Reflex-Hemodynamic Adjustments and Baroreflex Sensitivity During
advertisement

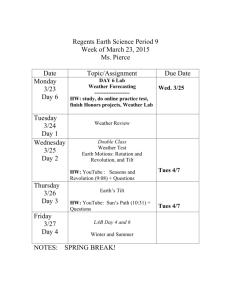
Reflex-Hemodynamic Adjustments and Baroreflex Sensitivity During Converting Enzyme Inhibition with MK-421 in Normal Humans HANS IBSEN, M.D., D . M . S c , BRENT EGAN, M.D., ARTHUR VANDER, M.D., KARL OSTERZIEL, AND STEVO JULIUS, M.D., M.D., Sc.D. SUMMARY Invasive hemodynamic measurements and determination of baroreflex sensitivity were carried out in 12 mildly sodium-depleted normotensive volunteers in a randomized double-blind crossover study with a single dose of converting enzyme inhibitor, MK-421, and placebo. In supine humans at rest, MK-421 caused a reduction in blood pressure through a fall in total peripheral resistance and an increase in arterial compliance. Thus, MK-421 appears to dilate both resistance vessels and larger arteries. Cardiac output increased, but contrary to the effects of other vasodilators, the increase was due to a higher stroke volume with an unchanged heart rate. The lack of heart rate response may well reflect enhanced central parasympathetic cardiac inhibition. Head-up tilt on MK421 caused an additional decrease in blood pressure in 65% of the subjects. The major determinant for the blood pressure fall during tilt and converting enzyme inhibition was a decrease in cardiac performance, while the reflex increase of arteriolar and venous tone was largely unimpaired. The decreased stroke volume may be secondary to elimination of a positive inotropic effect of angiotensin II (All). It is also conceivable that in the absence of AH the inotropic response to sympathetic activation is inadequate during tilt in these sodium-depleted normotensive individuals. Baroreflex sensitivity to blood pressure increase (i.v. phenylephrine) was enhanced after MK 421. Arterial compliance was increased, and this may explain the altered baroreceptor sensitivity. However, a possible central nervous enhancement of baroreceptor sensitivity after MK-421 could not be ruled out in this study. (Hypertension 5 (supp I): 1-184—1-191, 1983) KEY WORDS • adrenergic system • angiotensin II • baroreflex • blood pressure hemodynamics A NGIOTENSIN II (All) has been shown to facilitate the cardiovascular effect elicited by stimulation of the sympathetic nervous system.1"-1 These effects of All are exerted on the peripheral as well as the central part of the adrenergic system1 2 and involve a facilitation of ganglionic transmission through an increased norepinephrine release at the presynaptic level and to a minor degree by prevention of reuptake. Some data also suggest that All potentiates the effect of norepinephrine on postsynaptic receptors.' 4 Finally, All enhances the neuronally-mediated release of catecholamines from the adrenal medulla.2 This potentiating action of All has been investigated mainly in isolated animal preparations,-^ and very little is known as to the functional importance of this complicated interaction between the renin-angiotensin system (RAS) and the adrenergic system in humans.7 8 Angiotensin II antagonists and converting enzyme inhibitors (CEI) are useful tools in evaluating the importance of the RAS in cardiovascular homeostasis.9"" The absence of a significant increase in heart rate during a blood pressure fall due to All antagonists or CEI have directed some investigators to examine baroreflex mechanisms;12"17 some have proposed an increase12 14 and some a decrease11 in baroreflex sensitivity during CEI. The purpose of the present study was to examine: 1) to what extent the absence of All might impair reflex hemodynamic adjustments to head-up tilt in normal humans; and 2) whether changes in baroreflex sensitivity are involved in the hemodynamic response to CEI. A single dose of MK-421,18- l9 a new orally active CEI, was administered to normotensive male volunteers. From the Division of Hypertension. Department of Internal Medicine, and Department of Physiology. University of Michigan Medical School. Ann Arbor. Michigan Supported in part by Grants HL 21893 and HL 18575 from the National Institutes of Health. Address for reprints: Stevo Julius. M.D.. Division of Hypertension. Box 48. R6669 Kresge Building, University of Michigan Medical Center. Ann Arbor, Michigan 48109. I-184 HEMODYNAMICS AND CONVERTING ENZYME INHIBITION//*^ et al. Material and Methods Fifteen normotensive men with a mean age of 29 years (range 21-39 years) were studied. The study was approved by the Human Use Committee at the University of Michigan Hospitals, and its nature and purpose were explained to the volunteers, who gave written consent. Each individual had a medical history taken and underwent a physical examination. Routine blood and urine analyses were performed prior to and at the termination of the study. All investigations were carried out on an outpatient basis. The design was a randomized, single-dose double-blind crossover study with MK-421 20 mg and placebo. The individuals were placed on a diet containing approximately 20 mmol of sodium per day for 5 days prior to the hemodynamic measurements, in order to obtain a mild degree of sodium depletion. Adherence to the diet was checked by a 24-hour urine collection terminated on the morning of the day of the hemodynamic measurements. The individuals kept a food record, enabling them to adhere to the same diet prior to the second procedure. On the day of the hemodynamic measurements, the individuals came to the laboratory for clinical examination at 0800 hours after a light breakfast. After remaining supine for 1 hour, they had blood samples drawn through an indwelling needle for determinations of plasma renin activity (PRA), plasma angiotensin II concentration (PAII), plasma norepinephrine (PNE), plasma epinephrine (PE), and plasma angiotensin I converting enzyme concentration (P-ACE). At the same time, MK-421 or placebo was administered orally. Blood pressure and heart rate were recorded. Two hours later, after a light meal, the individuals were placed supine on a tilt table for insertion of catheters under local anesthesia. A short plastic cannula was introduced percutaneously into the brachial artery and connected to a pressure transducer. A Swan-Ganz catheter or a polyethylene, PE-50 catheter was introduced percutaneously into an antecubital vein and advanced to the right atrium. Heart rate was monitored by electrocardiogram. Intraarterial blood pressure, right atrial pressure, and heart rate were monitored continuously. While resting in the recumbent position 4 hours after intake of the tablet and at least 30 minutes after all catheters were introduced, the subjects underwent blood sample collections and hemodynamic measurements. After 20 minutes of 25° head-up tilt, the hemodynamic measurements were repeated, followed by blood sampling just before termination of the tilt procedure. At least 20 minutes later, the experimental procedure was concluded by determination of baroreflex sensitivity. Exactly the same procedure was repeated 2 weeks later, preceded by the low salt diet for 5 days. Cardiac output was determined by dye dilution (Cardiogreen). Details of the procedure have been published elsewhere.20-2I An average of two to three determinations was used. The central blood volume (CBV) was calculated by multiplication of cardiac output by 1-185 mean transit time, corrected for the delayin the withdrawal system. The ratio of stroke volume to pulse pressure (SV/PP) was used as a measure of arterial compliance. Forearm blood flow was determined by venous occlusion plethysmography and a mercury in Silastic strain gauge.20 Venous distensibility was also measured by venous occlusion plethysmography.22 Baroreflex sensitivity was determined by the ramp method described by Smyth et al." An intravenous bolus of phenylephrine 50-200 /ig was administered. The PRA was measured by radioimmunoassay of generated AI after 60 minutes of incubation at pH 6.0,20 PAII by radioimmunoassay,24 and PNE and PE by a single isotope radioenzymatic method.20 Measurement of P-ACE was based on the enzyme's ability to release dipeptides from a radio-labeled tripeptide25 a n c j expressed as the amount of released hippuric acid per milliliter per minute. All blood samples from each individual were analyzed in a single assay run. A mild degree of sodium depletion and head-up tilt (25°) were chosen in an attempt to avoid fainting episodes, necessitating termination of the procedures before hemodynamic measurements could be obtained. In spite of this precaution, three individuals experienced fainting episodes during the first procedure, two during introduction of catheters, and one after 1 minute of tilt. They were all on active treatment and had a very low urine sodium excretion (2-10 mmol/24 hr). They did not return for a second procedure. Furthermore, in three of the remaining 12 cases, fainting episodes occurred during tilt and required active treatment before hemodynamic measurements could be obtained. No fainting episodes were seen during placebo procedures. Statistical calculations were carried out by means of t test for paired data. Linear regression analyses were also used. Results are presented as means ± SEM. Results Recumbent Data Humoral Effects The humoral effects of MK-421 in the recumbent position before and 4 hours after intake of the tablet are summarized in table 1. The predrug values for PRA as well as PAII were normal in spite of the low salt diet. As stated above, we were not aiming at a severe degree of sodium depletion, and the urinary sodium excretion (UNa) reflects the mild degree of sodium depletion obtained. The predrug control values for PRA, PAII, and UNa were identical in the two situations: Similarly, there was no difference between P-ACE, PNE, and PE in the placebo and MK-421 situations before intake of the tablet. A high degree of CEI induced by MK-421 was documented by the marked increase in PRA and a significant fall in PAII. P-ACE was dramatically reduced, in most cases to an undetectable level. A small but statistically significant increase in PNE was found on MK-421 while PE did not change. 1-186 1982 BLOOD PRESSURE COUNCIL SUPP 1, HYPERTENSION, VOL 5, No 2, MARCH-APRIL 1983 TABLE 1. Humoral Effects of MK-421 in 12 Normotensive Men at Rest Supine Placebo PRA (ng/ml/hr) P-ACE (nmol/liter) PA II (pg/ml) PNE (pg/ml) PE (pg/ml) UNa (mmol/24 hr) MK-421 Control Placebo P Control 1.37±0.3 218±16 I3.7±2.2 197 ±30 34 + 4 55±11 1.11+0.2 218+18 11.6±1.7 225 + 29 49±9 n.s. n.s. <0 03 — — 1.88±0.4 219±19 15.0±2.7 204 ±24 37 ±7 48±9 n.s. n.s. MK-421 P 9.0±0.9 253 ±28 49 ±10 < 0.002 < 0.0001 <0.05 < 0.01 n.s. — — 9.32±2.2 6±3 No significant differences were observed between the two control periods (mean ± SEM). PRA = plasma renin activity; P-ACE = plasma angiotensin I converting-enzyme concentration; PA II (n = 8) = plasma angiotensin II concentration; PNE = plasma norepinephrine; PE = plasma epinephrine; UNa = 24-hour urinary sodium excretion. Hemodynamic Effects Hemodynamic results are illustrated in figures 1 and 2. As compared to placebo, MK-421 caused a significant fall in blood pressure. This was due to a decrease in total peripheral resistance (TPR) and took place in spite of an increase in cardiac output (CO) and stroke volume (SV). There was no change in heart rate (HR). Right atrial pressure (RAP) and central blood volume (CBV) did not change significantly. Not shown in figures 1 and 2 are forearm blood flow (FBF), forearm vascular resistance (FVR), and venous distensibility. All of these variables did not change significantly after MK-421. Baroreflex sensitivity, expressed as the slope of the regression line between SBP and the change in RR interval during phenylephrine injection, was 23.6 ± 2.8 msec/mm Hg before and 28.3 ± 4.1 msec/mm Hg after MK-421. This increase of baroreceptor sensitivity was significant ip < 0.02). The correlation coefficient for the individual regression lines varied between r = 0.70 and r = 0.96. The ratio of stroke volume to pulse pressure (SV/PP) was 1.76 ± 0.1 on placebo and 2.04 ± 0.1 on MK-421. This increase in the compliance index on MK-421 was significant (p < 0.01). Tilt Data Humoral Effects Tilt results are summarized in figure 3. The PRA increased significantly during tilt, more markedly so on MK-421 compared to placebo. The PAII increased by 85% on placebo but did not change on MK-421, indicating an effective CEI also during the tilt procedure. The PNE increased significantly to a similar degree on MK-421 and placebo while PE did not change consistently. Hemodynamic Effects Three individuals fainted during tilt on MK-421 before we could measure C O , FBF, and venous distensibility. The changes reported in BP, HR, and RAP are the values obtained just before termination of tilt in all TPR HR beats/mm n.s. 70- RAP mmHg O n.s. MAP mm Hg lOOn p<:.001 p<.001 20- 9060- 15- 8070- 106050-1 , P i MK FIGURE 1. Heart rate (HR), mean arterial pressure (MAP), and right atrial pressure (RAP) in normal men at rest supine on placebo (P) and on MK-421 (MK). MK FIGURE 2. Cardiac output (CO), stroke volume (SV), and total peripheral resistance (TPR) in normal men at rest supine on placebo (P) and on MK-421 (MK). HEM0DYNAM1CS AND CONVERTING ENZYME INHIBITION//foen et al. A 10l PRA ng Aj/ml/h 0J 10n A PA 11 P9/ml 5- A SVml A200PNE n g/mf 100- -10 J. 10 20 A MAP mmHg -20 0J n.s. n 0J -4Q- 9/ml 50- -60- 1 FIGURE 5. Correlation between changes in stroke volume (ASV) and mean arterial pressure (AMAP) in normal men during tilt and MK-421. 0- MK FIGURE 3. Changes in plasma renin activity (PRA), plasma angiotensin II concentration (PAH), plasma norepinephrine (PNE), and plasma epinephrine (PE) in normal men during tilt on placebo (P) and MKA2I (MK). 12 cases. The results on CO, SV, TPR, CBV, and FBF consist of data from the nine subjects who were without fainting episodes. Results are summarized in table 2 and figure 4. Compared to the changes during placebo, the BP decreased significantly during tilt on MK-421. The individual changes varied markedly from severe hypotension to no BP change. The RAP and CBV decreased to a similar degree on placebo and MK-421. The decrease in CO tended to be more pronounced on MK421 but not statistically significant, while the reduction in SV was significantly higher on MK-421. HR and ASBP -20 r = 0.67 p<.05 1-187 ADBP mmHg •20n TPR increased to a similar degree on placebo and on MK-421. FBF decreased significantly during tilt on placebo, but not on MK-421. However, the changes on placebo and on MK-421 did not differ significantly. Similarly, FVR increased significantly on placebo but not on MK-421. Venous distensibility did not change consistently. The decrease in MAP during tilt and MK-421 correlated with the decrease in SV (r = 0.67, p < 0.05) (fig. 5). The hemodynamic results in the nine complete cases were analyzed in more detail. Using the change in MAP during tilt as the criterion, we divided the group into two, consisting of one group of five individuals whose BP fell, and one group of four whose BP remained the same during tilt and MK-421 (figs. 6 and 7). The BP fall was due to a decrease in CO and SV, p<001 AMAP mmHg • 20-| • 20- • 10- • 10- o- o- •10- o-10- -10- -10- -20- -20J -20-30- FIGURE 4. Changes in systolic (SBP), diastolic (DBP), and mean arterial blood pressure (MAP) in normal men during tilt on placebo and on MK-421 (four individuals showed no fall in MAP on MK-421). 1-188 1982 BLOOD PRESSURE COUNCIL A 20 SBP mmHg SUPP I, HYPERTENSION, VOL 5, No 2, MARCH-APRIL 1983 n.s. A 1-1 n.s. h CO 0l/min -1 OH -20J -20J 20-. i i P MK l/min -1- -2 -2- -3- -3- <.O2 sv -20 SV ml -20- -40- -40- ml i i MK P A 20-| MAP mmHg -60 i P n.s. n.s. A TPR 0- Units -20BP-Resp. MK BP-Non Resp. FIGURE 6. Changes in systolic (SBP), diastolic (DBP), and TABLE 2. HR (bpm) SBP (mm Hg) DBP (mm Hg) MAP (mm Hg) CO (liter/min) SV (ml) RAP (mm Hg) TPR (units) FVR (units) 5- BP-Non Resp. FIGURE 7. Changes in cardiac output (CO), stroke wlume (SV), and total peripheral resistance (TPR) during tilt on placebo (P) and MK-421 (MK) in five normal men with and four without BP fall during tilt and MK-421. Changes in Hemodynamic Measurements during Head-Up Tilt in Subjects on Placebo (P) and MK-421 Hemodynamic measurement CBV (ml) n.s. 0J 0J BP-Resp. mean arterial blood pressure (MAP) during tilt on placebo (P) and MK-421 (MK) in five normal men who showed a BPfall and four who showed no BP fall during tilt and MK-421. i MK i P A TPR 5- Units 10- -60- i MK MK n.s. A 20] DBP mmHg 0- -20J i P Placebo + 7.0±1.6 0.0+1.6 + 7.5+1.3 + 2.9+1.8 -0.88 + 0.2 -23.7±4.3 -5.4±0.4 -282 + 37 + 3.4±0.7 + 8.1±1.3 MK-421 P a 0.001 NS c 0.001 NS C 0.005 C 0.001 C 0.001 C 0.001 C 0.001 C 0.001 P + 8.0 + 0.9 -11.4 + 3.7 -0.5 + 2.5 -2.5 + 3.0 -1.3 + 0.3 -31.1+3.9 -5.4 + 0.8 -387 + 77 + 2.9 + 0.5 + 6.2 + 5.0 C 0.001 C0.01 NS NS C 0.001 c: o.ooi =: 0.001 =: 0.001 c 0.001 NS Difference P vs MK-421 P NS < 0.01 < 0.001 <0.02 NS <0.05 NS NS NS NS Values are means ± SEM. HR = heart rate; SBP = systolic blood pressure; DBP = diastolic blood pressure; MAP = mean arterial blood pressure; CO = cardiac output; SV = stroke volume; RAP = right atrial pressure; CBV = central blood volume; TPR = total peripheral resistance; FVR = forearm vascular resistance. HEMODYNAMICS AND CONVERTING ENZYME INHIBITION///^ et al. while the four individuals who were able to maintain BP levels also maintained their levels of CO and S V as compared to placebo. The changes in HR and TPR were similar in the two subgroups. The changes in the remaining variables also did not differ significantly between the two groups. Discussion The present results verify that a single dose of MK421 induces a high degree of CEI:18 l9 P-ACE was reduced to an undetectable level. This led to a marked rise in PRA and a fall in PAII. This pattern was accentuated during head-up tilt. Acute CEI caused an approximately 10% decrease in resting BP, in accordance with other investigations.26-27 However, the hemodynamic mechanism of this decrease in normotensive individuals in our study was different than that in other studies on hypertensive subjects. In hypertension, no change28"30or even a decrease30 3I in CO and SV were found. In one study of hypertensives, a slight increase32 in CO during CEI has been reported. In our study of normal subjects, the BP decreased through a fall of vascular resistance, which exceeded the moderate CO increase. Data on normal humans are very scarce, but our results are in agreement with those of Niarchos et al., 26 who reported an increase in SV and CO in six sodium-depleted normal volunteers during acute CEI with teprotide. In our study, CEI caused a decrease of vascular resistance. In addition, the arterial compliance increased after MK-421. Both of these effects led to a substantial decrease of the cardiac afterload. The usual response to an acute decrease in afterload is a reflex increase of CO, predominantly through an increase in HR. After MK-421, however, the response to the decreased afterload was an increase in SV, without tachycardia. The absence of tachycardia after MK-421 cannot be attributed to an absence of sympathetic activation, since we observed a small but significant increase in PNE values after MK-421. There are two possible explanations for this absence of tachycardia: 1) the absence of angiotensin blunts postjunctional sympathetic responses;4-5 or 2) CEI elicits a central increase in the parasympathetic chronotropic inhibition.16-l7-31 With a relatively fixed heart rate, MK-421 elicited an increase of CO through a higher SV. The right atrial pressure and the cardiopulmonary blood volume did not increase, indicating that the cardiac preload remained unchanged after MK-421. Consequently, we believe that the increase of SV reflects a mechanical improvement of ejection in response to the MK-421induced decrease in afterload. In anticipation of fainting episodes, we only used a mild degree of tilt and sodium depletion. In spite of our precautions, syncope occurred in three subjects, with a very pronounced BP fall during tilt and MK-421 before CO measurements could be obtained. However, it seems unlikely that these three individuals responded qualitatively differently compared to the remaining in- 1-189 dividuals with a BP fall during CEI and tilt, as, until the point of faintness, their changes in HR and right atrial pressure followed the same pattern as the remaining subjects. An analysis of the individual BP changes during tilt and MK-421 in the nine complete cases revealed that the subjects could be divided into five individuals with and four without BP fall. In the five cases, the BP fall during tilt was obviously due to a marked decrease in SV as well as CO while the increase in TPR was similar during placebo and MK421. CEI affected the BP response to head-up tilt in this study. Since there was no evidence for increased venous pooling of blood in the tilted position after MK-421, the decrease of SV discloses an impairment of cardiac function in subjects who responded with a BP decrease. Apparently after CEI these subjects were unable to maintain a normal SV against the tilt-induced increase in afterload. The BP response to MK-421 in all normotensive subjects fully depends on their capability to maintain a SV, a fact clearly demonstrated in the correlation of these variables (fig. 5). Why does elimination of All lead to BP fall during tilt, mainly through a decrease in cardiac performance? An attenuation of venous return does not seem to be involved since the decrease in RAP and CBV during tilt was similar on placebo and MK-421. Furthermore, venous distensibility did not change in a consistent way. It is known that All has a pronounced positive inotropic effect on the isolated myocardium.33 This effect is not detectable during All infusion in vivo, probably due to baroreceptor response to increased vascular resistance and BP. '6 In the recumbent position in the present study, an elimination of the inotropic effect of All could not be uncovered; in fact, an increase in CO and SV was found. However, contrary to the findings during tilt, a reduction in afterload by CEI might well override a negative inotropic influence in recumbency. The decrease in SV and BP during tilt and CEI was not counterbalanced by augmentation of reflex adrenergic activity. The increase in HR and vascular resistance was the same on placebo and MK-421. This suggests that reflex sympathetic adjustments to tilt are less potent during CEI, which is in accordance with the results from animal research.3-* The lack of accentuation of HR increase in spite of BP fall might not solely be explained by decreased adrenergic function, but increased vagal tone could also be involved.31 Animal data indicate decreased adrenergic activity34 as well as increased vagal activity35 during sodium depletion. Furthermore, the central potentiating effects of All on the cardiovascular system involve both enhanced sympathetic activity and withdrawal of vagal tone.2-16-1? Consequently, All blockade during sodium depletion might well lead to increased vagal tone. A decrease in BP without a reflex increase in HR might also occur if at the same time an alteration in baroreflex sensitivity or a change in the setpoint12-l4 of the baroreflexes takes place. We found an increase in baroreflex sensitivity in response to increases in systolic BP during bolus injections of phenylephrine. The slope of the regression line between systolic BP and 1-190 1982 BLOOD PRESSURE COUNCIL increase in RR interval was slightly, but significantly steeper during CEI with MK-421. It is well known that baroreflex sensitivity is closely related to arterial compliance.36 The ratio SV/PP serves as an index of arterial compliance.37 The increase in SV/PP indicates an increase in arterial compliance during CEI, and this might explain the increase in BRS. Another possible explanation for the increase in baroreflex sensitivity is that All antagonizes baroreflexes at a central level;15"17 consequently CEI, with an attendant fall in All, leads to increases in baroreflex sensitivity.15 Contrary to our study, Mancia et al.14 found that, in patients with severe hypertension, the sensitivity to BP reduction with nitroglycerine was increased, while the sensitivity to BP elevation with phenylephrine was unchanged. Conclusions Acute CEI with MK-421 in mildly sodium-depleted normal men leads to a BP fall through a reduction in TPR, in spite of an increase in CO and SV. The increase in CO and SV is probably due to a reduction in afterload. The major determinant for the additional BP fall during tilt and CEI was a decrease in cardiac performance. We propose a dual mechanism responsible for this BP fall: CEI with a decrease in All level leads to an elimination of a positive inotropic effect of All. The attendant decrease in S V and CO is insufficiently counterbalanced because of an impairment of reflex adrenergic function. This is, in turn, caused by an attentuation of an All-mediated facilitation on the sympathetic nervous system. The hypothesis needs to be substantiated by more detailed measurements of left ventricular function during tilt and blockade of the RAS. Baroreflex sensitivity to BP increases was enhanced. This might be due to the increase in arterial compliance, but a central mechanism could also be responsible. A possible practical importance of this finding during long-term treatment in hypertension remains to be determined. Acknowledgments MK-421 was generously placed at our disposal by Dr. Richard Davies, Merck Sharp & Dohme Research Laboratories, West Point, Pennsylvania. References 1. Zimmerman BG: Adrenergic facilitation by angiotensin: does it serve a physiological function? Clin Sci 60: 343, 1981 2. Ferrario CM, Gildenberg PL, McCubbin JW: Cardiovascular effects of angiotensin mediated by the central nervous system. Circ Res 30: 257, 1972 3. Adigun SA, Clough DP, Conway J, Hatton R: The effects of the antagonists of the renin-angiotensin system on cardiovascular response to lower-body subatmospheric pressure in the anaesthetized cat. Clin Sci 58: 549, 1980 SUPP I, HYPERTENSION, VOL 5, No 2, MARCH-APRIL 1983 4. Antonaccio MJ. Kerwin L. Pre- and postjunctional inhibition of vascular sympathetic function by captopril in SHR. Implication of vascular angiotensin II in hypertension and antihypertensive actions of captopril. Hypertension 3 (suppl I): 1-54, 1981 5. Clough DP, Collis MG, Conway J, Hatton R. Keddie JR: Interaction of angiotensin-converting enzyme inhibitors with the function of the sympathetic nervous system. Am J Cardiol 49: 1410, 1982 6. Hatton R, Clough DP, Adigun SA, Conway J: Functional interaction between angiotensin and sympathetic reflexes in cat. Clin Sci 62: 51. 1982 7. Abboud FM: Effects of sodium, angiotensin, and steroids on vascular reactivity in man. Fed Proc 33: 143, 1974 8. Imai Y. Abe K, Seino M. Haruyama T, Tajima J, Sato M, Goto T, Hiwatari M, Kasai Y, Yoshinaga K, Sekino H: Attenuation of pressor responses to norepinephrine and pitressin and potentiation of pressor response to angiotensin II by captopril in human subjects. Hypertension 4: 444, 1982 9. SanchoJ, Re R. Burton J, Barger AC. Haber E: The role of the renin-angiotensin-aldosterone system in cardiovascular homcostasis in normal human subjects. Circulation 53: 400, 1976 10. Case DB, Wallace JM, Keim HJ, Weber MA, Drayer JIM, White RP, Sealey JE, Laragh JH. Estimating renin participation in hypertension: Superiority of converting enzyme inhibitor over saralasin. Am J Med 6 1 : 790, 1976 11. Ibsen H. Leth A, Hollnagel H. Kappelgaard AM, Nielsen MD, Christensen NJ, Giese J: Renin-angiotensin system in mild essential hypertension. The functional significance of angiotensin II in untreated and thiazide-treated hypertensive patients. Acta Med Scand 205: 547. 1979 12. Hatton R. Clough D, Faulkner K, Conway J: Angiotensinconverting enzyme inhibitor resets baroreceptor reflexes in conscious dogs. Hypertension 3: 676, 1981 13. Heavey DJ. Reid JL: The effect of SQ 14225 on baroreceptor reflex sensitivity in conscious normotensive rabbits. Br J Pharmacol 64: 389P, 1978 14. Mancia G, Parati F, Pomidossi G. Grassi G, Bertinieri G, Buccino N, Ferrari A, Gregorini L, Rupoli L, Zanchetti A: Modification of arterial baroreflexes by captopril in essential hypertension. Am J Cardiol 49: 1415, 1982 15. Lumbers ER, Potter EK, McCloskey DI, Ismay MJ, Lee WB, Stevens AD: The effects of intravenous angiotensin II on the cardiac baroreceptor reflex In Frontiers in Hypertension Research, edited by Laragh JH, Buhler FR, Seldin DW. New York: Springer-Vcrlag, 1981, p 556 16. Lee WB. Ismay MJ. Lumbers ER. Mechanisms by which angiotensin II affects the heart rate of the conscious sheep. Circ Res 47: 286. 1980 17. Marker JD, Miles TS, Scroop GC: Modulation of the baroreceptor reflex by angiotensin II and other vasoactive drugs in anaesthetized greyhounds. Clin Sci 58: 7, 1980 18. Gavras H, Waeber B, Gavras I, Biollaz J, BrunnerHR. Davies RO: Antihypertensive effects of the new oral angiotensin converting enzyme inhibitor " M K - 4 2 1 . " Lancet 2: 543, 1981 19. Brunner DB. Desponds G, Biollaz J, Keller I, Ferber F, Gavras H, Brunner HR, Schelling JL: Effect of a new angiotensin converting enzyme inhibitor MK 421 and its lysine analogue on the components of the renin system in healthy subjects. Br J Clin Pharmacol 11: 461, 1981 20. Kiowski W. Julius S: Renin response to stimulation of cardiopulmonary mechanoreceptors in man. J Clin Invest 62: 656, 1978 21. Julius S, Amery A, Whitlock LS, Conway J: Influence of age on the hemodynamic response to exercise. Circulation 36: 222, 1967 22. Simon G, Franciosa JA, Cohn JN: Decreased venous distensibility in essential hypertension: lack of systemic hemodynamic correlates. Angiology 30: 147, 1979 23. Smyth HS, Sleight P, Pickering GW: Reflex regulation of arterial pressure during sleep in man. A quantitative method of assessing baroreflex sensitivity. Circ Res 24: 109, 1969 24. Nicholls MG, Espiner EA: A sensitive, rapid radioimmunoassay for angiotensin II. NZ Med J 83: 399, 1976 HEMODYNAMICS AND CONVERTING ENZYME INHIBITION//*™?/! et al. 25. Chushrnan DW, Cheung HS: A simple substrate for assay of dog lung angiotensin converting enzyme. Fed Proc 28: 799, 1969 26. Niarchos AP, Pickering TG, Laragh JH: Cardiovascular responses to isometric exercise and standing in normotensive subjects during converting enzyme inhibition with teprotide. Hypertension 4: 538, 1982 27. Ibsen H, Kappelgaard AM, Nielsen MD, Giese J: The effect of angiotensin II blockade by saralasin (l-Sar-8-ala-angiotensin H) in normal man. Eur J Clin Pharmacol 14: 171, 1978 28. Tarazi RC, Bravo EL, Fouad FM, Omvik P, Cody RJ: Heroodynamic and volume changes associated with captopril. Hypertension 2: 576, 1980 29. Wenting GJ, De Bruyn HB, Man In't Veld AJ, Woittiez AJJ, Derkx FHM, Schalekamp MADH: Hemodynamic effects of captopril in essential hypertension, renovascular hypertension and cardiac failure: correlations with short- and long-term effects on plasma renin. Am J Cardiol 49: 1453, 1982 30. DeCarvalho JGR, Dunn FG, Kern DC, Chrysant SG, Frohlich ED: Hemodynamic correlates of saralasin-induced arterial pressure changes. Circulation 57: 373, 1978 31. Bravo EL, Tarazi RC: Hemodynamics of an angiotensin II 32. 33. 34. 35. 36. 37. 1-191 antagonist in normal, unanesthetized dogs. Circ Res 43 (suppl I): 1-27, 1978 Fagard R, Bulpitt C, Ujnen P, Araery A: Response of the systemic and pulmonary circulation to converting-enzyme inhibition (captopril) at rest and during exercise in hypertensive patients. Circulation 65: 33, 1982 Bunag RD: Circulatory effects of angiotensin. In Angiotensin, edited by Page IH, Bumpus FM. Berlin: Springer-Verlag, 1974, p 441 Rocchini AP, Cant JR, Barger AC: Carotid sinusreflexin dogs with low- to high-sodium intake. Am J Physiol 233: H196, 1977 Szilagyi JE, Masaki Z, Brosnihan KB, Ferrario CM: Neurogenic suppression of carotid sinusreflexesby vagal afferents in sodium-depleted dogs. Am J Physiol 241: H255, 1980 Randall O, Esler M, Culp B, Julius S, Zweifler A: Determinants of baroreflex sensitivity in man. J Clin Lab Invest 91: 514, 1978 Tarazi RC, Magrini F, Dustan HP: The role of aortic distensibility in hypertension. In Recent Advances in Hypertension, vol 2, edited by Milliez P, Safar M. Monaco: BoehringerIngelhcim, 1975, p 133