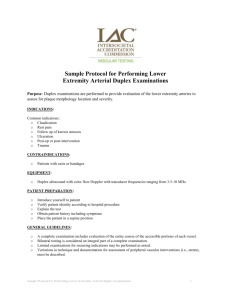
mesenteric arterial duplex evaluation
advertisement

MESENTERIC ARTERIAL DUPLEX EVALUATION Indications and Contraindications: Post-prandial pain Remarkable weight loss Avoidance of food Impaired gastrointestinal motility Mid-line abdominal bruit with associated symptoms Follow-up for revascularization Capabilities and Limitations: Useful for identification of flow-reducing mesenteric artery stenosis, occlusion, aneurysms, dissection, and arterial anomalies Capable of detecting mesenteric artery stenosis that is not yet of hemodynamic significance (< 60 % diameter reduction) Provides confirmation of patency of mesenteric artery bypass grafts and stents Excessive abdominal gas may preclude a complete examination Recent surgery may preclude moving the patient to positions that facilitate complete interrogation of the mesenteric circulation Patients who present with severe abdominal pain and clinical suspicion of acute mesenteric ischemia should be presented emergently for mesenteric angiography in preference to duplex imaging. Duplex scanning and color flow imaging are to be reserved for patients with suspected chronic mesenteric ischemia. Instrumentation: 1. High resolution duplex ultrasound system; Doppler color flow imaging may be used to complement the study 2. Pulsed Doppler transducers ranging in frequency from 2.0 to 5.2 MHz 3. Examination table that can be moved to the reverse Trendelenburg position Patient Preparation and Positioning: 1. The patient should have no food by mouth after midnight on the evening prior to the examination. Morning medications should be taken with sips of water only; no citrus juices; no dairy products. No smoking or chewing gum for at least 4 hours prior to the examination. 1 2. All patients are evaluated in the morning before the noon hour. 3. Initially, position the patient comfortably in the supine position with head slightly elevated and the bed in the reverse Trendelenburg position (feet 10-15 degrees lower than the heart) to allow the visceral contents to descend into the abdomen. Be certain that the patient is warm and the room is at ambient temperature. 4. If excessive abdominal gas is noted during the sonographic examination, the patients may be given 1-2 Simethicone tablets with a small amount of water. Wait approximately 15-20 minutes before commencing the examination. 5. Obtain a history and examine the patient for evidence of pulsatile abdominal mass, major abdominal collaterals surrounding the umbilicus, and abdominal or flank bruits. Technical Components: 1. With the patient lying in the supine position, the aorta is evaluated in the sagittal plane, using B-Mode imaging, from the level of the xiphoid process through the aortic bifurcation. Note evidence of atherosclerotic plaque, dissection, aneurysm, or other pathology. Repeat the examination using a transverse imaging plane. Note evidence of major collaterals and/or peri-aortic pathology 2. Obtain a Doppler velocity spectral signal in the aorta above the level of the celiac and superior mesenteric arteries using appropriate angle correction (< 60 degrees). 3. From a sagittal view of the aorta, note the origins of the celiac trunk and the superior mesenteric arteries. Color flow imaging may facilitate identification of the vessel origins, the presence of a common trunk, and turbulence associated with stenotic disease. 4. Sweep the Doppler sample volume slowly from the aortic lumen into the ostium of the celiac artery; note the change in vascular resistance in the celiac artery compared to the aorta (low diastolic flow in the aorta with increase in diastolic flow in the celiac artery). Special attention should be given to markedly increased velocity in the celiac ostium as this signifies stenosis. Retain the transition signal for interpretation. 5. Move the Doppler sample volume slowly along the visualized length of the celiac trunk, continuously noting the peak systolic velocity. Record angle-corrected Doppler waveforms from the proximal and mid and distal segments of the celiac artery. 6. Rotate the transducer to obtain a cross-sectional image of the aorta and the origin of the celiac trunk. Repeat the Doppler interrogation along the length of the celiac artery to the level of the bifurcation into the common hepatic and splenic arteries. 2 7. Follow the course of the common hepatic and splenic arteries using B-Mode, color, and/or power Doppler imaging. 8. Interrogate the common hepatic and splenic arteries with spectral Doppler taking care to use appropriate angle correction (angle < 60 degrees). Record diagnostic waveforms in both arteries. 9. Return to the sagittal image of the proximal aorta. Using B-Mode imaging complemented with color flow imaging as necessary, locate the origin of the superior mesenteric artery. 10. Record Doppler spectral waveforms from the proximal, mid, and distal segments of the superior mesenteric artery using appropriate angles of insonation. Color flow imaging may facilitate confirmation of the mid-to-distal segments of the artery. Note collateral vessels. 11. Return to the image of the proximal aorta. Using a transverse image plane, follow the course of the aorta distally to identify the origin of the inferior mesenteric artery. Color flow imaging may facilitate the examination. 12. Record Doppler spectral waveforms along the visualized length of the inferior mesenteric artery. Diagnostic Criteria: NOTE: Doppler spectral waveforms must define the stenosis profile in all regions where flow disturbance is noted by spectral Doppler or color flow imaging. It is mandatory to record a post-stenotic signal in all cases where flow-limiting disease is suspected. Normal: Celiac peak systolic velocity < 200 cm/sec; no evidence of a post-stenotic signal Superior mesenteric artery peak systolic velocity < 275 cm/sec; no evidence of a poststenotic signal No evidence of turbulent or disturbed flow in any arterial segment Flow-reducing Mesenteric Artery Stenosis: Celiac peak systolic velocity > 20 cm/sec; end-diastolic velocity > 55 cm/sec; a poststenotic signal is present Superior mesenteric artery peak systolic velocity > 275 cm/sec; end-diastolic velocity > 45 cm/sec; a post-stenotic signal is present 3 If flow-reducing stenosis is indicated in the celiac or superior mesenteric arteries, the inferior mesenteric artery should be interrogated and the diameter of the artery determined to demonstrate collateral potential. Mesenteric Artery Occlusion: No evidence of flow in an imaged mesenteric artery using optimized spectral, color, and/or power Doppler Required Documentation: 1. B-Mode images of the proximal, mid, and distal aorta including the aortic bifurcation. Document all evidence of pathology or anatomic anomalies. 2. B-Mode images of all mesenteric arterial segments with particular attention to evidence of stents or grafts, narrowed segments, dilated segments, masses, etc. 3. Doppler spectral waveforms from the proximal aorta, all segments of the celiac, superior and inferior mesenteric arteries. 4. Doppler spectral waveforms from the mesenteric veins as indicated. References: 1. Healy DA, Neumyer MM, Atnip RG, Thiele BL: Evaluation of celiac and mesenteric vascular disease with duplex ultrasonography. J Ultrasound Med.11: 481-85, 1999. 2. Nicoloff AD, Williamson WK, Moneta GL, et al: Duplex ultrasonography in evaluation iof splanchnic artery stenosis. Surg Clin North Am. 77: 339-55, 1997. 3. Jager K, Bollinger A, Valli C, Ammann R: Measurement of mesenteric blood flow by duplex scan. J Vasc Surg. 3:462-69, 1986. 4. Moneta GL, Yeager RA, Dalman R, et al: Duplex ultrasound criteria for diagnosis of splanchnic artery stenosis or occlusion. J Vasc Surg. 14: 511-20, 1991. 5. Moneta GL, Lee RW, Yeager RA, et al: Mesenteric duplex scanning: A blinded prospective study. J Vasc Surg. 17: 79-86, 1993. 6. Bowersox JC, Zwolak RM, Walsh DB, et al: Duplex ultrasonography in the diagnosis of celiac and mesenteric artery occlusive disease. J Vasc Surg. 14: 780-88, 1991. 4 7. Zwolak RM, Fillinger MF, Walsh DB, et al: Mesenteric and celiac duplex scanning: A validation study. J Vasc Surg. 27: 1078-88, 1998. 8. Rizzo RJ, Sandager G, Astleford P, et al: Mesenteric flow velocity variations as a function of angle of insonation. J Vasc Surg. 11: 688-94, 1990. 5