Integrative Physiology
Across-Species Transfer of Protection by Remote Ischemic
Preconditioning With Species-Specific Myocardial Signal
Transduction by Reperfusion Injury Salvage Kinase
and Survival Activating Factor Enhancement Pathways
Andreas Skyschally, Sabine Gent, Georgios Amanakis, Christiane Schulte, Petra Kleinbongard,
Gerd Heusch
Rationale: Reduction of myocardial infarct size by remote ischemic preconditioning (RIPC), that is, cycles of
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
ischemia/reperfusion in an organ remote from the heart before sustained myocardial ischemia/reperfusion, was
confirmed in all species so far, including humans.
Objective: To identify myocardial signal transduction of cardioprotection by RIPC.
Methods and Results: Anesthetized pigs were subjected to RIPC (4×5/5 minutes hindlimb ischemia/reperfusion)
or placebo (PLA) before 60/180 minutes coronary occlusion/reperfusion. Phosphorylation of protein kinase
B, extracellular signal–regulated kinase 1/2 (reperfusion injury salvage kinase [RISK] pathway), and signal
transducer and activator of transcription 3 (survival activating factor enhancement [SAFE] pathway) in the
area at risk was determined by Western blot. Wortmannin/U0126 or AG490 was used for pharmacological RISK
or SAFE blockade, respectively. Plasma sampled after RIPC or PLA, respectively, was transferred to isolated
bioassay rat hearts subjected to 30/120 minutes global ischemia/reperfusion. RIPC reduced infarct size in pigs to
16±11% versus 43±11% in PLA (% area at risk; mean±SD; P<0.05). RIPC increased the phosphorylation of signal
transducer and activator of transcription 3 at early reperfusion, and AG490 abolished the protection, whereas
RISK blockade did not. Signal transducer and activator of transcription 5 phosphorylation was decreased at
early reperfusion in both RIPC and PLA. In isolated rat hearts, pig plasma taken after RIPC reduced infarct size
(25±5% of ventricular mass versus 38±5% in PLA; P<0.05) and activated both RISK and SAFE. RISK or SAFE
blockade abrogated this protection.
Conclusions: Cardioprotection by RIPC in pigs causally involves activation of signal transducer and activator of
transcription 3 but not of RISK. Protection can be transferred with plasma from pigs to isolated rat hearts where
activation of both RISK and SAFE is causally involved. The myocardial signal transduction of RIPC is the same
as that of ischemic postconditioning. (Circ Res. 2015;117:279-288. DOI: 10.1161/CIRCRESAHA.117.306878.)
Key Words: myocardial infarction
■
myocardial ischemia
R
emote ischemic preconditioning (RIPC), that is, brief episodes of ischemia/reperfusion in an organ remote from
the heart before sustained myocardial ischemia and subsequent reperfusion, reduces myocardial infarct size (IS). This
cardioprotective maneuver is operative in all species tested
so far, including humans.1–3 Repetitive inflation/deflation of
a blood pressure cuff around a limb is easily feasible, safe,
and effective in reducing IS in patients undergoing elective
percutaneous coronary intervention4 or coronary artery bypass
graft surgery5,6 and in patients having an acute myocardial infarction.7–9 We have recently shown in patients undergoing
coronary artery bypass graft surgery that RIPC by 3 cycles
■
reperfusion injury
■
signal transduction
of 5 minutes arm ischemia/5 minutes reperfusion not only
attenuated periprocedural myocardial injury, as reflected by
the reduced area under the curve of troponin I release, but
also reduced all-cause mortality and the rate of major adverse
cardiac and cerebrovascular events during follow-up for up to
4 years10; similar data on improved clinical outcome have
been reported for patients with acute myocardial infarction
when undergoing RIPC before reperfusion.11
At present, it is not understood how the remote stimulus
is transferred from the ischemic/reperfused organ or limb to
the heart. On the other hand, the identification of such humoral transfer factor would be an attractive pharmacological
Original received May 19, 2015; revision received June 4, 2015; accepted June 9, 2015. In May 2015, the average time from submission to first decision
for all original research papers submitted to Circulation Research was 15.49 days.
From the Institute for Pathophysiology, West German Heart and Vascular Center, University of Essen Medical School, Essen, Germany.
The online-only Data Supplement is available with this article at http://circres.ahajournals.org/lookup/suppl/doi:10.1161/CIRCRESAHA.
117.306878/-/DC1.
Correspondence to Prof Dr med Dr hc Gerd Heusch, FRCP, Institut für Pathophysiologie, Westdeutsches Herz- und Gefäßzentrum, Universitätsklinikum
Essen, Hufelandstr. 55, 45122 Essen. Germany. E-mail gerd.heusch@uk-essen.de
© 2015 American Heart Association, Inc.
Circulation Research is available at http://circres.ahajournals.org
DOI: 10.1161/CIRCRESAHA.117.306878
279
280 Circulation Research July 17, 2015
Nonstandard Abbreviations and Acronyms
AKT
ERK1/2
IS
LAD
PLA
pPLA
pRIPC
RIPC
RISK
SAFE
STAT
protein kinase B
extracellular signal–regulated kinase 1/2
infarct size
left anterior descending coronary artery
placebo
PLA plasma
RIPC plasma
remote ischemic preconditioning
reperfusion injury salvage kinase
survival activating factor enhancement
signal transducer and activator of transcription
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
target to be reinforced in situations where cardioprotection is needed, for example, in acute myocardial infarction,
complex cardiovascular surgery, or interventions.8,9 There is
experimental evidence for both, a neuronal12 or a humoral13
transfer, as well for their interaction.14 Clearly, humoral
transfer of a cardioprotective signal from one individual
to another is possible,15 even if the recipient is an isolated
heart preparation from a different species.13,16 The transfer
factor(s) appear(s) to be <15 kDa in size because it is still
operative when dialyzed through a membrane with such cutoff.13 Some studies have identified specific factors, such as
stromal cell-derived factor 117, nitrite,16 micro-RNA-14418, in
specific models and species, but no unequivocal candidate
transfer factor has yet emerged. More systematic studies using proteomic approaches to identify the protective humoral
transfer factor in plasma have also failed.19–21 Apart from the
transfer signal, the recruited cardioprotective signaling pathways within the target myocardium are unclear in detail. To
what extent RIPC shares established cardioprotective signaling pathways, such as the reperfusion injury salvage kinase
(RISK) pathway22 or the survival activating factor enhancement (SAFE) pathway,23 with other conditioning strategies
remains still to be clarified.24,25
Against this background of a so far largely elusive search
for the enigmatic humoral transfer factor of RIPC’s protection, we have now taken a novel, retrograde approach to
characterize the properties of the upstream humoral transfer factor by the downstream myocardial signal transduction which it may activate. To this effect, we have used our
established and clinically relevant pig model26 and established IS reduction by a RIPC algorithm. To further evaluate the role of humoral transfer of the protective stimulus,
we obtained arterial plasma from pigs undergoing RIPC
or a placebo (PLA) procedure and tested its cardioprotective properties in an isolated, saline-perfused bioassay rat
heart undergoing global ischemia and reperfusion with IS
as end point. To test the involvement of the RISK and SAFE
pathways, we used both immunoblotting of the respective
kinase phosphorylation and a pharmacological antagonist
approach using combined phosphatidylinositol(4,5)-bisphosphate-3-kinase inhibition by wortmannin27 and mitogenERK-activator-kinase 1/2 inhibition by U012628 for RISK
blockade or janus kinase 2 inhibition with AG490 or inhibition of signal transducer and activator of transcription 3
(STAT3) phosphorylation with stattic for SAFE blockade,
respectively.29,30 In pigs, the antagonists were given before
the RIPC maneuver and covered both the potential release of
the protective factor and its potential action on the ischemic/
reperfused myocardium. Stattic could not be used in pigs in
situ because of its high toxicity.31 In the isolated rat hearts,
the antagonists were given before infusion of plasma from
pigs that had undergone RIPC or a PLA procedure and thus
only antagonized the action of the cardioprotective signal on
the ischemic/reperfused recipient heart.
Methods
The experimental protocols were approved by the Bioethical Committee
of the district of Düsseldorf (pigs: G1240/11; rats: B1322/12).
Experiments in Pigs
Experimental Preparation
Göttinger minipigs (weight, 29.9±2.2 kg; age, 15±2 months) were
sedated with flunitrazepam (0.4 mg/kg, Rohypnol; Roche,
Grenzach-Wyhlen). Anesthesia was induced by etomidate (0.3 mg/
kg, Hypnomidat; Janssen-Cilag, Neuss) and sufentanil (1 µg/kg IV,
Sufenta; Janssen-Cilag, Neuss). Anesthesia was maintained by artificial ventilation with isoflurane (2%) in oxygen-enriched air. This
anesthesia is identical to that used in our institution for patients undergoing surgical coronary revascularization.10 The pigs were placed
on a heated table and covered with drapes to prevent hypothermia.
Esophageal temperature was thus kept at 36.9±0.9°C. One jugular
vein was cannulated with a teflon catheter for volume replacement
and intravenous drug administration. ECG-lead II was continuously
monitored. The left hindlimb was shaved, and a tourniquet was placed
around it for later induction of RIPC. After completion of the RIPC or
PLA maneuver (see below), respectively, the common carotid arteries
were cannulated to measure arterial pressure and to withdraw blood
from the descending thoracic aorta as reference for the regional blood
flow measurement. After a left lateral thoracotomy, the heart was
exposed and instrumented with a micromanometer (P7; Konigsberg
Instr., Pasadena, CA) in the left ventricle. A teflon catheter was placed
in the left atrium for the injection of colored microspheres.32 A silk
suture was placed around the left anterior descending (LAD) coronary artery distal to its second diagonal branch for later coronary occlusion. Ventricular fibrillation during the protocol was immediately
terminated by electric countershock.
Experimental Protocols
RIPC (n=15)
RIPC was induced by tightening of the tourniquet around the left
hindlimb; pale skin was taken to indicate leg ischemia. The tourniquet was released after 5 minutes, and the hindlimb was reperfused
for 5 minutes. Skin blush indicated reperfusion. The ischemia/reperfusion cycle in the leg was repeated 4 times in total, just after
induction of anesthesia and establishment of venous access. Then,
the surgical preparation was completed. One hour after the RIPC maneuver, 100 to 120 mL arterial blood was withdrawn and sampled
in vials containing Lithium–heparin and immediately centrifuged at
4°C with 800g for 10 minutes. Separated plasma was centrifuged at
4°C with 4500g for additional 10 minutes. The separated plasma was
stored at −80°C for later use and again centrifuged for 10 minutes at
4500g and filtered (0.2 µm pore size) before use. The sampled blood
volume was replaced with saline. In preliminary experiments, we had
ascertained that storage of plasma for up to 83 days at −80°C did not
attenuate its IS reducing potential. After measurement of systemic
hemodynamics and regional myocardial blood flow, myocardial drill
biopsies (2–4 mg) were taken from the area at risk. Samples were immediately snap-frozen in liquid nitrogen and stored at −80°C for later
Western blot analysis.
Then, the suture around the LAD was carefully tightened against a
soft silicone plate for 60 minutes. At 5 minutes ischemia, systemic hemodynamics and regional myocardial blood flow were measured again.
Skyschally et al Signal Transduction of Remote Preconditioning 281
Reperfusion was induced by release and quick removal of the suture
and confirmed by the disappearance of the light blue color and the reappearance of red color on the surface of the reperfused myocardium.
Myocardial biopsies were again sampled at 10 minutes reperfusion, and
systemic hemodynamics were measured at 30, 60, and 120 minutes
reperfusion. Reperfusion was continued for 3 hours before the experiment was terminated.
PLA (n=13)
The experimental protocol was identical to that of that for RIPC, except that the RIPC maneuver was omitted.
RIPC With Pharmacological Blockade of the RISK
Pathway (RIPC+RISK-BL; n=3)
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
The experimental protocol was identical to that for RIPC, except
that the RIPC maneuver and the subsequent protocol were performed in the presence of blockade of the RISK pathway. RISK
blockade was induced 10 minutes before the RIPC maneuver by
intravenous injection of the phosphatidylinositol(4,5)-bisphosphate-3-kinase inhibitor wortmannin27 (300 µg/kg bolus) and the
mitogen-ERK-activator-kinase 1/2 inhibitor U012628 (3 mg/kg
bolus+15 µg/kg per min continuous infusion up to 10 minutes
reperfusion).
RIPC With Pharmacological Blockade of the SAFE
Pathway (RIPC+SAFE-BL; n=3)
The experimental protocol was identical to that for RIPC, except
that the RIPC maneuver and the subsequent protocol were performed in the presence of blockade of the SAFE pathway. SAFE
blockade was induced by repetitive intravenous infusion of 10 mg/
kg each of the janus kinase 2 inhibitor AG490 at 10 minutes before
the RIPC maneuver, at 10 minutes before LAD occlusion, and at 10
minutes before reperfusion. AG490 was dissolved in 8 mL dimethylsulfoxide+6 mL saline and slowly administered for 10 minutes
using a syringe pump.
We omitted additional protocols with only ischemia/reperfusion
in the presence of RISK or SAFE pathway blockade because we have
already shown before that blockade of these pathways per se does not
alter IS.31,33
IS in In Situ Pig Hearts
At the end of each experiment, the LAD was reoccluded, and 5 mL
blue dye (Patentblau V, Guerbet GmbH, Sulzbach, Germany) was
quickly injected into the left atrium to delineate the area at risk as
remaining unstained. Infarcted tissue was demarcated by triphenyl
tetrazolium chloride staining. The area at risk was calculated as fraction of the left ventricle, and the IS was calculated as fraction of the
area at risk.
Experiments in Isolated Rat Hearts
Experimental Preparation
Male Lewis rats (250–400 g) were anesthetized by an intraperitoneal
injection of sodium pentobarbital (Narcoren, Merial, Hallbergmoos,
Germany). The injection was supplemented with 1000 IU heparin to
attenuate coagulation. The heart was rapidly excised and placed in
ice-cold saline before it was mounted on a Langendorff apparatus.
Modified Krebs–Henseleit buffer (in mmol/L: NaCl, 118.0: KCl,
4.7: MgSO4, 1.6: KH2PO4, 1.2; glucose, 5.6: NaHCO3, 24.9; sodium pyruvate, 2.0; CaCl2, 2.0; gassed with 95% O2 and 5% CO2 in
a 37°C prewarmed reservoir) was used for retrograde perfusion at
constant pressure (65–68 mm Hg). The perfusate temperature was
held constant by a heat exchanger located next to the aortic cannula.
A fluid-filled latex balloon was inserted through the left atrium into
the left ventricle and connected to a pressure transducer (CODAN
pvb Medical, Lensahn, Germany). Minimal left ventricular pressure
was set to 5 to 15 mm Hg by balloon inflation, heart rate was set to
400 bpm by atrial pacing, and coronary flow was measured using
an inline ultrasonic flow probe (ME2-PXN TransSonic, Maastricht,
NL) connected to the aortic cannula. During the entire experiment,
the hearts were continuously immersed in 37°C warm buffer to avoid
hypothermia. Hearts were allowed to stabilize for 20 minutes before
a protocol was started.
Experimental Protocols
Common to all protocols in the isolated bioassay rat hearts is the infusion of plasma which had been taken during the experiments in
pigs. The plasma was added via a syringe pump to the perfusate (1:10
volume ratio) before passing the heat exchanger. The plasma dilution
and the volume and timing of its infusion into rat hearts had been
elaborated and optimized in preliminary experiments. When experiments were performed with specific blockade of either the RISK or
the SAFE pathway, the perfusate containing the respective blocker
substances was freshly prepared in a second preheated reservoir, and
perfusate reservoirs were then switched by a mechanical valve. The
efficacy of the respective signaling pathway blockade was estimated
by Western blot analysis of myocardial samples taken from the rat
heart at the end of each protocol. Sampled tissue was snap-frozen in
liquid nitrogen and stored at −80°C.
RIPC Plasma (pRIPC; n=15)
Plasma taken from a pig subjected to a RIPC maneuver was infused
for 8 minutes. After brief washout of plasma, global ischemia was induced for 30 minutes by full stop of retrograde perfusion. The plasma
infusion was continued during the initial 5 minutes of 120 minutes
reperfusion at constant pressure (65–68 mm Hg).
RIPC Plasma+In Vitro Blockade of the RISK Pathway
(pRIPC+RISK-BL; n=5)
Wortmannin and U0126 were dissolved in dimethylsulfoxide and
added to the perfusate at a final concentration of 1 µmol/L wortmannin and 1 µmol/L U0126 for 20 minutes before plasma infusion.
Thereafter, the protocol was identical to that for pRIPC.
RIPC Plasma+In Vitro Blockade of the SAFE Pathway
(pRIPC+SAFE-BL; n=4)
Stattic was dissolved in dimethylsulfoxide and added to the perfusate
at a final concentration of 10 µmol/L starting at 20 minutes before
plasma infusion and continued up to the end of the experiment. The
protocol was otherwise identical to that for pRIPC.
PLA Plasma (pPLA; n=13)
The protocol was identical to that for pRIPC, except that plasma taken from a pig subjected to a PLA maneuver was used.
PLA Plasma+In Vitro Blockade of the RISK Pathway
(pPLA+RISK-BL; n=5)
The protocol was identical to that for pRIPC with RISK blockade,
except that plasma taken from a pig subjected to a PLA maneuver
was used.
PLA Plasma+In Vitro Blockade of the SAFE Pathway
(pPLA+SAFE-BL; n=4)
The protocol was identical to that for pRIPC with SAFE blockade,
except that plasma taken from a pig subjected to a PLA maneuver
was used.
Each plasma sample that was subjected to a protocol with either
RISK or SAFE blockade was also used in protocols without blockade
(pRIPC and pPLA), respectively, so that paired comparisons for the
same plasma without and with RISK or SAFE blockade, respectively,
were possible.
At the end of each protocol, the apex of the heart (≈50 mg)
was cutoff and quickly frozen in liquid nitrogen for later analysis
by Western blot. The rest of the heart was frozen in Cryomatrix
(Thermo Fisher Scientific, Germany) at −20°C and cut into transverse 1-mm thick slices. Infarcted tissue was demarcated by staining with 2% triphenyl tetrazolium chloride solution containing
5% dextran at 37°C for 20 minutes. Stained slices were weighed
and photographed from both sides. The total slice area and the
infarcted area were measured by computer-assisted planimetry.
After normalization for weight, IS was calculated as fraction of
ventricular mass.
282 Circulation Research July 17, 2015
Results
Western Blot Analysis of Myocardial Samples (Pig
and Isolated Rat Heart Experiments)
Protein aliquots of 20 µg for pig myocardium or 30 µg for rat myocardium were electrophoretically separated on precasted sodium
dodecyl sulphate-polyacrylamide gel electrophoresis gels (BioRad,
Munich, Germany) and transferred to polyvinylidene fluoride membranes. After blocking, membranes were incubated with antibodies
(Online Table I) directed against the phosphorylated forms of protein
kinase B (AKT), extracellular-signal-regulated kinase 1/2 (ERK1/2),
STAT3, and STAT5. After incubation with the respective secondary
antibodies, immunoreactive signals were detected by chemiluminescence and quantified with ChemCam/LabImage1D software (INTAS,
Göttingen, Germany). Membranes were reprobed for detection of the
respective total form of each protein. Immunoreactivities of phosphorylated protein were normalized to those of the respective total
form of the protein.
Investigators assessing IS and performing Western blot analyses
were blinded to the RIPC versus PLA protocol or the origin of the
plasma, respectively.
Statistics
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
All data are mean±SD. Area at risk and IS were compared by
one-way ANOVA. Hemodynamics, transmural blood flow, and
the time courses of protein phosphorylation were analyzed by
two-way ANOVA for repeated measures (SigmaStat 3.5, Erkrath,
Germany). When a significant difference was detected, individual
mean values were compared by Fisher least significant difference
post hoc tests. Differences were considered significant at the level
of P<0.05.
Experiments in Pigs
Three pigs were retrospectively excluded from analysis. In
one pig each of the RIPC and the PLA group, ischemia was not
severe enough (transmural blood flow, >0.06 mL/min per g).
In one pig from the PLA group, the suture for LAD occlusion
was not fixed tightly enough such that there was no infarct at
all. Nevertheless, the plasma samples taken from these pigs before ischemia were used in the isolated rat heart experiments.
Systemic Hemodynamics in Pigs
Heart rate was not different between groups and remained
unchanged throughout the protocol. Left ventricular pressure
decreased with the onset of ischemia and remained below
preischemic values up to the end of the protocol (Table 1).
Regional Myocardial Blood Flow, Area at Risk, and IS in Pigs
Transmural blood flow in the area at risk was not different between groups before ischemia and during ischemia (Table 2).
The area at risk was not different between groups (Table 2).
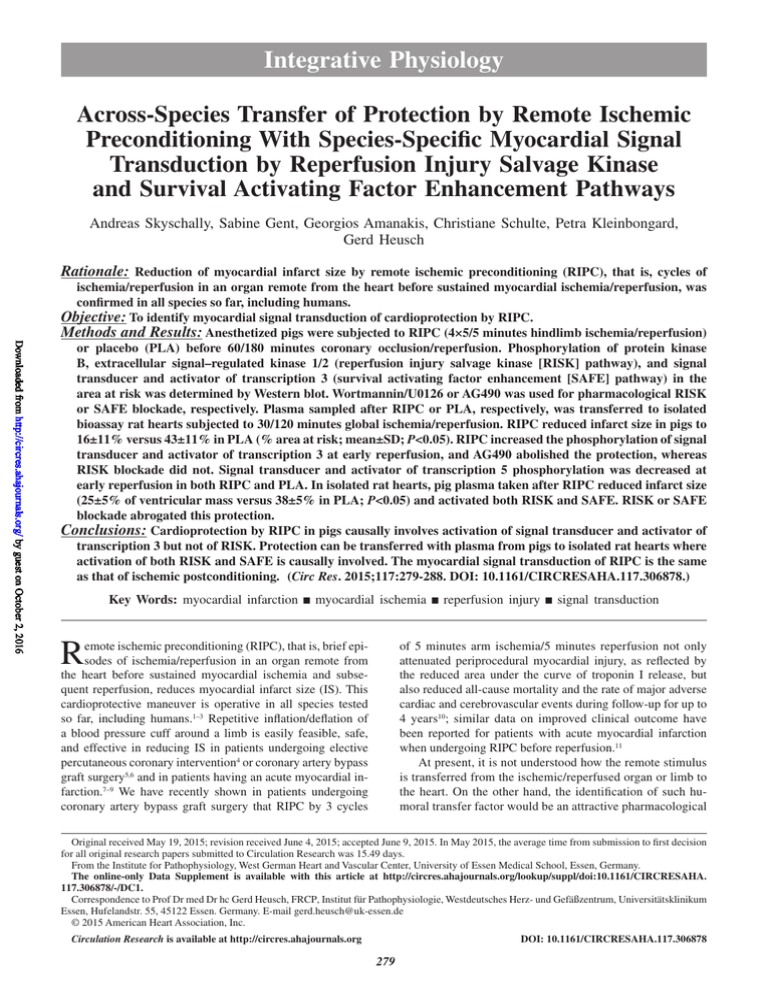
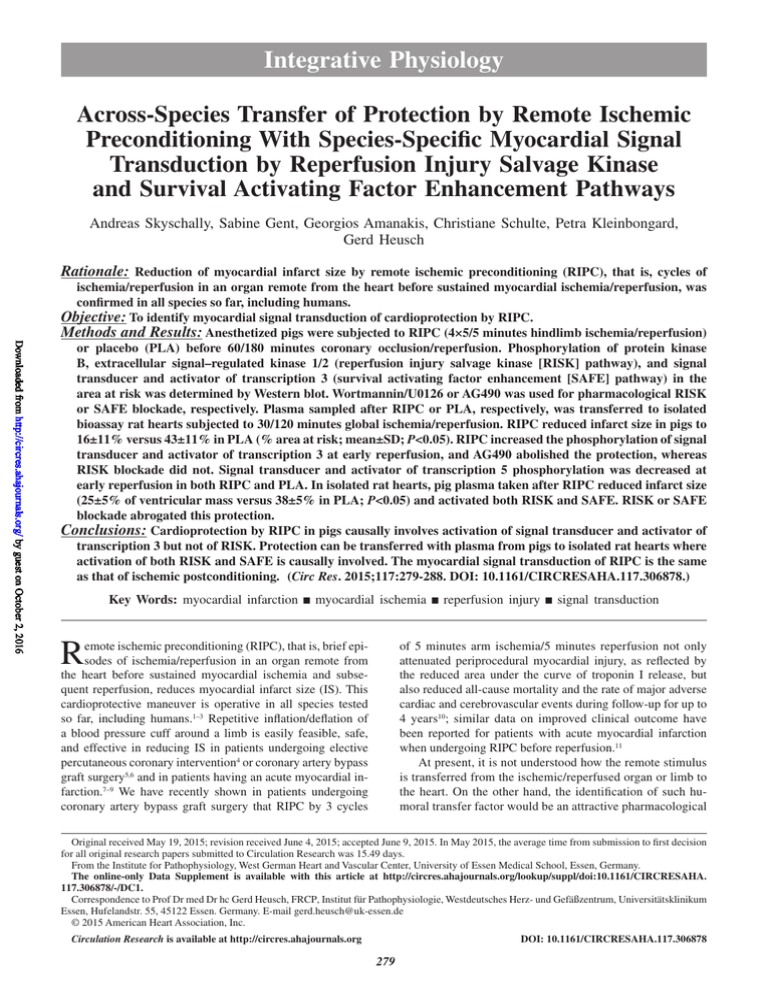
RIPC reduced IS when compared with PLA (Figure 1). RIPC
protected against infarction also in the presence of in vivo
RISK blockade (RIPC+RISK-BL), whereas RIPC’s protection
was completely abolished in the presence of in vivo SAFE
blockade (RIPC+SAFE-BL; Figure 1).
Table 1. Systemic Hemodynamics in Pigs
Time
PLA (n=11)
HR, 1/min
LVPmax, mm Hg
dP/dtmax, mm Hg/s
Preischemia
114±18
85±8
1588±369
isch5
113±15
77±8*
1407±271*
isch55
117±17
80±9*
1438±218
rep30
117±15
79±9*
1435±308
rep60
113±14
78±10*
1410±248*
rep120
112±11
75±10*
1223±308*
RIPC (n=14)
Preischemia
112±13
85±9
1433±293
isch5
112±15
77±5*
1225±267*
isch55
111±17
79±8*
1343±384
rep30
115±14
76±8*
1311±365
rep60
121±19
77±8*
1378±459
rep120
116±18
76±9*
1302±448
RIPC+RISK-BL (n=3)
Preischemia
111±20
80±1
1232±132
isch5
107±13
69±2*
985±146
isch55
120±34
72±9
1160±470
rep30
113±10
66±4*
907±193
rep60
101±9
65±6*
889±132*
rep120
99±2
59±3*
769±114*
RIPC+SAFE-BL (n=3)
Preischemia
111±17
91±7
1459±132
isch5
121±26
85±4
1316±177
isch55
110±19
79±12*
1581±274
rep30
124±24
86±9
1684±195
rep60
131±29
84±8
1758±273
rep120
125±16
75±10*
1520±63
Mean±SD. +RISK-BL/+SAFE-BL indicates RIPC in the presence of reperfusion injury salvage
kinase (RISK) pathway or survival activating factor enhancement (SAFE) pathway blockade,
respectively; dP/dtmax, maximal rate of rise of left ventricular pressure; HR, heart rate; isch5/55, 5/55
min ischemia; LVPmax, maximal left ventricular pressure; PLA, placebo; preischemia, 5 min before
ischemia; rep 30/60/120, 30/60/120 min reperfusion; and RIPC, remote ischemic preconditioning.
*P<0.05 vs preischemia.
Skyschally et al Signal Transduction of Remote Preconditioning 283
Table 2. TMBF and Area at Risk in Pigs
Protocol
TMBF Preischemia, mL/min per g
TMBF at 5 min Ischemia, mL/min per g
Area at Risk, % Left Ventricle
PLA (n=11)
0.74±0.10
0.03±0.01*
21±5
RIPC (n=14)
0.67±0.10
0.03±0.01*
22±3
RIPC+RISK-BL (n=3)
0.67±0.03
0.03±0.01*
19±1
RIPC+SAFE-BL (n=3)
0.69±0.05
0.02±0.01*
17±3
Mean±SD. +RISK-BL/+SAFE-BL indicates RIPC in the presence of reperfusion injury salvage kinase (RISK) pathway or survival activating
factor enhancement (SAFE) pathway blockade, respectively; PLA, placebo; RIPC, remote ischemic preconditioning; and TMBF, transmural
blood flow.
*P<0.05 vs TMBF preischemia.
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
Protein Phosphorylation in Pig Myocardium
The levels of phosphorylated AKT and ERK1/2, normalized
to their respective total protein, were higher at 10 minutes
reperfusion than before ischemia, but not different between
RIPC and PLA. With RIPC+RISK-BL, levels of phosphorylated AKT and ERK1/2 were attenuated, both before ischemia
and at 10 minutes reperfusion (Figure 2). The level of phosphorylated STAT3, normalized to total STAT3 protein, was
increased at 10 minutes reperfusion versus before ischemia
only with RIPC, but not with PLA or RIPC in the presence
of SAFE blockade by AG490 (Figure 2). AG490 did not attenuate the increased phosphorylation of AKT and ERK1/2
(Online Figures I and II). The level of phosphorylated STAT5,
normalized to total STAT5 protein, decreased with reperfusion
in both groups (Online Figure III).
Membranes and chemiluminescence signals for AKT,
ERK1/2, and STAT3 are displayed in Online Figures IV
to VI.
Experiments in Isolated Rat Hearts
Coronary Flow and Left Ventricular Developed Pressure in
Isolated Rat Hearts
Coronary flow and left ventricular developed pressure were
not different between groups at baseline. Infusion of pig
plasma slightly decreased developed pressure in all groups.
Developed pressure ceased ≈5 minutes after the onset of
global ischemia and recovered only partially during reperfusion. Coronary flow at reperfusion was lower than baseline but not different between pRIPC and pPLA. Except for
pRIPC+RISK-BL, coronary flow at reperfusion was lower in
the presence of RISK and SAFE blockade than in the respective untreated groups (Online Table II).
IS in Isolated Rat Hearts
IS was decreased with infusion of plasma taken from pigs
subjected to RIPC (pRIPC) when compared with infusion of
plasma from pigs subjected to PLA (pPLA; Figure 3). The
average IS with pPLA was similar to that observed after
30 minutes ischemia and 2 hours reperfusion without plasma
infusion (Online Figure VII). The protective effect of pRIPC
was abolished when either RISK blockade, that is, pretreatment with wortmannin and U0126, or SAFE blockade, that is,
pretreatment with stattic, were induced in the isolated bioassay rat heart before plasma infusion (pRIPC+RISK-BL and
pRIPC+SAFE-BL). The RISK or SAFE blockade, respectively, did not affect IS when the isolated rat hearts were treated
with plasma taken from pigs subjected to PLA (pPLA+RISKBL and pPLA+SAFE-BL; Figure 3).
IS reduction in the rat heart was also not observed with plasma taken from pigs in which the RIPC maneuver was performed
in the presence of RISK or SAFE blockade (Online Figure VII).
Protein Phosphorylation in Rat Myocardium
In myocardial samples from rat hearts after 120 minutes
reperfusion, the levels of phosphorylated AKT and ERK1/2,
normalized to their respective total protein, were higher with
pRIPC than with pPLA. The increases in AKT and ERK1/2
phosphorylation were abolished when RISK blockade was induced before pRIPC infusion (Figure 4). RISK blockade did not
affect STAT3 (Online Figure VIII). The level of phosphorylated
STAT3, normalized to total STAT3 protein, was higher with pRIPC than with pPLA, and this increase was abolished in the presence of SAFE blockade by stattic (Figure 4). SAFE blockade
did not affect AKT or ERK1/2 (Online Figure IX). The level of
phosphorylated STAT5, normalized to total STAT protein, was
not different between pRIPC and pPLA (Online Figure X).
Membranes and chemiluminescence signals for AKT,
ERK1/2, and STAT3 are displayed in Online Figures XI to XIII.
Discussion
Major Findings
We have taken a novel, retrograde approach to identify the
still enigmatic humoral transfer factor of RIPC’s protection by
Figure 1. Infarct size in pig hearts. Open symbols: individual
data points; closed symbols: mean±SD; *P<0.05 vs placebo
(PLA); #P<0.05 vs remote ischemic preconditioning (RIPC) and
RIPC+RISK-BL. +RISK-BL/+SAFE-BL indicates RIPC in the
presence of RISK or SAFE blockade (BL), respectively; RISK,
reperfusion injury salvage kinase; and SAFE, survival activating
factor enhancement.
284 Circulation Research July 17, 2015
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
Figure 3. Infarct size in isolated rat hearts with infusion
of pig plasma. pPLA: plasma taken from pigs after placebo
(PLA); pRIPC: plasma taken from pigs after remote ischemic
preconditioning (RIPC). Subsets of pPLA and pRIPC samples
(squares and diamonds) were retested in rat hearts subjected
to reperfusion injury salvage kinase (RISK; +RISK-BL; squares)
or survival activating factor enhancement (SAFE; +SAFE-BL;
diamonds) blockade, respectively, before plasma infusion. Open
symbols: individual data points; closed symbols: mean±SD;
*P<0.05 vs pRIPC. BL indicates blockade.
characterizing its properties through the downstream myocardial signal transduction which it might activate. Using this approach, we could first demonstrate that the myocardial signal
transduction pathways recruited by the humoral transfer factor of remote preconditioning are identical to those recruited
by local postconditioning, in both isolated perfused rat hearts
and in pigs in situ. Although admittedly we could not identify
the ultimate factor, our findings will further narrow down the
exhaustive and painful search for such needle in the haystack
and facilitate its identification.
Methodological Considerations
Figure 2. Phosphorylation of protein kinase B (AKT)
at ser473 and extracellular signal–regulated kinase 1/2
(ERK1/2) at thr202/tyr204 (reperfusion injury salvage kinase
[RISK] pathway) and STAT3 at tyr705 (survival activating
factor enhancement [SAFE] pathway) in pig myocardium
from the area at risk taken preischemia (black bars) and
at 10 minutes reperfusion (gray bars). Placebo (PLA): n=4;
remote ischemic preconditioning (RIPC): n=4; RIPC+RISK-BL:
n=3; RIPC+SAFE-BL: n=3; mean±SD; *P<0.05 vs respective
preischemia value; +P<0.05 vs PLA; #P<0.05 vs RIPC. BL
indicates blockade.
In the present study, we confirmed RIPC protection against
myocardial infarction in our clinically relevant pig model,26
in line with the recent CAESAR recommendations for experimental studies on cardioprotection.34 In our current study, we
have used the same anesthetic regime as was used in our studies on RIPC in patients undergoing surgical coronary revascularization.10 More specifically, we used isoflurane and not
propofol because propofol interferes with the cardioprotection
by RIPC.35,36 Of note in this context, the two studies on RIPC
in patients undergoing cardiac surgery under cardiopulmonary bypass (ERICCA and RipHeart), which have recently
presented preliminary neutral results at the hot line sessions of
the American College of Cardiology and the German Cardiac
Society, respectively, have used propofol in the majority of
patients. To further elucidate the underlying myocardial signal transduction of RIPC, we have collected pig plasma after
completion of the RIPC maneuver or PLA, respectively, and
transferred one or more potentially protective blood-borne
factor(s) from the in vivo pig model to isolated perfused rat
hearts, which were used as an in vitro bioassay. A technical
advantage of such bioassay is the abundance of plasma for
use in testing different signaling pathways. Plasma taken from
pigs after the RIPC maneuver and diluted 1:10 still reduced
IS in the isolated bioassay rat heart, whereas diluted plasma
taken from pigs after PLA did not. The rationale for taking the
plasma with 1 hour delay after the RIPC procedure was again
Skyschally et al Signal Transduction of Remote Preconditioning 285
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
to mimic the time course of our RIPC protocol in patients undergoing cardiac surgery.10 In preliminary studies, we found
no evidence that plasma taken with less delay caused greater
protection.
The samples for Western blot analysis were taken from
pig and rat hearts, in which IS was also determined by triphenyl tetrazolium chloride staining such that there was evidence
for protection or lack of it in each instance. In the pig hearts,
the first samples taken before myocardial ischemia reflect
not a truly naive baseline but the situation ≈1 hour after the
RIPC protocol or PLA, respectively, such that activation of
AKT, ERK1/2, or STAT3 at earlier time points after the RIPC
stimulus might have been missed. Nevertheless, just before
myocardial ischemia, there was no difference in the myocardial expression and phosphorylation status of AKT, ERK1/2,
and STAT3 between pigs which had undergone RIPC or PLA.
The increased phosphorylation of AKT, ERK1/2, and STAT3
at 10 minutes reperfusion in biopsy samples from pig hearts
probably reflects a situation where activated proteins might
play a causal role in attenuating reperfusion injury, and we
could ascertain such causal role for STAT3 through Western
blot analysis combined with a pharmacological antagonist approach. In contrast in the isolated rat hearts, tissue for Western
blot analysis was taken only after 2 hours reperfusion when
the increased phosphorylation levels probably are no longer
representative of earlier time points when protection has occurred. Nevertheless, the Western blot analysis after 2 hours
reperfusion still provided evidence that the pharmacological
antagonists indeed hit their targets.
Myocardial Signal Transduction of RIPC
Figure 4. Phosphorylation of protein kinase B (AKT)
at ser473 and extracellular signal–regulated kinase 1/2
(ERK1/2) at thr202/tyr204 (reperfusion injury salvage kinase
[RISK] pathway) and STAT3 at tyr705 (survival activating
factor enhancement [SAFE] pathway) in rat myocardium
subjected to infusion of plasma taken from pigs subjected
to placebo (pPLA) or remote ischemic preconditioning
(pRIPC), respectively, and in the presence of RISK blockade
(pRIPC+RISK-BL), n=5 each and in the presence of SAFE
blockade (pRIPC+SAFE-BL), n=3 each. Mean±SD; *P<0.05 vs
pPLA; #P<0.05 vs pRIPC.
The focus of our study was on those myocardial signal
transduction cascades that have already been identified in
cardioprotection by ischemic preconditioning and postconditioning,24,25 that is, AKT and ERK1/2 as central elements of
RISK22 and STAT3 as a central element of SAFE.31,37 As in
our previous studies on ischemic postconditioning,31,33 we assessed the time courses of phosphorylation of AKT, ERK1/2,
STAT3, and STAT5 by the RIPC maneuver in sequential biopsies taken from myocardium at risk in pigs. The observed IS
reduction by RIPC was not associated with a greater increase
in phosphorylation of AKT and ERK1/2 at reperfusion than
with PLA. RIPC in the presence of pharmacological RISK
blockade was still protective, although the increases in AKT
and ERK1/2 phosphorylation at reperfusion were largely attenuated, consistent with our previous study in which RISK
activation was not mandatory to confer protection by ischemic
postconditioning.33 Consequently, the activation of the RISK
pathway was apparently not causal for cardioprotection by
RIPC. In contrast, a recent study in pigs suggested an involvement of AKT in RIPC’s cardioprotection38; however, the findings of this particular study are somewhat ambiguous because
protection by RIPC was still observed when the phosphorylation of AKT was abrogated by the adenosine antagonist
8-sulfophenyltheophylline.
An obvious increase in the phosphorylation of STAT3
at reperfusion was observed only with RIPC and not with
PLA in pigs. The pretreatment of pigs with AG490, a blocker of janus kinase 2, attenuated such increase in STAT3
286 Circulation Research July 17, 2015
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
phosphorylation at reperfusion with RIPC and resulted in a
complete loss of RIPC protection, supporting a causal role
of STAT3 in RIPC protection. This observation is again consistent with our previous study which has shown a causal
role of STAT3 in cardioprotection by ischemic postconditioning in pigs.31
Plasma taken from pigs after the RIPC maneuver and
diluted 1:10 still reduced IS in the isolated bioassay rat
heart, whereas diluted plasma taken from pigs after PLA
did not. With RIPC plasma, the phosphorylation of AKT
and ERK1/2 in the rat myocardium at reperfusion was
greater than with PLA plasma. RISK blockade in the isolated bioassay rat heart before infusion of pRIPC abolished
the activation of both RISK and IS reduction. Such causal
involvement of RISK in cardioprotection in rodent hearts
is consistent with many previous studies.22,39 The lack of
protection with plasma taken from pigs in which the RIPC
maneuver was performed in the presence of a RISK blockade is then expected (Online Figure VII). Plasma taken from
pigs subjected to a RIPC maneuver when compared with
PLA plasma also increased the phosphorylation of STAT3
in the isolated bioassay rat heart. This observation supports
the notion that the SAFE pathway is also involved in cardioprotection in rodent hearts.40,41 Consequently, blockade of
STAT3 phosphorylation by stattic abolished the protective
effect of pRIPC. Plasma taken from pigs in which the RIPC
maneuver was performed in the presence of SAFE blockade also did not protect isolated bioassay rat hearts from
infarction. However, it cannot be distinguished whether the
SAFE pathway blockade in the pig before the RIPC maneuver prevented the release of a protective factor and thus
its transfer to the isolated rat heart or whether the residual
amounts of AG490 in the pig plasma prevented protection in
the rat heart per se.
The signal transduction of cardioprotection is highly species dependent. In small rodents, RISK activation is mandatory
to confer protection,22 but SAFE activation seems to play also
an important role.23,37 Apparently, there is a close interaction
of RISK and SAFE pathways in the rat heart such that either
blockade abrogates protection, consistent with previous studies.42,43 In contrast, RISK activation is not necessary for cardioprotection in pigs33 or humans,44 but an activation of STAT
is certainly involved.31,44 However, species differences are also
evident even within the SAFE signal transduction scheme.
Cardioprotection by ischemic postconditioning in pigs requires the activation of STAT3,31 whereas cardioprotection by
RIPC in humans is characterized by an activation of STAT5
and not STAT3.44 Such species differences in myocardial signal transduction of cardioprotection were also confirmed in
our current experiments. Only STAT3 activation was causally involved in cardioprotection by RIPC in the pig, whereas
phosphorylation of STAT5 decreased with reperfusion and
was not different between RIPC and PLA. In the isolated bioassay rat heart, both the RISK and the SAFE pathways were
activated by plasma taken from pigs after a RIPC maneuver.
Only STAT3, but not STAT5, was activated in the isolated bioassay rat heart. Obviously, the blood-borne factor(s) present
in the plasma of pigs after RIPC was/were able to activate
both the RISK and the SAFE pathways. Whether this transfer
factor is a protein, a micro-RNA, or an exosome, which again
might carry proteins or micro-RNAs, is not clear at this point.
The transfer with plasma (our study) seems to exclude cellular elements, and the transfer with dialysate when using a
15-kDa cutoff membrane13 seems to exclude larger particles
and molecules.
Our study now is the first to provide evidence that in
both isolated rat hearts and pigs in situ, the myocardial
signal transduction of RIPC is identical to that of local
ischemic postconditioning. Obviously, there is a point of
convergence for signal transduction of various conditioning forms, also upstream of mitochondria.25 Whether such
point of convergence is genuine to the cardiomyocyte or to
some other cellular compartment, for example, some sort of
resident cell which is activated to release a paracrine factor
which then acts on the cardiomyocyte, is unclear at present. Also, an additional involvement of neuronal pathways
either during the initiation of the RIPC stimulus, its transfer,
or the installation of protection in the pig myocardium cannot be excluded.45,46
Acknowledgments
This study will in part be used in the thesis of Christiane Schulte.
Sources of Funding
This study was supported by the German Research Foundation (He
1320/18-3 and SFB 1116 B8).
Disclosures
None.
References
1. Ovize M, Thibault H, Przyklenk K. Myocardial conditioning: opportunities for clinical translation. Circ Res. 2013;113:439–450. doi: 10.1161/
CIRCRESAHA.113.300764.
2. Przyklenk K, Sanderson TH, Hüttemann M. Clinical benefits of remote
ischemic preconditioning: new insights.and new questions. Circ Res.
2014;114:748–750. doi: 10.1161/CIRCRESAHA.114.303331.
3. Heusch G, Bøtker HE, Przyklenk K, Redington A, Yellon D. Remote ischemic conditioning. J Am Coll Cardiol. 2015;65:177–195. doi: 10.1016/j.
jacc.2014.10.031.
4. Davies WR, Brown AJ, Watson W, McCormick LM, West NE, Dutka
DP, Hoole SP. Remote ischemic preconditioning improves outcome at 6
years after elective percutaneous coronary intervention: the CRISP stent
trial long-term follow-up. Circ Cardiovasc Interv. 2013;6:246–251. doi:
10.1161/CIRCINTERVENTIONS.112.000184.
5. Hausenloy DJ, Mwamure PK, Venugopal V, Harris J, Barnard M, Grundy
E, Ashley E, Vichare S, Di Salvo C, Kolvekar S, Hayward M, Keogh B,
MacAllister RJ, Yellon DM. Effect of remote ischaemic preconditioning
on myocardial injury in patients undergoing coronary artery bypass graft
surgery: a randomised controlled trial. Lancet. 2007;370:575–579. doi:
10.1016/S0140-6736(07)61296-3.
6. Thielmann M, Kottenberg E, Boengler K, Raffelsieper C, Neuhaeuser M,
Peters J, Jakob H, Heusch G. Remote ischemic preconditioning reduces
myocardial injury after coronary artery bypass surgery with crystalloid
cardioplegic arrest. Basic Res Cardiol. 2010;105:657–664. doi: 10.1007/
s00395-010-0104-5.
7.Bøtker HE, Kharbanda R, Schmidt MR, Bottcher M, Kaltoft AK,
Terkelsen CJ, Munk K, Andersen NH, Hansen TM, Trautner S, Lassen
JF, Christiansen EH, Krusell LR, Kristensen SD, Thuesen L, Nielsen SS,
Rehling M, Sorensen HT, Redington AN, Nielsen TT. Remote ischaemic
conditioning before hospital admission, as a complement to angioplasty,
and effect on myocardial salvage in patients with acute myocardial infarction: A randomised trial. Lancet. 2010;375:727–734.
Skyschally et al Signal Transduction of Remote Preconditioning 287
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
8. Heusch G. Cardioprotection: chances and challenges of its translation to the
clinic. Lancet. 2013;381:166–175. doi: 10.1016/S0140-6736(12)60916-7.
9. Ibáñez B, Heusch G, Ovize M, Van de Werf F. Evolving therapies for myocardial ischemia/reperfusion injury. J Am Coll Cardiol. 2015;65:1454–
1471. doi: 10.1016/j.jacc.2015.02.032.
10. Thielmann M, Kottenberg E, Kleinbongard P, Wendt D, Gedik N, Pasa
S, Price V, Tsagakis K, Neuhäuser M, Peters J, Jakob H, Heusch G.
Cardioprotective and prognostic effects of remote ischaemic preconditioning in patients undergoing coronary artery bypass surgery: a single-centre
randomised, double-blind, controlled trial. Lancet. 2013;382:597–604.
doi: 10.1016/S0140-6736(13)61450-6.
11. Sloth AD, Schmidt MR, Munk K, Kharbanda RK, Redington AN, Schmidt
M, Pedersen L, Sørensen HT, Bøtker HE; CONDI Investigators. Improved
long-term clinical outcomes in patients with ST-elevation myocardial infarction undergoing remote ischaemic conditioning as an adjunct to primary percutaneous coronary intervention. Eur Heart J. 2014;35:168–175.
doi: 10.1093/eurheartj/eht369.
12. Kingma JG Jr, Simard D, Voisine P, Rouleau JR. Role of the autonomic
nervous system in cardioprotection by remote preconditioning in isoflurane-anaesthetized dogs. Cardiovasc Res. 2011;89:384–391. doi: 10.1093/
cvr/cvq306.
13.Shimizu M, Tropak M, Diaz RJ, Suto F, Surendra H, Kuzmin E, Li J,
Gross G, Wilson GJ, Callahan J, Redington AN. Transient limb ischaemia
remotely preconditions through a humoral mechanism acting directly on
the myocardium: evidence suggesting cross-species protection. Clin Sci
(Lond). 2009;117:191–200. doi: 10.1042/CS20080523.
14. Lim SY, Yellon DM, Hausenloy DJ. The neural and humoral pathways in
remote limb ischemic preconditioning. Basic Res Cardiol. 2010;105:651–
655. doi: 10.1007/s00395-010-0099-y.
15.Dickson EW, Lorbar M, Porcaro WA, Fenton RA, Reinhardt CP,
Gysembergh A, Przyklenk K. Rabbit heart can be “preconditioned” via
transfer of coronary effluent. Am J Physiol. 1999;277:H2451–H2457.
16.Rassaf T, Totzeck M, Hendgen-Cotta UB, Shiva S, Heusch G, Kelm
M. Circulating nitrite contributes to cardioprotection by remote ischemic preconditioning. Circ Res. 2014;114:1601–1610. doi: 10.1161/
CIRCRESAHA.114.303822.
17.Davidson SM, Selvaraj P, He D, Boi-Doku C, Yellon RL, Vicencio
JM, Yellon DM. Remote ischaemic preconditioning involves signalling through the SDF-1α/CXCR4 signalling axis. Basic Res Cardiol.
2013;108:377. doi: 10.1007/s00395-013-0377-6.
18. Li J, Rohailla S, Gelber N, Rutka J, Sabah N, Gladstone RA, Wei C, Hu P,
Kharbanda RK, Redington AN. MicroRNA-144 is a circulating effector of
remote ischemic preconditioning. Basic Res Cardiol. 2014;109:423. doi:
10.1007/s00395-014-0423-z.
19. Hepponstall M, Ignjatovic V, Binos S, Monagle P, Jones B, Cheung MH,
d’Udekem Y, Konstantinov IE. Remote ischemic preconditioning (RIPC)
modifies plasma proteome in humans. PLoS One. 2012;7:e48284. doi:
10.1371/journal.pone.0048284.
20.Hibert P, Prunier-Mirebeau D, Beseme O, Chwastyniak M, Tamareille
S, Pinet F, Prunier F. Modifications in rat plasma proteome after remote
ischemic preconditioning (RIPC) stimulus: identification by a SELDITOF-MS approach. PLoS One. 2014;9:e85669. doi: 10.1371/journal.
pone.0085669.
21.Helgeland E, Breivik LE, Vaudel M, Svendsen ØS, Garberg H,
Nordrehaug JE, Berven FS, Jonassen AK. Exploring the human plasma
proteome for humoral mediators of remote ischemic preconditioning–
a word of caution. PLoS One. 2014;9:e109279. doi: 10.1371/journal.
pone.0109279.
22.Hausenloy DJ, Yellon DM. New directions for protecting the heart
against ischaemia-reperfusion injury: targeting the Reperfusion Injury
Salvage Kinase (RISK)-pathway. Cardiovasc Res. 2004;61:448–460. doi:
10.1016/j.cardiores.2003.09.024.
23.Lecour S. Activation of the protective Survivor Activating Factor
Enhancement (SAFE) pathway against reperfusion injury: does it go
beyond the RISK pathway? J Mol Cell Cardiol. 2009;47:32–40. doi:
10.1016/j.yjmcc.2009.03.019.
24.Heusch G, Boengler K, Schulz R. Cardioprotection: nitric oxide, protein kinases, and mitochondria. Circulation. 2008;118:1915–1919. doi:
10.1161/CIRCULATIONAHA.108.805242.
25.Heusch G. Molecular basis of cardioprotection: signal transduction in
ischemic pre-, post-, and remote conditioning. Circ Res. 2015;116:674–
699. doi: 10.1161/CIRCRESAHA.116.305348.
26.Heusch G, Skyschally A, Schulz R. The in-situ pig heart with re
gional ischemia/reperfusion - ready for translation. J Mol Cell Cardiol.
2011;50:951–963. doi: 10.1016/j.yjmcc.2011.02.016.
27. Wymann MP, Bulgarelli-Leva G, Zvelebil MJ, Pirola L, Vanhaesebroeck
B, Waterfield MD, Panayotou G. Wortmannin inactivates phosphoinositide 3-kinase by covalent modification of Lys-802, a residue involved in the
phosphate transfer reaction. Mol Cell Biol. 1996;16:1722–1733.
28.Favata MF, Horiuchi KY, Manos EJ, Daulerio AJ, Stradley DA,
Feeser WS, Van Dyk DE, Pitts WJ, Earl RA, Hobbs F, Copeland RA,
Magolda RL, Scherle PA, Trzaskos JM. Identification of a novel inhibitor of mitogen-activated protein kinase kinase. J Biol Chem.
1998;273:18623–18632.
29. Boengler K, Buechert A, Heinen Y, Roeskes C, Hilfiker-Kleiner D, Heusch
G, Schulz R. Cardioprotection by ischemic postconditioning is lost in aged
and STAT3-deficient mice. Circ Res. 2008;102:131–135. doi: 10.1161/
CIRCRESAHA.107.164699.
30.Boengler K, Hilfiker-Kleiner D, Drexler H, Heusch G, Schulz R. The
myocardial JAK/STAT pathway: from protection to failure. Pharmacol
Ther. 2008;120:172–185. doi: 10.1016/j.pharmthera.2008.08.002.
31. Heusch G, Musiolik J, Gedik N, Skyschally A. Mitochondrial STAT3 activation and cardioprotection by ischemic postconditioning in pigs with regional myocardial ischemia/reperfusion. Circ Res. 2011;109:1302–1308.
doi: 10.1161/CIRCRESAHA.111.255604.
32.Kowallik P, Schulz R, Guth BD, Schade A, Paffhausen W, Gross R,
Heusch G. Measurement of regional myocardial blood flow with multiple
colored microspheres. Circulation. 1991;83:974–982.
33.Skyschally A, van Caster P, Boengler K, Gres P, Musiolik J, Schilawa
D, Schulz R, Heusch G. Ischemic postconditioning in pigs: no causal
role for RISK activation. Circ Res. 2009;104:15–18. doi: 10.1161/
CIRCRESAHA.108.186429.
34. Jones SP, Tang XL, Guo Y, et al. The NHLBI-sponsored Consortium for
preclinicAl assESsment of cARdioprotective therapies (CAESAR): a
new paradigm for rigorous, accurate, and reproducible evaluation of putative infarct-sparing interventions in mice, rabbits, and pigs. Circ Res.
2015;116:572–586. doi: 10.1161/CIRCRESAHA.116.305462.
35. Kottenberg E, Thielmann M, Bergmann L, Heine T, Jakob H, Heusch G,
Peters J. Protection by remote ischemic preconditioning during coronary
artery bypass graft surgery with isoflurane but not propofol - a clinical
trial. Acta Anaesthesiol Scand. 2012;56:30–38. doi: 10.1111/j.13996576.2011.02585.x.
36. Bautin AE, Galagudza MM, Datsenko SV, Tashkhanov DM, Marichev
AO, Bakanov A, Malaia E, Naimushin AV, Rubinchik VE, Gordeev
ML. Effects of remote ischemic preconditioning on perioperative
period in elective aortic valve replacement. Anesteziol Reanimatol.
2014;59:11–17.
37.Lacerda L, Somers S, Opie LH, Lecour S. Ischaemic postconditioning
protects against reperfusion injury via the SAFE pathway. Cardiovasc Res.
2009;84:201–208. doi: 10.1093/cvr/cvp274.
38.Hausenloy DJ, Iliodromitis EK, Andreadou I, Papalois A, Gritsopoulos
G, Anastasiou-Nana M, Kremastinos DT, Yellon DM. Investigating the
signal transduction pathways underlying remote ischemic conditioning in
the porcine heart. Cardiovasc Drugs Ther. 2012;26:87–93. doi: 10.1007/
s10557-011-6364-y.
39. Heusch G. No risk, no. cardioprotection? A critical perspective. Cardiovasc
Res. 2009;84:173–175. doi: 10.1093/cvr/cvp298.
40. Suleman N, Somers S, Smith R, Opie LH, Lecour SC. Dual activation
of STAT-3 and Akt is required during the trigger phase of ischaemic
preconditioning. Cardiovasc Res. 2008;79:127–133. doi: 10.1093/cvr/
cvn067.
41. Smith CC, Dixon RA, Wynne AM, Theodorou L, Ong SG, Subrayan S,
Davidson SM, Hausenloy DJ, Yellon DM. Leptin-induced cardioprotection involves JAK/STAT signaling that may be linked to the mitochondrial permeability transition pore. Am J Physiol Heart Circ Physiol.
2010;299:H1265–H1270. doi: 10.1152/ajpheart.00092.2010.
42. Tamareille S, Mateus V, Ghaboura N, Jeanneteau J, Croué A, Henrion D,
Furber A, Prunier F. RISK and SAFE signaling pathway interactions in
remote limb ischemic perconditioning in combination with local ischemic
postconditioning. Basic Res Cardiol. 2011;106:1329–1339. doi: 10.1007/
s00395-011-0210-z.
43. Hausenloy DJ, Lecour S, Yellon DM. Reperfusion injury salvage kinase
and survivor activating factor enhancement prosurvival signaling pathways in ischemic postconditioning: two sides of the same coin. Antioxid
Redox Signal. 2011;14:893–907. doi: 10.1089/ars.2010.3360.
288 Circulation Research July 17, 2015
44. Heusch G, Musiolik J, Kottenberg E, Peters J, Jakob H, Thielmann M.
STAT5 activation and cardioprotection by remote ischemic preconditioning in humans: short communication. Circ Res. 2012;110:111–115. doi:
10.1161/CIRCRESAHA.111.259556.
45.Donato M, Buchholz B, Rodríguez M, Pérez V, Inserte J,
García-Dorado D, Gelpi RJ. Role of the parasympathetic nervous system in cardioprotection by remote hindlimb ischaemic
preconditioning. Exp Physiol. 2013;98:425–434. doi: 10.1113/
expphysiol.2012.066217.
4 6. Mastitskaya S, Marina N, Gourine A, Gilbey MP, Spyer KM, Teschemacher
AG, Kasparov S, Trapp S, Ackland GL, Gourine AV. Cardioprotection
evoked by remote ischaemic preconditioning is critically dependent on the
activity of vagal pre-ganglionic neurones. Cardiovasc Res. 2012;95:487–
494. doi: 10.1093/cvr/cvs212.
Novelty and Significance
What Is Known?
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
• Brief cycles of ischemia/reperfusion in a limb or an organ remote from
the heart reduce myocardial infarct size resulting from subsequent
coronary occlusion/reperfusion, that is, there is cardioprotection by
remote ischemic preconditioning (RIPC).
• Protection by RIPC is also recruitable in humans undergoing interventional or surgical coronary revascularization.
• The protection by RIPC can be transferred with plasma from one individual to another.
What New Information Does This Article Contribute?
• In pigs, RIPC protection is mediated by activation of the signal transducer and activator of transcription 3 in the myocardium, similar to that
by ischemic postconditioning.
• In isolated rat hearts, plasma from pigs which have undergone a RIPC
protocol reduces infarct size.
• Infarct size reduction by RIPC plasma in isolated rat hearts is mediated
by activation of protein kinase B, extracellular signal–regulated kinase,
and signal transducer and activator of transcription 3.
RIPC, that is, repeated brief cycles of ischemia/reperfusion in a
limb or organ remote from the heart, reduces infarct size after coronary artery occlusion/reperfusion. Such remote cardioprotection
is also recruitable in humans with acute myocardial infarction or
during interventional or surgical coronary revascularization. The
protection by RIPC can be transferred with plasma or a plasma
dialysate from one individual to another, but the nature of the
humoral cardioprotective mediator(s) has not yet been identified.
We used a retrograde approach to characterize the cardioprotective humoral RIPC mediator by the signal transduction which
it activates in the myocardium. In pigs undergoing RIPC by repeated hindlimb ischemia/reperfusion, infarct size reduction was
mediated by activation of signal transducer and activator of transcription 3 in the myocardium. Plasma from pigs undergoing RIPC
reduced infarct size in isolated rat hearts by activation of protein
kinase B, extracellular signal–regulated kinase, and signal transducer and activator of transcription 3. Apparently, the myocardial
signal transduction which is activated by RIPC is species-specific
and identical to that of ischemic postconditioning in pigs and rats.
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
Across-Species Transfer of Protection by Remote Ischemic Preconditioning With
Species-Specific Myocardial Signal Transduction by Reperfusion Injury Salvage Kinase
and Survival Activating Factor Enhancement Pathways
Andreas Skyschally, Sabine Gent, Georgios Amanakis, Christiane Schulte, Petra Kleinbongard
and Gerd Heusch
Circ Res. 2015;117:279-288; originally published online June 9, 2015;
doi: 10.1161/CIRCRESAHA.117.306878
Circulation Research is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2015 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7330. Online ISSN: 1524-4571
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circres.ahajournals.org/content/117/3/279
Data Supplement (unedited) at:
http://circres.ahajournals.org/content/suppl/2015/06/09/CIRCRESAHA.117.306878.DC1.html
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Circulation Research can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further information
about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation Research is online at:
http://circres.ahajournals.org//subscriptions/
Supplemental Material
Across-species transfer of protection by remote ischemic
preconditioning with species-specific myocardial signal
transduction by RISK and SAFE pathways
Andreas Skyschally, PhD
Sabine Gent, PhD
Georgios Amanakis, MD
Christiane Schulte, MSc
Petra Kleinbongard, PhD
Gerd Heusch, MD, PhD
Institute for Pathophysiology, West German Heart and Vascular Center, University
of Essen Medical School, Essen, Germany
-1-
Non-standard abbreviations and acronyms used in the supplemental material
AKT
protein kinase B
ERK1/2
extracellular-signal-regulated kinase 1/2
IS
infarct size
PLA
placebo
STAT
signal transducer and activator of transcription
RIPC
remote ischemic preconditioning
RISK
reperfusion injury salvage kinases
SAFE
survival activating factor enhancement
Expanded Methods
Regional myocardial blood flow in pig myocardium
Regional myocardial blood flow was measured using colored microspheres1. In brief, microspheres (25·106; 15 µm diameter) were injected into the left atrium. During the injection, arterial blood was withdrawn
at a constant rate (5 ml/min over 3 min) via a teflon-coated catheter placed in the descending thoracic
aorta. The colored microspheres were recovered from myocardial tissue samples and the reference blood
sample by overnight digestion in 1 mol/l KOH and subsequent filtration. The dye was dissolved from the
recovered spheres, and the dye concentration was measured using a fluorescence photometer (Varian
Eclipse, Agilent Technologies, Böblingen, Germany). Transmural myocardial blood flow in the central area
at risk was calibrated against the reference withdrawal and normalized for the weight of the tissue sample.
1. Kowallik P, Schulz R, Guth BD, Schade A, Paffhausen W, Gross R, Heusch G, Measurement of regional
myocardial blood flow with multiple colored microspheres. Circulation 1991;83:974-982
Infarct size (IS) in in-situ pig hearts
At the end of each experiment, the left anterior descending coronary artery was re-occluded, and 5 ml blue
dye (Patentblau V, Guerbet GmbH, Sulzbach, Germany) was quickly injected into the left atrium to
delineate the area at risk as remaining unstained. The heart was then arrested by electrical induction of
fibrillation, removed from the chest and sectioned from base to apex into 5 transverse slices in a plane
parallel to the atrioventricular groove. Both sides of each myocardial slice were photographed, and the
slice shape and the unstained area at risk were traced manually on transparent film. Slices were then
immersed in 0.09 mol/l sodium phosphate buffer containing 1% triphenyl tetrazolium chloride (SigmaAldrich Chemie Gmbh, München, Germany) and 8% dextran for 20 min at 37°C to demarcate viable from
infarcted tissue. The infarcted triphenyl tetrazolium chloride-negative areas were traced on the same
transparent film as the area at risk. The total slice area, the area at risk, and the infarcted area were
measured by computer-assisted planimetry. After normalization for the weight of the tissue slices, the size
of the area at risk was calculated as fraction of the left ventricle, and the IS was calculated as fraction of
the area at risk.
-2-
Western blot analysis of tissue samples from pig and rat myocardium
Online Table I: Antibodies used for Western blot analyses
Kinase / Phosphorylation site
Manufacturer
Order number
Source Clonality
pAKTser473
Cell Signaling
#9271
rabbit
polyclonal
AKT
Cell Signaling
#9272
rabbit
polyclonal
pERK1/2thr202/tyr204
Cell Signaling
#9101
rabbit
polyclonal
ERK1/2
Cell Signaling
#9102
rabbit
polyclonal
pSTAT3tyr705
Cell Signaling
#9138
mouse
monoclonal
STAT3
Cell Signaling
#12640
rabbit
monoclonal
pSTAT5tyr694
Cell Signaling
#4322
rabbit
monoclonal
STAT5
Cell Signaling
#9363
rabbit
polyclonal
-3-
Online Table II: Hemodynamics in isolated bioassay rat hearts:
CFmean
[ml/min]
Time
pPLA (n=13)
pPLA+RISK-BL (n=5)
pPLA+SAFE-BL (n=4)
pRIPC (=15)
pRIPC +RISK-BL (n=5)
pRIPC+SAFE-BL (n=4)
DPmax
[mmHg]
baseline
12.7
±
1.6
87.6
±
21.5
plasma
12.7
±
1.8
80.0
±
27.2
isch5
0.0
±
0.0*
0.4
±
0.2*
isch25
0.0
±
0.0*
0.3
±
0.1*
rep10
9.0
±
1.6*
28.2
±
20.6*
rep30
8.0
±
1.9*
32.1
±
20.4*
baseline
10.8
±
1.2
83.4
±
11.3
plasma
11.3
±
3.5
71.5
±
26.4
isch5
0.0
±
0.0*
0.5
±
0.2*
isch25
0.0
±
0.0*
0.5
±
0.8*
rep10
6.5
±
1.7*#
24.9
±
20.6*
rep30
6.1
±
1.3*
28.6
±
21.9*
baseline
11.7
±
1.4
101.6
±
12.7
plasma
11.4
±
2.5
90.0
±
11.2
isch5
0.0
±
0.1*
0.8
±
0.5*
isch25
0.0
±
0.0*
1.7
±
1.1*
rep10
5.3
±
2.0*#
39.3
±
15.2*
rep30
4.5
±
2.1*#
31.0
±
23.2*
baseline
12.8
±
1.5
82.0
±
18.0
plasma
12.8
±
2.5
70.6
±
20.1
isch5
0.0
±
0.0*
0.3
±
0.3*
isch25
0.0
±
0.0*
0.4
±
0.7*
rep10
8.6
±
1.6*
27.0
±
21.1*
rep30
8.1
±
2.0*
25.8
±
19.1*
baseline
12.1
±
1.1
74.6
±
18.8
plasma
12.1
±
0.7
67.8
±
19.1
isch5
0.0
±
0.0*
0.1
±
0.0*
isch25
0.0
±
0.0*
0.3
±
0.4*
rep10
7.4
±
1.2*
17.8
±
18.3*
rep30
6.9
±
1.0*
21.1
±
24.1*
baseline
12.3
±
1.2
89.5
±
11.0
plasma
13.2
±
1.1
82.3
±
9.8
isch5
0.0
±
0.0*
0.2
±
0.1*
isch25
0.0
±
0.0*
1.3
±
1.2*
rep10
4.7
±
0.7*†
18.7
±
8.5*
rep30
4.4
±
0.2*†
13.1
±
7.6*
pPLA: infusion of plasma from pigs subjected to a PLA protocol; pRIPC: infusion of plasma from pigs
subjected to RIPC; +RISK-BL and +SAFE-BL: plasma infusion in the presence of RISK or SAFE blockade,
respectively; plasma: after plasma infusion; isch5/25: 5/25 min ischemia; rep 10/30: 10/30 min reperfusion;
CFmean: mean coronary perfusate flow; DPmax: maximal developed left ventricular pressure; mean±SD;
p<0.05 vs. baseline; # p<0.05 vs. pPLA; † p<0.05 vs. pRIPC
-4-
Ponceau
staining
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
RIPC
+SAFE-BL
RIPC
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
PLA
75 kDa
50 kDa
37 kDa
25 kDa
pAKTser473
56 kDa
total AKT
56 kDa
pAKT
total AKT
0.7
0.6
PRE-ISCHEMIA
REP10
0.5
0.4
*
*
0.3
0.2
0.1
0
PLA
RIPC
RIPC
+SAFE-BL
Online Figure I: Cross-over effects of SAFE blockade by AG490 on the phosphorylation of AKT in pig
myocardium. Samples were taken at pre-ischemia (black bars) and 10 min reperfusion (grey bars). From
top to bottom: Western blot membrane stained with Ponceau Red, immunoreactivity signals for AKT
phosphorylated at ser473 and total form of AKT, and mean±SD of the pAKT/total AKT ratio in the two
experimental groups. * p<0.05 vs. respective pre-ischemia value.
-5-
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
RIPC
+SAFE-BL
RIPC
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
Ponceau
staining
PRE-ISCHEMIA
PLA
75 kDa
50 kDa
37 kDa
25 kDa
pERK1/2 thr202/
42/44 kDa
total
ERK1/2
42/44 kDa
tyr204
pERK1/2
3.5
total ERK1/2
*#
3.0
PRE-ISCHEMIA
REP10
2.5
2.0
1.5
*
*
1.0
0.5
0
PLA
RIPC
RIPC
+SAFE-BL
Online Figure II: Cross-over effects of SAFE blockade by AG490 on the phosphorylation of ERK1/2 in pig
myocardium. Samples were taken at pre-ischemia (black bars) and 10 min reperfusion (grey bars). From
top to bottom: Western blot membrane stained with Ponceau Red, immunoreactivity signals for ERK1/2
phosphorylated at thr202/tyr204 and total form of ERK1/2, and mean±SD of the pERK1/2/total ERK1/2 ratio
in the two experimental groups. * p<0.05 vs. respective pre-ischemia value, # p<0.05 vs PLA & RIPC.
-6-
Ponceau
staining
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
RIPC
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
PLA
100 kDa
75 kDa
50 kDa
37 kDa
pSTAT5tyr694
91 kDa
total STAT5
91 kDa
pSTAT5
total STAT5
5
4
PRE-ISCHEMIA
REP10
*
p=0.056
3
2
1
0
PLA
RIPC
Online Figure III: Western blot analysis of STAT5 and its phosphorylation in myocardial samples from
pigs subjected to PLA or RIPC. Samples were taken at pre-ischemia (black bars) and 10 min reperfusion
(grey bars). From top to bottom: Western blot membrane stained with Ponceau Red, immunoreactivity
signals for STAT5 phosphorylated at tyr694 and total form of STAT5, and mean±SD of the pSTAT5/total
STAT5 ratio in the two experimental groups. * p<0.05 vs. respective pre-ischemia value.
-7-
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
Ponceau
staining
REP10
RIPC
+RISK-BL
RIPC
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
PLA
75 kDa
50 kDa
37 kDa
25 kDa
pAKTser473
56 kDa
total AKT
56 kDa
Online Figure IV: Western blot analysis of AKT and its phosphorylation in myocardial samples from pigs
subjected to PLA or RIPC and RIPC in the presence of RISK blockade (RIPC+RISK-BL). Samples were
taken pre-ischemia and at 10 min reperfusion. From top to bottom: Western blot membrane stained with
Ponceau Red, immunoreactivity signals for AKT phosphorylated at ser473, and total form of AKT.
-8-
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
RIPC
+RISK-BL
RIPC
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
Ponceau
staining
PRE-ISCHEMIA
PLA
75 kDa
50 kDa
37 kDa
25 kDa
pERK1/2 thr202/
42/44 kDa
total
ERK1/2
42/44 kDa
tyr204
Online Figure V: Western blot analysis of ERK1/2 and its phosphorylation in myocardial samples from
pigs subjected to PLA or RIPC and RIPC in the presence of RISK blockade (RIPC+RISK-BL). Samples
were taken pre-ischemia and at 10 min reperfusion. From top to bottom: Western blot membrane stained
with Ponceau Red, immunoreactivity signals for ERK1/2 phosphorylated at thr202/tyr204, and total form of
ERK1/2.
-9-
REP10
PRE-ISCHEMIA
REP10
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
Ponceau
staining
PRE-ISCHEMIA
RIPC
+SAFE-BL
RIPC
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
REP10
PRE-ISCHEMIA
PLA
150 kDa
100 kDa
75 kDa
50 kDa
86 kDa
pSTAT3tyr705
86 kDa
total STAT3
Online Figure VI: Western blot analysis of STAT3 and its phosphorylation in myocardial samples from
pigs subjected to PLA or RIPC and RIPC in the presence of SAFE blockade using AG490 (RIPC+SAFEBL). Samples were taken pre-ischemia and 10 min reperfusion. From top to bottom: Western blot
membrane stained with Ponceau Red, immunoreactivity signals for STAT3 phosphorylated at tyr705, and
total form of STAT3.
- 10 -
Infarct size [% ventricular mass]
50
45
40
35
30
25
20
15
10
5
0
I/R
n=10
pPLA
n=13
pRIPC / pig RISK‐BL
n=3
pRIPC / pig SAFE‐BL
n=3
Online Figure VII: Infarct size (mean±SD) in isolated rat hearts; I/R: 30 min ischemia and subsequent 120
min reperfusion; pPLA: infusion of plasma taken from a pig subjected to PLA; pRIPC/pig RISK-BL and /pig
SAFE BL: infusion of plasma taken from pigs in which RIPC was performed in presence of RISK or SAFE
blockade, respectively.
- 11 -
pRIPC+RISK‐BL
pRIPC
pRIPC+RISK‐BL
pRIPC
pRIPC+RISK‐BL
pRIPC
pRIPC+RISK‐BL
pRIPC
pRIPC+RISK‐BL
pRIPC
pSTAT3tyr705
86 kDa
total STAT3
100 kDa
0.5
pSTAT3
total STAT3
75 kDa
0.4
p=0.14
0.3
50 kDa
0.2
37 kDa
Ponceau
staining
0.1
0
pRIPC
pRIPC+
RISK-BL
pERK1/2 thr202/
pAKTser473
tyr204
56 kDa
42/44 kDa
total AKT
total
ERK1/2
pAKT
total AKT
2.0
pERK1/2
total ERK1/2
p<0.001
1.6
p=0.064
1.2
0.8
0.4
0
pRIPC pRIPC+
RISK-BL
pRIPC pRIPC+
RISK-BL
Online Figure VIII: Cross-over effects of RISK blockade by wortmannin and U0126 on the
phosphorylation of STAT3 in rat myocardium. Samples were taken at 2 h reperfusion. For the sake of
completeness, the impact of RISK blockade on AKT and ERK1/2 is shown in the lower panel. Top:
Western blot membrane stained with Ponceau Red, immunoreactivity signals for STAT3 phosphorylated at
tyr705, and total form of STAT3, and mean±SD of the pSTAT3/total STAT3 ratio; bottom: immunoreactivity
signals for AKT phosphorylated at ser473, and total form of AKT, and ERK1/2 phosphorylated at
thr202/tyr204, and total form of ERK1/2. Data are mean±SD; paired t-test.
- 12 -
pRIPC+SAFE‐BL
pRIPC
pRIPC+SAFE‐BL
pRIPC
pRIPC+SAFE‐BL
pRIPC
pAKTser473
56 kDa
total AKT
100 kDa
pERK1/2 thr202/
75 kDa
total ERK1/2
tyr204
42/44 kDa
1.2
50 kDa
pAKT
total AKT
p=0.42
1.0
p=0.36
37 kDa
Ponceau
staining
pERK1/2
total ERK1/2
0.8
0.6
0.4
0.2
0
pRIPC pRIPC+
SAFE-BL
pRIPC pRIPC+
SAFE-BL
pSTAT3tyr705
86 kDa
total STAT3
pSTAT3 0.25
total STAT3
p=0.003
0.20
0.15
0.10
0.05
0
pRIPC
pRIPC+
SAFE-BL
Online Figure IX: Cross-over effects of SAFE blockade by stattic on the phosphorylation of AKT and
ERK1/2 in rat myocardium. Samples were taken at 2 h reperfusion. For the sake of completeness, the
impact of SAFE blockade on STAT3 is shown in the lower panel. Top: Western blot membrane stained with
Ponceau Red, immunoreactivity signals for AKT phosphorylated at ser473, and total form of AKT, and
ERK1/2 phosphorylated at thr202/tyr204, and total form of ERK1/2, and mean±SD of the pAKT/total AKT and
pERK1/2/total ERK1/2 ratios; bottom: immunoreactivity signals for STAT3 phosphorylated at tyr705, and
total form of STAT3. Data are mean±SD; paired t-test.
- 13 -
pRIPC
pPLA
pRIPC
pPLA
pRIPC
pPLA
pRIPC
pRIPC
pPLA
pPLA
100 kDa
Ponceau
staining
75 kDa
50 kDa
pSTAT5tyr694
91 kDa
total STAT5
91 kDa
pSTAT5
0.5
total STAT5
0.4
0.3
0.2
0.1
0
pPLA
pRIPC
Online Figure X: Western blot analysis of STAT5 and its phosphorylation in myocardial samples from
isolated rat hearts after treatment with plasma taken from pigs subjected to PLA (pPLA) or RIPC (pRIPC).
Samples were taken at 2 h reperfusion. From top to bottom: Western blot membrane stained with
Ponceau Red, immunoreactivity signals for STAT5 phosphorylated at tyr694, and total form of STAT5, and
mean±SD of the pSTAT5/total STAT5 ratio in the two experimental groups.
- 14 -
pRIPC+RISK-BL
pRIPC
pPLA
marker lane
pRIPC+RISK-BL
pRIPC
pPLA
pRIPC+RISK-BL
pRIPC
pPLA
pRIPC+RISK-BL
pRIPC
pPLA
pRIPC+RISK-BL
pRIPC
pPLA
Ponceau
staining
75 kDa
50 kDa
37 kDa
25 kDa
pAKTser473
56 kDa
total AKT
56 kDa
Online Figure XI: Western blot analysis of AKT and its phosphorylation in myocardial samples from
isolated rat hearts after treatment with plasma taken from pigs subjected to PLA (pPLA) or RIPC (pRIPC)
and to RIPC-plasma with prior RISK blockade in the rat heart (pRIPC+RISK-BL). Samples were taken at 2
h reperfusion. From top to bottom: Western blot membrane stained with Ponceau Red, immunoreactivity
signals for AKT phosphorylated at ser473, and total form of AKT.
- 15 -
pRIPC+RISK-BL
pRIPC
pPLA
marker lane
pRIPC+RISK-BL
pRIPC
pPLA
pRIPC+RISK-BL
pRIPC
pPLA
pRIPC+RISK-BL
pRIPC
pPLA
pRIPC+RISK-BL
pRIPC
pPLA
Ponceau
staining
75 kDa
50 kDa
37 kDa
25 kDa
pERK1/2 thr202/
42/44 kDa
total ERK1/2
42/44 kDa
tyr204
Online Figure XII: Western blot analysis of ERK1/2 and its phosphorylation in myocardial samples from
isolated rat hearts after treatment with plasma taken from pigs subjected to PLA (pPLA) or RIPC (pRIPC)
and to RIPC-plasma with prior RISK blockade in the rat heart (pRIPC+RISK-BL). Samples were taken at 2
h reperfusion. From top to bottom: Western blot membrane stained with Ponceau Red, immunoreactivity
signals for ERK1/2 phosphorylated at thr202/tyr204, and total form of ERK1/2.
- 16 -
pRIPC+SAFE-BL
pRIPC
pPLA
pRIPC+SAFE-BL
pRIPC
pPLA
pRIPC+SAFE-BL
pRIPC
pPLA
Ponceau
staining
150 kDa
100 kDa
75 kDa
50 kDa
86 kDa
pSTAT3tyr705
total STAT3
86 kDa
Online Figure XIII: Western blot analysis of STAT3 and its phosphorylation in myocardial samples from
isolated rat hearts after treatment with plasma taken from pigs subjected to PLA (pPLA) or RIPC (pRIPC)
and to RIPC-plasma with prior SAFE blockade in the rat heart using stattic (pRIPC+SAFE-BL). Samples
were taken at 2 h reperfusion. From top to bottom: Western blot membrane stained with Ponceau Red,
immunoreactivity signals for STAT3 phosphorylated at tyr705, and total form of STAT3.
- 17 -