Cal Care IPA Utilization Management and Case Management
advertisement

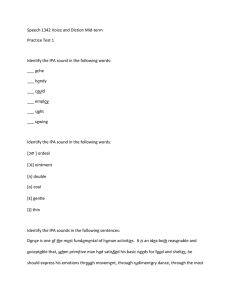
Cal Care IPA 2115 Compton Ave., Corona, CA 92881 phone 951.280.7700 | fax 951.280.8200 Utilization Management and Case Management The role of the Utilization Management (UM) Department and Case Management (CM) Department is to ensure consistent delivery of appropriate and quality health care services to our members. The UM and CM functions include pre-certification, inpatient concurrent reviews, discharge planning, and retrospective reviews. The Utilization Management and Case Management departments make decisions only on appropriateness of care and service, including existence of coverage. Cal Care IPA does not reward (directly or indirectly) practitioners or other individuals for issuing denials of coverage or service care. There are no financial incentives that would encourage UM and CM decision makers to make decisions that would result in under-utilization of services. Practitioners are ensured independence and impartiality in making referral decisions that will not influence: hiring, compensation, termination, promotion, and any other similar matters. The UM and CM Departments use clinically sound, nationally developed and accepted criteria for making medical necessity decisions. The following is a listing of the clinical criteria used, but is not limited to: Health Plan Developed Guidelines Milliman Care Guidelines, 17th Edition Apollo’s Medical Review Criteria, 13th Edition, 2014 Apollo’s Managing Behavioral Healthcare, 4th Edition, update 2014 CMS Guidelines Medi-Cal Guidelines Health Plan Benefit Manual American College of Obstetrics and Gynecology The American Academy of Pediatrics The United States Preventative Services Task Force Standards Health Plan Clinical Practice Guidelines including Behavioral Health guidelines To access the health services departments and/or the UM and CM Staff for questions about the UM process and how to obtain copies of UM and CM Criteria please call the UM and CM Departments at (951) 280-7700 or Toll Free 1-855-257-9964 during our regular business hours of 8:00 am to 5:00 pm. UM and CM criteria, policies and procedures used to authorize, modify, or deny healthcare services are available, upon request, to members or members’ designated representatives, contracted health care practitioners, providers and to the public. The UM and CM Criteria(s) are available as a copy, to be read over the phone, available for review at each provider office sites and/or group site, distributed via the internet, via fax, mailed, or sent via email. The IPA/PMG will provide a paper copy upon request. Notification of availability is posted on the IPA/PMG website and distributed annually or as needed as communication and updates.