pro1-results of alternative definitions for statin refill

RESULTS OF ALTERNATIVE DEFINITIONS FOR STATIN REFILL COMPLIANCE,
PERSISTENCE AND GAPS IN A RETROSPECTIVE DATABASE ANALYSIS
617 242 4332 Fax:617 8009
INTRODUCTION
This study compares different calculations of prescription refill compliance and persistence in a sample of statin users from a prescription claims database and shows how systematic adjustment for gaps and surpluses can improve precision.
Objectives
• To show the consequences of different calculation methods.
• To examine statin compliance from different measurement perspectives.
METHODS
Overview
• Standard calculations of compliance and persistence often do not account for surplus resulting from overlapping prescription refills (Rx) or from the last refills in an observation period.
• Calculations which assume patients eventually consume surplus medications from overlapping prescriptions and which appropriately allocate surplus from the last refills give more accurate estimates.
• We show the size and direction of differences with calculations based on a sample of statin users drawn from the Protocare health care claims database.
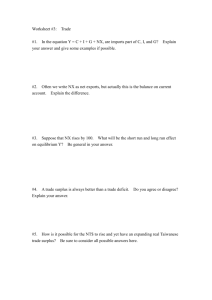
Figure 1: Compliance, Persistence, & Gaps: Surplus-Adjusted vs. Unadjusted Measures
Hypothetical Prescription History
30
Prescriptions
30 30 30
30
90
Prescription Gaps
Medication
Possession
240
30
Days 0 180 360
Study Period 1 Study Period 2
Total Days’
Supply
Overlap
Surplus
240 30
Final Surplus
(Study Period 1)
60
Compliance (MPR) ,
Study Period 1
Simple
MPR
“Adjusted”
MPR
133% 100%
Persistence (Days)
Simple Adjusted
120 240
Gaps (Days)
Simple Adjusted
30 0
Data Source
The Protocare database consists of medical claims and demographic information from a large (approximately 1.2 million patients annually) managed care organization. (Access to the dataset was provided by Pfizer, Inc.) Our analysis is based on claims data between January 1, 1996 and December 31, 2002.
Sample
Statin users were defined as patients 18 years of age or older with one or more pharmacy claims containing any NDC code for a statin. Analyses were based on patients continuously enrolled (no drop-out from the health plan greater than 30 days) for at least one year before their first statin Rx, and at least 2.5 years afterwards. Continuously enrolled patients were observed for a maximum of six years. The resulting sample of 45,482 patients was 53% female and had an average age of 64 years.
Analysis
The database contained age measured from the date of the patient’s first statin claim, sex, Rx dates and days supply for each Rx. We wrote syntax to model medication following the “simple” and “adjusted” assumptions described below. All analyses were done with SPSS version 12.0.1.
For prevalence and incidence of statin use, effects of different discontinuance thresholds, removal of drop-outs and statistics across six years, please see our detailed results at www.Kochevarresearch.com/ComplianceReportDetails.
Variable Definitions
•
ISPOR Medication Compliance and Persistence Special Interest Group (1) definitions:
Medication Compliance (synonym: Adherence) is the extent to which a patient acts in accordance with the prescribed interval and dose of and dosing regime.
The unit of measurement for compliance is administered doses per defined period of time, reported as a proportion (%) of prescribed does (D) taken as the prescribed time interval (T) as measured by the period of time, i.e., % of TD, measured by percentage.
•
•
Medication Persistence is the accumulation of time from initiation to discontinuation of therapy. Measured by time metric.
Measurement of medication compliance and persistence from prescription (Rx) refill claims requires additional definitions:
Supply . Day’s supply of medication in a prescription refill.
•
•
•
•
•
•
Observation period . The defined period of time (e.g. 1 year) over which prescription refill claims are observed.
Gap . The period of time between prescriptions when a patient does not have any observable supply of medication
Discontinuance . The point in time at which a patient stops refilling prescriptions. Typically identified by a minimum gap duration (e.g. >30 days).
Drop-outs . Patients who fill only one Rx, and have no subsequent refills, during an observation period.
Overlap Surplus . Accumulated surplus doses of medication due to prescription refills that overlap in time.
Final Surplus . Excess supply (from prior overlaps or last refills) remaining at the end of an observation period that could not have been consumed in the observation period.
Calculation: Compliance
There is wide variation in methods for calculating compliance, which is typically reported as a medical possession ratio (MPR). Some common calculations (2, 3):
A. MPR = [Total Days Supply] / [Observation Period]
B. MPR = ( [Observation Period] - [Total Gap Duration] ) / [Observation Period]
C. MPR = ([Medication Supply] – [Surplus]) / [Observation Period]
Calculation problems . Methods that do not account for surplus supply (A, B) may overestimate MPR, as surplus is added to the total supply even if it was not available during prescription gaps. Methods that remove all surplus medication from the MPR calculation (C) may discount surplus that could have been consumed during prescription gaps.
We based MPR on the usable medication supply in each observation period.
Usable medication supply includes overlap surplus the total days’ supply.
, but subtracts final surplus from
• Overlap surplus . Surplus medication that could potentially be consumed during prescription gaps in an observation period was included in the total days supply.
We assumed patients took medications as recommended and consumed accumulated surplus going forward in time only.
• Final surplus . When the remaining medication supply exceeded the days left in an observation period, the excess supply was considered final surplus and was subtracted from the total days’ supply. When observing multiple study periods, this final surplus was allocated to the following study period.
(Note: To simplify calculations we are assuming one dose per day. The correction factor for medications requiring multiple doses is (1/ [dose/day).
Calculation: Persistence
Persistence is the duration between the medication initiation date and the date at which the patient discontinues. Discontinuation is typically calculated based on a minimum defined gap between prescription refills, (e.g. 30 days).
• Calculation problems . Patients may consume surplus medication during supply gaps, reducing the gap length. Methods which do not account for surplus may erroneously classify some patients as having discontinued. Surplus can accumulate from before the beginning of the observation period or from overlaps.
• Definition problems . Discontinuation implies the end of use. Over a longer period, patients may fill another Rx after a defined discontinuation date, and might be more accurately defined as “intermittent” rather than “discontinued”.
We systematically accounted for surplus, examined the effects of different definitions of discontinuation and removal of “drop-outs”.
• Surplus before initiation date. Our sample consisted of first-time statin users.
There was no supply of statin before the first observed Rx.
• Overlap and final surplus.
Gaps between end of supply and next Rx were adjusted for accumulated surplus from overlapping Rx. Final surplus at the end of one observation period was carried over into the next.
• Definition of Discontinuation . We defined discontinuation as gaps without supply of 30, 60, and 90 days. Patients in each year-long observation period were followed for an additional six months to determine whether they were still without a refill.
• “Drop-outs” . A significant proportion of patients fill only one prescription ever.
We defined drop-outs as those who had only one statin Rx in the first 2.5 years.
We calculated scores with and without drop-outs.
Calculation: Gaps
Gaps between prescriptions are typically calculated as the duration between the end of the previous Rx supply and the date of the next Rx.
• Calculation problems . Methods that ignore medication surplus may overestimate actual gap duration. Methods that subtract all surplus ignore time order, and may discount surplus that could have been consumed during prescription gaps.
We accounted for surplus and time order.
• Overlap and final surplus . Surplus from overlaps was subtracted from gaps going forward in time only. Final surplus at the end of one observation period was carried over into the next.
RESULTS
Approximately 7% of patients had prescriptions with more than 30 days supply.
Prescriptions for 90 days were a major source of surplus.
Approximately half the sample had prescription overlaps and final/year-end surplus (Table 1).
N
N Rx Overlaps
0
1-3
4+
Rx Overlap Surplus (Days)
Mean (S.D.)
Rx Final Surplus at Year-End (Days)
Any
Mean (S.D.)
Table 1: Overlap and Final Surplus
11
Year 1
45,582 (100%)
21
9.2 (16.4)
8.4 (12.1)
40%
40
48%
Year 2
45,582 (100%)
17
30
13.9 (32.7)
7.5 (12.0)
42%
52%
“Adjusted” MPR scores were lower for approximately half the sample, and a significant proportion were lower by 21 days or more (Table 2).
Table 2: Simple vs. Surplus-Adjusted MPR
11
N
MPR
Mean (S.D.)
> 0.80
> 1.00
Patients with Lower
Adjusted MPR Score
Lower by >1 Day
Lower by >21 Days
Year 1
45,582 (100%)
Simple
0.62 (0.36)
42%
13%
Adjusted
0.59 (0.33)
38%
0%
25%
49%
Year 2
45,582 (100%)
Simple
0.47 (0.41)
33%
5%
Adjusted
0.47 (0.39)
33%
0%
21%
59%
Adjusting persistence for time-ordered surplus reduced gap length and led to longer persistence scores on average (Table 3).
Persistence scores were different for a relatively small proportion patients.
Table 3: Simple vs. Surplus-Adjusted Persistence (Discontinuance = 30+ Day Gap)
11
N
Persistence (Days)
Mean (S.D.)
Patients with Greater
Adjusted Persistence
Longer by >1 Day
Longer by >21 Days
45,582 (100%)
Simple
Year 1
207.0 (137.2)
6%
Adjusted
214.7 (138.0)
17%
Year 2
45,582 (100%)
Simple
97.3 (151.5)
Adjusted
110.6 (158.6)
10%
6%
In the first year about half (48%) of the sample had a lower average gap duration using the adjusted method (Table 4).
Eleven percent had an average duration that was lower by 21 days or more.
Table 4: Simple vs. Surplus-Adjusted Prescription Gaps
11
N
Number of Gaps
Mean (S.D.)
Simple
4.2 (2.6)
Year 1
45,582 (100%)
Adjusted
3.5 (2.4)
Year 2
45,582 (100%)
Simple
3.7 (3.0)
Adjusted
3.1 (2.6)
Avg. Gap Duration
Mean (S.D.) 48.7 (84.2)
Patients with Lower
Adjusted Avg. Gap Duration
Lower by >1 Day
Lower by >21 Days 11%
49.4 (85.0)
58%
55.0 (103.7)
12%
55.7 (104.6)
49%
An MPR of 0.80 or greater is often regarded as a “standard” of good compliance.
However, a score of 0.80 in a year is 73 days without supply.
One-third of high-compliance patients had gaps of 21 days or more without supply (Table 5).
Table 5: Prescription Gaps Among Patients with Adjusted MPR >0.8
11
Year 1
17,324 (38%) N
Gap Duration
Any Gap of 1 – 6 Days
Any Gap of 7 Days or More
Any Gap of 14 Days or More
Any Gap of 21 Days or More
32%
46%
72%
97%
DISCUSSION
Adjusting calculations for surplus led to lower MPR, higher persistence and shorter gap length scores. Differences between unadjusted and adjusted average scores were small but more than half the sample had lower MPR and gap scores; nearly one-quarter of the sample had 21 or more days without supply that were not apparent in the unadjusted calculations.
Accounting for surplus more precisely maps patient behavior if we assume they systematically consume surplus when they run out of refill supply. However, the statistics reported here all had high variance and it is impossible to grasp a patient’s behavior with any one measure. Individual patient reports with adjusted MPR, persistence and a chart showing patterns of gaps are necessary if physicians wish to track patient medication use.
Regardless of calculation method a majority of patients did not have effective statin supply on hand, were not persistent and had large gaps between refills.
Limitations
•
•
•
Adjusted refill compliance, persistence and gap scores may not mirror actual medication use if patients hoard medication or consume excess doses.
There are sound logical reasons for adjusting compliance, persistence and gap scores for surplus supply but it remains to be seen if adjusted scores show stronger relationships with medication efficacy or other outcomes.
Statin use in the Protocare sample may not be representative of statin compliance behavior in other health plans.
CONCLUSIONS
While Rx refill records are generally regarded as an accurate measure of overall compliance (4), some calculation methods are more accurate than others.
• MPR unadjusted for time order misclassifies some patients by assuming they have consumed unavailable supply during gaps in coverage.
• Unadjusted persistence does not account for surplus and will underestimate duration of medication use for some patients.
• Unadjusted gap length scores overestimate gaps in use. Patterns of gaps provide more information about compliance than gap length scores.
• Statin use in the Protocare sample was intermittent for most patients and unlikely to achieve positive clinical outcomes.
REFERENCES
• www.ispor.org/sigs/MCP_accomplishments.asp#definition. Accessed 5/10/06
• Sikka R, Xia F, Aubert R. Estimating medication persistency using administrative claims data. Am J Manag Care . 2005;11:449-457.
• Steiner JF, Prochazka, AV. The assessment of refill compliance using pharmacy records: Methods, validity and applications.
1997;50:105-116.
J Clin Epidemiol .
• Osterberg L, Blaschke T. Adherence to medication. N Engl J Med
487-497.
. 2005; 353:
ISPOR 11 th Annual International Meeting
May, 2006. Philadelphia PA