ABCA1 and ABCG1 Protect Against Oxidative Stress–Induced
advertisement

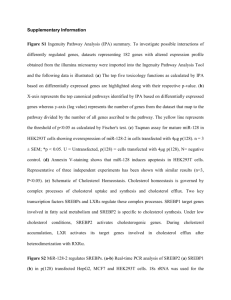
ABCA1 and ABCG1 Protect Against Oxidative Stress–Induced Macrophage Apoptosis During Efferocytosis Laurent Yvan-Charvet, Tamara A. Pagler, Tracie A. Seimon, Edward Thorp, Carrie L. Welch, Joseph L. Witztum, Ira Tabas, Alan R. Tall Rationale: Antiatherogenic effects of plasma high-density lipoprotein (HDL) include the ability to inhibit apoptosis of macrophage foam cells. The ATP-binding cassette transporters ABCA1 and ABCG1 have a major role in promoting cholesterol efflux from macrophages to apolipoprotein A-1 and HDL and are upregulated during the phagocytosis of apoptotic cells (efferocytosis). Objective: The goal of this study was to determine the roles of ABCA1 and ABCG1 in preserving the viability of macrophages during efferocytosis. Methods and Results: We show that despite similar clearance of apoptotic cells, peritoneal macrophages from Abca1ⴚ/ⴚAbcg1ⴚ/ⴚ, Abcg1ⴚ/ⴚ, and, to a lesser extent, Abca1ⴚ/ⴚ mice are much more prone to apoptosis during efferocytosis compared to wild-type cells. Similar findings were observed following incubations with oxidized phospholipids, and the ability of HDL to protect against oxidized phospholipid-induced apoptosis was markedly reduced in Abca1ⴚ/ⴚAbcg1ⴚ/ⴚ and Abcg1ⴚ/ⴚ cells. These effects were independent of any role of ABCA1 and ABCG1 in mediating oxidized phospholipid efflux but were reversed by cyclodextrin-mediated cholesterol efflux. The apoptotic response observed in Abca1ⴚ/ⴚAbcg1ⴚ/ⴚ macrophages after oxidized phospholipid exposure or engulfment of apoptotic cells was dependent on an excessive oxidative burst secondary to enhanced assembly of NADPH oxidase (NOX)2 complexes, leading to sustained Jnk activation which turned on the apoptotic cell death program. Increased NOX2 assembly required Toll-like receptors 2/4 and MyD88 signaling, which are known to be enhanced in transporter deficient cells in a lipid raft– dependent fashion. Conclusions: We identified a new beneficial role of ABCA1, ABCG1 and HDL in dampening the oxidative burst and preserving viability of macrophages following exposure to oxidized phospholipids and/or apoptotic cells. (Circ Res. 2010;106:1861-1869.) Key Words: ABC transporters 䡲 HDL 䡲 cholesterol 䡲 efferocytosis 䡲 oxidative stress P apoptotic macrophages in the lung, heart and lesions of Abcg1⫺/⫺ and Abca1⫺/⫺Abcg1⫺/⫺ mice.9,10,12 The relationship of macrophage apoptosis to lesion development is complex, and whereas in early lesions efficient clearance of apoptotic cells by phagocytic macrophages (efferocytosis) may be associated with decreased lesion development, it is thought that in advanced lesions impaired efferocytosis leads to postapoptotic necrosis, inflammation and necrotic core formation.13–15 In previous studies, we showed substantial induction of Abca1 and Abcg1 expression in efferocytes largely attributable to activation of liver X receptor (LXR) transcription factors and massive efflux of cholesterol to acceptors in media.16,17 However, even in the absence of lipoprotein acceptors in media viability of efferocytes was preserved, reflecting cholesterol esterification and activation of prosurvival signaling pathways.17 In view of the prominent accumulation of apoptotic cells in tissues of Abcg1⫺/⫺ and lasma high-density lipoproteins (HDLs) have a protective role in atherogenesis, related in part to their ability to promote cholesterol efflux and suppress vascular inflammation.1–3 The ATP-binding cassette transporters ABCA1 and ABCG1 promote cholesterol efflux to apolipoprotein (apo)A-1 and HDL particles, respectively, and have been shown to decrease macrophage inflammatory and chemokine gene expression by suppressing signaling via Toll-like receptor (TLR)4/MyD88.4 –7 HDL also has been shown to reduce macrophage apoptosis in response to oxidized LDL,8 an effect that in part reflects the ability of ABCG1 to promote efflux of toxic 7-oxysterols to plasma HDL.8,9 Transplantation of Abca1⫺/⫺Abcg1⫺/⫺ bone marrow into hypercholesterolemic Ldlr-deficient mice results in markedly accelerated atherosclerosis and foam cell accumulation in various tissues including the lung, heart, liver, and intestine.10,11 Moreover, there is evidence of increased numbers of Original received January 17, 2010; revision received April 19, 2010; accepted April 20, 2010. From the Division of Molecular Medicine (L.Y.-C., T.A.P., T.A.S., E.T., C.L.W., I.T., A.R.T.), Department of Medicine, Columbia University, New York; and Department of Medicine (J.L.W.), University of California at San Diego, La Jolla. Correspondence to Laurent Yvan-Charvet, Division of Molecular Medicine, Department of Medicine, 630 W 168th St, Columbia University, New York, NY 10032. E-mail ly2159@columbia.edu © 2010 American Heart Association, Inc. Circulation Research is available at http://circres.ahajournals.org DOI: 10.1161/CIRCRESAHA.110.217281 1861 1862 Circulation Research June 25, 2010 Non-standard Abbreviations and Acronyms ABC apo ER HDL LXR MAPK NAC NOX ox-PAPC ROS siRNA TLR ATP-binding cassette transporter apolipoprotein endoplasmic reticulum high-density lipoprotein liver X receptor mitogen-activated protein kinase N-acetylcysteine NADPH oxidase oxidized 1-palmitoyl-2-arachidonoyl-sn-glycero3phosphocoline reactive oxygen species small interfering RNA Toll-like receptor Abca1⫺/⫺Abcg1⫺/⫺ mice, we have directly examined the role of these transporters in preserving the viability of efferocytes. Subsequent mechanistic studies have uncovered a novel role of the transporters in suppressing the oxidative burst mediated by NADPH oxidase (NOX)2 during efferocytosis. Methods An expanded Methods section is available in the Online Data Supplement at http://circres.ahajournals.org. Animals Abca1⫺/⫺, Abcg1⫺/⫺, and Abca1⫺/⫺Abcg1⫺/⫺ littermates in a mixed C57BL/6⫻DBA background were as previously described.10 Myd88⫺/⫺ mice on the C57BL/6 background were from Dr. Katherine Fitzgerald (University of Massachusetts). CD36⫺/⫺ mice on the C57BL/6 background were originally provided by Dr Roy Silverstein (Weill Medical College of Cornell University, New York). All mice were housed at Columbia University Medical Center according to animal welfare guidelines. Animals had ad libitum access to both food and water. Results Increased Susceptibility of Abca1ⴚ/ⴚAbcg1ⴚ/ⴚ Macrophages to Apoptosis After Engulfment of Apoptotic Cells Following ingestion of apoptotic Jurkat cells, macrophages deficient in ABCA1 and/or ABCG1 underwent apoptosis in the order Abca1⫺/⫺Abcg1⫺/⫺⬎Abcg1⫺/⫺⬎Abca1⫺/⫺, whereas wild-type (WT) macrophages were resistant to death (Figure 1A). A time course experiment already showed a slight induction of apoptosis in Abca1⫺/⫺Abcg1⫺/⫺ macrophages at 3 hours following efferocytosis and a dramatic 9-fold increase at 16 hours (Figure 1B). Phagocytosis, as measured by phagocytic index at 30 minutes after efferocytosis, was unaffected (Figure 1C). However, ingestion of or contact with apoptotic cells by Abca1⫺/⫺Abcg1⫺/⫺ macrophages appears to be required because addition of conditioned medium from apoptotic Jurkat cell culture to Abca1⫺/⫺Abcg1⫺/⫺ macrophages did not elicit a similar apoptotic response (Figure 1D). In terms of the mechanism we first considered that accumulation of free cholesterol after ingestion of apoptotic cells may induce ER-stress with subsequent induction of apoptosis.17 However, similar to previous observations,17 Abca1⫺/⫺Abcg1⫺/⫺ efferocytes showed increased ACAT activity when compared to WT, as reflected by enhanced free cholesterol conversion into cholesteryl ester, thereby preventing induction of CHOP mRNA and other ER stress markers (Online Figure I). By contrast, the use of E06 antibody known to recognize oxidized phospholipids and inhibit uptake of apoptotic cells,18 reduced apoptosis in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes (Figure 1D). The potential pathophysiological relevance of our system was illustrated by the finding of regions of enhanced E06 staining surrounding clusters of apoptotic cells (TUNEL-positive staining) in the lungs of Abcg1⫺/⫺ and Figure 1. Enhanced susceptibility to apoptosis in Abca1ⴚ/ⴚ, Abcg1ⴚ/ⴚ, and Abca1ⴚ/ⴚAbcg1ⴚ/ⴚ macrophages after ingestion of apoptotic Jurkat cells. Thioglycollate-elicited macrophages from mice on mixed background C57BL/6⫻DBA were incubated with apoptotic Jurkat cells for 30 minutes, extensively washed, and kept in DMEM 10% FCS for 16 more hours (A) or the indicated time period (B) before quantification of apoptosis by Annexin V staining. In parallel experiments, macrophages were incubated with Cell-Tracker red prelabeled apoptotic Jurkat cells to quantify the phagocytic index (PI) (C). Macrophages were incubated for 30 minutes with cultured media from apoptotic Jurkat cells or in presence of 0.5 mg/mL E06 antibody competitor during the 30 minutes apoptotic Jurkat cells incubation period (D) before quantification of apoptosis. Apoptotic cells were expressed as percentage of total cells as described in Methods. Results are means⫾SEM of experiments performed in triplicate. §P⬍0.05 vs WT; *P⬍0.05 treatment effect. Yvan-Charvet et al ABCA1, ABCG1, and Efferocyte Apoptosis 1863 Figure 2. HDL protects macrophages from apoptosis induced by ox-PAPC through modulation of membrane cholesterol. Macrophages were exposed to different concentrations of ox-PAPC (A) or treated for 16hours with 50 g/mL control PAPC or oxidized PAPC (ox-PAPC) (B). Ox-PAPC–treated WT, Abcg1⫺/⫺, and Abca1⫺/⫺Abcg1⫺/⫺ macrophages were also incubated simultaneously with different concentrations of HDL (0 to 100 g/mL) for 16 hours (C and D). WT and Abca1⫺/⫺Abcg1⫺/⫺ macrophages were pretreated with indicated amount of HDL for 30 minutes before efferocytosis (E). Pretreatment of WT and Abca1⫺/⫺Abcg1⫺/⫺ macrophages with 5 mmol/L cyclodextrin (CD) for 30 minutes before exposure to 50 g/mL ox-PAPC or with cyclodextrincholesterol (CD-c, 2.5:1) for 3 hours before efferocytosis (F). Apoptosis was quantified at the end of the 16-hour incubation period and expressed as percentage of total cells as described in Methods. Results are means⫾SEM. §P⬍0.05 vs WT; *P⬍0.05 treatment effect. Abca1⫺/⫺Abcg1⫺/⫺ bone marrow–transplanted mice compared to controls and Abca1⫺/⫺ mice (Online Figure II). The findings suggest that HDL and ABCG1 may act to limit formation of oxidized phospholipids and associated apoptotic events in the lung. High-Density Lipoprotein Protects Macrophages From Apoptosis Induced by Oxidized Phospholipids in an ABC Transporter–Dependent Fashion We recently showed that Abcg1⫺/⫺ macrophages have enhanced susceptibility to oxidized LDL induced apoptosis, an effect related to a specific role of ABCG1 in promoting efflux of 7-oxysterols to HDL.8 However, 7-ketocholesterol was undetectable in apoptotic Jurkat cells and in phagocytic macrophages (data not shown). The uptake of apoptotic cells by macrophages has many similarities to the uptake of oxidized LDL and oxidized phospholipids are a major bioactive component of both oxidized LDL and apoptotic cells.19,20 Treatment of macrophages with oxidized phospholipids (ie, oxidized 1-palmitoyl-2arachidonoyl-sn-glycero-3phosphocoline [ox-PAPC]) revealed a dose dependent increase in apoptosis in Abca1⫺/⫺Abcg1⫺/⫺ macrophages starting as low as 10 g/mL ox-PAPC loading (Figure 2A) and at 50 g/mL led to ⫺/⫺ a marked increase in apoptosis in the order Abca1 Abcg1⫺/⫺⬎ Abcg1⫺/⫺⬎ Abca1⫺/⫺⬎WT (Figure 2B), paralleling the effects of apoptotic Jurkat cells (Figure 1A). We next investigated the role of HDL on macrophage viability in WT and Abca1⫺/⫺Abcg1⫺/⫺ macrophages after ox-PAPC exposure. HDL markedly reduced apoptosis induced by ox-PAPC in WT macrophages at all concentrations tested and the maximum suppression was reached at 50 g/mL HDL (Figure 2C). The protective effect of HDL was dramatically reduced in Abcg1⫺/⫺ macrophages (Figure 2C) and virtually abolished in Abca1⫺/⫺Abcg1⫺/⫺ macrophages except at the highest HDL concentration (Figure 2D). Similar findings were observed in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes (Figure 2F). Because ABCA1 promotes efflux of both cholesterol and phospholipids from cells,21,22 and a possible role of ABCG1 in phospholipid efflux has also been described,23,24 we first considered that both transporters might participate in the efflux of oxidized phospholipids to HDL and thereby also protect from apoptosis. To test this hypothesis, efflux of ox-PAPC was determined after loading cells with radiolabeled [14C]-ox-PAPC. The amount of incorporated [14C]oxPAPC is shown in Online Figure III, A. HDL but not apoA-I showed a slight ability to promote ox-PAPC efflux but surprisingly, this effect was independent of ABCA1 and ABCG1 (Online Figure III, B). Thus, the increased suscep- 1864 Circulation Research June 25, 2010 Figure 3. The enhanced ROS response in Abca1ⴚ/ⴚAbcg1ⴚ/ⴚ macrophages after ingestion of apoptotic Jurkat cells or ox-PAPC loading mediated the apoptotic response. Thioglycollate-elicited macrophages from WT and Abca1⫺/⫺Abcg1⫺/⫺ mice were incubated with apoptotic Jurkat cells for 30 minutes, extensively washed and kept in DMEM 10% FCS for the indicated time period (A) or treated for 3 hours with 20 g/mL ox-PAPC (B) before quantification of ROS generation by CM-H2DCFDA staining. Macrophages were incubated in presence of 100 g/mL NAC during exposure to ox-PAPC (B) or with 100 g/mL NAC or 10 mmol/L glutathione (GSH) during the course of efferocytosis and apoptosis was quantified 16 hour later (C). Treatment of WT and Abca1⫺/⫺Abcg1⫺/⫺ macrophages with 100 g/mL HDL or pretreatment with 5 mmol/L cyclodextrin (CD) for 30 minutes before efferocytosis. ROS generation was quantified 1 hour later (D). Apoptotic cells and ROS positive cells were expressed as percentage of total cells as described in Methods. Results are means⫾SEM of experiments performed in triplicate. §P⬍0.05 vs WT; *P⬍0.05 treatment effect. tibility to ox-PAPC-induced apoptosis in Abca1⫺/⫺Abcg1⫺/⫺ macrophages could not be explained by impaired oxidized phospholipid efflux. Thus, we next considered that effects of HDL and ABC transporters on macrophage viability could be mediated by cholesterol efflux. Consistent with this idea, depletion of membrane cholesterol by cyclodextrin reduced the percentage of apoptotic cells after ox-PAPC exposure in both WT and Abca1⫺/⫺Abcg1⫺/⫺ macrophages and completely abolished the apoptosis of Abca1⫺/⫺Abcg1⫺/⫺ efferocytes (Figure 2F). In contrast, the loading of macrophages with cyclodextrin-cholesterol enhanced the apoptotic response during efferocytosis when both transporters were missing (Figure 2F). efferocytes to apoptosis. Two antioxidants, glutathione and N-acetylcysteine (NAC) showed marked antiapoptotic effects in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes (Figure 3C). Similarly, NAC significantly reduced the apoptosis induced by ox-PAPC in Abca1⫺/⫺Abcg1⫺/⫺ macrophages (Figure 3B). Remarkably, depletion of membrane cholesterol by either high concentration of HDL or cyclodextrin clearly reduced the production of ROS following ingestion of apoptotic cells in both WT and Abca1⫺/⫺Abcg1⫺/⫺ efferocytes (Figure 3D). An Increased Oxidative Burst in Abca1ⴚ/ⴚAbcg1ⴚ/ⴚ Macrophages After ox-PAPC Exposure or Engulfment of Apoptotic Cells Is Responsible for the Enhanced Apoptosis During bacterial phagocytosis, ROS generation is mediated by an NADPH oxidase complex, in which gp91phox/NOX2 is the major catalytic component in macrophages.28 Recent data have shown that gp91phox/NOX2 may also be activated during efferocytosis.29 Immunostaining for p47phox clustering (red staining), one of the active components of the NADPH oxidase complex known to translocate from a cytosolic pool to the plasma membrane during active complex formation, revealed an increase in number of both cluster-positive cells and p47phox clusters per cell for Abca1⫺/⫺Abcg1⫺/⫺ macrophages compared to controls in the basal state (Figure 4A and 4B). Ox-PAPC increased the number of positive cells and the number of p47 clusters per cell in WT macrophages and this was further enhanced in Abca1⫺/⫺Abcg1⫺/⫺ macrophages (Figure 4A and 4B). As previously shown for bacterial phagocytosis, 30 minutes after ingestion of apoptotic cells (green staining), a considerable amount of p47phox staining was localized in phagolysosomal membranes surrounding the apoptotic cells (yellow staining: overlap between green apoptotic cells and red p47phox staining) compared to nonphagocytic cells as shown in Figure 4C (left). Performing crosssectional cuts through the phagolysosome indicate more We recently reported that ABCG1 deficiency induced an exaggerated ROS production in endothelial cells in response to 7-ketocholesterol.25 Oxidized phospholipids are also known to induce ROS formation,26,27 a mechanism that may play a crucial role during phagocytosis of bacteria and possibly apoptotic cells by macrophages.28,29 The ingestion of apoptotic Jurkat cells was associated with a transient increase in ROS formation in WT macrophages. The increase in ROS was exaggerated in Abca1⫺/⫺Abcg1⫺/⫺ macrophages (Figure 3A). An enhanced formation of ROS was observed after exposure to ox-PAPC in DKO macrophages (Figure 3B). Consistent with this finding, we found that the mRNA levels of heme oxygenase-1 (HO-1), a marker of oxidative stress were increased during the course of efferocytosis in Abca1⫺/⫺Abcg1⫺/⫺ macrophages as well as after ox-PAPC loading (Online Figure IV). These results led us to investigate if the enhanced oxidative response may be responsible for the increased susceptibility of Abca1⫺/⫺Abcg1⫺/⫺ Increased NOX2 Assembly After ox-PAPC Exposure or Efferocytosis in Abca1ⴚ/ⴚAbcg1ⴚ/ⴚ Macrophages Yvan-Charvet et al ABCA1, ABCG1, and Efferocyte Apoptosis 1865 Figure 4. Increased assembly of NADPH oxidase 2 (NOX2) in Abca1ⴚ/ⴚ Abcg1ⴚ/ⴚ macrophages after ox-PAPC exposure or ingestion of apoptotic Jurkat cells. Confocal analysis of p47phox stained (red) peritoneal macrophages from WT and Abca1⫺/⫺ Abcg1⫺/⫺ mice exposed to ox-PAPC for 1 hour (A and B) or to Cell-Tracker green prelabeled apoptotic Jurkat cells for 30 minutes (C and D). Arrows indicate p47phox clusters in nonphagocytic cells (red staining) (A). Representative images of an ingested apoptotic cell (green) localized within a phagolysosome (C left hand panel, in total five different confocal images were analyzed per genotype). Visualization of the phagolysosome surrounding p47phox staining by performing a horizontal (indicated by the green line) and a vertical (indicated by the red line) cross-cut through the z-stack (C right hand panels). Inserts on top and right hand side portray the flipped image of the phagolysosomes after the cross-cut. Quantification was performed as described in the Methods with the use of ImageJ software (B and D). Macrophages were incubated in presence of 10 mol/L NOX2 inhibitor (DPI) during the course of efferocytosis (E) or treated with scrambled or NOX2 siRNA before ingestion of apoptotic Jurkat cells (F). At the end of the 16 hour incubation, apoptosis was determined. Results are means⫾SEM of an experiment performed in triplicate. §P⬍0.05 vs WT; *P⬍0.05 treatment effect. clearly the p47phox lining (red) surrounding the apoptotic cell (green) (Figure 4C, right). Quantification of the phagolysosomal p47phox staining at 30 minutes after efferocytosis revealed a 3-fold increased signal in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes compared to WT (Figure 4C and 4D). The use of NOX2 inhibitor (Figure 4E) and knockdown experiments (Figure 4F) confirmed that the enhanced apoptotic response in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes required the activity of NOX2. ptotic Jurkat cells (Figure 5A). We also observed a corresponding increase in the cleaved form of caspase 3 in Abca1⫺/⫺Abcg1⫺/⫺ macrophages (Figure 5A) a marker for apoptosis.34 This time course of JNK and caspase-3 activation correlated well with the early induction of apoptosis in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes (Figure 1B). An inhibitor of JNK prevented apoptosis of Abca1⫺/⫺Abcg1⫺/⫺ efferocytes indicating that JNK is necessary in this pathway (Figure 5B). Sustained JNK Activation After Engulfment of Apoptotic Cells in Abca1ⴚ/ⴚAbcg1ⴚ/ⴚ Macrophages Apoptosis of Efferocytes Is Dependent on TLR4/MyD88 Signaling in Transporter-Deficient Cells Apoptosis is thought to represent the outcome of an imbalance between prosurvival and proapoptotic signaling pathways. Neither the prosurvival nuclear factor B or p38 mitogen-activated protein kinase (p38MAPK) pathway,30,31 appeared to be downregulated in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes as reflected by similar protein levels of IKKb and p38MAPK during the course of efferocytosis (Figure 5A). An important form of apoptotic signaling induced by ROS generation involves sustained activation of JNK.32,33 Western blot analysis of JNK phosphorylation revealed an increase in both early and late phases of JNK phosphorylation in Abca1⫺/⫺Abcg1⫺/⫺ macrophages following ingestion of apo- Myd88 signaling has been shown to play a key role in the assembly of the NADPH oxidase complex during phagocytosis of Gram-negative bacteria,35 and we have previously shown that ABC transporter deficient macrophages show increased signaling via TLR4 and TLR2 in a cholesterol lipid raft dependent fashion.7 Thus, we next determined if increased signaling via TLR/MyD88 was responsible for increased NOX2 assembly during efferocytosis. Treatment of elicited macrophages with LipidA dramatically increased the number of p47-immunopositive cells and the number of p47clusters per cell in Abca1⫺/⫺Abcg1⫺/⫺ macrophages compared to WT macrophages (Figure 6A and 6B). Although LipidA by itself 1866 Circulation Research June 25, 2010 line Figure V, A). We next tested whether inhibiting toll-like receptor signaling prevented the apoptotic response of Abca1⫺/⫺Abcg1⫺/⫺ efferocytes. Although knockdown of intracellular TLRs by small interfering (si)RNA, including TLR3, 7 and 8, did not show any beneficial effect, deficiency of TLR4 and to a lesser extent TLR2 reduced apoptosis in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes (Figure 6D). We also investigated a possible role of CD36 signaling because it has been implicated in the recognition of phospholipids present on the outer leaflet of the plasma membrane of apoptotic cells,19 and interacts with TLR2 and TLR4.36,37 However, CD36 did not contribute to apoptosis in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes when assayed by siRNA knockdown of ABCA1 and ABCG1 in Cd36⫺/⫺ macrophages, siRNA knockdown of CD36 in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes or by the use of CD36 blocking antibody (Online Figure V, B and C). These findings suggest that activation of Myd88 signaling through activation of plasma membrane TLR4, and to a lesser extent TLR2, contributes to the increased susceptibility of Abca1⫺/⫺Abcg1⫺/⫺ macrophages to apoptosis following ingestion of apoptotic cells. To confirm this, we generated Abcg1⫺/⫺Myd88⫺/⫺ mice and performed an efferocytosis assay in elicited macrophages. Lack of MyD88 clearly abrogated both the apoptosis and the ROS generation observed in Abcg1⫺/⫺ efferocytes (Figure 6E and 6F). Discussion Figure 5. Sustained JNK activation is required for the induction of apoptosis in Abca1ⴚ/ⴚAbcg1ⴚ/ⴚ efferocytes. Thioglycollate-elicited macrophages from WT and Abca1⫺/⫺Abcg1⫺/⫺ mice were incubated with apoptotic Jurkat cells for 30 minutes, extensively washed and kept in DMEM 10% FCS for the indicated time period. Immunoblots of IKKb, p-p38MAPK, p-JNK, and caspase 3 were performed in a time course experiment (A). The arrow in the caspase 3 immunoblot indicates the proactive cleaved form of caspase 3, and the upper band indicates the uncleaved form. Macrophages were incubated in presence of 10 mol/L JNK inhibitor (L-JNKI1) during the course of efferocytosis and analyzed for apoptosis 16 hours later (B). Results are means⫾SEM of an experiment performed in triplicate. §P⬍0.05 vs WT. did not induce significant ROS generation, pretreatment with LipidA before efferocytosis markedly amplified ROS production (Figure 6C) and enhanced TLR4 signaling led to an exaggerated apoptotic response during efferocytosis in the order Abca1⫺/⫺Abcg1⫺/⫺⬎Abcg1⫺/⫺⬎Abca1⫺/⫺⬎WT (On- Previous studies have shown an increased accumulation of apoptotic cells in atherosclerotic lesions, lungs and other tissues in Abcg1⫺/⫺ and Abca1⫺/⫺Abcg1⫺/⫺ mice.9,10,12 In addition, Abcg1⫺/⫺ macrophages are more susceptible to apoptosis induced by oxidized LDL or 7-oxysterols, related in part to a role of ABCG1 in promoting efflux of 7-oxysterols.8 Abca1⫺/⫺Abcg1⫺/⫺ macrophages show increased apoptosis in response to FC loading (AcLDL⫹ACAT inhibitor), likely related to the role of the transporters in promoting efflux of cholesterol from macrophages.10 In this study, we have uncovered an unexpected role of ABCA1 and ABCG1 in preserving the viability of macrophages during efferocytosis and also in mediating a protective role of HDL in defending macrophages against oxidized phospholipid-induced cell death. Interestingly, the underlying mechanism is not FCinduced ER stress as we had expected but appears to be related to a novel role of the ABC transporters and HDL in dampening the oxidative burst of NOX2 which is activated during efferocytosis and in response to oxidized phospholipid uptake. In turn this may be related to the role of the transporters in diminishing the signaling of TLRs, mediated by cholesterol efflux and transporter-dependent changes in membrane lipid organization.4 –7 TLR/MyD88 signaling is known to induce NOX2 assembly,35 and was shown to have an essential role in ROS formation and apoptosis in our system. In earlier studies, we showed a marked upregulation of ABCA1 and ABCG1 in efferocytes, mediated mainly by LXR activation (ABCA1 and ABCG1) and in part by tumor necrosis factor ␣ signaling via nuclear factor B (ABCA1).16,38 Consistent with these observations, efferocytes showed a massive efflux of cholesterol to HDL or apoA-1.17 Even in the absence of cholesterol efflux, there was only a Yvan-Charvet et al ABCA1, ABCG1, and Efferocyte Apoptosis 1867 Figure 6. TLR-dependent Myd88 signaling controls NADPH oxidase assembly, ROS production, and the apoptotic response of Abca1ⴚ/ⴚAbcg1ⴚ/ⴚ efferocytes. Confocal analysis of peritoneal macrophages from WT and Abca1⫺/⫺Abcg1⫺/⫺ mice exposed to 100 ng/mL LipidA for 3 hours (A). Arrows indicate stained p47phox clusters. Quantification was performed as described in Methods (B). Peritoneal macrophages from WT and Abca1⫺/⫺Abcg1⫺/⫺ mice were exposed to 100 ng/mL LipidA for 3 hours, following or not by ingestion of apoptotic Jurkat cells and ROS was quantified 3 hours later (C). Macrophages isolated from WT and Abca1⫺/⫺Abcg1⫺/⫺ mice were treated with scrambled or different TLR receptor siRNAs and analyzed for apoptosis after efferocytosis (D). Macrophages isolated from WT, Abcg1⫺/⫺, Myd88⫺/⫺, and Abcg1⫺/⫺Myd88⫺/⫺ littermate mice were analyzed for both apoptosis and ROS generation 16 and 3 hours after efferocytosis, respectively (E and F). Results are means⫾SEM of experiments performed in triplicate. §P⬍0.05 vs WT; *P⬍0.05 treatment effect. low level of apoptosis, reflecting compensatory cholesterol esterification as well as induction of antiapoptotic signaling pathways via AKT and nuclear factor B.17 The present study also revealed a compensatory increase in cholesterol esterification in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes, but clearly this mechanism was insufficient to protect these cells from death revealing that, although lipoprotein acceptors in media may not be essential, activity of the 2 main transporters involved in macrophage cholesterol efflux is crucial to the survival of macrophages following ingestion of apoptotic cells. Part of this apparent paradox may reflect the ability of ABCG1 to promote cholesterol efflux to BSA even in the absence of cholesterol efflux acceptors,23 as previously used to culture WT efferocytes.17 More importantly, it likely reflects a specific ability of ABCA1 and ABCG1 to promote transmembrane sterol redistribution even in the absence of cholesterol acceptors in the medium, as previously suggested.39,40 Consistent with this idea, we previously reported enhanced lipid raft formation in Abca1⫺/⫺Abcg1⫺/⫺ macrophages in the absence of lipoprotein acceptors.7 Interestingly, the mechanism underlying the increased plasma membrane cholesterol-dependent apoptosis in Abca1⫺/⫺Abcg1⫺/⫺ macrophages after ox-PAPC exposure or engulfment of apoptotic cells was found to be an amplified burst of oxidative stress secondary to increased assembly of NOX2, the major NADPH oxidase complex present in macrophages.28 Although macrophage ROS generation during bacterial phagocytosis is well known as an important killing mechanism,28 and oxidized phospholipids are also known to promote ROS generation at least in endothelial cells,26,27 this is the first report to our knowledge showing that such a mechanism can also occur in macrophages during efferocytosis. Our studies are also consistent with important recent observations showing that reconstituted HDL suppresses NOX2 assembly and activity in neutrophils treated with phorbol ester in a cholesterol lipid raft– dependent fashion,41 and together these studies suggest that this property of reconstituted HDL may be dependent on activity of the transporters. The new findings could indicate the importance of the localization of NOX2 in lipid rafts,42 and are consistent with the previous proposed role of NOX2 and ROS as signaling molecules in macrophages.43 Recent advances in this area of research have revealed a close relationship between NOX enzymes and toll-like receptor signaling during phagocytosis of bacteria.44 Similar to what was observed with phagocytosis of bacteria,35 we found that lack of MyD88 prevented the generation of ROS during efferocytosis in WT and Abcg1⫺/⫺ cells. We identified TLR4 as a major component of this regulation in Abca1⫺/⫺Abcg1⫺/⫺ efferocytes and to a lesser extent TLR2 consistent with our previous findings showing enhanced 1868 Circulation Research June 25, 2010 TLR2 and TLR4 signaling pathways in Abca1⫺/⫺Abcg1⫺/⫺ macrophages.7 Overall, our data are consistent with a mechanism wherein ABCG1 and to a lesser extent ABCA1 promote membrane sterol redistribution and efflux to HDL, decreasing lipid raft– dependent assembly of TLR4 and NOX2 signaling complexes. Recent studies have shown that in addition to upregulation of ABCA1 and ABCG1 during efferocytosis, there is induction of the efferocytotic receptor mer-TK by LXRs.38 Together, these studies suggest coordinate functions of LXRs and the ABC transporters in promoting both efferocytosis and in preserving viability of phagocytes in the face of the resultant loading with cholesterol. Defects in these processes may lead to auto-immune disease,28,38,45 accelerated atherosclerosis with increased accumulation of apoptotic material and necrotic core formation in advanced plaques,10,13–15 and here we show evidence as well of a role of these processes in diseased lungs with increased accumulation of apoptotic cells and oxidized phospholipids staining with E06 in Abcg1⫺/⫺ and Abca1⫺/⫺Abcg1⫺/⫺ bone marrow–transplanted mice extending a recent report identifying oxidative stress, formation of oxidized phospholipids and TLR4 signaling as a key pathway of acute lung injury.46 Sources of Funding This work was supported by NIH grant HL59541. Disclosures None. References 1. Barter PJ, Puranik R, Rye KA. New insights into the role of HDL as an anti-inflammatory agent in the prevention of cardiovascular disease. Curr Cardiol Rep. 2007;9:493– 498. 2. Navab M, Anantharamaiah GM, Fogelman AM. The effect of apolipoprotein mimetic peptides in inflammatory disorders other than atherosclerosis. Trends Cardiovasc Med. 2008;18:61– 66. 3. Tall AR, Yvan-Charvet L, Terasaka N, Pagler T, Wang N. HDL, ABC transporters, and cholesterol efflux: implications for the treatment of atherosclerosis. Cell Metab. 2008;7:365–375. 4. Koseki M, Hirano K, Masuda D, Ikegami C, Tanaka M, Ota A, Sandoval JC, Nakagawa-Toyama Y, Sato SB, Kobayashi T, Shimada Y, OhnoIwashita Y, Matsuura F, Shimomura I, Yamashita S. Increased lipid rafts and accelerated lipopolysaccharide-induced tumor necrosis factor-alpha secretion in Abca1-deficient macrophages. J Lipid Res. 2007;48: 299 –306. 5. Zhu X, Lee JY, Timmins JM, Brown JM, Boudyguina E, Mulya A, Gebre AK, Willingham MC, Hiltbold EM, Mishra N, Maeda N, Parks JS. Increased cellular free cholesterol in macrophage-specific Abca1 knock-out mice enhances pro-inflammatory response of macrophages. J Biol Chem. 2008;283:22930 –22941. 6. Baldan A, Gomes AV, Ping P, Edwards PA. Loss of ABCG1 results in chronic pulmonary inflammation. J Immunol. 2008;180:3560 –3568. 7. Yvan-Charvet L, Welch C, Pagler TA, Ranalletta M, Lamkanfi M, Han S, Ishibashi M, Li R, Wang N, Tall AR. Increased inflammatory gene expression in ABC transporter-deficient macrophages: free cholesterol accumulation, increased signaling via toll-like receptors, and neutrophil infiltration of atherosclerotic lesions. Circulation. 2008;118:1837–1847. 8. Terasaka N, Wang N, Yvan-Charvet L, Tall AR. High-density lipoprotein protects macrophages from oxidized low-density lipoprotein-induced apoptosis by promoting efflux of 7-ketocholesterol via ABCG1. Proc Natl Acad Sci U S A. 2007;104:15093–15098. 9. Baldan A, Pei L, Lee R, Tarr P, Tangirala RK, Weinstein MM, Frank J, Li AC, Tontonoz P, Edwards PA. Impaired development of atherosclerosis in hyperlipidemic Ldlr-/- and ApoE-/- mice transplanted with Abcg1-/- bone marrow. Arterioscler Thromb Vasc Biol. 2006;26: 2301–2307. 10. Yvan-Charvet L, Ranalletta M, Wang N, Han S, Terasaka N, Li R, Welch C, Tall AR. Combined deficiency of ABCA1 and ABCG1 promotes foam cell accumulation and accelerates atherosclerosis in mice. J Clin Invest. 2007;117:3900 –3908. 11. Out R, Hoekstra M, Habets K, Meurs I, de Waard V, Hildebrand RB, Wang Y, Chimini G, Kuiper J, Van Berkel TJ, Van Eck M. Combined deletion of macrophage ABCA1 and ABCG1 leads to massive lipid accumulation in tissue macrophages and distinct atherosclerosis at relatively low plasma cholesterol levels. Arterioscler Thromb Vasc Biol. 2008;28:258 –264. 12. Wojcik AJ, Skaflen MD, Srinivasan S, Hedrick CC. A critical role for ABCG1 in macrophage inflammation and lung homeostasis. J Immunol. 2008;180:4273– 4282. 13. Tabas I. Consequences and therapeutic implications of macrophage apoptosis in atherosclerosis: the importance of lesion stage and phagocytic efficiency. Arterioscler Thromb Vasc Biol. 2005;25:2255–2264. 14. Ait-Oufella H, Pouresmail V, Simon T, Blanc-Brude O, Kinugawa K, Merval R, Offenstadt G, Leseche G, Cohen PL, Tedgui A, Mallat Z. Defective mer receptor tyrosine kinase signaling in bone marrow cells promotes apoptotic cell accumulation and accelerates atherosclerosis. Arterioscler Thromb Vasc Biol. 2008;28:1429 –1431. 15. Thorp E, Cui D, Schrijvers DM, Kuriakose G, Tabas I. Mertk receptor mutation reduces efferocytosis efficiency and promotes apoptotic cell accumulation and plaque necrosis in atherosclerotic lesions of apoe-/mice. Arterioscler Thromb Vasc Biol. 2008;28:1421–1428. 16. Gerbod-Giannone MC, Li Y, Holleboom A, Han S, Hsu LC, Tabas I, Tall AR. TNFalpha induces ABCA1 through NF-kappaB in macrophages and in phagocytes ingesting apoptotic cells. Proc Natl Acad Sci U S A. 2006; 103:3112–3117. 17. Cui D, Thorp E, Li Y, Wang N, Yvan-Charvet L, Tall AR, Tabas I. Pivotal advance: macrophages become resistant to cholesterol-induced death after phagocytosis of apoptotic cells. J Leukoc Biol. 2007;82: 1040 –1050. 18. Chang MK, Bergmark C, Laurila A, Horkko S, Han KH, Friedman P, Dennis EA, Witztum JL. Monoclonal antibodies against oxidized lowdensity lipoprotein bind to apoptotic cells and inhibit their phagocytosis by elicited macrophages: evidence that oxidation-specific epitopes mediate macrophage recognition. Proc Natl Acad Sci U S A. 1999;96: 6353– 6358. 19. Fadok VA, Bratton DL, Frasch SC, Warner ML, Henson PM. The role of phosphatidylserine in recognition of apoptotic cells by phagocytes. Cell Death Differ. 1998;5:551–562. 20. Chou MY, Hartvigsen K, Hansen LF, Fogelstrand L, Shaw PX, Boullier A, Binder CJ, Witztum JL. Oxidation-specific epitopes are important targets of innate immunity. J Intern Med. 2008;263:479 – 488. 21. Wang N, Silver DL, Costet P, Tall AR. Specific binding of ApoA-I, enhanced cholesterol efflux, and altered plasma membrane morphology in cells expressing ABC1. J Biol Chem. 2000;275:33053–33058. 22. Oram JF, Lawn RM, Garvin MR, Wade DP. ABCA1 is the cAMPinducible apolipoprotein receptor that mediates cholesterol secretion from macrophages. J Biol Chem. 2000;275:34508 –34511. 23. Wang N, Lan D, Chen W, Matsuura F, Tall AR. ATP-binding cassette transporters G1 and G4 mediate cellular cholesterol efflux to high-density lipoproteins. Proc Natl Acad Sci U S A. 2004;101:9774 –9779. 24. Kobayashi A, Takanezawa Y, Hirata T, Shimizu Y, Misasa K, Kioka N, Arai H, Ueda K, Matsuo M. Efflux of sphingomyelin, cholesterol, and phosphatidylcholine by ABCG1. J Lipid Res. 2006;47:1791–1802. 25. Terasaka N, Yu S, Yvan-Charvet L, Wang N, Mzhavia N, Langlois R, Pagler T, Li R, Welch CL, Goldberg IJ, Tall AR. ABCG1 and HDL protect against endothelial dysfunction in mice fed a high-cholesterol diet. J Clin Invest. 2008;118:3701–3713. 26. Rouhanizadeh M, Hwang J, Clempus RE, Marcu L, Lassegue B, Sevanian A, Hsiai TK. Oxidized-1-palmitoyl-2-arachidonoyl-sn-glycero-3phosphorylcholine induces vascular endothelial superoxide production: implication of NADPH oxidase. Free Radic Biol Med. 2005;39: 1512–1522. 27. Gharavi NM, Baker NA, Mouillesseaux KP, Yeung W, Honda HM, Hsieh X, Yeh M, Smart EJ, Berliner JA. Role of endothelial nitric oxide synthase in the regulation of SREBP activation by oxidized phospholipids. Circ Res. 2006;98:768 –776. 28. Bedard K, Krause KH. The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev. 2007;87: 245–313. 29. Russell DG. New ways to arrest phagosome maturation. Nat Cell Biol. 2007;9:357–359. Yvan-Charvet et al 30. Seimon TA, Obstfeld A, Moore KJ, Golenbock DT, Tabas I. Combinatorial pattern recognition receptor signaling alters the balance of life and death in macrophages. Proc Natl Acad Sci U S A. 2006;103:19794–19799. 31. Seimon TA, Wang Y, Han S, Senokuchi T, Schrijvers DM, Kuriakose G, Tall AR, Tabas IA. Macrophage deficiency of p38alpha MAPK promotes apoptosis and plaque necrosis in advanced atherosclerotic lesions in mice. J Clin Invest. 2009;119:886 – 898. 32. Kamata H, Honda S, Maeda S, Chang L, Hirata H, Karin M. Reactive oxygen species promote TNFalpha-induced death and sustained JNK activation by inhibiting MAP kinase phosphatases. Cell. 2005;120: 649 – 661. 33. Dhanasekaran DN, Reddy EP. JNK signaling in apoptosis. Oncogene. 2008;27:6245– 6251. 34. Lakhani SA, Masud A, Kuida K, Porter GA, Jr., Booth CJ, Mehal WZ, Inayat I, Flavell RA. Caspases 3 and 7: key mediators of mitochondrial events of apoptosis. Science. 2006;311:847– 851. 35. Laroux FS, Romero X, Wetzler L, Engel P, Terhorst C. Cutting edge: MyD88 controls phagocyte NADPH oxidase function and killing of gram-negative bacteria. J Immunol. 2005;175:5596 –5600. 36. Moore KJ, Freeman MW. Scavenger receptors in atherosclerosis: beyond lipid uptake. Arterioscler Thromb Vasc Biol. 2006;26:1702–1711. 37. Stewart CR, Stuart LM, Wilkinson K, van Gils JM, Deng J, Halle A, Rayner KJ, Boyer L, Zhong R, Frazier WA, Lacy-Hulbert A, Khoury JE, Golenbock DT, Moore KJ. CD36 ligands promote sterile inflammation through assembly of a Toll-like receptor 4 and 6 heterodimer. Nat Immunol. 2010;11:155–161. 38. A-Gonzalez N, Bensinger SJ, Hong C, Beceiro S, Bradley MN, Zelcer N, Deniz J, Ramirez C, Diaz M, Gallardo G, de Galarreta CR, Salazar J, Lopez F, Edwards P, Parks J, Andujar M, Tontonoz P, Castrillo A. Apoptotic cells promote their own clearance and immune tolerance ABCA1, ABCG1, and Efferocyte Apoptosis 39. 40. 41. 42. 43. 44. 45. 46. 1869 through activation of the nuclear receptor LXR. Immunity. 2009;31: 245–258. Wang N, Ranalletta M, Matsuura F, Peng F, Tall AR. LXR-induced redistribution of ABCG1 to plasma membrane in macrophages enhances cholesterol mass efflux to HDL. Arterioscler Thromb Vasc Biol. 2006; 26:1310 –1316. Vaughan AM, Oram JF. ABCG1 redistributes cell cholesterol to domains removable by high density lipoprotein but not by lipid-depleted apolipoproteins. J Biol Chem. 2005;280:30150 –30157. Peshavariya H, Dusting GJ, Di Bartolo B, Rye KA, Barter PJ, Jiang F. Reconstituted high-density lipoprotein suppresses leukocyte NADPH oxidase activation by disrupting lipid rafts. Free Radic Res. 2009;43: 772–782. Ushio-Fukai M. Localizing NADPH oxidase-derived ROS. Sci STKE. 2006:re8. Forman HJ, Torres M. Reactive oxygen species and cell signaling: respiratory burst in macrophage signaling. Am J Respir Crit Care Med. 2002;166(12 Pt 2):S4 –S8. Ogier-Denis E, Mkaddem SB, Vandewalle A. NOX enzymes and Toll-like receptor signaling. Semin Immunopathol. 2008;30:291–300. Wilhelm AJ, Zabalawi M, Grayson JM, Weant AE, Major AS, Owen J, Bharadwaj M, Walzem R, Chan L, Oka K, Thomas MJ, Sorci-Thomas MG. Apolipoprotein A-I and its role in lymphocyte cholesterol homeostasis and autoimmunity. Arterioscler Thromb Vasc Biol. 2009;29: 843– 849. Imai Y, Kuba K, Neely GG, Yaghubian-Malhami R, Perkmann T, van Loo G, Ermolaeva M, Veldhuizen R, Leung YH, Wang H, Liu H, Sun Y, Pasparakis M, Kopf M, Mech C, Bavari S, Peiris JS, Slutsky AS, Akira S, Hultqvist M, Holmdahl R, Nicholls J, Jiang C, Binder CJ, Penninger JM. Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell. 2008;133:235–249. Novelty and Significance What Is Known? ● ● ● Expression of Abca1 and Abcg1 is induced in macrophages following ingestion of apoptotic cells. The numbers of apoptotic macrophages in lungs and atherosclerotic lesions are increased in Abcg⫺/⫺ and Abca1⫺/⫺ Abcg1⫺/⫺ mice. Oxidized LDL induces apoptosis of Abcg1⫺/⫺ and Abca1⫺/⫺Abcg1⫺/⫺ macrophage. What New Information Does This Article Contribute? ● ● ● Abcg1⫺/⫺ and Abca1⫺/⫺Abcg1⫺/⫺ macrophages undergo markedly increased apoptosis following ingestion of apoptotic cells or after exposure to oxidized phospholipids. The mechanism involves membrane cholesterol accumulation, increased signaling via TLR4/MyD88 that promotes assembly of NADPH oxidase (NOX)2 complexes, and excessive ROS formation. The apoptosis of macrophages following uptake of oxidized phospholipids or apoptotic cells likely leads to a chain reaction of cell death and inflammation. The ATP-binding cassette transporters ABCA1 and ABCG1 promote cholesterol efflux to apolipoprotein A-1 and HDL and likely mediate, in part, the antiatherogenic effect of HDL. Deficiency of ABCG1 or ABCA1 and ABCG1 in mice leads to accumulation of apoptotic macrophages in lungs and atherosclerotic lesions. ABCA1 and ABCG1 are highly induced in macrophages following phagocytosis of apoptotic cells (efferocytosis). Although Abcg1⫺/⫺ and Abca1⫺/⫺Abcg1⫺/⫺ macrophages could ingest apoptotic cells normally, soon afterward they themselves underwent apoptotic cell death. This was caused by an excessive oxidative burst attributable to increased assembly of the NADPH oxidase–NOX2 complex in the plasma and the endosomal membranes of transporter-deficient macrophages. The findings indicate that HDL and the ABC transporters normally act to maintain a correct cholesterol content and distribution in the plasma and endosomal membranes of cholesterol-loaded efferocytes, preventing excessive NOX2 activity. This represents a new extension of the idea that HDL and the transporters suppress inflammation during the innate immune response.