ARTICLE IN PRESS
Progress in Retinal and Eye Research 25 (2006) 249–276
www.elsevier.com/locate/prer
Visual function and dysfunction in early and late
age-related maculopathy
R.E. Hogg, U. Chakravarthy!
Ophthalmology and Vision Science, Queen’s University and Royal Victoria Hospitals, Belfast BT12 6BA, UK
Abstract
Late age-related maculopathy (ARM) is responsible for the majority of blind registrations in the Western world among persons over
50 years of age. It has devastating effects on quality of life and independence and is becoming a major public health concern. Current
treatment options are limited and most aim to slow progression rather than restore vision; therefore, early detection to identify those
patients most suitable for these interventions is essential.
In this work, we review the literature encompassing the investigation of visual function in ARM in order to highlight those visual
function parameters which are affected very early in the disease process. We pay particular attention to measures of acuity, contrast
sensitivity (CS), cone function, electrophysiology, visual adaptation, central visual field sensitivity and metamorphopsia. We also
consider the impact of bilateral late ARM on visual function as well as the relationship between measures of vision function and selfreported visual functioning.
Much interest has centred on the identification of functional changes which may predict progression to neovascular disease; therefore,
we outline the longitudinal studies, which to date have reported dark-adaptation time, short-wavelength cone sensitivity, colour-match
area effect, dark-adapted foveal sensitivity, foveal flicker sensitivity, slow recovery from glare and slower foveal electroretinogram
implicit time as functional risk factors for the development of neovascular disease.
Despite progress in this area, we emphasise the need for longitudinal studies designed in light of developments in disease classification
and retinal imaging, which would ensure the correct classification of cases and controls, and provide increased understanding of the
natural course and progression of the disease and further elucidate the structure–function relationships in this devastating disorder.
r 2005 Elsevier Ltd. All rights reserved.
Contents
1. Age-related maculopathy (ARM) . . . . . . . . .
1.1. Nomenclature . . . . . . . . . . . . . . . . . .
1.2. Clinical classification . . . . . . . . . . . . .
1.3. Histopathology . . . . . . . . . . . . . . . . .
1.4. Prevalence . . . . . . . . . . . . . . . . . . . . .
1.5. Symptoms . . . . . . . . . . . . . . . . . . . . .
2. Measures of visual resolution in ARM . . . . .
2.1. Distance visual acuity (DVA) . . . . . . .
2.2. Near visual acuity (NVA) . . . . . . . . . .
2.3. NVA and reading speed . . . . . . . . . . .
2.4. NVA and eye movements . . . . . . . . . .
2.5. Fixation pattern and rehabilitation . . .
2.6. Reading test design for AMD patients .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
!Corresponding author. Tel.: +44 2890 240503x2516; fax: +44 2890 330744.
E-mail address: u.chakravarthy@qub.ac.uk (U. Chakravarthy).
1350-9462/$ - see front matter r 2005 Elsevier Ltd. All rights reserved.
doi:10.1016/j.preteyeres.2005.11.002
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
250
250
251
251
252
252
252
252
253
253
253
254
255
ARTICLE IN PRESS
250
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
3. CS and ARM . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
3.1. CS in ARM . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
3.2. Luminance and CS in ARM . . . . . . . . . . . . . . . . . . . . .
3.3. CS and monitoring disease progression . . . . . . . . . . . . .
4. Cone function and ARM . . . . . . . . . . . . . . . . . . . . . . . . . . . .
4.1. Short-wavelength sensitive (SWS) cones and ARM . . . . .
4.2. Surface colour methods . . . . . . . . . . . . . . . . . . . . . . . .
4.3. Colour-matching procedures . . . . . . . . . . . . . . . . . . . . .
4.4. Short-wavelength automated perimetry (SWAP) . . . . . . .
4.5. Cone sensitivity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
4.6. Colour CS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
5. ARM, AMD and electrophysiology. . . . . . . . . . . . . . . . . . . . .
5.1. Focal ERG (fERG) . . . . . . . . . . . . . . . . . . . . . . . . . . .
5.2. Multi-focal ERG (mfERG) . . . . . . . . . . . . . . . . . . . . . .
5.3. Visually evoked potentials. . . . . . . . . . . . . . . . . . . . . . .
6. Visual adaptation and ARM. . . . . . . . . . . . . . . . . . . . . . . . . .
6.1. Photostress test . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
6.2. Dark adaptation and scotopic sensitivity . . . . . . . . . . . .
6.3. Cone adaptation . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
6.4. Flicker sensitivity . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
6.5. Cone flicker sensitivity . . . . . . . . . . . . . . . . . . . . . . . . .
6.6. Flicker sensitivity and progression to AMD . . . . . . . . . .
7. Central visual field sensitivity and ARM . . . . . . . . . . . . . . . . .
8. Indices of metamorphopsia and ARM . . . . . . . . . . . . . . . . . . .
8.1. Amsler charts. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
8.2. Preferential hyperacuity perimeter (PHP) . . . . . . . . . . . .
8.3. Shape-discrimination charts. . . . . . . . . . . . . . . . . . . . . .
9. Self-reported visual functioning and ARM . . . . . . . . . . . . . . . .
9.1. Evaluation of QOL . . . . . . . . . . . . . . . . . . . . . . . . . . .
9.2. Relationship between self-reported difficulties and clinical
10. Bilateral late AMD impact on visual function . . . . . . . . . . . . .
11. Predictive markers of nvAMD . . . . . . . . . . . . . . . . . . . . . . . .
12. Summary and future directions . . . . . . . . . . . . . . . . . . . . . . . .
13. Method of literature search . . . . . . . . . . . . . . . . . . . . . . . . . .
Acknowledgement . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
...........
tests of vision .
...........
...........
...........
...........
...........
...........
1. Age-related maculopathy (ARM)
(Gass, 1973; Bird, 1974), but more recently this was
considered to have pejorative tones and has been substituted by the term age-related macular degeneration
(AMD). More often than not the term AMD is used when
an exudative lesion is found in the posterior pole of the eye,
though it may also be employed to include a characteristic
confluent area of atrophy, which is also referred to as
geographic atrophy (GA). More recently the terms
neovascular (nvAMD) and geographic atrophy (gaAMD)
AMD have been utilised.
Prior to the development of noticeable vision loss, a
variety of other clinical manifestations are seen in the
macular retina. Typically, a reduction in the foveal reflex
and abnormalities of pigmentation are observed. Characteristic yellow-whitish spots known as drusen are seen
concentrated in, and around, the posterior pole of the eye.
Diffused as well as focal areas of depigmentation form due
to atrophy of the RPE (hypopigmentation) as well as areas
of increased pigmentation (hyperpigmentation). Usually,
these manifestations are not accompanied by overt visual
dysfunction. Epidemiological and histopathological studies
provided some evidence to link these features that appear
in the ageing macula with the subsequent development of
ARM is a degenerative disorder of the central retina,
most commonly encountered in older people. In this
condition, morphological changes in the macular retina
are observed in people over the age of 50 years, and a
proportion of those affected develops a profound irreversible loss of central vision in one or both eyes. When
central visual dysfunction is present, it is often due to either
an extensive atrophy of the tissues of the macular region
or because of scarring following the development of a
neovascular lesion.
1.1. Nomenclature
The terminology used to describe the different manifestations with or without vision loss of this ageing disorder
has undergone several modifications over time. Early in the
20th century, exudative lesions in the posterior pole were
referred to as Kuhnt Junius disease or disciform degeneration (Duke-Elder, 1940; Ryan et al., 1980) owing to the
circular disposition of the macular scar. In the nineteen
sixties, the term senile macular degeneration was coined
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
255
255
256
256
257
257
257
257
258
258
259
259
260
260
261
261
261
261
262
263
263
264
264
266
266
266
266
266
267
267
268
270
270
271
271
271
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
251
Table 1
The International Classification and Grading System for age-related maculopathy (ARM) and age-related macular degeneration (AMD) (Bird et al., 1995)
Early ARM
! Soft drusen X63 mm
! Areas of increased pigment or hyperpigmentation (in the outer retina or choroid)
! Areas of depigmentation or hypopigmentation of the RPE, more sharply demarcated than that of drusen,
without visibility of the underlying choroidal vessels associated with drusen
Late ARM (AMD)
Geographic atrophy (gaAMD)
Neovascular (nvAMD)
! Any sharply delineated roughly round oval area of depigmentation, or hypopigmentation or apparent absence
!
!
!
!
!
of the RPE in which choroidal vessels are more visible than that in surrounding areas that must be at least
175 mm in diameter
RPE detachment(s), which may be associated with neurosensory retinal detachment, associated with other
forms of ARM
Sub-retinal or sub-RPE neovascular membrane(s)
Epiretinal (with the exclusion of idiopathic puckers), intraretinal, sub-retinal, or sub-pigment epithelial scar/
glial tissue or fibrin-like deposits
Sub-retinal haemorrhages that may be nearly black, bright red or whitish yellow and that are not related to
other retinal vascular disease
Hard exudates (lipids) within the macular area related to any of the above and not related to other retinal
vascular disease
GA and/or a disciform scar. The absence of a universally
accepted definition of what truly constituted AMD led to
the use of a wide variety of terms in the many publications
on this topic and discordant epidemiological findings
(Bressler et al., 1990; Goldberg et al., 1988; Klein et al.,
1992). Therefore, the International Classification and
Grading System was developed to standardise the terminology used and to provide researchers with a common
nomenclature for undertaking, recording, analysing
and reporting their findings, enabling robust comparisons
to be made between studies (Bird et al., 1995) (Table 1).
This system proposed the use of the term ARM to
describe the entire spectrum of changes, ranging from the
early manifestations to advanced features accompanying
vision loss. A further sub-division was proposed to
distinguish the early manifestations from late disease with
vision loss; and the terms ARM or early ARM used to
describe the former, and late ARM or AMD the latter,
respectively.
All the features of nvAMD suggest the presence of
abnormal blood vessels derived from the choroidal
circulation that have breached the normal anatomical
barriers and make their presence in the subpigment epithelial or sub-retinal spaces. This process is
termed choroidal neovascularisation (CNV). Other studies
including the Eureye (Augood et al., 2004) and AgeRelated Eye Disease study (AREDS, 2001) have introduced the concept of staged disease severity with ARM
1, 2 and 3, representing combinations of drusen and
pigmentary irregularities, and 4 when CNV or GA is seen
(Fig. 1).
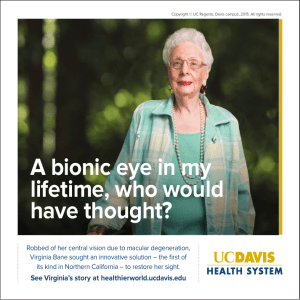
Fig. 1. Four stage ARM disease severity with ARM 1, 2 and 3
representing combinations of drusen and pigmentary irregularities and 4
when CNV or GA are present.
1.2. Clinical classification
1.3. Histopathology
Traditionally, clinicians and patients tend to refer to the
characteristic macular changes as dry or wet AMD. The
term dry is used to denote the absence of CNV, and thus
could refer to the presence of early ARM features or GA.
Histopathological techniques have revealed that eyes
from donors with AMD show accumulation of membranous debris on both the outer and inner aspects of the
ARTICLE IN PRESS
252
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
basement membrane of the retinal pigmented epithelium
known as basal linear deposit and basal laminar deposit,
respectively (Curcio, 2001). On the basis of immunohistochemical analyses, drusen have been shown to contain a
variety of complex lipid, protein and carbohydrate
moieties. These are most probably derived from the shed
outer segments of photoreceptor cells following phagocytosis by the RPE. Curcio et al. (1996) demonstrated cone
photoreceptor degeneration is present in most eyes with
early ARM. The investigators obtained post-mortem
material from donor eyes, and on application of a
systematic method of grading they noted shortening of
outer segments and broadening of the inner segments in
eyes with ARM when compared with those without ARM
features. It has, therefore, been suggested that the
morphological and functional changes in Bruch’s membrane and the RPE result in disordered phagocytosis and
recycling of the photoreceptor outer segments.
The onset of aberrant choroidal angiogenesis with
vessels transgressing Bruch’s membrane results in the
formation of the neovascular complex, which comes to lie
in the sub-pigment epithelial and sub-retinal spaces (Green
and Enger, 1993). The vessels are incompetent and leak
serous fluid and blood. Ultimately, the vessels involute
leaving behind a non-perfusing scar, which enmeshes the
delicate retina causing distortion and disorganisation of the
cellular architecture. These changes are incompatible with
normal visual function and often irreversible, and dense
central vision loss supervenes. The exact mechanism for
angiogenesis is unknown, although a variety of growth
factors have been postulated (Das and McGuire, 2003).
1.4. Prevalence
The prevalence of ARM increases markedly with
increasing age, although ARM is uncommon before the
age of 50 years; by the age of 90, one in four persons will
have lost vision owing to AMD. Therefore, it is feared it
will become one of the biggest health problems in the next
few decades. In the US, persons aged over 65 form the
fastest growing segment of the population and the
proportion is expected to increase by 53% between 2000
and 2020 (Bartlett et al., 2004b). Likewise, this sector of the
population of the UK is set to increase by over 29% in the
next 20 years (Owen et al., 2003). Nonetheless, in the UK,
3.7% of the population aged 75 years or older and 14.4%
of the population 90 years or older are visually impaired
due to AMD (Evans et al., 2004a, b). Although ARM has
been principally considered to be a disease confined to the
developed world, increasing evidence shows that it is also a
common cause of visual impairment in developing countries (Nirmalan et al., 2004).
1.5. Symptoms
In cases of bilateral early ARM, visual acuity may be
within normal limits in both eyes and many patients are
asymptomatic. A few may complain of symptoms, such as
difficulty in reading under dim light, metamorphopsia and
problems on dark adaptation after exposure to sunlight,
indicating retinal functional deficits not reflected in
traditional measures of visual acuity. The development of
GA can cause a corresponding central scotoma if it occurs
within the central 1–21. The onset of CNV is often
accompanied by a sudden dramatic reduction in
central visual function. The patient will complain of
distortion, inability to distinguish fine detail and central
blurring. In some people, the onset of nvAMD in the
first eye can be asymptomatic, particularly if the loss
has occurred in the non-dominant eye. Frequently, a
patient may only seek help when the second eye becomes
involved.
2. Measures of visual resolution in ARM
2.1. Distance visual acuity (DVA)
It has been reported that each of the early ARM lesions
(soft indistinct drusen, RPE degeneration, increased retinal
pigment, early ARM) is associated with a decrease in
acuity of approximately two letters or fewer, compared to
eyes without those lesions (Klein et al., 1995); although a
statistically significant result, this level of visual deficit is
neither clinically meaningful nor reliably detectable, given
that the test–retest variability of Log MAR charts between
one and two lines (Rosser et al., 2003; Arditi and
Cagenello, 1993; Lovie-Kitchin and Brown, 2000). Therefore, it is generally accepted that the measurement of visual
resolution by using the commonly available distance acuity
charts is inadequate for the assessment of functional
deficits in early ARM and also for monitoring progression
of the disorder (Sarks et al., 1988), and longitudinal studies
have confirmed that visual acuity is a poor predictor for
conversion to nvAMD (Mayer et al., 1994). Nonetheless, in
terms of the ease of use and widespread availability, acuity
testing using the Log MAR or EDTRS chart is commonly
undertaken as a large measurement range is possible
and crowding effects are better controlled. Log MAR
charts by virtue of their design have better reproducibility
and sensitivity to acuity changes when compared to
the standard Snellen chart (Ferris et al., 1982; LovieKitchin, 1988).
In advanced disease, distance acuity testing by itself
yields limited information. Notably, eyes with advanced
AMD with similar lesion characteristics exhibit a wide
range of acuity (Table 2) (MPS Group, 1994).
Measures of acuity are also often a poor indicator of
ability for visual tasks, such as face recognition and
mobility (Rubin et al., 2000). Despite these caveats,
distance acuity measured under standardised conditions
using the EDTRS Log MAR charts remains the most
commonly used outcome measure in studies and clinical
trials in AMD.
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
Table 2
Distribution of initial lesion size and initial visual acuity at study entry in
MPS study
Visual acuity
Log MAR
Poor (p1.0)
Medium (0.7–1.0)
Good (X0.70)
Lesion size at study entry, MPS disc areas (no.
of eyes)
Small
(p1)
Medium (41
to p2)
Large
(42)
21
34
48
48
48
49
62
34
28
Note the wide range of acuity despite similar lesion characteristics.
Adapted from Table 1, MPS Group (1994).
2.2. Near visual acuity (NVA)
NVA is routinely measured in the form of word acuity as
opposed to single-letter acuity and, therefore, disparities
may be expected when comparing this measure to distance
acuity as a result of the increased complexity of the task.
Despite this, it is generally assumed that a linear relationship is present between distance visual acuity (DVA) and
near visual acuity (NVA) (Bailey and Lovie, 1980). For
example, an individual with 0.0 Log MAR (6/6 Snellen)
would be expected to read 0.25 M (N2). However, in a
small study of 15 AMD sufferers, Kitchin and Bailey
(1981) found that word acuity was invariably worse than
what might be expected from the measured DVA,
regardless of its level with the magnitude of the difference
averaging 0.3 Log units (Kitchin and Bailey, 1981; LovieKitchin and Bowman, 1985). In a recent study to examine
the relationships between measures of vision, which are
normally used in clinical practice, in a population of 469
subjects with a diagnosis of AMD in one or both eyes,
Muldrew et al. (2003) found that the least concordance
between the DVA and NVA occurred in the mid-range,
suggesting that NVA decreases at a faster rate than that of
either DVA or contrast sensitivity (CS).
2.3. NVA and reading speed
Word reading has been suggested as a better discriminator of early deficits in visual function in ARM than that
of distance acuity. Word reading is a complex task
requiring visual resolution of the text, stable retinal images,
saccadic accuracy, word encoding, lexical accessing, and
short- and long-term memory (McMahon et al., 1991).
Reading rate is dependent not only on the functional
capability of the visual system but also on stimulus
conditions such as the numbers of characters in the field,
magnification, blur, contrast and the colours of the text
and background and non-visual features, such as cognitive
abilities, motivation, memory storage and proceduralfactors-associated reading (Legge et al., 1992).
Although all of these features are inter-related, it is
worth remembering that not all of these processes
253
primarily limit reading performance of patients with
advanced AMD (Baldasare et al., 1986). Since most
patients are typically adept readers before disease onset,
the decrease in reading ability can be attributed to factors
disrupting visual-processing ability. Reading speed has
been used in many studies and has been shown to be useful
in the evaluation of disability. In contrast to NVA, reading
speed provides an indication of reading performance and is
a function of both scanning rate and proportion of words
correctly read. Whether the central visual field is intact is
the single most important factor in reading (Legge et al.,
1985). It is acknowledged that considerable variability may
be experienced in reading speed rates despite similar near
acuities; therefore, Legge et al. (1992) attempted to predict
reading speed from a set of routine clinical measures, such
as age, Snellen distance acuity, central visual field status
(scotoma present or absent), ocular media status (clear or
cloudy) and disease diagnosis. These were found to account
for only 30% of the variance in reading rate, and the
authors speculate that the addition of letter CS to the
portfolio of tests would at best account for up to 55% of
the variance. A subsequent review of the literature by
Whittaker and Lovie-Kitchin (1993) looking at the
problem from the standpoint of a low-vision practitioner
highlighted four clinical measurements, which they showed
provided improved prediction of reading rates, they were
as follows: an accurate measure of field of view, central
scotoma size, contrast reserve and acuity. They derived
visual requirements for different types of reading rate from
published research. As expected, the reading rate of
patients with longstanding AMD was shown to decrease
rapidly with increasing scotoma size. They concluded that
contrast and print size needed to be several times threshold
and the diameter of the central scotoma needed to be
less than 221 to make fluent-reading possible. However,
correlations were weak and it is evident that non-visual
factors play an important role in a subject’s reading
performance. Thus, it appears that performances on other
clinical tests of vision are poor predictors of reading speed,
and emphasises the importance of routine measurement of
reading performance within a clinical setting.
2.4. NVA and eye movements
Reading performance is also strongly influenced by eyemovement control (Cummings et al., 1985; McMahon
et al., 1991). Saccadic eye movements are required to shift
the fovea along the retinal image of the text line, with the
fovea held in position using the fixational oculomotor
system (slow control and microsaccades). The sequence of
saccades and fixation is repeated over and over to bring the
text further along the line to the fovea, allowing the
experienced reader to read at the rate of hundred words per
minute (Timberlake et al., 1986). Eye movements have
been noted to be abnormal in patients with AMD
(Cummings et al., 1985; McMahon et al., 1991). Patients
with AMD and other maculopathies exhibit an increased
ARTICLE IN PRESS
254
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
number of fixations during a reading task (Rayner and
Bertera, 1979), abnormal eye movements (Whittaker et al.,
1988; Cummings et al., 1985), poor saccadic accuracy and
an increase in saccadic frequency to reach the intended
target (McMahon et al., 1991). However, a study by
Bullimore and Bailey (1995) found similar fixation rates in
ARM subjects to normals despite averaging fewer letters
per forward saccade and more backward regressions. They,
therefore, concluded that poor oculomotor control plays a
lesser role in comparison to reduced perceptual span. As
the tests were carried out over a range of luminances, this
study also highlighted the important relationship between
reading performance and illumination in AMD patients, as
reductions in luminance produced changes in scotoma size
and shape with resultant decreased acuity and reading
speed. This emphasises the clinical importance of determining optimal levels of illumination for reading for AMD
patients and advising them accordingly (Eldred, 1992;
Bowers et al., 2001).
The advent of scanning laser ophthalmoscopy (SLO)
microperimetry in the late eighties allowed many fundamental questions about reading with a macular scotoma to
be investigated and provided some crucial insights into the
relationships between reading rate, fixation stability and
eye movements. Initial reports showed that patients with
dense macular scotomas involving the fovea used a single
unique retinal area immediately adjacent to the scotoma to
fixate (Timberlake et al., 1986). This locus of fixation was
also used to inspect targets and read simple text. The
authors termed this as the preferred retinal locus (PRL).
Further, studies indicated that the PRL did not have a
predilection for any specific retinal quadrant, but did find
that the least-diseased area of the retina closest to the
foveola was used. This corresponded to an area of RPE
hyperplasia in well over half of the cases examined (Tezel
et al., 1996). In general, the PRL is located in an area
immediately adjacent to the scotoma (Timberlake et al.,
1987; White and Bedell, 1990; Sunness et al., 1996), in the
lower part (Weiter et al., 1984) and to the left of the visual
field (Guez et al., 1993; Fletcher and Schuchard, 1997).
This is surprising as subjects with normal eye sight obtain
textual information in the English language much more
efficiently from the right visual field than from the left,
implying that placement of a scotoma to the left of the
lesion would be more advantageous. The majority of
patients with a central scotoma due to AMD are thought
to develop a PRL. A large study of 825 patients with AMD
tested using SLO macular perimetry revealed that 84% had
an established PRL. Interestingly, a sixth of these patients
had a PRL that was surrounded by a dense scotoma
(Fletcher and Schuchard, 1997). More recently, it has been
recognised that patients often adopt multiple PRLs in
which each can be used predictably depending on the task
parameters (Duret et al., 1999; Lei and Schuchard, 1997;
Deruaz et al., 2002). This explains the finding of saccades
and eye movements that at first appear inappropriate and
uneconomical for the formation of a well-structured
reading strategy. It also helps understand eye movements
that involve purposeful changes of PRL (Safran et al.,
1999). The PRL can shift in response to change in stimulus
size (Guez et al., 1993) or illumination (Lei and Schuchard,
1997). In some cases, patients appear to use a combination
of PRLs. Thus, a patient may use a PRL, which has a high
spatial resolution, but textual information may fall
partially within a scotoma. To overcome this, the patient
may switch to another PRL where entire words are visible
but with lower spatial resolution. Switching allows the
patient to localise the word in its entirety (Duret et al.,
1999). Adaptation of the oculomotor system is also
necessary in order to accurately search for, position and
stabilise text at a non-foveal location (Heinen and
Skavenski, 1992). That a significant proportion of patients
choose a PRL so that it lies to the left of the scotoma in the
visual field necessitating forward saccades into the scotoma
has created much discussion. Recent evidence has suggested there may be a correlation between the retinal area
with higher attentional capability (which is patient specific)
and a patient’s choice of location of PRL when AMD
develops. This is based on the finding that eight out of
nine patients with AMD show a PRL position corresponding to a location with good attentional performance. The
authors caution that prospective studies will be required to
substantiate these findings (Mackeben, 1999; Alpeter et al.,
2000).
To investigate the extent to which fixation stability
influences reading speed, Crossland et al. (2004) undertook
a longitudinal study to assess the development of viewing
strategies in macular disease. They followed a cohort of
subjects for up to 1 year when the second eye developed
macular disease. A linear relationship between fixation
stability and reading speed was noted with 54% of the
variance in change of reading speed, accounted for, by
changes in fixation stability. As with other studies, there
was no relationship between scotoma size and fixation
stability (Timberlake et al., 1986,1987; White and Bedell,
1990) and nor did measured visual acuity and CS correlate
with fixation stability. On investigating, the correlation
between reading speed and size and nature of the scotoma
(absolute or relative) by using SLO microperimetry in
patients with AMD, Ergun et al. (2003) found that only the
size of the absolute scotoma demonstrated significant
relationships with measures of reading.
2.5. Fixation pattern and rehabilitation
A recent study investigating the success of training
patients in eccentric viewing confirmed the finding that a
PRL to the left of the retinal lesion is unfavourable for
reading. The investigators used the SLO to establish a new
trained retinal locus either above or below the retinal lesion
that is more favourable as there are no blind spots at
this horizontal level. The range achieved by most of the
AMD patients was between 50 and 106 words despite
the group being over 77 years of age and with an average
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
best-corrected distance visual acuity of 20/500 (Nilsson
et al., 2003). These findings are very encouraging as after
an average of 5–6 h of formal training, patients were able to
read at a speed close to that achieved by similar age-group
with normal visual acuity, who averaged a reading speed of
83 words/min (Lott et al., 2002).
2.6. Reading test design for AMD patients
Tests of reading function should contain unrelated
words as patients may mask their visual disability by
guessing words correctly on the basis of the context derived
from the sentence (Fine et al., 1999; Bailey and Lovie,
1980). Syntactic and semantic clues are absent in text
composed of unrelated words forcing the patient to rely
exclusively on the visual information gathered from the
printed page (Baldasare et al., 1986). It has been shown
that sentence context increases reading speed, regardless of
where the text is positioned on the retina (Fine et al., 1999).
The number of words per line must also be considered as
the crowding phenomenon may be more severe in AMD
patients (Rubinstein and Underwood, 1985; Kitchin and
Bailey, 1981) causing reading difficulty to increase as word
length increases. Large words require the use of increasingly more eccentric retinal locations. Performance measured in terms of accuracy or latency decreases as a
stimulus is moved further from the foveal centre (Eriksen
and Schultz, 1977; Lefton and Haber, 1974; Rayner and
Bertera, 1979; Baldasare et al., 1986). Varying the word
length of the textual information is an important parameter
to allow approximation to normal reading as the task
requires the planning and execution of saccadic eye
movements of various extents (Rayner, 1978).
While evaluating the Pepper visual skills for reading test,
which was designed to assess the visual components of the
reading process in low-vision individuals, Baldasere et al.
(1986) identified three categories of AMD patient. They
were those who are (a) inaccurate and slow, (b) accurate
but slow and (c) accurate and quick. These findings had
important implications for the most effective reading
strategy for each patient. Those who are inaccurate may
need eccentric viewing- or fixation training, whereas the
accurate but slow reader may need extensive word
recognition training. Elliott et al. (2001) have shown that
subjects with cataracts have an optimal reading speed
similar to that of a control group, whereas in those subjects
with AMD it was substantially worse. Therefore, reading
speed has also been proposed as a useful test to
differentiate loss of acuity due to lenticular changes from
that caused by undetected macular disease.
3. CS and ARM
CS is a measure of the threshold contrast for seeing a
target whereas acuity is a measure of the spatial-resolving
ability of the visual system under conditions of very high
contrast (Owsley, 2003). CS relies on lateral inhibitory
255
mechanisms mediated by horizontal and amacrine cells,
thus may enable subtle deficits to be detected when there is
widespread yet early pathological change.
3.1. CS in ARM
As early as 1977, Sjostrand and Frisen (1977) used a
television-based display and sinusoidal gratings of variable
contrast and spatial frequency to test patients with macular
disease against age-matched controls. In early ARM, there
were decreases in CS at high and intermediate frequencies
whereas in eyes with AMD, impairment across the whole
spatial frequency range was observed. Another small study
(Wolkstein et al., 1980) reported losses at both low and
high spatial frequencies and a high-frequency cut-off
frequency measured using a grating above that, which
would be expected from the patient’s letter acuity scores.
As only four patients with ARM were evaluated in this
study along with the absence of information on disease
severity, rendering comparisons between this study and
that of Sjostrand is difficult.
The concept of ‘‘hidden vision’’ in which patients with
macular degeneration may have greatly reduced visual
acuity or nearly normal CS at low spatial frequencies and
reasonably good CS at intermediate spatial frequencies was
first proposed by Hyvarinen et al. (1983). In this study, CS
function was measured in a group of 17 patients with
macular or optic nerve disease; only two patients had
AMD. The investigators found that when a small 51
grating field was used, threshold CS was low at all spatial
frequencies, however, when a 201 grating field was used,
threshold CS was nearly normal at spatial frequencies
below 0.7 cyc/deg, but above this there was a marked loss
of sensitivity. In contrast, Loshin and White (1984) tested
40 patients with AMD, and found a decrease in sensitivity
at all spatial frequencies. These findings highlight the
difficulties encountered when comparing studies that have
employed varying stimulus parameters.
Brown and Lovie-Kithchin (1987a) assessed the contrast
sensitivity functions in the central retina and at 21, 51 and
101 eccentricity in the paracentral retina of 8 patients with
varying degrees of early ARM and 8 age-matched controls.
ARM patients and controls had normal visual acuity.
Contrast sensitivity was depressed in ARM patients
compared to that of normals, when tested at the fovea
and at all levels of eccentricity. Although the overall
difference between ARM and normals failed to reach
significance, all individual points plotted for the former
were below those of the latter. A greater loss was found for
high spatial frequencies than for low spatial frequencies at
all eccentricities.
Further, evidence for the existence of a loss of vision in
ARM, which remains undetected by conventional acuity
measures, was reported by Kleiner et al. (1988). Regan
letter charts, which are similar to Log MAR charts, except
that the test letters are available in varying degrees of
contrast, were used in a group of 52 patients with macular
ARTICLE IN PRESS
256
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
drusen and VA of at least 20/20. An age-matched control
group of 27 normals were also assessed. The drusen groups
read fewer letter than the control group and the difference
increased as the contrast of the charts decreased. The
difference was also found to correlate with disease severity
when CS was measured using a Ginsburg CS chart. A
reduction in CS at high spatial frequencies along with a loss
of peak CS with increasing drusen severity was noted when
eyes were placed into four categories. Category 1 consisted
of eyes with a few fine discrete drusen, while category 4
demonstrated numerous large confluent drusen, with eyes
at grades 2 and 3 exhibiting changes of intermediate
severity. Stangos et al. (1995) also sought to evaluate CS in
eyes with drusen and good visual acuity, and found that CS
loss was found in all eyes with drusen and normal visual
acuity and although this loss occurred at all spatial
frequencies, it was more significant in the middle range
and high spatial frequencies. They did not, however, find a
greater CS loss with increasing drusen severity as found by
Kleiner et al. (1988).
The use of low-contrast Regan letter charts was also
investigated in a small case-control study of six ARM cases
and 12 normal controls (Abadi and Pantazidou, 1996).
Since differences in acuity between ARM and age-matched
controls were found at all letter contrast levels, the
investigators concluded that the use of low-contrast letter
charts was not warranted. However, a larger study that
investigated relationships between visual acuity and peak
CS in 100 patients with early and late ARM with visual
acuities ranging from 0.7 to o1.60 Log MAR (Alexander
et al., 1988) found a significant correlation between these
two measures (r ¼ 0:62) and also noted the wide range of
CS at every level of visual acuity. The authors recommend
that CS testing can provide important additional information over, and above, that obtained by measuring acuity
alone.
Although the majority of studies specifically designed to
assess contrast function in early ARM were of small size
and did not stringently evaluate disease severity, the
evidence is in favour of a loss of CS at mid-to-high spatial
frequencies and also suggests that lower spatial frequencies
may be spared in the early stages of the disease, especially
at low luminance.
3.2. Luminance and CS in ARM
The observation that patients with ARM often have
difficulties in adapting to changing luminance levels led
Brown and Garner (1983) to examine the effect of
luminance on the CS function in six patients with ARM
(pigmentary irregularities, drusen, serous and sub-retinal
detachment) and in five age-matched normal persons.
ARM patients showed a greater loss of CS at the higher
luminance levels, indicating that contrast detection mechanisms at low luminances were intact. In the ARM
patients, the peak of the curve was shifted to lower spatial
frequencies at all the luminance levels tested. The authors
also noted that despite ARM patients having similar
acuity, there was considerable variation in contrast
functional though this may have been due to poor control
of fixation. A subsequent study by Brown et al. (1984)
examined the effect of luminance on low-contrast visual
acuity in ARM and compared this with six normal
participants of approximately the same age. ARM patients
had difficulty in performing the tasks at the lower
luminances and showed little or no increase in visual
acuity with increasing contrast levels. All patients had
relatively good acuity, and yet small decreases in luminance
(about 1.7 Log units) had profound effects on acuity. Thus,
one may conclude that adaptation mechanisms that allow
the normal visual system to operate efficiently over a wide
range of luminances are affected in ARM, even when
clinically measured acuity is only moderately depressed.
3.3. CS and monitoring disease progression
Since CS is a measure of more extensive retinal
involvement with deficits noted in eyes with early ARM
features despite the presence of a normal visual acuity, this
measure was mooted as a potential prognostic indicator for
progression to more advanced disease. Stangos et al. (1995)
in their cross-sectional analysis of eyes with drusen and
good acuity concluded that CS was not a prognostic
indicator since all the eyes in this study with drusen had CS
loss, yet longitudinal studies have shown that only a small
proportion of eyes with drusen develop nvAMD. Similarly,
Midena et al. (1997) measured CS with sinusoidal gratings
at several different spatial frequencies in 34 eyes of patients
with drusen and normal visual acuity, 13 fellow eyes of
patients with AMD and 36 age-matched control eyes. They
found progressive impairment of spatio-temporal CS at all
spatial frequencies. Both static and dynamic CS measured
at 20 cyc/deg correlated with disease severity when this was
measured by the presence of focal hyperpigmentation or
GA. Since drusen number did not influence spatiotemporal CS, the investigators concluded that a reduction
in CS and the degree of CS loss were not prognostic
indicators for the development of nvAMD. One of the
limitations of CS is that a reduction is not specific to retinal
disease and may be seen in the presence of medial opacities.
However, CS may be useful in the monitoring of disease
progression particularly as a marker of outcome in clinical
trials. Various clinical trials of interventions for nvAMD
have measured multiple parameters such as visual acuity
and CS and these have provided opportunities for
examining relationships between these measures of vision
in a longitudinal manner (Bellmann et al., 2003). Only
moderate agreement was found between change in visual
acuity and change in CS. Therefore, the authors recommend that both be considered as important independent
parameters for visual impairment. Also, as CS loss at
middle and low spatial frequencies have important
consequences for tasks, such as recognition of faces, seeing
kerbs and low-contrast structures (Owsley et al., 1981;
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
Marron and Bailey, 1982), it may be useful as a surrogate
marker for a patient’s ability to undertake daily living
tasks.
4. Cone function and ARM
It has long been accepted that retinal diseases, including
degenerative macular conditions, lead to tritan-like defects
particularly in the early stages when visual acuity is within
the normal range (Francois and Verriest, 1961; Hart, 1987;
Campbell and Rittler, 1972; Bowman, 1980a, b; Barca and
Vaccari, 1978; Applegate et al., 1987; Trusiewicz et al.,
1984). Köllner’s rule states that generally blue–yellow
defects occur in retinal disease whereas red/green are
associated with optic nerve disease. These observations
imply that in early AMD, chromatic mechanisms necessary
for colour vision are selectively damaged (Hart, 1987)
whereas spatial discrimination and luminance detection are
spared.
4.1. Short-wavelength sensitive (SWS) cones and ARM
The blue on yellow deficits seen in retinal disorders has
evoked interest in the potential role of short-wavelength
sensitive (SWS) cones as a site of early involvement in
AMD. These cells, together with the small bistratified
ganglion cell layer (Dacey, 1993), are known to be
associated with an ‘‘opponent’’ psychophysical channel,
which sub-serve the discrimination of blue from yellow
hues (Calkins, 2001). The unique properties of SWS cones
in terms of morphology, distribution, origin and behaviour
have been extensively reported and summarised (Calkins,
2001). The apparent vulnerability of the SWS cone
function early in pathological processes has stimulated
debate on whether this system is selectively damaged, or is
intrinsically prone to injury (Hood and Greenstein, 1988),
since increased susceptibility of this system to light damage
has been shown (Marc and Sperling, 1977; de Monasterio
et al., 1981; Sperling et al., 1980). Their increased
vulnerability to biochemical perturbations is one of the
theories promoting a selective loss of SWS cones, as
changes that occur at the level of the RPE as a result of a
thickened Bruch’s membrane (Spraul et al., 1999) increased
diffusion distance for photopigment turnover may create
the conditions for the development of a prominent tritan
deficiency. However, SWS cones are fewer numerically and
more sparsely distributed as compared to the other cone
classes and their output appears to be pooled (Calkins
et al., 1996). Therefore, non-selective destruction of the
ganglion cell fibres would result in a more apparent blue/
yellow deficit when compared to red/green (Hart, 1987).
Thus, an alternative hypothesis for the occurrence of tritan
deficits in early disease processes is that blue cones are no
more vulnerable than other retinal cell types, but because
of the nature of their connections, the psychophysical
losses might appear greater than that for other modalities.
257
Psychophysical testing of the SWS system is facilitated
by its spectral properties, in that the peak in sensitivity of
440–450 nm is distinct from the other two cone types by
approximately 100 nm. This allows the selective isolation of
the channel that serves the s-cones when appropriately
designed stimuli and background are utilised (Calkins,
2001). The acquired trianopic defect can also be detected
by traditional colour-vision tests, such as the Farnsworth–
Munsell 100 hue test and the Farnsworth D-15 test.
4.2. Surface colour methods
The Farnsworth–Munsell 100 hue test has been used by
several groups to characterise the relationship between
early ARM and colour vision. These studies showed an
increase in the error scores with typically tritan defects in
patients with macular changes (Trusiewicz et al., 1984;
Bowman, 1980a, b; Applegate et al., 1987) and the extent of
the defect is affected by illuminance (Bowman, 1978;
Bowman, 1980a, b; Bowman and Cameron, 1984). An
improvement in colour discrimination is found as illuminance increases but reaches a threshold beyond which
further increases in illuminance do not improve colour
discrimination. Conversely, discrimination deceases as
illumination decreases and this takes place to a greater
extent in subjects with ARM as compared with an agematched elderly control group.
Despite only following three patients with varying
degrees of ARM, a longitudinal study for over 2 years
using Farnsworth–Munsell D-15 and Panel D-15 tests
suggested that tritan defects increased over time and
appeared to accelerate at or near the time when one of
the patients developed a small exudative pigment epithelial
detachment (Applegate et al., 1987). At this stage, an
increase in the number of red–green type errors also
became evident. The D-15 and the desaturated D-15 have
also been used to demonstrate significant and predominantly tritan dyschromatopsias in early ARM in comparison to normal controls (Collins, 1986). It is noteworthy
that increased sensitivity of the desaturated version is offset
by a lack of specificity (Cheng and Vingrys, 1993).
Midena et al. (1997), in a study of early ARM in 83
patients, found no colour discrimination abnormalities,
although other tests of vision indicated measurable visual
impairment. However, the authors acknowledge that their
findings are inconsistent with the majority of the literature
and they suggest that commercially available colour-vision
tests may not be sensitive enough to detect the subtle
changes.
4.3. Colour-matching procedures
The trichromatic nature of colour vision allows almost
any colour to be matched by a mixture of three colours.
This principal can be used to provide a method to assess
the integrity of the cone’s outer segments where the subject
matches a standard light of intermediate wavelength with
ARTICLE IN PRESS
258
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
a mixture of longer and shorter wavelength lights (Elsner
et al., 2002). This allows the quantification of the amount
of photopigment in long- and middle-wavelength cones.
Eisner et al. (1987) used a free viewing anomaloscope in
deutan mode to obtain Raleigh matches (primaries of peak
wavelengths 536, 588 and 649 nm with half bandwidths of
10 nm) in subjects whose fellow eye has nvAMD (Group 1)
and compared the results with a age-matched control
group (Group 2), which contained patients with no fundus
changes or drusen and/or hypopigmentation. Group 1
subjects were more likely to have a colour-match area of
magnitude zero or less in their good eye than Group 2
subjects in either eye. The size of the colour-match area
relates to the effective photopigment density of the foveal
cones, implying a substantially reduced density in those
whose fellow eye has suffered from nvAMD compared to
those eyes whose fellow eye has not suffered from nvAMD.
Eyes with colour-match area effects of less than 0.3 were
also found to have lower sensitivities at absolute threshold
which suggests defects can be found in both chromatic and
achromatic systems early in ARM when measured carefully. This was consistent with the data found by Smith
et al. (1988), who used an early classification system
proposed by Sarks (1976) to show that abnormalities of
colour matching increased with increasing retinal abnormality. In the longitudinal study, Eisner et al. (1992) followed
47 patients with nvAMD in the fellow eye for at least 18
months, using a similar battery of visual function tests and
fundus photographs to assess progression. During the
follow-up period, 11 subjects had neovascular outcomes
and four eyes had acuity loss outcomes but without
nvAMD. Morphologically, the summed area of confluent
drusen and atrophy within the central 3000 mm could be
used to effectively distinguish eyes with neovascular
outcomes from eyes with minimal-acuity loss outcomes.
Functional data suggested that the combinations of darkadaptation time constant and colour-match area effect
(implying low foveal quantum absorption capabilities)
were good at predicting outcome. The morphological risk
factors identified were systematically related to the functional risk factors. However, despite the association
between low s-cone sensitivity and a neovascular outcome,
as a prognostic test, its age dependence and association
with pre-retinal absorption makes its use in establishing
risk cross-sectionally problematic.
The awareness of functional damage to cone photoreceptors in early AMD prompted Elsner et al. (2002) to
investigate whether the damage caused by early ARM
(reduced photopigment density) could be explained principally by RPE/Bruch’s membrane changes slowing regeneration of photopigment, altering bleaching and kinetic
measurements, or whether it was just a more extreme form
of ageing causing decreased quantal catch and decreased
optical density of photopigment. This was achieved by
performing colour matching over a series of light levels in
patients with early ARM and a normative group. Although
visual acuity was not correlated with maximum optical
density, early ARM subjects had significantly lower optical
density than that of normals. Analysis of the data indicated
that the kinetic hypothesis (reduced trafficking through the
RPE) could not explain the changes in photopigment
density and they concluded that reduced photosensitivity
of the cones had the larger effect prior to severe vision loss.
This study also did not support the hypothesis that
abnormal cone orientation was the cause of the decreased
photosensitivity. The authors felt their results were
suggestive of an altered microenvironment reducing the
quantal catch of the cone.
4.4. Short-wavelength automated perimetry (SWAP)
Despite SWAP being principally used to detect visual
loss due to glaucoma, it has been applied to retinal
diseases, such as retinitis pigmentosa and macular oedema
(Greenstein et al., 1989, 1992). A standard HFA perimeter
modified for SWAP using a commercially available
program was chosen by Remky et al. (2001) to explore
SWS in ARM. They measured SWS cross sectionally in 126
patients with non-neovascular ARM (drusen, hyperpigmentation and/or small atrophic lesions o200 mm) with
visual acuity 420/50, 75 of these had a sight-threatening
complication in the fellow eye. Besides finding a significant
decrease in mean SWS with age, they found that eyes with
soft drusen had significantly reduced mean sensitivity
compared to those without despite no difference in age or
Log MAR visual acuity. They adhered to strict entry
criteria to ensure that media changes did not influence the
age-related findings. Comparison of the 75 patients with
neovascular or atrophic AMD with the rest showed that
while the incidence of soft drusen was not significantly
different between these two groups, hyperpigmentation
was more common in the unilateral AMD group. Despite
those with focal pigmentation having no significant
decrease in sensitivity as compared to those without, they
did have a significant decrease in the central part of the
field when compared with the more eccentric. The authors
suggest the use of this method to assess ARM progression
or treatment outcomes in future clinical trials; however,
the distinction between SWS loss due to media changes
and that due to retinal factors in a general, elderly clinic
population would be difficult.
4.5. Cone sensitivity
Several studies have specifically measured s-cone sensitivity or compared each of the three retinal cone mechanisms in early ARM. Applegate et al. (1987) used chromatic
backgrounds to optimise the individual sensitivities of
the short-, medium- and long-wavelength sensitive cone
mechanisms in three patients with ARM. They found that
sensitivities were within normal limits when test conditions
used the red and green cone mechanisms whereas
significant losses in the sensitivities of blue cone mechanisms were found in both non-neovascular and neovascular
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
eyes. This finding was confirmed by Eisner et al. (1987),
who measured s-cone sensitivity in eyes whose fellow eye
has nvAMD and age-matched controls and found a
statistically significant difference. Two-increment thresholds were measured in ARM patients and pre-ARM
patients with relatively small acuity losses as well as in a
group of elderly control patients, using conditions designed
to isolate each of the three cone mechanisms (Haegerstrom-Portnoy and Brown, 1989). The short(s) wavelength
sensitivities were corrected for losses due to media
absorption. Once again s-cone sensitivity was depressed
in the ARM group as compared to the pre-ARM and
elderly group, interestingly they found loss was significantly greater among females. Their findings were also
correlated with the error score on the D-15 test that is
consistent with receptoral loss. Despite finding only a weak
association between high-risk drusen characteristics (presence of soft drusen, confluence of drusen and focal
hyperpigmentation) and a lower s-cone pathway, Sunness
et al. (1989) suggested that alterations in s-cone sensitivity
might be indicative of more severe pathology not clinically
apparent since drusen alone do not appear to alter
sensitivity.
4.6. Colour CS
Colour CS tests, in which isoluminant stimuli are used,
allow the separation of a luminance defect from a
chromatic defect. The hues are modulated along colour
confusion lines for trichromatic vision, therefore, changes
in colour contrast are the only cues to image recognition
(Holz et al., 1995). Early studies using them as a perimetric
technique reported that all visual field defects, which were
demonstrable by conventional forms of perimetry were also
detectable by the colour contrast technique (Hart, 1987). A
computer graphics system developed by Arden and coworkers was used by Holz et al. (1995) to evaluate colourvision deficits in patients with macular drusen. In total, 84
eyes from 84 patients with macular drusen and clear media
were tested, and compared to an age-matched normal
control group. Interestingly, at baseline, foveal measurements showed a markedly elevated tritan threshold for the
drusen patients and protan and deutan thresholds which
were slightly above the normal limit, however, parafoveally
the tritan threshold was normal whereas the red and green
were abnormal. Throughout the 2-year follow-up, tritan
thresholds changes were significantly different from baseline in the fovea whereas colour sensitivity for red and
green showed no change at either a foveal or parafoveal
location. Within the follow-up period, eight patients
developed a complicating macular lesion (foveal GA in
one patient and CNV in the others) and these patients had
a significantly higher tritan threshold at baseline than those
who did not develop late-stage disease. More recently,
Arden and Wolf (2004) used two sizes of optotypes (6.51
and 1.51) to assess colour CS by using a computer graphics
technique along both protan and tritan confusion axes. He
259
assessed better eyes of 24 patients with unilateral AMD or
bilateral early ARM and found that the thresholds for both
sizes of optotypes were raised, but tritan losses were greater
in the smaller optotype and disproportionate to those seen
with the larger optotype. Even patients with minimal
fundal changes had results outside the normal range and
these thresholds varied with the severity of the ARM.
5. ARM, AMD and electrophysiology
Measuring gross electrical potentials provide an objective means of evaluating the functional capacity of a large
number of neurons. The methodology can be manipulated
in order to focus on the anatomical structures most
vulnerable to degenerative changes, such as the interaction
between the RPE, choroid and photoreceptor layer. Much
investigation has centred on the influence of various stages
of ARM on the electroculogram (EOG), the electroretinogram (ERG) and visually evoked potentials (VEPs).
Although notable pathological changes have been reported
in EOG and ERG in patients with AMD (Henkes, 1954;
Arden et al., 1984), other investigators have found no
significant EOG abnormalities in AMD eyes or in the
fellow eyes of AMD patients (Shirao et al., 1997; Marcus
et al., 1983; Holopigian et al., 1997; Sunness et al., 1985;
Sunness and Massof, 1986). Such inconsistent reports in
the literature have resulted in a debate on the value of
electrophysiological tests as diagnostic and prognostic
markers for AMD. Therefore, a more recent study by
Walter et al. (1999) sought to determine systematically
whether there were EOG and ERG changes in patients
with AMD and while doing so, they sought to answer two
important questions as: (1) are there any differences
between age-matched normal controls and AMD using
standardised test protocols? and (2) is the morphological
appearance of AMD related to abnormalities in EOG and
ERG? Sixty-six patients with AMD underwent EOG,
ERG, triple scotopic ERG and fluorescein angiography, 83
normal persons served as age-matched controls for EOG
and 47 for ERG. Both the Ganzfeld EOG and ERG
responses were found to be abnormal in AMD, suggesting
a global impairment of retinal function beyond that
suggested by fundoscopic appearance. Significant EOG
changes suggested that RPE function is also altered while a
significant increase in the light rise (ratio of light peak
portion to dark trough portion of the EOG trace) in
patients with soft drusen led the authors to suggest that this
may prove useful as a marker of risk in the development of
advanced disease. They also showed that both the conedriven and rod-dominated ERG were significantly different
in AMD patients when compared to normal controls, with
both reduced amplitude and prolonged implicit times
suggesting that not only are there fewer cells present but
also that those remaining have a slower synaptic transmission than that in elderly normals. Nonetheless, the absence
of clearly defined normal limits for some of these
parameters, the global nature of the full-field ERG, and
ARTICLE IN PRESS
260
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
the fact that the ERG is usually normal unless a disease
affects 20% or more of the retina limits the sensitivity of
the test, particularly when used in focal lesions such as
those typically seen in AMD.
5.1. Focal ERG (fERG)
The ERG recorded from the fovea was designed to test
for focal disease within the fovea by using a small flickering
spot to elicit a local response (Sandberg et al., 1993).
An early study using this methodology with a procedure
which involved testing temporal frequencies ranging from
10 to 60 Hz showed that besides a general amplitude loss
associated with macular degeneration, there appeared
to be a relative sparing of the mid-temporal frequencies
(Seiple et al., 1986). The value of fERG was further
acknowledged when Fish and Birch (1989) demonstrated
it to have a sensitivity of 87% for distinguishing between
eyes with macular disease and those eyes with other
causes of acuity loss, such as amblyopia, cataract and
optic neuropathy (Fish and Birch, 1989). This was
investigated further by Sandberg et al. (1993), who
measured foveal ERG in the asymptomatic fellow eye of
patients with unilateral nvAMD and compared this to agematched normal eyes. Although the amplitude of the
response was similar between groups, the AMD patients
had delayed implicit times, suggesting that these eyes
had normal numbers of foveal cones but they functioned
abnormally. It is suggested by some that vascular changes
are responsible for the global retinal dysfunction associated
with AMD (Friedman, 1997). Remulla et al. (1995) used
focal cone ERGs to explore this hypothesis by attempting
to establish a link between prolonged choroidal perfusion
in AMD and retinal malfunction. In 67 patients with
AMD, 42% had a choroidal perfusion defect and these
patients had significantly delayed implicit times after
controlling for age, acuity and extent of drusen. Abnormal
oscillatory potentials (OPs) found on the ascending
side of the b-wave in AMD patients also implicate a
vascular mechanism in the pathogenesis of AMD. OPs are
thought to reflect electrical activity in the amacrine cells
and these cells lie in the inner retina, which is nourished by
the retinal circulation. The focal nature of the test
prompted much attention to be focused on clarifying the
relationship between retinal morphology and function.
Falsini et al. (1999) used fERG and graded fundus
photographs and fluorescein angiograms in 25 patients
with bilateral early ARM, compared to 10 age- and gendermatched controls. They found the fERG paralleled
the extent and severity of the fundus lesions, which
were assigned severity stages based on the WARMGS
grading system. It was notable, however, that patients with
early ARM had a reduced amplitude in the fERG
compared with that seen in control eyes, suggesting that
this procedure enabled functional losses to be detected,
which precede the morphological changes, which characterise AMD.
5.2. Multi-focal ERG (mfERG)
The mfERG, which was developed and introduced by
Sutter and Tran (1992), allows retinal activity in the form
of fERGs to be recorded simultaneously from 100 or more
retinal locations over a brief period of time. As the
responses originate mainly from the outer retina with
relatively little contribution from the ganglion cells, much
attention has been focused on its ability to detect and
monitor the various stages of ARM. Attempts have been
made to evaluate both rod- and cone-mediated ERGs by
using this method and although the cellular origins of these
components are still not completely clear, both have
revealed deficits in early ARM (Gerth et al., 2003; Li
et al., 2001; Jurklies et al., 2002; Feigl et al., 2004).
Controversy exists, however, as to the spatial resolution
of the data and its ability to accurately reflect morphological abnormality. Palmowski et al. (1999) performed
mfERG on three patients with AMD and compared
the findings with fundus photography and fluorescein
angiography, and found that mfERG allowed accurate
topographic mapping of focal areas of retinal dysfunction
in all patients tested, including the abnormal changes
detected by fluorescein angiography. Other investigators
have reported poor morphologic-functional relationships
between mfERG and retinal appearance (Gerth et al.,
2003) and only weak-to-moderate statistical correlations
between the greatest linear dimension of the CNV lesion
and mfERG response density (Jurklies et al., 2002).
Despite the apparent lack of correlation, functional
changes in cone-driven pathways evaluated by the mfERG,
indexed by the first-order kernel implicit times have been
shown to occur consistently in patients with early ARM
and in asymptomatic fellow eyes, compared to normal
control eyes (Gerth et al., 2003; Li et al., 2001). Jurklies
et al. (2002) followed four patients with AMD on a
3-monthly basis over a period of 15 months, using mfERG
and concluded that it also has potential as a valuable
tool in the longitudinal monitoring of patients with CNV
in that response densities correlated well with visual
acuity and were reduced within the central 51, which was
the area affected by the CNV. A recent cross-sectional
study of 17 subjects with early ARM and 20 age-matched
normals, which involved a series of psychophysical tests
and fundus photographs as well as mfERG revealed
that the mfERG protocol employed was unable to
discriminate between the ARM and normal groups despite
significant differences between groups being apparent for
CS, high- and low-contrast visual acuity and colour vision
(Feigl et al., 2004). It is evident that this is burgeoning field
of technology and much of the apparently disparate
findings may be clarified as protocols are developed,
guidelines established, and analyses are refined to include
adequate age-related corrections, and in the case of rodmediated mfERGs, adequate lens density correction
factors (Marmor et al., 2003; Feigl et al., 2004; Jackson
et al., 2004).
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
5.3. Visually evoked potentials
VEPs are traditionally used to assess the integrity of the
optic nerve. The cortical magnification of foveal vision,
however, supports the view that the VEP is largely a foveal
phenomenon, particularly if it is recorded using a stimulus
of small check size and small field size. Therefore, eyes with
advanced AMD and low visual acuity may show no
recordable transient or steady-state VEP (Sokol, 1971;
Negishi et al., 2001) and several groups have shown
amplitude attenuation and latency delay of this measure in
eyes with AMD and moderate or good visual acuity
(Sokol, 1971; Celesia and Kaufman, 1985; Negishi et al.,
2001; Lennerstrand, 1982; Junghardt et al., 1995) as well as
in their fellow eye (Marcus et al., 1983).
6. Visual adaptation and ARM
Light adaptation refers to the remarkable ability of the
human eye to rapidly adjust to a large range of light
intensities from intense sunlight to low levels of illumination (Leibrock et al., 1998). Visual transduction involves
the capture of light by the photoreceptors, activation of the
photopigments, followed by their regeneration. These
processes require correctly aligned, structured and functioning photoreceptors, intact post-receptoral pathways, as
well as metabolic support from the surrounding tissues,
such as the RPE, choriocapillaris and Bruch’s membrane.
The integrity of these structures and processes can be
assessed using tests, such as glare recovery, cone and rod
adaptation and flicker sensitivity. Studies have shown that
many of these processes are compromised in the early
stages of ARM.
261
early ARM patients despite good visual acuity (Collins and
Brown, 1989a) and the measured times appear to parallel
the worsening of disease severity in the early stages (Collins
and Brown, 1989a; Sandberg and Gaudio, 1995; Midena
et al., 1997). The value of glare recovery as a prognostic
indicator of severe AMD was investigated by Sandberg
et al. (1998), using a method that flashed letters on a
computer screen in random order before and after a 10 s
bleach. One hundred and twenty-seven patients with
unilateral nvAMD were followed for 412 years, and macular
morphology was also graded based on the number and
type of drusen, presence of focal hyperpigmentation and
the presence and extent of atrophy. They showed that a
slower recovery from glare and the severity of ARM
features were independent risk factors for the development
of a CNV in fellow eyes. These results suggest the test that
reflects cone sensitivity and RPE integrity and has the
potential to be used as a prognostic marker.
Variability in the intensity and duration of the light
stimulus makes it difficult to compare the results from the
various studies. The Eger Macular Stressometer (EMS)
was developed in an attempt to provide a standardised
method applicable in clinical settings as well as a noninvasive screening test for AMD. A pilot study using this
instrument did not find a significant difference in the glarerecovery times between patients with AMD, cataract,
diabetic retinopathy and glaucoma (Schmitt et al., 2001).
However, when the instrument was used to obtain
normative data and to investigate the effect of ARM/
AMD on the photostress recovery time, the EMS displayed
a sensitivity of 29% for ARM and 50% for AMD (Bartlett
et al., 2004a, b).
6.2. Dark adaptation and scotopic sensitivity
6.1. Photostress test
Glare recovery, macular recovery or the photostress test
refers to the technique of assessing the integrity of the
dynamic response of the retina by exposing it to a
controlled glare source and measuring the time course to
the return of sensitivity (Collins and Brown, 1989a) (either
contrast discrimination (Collins and Brown, 1989a, b) or
visual acuity (Schmitt et al., 2001; Bartlett et al., 2004a;
Midena et al., 1997; Sandberg and Gaudio, 1995; Sandberg
et al., 1998)). It has traditionally been used as a tool to
differentiate macular disease from optic neuropathy and
early studies investigating a variety of retinal diseases
reported prolonged recovery times in ARM patients
(Glaser et al., 1977). One study investigating visual
function and prognosis in patients with bilateral drusen
found a poor correlation between photostress results, and
visual acuity or drusen severity (Smiddy and Fine, 1984).
Others, however, have reported significant correlations
with clinical measures of vision, such as visual acuity,
colour vision, contrast threshold and subjects’ subjective
complaints (Collins and Brown, 1989a, b). Studies have
also shown substantial delays in glare-recovery time in
Dark adaptation refers to the recovery of visual
sensitivity in darkness, following exposure of the eye to
intense illumination, which bleaches the photopigment
rhodopsin. The classical bi-phasic curve is obtained after
almost total bleach and contains an initial phase, which
reflects cone function and the slower component, which
occurs when rod threshold drops below cone threshold
(Leibrock et al., 1998) (Fig. 2).
Although age-related increases in the time constant of
rod-mediated dark adaptation and scotopic sensitivity have
been reported (Jackson et al., 1999), numerous psychophysical studies have shown these to occur to a significantly
greater extent in those with early ARM (Owsley et al.,
2000, 2001; Steinmetz et al., 1993; Haimovici et al., 2002;
Brown and Lovie-Kitchin, 1983; Eisner et al., 1987; Sturr
et al., 1997) (Fig. 3).
These findings are in accord with histopathological
observations that rods are lost earlier than cones in both
ageing and early AMD (Curcio et al., 1993, 2000). It is
interesting to note that studies have shown deficits in dark
adaptation are not always correlated with scotopic
sensitivity, suggesting that the mechanisms underlying
ARTICLE IN PRESS
262
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
Agematched
Normals
8
Cones
7
Rod-Cone Break
20
6
No. of ARM patients
Log intensity (!!L)
Mean
Median
Early and late ARM
Rods
5
4
3
Abnormal (48% of patients)
(mean –2SD)
15
10
5
55 52 49 46 43 40 37 34 31 28 25 22
2
0
5
10
15
20
Time in dark (min)
25
30
Fig. 2. Dark-adaptation curve. Adapted from web-vision (http://webvision.med.utah.edu/light_dark.html#dark) with permission. The shaded
area represents 80% of the group of subjects. Hecht and Mandelbaum’s
data from Perenne M.H. (1962). Dark adaptation and night vision. In:
Davidson (Ed.), The Eye, vol. 12. London Academic Press (Chapter 5).
these parameters are not the same (Jackson and Owsley,
2000); therefore, a patient with early AMD may have
normal scotopic sensitivity but abnormal dark adaptation,
the reverse scenario, however, is uncommon.
A common complaint made by the most ARM patients
is that they experience difficulty when transiting from a
bright to a dark environment. In exploring this observation, several groups have shown good correlations between
subjective complaints and tests of scotopic threshold and
dark-adaptation kinetics (Brown and Lovie-Kitchin, 1983;
Steinmetz et al., 1993). Measurement of the dark-adaptation time constant was incorporated into a battery of tests
by Eisner et al. (1992) in their longitudinal study of eyes
whose fellow eyes had nvAMD (Group 1) and an agematched control group (normals+bilateral early ARM).
The initial cross-sectional analysis found that eyes with the
most drusen and/or atrophic change were the ones with the
slowest rates of sensitivity recovery during dark adaptation
(Eisner et al., 1987,1991). The subsequent longitudinal
analysis of 47 patients after 18 months follow-up found
that the dark-adaptation time constant together with
colour-match area effect was positively correlated and also
provided the best predictor for the development of a
neovascular lesion (Eisner et al., 1992).
The nature of these tests is such that they should be
particularly sensitive at evaluating those eyes with substantial RPE disturbance, i.e., multiple drusen, pigment
irregularities, RPE detachments and choroidal perfusion
defects. It is recognised that CNV can occur in the absence
of these defects and, therefore, Haimovici et al. (2002)
postulated that dark adaptation would be significantly
worse in the fellow eyes of patients with pigment epithelial
detachments and tears of the retinal pigment epithelium,
compared to the fellow eyes of patients with just CNV or
19 16 13
Mean Field dark-adapted sensitivity (dB,lens corrected)
Fig. 3. Frequency histogram of mean field (central 191 radius visual field)
dark-adapted sensitivity in patients with early ARM. Box plots above the
histogram compare the distribution of ARM patients to a group of agematched subjects with good retinal health. Box represents 25th and 75th
percentile and whiskers, 10th and 90th percentile. Solid line within the box
is the median and the filled symbols, the mean. Vertical line in the
histogram represents the lower normal limit (mean#2.5 SD). Investigative
ophthalmology and vision science by Owsley et al., Copyright 2000 by
Investigative Ophthalmology and Visual Science. Reproduced with
permission of Investigative Ophthalmology and Visual Science in the
format journal via Copyright Clearance Centre.
just drusen. Although the differences that were noted
between the groups were in the direction expected, they did
not reach statistical significance due to the small sample
size. Therefore, this area merits further investigation and
the authors’ recommend using a more rigorous classification of CNV sub-type and increasing the sample sizes.
6.3. Cone adaptation
Cone dysfunction in the early stages of AMD was
initially identified by Brown and Lovie-Kitchin (1983)
while undertaking experiments that were designed primarily to test rod threshold. Cone thresholds were shown to be
elevated in early AMD despite the eyes having good visual
acuity. In further work, Brown et al. (1986) measured cone
adaptation at 51, 101, 201 and 401 eccentricity, using
incremental thresholds in six patients with early AMD
(drusen and pigmentary irregularities) and an unspecified
number of age-matched controls. Elevated cone thresholds
were found in ARM patients in the central and peripheral
retina when compared to the age-matched controls.
Surprisingly, time constants for photopigment recovery
appeared unaffected. This study provided evidence that the
functional consequences of early ARM are not limited to
the macula. In an effort to compare static and kinetic
aspects of cone function, Phipps et al. (2003) tested various
aspects of cone function, using spatial and temporal CS,
colour thresholds and light- and dark-adaptation dynamics. In all cases, contrast thresholds were measured in
order to minimise the effect of pre-retinal absorption in the
ARTICLE IN PRESS
263
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
ageing eye. In the high-risk patients (good acuity but either
multiple soft drusen bilaterally with or without pigmentary
changes, or unilateral soft and a CNV in the other eye),
44% had abnormal cone steady-state thresholds. The
constant of cone adaptational recovery was the single most
affected parameter in most patients with ARM (69%) and
this was found to be a more sensitive discriminator than
steady-state thresholds. The time constant did not correlate
significantly with steady-state functions (photopic, spatiotemporal and colour) and, therefore, appears to identify a
unique aspect of visual function in ARM that is not covered
by the other tests. These functional deficits are thought to
involve a slowing of cone photopigment regeneration in
both ageing and disease. Possible causes for these functional
deficits that occur in ARM eyes include morphological
alterations in Bruch’s membrane and RPE, which would
slow the recycling of visual photopigments (Leibrock et al.,
1998; Pianta and Kalloniatis, 2000), misalignment of the
cone’s outer segments resulting in a lower optical density of
photopigment and reduced quantal catch by the photopigment (Eisner et al., 1992; Elsner et al., 2002).
6.4. Flicker sensitivity
Flicker sensitivity is a useful marker of retinal integrity.
The detection of flicker of a spectral light on a bright white
background is mediated by both the opponent or chromatic
system for low alteration rates and by the luminance or
non-opponent system for high alteration rates (Applegate
et al., 1987; Mayer et al., 1994). It may also be able to detect
metabolic compromise of the outer retina better than a
static stimulus because of the increased metabolic demand
needed to detect flicker (Anderson and Vingrys, 2001;
Phipps et al., 2004). Investigators commonly use two
different types of flickering stimuli, which are drawn
schematically in Fig. 4 (Anderson and Vingrys, 2000):
1. Mean-modulated flicker: Modulating a stimulus about a
mean background level in order that there is no change
in the time-averaged luminance (Mayer et al., 1994).
2. Pedestal flicker: This involves modulating a stimulus
concurrent with a light increment. This results in both a
flickering component and an increase in time-averaged
luminance above background level. Detection thresholds are increased by the low-frequency luminous
pedestal created for the stimulus duration, by invoking
local adaptation and contrast-dependent masking effects
or rod–cone and cone–cone interactions from surrounding regions. A loss suggests adaptational abnormalities,
which have been reported previously in ARM patients
(Phipps et al., 2003; Owsley et al., 2001).
The loss of sensitivity for medium temporal frequencies,
in patients with early ARM, but good visual acuity, was
first proposed by Brown and Lovie-Kitchin (1987b). Using
the classification of ARM based on visual acuity as well as
morphology, they found that the ARM (VA46/6) patients
Luminance-Pedestal Flicker
Mean-Modulated Flicker
L
B
P
L
Time
B
Time
B Background Luminance
L Luminance
Time averaged Luminance
P Luminance Pedestal
Fig. 4. Diagram illustrating the differences between mean-modulated
flicker and luminance-pedestal flicker. Adapted from Anderson and
Vingrys (2000), used with permission.
possessed a significant depression of the temporal contrastfunction across a wide range of frequencies whereas the
pre-ARM (VAo6/6) showed similar results to the normal
control group except for mid-temporal frequencies. A
subsequent study suggested that the processes responsible
for temporal summation spared in ARM in contrast to
those mediating temporal discrimination (Brown and
Lovie-Kitchin, 1989). A study principally investigating
two-increment colour thresholds in ARM revealed that the
ability to detect 25 Hz flicker was significantly depressed in
a group of ARM patients group when compared to the
elderly control subjects despite these patients having
normal L-cone increment thresholds (Haegerstrom-Portnoy and Brown, 1989). Whether a loss of flicker sensitivity
reflects retinal or post-receptoral damage has stimulated
much debate. It is thought that the luminosity channel
involved in flicker detection receives a summed input from
both medium (M) and long (L) wavelength receptors with
the long-wavelength receptors predominating by a ratio of
around 2:1. Therefore, Haegerstrom-Portnoy and Brown
(1989) postulated that the change of 0.3 Log unit in M-cone
sensitivity noted in the study yet no significant change in
L-cone sensitivity, would have only produced minor
changes in the flicker sensitivity if the loss had occurred
at the receptoral level. They, therefore, proposed the
alternative hypothesis that a post-receptoral channel for
detecting flicker may be affected by the disease, as this was
also suggested by Applegate et al. (1987), who noted that
flicker sensitivity was depressed by 0.5 Log units in the nonneovascular eye of an ARM patient with L–M-cone
sensitivities remaining normal.
6.5. Cone flicker sensitivity
Recently, Falsini et al. (2000) used focal electrogram
modulation sensitivity to evaluate retinal cone flicker
sensitivity. Focally recorded electroretinography is thought
ARTICLE IN PRESS
264
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
to reflect the activity of cone photoreceptors and bipolar
cells and, therefore, provides a functional index of the
outer retina. The investigators reasoned that the assessment of outer retinal sensitivity using this method might
help to evaluate early cone dysfunction in ARM. They
undertook a cross-sectional study in which fERGs as a
function of sinusoidal flicker modulation was recorded in
patients with early ARM and in age-matched control
subjects. Response gain losses and modulation depthdependent phase delays, with normal thresholds, were
associated with early lesions. It is thought that these may
result from early degenerative changes of cone photoreceptors whose numbers at this stage may be normal or
near normal. Retinal gain may be affected by both
shortening of cone outer segments, thereby reducing
quantum catch and the effective retinal intensity of
the stimulus, as well as by the alteration of photoreceptor
membrane properties (time constants) by delaying reestablishment of equilibrium. Increased thresholds, in addition
to gain and phase abnormalities, were found in more
advanced lesions, which suggest more widespread disease.
The investigators also found that the temporal characteristics of foveal cone photoreceptors are altered in AMD.
The possibility that the changes in temporal characteristics of the retina may be associated with early metabolic
changes in the choriocapillaris and Bruch’s membrane was
proposed by Anderson and Vingrys (2001) and Phipps
et al. (2004). This impairment, which is thought to occur
early in AMD, should therefore be more readily detected
by a flickering stimulus than by a static one. They chose to
use a pedestal flicker as it has been shown to be robust to
the effects of both blur and pre-retinal absorption, which is
particularly important when testing an elderly population.
It also exposes rod–cone interactions and, therefore, may
allow detection of early rod dysfunction as well as
providing a good indication of local adaptation and
temporal sensitivity changes (Anderson and Vingrys,
2001; Phipps et al., 2004). Individuals with early AMD
were compared with control subjects of a similar age, using
both static and flicker perimetry. The use of flickering
targets resulted in larger and deeper visual field deficits
than static targets, and the investigators postulate that the
selective loss to flickering targets may be seen earlier in the
disease process and perhaps act as a better prognostic
indicator. It has been suggested that the increase in local
metabolic demand and thus retinal blood flow required by
a flickering stimulus may be hindered by the pathological
changes that occur in the RPE, choriocapillaris and
Bruch’s membrane in the early stages of AMD (Van Toi
and Riva, 1994; Kiryu et al., 1995).
6.6. Flicker sensitivity and progression to AMD
A series of studies by Mayer et al. (1992a–c, 1994, 1995)
provided valuable insights both into the visual mechanisms
underlying flicker sensitivity and its value as a method for
detecting and monitoring progression in ARM. They
measured sensitivity as a function of flicker rate in eyes
at risk for AMD (‘‘good’’ eye of patients with unilateral
AMD) and age-matched healthy older eyes. ARM eyes
were less sensitive overall to flicker than healthy older eyes,
especially at mid-temporal frequencies. Eyes with ARM
features were significantly less sensitive to frequencies
between 10 and 28 Hz when compared with the healthy
older group (Mayer et al., 1992a). In a second paper, they
used stepwise discriminant analysis to classify ARM-risk
eyes from healthy older eyes with 78% accuracy based on
foveal flicker sensitivity at the two most affected midtemporal frequencies, 10 and 14 Hz (in order of estimated
weight) (Mayer et al., 1992b). Preliminary data suggested
that sensitivity at these temporal frequencies may also
predict which eyes would develop nvAMD (Mayer et al.,
1992c). They tested their hypothesis using follow-up data
collected over a 4-year period at which point seven of the
initial group of 13 patients had converted to nvAMD. By
comparing the baseline characteristics of foveal flicker
sensitivity along with the fundus appearance of eyes with
ARM but without CNV, with the healthy, age-matched
eyes, the investigators showed that a linear combination of
flicker determined at 5 and 10 Hz could discriminate
between eyes that went on to develop nvAMD from those
that did not, with an accuracy of 100%. Despite a similar
fundus appearance, eyes without nvAMD and nonconverted eyes had very different outcomes weakening
the prognostic value of fundus grading. Thus, the
researchers concluded that neovascular changes might
occur in the absence of RPE abnormalities. Mayer et al.
(1992c) proposed a variety of causes for the loss of
temporal CS. They felt that it was unlikely to be due to a
decrease in photoreceptors as when the groups were
restricted to subjects with acuities better than 20/25, the
differences in sensitivity still remained. Furthermore,
spatial blurring of up to four dioptres of the flicker test
had no effect on flicker sensitivity. They then considered
the temporal CS curve as a de Lange function (an envelope
that describes the combined response profile of the
mechanisms whose individual response spectra are overlapping). Within the context of this multi-channel temporal
processing model, the mid-temporal frequency losses
reported in this study could be attributed to reduction in
sensitivity in a ‘‘high-temporal frequency’’ mechanism
(Mayer et al., 1995). Given that the magnocellular pathway
is believed to be principally responsible for high-temporal
and low spatial frequency vision, the authors suggested
that it may be particularly susceptible to changes in the
early stages of ARM. However, most eyes with late AMD
continue to maintain low spatial frequency CS and this is
not in accord with an early dysfunction of the magnocellular pathway.
7. Central visual field sensitivity and ARM
Central field defects have been reported in the eyes of
patients exhibiting features of early ARM, with the defect
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
microperimetry and anatomic abnormalities in patients
with sub-foveal neovascularisation. They superimposed
SLO microperimetry on colour fundus photographs and
fluorescein angiograms of 21 eyes with sub-foveal neovascular membranes secondary to AMD (14 eyes) and POHS
(7 eyes). They found that the relative risk of an absolute
scotoma is highest over areas of chorioretinal scars
(RR ¼ 107.61), RPE atrophy (RR ¼ 9.97), sub-retinal
haemorrhage (RR ¼ 2.88) and the neovascular membrane
(RR ¼ 1.86). Schneider et al. (1996) combined SLO
microperimetry with simultaneous Indocyanine Green
angiography and noted that the depth of the CNV
correlated with both duration of symptoms (Fig. 5) and
the size and type of CNV with well-defined CNV producing
significantly deeper scotomata than eyes with occult CNV.
Clinically, these findings emphasise the necessity of prompt
referral and treatment with the aim of keeping the
associated scotoma as small as possible.
The application of SLO in monitoring visual function in
longitudinal studies has provided crucial insights into the
natural history of vision loss. Sunness et al. (1997)
undertook a longitudinal study of the visual function
abnormalities and prognosis in eyes with GA. They found
that areas of GA are associated with absolute scotomas
and that GA tends to spare the foveal centre until late in
the disease, providing further evidence of the limitation of
visual acuity at reflecting visual function.
The sequence of events in AMD, which leads to loss of
visual function was investigated by Fujii et al. (2003), using
the SLO in 175 eyes with CNV. In addition, 15 patients
who elected not to have any treatment for CNV were also
kept under observation with SLO testing every 3 months
for up to 18 months after the onset of visual symptoms.
Visual impairment in eyes with sub-foveal CNV secondary
to AMD was seen to be associated with decreased fixation
stability, loss of central fixation and impaired retinal
sensitivity. Thus, the authors postulate that the sequence
of events consists of an initial mild decrease in central
Depth of Scotoma (dB)
most commonly located in the parafovea (Swann and
Lovie-Kitchin, 1991; Cheng and Vingrys, 1993; Midena et
al., 1994, 1997; Hart and Burde, 1983). In contrast to these
findings, Atchison et al. (1990) using the Humphrey field
analyser found no significant differences between eyes with
early ARM (ophthalmoscopically visible hard drusen and/
or fine pigmentary stippling or depigmentation with a
Snellen visual acuity of 6/6 or better) and the eyes of 15
age-matched normal controls. Similarly, Midena et al.
(1994) examined the relationship between severity of ARM
changes and central visual field sensitivity. Although mean
sensitivity did not correlate with the number of drusen,
presence of focal hyperpigmentation or RPE atrophy, it
was significantly decreased in eyes with confluent drusen.
On the other hand, Tolentino et al. (1994) concluded that
drusen had little effect on the central visual field whereas
the deficits in sensitivity were correlated with RPE
attenuation or atrophy.
The lack of consistency in the evidence may be a
reflection of the limited ability of both kinetic and static
perimetry to accurately measure macular function as they
assume stable foveal fixation, which is rarely present in
AMD (Sunness, 1999). Many of these limitations are
overcome by the use of microperimetry through SLO.
Compared to traditional perimetry, the SLO offers many
advantages such as real time ophthalmoscopic imaging,
which allows fixation control with correction for eye
movements, an accurate determination of preferential
fixation location and point-to-point correlation of fundus
pathology and related functional deficits (Sunness et al.,
1995).
By using a fundus camera stimulator, it was demonstrated that the retinal sensitivity over drusen and nondrusen areas was not significantly different, a finding that
was in accord with those obtained on static perimetry
(Sunness et al., 1988). Nonetheless, a more recent study has
questioned these findings and shown a decrease in
sensitivity in retina overlying drusen (Takamine et al.,
1998). In this study, more than half of the retinal areas with
underlying drusen, which were sampled, showed decreases
in sensitivity. The decrease was only noted over large
drusen (amorphous substance with a clear border) as
opposed to soft drusen (amorphous substance with an
indistinct border); however, no relationship was found
between drusen size and the amount by which retinal
sensitivity was decreased, implying that small differences in
the degree of separation between the RPE and choriocapillaris do not influence retinal function. The incongruity
between these results and those of Sunness et al. (1988) was
attributed by the authors to the better instrumentation,
which allowed them to delineate the margins of the retinal
areas overlying the drusen and to undertake selective
stimulation of these areas without a contribution from the
surrounding normal retina.
The impact to visual function of the various morphological features of late AMD has also been investigated.
Tezel et al. (1996) explored the relationship between SLO
265
22
20
18
16
14
12
10
8
6
4
2
0
0
5 10 15 20 25 30 35 40 45 50 55 60 65
Symptom Duration (weeks)
70 75 80
Fig. 5. Relationship between the depth of the scotoma measured using
SLO microperimetry and the duration of symptoms. Taken from
Schneider et al. (1996), used with permission.
ARTICLE IN PRESS
266
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
retinal sensitivity and visual acuity, which is followed by a
progressive increase in fixation instability and ultimately,
the development of an absolute central scotoma with
eccentric fixation. Once again the necessity of prompt
treatment is reinforced because in the sub-group of patients
with symptoms for 3 months or less, 89% had predominantly central fixation and 58% had stable fixation
suggesting the presence of viable photoreceptors. In this
sample, considerable functional variability was observed
among lesions occupying a similar area and thus implying
that inferences on retinal viability should not be made
based solely on lesion size.
SLO microperimetry has also proved useful in the
monitoring of response to new treatment modalities.
Schmidt-Erfurth et al. (2004) used SLO perimetry to
document the size of absolute and relative scotomas during
a single centre double-masked study of verteporfin therapy
in 46 consecutive patients with sub-foveal CNV. Thirtythree patients received verteporfin and 13 received placebo
and all underwent SLO at 3-monthly intervals over the 2year follow-up time. Statistical analysis showed that the
mean absolute and relative scotoma sizes were significantly
smaller in the verteporfin group than that in the placebo
group, at all points beyond 6 months after baseline. These
findings have important implications for reading ability
and visual rehabilitation.
8. Indices of metamorphopsia and ARM
Distortion or metamorphopsia is one of the earliest
symptoms reported by patients at the onset of neovascular
macular disease. Therefore, there has been considerable
interest in the development of methods to identify and
quantify distortion.
8.1. Amsler charts
In 1947, a simple grid of squares known as the Amsler
charts were printed and proposed as a screening test for
macular disease (Marmor, 2000). They have traditionally
been used as a screening test for diagnosis of nvAMD;
however, most studies have found poor specificity and
sensitivity, and its usefulness for this purpose has been
questioned (Zaidi et al., 2004; Schuchard, 1993). Amsler
charts have the obvious disadvantage of providing a suprathreshold stimulus that is insensitive for the detection of
relative scotomas and depressed retinal sensitivity (Wall
and May, 1987). An improvement to the Amsler was
proposed by Wall and May (1987), who used crosspolarised filters to vary the luminance to a threshold level
where even a small drop in retinal sensitivity could be
measured. This modification yielded a six-fold increase in
scotoma detection over standard testing. As it involves a
change in luminance levels, Wall’s method was found to
yield inconsistent results (Cheng and Vingrys, 1993) if a
period of dark adaptation is not built into the test protocol.
Recently, a computerised automated version of the
Amsler has been developed which incorporates resolution
and retinal CS to produce a 3-D map of the central visual
field to reveal the shape, location, extent, slope and depth
of the retinal deficit at a resolution of 11 (Fink and Sadun,
2004). This test may have potential as a screening tool in
macular disease.
8.2. Preferential hyperacuity perimeter (PHP)
The PHP is another screening device that has recently
become commercially available (Lowenstein et al., 2003). It
exploits the high sensitivity of hyperacuity to detect very
early retinal elevations. Hyperacuity may be defined as the
ability to discern misalignment of objects at the fovea and
is about 10 times higher than resolution acuity. Hyperacuity also has the advantages of being much more robust to
optical blur and age-related decline than other measures of
acuity (Lakshminarayanan and Enoch, 1995). The test
involves a dotted line flashed on a computer screen, and
any perceived distortion or scotoma is recorded and
analysed. A macular map is obtained with quantitative
values of the area and intensity of the metamorphopsia.
Initial validation studies showed that the PHP was better
than the Amsler grid at detecting AMD-related lesions and
that it may be able to differentiate between intermediate
ARM (the presence of large drusen) and incipient CNV,
and thus may be beneficial for monitoring progression
from early ARM to late AMD.
8.3. Shape-discrimination charts
The recently developed shape-discrimination charts may
also prove useful in detecting and monitoring macular
disease (Wang et al., 2002). These require patients to
identify a deformed circle from a group of perfect circles;
this also represents a form of hyperacuity (Fig. 6).
Viewing of the test target results in integration across a
wide retinal area and consequently may be more sensitive
than visual acuity to irregular sampling or under sampling
by the photoreceptors, especially when patients have
parafoveal or paracentral visual defects common in early
ARM. It also has the advantage that patients are unable to
achieve artificially good results by using visual search as
they would need to locate a large enough healthy area to
process the whole stimulus. In a computerised version of
the test, 97% of early ARM patients showed a significant
elevation in threshold in comparison with normal older
volunteers.
9. Self-reported visual functioning and ARM
Within a clinical setting, it is often evident that
performance on conventional tests of vision such as Snellen
acuity is at variance with the patient’s perception of their
visual disability. To better understand these relationships,
a number of quality of life (QOL) instruments have been
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
267
Fig. 6. Examples of test targets used in the shape-discrimination charts: (a) a radial frequency pattern without radial modulation and (b) a radial
frequency pattern with 4% of radial modulation with a radial frequency of 8 cyc/2p. Investigative Ophthalmology and Visual Science by Zi-Zhong Wang
et al., Copyright 2002 by Investigative Ophthalmology and Visual Science. Reproduced with permission of Investigative Ophthalmology and Visual
Science in the format Journal via Copyright Clearance Centre.
devised, which provide a semi-quantitative measure of selfreported health and visual functioning.
9.1. Evaluation of QOL
QOL encompasses four dimensions as: a physical
dimension (disease symptoms and their treatment), a
functional dimension (self-care, mobility, activity level
and activities of daily living), a social dimension (social
contact and interpersonal relationships) and a psychological dimension (cognitive function, emotional status, wellbeing, satisfaction and happiness) (Aaronson, 1988; de
Boer et al., 2004). Questionnaires or instruments can be
disease specific or generic. A keen interest in this area has
led to the proliferation of instruments making it difficult to
both to compare outcomes and for researchers in the
choice of an appropriate outcome measure. Several helpful
reviews of vision-related questionnaires have been published (Massof and Rubin, 2001; Margolis et al., 2002; de
Boer et al., 2004). de Boer et al. provided a systematic
review of 31 vision-related QOL questionnaires, which they
rated on their psychometric quality using a pre-defined
rating list. They also emphasised the advantage of applying
Rasch theory to aid analysis and interpretation of data.
The majority of questionnaires on vision have been
developed for use in patients with cataract, although other
disease-specific questionnaires exist for AMD, retinitis
pigmentosa, glaucoma, ocular melanoma, cytomegalovirus
and Graves ophthalmopathy. Although some instruments
were initially developed to assess the impact of visual
impairment due to cataract, and the alleviation of
symptoms by surgery (VF-14 and activities of daily vision
scale (ADVS)) their validity as a tool in the measurements
of functional impairment in retinal diseases has been
demonstrated (Linder et al., 1999; Mangione et al., 1999).
9.2. Relationship between self-reported difficulties and
clinical tests of vision
Various studies have attempted to identify those aspects
of visual functioning which correlate with different
objective clinical tests. Thus, e.g., the relationships between
measured visual acuity, CS and visual field have been
correlated with the scores obtained on self-reported
questionnaires (Carta et al., 1998; Rubin et al., 2001).
Rubin et al. found that measured stereoacuity and glare
exhibited weak correlations with self-reported difficulty
with everyday tasks. Interestingly, each of these measures
was significantly associated with the questionnaire scores
independently suggesting that reduction in visual functioning along several dimensions contributes to the difficulty
experienced in the undertaking of daily living tasks. Other
studies have attempted to identify which daily living tasks
are represented by which clinical measure of vision. Hazel
et al. (2000) found that low-contrast visual acuity and CS
account for most of the variance (83%) reading performance whereas binocular text-reading speed provided the
best indicator of overall visual function. They highlighted
the fact that discrepancies often exist between self-reported
visual performance and measured reading speed, which
they suggested, was because spot-reading tasks are
considerably more important to patients with low vision,
so visual resolution is more important than fluency.
McClure et al. (2000) used a QOL instrument constructed
and validated specifically for patients with AMD (the daily
living tasks dependent on vision DLTV) with the ability to
discriminate between AMD sufferers, cataract sufferers
and those with no history of visual problems. Reading
index (a novel derivative of reading speed) and DVA
showed the strongest correlations with tasks such as
reading correspondence and newspapers, ability to sign
documents, detect facial features across a room and
ARTICLE IN PRESS
268
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
identify cash, emphasising the important role the resolution
plays in the performance of many daily tasks.
It would be expected that habitual acuity would correlate
more closely than best-corrected acuity with self-reported
visual function. However, a recent report has questioned
this assumption and shown that best-corrected acuity was a
better predictor of self-rated health than habitual acuity
(Wang et al., 2000). Scilley et al. (2002) observed that even
in the early stages of ARM when eyes have good acuity
patients are more likely to experience difficulty in nightdriving, near-vision activities and glare disability as
compared to normal controls. In particular, the most
frequently reported difficulty in the early stages of the
disease is difficulty with night driving, a low-luminance
task. Difficulty with night driving was also related to
scotopic sensitivity, which supports the hypothesis that rod
photoreceptor dysfunction occurs early in the disease
process. The profound impact of bilateral severe AMD
on vision-related QOL has recently been demonstrated in a
group of patients by using the National Eye Institute
Visual Function Questionnaire (Cahill et al., 2005); QOL is
significantly worse in these patients than that in patients of
varying AMD severity and in persons without ocular
disease. The study also highlighted the more important
NEI-VFQ-25 sub-scales, such as general vision, difficulty
with distance tasks and difficulty with near-task sub-scales
as these proved sensitive to different levels of VA. A higher
level of anxiety concerning vision was also noted when
compared with a low-vision group who would have had
longer to adapt and come to terms with their vision loss.
This is in accordance with several studies, which have
highlighted the significant emotional distress and prevalence of syndromal depression associated with the disease
(Williams et al., 1998; Brody et al., 2001; Rovner et al.,
2002), and the fact that both clinicians and community
members often underrate the impact of this disease on
health-related QOL (Stein et al., 2003).
The ability of various instruments to detect clinical
changes has also been investigated. The summary score
from the ADVS instrument and the domain scores relating
to daytime driving, near vision and glare disability were
found to correlate significantly with ARM severity by
Mangione et al. (1999). However, after adjustment of the
models for visual acuity, morphological severity was not an
independent correlate of reported difficulty with common
visual tasks. This was also found to be the case in a study
using VF-14 scale; however, when the population was
restricted to those with 20/20 vision in the better eye, AMD
severity was found to be an independently significant
predictor of the VF-14 score after adjusting for visual
acuity in the worse eye (Mackenzie et al., 2002).
10. Bilateral late AMD impact on visual function
In normal subjects, the old adage that ‘‘two are better
than one’’ appears true. There is a 40–50% improvement in
grating CS with a 7–8% increase in the high-frequency cut-
off when stimuli are viewed binocularly (Campbell and
Green, 1965; Legge, 1984; Zlatkova et al., 2001), with the
greatest summation occurring under conditions of reduced
illuminance (Home, 1978). Faubert and Overbury (2000)
first reported the phenomenon of contrast inhibition when
AMD patients view stimuli binocularly. The investigators
tested a group of 59 subjects, 49 of whom had AMD and 10
normal participants of similar age range. Almost half of the
subjects with AMD had worse spatial CS when recordings
were made from both eyes simultaneously when compared
with the peak contrast achieved when stimuli were viewed
with one eye only. This binocular inhibition was not related
to the CS of the better eye or to acuity. The inhibition
effect occurred mainly in the medium and lower spatial
frequencies that are generally related to tasks, such as
orientation and mobility. Valberg and Fosse (2002)
confirmed these findings. They used a group of 13 AMD
patients with unequal acuities, and again showed that
many subjects had a better monocular than binocular
contrast function, indicating inhibition of CS in the better
eye. This may be due to the stimulation of noncorresponding retinal areas for binocular viewing. On the
other hand, this inhibitory effect is not a feature of
resolution. In a study of 2520 subjects over the age of 65
(Rubin et al., 2000), a small binocular summation of
approximately 0.03 Log MAR units of DVA was found in
those subjects with less than a one-line acuity difference
between eyes, which the authors conceded was of doubtful
clinical significance. Interestingly, binocular distance acuity
was shown to be able to be predicted with reasonable
accuracy (less than a one-letter difference) from the
monocular acuity in the better eye.
Doris et al. (2001) examined the relationships between
clinical measures of vision and macular pathology, and
found that these were more strongly correlated when the
study eye was the worse eye. They observed that when not
completely depended upon, visual function in that eye (the
worse eye) is more closely correlated with the pathology
observed in the macula. Whereas when the study eye was
the better eye, the relation was less clear, possibly owing to
interplay of psychophysical factors, such as retinal reserve.
Perceptual filling-in is another visual phenomenon that has
been shown to occur principally in patients with bilateral
scotomas. Cohen et al. (2003) used scotometry to delineate
the anatomic edges of the lesion in patients with unilateral
and bilateral central scotomas, as well as the perceived
scotoma. They found that the perceptual filling-in phenomenon was more likely to occur in the eye with the
smaller lesion.
Longitudinal studies have made some interesting observation on the impact to visual function of a patient
developing bilateral disease. An improvement in visual
acuity in the eye with the primary AMD lesion has been
noted to occur in the event of vision loss in the betterseeing eye; this is thought to be due to an improvement in
fixation in the worse-seeing eye (Sunness et al., 2000). A
similar trend has been noted in patients with a history of
Average follow-up
4.3 years
18 months
45 months
4.5 years
1.5–4 years
Study
Smiddy and Fine (1984)
Eisner et al. (1992)
Sunness et al. (1989)
Sandberg (1998)
Mayer et al. (1994)
20 normals
16 (unilateral nvAMD)
127 (unilateral nvAMD)
18 (unilateral nvAMD), 7
(bilateral ARM)
47 (unilateral nvAMD)
71 (bilateral drusen)
No. subjects enrolled
7 with unilateral nvAMD
converted to bilateral
nvAMD
27 developed nvAMD
(8.8%/year)
3 PED
1 GA
1 eye nvAMD
11 eyes (16.5%/year)
8 eyes in 7 patients
No. subjects progressed to
neovascular AMD
Table 3
Longitudinal studies investigating visual function parameters which may predict neovascular AMD development
Foveal flicker sensitivity
Macular visual field
Glare-recovery time
Foveal ERG amplitude
and implicit time
DVA
Foveal dark-adapted
sensitivity
Rayleigh colour matching
D-15
Fundus appearance could not
discriminate ARM from prenvAMD eyes
Flicker sensitivity at 5 and 10 Hz
predicted converting eyes from
non-converting and healthy older
eyes with 100% accuracy
Time to CNVM development was
inversely related to
FERG implicit time
Independent risk factors for CNV
development were slow glare
recovery and extent of
fundoscopic changes
High-risk drusen characteristics
predicted development with 100%
sensitivity and 55% specificity
Foveal dark-adapted sensitivity
predicted development of
advanced AMD with 100%
sensitivity and 92% specificity
Summed drusen and atrophic area
also good
s-Cones good at distinguishing
outcome groups
Absolute sensitivity
Dark adaptation
Flicker sensitivity
Strong correlation for dark
adaptation time and colour-match
area effect
No correlation with photostress
Results
s-Cone sensitivity
Visual acuity photostress
test
Visual function parameters
measured
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
269
ARTICLE IN PRESS
270
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
amblyopia, with apparent recovery of visual function in the
amblyopic eye over a period of time after the previously
normal eye develops visual loss due to advanced AMD (El
Mallah et al., 2000).
These studies suggest that the functional status of the
fellow eye is an important factor that should be taken into
consideration. This has important implications for controlled clinical trials that employ change in visual acuity in
the study eye as a primary outcome measure.
11. Predictive markers of nvAMD
Table 3 summarises the longitudinal studies investigating
functional risk factors for the development of nvAMD.
Despite substantial variety in follow-up time, patient
characteristics and AMD classification, the functional
deficits consistently noted to predict conversion to nvAMD
appear to be a combination of s-cone sensitivity, flicker
sensitivity and dark-adapted sensitivity and glare recovery.
Larger-scale studies are required to substantiate these
findings, with particular attention to AMD classification
and the sub-type of the CNV, which may subsequently
develop. Such markers of risk could have considerable
value when designing controlled clinical trials of prevention
or when longitudinal follow-up is occurring as part of
therapeutic trials in subjects with unilateral AMD.
12. Summary and future directions
This review has highlighted the various functional
consequences of the alteration in retinal architecture that
occurs in early and late ARM (Table 4).
The early detection of nvAMD is becoming increasingly
important as new treatments continue to emerge, which are
able to minimise disease progression with the potential to
arrest visual decline (Comer et al., 2004). To date, there has
been a heavy reliance on DVA and it has been used as the
outcome measure in both therapeutic, as well as prevention
trials. As DVA is insensitive to subtle changes in vision and
is a poor marker for progression, rapid, reliable and simple
psychophysical methods of monitoring progression from
early ARM to AMD are needed. Ideally, the tests would be
robust to physiological age-related decline of visual
function as well as functional impairment due to medial
opacities and other co-existing pathology. Reliable screening tests are also required, and should be inexpensive and
easy to perform to facilitate self-monitoring at home.
While a plethora of studies have investigated visual
function and dysfunction in early ARM, many of the study
samples were not well defined. Recent improvements in
retinal imaging, such as ultra-high-resolution optical
coherence tomography (Drexler et al., 2003), multi-modal
macular mapping (Bernardes et al., 2002) and polarisationsensitive retinal imaging (Burns et al., 2003) will permit
Table 4
Relationship between the structural changes that occur in ARM and their functional consequences
Structural changes that occur in AMD
Functional consequences
Increased rod cell loss
Convolution, deflection and shortening of the rod’s outer segments
Abnormalities of the synaptic terminals of the rod’s outer segments
Reduced scotopic sensitivity
Prolonged dark adaptation
Decrease the amplitude of the rod a-wave in the ERG
Short-wavelength sensitive cone loss
Tritan defects on surface colour tests
Reduced s-cone sensitivity
Abnormal colour-match area
Loss of photopigment reducing the quantum-catching ability of the
photoreceptors
Decrease the intensity of a stimulus on the retina
Reduced photopic sensitivity, visual acuity and contrast sensitivity
Altered retinal gain
Slowed recycling of photopigments
Increase in the time constant of adaptation
Geographic atrophy (photoreceptors can be viable over areas of RPE
atrophy)
Gradual vision loss
Poor dark adaptation
Decreased scotopic sensitivity
Decreased contrast sensitivity
Scotomas near fixation
Reduced reading speed
Compromised retinal metabolism
Reduced kinetic functions such as dark adaptation, glare recovery and
flicker sensitivity losses
Collection of blood and fluid under the retina causing surface
irregularities
Metamorphopsia
Extensive photoreceptor loss
Scotoma
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
better classification of potential cases and controls in future
studies and thus more accurate correlations of structure–
function relationships while reducing the possibility of
uncontrolled confounding. ARM encompasses a broad
morphological spectrum of disease. The substantial variety
in presentation, natural history of progression and
associated risk factors suggests that several phenotypes of
ARM may exist and different patterns of disease progression and functional impairment may reflect distinct underlying aetiologies. In order to investigate this further,
longitudinal studies are required and should involve a
detailed analysis of macular retinal function (spatial
and temporal measures), careful morphological phenotyping (lesion components, classification, extent and location
of abnormalities) along with systematic recording of
exposure to putative risk factors and genetic profiling in
order to achieve a better understanding of the pathogenesis
of ARM.
13. Method of literature search
References for this review were identified through a
comprehensive literature search of the following electronic
databases: MEDLINE, 1966–2005, Science Direct (all
years). The literature search was not confined to the
English language as non-English language publications
were translated. Additional articles, textbooks and abstracts thought relevant were selected from review of the
bibliographies of the articles generated from the above
search. To ensure the up-to-date nature of our review
article, e-mail alerts were set up through Science Direct.
The following key words and combinations of these words
were used in compiling the search: age-related macular
degeneration/maculopathy, visual acuity, contrast sensitivity, colour vision, short-wavelength cone, electrophysiology,
flicker sensitivity, rod/cone adaptation, vision-related quality
of life, scotopic/photopic sensitivity, macula imaging.
Acknowledgement
This work was supported by a grant from The Health
Foundation.
References
Aaronson, N.K., 1988. Quality of life: what is it? How should it be
measured? Oncology (Huntingt.) 2, 69–76.
Abadi, R.V., Pantazidou, M., 1996. Low contrast letter acuity in agerelated maculopathy. Ophthalmic Physiol. Opt. 16, 455–459.
Alexander, M.F., Maguire, M.G., Lietman, T.M., Snyder, J.R., Elman,
M.J., Fine, S.L., 1988. Assessment of visual function in patients with
age-related macular degeneration and low visual acuity. Arch.
Ophthalmol. 106, 1543–1547.
Alpeter, E., Mackeben, M., Trauzettel-Klosinski, S., 2000. The importance of sustained attention for patients with maculopathies. Vision
Res. 40, 1539–1547.
Anderson, A.J., Vingrys, A.J., 2000. Interactions between flicker thresholds and luminance pedestals. Vision Res. 40, 2579–2588.
271
Anderson, A.J., Vingrys, A.J., 2001. Multiple processes mediate flicker
sensitivity. Vision Res. 41, 2449–2455.
Applegate, R.A., Adams, A.J., Cavender, J.C., Zisman, F., 1987. Early
color vision changes in age-related maculopathy. Appl. Opt. 26,
1458–1462.
Arden, G.B., Wolf, J.E., 2004. Colour vision testing as an aid to diagnosis
and management of age related maculopathy. Br. J. Ophthalmol. 88,
1180–1185.
Arden, G.B., Carter, R.M., Macfarlan, A., 1984. Pattern and Ganzfeld
electroretinograms in macular disease. Br. J. Ophthalmol. 68, 878–884.
Arditi, A., Cagenello, R., 1993. On the statistical reliability of letter-chart
visual acuity measurements. Invest. Ophthalmol. Vis. Sci. 34, 120–129.
AREDS, 2001. The AREDS system for classifying age-related macular
degeneration from stereoscopic color fundus photographs. AREDS
Report No. 6. Am. J. Ophthalmol. 132, 668–681.
Atchison, D.A., Lovie-Kitchin, J.E., Swann, P.G., 1990. Investigation of
central visual fields in patients with age-related macular changes.
Optom. Vis. Sci. 67, 179–183.
Augood, C., Fletcher, A., Bentham, G., Chakravarthy, U., de Jong, P.T.,
Rahu, M., Seland, J., Soubrane, G., Tomazzoli, L., Topouzis, F.,
Vioque, J., Young, I., 2004. Methods for a population-based study of
the prevalence of and risk factors for age-related maculopathy and
macular degeneration in elderly European populations: the EUREYE
study. Ophthalmic Epidemiol. 11, 117–129.
Bailey, I.L., Lovie, J.E., 1980. The design and use of a new near vision
chart. Am. J. Optom. Physiol. Opt. 57, 378–387.
Baldasare, J., Watson, G.R., Whittaker, S.G., Miller-Shaffer, H., 1986.
The development and evaluation of a reading test for low vision
individuals with macular loss. J. Impairment Blindness June, 785–789.
Barca, L., Vaccari, G., 1978. Diabetic retinopathy and color discrimination under various illuminants. Mod. Probl. Ophthalmol. 19, 301–304.
Bartlett, H., Davies, L.N., Eperjesi, F., 2004a. Reliability, normative data
and the effect of age-related macular diseases on the Eger Macular
Stressometer photostress recovery time. Ophthalmic Physiol. Opt. 24,
594–599.
Bartlett, H., Eperjesi, F., Ali, A., Fowler, C.W., 2004b. Risk factors
associated with age-related macular disease. Optom. Practise 5, 15–32.
Bellmann, C., Unnebrink, K., Rubin, G.S., Miller, D., Holz, F.G., 2003.
Visual acuity and contrast sensitivity in patients with neovascular agerelated macular degeneration. Results from the radiation therapy for
age-related macular degeneration (RAD-) study. Graefe’s Arch. Clin.
Exp. Ophthalmol. 241, 968–974.
Bernardes, R., Lobo, C., Cunha-Vaz, J.G., 2002. Multimodal macula
mapping: a new approach to study diseases of the macula. Surv.
Ophthalmol. 24, 580–589.
Bird, A.C., 1974. Recent advances in the treatment of senile disciform
macular degeneration by photocoagulation. Br. J. Ophthalmol. 58,
367–376.
Bird, A.C., Bressler, N.M., Bressler, S.B., Chisholm, I.H., Coscas, G.,
Davis, M.D., de Jong, P.T., Klaver, C.C., Klein, B.E., Klein, R., et al.,
1995. An international classification and grading system for agerelated maculopathy and age-related macular degeneration. The
International ARM Epidemiological Study Group. Surv. Ophthalmol.
39, 367–374.
Bowers, A.R., Meek, C., Stewart, N., 2001. Illumination and reading
performance in age-related macular degeneration. Clin. Exp. Optom.
84, 139–147.
Bowman, K.J., 1978. The effect of illuminance on color discrimination in
senile macular degeneration. Mod. Probl. Ophthalmol. 19, 71–76.
Bowman, K.J., 1980a. The clinical assessment of colour discrimination
in senile macular degeneration. Acta Ophthalmol. (Copenh.) 58,
337–346.
Bowman, K.J., 1980b. The relationship between color discrimination and
visual acuity in senile macular degeneration. Am. J. Optom. Physiol.
Opt. 57, 145–148.
Bowman, K.J., Cameron, K.D., 1984. A quantitative assessment of colour
discrimination in normal vision and senile macular degeneration using
some colour confusion tests. Doc. Ophthalmol. Proc. 39, 363–369.
ARTICLE IN PRESS
272
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
Bressler, S.B., Maguire, M.G., Bressler, N.M., Fine, S.L., 1990. Relationship of drusen and abnormalities of the retinal pigment epithelium to
the prognosis of neovascular macular degeneration. The macular
photocoagulation study group. Arch. Ophthalmol. 108, 1442–1447.
Brody, B.L., Gamst, A.C., Williams, R.A., Smith, A.R., Lau, P.W.,
Dolnak, D., Rapaport, M.H., Kaplan, R.M., Brown, S.I., 2001.
Depression, visual acuity, comorbidity, and disability associated with
age-related macular degeneration. Ophthalmology 108, 1893–1900
(discussion 1900-1).
Brown, B., Garner, L.F., 1983. Effects of luminance on contrast sensitivity
in senile macular degeneration. Am. J. Optom. Physiol. Opt. 60,
788–793.
Brown, B., Lovie-Kitchin, J.E., 1983. Dark adaptation and the acuity/
luminance response in senile macular degeneration. Am. J. Optom.
Physiol. Opt. 60, 645–650.
Brown, B., Lovie-Kitchin, J., 1987a. Contrast sensitivity in central and
paracentral retina in age-related maculopathy. Clin. Exp. Optom. 70.5,
145–148.
Brown, B., Lovie-Kitchin, J., 1987b. Temporal function in age-related
maculopathy. Clin. Exp. Optom. 70.4, 112–116.
Brown, B., Lovie-Kitchin, J.E., 1989. Temporal summation in age-related
maculopathy. Optom. Vis. Sci. 66, 426–429.
Brown, B., Zadnik, I.L., Bailey, I.L., Colenbrander, A., 1984. Effect of
luminance, contrast, and eccentricity on visual acuity in senile macular
degeneration. Am. J. Optom. Physiol. Opt. 61, 265–270.
Brown, B., Tobin, C., Roche, N., Wolanowski, A., 1986. Cone adaptation
in age-related maculopathy. Am. J. Optom. Physiol. Opt. 63, 450–454.
Bullimore, M.A., Bailey, I.L., 1995. Reading and eye movements in agerelated maculopathy. Optom. Vis. Sci. 72, 125–138.
Burns, S.A., Elsner, A.E., Mellem-Kairala, M.B., Simmons, R.B., 2003.
Improved contrast of subretinal structures using polarization analysis.
Invest. Ophthalmol. Vis. Sci. 44, 4061–4068.
Cahill, M.T., Banks, A.D., Stinnett, S.S., Toth, C.A., 2005. Vision-related
quality of life in patients with bilateral severe age-related macular
degeneration. Ophthalmology 112, 152–158.
Calkins, D.J., 2001. Seeing with S cones. Prog. Retin. Eye Res. 20,
255–287.
Calkins, D.J., Tsukamoto, Y., Sterling, P., 1996. Microcircuitary and
mosaic of a blue/yellow ganglion cell in the primate retina. J. Neurosci.
18, 3373–3385.
Campbell, F.W., Green, D.G., 1965. Monocular vs. bionocular acuity.
Nature 208, 191–192.
Campbell, C., Rittler, M.C., 1972. Colour vision in retinal pathology.
Mod. Probl. Ophthalmol. 11, 98–105.
Carta, A., Braccio, L., Belpoliti, M., Soliani, L., Sartore, F., Gandolfi,
S.A., Maraini, G., 1998. Self-assessment of the quality of vision:
association of questionnaire score with objective clinical tests. Curr.
Eye Res. 17, 506–511.
Celesia, G.G., Kaufman, D., 1985. Pattern ERG’s and visual evoked
potentials in maculopathies and optic nerve disease. Invest. Ophthalmol. Vis. Sci. 26, 726–735.
Cheng, A.S., Vingrys, A.J., 1993. Visual losses in early age-related
maculopathy. Optom. Vis. Sci. 70, 89–96.
Cohen, S.Y., Lamarque, F., Saucet, J.C., Provent, P., Langram, C.,
LeGargasson, J.F., 2003. Filling-in phenomenon in patients with agerelated macular degeneration: differences regarding uni- or bilaterality
of central scotoma. Graefe’s Arch. Clin. Exp. Ophthalmol. 241,
785–791.
Collins, M., 1986. Pre-age related maculopathy and the desaturated D-15
colour vision test. Clin. Exp. Optom. 69, 223–227.
Collins, M., Brown, B., 1989a. Glare recovery and age-related maculopathy. Clin. Vis. Sci. 4, 145–153.
Collins, M., Brown, B., 1989b. Glare recovery and its relation to other
clinical findings in age related maculopathy. Clin. Vis. Sci. 4,
155–163.
Comer, G.M., Ciulla, T.A., Criswell, M.H., Tolentino, M., 2004. Current
and future treatment options for nonneovascular and neovascular agerelated macular degeneration. Drugs Aging 21, 967–992.
Crossland, M.D., Culham, L.E., Rubin, G.S., 2004. Fixation stability and
reading speed in patients with newly developed macular disease.
Ophthalmol. Physiol. Opt. 24, 327–333.
Cummings, R.W., Whittaker, S.G., Watson, G.R., Budd, J.M., 1985.
Scanning characters and reading with a central scotoma. Am. J.
Optom. Physiol. Opt. 62, 833–842.
Curcio, C.A., 2001. Photoreceptor topography in ageing and age-related
maculopathy. Eye 15, 376–383.
Curcio, C.A., Millican, C.L., Allen, K.A., Kalina, R.E., 1993. Aging of the
human photoreceptor mosaic: evidence for selective vulnerability of
rods in central retina. Invest. Ophthalmol. Vis. Sci. 34, 3278–3296.
Curcio, C.A., Medeiros, N.E., Millican, C.L., 1996. Photoreceptor loss in
age-related macular degeneration. Invest. Ophthalmol. Vis. Sci. 37,
1236–1249.
Curcio, C.A., Owsley, C., Jackson, G.R., 2000. Spare the rods, save the
cones in aging and age-related maculopathy. Invest. Ophthalmol. Vis.
Sci. 41, 2015–2018.
Dacey, D.M., 1993. Morphology of a small-field bistratified ganglion cell
type in the macaque and human retina. Vis. Neurosci. 10, 1081–1098.
Das, A., McGuire, P.G., 2003. Retinal and choroidal angiogenesis:
pathophysiology and strategies for inhibition. Prog. Retin. Eye Res.
22, 721–748.
de Boer, M.R., Moll, A.C., de Vet, H.C.W., Terwee, C.B., Vöiker-Dieben,
H.J.M., van-Rens, G.H.M.B., 2004. Psychometric properties of visionrelated quality of life questionnaires: a systematic review. Ophthalmol.
Physiol. Opt. 24, 257–273.
de Monasterio, F.M., Schein, S.J., McCrane, E.P., 1981. Staining of the
blue-sensitive cones of the macaque retina by a fluorescent dye. Science
213, 1278.
Deruaz, A., Whatham, A.R., Mermoud, C., Safran, A.B., 2002. Reading
with multiple preferred retinal loci: implications for training a more
efficient reading strategy. Vision Res. 42, 2947–2957.
Doris, N., Hart, P.M., Chakravarthy, U., McCleland, J., Stevenson, M.,
Hudson, C., Jackson, J., 2001. Relation between macular morphology
and visual function in patients with choroidal neovascularisation of
age related macular degeneration. Br. J. Ophthalmol. 85, 184–188.
Drexler, W., Sattmann, H., Hermann, B., Ko, T.H., Stur, M., Unterhuber,
A., Scholda, C., Findl, O., Wirtitsch, M., Fujimoto, J.G., Fercher,
A.F., 2003. Enhanced visualization of macular pathology with the use
of ultrahigh-resolution optical coherence tomography. Arch. Ophthalmol. 121, 695–706.
Duke-Elder, W.S., 1940. Textbook of Ophthalmology. Henry Kimpton,
London (pp. 2116–2372).
Duret, F., Issenhuth, M., Safran, A.B., 1999. Combined use of several
preferred retinal loci in patients with macular disorders when reading
single words. Vision Res. 39, 873–879.
Eisner, A., Fleming, S.A., Klein, M.L., Mauldin, W.M., 1987. Sensitivities
in older eyes with good acuity: eyes whose fellow eye has exudative
AMD. Invest. Ophthalmol. Vis. Sci. 28, 1832–1837.
Eisner, A., Stoumbos, V.D., Klein, M.L., Fleming, S.A., 1991. Relations
between fundus appearance and function. Eyes whose fellow eye has
exudative age-related macular degeneration. Invest. Ophthalmol. Vis.
Sci. 32, 8–20.
Eisner, A., Klein, M.L., Zilis, J.D., Watkins, M.D., 1992. Visual function
and the subsequent development of exudative age-related macular
degeneration. Invest. Ophthalmol. Vis. Sci. 33, 3091–3102.
El Mallah, M.K., Chakravarthy, U., Hart, P.M., 2000. Amblyopia: is
visual loss permanent? Br. J. Ophthalmol. 84, 952–956.
Eldred, K.B., 1992. Optimal illumination for reading in patients with agerelated maculopathy. Optom. Vis. Sci. 69, 46–50.
Elliott, D.B., Patel, B., Whitaker, D., 2001. Development of a reading
speed test for potential-vision measurements. Invest. Ophthalmol. Vis.
Sci. 42, 1945–1949.
Elsner, A.E., Burns, S.A., Weiter, J.J., 2002. Cone photopigment in older
subjects: decreased optical density in early age-related macular
degeneration. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 19, 215–222.
Ergun, E., Maar, N., Radner, W., Barbazetto, I., Schmidt-Erfurth, U.,
Stur, M., 2003. Scotoma size and reading speed in patients with
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
subfoveal occult choroidal neovascularization in age-related macular
degeneration. Ophthalmology 110, 65–69.
Eriksen, C.W., Schultz, D.W., 1977. Retinal locus and acuity in visual
information processing. Bull. Psychon. Soc. 9, 81–84.
Evans, J.R., Fletcher, A.E., Wormald, R.P., 2004a. Age-related macular
degeneration causing visual impairment in people 75 years or older in
Britain: an add-on study to the medical research council trial of
assessment and management of older people in the community.
Ophthalmology 111, 513–517.
Evans, J.R., Fletcher, A.E., Wormald, R.P., MRC trial of assessment and
management of older people in the community, 2004b. Causes of
visual impairment in people aged 75 years and older in Britain: an addon study to the MRC trial of assessment and management of older
people in the community. Br. J. Ophthalmol. 88, 365–370.
Falsini, B., Serrao, S., Fadda, A., Iarossi, G., Porrello, G., Cocco, F.,
Merendino, E., 1999. Focal electroretinograms and fundus appearance
in nonexudative age-related macular degeneration. Quantitative
relationship between retinal morphology and function. Graefe’s Arch.
Clin. Exp. Ophthalmol. 237, 193–200.
Falsini, B., Fadda, A., Iarossi, G., Piccardi, M., Canu, D., Minnella, A.,
Serrao, S., Scullica, L., 2000. Retinal sensitivity to flicker modulation:
reduced by early age-related maculopathy. Invest. Ophthalmol. Vis.
Sci. 41, 1498–1506.
Faubert, J., Overbury, O., 2000. Binocular vision in older people with
adventitious visual impairment: sometimes one eye is better than two.
J. Am. Geriatr. Soc. 48, 375–380.
Feigl, B., Brown, B., Lovie-Kitchin, J., Swann, P., 2004. Cone- and rodmediated multifocal electroretinogram in early age-related maculopathy. Eye July 30.
Ferris, F.L., Kassoff, A., Bresnick, G.H., Bailey, I.B., 1982.
New visual acuity charts for clinical research. Am. J. Ophthalmol.
94, 91–96.
Fine, E.M., Hazel, C.A., Petre, K.L., Rubin, G.S., 1999. Are the benefits
of sentence context different in central and peripheral vision? Optom.
Vis. Sci. 76, 764–769.
Fink, W., Sadun, S., 2004. Three-dimensional computer automated
threshold Amsler grid test. J. Biomed. Opt. 9, 149–153.
Fish, G.E., Birch, D.G., 1989. The focal electroretinogram in the clinical
assessment of macular disease. Ophthalmology 96, 109–114.
Fletcher, D.C., Schuchard, R.A., 1997. Preferred retinal loci relationship
to macular scotomas in a low-vision population. Ophthalmology 104,
632–638.
Francois, J., Verriest, G., 1961. On acquired deficiency of colour vision.
Vision Res. 1, 201–219.
Friedman, E., 1997. A hemodynamic model of the pathogenesis
of age-related macular degeneration. Am. J. Ophthalmol. 124,
677–682.
Fujii, G.Y., De Juan Jr., E., Humayun, M.S., Sunness, J.S., Chang, T.S.,
Rossi, J.V., 2003. Characteristics of visual loss by scanning laser
ophthalmoscope microperimetry in eyes with subfoveal choroidal
neovascularization secondary to age-related macular degeneration.
Am. J. Ophthalmol. 136, 1067–1078.
Gass, J.D., 1973. Drusen and disciform macular detachment and
degeneration. Arch. Ophthalmol. 90, 206–217.
Gerth, C., Hauser, D., Delahunt, P.B., Morse, L.S., Werner, J.S., 2003.
Assessment of multifocal electroretinogram abnormalities and their
relation to morphologic characteristics in patients with large drusen.
Arch. Ophthalmol. 121, 1404–1414.
Glaser, J.S., Savino, P.J., Sumers, K.D., McDonald, S.A., Knighton,
R.W., 1977. The photostress recovery test in the clinical assessment of
visual function. Am. J. Ophthalmol. 83, 255–260.
Goldberg, J., Flowerdew, G., Smith, E., Brody, J.A., Tso, M.O., 1988.
Factors associated with age-related macular degeneration. An analysis
of data from the first national health and nutrition examination
survey. Am. J. Epidemiol. 128, 700–710.
Green, W.R., Enger, C., 1993. Age-related macular degeneration
histopathologic studies. The 1992 Lorenz E. Zimmerman Lecture.
Ophthalmology 100 (10), 1519–1535.
273
Greenstein, V.C., Hood, D.C., Ritch, R., Steinberger, D., Carr, R.E.,
1989. S (blue) cone pathway vulnerability in retinitis pigmentosa,
diabetes and glaucoma. Invest. Ophthalmol. Vis. Sci. 30, 1732–1737.
Greenstein, V.C., Shapiro, A., Zaidi, Q., Hood, D.C., 1992. Psychophysical evidence for post-receptoral sensitivity loss in diabetics. Invest.
Ophthalmol. Vis. Sci. 33, 2781–2790.
Guez, J.E., Francois, J.F., Rigaudiere, F., O’Regan, J.K., 1993. Is there a
systematic location for the pseudo-fovea in patients with central
scotoma? Vision Res. 33, 1271–1279.
Haegerstrom-Portnoy, G., Brown, B., 1989. Two-color increment thresholds in early age-related maculopathy. Clin. Vis. Sci. 4, 165–172.
Haimovici, R., Owens, S.L., Fitzke, F.W., Bird, A.C., 2002. Dark
adaptation in age-related macular degeneration: relationship to the
fellow eye. Graefe’s Arch. Clin. Exp. Ophthalmol. 249, 90–95.
Hart Jr., W.M., 1987. Acquired dyschromatopsias. Surv. Ophthalmol. 32,
10–31.
Hart Jr., W.M., Burde, R.M., 1983. Three-dimensional topography of the
central visual field. Sparing of the foveal center in macular disease.
Ophthalmology 90, 1028–1038.
Hazel, C.A., Petre, K.L., Armstrong, R.A., Benson, M.T., Frost, N.A.,
2000. Visual function and subjective quality of life compared in
subjects with acquired macular disease. Invest. Ophthalmol. Vis. Sci.
41, 1309–1315.
Heinen, S.J., Skavenski, A.A., 1992. Adaptation of saccades and fixation
to bilateral foveal lesions in adult monkey. Vision Res. 32, 365–373.
Henkes, H.E., 1954. ERG in circulatory disturbances in the retina. III.
ERG in cases of senile degeneration of the macular area. Arch.
Ophthalmol. 51, 54–66.
Holopigian, K., Seiple, W., Greenstein, V., Kim, D., Carr, R.E., 1997.
Relative effects of aging and age-related macular degeneration on
peripheral visual function. Optom. Vis. Sci. 74, 152–159.
Holz, F.G., Gross-Jendroska, M., Eckstein, A., Hogg, C.R., Arden, G.B.,
Bird, A.C., 1995. Colour contrast sensitivity in patients with agerelated Bruch’s membrane changes. Ger. J. Ophthalmol. 4, 336–341.
Home, R., 1978. Binocular summation: a study of contrast sensitivity,
visual acuity and recognition. Vision Res. 18, 579–585.
Hood, D.C., Greenstein, V.C., 1988. Blue (S) cone pathway vulnerability:
a test of the fragile receptor hypothesis. Appl. Opt. 27, 1025–1029.
Hyvarinen, L., Laurinen, P., Rovamo, J., 1983. Contrast sensitivity in
evaluation of visual impairment due to macular degeneration and optic
nerve lesions. Acta. Ophthalmol. 61, 161–170.
Jackson, G.R., Owsley, C., 2000. Scotopic sensitivity during adulthood.
Vision Res. 40, 2467–2473.
Jackson, G.R., Owsley, C., McGwin Jr., G., 1999. Aging and dark
adaptation. Vision Res. 39, 3975–3982.
Jackson, G.R., McGwin, G., Phillips, J.M., Klein, R., Owsley, C., 2004.
Impact of aging and age-related maculopathy on activation of the awave of the rod-mediated electroretinogram. Invest. Ophthalmol. Vis.
Sci. 45, 3271–3278.
Junghardt, A., Wildberger, H., Török, B., 1995. Pattern electroretinogram, visual evoked potential and psychophysical functions in
maculopathy. Doc. Ophthalmol. 90, 229–245.
Jurklies, B., Weismann, M., Hüsing, J., Sutter, E.E., Bornfield, N., 2002.
Monitoring retinal function in neovascular maculopathy using multifocal electroretinography—early and
long-term correlation
with clinical findings. Graefe’s Arch. Clin. Exp. Ophthalmol. 240,
244–264.
Kiryu, J., Asrani, S., Shahidi, M., Mori, M., Zeimer, R., 1995. Local
response of the primate retinal microcirculation to increased metabolic
demand induced by flicker. Invest. Ophthalmol. Vis. Sci. 36,
1240–1246.
Kitchin, J.E., Bailey, I., 1981. Task complexity and visual acuity. Aust. J.
Optom. 64, 235–242.
Klein, R., Klein, B.E., Linton, K.L., 1992. Prevalence of age-related
maculopathy. The beaver dam eye study. Ophthalmology 99, 933–943.
Klein, R., Wang, Q., Klein, B.E., Moss, S.E., Meuer, S.M., 1995. The
relationship of age-related maculopathy, cataract, and glaucoma to
visual acuity. Invest. Ophthalmol. Vis. Sci. 36, 182–191.
ARTICLE IN PRESS
274
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
Kleiner, R.C., Enger, C., Alexander, M.F., Fine, S.L., 1988. Contrast
sensitivity in age-related macular degeneration. Arch. Ophthalmol.
106, 55–57.
Lakshminarayanan, V., Enoch, J.M., 1995. Vernier acuity and aging. Int.
Ophthalmol. 19, 109–115.
Lefton, L., Haber, R.N., 1974. Information extraction from different
retinal locations. J. Exp. Psychol. 102, 975–980.
Legge, G.E., 1984. Binocular contrast summation—1. Detection and
discrimination. Vision Res. 24, 373–383.
Legge, G.E., Rubin, G.S., Pelli, D.G., Schleske, M.M., 1985. Psychophysics of vision—II. Low vision. Vision Res. 25, 253–266.
Legge, G.E., Ross, J.A., Isenberg, L.M., LaMay, J.M., 1992. Psychophysics of reading: clinical predictors of low vision reading speed.
Invest. Ophthalmol. Vis. Sci. 33, 677–687.
Lei, H., Schuchard, R.A., 1997. Using two preferred retinal loci for
different lighting conditions in patients with central scotomas. Invest.
Ophthalmol. Vis. Sci. 38, 1812–1818.
Leibrock, C.S., Reuter, T., Lamb, T.D., 1998. Molecular basis of dark
adaptation in rod photoreceptors. Eye 12, 511–520.
Lennerstrand, G., 1982. Delayed visual evoked cortical potentials in
retinal disease. Acta Ophthalmol. (Copenh.) 60, 497–504.
Li, J., Tso, M.O., Lam, T.T., 2001. Reduced amplitude and delayed
latency in foveal response of multifocal electroretinogram in early age
related macular degeneration. Br. J. Ophthalmol. 85, 287–290.
Linder, M., Chang, T.S., Scott, I.U., Hay, D., Chambers, K., Sibley,
L.M., Weis, E., 1999. Validity of the visual function index (VF-14) in
patients with retinal disease. Arch. Ophthalmol. 117, 1611–1616.
Loshin, D.S., White, J., 1984. Contrast sensitivity: the visual rehabilitation
of the patient with macular degeneration. Arch. Ophthalmol. 102,
1303–1306.
Lott, L.A., Haegerstrom-Portnoy, G., Schneck, M.E., Brabyn, J.A.,
Gildengorin, G.L., 2002. Predicting reading performance in older
adults with good acuity. Invest. Ophthalmol. Vis. Sci. 43 (12)
(E-abstract 3829).
Lovie-Kitchin, J.E., 1988. Validity and reliability of visual acuity
measurements. Ophthalmic Physiol. Opt. 8, 363–370.
Lovie-Kitchin, J.E., Bowman, K.J., 1985. Senile Macular Degeneration:
Management and Rehabilitation. Butterworth Publishers, Boston
(pp. 63–64).
Lovie-Kitchin, J.E., Brown, B., 2000. Repeatability and intercorrelations
of standard vision tests as a function of age. Optom. Vis. Sci. 77,
412–420.
Lowenstein, A., Malach, R., Goldstein, M., Leibovitch, I., Barak, A.,
Baruch, E., Alster, Y., Rafaeli, O., Avni, I., Yassur, Y., 2003.
Replacing the Amsler Grid. A new method for monitoring patients
with age-related macular degeneration. Ophthalmology 110, 966–970.
Mackeben, M., 1999. Sustained focal attention and peripheral letter
recognition. Spat. Vis. 12, 51–72.
Mackenzie, P.J., Chang, T.S., Scott, I.U., Linder, M., Hay, D., Feuer, W.J.,
Chambers, K., 2002. Assessment of vision-related function in patients
with age-related macular degeneration. Ophthalmology 109, 720–729.
Macular Photocoagulation Study (MPS) Group, 1994. Visual outcome
after laser photocoagulation for subfoveal choroidal neovascularization secondary to age-related macular degeneration. The influence of
initial lesion size and initial visual acuity. Arch. Ophthalmol. 112,
480–488.
Mangione, C.M., Gutierrez, P.R., Lowe, G., Orav, E.J., Seddon, J.M.,
1999. Influence of age-related maculopathy on visual functioning and
health-related quality of life. Am. J. Ophthalmol. 128, 45–53.
Marc, R.E., Sperling, H.G., 1977. Chromatic organization of primate
cones. Science 196, 487.
Marcus, M., Merin, S., Wolf, M., Feinsod, M., 1983. Electrophysiological
tests in assessment of senile macular degeneration. Ann. Ophthalmol.
15, 235–238.
Margolis, M.K., Coyne, K., Kennegy-Martin, T., Baker, T., Schein, O.,
Revicki, D., 2002. Vision-specific instruments for the assessment of
health-related quality of life and visual functioning: a literature review.
Pharmacoeconomics 20, 791–812.
Marmor, M.F., 2000. A brief history of macular grids: from Thomas Reid
to Edvard Munch and Marc Amsler. Surv. Ophthalmol. 44, 343–353.
Marmor, M., Hood, D., Keating, D., Kondo, M., Seeliger, M., Miyake,
Y., 2003. Guidelines for basic multifocal electroretinography
(mfERG). Doc. Ophthalmol. 106, 105–115.
Marron, J.A., Bailey, I.L., 1982. Visual factors and orientation-mobility
performance. Am. J. Optom. Physiol. Opt. 59, 413–426.
Massof, B.K., Rubin, G.S., 2001. Visual function assessment questionnaires. Surv. Ophthalmol. 45, 531–548.
Mayer, M.J., Spiegler, S.J., Ward, B., Glucs, A., Kim, C.B., 1992a.
Preliminary evaluation of flicker sensitivity as a predictive test for
exudative age-related maculopathy. Invest. Ophthalmol. Vis. Sci. 33,
3150–3155.
Mayer, M.J., Spiegler, S.J., Ward, B., Glucs, A., Kim, C.B., 1992b. Foveal
flicker sensitivity discriminates ARM-risk from healthy eyes. Invest.
Ophthalmol. Vis. Sci. 33, 3143–3149.
Mayer, M.J., Spiegler, S.J., Ward, B., Glucs, A., Kim, C.B., 1992c. Midfrequency loss of foveal flicker sensitivity in early stages of age-related
maculopathy. Invest. Ophthalmol. Vis. Sci. 33, 3136–3142.
Mayer, M.J., Ward, B., Klein, R., Talcott, J.B., Dougherty, R.F., Glucs,
A., 1994. Flicker sensitivity and fundus appearance in pre
-exudative age-related maculopathy. Invest. Ophthalmol. Vis. Sci. 35,
1138–1149.
Mayer, M.J., Dougherty, R.F., Hu, L.T., 1995. A covariance structure
analysis of flicker sensitivity. Vision Res. 35, 1575–1583.
McClure, M.E., Hart, P.M., Jackson, A.J., Stevenson, M.R., Chakravarthy, U., 2000. Macular degeneration: do conventional measurements of impaired visual function equate with visual disability? Br. J.
Ophthalmol. 84, 244–250.
McMahon, T.T., Hansen, M., Viana, M., 1991. Fixation characteristics in
macular disease—relationship between saccadic frequency, sequencing
and reading rate. Invest. Ophthalmol. Vis. Sci. 32, 567–574.
Midena, E., Segato, T., Blarzino, M.C., Angeli, D.G., 1994. Macular
drusen and sensitivity of the central visual field. Doc. Ophthalmol. 88,
179–185.
Midena, E., Degli Angeli, C., Blarzino, M.C., Valenti, M., Segato, T.,
1997. Macular function impairment in eyes with early age-related
macular degeneration. Invest. Ophthalmol. Vis. Sci. 38, 469–477.
Muldrew, K.A., Hogg, R.E., McClure, M.E., Stevenson, M.R., Chakravarthy, U., 2003. Cross-sectional relationships between clinical
measures of vision in an AMD population. Invest. Ophthalmol. Vis.
Sci. 44 (E-abstract 11783).
Negishi, C., Takasoh, M., Fujimoto, N., Tsuyama, Y., Adachi-Usami, E.,
2001. Visual evoked potentials in relation to visual acuity in macular
disease. Acta Ophthalmol. Scand. 79, 271–276.
Nilsson, U.L., Frennesson, C., Nilsson, S.E., 2003. Patients with AMD
and a large absolute central scotoma can be trained successfully to use
eccentric viewing, as demonstrated in a scanning laser ophthalmoscope. Vision Res. 43, 1777–1787.
Nirmalan, P.K., Katz, J., Robin, A.L., Tielsch, J.M., Namperumalsamy,
P., Kim, R., Narendran, V., Ramakrishnan, R., Krishnadas, R.,
Thulasiraj, R.D., Suan, E., 2004. Prevalence of vitreoretinal disorders
in a rural population of southern India: the Aravind Comprehensive
Eye Study. Arch. Ophthalmol. 122, 581–586.
Owen, C.G., Fletcher, A.E., Donoghue, M., Rudnicka, A.R., 2003. How
big is the burden of visual loss caused by age related macular
degeneration in the United Kingdom? Br. J. Ophthalmol. 87, 312–317.
Owsley, C., 2003. Contrast sensitivity. Ophthalmol. Clin. N. Am. 16,
171–177.
Owsley, C., Sekuler, R., Boldt, C., 1981. Aging and low-contrast vision:
face perception. Invest. Ophthalmol. Vis. Sci. 21, 362–365.
Owsley, C., Jackson, G.R., Cideciyan, A.V., Huang, Y., Fine, S.L., Ho,
A.C., Maguire, M.G., Lolley, V., Jacobson, S.G., 2000. Psychophysical evidence for rod vulnerability in age-related macular degeneration. Invest. Ophthalmol. Vis. Sci. 41, 267–273.
Owsley, C., Jackson, G.R., White, M., Feist, R., Edwards, D., 2001.
Delays in rod-mediated dark adaptation in early age-related maculopathy. Ophthalmology 108, 1196–1202.
ARTICLE IN PRESS
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
Palmowski, A.M., Sutter, E.E., Bearse Jr., M.A., Fung, W., 1999.
Multifocal electroretinogram (MF-ERG) in diagnosis of macular
changes. Example: senile macular degeneration. Ophthalmology 96,
166–173.
Phipps, J.A., Guymer, R.H., Vingrys, A.J., 2003. Loss of cone function in
age-related maculopathy. Invest. Ophthalmol. Vis. Sci. 44, 2277–2283.
Phipps, J.A., Dang, T.M., Vingrys, A.J., Guymer, R.H., 2004. Flicker
perimetry loses in age-related macular degeneration. Invest. Ophthalmol. Vis. Sci. 45, 3355–3360.
Pianta, M.J., Kalloniatis, M., 2000. Characterisation of dark adaptation
in human cone pathways: an application of the equivalent background
hypothesis. J. Physiol. 528, 591–608.
Rayner, K., 1978. Eye movement in reading and information processing.
Psychol. Bull. 85, 65–81.
Rayner, K., Bertera, J.H., 1979. Reading without a fovea. Science 206,
468.
Remky, A., Lichtenberg, K., Elsner, A.E., Arend, O., 2001. Short
wavelength automated perimetry in age related maculopathy. Br. J.
Ophthalmol. 85, 1432–1436.
Remulla, J.F., Gaudio, A.R., Miller, S., Sandberg, M.A., 1995. Foveal
electroretinograms and choroidal perfusion characteristics in fellow
eyes of patients with unilateral neovascular age-related macular
degeneration. Br. J. Ophthalmol. 79, 558–561.
Rosser, D.A., Cousens, S.N., Murdoch, I.E., Fitzke, F.W., Laidlaw, D.A.,
2003. How sensitive to clinical change are ETDRS logMAR visual
acuity measurements? Invest. Ophthalmol. Vis. Sci. 44, 3278–3281.
Rovner, B.W., Casten, R.J., Tasman, W.S., 2002. Effect of depression on
vision function in age-related macular degeneration. Arch. Ophthalmol. 120, 1041–1044.
Rubin, G.S., Munoz, B., Bandeen-Roche, K., West, S.K., 2000.
Monocular versus binocular visual acuity as measures of vision
impairment and predictors of visual disability. Invest. Ophthalmol.
Vis. Sci. 41, 3327–3334.
Rubin, G.S., Bandeen-Roche, K., Huang, G.H., Munoz, B., Schein, O.D.,
Fried, L.P., West, S.K., 2001. The association of multiple visual
impairments with self-reported visual disability: SEE project. Invest.
Ophthalmol. Vis. Sci. 42, 64–72.
Rubinstein, M.P., Underwood, J., 1985. The crowding phenomenon and
its significance in senile macular degeneration. Br. Orthopt. J. 42,
45–53.
Ryan, S.J., Mittl, R.N., Maumenee, A.E., 1980. The disciform response, a
historical perspective. Graefe’s Arch. Clin. Exp. Ophthalmol. 215,
1–20.
Safran, A.B., Duret, F., Issenhuth, M., Mermoud, C., 1999. Full text
reading with a central scotoma: pseudo regressions and pseudo line
losses. Br. J. Ophthalmol. 83, 1341–1347.
Sandberg, M.A., Gaudio, A.R., 1995. Slow photostress recovery and
disease severity in age-related macular degeneration. Retina 15,
407–412.
Sandberg, M.A., Miller, S., Gaudio, A.R., 1993. Foveal cone ERG’s in
fellow eyes of patients with unilateral neovascular age-related macular
degeneration. Invest. Ophthalmol. Vis. Sci. 34, 3477–3480.
Sandberg, M.A., Weiner, A., Miller, S., Gaudio, A.R., 1998. High-risk
characteristics of fellow eyes of patients with unilateral neovascular
age-related macular degeneration. Ophthalmology 105 (3), 441–447.
Sarks, S.H., 1976. Ageing and degeneration in the macular region: a
clinico-pathological study. Br. J. Ophthalmol. 60, 324–341.
Sarks, J.P., Sarks, S.H., Killingsworth, M.C., 1988. Evolution of
geographic atrophy of the retinal pigment epithelium. Eye 2, 552–577.
Schmidt-Erfurth, U.M., Elsner, H., Terai, N., Benecke, A., Dahmen, G.,
Michels, S.M., 2004. Effects of verteporfin therapy on central visual
field function. Ophthalmology 111, 931–939.
Schmitt, N.J., Grover, D.A., Feldon, S.E., 2001. The Eger maculometer
stressometer: pilot study. Am. J. Ophthalmol. 136, 314–317.
Schneider, U., Inhoffen, W., Gelisken, F., Kreissig, I., 1996. Assessment of
visual function in choroidal neovascularization with scanning laser
microperimetry and simultaneous indocyanine green angiography.
Graefe’s Arch. Clin. Exp. Ophthalmol. 234, 612–617.
275
Schuchard, R.A., 1993. Validity and interpretation of Amsler grid reports.
Arch. Ophthalmol. 111, 776–780.
Scilley, K., Jackson, G.R., Cideciyan, A.V., Maguire, M.G., Jacobson,
S.G., Owsley, C., 2002. Early age-related maculopathy and selfreported visual difficulty in daily life. Ophthalmology 109, 1235–1242.
Seiple, W.H., Siegel, I.M., Carr, R.E., Mayron, C., 1986. Evaluating
macular function using focal ERG. Invest. Ophthalmol. Vis. Sci. 27,
1123–1130.
Shirao, Y., Ushimura, S., Kawasaki, K., 1997. Differentiation of
neovascular maculopathies by nonphotic electrooculogram responses.
Jpn. J. Ophthalmol. 41, 174–179.
Sjostrand, J., Frisen, L., 1977. Contrast sensitivity in macular disease.
Acta Ophthalmol. (Copenh.) 55, 507–513.
Smiddy, W.E., Fine, S.L., 1984. Prognosis of patients with bilateral
macular drusen. Ophthalmology 91, 271–277.
Smith, V.C., Pokorny, J., Diddie, K.R., 1988. Color matching and the
Stiles–Crawford effect in observers with early age-related macular
changes. J. Opt. Soc. Am. A 5, 2113–2121.
Sokol, S., 1971. An electrodiagnostic index of macular degeneration.
Arch. Ophthalmol. 88, 619–624.
Sperling, H.G., Johnson, C., Harwerth, R.S., 1980. Differential spectral
photopic damage to primate cones. Vision Res. 20, 1117.
Spraul, C.W., Lang, G.E., Grossniklaus, H.E., Lang, G.K., 1999.
Histologic and morphometric analysis of the choroid, Bruch’s
membrane, and retinal pigment epithelium in postmortem eyes with
age-related macular degeneration and histologic examination of
surgically excised choroidal neovascular membranes. Surv. Ophthalmol. 44 (Suppl. 1), S10–S32.
Stangos, N., Voutas, S., Topouzis, F., Karampatakis, V., 1995. Contrast
sensitivity evaluation in eyes predisposed to age-related macular
degeneration and presenting normal visual acuity. Ophthalmologica
209, 194–198.
Stein, J.D., Brown, M.M., Brown, G.C., Hollands, H., Sharma, S., 2003.
Quality of life with macular degeneration: perceptions of
patients, clinicians and community members. Br. J. Ophthalmol. 87,
8–12.
Steinmetz, R.L., Haimovici, R., Jubb, C., Fitzke, F.W., Bird, A.C., 1993.
Symptomatic abnormalities of dark adaptation in patients with agerelated Bruch’s membrane change. Br. J. Ophthalmol. 77, 549–554.
Sturr, J.F., Zhang, L., Taub, H.A., Hannon, D.J., Jackowski, M.M., 1997.
Psychophysical evidence for losses in rod sensitivity in the aging visual
system. Vision Res. 37, 475–481.
Sunness, J.S., 1999. Evaluating macular function. Int. Ophthalmol. Clin.
39, 19–31.
Sunness, J.S., Massof, R.W., 1986. Focal electro-oculogram in age-related
macular degeneration. Am. J. Optom. Physiol. Opt. 63, 7–11.
Sunness, J.S., Massof, R.W., Johnson, M.A., Finkelstein, D., Fine, S.L.,
1985. Peripheral retinal function in age-related macular degeneration.
Arch. Ophthalmol. 103, 811–816.
Sunness, J.S., Johnson, M.A., Massof, R.W., Marcus, S., 1988. Retinal
sensitivity over drusen and nondrusen areas. A study using fundus
perimetry. Arch. Ophthalmol. 106, 1081–1084.
Sunness, J.S., Massof, R.W., Johnson, M.A., Bressler, N.M., Bressler,
S.B., Fine, S.L., 1989. Diminished foveal sensitivity may predict the
development of advanced age-related macular degeneration. Ophthalmology 96, 375–381.
Sunness, J.S., Schuchard, R.A., Shen, N., Rubin, G.S., Dagnelie, G.,
Haselwood, D.M., 1995. Landmark-driven fundus perimetry using the
scanning laser ophthalmoscope. Invest. Ophthalmol. Vis. Sci. 36,
1863–1874.
Sunness, J.S., Applegate, C.A., Haselwood, D., Rubin, G.S., 1996.
Fixation patterns and reading rates in eyes with central scotomas from
advanced atrophic age-related macular degeneration and stargardt
disease. Ophthalmology 103, 1458–1466.
Sunness, J.S., Rubin, G.S., Applegate, C.A., Bressler, N.M., Marsh, M.J.,
Hawkins, B.S., Haselwood, D., 1997. Visual function abnormalities
and prognosis in eyes with age-related geographic atrophy of the
macula and good visual acuity. Ophthalmology 104, 1677–1691.
ARTICLE IN PRESS
276
R.E. Hogg, U. Chakravarthy / Progress in Retinal and Eye Research 25 (2006) 249–276
Sunness, J.S., Applegate, C.A., Gonzalez-Baron, J., 2000. Improvement of
visual acuity over time in patients with bilateral geographic atrophy
from age-related macular degeneration. Retina 20, 162–169.
Sutter, E., Tran, D., 1992. The field topography of ERG components in
man—I: the photopic luminance response. Vision Res. 32, 433–446.
Swann, P.G., Lovie-Kitchin, J.E., 1991. Age-related maculopathy. II: the
nature of the central visual field loss. Ophthalmic Physiol. Opt. 11, 59–70.
Takamine, Y., Shiraki, K., Moriwaki, M., Yasunari, T., Miki, T., 1998.
Retinal sensitivity measurement over drusen using scanning laser
ophthalmoscope perimetry. Graefe’s Arch. Clin. Exp. Ophthalmol.
236, 285–290.
Tezel, T.H., Del Priore, L.V., Flowers, B.E., Grosof, D.H., Benenson,
I.L., Zamora, R.L., Kaplan, H.J., 1996. Correlation between scanning
laser ophthalmoscope microperimetry and anatomic abnormalities in
patients with subfoveal neovascularization. Ophthalmology 103,
1829–1836.
Timberlake, G.T., Mainster, M.A., Peli, E., Augliere, R.A., Essock, E.A.,
Arend, L.E., 1986. Reading with a macular scotoma—I: retinal location
of scotoma and fixation area. Invest. Ophthalmol. Vis. Sci. 27, 1137–1147.
Timberlake, G.T., Peli, E., Essock, E.A., Augliere, R.A., 1987. Reading
with a macular scotoma. II. Retinal locus for scanning text. Invest.
Ophthalmol. Vis. Sci. 28, 1268–1274.
Tolentino, M.J., Miller, S., Gaudio, A.R., Sandberg, M.A., 1994. Visual
field deficits in early age-related macular degeneration. Vision Res. 34,
409–413.
Trusiewicz, D., Kordalewska, A., Zebrowska, K., 1984. Colour vision in
relation to other visual functions in the presence of slight macular
degeneration. In: Verriest, G. (Ed.), Colour Vision Deficiencies VII.
Dr. W. Junk Publishers, The Hague, Boston Lancaster, pp. 371–376.
Valberg, A., Fosse, P., 2002. Binocular contrast inhibition in subjects with
age-related macular degeneration. J. Opt. Soc. Am. A 19, 223–228.
Van Toi, V., Riva, C., 1994. Variations of blood flow at optic nerve head
induced by sinusoidal flicker stimulation in cats. J. Physiol. 482,
189–202.
Wall, M., May, D.R., 1987. Threshold Amsler grid testing in maculopathies. Ophthalmology 94, 1126–1133.
Walter, P., Widder, R.A., Lüke, C., Königsfeld, P., Brunner, R., 1999.
Electrophysiological abnormalities in age-related macular degeneration. Graefe’s Arch. Clin. Exp. Ophthalmol. 237, 962–968.
Wang, J.J., Mitchell, P., Smith, W., 2000. Vision and low self-rated health:
the Blue Mountains eye study. Invest. Ophthalmol. Vis. Sci. 41,
49–54.
Wang, Y.Z., Wilson, E., Locke, K.G., Edwards, A.O., 2002. Shape
discrimination in age-related macular degeneration. Invest. Ophthalmol. Vis. Sci. 43, 2055–2062.
Weiter, J.J., Wing, G.L., Trempe, C.L., Mainster, M.A., 1984. Visual
acuity related to retinal distance from the fovea in macular disease.
Ann. Ophthalmol. 16, 174–176.
White, J.M., Bedell, H.E., 1990. The oculomotor reference in human
with bilateral macular disease. Invest. Ophthalmol. Vis. Sci. 31,
1149–1161.
Whittaker, S.G., Lovie-Kitchin, J., 1993. Visual requirements for reading.
Optom. Vis. Sci. 70, 54–65.
Whittaker, S.G., Budd, J.M., Cummings, R.W., 1988. Eccentric
fixation with macular scotoma. Invest. Ophthalmol. Vis. Sci. 29,
268–278.
Williams, R.A., Brody, B.L., Thomas, R.G., Kaplan, R.M., Brown, S.I.,
1998. The psychosocial impact of macular degeneration. Arch.
Ophthalmol. 116, 514–520.
Wolkstein, M., Atkin, A., Bodis-Wollner, I., 1980. Contrast sensitivity in
retinal disease. Ophthalmology 87, 1140–1149.
Zaidi, F.H., Cheong-Leen, R., Gair, E.J., Weir, R., Sharkawi, E., Lee, N.,
Gregory-Evans, K., 2004. The Amsler chart is of doubtful value in
retinal screening for early laser therapy of subretinal membranes.
The West London Survey. Eye 18, 503–508.
Zlatkova, M.B., Anderson, R.S., Ennis, F.A., 2001. Binocular summation
for grating detection and resolution in foveal and peripheral vision.
Vision Res. 41, 3093–3100.