Hyperhomocysteinemia Is Associated With the Presence of
Left Atrial Thrombus in Stroke Patients With Nonvalvular
Atrial Fibrillation
Hakan Ay, MD; E. Murat Arsava, MD; S. Lale Tokgözoğlu, MD; Necla Özer, MD; Okay Sarıbaş, MD
Downloaded from http://stroke.ahajournals.org/ by guest on October 2, 2016
Background and Purpose—Blood stasis is the fundamental mechanism leading to thrombus formation in the venous
system. Homocysteine also poses a significant risk for venous thrombosis through its endothelial toxic and
prothrombotic properties. In the present study, we hypothesized that high homocysteine might be associated with
thrombus formation in another stasis-related condition, atrial fibrillation.
Methods—Forty-two consecutive patients with ischemic stroke caused by nonvalvular atrial fibrillation and admitted
within the first day of symptom onset were included. Total fasting plasma homocysteine, serum folic acid, and vitamin
B12 levels were measured. All patients were evaluated by transesophageal echocardiography for the presence of a left
atrial (LA) thrombus. Homocysteine and vitamin levels were compared between groups with or without LA thrombus.
Results—Transesophageal echocardiography revealed LA thrombus in 20 patients. Mean homocysteine levels were
significantly higher in patients with LA thrombus (20.75 versus 13.34 mol/L, P⬍0.001). Multivariate logistic
regression analysis showed that the effect of high homocysteine was independent of other clinical or echocardiographic
variables known to increase LA thrombus (P⫽0.017). There was no difference in vitamin B12 levels between groups
(P⫽0.118), whereas the mean folic acid level was significantly lower in patients with LA thrombus (P⫽0.004).
Conclusions—High plasma homocysteine conveys an independent risk for LA thrombus formation in patients with stroke
caused by nonvalvular atrial fibrillation. This finding further supports the thrombogenic role of high homocysteine in
conditions associated with blood stasis. (Stroke. 2003;34:●●●-●●●.)
Key Words: atrial fibrillation 䡲 homocyst(e)ine 䡲 stroke 䡲 thrombosis
N
onvalvular atrial fibrillation (AF) is a common problem
in the elderly, occurring in 2% to 4% of the population
⬎60 years of age. It is 1 of the most common causes of
stroke, estimated to be responsible for 1 of every 10 ischemic
strokes in this age group.1 Transesophageal echocardiography
(TEE) reveals a thrombus lodged within the left atrial
appendage (LAA) in up to 43% of patients with a recent
embolic event.2 Even if not seen in TEE, a minute but still
clinically important–sized thrombus trapped within the trabeculae of the LAA can frequently be identified at autopsy.3
The fundamental mechanism that leads to thrombus formation in AF is blood stasis in the LAA. Stagnant flow or stasis
not only is unique to AF but also is a key feature of thrombus
formation in the venous system.4 LA and venous thrombi also
resemble each other microscopically. Therefore, factors in
addition to stasis contributing to the formation of thrombus in
the venous system might also operate in AF.
Homocysteine, an intermediate amino acid formed during
the metabolism of dietary methionine, has been linked to a
variety of vascular diseases. Large case-control and prospective studies have shown that elevated fasting and post–
methionine-loading homocysteine levels are an independent
risk factor for arterial and venous thrombotic events.5–7
Meta-analyses have found odds ratios (ORs) of 2.5 (95% CI,
1.8 to 3.5) to 2.95 (95% CI, 2.08 to 4.17) for venous
thrombosis in patients with high homocysteine levels.6,7
Hyperhomocysteinemia is also a risk factor for recurrent
venous thrombosis, increasing the risk ⬎2-fold.8 Given that
elevated homocysteine enhances venous thrombosis, we hypothesized that it may also convey a risk for the formation of
LA thrombus in AF.
Methods
Over a 1-year period, 71 consecutive ischemic stroke patients with
nonvalvular AF who were admitted within the first 24 hours after
symptom onset were included. Baseline clinical characteristics—
including age, sex, and history of hypertension, diabetes mellitus,
and congestive heart failure—were recorded. A complete diagnostic
evaluation was performed for each patient; this included blood
chemistry, blood cell counts, erythrocyte sedimentation rate, ECG,
coagulation panel (antiphospholipid and anticardiolipin antibodies,
activated partial thromboplastin time, prothrombin time, international normalized ratio, protein C, protein S, antithrombin III,
fibrinogen, protein C resistance, and factor 5 Leiden), carotid duplex
Received August 14, 2002; final revision received October 5, 2002; accepted October 11, 2002.
From Departments of Neurology (H.A., E.M.A., O.S.) and Cardiology (L.T., N.O.), Hacettepe University Hospital, Ankara, Turkey.
Correspondence to Hakan Ay, MD, Associate Professor of Neurology, Hacettepe University Hospitals, Department of Neurology, Sıhhıye 06100,
Ankara, Turkey. E-mail ayhmgh@hotmail.com
© 2003 American Heart Association, Inc.
Stroke is available at http://www.strokeaha.org
DOI: 10.1161/01.STR.0000060202.63475.BA
1
2
Stroke
April 2003
Baseline Characteristics and Univariate Associations
LA Thrombus (⫺)
(n⫽22)
LA Thrombus (⫹)
(n⫽20)
69.68 (60–79)
67.65 (51–78)
0.464
11/11
13/7
0.327
15
14
0.899
Diabetes mellitus, n
4
3
1.000
Congestive heart failure, n
3
4
0.691
Coronary artery disease, n
7
9
0.380
LA diameter⬎4 cm, n
7
11
0.129
Spontaneous echo contrast, n
5
14
13.34
20.75
Mean age (range), y
Sex, M/F
Hypertension, n
Mean homocysteine levels, mol/L
Mean folic acid levels (range), ng/mL
Mean vitamin B12 levels (range), pg/mL
P
0.002
⬍0.001
11.65 (7.5–24)
7.51 (3–13.3)
0.004
412.42 (180–857)
294.64 (133–584)
0.118
Downloaded from http://stroke.ahajournals.org/ by guest on October 2, 2016
ultrasonography, transcranial Doppler ultrasonography, CT, MRI,
and MR angiography.
After a 12-hour overnight fast, total plasma homocysteine level
was measured in subjects within the first 48 hours after stroke onset.
Venous blood was drawn into Vacutainer tubes the morning after
admission and placed in crushed ice. The blood was immediately
centrifuged, and homocysteine levels were measured within the
following 2 hours. Plasma homocysteine levels were determined
with the Fluorescence Polarisarization Immunoassay (IMX System,
Abbott Diagnostics). The upper limit of the manufacturer and the
laboratory was 15 mol/L. Serum folic acid and vitamin B12 levels
were also determined in a subset of patients admitted within the last
8 months of the present study. The levels of these vitamins were
measured simultaneously with the blood sample collected for homocysteine measurements. Serum folic acid and vitamin B12 levels
were measured with an IMMULITE analyzer (Diagnostic Products
Corp). The reference ranges for folic acid and vitamin B12 were 3 to
17 ng/mL and 160 to 900 pg/mL, respectively.
All patients initially underwent transthoracic echocardiography
study (Vivid Five Vigmed Technology, GE Ultrasound Device) to
exclude any valvular disease as the cause of AF. Studies were
performed with the patient in the left lateral recumbent position with
standard parasternal and apical views. This was followed by a
standard pulse, continuous, and color Doppler examinations. LA
diameter was obtained from the parasternal long-axis view as
suggested by the American Society of Echocardiography.9 Ejection
fraction, wall motion abnormalities, and other ventricular abnormalities on transthoracic echocardiography were also noted. After an
overnight fast, TEE was performed with a multiplane TEE 5-MHz
probe. Lidocaine was used for local anesthesia of the hypopharynx.
Sedation was not performed. After standard examination of the
cardiac chambers and valves, the LAA was visualized in both the
basal short-axis view in the transverse and the left ventricular–LA
2-chamber view in the vertical scans. The images were analyzed
online by the echocardiographer, who remained blinded to the
homocysteine and vitamin levels, for the presence of LA thrombus,
spontaneous echo contrast (SEC), and interatrial septal abnormalities. Thrombus was defined as a discrete echodensity distinct from
the underlying endocardium and visible in ⬎1 plane. SEC was
considered to be present if a nonhomogeneous echo swirling in the
left atrium and distinguishable from background noise by manipulation of gain settings was seen.
Differences in categorical variables between patients with and
without LA thrombus (history of hypertension, diabetes mellitus, or
congestive heart failure; presence of SEC and left atrial dilatation)
were compared by use of a 2 test or Fisher’s exact test. Homocysteine, folic acid, and vitamin B12 levels between groups were
compared by the Mann-Whitney U test. A multivariate logistic
regression analysis was performed to show whether the effect of high
homocysteine was independent of other variables known to increase
the LA thrombus (variables with a value of P⬍0.15 were included in
the model). The association between high homocysteine levels and
LA thrombus was expressed by the use of ORs with 95% CIs.
Spearman’s rank correlation coefficients were calculated to describe
associations between folic acid, vitamin B12, and homocysteine
levels. A value of P⬍0.05 was considered significant.
Results
Of the 71 patients with AF, 8 died before a TEE study could
be performed, and 12 declined a TEE study. Nine additional
patients were also excluded because the cause of their stroke
was judged not to be AF: 6 had either severe internal carotid
artery stenosis or occlusion ipsilateral to the acute hemispheric infarction; 1 had distal vertebral artery occlusion and
a cerebellar infarction in the territory of the ipsilateral
posterior inferior cerebellar artery; and 2 had hypertension
and a lacunar infarction on MRI (small-vessel disease). The
remaining 42 patients with nonvalvular AF as the cause of
their stroke met the inclusion criteria. There were 18 female
and 24 male patients; their mean age was 68.7 years. Except
for 1 patient who presented with transient ischemic attack, all
patients had a long-lasting deficit. Diffusion-weighted MRI
revealed an acute infarction in each patient, including the one
with transient ischemic attack. The cerebral lesions involved
the territories of the middle cerebral artery in 33, the anterior
cerebral artery in 3, the posterior cerebral artery in 3, the
posterior inferior cerebellar artery in 2, and the anterior
inferior cerebellar artery in 1 patient. Other baseline characteristics and echocardiography findings are presented in the
Table.
A TEE was obtained within a mean of 9 days after stroke
(range, 3 to 12 days). LA thrombus was identified in 20 of the 42
patients (47.6%). LA thrombus was limited to within the LAA in
13 of the 20 patients. In the remaining 7 patients, the thrombus
extended beyond the limits of the LAA and protruded into the
LA cavity. There was no difference between patients with or
without LA thrombus with respect to age, sex, and history of
hypertension, diabetes mellitus, and congestive heart failure (the
Table). Likewise, LA diameter did not differ between groups,
whereas SEC was more common in patients with LA thrombus.
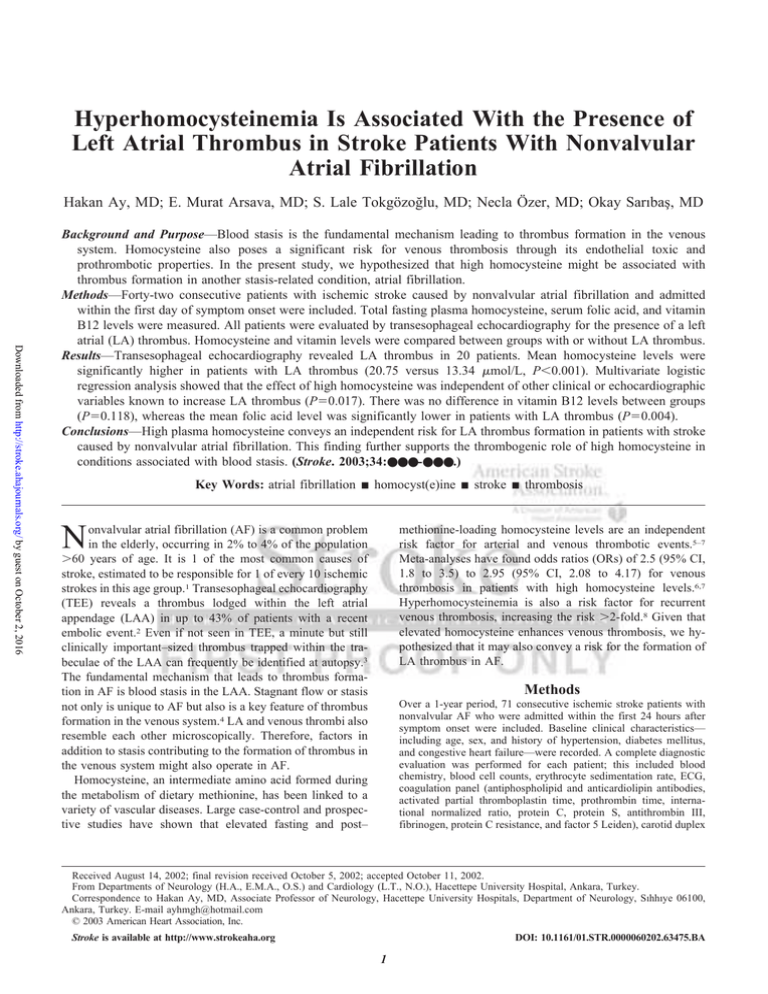
The mean⫹SE fasting plasma homocysteine level was
higher in patients with than in those without LA thrombus
(20.75 versus 13.34 mol/L; P⬍0.001; the Figure). Homo-
Ay et al
Downloaded from http://stroke.ahajournals.org/ by guest on October 2, 2016
Mean (SE) homocysteine levels with respect to the presence of
LA thrombus.
cysteine values ranged from 11.64 to 40.55 mol/L in
patients with LA thrombus and from 10.47 to 22.00 mol/L
in those without LA thrombus. Sixteen of 20 patients with
and 4 of 22 patients without LA thrombus had homocysteine
levels exceeding the cutoff value of 15 mol/L (P⬍0.001).
Multivariate logistic regression analysis identified elevated
fasting plasma homocysteine as an independent risk factor for
LA thrombus (P⫽0.017). The OR adjusted for the presence
of SEC and LA dilatation was 14.25 (95% CI, 2.70 to 75.14)
for homocysteine levels ⬎15 mol/L.
Serum folic acid and vitamin B12 measurements were
obtained in a subset of 26 patients admitted consecutively
within the last 8 months of the study period. An LA thrombus
was found on TEE in 12 of the 26 patients. The Table
summarizes the mean, lowest, and highest values of vitamin
B12 and folic acid in each group. Vitamin B12 and folic acid
levels were below the lower reference value in 1 patient each.
Both of these patients exhibited LA thrombus on TEE. There
was no difference in vitamin B12 levels with respect to
the presence of LA thrombus (P⫽0.118). In contrast, the
mean serum folic acid level was significantly lower in
patients with LA thrombus on TEE (P⫽0.004). The levels
of folic acid were inversely correlated with homocysteine
levels (r⫽⫺0.477, P⫽0.014).
Discussion
Homocysteine is a multipotent molecule exerting various
modes of injury to the endothelium. It facilitates oxidative
arterial injury, damages the vascular matrix, and induces
vascular smooth muscle proliferation.10,11 Moreover, homocysteine alters the thrombotic properties of the endothelium
by inhibiting the expression of thrombomodulin, activating
protein C, enhancing the activity of factors 12 and 5, and
augmenting platelet adhesion to the endothelial cells.12,13 The
interference of homocysteine with the coagulation system
creates a prothrombotic milieu. Virchow’s postulates for
thrombogenesis require abnormalities of blood flow, vessel
Homocysteine and Left Atrial Thrombus in AF
3
wall, and blood constituents. High homocysteine fulfills the 2
criteria of Virchow’s triad by its endothelial toxic and
prothrombotic properties. Therefore, one can postulate that in
conditions associated with abnormal blood flow such as
stasis, high levels of homocysteine enhance thrombus formation. Indeed, elevated homocysteine has been linked closely
to venous thrombosis, which is almost always associated with
blood stasis.4 The present study is the first to question the
thrombogenic role of homocysteine in another stasis-related
condition, AF. In accordance with the venous thrombosis
data, elevated homocysteine exhibited an association with the
presence of LA thrombus; the mean fasting plasma homocysteine level was significantly higher in patients with LA
thrombus compared with that in patients with no thrombus.
Moreover, this association was independent of other clinical
and echocardiographic parameters known to be associated
with LA thrombus formation. The only other study of
homocysteine in patients with AF, by Friedman,14 revealed
no difference in homocysteine levels among those with or
without AF. However, homocysteine levels were significantly higher in a subset of AF patients with a history of
stroke than in those who had AF but no stroke. Although
Friedman did not stratify AF patients with respect to the
presence of thrombus, his results are still in line with those of
the present study because patients with AF and stroke are
more likely to harbor an LA thrombus.1
In AF, the fibrillating LA creates a milieu for blood stasis,
most prominently in the LAA. This can be qualitatively
detected on echocardiography as SEC, a phenomenon characterized by smokelike echoes swirling in the LA, resulting
from a stasis-induced, increased erythrocyte aggregation.15
Likewise, LAA outflow velocity measurements serve as a
quantitative marker for blood stasis in LAA. Both the
presence of SEC and reduced LAA peak outflow velocity
(⬍20 cm/s) have been shown to convey an independent risk
for thrombus formation in LAA.16 In addition to stasis,
various markers of hypercoagulable state such as factor 8,
fibrinogen, D-dimer, prothrombin fragment 1.2, and von
Willebrand factor have been shown to increase in AF.17–20
The presence of a prothrombotic state is important because it
ties Virchow’s criteria to thrombus formation in AF. However, this is not sufficient to establish a causal relationship
because LA thrombus in AF might be a trigger rather than a
result of elevated hemostatic markers. Homocysteine is different than conventional hemostatic factors because it is
neither a direct contributor to the coagulation pathway such
as coagulation factors nor a byproduct of the thrombotic
(such as fibrinopeptide A and prothrombin fragment 1.2) or
fibrinolytic (such as D-dimer) systems. Unlike most other
hemostatic factors, homocysteine levels do not increase in the
acute phase of thrombotic episodes such as acute coronary
events and stroke.21,22 Therefore, the independent association
between high homocysteine and LA thrombus demonstrated
in the present study is highly suggestive of a causal relationship. However, it is not possible to be certain about a causal
relationship without confirming such an association in a
prospective design.
The present study is the first to demonstrate a relationship
between LA thrombus in AF and lower folic acid levels. Folic
4
Stroke
April 2003
Downloaded from http://stroke.ahajournals.org/ by guest on October 2, 2016
acid plays a key role as a cofactor in the process of the
remethylation of homocysteine to form methionine.23 It has
previously been shown that as folic acid levels decrease,
homocysteine levels increase.24 Subnormal levels of folic
acid are associated with moderately elevated homocysteine
levels.25,26 Accordingly, homocysteine levels showed an inverse but modest correlation with serum levels of folic acid in
the present study. This association suggests that the homocysteine elevations observed in our cohort might have been
caused in part by low folic acid levels.
Some limitations may apply to the present study. First,
LAA outflow velocities were not measured and therefore
were not included in the logistic regression analysis. However, the presence of SEC and the increased LA diameter are
also strong markers of LA stasis and were included in the
analyses. The persistence of a significant association between
high homocysteine and LA thrombus after adjustment for
these factors strongly suggests that the effect of homocysteine
on the LA thrombus is independent of the degree of LA stasis.
Second, homocysteine levels increase after stroke; thus,
measurements obtained after stroke may not reflect the levels
before stroke.22 It has previously been shown that homocysteine levels in stroke patients and in control subjects are
similar when measured in the acute phase of stroke (mean, 2
days).22 However, prominent increases occur in the convalescent phase.22,27 Therefore, we performed homocysteine
measurements within 48 hours of stroke onset. It is also
conceivable that any change with respect to baseline would
have an impact on our whole study population because all
patients had stroke, thereby reducing the bias that might
influence comparisons.
Accurate identification and proper management of risk
factors predisposing to thrombus formation in the LA are
critical to minimize the embolic complications of AF. Such
attempts might be more important in patients who cannot
continuously and effectively use warfarin because of contraindications. The link between high homocysteine levels and
LA thrombus established in the present study raises the
question of whether homocysteine-lowering therapies could
be an appropriate candidate for this task. It is possible to
reduce plasma homocysteine levels with folic acid therapy at
a dosage between 0.5 and 5 mg/d by ⬇25%, even in people
who are not vitamin deficient.28 The efficacy of such a
measure in reducing the stroke rate in AF remains to be tested
in future studies.
References
1. Hart RG, Halperin JL. Atrial fibrillation and stroke: concepts and controversies. Stroke. 2001;32:803– 808.
2. Manning WJ, Silverman DI, Waksmonski CA, Oettgen P, Douglas PS.
Prevalence of residual left atrial thrombi among patients with acute
thromboembolism and newly recognized atrial fibrillation. Arch Intern
Med. 1995;155:2193–2198.
3. Fisher CM. Embolism in atrial fibrillation. In: Kulbertus HE, Olsson SB,
Schlepper M, eds. In: Atrial Fibrillation. Moindal, Sweden: Alindgren &
Soner AB; 1981:192.
4. Thomas D. Venous thrombogenesis. Br Med Bull. 1994;50:803– 812.
5. Ford ES, Smith SJ, Stroup DF, Steinberg KK, Mueller PW, Thacker SB.
Homocyst(e)ine and cardiovascular disease: a systematic review of the
evidence with special emphasis on case-control studies and nested casecontrol studies. Int J Epidemiol. 2002;31:59 –70.
6. den Heijer M, Rosendaal FR, Blom HJ, Gerrits WB, Bos GM. Hyperhomocysteinemia and venous thrombosis: a meta analysis. Thromb
Haemost. 1998;80:874 – 877.
7. Ray JG. Meta-analysis of hyperhomocysteinemia as a risk factor for
venous thromboembolic disease. Arch Intern Med. 1998;158:2101–2106.
8. Eichinger S, Stumpflen A, Hirschl M, Bialonczyk C, Herkner K, Stain M,
Schneider B, Pabinger I, Lechner K, Kyrle PA. Hyperhomocysteinemia is
a risk factor of recurrent venous thromboembolism. Thromb Haemost.
1998;80:566 –569.
9. Henry WL, DeMaria A, Gramiak R, King DL, Kisslo JA, Popp RL, Sahn DJ,
Schiller NB, Tajik A, Teichholz LE, Weyman AE. Report of the American
Society of Echocardiography Committee on Nomenclature and Standards in
Two-Dimensional Echocardiography. Circulation. 1980;62:212–217.
10. Tsai JC, Perrella MA, Yoshizumi M, Hsieh CM, Haber E, Schlegel R, Lee ME.
Promotion of vascular smooth muscle cell growth by homocysteine: a link to
atherosclerosis. Proc Natl Acad Sci U S A. 1994;91:6369–6373.
11. Lang D, Kredan MB, Moat SJ, Hussain SA, Powell CA, Bellamy MF,
Powers HJ, Lewis MJ. Homocysteine-induced inhibition of endotheliumdependent relaxation in rabbit aorta: role for superoxide anions. Arterioscler Thromb Vasc Biol. 2000;20:422– 427.
12. Ling Q, Hajjar KA. Inhibition of endothelial cell thromboresistance by
homocysteine. J Nutr. 2000;130(suppl 2S):373S–376S.
13. Dardik R, Varon D, Tamarin I, Zivelin A, Salomon O, Shenkman B, Savion
N. Homocysteine and oxidized low density lipoprotein enhanced platelet
adhesion to endothelial cells under flow conditions: distinct mechanisms of
thrombogenic modulation. Thromb Haemost. 2000;83:338–344.
14. Friedman HS. Serum homocysteine and stroke in atrial fibrillation. Ann
Intern Med. 2001;134:253–254.
15. Fatkin D, Herbert E, Feneley MP. Hematologic correlates of spontaneous
echo contrast in patients with atrial fibrillation and implications for
thromboembolic risk. Am J Cardiol. 1994;73:672– 676.
16. Shively BK, Gelgand EA, Crawford MH. Regional left atrial stasis during
atrial fibrillation and flutter: determinants and relation to stroke. J Am
Coll Cardiol. 1996;27:1722–1729.
17. Gustafsson C, Blomback M, Britton M, Hamsten A, Svensson J. Coagulation factors and the increased risk of stroke in nonvalvular atrial
fibrillation. Stroke. 1990;21:47–51.
18. Lip GY, Lowe GD, Rumley A, Dunn FG. Fibrinogen and fibrin D-dimer
levels in paroxysmal atrial fibrillation: evidence for intermediate elevated
levels of intravascular thrombogenesis. Am Heart J. 1996;131:724 –730.
19. Mitusch R, Siemens HJ, Garbe M, Wagner T, Sheikhzadeh A, Diederich
KW. Detection of a hypercoagulable state in nonvalvular atrial fibrillation
and the effect of anticoagulant therapy. Thromb Haemost. 1996;75:219–223.
20. Li-Saw-Hee FL, Blann AD, Lip GY. A cross-sectional and diurnal study
of thrombogenesis among patients with chronic atrial fibrillation. J Am
Coll Cardiol. 2000;35:1926 –1931.
21. Egerton W, Silberberg J, Crooks R, Ray C, Xie L, Dudman N. Serial
measures of plasma homocyst(e)ine after acute myocardial infarction.
Am J Cardiol. 1996;77:759 –761.
22. Lindgren A, Brattstrom L, Norrving B, Hultberg B, Andersson A,
Johansson BB. Plasma homocysteine in the acute and convalescent
phases after stroke. Stroke. 1995;26:795– 800.
23. Finkelstein JD. The metabolism of homocysteine: pathways and regulation. Eur J Pediatr. 1998;157(suppl 2):S40 –S44.
24. Brattstrom L. Vitamins as homocysteine lowering agents. J Nutr. 1996;
126(suppl 4):1276S–1280S.
25. Kang SS, Wong PW, Norusis M. Homocysteinemia due to folate deficiency. Metabolism. 1987;36:458 – 462.
26. Stabler SP, Marcell PD, Podell ER, Allen RH, Savage DG, Lindenbaum
J. Elevation of total homocysteine in the serum of patients with cobalamin
or folate deficiency detected by capillary gas chromatography-mass spectrometry. J Clin Invest. 1988;81:466 – 474.
27. Meiklejohn DJ, Vickers MA, Dijkhuisen R, Greaves M. Plasma homocysteine concentrations in the acute and convalescent periods of atherothrombotic stroke. Stroke. 2001;32:57– 62.
28. Lowering blood homocysteine with folic acid based supplements: metaanalysis of randomised trials: Homocysteine Lowering Trialists’ Collaboration. BMJ. 1998;316:894 – 898.
Hyperhomocysteinemia Is Associated With the Presence of Left Atrial Thrombus in
Stroke Patients With Nonvalvular Atrial Fibrillation
Hakan Ay, E. Murat Arsava, S. Lale TokgözoGlu, Necla Özer and Okay Saribas
Downloaded from http://stroke.ahajournals.org/ by guest on October 2, 2016
Stroke. published online February 27, 2003;
Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2003 American Heart Association, Inc. All rights reserved.
Print ISSN: 0039-2499. Online ISSN: 1524-4628
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://stroke.ahajournals.org/content/early/2003/02/27/01.STR.0000060202.63475.BA.citation
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click
Request Permissions in the middle column of the Web page under Services. Further information about this
process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Stroke is online at:
http://stroke.ahajournals.org//subscriptions/