Potential Dangers of the Valsalva Maneuver
advertisement

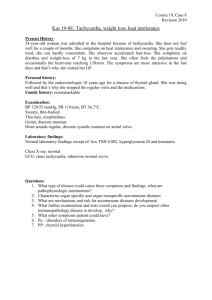
Potential Dangers of the Valsalva Maneuver and Adenosine in Paroxysmal Supraventricular Tachycardia – Beware Preexcitation R. NAGAPPAN*, S. ARORA*, C. WINTER† *Intensive Care Unit & †Emergency Department, Latrobe Regional Hospital, Traralgon, VICTORIA ABSTRACT Paroxysmal supraventricular tachycardia (PSVT) is a common clinical problem. Valsalva maneuver and adenosine are effective therapies for many patients with PSVT, although any conversion to an irregular or wide complex tachycardia should prompt consideration of a preexcitation syndrome. We report a case where the Valsalva maneuver and adenosine, in a patient with PSVT and previously undiagnosed Wolff-Parkinson-White syndrome, caused atrial fibrillation and led to a haemodynamically unstable wide complex tachycardia and ventricular fibrillation. In PSVT, where preexcitation has not been excluded, the Valsalva maneuver and adenosine can be potentially dangerous. (Critical Care and Resuscitation 2002; 4: 107-111) Key words: Paroxysmal supraventricular tachycardia, Wolff-Parkinson-White syndrome, Valsalva, adenosine, wide complex tachycardia Supraventricular tachycardias (SVTs) are a relatively common cardiac dysrhythmia,1 with 40 % being paroxysmal supraventricular tachycardia (PSVT) caused by an atrioventricular (AV) nodal reentrant mechanism.2 The Valsalva maneuver enhances vagal tone and can terminate AV reentrant tachycardias in 80% of cases, although rarely it may cause atrial dyssynchrony. Adenosine produces an acute inhibition of AV nodal function rendering it a suitable agent for treating AV nodal reentrant tachycardias. However, adenosine can be harmful in patients who have an irregular tachycardia. For example, if it is administered to patients with atrial fibrillation who have AV preexcitation, it can cause ventricular fibrillation. We report a case of PSVT in a patient with previously undiagnosed Wolff-Parkinson-White (WPW) syndrome who developed serious haemodynamic instability following Valsalva maneuver and adenosine. After reversion to sinus rhythm, an underlying preexcitation (WPW) syndrome was evident. CASE REPORT A 25-year-old woman presented to the emergency department with headache, nausea and chest pain. She had been in good health previously with no past history of hypertension, diabetes or cardiac disease. An electrocardiogram (ECG) had not been performed prior to her admission. On examination she was not distressed but complained of precordial discomfort that radiated down her left arm. Her pulse rate was 168 beats per minute and blood pressure was 128/78 mmHg. An ECG performed at this stage revealed a narrow complex tachycardia (Figure 1). As a therapeutic measure she was asked to perform the Valsalva maneuver. The ECG recorded post-Valsalva revealed an irregular rhythm (i.e. atrial fibrillation) with a mixture of broad and narrow QRS complexes (Figure 2). As this was associated with a worsening of her chest pain, 6 mg of intravenous adenosine was administered which only aggravated her chest pain. Her blood Correspondence to: Dr. R. Nagappan, Intensive Care Unit, Monash Medical Centre, Clayton, Victoria 3168 (e-mail: ramesh@bigpond.net.au) 107 R. NAGAPPAN, ET AL Critical Care and Resuscitation 2002; 4: 107-111 Figure 1. The 12-lead ECG on presentation showing a supraventricular tachycardia with a ventricular rate of 166 beats per minute. Figure 2. The ECG post-Valsalva showing a mixture of narrow and broad complex tachycardias. pressure at this stage was 126/96 mmHg. An ECG after the intravenous adenosine (Figure 3) was similar to that following the Valsalva maneuver, although the QRS complexes appeared to be wider. Her clinical condition then deteriorated rapidly as she developed an episode of rapid wide complex tachycardia due to atrial fibrillation with antegrade conduction through the by-pass tract (Figure 4). While the defibrillator was being prepared, a 300 mg bolus of intravenous amiodarone was given. This was followed by an episode of pulseless wide complex tachycardia and immediately a 300 J direct 108 current shock was given. She became unconscious and was rapidly intubated and ventilated. She then developed ventricular fibrillation and a further four direct current 360 J shocks were used to revert her to stable sinus rhythm. Following this her pulse returned, she regained consciousness and was finally extubated. The post-resuscitation ECG revealed the characteristic features of Wolff-Parkinson-White (WPW) syndrome (Figure 5). She was commenced on flecainide 50 mg twice daily and her remaining course in the intensive care unit was brief and uneventful. Critical Care and Resuscitation 2002; 4: 107-111 R. NAGAPPAN, ET AL Figure 3. The ECG post-adenosine showing a wide complex tachycardia. Figure 4. The ECG following clinical deterioration showing an episode of rapid irregular wide complex tachycardia. An echocardiogram revealed a fractional shortening of 29 % (normal > 26 %) and a structurally normal heart. A subsequent electrophysiology study confirmed WPW syndrome with a para septal atrioventricular accessory pathway. The accessory pathway was managed successfully with radiofrequency ablation. She has since remained well and asymptomatic. DISCUSSION Supraventricular tachycardias affect more than 1 % of the population, making them a relatively common clinical problem.1 Approximately 60 % of are due to an atrioventricular nodal reentrant tachycardia (AVNRT). The second most common form of paroxysmal PSVT is AV reentrant tachycardia (AVRT) using an accessory pathway.2 The term WPW syndrome is applied to patients with both preexcitation on the ECG and paroxysmal tachycardias.3-4 The AV bypass tract conducts in an antegrade direction producing, in sinus rhythm, a typical ECG pattern of a short PR interval (< 0.12 s), a 109 R. NAGAPPAN, ET AL Critical Care and Resuscitation 2002; 4: 107-111 Figure 5. The ECG following cardioversion showing the typical features of Wolff-Parkinson-White syndrome. slurred upstroke of the QRS complex (delta wave) and a wide QRS complex (Figure 5). In 95% of WPW patients with PSVT, the reentrant impulse is conducted antegradely through the AV node and retrogradely through the bypass tract (orthodromic AVRT).1 In the other 5% of WPW patients the reverse is true with antegrade conduction through the bypass tract and retrograde conduction through the AV node (antidromic AVRT).3-4 The latter also predisposes to ventricular fibrillation during atrial flutter or atrial fibrillation. The Valsalva maneuver, is a voluntary expiratory effort against a closed glottis. This increases the intrathoracic pressure, intra-abdominal pressure, blood pressure and, due to the resultant increase in vascular baroreceptor stimulation, the vagal tone. The increase in vagal tone often terminates AV nodal reentrant tachycardias and many orthodromic AVRT’s. Adenosine is an endogenous nucleoside that produces acute inhibition of sinus node and AV nodal function. This profound but short-lived effect also makes adenosine suitable for treating AVNRT’s and many orthodromic AVRT’s.5 However, in wide-complex tachycardias, not caused by an AV nodal reentrant mechanism with aberrancy,6 it can be hazardous. Our patient had been previously asymptomatic until she presented with a narrow complex tachycardia. Following the Valsalva maneuver she developed an irregular rhythm with a mixture of broad and narrow complexes (Figure 2). The wide complexes at the beginning and end of the strip were irregular with a peak rate of 300/min, a prolonged episode is also shown in Figure 4. While it is often confused with VT, in our case it was due to AF with a rapid and aberrant ventricular 110 response caused by an AV bypass tract. Atrial fibrillation in the absence of an accessory pathway has a maximum ventricular response of approximately 220 beats per minute due to the intrinsic properties of the AV node. It is not uncommon for patients in PSVT to change spontaneously to atrial fibrillation. The occurrence of an irregular tachycardia after the Valsalva maneuver in our patient, was either a coincidence or due to the Valsalva maneuver. Possibly the Valsalva maneuver increased the vagal tone increasing the AV block and therefore promoted the conduction of the irregular atrial rhythm through the accessory pathway causing a wide complex tachycardia (Figures 2, 3 and 4). This has been reported previously in a patient with AVRT and WPW syndrome.7 Keidar et al,8 also reported a patient in whom swallowing (i.e. a vagotonic process) induced atrial tachycardia and fibrillation in a patient with WPW syndrome. The presenting ECG did not show any evidence of preexcitation (Figure 1). The attempt to convert the SVT to sinus rhythm by the use of a Valsalva maneuver was standard clinical practice. However, the subsequent use of adenosine resulted in haemodynamic instability, an irregular tachycardia, persistence of the tachycardia (Figure 3) and finally worsening of the dysrhythmia (Figure 4). The role of adenosine in the management of haemodynamically stable wide complex tachycardia has been reported previously.9-11 Adenosine’s proarrhythmic tendency is well described.12-14 In a prospective analysis of 200 consecutive patients with PSVT undergoing an electrophysiological examination, adenosine terminated the PSVT in 99% of Critical Care and Resuscitation 2002; 4: 107-111 patients but caused atrial fibrillation in 12%.15 In our patient, the dysrhythmia degenerated into a rapid irregular wide complex tachycardia and ventricular fibrillation. The Valsalva maneuver and adenosine blocked AV nodal conduction and thus aided conduction down the previously unknown accessory pathway. The Valsalva maneuver and adenosine are effective in many cases of PSVT. They are usually successful in AV nodal reentrant tachycardia (i.e. where an antegrade slowly conducting limb and a retrograde rapidly conducting limb exist within the AV node) and in AV reentrant tachycardia with a concealed accessory pathway (i.e. where the accessory pathway only conducts retrogradely). In the preexcitation (WPW) syndrome, the accessory pathway may conduct the impulse in both directions and in 5 % of cases it is exclusively antegrade.3 Our case illustrates the potential danger of the Valsalva maneuver in PSVT where the WPW syndrome has not been excluded and highlights the consequences of adenosine in the presence of an irregular tachycardia. While adenosine has a short half-life and a relatively safe risk profile it should not reduce the application of clinical skills in the diagnosis of tachyarrhythmias particularly as adenosine is only beneficial in the minority of cases of wide complex tachycardias. The clinician should suspect preexcitation whenever a narrow complex tachycardia changes in to a wide complex tachycardia, especially when it is irregular. The potential for the Valsalva maneuver to precipitate atrial dyssynchronisation should also be recognised. Acknowledgments The authors wish to thank Dr Jack Krafschek, Monash Medical Centre, Melbourne for electrophysiological confirmation and radiofrequency ablation. Received: 27 December 2001 Accepted: 25 January 2002 R. NAGAPPAN, ET AL 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Chauhan VS, Krahn AD, Klein GJ, Skanes AC, Yee R. Supraventricular tachycardia. Med Clin North Am 2001;85:193-223. Gallagher JJ, Pritchett EL, Sealy WC, Kasell J, Wallace AG. The preexcitation syndromes. Prog Cardiovasc Dis 1978;20:285-327. Josephson ME, Buxton AE, Marchlinski FE. Mechanisms of tachyarrhythmias in Harrison’s Principles of Internal Medicine. 13 th edition. New York. McGraw-Hill Inc 1994:1028. Wolff L, Parkinson J, White PD. Bundle branch block with short P-R interval in healthy young people prone to paroxysmal tachycardia. Am Heart J 1930;5:685-692. Wilbur SL, Marchlinski FE. Adenosine as an antiarrhythmic agent. Am J Cardiol 1997;79:30-37. Section 7: Algorithm approach to ACLS emergencies. 7 D : The Tachycardia algorithms. Resuscitation 2000;46:185-193. Martini B, Buja GF, Canciani B, Maddalena F, Nava A. Atrial desynchronization induced by Valsalva in a patient with reciprocating SVT and WPW syndrome. J Ital Cardiol 1987;17:830-833. Keidar S, Grenadier E, Fleischman P, Palant A. Swallowing induced atrial tachycardia and fibrillation in a patient with WPW syndrome. Am J Med Sci 1984;288:32-34. Ilkhanipour K, Berrol R, Yealey DM. Therapeutic and diagnostic efficacy of adenosine in wide-complex tachycardia. Ann Emerg Med 1993;22:1360-1364. Rankin AC, Oldroyd KG, Chong E, Rae AP, Cobbe SM. Value and limitations of adenosine in the diagnosis and treatment of narrow and broad complex tachycardias. Br Heart J 1989; 62:195-203. Sharma AD, Klein GJ, Yee R. Intravenous adenosine triphosphate in wide QRS complex tachycardia: safety, therapeutic efficacy and diagnostic utility. Am J Med 1990; 88:337-342. Jaeggi E, Chiu C, Hamilton R, Gilljam T, Gow R. Adenosine-induced atrial pro-arrhythmia in children. Can J Cardiol 1999;15:169-172. Crijns HJ, Lie KI. Haemodynamic deterioration after treatment with adenosine. Br Heart J 1995;73:103. Exner DV, Muzyka T, Gillis AM. Proarrhythmia is patients with WPW syndrome after standard doses of intravenous adenosine. Ann Intern Med 1995;122:351352. Strickberger SA, Man KC, Daoud EG et al. Adenosineinduced atrial arrhythmia: a prospective analysis. Ann Intern Med 1997;127:417-422. REFERENCES 111