Numbness - Research portal
advertisement

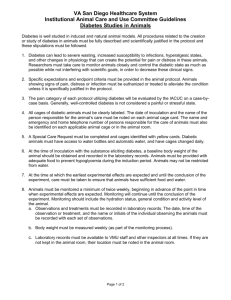
Tilburg University 'Numbness of the feet' is a poor indicator for polyneuropathy in type 2 diabetic patients van de Poll-Franse, L.; Valk, G.D.; Dekker, J.H.; Heine, R.J.; van Eijk, J.T. M. Published in: Diabetic Medicine: Journal of the British Diabetic Association Publication date: 2000 Link to publication Citation for published version (APA): Franse, L. V., Valk, G. D., Dekker, J. H., Heine, R. J., & van Eijk, J. T. M. (2000). 'Numbness of the feet' is a poor indicator for polyneuropathy in type 2 diabetic patients. Diabetic Medicine: Journal of the British Diabetic Association, 17(2), 105-110. General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. ? Users may download and print one copy of any publication from the public portal for the purpose of private study or research ? You may not further distribute the material or use it for any profit-making activity or commercial gain ? You may freely distribute the URL identifying the publication in the public portal Take down policy If you believe that this document breaches copyright, please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 02. okt. 2016 `Numbness of the feet' is a poor indicator for polyneuropathy in Type 2 diabetic patients L. V. Franse*, G. D. Valk*, J. H. Dekker*, R. J. Heine*² and J. T. M. van Eijk³ Abstract *Institute for Research in Extramural Medicine, Vrije Universiteit, Amsterdam, The Netherlands ²Department of Endocrinology, Academisch Ziekenhuis Vrije Universiteit, Amsterdam, The Netherlands ³Department of Medical Sociology, Universiteit van Maastricht, The Netherlands Received 10 November 1998; revised 2 September 1999; accepted 17 October 1999 Aims To identify neuropathic sensory symptoms associated with a clinical neurological examination (CNE) and to investigate whether these symptoms could be used as a diagnostic or screening tool for diabetic polyneuropathy in general practice. Methods Five hundred and eighty-eight patients with Type 2 diabetes, recruited from 26 general practices in the Netherlands, underwent a CNE and completed a diabetes symptom checklist that included 10 items on neuropathic sensory symptoms. Linear regression analyses were performed to assess the association between neuropathic symptoms and CNE. Receiver operating characteristic (ROC) curves were created to assess the diagnostic properties of neuropathic symptoms. Results In this population, with a mean age of 66.8 years, 32% were identi®ed with diabetic polyneuropathy according to the CNE. Variables that showed the strongest association with CNE score were age (b = 0.41), symptoms of sensory alteration (b = 0.27), and the item `numbness of the feet' (b = 0.35) in particular. ROC curves showed that prediction of diabetic polyneuropathy from these symptoms was unsatisfying. The sensitivity and speci®city of daily symptoms of `numbness of the feet' were 28% and 93%, respectively, in patients < 68 years, and 22% and 92%, respectively, in patients > 68 years. Conclusions Identi®cation of neuropathic sensory symptoms is not useful as a diagnostic or even a screening tool in the assessment of diabetic neuropathy in daily practice. Therefore, the results reported in this paper mandate an annual foot examination by the general practitioner. Diabet. Med. 17, 105±110 (2000) Keywords diabetic neuropathies, healthcare, Type 2 diabetes mellitus neurological examination, primary Abbreviations CNE, clinical neurological examination; GP, general practi- tioner Introduction Foot ulceration and lower limb amputation are common complications of diabetes. In a primary healthcare setting, Correspondence to: Lonneke Franse MPH, Institute for Research in Extramural Medicine, Vrije Universiteit, Van der Boechorststraat 7, 1081 BT Amsterdam, The Netherlands. E-mail: lv.franse.emgo@med.vu.nl ã 2000 British Diabetic Association. Diabetic Medicine, 17, 105±110 one in every seven (14.3%) patients with Type 2 diabetes was found to have an active foot ulcer (Wagner stage 1 or 2: super®cial to deep ulcer) or pre-ulcer (Wagner stage 0: hard skin with or without macerating changes) [1,2]. Diabetesrelated amputations accounted for 46.9% of the total number of lower extremity amputations (n = 6680) in the Netherlands in 1991 and 1992 [3]. 105 106 `Numbness of feet' and polyneuropathy · L. V. Franse et al. Early diagnosis of diabetic polyneuropathy can reduce patient morbidity by allowing preventive therapeutic interventions, including patient education and regular foot examinations [4,5]. Established tests to identify patients at risk for developing diabetic foot complications are tests of warm and cold thermal perception [6], and nerve conduction [7]. These involve the use of expensive equipment and are not quick or easy. For the detection of diabetic polyneuropathy in daily clinical practice, a simple, sensitive and inexpensive screening method is the clinical neurological examination (CNE) which includes pinprick sense, light touch sense, vibration sense and ankle jerk. This simple CNE has recently been validated and shown to be adequate for use in daily clinical practice [8,9]. Despite the fact that guidelines recommend an annual foot examination by the general practitioner (GP) for patients with diabetes [10,11], chart reviews reveal that foot assessment for neuropathy is only seldom performed [12]. Only one-third of all GPs perform a CNE, owing to lack of time. Instead, the identi®cation of patients with diabetic polyneuropathy in daily practice is often based on interpretation of the symptoms reported by the patient. Symptoms of sensory alteration have been associated with both the CNE and the neurophysiological examination [13]. The question arises as to whether or not patient history can replace the CNE in daily clinical practice. The aim of this study was to identify neuropathic sensory symptoms associated with CNE outcome and to investigate whether those symptoms could be used as a diagnostic or screening tool for diabetic polyneuropathy in general practice. Patients and methods Five hundred and eighty-eight patients with Type 2 diabetes were recruited from 26 general practices in the Netherlands. Participants were identi®ed by their GP. Known and newly diagnosed patients with Type 2 diabetes who received diabetes care in general practice and were able to complete a questionnaire in Dutch were eligible, if the diagnostic evidence met the criteria of the Dutch College of General Practitioners for Type 2 diabetes [10]. Patients were excluded if they received diabetes care in hospital outpatient clinics, but not if they were under specialist care for retinopathy or cardiovascular comorbidity. Participating GPs were known to refer about 30% of their Type 2 diabetes patients to hospital outpatient clinics for diabetes care [14]. Patients with other aetiological factors that might in¯uence sensory functions of the skin of the lower extremities (e.g. alcohol abuse, use of neurotoxic drugs, abnormal kidney function) were excluded from the analyses. One patient was excluded for this reason (serum creatinine 333 mmol/l). Patients who agreed to participate and gave written informed consent were included in the study. Forty-nine refused to participate. They did not differ from the participating patients in age or sex, but their diabetes duration was on average 2 years' longer (P = 0.025). The study was approved by the Medical Ethics Committee of the Academic Hospital of the Vrije Universiteit in Amsterdam, The Netherlands. Measurements Participants were sent a diabetes symptom checklist to complete before the clinical examination. These were performed by a trained research fellow at the practice of the patient's GP. The checklist was not looked at before the examination. Blood samples were drawn within 1 week after the clinical examination, after an overnight fast. Glycated haemoglobin (HbA1c) was determined by ion-exchange high-performance liquid chromatography, using a Modular Diabetes Monitoring System (Bio-Rad, Veenendaal, the Netherlands). Assessment of the severity of symptoms The Type 2 Diabetes Symptom Checklist (DSC-Type 2) was used to measure the severity of neuropathic sensory symptoms. This comprises 34 questions, and measures the occurrence of physical and psychological symptoms related to Type 2 diabetes and its possible complications. Ten concern symptoms related to sensory polyneuropathy. Grootenhuis and Valk factor-analysed the 10 questions included in the DSC-Type 2 [13,15] and found two dimensions (factors): the ®rst apparently represent symptoms of sensory alteration (tingling sensations in the hands/ ®ngers, numbness ± diminished sensation ± of the hands, strange sensation in the legs or feet, tingling sensation in the lower legs, numbness ± diminished sensation ± of the feet, tingling sensation in the arms/legs at night), while the second dimension represents symptoms of neuropathic pain (shooting pain in the legs, burning pain in the legs, pain in the legs during walking, burning pain in the calves at night). The patients were asked how often the symptoms had occurred during the past month. The answers were scored as 0 ± not at all; 1 ± one or more times per month; 2 ± one or more times per week; 3 ± daily. The total score for the sensory alteration dimension could thus vary between 0 and 18 and the total score for the neuropathic pain dimension could vary between 0 and 12. Scoring system for the clinical neurological examination All patients underwent a CNE as described by Valk et al. [9], modi®ed by excluding assessments of muscle strength and great toe joint position sense [16]. All tests were scored based on two similar results out of three tests. Pinprick sense and light touch sense (cotton wool) of the dorsum of the feet were tested on the mid-foot and compared to proximal sensation (ankles). Vibration sense (128 Hz tuning fork) of ®rst toes was compared to vibration sense of ankles, and vibration sense of ankles was compared to vibration sense of patella. Ankle jerks were compared to knee re¯exes. Pinprick sense, light touch sense, vibration sense of toes and ankles, and ankle re¯exes were separately scored for both feet as 0 ± normal, 1 ± impaired in comparison with proximal and 2 ± absent; summing up to a maximum score of 20. Additionally, light touch sense was related to the anatomical level below which it was impaired, and ã 2000 British Diabetic Association. Diabetic Medicine, 17, 105±110 Original articles was scored as 0 ± no abnormalities, 1 ± toe, 2 ± mid-foot, 3 ± ankle, 4 ± mid-calf and 5 ± knee. If there was a difference at this level between the right and the left side, the more abnormal side was scored. The outcome of the total score of the CNE (the sum of the scores of the sensory modalities, the ankle re¯exes, and the anatomical level below which light touch sense was impaired) could vary between 0 and 25. As muscle strength and position sense do not add to the total score, the actual distribution of the modi®ed CNE score was assumed to be the same as in the original description. Valk et al. [8] determined the best diagnostic polyneuropathy cut-off point on the scale of measurement to achieve maximum sensitivity (87.0%) and reasonable speci®city (62.2%) to be > 4 for the CNE. Therefore, a total score higher than 4 was graded as polyneuropathy. Statistical analyses Results were analysed with SPSS for Windows software (SPSS, Chicago, IL) [17]. Linear regression analysis was applied to assess the univariate association between the different variables and the CNE outcome. Standardized residuals plots showed that linear regression analyses were appropriate. In addition, linear regression analyses with natural log transformed, normally distributed variables showed no different results. Two-by-two contingency tables were formed for various cutoff points to examine the performance characteristics of neuropathic symptoms as a diagnostic tool for neuropathy (CNE > 4). Sensitivity and speci®city data were summarized in Receiver operating characteristics (ROC) curves. ROC curve analyses used MedCalc for Windows software (Mariakerke, Belgium). Results The characteristics of the study population are shown in Table 1. Thirty-two per cent of the participants had a CNE score > 4 and were graded as polyneuropathy. In univariate regression analyses, age, diabetes duration, symptoms of pain, and symptoms of sensory alteration were signi®cantly associated with the CNE score (Table 2). Analyses of the association between the single items of neuropathic symptoms and CNE score were performed to investigate whether one question would show a stronger association and have the same or better diagnostic properties compared to a complete dimension or checklist. The single item `numbness of the feet' showed the strongest association with CNE score, stronger than the complete subdimensions `sensory alteration' or `pain'. The other nine items were all signi®cant, but the association with CNE score was weaker; the standardized b varied from 0.09 to 0.23 (data not shown). As age showed the strongest association with CNE score, the diagnostic value of subdimensions `pain', and `sensory alteration', and the single item `numbness of the feet' according to age were examined by dichotomizing age by its median value (68 years). Figures 1,2,3 present the ROC curve analyses of the predictive value of `pain', `sensory alteration', and `numbness of the feet' for a CNE score > 4 in patients < 68 years and patients > 68 years. For symptoms of `pain', the area Table 2 Univariate linear regression analyses with the clinical neurological examination as outcome variable Variable Age (years) Sex, male Diabetes duration (years) HbA1c (%) Neuropathic symptom(s) Pain (4 items) Sensory alteration (6 items) Numbness of the feet (1 item) Standardized coef®cients/beta P 0.41 ± 0.04 0.13 0.08 < 0.001 0.34 0.002 0.06 0.16 0.27 0.35 < 0.001 < 0.001 < 0.001 Table 1 Characteristics of the Type 2 diabetic patients (n = 588) Variable Age (years) Sex (men) Diabetes duration (years) HbA1c (%) CNE-score (0±25) CNE > 4 (neuropathy) Neuropathic symptoms score Pain (0±12) Sensory alteration (0±18) 66.8 6 10.4² 47% (276)³ 5 (2±10)§ 7.3 6 1.4² 4 (0±6)§ 32% (190)³ 0 (0±3)§ 1 (0±6)§ CNE, clinical neurological examination. ²Mean 6 SD. ³Per cent (n). §20th to 80th percentile. ã 2000 British Diabetic Association. Diabetic Medicine, 17, 105±110 107 Figure 1 Receiver operating characteristic curve for neuropathic symptoms of `pain'. 108 `Numbness of feet' and polyneuropathy · L. V. Franse et al. under the curve (AUC) for both age groups was not signi®cantly different from 0.5. Symptoms of sensory alteration and `numbness of the feet' both showed better performance characteristics, but the AUC was never greater than 0.66. At the cut-off point `daily symptoms of numbness of the feet', 28% of the patients < 68 years with CNE > 4 (polyneuropathy) were detected as such (sensitivity), and 93% of the patients with CNE < 4 were categorized with no polyneuropathy according to this symptom (speci®city) (Fig. 3). For those > 68 years, the sensitivity and speci®city were virtually the same, 22% and 92%, respectively. However, as the prevalence of polyneuropathy was signi®cantly higher among those > 68 years compared to those < 68 years (P < 0.001) (Table 3), the positive predictive value of `daily symptoms of numbness of the feet' was higher in those > 68 years (71.7%) compared to those < 68 years (41.4%). In the younger age group, 200 (89.7%) patients who had neverhadsymptomsof`numbnessofthefeet'duringthepast month were identi®ed with no polyneuropathy according to the CNE score. Of the 23 (10.3%) patients who never had symptoms of `numbness of the feet', but were identi®ed with polyneuropathy, 19 had aCNEscore < 8,twohad ascore of 10 and two had a score of 12 (data not shown). A previously reported validation study mainly involved relatively younger patients [8]. Additional analysis revealed that in the present study, 40% of the patients > 68 years were identi®ed with an impaired or absent vibration sense, whereas only 10% of those < 68 years had an impaired or absent vibration sense (data not shown). Figure 2 Receiver operating characteristic curve for neuropathic symptoms of `sensory alteration'. 100 Sensitivity (%) 80 < 68 60 ≥ 68 40 Area under curve (95% CI) < 68: 0.66 (0.57– 0.75) ≥ 68: 0.59 (0.50– 0.68) 20 0 0 20 40 60 80 1-specificity (%) Figure 3 Receiver operating characteristic curve for neuropathic symptoms of `numbness of the feet'. 100 Discussion This study demonstrates that the identi®cation of neuropathic sensory symptoms cannot replace the CNE as a diagnostic tool in the assessment of early diabetic polyneuropathy in Type 2 diabetic patients in general practice. Although symptoms of pain, sensory alteration and `numbness of the feet' in particular, showed a signi®cant association with CNE score, the prediction of polyneuropathy from the neuropathic symptoms was not satisfactory. Table 3 Prevalence of polyneuropathy (clinical neurological examination (CNE) score > 4) by age and frequency of symptoms of `numbness of the feet' CNE score > 4 (neuropathy) How often in the past month have you had symptoms of `numbness of the feet'? < 68 years (n = 286) > 68 years (n = 302) Not at all One or more times per month One or more times per week Daily P-trend Total prevalence of neuropathy 23 (10.3%) 5 (22.7%) 3 (27.3%) 12 (41.4%) < 0.001 15.0% (n = 43) 90 (41.7%) 8 (53.3%) 16 (64.0%) 33 (71.7%) < 0.001 48.7% (n = 147) ã 2000 British Diabetic Association. Diabetic Medicine, 17, 105±110 Original articles The results of this study con®rm earlier ®ndings in a hospital setting using the same symptom checklist [13]. Among 68 patients referred to the neurologist with suspected polyneuropathy, symptoms of sensory alteration showed a stronger association with CNE score than symptoms of pain [13]. Dyck et al. [18] also found that the number of neuropathic symptoms was signi®cantly associated with the neurological abnormality score according to the Neurological Disability Score but did not make a distinction between the different dimensions of sensory alteration and pain. The weak association, found between diabetes duration and the CNE score was explained by the association of age with CNE score (data not shown). Other studies have been found to be inconsistent with regard to the association of diabetic neuropathy with age, duration of diabetes and hyperglycaemia [19±23]. ROC curves showed that prediction of diabetic polyneuropathy from the different neuropathic symptoms was unsatisfactory. The discriminating ability of symptoms of pain was not better than chance. The ROC curves of symptoms of sensory alteration and `numbness of the feet' showed better discriminating abilities, but were still poor. Daily symptoms of `numbness of the feet' had high speci®city, but low sensitivity. To calculate the positive and negative predictive values of a diagnostic instrument, the prevalence (prior odds) of a `disease' in the studied population is also important [24]. As the prevalence of polyneuropathy differed more than 30% between the two age groups, the positive and negative predictive values were also different. Although the positive predictive value of `daily symptoms of numbness of the feet' was highest among those > 68 years, in this age group 28% of the patients who reported daily symptoms still did not have objective evidence of diabetic neuropathy while 45% of patients who did not report daily symptoms of `numbness of the feet', did. Feldman et al. [25] also concluded that symptoms might not always indicate underlying neuropathy, ®nding that an equal number of patients with and without diabetic neuropathy answered up to six relevant questions positively. Almost 90% of those aged < 68 years who never had symptoms of `numbness of the feet' had no evidence of diabetic polyneuropathy at examination. The `missed' 10% who did have diabetic polyneuropathy had relatively low CNE scores. This suggests that asking younger Type 2 patients about `numbness of the feet' might be a useful screening instrument. However, as there are no longitudinal data of the consequences of not performing a CNE among the 10% that do not have complaints but suffer a mild neuropathy, even avoiding CNE is this group is inadvisable. The limitations of the present study should be considered. Patients receiving diabetes care in hospital outpatient clinics were excluded. Although this does not ã 2000 British Diabetic Association. Diabetic Medicine, 17, 105±110 109 in¯uence the conclusions in the general practice population, these cannot be extrapolated to hospital clinic patients or indeed to patients unable to complete a questionnaire in Dutch. It is possible that the patients referred to a specialist for diabetes care had a worse HbA1c, explaining the fairly good HbA1c values seen in the study population. Although, the 49 participants who refused participation had a longer duration of Type 2 diabetes, it is unlikely that this in¯uenced the main outcome as diabetes duration was weakly associated with CNE outcome. The allocation of `aching in the calves when walking' to the domain of polyneuropathic pain is open to criticism. It is debatable whether one item can differentiate between neuropathic pain and peripheral vascular pain. Based on content, and also for statistical reasons, the allocation of this item to the pain dimension seemed plausible at the time of development and validation of the symptom checklist [13,15]. There is no gold standard for the assessment of polyneuropathy, with which new tests can be compared. Although warm and cold thermal perception [6], and nerve conduction tests [7] are extensively studied and generally accepted, they are not very suitable for use in daily clinical practice. It is questionable whether a CNE cut-off score > 4 for diabetic neuropathy is useful in older patients as it is well documented (and con®rmed in the present study) that vibration sense in the elderly is often absent [26,27]. Raising the CNE cut-off point to > 8 for the diagnosis of neuropathy in patients > 68 years decreased the prevalence of neuropathy in this subgroup to 18%. However, it did not change the sensitivity or speci®city of the question `numbness of the feet' and therefore did not change the outcome of interest. In conclusion, identi®cation of neuropathic sensory symptoms is not useful as a diagnostic or even a screening tool in the assessment of diabetic neuropathy in daily practice. Therefore, the results reported in this paper mandate an annual foot examination by the general practitioner. Acknowledgements The authors would like to thank Jos Twisk PhD for his help in the statistical analyses. References 1 de Sonnaville JJ, Colly LP, Wijkel D, Heine RJ. The prevalence and determinants of foot ulceration in type II diabetic patients in a primary health care setting. Diabetes Res Clin Pract 1997; 35: 149± 156. 2 Wagner FWJ. The dysvascular foot: a system for diagnosis and treatment. Foot Ankle 1981; 2: 64±122. 3 Lavery LA, van Houtum WH, Harkless LB. In-hospital mortality and disposition of diabetic amputees in The Netherlands. Diabet Med 1996; 13: 192±197. 110 `Numbness of feet' and polyneuropathy · L. V. Franse et al. 4 Bild DE, Selby JV, Sinnock P, Browner WS, Braveman P, Showstack JA. Lower-extremity amputation in people with diabetes. Epidemiology and prevention. Diabetes Care 1989; 12: 24±31. 5 Boulton AJ. Lowering the risk of neuropathy, foot ulcers and amputations. Diabet Med 1998; 15: S57±9: S57±S59. 6 Vinik AI, Suwanwalaikorn S, Stansberry KB, Holland MT, McNitt PM, Colen LE. Quantitative measurement of cutaneous perception in diabetic neuropathy. Muscle Nerve 1995; 18: 574±584. 7 Eriksson KF, Nilsson H, Lindgarde F et al. Diabetes mellitus but not impaired glucose tolerance is associated with dysfunction in peripheral nerves. Diabet Med 1994; 11: 279±285. 8 Valk GD, de Sonnaville JJ, van Houtum WH et al.The assessment of diabetic polyneuropathy in daily clinical practice: reproducibility and validity of Semmes Weinstein mono®laments examination and clinical neurological examination. Muscle Nerve 1997; 20: 116± 118. 9 Valk GD, Nauta JJ, Strijers RL, Bertelsmann FW. Clinical examination versus neurophysiological examination in the diagnosis of diabetic polyneuropathy. Diabet Med 1992; 9: 716±721. 10 Cromme PVM, Mulder JD, Rutten GEHM, Zuidweg J, Thomas S. A Standard for Diabetes Mellitus Type II. Amsterdam: Dutch College of General Practitioners, 1989. 11 Boulton AJ, Gries FA, Jervell JA. Guidelines for the diagnosis and outpatient management of diabetic peripheral neuropathy. Diabet Med 1998; 15: 508±514. 12 Wilm S, Gotz C. Patients with a `diabetic foot': prevention, diagnostics and therapy as seen by general practitioners. Huisarts Wet 1994; 37: 30±32. 13 Valk GD, Grootenhuis PA, Bouter LM, Bertelsmann FW. Complaints of neuropathy related to the clinical and neurophysiological assessment of nerve function in patients with diabetes mellitus. Diabetes Res Clin Pract 1994; 26: 29±34. 14 Bouma M, Dekker JH, van Eijk JTM, Schellevis FG, Kriegsman DMW, Heine RJ. Improving Diabetes Care in General Practice: Metabolic Control, Symptoms and Morbidity of Type 2 Diabetic Patients in a General Practice Network, Dissertation. Amsterdam: EMGO-Institute, Vrije Universiteit, 1999. 15 Grootenhuis PA, Snoek FJ, Heine RJ, Bouter LM. Development of a 16 17 18 19 20 21 22 23 24 25 26 27 type 2 diabetes symptom checklist: a measure of symptom severity. Diabet Med 1994; 11: 253±261. Brown MJ, Asbury AK. Diabetic neuropathy. Ann Neurol 1984; 15: 2±12. Anonymous. Statistical Package for the Social Sciences Advanced Statistics Reference Guide. Chicago: SPSS Inc, 1997. Dyck PJ, Karnes JL, Daube J, O'Brien P, Service FJ. Clinical and neuropathological criteria for the diagnosis and staging of diabetic polyneuropathy. Brain 1985; 108: 861±880. Anonymous. Factors in development of diabetic neuropathy. Baseline analysis of neuropathy in feasibility phase of Diabetes Control and Complications Trial (DCCT). The DCCT Research Group. Diabetes 1988; 37: 476±481. Allen C, Shen G, Palta M, Lotz B, Jacobson R, D'Alessio D. Longterm hyperglycemia is related to peripheral nerve changes at a diabetes duration of 4 years. The Wisconsin Diabetes Registry. Diabetes Care 1997; 20: 1154±1158. Franklin GM, Kahn LB, Baxter J, Marshall JA, Hamman RF. Sensory neuropathy in non-insulin-dependent diabetes mellitus. The San Luis Valley Diabetes Study. Am J Epidemiol 1990; 131: 633±643. Harris M, Eastman R, Cowie C. Symptoms of sensory neuropathy in adults with NIDDM in the U.S. population. Diabetes Care 1993; 16: 1446±1452. Walters DP, Gatling W, Mullee MA, Hill RD. The prevalence of diabetic distal sensory neuropathy in an English community. Diabet Med 1992; 9: 349±353. Bouter LM, Dongen Mv. Epidemiological Research: Design and Interpretation. Bohn: Scheltema & Holkema, 1988. Feldman EL, Stevens MJ, Thomas PK, Brown MB, Canal N, Greene DA. A practical two-step quantitative clinical and electrophysiological assessment for the diagnosis and staging of diabetic neuropathy. Diabetes Care 1994; 17: 1281±1289. Maser RE, Laudadio C, DeCherney GS. The effects of age and diabetes mellitus on nerve function. J Am Geriatr Soc 1993; 41: 1202±1204. Thomson FJ, Masson EA, Boulton AJ. The clinical diagnosis of sensory neuropathy in elderly people. Diabet Med 1993; 10: 843± 846. ã 2000 British Diabetic Association. Diabetic Medicine, 17, 105±110