Cell Transplantation, Vol. 21, pp. 2621–2634, 2012
Printed in the USA. All rights reserved.
Copyright 2012 Cognizant Comm. Corp.
0963-6897/12 $90.00 + .00
DOI: http://dx.doi.org/10.3727/096368912X647153
E-ISSN 1555-3892
www.cognizantcommunication.com
Application of Human Persistent Fetal Vasculature Neural
Progenitors for Transplantation in the Inner Retina
Guochun Chen,*† Jie Ma,† Marie A. Shatos,† Huihui Chen,† Desirée Cyr,† and Kameran Lashkari†
*Department of Nephrology, The Second Xiangya Hospital,
Central South University, Changsha, Hunan, P.R. China
†Schepens Eye Research Institute, Massachusetts Eye and Ear,
Department of Ophthalmology, Harvard Medical School, Boston, MA, USA
Persistent fetal vasculature (PFV) is a potentially serious developmental anomaly in human eyes, which results
from a failure of the primary vitreous and the hyaloid vascular systems to regress during development. Recent
findings from our laboratory indicate that fibrovascular membranes harvested from subjects with PFV contain
neural progenitor cells (herein called NPPFV cells). Our studies on successful isolation, culture, and characterization of NPPFV cells have shown that they highly express neuronal progenitor markers (nestin, Pax6, and Ki67)
as well as retinal neuronal markers (b-III-tubulin and Brn3a). In the presence of retinoic acid and neurotrophins,
these cells acquire a neural morphological appearance in vitro, including a round soma and extensive neurites,
and express mature neuronal markers (b-III-tubulin and NF200). Further experiments, including real-time qRTPCR to quantify characteristic gene expression profiles of these cells and Ca2+ imaging to evaluate the response
to stimulation with different neurotransmitters, indicate that NPPFV cells may resemble a more advanced stage
of retinal development and show more differentiation toward inner retinal neurons rather than photoreceptors.
To explore the potential of inner retinal transplantation, NPPFV cells were transplanted intravitreally into the
eyes of adult C57BL/6 mice. Engrafted NPPFV cells survived well in the intraocular environment in presence
of rapamycin and some cells migrated into the inner nuclear layer of the retina 1 week posttransplantation. Three
weeks after transplantation, NPPFV cells were observed to migrate and integrate in the inner retina. In response
to daily intraperitoneal injections of retinoic acid, a portion of transplanted NPPFV cells exhibited retinal ganglion cell-like morphology and expressed mature neuronal markers (b-III-tubulin and synaptophysin). These
findings indicate that fibrovascular membranes from human PFV harbor a population of neuronal progenitors
that may be potential candidates for cell-based therapy for degenerative diseases of the inner retina.
Key words: NPPFV (persistent fetal vasculature-derived neural progenitor) cell; Transplantation; Differentiation;
Retinal ganglion cell (RGC); Retina
INTRODUCTION
Inner retinal degenerative diseases, such as selective
and progressive loss of retinal ganglion cells (RGCs),
pose a major threat to vision (50,51). Currently, there
is no effective cure or treatment to reverse the loss of
RGCs. Transplantation of stem or progenitor cells may
have great therapeutic potential for treatment of neurodegenerative diseases, in general, and for the retina, in
particular, by providing therapeutic benefits through both
neuroprotective and cell replacement mechanisms (7,38).
In recent years, various neural stem or progenitor cells
have been tested to determine their potential to integrate
into the host retina after transplantation (1,2,8,31). The
regenerative potential of cell transplantation has already
been shown for the outer retina (1,35). Studies have shown
that subretinal transplantation of postmitotic photoreceptor progenitors or embryonic stem cell-derived photoreceptors permitted integration and photoreceptor-specific
differentiation of engrafted cells, and even functional
recovery in rhodopsin-deficient or cone-rod homeobox
(Crx)-deficient host mice (35,43). However, it seems to
be more difficult to achieve similar success for replacement of RGCs, as they adopt highly specialized properties
and form numerous synaptic connections with other neurons (24). Due to the inhibitory environment present in
the adult neural retina and lineage restriction of engrafted
cells, limited integration and RGC-specific differentiation of engrafted cells has been found in the inner retina
when cells have been intravitreally transplanted into the
uninjured eye (6,26,47). Targeted disruption of glial cell
Received September 8, 2010; final acceptance February 10, 2012. Online prepub date: June 15, 2012.
Address correspondence to Kameran Lashkari, M.D., Schepens Eye Research Institute, Massachusetts Eye and Ear, Harvard Medical School,
20 Staniford Street, Boston, MA 02114, USA. Tel: +1-617-912-7461; E-mail: kameran.lashkari@schepens.harvard.edu
2621
2622
activity and modification of the local environment with
chemicals or by genetic manipulation have proven to
facilitate infiltration of engrafted cells (23,30).
However, few of these methods can be directly applied
in a clinical setting, considering the obvious side effects
on other retinal resident cells. If any possible therapeutic effects of replacing lost RGCs with transplanted stem
cells are to be achieved for degenerative inner retinal
conditions, it is essential that a suitable cell type be chosen for transplantation and a more biocompatible method
be used to facilitate the integration and differentiation of
engrafted cells in the host tissue. Indeed, glaucoma may
not be the only inner retinal condition that could benefit
from restoration of the RGCs. It is possible that RGC
replacement could be applied to other diseases that result
in the death or dysfunction of RGCs, such as ischemic
optic neuropathy, optic neuritis, and inherited mitochondrial optic neuropathies.
In this study, we report a novel neural progenitor cell
type isolated from human persistent fetal vascular tissue.
In this condition, the hyaloidal vascular system that nourishes the developing lens fails to regress, leaving a whitish membrane in the anterior vitreous behind the lens.
We recently discovered that this tissue contains neural
progenitor cells. We first examined whether these persistent fetal vasculature-derived neural progenitor (NPPFV)
cells exhibited characteristics of neuronal progenitor cells
(such as antigenic and genetic profiles) and whether they
were capable of differentiating into retinal neurons in
vitro. To explore whether NPPFV cells have potential for
cell-based inner retinal transplantation therapy, we intravitreally transplanted NPPFV cells into adult C57BL/6
mice and examined their integration and differentiation
in the inner retina.
MATERIALS AND METHODS
Isolation and PFV Cell Culture
Persistent fetal vasculature (PFV) membranes (Fig. 1A,
insert) were obtained from young donors during corrective surgery performed by Dr. Tatsuo Hirose at the
Massachusetts Eye and Ear Infirmary (MEEI). Removal
of the membranes strictly adhered to the tenets of the
Declaration of Helsinki approved by the Human Subjects
Internal Review Board of MEEI and Schepens Eye
Research Institute. Upon receipt of the PFV membrane, the
tissue was placed in 1× phosphate-buffered saline (PBS)
containing 3× concentration of penicillin–streptomycin,
finely minced, placed in 0.1% type 1 collagenase (Invitrogen,
Carlsbad, CA, USA), and agitated for 20–30 min
at room temperature. Liberated cells in the collagenase
solution were collected, forced through a 70-µm sieve,
centrifuged, and plated in X-vivo medium (Lonza,
Watersville, MD, USA) supplemented with 10% fetal
bovine serum (FBS, Invitrogen), 1:50 B27 (Invitrogen),
Chen ET AL.
1:100 N2 (Invitrogen), 10 ng/ml basic fibroblast growth
factor (bFGF; Invitrogen), 20 ng/ml epidermal growth
factor (EGF; Invitrogen), and 50 μg/ml nystatin (Sigma,
St. Louis, MO, USA). Additional collagenase was added
to the remaining tissue until all tissue was dissociated.
Cells were seeded on 24-well tissue culture plates following each cycle and incubated at 37°C in a humidified 95% air and 5% CO2 environment. After 24–48 h,
neurospheres were observed in the culture medium and
transferred to fibronectin-coated tissue culture flasks
in X-vivo medium with supplements described above.
Cells were fed every 2 days and passaged or frozen
down 75–80% confluence. At passage 5, a subset of cells
was also cultured in differentiation medium consisting
of all-trans-retinoic acid (100 nM, Sigma), brain-derived
neurotrophic factor (BDNF; 50 ng/ml, Invitrogen), ciliary neurotrophic factor (CNTF; 20 ng/ml, Invitrogen),
nerve growth factor (NGF; 20 ng/ml, Invitrogen), and
10% FBS. Cells then were examined for morphological
features, antigenic profiles, gene expression, and neuro­
transmitter receptors.
Immunocytochemical Examination
NPPFV cells were seeded on slide chambers (VWR,
Batavia, IL, USA) and cultured in a differentiationconditioned medium for at least 7 days or in normal
growth medium for examining their antigenic profiles.
Cells were fixed for 10 min in 4% buffered parafor­
maldehyde, washed in PBS, and blocked with 10%
goat serum (Vector, Burlingame, CA, USA)/PBS solution for 30 min before immunocytochemical staining.
Primary antibodies [including b-III-tubulin (Sigma),
nestin (Sigma), paired box 6 (Pax6; Chemicon-Millipore,
Billerica, MA, USA), Ki67 (Vector), brain-specific
homeobox/POU domain protein 3A (Brn3a; Chemicon),
bromodeoxyuridine (Brdu; Abcam, Cambridge, MA,
USA), NF200 (neurofilament-200, Sigma), recoverin
(Chemicon), retinal pigment epithelium-specific 65 kDa
protein (RPE-65; Chemicon), cellular retinaldehydebinding protein (CRALBP; Abcam), glial fibrillary
acidic protein (GFAP; Sigma), a-smooth muscle actin
(a-SMA; Abcam), fibroblast-specific protein 1 (FSP1;
Sigma), cluster of differentiation 31 (CD31; Abcam)]
were diluted in 2% goat serum/PBS solution to appropriate concentrations for incubating cells at 4°C overnight. Cells were rinsed with PBS and incubated with a
secondary antibody consisting of either cyanine 3 (Cy3;
Chemicon 1:500) or fluorescein isothiocyanate (FITC;
Chemicon 1:300) at room temperature for 30 min on the
following day. After rinsing in PBS, slides were mounted
with Vectashield mounting medium containing DAPI
(Vector) and visualized under an inverted fluorescence
microscope (Olympus 1X51). All immunocytochemical
analyses were repeated three or more times from the cells
hNPPFV FOR RETINAL TRANSPLANTATION
2623
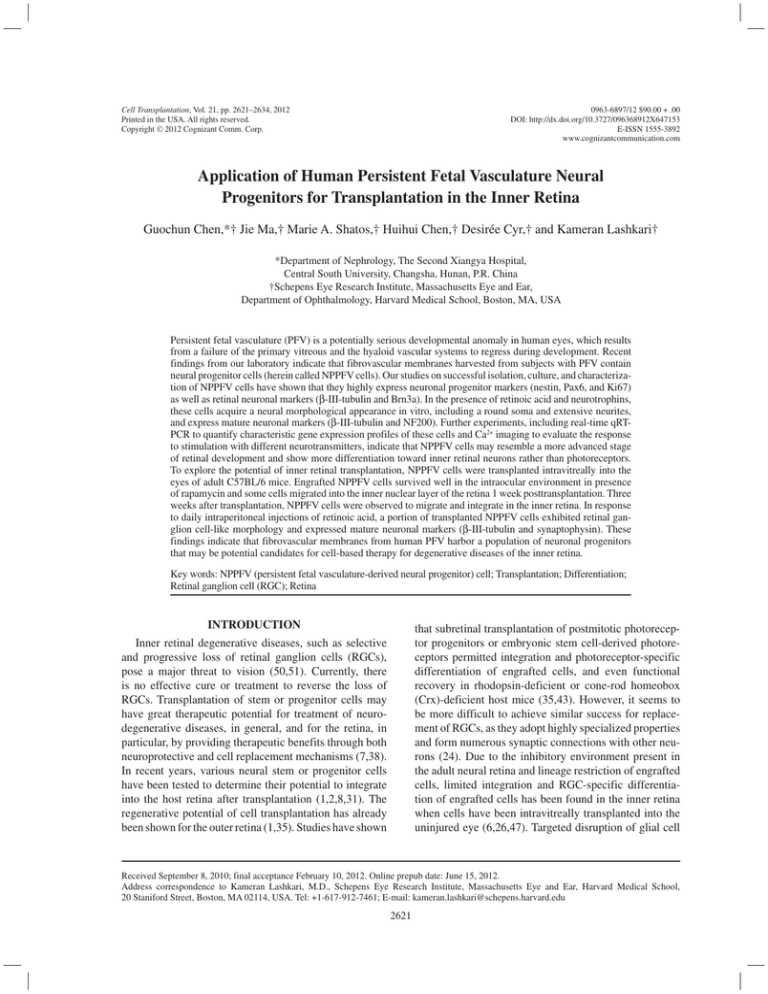
Figure 1. Characterization of neural progenitors derived from persistent fetal vasculature (NPPFV) cells. Fundus view of a subject
with persistent fetal vasculature (PFV) shows a whitish membrane in the anterior vitreous behind the lens (A, insert). Neurospheres
of liberated NPPFV cells in subsequent passage (A). Neurospheres spread on fibronectin-coated plates (B). Coexpression of nestin
(green fluorescence) and paired box protein 6 (Pax6; nuclear red fluorescence) in freshly dissected PFV membrane indicates presence of neural progenitors (C). Immunostaining of typical markers expressed by undifferentiated NPPFV cells (D–H) at passage 2.
Incorporation of bromodeoxyuridine (Brdu; red nuclear fluorescence) and b-III-tubulin (green fluorescence) indicates that NPPFV
cells have distinct populations. Proliferative NPPFV cells uptake Brdu have smaller morphology and fewer projections (I). Cultured
NPPFV cells differentiated at passage 2 in a retinoic acid (RA) enriched conditioned medium and develop mature neuronal morphological appearance including a round soma and extensive neurites (J). Expression of b-III-tubulin (K) and neurofilament 200 (NF200) (L)
in RA-differentiated NPPFV cells. Scale bar: 100 µm. Brn3a, brain-specific homeobox/POU domain protein 3A.
at passages 2–5. Related isotype immunoglobulins were
used as negative controls (Chemicon).
Evaluation of Gene Expression by Real-Time qRT-PCR
To determine the gene profiles of NPPFV cells, realtime qRT-PCR was performed to compare designated
mRNA expression of NPPFV cells with those of human
retinal progenitor cells (hRPCs). hRPCs have been isolated from human fetal tissue and well characterized
in vitro (1,32,62). The hRPCs used in this study were
supplied by the laboratory of Dr. Michael J. Young at
SERI, and the isolation procedures for those cells have
been well addressed in a previous study (32). In brief,
retinas of donors with an estimated age of 18 weeks of
gestation were cut into small pieces on a dry Petri dish
under a tissue culture hood and enzymatically digested
in a sterile container at 37°C with periodic removal of
supernatants and refilling with fresh digestion solution.
2624
Chen ET AL.
Harvested cells from the supernatants after centrifugation were resuspended in cell-free retinal progenitorconditioned medium, and then cells were transferred to
fibronectin-coated tissue culture flasks containing fresh
media. In the present study, both cell types (NPPFV and
RPC) from passage 0 were cultured in the same medium
after the original isolation from tissue samples to eliminate any possible influence from different culture conditions on their respective gene expressions. The mRNA
expression of various transcription factors and retinalspecific proteins has been detected by PCR in early
passages of cultured hRPCs (1). Therefore, hRPCs can
serve as a well-established control for NPPFV cells in
real-time qPCR experiments. Total RNA was extracted
from NPPFV cells and hRPCs (both at passage 5) using
an RNA isolation kit (Qiagen, RNeasy Mini Kit). To
ensure samples without genomic DNA contamination,
total RNA was treated with DNase (Qiagen, RNase-Free
DNase Set) and cDNA was synthesized using a Synthesis
Kit (Bio-rad). Total cDNA (1 µl) was loaded in each well,
mixed with PCR master mix (TaqMan Universal, Applied
Biosystems, Foster City, CA) and predesigned primers
(IDT, San Diego, CA) for Pax6, nestin, atonal homolog 7
(ATOH7), recoverin, rhodopsin, synaptosomal-associated protein 25 (SNAP25), syntaxin-binding protein 1
(STXBP1), receptor-associated protein of the synapse
(RAPSN), and THY1, respectively (listed in Table 1). The
procedure for real-time qRT-PCR included 2 min at 50°C,
15 min at 95°C, followed by 40 cycles of 15 s at 95°C,
30 s at 55°C, and 30 s at 72°C (ABI PRISM 7900 HT;
Applied Biosystems). Expression (evaluated as fold
change for each target gene) was normalized to glyceraldehyde 3-phosphate dehydrogenase (GAPDH; a housekeeping gene) in hRPCs following the well-established
∆-∆ method (52). All assays were performed in triplicate.
In addition, a nontemplate control was included in the
experiment to estimate DNA contamination of isolated
RNA and reagents.
Estimation of Intracellular Ca2+ in NPPFV Cells
To investigate the neurotransmitter receptor expression
on NPPFV cells, Ca2+ imaging was performed by loading
cells with the ratiometric Ca2+-sensitive Fura-2 dye. Briefly,
cells were incubated at 37°C for 30 min in X-vivo medium
(containing 3% FBS, 5 μM Fura-2 tetra-acetoxymethyl
ester, 8 μM pluronic acid F127, and 250 μM sulfinpyrazone).
Cells were washed in modified Mg2+-free Hank’s balanced
salt solution (HBSS, 2.6 mM CaCl2, 15 mM HEPES pH 7.4,
and 250 μM sulfinpyrazone). Five types of neurotransmitters, g-aminobutyric acid (GABA), glutamate (Glu), glycine
(Gly), dopamine (Dopa), and acetylcholine (Ach) were dissolved in modified HBSS at a concentration of 0.1 mM. The
largest dynamic range for Ca2+-dependent fluorescence signals is obtained by excitation at 340 and 380 nm, and their
ratio of emission fluorescence intensities was detected at
around 510 nm. From this ratio, the concentration of intracellular Ca2+ ([Ca2+]i) can be estimated, using dissociation
constants that are derived from calibration curves. By using
the ratio of fluorescence intensities produced by excitation
at two wave lengths, factors such as uneven dye distribution
and photo bleaching are minimized (InCyt Im2TM Ratio
Imaging System, Cincinnati, OH) (16,33). The change of
[Ca2+]i was calculated from the difference between the peak
Ca2+ concentration evoked by each agonist and the control
value of HBSS (before the addition of agonist). At least
80 cells were selected for analyzing the change of [Ca2+]i
evoked by each agonist, averaged over three repetitions.
Inner Retinal Transplantation
For studying their potential for inner retinal transplantation, NPPFV cells or hRPCs were intravitreally injected
to 20 and 10 C57BL/6 mice, respectively. Animals were
maintained in the animal facility of Schepens. All experimental procedures for transplantation were approved by
the Institute’s Animal Care and Use Committee and adhere
to the statement for the Use of Animals in Ophthalmic and
Vision Research. To trace the transplanted cells, NPPFV
Table 1. Applied Primers for Real-Time qRT-PCR
Genes
GenBank Accession
PAX6
NES
ATOH7
RCVRN
RHO
SNAP25
STXBP1
RAPSN
THY1
GAPDH
NM_000280
X65964
NM_145178
NM_002903
NM_000539
NM_003081
D63851
NM_005055
NM_006288
NM_002046
Sense Primers
5¢-AGGTATTACGAGACTGGCTCC-3¢
5¢-GAAACAGCCATAGAGGGCAAA-3¢
5¢-ACTGCCTTCGACCGCTTAC-3¢
5¢-CTCCTTCCAGACGATGAAAACA-3¢
5¢-GCTTCCCCATCAACTTCCTCA-3¢
5¢-ATGCCCGAGAAAATGAAATG-3¢
5¢-CGCCTCATCATTTTCATCCT-3¢
5¢-CTGCACTGTCTGAGCGAGAG-3¢
5¢-TGAAGGTCCTCTACTTATCCGC-3¢
5¢-ATGGGGAAGGTGAAGGTCG-3¢
Antisense Primers
5¢-TCCCGCTTATACTGGGCTATTT-3¢
5¢-TGGTTTTCCAGAGTCTTCAGTGA-3¢
5¢-CAGAGCCATGATGTAGCTCAG-3¢
5¢-GCCAGTGTCCCCTCAATGAA-3¢
5¢-AGTATCCATGCAGAGAGGTGTAG-3¢
5¢-AGCATCTTTGTTGCACGTTG-3¢
5¢-CATTGTTGGAGCCTGATCCT-3¢
5¢-ACCTGAGGTGGAAGATGTGG-3¢
5¢-GCACTGTGACGTTCTGGGA-3¢
5¢-GGGGTCATTGATGGCAACAATA-3¢
PAX6, paired box 6; NES, nestin; ATOH7, atonal homolog 7; RCVRN, recoverin; RHO, rhodopsin; SNAP25, synaptosomal-associated protein
(25 kDa); STXBP1, syntaxin-binding protein 1; RAPSN, receptor-associated protein of the synapse; THY1, Thy-1 cell surface antigen; GAPDH,
glyceraldehyde 3-phosphate dehydrogenase.
hNPPFV FOR RETINAL TRANSPLANTATION
cells and hRPCs were infected with an adeno-associated
virus 2 (AAV2) or retrovirus vector harboring enhanced
green fluorescent protein (EGFP; HGTI, Boston, MA)
following the instructions of each transfection kit, respectively. Mice (4–6 weeks of age) were deeply anesthetized
with an intraperitoneal injection of ketamine (120 mg/kg)
and xylazine (20 mg/kg), and pupils were dilated with 0.5%
topical tropicamide. Dissociated GFP-positive cells (1 × 105 cells/2 µl) were suspended in HBSS were transplanted
into the vitreous cavity of the eye through a glass micropipette connected to a 10-µl Hamilton syringe via polyethylene
tubing. Sham-injected mice received HBSS without cells.
All experimental animals received injection in one eye, and
the other eye was used as an untreated control. A small puncture in the cornea (paracenthesis) was used to reduce the
intraocular pressure during the transplantation surgery (1).
Rapamycin (2 mg/kg day) (LC Laboratories, Woburn, MA,
USA) was administered to all surgical animals to ensure
the survival of the xenograft (6,15). To facilitate the differentiation of engrafted NPPFV cells, 10 mice were given
intraperitoneal injections of retinoic acid (RA, 2 mg/kg day,
Sigma) starting 1 day prior to transplantation and continuing
until termination of the experiment. Of the 10 mice transplanted with hRPCs, five received rapamycin and the other
five received rapamycin and RA. Animals received terminal
anesthesia on week 1 or week 3 after transplantation, and
the eyes were harvested after intracardial perfusion with 4%
paraformaldehyde in PBS. Eyes were cryosectioned at 10 μm
and examined under a Lecia TSC SP5 confocal microscope
to evaluate the expression and location of different markers. Anti-GFP antibody (1:100, Abcam) was used to enhance
the fluorescence of prelabeled-GFP, while anti-b-III-tubulin
(1:500, Sigma, USA), anti-GFAP (1:300, Sigma, USA), and
anti-synaptophysin (1:100, Dako, Carpinteria, CA) antibodies helped to assess the differentiation of transplanted cells.
To estimate the survival and migration of grafted cells, we
performed serial sections on four randomly selected eyes
that had undergone NPPFV transplantation. We manually
counted every 10th serial section, measuring 10 µM in thickness as to avoid redundancy of cell counts.
Statistical Analysis
Statistical analysis was performed using the SPSS 12.0
software package. Results are expressed as mean ± SEM
(standard error of mean). Differences between groups
were compared by using one-way ANOVA followed up
with Tukey’s test or t test, as appropriate, and two-tailed
p values are reported.
RESULTS
Immunocytochemical Characterization of NPPFV Cells
Following surgical dissection of clinical PFV membranes (funduscope of PFV subject) (Fig. 1A, inset) and
subsequent isolation of cell contents, cells were collected
2625
and seeded in neural-supporting medium. As the cells were
passaged, neurospheres began to emerge from the cultured
NPPFV cells (Fig. 1A). Neurospheres were spread onto
fibronectin-coated plates from which some cells grew long
and slender projections shortly after the transfer (Fig. 1B).
Immunofluorescent imaging of PFV tissue confirmed that
some cellular elements in PFV coexpressed Pax6 (red
nuclei) and nestin (green filaments) (Fig. 1C), indicating
that PFV tissue contains some neural progenitors. Using
immunochemical staining for nestin and/or Pax6, we estimate that about 0.2% (±0.16%) of resident cells in PFV
membrane are neuronal progenitors (Fig. 1C). Although the
population of those cells is relatively small, the cells are
able to stably maintain their progenitor phenotype and normally proliferate in cultural conditions (see Materials and
Methods). After being expanded up to 20 passages, characteristic markers of neuronal progenitors and retinal neurons were confirmed in the cultured NPPFV cells, including
b-III-tubulin, nestin, Pax6, ki67, and Brn3a (Fig. 1D–H).
Further incorporation of Brdu and β-III-tubulin staining revealed a subpopulation of proliferating NPPFV
cells that were smaller in size with fewer projections than
their nondividing counterparts in the same batch (Fig. 1I).
After treatment with RA-enriched medium, NPPFV cells
exhibited a typical neuronal morphological appearance,
including a round soma and extensive neurites (Fig. 1J).
Immunolabeling confirmed that differentiated NPPFV
cells only expressed β-III-tubulin (Fig. 1K) and NF200
(Fig. 1L) and not the other aforementioned markers.
NPPFV cells were also investigated to exclude any possible contamination with other cell types by screening
for the following markers: photoreceptors (recoverin),
retinal pigment epithelia (RPE65), astroglia (CRALBP,
GFAP), myofibroblasts (a-SMA), fibroblasts (FSP1),
and endothelia (CD31). But none of these markers were
detected in NPPFV cells (summarized in Table 2).
Gene Expression Profile of NPPFV Cells
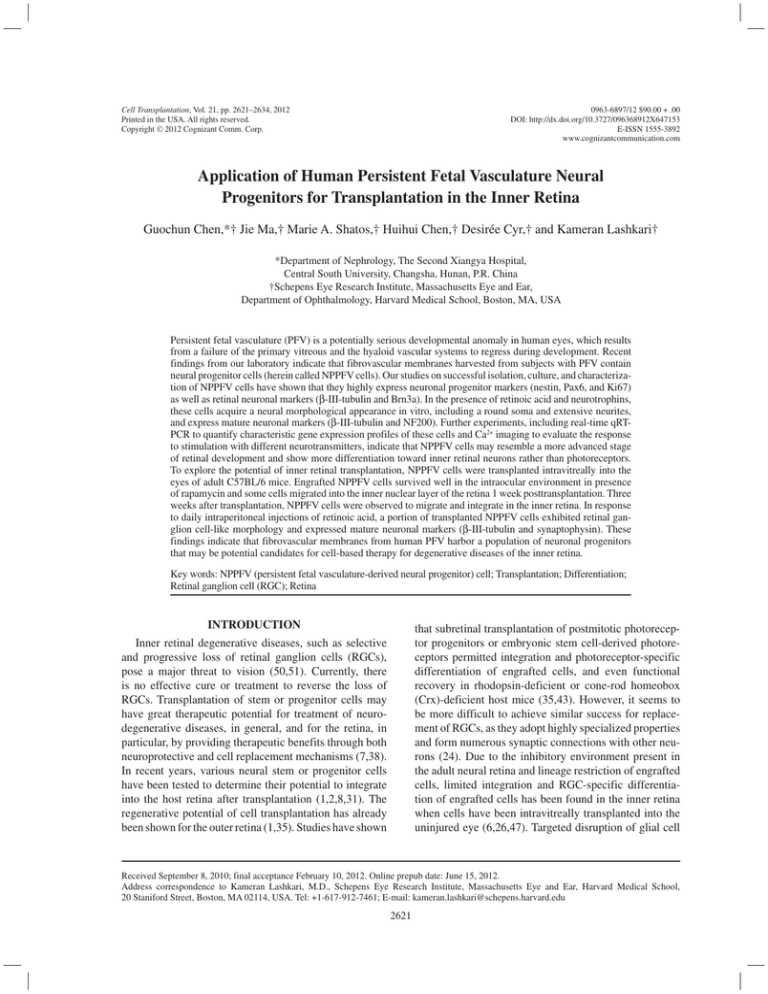
Characteristic markers of retinal progenitors [Pax6,
nestin (NES) and ATOH7], photoreceptors [recoverin
(RCVRN) and rhodopsin (RHO)], synapse-related proteins (SNAP25, STXBP1, and RAPSN), and retinal ganglion cell (THY1) were selected to establish the gene
expression profile of NPPFV cells. Real-time qRT-PCR
revealed lower expression of retinal progenitor and photoreceptor markers in NPPFV cells than in hRPCs (t test, all
p < 0.05) (Fig. 2). However, mRNA levels of the synapserelated proteins and of THY1 (a mature retinal ganglion
cell marker) were significantly higher in NPPFV cells than
in hRPCs (t test, all p < 0.05) (Fig. 2). These observations
indicated that NPPFV cells are a type of tissue-specific
progenitor in the retina with higher potential for differentiating toward inner retinal neurons (such as retinal ganglion cells) rather than photoreceptors.
2626
Chen ET AL.
Table 2. Antigenic Profiles of Cultured NPPFV Cells
Antigens
Specification of Cell Types
Undifferentiated Cells
Differentiated Cells
β-III-tubulin
Nestin
Pax6
Ki67
Brn3a
Brdu
NF200
Recoverin
RPE-65
CRALBP
GFAP
α-SMA
FSP1
CD31
Neuron
Neuronal progenitor
Neuronal progenitor
Proliferative cell
Neuron
Proliferative cell (S phase)
Neuron
Photoreceptor
Retinal pigment epithelium
Müller glial cell
Glial/astrocytic cell
Myofibroblast
Fibrocyte/fibroblast
Endothelial cells
+
+
+
+
+
+
Equivocal
−
−
−
−
−
−
−
+
−
−
−
Equivocal
−
+
−
−
−
−
−
−
−
Brn3a, brain-specific homeobox/POU domain protein 3A; Brdu, bromodeoxyuridine; NF200, neurofilament-200; RPE-65,
retinal pigment epithelium-specific 65 kDa protein; CRALBP, cellular retinaldehyde-binding protein; GFAP, glial fibrillary
acidic protein; α-SMA, α-smooth muscle actin; FSP1, fibroblast-specific protein 1; CD31, cluster of differentiation 31.
Determination of Relative Levels
of Intracellular Calcium
The relative number of undifferentiated and differentiated NPPFV cells was determined, and their Ca2+ concentration was tested using Fura-2 dye after stimulation with
different neurotransmitters. A very small portion of undifferentiated and differentiated NPPFV cells responded to Dopa
(6.41 ± 7.14% vs. 7.89 ± 9.18%), Ach (10.96 ± 8.12% vs.
8.23 ± 5.41%), GABA (14.94 ± 11.73% vs. 12.99 ± 4.86%),
and Gly (16.67 ± 10.62% vs. 21.05 ± 9.72%), and no
Figure 2. Gene expression profiles of undifferentiated NPPFV
and human retinal progenitor cells (hRPCs) by the real-time
qRT-PCR at passage 5. NES, nestin; RCVRN, recoverin;
RHO, rhodopsin; SNAP25, synaptosomal-associated protein
(25 kDa); STXBP1, syntaxin-binding protein 1; RAPSN, receptor-associated protein of the synapse; THY1, Thy-1 cell surface
antigen; hRPC, human retinal progenitor cell; P5, passage 5.
*p < 0.05 and **p < 0.01.
significant difference was found in each group (t test,
all p > 0.05). However, Glu stimulation elicited a large
response in undifferentiated and differentiated NPPFV cells
(48.98 ± 11.67% vs. 87.88 ± 4.97%) compared to other transmitters (one-way ANOVA, p < 0.01). In addition, Glu evoked
a response in a higher proportion of differentiated NPPFV
cells than undifferentiated cells (t test, p < 0.01) (Fig. 3A).
Some cells that responded to neurotransmitter stimulation were selected for measurements of relative [Ca2+]i
(Fig. 3B, white arrows). A limited number of NPPFV cells
responded to stimulation with Dopa, Ach, GABA, and
Gly. Interestingly, the elicited [Ca2+]i of these cells was
also quite low, with little or no difference between differentiated and undifferentiated NPPFV cells. Glu elicited a
significant increase in the concentration of Ca2+ in undifferentiated and differentiated NPPFV cells compared
to the rest of the neurotransmitters examined (one-way
ANOVA, all p < 0.01) (Fig. 3C). Glu stimulation elicited
a higher [Ca2+]i in differentiated than in undifferentiated
cells (t test, p < 0.01) (Fig. 3C).
Survival and Migration of Transplanted
NPPFV Cells and hRPCs
Transplanted NPPFV cells were tracked in vivo by their
expression of EGFP, which was enhanced by anti-GFP
antibody staining. DAPI was used to identify the nuclei of
live cells. Generally, engrafted cells pooled together in the
posterior vitreous and remained as discrete clumps adjacent
to the ganglion cell layer (GCL) at week 1 posttransplantation
(Fig. 4A). Some transplanted cells were observed in the inner
retina, and among these cells, some exhibited migratory-like
morphological features in the outer or inner plexiform layers (Fig. 4A, white arrows). A number of engrafted cells
were observed at 3 weeks posttransplantation in the inner
hNPPFV FOR RETINAL TRANSPLANTATION
2627
Figure 3. Evaluation of responses of NPPFV cells to neurotransmitters by labeling the calcium indicator dye Fura-2. (A) The percentage of responding NPPFV cells after stimulation with different neurotransmitters at a concentration of 0.1 M. (B) Pseudocolor images
of representative NPPFV cells before and shortly after the applications of different neurotransmitters. The rainbow scale from blue to
violet indicates the gradual change from low to high level of [Ca2+]i. (C) The peak [Ca2+]i of responding NPPFV cells after stimulation
with different neurotransmitters at a concentration of 0.1 M. **p < 0.01. HBSS, Hank’s balanced salt solution (vehicle); Dopa, dopamine; Ach, acetylcholine; GABA, g-aminobutyric acid; Gly, glycine; Glu, glutamate.
2628
Chen ET AL.
Figure 4. Survival and migration of transplanted eGFP-expressing NPPFV cells (A–B) and hRPCs (C) to the retina of adult C57BL/6
mice. NPPFV cells survived well on day 7 posttransplantation and remained as discrete clumps in the host retina above the ganglion cell
layer (GCL), and some cells migrated into the inner nuclear layer (INL) (A, white arrows). On day 21 posttransplantation, migrations of
engrafted cells were observed in the INL and outer nuclear layer (ONL) (B). The engrafted hRPCs (enhanced green fluorescent protein
[eGFP] labeled) survived well and clustered onto the GCL at week 3 posttransplantation, but few cells migrated into the host retina (C).
Scale bar: 20 µm.
and outer retina (Fig. 4B). EGFP-labeled NPPFV cells
could be observed in retinal tissues extending up to the
outer nuclear layer (ONL) (Fig. 4B). Based on the observations, we estimated that approximately 3.51 ± 2.60% (range,
0.83–6.22%) grafted cells migrated in the retina, but many
surviving NPPFV cells still adhered to the ganglion cell
layer (Figs. 4–5). As some of the cellular segments may not
have been clearly stained by immunohistochemistory and
that we may have missed some intervening cells, the percentage cited above may be an underestimate.
Some migratory NPPFV cells exhibited characteristically neural cell morphology, including long and slender projections. Although some migration of engrafted
NPPFV cells was found in host retina, the anatomic structure of the retina appeared morphologically normal with
distinct structural layers as revealed by DAPI labeling
(Fig. 4B). In addition, EGFP-labeled hRPCs were also
injected into the posterior vitreous of adult C57BL/6 using
the same procedures as NPPFV cells. Engrafted hRPCs
survived well and clustered above the GCL at 3 weeks
posttransplantation; however, few engrafted hRPCs could
be found in the inner retina (Fig. 4C). To our knowledge,
this is the first observation that engrafted human progenitor cells can survive and migrate into the inner retina of
adult animals through intravitreal transplantation.
Integration and Differentiation of Transplanted
NPPFV Cells
Typical markers of glial cells and mature neurons
were applied for checking the neuronal behaviors of
hNPPFV FOR RETINAL TRANSPLANTATION
2629
Figure 5. Integration and differentiation of the engrafted NPPFV cells in the host retina. Immunohistochemical examination revealed
that the engrafted NPPFV cells can differentiate into retinal ganglion-like neurons and form synaptic connections within the host
inner retina after modulating the host retinal microenvironment by treating with RA. We observed that some engrafted cells migrated
in the retina and integration into the GCL at week 3 posttransplantation (A, Merge) by immunolabeling with GFP (green) and b-IIItubulin (red). We also saw that glial reactivity significantly increased in host retina but not in the PFV cells by immunostaining with
GFAP (red) after transplantation at week 3 (B). Integration of NPPFV cells into the GCL was found after 3 weeks RA treatment; the
engrafted cells displayed retinal ganglion-like phenotype with b-III-tubulin expression (C, white arrows) and a typical area covered in
the white box in (C) is shown in (D) at higher magnification. Synaptophysin (red) indicated that connections had formed between the
transplanted NPPFV cells and the host inner retina (E). RGC, retinal ganglion cell; GCL, ganglion cell layer; INL, inner nuclear layer;
ONL, outer nuclear layer; GFAP, glial fibrillary acidic protein.
2630
NPPFV cells in the host retina. Immunolocalization of
b-III-tubulin (red fluorescence) expression of engrafted
cells indicated that a small number of the engrafted cells
had already merged in the GCL at 3 weeks posttransplantation (Fig. 5A). Similarly, glial reactivity, indicated by
GFAP (red fluorescence), was significantly increased in
the host retina, but few NPPFV cells were GFAP positive
(Fig. 5B). We speculate that glial activation seems to be
a significant obstacle for migration of engrafts, as some
NPPFV cells were observed in a gliosis.
Posttransplanted differentiation into mature retinal
neurons or glial cells was not clearly observed in the
engrafted cells. We attempted to induce the differentiation of the transplanted cells by modulating the retinal
microenvironment with intraperitoneal treatment of RA.
After 3 weeks of treatment, b-III-tubulin was detected in
these GFP-positive engrafts that naturally integrated into
the GCL and inner nuclear layer of the host retina (Fig. 5C,
white arrows). Interestingly, some integrated NPPFV cells
in the GCL presented as mature retinal ganglion-like cells,
such as a round soma and extensive neurites (Fig. 5D).
Furthermore, immunostaining for synaptophysin (a functional marker of mature neurons) revealed that synaptic
connections had formed between the NPPFVs and the
inner retinal cells (Fig. 5E, white arrows). The percentage
of differentiated NPPFVs may be relatively low, but they
were not rare. These findings indicated that the NPPFV
cells could differentiate into retinal ganglion-like neurons
in the host retina in response to RA.
DISCUSSION
Although numerous recent studies have highlighted
the possibility of applying stem cell-based therapy for
retinal degenerative diseases, multiple fundamental
problems must be resolved before it can be used clinically (7,36–38,60). One of the key hurdles to the application of cell transplantation for human retinal disease
is finding an acceptable source of stem cells or their
derivatives. Successful experiments with animal models
of stem cell-based replacement for photoreceptor degeneration have proved that an appropriate cell candidate
could lead to the integration of engrafted cells into the
host retina circuit and even achieve functional improvement of vision (35,43). However, the structural and functional benefits of stem cell transplantation for the inner
retina mostly come from strategies for neuroprotection
of endogenous surviving neurons, including supplying
neurotrophic factors, regulating the host microenviroment, and promoting endogenous self-repair, rather than
targeted cell replacement (5).
Various cell types, including hippocampal stem cells
(56,63), bone marrow-derived mesenchymal stromal
cells (64), oligodendrocyte precursor cells (4), and some
human Müller stem cells (6), have been tested but have
Chen ET AL.
failed to integrate into the inner retina if transplanted
intravitreally into healthy adult animals. Physical barriers
for engrafted cell migration have been identified in the
inner retina (23). Targeted disruption of glial activity and
modification of the local microenvironment with genetic
manipulation or chemicals has been proven to facilitate
retinal infiltration of engrafted cells (23,30). However,
few of these methods can be directly transferred to clinical application, considering the obvious side effects on
other retinal resident cells. Therefore, it would be essential to find a suitable cell type and establish some clinically feasible methods if any cell-based therapy is to be
considered for inner retinal diseases in the future.
In this study, we have successfully cultured and characterized neural progenitor cells derived from human
PFV membranes in vitro. Although the population of
those cells in PFV membrane was relatively small, they
were able to stably maintain the same characteristics as
progenitor cells and normally proliferate in cultural conditions (Fig. 1A, B). Therefore, it would not be difficult to
harvest enough cells for further studies. PFV results from
a failure of the primary vitreous and the hyaloid vascular systems to regress during development (14) and has
been described as one of the most serious developmental anomalies in the human eyes (46). The pathogenesis
of PFV is still unknown. Recent studies have indicated
that deficiency of transcriptional factors (19), and an
imbalance of angiogenic growth factors (11) may play
important roles in the pathogenesis of PFV. Considering
the derivation and location of PFV membranes, we
hypothesized that these membranes may contain some
type of retinal progenitor cell. Repeated screening for
different antigenic markers indicated that undifferentiated NPPFV cells exhibit characteristics of neural progenitors instead of other retinal cell types (Table 2).
However, these NPPFV cells could be differentiated in
vivo into a retinal ganglion cell-like morphology and
express neuronal markers. We observe high expression
of b-III-tubulin in undifferentiated NPPFV cells as well.
b-III-tubulin is usually considered to be one of the earliest neuron-associated cytoskeletal markers and plays a
significant role in neuritogenesis and cell motility during
retinal development (28). Recent studies have revealed
that expression of b-III-tubulin could be found in immature neurons of the fetal retina (27) and different neuronal
progenitor cells (29,42). Some premigratory neuroblasts
in the postnatal human brain also express b-III-tubulin
(59). Therefore, high expression of b-III-tubulin in undifferentiated NPPFV cells may also indicate that these
progenitors exhibit a migratory phenotype, which could
possibly facilitate their migration and integration after
transplantation.
hRPCs have been isolated from human fetal tissue and well characterized in vitro by different groups
hNPPFV FOR RETINAL TRANSPLANTATION
(1,62). The mRNA expression of various transcriptional
factors and retinal-specific proteins has been detected
by PCR in early passages of cultured hRPCs (1). Realtime qRT-PCR results revealed that, compared to hRPCs,
NPPFV cells expressed lower mRNA levels of retinal
progenitor cell markers and photoreceptor cell markers,
but higher mRNA levels of synapse-related protein and
THY1 (a mature RGCs marker) (Fig. 2). Aftab et al.
found that hRPCs only migrated and integrated in ONL
of the host retina and expressed the mature rod marker
rhodopsin after subretinal space injection in mice (1).
They suggested that hRPCs could be differentiated along
the photoreceptor lineage. Therefore, given the different
derivations of these two cell types, it is rational to consider that NPPFV cells may reside in a later developmental stage than hRPCs and that NPPFV cells could have
more potential to differentiate into inner retinal neurons
in preference to photoreceptors.
We also examined the neurotransmitter profile of
NPPFV cells using Ca2+ imaging analysis, which is widely
used to evaluate neural precursors (9,25,49). Unlike
neurons from the central nervous system, differentiated
NPPFV cells exhibited limited responses to Dopa, Ach,
GABA, and Gly, but robust responses to Glu (Fig. 3).
It has been shown that Glu, GABA, and Gly are major
neurotransmitters for conducting visual signals in the vertebrate retina (61). Although neurotransmitter content of
several lateral synapses are yet to be determined, the vast
majority of synapses mediating center inputs to bipolar
cells and ganglion cells are glutamatergic (61), and those
mediating lateral synapses are GABAergic (horizontal cells and amacrine cells) and glycinergic (amacrine
cells) (12,13,17,18,20,53). Ca2+ imaging examinations
indicated that the majority of differentiated NPPFV cells
exhibited a receptor profile similar to glutamatergic neurons. Collectively, our studies indicate that NPPFV cells
exhibit a neuronal progenitor phenotype and have potential to differentiate along the ganglion cell lineage.
One encouraging finding of our study is that cell
migration into the uninjured inner retina was observed
as early as 1 week and became more significant at
3 weeks posttransplantation. This indicated that these
cells adopted an energetic migratory phenotype after
transplantation. As supported by the literature, the number of cells that generally penetrate the retina is usually
modest. Although some of our colleagues transplant millions of cells, our transplants have been limited to 50,000
cells, which is relatively a small number. Yet our yield of
cellular penetration is similar to other published studies
(1,30). Some engrafted cells exhibited long and slender
projections across the inner plexiform layer. This is the
first observation of migration and integration of human
cells into uninjured inner retina of adult mice. Of interest,
transplanted NPPFV cells seemed to be restricted from
2631
migrating into the ONL. Few engrafted cells were found
in the outer retina, although sufficient migration was
observed in the inner retina. Our previous experiments on
subretinal transplantation of NPPFV cells revealed that
transplanted cells pooled around the injection site and
were restricted from migrating through the ONL. Given
that no physical barrier has been reported on the inner
side of ONL, it may be possible that the microenvironment in the ONL is inhibitory for NPPFV cell migration.
Studies have shown that when progenitor cells are transplanted intravitreally into the adult rodent eye, they do
not generally penetrate the retinal barriers and reside on
the retinal surface. In order for these cells to penetrate the
retina, the retinal barriers need to be weakened or broken.
This is achieved by either creating a break in the internal limiting membrane or by disturbing Müller/astroglia
with glutamate agonists such as a-aminoadipate. In this
study, we have shown that NPPFV cells can penetrate
(albeit modestly) the intact inner retina. The purpose of
the current study was not to increase the yield of NPPFV
penetration, although we are currently working on strategies to increase this yield. Further experiments are necessary to investigate the detailed mechanisms that allow
NPPFV cells to overcome the barriers and migrate into
the inner retina, especially with respect to any involvement of matrix metalloproteinases. Although plenty of
engrafted NPPFV cells were seen in the host retina, the
recipient retinal tissue appeared morphologically unremarkable with clear structural layers. It is possible that
the immunosuppressant effect of rapamycin may have
protected the retina, at least partly, from serious xenograft
rejection, as severe inflammation usually leads to damage
of host tissue after transplantation. Further experiments
are necessary to clarify whether the inhibitory effect of
rapamycin on mammalian targets of rapamycin pathway
plays a role in protecting retina from injuries.
As shown by other groups, the host retinal environment
plays a vital role in neural differentiation of transplanted
cells, and additional modulation of retinal environment
has been proven to improve migration, integration, and
differentiation of engrafted cells (6,22,34,45,55,58). RA
is an established signaling molecule that is involved in
neuronal patterning, neuronal differentiation, and the
maintenance of the differentiated state of adult neurons and neural stem cells (44). Embryonic stem cells,
hematopoietic stem cells, and neural stem cells can be
diverted down the neural differentiation pathway using
combinations of RA and growth factors, or neurotrophins,
which have also been implicated in vivo for their ability
to enhance survival and replace lost neurons in the adult
brain (21,39,48).
In this study, we tested the possibility of inducing
differentiation of transplanted NPPFV cells using by
RA in vivo. We found that some transplanted NPPFV
2632
cells integrated into the host GCL and exhibited a retinal ganglion cell-like morphology after RA treatment.
Expression of synaptophysin was observed, albeit in
low frequency, between the connections of differentiated
NPPFV cells and host retinal neurons. Similar connections were observed between the engrafted cells and host
cells in previous studies (3,10,34,63). Although our estimation of the number of differentiated NPPFV cells was
very low by visualization of EGFP expression, it is possible that they were underestimated, as the variation of
EGFP expression is still a common unsolved problem in
tracing transplanted human cells (6).
However, successful application of RA has proven that
it is possible to modify the in vivo environment to enhance
the integration and differentiation of transplanted cells in
the inner retina. Although we have identified that NPPFV
cells have the potential to differentiate into RGC-like
cells, this does not mean that native (in situ) NPPFV cells
nested within the retrolental membrane are able to directly
migrate from the retrolental membrane into the INL toward
areas of retinal pathology. The migration mechanisms that
specifically drive these progenitor cells are yet unknown.
There are many organic and microenvironmental factors
that can affect the fate shift and migration of stem cells
(40,41,54,57). In addition, only a relatively small population of engrafted cells successfully integrated and differentiated in host retina even if with RA application. This
remains a major limitation of the current xenotransplantation experiment. Therefore, it is necessary and important
to explore the mechanisms by which RA regulates NPPFV
cell differentiation in vivo, as this would help increase the
yield and efficiency of inner retina migration and differentiation of NPPFV cells and raise the possibility of its clinical application in neural stem cell therapy.
CONCLUSION
In summary, our findings from immunohistochemical examination, real-time qRT-PCR, and Ca2+ imaging
confirm that NPPFV cells exhibit characteristics of novel
neuronal progenitor cells and can be induced to differentiate into mature neurons in vitro. As an appropriate
source of stem cells is fundamental to transplantation
therapy, NPPFV cells can be easily grown from the surgically dissected tissue from human subjects with PFV,
cryopreserved, and passaged for relatively long periods
of time. This suggests that these cells may have potential for clinical application. Intravitreal transplantation
of NPPFV cells demonstrated that they could survive
well and migrate into the inner retina. Furthermore, we
have found that modulation of the retinal microenvironment by intraperitoneal injection of RA can significantly
increase the differentiation of engrafts into retinal ganglionlike mature neurons, which highlights the possibility of
facilitating engraft integration by modulating the in vivo
Chen ET AL.
microenvironment. Together, these results suggest that
neural progenitor cells derived from the PFV membrane
could potentially be applied to cell-based therapy for
some inner retinal neurodegenerative diseases, such as
glaucoma. The therapeutic effects of these cells in animal
models of glaucoma and their ability to provide neuroprotection for remaining RGCs in other retinal injury models
are important topics for future investigation.
ACKNOWLEDGMENTS: This study was supported in part by
a Seed Grant from the Harvard Stem Cell Institute, Harvard
Medical School (Boston, MA), and in part by the Canary
Charitable Foundation (NY, NY). We are grateful to the anonymous reviewers for their helpful comments. We are very grateful
to Dr. Michael J. Young for providing the human retinal progenitor cells. We also thank Dr. Dongfeng Chen for useful discussion on this manuscript preparation and Dr. Kinsang Cho
for the technical assistance in the animal surgery. The authors
declare no conflicts of interest.
REFERENCES
1. Aftab, U.; Jiang, C.; Tucker, B.; Kim, J. Y.; Klassen, H.;
Miljan, E.; Sinden, J.; Young, M. J. Growth kinetics and
transplantation of human retinal progenitor cells. Exp. Eye
Res. 89(3):301–310; 2009.
2. Baker, P. S.; Brown, G. C. Stem-cell therapy in retinal disease. Curr. Opin. Ophthalmol. 20(3):175–181; 2009.
3. Blandini, F.; Cova, L.; Armentero, M.-T.; Zennaro, E.;
Levandis, G.; Bossolasco, P.; Calzarossa, C.; Mellone, M.;
Giuseppe, B.; Deliliers, G. L.; Polli, E.; Nappi, G.; Silani, V.
Transplantation of undifferentiated human mesenchymal
stem cells protects against 6-hydroxydopamine neurotoxicity in the rat. Cell Transplant. 19(2):203–217; 2010.
4. Bull, N. D.; Irvine, K. A.; Franklin, R. J.; Martin, K. R.
Transplanted oligodendrocyte precursor cells reduce neurodegeneration in a model of glaucoma. Invest. Ophthalmol.
Vis. Sci. 50(9):4244–4253; 2009.
5. Bull, N. D.; Johnson, T. V.; Martin, K. R. Stem cells for
neuroprotection in glaucoma. Prog. Brain Res. 173:511–
519; 2008.
6. Bull, N. D.; Limb, G. A.; Martin, K. R. Human Muller
stem cell (MIO-M1) transplantation in a rat model of glaucoma: Survival, differentiation, and integration. Invest.
Ophthalmol. Vis. Sci. 49(8):3449–3456; 2008.
7. Bull, N. D.; Martin, K. R. Using stem cells to mend the
retina in ocular disease. Regen. Med. 4(6):855–864; 2009.
8. Canola, K.; Angénieux, B.; Tekaya, M.; Quiambao, A.;
Naash, M. I.; Munier, F. L.; Schorderet, D. F.; Arsenijevic,
Y. Retinal stem cells transplanted into models of late
stages of retinitis pigmentosa preferentially adopt a glial
or a retinal ganglion cell fate. Invest. Ophthalmol. Vis. Sci.
48(1):446–454; 2007.
9. Carpenter, M. K.; Inokuma, M. S.; Denham, J.; Mujtaba, T.;
Chiu, C. P.; Rao, M. S. Enrichment of neurons and neural
precursors from human embryonic stem cells. Exp. Neurol.
172(2):383–397; 2001.
10. Daadi, M. M.; Lee, S. H.; Arac, A.; Grueter, B. A.;
Bhatnagar, R.; Maag, A.-L.; Schaar, B.; Malenka, R. C.;
Palmer, T. D.; Steinberg, G. K. Functional engraftment of
the medial ganglionic eminence cells in experimental stroke
model. Cell Transplant. 18(7):815–826; 2009.
11. Feeney, S. A.; Simpson, D. A.; Gardiner, T. A.; Boyle, C.;
Jamison, P.; Stitt, A. W. Role of vascular endothelial growth
hNPPFV FOR RETINAL TRANSPLANTATION
factor and placental growth factors during retinal vascular
development and hyaloid regression. Invest. Ophthalmol.
Vis. Sci. 44(2):839–847; 2003.
12. Frech, M. J.; Perez-Leon, J.; Wassle, H.; Backus, K. H.
Characterization of the spontaneous synaptic activity
of amacrine cells in the mouse retina. J. Neurophysiol.
86(4):1632–1643; 2001.
13. Gao, F.; Wu, S. M. Characterization of spontaneous inhibitory synaptic currents in salamander retinal ganglion cells.
J. Neurophysiol. 80(4):1752–1764; 1998.
14. Goldberg, M. F. Persistent fetal vasculature (PFV): An
integrated interpretation of signs and symptoms associated
with persistent hyperplastic primary vitreous (PHPV). LIV
Edward Jackson Memorial Lecture. Am. J. Ophthalmol.
124(5):587–626; 1997.
15. Grisanti, S.; Szurman, P.; Jordan, J.; Kociok, N.; BartzSchmidt, K. U.; Heimann, K. Xenotransplantation of retinal
pigment epithelial cells into RCS rats. Jpn. J. Ophthalmol.
46(1):36–44; 2002.
16. Grynkiewicz, G.; Poenie, M.; Tsien, R. Y. A new generation
of Ca2+ indicator with greatly improved fluorescence properties. J. Biol. Chem. 260(6):3440–3450; 1985.
17. Guo, C. Y.; Hirano, A. A.; Stella, S. L.; Bitzer, M.; Brecha,
N. C. Guinea pig horizontal cells express GABA, the GABAsynthesizing enzyme GAD65, and the GABA vesicular
transporter. J. Comp. Neurol. 518(10):1647–1669; 2010.
18. Guo, C. Y.; Stella, S. L.; Hirano, A. A.; Brecha, N. C.
Plasmalemmal and vesicular g-aminobutyric acid transporter expression in the developing mouse retina. J. Comp.
Neurol. 512(2):6–26; 2009.
19. Hahn, P.; Lindsten, T.; Tolentino, M.; Thompson, C. B.;
Bennett, J.; Dunaief, J. L. Persistent fetal ocular vasculature in mice deficient in bax and bak. Arch. Ophthalmol.
123(6):797–802; 2005.
20. Hartwick, A. T.; Lalonde, M. R.; Barnes, S.; Baldridge,
W. H. Adenosine A1-receptor modulation of glutamateinduced calcium influx in rat retinal ganglion cells. Invest.
Ophthalmol. Vis. Sci. 45(10):3740–3748; 2004.
21. Ikeda, R.; Kurokawa, M. S.; Chiba, S.; Yoshikawa, H.;
Ide, M.; Tadokoro, M.; Nito, S.; Nakatsuji, N.; Kondoh, Y.;
Nagata, K.; Hashimoto, T.; Suzuki, N. Transplantation of
neural cells derived from retinoic acid-treated cynomolgus
monkey embryonic stem cells successfully improved motor
function of hemiplegic mice with experimental brain injury.
Neurobiol. Dis. 20(1):38–48; 2005.
22. Ikegami, T.; Nakamura, M.; Yamane, J.; Katoh, H.; Okada,
S.; Iwanami, A.; Watanabe, K.; Ishii, K.; Kato, F.; Fujita,
H.; Takahashi, T.; Okano, H. J.; Toyama, Y.; Okano, H.
Chondroitinase ABC combined with neural stem/progenitor cell transplantation enhances graft cell migration and
outgrowth of growth-associated protein-43-positive fibers
after rat spinal cord injury. Eur. J. Neurosci. 22(12):3036–
3046; 2005.
23. Johnson, T. V.; Bull, N. D.; Martin, K. R. Identification of
barriers to retinal engraftment of transplanted stem cells.
Invest. Ophthalmol. Vis. Sci. 51(2):960–970; 2010.
24. Johnson, T. V.; Bull, N. D.; Martin, K. R. Transplantation
prospects for the inner retina. Eye 23(10):1980–1984; 2009.
25. Kalyani, A. J.; Piper, D.; Mujtaba, T.; Lucero, M. T.; Rao, M.
S. Spinal cord neuronal precursors generate multiple neuronal
phenotypes in culture. J. Neurosci. 18(19):7856–7868; 1998.
26. Kass, M. A.; Heuer, D. K.; Higginbotham, E. J.; Johnson,
C. A.; Keltner, J. L.; Miller, J. P.; Parrish, 2nd, R. K.;
Wilson, M. R.; Gordon, M. O. The ocular hypertension
2633
treatment study: A randomized trial determines that topical ocular hypotensive medication delays or prevents the
onset of primary open-angle glaucoma. Arch. Ophthalmol.
120(6):701–713; discussion 829–830; 2002.
27. Katsetos, C. D.; Herman, M. M.; Frankfurter, A.; Uffer, S.;
Perentes, E.; Rubinstein, L. J. Neuron-associated class III
beta-tubulin isotype, microtubule-associated protein 2,
and synaptophysin in human retinoblastomas in situ.
Further immunohistochemical observations on the FlexnerWintersteiner rosettes. Lab. Invest. 64(1):45–54; 1991.
28. Katsetos, C. D.; Herman, M. M.; Mork, S. J. Class III betatubulin in human development and cancer. Cell Motil.
Cytoskeleton 55(2):77–96; 2003.
29. Katsetos, C. D.; Legido, A.; Perentes, E.; Mork, S. J. Class III
beta-tubulin isotype: A key cytoskeletal protein at the crossroads of developmental neurobiology and tumor neuropathology. J. Child Neurol. 18(12):851–866; discussion 867; 2003.
30. Kinouchi, R.; Takeda, M.; Yang, L.; Wilhelmsson, U.;
Lundkvist, A.; Pekny, M.; Chen, D. F. Robust neural integration from retinal transplants in mice deficient in GFAP
and vimentin. Nat. Neurosci. 6(8):863–868; 2003.
31. Klassen, H. J.; Ng, T. F.; Kurimoto, Y.; Kirov, I.; Shatos,
M.; Coffey, P.; Young, M. J. Multipotent retinal progenitors express developmental markers, differentiate into retinal neurons, and preserve light-mediated behavior. Invest.
Ophthalmol. Vis. Sci. 45(11):4167–4173; 2004.
32. Klassen, H. J.; Ziaeian, B.; Kirov, I. I.; Young, M. J.;
Schwartz, P. H. Isolation of retinal progenitor cells from
postmortem human tissue and comparison with autologous
brain progenitors. J. Neurosci. Res. 77:334–343; 2004.
33. Kmetzsch, L.; Staats, C. C.; Simon, E.; Fonseca, F. L.; de
Oliveira, D. L.; Sobrino, L.; Rodrigues, J.; Leal, A. L.;
Nimrichter, L.; Rodrigues, M. L.; Schrank, A.; Vainstein, M. H.
The vacuolar Ca2+ exchanger vcx1 is involved in calcineurindependent Ca2+ tolerance and virulence in Cryptococcus
neoformans. Eukaryotic Cell 9(11):1798–1805; 2010.
34. Lafreniere, J.-F.; Caron, M.-C.; Skuk, D.; Goulet, M.;
Cheikh, A. R.; Tremblay, J. P. Growth factor coinjection
improves the migration potential of monkey myogenic precursors without affecting cell transplantation success. Cell
Transplant. 18(7):719–730; 2009.
35. Lamba, D.; Gust, J.; Reh, T. A. Transplantation of human
embryonic stem cell-derived photoreceptors restores some
visual function in Crx-deficient mice. Cell Stem Cell
4(1):73–79; 2009.
36. Lamba, D.; Karl, M.; Reh, T. Neural regeneration and
cell replacement: A view from the eye. Cell Stem Cell
2(6):538–549; 2008.
37. Lamba, D. A.; Karl, M. O.; Reh, T. A. Strategies for retinal
repair: Cell replacement and regeneration. Prog. Brain Res.
175:23–31; 2009.
38. Levin, L. A.; Ritch, R.; Richards, J. E.; Borras, T. Stem
cell therapy for ocular disorders. Arch. Ophthalmol.
122(4):621–627; 2004.
39. Li, Q.; Hosaka, N.; Cui, W.; Wang, X.; Cui, Y.; Cui, Y.;
Song, C.; Li, Q.; Ryu, T.; Fan, T.; Kawamoto, K.; Ikehara,
S. Lin(–)CD34(–) bone marrow cells from adult mice
can differentiate into neural-like cells. Neurosci. Lett.
408(1):51–56; 2006.
40. Livesey, F. J.; Cepko, C. L. Vertebrate neural cell-fate
determination: Lessons from the retina. Nat. Rev. Neurosci.
2(2):109–118; 2001.
41. Lovell-Badge, R. The future for stem cell research. Nature
414:88–91; 2001.
2634
42. Luskin, M. B.; Zigova, T.; Soteres, B. J.; Stewart, R. R.
Neuronal progenitor cells derived from the anterior subventricular zone of the neonatal rat forebrain continue to
proliferate in vitro and express a neuronal phenotype. Mol.
Cell. Neurosci. 8(5):351–366; 1997.
43. MacLaren, R. E.; Pearson, R. A.; MacNeil, A.; Douglas, R.
H.; Salt, T. E.; Akimoto, M.; Swaroop, A.; Sowden, J. C.;
Ali, R. R. Retinal repair by transplantation of photoreceptor
precursors. Nature 444(7116):203–207; 2006.
44. Maden, M. Retinoic acid in the development, regeneration
and maintenance of the nervous system. Nat. Rev. Neurosci.
8(10):755–765; 2007.
45. Matsuda, R.; Yoshikawa, M.; Kimura, H.; Ouji, Y.; Nakase, H.;
Nishimura, F.; Nonaka, J.-I.;Toriumi, H.;Yamada, S.; Nishiofuku,
M.; Moriya, K.; Ishizaka, S.; Nakamura, M.; Sakaki, T.
Cotransplantation of mouse embryonicstem cells and bone marrow stromal cells following spinal cord Injury suppresses tumor
development. Cell Transplant. 18(1):39–54; 2009.
46. Müllner-Eidenböck, A.; Amon, M.; Moser, E.; Klebermass,
N. Persistent fetal vasculature and minimal fetal vascular
remnants: A frequent cause of unilateral congenital cataracts. Ophthalmol. 111(5):906–913; 2004.
47. Nishida, A.; Takahashi, M.; Tanihara, H.; Nakano, I.;
Takahashi, J. B.; Mizoguchi, A.; Ide, C.; Honda, Y.
Incorporation and differentiation of hippocampus-derived
neural stem cells transplanted in injured adult rat retina.
Invest. Ophthalmol. Vis. Sci. 41(13):4268–4274; 2000.
48. Nonaka, M.; Yoshikawa, M.; Nishimura, F.; Yokota, H.;
Kimura, H.; Hirabayashi, H.; Nakase, H.; Ishizaka, S.;
Wanaka, A.; Sakaki, T. Intraventricular transplantation of
embryonic stem cell-derived neural stem cells in intracerebral hemorrhage rats. Neurol. Res. 26(3):265–272; 2004.
49. Piper, D. R.; Mujtaba, T.; Keyoung, H.; Roy, N. S.; Goldman,
S. A.; Rao, M. S.; Lucero, M. T. Identification and characterization of neuronal precursors and their progeny from human
fetal tissue. J. Neurosci. Res. 66(3):356–368; 2001.
50. Quigley, H. A. Number of people with glaucoma worldwide. Br. J. Ophthalmol. 80(5):389–393; 1996.
51. Quigley, H. A.; Broman, A. T. The number of people with
glaucoma worldwide in 2010 and 2020. Br. J. Ophthalmol.
90(3):262–267; 2006.
52. Schmittgen, T. D.; Livak, K. J. Analyzing real-time
PCR data by the comparative C(T) method. Nat. Protoc.
3(6):1101–1108; 2008.
Chen ET AL.
53. Shen, W.; Jiang, Z. Characterization of glycinergic synapses
in vertebrate retinas. J. Biomed. Sci. 14(1):5–13; 2007.
54. Spradling, A.; Drummond-Barbosa, D.; Kai, T. Stem cells
find their niche. Nature 414(6859):98–104; 2001.
55. Suzuki, T.; Mandai, M.; Akimoto, M.; Yoshimura, N.;
Takahashi, M. The simultaneous treatment of MMP-2
stimulants in retinal transplantation enhances grafted cell
migration into the host retina. Stem Cells 24(11):2406–
2411; 2006.
56. Takahashi, M.; Palmer, T. D.; Takahashi, J.; Gage, F. H.
Widespread integration and survival of adult-derived neural progenitor cells in the developing optic retina. Mol.
Cell. Neurosci. 12(6):340–348; 1998.
57. Temple, S. The development of neural stem cells. Nature
414(6859):112–117; 2001.
58. Wang, L.; Zhang, Z. G.; Zhang, R. L.; Gregg, S. R.;
Hozeska-Solgot, A.; LeTourneau, Y.; Wang, Y.; Chopp, M.
Matrix metalloproteinase 2 (MMP2) and MMP9 secreted
by erythropoietin-activated endothelial cells promote neural progenitor cell migration. J. Neurosci. 26(22):5996–
6003; 2006.
59. Weickert, C. S.; Webster, M. J.; Colvin, S. M.; Herman,
M. M.; Hyde, T. M.; Weinberger, D. R.; Kleinman, J. E.
Localization of epidermal growth factor receptors and putative neuroblasts in human subependymal zone. J. Comp.
Neurol. 423(3):359–372; 2000.
60. West, E. L.; Pearson, R. A.; MacLaren, R. E.; Sowden,
J. C.; Ali, R. R. Cell transplantation strategies for retinal
repair. Prog. Brain Res. 175:3–21; 2009.
61. Wu, S. M.; Maple, B. R. Amino acid neurotransmitters in the
retina: A functional overview. Vis. Res. 38(10):1371–1384;
1998.
62. Yang, P.; Seiler, M. J.; Aramant, R. B.; Whittemore, S. R.
In vitro isolation and expansion of human retinal progenitor
cells. Exp. Neurol. 177(1):326–331; 2002.
63. Young, M. J.; Ray, J.; Whiteley, S. J. O.; Klassen, H.;
Gage, F. H. Neuronal differentiation and morphological
Integration of hippocampal progenitor cells transplanted
to the retina of immature and mature dystrophic rats. Mol.
Cell. Neurosci. 16(3):197–205; 2000.
64. Yu, S.; Tanabe, T.; Dezawa, M.; Ishikawa, H.; Yoshimura,
N. Effects of bone marrow stromal cell injection in an
experimental glaucoma model. Biochem. Biophys. Res.
Commun. 344(4):1071–1079; 2006.