Untitled
advertisement

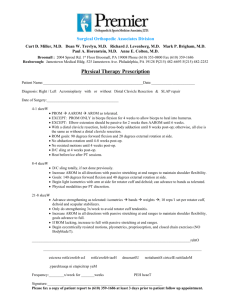
Physical Therapy Management of Shoulder Pain Jill Hipskind, PT, DPT, OCS, CSCS, CMT Rock Valley Physical Therapy What should trigger a referral to PT from PCP? • Complaints of musculoskeletal shoulder pain • Complaints of ROM limitations • Complaints of upper extremity weakness • Inability or difficulty performing ADLs • Inability or difficulty performing work-related tasks/activities • Inability or difficulty performing recreational activities Initial Physical Therapy Evaluation #1 priority – make sure patient is appropriate for PT and symptoms are musculoskeletal in nature Initial Evaluation (cont) Determine if symptoms are from a local source or proximal referral (cervical spine) Initial Evaluation — Subjective • Duration of Current Episode • Mechanism of Injury • Description and Location of Symptoms • Latency of Symptoms • Aggravating and Relieving Positions/Activities • 24-Hour Pattern • Functional Limitations Initial Evaluation — Subjective • Current or Previous Treatment • History of Previous Shoulder Problems • History of Cervical Spine Problems • Past Medical History • Functional Outcome Tool Initial Evaluation — Objective Observation of Posture Vitals Neurological Examination Cervical Spine Screen Shoulder Assessment – AROM – PROM – Strength – Special Tests – Joint Mobility—AC, SC, ST, GH – Neural Mobility Screen • Quick screen of distal joints • Thoracic Spine Mobility • • • • • Differential Diagnosis/ Pattern Recognition • Rotator Cuff Pathology/Dysfunction – Difficulty laying on shoulder and difficulty sleeping – Painful/limited AROM (PROM may or may not be impaired) – Lateral upper arm pain – Functional limitations with overhead activities & ADLs, such as: fastening bra behind back, tucking in shirts, don/doff shirts or jackets – Special Tests: Empty can test, Drop arm test, Hornblower’s, Lift-off, Bear Hug Test, or Belly Press Test • Subacromial Impingement/Bursitis – See above – Special Tests: Hawkins-Kennedy, Neer Differential Diagnosis/ Pattern Recognition • Labral Pathology/Dysfunction – May be traumatic or can see with repetitive overhead activities such as throwing – Deep pain, anterior or posterior depending on location of pathology – Catching, clicking, locking, slipping – Special Tests: Speeds, O’Brien Active Compression Test, Crank Test, Biceps Load II • Biceps Pathology/Dysfunction – Anterior shoulder pain – Pain with behind back IR – Pain with end-range overhead positions Differential Diagnosis/ Pattern Recognition • OA – > 60 yo, – Pain/stiffness first thing in the morning – History of trauma, injury, or surgery – More common at AC joint than GH joint – Clicking/creaking/popping – PROM and AROM limitation • Adhesive Capsulitis – 40-60 yo, female > male, diabetes, thyroid issues, cardiovascular disease, recent immobilization – ROM restriction (ER > ABD > IR) – PROM = AROM Differential Diagnosis/ Pattern Recognition • Instability – Complaints of instability/slipping/catching – History of trauma (especially ABD/ER position) – Hypermobility elsewhere in the body – Special Tests: Apprehension/Relocation Test, Load & Shift • Fracture – History of trauma – Unwilling to move shoulder – Localized tenderness • AC joint sprain – Fall on tip of the shoulder – Pain very localized to AC joint – Pain with horizontal adduction Interventions • Dependent on suspected source of symptoms • Postural education, exercises, and manual interventions • Dependent on stage & irritability of the patient’s condition • Dependent on impairments identified – Weakness Strengthening – Range of Motion limitations AROM, PROM, AAROM – Joint hypomobility Manual interventions – Joint hypermobility Stabilization Referring the Patient to Ortho/PCP from PT • The patient is not appropriate for PT – History of trauma and patient is unwilling to move UE – Suspicion of fracture – Presence of constant, unrelenting pain that is unchanged (improved or worsened) with any activity – Reproduction of pain with exertion but no reproduction with objective examination • The patient is not responding to PT – If no change in symptoms within 3-4 treatment sessions, further assessment or imaging may be warranted – If patient’s irritability is too high and pain cannot be managed with PT initially Rehabilitation for Rotator Cuff Pathology • • • • Patient education Pain modulation Postural treatments Regain ROM – AROM, AAROM, PROM – Joint mobilizations • Strengthen remaining rotator cuff – Isometrics – Isotonics against gravity – Isotonics with external resistance Rehabilitation (cont.) • Strengthen scapular stabilizers – Middle and lower traps • Return to functional daily activities • Return to functional recreational activities Pre-hab Prior to Surgery • Regain ROM • Strengthen as much as possible • Patient Education • Patient Education • Patient Education thank you! Jill Hipskind, PT, DPT, OCS, CSCS, CMT Rock Valley Physical Therapy jill.hipskind@rockvalleypt.com