04 Mene - Società Italiana di Nefrologia
advertisement
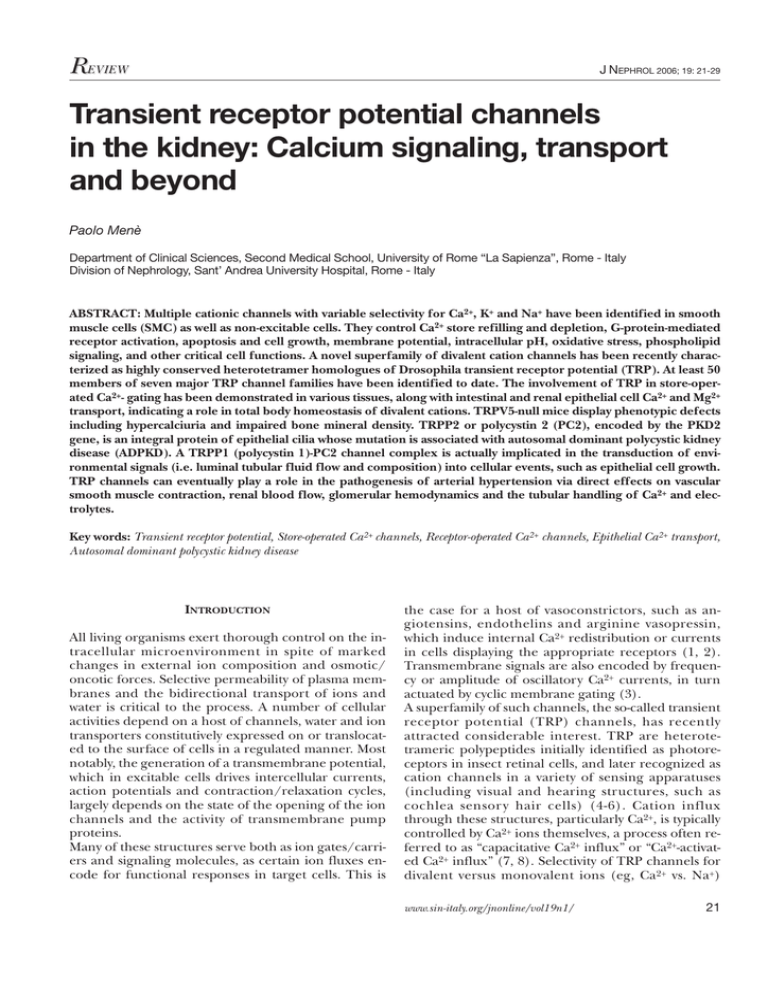
R EVIEW J NEPHROL 2006; 19: 21-29 Transient receptor potential channels in the kidney: Calcium signaling, transport and beyond Paolo Menè Department of Clinical Sciences, Second Medical School, University of Rome “La Sapienza”, Rome - Italy Division of Nephrology, Sant’ Andrea University Hospital, Rome - Italy ABSTRACT: Multiple cationic channels with variable selectivity for Ca2+, K+ and Na+ have been identified in smooth muscle cells (SMC) as well as non-excitable cells. They control Ca2+ store refilling and depletion, G-protein-mediated receptor activation, apoptosis and cell growth, membrane potential, intracellular pH, oxidative stress, phospholipid signaling, and other critical cell functions. A novel superfamily of divalent cation channels has been recently characterized as highly conserved heterotetramer homologues of Drosophila transient receptor potential (TRP). At least 50 members of seven major TRP channel families have been identified to date. The involvement of TRP in store-operated Ca2+- gating has been demonstrated in various tissues, along with intestinal and renal epithelial cell Ca2+ and Mg2+ transport, indicating a role in total body homeostasis of divalent cations. TRPV5-null mice display phenotypic defects including hypercalciuria and impaired bone mineral density. TRPP2 or polycystin 2 (PC2), encoded by the PKD2 gene, is an integral protein of epithelial cilia whose mutation is associated with autosomal dominant polycystic kidney disease (ADPKD). A TRPP1 (polycystin 1)-PC2 channel complex is actually implicated in the transduction of environmental signals (i.e. luminal tubular fluid flow and composition) into cellular events, such as epithelial cell growth. TRP channels can eventually play a role in the pathogenesis of arterial hypertension via direct effects on vascular smooth muscle contraction, renal blood flow, glomerular hemodynamics and the tubular handling of Ca2+ and electrolytes. Key words: Transient receptor potential, Store-operated Ca2+ channels, Receptor-operated Ca2+ channels, Epithelial Ca2+ transport, Autosomal dominant polycystic kidney disease INTRODUCTION All living organisms exert thorough control on the intracellular microenvironment in spite of marked changes in external ion composition and osmotic/ oncotic forces. Selective permeability of plasma membranes and the bidirectional transport of ions and water is critical to the process. A number of cellular activities depend on a host of channels, water and ion transporters constitutively expressed on or translocated to the surface of cells in a regulated manner. Most notably, the generation of a transmembrane potential, which in excitable cells drives intercellular currents, action potentials and contraction/relaxation cycles, largely depends on the state of the opening of the ion channels and the activity of transmembrane pump proteins. Many of these structures serve both as ion gates/carriers and signaling molecules, as certain ion fluxes encode for functional responses in target cells. This is the case for a host of vasoconstrictors, such as angiotensins, endothelins and arginine vasopressin, which induce internal Ca2+ redistribution or currents in cells displaying the appropriate receptors (1, 2). Transmembrane signals are also encoded by frequency or amplitude of oscillatory Ca2+ currents, in turn actuated by cyclic membrane gating (3). A superfamily of such channels, the so-called transient receptor potential (TRP) channels, has recently attracted considerable interest. TRP are heterotetrameric polypeptides initially identified as photoreceptors in insect retinal cells, and later recognized as cation channels in a variety of sensing apparatuses (including visual and hearing structures, such as cochlea sensor y hair cells) (4-6). Cation influx through these structures, particularly Ca2+, is typically controlled by Ca2+ ions themselves, a process often referred to as “capacitative Ca2+ influx” or “Ca2+-activated Ca2+ influx” (7, 8). Selectivity of TRP channels for divalent versus monovalent ions (eg, Ca2+ vs. Na+) www.sin-italy.org/jnonline/vol19n1/ 21 TRP channels and calcium in the kidney ranges from >100:1 to 1:1, based on isoform structure and tissue type. It is now recognized that TRP channels are expressed in many different structures and organs, and play a key role in Ca2+ transport in excitable cells, including vascular contractile smooth muscle cells (SMC), as well as in renal tubular cells and other epithelia. In the kidney, one such channel is involved in the regulation of the Ca2+ external balance, as recently shown by the TRP-knockout mouse model, which exhibits hypercalciuria and skeletal defects consistent with altered distal tubular reabsorption of Ca2+(9, 10). The mutation of the components of the TRP superfamily of proteins are associated with long-known genetic diseases, such as adult polycystic kidney disease (PKD), linked to polycystine 1 and/or 2 (PC2) defects (11, 12). Inasmuch as renal ion transport is the key to external balance and fluid homeostasis, and intracellular [Ca2+] ([Ca2+]i) is a major modulator of vascular reactivity, it is likely that TRP cation channels play a role in the control of blood pressure (BP) and, therefore, also in the pathogenesis of arterial hypertension. TRP, A SUPERFAMILY OF UBIQUITOUS DIVALENT CATION CHANNELS Mammalian homologues of Drosophila TRP proteins form an ever growing list of ubiquitous Ca2+ and/or Mg 2+-permeant, non-selective cation channels, of which some 50 members have been identified to date (4, 6, 13, 14). The TRP superfamily includes TRPA channels, mostly involved in hearing, three homologous subfamilies (TRPC, TRPV and TRPM), and three distantly related subfamilies (TRPP, TRPML and TRPN or ANKTM1) (Tab. I). Importantly, TRP proteins assemble into heterotetramers to form native channels, for example, variable combinations of distinct isoforms in ratios of 1:3, 1:2:1, etc. This implies that the electrophysiology and the selectivity of a channel are dictated by the heterogeneity of the assembled channels (13, 14). A typical classical - or canonic (C) TRP protein, such as human TRPM3, is composed of 1555 amino acids, encoded by a gene comprising 24 exons mapping to chromosome 9q-21.12. Its structure includes six transmembrane domains with cytoplasmic N- and C-termini, incorporating several putative regulator y sites, including calmodulin/inositol (1, 4, 5)-trisphosphate (InsP3) receptor binding sites, PDZ binding motifs, phosphorylation sites for protein kinases, ankyrin-like repeats and proline-rich motifs (4, 6, 13, 14) (Fig. 1). The N- terminus displays a diacylglycerol (DAG) regulatory site. Many studies show direct TRPC regulation by DAG, as in the case of TRPC3 expressed in Chinese hamster ovary cells, or by related metabolites of phospholipase C, such as polyunsaturated fatty acids or 22 Fig. 1 - A schematic diagram of the structure of two prototypical TRP channels with six transmembrane-spanning domains. TRPM2 (also labeled TRPC7 or LTRPC2) is a nonselective Ca2+ channel sensitive to H2O2, oxidative stress and α. Note the C-terminal NUDT9 Nudix hydrolase domain, TNF-α which binds ADP-ribose or NAD with resulting conformational and ion gating changes. The TRP domain near the Cterminus is a highly conserved 25-amino acid stretch, sometimes replaced by a kinase or phosphatase domain (“chanzymes”, see text). TRPV6 is a duodenal epithelial Ca2+ channel (EcaC-2)/calcium transporter (CaT1) displaying ankyrin repeats towards the N-terminus. phosphatidylinositol 4,5-bisphosphate (15, 16). Conserved molecular domains in all members of the TRP family include ankyrin-like repeats near the N- terminus and a “TRP domain” at the C- terminus, which is a highly conserved 25-amino acid stretch with still unknown functions (Fig. 1). At least one member of the superfamily, TRPM5, displays voltage modulation, despite the general absence of positively charged amino acid residues in the 4th transmembrane segment, a typical feature of voltage-gated cation channels (17). Members of the TRP superfamily are fairly ubiquitous and display a highly conserved structure throughout the evolutionary path, serving a variety of functions in several tissues, as listed in Table I (4, 11). The central nervous system and peripheral sensing apparatuses are the main areas of TRP channel distribution. Nevertheless, the list of tissues expressing one or more members of the superfamily is continuously expanding, as are their proposed functions. The early concept of TRP as signaling molecules has evolved into that of multifunctional ion channels, also responsible for the bulk transport of electrolytes by specialized epithelia (kidney, intestine) (6). TRP CHANNELS AND TRANSMEMBRANE CA2+ SIGNALING The involvement of TRP proteins in capacitative Ca2+ influx has been definitively demonstrated almost 10 Menè TABLE I - PROPOSED FUNCTIONS OF MEMBERS OF THE SEVEN MAJOR KNOWN TRP CHANNEL SUBFAMILIES IN VARIOUS SPECIES TRPA (Ankyrin) 1 hearing in vertebrates TRPC (Canonical) 1 2 3 4 5 6 7 sperm acrosome reaction, pheromone sensing neurodifferentiation, synaptic development vasorelaxation, microvascular permeability vascular tone regulation slit diaphragm/podocyte foot processes, structural TRPM (Melastatin) TRPML (Mucolipin) 1 2 3 4 5 6 7 8 melanoma tumor suppressor redox-sensing, oxidative stress-induced apoptosis 1 2 3 mucolipidosis cation selective channel taste cells familial hypomagnesemia cell survival, proliferation thermal sensing, tumor marker TRPN (NOMP), TRPL, Drosophila TRP phototransduction (insect), mechanosensation TRPP (Polycystin) 1 2 3 5 autosomic dominant polycystic kidney disease (ADPKD) ADPKD left-right asymmetry in embryogenesis ADPKD ADPKD TRPV (Vanilloid) 1 2 3 4 5 6 OSM-9 nociception nociception nociception hearing, osmotic sensing Ca2+ transport, kidney tubules Ca2+ transport, duodenum years ago (14, 18). The process accounts for the ability of various stimuli of the discharge of intracellularly stored Ca2+ (namely all agents that trigger phospholipase C-γ-mediated breakdown of phosphoinositides, releasing inositol (1, 4, 5)-trisphosphate, InsP3) to activate an inward Ca2+ conductance that refills the stores and maintains a persistent elevation of [Ca2+]i (2, 16). This relatively non-selective influx pathway is currently known as store-operated Ca 2+ channel (SOC) or ICRAC (intracellular Ca2+ release-activated Ca2+ influx channel) (1, 2, 5, 7). Some controversy exists in the literature concerning the definition of the channel as a receptor-operated channel (ROC). Such structures should involve receptors releasing InsP3 upon direct binding of a ligand, with a possible intermediation of G-proteins. InsP3 itself apparently binds to a receptor expressed on Ca2+ stores, such as the endoor sarcoplasmic reticulum (also called “calciosomes”), and possibly other organelles (7, 14). There seems to be no direct binding of extracellular ligands to the TRP channel, whose operation seems instead controlled by calmodulin/InsP 3 or protein kinases. Therefore, it seems more appropriate to consider it as a SOC, with Ca2+ acting as a second messenger, perhaps in concert with another store-associated, simultaneously released, putative signaling molecule (5, 7, 14). Cells from genetically engineered TRP-null mutants display minimal or no capacitative Ca2+ influx; on the other hand, it has been possible to express Ca2+ currents in Xenopus oocytes by transfecting TRP homologues (5, 8, 14). Again, functional behavior as ROC or SOC can also depend on the different subunits assembled to form the native channel (6). In the kidney, there is extensive evidence of SOC activity, as revealed by our own continuous fluorescence monitoring of [Ca2+]i in cultured rat and human smooth muscle-like glomerular mesangial cells (19-21). These and other experiments in renal cells 23 TRP channels and calcium in the kidney occurs when CaCl2 is added extracellularly. Thirdly, releasing intracellular stores by pharmacologic means, i.e. by any of the above-mentioned vasoconstrictors or bypassing InsP3-coupled receptors with the sarcoplasmic reticulum Ca 2+-ATPase (SERCA) inhibitor, thapsigargin, potently enhances Ca2+ influx (Fig. 2, panel C). These SOC features seem quite suited for the “tonic” regulation of contractile cell activity, since they grant a constant influx of Ca2+, amplifying the effects of rapid spikes of [Ca2+]i induced by vasoconstrictors (1, 3, 7). Therefore, intermittent ANG II generation could produce long-lasting contraction of the glomerular microcirculation, in turn critical for the so-called autoregulation of renal blood flow. The issue is also relevant to systemic circulation and to other vascular districts, since mesangial cells can be considered vascular SMC (VSMC) of the glomerulus (23, 24). Both cardiac myocytes and pulmonary artery SMC display fully functional TRPC isoforms (25, 26). In cardiac myocytes, gene knock-out of SERCA pumps (duplicating the effects of thapsigargin) translates into TRPC4 and -5 upregulation (27). Fig. 2 - Evidence for capacitative Ca2+ influx through storeoperated Ca2+ channels in cultured human glomerular mesangial cells (HMC). Panel A, a [Ca2+]i transient induced by 1 uM angiotensin II (ANG II) in the presence (upper trace) or absence of extracellular Ca2+ in the bathing media (Ca2+-free). Note the disappearance of the persistent [Ca2+]i elevation of lesser amplitude in the absence of external Ca2+. B, Ca2+ influx upon previous discharge of intracellular Ca2+ stores by switching media to a Ca2+-free solution. C, thapsigargin (TPS, 0.1 mM), a SERCA inhibitor, transiently increases [Ca2+]i in cells held in Ca2+-free solutions by releasing intracellular stores; this potentiates subsequent Ca2+ influx once 1-10 mM Ca2+ (as CaCl2) is added (compare amplitude of the [Ca2+]i responses with panel B). Similar effects can be obtained with ANG II or other receptor-mediated vasoconstrictors (not shown). Fluorescence monitoring of fura 2-loaded monolayers of HMC, alternate excitation/emission wavelengths 340/380 and 500 nm, respectively. have clearly shown that releasing intracellularly stored Ca2+ through receptor-operated and receptor-independent mechanisms promotes subsequent Ca2+ influx (9, 19-22). This is illustrated by three lines of evidence, summarized by the representative tracings in Figure 2. First, conventional phospholipase C agonists (angiotensin II (ANG II), vasopressin and thromboxane A2) transiently increase [Ca2+]I; this initial “spike” is followed by the sustained elevation of [Ca2+]i only if the cells are bathed by media containing extracellular Ca2+, but not in Ca2+-free media. Secondly, holding the cells in a Ca2+-free solution is followed by a reduction in baseline [Ca2+]i. This protocol quickly depletes the intracellular stores, in an attempt to balance the outward Ca2+ flow down a reversed transmembrane gradient. A substantial, progressive influx of Ca2+ then 24 TUBULAR EPITHELIAL CA2+ AND MG2+ TRANSPORT THROUGH TRP CHANNELS Recent studies clarified that TRP do not only exist in most cell lines as a sensing/signaling apparatus, but also serve as classical ports for transepithelial Ca2+, Mg2+ (and perhaps other ions) fluxes. TRPV5 cloning from vitamin D-responsive rabbit tubular epithelial cells, and the cloning of TRPV6 (which shares a 75% homology with the 5 isoform of subfamily V) from rat duodenum suggests that these channels are responsible for vitamin D-stimulated Ca2+ absorption in the distal nephron and in enterocytes, respectively (9, 10, 28) (Fig. 1). They have been previously referred to as epithelial Ca2+ channels 1 and 2 (EcaC1, EcaC2). Notably, TRPV5 and -6 tissue expression seems under the transcriptional control of 1,25 (OH)2D3, estrogens and plasma Ca2+ levels, consistent with a candidate role in divalent ion homeostasis at the whole body level (9, 10, 28). In the kidney, the parallel activity of a Na+/Ca2+ exchanger and Ca2+-ATPase of tubular cells appears to maintain the cytosolic inward gradient supporting passive reabsorption of filtered Ca2+ through apical TRPV6 channels in distal convoluted tubules (29). This isoform is also expressed in the medullary collecting tubule, a segment apparently not involved in Ca2+ reabsorption (30). TRPV5 and -6 also form multimers in the distal convoluted tubule. A recent report by Hoenderop et al employed genetic ablation of TRPV5 in the distal convolute tubule of the murine nephron, where a substantial amount of Ca2+ reab- Menè sorption takes place (10). These TRPV5-null mice failed to reabsorb Ca2+, with resulting hypercalciuria and polyuria, leading to altered bone mineral density, elevated circulating 1,25-(OH)2D3 levels and skeletal abnormalities (10). The observation seems relevant to the pathogenesis of a number of human disorders linked to hypercalciuria, ranging from idiopathic hypercalciuria to kidney stones to various forms of nephrocalcinosis, such as the medullary sponge kidney. Even osteoporosis has been suggested to result from age- or hormonal-dependent TRPV5/-6 dysregulation (10). TRPM6 and TRPM7, among the eight members of the melastatin subfamily of TRP channels, are currently believed responsible for epithelial Mg 2+ transport (Tab. I, Fig. 1). TRPM6 mutations have been linked to hereditary hypomagnesemia, a syndrome also characterized by secondary hypocalcemia. The unique atypical kinase activity exhibited at the C-terminus by both TRPM channels has suggested the use of the term “chanzymes” to describe non-conventional channel proteins, endowed with dual functions (31). TRP CHANNELS AND RENAL CYSTIC DISEASES The appreciation that TRPC are integral components of the luminal plasma membrane of tubular epithelial cells has led to the evaluation of other possible roles of these molecules. Epithelial cell cyst formation in autosomic dominant polycystic kidney disease (ADPKD) has recently been linked to the PKD2 gene product, a TRP Ca2+-permeable, non-selective channel protein of the P subfamily, isoforms 1-5 (6, 11, 12). TRPP2 shares 25% amino acid identity with TRPC3 and -6 proteins, at the level of the transmembrane spanning segments IV-VI. The homologues TRPP3 and -5 are reportedly not mutated in ADPKD. On the other hand, TRPP1 corresponding to PKD1 is a non-channel, larger polypeptide with 11 transmembrane-spanning regions, which can complex and regulate PKD2. It has recently been suggested that this protein, expressed on a restricted area next to the basal body/centrosome area of the cilium displayed by many tubular cells, serves as a Ca2+ gating mechanism activated by the bending of the cilium under the luminal flow (32). The stimulation of cilia in cultured epithelial cells exposed to a flux of bathing media results in Ca2+ entry (33). On the other hand, PKD1-null or cells lacking the cilium itself display reduced Ca2+ responses upon flow exposure; similarly, blocking Abs to PKD1 or PKD2 impair Ca2+ influx in tubular epithelial cells (32-34). Consistent with the concept of TRP-related ciliary protein defects in ADPKD, the Tg737orpk mouse, a recently developed animal model, displays increased ciliary PKD2 levels (35). Therefore, defective sensing of transepithelial flow could play a role in the formation and growth of cysts in the kidney and perhaps other organs. Ciliar y mechanosensing can also bear relevance to the embr yology and biology of other organisms such as C. elegans, which possesses homologues of PKD1 and 2 (36). Recent development in the research on ciliary proteins has led to the identification of a number of other mutated components that could provide a pathophysiologic basis for cystic kidney diseases. This seems to be the case for 450 KDa PKHD1 or fibrocystin, defective in autosomic recessive polycystic kidney disease, NPHP1 or nephrocystine, altered in nephronophtysis, and BBS4-8, mutated in the BardetBiedl oro-facial-digital syndrome (37, 38). TRP CHANNELS: LINKS TO ARTERIAL HYPERTENSION? Following the characterization of TRPC as SOC in most non-excitable cell types, recent studies link defective TRP activity to impaired vasorelaxation, as in aortic rings or endothelial cells from TRPC4-/- null mice (39). Interestingly, the phenomenon is associated with reduced nitric oxide synthesis and the resulting attenuation of agonist-induced, L-nitroargininesensitive vasorelaxation. In the same experimental model, thrombin-induced microvascular permeability is reportedly decreased, along with impaired endothelial cell motility and stress-fiber morphology (40). This is further proof that TRP/SOC operation is implicated in VSMC contractility and/or endothelial function, with potential links to arterial hypertension. A role of TRPC6 in the control of vascular tone and, hence, of BP is shown by studies on the Ca2+ currents activated by α-adrenoceptors, and by the ability of antisense oligodeoxynucleotides (ODNs) to TRPC6 to reduce arterial smooth muscle depolarization and constriction induced by elevated pressure in intact cerebral arteries (41). Anti-TRPC6 ODNs also inhibit a cation current involved in pressure-induced myogenic depolarization, similar to micromolar concentrations of gadolinium, a blocking substitute for mono- or divalent cations (42). Studies in VSMC cultures from SHR hypertensive/ WKY normotensive rats, point to differential regulation of TRP channel proteins and their induction by vasoconstrictors, such as ANG II. TRPM7 content has been reported to be lower in SHR cells compared to their WKY counterparts, translating in decreased intracellular Mg2+, a divalent cation selectively internalized through this channel. TRPM6 is upregulated by ANG II, while the vasoconstrictor failed to affect TRPM7 levels in SHR-derived VSMC, resulting in reduced translocation of annexin-1, a specific TRPM-7 substrate involved in the enzymatic cascades of apop25 TRP channels and calcium in the kidney tosis (43). This could affect the proliferation/apoptosis balance in VSMC, with implications for the cellular composition of vessels in hypertensive rats (44). Moreover, regulation of the expression and/or operation of TRP channels by ANG II is further evidence of their implication in signal transduction for vasoconstrictors, partly through persistent Ca 2+ (and perhaps Mg2+) inward currents following the initial release of stored Ca2+. Hyperexpression of TRPC 3 and -6 in VSMC from patients with primar y pulmonar y hypertension could indicate a pathogenetic role of these channels in this setting (26, 42). Since systemic, “essential” arterial hypertension is often associated with increased sensitivity to vasoconstrictors, and altered [Ca 2+] i responses have been described in animal models and human hypertension, there is a potential for TRPC to be involved in this area as well. Moreover, VSMC proliferation is sensitive to [Ca2+]i, with impaired cell growth by the removal of extracellular Ca2+ or the blockade of voltage-gated Ca2+ entry. Increased [Ca2+]i appears instead to promote cell cycling and gene transcription, a mechanism that can apply to ciliary defects leading to cyst formation in ADPKD (32-35, 44). The correlation between TRPC6 expression and VSMC entry in the S and G2/M phases of the cell cycle shown by Yu et al (26) points to capacitative Ca2+ influx as one mechanism controlling hypertrophy of VSMC and perhaps myocardial cells, relevant to pulmonar y and systemic hypertension (26, 39, 40). The role of SOC in providing sustained [Ca2+]i in VSMC isolated from human pulmonary arteries is backed by and possibly functionally coupled to a Na+/Ca2+ exchanger (25). TRP could be implicated in other cellular functions relevant to vascular disease, atherosclerosis and hypertension. Their involvement in apoptosis and cellular proliferation ranges from the upregulation of TRPM members (melastatin) in tumors (45, 46) to enhanced apoptosis in response to reactive oxygen species (ROS), as in the case of TRPM2, regulated by H2O2 , ADP-ribose, and tumor necrosis factor alpha (TNF-α) (47, 48) (Fig. 1). TRP Ca2+ channels have been shown to serve as redox sensors in the vascular endothelium (47). TRPC3 expression mediates the nitric oxide sensitivity of SOC. Overexpression in HEK293 cells confirmed that TRPC3 and TRPC4 have features of redox sensitive cation channels (48, 49). ROS-activated protein tyrosine phosphorylation and phospholipase C are involved in redox activation of TRPC3. Furthermore, oxidative stress-induced disruption of caveolin 1-rich lipid raft domains interferes with functional TRPC channels, contributing to redox modulation of TRP proteins and to oxidative stress-induced changes in cellular Ca2+ signaling (48). Apoptosis can be pharmacologi26 cally modulated through the depression or the activation of Ca 2+ currents (50). Pathological redox states can promote cell death through TRP channelmediated Ca2+ fluxes, as shown for TRPM2 (47, 48). This protein, already labeled LTRPC2 or TRPC7 (Fig. 1) contains an ADP-ribose pyrophosphatase domain, which catalyzes the hydrolysis of nucleoside diphosphates. As mentioned earlier, this is an example of a subfamily of channels endowed with enzymatic activity, the so-called chanzymes. The Nudix hydrolase domain at the C-terminus of TRPM2 serves as a binding site for nucleotides (ADP-ribose, NAD), which then promote Ca2+ entry and apoptosis of cells exposed to ROS and/or to a high redox microenvironment (47-49). In summary, TRP channels are implicated at various levels at the vascular cell/circulating inflammatory cell interface, where oxidative stress, leukocyte activation and disorderly proliferation of endothelial cells are associated with atherosclerotic plaques, often in the context of arterial hypertension (51, 52). TRP CHANNELS, PODOCYTES AND FOCAL GLOMERULOSCLEROSIS One recent advance in the pathophysiologic roles of TRP channels is the parallel description by two independent research groups of a mutation of the TRPC6 gene on chromosome 11q in six families with autosomal dominant focal segmental glomerulosclerosis (FSGS) (53, 54). TRPC6 is apparently expressed in the foot processes of podocytes, which are severely effaced in this disorder, a lesion responsible for massive proteinuria with resulting nephrotic syndrome. Mutation is located at the level of proline 112, replaced by glutamine in one of three ankyrin repeats. This breakthrough discovery, if confirmed, will shed new light on the role of ion channels in podocyte physiology, as TRPC6 protein displays altered intracellular distribution in podocytes from subjects with FSGS, along with increased current amplitudes and ANG II-induced [Ca2+]i signals (53, 54). TRPC6 could be involved in guiding slit diaphragm assembly around the foot processes, and perhaps control podocyte proliferation, apoptosis or other cellular functions through enhanced Ca2+ signaling (55, 56). These data, taken together with recent evidence of a role of mutated podocyte proteins in other congenital forms of nephrotic syndrome, as in the case of the nephrin-podocin complex, could contribute to a new approach in the study of proteinuric glomerular diseases (55). At the same time, they provide further support to the concept of a structural and functional role of TRP channels well beyond ion gating and signal transduction. Menè CONCLUSIONS The identification and the characterization of TRP cation channels is one of the most exciting recent developments of research concerning signaling and ion transport. These cellular processes are becoming increasingly linked by the discovery of multifunctional proteins that assemble in a variety of combinations, according to the required functions. The involvement of Ca2+ in intracellular signaling has been known for almost 20 yrs. It is now becoming apparent that the same mechanisms that allow instantaneous firing of action potentials in the visual apparatus of insects, also serve as sensors of luminal flow in renal tubules, and at the same time as regulators of foot process morphology in podocytes or ion transporters in the distal nephron. This is remarkable in evolutionary terms, and constitutes evidence of an additional, novel role of ion carriers as sensors of the surrounding environment (57, 58). TRP are also apparently implicated in the pathogenesis of a host of long-known genetic and acquired diseases. The development of pharmacologic inhibitors of non-voltage gated Ca2+ entry (59) is underway, with promising potential in the treatment of cardiovascular and renal disorders ranging from arrhythmias to hypertension, from mineral and electrolyte disturbances to nephrolithiasis and to hereditary cystic diseases. ACKNOWLEDGEMENTS This work has been supported by research grants from the Ministry of the University of Italy (MIUR - Ricerche di Facoltà, Ricerche di Ateneo). Address for correspondence: Paolo Menè, M.D. U.O.C. Nefrologia Azienda Ospedaliera Sant’ Andrea Via di Grottarossa 1035-1039 00189 Rome, Italy Paolo.Mene@uniroma1.it REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Berridge MJ, Bootman MD, Roderick HL. Calcium signalling: dynamics, homeostasis and remodelling. Nat Rev Mol Cell Biol 2003; 4: 517-29. Bird GS, Aziz O, Lievremont JP, Wedel BJ, Trebak M, Vazquez G, Putney JW Jr. Mechanisms of phospholipase C-regulated calcium entry. Curr Mol Med 2004; 4: 291-301. Berridge MJ. The endoplasmic reticulum: a multifunctional signaling organelle. Cell Calcium 2002; 32: 235-49. Montell C, Birnbaumer L, Flockerzi V. The TRP channels, a remarkably functional family. Cell 2002; 108: 595-8. Putney JW Jr. The enigmatic TRPCs: multifunctional cation channels. Trends Cell Biol 2004; 14: 282-6. Huang CL. The transient receptor potential superfamily of ion channels. J Am Soc Nephrol 2004; 15: 1690-9. Putney JW Jr, Broad LM, Braun FJ, Lievremont JP, Bird GS. Mechanisms of capacitative calcium entry. J Cell Sci 2001; 114: 2223-9. Elliott AC. Recent developments in non-excitable cell calcium entry. Cell Calcium 2001; 30: 73-93. Hoenderop JG, van der Kemp AW, Hartog A, van de Graaf SF, van Os CH, Willems PH, Bindels RJ. Molecular identification of the apical Ca 2+ channel in 1,25-dihydroxyvitamin D3responsive epithelia. J Biol Chem 1999; 274: 8375-8. Hoenderop JG, van Leeuwen JP, van der Eerden BC, Kersten FF, van der Kemp AW, Merillat AM, Waarsing JH, Rossier BC, 11. 12. 13. 14. 15. 16. 17. 18. Vallon V, Hummler E, Bindels RJ. Renal Ca2+ wasting, hyperabsorption, and reduced bone thickness in mice lacking TRPV5. J Clin Invest 2003; 112: 1906-14. Venglarik CJ, Gao Z, Lu X. Evolutionary conservation of Drosophila polycystin-2 as a calcium-activated cation channel. J Am Soc Nephrol 2004; 15: 1168-77. Cantiello HF. Regulation of calcium signaling by polycystin-2. Am J Physiol Renal Physiol 2004; 286: F1012-29. Clapham DE, Montell C, Schultz G, Julius D. International Union of Pharmacology. XLIII. Compendium of voltagegated ion channels: transient receptor potential channels. Pharmacol Rev 2003; 55: 591-6. Inoue R, Hanano T, Shi J, Mori Y, Ito Y. Transient receptor potential protein as a novel non-voltage-gated Ca2+ entry channel involved in diverse pathophysiological functions. J Pharmacol Sci 2003; 91: 271-6. Venkatachalam K, Zheng F, Gill DL. Regulation of canonical transient receptor potential (TRPC) channel function by diacylglycerol and protein kinase C. J Biol Chem 2003; 278: 29031-40. Hardie RC. Regulation of TRP channels via lipid second messengers. Annu Rev Physiol 2003; 65: 735-59. Hofmann T, Chubanov V, Gudermann T, Montell C. TRPM5 is a voltage-modulated and Ca2+-activated monovalent selective cation channel. Curr Biol 2003; 13: 1153-8. Spassova MA, Soboloff J, He LP, Hewavitharana T, Xu W, Venkatachalam K, van Rossum DB, Patterson RL, Gill DL. Cal- 27 TRP channels and calcium in the kidney 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 28 cium entry mediated by SOCs and TRP channels: variations and enigma. Biochim Biophys Acta 2004; 1742: 9-20. Menè P, Teti A, Pugliese F, Cinotti GA. Calcium releaseactivated calcium influx in cultured human mesangial cells. Kidney Int 1994; 46: 122-8. Menè P, Pugliese F, Cinotti GA. Regulation of capacitative calcium influx in cultured human mesangial cells: roles of protein kinase C and calmodulin. J Am Soc Nephrol 1996; 7: 983-90. Menè P. Calcium channel blockers: what they can and what they can’t. Nephrol Dial Transplant 1997; 12: 25-8. Wang X, Pluznick JL, Wei P, Padanilam BJ, Sansom SC. TRPC4 forms store-operated Ca2+ channels in mouse mesangial cells. Am J Physiol Cell Physiol 2004; 287: C357-64. Menè P, Simonson MS, Dunn MJ. Physiology of the mesangial cell. Physiol Rev 1989; 69: 1347-424. Rupprecht HD, Sterzel RB. Glomerular mesangial cells. In Neilson EG, Couser WG Eds. Immunologic Renal Diseases. Philadelphia: Lippincott-Raven 1997; 595-626. Zhang S, Yuan JX, Barrett KE, Dong H. Role of Na+/Ca2+ exchange in regulating cytosolic Ca2+ in cultured human pulmonary artery smooth muscle cells. Am J Physiol Cell Physiol 2004; 288: C245-52. Yu Y, Fantozzi I, Remillard CV, Landsberg JW, Kunichika N, Platoshyn O, Tigno DD, Thistlethwaite PA, Rubin LJ, Yuan JX. Enhanced expression of transient receptor potential channels in idiopathic pulmonary arterial hypertension. Proc Natl Acad Sci U S A 2004; 101: 13861-6. Seth M, Sumbilla C, Mullen SP, Lewis D, Klein MG, Hussain A, Soboloff J, Gill DL, Inesi G. Sarco(endo)plasmic reticulum Ca2+ ATPase (SERCA) gene silencing and remodeling of the Ca2+ signaling mechanism in cardiac myocytes. Proc Natl Acad Sci U S A 2004; 101: 16683-8. Peng JB, Chen XZ, Berger UV, Vassilev PM, Tsukaguchi H, Brown EM, Hediger MA. Molecular cloning and characterization of a channel-like transporter mediating intestinal calcium absorption. J Biol Chem 1999; 274: 22739-46. Hoenderop JG, Voets T, Hoefs S, Weidema F, Prenen J, Nilius B, Bindels RJ. Homo- and heterotetrameric architecture of the epithelial Ca2+ channels TRPV5 and TRPV6. EMBO J 2003; 22: 776-85. Nijenhuis T, Hoenderop JG, van der Kemp AW, Bindels RJ. Localization and regulation of the epithelial Ca2+ channel TRPV6 in the kidney. J Am Soc Nephrol 2003; 14: 2731-40. Schlingmann KP, Gudermann T. A critical role of TRPM channel-kinase for human magnesium transport. J Physiol 2005; 566: 301-8. Yoder BK, Hou X, Guay-Woodford LM. The polycystic kidney disease proteins, polycystin-1, polycystin-2, polaris, and cystin are co-localized in renal cilia. J Am Soc Nephrol 2002; 13: 2508-16. Praetorius HA, Spring KR. The renal cell primary cilium functions as a flow sensor. Curr Opin Nephrol Hypertens 2003; 12: 517-20. Nauli SM, Alenghat FJ, Luo Y, Williams E, Vassilev P, Li X, Elia AE, Lu W, Brown EM, Quinn SJ, Ingber DE, Zhou J. Polycystins 1 and 2 mediate mechanosensation in the primary cilium of kidney cells. Nat Genet 2003; 33: 129-37. Liu W, Murcia NS, Duan Y, Weinbaum S, Yoder BK, Schwiebert E, Satlin LM. Mechanoregulation of intracellular Ca 2+ concentration is attenuated in collecting duct of monocilium-impaired orpk mice. Am J Physiol Renal Physiol 2005; 289: F978-88. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. Minke B, Cook B. TRP channel proteins and signal transduction. Physiol Rev 2002; 82: 429-72. Menezes LF, Cai Y, Nagasawa Y, Silva AM, Watkins ML, Da Silva AM, Somlo S, Guay-Woodford LM, Germino GG, Onuchic LF. Polyductin, the PKHD1 gene product, comprises isoforms expressed in plasma membrane, primary cilium, and cytoplasm. Kidney Int 2004; 66: 1345-55. Parisi MA, Bennett CL, Eckert ML, Dobyns WB, Gleeson JG, Shaw DW, McDonald R, Eddy A, Chance PF, Glass IA. The NPHP1 gene deletion associated with juvenile nephronophthisis is present in a subset of individuals with Joubert syndrome. Am J Hum Genet 2004; 75: 82-91. Freichel M, Suh SH, Pfeifer A, Schweig U, Trost C, Weissgerber P, Biel M, Philipp S, Freise D, Droogmans G, Hofmann F, Flockerzi V, Nilius B. Lack of an endothelial store-operated Ca2+ current impairs agonist-dependent vasorelaxation in TRP4-/- mice. Nat Cell Biol 2001; 3: 121-7. Tiruppathi C, Minshall RD, Paria BC, Vogel SM, Malik AB. Role of Ca2+ signaling in the regulation of endothelial permeability. Vascul Pharmacol 2002; 39: 173-85. Welsh DG, Morielli AD, Nelson MT, Brayden JE. Transient receptor potential channels regulate myogenic tone of resistance arteries. Circ Res 2002; 90: 248-50. Fantozzi I, Zhang S, Platoshyn O, Remillard CV, Cowling RT, Yuan JX. Hypoxia increases AP-1 binding activity by enhancing capacitative Ca 2+ entr y in human pulmonar y arter y endothelial cells. Am J Physiol Lung Cell Mol Physiol 2003; 285: L1233-45. Touyz RM, He Y, Montezano AC, Yao G, Chubanov V, Gudermann T, Callera GE. Differential regulation of TRPM6/7 cation channels by ANG II in vascular smooth muscle cells from spontaneously hypertensive rats. Am J Physiol Regul Integr Comp Physiol 2005; 290: R73-8. Landsberg JW, Yuan JX. Calcium and TRP channels in pulmonary vascular smooth muscle cell proliferation. News Physiol Sci 2004; 19: 44-50. Duncan LM, Deeds J, Hunter J, Shao J, Holmgren LM, Woolf EA, Tepper RI, Shyjan AW. Down-regulation of the novel gene melastatin correlates with potential for melanoma metastasis. Cancer Res 1998; 58: 1515-20. McNulty S, Fonfria E. The role of TRPM channels in cell death. Pflugers Arch 2005:451: 235-42. Perraud AL, Fleig A, Dunn CA, Bagley LA, Launay P, Schmitz C, Stokes AJ, Zhu Q, Bessman MJ, Penner R, Kinet JP, Scharenberg AM. ADP-ribose gating of the calcium-permeable LTRPC2 channel revealed by Nudix motif homology. Nature 2001; 411: 595-9. Groschner K, Rosker C, Lukas M. Role of TRP channels in oxidative stress. Novartis Found Symp 2004; 258: 222-30. Trebak M, St J, Bird G, McKay RR, Birnbaumer L, Putney JW, Jr. Signaling mechanism for receptor-activated canonical transient receptor potential 3 (TRPC3) channels. J Biol Chem 2003; 278: 16244-52. Hara Y, Wakamori M, Ishii M, Maeno E, Nishida M, Yoshida T, Yamada H, Shimizu S, Mori E, Kudoh J, Shimizu N, Kurose H, Okada Y, Imoto K, Mori Y. LTRPC2 Ca2+-permeable channel activated by changes in redox status confers susceptibility to cell death. Mol Cell 2002; 9: 163-73. Heiner I, Esfeld J, Luckoff A. Role and regulation of TRP channels in neutrophil granulocytes. Cell Calcium 2003; 33: 533-40. Ross R. Atherosclerosis - an inflammatory disease. N Engl J Med 1999; 340: 115-26. Menè 53. 54. 55. 56. Winn MP, Conlon PJ, Lynn KL, Farrington MK, Creazzo T, Hawkins AF, Daskalakis N, Kwan SY, Ebersviller S, Burchette JL, Pericak-Vance MA, Howell DN, Vance JM, Rosenberg PB. A mutation in the TRPC6 cation channel causes familial focal segmental glomerulosclerosis. Science 2005; 308: 1801-4. Reiser J, Polu KR, Moller CC, Kenlan P, Altintas MM, Wei C, Faul C, Herbert S, Villegas I, Avila-Casado C, McGee M, Sugimoto H, Brown D, Kalluri R, Mundel P, Smith PL, Clapham DE, Pollak MR. TRPC6 is a glomerular slit diaphragm-associated channel required for normal renal function. Nat Genet 2005; 37: 739-44. Walz G. Slit or pore? A mutation of the ion channel TRPC6 causes FSGS. Nephrol Dial Transplant 2005; 20: 1777-9. Kriz W. TRPC6 - a new podocyte gene involved in focal segmental glomerulosclerosis. Trends Mol Med 2005; 11: 527-30. 57. 58. 59. Montell C. Drosophila TRP channels. Pflugers Arch 2005; 451: 19-28. Nilius B, Voets T. TRP channels: a TR(I)P through a world of multifunctional cation channels. Pflugers Arch 2005; 451: 110. Li S, Gosling M, Poll CT, Westwick J, Cox B. Therapeutic scope of modulation of non-voltage-gated cation channels. Drug Discov Today 2004; 9: 1045-54. Received: September 25, 2005 Revised: November 28, 2005 Accepted: December 19, 2005 © Società Italiana di Nefrologia 29