Newly Born
advertisement

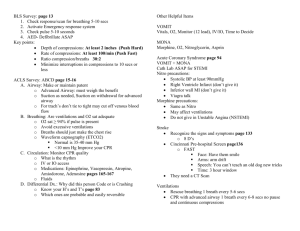
Newly Born History Signs and Symptoms · · · · · · · · · · · · Due date and gestational age Multiple gestation (twins etc.) Meconium Delivery difficulties Congenital disease Medications (maternal) Maternal risk factors substance abuse smoking Differential Term Gestation Breathing or Crying Good Muscle Tone Care of mother Appropriate Protocol · Respiratory distress Peripheral cyanosis or mottling (normal) Central cyanosis (abnormal) Altered level of responsiveness Bradycardia · · · · · · Airway failure Secretions Respiratory drive Infection Maternal medication effect Hypovolemia Hypoglycemia Congenital heart disease Hypothermia Provide warmth / Dry infant Clear airway if necessary YES Monitor and Reassess NO Warm, Dry and Stimulate Clear airway if necessary NO Heart Rate < 100 Agonal breathing or Apnea Labored breathing Persistent Cyanosis NO YES Airway Suctioning YES BVM Ventilations B Pulse Oximetry P Cardiac Monitor Meconium present: Non-vigorous newborns may undergo Direct Endotracheal I Suctioning Heart Rate < 100 Supplemental Oxygen Maintain SpO2 greater than or equal to 94 % NO YES Maintain warmth BVM Ventilations Monitor and Reassess NO Heart Rate < 60 YES Pediatric and OB Protocols Clear amniotic fluid: Suction only when obstruction is present and / or if BVM is needed. BVM Ventilations Chest Compressions Most newborns requiring resuscitation will respond to ventilations / BVM, compressions and / or epinephrine. If not responding consider hypovolemia, pneumothorax and / or hypoglycemia (< 40.) I IV / IO Procedure Pediatric Airway Protocols Heart Rate < 60 YES NO I Epinephrine 1:10,000 0.01 mg IV / IO Every 3 to 5 minutes as needed Normal Saline Bolus 10 mL / kg IV / IO Notify Destination or Contact Medical Control Protocol 39 Any local EMS System changes to this document must follow the NC OEMS Protocol Change Policy and be approved by OEMS 2012 Newly Born Approximately 10 % of newborns will require some assistance to begin breathing at birth. Less than 1 % will require extensive resuscitation. Initial Assessment: Initial assessment should include is this a Term Gestation, is the newborn Crying or Breathing and does the newborn have good Muscle Tone? If all three are present then general care should be utilized. Dry the baby and place skin-to-skin with mother and cover with dry linen to maintain temperature. If following the initial assessment you find the newborn is not Term, not Crying or Breathing and / or does not have good Muscle Tone then the initial steps to stabilize the newborn will include: 1. Warm, dry, stimulate and clear airway if necessary. 2. BVM ventilations / oxygen. 3. Chest Compressions. 4. Administration of Epinephrine or Normal Saline Bolus. The initial assessment should take about 60 seconds. Temperature Control: Important and becomes more important with low birth weight infants (<1500 g) and pre-term infants. For the low birth weight infant, in addition to warming, drying, wrapping in dry linens, placing skin-to-skin with mother and providing a warm ambient environment consider wrapping infant in saran type wrap. Oxygen Utilization: Oxygen saturations should be maintained at or above 94 %. Pulse oximetry may not be accurate initially. Pulse oximetry readings will be low during the first 10 minutes of life. The pulse ox device should be place on the right arm / hand. Initial readings will range from 60 – 75 % and by 5 to 10 minutes will rise to 85 – 95 %. Initial Breaths and Ventilations: Initial use of BVM may require up to 30 – 40 cmH2O pressure to establish a functional residual capacity. Use enough force to effect a chest rise only. Assist ventilations at a rate of 40 – 60 per minute to effect a heart rate > 100 beats per minute. Chest Compressions: Ensure correct BVM, oxygenation and airway measures are optimal most infants require adequate breathing and oxygenation to establish heart rate > 100. Compressions and ventilations should be coordinated to avoid simultaneous delivery. Compressions to ventilations should be 3:1. Pediatric and OB Protocols Assessment of heart rate: Should obtain by listening to the heart and feeling the umbilical pulse. Epinephrine: IV / IO is the preferred route of delivery. If access cannot be obtained then Epinephrine 1:10,000 0.1 mg / kg can be administered via the endotracheal tube. Hypoglycemia: Give 10 mL / kg (typically 35 mL) of D10 IV / IO if Blood Glucose Analysis is less than 40. Normal Saline Bolus: If pre-term infant given 10 mL / kg over 5 minutes. Rapid infusion may precipitate cerebral hemorrhage. Pearls · Recommended Exam: Mental Status, Skin, HEENT, Neck, Chest, Heart, Abdomen, Extremities, Neuro · CPR in infants is 120 compressions/minute with a 3:1 compression to ventilation ratio · It is extremely important to keep infant warm · Maternal sedation or narcotics will sedate infant (Naloxone NO LONGER recommended-supportive care only). · Consider hypoglycemia in infant. · Document 1 and 5 minute Apgars in PCR · D10 = D50 diluted (1 ml of D50 with 4 ml of Normal Saline) Protocol 39 Any local EMS System changes to this document must follow the NC OEMS Protocol Change Policy and be approved by OEMS 2012