Intrauterine Devices (IUDs)
advertisement

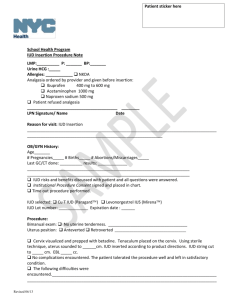
Intrauterine Devices (IUDs) What is an IUD? An IUD (intrauterine device) is a small plastic device that is inserted into a woman’s uterus by a clinician. It provides highly effective and convenient birth control for the appropriate woman. The two brands of IUDs available in the United States are the ParaGard, which uses a copper wire wrapped around the plastic device, and Mirena, which contains the hormone progesterone. The ParaGard can remain in place up to 10 years with an annual pregnancy rate of less than 1 out of 100 users, making it one of the most effective reversible birth control methods available today. Mirena must be replaced every 5 years. It is also a highly effective contraceptive (less than 1 out of 100 women become pregnant during five years of Mirena use). The progesterone in the Mirena decreases the bleeding and cramping sometimes associated with IUD use. How does the IUD work? The exact mechanisms of action of the IUD are not completely understood. The Paragard and the Mirena probably work quite differently: The Paragard IUD causes an inflammatory reaction in the lining of the uterus that interferes with egg and sperm transport. In addition, copper is toxic to sperm. The few sperm actually reaching the egg are unlikely to accomplish fertilization. The progesterone in the Mirena IUD causes the lining of the uterus to become very thin and stable, which makes the environment inhospitable to sperm and effectively prevents fertilization. Who can use the IUD? An IUD is best suited for women who are in a long term, mutually monogamous relationship and have no history of pelvic inflammatory disease (PID). Women who are not in a stable monogamous relationship are at increased risk for developing PID, which can lead to fertility problems and/or chronic pain. Never having been pregnant is not an absolute contraindication to the use of IUDs, but women who have never been pregnant have a higher rate of IUD removal due to bleeding and cramping, and a higher rate of IUD expulsion (7.5%). Both the Paragard and Mirena IUDs should NOT be prescribed for women with: History of pelvic inflammatory disease (PID) Current abnormal Pap smear Previous ectopic pregnancy Certain abnormalities of the cervix, uterus, Fallopian tubes or ovaries Conditions such as leukemia, AIDS or drug abuse that may increase their susceptibility to infections The Paragard IUD is NOT advised for women with: Severe menstrual cramps and/or heavy periods Abnormal bleeding or anemia Some heart valve disorders Allergy to copper Blood clotting problems The Mirena IUD is NOT advised for women with: Allergy to levonorgestrel, silicone, or polyethylene Breast cancer now or in the past Liver disease or a liver tumor Talk to your clinician or to our Family Planning Counselor to determine if an IUD is an appropriate form of contraception for you. What are the most common side effects associated with using an IUD? Most women will have spotting and cramping immediately after insertion of an IUD. The cramping usually subsides over several hours or a few days. The spotting gradually diminishes, but intermittent spotting between periods may continue for 3-6 months. With the Paragard IUD, many women experience increased bleeding, cramping and backache with their periods. Taking ibuprofen at the start of menses usually helps. The opposite usually occurs with the Mirena IUD: periods become lighter and cramping less intense; about 20-40% of women stop having periods after one year of Mirena use. Ten percent of women using Mirena will develop a small cyst on the ovary related to ovulation; it usually disappears on its own in a month or two. Such cysts are usually asymptomatic, but can occasionally cause pain and rarely need surgery. What risks are associated with IUD use? Pelvic Inflammatory Disease (PID) PID is a serious infection of the uterus, fallopian tubes and the ovaries that can lead to infertility, sterility and chronic pain. The risk of acquiring PID is highest within the first 20 days after IUD insertion. The rate of PID decreases from almost 10/1000 women to 1/1000 women after 21 days of IUD use. Symptoms of PID include: abdominal pain, pain with intercourse, vaginal bleeding or discharge, and fever. Call our clinic at (206) 685-1031 immediately if you experience any of these. PID is usually sexually transmitted. Women who have had PID, chlamydia or gonorrhea, or who have more than one sexual partner, or whose sexual partner has other partners, are at a greater risk of getting PID. Expulsion During the first year of use approximately 2-10% of women may expel their IUD with the majority of expulsions occurring within the first month after insertion. Only 2-3% of women who have had children expel the IUD in the first year. Expulsions after the first year of IUD use drop to 1-3%. If the IUD is expelled without the woman realizing it, she could become pregnant. Perforation of the uterus Rarely the IUD may puncture the wall of the uterus and move into the abdomen. Surgery may be necessary to remove the IUD. The rate of perforations is low (1/1000 users each year.) Pregnancy A woman who becomes pregnant with an IUD in place should have the IUD removed immediately. Continuing a pregnancy with an IUD in place has been associated with a two-fold risk of spontaneous abortion or miscarriage and a four-fold increase in the incidence of preterm labor and delivery. It is not known if Mirena can cause long-term effects on the fetus if it stays in place during a pregnancy. In rare instances women in their second trimester of pregnancy with an IUD in place have died because of an infection thought to be related to the IUD. A woman who becomes pregnant with an IUD in place is more likely to have an ectopic pregnancy (pregnancy outside the uterus) than if she were using some other forms of contraception. Five percent of pregnancies occurring with a copper IUD in place are ectopic. Half of all pregnancies detected during large clinical trials of Mirena were ectopic. A missed period, irregular bleeding, or pregnancy symptoms (nausea, breast tenderness, frequent urination, fatigue) should be reported to our clinic. Ectopic pregnancy can cause death if it is not treated in time. How do I get an IUD? Call to schedule an appointment for a complete exam, including a Pap smear and STD screening, and an appointment with the family planning counselor. The IUD will be inserted during a separate appointment while you are menstruating., or soon thereafter. We recommend that you eat something and take 600mg of ibuprofen 1-2 hours before having the IUD inserted. Before the IUD is inserted the clinician will measure the depth of your uterus with an instrument called a “sound.” The IUD will then be gently placed into the uterus. There may be some cramping during the insertion and some bleeding afterwards. After insertion do not have intercourse or put anything (e.g. tampons) in the vagina for five days. This will reduce the chance of infection. Mild cramping may occur for a few days after the IUD is inserted. Acetaminophen (Tylenol) or ibuprofen (Advil, Nuprin) may be used. If the pain is severe, call our clinic at (206) 685-1031. Following IUD Insertion: 1. 2. 3. Return to the clinic for an IUD check within the following two months, or sooner if you have problems. Check the IUD string by putting a clean finger into the vagina. Your clinician will show you how to check. We recommend you check for the string after each menstrual period to make sure the IUD is still in place. If you or your partner cannot feel the string, check again in a day or two. If you still can’t feel the string, call our clinic. In the meantime, abstain from sexual intercourse or use condoms or some other form of birth control. Also, call our clinic if the string increases in length. Routine annual exams and Pap smears are required for all women with an IUD in place. What are the IUD danger signs? Call our clinic at (206) 685-1031 immediately if you have any of the following: heavy bleeding or cramping abdominal pain fever unusual vaginal discharge or genital sores irregular bleeding missed period pregnancy signs such as nausea, vomiting, breast tenderness, frequent urination, fatigue severe or migraine headaches yellowing of the skin or whites of the eyes stroke or heart attack your partner becomes HIV positive How is the IUD removed? Most IUDs are removed easily by the clinician. Removal is best done during a menstrual period, but the IUD can be removed at other times if necessary. An IUD must be removed before another one can be inserted. Paragard IUD must be removed by 10 years and Mirena must be removed by 5 years. Either can be removed earlier if a pregnancy is desired or for other reasons. Never attempt to remove the IUD yourself. This article was adapted from material originally found on the UW-Seattle Hall Health Center website, http://www.hallhealthcenter.com.