72x36 Poster Template - Sunesis Pharmaceuticals
advertisement

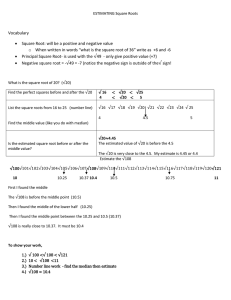
Results of a Phase 2 Pharmacokinetic/Pharmacodynamic (PK/PD) Study of Combination Voreloxin and Cytarabine in Patients With Relapsed or Refractory Acute Myeloid Leukemia GJ Roboz1, JE Lancet2, LD Cripe3, F Ravandi4, RK Stuart5, AF List2, JA Fox6, G Michelson6, JE Karp7 University / NY Presbyterian Hospital, New York, NY; 2H Lee Moffitt Cancer Center, Tampa, FL; 3Indiana University Cancer Center, Indianapolis, IN; 4University of Texas MD Anderson Cancer Center, Houston,TX; 5Medical University of South Carolina, Charleston, SC; 6Sunesis Pharmaceuticals, Inc., South San Francisco, CA; 7Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins, Baltimore, MD Study Design Phase 2 voreloxin in combination with cytarabine in primary refractory and first relapse AML Population Primary refractory: failed to achieve CR or CRp following 1 or more cycles of induction, or CR1 < 90 days First relapse: relapse following CR1 ≥ 90 days and ≤ 24 months Voreloxin and Cytarabine Dose Regimens Objectives ASCO 2010 80 or 90 mg/m2 voreloxin on days 1 and 4 by short ≤ 10 minute IV infusion in combination with 400 mg/m2/d CIV cytarabine on days 1-5 or 1 g/m2/d 2-hr IV infusion cytarabine on days 1-5 Safety, pharmacokinetics, antileukemic activity VORELOXIN: AN ANTICANCER QUINOLONE DERIVATIVE (AQD) (PLoS ONE, 2010) ● Novel, stable scaffold offers advantages over anthracyclines ● Intercalates DNA and inhibits topoisomerase II Voreloxin H3C HN ● Evades common drug resistance mechanisms – Not a P-glycoprotein substrate – Activity unaffected by p53, p63 or p73 status OH N N Primary refractory O OH H3C OH O O OH O 4 CR 7 CR, 1 CRp, 1 CRi Primary refractory nr (260 – nr) days First relapse 329 (175 – nr) days N = 33 48% 34% 60 years 2 (1-6) 216 (140, 307) days First relapse median OS 218 (131, 377) days Primary refractory median OS 209 (124, 307) days 85% Unf 21% N = 23 33% Early Mortality N % N = 13 19% 30-day all-cause mortality 2 of 69 3% 61 (35-73) 64% 60 years 60-day all-cause mortality 6 of 69 9% 7.3 (3.3 – 23.7) mos ECOG 0-1 89% Fav 3% Int 64% Unf 28% 2-hr IV Cytarabine N = 38 None or Consol. Only N (%) HSCT N (%) Other** N (%) Death N (days) Surviving N (days) Overall N = 68 Prim. Refr. N=7 0 7 (100%) 0 1 (307) 6 (222-611) 1st Relapse N = 13 4 (31%) 6 (46%) 3 (23%) 8 (74-530) 5 (299-515) Overall N = 20 20% 65% 15% 45% 55% 20% 11% 15% Febrile neutropenia 53% 34% 43% Sepsis/Bacteremia* 30% 24% 27% Infections* 10% 13% 12% Pneumonia* 17% 8% 12% Hypokalemia 27% 13% 19% Hypophosphatemia 13% 0% 6% *Includes multiple preferred terms 100 150 200 250 300 350 400 450 500 550 600 650 Time (Days) Primary Refractory Pref Censored First Relapse FRel Censored All All Censored Median LFS of 329 days (10.8 mos) CONCLUSIONS CR* mucositis* 50 ● 20 patients continue in survival follow-up, with 12 patients to date surviving one year or more POSTREMISSION THERAPY AND OUTCOME NONHEMATOLOGIC GRADE 3 OR HIGHER ADVERSE EVENTS 10% CIV Cytarabine N = 30 0 Median Overall Survival (95% CI) CR1 < 12 mos Cytogenetics (NCCN 2010) 0.00 CLINICAL ACTIVITY WITH LOW EARLY MORTALITY TRANSLATES TO FAVORABLE SURVIVAL OUTCOME CR1 12 – 24 mos Median age (range) 0.50 * Leukemia-free survival (LFS) is defined as time from complete remission (CR, CRp, or CRi) to relapse or death. **nr = not reached, 11 CR patients continue in follow-up. 57.5 (18.5-71) Int 58% Median overall survival of 216 days (7.1 mos) 0.75 329 (222 – nr**) days OH N = 69 Fav 3% KAPLAN-MEIER CURVES FOR OVERALL SURVIVAL AND LFS 1.00 0.25 Median Leukemia-Free Survival* (95% CI) CH3 O NH2 Median duration of CR1 (range) Upper GI 6 CR, 1 CRp First relapse (CR1 12 – 24 mos) O OH ECOG 0-1 Adverse Event 25% First relapse (CR1 < 12 mos) Anthracycline Core Median prior induction cycles (range) First Relapse 17 of 69 Doxorubicin Overall Cytogenetics (NCCN 2010) CR Rate N DEMOGRAPHICS AND BASELINE CHARACTERISTICS Median age (range) 29% CH3 ● Unlike anthracyclines, does not produce in vitro substantial reactive oxygen species implicated in cardiotoxicity Primary Refractory 20 of 69 N S O O O Quinolone Core COMPLETE REMISSIONS COUPLED WITH LONG-TERM LEUKEMIA-FREE SURVIVAL CR Rate (CR+CRp+CRi) Overall Survival ABSTRACT - UPDATED Background: Voreloxin, an anticancer quinolone derivative that inhibits topoisomerase II, is active in ovarian cancer and acute myeloid leukemia (AML). Nonclinical studies showed synergistic activity of voreloxin and cytarabine in vitro and in vivo (Scatena Cancer Chemother Pharmacol 2010). Methods: Phase 1b results were presented previously (Proc ASCO 2009). Phase 2 expansions studied voreloxin in combination with cytarabine in first relapsed or primary refractory AML. Dose regimens were 80 or 90 mg/m2 voreloxin administered by short IV infusion 10 minutes on days 1 and 4, in combination with either 400 mg/m2/d CIV cytarabine for 5 days or 2-hr IV infusion 1 g/m2/d cytarabine (IDAC) for 5 days. Patients could complete up to 4 cycles of therapy (2 induction and 2 consolidation). Response was determined by IWG criteria. Blood, urine, and bone marrow aspirate (BMA) were collected for PK or PD analysis. Results: Safety and activity were similar for both cytarabine schedules and thus phase 2 data were pooled for 69 patients. Thirty-three patients with primary refractory AML (defined as persistent AML after induction therapy or relapsed < 90 days after initial CR1) and 36 patients with first relapsed AML (defined as CR1 90 days to 24 months) were studied; most had a poor prognosis (81% primary refractory or first relapse with CR1 < 12 months). The overall median age was ~60 years; most patients were male, and 85% had an ECOG performance status of 0 or 1. Primary refractory patients had induction failure with a median 2 attempts (range, 1–6). First relapsed patients had a median duration of CR1 of 7.3 months. Nonhematologic grade 3 or higher adverse events ≥ 10% included upper GI mucositis 15%, febrile neutropenia 43%, sepsis/bacteremia 27%, infections 12%, pneumonia 12%, and hypokalemia 19%. All-cause mortality was low, 3% (2 of 69) at 30 days and 9% (6 of 69) at 60 days. CR+CRp+CRi (ORR) was 29% (20 of 69). The vast majority (17 of 20) were CR, for a CR rate of 25% (17 of 69). By study population, ORR for primary refractory was 21% (7 of 33; 6 CR, 1 CRp) and for first relapse was 36% (13 of 36). For first relapse, CR was achieved in 4 patients with CR1 < 12 months and 9 with CR1 ≥ 12 months (7 CR, 1 CRp, 1 CRi). Postremission, 13 of 20 patients went to transplant and 3 received maintenance therapy with azacitidine or decitabine. One with partial remission and one with treatment failure also went to transplant, for a total of 15 of 69 patients (22%). Median overall survival was 216 days or 7.1 months (95% CI 4.6–10.1 months) and was similar for both primary refractory and first relapse; median leukemia-free survival was 329 days or 10.8 months (95% CI 7.3 – not reached). Twenty of 69 patients remain in survival follow-up (range, 211-611 days), with 12 surviving a year or more thus far. PK/PD: voreloxin PK was dose proportional and unaffected by cytarabine. Voreloxin elimination is nonrenal, < 5% of voreloxin total dose was in urine. DNA damage response was seen in BMA consistent with voreloxin’s mechanism of action (ASH 2009) Conclusions: Activity of voreloxin in combination with cytarabine is promising in this difficult to treat patient population and was well-tolerated with a 29% ORR, median overall survival of 7.1 months, and low early mortality (3% at 30 days and 9% at 60 days). Twenty of 69 patients remain in survival follow-up, with 12 surviving a year or more thus far. The regimen allowed a bridge to bone marrow/stem cell transplant. Safety and activity profile in this population compares favorably with recent data for other AML therapies. A multinational, randomized, double-blind, placebo-controlled, pivotal phase 3 study of voreloxin or placebo in combination with IDAC in patients with relapsed or refractory AML (persistent AML after 1-2 cycles of therapy or relapsed < 90 days after initial CR1 or CR1 3-24 months) is planned. STUDY DESIGN Leukemia Free Survival or Overall Survival 1Cornell *Complete Remissions: 17 CR, 2 CRp, 1 CRi **3 patients received a hypomethylating agent as maintenance therapy; one additional patient received a hypomethylating agent while awaiting transplant. ● Majority of CR patients went to transplant http://www.sunesis.com/products-in-development/presentations_and_publications.php ● Voreloxin demonstrated encouraging clinical activity and tolerability in this study of patients with relapsed or refractory AML ● Voreloxin can be readily combined with CIV or 2-hour IV cytarabine regimens ● Favorable median overall survival of 7.1 months with 20 of 69 patients continuing in survival follow-up, reflecting 29% remission rate (CR + CRp + CRi) and 25% CR rate Leukemia-free survival (median 10.8 months) Low 30- & 60-day all-cause mortality of 3% and 9%, respectively ● The combination of voreloxin and cytarabine was successfully used as a “bridge to transplant” for relapsed/refractory patients in this study ● A multinational, randomized, double-blind, placebo-controlled, pivotal phase 3 study in relapsed or refractory AML is planned to initiate in 2H 2010 This poster and poster 6525, board # 17 (single agent voreloxin in frontline, poor-risk AML) will be discussed: RM E354a 5 – 6PM.