Changes in Corneal Wavefront Aberrations with Aging
advertisement
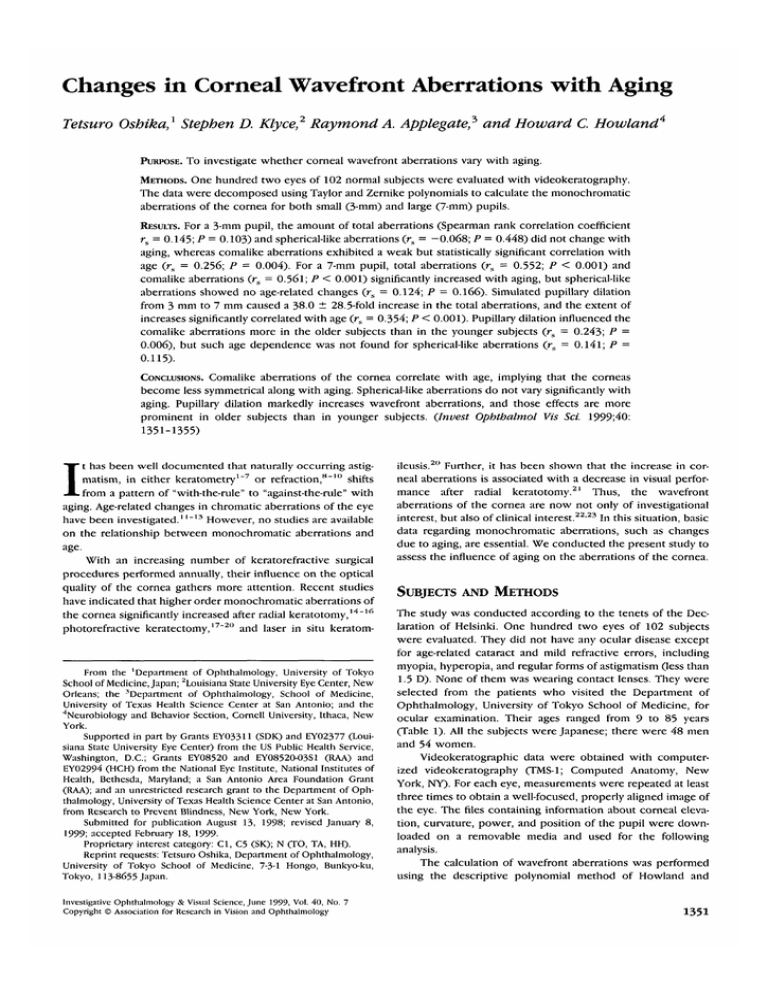
Changes in Corneal Wavefront Aberrations with Aging Tetsuro Oshika,1 Stephen D. Klyce,2 Raymond A. Applegate,5 and Howard C. Howland4 PURPOSE. TO investigate whether corneal wavefront aberrations vary with aging. METHODS. One hundred two eyes of 102 normal subjects were evaluated with videokeratography. The data were decomposed using Taylor and Zernike polynomials to calculate the monochromatic aberrations of the cornea for both small (3-mm) and large (7-mm) pupils. RESULTS. For a 3-mm pupil, the amount of total aberrations (Spearman rank correlation coefficient rs = 0.145; P = 0.103) and spherical-like aberrations (rs = -0.068; P = 0.448) did not change with aging, whereas comalike aberrations exhibited a weak but statistically significant correlation with age (rs = 0.256; P = 0.004). For a 7-mm pupil, total aberrations (rs = 0.552; P < 0.001) and comalike aberrations (rs = 0.561; P < 0.001) significantly increased with aging, but spherical-like aberrations showed no age-related changes (rs = 0.124; P = 0.166). Simulated pupillary dilation from 3 mm to 7 mm caused a 38.0 ± 28.5-fold increase in the total aberrations, and the extent of increases significantly correlated with age (rs = 0.354; P < 0.001). Pupillary dilation influenced the comalike aberrations more in the older subjects than in the younger subjects (rs = 0.243; P = 0.006), but such age dependence was not found for spherical-like aberrations (rs = 0.141; P = 0.115). Comalike aberrations of the cornea correlate with age, implying that the corneas become less symmetrical along with aging. Spherical-like aberrations do not vary significantly with aging. Pupillary dilation markedly increases wavefront aberrations, and those effects are more prominent in older subjects than in younger subjects. (Invest Ophthalmol Vis Sci. 1999;40: 1351-1355) CONCLUSIONS. I t has been well documented that naturally occurring astigmatism, in either keratometry1"7 or refraction,8"10 shifts from a pattern of "with-the-rule" to "against-the-rule" with aging. Age-related changes in chromatic aberrations of the eye have been investigated.1 '~13 However, no studies are available on the relationship between monochromatic aberrations and age. With an increasing number of keratorefractive surgical procedures performed annually, their influence on the optical quality of the cornea gathers more attention. Recent studies have indicated that higher order monochromatic aberrations of the cornea significantly increased after radial keratotomy,14-16 photorefractive keratectomy,17"20 and laser in situ keratom- From the 'Department of Ophthalmology, University of Tokyo School of Medicine, Japan; Louisiana State University Eye Center, New Orleans; the 'Department of Ophthalmology, School of Medicine, University of Texas Health Science Center at San Antonio; and the "'Neurobiology and Behavior Section, Cornell University, Ithaca, New York. Supported in part by Grants EYO3311 (SDK) and EY02377 (Louisiana State University Eye Center) from the US Public Health Service, Washington, D.C.; Grants EY08520 and EYO852O-O3S1 (RAA) and EY02994 (HCH) from the National Eye Institute, National Institutes of Health, Bethesda, Maryland; a San Antonio Area Foundation Grant (RAA); and an unrestricted research grant to the Department of Ophthalmology, University of Texas Health Science Center at San Antonio, from Research to Prevent Blindness, New York, New York. Submitted for publication August 13, 1998; revised January 8, 1999; accepted February 18, 1999Proprietary interest category: Cl, C5 (SK); N (TO, TA, HH). Reprint requests: Tetsuro Oshika, Department of Ophthalmology, University of Tokyo School of Medicine, 7-3-1 Hongo, Bunkyo-ku, Tokyo, 113-8655 Japan. Investigative Ophthalmology & Visual Science, June 1999, Vol. 40, No. 7 Copyright © Association for Research in Vision and Ophthalmology ileusis.20 Further, it has been shown that the increase in corneal aberrations is associated with a decrease in visual performance after radial keratotomy.21 Thus, the wavefront aberrations of the cornea are now not only of investigational interest, but also of clinical interest.22'23 In this situation, basic data regarding monochromatic aberrations, such as changes due to aging, are essential. We conducted the present study to assess the influence of aging on the aberrations of the cornea. SUBJECTS AND METHODS The study was conducted according to the tenets of the Declaration of Helsinki. One hundred two eyes of 102 subjects were evaluated. They did not have any ocular disease except for age-related cataract and mild refractive errors, including myopia, hyperopia, and regular forms of astigmatism (less than 1.5 D). None of them was wearing contact lenses. They were selected from the patients who visited the Department of Ophthalmology, University of Tokyo School of Medicine, for ocular examination. Their ages ranged from 9 to 85 years (Table 1). All the subjects were Japanese; there were 48 men and 54 women. Videokeratographic data were obtained with computerized videokeratography (TMS-1; Computed Anatomy, New York, NY). For each eye, measurements were repeated at least three times to obtain a well-focused, properly aligned image of the eye. The files containing information about corneal elevation, curvature, power, and position of the pupil were downloaded on a removable media and used for the following analysis. The calculation of wavefront aberrations was performed using the descriptive polynomial method of Howland and 1351 1352 Oshika et al. IOVS, June 1999, Vol. 40, No. 7 TABLE 1. Age Range and Refractive Status of Subjects Age <20 21-30 31-40 41-50 51-60 61-70 ^71 Total group Eyes 16 15 14 15 14 15 13 102 Spherical equivalent (D) -1.0 ± -0.8 ± -1.2 ± -1.4 ± -1.1 ± -0.7 ± -0.9 ± -1.1 ± 1.3 1.4 2.0 0.8 1.6 1.1 1.2 1.6 Astigmatism (D) 0.15 0.17 0.18 0.26 0.19 0.21 0.25 0.19 ±0.19 ± 0.24 ± 0.37 ± 0.26 ± 0.36 ± 0.44 ± 0.35 ± 0.37 Data are expressed as means ± SD. Howland.24 The center of the pupil was identified on the topography video screen, and its deviation from the videokeratographic axis was measured. Using the method of least squares, the reference sphere for each eye was calculated by determining the best-fit sphere to the elevation data over the 3-mm area centered on the pupil. The elevations of the best-fit sphere were subtracted from the measured elevations to define a surface termed the remainder lens. To calculate the optical effects of the remainder lens, the elevations of that lens were multiplied by 0.3375 (the keratometric index of refraction of the cornea minus the refractive index of air). Using the method of least squares, the resultant data were fit with the Taylor polynomial of the form24 ~26: W(x,y) = A + Bx + Cy + Dx2 + Exy + Fy2 + Gx5 + Hx2y + Ixy2 + Jy5 + Kx4 + Lx^y + Mx2y2 + Nxy* + Oy4 + Px5 + Qx4y + Rx5y2 + SxY + Txy4 + Uy5 + Vx6 (7) + Wx^y + Xx4y2 + Yx*y* + Zx2y4 + A&y5 + where (x(y) are Cartesian coordinates of the cornea in millimeters with their origin being taken on the pupil center. This is a two-dimensional, sixth-order Taylor representation of the wave-aberration surface with the positive axis pointing away from the retina. The coefficients were scaled so that the function W(x j/) was expressed in micrometers when x and y were expressed in millimeters. A represents a shift of the entire wavefront along the optical axis; B and C represent the vertical and horizontal prism components. D through E include the conventional ophthalmic prescription: sphere, cylinder, and axis. G through / express comalike aberration, and K through O express spherical-like aberration.24 P through U are the fifth-order Taylor coefficients, and V through A^ denote the sixth-order Taylor coefficients. The Taylor polynomial was then converted to the Zernike polynomial to obtain orthogonal coefficients.24'27 Zernike coefficients 7 through 28 (Z7 through Z28) were calculated from linear combinations of Taylor coefficients as described by Howland and Howland.23 Coefficients Z7 through Z10 correspond to comalike aberration, Z n through Z l 5 correspond to spherical-like aberration, Z, 6 through Z2, express the fifth-order Zernike coefficients, and Z22 through Z 28 are the sixth-order Zernike coefficients. These Zernike coefficients were then used to calculate the global descriptors of monochromatic corneal aberrations, which are represented by the terms, S3, S4, 55, and S6. Because spherical and coma aberrations refer to symmetrical systems and the eye is not rotationally symmetrical, the terms sphericallike and comalike aberrations are used in this article. The 5 3 (third-order component of the wavefront aberration) represents the mean squared wavefront variance from that of a perfect spherocylinder caused by comalike aberration. Similarly, S4 (fourth-order component of the wavefront aberration) represents the mean squared wavefront variance from that of a perfect spherocylinder caused by spherical-like aberration. 55 and S6 are the fifth- and sixth-order components of the wavefront aberrations, respectively. Because the variances of each term are independent, the total wavefront variance was computed by summing the individual variances and served as a parameter of total wavefront aberrations (Su). The odd-order aberrations (S3 + 55) were summed to examine the magnitude of comalike aberrations, and the even-order aberrations (54 + 56) were summed to evaluate the changes in spherical-like aberrations. These calculations were used for both 3-mm and 7-mm pupils.20 RESULTS For a 3-mm pupil, the amount of total aberrations (Su) did not change with aging (Spearman rank correlation coefficient rs — 0.145; P = 0.103; Fig. 1), whereas comalike aberrations (S3 + 55) exhibited a weak, but statistically significant correlation with age (rs = 0.256; P = 0.004; Fig. 2). Spherical-like aberrations (S4 + 5g) did not correlate with age (rs = -0.068; P = 0.448; Fig. 3). For a 7-mm pupil, total aberrations (rs = 0.552; P < 0.001; Fig. 4) and comalike aberrations (rs = 0.561; P < 0.001; Fig. 5) exhibited statistically significant positive correlations with age. Even when two extremely large values in Figures 4 and 5 were excluded from the analyses, the correlations remained statistically significant for total aberrations (rs = 0.533; P < 0.001) and comalike aberrations (rs = 0.543; P < 0.001). Sphericallike aberrations showed no age-related changes (rs = 0.124; P = 0.166; Fig. 6). Simulated pupillary dilation from 3 mm to 7 mm caused a 38.0 ± 28.5-fold increase (mean ± SD) in total aberrations, and 0.10 40 60 100 Age (years) FIGURE 1. Correlation between age and total wavefront aberrations (Su) for a 3-mm pupil (nonsignificant; Spearman rank correlation coefficient r s = 0.145; P = 0.103). Corneal Aberrations and Age IOVS, June 1999, Vol. 40, No. 7 0.04 • CO c .2 _ Q. IK (D co 0.02 • it V ^ • • • CO • • ' * . . -A 0.00 2 '"•• 40 •• o • *t • • 0 I 60 100 20 Age (years) N • • • • • —•— —*c • 40 • t • • • • • • > co 5 .2 CO • • If P o O • •B I 0.03 0.01 .j£ 1353 •• • • —•— • »• • • 1 • • # • • •• • • 60 80 100 Age (years) FIGURE 2. Statistically significant correlation between age and comalike aberrations (5 3 + 55) for a 3-mm pupil (Spearman rank correlation coefficient rs = 0.256; P = 0.004). FIGURE 4. Statistically significant correlation between age and total wavefront aberrations (Su) for a 7-mm pupil (Spearman rank correlation coefficient rs = 0.552; P < 0.001). the extent of increases by pupillary dilation showed statistically significant correlation with age (rs = 0.354; P < 0.001; Fig. 7). Similarly, pupillary dilation influenced the comalike aberrations more in the older subjects than in the younger subjects (rs = 0.243; P = 0.006; Fig. 8), but such age dependence was not found for spherical-like aberrations (rs = 0.141; P = 0.115; Fig. 9). did not show any age-related changes for both 3- and 7-mm pupils, implying that the central-to-peripheral balance of the corneal curvature is not significantly affected by increasing age. It should be noted that increases in the corneal comalike aberrations in the elderly do not directly indicate the deterioration of visual function in their eyes for several reasons. First, the pupils of older subjects tend to be more miotic,28'29 resulting in a smaller influence of the corneal wavefront aberrations on visual performance. Secondly, aberrations of the crystalline lens were not considered in the present study. In contrast to the spherical aberrations of the lens,30"32 little is known about the lenticular coma aberrations. It was anticipated that comalike aberrations introduced by corneal asymmetries are similar in magnitude to those measured for the eye as a whole, suggesting that these aberrations originate mainly in the cornea.33 However, proof of this hypothesis must wait until the relative contributions of cornea and crystalline lens are elucidated. Thirdly, the Stiles-Crawford effect34 was not considered in these calculations. However, the Stiles-Crawford effect is retinal in origin and does not alter the aberration or the change of aberration with age of the cornea or eye. Although it has DISCUSSION In our study population of 102 eyes, we found a weak but statistically significant correlation (rs = 0.256; P = 0.004) between age and comalike aberrations for a 3-mm pupil. For a 7-mm pupil, comalike aberrations exhibited significant positive correlations with age (rs = 0.561; P < 0.001). Although we may not be able to apply the current results to subjects of all races and refractive status, it is suggested that comalike aberrations of the cornea tend to show age-related changes. Because comalike aberrations consist of tilt and/or asymmetry, these results imply that the corneas become less symmetric along with aging. On the contrary, spherical-like aberrations 0.04 . + CO o ? E 0.03 pil erf Q. CO E E ch 0.02 m * • • CO CO 0.01 t Sphe o 0.00 • i * 20 40 60 • • 'v • : :ft: 80 o 100 Age (years) FIGURE 3. Correlation between age and spherical-like aberrations (54 + 56) for a 3-mm pupil (nonsignificant; Spearman rank correlation coefficient r s = -0.068; P = 0.448). 40 60 80 100 Age (years) FIGURE 5. Statistically significant correlation between age and comalike aberrations (5 3 + 55) for a 7-mm pupil (Spearman rank correlation coefficient r s = 0.561; P < 0.001). 1354 Oshika et al. IOVS, June 1999, Vol. 40, No. 7 • 0.8 w 0.6 re o. re 0 | 0.4 = « u. • • • • • 0.2 Q. 0.0 in 20 •'*.: 40 .'# 60 80 40 100 80 60 100 Age (years) Age (years) FIGURE 6. Statistically significant correlation between age and spherical-like aberrations (SA + 56) for a 7-mrn pupil (Spearman rank correlation coefficient rs = 0.124; P - 0.166). been claimed that the Stiles-Crawford effect reduces the impact of optical aberrations on vision, a recent analysis showed that the effect on vision is very small.35 Simulated pupillary dilation from 3 mm to 7 mm markedly increased the total aberrations and comalike aberrations; those influences were significantly larger in the older subjects than in the younger subjects (Figs. 7, 8). The data, especially in those with a 7-mm pupil, may have been influenced by the limitations of the Placido-based videokeratography in accurately capturing data from the peripheral cornea, although the obvious increases (38.0-fold increases) associated with pupillary dilation seemed to be sufficiently meaningful. These results have clinical relevance in situations in which pupillary abnormalities are encountered as a consequence of complications of intraocular surgery, such as atonic,36"38 eccentric,39'40 and overly stretched pupils.41'42 It has been known that when the pupil is made eccentric, spherical aberrations cause coma,43 which adds to the preexisting comalike aberrations. Even under normal concessions, the pupillary size increases with dim illumination in all age groups.44 Applegate et al.21 have reported that FIGURE 8. Statistically significant correlation between age and the magnitude of increases in comalike aberrations (5 3 + 5 5 ) induced by simulated pupillary dilation from 3 mm to 7 mm (Spearman rank correlation coefficient rs = 0.243; P = 0.006). a 1-log-unit change in wavefront variance induces a 0.23 change in the area under the log contrast-sensitivity function. They also reported that a 1-log-unit change in wavefront variance induces a 0.22 logarithmic minimum angle of resolution (logMAR) loss in high-contrast Bailey-Lovie visual acuity (2+ line) and a 0.32 logMAR loss in low-contrast Bailey-Lovie visual acuity (3+ line) for a 7-mm pupil.45 With this in mind, it is interesting that contrast sensitivity has been reported to be stable through the fifth decade,46'47 followed by a monotonic decrease from the sixth decade on.''5 In the present study, we found little, if any, systemic changes in the aberration through the fifth decade, with most large aberration values occurring after the age of 60 (Fig. 4). Although this armchair analysis is intriguing and worth noting in passing, it is likely that other factors such as lens scattering may play a significant role in the loss of visual function in the over-60 group. We offer the current results as a reference for future studies on the monochromatic aberrations of the cornea and their contribution to the total aberrations of the eye. 300 150 • •S re rr £ 0 CI z 200 n • • re ir • •="§• Q.^" 100 • re cc 40 60 100 Age (years) FIGURE 7. Statistically significant correlation between age and the magnitude of increases in total wavefront aberrations (Su) induced by simulated pupillary dilation from 3 mm to 7 mm (Spearman rank correlation coefficient r s = 0.354; P < 0.001). • • • • • 20 • • • s. —-•— 40 • •• •• 60 • e 80 100 Age (years) FIGURE 9. Statistically significant correlation between age and the magnitude of increases in spherical-like aberrations (5 4 + 56) induced by simulated pupillary dilation from 3 mm to 7 mm (Spearman rank correlation coefficient rs = 0.141; P = 0.115). IOVS, June 1999, Vol. 40, No. 7 References 1. Leighton DA, Tomlinson A. Changes in axial length and other dimensions of the eyeball with increasing age. Ada Ophthalmol. 1972;50:815-826. 2. Baldwin WR, Mills D. A longitudinal study of corneal astigmatism and total astigmatism. AmJOptomPhysiolOpt. 1981;58:206-211. 3. Kame RT, Jue TS, Shigekuni DM. A longitudinal study of corneal astigmatism changes in Asian eyes. J Am Optom Assoc. 1993;64: 215-219. 4. Goh WSH, Lam CSY. Changes in refractive trends and optical components of Hong Kong Chinese aged 19-39 years. Ophthalmic Physiol Opt. 1994;l4:378-382. 5. Lam CSY, Goh WSH, Tang YK, Tsui KK, Wong WC, Man TC. Changes in refractive trends and optical components of Hong Kong Chinese aged over 40 years. Ophthalmic Physiol Opt. 1994; 14:383-388. 6. Hayashi K, Hayashi H, Hayashi F. Topographic analysis of the changes in corneal shape due to aging. Cornea. 1995;l4:527-532. 7. Ninn-Pedersen K. Relationships between preoperative astigmatism and corneal optical power, axial length, intraocular pressure, gender, and patient age./Refract Surg. 1996;12:472-482. 8. Sanders H. Age-dependence of human refractive errors. Ophthalmic Physiol Opt. 1981;1:159-174. 9- Fledelius HC. Prevalences of astigmatism and anisometropia in adult Danes. Ada Ophthalmol. 1984;62:391-400. 10. Saunders H. Changes in the orientation of the axis of astigmatism associated with age. Ophthalmic Physiol Opt. 1984;6:343-344. 11. Millodot M, Newton LA. A possible change of refractive index with age and its relevance of chromatic aberration. Graefes Arch Klin Exp Ophthalmol. 1976;201:159-l67. 12. Ware C. Human axial chromatic aberration found not to decline with age. Graefes Arch Klin Exp Ophthalmol. 1982;218:39-41. 13. Mordi JA, Adrian WK. Influence of age on chromatic aberration of the human eye. AmJ Optom Physiol Opt. 1985;62:864-869. 14. Hemenger RP, Tomlinson A, Caroline PJ. Role of spherical aberration in contrast sensitivity loss with radial keratotomy. Invest Ophthalmol Vis Sci. 1989:30:1997-2001. 15. Applegate RA, Howland HC, Buettner J, Cottingham AJ Jr, Sharp PP, Yee RW. Changes in the aberration structure of the RK cornea from videokeratographic measurements [ARVO Abstract]. Invest Ophthalmol Vis Sci. 1994;35(4):S1740. Abstract nr 2253. 16. Applegate RA, Hilmantel G, Howland HC. Corneal aberrations increase with the magnitude of radial keratotomy refractive correction. Optom Vis Sci. 1996;73:585-589. 17. Seiler T, Reckmann W, Maloney RK. Effective spherical aberration of the cornea as a quantitative descriptor in corneal topography. / Cataract Refract Surg. 1993;19:155-l65. 18. Oliver KM, Hemenger RP, Corbett MC, et al. Corneal optical aberrations induced by photorefractive keratectomy. / Refract Surg. 1997;13:246-254. 19. Martinez CE, Applegate RA, Klyce SD, McDonald MB, Medina JP, Howland HC. Effect of pupil dilation on corneal optical aberrations after photorefractive keratectomy. Arch Ophthalmol. 1998; 116: 1053-1062. 20. Oshika T, Klyce SD, Applegate RA, Howland HC, El Danasoury MA. Comparison of corneal wavefront aberrations after photorefractive keratectomy and laser in situ keratomileusis. AmJ Ophthalmol. 1999; 127:1-7. 21. Applegate RA, Howland HC, Sharp RP, Cottingham AJ, Yee RW. Corneal aberrations, visual performance and refractive surgery. / Refract Surg. 1998;l4:397-407. 22. Charman WN. Wavefront aberration of the eye: a review. Optom Vis Sci. 1991:68:574-583. 23. Applegate RA, Howland HC. Refractive surgery, optical aberrations, and visual performance. / Refract Surg. 1997;13:295-299. Corneal Aberrations and Age 1355 24. Howland HC, Howland B. A subjective method for the measurement of monochromatic aberrations of the eye. / Opt Soc Am. 1977:67:1508-1518. 25. Walsh G, Charman WN. Measurement of the axial wavefront aberration of the human eye. Ophthalmic Physiol Opt. 1985;5:2331. 26. Howland HC, Beuttner J. Computing high order wave aberration coefficient from variations of best focus for small artificial pupils. Vision Res. 1989;29:979-983. 27. Malacara D, DeVore SL. Interferogram evaluation and wavefront fitting. In: Malacara D, ed. Optical Shop Testing. 2nd ed. New York: John Wiley & Sons; 1992:455-49928. Eriksson AW, Fellman J, Nieminen H, Forsius H. Influence of age on the position and size of the iris frill and the pupil. Ada Ophthalmol. 1965;43:629-64l. 29. Buckley C, Curtin DM, Docherty J, Eustace P. Ageing and alpha 1 adrenoreceptors in the iris. Eye. 1987;1:211-216. 30. El Hage S, Berny F. Contribution of the crystalline lens to the spherical aberration of the eye. / Opt Soc Am. 1973;63:205-211. 31. Millodot M, Sivak JG. Contribution of the cornea and lens to the spherical aberration of the eye. Vision Res. 1979:19:685-687. 32. Sivak JG, Kreuzer RO. Spherical aberration of the crystalline lens. Vision Res. 1983;23:59-70. 33. Hemenger RP, Tomlinson A, Oliver K. Optical consequences of asymmetries in normal corneas. Ophthalmic Physiol Opt. 1996; 16:124-129. 34. Stiles WS, Crawford BH. The luminous efficiency of rays entering the eye pupil at different points. Proc R Soc Loncl IS. 1933; 112: 428-450. 35. Atchison, DA, Joblin, A, Smith, G. Influence of Stiles-Crawford effect apodization on spatial visual performance./ Opt Soc Am A. 1998;15:2545-2551. 36. Lam S, Beck RW, Hall D, Creighton JB. Atonic pupil after cataract surgery. Ophthalmology. 1989:96:589-590. 37. Saiz A, Angulo S, Fernandez M. Atonic pupil: an unusual complication of cataract surgery. Ophthalmic Surg. 1991;22:20-22. 38. Golnik KC, Hund PW III, Apple DJ. Atonic pupil after cataract surgery. / Cataract Refract Surg. 1995;21:170-175. 39- Apple DJ, Mamalis N, Loftfield K, et al. Complications of intraocular lenses. A historical and histopathological review. Surv Ophthalmol. 1984;29:l-54. 40. Oshika T. Transscleral suture fixation of subluxated posterior chamber lens within the capsular bag. / Cataract Refract Surg. 1997;23:1421-1424. 41. Masket S. Avoiding complications associated with iris retractor use in small pupil cataract extraction. / Cataract Refract Surg. 1996; 22:168-171. 42. Yuguchi T, Oshika T, Sawaguchi S, Kaiya T. Pupillary functions after cataract surgery using flexible iris retractor in patients with small pupil. Jpn J Ophthalmol. 1999;43:20-24. 43- Meeteren AV, Dunnewold CJW. Image quality of the human eye for eccentric entrance pupils. Vision Res. 1983:23:573-579. 44. Koch DD, Samuelson SW, Haft EA, Merin LM. Pupillary size and responsiveness: implications for selection of a bifocal intraocular lens. Ophthalmology. 1991:98:1030-1035. 45. Applegate RA, Hilmantel G, Ballantine CS, Tu EY, Starck T, Zayac EJ. Corneal first surface optical aberrations from various causes are significantly correlated to high and low contrast acuity. Optom Vision Sci. 1998;75(suppl):69. 46. Harrison JM, Applegate RA, YatesJT, Ballentine C. Contrast sensitivity and disability glare in the middle years. / Opt Soc Am A. 1993:10:1849-1855. 47. Owsley C, Sekuler R, Siemsen D. Contrast sensitivity throughout adulthood. Vision Res. 1983;23:689-699.