as a PDF
advertisement

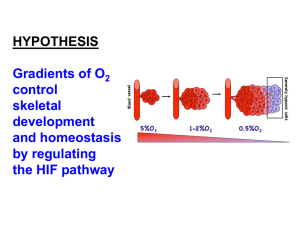
Articles in PresS. Am J Physiol Lung Cell Mol Physiol (May 7, 2004). 10.1152/ajplung.00203.2003 Greater vascularity, lowered HIF-1/DNA binding and elevated GSH as markers of adaptation to in vivo chronic hypoxia. 1 Tissot van Patot, M.C., 1Bendrick-Peart, J., 1Beckey, V.E., 1Serkova, N., 2Zwerdlinger, L. 1 University of Colorado Health Sciences Center, Dept. of Anesthesiology, Denver, Colorado, 80262, 2St. Vincent’s General Hospital, Leadville, Colorado, 80461. Corresponding Author Information Martha C. Tissot van Patot Dept. Anesthesiology, B-113 University of Colorado Health Sciences Center 4200 E. 9th Avenue Denver, CO 80262 Phone: 303 315-1869 Fax: 303 315-1899 email: martha.tissotvanpatot@uchsc.edu Running Head: Adaptation to Chronic Hypoxia Copyright © 2004 by the American Physiological Society. Abstract Vascularity is increased in placentae from high as compared to low altitude pregnancies. An angiogenic response to hypoxia may protect an organ from further hypoxic insult by increasing blood flow and oxygen delivery to the tissue. We hypothesized that increased placental vascularity is sufficient to adapt to high altitude. Therefore, indices of hypoxic stress would not be present in placentae from successful high altitude pregnancies. Methods: Full-thickness placental biopsies were A) collected and frozen in liquid nitrogen within 5 minutes of placental delivery and B) fixed in formalin for stereologic analyses, at high (3100 m, n = 10) and low (1600 m, n = 10) altitude. HIF-1 activity was analyzed by enzyme-linked immunoabsorbance assay (ELISA). Western blot analyses were used to evaluate HIF-1!, HIF-1", HIF-2!, von Hippel-Lindau protein (pvHL), VEGF, Flt-1, enolase, and GAPDH. Magnetic resonance spectroscopy (MRS) was used to evaluate endogenous metabolism. Results: The ratio of placental capillary surface density to villous surface density was 70% greater at high as compared to low altitude. HIF-1 activity and HIF-1 associated proteins were unchanged in placentae from high vs. low altitude pregnancies. Placental expression of HIF-1-mediated proteins VEGF, Flt-1, enolase, and GAPDH were unchanged at high vs. low altitude. Succinate, GSH, phosphomonoesters and ADP were elevated in placenta from high as compared to low altitude. Conclusion: Placentae from uncomplicated high altitude pregnancies have greater vascularity and no indication of significant hypoxic stress at term as compared to placentae from low altitude. Key Words: GSH, succinate, HIF-1-DNA binding, placenta, stereology 2 Introduction Previously, we and others have reported increased vascularity in placentae that have developed during healthy pregnancies at high as compared to low altitude (3, 17, 30). A hypoxia-induced increase in vascularity is believed to assist in ‘rescuing’ the tissue from hypoxia by increasing blood and thereby oxygen delivery to the area. Hypoxia can activate hypoxia-inducible transcription factor (HIF-1) (6, 7). HIF-1 enhances transcription of genes encoding hypoxia-sensitive proteins that are instrumental in protecting the tissue from hypoxia, such as; erythropoietin, which increases the oxygen carrying capacity of the blood, vascular endothelial growth factor (VEGF) and its receptor Flt-1, which stimulate angiogenesis, and glycolytic proteins such as glyceraldehydes 3-phosphate dehydrogenase (GAPDH) and enolase, which increase energy production through anaerobic glycolysis (8, 16, 25, 31). If the response to hypoxia is successful, for example vascularity (oxygen delivery) is increased sufficiently to protect the tissue from hypoxia, the principle of negative feedback dictates that HIF-1 activity, expression of hypoxia-sensitive proteins, oxidative stress and increased glycolysis should be attenuated. Because placental vascularity is established in early pregnancy, a hypoxia or altitude-induced increase in vascularity probably occurs in early pregnancy as well (1). Therefore, establishing an increase in oxygen delivery early in gestation should protect the placentae from hypoxia so that term placentae of successful high altitude pregnancies should not be associated with markers of hypoxic stress. 3 Thus, we hypothesized that greater vascularity in placentae from uncomplicated pregnancies at high altitude would not be associated with markers of hypoxic metabolic stress including enhanced HIF-DNA binding, expression of HIF-related and hypoxiasensitive proteins and metabolic hypoxic markers. Our approach was to examine placentae from high- and low-altitude pregnancies in order to determine vascular responses including; capillary and villous surface densities, HIF-DNA binding activity, the presence of proteins associated with HIF-1 activation, including HIF-1!, HIF-2!, HIF-1", and pvHL, and the expression of HIF-mediated proteins, VEGF, Flt-1. We also determined metabolic stress markers including; GAPDH, enolase and metabolic adaptation at each altitude. This strategy was designed to determine whether enhanced placental vascularity in hypoxic placentae is associated with indicators of hypoxic stress. This study is important because hypoxia is implicated in the pathogenesis of many pregnancy complications including preeclampsia, intra-uterine growth restriction and anemia, and poses a serious threat to the health of both fetus and mother (14). Fetal growth and development are impaired in the presence of hypoxia. However, successful pregnancy at high altitude represents successful adaptation to hypoxia. Therefore, determining the mechanisms of successful adaptation to chronic hypoxia during pregnancy and markers of adaptation failure may be a critical first step in determining successful therapeutic intervention in hypoxia-mediated diseases of pregnancy. Materials and Methods Study Design. Approval from the Colorado Multiple Institutional Review Board 4 (COMIRB) at the University of Colorado Health Sciences Center was obtained to collect term placentae from uncomplicated, singleton gestational women at University Hospital in Denver, Colorado (1600 m). Permission was also obtained from St. Vincent’s Hospital in Leadville, Colorado (3100 m). Ten subjects at low altitude and ten subjects at high altitude were consented according to COMIRB guidelines and placentae were collected immediately following placental delivery. Subjects were between the ages of 18-34 and gestational age was 39-41 weeks. Two g of tissue (full thickness of the placentae, including basal and chorionic plates) were collected from random locations and placed in liquid nitrogen within 5 minutes of placental delivery, to stop the metabolic activity. Previous data from our lab (26) indicates that placental samples must be placed into liquid nitrogen within 9 minutes of placental delivery to avoid introducing artifact by hypoxic/ischemic induction of glycolysis. The placenta was then dissected into 5 sections from which 2 blocks extending from basal plate to chorionic plate were dissected, placed into 10% formalin for 4 days and then paraffin embedded at less than 58oC for stereologic analyses. Immunhistochemistry. Placental sections were stained to label endothelium using a polyclonal mouse anti-human CD34+ antibody (1:20; BioGenex, Napa, CA, USA), followed by an ABC reagent (ABC, Vectastain Elite, Vector Labs, Burlingame, CA, USA) labeled with peroxidase for which 3’ 3’-diaminobenzidine (Sigma, St. Louis, MO) was used as a substrate. Negative controls were performed using mouse IgG in place of primary antibody. 5 Stereologic Analysis. Stereology was performed as previously reported (30). Briefly, 4 slides from 4 sections (4 !m) of each placenta, and 16 fields per slide were evaluated. A 25-box microscope grid (25 X 25 !m) was used under 40X magnification; box size was chosen to minimize the number of capillaries per box. The guidelines of a 125 !m2 (25 !m2 per box) grid were applied and capillary surface density of capillary luminal margins (Vvcap) was calculated by 2*total capillary intersects/ number of points on villous tissue * total test line length (= 2D, where D = distance between points on grid (25 !m)) (3). The capillary (and villous) intersects were calculated by counting the villous tissue each time it crossed a horizontal line within the square lattice parameters specified (3). Villous surface density (Svvill) was calculated in a similar manner, using the villous intersects as the numerator. A ratio of Svcap/Svvill is reported. Western blot. For immunoblot assays, 30 µg total protein/lane or 50 µg nuclear protein/lane were fractionated by electrophoresis using a NUPAGETM 4-12% bis-tris gradient gel (Invitrogen, Carlsbad, CA). The proteins were then transferred to a methanol-soaked polyvinylidene difluouride (PVDF) membrane using the semidry immunoblot method (Owl Model HEP-1 Panther Semi-Dry Electroblotter – Nunc, Rochester, NY). The membranes were immunoblotted using either HIF-1!, HIF-1", HIF2!, (Nuclear proteins, Novus Biologicals, Littleton. Colorado: NB100-105, 100-124, 100-132), pvHL, VEGF or Flt-1 (Santa Cruz Biotechnology, Santa Cruz, CA, Fl-181, C1, H-225), secondary antibodies conjugated with horseradish peroxidase (IgG-HRP) were used for detection and visualization by Pierce-SuperSignalRcircle West Dura Extended Duration Substrate (Pierce Biotechnology, Inc., Rockford, IL). Images were visualized 6 using the UVP BioChemi Imaging System and relative quantification by densitometry was performed using LabWorks 4.0 software (UVP, Inc., Upland, CA). !-actin (Sigma, St. Louis, MO, A-5441) was used as an internal control for protein loading and data are expressed as a ratio of the protein of interest to !-actin. Enzyme-linked immunoabsorbance assay (ELISA). An ELISA was used kit to assess HIF1 activity on all samples in a single experiment (BD Biosciences, Clontech, Palo Alto, CA, K2077-1). Briefly, nuclear extract (20 !g) was added to a 96-well plate coated with the DNA consensus binding sequence for HIF-1. Bound HIF-1 was detected by the addition of mouse monoclonal primary antibody to HIF-1", followed by horseradish peroxidase-conjugated secondary antibody. A microtiter plate reader (ThermoLab Systems, Helsinki, Finland, Multiskan Ascent) was used to measure the enzymatic product. A HIF-1 wild-type competitor oligonucleotide control was used to demonstrate DNA-HIF-1 binding specificity. Samples were run in duplicate and CV values were less than 10%. Dual Perchloric Acid (PCA) lipid extraction of placental tissues. To perform high-resolution magnetic resonance spectroscopy (MRS) on placental tissues, we extracted the frozen placental samples using a dual perchloric acid (PCA)/lipid extraction procedure developed in our laboratory (27). Snap frozen tissues were powdered in a mortar grinder in the presence of liquid nitrogen. The powdered frozen tissue was added to 6 ml of ice-cold 12% PCA and subsequently homogenized using electrical homogenizer Poly Tron PT 2100 (Kinematica AG, Luzern, Switzerland). The PCA homogenates were put into an ice-cold ultrasound bath for 5 min. Then, the 7 homogenates were centrifuged at 3000 x g and 4oC for 20 min. The aqueous phase was collected, and the pellet was re-suspended with 2 ml of ice-cold PCA. The resuspended homogenates were put in an ultrasound bath and centrifuged again in the same conditions. The aqueous phase was added to the previously collected supernatant. The supernatants, containing placental water-soluble metabolites, were then neutralized with KOH, centrifuged for 20 min at 3000 x g and 4oC to remove potassium perchlorate, and lyophilized overnight for PCA extracts. The tissue pellets, remaining after the first centrifugations, were re-dissolved in 4 ml ice-cold water. The re-dissolved pellets, containing placental lipids, were neutralized with KOH and lyophilized overnight for lipid extracts. The lyophilized PCA extracts, containing water-soluble metabolites, were reconstituted in 0.45 ml deuterium oxide (D2O, Cambridge Isotope Laboratories Inc., Andover, MA). The lyophilized lipid extracts were reconstituted in 1.5 ml of deuterated chloroform/methanol mixture (CDCl3/CD3OD, 2 : 1 vol/vol). After centrifugation, the supernatants were analyzed by MRS. Magnetic Resonance Spectroscopy (MRS) on PCA and lipid extracts. To calculate the absolute concentrations of water-soluble and lipid metabolites, one dimensional MRS experiments were carried out using a 500 MHz Bruker NMR spectrometer with an Avance console (Bruker, Karlsruhe, Germany). A dual QNP 5-mm Bruker probe head was used for all experiments. For proton MRS, the operating frequency was 500 MHz, and a standard pre-saturation pulse program was used for water suppression. The other parameters were: 40 accumulations; 90o pulse angle; 0 dB power level; 7.35 !s pulse width; 10 ppm spectral width; 12.85 s repetition time. Trimethylsilyl 8 propionic-2,2,3,3,-d4 acid (TMSP, 0.6 mmol/l for PCA extracts and 1.2 mmol/l for lipid extract) was used as an external standard for the quantification of metabolites based on 1 H-MRS signals. 1H chemical shifts were referenced to TSP at 0 ppm. Before the 31P - MRS experiments were recorded, 100 mmol/l EDTA was added to each PCA extract for complexation of divalent ions. This resulted in 31P peaks with significant narrow line width (especially important for ATP signals). The pH was adjusted again to 7. The following NMR parameters with a composite pulse decoupling (CPD) program were used: 202.1 MHz operating 31P frequency; 800 accumulations; 90o pulse angle; 12 dB power level for 31P channel; 9 !s pulse width; 35 ppm spectral width; 2.0 s repetition time. The absolute concentration of glycerophosphocholine (GPC), calculated from 1HMRS of the same extract, was used as an internal standard for quantification of phosphorus metabolites in 31P -MR spectra. The chemical shifts of !-ATP at -10 ppm were used as shift references. All MRS data were processed using the 1D WINNMR programme (Bruker, Karlsruhe, Germany). 9 Statistical Analyses. Stereology, densitometry and ELISA data were analyzed using a Student t-Test. MRS data were analyzed by ANOVA. Scheffe’s Post-hoc test to was used to determine differences between variables. Significance for all statistical analyses was accepted at p ! 0.05. Data are presented as representative immunoblots indicating subject number in each lane and accompanied by densitometry analysis of immunoblots for the entire study group (n = 10 per altitude). Results The characteristics of the subjects at1600 and 3100 M were similar with respect to maternal age, gestational age of delivery, birth weight, placental weight, placental volume and the ratio of placental weight to birth weight (Table 1). Placental stereologic analyses indicated that the ratio of capillary surface density (Svcap) to villous surface density (Svvill) was greater in high- vs. low-altitude pregnancies (low altitude 5.65, high altitude 9.52, p = 0.03) (30) (Figure 1D). In order to determine if greater vascularity protected the placentae from the hypoxic stress of high altitude, we determined hypoxia-inducible transcription factor-1 (HIF-1)/DNA binding activity in placentae collected at high and low altitude. ELISA results indicated that HIF-1/DNA binding was 1.455 ng/ml (± 0.182) at low and 0.476 ng/ml (± 0.347) at high altitude, 3 fold less at high altitude (Figure 2) (p = 0.0001). Because HIF-1 activity is primarily determined by the presence of the activated HIF-1! subunit in the nucleus, we determined the presence of nuclear HIF-1! by Western blot analyses. Nuclear HIF-1! was equivalent in placentae from low (n = 10) and high (n = 10 10) altitude pregnancies, as determined by densitometric analyses (Figure 3). To further investigate reasons for less HIF-1 activity at high altitude, we determined nuclear HIF1!, to which HIF-1" must bind in order to create active HIF-1. Nuclear HIF-1! was greater in placentae from high- (n = 10) as compared to low- (n = 10) altitude pregnancies, as determined by densitometric analyses (Figure 4). However, individual densitometry data indicated that placenta #3 expressed 2-3 fold more HIF-1! than other placentae (Figure 4). When data were compared without placenta #3 there was no significant difference in HIF-1! expression between low- and high-altitude placentae. The von Hippel-Lindau protein (pvHL) binds to HIF-1" during normoxia, targeting HIF1" for ubiquitination and proteosomal degradation. In the presence of normoxia, as suggested by unaltered HIF-1" at high altitude, there should be no difference in pvHL at high as compared to low altitude. In Western blot analysis of total placental protein extracts from 10 low- and 10 high-altitude pregnancies, there were, as expected, no differences in pvHL expression (Figure 5). Thus, less HIF-1 activity in placentae from high- vs. low-altitude pregnancies was not associated with any change in the presence of HIF-1" or –1! subunits or expression of pvHL. In some tissues, HIF-2 is activated under less severe hypoxic conditions than HIF-1 and may be responsible for increased transcription of hypoxia-sensitive genes (32). To determine if placental tissue at high altitude was responding to hypoxia via HIF-2 rather than HIF-1, we analyzed placentae from 10 low- and 10 high-altitude pregnancies for nuclear HIF-2" by Western blot analyses (Figure 6). HIF-2" was not different between 11 placental nuclear extracts from low and high altitude pregnancies, although there was a trend toward greater expression at high altitude, which may prove significant in a larger sample of placentae. To further test whether placentae at high altitude are experiencing hypoxic stress expression of hypoxia-sensitive angiogenic and glycolytic proteins was analyzed. Expression of VEGF, a hypoxia-sensitive angiogenic protein, was not altered in placentae from high (n = 10) as compared to low (n = 10) altitude as determined by Western blot and densitometric analysis (Figure 7). Because a hypoxia-stimulated increase in the VEGF receptor, Flt-1, could increase the biological activity of VEGF, further Western blot analyses for Flt-1 expression in 10 lowand 10 high- altitude placentae were performed and densitometric analysis indicated that expression did not differ between placentae from high- vs. low-altitude pregnancies (Figure 7). Due to the fact that cellular response to hypoxia initiates an increase in expression of glycolytic enzymes and hence glycolysis, we determined the expression of glycolytic enzymes enolase and GAPDH placentae from low (n = 10) and high (n = 10) altitude pregnancies by Western blot and subsequent densitometric analyses. There was no change in the expression of placental enolase and GAPDH between low and high altitude pregnancies (Figure 8). 12 Because there was no evidence of HIF-1 activation or glycolytic stress, we sought to determine if there were metabolic markers for hypoxia at high as compared to low altitude, utilizing magnetic resonance spectroscopy (MRS). 1H and 31P- MRS analysis indicated that metabolites succinate, glutathione-SH (GSH), phosphomonoesters (PME) and ADP were increased in placentae collected at high altitude (Table 2). Thus the ratio of PME to phosphodiesters (PDE) was also increased; however the ATP/ADP ratio did not change, since ATP also showed a tendency to increase. No significant increase in lactate, a marker for anaerobic glycolysis, was seen. There were no changes in polyunsaturated fatty acid (PUFA) concentrations in lipid spectra of high vs. low altitude placentae, indicating no increase in lipid peroxidation (Table 3). Discussion In the present study, the main finding was that placentae from successful pregnancies exposed to hypoxia through out gestation had greater placental vascularity and no evidence of severe hypoxic stress. Placental HIF-1/DNA binding activity was actually lower at altitude and there was no increase in the expression of hypoxia-sensitive proteins. Interestingly, the reduction in HIF-1 activity was not associated with changes in pvHL, nuclear HIF-1!, HIF-1", nor was HIF-2! increased in the nucleus. In regard to metabolism, succinate was elevated as is often found during hypoxia, however GSH was also elevated. Furthermore, there was no evidence of lipid peroxidation or glycolytic activity. The reduction in HIF-1 activity was not caused by introducing hypoxia during placental collection, as all placental samples were minced and collected into liquid nitrogen within 13 5 minutes of vaginal delivery and stored at –80o C until nuclear proteins were extracted for analyses. Further, MRS analysis did not indicate acute hypoxic insult in any of the tissues since no increase in lactate nor decrease in the ATP/ADP ratio or glucose was seen. Each Western blot was performed a minimum of 3 times, and each ELISA sample was analyzed in triplicate (coefficient of variance less than 10%), producing consistent results each time. The number of subjects within each group (n = 10 low-, n = 10 highaltitude placentae) was sufficient to achieve 98% power, showing less HIF-1 activity at high altitude. The investigators are aware that Denver is not sea level. Low-altitude placentae in this study were collected at 1600 m, where the partial pressure of inspired oxygen (PiO2) is 122 mmHg as compared to 149 mmHg at sea level. Although, the change in PiO2 at 1600 m is not enough to cause altitude-induced illness (13), there may be metabolic, enzymatic or protein changes in tissue without associated clinical complications. Therefore, future studies examining sea level placental tissue in comparison to those at 1600 and 3100 m are planned. Because these placentae were collected following labor and delivery, it is possible that changes in HIF-1 activity occurred as a result of labor and delivery and did not reflect in vivo values prior to labor. Ideally, placentae from Cesarean sections should be used to most closely assess in vivo values. This was a potential problem for our collections in Leadville, Colorado, as all pre-planned Cesarean sections are performed in one of several low-altitude facilities, making Cesarean section material impractical for collection in our study design. However, in a large number of placentae from high altitude pregnancies all had less HIF-1 activity suggesting that the results are reliable. 14 Because HIF-1 is important in promoting transcription of VEGF, Flt-1, GAPDH and enolase and HIF-1 activity was not greater at high as compared to low altitude, it is not surprising that there was no increase in the expression of hypoxia-sensitive proteins. Although VEGF and Flt-1 are important for promoting vasculogenesis (2, 15, 21), it is not surprising that there was no increased expression in the highly vascular placentae. Placental vascular development occurs primarily during the first and early second trimesters and is most likely no longer taking place at term. Furthermore, failure to increase expression of glycolytic enzymes GAPDH and enolase at high altitude was supported by MRS data indicating no change in glucose, lactate or ATP in high altitude placentae. Although, with the glycolytic enzymes, protein expression may not change whereas the activity of the enzyme might; changes in molecules such as ADP suggest this may be the case. Metabolic profiles of our high altitude placental tissue did not reveal changes which are characteristic for acute short term hypoxia (Table 3) (4, 22, 28, 29). This suggests that placentae from high altitude uncomplicated pregnancies are not exposed to hypoxic conditions (possibly due to increased vascularity), but rather showed metabolic adaptation to increased oxygen delivery. Phosphomonoestsers, precursors for membrane phospholipids, were increased, indicating increased membrane synthesis, in accordance with the data indicating greater capillary development in high altitude placentae. ADP was elevated, but the ATP/ADP ratio indicating energy state was unchanged. ATP may be converted to ADP more quickly to provide energy for enhanced membrane synthesis. 15 Previous studies on hypoxic tissue indicate that succinate is increased during hypoxia, while GSH is reduced (4, 18, 28). During hypoxia, complex II in the mitochondrial respiratory chain appears to switch from succinate dehydrogenase to fumerate reductase, resulting in an accumulation of succinate (18). Because succinate is produced in the mitochondrial respiratory chain, succinate concentrations are dependent on tissue PO2 (18). Glutathione-SH (GSH) is reduced during hypoxia by conversion to glutathione-S-Sglutatione (GSSG) and is more dependent on oxygen content than PO2 (4). Previous studies in which succinate was greater and GSH lower during hypoxia were designed such that PO2 and oxygen content were reduced. In contrast, in the current study placentae from high altitude pregnancies most likely experienced lowered PO2 as a result of hypobaric hypoxia, but greater oxygen content as a result of greater vascularity. Therefore, we propose that the greater succinate concentration was due to the lower PO2 and the greater GSH concentration was due to greater oxygen content. Also, the equal concentrations of PUFA in low and high altitude placentae indicated no evidence of increased LPO (30), related to hypoxia. Because GSH has been reported to reduce HIF-1 activity when exogenously administered to hypoxic tissue (10, 11), greater GSH concentrations may have inhibited the activity of HIF-1 in our high- as compared to low-altitude placentae. Our findings regarding HIF activity do not dispute what others have found; that the placentae can increase HIF activity when hypoxic and have greater HIF-1! early rather than late in pregnancy (5, 9, 23, 24). Canniggia et al. (5) reported that in normal, low-altitude pregnancies placental 16 HIF was elevated in early gestation (prior to 10 weeks) during the most severe placental hypoxia, but decreased as the placenta invaded the uterus and was exposed to maternal circulation. The altitude-induced increase in placental vascularity probably occurred during the same early gestation time period; however, that could not be determined at this time as sampling of early pregnancy placentae was not possible in our study. Data from the literature report HIF consistently elevated during hypoxia in pathologic conditions (25). Similarly, our current study reports no increase in HIF activity in placentae from women who successfully completed pregnancy at high altitude. Therefore, we consider that lack of HIF activity in placentae collected at high altitude does not represent a pathologic condition but is rather a surrogate marker for successful adaptation to high altitude. Our data suggesting that reduced HIF-1 activity represents adaptation to high altitude are supported by a report from Hochachka and Rupert (12), in which Andean natives had lower erythropoietin synthesis in response to hypoxia than lowlanders, however the genetic sequences encoding erythropoietin and HIF-1! were unchanged in the native population. Hochachka and Rupert hypothesized that their results suggested ‘that the altered erthropoietic response in Andean natives reflects adaptations in hypoxia sensing, rather than hypoxia response, mechanisms’ (12). For example, failure to attain normal pregnancy at high altitude most often results in preeclampsia, at rates 3-4 times those of low-altitude pregnancies (19) and HIF is elevated 1.5 – 2.5 fold in placentae from preeclamptic pregnancies at low altitude (24). Preeclampsia is characterized by greatly elevated blood pressure, poor placental 17 development and impaired placental blood flow (20). In contrast, the current study indicates greater placental vascular development and less HIF activity in placentae from normal pregnancies at high altitude. Long-term hypoxia is a complication of many diseases including pregnancy-related disorders, pulmonary and cardiovascular diseases. Determining the mechanisms by which tissues successfully adapt to chronic hypoxia is crucial for survival of tissues challenged by chronic hypoxia. Our data suggest that greater GSH concentration and less HIF activity may be implicated in the mechanism of successful adaptation to chronic hypoxia. However, our study design did not allow for establishing cause-effect relationships. It remains to be evaluated, if the observed changes are evidence of adaptation or markers for a yet unidentified mechanism. Acknowledgments The authors would like to thank Dr. John Reeves and Dr. Uwe Christians for their invaluable mentorship and assistance in preparing this manuscript. We would also like to acknowledge the invaluable assistance of the nursing staff on the labor and delivery wards of University Hospital, Denver and St. Vincent’s General Hospital, Leadville, Colorado without whom this study would not have been feasible. Also, we would like to thank St. Vincent’s General Hospital for providing excellent facilities and a supportive collaborative environment in which to work. References 1. Benirschke K and Kaufmann P. Pathology of the Human Placenta. New York: Springer-Verlag, 1995. 2. Brekken RA and Thorpe PE. Vascular endothelial growth factor and vascular targeting of solid tumors. Anticancer Research 21: 4221-4229, 2001. 18 3. Burton GJ, Reshetnikova OS, Milovanov AP, and Teleshova OV. Stereological evaluation of vascular adaptations in human placental villi to differing forms of hypoxic stress. Placenta 17: 49-55, 1996. 4. Caceda R, Gamboa JL, Boero JA, Monge CC, and Arregui A. Energetic metabolism in mouse cerebral cortex during chronic hypoxia. Neuroscience Letters 301: 171-174, 2001. 5. Caniggia I, Mostachfi H, Winter J, Gassmann M, Lye SJ, Kuliszewski M, and Post M. Hypoxia-inducible factor-1 mediates the biological effects of oxygen on human trophoblast differentiation through TGFbeta(3). Journal of Clinical Investigation 105: 577-587, 2000. 6. Chandel NS, McClintock DS, and Feliciano CE. Reactive oxygen species generated at mitochondrial complex III stabilize hypoxia-inducible factor-1alpha during hypoxia: a mechanism of O2 sensing. Journal of Biological Chemistry 275: 2513025138, 2000. 7. Ehleben W, Bolling B, Merten E, Porwol T, Strohmaier AR, and Acker H. Cytochromes and oxygen radicals as putative members of the oxygen sensing pathway. Respiration Physiology 114: 25-36, 1998. 8. Forsythe JA, Jiang BH, Iyer NV, Agani F, Leung SW, Koos RD, and Semenze GL. Activation of vascular endothelial growth factor gene transcription by hypoxia -inducible factor 1. Molecular and Cell Biology 16: 4604-4613, 1996. 9. Genbacev O, Krtolica A, Kaelin W, and Fisher SJ. Human cytotrophoblast expression of the von Hippel-Lindau protein is downregulated during uterine invasion in situ and upregulated by hypoxia in vitro. Developmental Biology 233: 526-536, 2001. 10. Haddad JJ and Land SC. O(2)-evoked regulation of HIF-1alpha and NFkappaB in perinatal lung epithelium requires glutathione biosynthesis. Am J Physiol Lung Cell Mol Physiol 278: L492-503, 2000. 11. Haddad JJ, Olver RE, and Land SC. Antioxidant/pro-oxidant equilibrium regulates HIF-1alpha and NF-kappa B redox sensitivity. Evidence for inhibition by glutathione oxidation in alveolar epithelial cells. Journal of Biological Chemistry 275: 21130-21139, 2000. 12. Hochachka PW and Rupert JL. Fine tuning the HIF-1 'global' O2 sensor for hypobaric hypoxia in Andean high-altitude natives. Bioessays 25: 515-519, 2003. 13. Hultgren HN. High Altitude Medicine. Stanford, CA: Hultgren Publications, 1997. 14. Kingdom JCP and Kaufmann P. Oxygen and placental villous development: Origins of fetal hypoxia. Placenta 18: 613-621, 1997. 15. Kumazaki K, Nakayama M, Suehara N, and Wada Y. Expression of vascular endothelial growth factor, placental growth factor, and their receptors Flt-1 and KDR in human placenta under pathologic conditions. Human Pathology 33: 1069-1077, 2002. 16. Lu S, Gu X, Hoestje S, and Epner DE. Identification of an additional hypoxia responsive element in the glyceraldehyde-3-phosphate dehydrogenase gene promoter. Biochimica et Biophysica Acta 1574: 152-156, 2002. 17. Mayhew TM. Changes in fetal capillaries during preplacental hypoxia: Growth, shape remodelling and villous capillarization in placentae from high-altitude pregnancies. Placenta 24: 191-198, 2003. 19 18. Paddenberg R, Goldenberg A, Faulhammer P, Braun-Dullaeus RC, and Kummer W. Mitochondrial complex II is essential for hypoxia-induced ROS generation and vasoconstriction in the pulmonary vasculature. 163-169, 2003. 19. Palmer SK, Moore LG, Young DZ, Cregger B, Berman JC, and Zamudio S. Increased preeclampsia and altered blood pressure course during normal pregnancy at high (3100 m) altitude in Colorado. American Journal of Obstetrics and Gynecology 18O: 1161-1168, 1999. 20. Pridjian G and Puschett JB. Preeclampsia. Part 1: clinical and pathophysiologic considerations. Obstetrical & Gynecological Survey 57: 598-618, 2002. 21. Pufe T, Petersen W, Tillmann B, and Mentlein R. The angiogenic peptide vascular endothelial growth factor is expressed in foetal and ruptured tendons. Virchows Archiv 439: 579-585, 2001. 22. Punkt K, Welt K, and Schaffranietz L. Changes of enzyme activities in the rat myocardium caused by experimental hypoxia with and without ginkgo biloba extract EGb 761 pretreatment. A cytophotometrical study. Acta Histochemica 97: 67-79, 1995. 23. Rajakumar RA and Conrad KP. Expression, ontogeny and regulation of hypoxia inducible transcription factors in the human placenta. Journal of the society for Gynecologic Investigation 7: 184A, 2000. 24. Rajakumar RA, Whitelock KA, Weissfeld LA, Daftary AR, Markovic N, and Conrad KP. Selective overexpression of the hypoxia-inducible transcription factor, HIF2!, in placentas from women with preeclampsia. Biology of Reproduction: 499-506, 2001. 25. Semenza GL. HIF-1: mediator of physiological and pathophysiological responses to hypoxia. Journal of Applied Physiology 88: 1474-1480, 2000. 26. Serkova N, Bendrick-Peart J, Alexander B, and Tissot van Patot MC. Metabolite concentrations in human placentae and their changes due to the collection time after delivery. Placenta 24: 227-235, 2003. 27. Serkova N, Jacobsen W, Niemann CU, Litt L, Benet LZ, Leibfritz D, and Christians U. Sirolimus, but not the structurally related RAD (everolimus), enhances the negative effects of cyclosporine on mitochondrial metabolism in the rat brain. British Journal of Pharmacology 133: 875-885, 2001. 28. Singh SN, Vats P, Kumria MM, Ranganathan S, Shyam R, Arora MP, Jain CL, and Sridharan K. Effect of high altitude (7,620 m) exposure on glutathione and related metabolism in rats. European Journal of Applied Physiology 84(3): 233-237, 2001. 29. Sumbayev VV, Budde A, Zhou J, and Brune B. HIF-1 alpha protein as a target for S-nitrosation. FEBS Letters 535: 106-112, 2003. 30. Tissot van Patot MC, Grilli A, Chapman P, Broad E, Tyson W, Heller DS, Zwerdlinger L, and Zamudio S. Remodelling of Uteroplacental Arteries is Decreased in High Altitude Placentae. Placenta 24: 326-335, 2003. 31. Wenger RH. Cellular adaptation to hypoxia: O2-sensing protein hydroxylases, hypoxia-inducible transcription factors, and O2-regulated gene expression. FASEB 16: 1151-1162, 2002. 32. Wiesener MS, Jurgensen JS, Rosenberger C, Scholze CK, Horstrup JH, Warnecke C, Mandriota S, Bechmann I, Frei UA, Pugh CW, Ratcliffe PJ, Bachmann S, Maxwell PH, and Eckardt KU. Widespread hypoxia-inducible 20 expression of HIF-2alpha in distinct cell populations of different organs. FASEB Journal 17: 271-273, 2003. 21 Table 1. Subject Characteristics Maternal Age (yrs) Gestational Age (days) Birth Weight (g) Placental Weight (g) Placental Volume (ml) Placental Wt/Birth Wt 1600 M 24.89 (2.2) 274.8 (4.42) 3246.1 (192.38) 633.62 (58.1) 526.5 (27.25) 0.2 (0.027) 3100 M 25.5 (2.1) 275.17 (2.28) 3192.1 (108.84) 550 (31.7) 455 (37.12) 0.17 (0.013) 22 Table 2. Metabolites Val,Leu,Ile Lactate Alanine Acetate Glutamate *Succinate Glutamine *GSH Aspartate PCr/ Cr PC/GPC Taurine myo-Inositol Glucose Glycogen *PME PDE *PME/PDE ATP *ADP ATP/ADP NAD UDPG Low Altitude High Altitude p Value 0.754 (0.052) 3.838 (0.418) 0.503 (0.019) 0.141 (0.046) 1.205 (0.046) 0.888 (0.068) 4.728 (0.523) 0.518 (0.056) 0.054 (0.009) 1.308 (0.17) 0.178 0.243 0.828 0.076 0.617 0.140 (0.016) 0.643 (0.08) 0.218 (0.02) 0.508 (0.053) 0.023 0.188 0.215 (0.019) 0.513 (0.079) 0.401 (0.036) 0.585 (0.029) 2.769 (0.25) 0.926 (0.066) 1.47 (0.047) 0.366 (0.252) 0.762 (0.089) 0.418 (0.036) 0.456 (067) 0.798 (0.206) 2.264 (0.420) 0.774 (0.09) 1.364 (0.163) 0.014 (0.014) 0.001 0.276 0.528 0.397 0.368 0.236 0.592 0.157 2.342 (0.193) 2.378 (0.08) 4.366 (0.404) 2.758 (.405) 0.004 0.441 0.985 (0.075) 0.757 (0.029) 1.65 (0.145) 0.986 (0.139) 0.007 0.195 0.318 (0.016) 2.394 (0.117) 0.691 (0.056) 0.18 (0.038) 0.526 (0.048) 1.9 (0.245) 0.72 (0.90) 0.254 (0.086) 0.008 0.139 0.805 0.491 *Significantly different in high as compared to low altitude pregnancies (p ! 0.05). Bold: classic markers for short-term hypoxia, which did not change in this study. 23 Table 3. Lipids PUFA TAG Total FA Cholesterol Low Altitude High Altitude p-Value 23.282 (3.589) 27.193 (1.478) 6.155 (0.917) 6.924 (0.591) 27.466 (4.264) 31.639 (1.041) 3.594 (0.567) 4.154 (0.273) 24 0.4326 0.5120 0.3969 0.3896 Figure Legends. Figure 1. Placental tissues from low- (1600 M) and high (3100 M) -altitude placentae were fixed in 10% buffered formalin, paraffin embedded and immunohistochemically studied using anti-CD34+ antibody and haematoxylin background stain, 200X. A. Low altitude placenta negative, using mouse IgG in place of primary antibody. B. Low altitude placenta (serial section from 1A). C. High altitude placenta. D. Ratio of capillary density to villous surface density in placentae from pregnancies at low- (n = 10) and high (n = 10) altitude. C - capillaries, V- villi, *p = 0.038 Figure 2. Nuclear protein was extracted from low (1600 M) and high (3100 M) altitude placentae and analyzed for HIF-1-DNA binding using an ELISA transcription factor activity assay (n = 10 low altitude and n = 10 high altitude subjects). *p < 0.0001. Data presented as mean ± the standard error of the mean. Figure 3. Nuclear proteins, extracted from low (1600 M) and high (3100 M) altitude placentae, were analyzed for HIF-1! and "-actin using Western blot analysis (Top). Data are expressed as the ratio of relative densitometry units of the protein of interest to "actin for total protein (mean ± the standard error of the mean) (Bottom). Figure 4. Nuclear protein, extracted from placentae from low- (1600 M) and high- (3100 M) altitude pregnancies were analyzed for HIF-1" and "-actin using Western blot analysis (Top). Data are expressed as the ratio of relative densitometry units of the protein of interest to "-actin for total protein (Bottom). The graph on the left depicts 25 individual data to demonstrate the variability of HIF-1! between subjects, while the graph on the right depicts the mean ± the standard error of the mean at each altitude with and without #3 at high altitude. *p = 0.033 greater than low altitude. Figure 5. Total protein, extracted from low (1600 M) and high (3100 M) altitude placentae, was analyzed for vHL and !-actin using Western blot analysis (Top). Data are expressed as the ratio of relative densitometry units of the protein of interest to !-actin for total protein (mean ± the standard error of the mean) (Bottom). Figure 6. Nuclear protein, extracted from placentae from low- (1600 M) and high- (3100 M) altitude pregnancies were analyzed for HIF-2" and !-actin using Western blot analysis (Top). Data are expressed as the ratio of relative densitometry units of the protein of interest to !-actin for total protein (mean ± the standard error of the mean) (Bottom). Figure 7. Total protein, extracted from low (1600 M) and high (3100 M) altitude placentae, was analyzed for VEGF, Flt-1 and !-actin using Western blot analysis (Top). Data are expressed as the ratio of relative densitometry units of the protein of interest to !-actin for total protein (mean ± the standard error of the mean) (Bottom). Figure 8. Total protein, extracted from low (1600 M) and high (3100 M) altitude placentae, was analyzed for GAPDH, enolase and !-actin using Western blot analysis (Top). Data are expressed as the ratio of relative densitometry units of the protein of interest to !-actin for total protein (mean ± the standard error of the mean) (Bottom). 26 27 V 12 * 10 A V EC Svvcap/Svvill (cm3) EC 8 6 4 2 0 B 1600 M V EC C D. Figure 1. 3100 M 1.8 1.6 HIF Binding (ng /ml) (ng/ml) 1.4 1.2 1 * 0.8 0.6 0.4 0.2 0 1600 M Figure 2. 3100 M HIF-1!/"-actin 0.5 0.4 0.3 0.2 0.1 0 1600 m Figure 3. 3100 m Figure 4. 2.5 * 1.5 HIF-1!/!-actin HIF-1!/!-actin 2 1 0.5 0 1 2 3 4 5 1600 m 6 7 8 9 1 Subjects 2 3 4 3 3100 m 4 5 6 7 * 1.4 1.2 1 0.8 0.6 0.4 0.2 0 1600 m 3100 m 3100 m (without #3) 1600 m vHL/!-actin 3100 m 3100 m 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 1600 m Figure 5. 1600 m 3100 m HIF-2!/"-actin 1 0.8 0.6 0.4 0.2 0 Figure 6. 1600 m 3100 m Figure 7. 1.2 1 Flt-1/!-actin VEGF/!-actin 3.5 3 2.5 2 1.5 1 0.5 0 0.8 0.6 0.4 0.2 0 1600 m 3100 m 1600 m 3100 m 1.2 Enolase/!-actin GAPDH/!-actin 2 1.5 1 0.5 0.8 0.6 0.4 0.2 0 0 1600 m Figure 8. 1 3100 m 1600 m 3100 m