonatopic population. They showed that the basal (pretreatment) TEWL rate correlates with the elevated rate observed after SLS exposure [23]. I have observed that TEWL rate after 24 h of surfactant exposure is a strong predictor of the TEWL rates after a 2nd day of occlusive patching using the modified soap chamber test [24]. This suggests that the “leakiness” of the stratum corneum to water loss will make it more vulnerable to surfactant-induced irritation. In the skin strata model, shown in Fig. 2, damage to the stratum corneum implies that the irritants can penetrate more deeply into the skin and produce 53 In Vivo Models of Skin Irritation more intense forms of irritation than if the stratum corneum were intact. 53.5 Models for Assessing Skin Irritation 53.5.1 Closed Patch Testing for Assessing Hazard Closed patch testing is used to assess the overall dermal primary irritation potential (toxicological hazard) of chemicals, including surfactants, and products. Frequently the Draize test in rabbits has been used as the standard, especially for regulatory assessments. However, there is experimental data that questions how predictive rabbit skin is of human skin’s response. Phillips et al. assessed the primary irritation potential (hazard) of a large variety of chemicals in human volunteers by occlusive patching for up to 21 consecutive days, i.e., the cumulative irritation test [25]. They found that while the Draize test could differentiate strong irritants from chemicals that were not irritating to humans, it was not effective at comparing materials of mild and moderate irritation potential. For more refined comparison, human models appear to be required. For cosmetic ingredients and products, Burger and Bowman reduced the original 21-day cumulative irritation test to only 14 days, by demonstrating that the relative magnitude of irritation does not change between 14 and 21 days. Reducing study duration greatly reduces the risk of tape reactions. Inclusion of positive and negative controls (0.1% SLS and a blank, respectively) can be used to standardize the results between studies. Another, similar approach that can be used in product safety assessments is to assess irritation potential of a material from the induction phase of the Maibach-Marzulli Human Repeated Insult Patch Test (HRIPT). In this procedure, 100 panelists or more are occlusively patched almost continually for 3 weeks. The erythema produced is recorded, when patches are replaced, three times a week. Recently a 4-h human exposure test has been developed as an assessment of hazard [26]. Volunteers are patched occlusively with test material and a standard (positive control, 20% SLS aqueous solution) for up to 4 h. At specified times, the test site is checked to determine if erythema has been induced. Once this occurs, that particular chemical is removed from the test site. The response is then statistically compared with the positive control. Initially, 20% SLS was used for this purpose, as in European Regulations this solution is defined as an irritant (R38). Those materials that are not statistically different from 20% SLS in this procedure are also regarded as irritants. Frequently companies are interested in the primary irritation potential of cosmetics and cleansers, both as a measure of consumer acceptability in the marketplace and as the basis of commercial claims support. Since the intrinsic hazard of these products is actually very similar, they are difficult to differentiate using tests designed to assess intrinsic hazard. Instead, the sensitivity of the test must be increased, and the type of response expected must be a focus. One example of a high-resolution test is the soap chamber method developed by Frosch and Kligman [27]. This requires a panel of sensitive skin individuals – defined as people who will give a strong erythema reaction (≥1.5 on a 0–4 scale) when patched overnight with either 1% sodium lauryl sulfate (SLS) or 5% soap. Panelists are then occlusively patched for 24-h occlusive patch with 5%–8% soap solution (inuse concentration). This is followed by a series of four 6-h patches on subsequent days. The skin is evaluated for erythema and dryness (scaling and fissures) 3 days after the application of the last patch. This method differentiated soap bars from a synthetic detergent based on sodium cocoyl isethionate (Dove1), the latter inducing less primary irritation (erythema) and dryness. Dove and soap are frequently used as the mild and irritating controls, respectively, to ensure adequate test sensitivity. This methodology has also been applied to differentiate the irritation potential of dishwashing liquids. A modified soap chamber test was developed to decrease testing time without reducing the ability to differentiate between soap and synthetic detergent bars based on irritation potential only [28]. This methodology involves a single 24-h exposure only – Day 1 of the Frosch-Kligman soap chamber test. Erythema is assessed by a trained observer and by use of a colorimeter, and stratum corneum barrier damage is measured as the increase in transepidermal water loss (TEWL) rate using an evaporimeter. To differentiate between products that are milder than Dove, exposure time may be increased to two consecutive days of patching. This closed patch test only produces 1 Zest and Ivory are registered trademarks of the Procter and Gamble Co. and Dove is a registered trademark of Lever Bros. Co. 493 494 F. Anthony Simion dryness if there is sufficient irritation and then only several days after patching is completed. This suggests that dryness produced by this method is a result of the primary irritation – perhaps part of the repair response. In subjects with darker skin tones, especially FitzPatrick types IV, V, and VI, hyperpigmentation is also a major response to primary dermal irritation [29]. Skin responses in the closed patch test are very dependent on climate and season. Agner and Serup showed that during the summer, the erythema and TEWL responses to SLS are greatly diminished. This emphasizes the importance of running mild and irritating controls, in order to ensure that the test has sufficient resolving power. If the soap and syndet bar cannot be distinguished, other null results should be strongly questioned. Patch testing is an assessment of hazard, the maximum potential primary irritation that could be produced. It takes no account of the way the product is used, which may modify the amount of irritation induced. To develop a better understanding of the type and severity of irritation produced in normal usage, alternative approaches such as open application and exaggerated usage tests were developed. 53.5.2 Exaggerated Usage Tests Intuitively we understand that the closer a clinical test mimics the way it is used by consumers, the more predictive of in-use problems, such as irritation, it will be. This has led to development of exaggerated wash tests for personal cleansers and immersion testing for dishwashing liquids. For personal cleansers, the physical nature of a product, such as lubricity or the presence of abrasive beads, and the method or tool used for product application will greatly influence the level of irritation experienced by consumers. For dishwashing liquids, chemical composition, dosage, and water temperature are key determinants of irritation potential. 53.5.2.1 Exaggerated Wash Tests Initially, Frosch used an exaggerated half-face wash method to distinguish soap and synthetic detergent based cleansing bars. After 2-min washes twice a day for 4–5 days, Dove was demonstrated to be milder than Zest or Ivory based on lower observable erythema and panelist self-assessed tightness and stinging. Since then, two types of exaggerated arm wash studies have been developed. Strube, Sharko, and their colleagues at Unilever have developed methods that focus on irritation (erythema and increased TEWL rates) as the primary endpoints, parameters to differentiate between products. These methods are characterized by longer periods (minutes) of washing the skin. In contrast, the methods developed by Lukacovik, Ertel, and their colleagues at Procter and Gamble (P&G) focus on skin dryness as the primary endpoint. These methods are characterized by short washes (seconds) after which the lather remains on the skin for more than 1 min, before it is rinsed away. Arm Wash Methods Using Irritation as the Primary Endpoint The antecubital flex test developed by Strube et al. uses repeated washes with an abrasive applicator to damage the stratum corneum and produce erythema in the fold of the elbow [30]. The erythema is evaluated by a trained observer and can be measured instrumentally using a colorimeter, e.g., a chromameter. Measuring increases in TEWL rates using an evaporimeter assesses stratum corneum barrier damage. The flex test is relatively sensitive to product differences, since it can distinguish between soap and bars that have about 10% of the soap replaced with a milder synthetic detergent such as sodium cocoyl isethionate. The soap chamber test was not able to differentiate between these bars. The irritation response to the products in the flex test does not vary greatly with season. This is an advantage over closed patch testing (see above) and the arm wash method of Lukacovic et al. [31], where the response is reduced by higher humidity in the summer. As the test is aggressive, the effects of damage to the outer stratum corneum are readily overwhelmed and dryness is not observed. The flex test has been criticized for being overly traumatic and very dependent on the roughness of the accessory, e.g., sponge, used to apply the product to the skin [32]. Sharko et al. developed a method able to detect differences in both dryness and primary irritation (erythema and TEWL rates) induced by a soap and Dove, a synthetic detergent bar, after 4.5 days of twice-daily treatment [33]. For smaller product differences, Sharko, Nicoll, and their colleagues showed that this method could distinguish between a soap bar and a bar soap and a low level of sodium cocoyl isethionate based on erythema and TEWL rates but not on observed dryness scores [34]. The reason for this greater discriminatory power for primary irritation rather than dryness is uncertain. Lather is applied to the volar forearms by rubbing with gloved hands for 1 min or more, several times a day. The 53 In Vivo Models of Skin Irritation increased rubbing may slightly damage the stratum corneum, enabling the surfactants to penetrate more readily. Thus irritation rather than drying potential is the main basis for differentiating between products. Furthermore the rubbing may mechanically remove the scaling of upper stratum corneum, so flaking is less apparent. (e.g. hairdressers, bar tenders and kitchen workers) have a significantly higher incidence of hand irritation than the general population [37, 38],. Therefore it is important to be able to model these effects in vivo. Below three approaches are described: immersion testing, repeated hand washing, and open application tests. Washing Studies Using Dryness as the Primary Endpoint In the method developed by Lukacovic et al., lather is applied to the forearms with a towel or muslin cloth for 10 s and remains there for an additional 90 s. The surfactant remains on the surface of the skin, and primarily damages the outer stratum corneum. This leads to visible dryness and skin roughness. Without the additional abrasion, little surfactant penetrates into the viable epidermis and primary irritation is not induced. Thus soap and mild syndet bars are differentiated based on observable dryness, tactile softness, and when the differences between products are large, on erythema as well. This methodology produces lower responses than that used by Sharko et al. and appears to differentiate products more on their ability to induce dryness, rather than on irritation potential (method II with products C and D in Nicoll et al. 1995). It is, however, very sensitive to prevailing weather conditions, especially humidity. Increasing the number of wash cycles each day may overcome this limitation. In the past, the number of samples that could be tested simultaneously has been limited for both approaches. Original published reports had focused on running a single product on each arm. In contrast, the soap chamber test could evaluate eight samples simultaneously on the same panelist. Two approaches have been described to overcome this limitation, especially for less exaggerated methods where dryness, not primary irritation (observed in closed patch tests), is the key endpoint. First, Ertel et al. described modifications to the original method that allowed up to eight products to be tested simultaneously, four on each leg [35]. Another approach is to combine different studies using meta-analysis [36]. Immersion Testing To fully assess the in-use effects of the dishwashing liquids a realistic exposure, immersion testing should be used. Repeated short-term (15- to 30-min) immersions of the hands and/or forearms are used to assess primary irritation and dryness [39, 40]. Paye et al. showed that two products that could be differentiated in a Frosch and Kligman soap chamber test could also be differentiated in a hand immersion test, if the dominant and nondominant hands are assessed separately. The products could also be differentiated using bioengineering methods such as skin conductance, and squamometry [41]. Interestingly, the dominant hand was observed to have a lower conductance, at baseline, than the nondominant hand. Similarly Grammer-West et al. showed that the Closed patch (soap chamber) test differentiates the primary irritation potential of anionic- and nonionic surfactantbased dishwashing liquids [42]. This enables a formulator to screen up to eight samples at one time, making formula optimization based on irritation potential more efficient. The method of usage or the applicator does not usually play a significant role in the amount of irritation produced in an in-use situation. However, the intensity of skin effects is dependent on the products’ composition, concentration, and temperature [43], as well as the reactivity of the subjects’ skin. 53.5.2.2 Use Testing A major cause of irritation in both the home and the work place is repeated exposure to dilute detergent solutions used for dishwashing and housekeeping, i.e., wet work. Epidemiological studies indicate that occupations that involve a great deal of hand washing, such as nursing, or repeated exposures to surfactants Repeated Hand Washing Repeated hand washing with soap has been used generate skin dryness [44]. Initially, dryness and surface corneocyte damage is produced. This can be assessed by a trained observer, by conductance measurements, and by squamometry. With more washings, erythema and stratum corneum barrier damage, measured by TEWL, are produced [45]. However, this method is more frequently used to assess the efficacy of moisturizers to prevent dryness than to compare the ability of different surfactants to elicit it. Open Application Tests Repeated exposure of a small test site to surfactantbased cleansers or other cosmetics can produce irritation even when the skin is left open to the environment, i.e., not occluded. This has been used as a 495 496 F. Anthony Simion diagnostic tool in identifying products or ingredients that have caused adverse reactions (repeated open application test – ROAT) [46]. It has also been used predictively and as a test model. Wigger-Albert, Elsner, and their colleagues have used the repeated irritation test to elicit dryness and stratum corneum barrier damage and assess the ability of protective (barrier) creams to inhibit the irritation [47]. In two related papers Wilhelm et al. compared the response of different surfactants to induce irritation and dryness in open and closed patch testing [48, 49]. They showed that closed patch testing produced more erythema rather than the dryness observed in open patch exposure. In open patching, the response was observed at higher surfactant concentration: 7.5% compared with 0.5% in occlusive patches. Furthermore, in occlusive patches the anionic surfactant SLS gave stronger stratum corneum barrier disruption as measured by TEWL and dryness as measured by conductance. However, the erythema response was similar with observer and colorimeter measurements. the flex wash or the volar forearm wash test have the potential of removing skin flakes, resulting in a loss of sensitivity. 53.6.1 In order to demonstrate that the cleanser delivers a benefit to the skin, the skin must start out in poor condition. As with moisturizer efficacy studies, the skin should be dry at baseline (dryness score of 2 or more on a 0–4 scale). It is best to run the test on a body site that readily showed skin dryness, such as the lower legs or the dorsal aspect of the forearms. The former has sufficient area to enable multiple products (and a no-product control) to be tested simultaneously. Using a within-subject design enables potentially large person-to-person variations to be eliminated. There are three main ways of producing dry skin: • 53.6 Models for Measuring the Moisturizing Potential of Cleansers • • Previously, most evaluations of cleanser effects on the skin have been to assess primary irritation or drying potential. Such studies start with the skin in good condition and the extent by which parameters such as erythema and dryness worsen is evaluated. However, moisturization potential has the implication that the skin condition is improved. Therefore, a different experimental design is required. Such studies incorporate various aspects of moisturizer efficacy testing, especially with regard to: • • Starting with dry skin, to enable improvement to be observed Using moisturizer end-points, such as assessments of skin dryness and skin hydration Testing on Dry Skin Rely on cold weather frequently occurring during the winter to produce dryness. Select people that have a predisposition to dry skin. As people age, they exhibit more dry skin, especially at the extremities. Prewash their test area with a drying cleanser. Combining the first and second methods is probably the best approach. Relying on the weather alone can be risky, as a few warm, humid days will significantly reduce the level of dryness observed. Giving the panelists a drying soap bar for regular cleansing has two great disadvantages. Firstly, the soap bar may interfere with the effects of the moisturizing cleanser, and consumers do not use two cleansing products on the same body sites. Secondly, Ertel et al. suggested that artificially drying out the skin with soap reduces the response compared with naturally dry skin. The basis of this is unclear, but it contrasts with the enhanced irritation response observed when subclinically or mildly irritated skin is exposed to an irritant. Together with: • Application methods that reflect how the cleansing products are used. Ideally the application method should not greatly affect dry skin, especially removing it. Thus the method initially described by Lukakovic et al. in 1988 is probably most appropriate method. Methods that involve rubbing for a longer time, for example, 53.6.2 Measuring the Clinical Effects of Moisturizing Cleansers on the Skin Based on the approaches used to assess moisturizer efficacy, the two main parameters to assess the moisturizing potential of cleansing products are: • Skin dryness 53 In Vivo Models of Skin Irritation Table 1. Overview of bioengineering instruments used to assess skin irritation Skin characteristic Interpretation Issues Instrumentation Transepidermal water loss Measure of stratum corneum barrier integrity/damage Measures water regardless of source, e.g., sweat Must use in temperature and humidity controlled environment Evaporimeter DermaLab TEWL probe Tewameter Skin color/redness Erythema Chromameter Erythema meter Dermaspectrometer Blood flow Irritation increases blood blow Due to laser, cannot in the superficial dermis be used near eyes Laser Doppler velocimeter Desquamation index Skin dryness (scaling/flaking) Reproducible sampling of the skin D-Squame tape Image analysis Skin conductance/capacitance Skin hydration Materials that change dielectrics of skin will effect reading Skicon 200 DermaLab Nova meter Stained D-Squame (squamometry) Reproducible sampling of the skin High levels of damage can disintegrate cells and cause loss of dye D-Squame tape Polymultichrome stain Chromameter • Skin surface integrity Skin hydration It is always advisable to use multiple methods for assessing efficacy, as each individual method has potential shortcomings. The use of a panoply of methods will yield a fuller assessment of skin condition. Skin Dryness. Traditionally, a trained observer, using an ordinal scale, has evaluated skin dryness. However, this approach has two major drawbacks. Firstly, it is very dependent on the evaluator, and great care must be taken to ensure reproducibility between evaluators, studies, and between different testing laboratories. In this, a standardized photographic scale is very helpful. Secondly, there are many factors that can reduce the appearance of dryness without any benefit to the skin. These include short-term humidity and occlusive lotions that matte the dry skin flakes down without removing them. These problems can be overcome by using a sticky tape to sample the skin's surface, such as DeSquame tape (CuDerm Inc. Dallas TX). The tape is pressed on to the skin's surface and then removed. The greater the scaling, the more skin flakes are removed by the tape. These can be quantified by using an analog scale or by image analysis [50]. The tape will remove the flakes even if they are matted down or obscured by hydration. The use of DeSquame tape has been expanded to assess the damage to surface corneocytes, i.e., squamometry. This is discussed in greater detail above, but has been shown to detect damage to the skin's surface before any visible dryness is apparent [51]. Conductance and Capacitance. Conductance and/ or capacitance are frequently used to measure skin hydration. This approach has been supported empirically by Morrison and Scala [52], who showed a strong correlation between dryness and reduction in skin conductance (measured by a Skicon 200) and capacitance (measured by a Nova dermal phase meter). There are two explanations of how skin conductance measures dryness. Firstly, as the skin becomes drier, the concentration of water in the stratum corneum is reduced. As water is a good conductor compared with the more hydrophobic stratum corneum, a reduction in water activity will reduce conductance. Another possible mechanism by which dryness reduces conductance is that as scales develop, air pockets are formed in the damaged stratum corneum. As air is a poor conductor, this scaling also results in reduced conductance. Clearly these two mechanisms are not mutually exclusive and may occur simultaneously. It should be stressed that residues left on the skin's surface may modify conductance in the absence of 497 498 F. Anthony Simion dryness. For instance, petrolatum, silicones, and mineral oil are good insulators and can reduce conductance even as they moisturize the skin. Conductance data should be evaluated based on the product's composition and an understanding of which ingredients may remain on the skin after rinsing. 53.7 Bioengineering Measurements of Skin Condition The last 20 years have seen a great expansion in the number and sophistication of bioengineering instruments to assess skin condition. These instruments provide a quantitative assessment of a single characteristic of the skin. Based on our knowledge of skin physiology and irritation processes, this is used as a measure of irritation. Like all metrics, bioengineering methods can be misleading, when used inappropriately. They do give objective responses that can be reduced to a single number or series of numbers. However, each measurement can be effected by parameters that have nothing to do with skin irritation. For instance an evaporimeter measures water loss from the skin's surface and cannot differentiate water loss due to sweating from water loss caused by disruption of the stratum corneum barrier. Thus the environmental temperature must be kept below that causing most panelists to sweat (70°F). For most bioengineering methods, the environmental and other experimental conditions must be tightly controlled and the data carefully interpreted. Guidelines published for many instrumental methods such as transepidermal water loss should be followed. Table 1 shows the bioengineering methods most frequently used to measure irritation. References 1. Malten KE. Thoughts on irritant contact dermatitis. Contact Dermatitis 1981; 7:238–247 2. Kligman AM. The invisible dermatoses. Arch Dermatol 1991; 127:1375–1382 3. Freeman S, Maibach HI. Study of irritant contact dermatitis produced by repeated patch testing with sodium lauryl sulfate and assessed by visual methods, transepidermal water loss and laser Doppler velocimtery. J Am Acad Dermatol 1988; 19:496 4. De Groot AC, Nater JP, van der Lende R, Ricken B. Adverse effects of cosmetics and toiletries – a retrospective study in a general population. Int J Cosmet Sci 1987; 9:255 5. Frosch PJ, Kligman AM. A method for appraising the stinging capacity of topically applied substances. J Soc Cosmet Chem 1977; 28:197 6. Green BG, Bluth J. Measuring the chemosensory irritability of human skin. J Toxicol Cut Ocular Toxicol 1995; 14:23–48 7. Yosipovitch G, Maibach HI. Effect of topical pramoxine on experimentally induced pruritus in humans. J Am Acad. Dermatol 1997; 37:278–280 8. Leopold CS, Maibach HI. Percutaneous penetration of local anesthetic bases: Pharmacodynamic measurements. J Invest Dermatol 1999; 113:304–307 9. Simion FA, Rhein LD, Morrison BM Jr, Scala DD, Salko DM, Kligman AM, Grove GL. Self-perceived sensory responses to soap and synthetic detergent bars correlate with clinical signs of irritation. J Am Acad Dermatol 1995; 32:205–211 10. Paye M, Cartiaux Y. Squamometry: a tool to move from exaggerated to more realistic application conditions for comparing the skin compatibility of surfactant based products. Int J Cosmet. Sci 1999; 21:59–68 11. Pierard GE, Arrese JE, Rodriguez C, Daskaleros PA. Effects of softened and unsoftened fabrics on sensitive skin. Contact Dermatitis 1994; 30:286–291 12. Wilhelm K-P, Cua AB, Wolff HH, Maibach HI. Surfactant induced stratum corneum hydration in vivo: prediction of the irritation potential of anionic surfactants. J Invest Dermatol 1993; 101:310–315 13. Rhein LD, Robbins CR, Fernee K, Cantore R. Surfactant structure effects on swelling of isolated human stratum corneum. J Soc Cosmet Chem 1986; 37:125–139 14. Imokawa G, Mishima Y. Cumulative effect of surfactants on cutaneous horny layers: adsorption onto human keratin layers in vivo. Contact Dermatitis 1979; 5:357–366 15. Kawai M, Imokawa G. The induction of skin tightness by surfactants. J Soc Cosmet Chem 1984; 147–156 16. Cua A, Wilhelm KP, Maibach HI. Cutaneous sodium lauryl sulfate irritation potential: age and regional variability. Br J Dermatol 1990; 123:607–613 17. Rougier A, Lotte C, Maibach HI. In vivo relationship between absorption and transepidermal water loss. In: Bronaugh RL, Maibch HI (eds) Topical absorption of dermatological products. Marcel Dekker, New York, p 115–128 18. Allenby CF, Basketter DA, Dickens A et al. An arm immersion model of compromised skin. (I) Influence on irritation reactions. Contact Dermatitis 1993; 28:84–88 19. Frosch PJ, Kligman AM. The chamber scarification test for irritancy. Contact Dermatitis 1976; 2:314–324 20. Berardesca E, Cespa M, Farinelli N, Rabbiosi G, Maibach H. In vivo transcutaneous penetration of nicotinates and sensitive skin. Contact Dermatitis 1991; 25:35–38 21. Agner T, Serup J. Seasonal variation of skin resistance to irritants. Br J Dermatol 1989; 121:323–328 22. Agner T. Susceptibility of atopic dermatitis patients to irritant dermatitis caused by sodium lauryl sulfate. Atcta Derm Vernerol (Stockh) 1990; 71:296–300 53 In Vivo Models of Skin Irritation 23. Pinnagoda J, Tupker RA, Ceonraads PJ, Nater JP. Prediction of susceptibility to an irritant response by transepidermal water loss. Contact Dermatitis 1989; 20:341–346 24. Simion FA, Rhein LD, Grove GL, Wojtowski J, Cagan RH, Scala DD, Sequential order of skin responses to surfactants in a soap chamber test. Contact Dermatitis 1991; 25:242– 249 25. Phillips L, Steinberg M, Maibach HI, Akers WA. A comparison of rabbit and human skin response to certain irritants. Toxicol Appl Pharmacol 1972; 21:369–382 26. Robinson MK, McFadden JP, Basketter DA. Validity and ethics of the human 4-h patch test as an alternative method to assess acute skin irritation potential. Contact Dermatitis 2001; 45:1–12 27. Frosch PJ, Kligman AM. The soap chamber test: a new method for assessing irritancy of soaps. J Am Acad Dermatol 1979; 1:35–41 28. Babulak SW, Rhein LD, Scala DD, Simion FA, Grove GL. Quantitation of erythema in a soap chamber test using a Minolta Chroma (Reflectance) meter: comparison of instrumental results with visual assessments. J Soc Cosmet Chem 1986; 37:475 29. Morrison BM, Babulak SW, Scala DD, Simion FA, WooMing G, Gyening I, Kenney JA, Kligman AM. Evaluation of the response of African-American skin to facial cleansing products using a soap chamber test. Scientific exhibit at the 51st American Academy of Dermatology Annual Meeting San Francisco CA, 1992 30. Strube DD, Koontz SW, Murahata RI, Theiler RF. The flex wash test: a method for evaluating the clinical mildness of cleansing products. J Soc Cosm Chem 1988; 39:355 31. Lukacovic MF, Dunlap FE, Michaels SE, Visscher MO, Watson DD. Forearm wash test to evaluate the clinical mildness of cleansing products. J Soc Cosm. Chem 1988; 39:355 32. Keswick BH, Ertel KD, Visscher MO. Comparison of exaggerated and normal use techniques for assessing the mildness of personal cleansers. J Soc Cosmet Chem 1992; 43:187 33. Sharko PT, Murahata RI, Leyden JJ, Grove GL. Arm wash with instrumental evaluation – a sensitive technique for differentiating irritation potential of personal washing products. J Dermal Clin Eval Soc 1991; 2:19 34. Nicoll GA, Murahata RI, Grove GL Barrows J, Sharko PT. The relative sensitivity of two arm-wash methods for evaluating the mildness of personal washing products. J Soc Cosmet Chem 1995; 46:129–140 35. Ertel KD, Neumann PB, Hartwig PM, Rains GY, Keswick BH. Leg wash protocol to assess the skin moisturization potential of personal cleansing products. Int J Cosmet Sci 1999; 21:383–397 36. Neumann PB, Ertel KD, Keswick BH, Rains GY. Meta analysis is a cost effective tool for estimating mildness differences. J Soc Cosmet Chem 1997; 48:283–288 37. Halkier-Sorensen L. Notified occupational skin diseases in Denmark. Contact Dermatitis 1996; 35 [Suppl 1]:1 38. Wall LM, Gebauer KA. Occupation skin disease in Western Australia. Contact Dermatitis 1991; 24:101–109 39. Kooyman DJ, Snyder FH. Tests for mildness of soap. Arch Dermatol 1942; 46:846 40. Justice JD, Travers JJ, Vinson LJ. The correlation between animal tests and human tests in assessing product mildness. Toilet Goods Assoc Proced of the Scientific Section 1961; 35:12 41. Paye M, Gomes G, Zerwick CR, Pierard GE, Grove GL. A hand immersion test under laboratory controlled usage conditions: the need for sensitive and controlled assessment methods. Contact Dermatitis 1999; 40:133–138 42. Grammer-West NY, Fitzpatrick JE, Jackson RL, Horton H, Daminano MA. Comparison of the irritancy of hand dishwashing liquids with modified patch testing methods. J Am Acad Dermatol 1996; 35:258–260 43. Clarys P, Manou I, Barel AO. Influence of temperature on irritation in the hand/forearm immersion test. Contact Dermatitis 1997; 36:240–245 44. Highley DR, Savoyka VO O’Neill JJ, Ward JB. A stereomicroscopic method for determination of moisturizing efficacy in humans. J Soc Cosmet Chem 1976; 27:351–363 45. Simion FA, Babulak SW, Morrison BM Jr, Rhein LD, Scala DD. Experimental method for soap-induced dryness in absence of erythema. Scientific Exhibit at the American Academy of Dermatology 50th Annual Meeting. December 1991 46. Hannuksela M, Salo H. The repeated open application test. Contact Dermatitis 1986; 14:221–227 47. Wigger-Alberti W, Krebs A, Elsner P. Experimental irritant contact dermatitis due to cumulative exposure to sodium lauryl sulphate and toluene: single and concurrent application. Br J Dermatol 2000; 143:551–556 48. Wilhelm KP, Freitag G, Wolff HH. Surfactant induced skin irritation and skin repair: evaluation of an acute human irritation model by non-invasive techniques. J Am Acad Dermatol 1994; 30:944–949 49. Wilhelm KP, Freitag G, Wolff HH. Surfactant induced skin irritation and skin repair: evaluation of a cumulative human irritation model by non-invasive techniques. J Am Acad Dermatol 1994; 31:981–987 50. Schatz. H, Kligman AM, Manning S, Stoudemayer T. Quantification of dry (xerotic) skin by image analysis of scales removed by adhesive discs (D-Squames). J Soc Cosmet Chem 1993; 44:53–63 51. Simion FA, Witt PS, Rau AH, Thueneman PJ, Peters HE. Stratum corneum damage produced by surfactants during dry skin induction. Scientific exhibit at the American Academy of Dermatology Meeting, 1995 52. Morrison BM Jr, Scala DD. Comparison of instrumental measurements of skin hydration J Toxicol Cut Ocular Toxicol 1996; 14:305–414 499