31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum
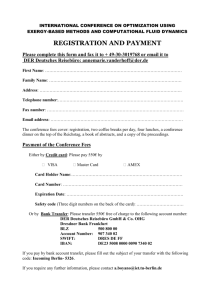
advertisement

Abstracts 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber Datum/Ort: 30.–31. Januar 2015, M!nchen Kongresspr!sidentin: Kongresssekret!r: Prof. Dr. Ulrike Protzer Prof. Dr. Jacob Nattermann A1 1. Fibrogenesis 1. Fibrogenesis Rolle des Mas Rezeptors in der Leberfibrose A18 2. Clinical Hepatology A27 3. Metabolism/Transport A36 4. Tumors/Liver Surgery A53 5. Virus Immunology 1.1 Klein S1, Thies SJ2, Beck J2, Schierwagen R1, Masing N1, Hiththetiya K3, Sch!tz E2, Strassburg CP1, Sauerbruch T1, Trebicka J1 1 University Hospital Bonn, Internal medicine I, Bonn, Germany; 2Chronix, Biomedical GmbH, G"ttingen, Germany; 3 University Hospital Bonn, Pathology, Bonn, Germany Hintergrund: Das Renin-Angiotensin-System spielt eine wichtige Rolle in der Entwicklung der Leberfibrose. Neben dem klassischen Signalweg, !ber den profibrotischen Angiotensin II typ 1 Rezeptor (AT1R), besteht ein alternativer Signalweg, der !ber den MasR antifibrotische Effekte vermittelt. In der Leberfibrose dominiert der AT1R vermittelte klassische Signalweg, der zur Aktivierung der hepatischen Sternzellen (HSCs) f!hrt. Die Rolle des alternativen Signalwegs !ber den MasR und dessen Bedeutung in der Leberfibrose sind bislang noch nicht vollst"ndig aufgekl"rt. Deshalb untersuchten wir die hepatische Expression des MasR und involvierte Signalwege im Menschen und in MasR-/- M"usen bei der Leberfibrose. Methoden: Aus MasR-/- und wt M"usen wurden HSCs isoliert und mit Ang-(1 – 7) stimuliert, oder unbehandelt gelassen. Mittels Next Generation Sequencing wurde das Transkriptom dieser HSCs untersucht. Die Leberfibrose wurde in MasR-/- und wt M"usen durch die Gallengangsligatur (BDL) oder durch eine CCl4-Intoxikation induziert. Die Leberfibrose wurde mittels Western Blots, Hydroxyprolin-Gehalt und F"rbungen untersucht. In menschlichen und murinen Lebern wurden die Komponenten des Renin-Angiotensin-Systems mittels Western Blots, RT-RCRs und immunohistochemisch analysiert. Ergebnisse: Mehr als 600 Gene sind signifikant runterreguliert in MasR-/- HSCs im Vergleich zu wt HSCs. Gleichzeitig sind in MasR-/- HSCs Gene der Extrazellul"ren Matrix, des Zytoskelets, des MAPK Signalwegs, des PI3K Akt Signalwegs, des Wnt Signalwegs und Gene im Zellzyklus hochreguliert im Vergleich zu wt HSCs. Nach der Stimulation des MasR mit Ang-(1 – 7) sind in wt HSCs mehr als 300 Gene hochreguliert. In fibrotischen MasR -/- M"usen ist der hepatische RhoA/Rho-Kinase Signalweg st"rker aktiviert als in wt M"usen. Ebenfalls ist der Hydroxyprolin-Gehalt in fibrotischen BDL MasR-/- M"usen erh#ht im Vergleich zu wt M"usen. Nach der CCl4-Intoxikation ist in MasR-/- M"usen die hepatische aSMA Expression und die Sirius Rot F"rbung erh#ht verglichen mit fibrotischen wt M"usen. In Patienten mit Leberzirrhose ist der MasR !berexprimiert und auf den HSCs lokalisiert. Zusammenfassung: Die Ergebnisse geben neue Einblicke in die MasR vermittelten Signalwege in HSCs. Die MasRStimulation hemmt in HSCs wichtige zellul"re Prozesse, wie z. B. ECMRemodelling, Migration, Kontraktion, Zellzyklus, die f!r die Fibroseentwicklung notwendig sind. Somit stellt die Stimulation des MasR eine therapeutische Strategie in der Leberfibrose dar. Korrespondierender Autor: Klein, Sabine E-Mail: Sabine.Klein@ukb.uni-bonn.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A1 A2 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 1.2 Three-dimensional reconstruction and quantification of key features of liver microarchitecture Othman A1, Friebel A2, Hoehme S2, Johanen T2, BegherTibbe B1, Drasdo D3, Hengstler JG1, Hammad S4 1 Leibniz Research Centre for Working Environment and Human Factors (IfADo), TU Dortmund University, Systems Toxicology, Dortmund, Germany; 2Interdisciplinary Centre for Bioinformatics (IZBI), University of Leipzig, Leipzig, Germany; 3INRIA, Unit Rocquencourt B.P.105, 78153 Le Chesnay Cedex-France, France Universit# of Paris 06, CNRS UMR 7598, Laboratoire Jacq, Paris, France; 4Faculty of Veterinary Medicine, South Valley University, Qena-Egypt, Deptartment of Forensic Medicine and Veterinary Toxicology, Qena, Egypt Liver disease is often associated with altered tissue microarchitecture. However, robust techniques for immunostaining, 3D reconstruction and quantification still represent a bottleneck. To bridge this gap, we have established protocols of antibody combinations for immunostaining, confocal imaging, three-dimensional reconstruction of 100 mm thick tissue blocks, and quantification of key architectural features in the liver. For the simultaneous visualization of bile canaliculi, sinusoidal endothelial cells and central veins as well as DNA, dipeptidyl-peptidase IV/CD26, donkey anti-mouse IgG, glutamine synthetase (GS) antibodies as well as DAPI were applied, respectively. In the second protocol -where the Sphase positive and negative nuclei (BrdU positive versus DAPI), sinusoidal endothelial cells and GS were co-stained. The protocols include three-dimensional reconstruction of the bile canalicular (BC) and sinusoidal networks from the same tissue block, robust capture of position, size and shape of individual hepatocytes as well as entire lobules from the same tissue block. Image processing and analysis were performed by freely available software-TiQuant-(www.msysbio.com/tiquant) developed in the group of Dirk Drasdo. The routinely quantified parameters in adult mice (C 57Bl6 /N) are the hepatocyte volume (5128.3 € 837.8 mm3), the fraction of the hepatocyte surface in contact with the sinusoids (22.1 € 4.8 %) and neighboring hepatocytes (67.4 € 6.7 %) as well as bile canaliculi (9.9 € 3.8 %). Furthermore, fundamental parameters can be quantified in the sinusoidal network such as the branching angle (32.5 € 11.2 %), the radius of the sinusoids (4.8 € 2.25 mm), the length of intersection branch (23.93 € 5.9 mm), the number of intersection nodes per mm3 (120.3 x 103 € 42.1 x103), the average length of sinusoidal vessel per mm3 (5.4 x 103 € 1.4 x 103 mm) and the percentage of vessel volume in tissue volume (15.3 € 3.9) (means € standard deviation). Several parameters of the BC network can be routinely extracted: the number of intersection node per mm3 (819.1 x 103 € 180.7 x103), the length of the BC network per mm3 (9.4 x 103 € 0.7 x 103 mm) and the percentage of BC volume of the total volume (3.4 € 0.005). The current protocols have several advantages: i) The quantitative parameters of hepatocytes and BC as well as sinusoidal networks can be extracted from the same tissue block; ii) Reconstructions and quantifications performed as described in the current protocols can be used for quantitative mathematical modelling of the underlying mechanisms; iii) Protocols are presented for rat, pig and human livers and iv) The technique can be applied also with conventional paraffin slices. References: Hammad S. et al. (2014) Protocols for staining of bile canalicular and sinusoidal networks of human, mouse and pig livers, three-dimensional reconstruction and quantification of tissue microarchitecture by image processing and analysis. Arch Toxicol 88:1161 – 83. Corresponding author: Hammad, Seddik E-Mail: el-kariem@ifado.de 1.3 Delta like ligand4 ameliorates liver fibrogenesis through inhibiting chemokines Weng HL1, Liu Y1, Shen Z2, Hu J3, Feng T1, Dewidar B1, Park O4, Augustin HG3, Gao B4, Li Y2, Dooley S1 1 University of Heidelberg, Department of Medicine II, Section Molecular Hepatology, Mannheim, Germany; 2 Zhejiang University, Department of Gastroenterology, Hangzhou, China; 3German Cancer Research Center, Division of Vascular Oncology and Metastasis, Heidelberg, Germany; 4National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism, Maryland, USA Introduction: Humans have five Notch ligands (Jagged1, Jagged2, Delta like ligand (Dll)1, Dll3 and Dll4) and four receptors (Notch1, 2, 3 and 4). Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York Mutation of Jagged1 or Notch2 causes Alagille syndrome, a disease characterized by defective development of intralobular bile ducts and liver injury but no overt fibrosis. However, the roles of Notch ligands in liver fibrogenesis remain largely unknown. Methods: Immunohistochemical and immunofluorescent staining were used to investigate the potential association between Notch ligands and liver fibrosis in patients with chronic HBV infection. The impact of Notch ligand on liver damage was subsequently examined in carbon tetrachloride (CCl4)-induced mouse model and in cultured mouse hepatic stellate cells (HSC), Kupffer cells (KC) and hepatocytes. Results: Only Dll4 expression was detected in myofibroblasts of cirrhotic livers with chronic HBV infection. Dll4 immunohistochemical score correlated with inflammatory grades and fibrotic stages in these patients. Administration of recombinant Dll4 protein (rDll4) remarkably ameliorated apoptosis of hepatocytes, inhibited inflammatory cell infiltration, decreased expression of cytokines and chemokines, and improved fibrosis in mice following 4 weeks of CCl4 challenge. In vitro, incubation with rDll4 did not significantly influence apoptosis of hepatocytes, collagen I production in HSCs, and lipopolysaccharide (LPS)-induced pro-fibrotic cytokines in KCs. However, rDll4 administration remarkably decreased LPS-induced chemokines (e.g. CCL2 and CCL5) in both KCs and HSCs. Conclusion: Dll4 exerts a compelling anti-inflammatory and anti-fibrotic role in CCl4induced liver fibrosis via inhibiting expression of chemokines. Upregulated expression of Dll4 might play a compensatory role in preventing liver fibrogenesis in patients with HBV infection. Corresponding author: Weng, Hong-Lei E-Mail: Honglei.Weng@medma.uni-heidelberg.de 1.4 Aldosterone stimulates the non-genomic signaling pathway of the mineralocorticoid receptor in hepatic stellate cells M!nzberg C1, Hellerbrand C2, Seufferlein T1, Gekle M3, Dollinger M1 1 University of Ulm, Internal Medicine I, Ulm, Germany; 2 University of Regensburg, Internal Medicine I, Regensburg, Germany; 3Martin-Luther University of Halle-Wittenberg, Julius-Bernstein-Institute for Physiology, Halle, Germany The number of chronic inflammatory liver diseases and secondary complications caused by their progression has risen in recent years. The renin-angiotensin-aldosterone system seems to play an important role in liver fibrosis as well as in portal hypertension. The mineralocorticoid hormone aldosterone is known to regulate blood pressure and sodium retention. Furthermore proliferative and pro-fibrotic effects of aldosterone have been described in other organ systems that have been shown to be mediated by a non-genomic signaling pathway of the mineralocorticoid receptor. Therefore we investigated whether aldosterone could have an impact in the development or progression of liver fibrosis and which cell type could mediate pro-fibrotic effects of aldosterone in the liver. To evaluate possible effects of the mineralocorticoid receptor mediating pro-fibrotic effects in the liver we stimulated different human cell lines with aldosterone. The hepatic stellate cell line hTERT-HSC as well as the hepatoma cell lines HepG2 and Hep3B were stimulated with aldosterone in concentrations between 0.1 and 100 nM. In addition HEK-293 cells were used as negative control. Already after a short time incubation of aldosterone we detected an increase in phosphorylation of ERK2 in hTERT-HSCs. ERK phosphorylation in hTERT-HSCs was dependent on concentration and incubation time of aldosterone. Neither in the hepatocellular carcinoma cell line HepG2 nor Hep3B aldosterone caused a fast activation of intracellular signaling cascades by activation of ERK1 / 2 that was also not observed in HEK-293 cells. Furthermore aldosterone stimulated c-Src phosphorylation exclusively in hTERTHSCs. These fast effects of aldosterone are mediated by a non-genomic activity of the mineralocorticoid receptor that has also been shown to be c-Src-dependent in other models of fibrosis. As hepatic stellate cells are known to be the central cell type with fibrogenic activity in the liver, pathophysiological effects of aldosterone during liver fibrosis could possibly be mediated by the non-genomic actions of the mineralocorticoid receptor in hepatic stellate cells. Corresponding author: M!nzberg, Christin E-Mail: christin.muenzberg@uni-ulm.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 1.5 All-In-One: Advanced human parenchymal and non-parenchymal liver cell preparation 1 1, 1 Lutterbeck M , Kleinehr K Driftmann S , Treckmann JW2,Math# Z2, Kaiser G2,Paul A2, Skibbe K3, Timm J3, Canbay A1, Gerken G1, Schlaak JF1, Broering R1 1 University Hospital of Duisburg-Essen, Department of Gastroenterology and Hepatology, Essen, Germany; 2 University Hospital of Duisburg-Essen, Dept. of General-, Visceral- and Transplantation Surgery, Essen, Germany; 3 University Hospital of Essen, Institute of Virology, Essen, Germany Introduction: Human liver cells are key players in liver health and disease. Liver cell preparations allow the investigation of diverse issues regarding liver physiology and pathophysiology. In particular, the quantity and quality of isolated cells are critical factors to study their function. Also, the usage of primary cells obtained from the same donor is important for comparative studies when using human cells. Aim of the study was the isolation of high quantity and quality primary human hepatocytes (PHH), Kupffer cells (KC), liver sinusoidal endothelial cells (LSEC) and hepatic stellate cells (HSC) from a single human liver specimen. Methods: A two-step perfusion technique combined with lowspeed centrifugation, density gradient centrifugation, magnetic-activated cell sorting and selective adherence was used to separate and purify PHH, KC, LSEC and HSC. To determine cell yields, viable cells were counted using trypan blue staining (n= 10). Cells were seeded and cultured for different time periods. The cultured cell populations were initially assessed by their morphology. Identity of cell populations was evaluated by immunofluorescence staining of cell-type specific markers (n= 5). Total cells (DAPI-stained) and marker-positive cells were counted to quantify the purity of the diverse cell populations. RNA was extracted and the expression of discriminative cell markers was determined by quantitative RT-PCR (n= 10). In addition, cell type-related functionality assays were performed to analyze the functional activity of cultured cells (n = 3). Results: The weight of liver specimens varied between 25 g and 100 g and consistent cell yields of about 4.2 € 0.9 x 108 PHH (mean € SEM), 4.2 € 0.7 x 107 KC (mean € SEM), 7.5 € 1.6 x 106 LSEC (mean € SEM) and 1.1 € 0.6 x 107 HSC (mean € SEM) were obtained. The following qualities were demonstrated: 96.1 € 1.4 % (mean € SEM) albumin-positive PHHs, 94.4 € 2.0 % (mean € SEM) CD 68-positive KC, 98.1 € 0.3 % (mean € SEM) CD 146-positive LSEC and 96.6 € 0.9% (mean € SEM) a-SMA-positive HSC, respectively. Moreover, PHHs were identified by the expression of the apolipoprotein B (APOB) and asialoglycoprotein receptor 1 (ASGPR1) and showed a strong cytochrome P450 enzyme activity. KC expressed the markers CD163 and CD14 and retained their phagocytic activity, shown by the uptake of 1 mm latex beads. LSEC expressed the markers CD31 and von Willebrand factor (VWF) and retained their endocytic activity, demonstrated by the uptake of acetylated low-density lipoprotein. HSC expressed vinculin (VCL) and desmin (DES) and showed vitamin A-mediated autofluorescence. Conclusion: We developed an all-in-one isolation procedure for primary liver cells, resulting in high yields and quality of primary cells with retained physiological functionality in vitro, which makes this system a powerful tool for investigations regarding liver function and disease. Corresponding author: Lutterbeck, Melanie E-Mail: melanie.lutterbeck@uni-due.de 1.6 An in vitro system for the identification of DILI related signaling? Wewering F1, Luch A1, Zellmer S1 1 German Federal Institute for Risk Assessment (BfR), Department of Chemicals and Product Safety, Berlin, Germany Chemicals present in consumer products or drugs might pose a potential hazard to humans. The conversion of these chemicals into reactive intermediates by cellular metabolism may lead to the production of reactive oxygen species (ROS) and the formation of DNA or protein adducts. At low, non-toxic doses, Drug-Induced Liver Injury (DILI) can occur in rare incidence. It involves the immune system and often results in the withdrawal of drugs from the market once it becomes apparent. Here we investigated the toxic effects of the DILI-inducing drug, ketoconazole, on hepatocytes in vitro. Ketoconazole, a drug used to treat fungal infections, is metabolized by CYP1A1. In July 2013 the European Medicines Agency recommended suspension of marketing authorization for oral ketoconazole as it can induce DILI by as yet unknown mechanisms. Two hepatoma cell lines (HepG2 and Huh-7) and murine primary cells were cultivated and incubated with different concentrations of ketoconazole for 24 h. Viability was quantified using the MTT and LDH assay while ROS were measured by 2’,7’-dichlorodihydrofluorescein diacetate (H2DCFDA). Expression and concentration of IL-8, an important chemokine, were measured by qPCR and ELISA. In human hepatoma cell lines as well as in primary cells ketoconazole induced a concentration-dependent generation of ROS (EC50 of 42 – 53 mM), which is an important prerequsite for DILI induction. The CYP1A1 expression was increased under treatment conditions, thus indicating an activated metabolism of ketoconazole. Although no increase of IL-8 mRNA expression was detected, the concentration of IL8 was found well elevated in the supernatant though. Here we could show that ketoconazole induces ROS formation, CYP1A1 induction and IL-8 release in human hepatoma cell lines in vitro. In future experiments the expression levels of additional cytokines like TNF-a or IL-1 will be quantified in order to elucidate the underlying signaling pathways. Corresponding author: Wewering, Franziska E-Mail: franziska.wewering@bfr.bund.de 1.7 Cholestasis and bile acids induce expression of the oncofetal marker Nope in adult murine hepatocytes independent of Fxr Bowe A1, Hoffmann V1, Morton CH2, Fickert P3, Nierhoff D1 1 University Hospital of Cologne, Department of Gastroenterology and Hepatology, Cologne, Germany; 2 University of Cologne, Institute for Genetics, Centre for Molecular Medicine, Cologne, Germany; 3Medical University of Graz, Department of Internal Medicine, Unit for Experimental and Molecular Hepatology, Division of Gastroenterology and Hepatology, Graz, Austria; 4Medical University of Graz, Institute of Pathology, Graz, Austria Background: Neighbor of Punc E11 (Nope) is strongly expressed in hepatic stem/progenitor cells and in hepatocellular carcinoma but not in terminally differentiated hepatocytes. We here investigated the expression pattern of Nope in adult mice after biliary liver injury. Methods: Liver tissue was extracted from adult C 57Bl/ 6 mice and Fxr-/- mice 24 hours up to 4 weeks after bile duct ligation (BDL) or after a 1 week diet containing cholic (0.5 %) or ursodeoxycholic acid (0.5%). Liver tissue was tested for expression levels of Nope via quantitative RT-PCR. Costainings were performed for Nope in combination with CK19 (biliary), E-cadherin (epithelial) or the canalicular marker dipeptidylpeptidase (DPP) IV. Results: Bile duct ligation leads to a significantly increasing expression level of Nope (after 1 week 87-fold vs. adult liver, p = 0.00016). Costainings with E-cadherin and DPPIV demonstrate a sinusoidal expression pattern of Nope on hepatocytes, but no expression on CK19-positive cholangiocytes (after 4 weeks 676-fold vs. adult liver). At later stages after BDL, almost all of the hepatocytes stain positive for Nope. In Fxr-/mice, Nope is expressed without additional biliary injury (28-fold vs. adult liver, p < 0.0007) and shows a further and significant increase after BDL (440- vs. 28-fold, p = 0.03). A diet with cholic (26-fold vs. adult liver, p = 0.002) or ursodeoxycholic acid (8-fold vs. adult liver, p = 0.004) also leads to a significant expression of Nope with a membranous staining pattern on hepatocytes. A diet with hydrophobic acids results in a significantly higher expression of Nope (p = 0.04). Conclusion: We here report the bile acid-induced expression of the oncofetal marker Nope on adult hepatocytes probably indicating their dedifferentiation. The induction of Nope is not mediated through Fxr but a lack of the receptor leads to a higher expression level probably due to limited compensatory mechanisms of bile acid homeostasis in hepatocytes. Corresponding author: Bowe, Andrea E-Mail: andrea.bowe@uk-koeln.de 1.8 Comparative analysis of C 5aR and C 5L2 receptor deficiency in liver and kidney fibrosis Martin IV2, Boor P2, Ostendorf T2, Floege J2, Lammert F1, Weber SN1 1 Saarland University Hospital, Department of Medicine II, Homburg, Germany; 2RWTH Aachen, Department of Medicine II, Aachen, Germany Background: Complement factor C 5a has two known receptors, C 5aR and C 5L2. C 5aR is involved in transduction of the proinflammatory effects of C 5a, whereas C 5L2 has been suggested as a decoy receptor. We previously demonstrated a pro-fibrotic role of C 5a and C 5aR in kidney and liver, but nothing is known concerning the potential involve- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A3 A4 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen ment of C 5L2 in organ fibrosis. Methods: C 5aR-/-, C 5L2-/- and wildtype (WT) control mice were challenged with CCl4 for 6 weeks to induce liver fibrosis or subjected to 5 days of unilateral ureteral obstruction (UUO), a model of renal fibrosis. Extracellular matrix (ECM) deposition, the inflammatory status and injury markers were analyzed by gene expression analyses and immunohistochemistry. Results: Following induction of liver fibrosis, collagen contents were significantly lower in C 5aR-/- but unchanged in C 5L2-/- mice. Transcript analyses of cytokines in the chronic fibrosis model (TGFb-1, TNFa, IL6, IL12, IL23, IL27) showed a prominent reduction in both receptor-deficient lines vs. WT mice. Twenty-four hours after an acute single CCl4 challenge, these cytokines were highly induced specifically in C 5L2-/- mice as compared to WT and C 5aR-/- mice. During progression of kidney fibrosis both C 5a receptors were overexpressed. Compared to WT mice, C 5aR deficiency led to a significant reduction of renal collagen I and IV, a-smooth muscle actin and vimentin expression; C 5L2 deficiency in renal fibrosis resulted in only mild reduction of ECM, whereas MCP-1, RANTES, TNFa and IL-6 expression increased. Transcripts of TGFb-1 and KIM-1, a tubular injury marker, were markedly reduced in both C 5aR-/- and C 5L2-/- mice vs. WT controls. Conclusions: Our findings taken together demonstrate that C 5aR is involved in chronic fibrogenesis in both liver and, although less potently, also in the kidney. In the liver, C 5L2 provides protection from early inflammatory insults, and in kidney fibrosis C 5L2 might also play a weak anti-inflammatory role, indicating organ-specific regulatory effects of C5 during fibrogenesis. Corresponding author: Lammert, Frank E-Mail: frank.lammert@uks.eu 1.9 Damage and recovery of hepatic tissue of Mus musculus inhabited at metallurgical workshop Abbasi MH1, Sheikh N2, Sharif Z1, Kanwal S1, Khawar B2 1 Govt. College of Science, Wahdat Road, Department of Zoology, Lahore, Pakistan; 2University of the Punjab, Department of Zoology, Cell and Molecular Biology Lab, Lahore, Pakistan Increased industrial application of metals and rapid urbanization resulted in contamination of terrestrial environment. Heavy metals from industrial waste, vehicular emissions, incinerators, the atmospheric deposition of dust and aerosols and other activities are continuously adding to the pool of contaminants in the environment. The present study was therefore, conducted to investigate the hepatic damage with noninjured liver due to occupational exposure of metals in the metallurgical workplace. The male albino mice (Mus musculus) were exposed in metallurgical workshop (Lahore-Pakistan) and grouped into three; E (exposed for consecutive 30 days), R (exposed to normal conditions for 10 uninterrupted days after 30 days of exposure) and control (Co) is without treatment (n= 5). Livers were excised after dissection and processed by standard methods and stained for Hematoxylin and Eosin (H & E) and Masson trichrome using the protocol provided by the manufacturer to study the extent of damage. Group E, showed signs of necrosis and congestion of central vein. Dilated sinusoidal spaces were also distinctly visible along with hepatic mitotic figures. Group R, showed abnormal nuclei near portal triad with some degree of fibrosis observed by Masson’s trichrome staining. In conclusion, extensive human exposure to such conditions may result in oxidative stress that may lead to sever histological changes with disturbed physiological function. Corresponding author: Sheikh, Nadeem E-Mail: s_nadeem77@yahoo.com 1.10 Damage of the non parenchymal cells after acetaminophen intoxication is critical for liver regeneration Ghallab A1, Hassan R1, Reif R1, Hengstler JG1 1 Leibniz Research Centre for Working Environment and Human Factors (IFADo), Systems Toxicology, Dortmund, Germany; 2Faculty of Veterinary Medicine, South Valley University, Forensic Medicine and Toxicology, Qena, Egypt Acetaminophen (APAP)is a safe antipyretic and pain relieving drug when used at normal therapeutic doses. However, overdoses of APAP are commonly associated with acute liver damage. Due to the vital functions of the liver, a rapid well-orchestrated regeneration is essential after injury, in contrast to the quiescent state of healthy liver. The aim of this study is to investigate the influence of APAP intoxication on various hepatic cells in mice and the impact of each individual cell type on liver regeneration. Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York For this purpose male C 57B6/n mice received a single low (200 mg/kg) or high (450 mg/kg) dose of APAP. Blood as well as liver tissue samples were collected in a time resolved manner after APAP injection. Histopathological analysis revealed pericentral liver damage after intoxication with 200 mg/kg. In addition to the centrilobular damage, a wide spread haemorrhage was observed after injection of 450 mg/kg. Moreover, in contrast to the complete regeneration of the dead cell area by day four after intoxication with 200 mg/kg, delayed liver regeneration was observed following intoxication with high doses of acetaminophen. Alpha-smooth muscle actin staining, a marker of activate stellate cells, showed a strong positive signal started as early as day one after injection of 200 mg/kg. In contrast, a very weak and delayed signal of alphasmooth muscle actin, started after day three, was observed following injection of high doses of APAP. Moreover, the sinusoidal endothelial cells were highly compromised after injection of high doses of APAP as assessed by CD31 staining. In order to prove the critical role of the non parenchymal cells in liver regeneration, a defined region of the liver lobule was burned by laser using two-photon microscope. The laser was adjusted to target only hepatocytes or hepatocytes plus the non parenchymal cells in this region. Killing of only hepatocytes resulted in full recovery within six days. In contrast, after damage of the non parenchymal cells collagen deposition was observed in the dead cell area. In summary, the results revealed that loss of hepatocytes is not critical for liver regeneration. In contrast, damage of the non parenchymal cells might leads to the switch from regenerative to fibrotic signal. Corresponding author: Ghallab, Ahmed E-Mail: Ghallab@ifado.de Die Aktivit!t von cSRC bei der Leberfibrose 1.11 G"rtzen J1, Klein S1,Schierwagen R1, Uschner FE1, Strassburg CP1, Laleman W2, Trebicka J1 1 University of Bonn, Medical Clinic and Polyclinic I, Bonn, Germany; 2University Hospital Gasthuisberg, Department of Hepatology, Leuven, Belgium Einleitung: Die aktivierten hepatischen Sternzellen (HSC) f!hren !ber den RhoA/ROCK-Signalweg zur Fibrosierung der Leber. Neben ROCK-vermittelten Kontraktion und Fibrogenese, reguliert Rho-GTPase !ber mDia1 die Zellmigration und Zytoskelettbildung. Außerdem interagiert Rho-GTPase !ber mDia1 mit cSRC, einer transmembran#sen Tyrosinkinase und Regulator von fokalen Adh"sionen. W"hrend RhoA/ROCK bei der Leberfibrose hochreguliert sind, ist die Rolle von cSRC und mDia bei der Leberfibrose nicht hinreichend bekannt. In dieser Arbeit wurden die Aktivit"t und Expression von cSRC bei der Leberfibrose untersucht. Methoden: In Ratten wurde entweder durch Gallengangsligatur (BDL), Thioacetamid-Intoxikation (TAA) oder CCl4-Inhalation eine Leberfibrose induziert. Außerdem wurden bei Lebertransplantationen oder Leberresektionen humane Proben aus fibrotischen oder zirrhotischen Lebern gewonnen. Die Proben wurden mittels qRT-PCR und Western Blot untersucht und die Ergebnisse mit der jeweiligen Sham-Gruppe verglichen. Hierbei kamen Site- und Phospho-spezifische Antik#rper gegen aktiviertes p-418-cSRC (phosphoryliert an Tyr-418) und inaktiviertes p-530-cSRC (phosphoryliert an Tyr-530) zum Einsatz. Ergebnisse: Bei der Leberfibrose zeigten fibrotische Leberhomogenate deutlich h#here RhoA und ROCK Expression (p < 0.01). Allerdings lag eine signifikante Ver"nderung der Gesamtexpression von cSRC nicht vor. Interessanterweise wurde bei der Leberfibrose signifikant mehr inaktiviertes p-530-cSRC exprimiert (p < 0.05) und es lag deutlich weniger aktiviertes p-418-cSRC vor (p < 0.05). In fibrotischen Lebern wurde außerdem signifikant weniger mDia1 exprimiert (p < 0.05). Das Ergebnis war unabh"ngig von der Art der induzierten Leberzirrhose. Diese Ergebnisse best"tigten sich auch in den humanen Leberproben. Diskussion: Hiermit konnten wir erstmals einen Zusammenhang zwischen der Leberfibrose und der Aktivierung von cSRC/mDia zeigen. Vermutlich f!hrt die Aktivierung von RhoA/ROCK in aktivierten HSC zur Deaktivierung von cSRC/ mDia. Die weitere Erforschung dieses Stoffwechselweges kann in Zukunft einen m#glichen therapeutischen Ansatz darstellen. Korrespondierender Autor: G#rtzen, Jan E-Mail: jan.goertzen@ukb.uni-bonn.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 1.12 Die Hemmung der Glyoxalase-I durch Ethylpyruvat vermindert die LPS-induzierte Aktivierung von hepatischen Sternzellen Hollenbach M1, Thonig A1, Pohl S1, Ripoll C1, Zipprich A1 1 University Hospital of Halle (Saale), University Clinic and Polyclinic, Internal Medicine I, Halle (Saale), Germany Einleitung: Hohe Konzentrationen von Methylglyoxal (MGO) wirken !ber die Bildung von Sauerstoffradikalen sowie die Freisetzung proinflammatorischer Zytokine zytotoxisch. MGO wird durch die Glyoxalase-I (Glo-I) enzymatisch detoxifiziert. Ethylpyruvat (EP) ist ein Inhibitor der Glo-I und zeigt antiinflammatorische Effekte auch !ber eine verminderte Aktivit"t von NF-kB. Eigene Vorarbeiten zeigten eine reduzierte Expression der Glo-I in der Zirrhose. Ein wesentlicher Mechanismus in der Zirrhosentstehung ist die Aktivierung der Sternzellen (HSC) durch Radikale bzw. Inflammation. Ziel der Arbeit war die Untersuchung des Glo-I-Inhibitors EP auf die LPS-induzierte Aktivierung von HSC. Methode: In der HSC HSZ-B-S1 Zelllinie erfolgte mittels Enzymkinetikmessung, RT-PCR und Western-Blot die Bestimmung der Aktivit"t und der Expression der Glo-I. Nach Behandlung der Zellinie mit LPS !ber 24 Stunden wurde die Freisetzung sowohl von TNF-alpha als auch Kollagen-I und Alpha-SMA via ELISA gemessen. Weiterhin erfolgte die Bestimmung von NF-kB, nrf2, ERK 1/ 2 und phospho ERK 1/ 2 in den stimulierten HSC. Ergebnisse: EP zeigte in den HSC eine konzentrationsabh"ngige Hemmung der Glo-I. Die Behandlung der HSC mit LPS f!hrte zu einer Zunahme der Expression von TNF-alpha, Kollagen-I und AlphaSMA, welche in ihrer Expression durch steigende Konzentrationen von EP gehemmt werden konnte. Die Behandlung mit EP f!hrte zu einer konzentrationsabh"ngigen Reduktion der LPS-induzierten Expression von NF-kB und Zunahme von nrf2. Weiterhin konnte eine konzentrationsabh"ngige Reduktion von phospho-ERK 1/ 2 bei gleichbleibender Expression von ERK 1 /2 gezeigt werden. Schlussfolgerung: Ethylpyruvat vermindert durch Hemmung der Glo-I-Aktivit"t die LPS-induzierte Aktivierung von hepatischen Sternzellen. Ethylpyruvat reduziert in diesem Zusammenhang die NF-kB und die phospho MAPK Expression bzw. erh#ht die Expression von nrf2 und k#nnte daher ein neuer Therapieansatz in der Aktivierung von Sternzellen bei Entstehung einer Zirrhose sein. Korrespondierender Autor: Hollenbach, Marcus E-Mail: marcus.hollenbach@medizin.uni-halle.de 1.13 Die Interaktion zwischen beta-Arrestin-2 und der AT1-Rezeptor abh!ngigen Signalkaskade in der Leberfibrose Schierwagen R1, Heinzen J1, Granzow M1, Br$gelmann C1, Klein S1, Uschner FE1, Hiththetiya K2, Strassburg CP1, Sauerbruch T1, Trebicka J1 1 University of Bonn, Medical Clinic and Polyclinic I, Bonn, Germany; 2University of Bonn, Institute of Pathology, Bonn, Germany Hintergrund: Der AT1-Rezeptor (AT1R) spielt !ber G-Protein gekoppelte Signalkaskaden eine entscheidende Rolle bei der Leberfibrogenese. BetaArrestin-2 (bArr2) kann an den AT1R binden und verhindert dadurch die Bindung anderer Proteine an den Rezeptor. bArr2 hemmt dadurch die Aktivierung der G-Protein gekoppelten Signalkaskade !ber JAK2 /Rho-kinase und ist somit ein negativer Regulator des AT1R. bArr2 aktiviert jedoch auch ERK1/ 2 !ber Ras/Raf1. In dieser Arbeit wurden die Effekte der bArr2 vermittelten Signalkaskade in der Leberfibrose untersucht. Methoden: Proben von Patienten mit Leberzirrhose wurden mit Proben von Patienten ohne Leberzirrhose verglichen. Bei bArr2-, AT1R-, und Wildtyp (WT) M"usen wurde durch CCl4 Intoxikation (f!r 28 Tage) oder Gallengangsligatur (BDL, 14 Tage) eine Leberfibrose induziert. Mittels osmotischer Mini-Pumpen wurde der AT1R f!r 14 Tage durch die kontinuierliche Gabe von Angiotensin II (AngII) stimuliert. Eine Hemmung der JAK2 Aktivit"t wurde durch subkutane Injektionen von AG490 in den letzten 7 Tagen der AngII-Gabe erreicht. Der hepatische Hydroxyprolingehalt, mRNA-Spiegel (mittels Taqman-PCR) und die Proteinexpression und -phosphorylierung (mittels Western blot) wurden in Leberproben dieser Tiere untersucht. Leberfibrose (aSMA und SiriusRot) und die hepatische Inflammation (F4 / 80 und Ki67) wurden zudem immunhistochemisch untersucht. Ergebnisse: Die Spiegel von bArr2 und wichtigen Proteinen der nachgeschalteten Signalkaskade waren in der humanen und experimentellen Fibrose !berexprimiert. Nach AT1R Stimulation (mittels AngII) zeigte sich eine st"rkere Transkription dieser Komponenten bei den bArr2-/- M"usen. Dabei wurde JAK2 vermehrt aktiviert, jedoch nicht die Ras/Erk Signalkaskade. Nach Fibroseinduktion (BDL, CCl4) konnte in bArr2-/- M"usen weniger Fibrose als in WT M"usen festgestellt werden, was auf AT1R unabh"ngige Effekte schließen l"sst. Wichtige Komponenten des Renin-Angiotensin-Systems (RAS; Renin, Angiotensinogen, ACE, ACE2, AT1-Rezeptor) und profibrotische Marker waren in bArr2-/- M"usen im Vergleich zu WT M"usen signifikant herunterreguliert. Zusammenfassung: bArr2 scheint bei der Entstehung der experimentellen und humanen Leberfibrose eine wichtige Rolle zu spielen. Die zu Grunde liegenden Mechanismen sind noch nicht vollst"ndig aufgekl"rt. Die verringerte Aktivit"t des RAS oder aber die ver"nderte Signalweiterleitung unterhalb des AT1R k#nnten daf!r verantwortlich sein. Aus diesen Daten konnte auf einen AT1R abh"ngigen und einen AT1R unabh"ngigen Effekt von bArr2 f!r die Leberfibrose geschlossen werden. Korrespondierender Autor: Schierwagen, Robert E-Mail: robert.schierwagen@ukb.uni-bonn.de 1.14 Effekte der akuten Gabe von Udenafil auf den Pfortaderdruck bei Ratten mit Leberzirrhose Uschner FE1, Klein S1, Schierwagen R1, Tewes B3,Strassburg CP1, Kreisel W2, Sauerbruch T1, Trebicka J1 1 University Hospital of Bonn, Medical Clinic I, Bonn, Germany; 2University Hospital of Freiburg, Medical Clinic II, Freiburg, Germany; 3Dr. Falk Pharma GmbH, Freiburg, Germany Einleitung: Hepatische Vasokonstriktion und Leberfibrose f!hren zu einem Anstieg des intrahepatischen Widerstandes und damit zur portalen Hypertension. In Ratten nach Gallengangsligatur (BDL) konnte der oral verf!gbare PDE – 5 – Hemmer Udenafil die Entstehung einer Fibrose verringern. Der akute Effekt von Udenafil bei Zirrhose wurde nicht betrachtet. Wir untersuchten die Effekte der akuten Gabe von Udenafil auf den intrahepatischen Widerstand und den Pfortaderdruck, sowie seine systemische Wirkung, an zwei Tiermodellen. Methoden: Zirrhose wurde in Ratten mittels BDL oder CCl4 – Intoxikation induziert. Die Experimente wurden durchgef!hrt, wenn Aszites, als sicheres Zeichen einer portalen Hypertension, vorhanden war (5 – 6 Wochen BDL und 14 – 16 Wochen CCl4). Sowohl Portaldruck, als auch Mittelarterieller Druck wurden in vivo invasiv kontinuierlich vor und nach Udenafil- Applikation in unterschiedlichen Dosen (1 mg/kg, 5 mg/kg KG) gemessen. Als Vergleich diente eine Placebogruppe. Portale und systemische H"modynamik wurden mittels kolorierter Mikrosph"rentechnik ermittelt. Die isolierte, kontinuierliche in situ Leberperfusion wurde angewendet, um die Relaxation des Lebergef"ßbettes in zirrhotischen Ratten zu untersuchen. Dabei erfolgte nach initialer Vorkontraktion mit Methoxamin (200 mM) die Inkubation des Perfusates mit ansteigenden Udenafildosen (0,1 mg/ ml, 0,5 mg/ml, 1 mg/ml Perfusat). Ergebnisse: Udenafil senkte den intahepatischen Widerstand und in der Folge den Pfortaderdruck in beiden Zirrhosemodellen im Vergleich zu den Placebo behandelten Tieren signifikant. Vor allem in h#heren Dosen zeigte Udenafil eine systemische Komponente. Die niedrigste Dosis zeigte den gr#ßten Portaldruck – senkenden Effekt ohne den systemischen Druck zu beeinflussen. Wie zu erwarten war, reduzierte Udenafil dosisabh"ngig den Perfusionsdruck in der in situ Leberperfusion. Diskussion: Udenafil konnte den Portaldruck signifikant senken. Die h#here Dosis zeigte keinen Vorteil, f!hrte aber zu systemischen Nebeneffekten, welche durch die Vasodilatation des splanchnischen Systems erkl"rt werden k#nnen. In einer moderaten Dosis k#nnte Udenafil ein geeignetes Therapeutikum in der Behandlung der portalen Hypertension darstellen. Korrespondierender Autor: Uschner, Frank Erhard E-Mail: frank.uschner@ukb.uni-bonn.de 1.15 Einfluss von Arginin auf die Entstehung einer Western Style Di!t-induzierten nicht alkoholbedingten Fettlebererkrankung (NAFLD): Untersuchungen im Mausmodell Degen C1, Sellmann C1, Jin C1, Engstler J1, De Bandt JP2, Bergheim I1 1 Friedrich-Schiller-Universit$t Jena, LB Modellsysteme molekularer Ern$hrungsforschung, Jena, Deutschland; 2 Universit# Paris Descartes, Laboratoire de Biologie de la Nutrition, Facult# de Pharmacie, Paris, France Die Pr"valenz der nicht-alkoholbedingten Fettlebererkrankung (NAFLD) hat weltweit in den letzten Jahrzehnten stark zugenommen. Neben einer generellen &berern"hrung, aber auch einer fett- und zuckerreichen Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A5 A6 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen Ern"hrung, werden genetische Faktoren und Ver"nderungen der Darmbarrierefunktion zu den Risikofaktoren gez"hlt. Ver"nderungen im Arginin/Citrullin-Stoffwechsel sind anhand von tierexperimentellen Studien aber auch Humanstudien deutlich erkennbar. Ziel der vorliegenden Studie war es den Effekt einer oralen Supplementation von Arginin (2,49 g/kg KG) auf die Entstehung einer Western Style Di"t (WSD)-induzierten NAFLD im Mausmodell zu untersuchen. C 57BL/ 6 J-M"use erhielten 6 Wochen lang entweder eine modifizierte Standard-Fl!ssigdi"t (= Kontrolle) oder eine mit Fruktose, Fett und Cholesterin angereicherte Fl!ssigdi"t (= WSD) € 2,49 g/kg KG Arginin pro Tag, paargef!ttert. K#rper- und Lebergewicht, Parameter der Lebersch"digung, Fetts"urenverteilung der Lebergesamtlipide sowie Marker der Darmbarriere wurden bestimmt. Die F!tterung der WSD f!hrte nach 6 Wochen zur Entstehung einer Lebersteatose mit beginnenden entz!ndlichen Ver"nderungen. Dieser Effekt der WSD auf die Leber war bei den mit Arginin behandelten Tieren vermindert. Der protektive Effekt der oralen Suppelementation von Arginin auf die Leber war mit einer Ver"nderung der prozentualen Fetts"urenverteilung, sowie einer deutlich geringeren Tumornekrosefaktor-alpha-Konzentration und der verminderten Anzahl an neutrophilen Granulozyten assoziiert. Auch die Darmbarriere der M"use, gemessen an der Ver"nderung des Tight-Junction-Proteins Occludin, blieb bei den Kontrolltieren sowie unter Gabe von Arginin verglichen zu ausschließlich mit WSD gef!tterten Tieren unvermindert. Insgesamt weisen die bisherigen Ergebnisse darauf hin, dass die orale Supplementation von Arginin einen pr"ventiven, verlangsamenden Einfluss auf die Entstehung der WSD-induzierten NAFLD im Mausmodell hat. (Gef#rdert durch die DFG: BE 2376 / 6 – 1) Korrespondierender Autor: Degen, Christian E-Mail: b0dech@uni-jena.de 1.16 Endoglin Knockdown inhibits Proliferation and NO Production in murine Sinusoidal Endothelial Cells in vitro Sterzer V1, Al-Samman M1, Trautwein C1, Scholten D1 1 University Hospital Aachen, Department of Medicine III, Aachen, Germany Introduction: Endoglin (ENG) is a 180 kDA homodimeric membrane protein which acts as an auxiliary TGF-b Receptor modulating TGF-b downstream signalling. It plays an important role in various cellular processes like proliferation and differentiation. ENG is also involved in VEGF/eNOS signalling and nitric oxide (NO) production thereby finetuning angiogenetic processes. However, the interplay between ENG, eNOS and VEGF has still not been clarified and is an object of current research. Aim: Here we investigate the influence of ENG on NO production and VEGF-induced proliferation in primary murine liver sinusoidal endothelial cells (LSECs). Methods: Endothelial cells were isolated from C 57BL/ 6 mice and purified by a magnetic separation with CD146 MACS beads. The purified cells were allowed get adherent overnight on 6-well plates. Thereafter cells were transfected with an anti-ENG or non-target siRNA (5 nmol/well with 5 ml lipofectamine) for 48 h followed by stimulation with recombinant murine VEGF (5 ng/ml) or the eNOS activator calcium ionophore A32187 (Ca-I, 1 mM) for 48 hours. Supernatant aliquots were taken every 24 h for determination of NO production. A scratch was made with a sterile 1000 ml pipette tip in each well after the cell were adherent and the cell proliferation was monitored by photographic measurement every 24 h after stimulation. The NO production was determined by measuring the nitrite and nitrate concentration of the supernatant (Griess Test). At the end of the stimulation step cell lysates were used for western blot analysis of ENG-, VEGF-, eNOSand b-actin expression. Results: We observed an ENG knockdown efficiency of > 70%. Furthermore the ENG knockdown samples showed a 29 % ( € 7%) and 52 % ( € 12%), p < 0.05, decrease in NO production in VEGF and Ca-I stimulated samples respectively compared to the ENG wt controls. The proliferation of ENG deficient LSECs decreased by 28% ( € 9%) in the photographically analyzed scratch assays compared to wt controls. Western blots revealed a 34 % ( € 8 %) decrease in eNOS expression in ENG deficient LSECs compared to wt cells. Conclusion: This study shows the interaction between ENG and the VEGF-eNOS pathway and its influence on LSEC proliferation. The results bring new insights into the role of endoglin in LSEC pathophysiology and liver perfusion. Corresponding author: Scholten, David E-Mail: dscholten@ukaachen.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York 1.17 Evaluation of the effect of genetic variation in the natural killer cell receptor on liver stiffness and survival in patients with chronic liver disease Gr!nhage F1, Krawczyk M1, Lammert F1 1 Saarland University Hospital, Medical Department II, Homburg, Germany Introduction: Recently the natural killer cell receptor G2D (NKG2D) has been shown to be involved in NK-cell induced apoptosis of hepatic stellate cells in chronic hepatitis C virus (HCV) infection. Given the critical role of stellate cells in the development of liver fibrosis we speculate that functional polymorphisms in this gene influence fibrosis progression or even survival of patients with advanced cirrhosis. Thus we studied the influence of a common NKG2D polymorphism that has also been associated to cholangiocarcinoma on liver stiffness and survival in two different cohorts of patients with liver disease Patients & Methods: Two different cohorts of patients with chronic liver disease were recruited. The first group of patients all received VCTE and/or a liver biopsy for the assessment of liver stiffness or fibrosis stage (according to Desmet-Scheuer), respectively. Patients were subdivided in different TE classes (55 %: < 7.5 kPa; 23%: 7.5 – 13 kPa; 22 %: > 13 kPa, indicating presence of cirrhosis). All patients were genotyped for the single nucleotide polymorphism rs2617167. Association testing was performed using Chi-square statistics for allelic discrimination and Armitage’s trend test for associations with genotypes.. The second group of patients consistet of patiens with advance liver cirrhosis that were followed up for survival. To test the effect of rs2617167 on survival log rank statistics and Kaplan-Meier curve were applied. Results: A total of 691 patients with chronic liver disease and Caucasian descent were included for the effect on liver stiffness. Survival was tested in 92 indepent patients with advanced cirrhosis that were followed up for survival. In both groups the majority of patients were men (60 % and 66 % respectively). While in the liver stiffness cohort most patients suffered from HCV infection (N= 433, 63 %) in the survival group the majority of patients suffered from alcoholic liver disease (60 %). Liver stiffness did neither correlate with alleles nor with genotypes (P > 0.05). To exclude that the SNP is relevant in early but not in late-stage liver disease progression, we also tested whether rs2617167 was associated with liver stiffness within classes but no association with stiffness was detected. Liver histology was not associated with liver fibrosis stage either. Albeit the relevance of NKG2D has been shown for HCV infected patients, this subgroup of HCV patients did not show an association. Moreover we could not detect any effect on any genotype of rs2617167 on survival. (P > 0.05) Conclusions: Despite theoretical evidence for the an important role of rs2617167 on liver fibrosis development this study in patients phenotyped with liver stiffness and followed up for survival did not indicate that common genetic variation in the NKG2D gene has an impact on the progression of chronic HCV infection and mortatility. Corresponding author: Gr!nhage, Frank E-Mail: frank.gruenhage@uks.eu 1.18 Fibroblast growth factor 7 inhibits hepatic steatosis, inflammation and fibrosis in murine models of on non-alcoholic steatohepatitis Czech B1, Valletta D1, Amann T1, Bosserhoff A2, Hellerbrand C1 1 University Hospital Regensburg, Internal Medicine I, Regensburg, Germany; 2University Regensburg, Institute of Pathology, Regensburg, Germany The activation of hepatic stellate cells (HSCs) is the key event of hepatic fibrosis, and we have previously shown that fibroblast growth factor 7 (FGF7) expression is de novo expressed during HSC-activation while its highly specific receptor FGFR2IIIb is exclusively expressed on hepatocytes in the liver. The aim of this study was characterize the function of FGF7 in chronic liver disease with a focus on non-alcoholic steatohepatitis (NASH). Methods and Results: FGF7-deficient (FGF7-ko) and wildtype (wt) control mice were subjected to two different NASH-models, namely feeding a (i) methionine-choline deficient diet (MCD) or (ii) high-fat diet (HFD). In both models FGF7-deficient mice exhibited significantly elevated hepatic steatosis. Furthermore, FGF7-deficient mice showed higher serum transaminases, histological inflammation and hepatic TNF and IL-1 expression compared to wt-mice. Further, FGF7-ko showed advanced HSC activation, profibrogenic gene expression (Collagen I and TGF-beta) and fibrosis. In contrast, application of recombinant FGF7 to wildtype mice ameliorated enhanced stetaosis as well as inflammation and fibrosis in the MCD-model. Summary and conclu- 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen sion: Recombinant FGF7 therapy is already approved in the US and Europe for decreasing the incidence and duration of oral mucositis, and has been shown to be safe. Furthermore, we have previously shown that FGFR2IIIb, which is the exclusive receptor for FGF7, acts as a tumorsuppressor in hepatocellular carcinoma. Thus, FGF7 appears as promising novel anti-fibrogenic drug for the treatment of hepatic fibrosis in patients with chronic liver disease especially NASH. Corresponding author: Hellerbrand, Claus E-Mail: claus.hellerbrand@ukr.de 1.19 Functional effects of monocarboxylate transporter 1 expression in activated hepatic stellate cells Czech B1, Valletta D1, Thasler W2, M!ller M1, Bosserhoff A3, Hellerbrand C1 1 University Hospital Regensburg, Internal Medicine I, Regensburg, Germany; 2Ludwig-Maximilians-University Munich, Großhadern Tissue Bank and Center for Liver Cell Research, Department of Surgery, Munich, Germany; 3 University Regensburg, Institute of Pathology, Regensburg, Germany Monocarboxylate transporter 1 (MCT1) belongs to the SLC16 transporter gene family. MCT1 is involved in the transmembrane transport of lactic acid and other monocarboxylic acids in healthy tissue. Furthermore, it has been recognized that MCT1 contributes to the maintenance of the metabolic phenotype of tumor cells but the role of MCT1 in liver disease is unknown. The aim of this study was to assess the expression and function of MCT1 and its chaperone CD 147 (basigin), a transmembrane protein that is responsible for targeting MCT1 to the cell membrane, in hepatic fibrosis. Methods and Results: Quantitative PCR and western blot analysis revealed significantly increased hepatic MCT1 and CD147 expression in different murine models of hepatic fibrosis, namely chronic TAA- or CCl4-application, bile-duct-ligation and dietary models of non-alcoholic steatohepatitis (NASH). Also in human NASH and cirrhotic liver tissue MCT1 and CD147 expression were increased compared to normal liver tissue. Immunohistochemical analysis showed strong MCT1 and CD147 staining in fibrotic septa, and coimmunofluorescence analysis with alpha-smooth muscle actin, a specific marker for activated hepatic stellate cells (HSCs) revealed strong expression of MCT1 and CD147 in these cells. In line with this, we found that MCT1 and CD147 expression increased during in vitro activation of primary murine and human HSCs. Hypoxia, a pathological factor known to promote hepatic fibrosis, further increased MCT1 and CD147 expression in activated HSCs in vitro. Also secretion of lactate increased time dependently during in vitro activation of HSCs and was further increased by hypoxia. In contrast, inhibition of MCT1 led to a significant reduction of lactate secretion in HSCs. Stimulation with exogenous lactate dose dependently induced proliferation of activated HSCs. Furthermore, lactate induced increased activation of NFkappaB and expression of NFkappaB regulated proinflammatory genes such as MCP-1 in activated HSCs. Conclusions: Our study identified MCT1 and likely also its chaperone CD147 as regulators of autocrine lactate secretion of HSCs and herewith also as critical mediators of the profibrogenic phenotype of HSCs. Strong expression in contrast to other liver cell types favors MCT1 and its chaperone as targets for antifibrogenic therapy in chronic liver disease. Corresponding author: Czech, Barbara E-Mail: barbara.czech@ukr.de 1.20 Gender linked counter effect of N. sativa seeds and P. ovata husks on fibrosis in NAFLD Abbas AS1, Sheikh N1 1 University of the Punjab, Department of Zooloy, Lahore, Pakistan areas in comparison with F-II group while peri lobular fibrosis bridging among portal triades was evident in the M-III and F-III groups. It is concluded that livers of males were more susceptible to HFD induced fibrosis. N. sativa seeds were helpful to minimize fibrosis while P. ovata husks along with HFD induced advanced fibrosis of the liver. Corresponding author: Sheikh, Nadeem E-Mail: s_nadeem77@yahoo.com 1.21 Hepatic detoxification and anti-oxidative response in liver tissue with cholestasis: analysis of Nrf2 dependent gene expression Sahin A1, Dayoub R1, Thomas M2, Zanger U2, Melter M1, Weiss TS1 1 University of Regensburg, University Children Hospital, Regensburg, Germany; 2Dr. Margarete Fischer-Bosch Institute of Clinical Pharmacology, Stuttgart, Germany Cholestasis is a reduction in bile flow induced by a variety of factors resulting in enhanced concentrations of toxic bile acids. It may lead to hepatocellular injury, inflammation, fibrosis, cirrhosis and finally to liver failure. Studies demonstrate that oxidative stress occurs in cholestatic liver tissue and reduction of reactive oxygen species during cholestasis diminish fibrosis. A crucial player in the defense against oxidative stress is the transcription factor NF-E2-related factor 2 (Nrf2). It has been shown that Nrf2 controlls expression of many antioxidant and transporter proteins. Activation of Nrf2 dependent gene expression may neutralize oxidative stress, reduces toxic metabolites and therefore may have an impact on pathologic changes that occur during cholestasis. In this study we analyzed mRNA expression of anti-oxidative genes and transporters regulated by transcription factor Nrf2 in liver tissue with cholestasis. Total RNA was isolated from human liver tissue samples characterized by a pathologist for cholestasis (132 patients) and normal liver tissue (40 patients). Liver samples with cholestasis were classified to grade 1 (26) mild, 2 (9) and 3 (43) severe. Primary diseases were Klatskin-tumors (19), liver metastasis (48), liver cirrhosis (37 including 4 PSC), liver cancer (9) and others (19). RNA expression levels were analyzed by qRT-PCR (TaqMan) and correlation studies were performed with histopathological as well as clinical parameters. When we compared mRNA profile of total cholestatic liver samples with normal liver tissue we found reduced expression levels of antioxidant genes GCLC, GPX, GST and HO1, phase II enzymes UGT2B4 UGT2B7, and transporters MRP2 MRP3 and BSEP. The observed reduced gene expression correlated positively with grading of cholestasis. Furthermore, cholestatic liver samples with grade 3 demonstrated increased NQO1 and MRP4 expression levels. Comparing normal liver tissue with cholestatic liver tissue samples without (53) and with bile duct proliferation (36) we found identical results as described before with enhanced NQO1 and MRP4 levels as well as reduced Nf2 levels in bile duct proliferating tissue. These results were also mirrored when we compared cholestatic liver samples with cirrhosis as primary disease with normal liver tissue. Interestingly, only in liver tissue from patients with extra hepatic Klatskin tumors we found increased NOX2 expression as an indicator of enhanced ROS production. Furthermore, in the latter samples we also found MRP4 increased while the reduced genes were the same as for total cholestasis, except for HO1 expression and Nrf2 expression were unchanged. In liver cholestasis several anti-oxidant genes are down regulated and correlated to the degree of disease. Only at the most severe level of cholestasis transporters such as MRP4 are up-regulated enhancing export of bile acids and toxic metabolites. Furthermore, transcription factor Nrf2, which regulates a variety of anti-oxidant and detoxifying genes is down regulated. Therefore, strategies to induce Nrf2 activity to activate anti-oxidant gene expression as well as reduction of increased bile acids and may be a promising therapeutic option in cholestatic liver disease. Corresponding author: Weiss, Thomas S E-Mail: thomas.weiss@ukr.de Nonalcoholic fatty liver disease (NAFLD) is an emerging hepatic disorder both in males and females of Asian countries mainly linked with high fat diet (HFD) consumption. The purpose behind the current project was to assess the counter effect of fat reducing agents against HFD induced fibrosis. Forty males (M) and forty female (F) Rattus norvegicus were subdivided into four groups (0, I, II and III) depending upon different diet compositions. Group 0 was fed on 100% rat chow, Groups I, II and III were provided with HFD. The diets of group II and III were supplemented with 5% Nigella sativa seeds or Plantago ovata husks per kg of HFD respectively. The histopathology of livers revealed portal and peri cellular fibrosis in M-I and F-I groups. M-II had radiating fibrosis in portal Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A7 A8 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 1.22 Hepatocytes secret a mediator pattern that induces macrophage phenotype with properties of wound healing type and regulatory macrophages Wolf S1, H$ussinger D1, Bode JG1 1 Heinrich-Heine University Hospital, Department of Gastroenterology, Hepatology and Infectious Diseases, Duesseldorf, Germany serological and histological aspects whereas Nerium oleander leaves extract has potential activity against TAA-induced liver damage. Corresponding author: Sheikh, Nadeem E-Mail: s_nadeem77@yahoo.com 1.24 Introduction: The liver comprises the body’s largest pool of macrophages constituting approximately 80 % of all sessile tissue macrophages of the body. Thereby macrophages have a remarkable plasticity since their differentiation and function is continuously adapted to the microenvironment, which among others is defined by direct and indirect intercellular communication including cell-cell contact and paracrine acting mediators. Up to now the complex network that determines the differentiation and function of liver macrophages and the impact of the intercellular communication between macrophages and the other parenchymal and non-parenchymal cell types of the liver is not well understood. Objectives: The present study investigates the role of the intercellular communication between macrophages and hepatocytes on macrophage differentiation and function. Under physiological conditions the sinusoidal endothelial cell layer and the space of Diss' separate macrophages and hepatocytes from each other. Therefore the study focuses on the impact of the intercellular communication via soluble mediators on the differentiation of bone marrow derived macrophages (BMDM) employing co-culture models with highly purified primary murine hepatocytes embedded in a sandwich collagen matrix. Results: Evidence is provided that in the presence of hepatocytes BMDM times dependently differentiate into a macrophage population that is characterized by the up-regulation of Gr-1, CD163, CD206, MHC class II and TLR4. In particular with respect to CD163 and CD206 this expression profile closely resembles to that of macrophages derived from the liver (Kupffer cells). These changes essentially depend on direct co-culture and were accompanied by alterations of the inflammatory response of co-cultured macrophages towards LPS treatment with increased expression of IL-10 and IFNb and a reduced and/or less sustained expression of TNFa, IL-6 and IL-12. Conclusion: The data provided indicate that the intercellular communication of hepatocytes and macrophages results in macrophages characterized by the expression of markers indicative for wound-healing type sessile tissue macrophages displaying a predominant anti-inflammatory cytokine release upon activation with LPS characterized by an increase of the IL-10/IL-12 ratio. Corresponding author: Bode, Johannes G. E-Mail: johannes.bode@med.uni-duesseldorf.de 1.23 Hepatoprotective Role of Nerium Oleander in Thioacetamide-Induced Chronic Inflammation Akhar T1, Sheikh N1 University of the Punjab, Department of Zoology, Lahore, Pakistan 1 Background and Aims: Many plant extracts and their bioactive substances are well recognized for their potential chemoprotective role in the treatment of liver injury induced by viruses, chemicals and drugs. This study is an attempt to evaluate the hepatoprotective potential of Nerium oleander leaves extract against thioacetamide (TAA) induced liver damage. Methods: Fifteen Wistar rats of either sex were randomly divided into three groups. Group I is provided with normal drinking water while group II and III were orally given TAA (200 mg/l) in drinking water for 18 weeks. Additionally Group III was treated with Nerium oleander leaves extract for seven days. Liver damage was assessed by hematological, biochemical parameters and histopathological observations. Data were analyzed by using one way ANOVA test with Tukey’s post hoc test and Prussian blue staining. Results: Significant variations were observed in TLC, hematocrit, hemoglobin, and MCHC with P= 0.009, P= 0.0001, P= 0.01 and P= 0.03, respectively. Serological analysis also showed significant variations in total lipids, triglycerides, H.D.L., L.D.L, and BSR with P= 0.0001, P=< 0.0001, P= 0.02, P= 0.002 and P= 0.03 respectively. Blue stained hemosiderin granules were observed in the peripheral area of hepatic lobules and mainly in kupffer cells in group II while lesser degree of iron deposition was observed in group III. Meanwhile, there was no noticeable hemosiderin granule in the group I. Conclusion: These finding indicate that TAA disturbs hematological, Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York HMGB1 inflammosome activity modulates HIF-1a in a rat model of thioacetamide (TAA)-induced chronic liver damage and cholangiocarcinoma development Ahmad S1, Moriconi F2 1 University Medical Center Goettingen, Gastroenterology and Endocrinology, Goettingen, Germany; 2University Hospital of Basel, Gastroenterology and Hepatology, Basel, Switzerland Background: HIF-1a and HIF-2a have been identified as key mediators of angiogenesis, inflammation, and metabolism and can activate simultaneously distinct target genes with different functions regarding the regulation of hypoxia-related-genes. Methods: Male Wistar rats and TLR-4-/- mice were administrated thioacetamide (TAA) in drinking water up to 20 weeks and sacrificed at 4, 8, 12, 16, 20 weeks. Expression of HIF-1a and HIF-2a was evaluated during liver damage and cholangiocarcinoma. Expression of HIF-1a, HIF-2a, HMGB1 was measured by RT-PCR and Western blot. HIF-1a, HIF-2a, a-SMA, CK-19, ED1 and ED2 were localized by immunofluorescence staining. Results: HIF-1a was colocalized with a-SMA during 8 and 16 weeks after TAA administration suggesting its role in liver fibrogenesis. However HIF-2a appeared in aSMA-positive-cells after 16 weeks. HIF-2a was localized mainly in proximity to the sinusoidal spaces and in the endothelial cells, showed positivity in ED 1-cells at 8w while HIF-1a positivity in ED 1-cells was detected only 16w after treatment. Immunohistochemistry of liver from TAA-treated rat revealed HIF-2a strong positivity in ED 2-cells but not for HIF-1a. RT-PCR and Western Blot data confirmed the immunohistochemical analysis showing a sharp increase of HIF-1a at 8w and of HIF2a at 16w. Western blot analysis showed increased accumulation of HMGB1 after liver damage and cholangiocarcinoma development. In TLR-4 Knockout mice by Western blot analysis, expression of HIF-1a and HMGB1 was switched off. Conclusion: HIF-1a expression in the hypoxic liver area during early time point after TAA-administration and its reduction during the experiment describes its role during hepatic repair and fibrogenesis. We highlight for the first time the role of HMGB1 in inducing HIF-1a gene expression during tumor development. The detection of HIF-2a at a late time point (16w) highlights a role of HIF-2a during the recovery phase. HIF-2a localization in endothelial cells during hepatic damage confirms its involvement in angiogenesis and vascularization. As HIF-2a seems to have a crucial role in the induction of the hepatic erythropoietin (EPO), its co-localization in ED-2+ cells opens a new scenario in the role of the macrophage compartment in the process of erythropoiesis. Corresponding author: Moriconi, Federico E-Mail: federico.moriconi@usb.ch 1.25 Impairment of insulin signaling in hepatocytes by supernatants of insulin-activated macrophages Camargo RG2, Henkel J1, Manowsky J1, Schanze N1, Coleman D1, Pathe-Neusch$fer-Rube A1, Seelaender M2, P!schel GP1 1 University of Potsdam, Institute of Nutrition, Department of Nutritional Biochemistry, Nuthetal, Germany; 2University of S¼o Paulo, Institute of Biomedical Science, Cancer Metabolism Research Group, S¼o Paulo, Brazil Background: Hepatic insulin resistance and hyperinsulinemia are hallmarks in pre-diabetic obese patients. It is generally assumed that hyperinsulinemia is a consequence of the attempt of the body to compensate insulin resistance by enhanced release of insulin from b-cells. Here, evidence is provided that hyperinsulinemia itself might contribute to the development of hepatic insulin resistance by enhancing cytokine production in macrophages. Methods: U937 cells were differentiated into macrophages by PMA treatment. These macrophages were stimulated with 100 nM insulin for 24 h and cytokine gene expression was determined by qPCR. Supernatants of control and insulin-stimulated macrophages were added simultaneously with insulin to primary cultures of hepatocytes. Activation of insulin and cytokine signaling was quantified by westernblot and RT-qPCR. Results: Incubation of macro- 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen phages with insulin for 24 h significantly increased the mRNA level of IL1b, TNFa, IL-6 and Oncostatin M and enhanced the LPS-dependent induction of these cytokines. It also enhanced the prostaglandin E2-dependent induction of IL-1b whereas it attenuated the PGE2-dependent repression of TNFa. In contrast to supernatants of untreated macrophages, supernatants of insulin-treated macrophages reduced the insulin-dependent induction of glucokinase in primary cultures of rat hepatocytes, activated ERK1/ 2 kinase and provoked an inhibitory serine phosphorylation of the insulin receptor substrate. Discussion: The current data provide evidence that hyperinsulinemia in a vicious cycle feed forward loop may both elicit cytokine release and enhance LPS-stimulated cytokine release from macrophages and thereby contribute to the development of hepatic insulin resistance. Corresponding author: Henkel, Janin E-Mail: jhenkel@uni-potsdam.de 1.26 In vitro generation of 3-dimensional organoid liver structures using differentiatedhuman cells Breitkopf-Heinlein K1, Ramachandran SD2, Schirmer K1, Ebert M1, Ghafoory S3, W"lfl S3, M!nst B2, Heinz S2, Braspenning J2 1 University of Heidelberg, II. Medical Clinic, Molecular Hepatology – Alcohol-dependent Diseases, Faculty of Medicine at Mannheim, Mannheim, Germany; 2Medicyte, Heidelberg, Germany; 3University of Heidelberg, Institute of Pharmacy and Molecular Biotechnology, Ruprecht-KarlsUniversity Heidelberg, Heidelberg, Heidelberg, Germany 3D structures resembling embryonic liver buds have recently been described using stem cell-derived cell types (Takebe et al., 2013). Such structures can be transplanted into animals/patients but may also be useful for applications like ex vivo drug toxicity tests. We here used differentiated upcyte! cells which are derived from primary human cells that underwent targeted genetic modification (upcyte! process) in order to transiently induce or extend proliferation resulting in mortal, but expandable, differentiated cells. upcyte! cells can undergo up to 40 additional population doublings, and when contact-inhibited they differentiate into functional cells while maintaining most of their specific characteristics. We combined human upcyte! cell suspensions (composed of hepatocytes, liver sinusoidal endothelial cells (LSECs) and mesenchymal stem cells (MSCs)) that spontaneously formed organoids in vitro which were then cultured in a bioreactor (kirkstall! quasi vivo system) for up to 10 days. These self-organized, liver-like structures harbor healthy, living cells showing typical functional characteristics of liver parenchym, including basal as well as drug-induced activity of Cyp3A4 and spatial organization of the cells into a bar-like hepatic architecture. We further characterized the expression profiles of these organoids by immunohistochemistry and in situ hybridization. Our results show that 3D functional liver structures can be generated in vitro using quasi primary upcyte! cells. These organoids represent a promising new system to study acute and long-term effects of drugs or pathologic conditions (e.g. hypoxia or inflammation) on human liver functions ex vivo. Corresponding author: Breitkopf-Heinlein, Katja E-Mail: katja.breitkopf@medma.uni-heidelberg.de 1.27 Increased expression of the Glucose-transporter GLUT1 during hepatic stellate cell activation promotes hepatic fibrosis Czech B1, Valletta D1, Koch A1, Saugspier M1, Bosserhoff A2, Hellerbrand C1 1 University Hospital Regensburg, Internal Medicine I, Regensburg, Germany; 2University Regensburg, Pathology, Regensburg, Germany Normal liver reveals only low expression of the facilitative glucose transporter (GLUT) 1. Recently, we have shown that GLUT1 expression is increased in hepatocellular carcinoma (HCC), where GLUT1 acts as a tumor promotor. Hyperglycemia is one of the factors known to induce and promote hepatic fibrogenesis, and the activation of hepatic stellate cells (HSCs) is the key event of hepatic fibrosis. Furthermore, these cells form and transduce the HCC stroma. The aim of this study was to assess the expression and functional role of GLUT1 in hepatic fibrosis. Methods and Results: Hepatic GLUT1 expression was significantly increased in different murine models of hepatic fibrosis, namely chronic TAA or CCl4application, bile-duct-ligation and dietary models of non-alcoholic stea- tohepatitis (NASH). Also in cirrhotic human livers and human NASH GLUT1 expression was increased. Interestingly, hepatic GLUT1 expression revealed a significant correlation with collagen I and alpha-sma levels indicating activated HSCs as cellular source of GLUT1, which was confirmed by immunohistochemical analysis. In line with this, we found that GLUT1 expression increased during in vitro activation of primary murine and human HSCs. To gain insight in the functional role of GLUT1 in activated HSCs we inhibited GLUT1 expression with siRNA or the specific GLUT1 inhibitor WZB117 and found that GLUT1 suppression impaired glucose uptake and lactate secretion of HSCs indicative for reduced anaerobic glycolysis. Functional analysis demonstrated that reduced GLUT1 expression led to lower apoptosis resistance of HSCs. Transgenic GLUT1 knockdown mice subjected to TAA induced liver fibrosis model revealed less pronounced liver damage than WT animals confirmed by hepatic sirius red staining and alpha-sma protein expression. In line with this, treatment with GLUT1 inhibitor WZB117 in combination with the NASH inducing MCD diet resulted in less hepatic alpha-sma and collagen I expression than animals treated with vehicle. Conclusions: Increased GLUT1 expression during HSC activation functionally affects HSCs, and herewith, likely promotes the development and progression of hepatic fibrosis. Therefore and based on its known role as tumor-promotor, GLUT1 appears as attractive novel target to inhibit the progression of chronic liver disease. Corresponding author: Czech, Barbara E-Mail: barbara.czech@ukr.de 1.28 Increased Lysyl oxidase-like 2 (LOXL2) gene expression accurately designates advanced liver fibrosis induced by the Hepatitis C Virus (HCV) regardless race, blood specimen or co-infection with the Human Immunodeficiency Virus (HIV) Katsounas A1, Trippler M1, Meissner EG2, Schlaak JF1, Gerken G1, Kottilil S2 1 University Hospital Essen, Gastroenterology and Hepatology, Essen, Germany; 2National National Institute of Allergy and Infectious Disease/NIH, Laboratory of Immunoregulation, Bethesda, Maryland, USA Background: The LOX gene encodes a member of the lysyl-oxidase (LOX) gene family, which is involved in biogenesis of connective tissue, and 4 LOX-like proteins (LOXL1 – 4) have been identified so far. This study was aimed to investigate gene expression of LOXL1 – 4 in association with fibrogenesis in Hepatitis C Virus (HCV) infected patients with and without co-infection with the Human Immundeficiency Virus (HIV) in peripheral blood mononuclear cells (PBMC), peripheral whole blood (PwB) and liver tissue (LT) samples. Materials and Methods: PwB samples from 34 therapy-naive patients (34/ 34 Caucasians, 18/ 34 males, 28 /34 with HCV-genotype-1) with chronic HCV infection treated at the University Hospital Essen (Germany) and PBMC samples from 23 HIV/HCV co-infected subjects (11/ 23 African Americans and none Caucasian, 20 / 23 males, 23 / 23 with HCV-genotype-1) recruited at the NIAID/NIH (MD/U.S.A.) were enrolled in this study. Liver biopsies obtained at baseline were evaluated using the Batts-Ludwig staging (BL-S) system for HCV mono-infected patients and the Ishak score (IS) for HIV/ HCV co-infected donors. 34 PwB and 23 PBMC samples (and 7 LT samples from HIV/HCV co-infected participants) were subjected to microarray analysis. For all statistical analyses (i.e. pair-wise group comparison) 1-way-ANOVA was performed. Overall, a P< 0.05 was considered significant. Results: PwB samples from 34 HCV mono-infected patients were grouped according to BL-S as early fibrosis (BL-S: 0 – 1, “EF”, N= 20,) and late fibrosis (BL-S: 2 – 4, “LF”, N= 14) and PBMC samples from 23 HIV/HCV co-infected patients were grouped based on IS as early fibrosis (IS: 0 – 2, “EF”, N= 20) and late fibrosis (IS: 3 – 6, “LF”, N= 14). We consistently detected significantly increased LOXL-2 gene expression levels in association with “LF” in HCV mono-infected patients (PwB, P< 0.041) and HIV/HCV co-infected subjects (PBMC, P< 0.038). In addition, linear regression analysis was performed between fibrosis grades (IS: 0 – 6) and LOXL1 – 4 gene expression levels measured in LT samples of 7 HIV/HCV co-infected subjects; here, a significant correlation was found only for LOXL 1 (r= 0.8, P> 0.031). These results are currently being validated by quantitative real-time polymerase chain reaction (qRT-PCR). Conclusions: This study suggests significant involvement of LOX-like proteins, especially LOXL2, in the fibrogenic liver transformation process during chronic HCV infection. Previous research reported: 1. Association between increased mRNA levels of LOXL2 and type-III-procollagen in liver fibrosis in mice. 2. Abnormal deposition of collagen in hepatocytes obtained from humans with Wilson’s disease. 3. LOXL2 involvement in Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A9 A10 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen fibroblast activation. These findings (1.-3.) along with the present data demonstrating consistent significance in two demographically very heterogeneous cohorts further highlight the pathogenic role suggested for LOXL in fibrogenesis and the importance of generating LOXL 2-targeted therapies for the prevention/treatment of liver fibrosis. Corresponding author: Katsounas, Antonios E-Mail: antonios.katsounas@uk-essen.de 1.29 Inflammatory cell infiltration in experimental liver fibrosis is affected by inhibition of fibronectin matrix assembly Altrock E1, Vasel M2, Kawelke N2, Dooley S3, Sottile J4, Nakchbandi IA2 1 University of Heidelberg, Institute for Immunology, Heidelberg, Germany; 2Max-Planck Institute for Biochemistry, Martinsried, Germany; 3University of Heidelberg at Mannheim, Department of Medicine I, Mannheim, Germany; 4University of Rochester School of Medicine and Dentistry, AAB Cardiovascular Research Institute, Rochester, New York, USA Background and Aims: The accumulation of inflammatory cells is an important step in liver fibrosis. Fibronectin has been shown to enhance tissue infiltration of various cell types including immune cells. Our aim was to determine how the loss of fibronectin in the liver might affect the inflammatory response to liver injury. In prior work by our group, deletion of fibronectin production by the myofibroblasts resulted in an increase in available TGF-b and hence an increase in fibrotic signals within the liver precluding an examination of the direct effect of fibronectin on inflammation in the response to fibrosis induction. We therefore instead inhibited fibronectin fibril formation pharmacologically and evaluated the various inflammatory cells in a toxic liver injury model. Methods: Liver fibrosis was induced by injecting carbontetrachloride (CCl4) for 42 days in 8-week-old wild-type male mice. In order to diminish fibronectin assembly, the inhibitor pUR4 was injected during the last 10 days of fibrosis induction in the parallel model or for 10 days after the end of fibrosis induction in the successive model. At the end of the experiments, the inflammatory cells accumulating in the liver were examined by flow cytometry and by immunhistochemical staining of liver sections. The relative cytokine expression in the liver was measured using qPCR. Results: In vitro studies on hepatic stellate cells confirmed that the fibronectin assembly inhibitor, pUR4 suppresses accumulation of both fibronectin and collagen in the extracellular matrix by more than 60 %, but does not affect hepatic stellate cell activation, collagen mRNA expression, and availability or activity of TGF-b. Induction of fibrosis over 6 weeks using CCl4 was therefore combined with treatment with pUR4. pUR4 normalized the amount of fibrotic tissue that accumulated with injury, and improved liver function. Specifically, pUR4 treatment decreased collagen and fibronectin matrix accumulation to levels similar to healthy controls. Interestingly, despite a significant decrease in the total number of inflammatory cells in the liver (CD 45+) by 42 %, no changes were detected in Kupffer (F4 / 80+) or alpha-smooth muscle actin-expressing hepatic stellate cell (a-SMA+) numbers. In line with these findings, neither at the mRNA level nor at the protein level could we detect a change in TGF-b. Similarly, mRNA expression of IFN-g or TNF-a remained unaffected. The decrease in CD 45+ cells was largely due to diminished infiltration by T- and B-lymphocytes in the pUR4treated group (by 60 %). In line with the decrease in the lymphocyte numbers, we found a significant decrease (also by 60 %) in IL-6, IL-1b, CCl-2 and SDF-1 mRNA in the pUR4-treated group. Thus, the normal matrix composition seems to normalize inflammatory cell infiltration. Conclusion: In summary, interference with fibronectin matrix assembly results in decreased fibronectin and collagen accumulation, improved liver function and reduced inflammatory cell infiltration during liver fibrogenesis. Thus, these data suggest that not only does fibronectin matrix modulation offer a therapeutic benefit in preclinical models of liver fibrosis but that changes in matrix composition also affect the immune response in liver fibrosis. Corresponding author: Altrock, Eva E-Mail: eva.altrock@immu.uni-heidelberg.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York 1.30 Influence of vitamin D supplementation on liver function tests, vitamin D levels and liver stiffness in patients with chronic liver diseases in an outpatient setting K"nig A1, Lammert F1, Gr!nhage F1 1 Saarland University Hospital, Medical Department II, Homburg, Germany Introduction: Patients with chronic liver disease are prone to vitamin D deficiency (< 20 ng/ml). It has been suggested from previous studies that patients with very low vitamin D levels may have an unfavorable outcome concerning antiviral treatment of chronic hepatitis C, presence of advanced disease and even mortality. Thus, we performed a retrospective cohort analysis investigating patients with low serum vitamin D concentrations and supplementation of vitamin D (group 1); patients with low levels of vitamin D and no supplements (group 2); and patients with normal vitamin D levels (group 3). Read-out measures were serum vitamin D levels, liver function tests and the development of liver stiffness. Patients and Methods: We aimed to study the data of an equal number of patients from our outpatient clinic with chronic liver diseases, who we identified by data base analysis between 2008 and 2013. The patient files were screened for vitamin D levels at initial presentation, liver function tests (AST, ALT), and liver stiffness measurements by Fibroscan. Patient records were then followed for development of liver function tests under no treatment (all groups) for 1 year. In addition, we studied the development of liver function tests and liver stiffness after one year in the group that received vitamin D supplementation. Results: Overall we included 101 patients in group 1, 100 in group 2 and 35 in group 3. As expected, patients in groups 1 and 2 presented with lower vitamin D levels as in group 3 (10.6 € 5.2 ng/ml and 14.0 € 6.5 ng/ml vs. 33.3 € 8.5 ng/ml; p < 0.05 for all comparisons). During follow-up without intervention, we noticed a significant increase in mean liver stiffness after 1 year in group 1 from 16.3 kPa to 27.3 kPa (P< 0,05), while there was no change in group 2. Of note after one year of treatment with vitamin D, the patients in group 1 experienced a significant decrease in mean liver stiffness values from 27.3 kPa to a mean of 12.3 kPa (p < 0,05), while no significant changes were detected in the other parameters studied. Discussion: Despite all limitations of a retrospective study, these results further support the important role of vitamin D in the course of chronic liver disease and its potential for an influence of liver stiffness. Furthermore, these results should encourage interested investigators to follow this concept in a prospective randomized trial. Corresponding author: Gr!nhage, Frank E-Mail: frank.gruenhage@uks.eu 1.31 Lineage fate of ductular reactions in liver injury and carcinogenesis J"rs S1, Jeliazkova P1, Ringelhan M1, Thalhammer J1, D!rl S1, Ferrer J2, Sander M3, Heikenw$lder M4, Schmid RM1, Siveke JT1, Geisler F1 1 Klinikum rechts der Isar, Technische Universit$t M!nchen, II. Department of Medicine, Munich, Germany; 2Imperial College London, Department of Medicine, London, UK; 3 University of California, Department of Pediatric and Cellular & Molecular Medicine, San Diego, USA; 4Technische Universit$t M!nchen, Institute of Virology, Munich, Germany Ductular reactions (DRs) are observed in virtually all forms of human liver disease. Nevertheless, the histogenesis and function of DRs in liver injury are not entirely understood. It is widely believed that DRs contain bipotential liver progenitor cells (LPCs) that serve as an emergency cell pool to regenerate both, cholangiocytes and hepatocytes, and may eventually give rise to hepatocellular carcinoma (HCC). Here we provide a thorough analysis on the histogenesis of DRs and their potential contribution to liver regeneration and carcinogenesis. Using a mouse model that allows highly efficient and specific lineage labeling of the biliary compartment, we demonstrate that biliary cells are the predominant precursors of DRs found in multiple experimental and genetic liver injury models but lack significant capacity to produce new hepatocytes, even during prolonged liver injuries up to 12 months. Genetic modulation of Notch and/or Wnt/b-catenin signaling within lineage-tagged DRs impaired DR expansion but failed to deliberate DRs from their biliary fate towards the hepatocyte lineage. Further, lineage-labeled DRs did not produce tumors in genetic and chemical HCC mouse models. Our findings question the presence of an adult LPC compartment within biliary- 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen derived DRs that physiologically functions to replenish hepatocytes or give rise to HCCs. Corresponding author: Geisler, Fabian E-Mail: fabian.geisler@lrz.tum.de Lipocalin 2 (LCN2) in hepatic inflammation 1.32 Asimakopoulou A1, Borkham-Kamphorst E1, Weiskirchen R1 1 RWTH University Hospital Aachen, Institute of Molecular Pathobiochemistry, Experimental Gene Therapy and Clinical Chemistry, Aachen, Germany Background: Lipocalin-2 (LCN2), also known as neutrophil gelatinaseassociated lipocalin (NGAL), is a small secreted adipokine that belongs to the family of lipocalins that are known for binding and transporting small hydrophobic molecules such as fatty acids, steroids and iron [1]. In the liver, LCN2 plays a protective role in inflammation, infection, injury and other forms of cellular stress. This was proven in the bile duct ligation and the carbon tetrachloride model [2]. Recently, we demonstrated that LCN2 regulates perilipin 5 (PLIN5) expression in primary hepatocytes [3]. Material and Methods: In the present study, we analysed the role of LCN2 in an experimental model of non-alcoholic steatohepatitis (NASH). A methionine- and choline-deficient (MCD) diet was fed in wild type (WT) and LCN2-deficient (Lcn2-/-) mice for four to six weeks as an experimental model for NASH. Hepatic inflammation, injury and fibrosis were scored in specimen subjected to Haematoxylin and Eosin stain, Sirius Red stain, and by immunohistochemistry using antibodies specific for the common leukocyte marker CD45 and Myeloperoxidase (MPO) representing a marker for neutrophil granulocytes. Moreover, we comparatively analysed the mRNA expression of inflammatory cytokines such as IL-6, TNF-a, IL-1b, CCL2 and CCR2. Furthermore, the expression and phosphorylation of the STAT1 and STAT3 proteins was investigated. Results: WT mice developed more severe liver inflammation than the Lcn2-/-. They had significant more multiple leukocyte and bigger neutrophil infiltrates, showed higher expression of CD45 and MPO. Strong upregulation of LCN2 during administration of the MCD diet was observed in the WT mice. In addition, a significant stronger activation of STAT3 and STAT1 was observed in WT mice. In summary, inflammation at 4 weeks and fibrosis scores at 6 weeks in animals fed with MCD diet were higher in WT animals. Conclusions: Our data indicate that the biological activity of LCN2 in experimentallyinduced liver injury depends on the model analysed. While LCN2 acts protectively in models that are commonly used to induce liver cirrhosis, the presence of LCN2 during MCD diet results in more severe liver damage. References cited: [1] Flower DR. The lipocalin protein family: structure and function. Biochem. J. 1996;318:1 – 14. [2] Borkham-Kamphorst E, van de Leur E, Zimmermann HW, Karlmark KR, Tihaa L, Haas U, Tacke F, Berger T, Mak TW, Weiskirchen R. Protective effects of lipocalin2 (LCN2) in acute liver injury suggest a novel function in liver homeostasis. Biochim Biophys Acta 2013;1832:660 – 73. [3] Asimakopoulou A, Borkham-Kamphorst E, Henning M, Yagmur E, Gassler N, Liedtke C, Berger T, Mak TW, Weiskirchen R. Lipocalin-2 (LCN2) regulates PLIN5 expression and intracellular lipid droplet formation in the liver. Biochim Biophys Acta 2014;1841:1513 – 24. Corresponding author: Weiskirchen, Ralf E-Mail: rweiskirchen@ukaachen.de 1.33 Loss of gap junctions in biliary atresia occurs simultaneously with declined expression of Protein kinase Ca Andruszkow JHK1, Groos S2, Klaus C1, Schneider U1, Petersen C3, Gassler N4, Kn!chel R1, Luciano L2 1 University Hospital RWTH Aachen, Institute of Pathology, Aachen, Germany; 2Hannover Medical School, Institute of Cell Biology, Hannover, Germany; 3Hannover Medical School, Center of Pediatric Surgery, Hannover, Germany; 4 Klinikum Braunschweig, Institute of Pathology, Braunschweig, Germany Biliary atresia (BA) is known as an inflammatory process of the extra hepatic bile ducts, resulting in persistent cholestasis of the newborn. Without surgical intervention and subsequent liver transplantation, progressive cirrhosis leads to death of patients prior to the age of two years. Previous studies detected alterations of gap junctions (GJ) in cholestatic disorders. GJ consist of six connexins (Cx) and form intercellular channels between neighboring cells. By enabling diffusion of ions and small molecules, GJ play a pivotal role e.g. in apoptotic cell death which is known to be a characteristic feature in BA. Therefore, we aimed at investigating modifications of GJ in both a mouse model of BA and in human infant patients. In compliance with the German national regulations on the protection of animals and after approval by the local Committee for Animal Research, newborn BALB/c mice were injected either with Rhesus Rotavirus to induce BA (RRV, M1) or phosphate buffered saline for control (M2). Monitoring the clinical course, mice were sacrificed on days 3, 7, 9 and 14. In combination with assessment of clinical findings, quantitative real time PCR (PCR) and Western Blot (WB) were performed regarding expression of RRV, Cx43, phosphorylated Cx43 and Protein kinase Ca (PKCa) in liver tissue. In addition, murine liver specimen from both animal groups as well as liver tissue from infant BA patients were analyzed by freeze fracture electron microscopy (FFEM). In our murine test group M1, PCR revealed detectable RRV expression on days 3 and 7 but not on day 14. While RNA expression of Cx43 did not show differences between M1 and M2 (p = 0.83), WB analysis revealed a decrease of Cx43 in M1 on days 7 and 14 (p = 0.01). In contrast, there was an increase of phosphorylated Cx43 in M1 on day 14 (p = 0.01). Simultaneously, we observed a 3fold decrease of PKCa in M1 on day 7 and 14 (p = 0.01). Morphologically, FFEM replicae showed a decrease in GJ number and size in M1 compared to M2. Furthermore, a loss of GJ and a morphological alteration of tight junctions lining the biliary canaliculi in human infant BA patients were observed. Our study revealed a decrease of GJ protein Cx43 in experimental BA. In addition, phosphorylated and therefore functionally ineffective Cx43 was increased in these mice. These findings correlate with both, the FFEM observations in the experimental mouse model as well as those in human BA patients. Due to the fact that there were no differences in Cx43 RNA expression, we hypothesize that posttranscriptional modification is the major cause for alterations of GJ. PKCa is known as a possible modifier of GJ via phosphorylation of Cx43. However, our data showed a significant decline of PKCa in BA mice, raising the question if established PKCa and/or other candidate proteins are involved in the loss of GJ in BA. Further studies are needed to specify the background of GJ alterations in order to obtain superior therapeutic options for BA. Corresponding author: Andruszkow, Julia H.K. E-Mail: jandruszkow@ukaachen.de 1.34 Loss of Integrin-b1 in Hepatocytes Induces Liver Fibrosis Altrock E1, Sens C1, Kawelke N2, Nakchbandi IA2 1 University of Heidelberg, Institute of Immunology, Heidelberg, Germany; 2Max-Planck Institute for Biochemistry, Martinsried, Germany Background and Aims: Integrins are receptors located on cell surfaces that mediate the interaction between cells and the extracellular matrix (ECM) by directly binding components of the ECM like fibronectin and collagen. Integrin-b1 is a major integrin subunit that is involved in a variety of vital functions resulting in embryonal lethality in knockout mice. In the liver, integrin b1 was shown to support liver regeneration. Further, in vitro studies have shown that it supports matrix turnover. We therefore asked whether integrin b1 might affect the amount of matrix produced or accumulating in the matrix under physiologic conditions. Methods: Conditional knockout mice lacking integrin-b1 in hepatocytes (HCs) were used to investigate the role of integrin-b1 in the liver (cKO: Alb-cre+/- b1fl/fl; CT: b1fl/fl). Results: The loss of integrin-b1 in HCs is associated with significant increases in ALT and AST and enhanced HCs apoptosis. Furthermore, matrix accumulated in a pattern suggestive of fibrosis and was associated with collagen I and IV accumulation in cKO mice compared with CT. We therefore evaluated whether a cytokine might be responsible for this effect in the absence of b1 integrin. We found that TGF-b1, a pro-inflammatory cytokine, was increased by 44% in the liver and 56 % in isolated HCs. The canonical signaling pathway of TGF-b exemplified by nuclear translocation of SMAD3 and 4 in isolated HCs was activated. Because the increase of TGF-b could be either due to enhanced TGF-b production or diminished breakdown we evaluated its mRNA expression and found that it was diminished. We therefore embarked on evaluating whether TGF-b degradation was diminished in the absence of integrin-b1. TGF-b can be internalized either through caveolae or clathrin-coated pits, whereby the caveolar endocytotic pathway is important for degradation. In isolated HCs from cKO mice caveolin-1, the main component of caveolae, is diminished by both staining and western blot. In addition, treatment of CT HCs with the caveolin inhibitor genistein resulted in decreased caveolin-1 and increased EEA-1 staining showing a similar pattern as untreated cKO HCs. In contrast, the early endosome protein EEA-1, a mar- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A11 A12 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen ker for clathrin-coated pits, was increased by staining and western blot analysis of cKO HCs. This was associated with increased SMAD 4 translocation to the nucleus indicating activation of the canonical pathway in cKO HCs. A similar effect was obtained when CT HCs were treated with genistein. This suggests that the defect in cKO HCs is due to a decrease in caveolin-mediated degradation of TGF-b. Conclusion: These findings suggest that the loss of integrin-b1 results in an increase in matrix accumulation that is mediated by an elevation of TGF-b. The increase in TGF-b is not due to an increase in its production, but instead to a decrease in its caveolin-mediated degradation. The mechanism by which b1 integrin affects caveolin-1 levels remains to be elucidated, however. Corresponding author: Altrock, Eva E-Mail: eva.altrock@immu.uni-heidelberg.de 1.35 MIF shows profibrotic properties after MCD diet via NKT cell population Heinrichs D1, Knauel M1, Berres ML2, Fischer P2, Trautwein C2, Wasmuth HE2, Bernhagen J1 1 RWTH Aachen University, Institute of Biochemistry and Molecular Cell Biology, Aachen, Germany; 2RWTH Aachen University, Medical Department III, Aachen, Germany Background: Macrophage migration inhibitory factor (MIF) is a pleiotropic inflammatory cytokine. It has recently been recognized to function as a chemokine-like molecule in chronic inflammatory diseases. In a model of hepatotoxic liver injury, MIF shows anti-fibrotic properties via CD74 and AMPK. In a model of non-alcoholic steatohepatitis, MIF has anti-steatotic properties. Because NASH is also associated with fibrosis within the liver, we compared Mif -/- with wild-type mice in an experimental liver fibrosis and metabolic disease model. Methods: Mif -/- and wild-type mice were fed a methionine- and choline deficient diet (MCD diet) for eight weeks. Fibrosis was analyzed by histology (Sirius red staining), hydroxyproline content and intrahepatic mRNA expression of fibrosis-related genes (Col1a1, Timp1, Tgfb1 and Mmp2). Recruitment of immune cells, like T cells, NK cells, NKT cells was assessed by FACS analysis, while macrophages were quantified by immunohistochemical staining with F4 / 80. Expression of a cytokine profile which is associated with NKT cells was determined with quantitative RT-PCR. Results: Constitutive Mif knockout mice (Mif -/-) showed decreased fibrosis after eight weeks of MCD diet as assessed by histology and hepatic collagen levels. Reduced liver fibrosis in Mif -/- mice was associated with strong alterations in fibrosis-relevant genes (Col1a1, Timp1, Mmp2 and Tgfb1). The livers of Mif -/- mice showed less activated stellate cells compared to wild-type mice. Interestingly, FACS analysis revealed no major differences in immune cell infiltration between Mif -/- and wild-type mice, only the NKT population is strongly increased in Mif -/- mice. Cytokine profile analysis showed that NKT cells in livers of Mif -/- mice were skewed toward type II NKT cells. Conclusions: In our metabolic NASH model MIF shows profibrotic effects which are probably mediated through type II NKT cells. These results describe a yet undiscovered relation of MIF and NKT cell subsets and are the basis for further evaluation of this chemokine in this liver disease model. Corresponding author: Heinrichs, Daniel E-Mail: dheinrichs@ukaachen.de 1.36 MK2 mediates induction and sensing of Oncostatin M-induced intercellular signalling in the liver but is dispensable for negative feedback regulation via SOCS 3 B"hmer O1, Ehlting C1, Hahnel MJ1, Thomas M2, Zanger UM2, Gaestel M3, Knoefel WT4, Schulte am Esch J4, H$ussinger D1, Bode JG1 1 Heinrich-Heine University Hospital, Department of Gastroenterology, Hepatology and Infectious Diseases, Duesseldorf, Germany; 2Robert Bosch Hospital, Dr. Margarete Fischer-Bosch Institute of Clinical Pharmacology, Stuttgart, Germany; 3Hannover Medical School, Institute of Physiological Chemistry, Hannover, Germany; 4HeinrichHeine University Hospital, Department of Surgery, University Hospital, Duesseldorf, Germnay Oncostatin M (OSM) is expressed in the context of several inflammatory diseases and plays a role in liver regeneration after liver injury. It is mainly secreted by activated T lymphocytes, monocytes and macrophages such as the Kupffer cells of the liver. As a member of the IL-6- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York type cytokine family it is also involved in the regulation of acute phase protein expression in hepatocytes. Binding of OSM to its cognate receptor complex, activates several signaling cascades. This includes signals mediated via the Janus kinase (JAK)/signal transducer and activator of transcription (STAT) pathway and those mediated via mitogen-activated protein kinase (MAPK) activating kinase (MEK)1 and subsequent activation of extracellular signal regulated kinase (ERK)1 and 2. Apart from this OSM also strongly induces activation of p38MAPK and its downstream effector kinase MAPK activated protein kinase (MK)2. Our data reveal that in macrophages MK2 is required to produce OSM in response to inflammatory stimuli such as lipopolysaccharides (LPS). Of note, although macrophages are able to produce OSM, they are not able to sense OSM since they lack the b subunit of the OSM receptor (OSMRb). Contrariwise, in hepatocytes MK2 negatively controls the availability of the OSMRb subunit, which is highly expressed in hepatocytes. Hence, during LPS-induced inflammation OSM represents a one-directional signal released from the macrophages and sensed by hepatocytes. Interestingly, the data suggest that MK2 controls both the intensity of the signal as well as the receptiveness of the recipient. Thereby MK2 controls the receptiveness of hepatocytes towards OSM at the receptor level, but not at the level of feed back regulators of intracellular signalling, such as suppressor of cytokine signalling (SOCS)3. Evidence is provided that the regulation of the OSM-induced expression of this major endogenous negative regulator of STAT3 signalling involves MEK-1- and Erk1/ 2-dependent stabilization of the SOCS transcript but does not require MK2. Thus, in the context of liver injury MK2 is essential for the induction and sensing of OSM-mediated intercellular signaling between macrophages and hepatocytes, but it is dispensable for intracellular negative feedback regulation of the STAT3-dependent intra-cellular signal-transduction of OSM. Corresponding author: Bode, Johannes G. E-Mail: johannes.bode@med.uni-duesseldorf.de 1.37 Mouse hepatic stellate cells are responsive to LPS and contribute to the acute phase response of hepatocytes Liebe R1, Breitkopf-Heinlein K1, Waldow K2, Braun S2, Thomas M3, Schildberg F4, Knolle P4, Zanger U3, Klingm!ller U2, Ebert M1, Dooley S1 1 University of Heidelberg, Department of Medicine II; Section Molecular Hepatology – Alcohol Associated Diseases; Medical Faculty Mannheim, Mannheim, Germany; 2 University of Heidelberg, Systems Biology of Signal Transduction (B200) DKFZ, Heidelberg, Germany; 3 University of Stuttgart, Margarete Fischer-Bosch Institute of Clinical Pharmacology, Stuttgart, Germany; 4University of Bonn, Institute of Molecular Medicine and Experimental Immunology, Bonn, Germany Background: The acute phase response (APR) is a systemic inflammatory condition initiated by activated phagocytic cells, fibroblasts and endothelial cells to prevent tissue damage and initiate repair processes. The aim of our study was to quantify the contribution of hepatic stellate cells (HSC) towards the APR induction. To this end, we quantified the secretory output of HSC with respect to the main acute phase cytokines. Hepatocytes’ response to the secretory HSC output was analysed by Fluidigm real time PCR analysis. Methodology: Primary HSC were cultivated for 48 hours before adding LPS to the medium. The release of 23 cytokines and chemokines was analysed by Luminex cytokine array technology after 24 hours of LPS stimulation (50 ng/ml). The main acute phase cytokines IL6, IL 1-beta and TNF-alpha were quantified after 2, 6 and 24 hours of LPS stimulation (0 / 10 / 50 / 100 ng/ml). Tissue culture supernatant of HSC following 24 hours stimulation with 100 ng/ml LPS was used to stimulate primary hepatocytes for 24 hours. Expression of 48 acute phase proteins (APP) in hepatocytes was analysed by Fluidigm real time PCR analysis and compared to hepatocytes treated with LPS or IL6 only for 6, 12 or 24 hours. Results: In HSC, G-CSF, KC (Cxcl1), IL-12 (p70), MCP-1a (Ccl2), TNFa and MIP1a (Ccl3) were the most prominently and significantly upregulated secreted cytokines after 24 hours and transcription of Ccls -2, -3, -4, -5 and -7, as well as Cxcls -1, -2, -3 and -5 were upregulated by LPS together with IL 1b, IL6 and TNFa in HSC. Stimulation of hepatocytes with conditioned medium from LPStreated HSC led to increased mRNA levels of Saa1, Saa2 and Orm1. Other targets like Hepcidin, Saa3 and IL-33 were already upregulated by direct treatment with LPS alone. Conclusion: Cytokine secretion data from HSC and expression data from hepatocytes exposed to HSC supernatant show a specific and intriguing role for HSC during the orchestration of 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen the acute phase response following endotoxemia. Besides being amplifiers of macrophage-induced cytokine signalling, these cells produce an independent secretory profile with an impact on hepatocytes that is different from effects induced by IL6 or LPS only. Corresponding author: Breitkopf-Heinlein, Katja E-Mail: katja.breitkopf@medma.uni-heidelberg.de 1.38 NLRP3 inflammasome expression in cultured hepatocytes is regulated by nuclear factor-kB (NF-kB) Boaru SG1, Borkham-Kamphorst E1, Van de Leur E1, Liedtke C2, Weiskirchen R1 1 RWTH University Hospital Aachen, Institute of Molecular Pathobiochemistry, Experimental Gene Therapy and Clinical Chemistry, Aachen, Germany; 2RWTH University Hospital Aachen, Department of Internal Medicine III, Aachen, Germany Background: The inflammasomes are cytoplasmic multiprotein complexes that are responsible for activation of inflammatory reactions. In principal, there are four individual inflammasome branches (i.e. NLRP1, NLRP3, NLRC 4/NALP4, and AIM2) that mediate the cleavage and activation of caspase-1 and IL-1b that in turn leads to a complex network of cellular reactions that at the end initiate local and systemic inflammatory reactions [1]. We have recently shown that NLRP3 is virtually absent in cultured hepatocytes and that in vitro the stimulation of hepatocytes with lipopolysaccharides (LPS) results in strong activation of NLRP3 expression [2]. In this study we investigated the impact of NFkB signalling on NLRP3 activation in primary hepatocytes. Methods: Murine primary hepatocytes were isolated after the collagenase method established by Seglen [3]. Cells were plated on collagen-coated plates. The NF-kB activation inhibitor QNZ (N4-[2-(4-phenoxyphenyl)ethyl]4,6-quinazolinediamine) and the adenoviral expression vector Ad5CMV-IkB(S 32A/S 36A) expressing a hemagglutinin-tagged human superrepressor of NF-kB [4] were used to block NF-kB signalling. After LPS challenge, the expression of TNF-a, IL-1b and NLRP3 was analysed by qRT-PCR, Western blot and immunohistochemistry. The influence of NFkB signalling on NLRP3 expression was further investigated in a novel murine hepatocytic cell system allowing directed depletion of the NF-kB essential modulator (NEMO). Results: We found that QNZ blocks NF-kBdependent expression of TNF-a, IL-1b and NLRP3. Likewise, the superrepressor of NF-kB prevents expression of NLRP3 and significantly reduces expression of inflammatory marker genes in liver cells. In cells that were depleted for NEMO, we could confirm that there is a close link of NF- kB activity and NLRP3 expression suggesting that the NF-kB pathway is the major pathway that controls NLRP3 expression. Conclusions: We conclude that NF-kB signalling is a necessary prerequisite for proper activation of the NLRP3 inflammasome in primary hepatocytes. Our data further suggests that targeting NF-kB will be therapeutic useful to interfere with NLRP3 inflammasome activation. References cited: [1] Martinon F, Mayor A, Tschopp J. The inflammasomes: guardians of the body. Annu. Rev. Immunol. 2009;27:229 – 265. [2] Boaru SG, Borkham-Kamphorst E, Tihaa L, Haas U, Weiskirchen R. Expression analysis of inflammasomes in experimental models of inflammatory and fibrotic liver disease. J. Inflamm. (Lond). 2012;9(1):49. [3] Seglen PO. Preparation of isolated rat liver cells. Methods Cell Biol. 1976;13:29 – 83. [4] Iimuro Y, Nishiura T, Hellerbrand C, Behrns KE, Schoonhoven R, Grisham JW, Brenner DA. NFkappaB prevents apoptosis and liver dysfunction during liver regeneration. J Clin Invest. 1998;101:802 – 11. Corresponding author: Weiskirchen, Ralf E-Mail: rweiskirchen@ukaachen.de 1.39 Pharmakologische oder genetische Intervention des CCL 5/RANTES Signalweges im in vivo Modell einer chronischer Leberentz"ndung vermindert die Fibrogenese und Progression zum Hepatozellul!ren Karzinom Mohs A1, Cubero FJ1, Kuttkat N1, de Bruin A2, Proudfoot Fichard A3, Trautwein C1 1 RWTH Aachen University Hospital, Medizinische Klinik III, Aachen, Deutschland; 2University of Utrecht, Department of Veterinary Medicine, Utrecht, The Netherlands; 3Merck Serono Geneva Research Centre, Geneva, Switzerland Hintergrund: Das Hepatozellul"re Karzinom (HCC) entwickelt sich auf Basis einer chronischen Leberentz!ndung, daraus resultierender Fibrose und schließlich maligner Transformation von Hepatozyten. In diesem multifaktoriellen Prozess spielen Immunzellen eine entscheidende Rolle. Im aktuellen Projekt, sollte daher die Relevanz des Chemokins CCL 5/RANTES und dessen therapeutische Beeinflussung durch Evasin-4, einem CCL5 Inhibitor, auf die Entstehung der Leberfibrose untersucht warden. Zugleich sollte die Rolle von CCL 5/RANTES auf die Entwicklung des HCCs charakterisiert werden. Methoden: Hepatozyten – spezifische NEMO knockout (NEMODhepa) M"use wurden mit mit konstitutiven CCL 5/RANTES M"usen verpaart (NEMODhepa/CCL 5-/-) und die Rolle von CCL5 auf die Fibroseentwicklung und die Initiation und Progression von HCCs analysiert. Zus"tzlich wurden 6 Wochen alte (NEMODhepa) M"use t"glich mit Evasin-4 !ber einen Zeitraum von 8 Wochen behandelt. Die Progression der Fibrose- und HCC-Entwicklung wurden mittels molekularbiologischer Methoden (Western Blot, qPCR und Immunhistochemie) analysiert. Ergebnisse: Die genetische Modifikation des CCL 5/RANTEs Signalweges in NEMODhepa M"usen f!hrte zu einer verminderten Firboseentstehung. Dies konnte mittels Proteinanalysen und immunohistochemischen Methoden gezeigt werden. In der HCC-Initiation zeigten sich keine Unterschiede im Vergleich von NEMODhepa/CCL 5-/- M"use und NEMODhepa M"usen. Allerdings wurde beobachtet, dass NEMODhepa/ CCL 5-/- M"use significant kleinere und weniger maligne Karzinome entwickeln. Dar!ber hinaus konnte nachgewiesen warden, dass die Tumore der NEMODhepa/CCL 5-/- M"use eine significant geringere Proliferationsrate und eine schw"cher ausgepr"gte Angiogenese aufwiesen. Aus diesen Ergebnissen resultierend, wurden NEMODhepa M"use !ber einen Zeitraum von 8 Wochen mit Evasin-4 therapiert. Die pharmakologische Intervention des CCL 5/RANTES Signalweges f!hrte zu einer signifikanten Verminderung der Fibrose in NEMODhepa M"usen. Dies konnte gezeigt werden, durch F"rbungen f!r Collagen 1AI, sowie einer Sirius Red F"rbung. Außerdem konnte die Fibrosereduktion anhand von etablierten Fibrosemarkern (aSMA, Collagen IA1, TGF-b, MMP-2 und MMP-3) best"tigt werden. Zusammenfassung: Die CCL5 Deletion in NEMODhepa M"usen f!hrte zu einer Inhibition der Fibroseprogression und des HCCWachstums. Durch pharmakologische Modulation des CCL 5/RANTES Signalweges konnte die Fibroseentstehung signifikant vermindert warden, daher k#nnte CCL5 eine attraktive Zielstruktur zur Prgressionshemmung chronischer Lebererkrankungen sein. Korrespondierender Autor: Mohs, Antje E-Mail: amohs@ukaachen.de 1.40 Platelet-derived growth factor-D intensifies fibrogenesis through upregulation of TIMP-1 expression and signalling through both platelet-derived growth factor receptors type a and b Borkham-Kamphorst E1, Van de Leur E1, Haas U1, Tihaa L1, Meurer SK1, Weiskirchen R1 1 RWTH University Hospital Aachen, Institute of Molecular Pathobiochemistry, Experimental Gene Therapy and Clinical Chemistry, Aachen, Germany Background: Platelet-derived growth factor-D (PDGF-D) is a more recent recognized growth factor of the PDGF family [1]. It regulates several cellular processes including cell proliferation, transformation, invasion, and angiogenesis through specifically binding to and activating its cognate receptor PDGFR-b. In experimental liver fibrotic models (BDL and carbon tetrachloride), we have shown that PDGF-D is upregulated comparable to that of PDGF-B [2, 3]. Moreover, adenoviral expression of PDGF-D induces hepatic stellate cell (HSC) proliferation and liver fibrosis [4]. We now seek to investigate the molecular mechanism of PDGF-D involvement in liver fibrogenesis. Material and Methods: PDGF-D stimulation was performed in profibrogenic primary cells including rat portal myofibroblasts (PMF), rat HSC and immortalized murine HSC cell line GRX. Expression of PDGF-D signaling of fibrogenic markers was done by qRT-PCR, Western blot analysis, MMP zymography, and immunohistochemistry. The binding activity of PDGF-D to the PDGF-a receptor was compared to the other PDGF isoforms in ligand-receptor binding assays. Results: We found that PDGF-D is not capable to enhance expression of collagen type I and a-smooth muscle actin. Instead it significantly upregulates TIMP-1 expression at both mRNA and protein levels resulting in attenuation of MMP2 and MMP9 gelatinase activity as indicated by gelatinase zymography. The MMP activity was restored after administration of a PDGF-D neutralizing antibody. Furthermore, PDGF-D incubation decreases both PDGFR-a and -b mRNA and protein levels. In addition, PDGF-D phosphorylates Tyr754 and Tyr1018 in PDGFR-a comparable to that observed after treatment with PDGF-B. Most interestingly, we could demonstrate for the first time that PDGF- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A13 A14 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen D binds with high affinity to the recombinant PDGFR-a-Fc chimera. Conclusions: PDGF-D intensifies fibrogenesis by interfering with the fibrolytic activity of the TIMP-1 /MMP system. Moreover, our data suggests that PDGF-D signals through both PDGF-a and -b receptors. References cited: [1] Reigstad LJ, Varhaug JE, Lillehaug JR. Structural and functional specificities of PDGF-C and PDGF-D, the novel members of the platelet-derived growth factors family. FEBS J. 2005;272:5723 – 41. [2] Borkham-Kamphorst E, van Roeyen CR, Ostendorf T, Floege J, Gressner AM, Weiskirchen R. Pro-fibrogenic potential of PDGF-D in liver fibrosis. J Hepatol. 2007;46:1064 – 74. [3] Borkham-Kamphorst E, Kovalenko E, van Roeyen CR, Gassler N, Bomble M, Ostendorf T, Floege J, Gressner AM, Weiskirchen R. Platelet-derived growth factor isoform expression in carbon tetrachloride-induced chronic liver injury. Lab Invest. 2008;88:1090 – 100. [4] Hudkins KL, Gilbertson DG, Carling M, Taneda S, Hughes SD, Holdren MS, Palmer TE, Topouzis S, Haran AC, Feldhaus AL, Alpers CE. Exogenous PDGF-D is a potent mesangial cell mitogen and causes a severe mesangial proliferative glomerulopathy. J Am Soc Nephrol. 2004;15:286 – 98. Corresponding author: Weiskirchen, Ralf E-Mail: rweiskirchen@ukaachen.de 1.41 Promoter regulation of the miR-29a/b1 gene by transforming growth factor-b in hepatic stellate cells and in hepatoma cells Huang J1, Amer W1, Dienes HP1, B!ttner R1, Odenthal M1 1 University of Cologne, Institute for Pathology, Cologne, Germany Introduction: The members of the miR-29 family, targeting genes involved in apoptosis and gene methylation, are downregulated during hepatocarcinogenesis. Furthermore, in hepatic stellate cells (HSC) they inhibit extracellular matrix formation and are markedly reduced during fibrogenesis and after exposure to TGF-b. Since in both, liver fibrogenesis and carcinogenesis, TGF-b is a central mediator, we studied miR-29 promoter regulation by TGF-b in hepatic stellate and hepatoma cells as representative cell types for hepatic fibrosis and cancer. Methods: Primary and mature miR-29 transcripts were quantified in HSC and hepatoma cells after TGF-b stimulation by Real-Time PCR. Transcriptional miR-29a/b promoter regulation was studied by reporter assays and electrophoresis mobility shift assays (EMSA). Putative binding sites were further characterized by site-specific mutation analyses and transgenic transcription factor activation. Results: Quantification of cellular levels of primary transcripts of the miR-29a/b1 gene in addition to the mature processed forms revealed a pronounced upregulation in TGF-b stimulated hepatoma cells, but a downregulation in HSC. Reporter assays of truncated promoter constructs revealed that the core promoter, including a wide spectrum of putative transcription binding sites, is mainly involved in the TGF-b control. Whereas in HSC miR-29 repression by TGF-b stimulation is mainly affected by Smad binding sites, reporter assays of numerous site-specific mutation constructs as well as binding studies and supershift analyses, confirmed the central function of a Ap1 / Ets-1 binding region in TGF-b mediated miR-29 induction in liver cancer cells. Conclusion: miR-29a/b gene is controlled by a complex signaling network, in which Ets/Ap1 binding alteration is crucial for transcriptional induction in hepatoma cells. Corresponding author: Odenthal, Margarete E-Mail: m.odenthal@uni-koeln.de 1.42 Reconstruction and quantification of periportal bile ducts and Hering canal after bile duct ligation Vartak A1, Richter B2, Dahmen U2, Dirsch O3, Hengstler JG1, Hammad S4 1 Leibniz Research Centre for Working Environment and Human Factors (IfADo), TU Dortmund University, Dortmund-Germany, Systems Toxicology, Dortmund, Germany; 2Friedrich-Schiller-University Jena, Experimental Transplantation Surgery, Department of General, Visceral and Vascular Surgery, Jena, Germany; 3Institute for Pathology, University Hospital of Jena, Jena, Germany; 4 Faculty of Veterinary Medicine, South Valley University, Qena-Egypt, Deptartment of Forensic Medicine and Veterinary Toxicology, Qena, Egypt Introduction: Bile duct ligation (BDL) is commonly used to study cholestasis and periportal fibrosis. Despite extensive studies, the spatial- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York temporal organization of the biliary tree in BDL remains unclear. Methods: To analyze and quantify the biliary tree after BDL, C 57Bl/ 6N mice underwent BDL or sham operation and were observed for 6 hours to 28 days (n = 6/group). At predefined time-points (6 h, 1 d, 3 d, 5 d, 7 d, 14 d and 28 d), blood and liver samples were collected for analysis of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) to assess hepatic parenchymal injury and alkaline phosphatase (AP) activities as well as bilirubin for biliary damage. Liver samples were subjected to routine histology and confocal microscopy. Confocal 3D-reconstructions were performed for periportal bile ducts and their links to lobular bile canaliculi. Immunostaining was performed combining antibodies directed against DPPIV/CD26 to visualize the bile canaliculi and the apical membrane of the bile ducts, anti-keratin19 (KRT19) to stain the bile duct epithelial cells, glutamine synthetase to identify the pericentral region of the lobules, anti-donkey mouse IgG which served as an immunoglobulin binds to the sinusoidal endothelial cells thereby visualizing sinusoids. Hepatocyte nuclei were counter stained by DAPI. Results: BDL caused damage to hepatic parenchyma and biliary epithelia cells, as indicted by a significant substantial elevation of transaminases and AP, which peaked on POD28. Histopathological examination of the liver revealed that the fraction of BrdU positive bile duct cells at day 3, 5 and 7 increased in BDL livers with a peak on POD3 compared to shamoperated livers. Morphometric analysis revealed that the total number of bile duct cells per periportal field significantly increased by days 7, 14 and 28 in BDL but peaked a little later. Confocal microscopy revealed that the periportal bile ducts showed extensive branching and increased diameter in BDL mice as compared to sham operated mice. The average numbers of Hering canals occurring per unit length of the bile duct were significantly decreased at days 14 and 28 after BDL. Conclusion: Bile duct ligation leads to biliary tree damage, thus initiating a regenerative response which is culminated in a maximal hepatobiliary cell proliferation 3 days post BDL. Increased hepatobiliary cell proliferation likely manifest as a general enlargement of the biliary tree through enhanced branching and dilation of the ducts. References: Hammad S. et al. (2014) Protocols for staining of bile canalicular and sinusoidal networks of human, mouse and pig livers, three-dimensional reconstruction and quantification of tissue microarchitecture by image processing and analysis. Arch Toxicol 88:1161 – 83. Corresponding author: Hammad, Seddik E-Mail: el-kariem@ifado.de 1.43 Regulation der Expression von MMPs und TIMPs nach Transplantation von mesenchymalen Stammzellen im Rattenmodell der chronisch-toxischen Lebersch!digung Schwill F1, Brueckner S2, Roderfeld M1, Tschuschner A1, Zipprich A3, Roeb E1, Christ B2 1 Justus-Liebig-Universit$t, Gastroenterologie, Medizinische Klinik II, Gießen, Deutschland; 2Universit$t Leipzig, Klinik und Poliklinik f!r Viszeral-, Transplantations-, Thorax- und Gef$ßchirurgie, Leipzig, Deutschland; 3Martin-LutherUniversit$t, Universit$tsklinik und Poliklinik f!r Innere Medizin I, Halle-Wittenberg, Deutschland *geteilte Erstautorenschaft Einleitung: Eine akute oder chronische Lebersch"digung f!hrt durch die vermehrte Bildung von extrazellul"rer Matrix zur Leberfibrose. Matrixmetalloproteinasen (MMPs) und ihre spezifischen Inhibitoren, die Tissue Inhibitors of Metalloproteinases (TIMPs) sind essentiell f!r den Gewebeumbau. Die progressive Leberfibrose f!hrt zu Funktionsverlust und Karzinogenese. Methoden: Ratten wurden nach Standardprotokollen f!r 12 Wochen inhalativ mit CCl4 behandelt. Einer Gruppe (n= 4) wurden systemisch 1,5 Mio hepatogen differenzierte mesenchymale Stammzellen aus Rattenfettgewebe !ber die Schwanzvene injiziert. Die andere Gruppe (n= 4) blieb ohne Zellapplikation. Ratten (n= 4) ohne CCl4-Behandlung stellten die unbehandelte Kontrollgruppe dar. Mittels qRT-PCR haben wir die Expression von MMPs- und TIMPs analysiert und mittels der Delta-Delta Ct Methode quantifiziert. Ergebnisse: Die Behandlung der Tiere mit CCl4 f!hrte im Vergleich zu den unbehandelten Kontrollratten zur signifikanten Ausbildung einer Leberzirrhose. Damit einhergehend war die Expression der folgenden MMPs und TIMPs statistisch signifikant erh#ht: MMP-2, MMP-7, MMP-11, MMP-12, MMP-15, MMP-23, MMP-24, MMP-27, MMP-28, sowie TIMP-1,2,3 und TIMP-4. Erniedrigt war im Vergleich zur Kontrolle die Expression der MMP-16. Die zus"tzliche Behandlung mit mesenchymalen Stammzellen verst"rkte die Expression von MMP-2, MMP-8, MMP-9, MMP-11, TIMP-3 und TIMP-4 weiter !ber die in Tieren ohne Zellapplikation hinaus. allerdings war die Expression von MMP-3 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen signifikant vermindert, Die Expression von MMP-16 und MMP-19, die durch die CCl4-Behandlung erniedrigt waren, wurden durch die Stammzellen teilweise, jedoch nicht wieder auf Kontrollwerte erh#ht. Schlussfolgerung: Die toxisch induzierte Leberfibrose beeinflusste die Expression verschiedener MMPs und TIMPs, die durch intraven#se Stammzellapplikation verst"rkt oder abgeschw"cht wurde. Dies l"sst den R!ckschluss zu, dass mesenchymale Stammzellen den Umbau extrazellul"rer Matrix beeinflussen k#nnen. Da wir bereits die antifibrotische Wirkung der Stammzellen gezeigt haben, scheint der Mechanismus !ber die Beteiligung von MMPs und TIMPs und deren Regulation durch von den MSC sezernierte parakrine Faktoren zu wirken. Korrespondierender Autor: Schwill, Fabian E-Mail: fabian.schwill@med.uni-giessen.de 1.44 Riboflavin Kinase Inhibitor 1 (RKIP1): A Potential Modifier of Fibrogenesis in Liver and Heart Hall RA1, Kazakov A2, Laufs U2, B"hm M2, Lammert F1 1 Saarland University Medical Center, Department of Medicine II, Homburg, Germany; 2Saarland University Medical Center, Department of Medicine III, Homburg, Germany Background: Recently we observed that long-term administration of carbon tetrachloride (CCl4) induces fibrosis in both liver and heart in the mouse. To dissect common and organ-specific mechanisms of fibrosis, we challenged BXD recombinant inbred lines with CCl4. BXD lines represent a genetic reference population (GRP) that is genetically mosaic but homozygous for all loci. Our aim was to identify potential candidate genes with effects on hepatic and cardiac fibrogenesis. Methods and results: Thirty BXD lines were used as a GRP for genome-wide quantitative trait loci (QTL)-analyses. Fibrosis was induced by CCl4 for six weeks (0.7 ml/kg, 12 i.p. injections). We observed significant differences for hepatic and cardiac fibrosis among the BXD lines and using a genome-wide marker panel, we mapped co-localizing loci linked to collagen accumulation for liver and heart on chromosomes 5 and 18. These QTL were further screened for candidate genes by expression QTL (eQTL)mapping. Hence, gene expression levels (Affy 1.0 ST whole genome arrays) were included into the mapping analysis as quantitative traits. Among all locally regulated quantitative trait genes (cis-QTGs) within the QTL on chromosome 5, Rkip1was identified as major cis-QTG (LRS= 64.6) and further in silico analyses affirmed it as a potential candidate gene. Therefore, we compared fibrosis progression in CCl4-challenged Rkip1-knockout (Rkip-/-) and C 57Bl/ 6N wild-type mice by quantification of collagen accumulation in liver and heart. After six weeks of fibrosis induction, Rkip-/- mice showed significantly less cardiac collagen accumulation (p < 0.05), as assessed by Sirius red staining. However, in the liver hydroxyproline levels were enhanced (p < 0.001) in Rkip-/- mice, and so were Col1a2 expression levels (p < 0.05). Conclusions: This study reveals that CCl4-induced fibrosis is a systemic model that allows comparative analysis of fibrosis mechanisms in liver and heart in genetically identical individuals. Genome-wide analysis of hepatic and cardiac fibrosis identified common and regulatory QTLs of fibrogenesis. Rkip1 deficiency appears to have anti-fibrotic effects in heart but not liver, pointing to organ-specific mechanisms of fibrosis progression. Corresponding author: Hall, Rabea A. E-Mail: rabea.hall@uks.eu 1.45 Specific Endoglin deletion in primary mouse hepatic stellate cells shows a modulation of TGF-b signaling pathways, aggravating liver fibrosis Alsamman M1, Sterzer V1, Trautwein C1, Scholten D1 1 RWTH University Hospital Aachen, Medical Clinic III, Aachen, Germany Background: Hepatic stellate cells (HSCs) are the major source for extracellular matrix (ECM) production in liver fibrosis. TGF-beta and its auxiliary receptor endoglin (ENG, S- and L-Endoglin splicing variants), which is expressed on HSCs, are important cytokines, mediating cellular responses in liver injury. This study analyzes the role of specific Endoglin deletion in primary mice HSCs using Cre-LoxP genetic recombination and the effect of this deletion on stellate cell activation. Methods: HSCs were isolated from ENGflox/flox and GFAPCre-ENGDHSC mice in a two step pronase/collagenase digestion. After FACS sorting cells were activated on plastic surface or stimulated with TGF-beta for 1 and 24 h. Alternatively ENGflox/flox cells were treated with adenoviral CMVCreRSVGFP and RSVGFP (control) expressing vector. Cells were suspended for 24 h after isolation and infected for 48 h with the adenoviral vectors (4000 MOI). Subsequently HSCs as well were stimulated with TGF-beta for 4 and 24 h. TGF-beta downstream signaling was analyzed by western blots and qPCR. Results: Comparison of Alk5-Smad2 / 3 and Alk1Smad1 / 5/ 8 pathways showed downregulation of Smad1 / 5/ 8 in GFAPCre+-ENGDHSC HSCs after activation on plastic surface or TGF-beta stimulation (> 45 %). Moreover GFAPCre+-ENGDHSC HSCs showed less Smad2 / 3 expression. However collagen production was upregulated indication a differential ENG modulation of the Alk5-Smad2 / 3 and Alk1Smad1 / 5/ 8 TGF-beta signaling pathways. Western blot analysis of TGFbeta signaling of adenoviral Cre (AdCre+) treated ENGflox/flox primary HSCs showed an effective downregulation of ENG in AdCre+ treated cells (> 90 %). In the absence of ENG activation of Smad1 / 5/ 8 as well as Smad2 / 3 was downregulated. However PAI-1, a downstream target of Alk5-Smad2 / 3 was increased compared to Id1 (downstream target of Alk1-Smad1 / 5/ 8). Since L-ENG is the predominantely expressed ENG isoform (> 90 %) signaling mainly through Alk1-Smad1 / 5/ 8 and promoting antifibrotic effects, deletion of ENG (S- and L-ENG isoforms) shifts the TGF-beta signaling to the profibrotic Alk5-Smad2/ 3 pathway leading to higher collagen expression and aggravated fibrosis in vivo. Conclusion: Endoglin deficiency in hepatic stellate cells has an effect on the modulation of SMADs pathway signaling in HSCs leading to aggravation of liver fibrosis. Corresponding author: Scholten, David E-Mail: dscholten@ukaachen.de Targeting TGF-b2 in chronic liver diseases 1.46 Dropmann A1, Korhonen H2, Jaschinski F2, Janicot M2, Meindl-Beinker N1, Dooley S1 1 University of Heidelberg, Molecular Hepatology – Alcohol Associated Diseases Department of Medicine II Medical Faculty Mannheim Heidelberg University, Mannheim, Germany; 2Isarna Therapeutics GmbH, Isarna Therapeutics GmbH, Munich, Germany Abstract: Background and aims: Expression and function of TGF-b2 have not been investigated thoroughly in chronic liver disease (CLD) progression and HCC. Upon providing further evidence that TGF-b2, like TGF-b1 plays a putative role in fibrogenesis, we now aim to selectively target TGF-b2 expression or both, TGF-b2 and TGF-b1 together using antisense oligonucleotides (AONs) for attenuation or even blockage of human liver disease progression. Methods: For our study three CLD mouse models (CCl4, BDL & Mdr2-/-) were investigated representing different types of CLD background. TGF-b2 expression was compared to TGF-b1 expression by quantitative realtime (qRT)-PCR. In vivo, we selectively inhibited TGF- b2 using AONs. In detail, for induction of chronic liver damage, 12 weeks old mice were injected intraperitoneally (i.p.) with 0,2 ml/kg BW CCl4 twice per week for four weeks. After 2 weeks, subcutaneous AON application started parallely with a dosage of 30 mg/Kg twice per week. In the MDR2-KO mouse model the AON was administered for 4 weeks. The effect and efficacy of AON treatment was evaluated on protein and mRNA level. Typical fibrotic markers are currently investigated using qRT-PCR. Results: In the CCl4 liver injury and regeneration model expression levels of both TGF-b isoforms were equal. Further, HSC activation and collagen expression was accompanied with transient increases of TGF-b2 expression. Samples of Mdr2-KO mice showed frequent TGF-b2 upregulation within 3 to 15 month as compared to wild types. Accordingly, an elevation of TGF-b2 expression was determined within a time course of 14 days after bile duct ligation (BDL). Interestingly, induction of TGF-b2 was about 10-fold stronger as compared to TGF-b1. Immunohistological assessment of in vivo AON distribution after 24 h and 5 days revealed strongest signals in the liver and kidneys. Hydroxyproline content was significantly reduced in injured AON-treated animals compared to controls. Sirius Red staining revealed a significant reduction (~34 %) of collagen deposition in AONtreated mice. Discussion/Conclusion: Taken together, our results indeed suggest a role of TGF-b2 in the process of CLD. We further conclude that in vivo application of TGF-b2 directed AON to CLD mouse models attenuate fibrogenesis. Further studies are currently performed to determine mechanistic details of AON effects and define specifications of a potential AON based treatment of CLD, e.g. dosage and stage of disease, when application is feasible. Corresponding author: Dropmann, Anne E-Mail: Anne.dropmann@medma.uni-heidelberg.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A15 A16 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 1.47 The extracellular proteinase Expi/Wfdc18 in liver damage and tumour development: A new connection between inflammation, fibrogenesis and malignant growth Liebe R1, Hall R2, Burgermeister E1, Ebert M1, Lammert F2, Dooley S1 1 University of Heidelberg, Department of Medicine II, Medical Faculty Mannheim, Mannheim; 2Saarland University Hospital, Department of Medicine II, Homburg, Germany Introduction: Recently we have identified quantitative trait loci (QTLs) that determine susceptibility to TGF-beta signalling in mouse hepatocytes in vitro and fibrogenesis in vivo (Liebe et al. Physiol Genomics 2013). Expi/Wfdc18 candidacy was identified by eQTL and DNA variant analyses. Expi/Wfdc18 knockout animals showed decreased hepatic collagen contents following 6 weeks of CCl4 challenge. Methods: To assess the function of Expi outside its normal role in mammary gland development and antibacterial defence in salivary glands, we performed an in silico analyses of Expi/Wfdc18 expression and a systematic search for pathobiological roles of WFDC molecules. Results: GEO microarray data revealed TLR9-mediated induction of Expi/Wfdc18 in RAW 264.7 macrophages by unmethylated CpG (Tross et al. J Immunol 2009). The adjacent Wfdc17/AMWAP peptide (70% amino acid identity) is a negative regulator of macrophage activity in microglia with antibacterial activities (Karlstetter et al. J Immunol. 2011). Expi/Wfdc18 was overexpressed 6to 20-fold in adenomas from ApcMin/+ mice (Reichling et al. Cancer Res 2005) and increased 4-fold in ErbB2 /Neu positive mammary tumours compared to normal control tissue (Landis et al. Oncogene 2005). In humans, WFDC 2/HE4 is a serum marker for ovarial and endometrial tumours as well as gastric and pancreatic carcinoma, and has recently been described as a fibroblast-derived mediator of fibrosis in kidney (LeBleu et al. NatMed 2013). Conclusions: Expi/Wfdc18 increases hepatic fibrogenesis following chronic CCl4 challenge in the mouse. Its expression is induced by TLR9 ligand CpG dinucleotide in macrophages. We conclude that Expi/Wfdc18 is an alarm peptide involved in the TLR9mediated innate defence against invading microbial pathogens and primes liver cells for pro-apoptotic signals. Expi/Wfdc18 is ectopically overexpressed in murine gastrointestinal and mammary tumours. We suspect that Wfdc18/Expi may play a similar role as WFDC 2/HE4. The Expi/Wfdc18 knockout mouse represents a new animal model to study the impact of the innate immune system on fibrogenesis and malignant growth. Corresponding author: Liebe, Roman E-Mail: Roman.Liebe@medma.uni-heidelberg.de 1.48 The pluripotency involved factors, Lin28 and Notch1 are targets of neuronal miRNAs in hepatic stellate cells Huang J1, Macheleidt I1, Perrech M2, Noetel A1, Dienes HP1, Hescheler J2, B!ttner R3, Saric T2, Odenthal M3 1 University of Cologne, Institute for Pathology, Cologne, Germany; 2University of Cologne, Department of Physiology, Cologne, Germany; 3University of Cologne, Center of Molecular Medicine, Cologne, Germany Background and Aim: Myofibroblastic hepatic stellate cells (HSC) are the central cell types of liver fibrosis due to their excessive matrix production. By deep sequencing of the Ago2 interacting transcriptome we have demonstrated that neuronal miR-9, miR-125b, miR -128 are involved in regulation of chemokine signaling during myofibroblastic HSC activation (Noetel et al., 2013). In the present study, we aimed to analyse further putative targets of the Ago2 neuronal miRNA complex, namely Notch1, KLF4, and Lin28. Methods: Notch1 and Lin28 gene expression was quantified in primary rat HSC cultures by real time PCR. 3’UTR sites of Notch1 and Lin28 transcripts, putatively targeted by neuronal miR-9, miR-125b, miR-128, were cloned downstream to a luciferase reporter gene and used for reporter assays in myofibroblastic HSC treated with miRNA mimics or with scrambled miRNA. Notch1 and Lin28 were overexpressed by lentiviral vector transduction and the influence on HSC was determined by expression profiling using PCR arrays. Results: Since the pluripotency involved factors, Notch1 and Lin28 were suggested to be targets of posttranscriptional neuronal miRNA repression, we investigated the expression of these mediators during myofibroblastic HSC transition. Whereas the neuronal miRNAs miR-9, miR-125b, and miR-128 were highly increased, the putative targets Notch-1 and Lin28. Next, we analysed the 3-’UTR of Notch-1 and Lin28 Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York transcripts for putative binding sites of the three neuronal miRNAs. Reporter assays of the luciferase constructs, harboring the putative 3’UTR sites of Notch1, KLF4, and Lin28 mRNA in comparison to the corresponding mutants definitively demonstrate the inhibitory interaction of all neuronal miRNAs to Lin28 and Notch. Furthermore, neuronal miRNA overexpression in HSC resulted in a prominent decrease of Notch1 and Lin28. In order to proof the impact of the neuronal miRNA Notch1 axis, lentiviral overexpression was performed. Expression profiling of Notch1 overexpressing cells revealed that members of the Notch signaling pathway were highly upregulated whereas some fibrogenic mediators are downregulated. Importantly the receptors and ligands of the chemokine family were highly effected by Notch signalling. Conclusion: Upregulation of neuronal miR-9, miR-125b, and miR-128 during myofibroblastic transition and the identified interaction with factors involved in pluripotency and cell differentiation suggests a prominent role of these miRNAs in HSC differentiation and activation during fibrosis. Corresponding author: Odenthal, Margarete E-Mail: c0d1953e@opayq.com 1.49 The vicious circle of prostaglandin- and cytokine-dependent hepatic insulin resistance: a key role of prostaglandin E2 Henkel J1, Lieske S3, Camargo RG1, Schanze N1, Sauer I2, Birkenfeld AL3, P!schel GP1 1 University of Potsdam, Institute of Nutrition, Department of Nutritional Biochemistry, Nuthetal, Germany; 2Charit#, General, Visceral, and Transplantation Surgery, Campus Virchow Klinikum, Berlin, Germany; 3Charit#, Department of Endocrinology, Diabetes and Nutrition, Center for Cardiovascular Research, Berlin, Germany Background & aims: Hepatic insulin resistance and the ensuing impairment of hepatic glucose metabolism is a major contributor to hyperglycemia in metabolic syndrome and type II diabetes. In patients suffering from these ailments, a low-grade inflammation prevails besides an impaired fatty acid handling. Both contribute to the development of insulin resistance. While the impact of fatty acids and pro-inflammatory cytokines on the insulin signalling cascade are well established, the role of small lipid mediators like prostaglandins, which are released from resident liver macrophages and infiltrating immune cells, is not well characterized. The current study addressed this question. Material & Methods: Male C 57BL/ 6 mice were fed chow or a modified western diet containing high fat, cholate and cholesterol as well as high fructose in drinking water. Human macrophages (cell line U937) or primary mouse macrophages were incubated with LPS or PGE2. Human or primary rat hepatocytes were pre incubated either with PGE2, IL 6, OSM or with conditioned media of PGE2-stimulated macrophages and subsequently stimulated with insulin. Gene expression and activation of insulin- and cytokine signalling were quantified by westernblot and RT qPCR. Results: Hepatic expression of key enzymes in prostaglandin E2 (PGE2) formation, namely cyclooxygenase 2 (COX2) and microsomal PGE2 synthase 1 (mPGES1), was induced 2 to 4-fold in mice fed a modified western diet suggesting an enhanced capacity for local PGE2 formation in these mice. In primary human and rat hepatocytes PGE2 interrupted Akt-dependent insulin signalling. It enhanced hepatic lipid accumulation by inhibiting hepatic lipid utilisation. The underlying molecular mechanisms involved a PGE2-mediated sustained ERK1/ 2 kinase activation, which resulted in an inhibitory serine phosphorylation of IRS. PGE2 acted synergistically with IL-6 or OSM, which attenuated insulin signalling by inducing SOCS3. In mouse and human macrophages the production of these cytokines was stimulated by PGE2. While PGE2 enhanced IL-6, OSM and IL-1b formation, TNFa expression remained unchanged or was reduced. Cytokines and PGE2 induced the PGE2-generating enzymes COX2 and mPGES1. Conditioned medium of murine or human macrophages treated with PGE2 stimulated the phosphorylation of STAT3 and induced SOCS3 in hepatocytes, while insulin-dependent glucokinase induction was attenuated. These effects were abolished after parallel incubation with an OSM-neutralizing antibody or treatment of macrophages with the COX2-inhibitor indomethacin. Conclusion: In addition to directly interrupting insulin signalling pathway in hepatocytes, PGE2 may further impair hepatic insulin sensitivity in an autocrine feed-forward vicious cycle by inducing cytokines like OSM and its own synthesis in macrophages. The enzymes involved in the PGE2 synthesis might therefore be potential new drug targets for the treatment of hepatic insulin resistance. Corresponding author: Henkel, Janin E-Mail: jhenkel@uni-potsdam.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 1.50 UDCA-LPE modulates different signaling pathways involved in hepatic fibrogenesis 1 1 1 1 Su J , Chamulitrat W , Stremmel W , Pathil A 1 University of Heidelberg, Department of Internal Medicine IV, Gastroenterology and Hepatology, Heidelberg, Germany Background: Liver fibrosis with deposition and remodeling of extracellular matrix (ECM) is regulated.by different signaling pathways. Ursodeoxycholyl Lysophosphatidylethanolamide (UDCA-LPE) is a synthetic bile acid-phospholipid conjugate with hepatoprotective and anti-fibrotic functions in vitro and in vivo. In this study we aim to elucidate signaling pathways, which mediate anti-fibrogenic action of UDCA-LPE. Results: At membrane level ECM interacts with integrin receptors, which promotes pro-fibrogenic signaling. Focal Adhesion Kinase (FAK) and SRC play a central role in integrin signaling. After phosphorylation in response to integrin engagement, FAK and SRC kinase mediate activation of myofibroblasts. After UDCA-LPE treatment, p-FAK (Tyr 925 and Tyr 576/ 577) and p-SRC (Tyr416) are reduced in CL48 liver cells. The reduction of p-FAK and p-SRC is time dependent. The second messenger cAMP and cAMP dependent Protein Kinase A (PKA) can also suppress ECM production by inhibiting hepatic stellate cells differentiation. We determined PKA activity by using the antibody for PKA substrates (RRXS*/T*). PKA is activated 1 minute after UDCA-LPE treatment with a peak after 15 min. Phosphorylation of ERK, B-RAF and C-RAF by UDCA-LPE was also investigated by western blot. UDCA-LPE induced pERK (Thr 202 /Tyr 204) after 1 minute, the activation maximized at 15 min and lasted more than 2 hours. ERK is phosphorylated by MEK, which is mediated by BRAF and C-RAF in CL48 cells. UDCA-LPE induced pB-RAF (Ser 445) and pC-RAF (Ser 338) after 1 minute. We next investigated the crosstalk between FAK, ERK and PKA signaling pathways. FAK autophosphorylation inhibitor Y15 significantly increased the phosphorylation of ERK. After Y15 treatment phosphorylation of ERK became less sensitive to UDCA-LPE and activation of C-RAF by UDCA-LPE was inhibited. These results suggest that activation of C-RAF and ERK by UDCA-LPE is dependent on FAK inhibition. EGFR inhibitor AG1478 also reduced UDCA-LPE mediated accumulation of pERK and inhibited C-RAF phosphorylation, suggesting activation of C-RAF and ERK by UDCA-LPE is EGFR dependent. PKA inhibitor Rp-cAMP reduced pERK and inhibited B-RAF phosphorylation, suggesting activation of B-RAF and ERK is PKA dependent. Conclusions: UDCA-LPE disturbs pro-fibrogenic integrin signaling by inhibiting FAK and SRC activity. FAK inhibition was identified as an upstream event of activation of the EGFR/C-RAF/ERK pathway. UDCA-LPE further activates PKA, which subsequently induces B-RAF/ERK signaling. By inhibiting pro-fibrogenic pathways with concomitant activation of pro-proliferative ERK signaling, UDCA-LPE may improve hepatofibrogenesis and accelerate liver regeneration. Corresponding author: Pathil, Anita E-Mail: Anita.Pathil-Warth@med.uni-heidelberg.de 1.51 Verst!rkte hepatische Expression neuer MicroRNA bei ABCB4-/- M!usen im Langzeitmodell W!rger T1, Churin Y1, Roderfeld M1, Roeb E1 1 Justus-Liebig-Universit$t Gießen, Gastroenterologie, Gießen, Deutschland Einleitung: MicroRNA spielen in der Aufrechterhaltung der Leberhom#ostase und in der Modulation verschiedener pathologischer Prozesse, welche mit einer Lebersch"digung assoziiert sind, eine bedeutende Rolle. Ziel der vorliegenden Studie war die Untersuchung der MicroRNAExpression in der Leber von Mausmodellen f!r die sklerosierende Cholangitis, die &berexpression des großen Hepatitis B Virus (HBV)-H!llproteins sowie einem Kombinationsmodell (Hybridm"use). Methoden: Zun"chst wurden 92 MicroRNA in der Leber von 16 Wochen alten HBV+/–ABCB4-/-Hybrid-M"usen mittels miFinder-MicroArray (Qiagen!) analysiert. Als Kontrolle wurde MicroRNA von entsprechenden transgenen M"usen, Knock-out M"usen und Wildtypen verwendet. Nach Auswertung der Array-Analysen wurden ausgew"hlte MicroRNA mittels qPCR in der Leber von 8, 16, 26 sowie 52 Wochen alten M"usen verifiziert. Ergebnisse: Die Array-Analyse ergab eine mehr als zweifache Hochregulation bei folgenden MicroRNA: miR-34c-5 p, 182 – 5 p, miR-214 – 3 p, miR-141 – 3 p, miR-411 – 5 p, miR-27a-3 p, miR-125b-5 p, miR-199a-5 p, miR-199a-3 p, miR-96 – 5 p, miR-15b-5 p sowie miR-16 – 5 p. In der anschließenden quantitativen Real-Time-PCR konnten diese Ergebnisse in ABCB4-/- M"usen best"tigt werden. In HBVtransgenen M"usen (Churin 2014) hingegen zeigte sich keine signifikante (nderung der MicroRNA-Expression. Schlussfolgerung: Die vorlie- gende Studie zeigt, dass neben den bislang bekannten MicroRNA im Rahmen einer spezifischen Lebersch"digung (ABCB4-/-) noch weitere bisher nicht mit Lebersch"den assoziierte MicroRNA in ihrer Expression ver"ndert werden. Insgesamt k#nnen diese neuen Befunde beitragen, die Pathogenese cholestatischer Lebererkrankungen zu verstehen und therapeutische Optionen zu erarbeiten. Literatur: Churin Y, Roderfeld M, Stiefel J, W!rger T, Schr#der D, et al. (2014) Pathological Impact of Hepatitis B Virus Surface Proteins on the Liver Is Associated with the Host Genetic Background. PLoS ONE 9(3): e90608. Korrespondierender Autor: W!rger, Tilman E-Mail: tilman.wuerger@googlemail.com 1.52 Y-box-binding protein (YB-1) in murine models of hepatic and renal fibrosis Weiskirchen R1, Hermert D2, Alidousty C2, Ostendorf T2, Floege J2, Raffetseder U2 1 RWTH University Hospital Aachen, Institute of Molecular Pathobiochemistry, Experimental Gene Therapy and Clinical Chemistry, Aachen, Germany; 2RWTH University Hospital Aachen, Department of Clinical Immunology and Nephrology, Aachen, Germany Background: The Y-box binding protein-1 (YB-1) exerts pleiotropic functions in gene transcription and in translation, e.g. of fibrosis-related genes. Recent in vitro findings point to opposite regulatory effects on fibrogenesis by YB-1 that depend on its subcellular localization. YB-1 might even accomplish opposite functions on gene transcription and mRNA translation of the same gene product, e.g. that of type I collagen (Col1A), a major constituent of the extracellular matrix (ECM) [1]. This led us to in vivo investigations that analyze the outcome of half-maximal YB-1 depletion in a model of liver fibrosis (bile duct ligation (BDL)) and compared the results to renal fibrosis, investigated by unilateral ureteral obstruction (UUO). Additionally, the impact of BDL on kidney damage was assessed. Material and Methods: BDL (for 2 weeks) and UUO (for 5 days) was performed in wildtype (wt) and heterozygous YB-1 knockout (Yb-1+/-) mice that are characterized by half-normal YB-1 content on mRNA and protein level [2,3]. YB-1-/- mice are not viable. Parameters of hepatic and renal fibrosis were determined by serum parameters, IHC, qRT-PCR and Western blot analyses. Comparative reporter gene expression studies were performed in primary hepatic cells isolated from Yb-1+/- and wt mice. Results: Hepatic serum parameters (e.g. alkaline phosphatase, ALT) and expression of ECM proteins such as type I collagen (Col1A) were significantly reduced in Yb-1+/- compared to wt mice. Col1A promoter activation in primary wt hepatocytes following TGF-b challenge was weak and further diminished when cells were obtained from Yb-1+/- mice. In line with this, half-maximal expression of YB-1 resulted in a significant protection against renal fibrosis (UUO). However, the strong BDL-induced damage that was observed in kidneys (expression of renal damage marker KIM-1 and the tubular damage score was elevated 4-fold) was not reduced in Yb-1+/- mice. Conclusions: In summary, we demonstrate that YB-1 crucially contributes to hepatic and renal fibrosis, however not to the organ crosstalk between liver and kidney herein. References cited: [1] Hanssen et al. Ybox binding protein-1 mediates profibrotic effects of calcineurin inhibitors in the kidney. J Immunol. 2011;187:298 – 308. [2] Hanssen et al. YB1 is an early and central mediator of bacterial and sterile inflammation in vivo. J Immunol. 2013 191:2604 – 13. [3] Raffetseder et al. Extracellular YB-1 blockade in experimental nephritis upregulates Notch-3 receptor expression and signaling. Nephron Exp Nephrol. 2011;118:e100 – 8. Corresponding author: Weiskirchen, Ralf E-Mail: rweiskirchen@ukaachen.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A17 A18 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 1.53 Zusammenhang der zirkulierenden miRNA-122 Spiegel mit der portalen Hypertension bei HIV/ HCV-positiven Patienten Jansen C1, Reiberger T2, Schierwagen R1, Mandorfer M2, Anadol E1, Schwabl P2, Wasmuth JC1, Strassburg CP1, Rockstroh J1, Peck-Radosavljevic M2, Odenthal M3, Trebicka J1 1 University of Bonn, Department of Internal Medicine, Bonn, Germany; 2Medical University of Vienna, Division of Gastroenterology and Hepatology Department of Internal Medicine III, Vienna, Austria; 3University of Cologne, Pathology, Cologne, Germany Hintergrund: Die Behandlung von HIV-infizierten Patienten mit cART verbesserte das &berleben dieser Patientengruppe, w"hrend gleichzeitig die leberassoziierten Todesf"lle anstiegen. Insbesondere bei Patienten mit HIV/HCV-Co-Infektionen ist die Fibrose und die portale Hypertension haupts"chlich verantwortlich f!r die leberassoziierte Morbidit"t und Mortalit"t. Zirkulierenden miRNA-122 ist bei Patienten mit einer HIV/ HCV-Co-Infektionen erh#ht und korreliert mit dem vorliegen einer Lebersch"digung und Fibrose. Allerdings ist ein Zusammenhang mit dem Grad des portalen Hypertonus noch nicht beschrieben. Methoden: 77 Patienten (30 % weiblich) mit einer HIV/HCV-Co-Infektion wurde eingeschlossen. Der Lebervenendruck-Gradient wurde in 55, das Fibrosestadium durch FibroScan bei 52 Patienten bestimmt. miRNA-122 wurde im peripheren Blut mittels quantitativer Polymerase-Kettenreaktion (qPCR) mit anschließender Normierung durch SV-40 analysiert. Ergebnisse: Das durchschnittliche Alter der Patienten betrug 37 mit einer Spannbreite von 19 bis 63 Jahren. 11 Patienten wiesen im FibroScan eine F0 /F1 Fibrose auf, 36 Patienten eine F2 /F3 und 5 Patienten zeigte eine F4-Fibrose. Es zeigte sich, wie bereits beschrieben, eine starke Korrelation zwischen dem Lebervenendruck-Gradienten und dem Fibrosestadium gemessen mittels FibroScan (Rs= 0.689; p = 1.47*10 – 7). Die Spiegel der zirkulierendem miRNA-122 zeigten signifikante Korrelationen mit Alanin-Aminotransferase (Rs= 0,383, p = 0,003) und damit mit der Leberfunktionsst#rungen. Weiterhin zeigte miRNA-122 eine signifikante inverse Korrelation mit dem Lebervenendruck-Gradienten (Rs=-0,302, p = 0,03). Schlussfolgerung: miRNA-122 weist eine signifikante inverse Korrelationen mit dem Lebervenendruck-Gradienten, sowie eine direkte mit der Leberfunktionsst#rung auf. Diese Daten best"tigen unsere fr!heren Beobachtungen, dass bei Leberfibrose die miRNA-122 Spiegel im Verlauf der Erkrankung abfallen. Korrespondierender Autor: Jansen, Christian E-Mail: Christian.Jansen@ukb.uni-bonn.de 2. Clinical Hepatology 2.1 A common polymorphism of tumor necrosis factor receptor-associated factor 6 (TRAF6) is associated with an increased risk for spontaneous bacterial peritonitis Mai M2, Stengel S1, Al-Herwi E1, Reuken P1, Stallmach A1, Bruns T1 1 Jena University Hospital, Internal Medicine IV, Jena, Germany; 2Jena University Hospital, Center for Sepsis Control and Care, Jena, Germany Background: Spontaneous bacterial infection (SBP) is a frequent complication of decompensated cirrhosis contributing to high mortality rates exceeding 60 % per year. Monocytes and peritoneal macrophages are potential cellular immune regulators in SBP exhibiting pattern-recognition-receptors (PRR) to detect bacterial infections. In this context, tumor necrosis factor receptor-associated factor 6 (TRAF6) is a critical mediator in PRR signaling. Aims: We hypothesized that genetic polymorphisms of TRAF6 are associated with an increased risk of SBP by modulating monocytic immune responses in patients with decompensated cirrhosis. Methods: TRAF6 haplotype-tagging single nucleotide polymorphisms (SNPs) rs331457 (G/A) and rs5030419 (C/G) were determined by Fluorescence Resonance Energy Transfer/Melting Curve analysis in 404 prospectively characterized hospitalized patients with decompensated cirrhosis who underwent diagnostic paracentesis at the Jena University Hospital. Episodes of SBP were identified from electronic records. We investigated the expression of TRAF6 mRNA by real-time reverse transcription polymerase chain reaction (qRT-PCR) in immunomagnetically isolated monocytes and peritoneal macrophages. IL-6 secretion of these cells was quantified by Enzyme Linked Immunosorbent Assay (ELISA) 24 hours after stimulation with 10 ng/ml lipopolysacchar- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York ide (LPS). Results: The minor allele frequency for rs331457 was 16.5 % and 14.4 % for rs5030419. 193 (48 %) patients presented the TRAF6 wildtype (GGCC), 113 (28%) were carriers of the rs5030419 mutation (AGCG; GGCG; GGGG) and 98 (24%) were carriers of a haplotype indicated by the rs5030419 wild-type and the rs331457 mutation (AGCC; AACC). 117 (29%) patients had at least one episode of SBP. Patients carrying the AGCC/AACC genotype had an increased risk of SBP (OR 1.93; 95 % CI 1.20 – 3.12; p = 0.007) compared to patients not carrying this variant, which remained significant after adjustment for sex, age and MELD score. However, TRAF6 mRNA expression in monocytes and peritoneal macrophages and secretion of IL-6 after TLR4 stimulation in vitro did not differ significantly between the investigated haplotypes. Conclusion: A common variant in TLR signaling is associated with an increased risk of SBP in patients with decompensated cirrhosis, which may be employed for genotype-based primary prophylaxis. The biological mechanism underlying the clinical association is subject of our current studies. Corresponding author: Bruns, Tony E-Mail: Tony.Bruns@med.uni-jena.de 2.2 Prevalence of hyperdynamic circulation in cirrhosis: lack of association to presence and severity of ascites Ripoll C1, Hohaus P1, Hollenbach M1, Greinert R1, Zipprich A1 1 Martin-Luther University Halle-Wittenberg, University Hospital of Halle, Internal Medicine I, Halle (Saale), Germany Patients with cirrhosis develop hyperdynamic circulation with an increase in cardiac output (CO) and a decrease in systemic vascular resistance (SVR). Patients with hyperdynamic circulation can develop circulatory dysfunction(CD) when this compensatory mechanism is insufficient. Although this takes place theoretically in decompensated patients, namely in patients with ascites, its prevalence has never been specifically analysed. The aim was to evaluate the prevalence of hyperdynamic circulation in patients with compensated and decompensated cirrhosis and it association to liver function, portal hypertension and CD. Methods: Secondary analysis of a prospectively collected dataset of patients with cirrhosis who underwent a hepatic hemodynamic study and right heart catheterization. SVR and CO were categorized according to the presence of abnormal values (below 800 dyn.cm.s5 and above 8 l/m, respectively). Hyperdynamic circulation was defined when both parameters were abnormal. CD was defined by the presence of creatinin > 1.5 mg/dL and/or hyponatremia < 130 mmol/L. Variables are reported as percentages or medians(IQR). Comparison were performed by means of U-mann Whitney and ANOVA. Kaplan-Meyer curves were constructed and compared with the log rank test. Results: 437 patients were included (65% male, 71% had alcohol related disease, Child A 102 (23 %), B 182 (42%), and C 130 (30 %), 57 % with ascites (n= 249) and 30 % with refractory ascites (n= 130). 22 % had hyperdynamic circulation, interestingly 18% of patients without ascites and 25 % of patients with ascites had hyperdynamic circulation. Patients with hyperdynamic circulation had greater HVPG [18 (13 – 20) mm Hg vs. 16 (11 – 19) mm Hg](p = 0.007) although no difference in creatinin and serum sodium were observed compared to patients without hyperdynamic circulation. Among patients with ascites, no difference in the prevalence of hyperdynamic circulation was observed according to the presence of diuretic responsive (26 %) or refractory ascites (23 %). CD was observed in 20 % of patients, most frequently in patients with refractory ascites (61 %). No association was observed between the presence of hyperdynamic circulation and CD. Patients with CD had greater HVPG [19 (16 – 21) mm Hg vs 15 (11 – 19) mm Hg](p < 0.001) and lower SVR [834 (683 – 1057) dyn.cm.s-5 vs. 938 (751 – 1182) dyn.cm.s-5] (p = 0.006), nevertheless no differences in CO [6.9 (5.6 – 8.4) l/min vs. 6.7 (5.7 – 8.3) l/min] were observed. Conclusions: Approximately 25 % of patients with cirrhosis have hyperdynamic circulation, irrespective of ascites. CD is associated to refractory ascites. Patients with CD have lower SVR, without differences in CO. Corresponding author: Ripoll, Cristina E-Mail: cristina_ripoll@yahoo.es 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 2.3 Eligibility and safety of sofosbuvir in a real-world single center cohort of patients with advanced cirrhosis, including decompensated cirrhosis Christoph HzS1, Deterding K1, Port K1, Maasoumy B1, Manns MP1, Heiner W1, Cornberg M1 1 Hannover Medical School (MHH), Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany Background: With the approval of sofosbuvir (SOF) effective treatment with and without interferon has become available. We aim to assess the eligibility and safety of a SOF based therapy in patients (pts) with primarily advanced liver cirrhosis, including decompensated cirrhosis, in a real world setting. Methods: 207 patients have been evaluated in our outpatient clinic since the approval of SOF in January 2014. Reasons for eligibility for therapy as well as reasons for non-treatment were assessed. In 84 patients, primarily with advanced cirrhosis, including 15 patients with Child B and C cirrhosis, therapy was commenced. So far, safety data of the first 8 weeks is available and has been analysed for serious adverse events. Results: Of the 207 evaluated patients, 25 patients did not receive treatment due to safety reasons (12%). Common causes have been severe concomitant cardiac disease (7 pts, 3.4 %), advanced renal disease (5 pts, 2.4 %), need for other urgent procedures (i.e. treatment of varices, 5 pts, 2.4 %) or ongoing drugs abuse (4 pts, 1.9 %). Autoimmune disease, (severe) thrombopenia, anemia or hepatic dysfunction did not prevent treatment in any case. The most common cause for non-treatment has been lack of urgency in patients without severe liver disease and the option to receive interferon-free DAA combination in 2015 (79 pts, 38%). 84 pts have started treatment. At baseline, 73 pts (87%) had a degree of fibrosis of F3 or higher (METAVIR-Score). 15 pts had decompensated cirrhosis (Child B or C cirrhosis). 31 pts (37%) had a platelet count of less than 9 x 103 /L and 21 (25%) had anaemia at start of treatment (Hb< 13 g/dl). 16 pts received triple therapy (19%), whereas 68 pts commenced treatment with SOF and ribavirin (81 %), mostly owing to interferon intolerance. 12 pts (14.3 %) had to be hospitalized within the first 8 weeks of treatment, primarily due to complications of advanced cirrhosis. In 3 patients treatment was stopped prematurely (1 patients had symptomatic LAD stenosis and was referred for cardiac surgery, 1 patient suffered from gastrointestinal bleeding, 1 patient reported allergic symptoms after the first dose of sofosbuvir and did not return for follow up). All patients on treatment became HCV-RNA negative at week 8. Conclusion: With the approval of SOF, the eligibility for HCV treatment has expanded broadly, including patients with decompensated cirrhosis. Patients with advanced liver cirrhosis have a high risk for hospitalization, but can continue HCV treatment in most cases. Full data will be presented at GASL 2015. Corresponding author: Christoph, H#ner zu Siederdissen E-Mail: hoenerzusiederdissen.christoph@mh-hannover.de 2.4 25-hydroxyvitamin D deficiency is associated with infections and mortality in cirrhosis Finkelmeier F1, Kronenberger B1, Zeuzem S1, Piiper A1, Waidmann O1 1 Goethe University Hospital Frankfurt, Gastroenterology, Frankfurt am Main, Germany Objective: Vitamin D is involved in many biological functions such as proliferation, apoptosis, cellular signaling and anti-inflammation. Recently, an increased incidence of 25(OH)D3 deficiency has been found in subjects suffering from chronic liver diseases and the extent of 25(OH)D3 deficiency in the patients correlated with the severity of liver dysfunction. We hypothesized that low vitamin D levels might be associated with inflammatory responses and infectious complications in cirrhotic patients. Therefore, we performed a prospective cohort study investigating the relation of 25(OH)D3 levels with stages of cirrhosis and mortality as well as the association of 25(OH)D3 concentrations and complications of cirrhosis including infectious complications. Methods: From May 2009 to July 2011, 270 patients with cirrhosis presenting at the Department of Internal Medicine 1 of the Frankfurt University Hospital outpatient clinic were consecutively enrolled into the present prospective cohort study. Patient characteristics, treatment and outcome were entered into a prospectively conducted database. 25-hydroxyvitamin (25(OH)D3) levels were quantified by radioimmunoassay from serum samples obtained at the day of study inclusion. Patients were followed until death or last contact. The primary end point was overall survival (OS). Results: The mean follow-up time was 422 +/- 399 days with a range of 1 – 1382 days. 37 (13.7 %) patients underwent liver trans- plantation and were excluded from further analysis from the day of transplantation. 85 (31.5 %) individuals died within the study. The mean serum 25(OH)D3 concentration was 9.3 € 7.5 ng/ml with a range of 0.9 to 46.1 ng/ml. 180 (66.7 %) patients had very low 25(OH)D3 levels (< 10 ng/ ml) and were classified as insufficient, 66 (24.4 %) patients had low levels (10 – 20 ng/ml) and were classified as deficient. 24 (8.9 %) patients had normal 25(OH)D3 levels (> 20 ng/ml). 25(OH)D3 levels differed significantly between Child Pugh stages and showed a negative correlation with the MELD score. Patients with decompensated cirrhosis had significantly lowered 25(OH)D3 levels. 25(OH)D3 levels significantly differed between patients with infectious complications compared to those without infections and individuals with SBP (spontaneous bacterial peritonitis) had significantly lower 25(OH)D3 levels compared to patients without SBP. Patients with low serum vitamin D had a significantly higher risk for occurrence of MDR (multi-drug resistant) bacteria (HR 2.36). 25(OH)D3 levels £ 6 ng/ml as well as serum 25(OH)D3 concentrations £ 10 ng/ml levels were associated with higher mortality compared to higher 25(OH)D3 levels (HR 1.82 for 6 ng/ml and HR 1.71 for 10 ng/ml, respectively). In a multivariate Cox regression model 25(OH)D3 levels were independently associated with mortality. Conclusion: We conclude, that 25(OH)D3 deficiency is associated with advanced liver disease and it is a prognostic indicator for a poor outcome. Furthermore low vitamin D levels are associated with infectious complications. In conclusion our work adds further evidence that vitamin D might be a factor influencing the prognosis of cirrhotics. Corresponding author: Finkelmeier, Fabian E-Mail: fabian.finkelmeier@kgu.de 2.5 A common FUT2 variant correlates with serum carcinoembryonic antigen levels and affects cancer screening in patients with primary sclerosing cholangitis Wannhoff A1, Folseraas T2, Brune M3, Rupp C1, Friedrich K1, Knierim J1, Weiss KH1, Flechtenmacher C4, Schirmacher P4, Stremmel W1, Hov JR2, Gotthardt DN1 1 University Hospital Heidelberg, Department of Internal Medicine IV, Heidelberg, Germany; 2Oslo University Hospital, Rikshospitalet, Norwegian PSC Research Center, Division of Cancer Medicine, Surgery and Transplantation, Oslo, Norway; 3University Hospital Heidelberg, Department of Internal Medicine I and Clinical Chemistry, Heidelberg, Germany; 4University Hospital Heidelberg, Institue of Pathology, Heidelberg, Germany Primary sclerosing cholangitis (PSC) can be complicated by the development of biliary malignancy as cholangiocarcinoma (CCA) and gallbladder carcinoma (GBCA). Besides the most commonly used serum screening parameter, namely CA19 – 9, screening with serum levels of carcinoembryonic antigen (CEA) is less examined. We thus conducted a study to investigate carcinoembryonic antigen (CEA) as a screening parameter for biliary malignancy in PSC patients. Based upon findings of a recent genome-wide association study that described an association between the genes of fucosyltransferases (FUT) and CEA, we thought to analyze how serum CEA levels were affected by common genetic variants of FUT2 and FUT3. In a retrospective cohort analysis we evaluated CEA levels in 226 PSC patients treated at the University Hospital Heidelberg. Among them were 19 with biliary malignancy. We investigated how FUT2 and FUT3 SNPs affected CEA levels. A receiver operating characteristic (ROC) analysis was performed. Optimal cut-off values for CEA were determined based on Youden’s index. A validation cohortof 240 patients, including 28 with biliary malignancy, treated at the University Hospital Oslo was included. Median CEA concentration was lower in cancer-free patients (1.4 ng/mL, IQR: 0.9 – 2.1) than in cancer patients (2.0 ng/mL, IQR: 1.4 – 3.8, P= 0.014). ROC analysis revealed an area under the curve (AUC) of 0.671 and the optimal cut-off was 3.2 ng/mL. The FUT2 variant rs601338 (G428A) correlated with CEA levels (P < 0.001 according to Kruskal-Wallis test): Median CEA values according to genotype were 1.1 ng/mL (IQR: 0.7 – 1.6) for wild-type, 1.4 ng/mL (IQR: 0.9 – 1.9) for heterozygous mutated, and 2.1 ng/mL (IQR: 1.4 – 2.9) for homozygous mutated. This effect was as well found and even more prominent in a subgroup of patients genetically incapable of expressing CA19 – 9. Overall, the AUC improved if ROC analysis was performed separately for FUT2 wild-type (AUC: 0.731) and homozygous mutant (AUC: 0.816) G428A. In contrast, the use of CEA resulted in a diminished ability to discriminate between cancer and no cancer in patients with a heterozygous mutation (AUC: 0.610). These results are reflected in different optimal cut-off values according to FUT2 genotype. The cut-off was Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A19 A20 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 2.2 ng/mL for the wild-type group, 1.5 ng/mL for the heterozygous mutant group and 26.2 ng/mL ind the homozygous mutant group. The influence of FUT2 on CEA was confirmed in the validation cohort. In conclusion, CEA is suitable for biliary-malignancy screening in PSC patients, especially in patients who do not express CA19 – 9. This is the first study to show that the combined use of CEA measurement and FUT genotyping is clinically beneficial and that it might enhance the early detection of biliary malignancy in clinical practice. This approach could also be effective when screening for other common gastrointestinal malignancies. Corresponding author: Wannhoff, Andreas E-Mail: andreas_wannhoff@med.uni-heidelberg.de 2.6 Bacterial infection is a common complication in patients with severe alcoholic hepatitis Beisel C1, Blessin U1, Benten D1, Lohse AW1, Kluwe J1 1 University Hospital Hamburg-Eppendorf, I. Department of Internal Medicine, Hamburg, Germany Background: Alcoholic hepatitis (AH) has a poor short-term prognosis. Although these patients are at high risk of infection, data about sites of infection, pathogen spectrum and effective treatment strategies is lacking. Methods: 41 cases of severe alcoholic hepatitis (MELD > 20), admitted to the Hepatology Unit of the Hamburg University Medical Center between 2010 and 2014, were analyzed retrospectively by chart review with special focus on demographic, clinical and microbial data as well as treatment outcome. Results: 39 of 41 patients (95%) received treatment of corticosteroids, whereof 41% (n= 16 of 39) were classified as treatment responder in accordance to the Lille model. Overall mortality was 39 % (n= 16 of 41). Infection was observed in 24 patients (61%) of which nine patients (36%) developed infection during treatment with corticosteroids. Mortality was higher when infection occurred during treatment with corticosteroids compared to those cases when infection was diagnosed before treatment with corticosteroids was initiated (55% versus 31%). The most common site of infection was the urinary tract system (n= 14, 56%), followed by positive blood cultures (n= 8, 32 %). Enterococcus species were the most frequently identified causative pathogen (42%, n= 9 of 21). Conclusion: Patients with severe AH are at high risk for infections that correlate with high mortality rates. Infection screening should be mandatory at the time of admission and early antibiotic and potent treatment should be considered, especially in view of the fact that a significant number of infections were not covered by the initial treatment with cephalosporines or chinolones. Corresponding author: Beisel, Claudia E-Mail: c.beisel@uke.de 2.7 Budesonide in autoimmune liver disease: treatment response in a large real life cohort Peiseler M1, Liebscher T1, Pannicke N1, Sebode M1, Hartl J1, Ehlken H1, Zenouzi R1, Weiler-Normann C1, Lohse AW1, Schramm C1 1 University of Hamburg, I. Department of Internal Medicine, Hamburg, Germany Introduction: Autoimmune hepatitis (AIH) is a chronic inflammatory liver disorder that leads to end stage liver disease if left untreated. The standard therapeutic regimen consists of prednisolone in combination with azathioprine. AIH generally responds well to immunosuppressive treatment, yet many patients suffer from steroid-specific side effects. Budesonide (a steroid with a high hepatic first-pass metabolism) is an alternative drug and was shown to be effective in inducing and maintaining remission with few steroid-specific side effects (Manns et al. 2010 Gastroenterology). We here report real life data of a large cohort of patients treated with budesonide at our liver unit. Methods: A total of 80 patients (64 AIH and 16 overlap) were identified who had received budesonide. Start of treatment was with 9 mg per day and the mean maintenance dose of budesonide was 6.2 mg. Initial immunosuppressive treatment included azathioprine in 49 patients patients, MMF in 6 patients and tacrolimus in 1 patient. Patients were evaluated at 6, 12, 24 and 36 months. Reasons for changing the therapeutic regimen to budesonide were recorded. Treatment response was defined as normal serum levels of aminotransferases. This was chosen in order to be able to compare the results with the published study results. Results: 80 patients had received budesonide treatment for a mean of 27.3 months. Of the patients included in this study, 37 (46%) were given budesonide due to steroid-specific side effects, 32 (40 %) because of a steroid-dependent Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York course of disease and 11 (14%) patients as initial therapy. In total, 25 % of the patients were in biochemical remission when budesonide treatment was initiated. After 6, 12, 24 and 36 months, 53%, 67%, 75 % and 67% of patients achieved a biochemical remission and serum ALT levels were significantly reduced at all time points analysed (p < 0.004). Patients, who were given budesonide due to steroid-specific side effects, responded in 47% after 6 months, in 66 % after 12 months, in 92 % after 24 months and in 75% after 36 months of treatment. Patients with a steroid dependent course achieved normal AST and ALT levels in 56% after 6 months, in 71% after 12 months, in 55% after 24 months and in 67% after 36 months. The group of patients who were administered on budesonide as initial therapy responded in 50 % after 6 months, in 85% after 12 months, in 67% after 24 months and in 25% after 36 months. We identified 13 patients with a steroid-induced osteopenia at the beginning of budesonide treatment. In follow up DXA we saw improvement in 5 patients, stable results in 5 patients, worsening in 1 patient and 2 patients had no follow up measurement. 18 patients were treated with budesonide alone, including 8 patients with an AIH/PBC overlap. Overlap patients seemed to respond favourably to budesonide treatment with 75% reaching remission after 6 months compared to only 40 % of AIH patients. Conclusion: The treatment of AIH is highly individual as is the course of disease. Budesonide as part of a combination therapy is effective in inducing and maintaining remission for some patients. Patients with an overlap syndrome respond favourably to budesonide treatment and budesonide monotherapy may be sufficient in some of these patients. Corresponding author: Peiseler, Moritz E-Mail: moritz.peiseler@gmx.de 2.8 Cardiac volume overload after long-term follow-up in TIPS patients Wannhoff A1, Hippchen T1, Friedrich K1, Rupp C1, Weiss KH1, Weiss C2, Schemmer P3, Radeleff B4, Stremmel W1, Gotthardt DN1 1 University Hospital Heidelberg, Department of Internal Medicine IV, Heidelberg, Germany; 2University Hospital Heidelberg, Department of Internal Medicine III, Heidelberg, Germany; 3University Hospital Heidelberg, Department of General and Transplant Surgery, Heidelberg, Germany; 4 University Hospital Heidelberg, Department of Diagnostic and Interventional Radiology, Heidelberg, Germany Transjugular intrahepatic portosystemic shunt (TIPS) is an effective treatment to reduce portal pressure in cirrhotic patients with symptomatic portal hypertension. Insertion of TIPS can be complicated by acute cardiac decompensation in rare cases, yet less is known about long-term cardiac outcome in these patients. Thus we analysed cardiac function during long-term follow-up after TIPS. Patients that received TIPS or were seen for TIPS follow-up at the University Hospital Heidelberg between 2000 and 2013 were included for retrospective analysis. Patients with Budd Chiari syndrome (BCS) were excluded, as were patients without any clinical follow-up after TIPS placement. Cardiac Laboratory (high-sensitivity troponin T [hs-TnT] and N-terminal of the prohormone brain natriuretic peptide [NT-proBNP]) as well as findings on echocardiography were included for analysis. Last echocardiography before TIPS and last one at least 1 year after TIPS were included for each patient if available. Values are reported as means and standard deviation, the Wilcoxon test for paired samples was used to compare results. Continuous variables from echocardiography were dichotomized according to clinically relevant cut-off values and results pre- and post- TIPS were compared using Fisher’s exact test. Statistical analyses were performed using SPSS. A total of 157 patients were included in the final study cohort after 22 were excluded due to BCS and 31 because no follow-up after TIPS was available. Mean age at placement of TIPS was 61 years ( € 12) and 51 (32.9 %) patients were female. 31 patients were classified as having Child A, 93 as Child B and 33 as Child C cirrhosis at time of TIPS insertion. With regards to NT-proBNP and hs-TNT we found no significant difference after the first year of follow-up. An enlarged (> 40 mm) left atrial diameter (LAD) was found in 43 of 102 patients before and in 28 of 45 patients at greater one year after TIPS insertion (P= 0.032). A trend towards more pathological results (> 55 mm) postTIPS (2 of 46) were also observed for the End-diastolic diameter (EDD) compared to pre-TIPS (0 of 103, P= 0.094). The ratio of increased (> 35 mm Hg) systolic pulmonary artery pressure (sPA) rose from 5 of 65 patients pre-TIPS to 13 of 42 after TIPS (P= 0.003). No difference was observed for septal thickness. Analysis of paired samples revealed an increase of mean LAD from 37.41 mm ( € 6.17) pre-TIPS to 41.67 mm 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen ( € 6.55) at more than one year post-TIPS (P= 0.001, n= 24). EDD increased from 44.00 mm ( € 6.27) to 48.49 mm ( € 4.50) (P= 0.002, n= 23). E’/A’ ratio increased from 1.25 ( € 0.69) to 1.35 ( € 0.58) (P= 0.046, n= 6). Septal thickness was 10.93 mm ( € 1.59) before and 11.56 mm ( € 1.37) after TIPS (P= 0.012, n= 27). No significant differences were found for the end-systolic diameter, the right ventricular diameter and sPA. In conclusion, TIPS is accompanied by long-term effects on cardiac function in cirrhotic patients. Our findings indicate that cardiac volume stress and an increase in pulmonary artery pressure is present in these patients. Thorough cardiac evaluation before TIPS should be performed and patients should undergo regular cardiopulmonary followup. Corresponding author: Wannhoff, Andreas E-Mail: andreas_wannhoff@med.uni-heidelberg.de 2.9 Early on-treatment HDV-RNA kinetics are not predictive for long-term response to a PEG-IFNa therapy of hepatitis delta W"bse M1, Yurdaydin C2, Ernst S3, Hardtke S1, Heidrich B1, Bremer B1, Keskin O2, Idilman R2, Koch A3, Manns MP1, Wedemeyer H1 1 Hannover Medical School, Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany; 2 Ankara University, Department of Gastroenterology, Ankara, Turkey; 3Hannover Medical School, Institute for Biometry, Hannover, Germany; 4German Center for Infection Research, Hannover, Germany Introduction: PEG-Interferon alfa (PEG-IFNa) is the only currently available treatment option for hepatitis delta. One main goal of therapy is sustained HDV-RNA suppression which is achieved in less than 30 % of cases. In PEG-IFNa therapy of HCV infection, early viral kinetics have high positive and negative predictive values for SVR, allowing individualization of treatment. Similar data are not available for HDV infection. Aims: Analysis of early HDV-RNA kinetics during PEG-IFNa therapy of hepatitis delta to establish stopping rules to avoid unnecessary treatment. Methods: In the HIDIT-2 study 120 HDV-RNA-positive patients were treated for 96 weeks with PEG-IFNa-2a in combination with tenofovir or placebo. Tenofovir had no significant effect on the post-treatment HDV RNA response. For this analysis all patients were selected who received at least 80 weeks of therapy and for whom HDV-RNAvalues 24 weeks after the end of therapy were available (n= 91). HDVRNA was measured in treatment weeks 4, 8, 12, 24 and 48. Results: HDV RNA was undetectable at post-treatment week 24 in 28 of the 91 patients (31 %). Early on-treatment mean HDV-RNA declines were 0.92, 1.61, 1.76, 2.49 and 2.78 log cop/ml at weeks 4, 8, 12, 24 and 48. An HDV-RNA reduction of at least 1 log was detected in 33% of patients at week 4, and in 64%, 68%, 74% and 79 % at weeks 8, 12, 24 and 48. HDV RNA was negative in 5, 15, 19, 34 and 42 patients at the respective time points. Negative predictive values for long-term response to PEG-IFNA therapy for a 1log HDV RNA decline during treatment were clinically not useful with 73%, 75 % and 54 % until week 12 of therapy but increased to 85 % and 95% at weeks 24 and 48. The corresponding positive predictive values were low with 13%, 12%, 16 %, 30 % and 37%. Undetectable HDVRNA values at the respective time points were not associated with a HDV post-treatment week 24 response (week 4: 4/ 5; week 8: 7/ 15; week 12: 10 / 19 week 24: 20 / 34; week 48 26 / 42). Conclusion: Early HDV-RNA viral kinetics do not allow individualization of PEG-IFNa therapy of hepatitis delta which is in contrast to hepatitis C. Treatment should be continued independently of the initial HDV-RNA response for at least 48 weeks but patients not achieving at least a 1log HDV RNA decline until week 48 should not prolong therapy. Corresponding author: W#bse, Michael E-Mail: MichaelWoebse@gmx.de 2.10 Echokardiographische Speckle Tracking Analysen bei Patienten mit einer Leberzirrhose k#nnen das $berleben vorhersagen Jansen C1, Cox A1, Schueler R2, Lehmann J1, G"rtzen J1, Nickenig G2, Strassburg CP1, Hammerstingl C2, Trebicka J1 1 University Hospital Bonn, Department of Internal Medicine I, Bonn, Germany; 2University Hospital Bonn, Department of Internal Medicine II, Bonn, Germany Hintergrund: Die kardiale Reserve bei der Leberzirrhose ist mit dem &berleben assoziiert. Die kardiale Dysfunktion bei der Leberzirrhose ist meist latent und zeigt sich erst, wenn der Patient einer k#rperlichen Belastung (Infektionen, H"morrhagie, chirurgische Eingriff) ausgesetzt wird. Speckle Tracking Analysen in der Echokardiografie erfassen die kardiale Funktion und haben einen prognostischen Wert bei Patienten ohne Leberzirrhose. Wir untersuchten diese Parameter bei Patienten mit einer fortgeschrittenen Leberzirrhose gelistet f!r eine Lebertransplantation. Methoden: In diese Studie wurden retrospektiv 149 Patienten (49 weiblich) mit einer Leberzirrhose eingeschlossen, die sich aufgrund der Evaluation zur Lebertransplantation in unserer Behandlung befanden. Wir analysierten aus dem im apikalen Vierkammerblick den longitudinal 2D Strain des rechten und linken Ventrikels. Um die linksventrikul"ren diastolischen Dysfunktion zu beurteilen, benutzten wir den herk#mmlichen gepulsten Gewebsdoppler. Die erhobenen Daten verglichen wir mit den klinischen Parametern und dem Verlauf der Patienten. Als Endpunkt f!r die univariaten time-to-event Analyse w"hlten wir den Tod oder die Transplantation. Ergebnisse: Das mediane Alter der eingeschlossenen Patienten betrug 58 Jahre mit einer Spannbreite von 25 bis 71. Die (tiologie der Leberzirrhose war bei 62 Patienten ein chronischer Alkoholabusus, 44 Patienten eine virale Hepatitis und bei 43 Patienten eine andere (tiologie. Bei 51 Patienten lag ein Child A, 63 ein Child B und bei 35 eine Child C Leberzirrhose vor. Die Patienten wiesen einen MELD-Score im Median von 18 auf. 78 Patienten zeigten Aszites. In der Vorgeschichte konnte bei 27 Patienten eine SBP, bei 46 eine Episode einer hepatischen Enzephalopathie und bei 36 ein HRS dokumentiert werden. Interessanterweise ist neben den klassischen Parametern wie MELD-Score und Child-Score der longitudinale links- (p = 0,002) als auch der rechtsventrikul"re Strain (p = 0,018) ein prognostischer Marker in der univariaten time-to-event Analyse. In der Cox Regressionsanalyse konnte der linksventrikul"re longitudinale Strain (p = 0,046) als unabh"ngiger Pr"diktor f!r das &berleben von Patienten mit einer Leberzirrhose identifiziert werden. Besondere Aussagekraft kommt dem linksventrikul"ren longitudinalen Strain bei den Patienten zu, bei einem MELD-Score von weniger als 18 Punkten vorliegt. Schlussfolgerung: Diese Studie zeigt, dass Speckle Tracking mittels Echokardiografie einen prognostischen Wert f!r Patienten mit einer Leberzirrhose darstellen k#nnte. Insbesondere, der longitudinale linksventrikul"re Strain konnte als unabh"ngiger Pr"diktor f!r das &berleben dieser Patienten identifiziert werden. Korrespondierender Autor: Jansen, Christian E-Mail: Christian.Jansen@ukb.uni-bonn.de 2.11 Einfluss von akuten Komplikationen der Leberzirrhose auf die Lebensqualit!t von Patienten mit Leberzirrhose im Verlauf Jara M1, Bias K1, Rolle S1, Schott E1, Pratschke J1, Stockmann M1 1 Charit#, Campus Virchow Klinikum, Klinik f!r Allgemein-, Visceral- und Transplantationschirurgie, Berlin, Deutschland; 2Charit#, Campus Virchow Klinikum, Medizinische Klinik m.S. Hepatologie und Gastroenterologie, Berlin, Deutschland Hintergrund: Die Lebensqualit"t [engl. Health-related quality of life (HRQOL)] von Patienten mit Leberzirrhose ist nachweislich schlechter im Vergleich zur gesunden Normalbev#lkerung. Durch verbesserte therapeutische Ans"tze konnte in den letzten Jahren das Langzeit!berleben von chronisch-leberkranken Patienten deutlich verbessert werden. In diesem Kontext ist der Einfluss von h"ufigen Komplikationen – wie aszitische Dekompensation auf die Lebensqualit"t – zu evaluieren, um gegebenenfalls symptomspezifisch Behandlungsstrategien zu entwickeln, um das l"ngere &berleben auch mit einem m#glichst hohen Maß an Lebensqualit"t zu gew"hrleisten. Material und Methoden: Wir analysierten anhand der deutschen Version des Chronic Liver Diseae Questionnaires (CLDQ-D) die Lebensqualit"t von 142 Kandidaten zur Lebertransplantation. Hier versuchten wir Faktoren, welche unabh"ngig Einfluss auf die Lebensqualit"t zeigten, anhand eines schrittweisen multivariaten Regressionsmodells zu identifizieren. In weiteren 137 Patient mit Leberzirrhose analysierten wir deren Lebensqualit"t zum Zeitpunkt des Einschlusses 2 sowie 4 Monaten danach anhand des CLDQ-D und ließen den Gesundheitszustand anhand eines Patiententagebuchs dokumentieren. Resultate: Unabh"ngige pr"diktive Faktoren, welche mit einer verminderten CLDQ-D Gesamtscore (R2 = 0,474) einhergingen waren der Aszites-Grad (Bs = 0,486; p < 0,001) und verringerte Butyrylcholinesterase Serumkonzentration (Bs= 0.196; p = 0,002). Die Responserate der 137 eingeschlossenen Patienten im Verlauf war gut mit 92 % zum Zeitpunkt des Einschlusses, 78 % nach 2 Monaten und 72% nach 4 Monaten. Es zeigte sich, dass bei Einschluss Patienten, welche bereits aufgrund Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A21 A22 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen von aszitischen Episoden hospitalisiert wurden trendm"ßig geringere CLDQ-D Gesamtscore angaben, als jene welche keine aszitische Symptomatik in der Vorgeschichte hatten (p = 0,069). Ein geringere Gesamtscore ist mit einer geringeren Lebensqualit"t gleichzusetzten. Dieser Trend best"tigte sich im Verlauf; Patienten, welche w"hrend der Beobachtungsdauer hospitalisiert wurden gaben weiterhin zum Teil signifikant geringere CLDQ-D Gesamtscores an (nach 2 Monaten – p = 0,002; nach 4 Monaten – p = 0,051). Schlussfolgerung: Die Entwicklung von Aszites und damit verbundenen Episoden klinischer Dekompensation scheint einen starken Einfluss auf die Lebensqualit"t von Patienten mit Leberzirrhose zu haben. In weiter Konsequenz sollten neue (telemedizinische) Management-Strategien entwickelt werden, welche fr!hzeitig Hinweis auf eine m#gliche Dekompensation geben und so eine schnelle zielgerichtete Therapie erm#glichen. Korrespondierender Autor: Jara, Maximilian E-Mail: maximilian.jara@charite.de 2.12 Higher thyroid hormone levels are associated with better outcome in acute liver failure Anastasiou O1, Sowa JP1, Manka P1, Katsounas A1, Syn WK2, F!hrer D3, Gieseler RK4, Bechmann LP1, Gerken G1, Moeller LC3, Canbay A1 1 University of Duisburg-Essen, Gastroenterology and Hepatology, Essen, Germany; 2University of London, The Institute of Hepatology, Regeneration and Repair Group, London, United Kingdom; 3University of Duisburg-Essen, Endocrinology and Metabolic Diseases, Essen, Germany; 4 Rodos Bio-Target GmbH, Rodos Bio-Target GmbH, Medical Park Hannover, Hannover, Germany Background: Changes in thyroid stimulating hormone (TSH) and thyroid hormone levels, mostly in the form of non-thyroidal illness syndrome (NTIS), have been described in many disease entities including myocardial infarction and sepsis. However, the relationship of acute liver failure (ALF) and thyroid hormone levels has not yet been clarified. The purpose of our present study was to evaluate potential correlations of select thyroid functional parameters with ALF. Methods: 84 consecutively recruited ALF patients were divided in groups according to the outcome of ALF (spontaneous recovery: SR; transplantation or death: NSR). TSH, free thyroxine (fT4), free triiodothyronine (fT3), total thyroxine (TT4), and total triiodothyronine (TT3). NTIS was defined as low or normal TSH, low fT3 or low fT4 without known pre-existing thyroid illness. Results: More than 50 % of patients with ALF presented with abnormal thyroid parameters. These patients had a greater risk for an adverse outcome than euthyroid patients. Patients in the SR group had significantly higher TSH, TT4, and TT3 (but not fT4) concentrations than NSR patients. Albumin concentrations were significantly higher in SR than in NSR. Conclusions: In patients with ALF, TSH and total thyroid hormone levels differed significantly between SR patients and NSR patients. This might be related to a diminished production of liver derived transport proteins, such as albumin, in more severe forms of ALF. In more than 50 % of patients with ALF various degrees of NTIS were apparent upon initial presentation. Thyroid parameters may serve as additional indicators for severity of ALF. Corresponding author: Canbay, Ali E-Mail: ali.canbay@uni-due.de 2.13 Hohe Pr!valenz von Leberwerterh#hungen in einer monozentrischen CED-Patienten Kohorte R!hrup J1, Breunig I1, Tebr!gge I1, Tischendorf S1, Kroy D1, Tischendorf J1, Trautwein C1,Sellge G1, Streetz KL1 1 University Hospital Aachen, Department of Medicine III, Aachen, Germany Hintergrund: Patienten mit chronisch entz!ndlichen Darmerkrankungen (CED) zeigen geh"uft Leberwerterh#hungen. Die Ursachen und Zusammenh"nge sind jedoch noch unzureichend charakterisiert. Methoden: Eine monozentrische Kohorte von 181 CED-Patienten wurde auf Leberwerterh#hungen (erh#hte Werte an > 2 Messtagen) und sonographische Auff"lligkeiten (Struktur, Verfettungsgrad) gescreent. Bei 76 Patienten erfolgte zus"tzlich eine Elastizit"tsmessung der Leber mittels Fibroscan. Ergebnisse: Unsere Ergebnisse zeigen, dass bei insgesamt 115 Patienten (63,5 %) der CED-Kohorte erh#hte Leberwerte bei Verlaufsuntersuchungen nachweisbar sind. Dabei zeigte sich zumeist ein gemischtes hepatisch (ALT, AST) und cholestatisches (AP, gGT) Muster. Bei 30,4 % (bei 55 Patienten) persistierte die Leberwerterh#hung !ber den Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York Beobachtungszeitraum. 33,1% (60 Patienten) zeigten in den letzten 5 Messungen der Datenerhebung anhaltend erh#hte Leberwerte. Bei 8,7 % der Patienten mit Leberwerterh#hungen lag eine diagnostizierte PSC vor, in weiteren Einzelf"llen konnte eine andere Grunderkrankung (AIH, virale Hepatitis, Porphyrie, Pankreatitis und NASH) nachgewiesen werden. Bei 8,7 % ist eine direkte Assoziation mit einer Medikamentengabe sehr wahrscheinlich (meist direkte Korrelation mit einer Azathioprin-Therapie). Die Gabe von Anti-TNFa Antik#rperpr"paraten war hingegen deutlich seltener mit Leberwerterh#hungen assoziiert. In etwa 64,82 % der F"lle (etwa 56 Patienten) ließ sich zun"chst keine eindeutige Ursache f!r die Leberwerterh#hungen finden. Allerdings konnten geh"uft Assoziationen zu hohen Schubaktivit"ten (in 4,3 %), zu vorhergegangen Operationen (8,7 %), sowie bei isolierten Bilirubin-Erh#hungen ein vermutlich bisher noch nicht diagnostizierter M. Meulengracht (9,6 %) als m#gliche Ursache gefunden werden. 36,7 % der CED-Patienten wiesen zudem sonographische Ver"nderungen in Form vermehrter Leberverfettung (davon 52,8 % Grad 1, 33,3% Grad 2, 13,9 % Grad 3) auf. Bei 2,5 % der Patienten wurde ein h#hergradiger Umbau der Leber (Fibrose/ Zirrhose) nachgewiesen. Die Erh#hung gemessener Leberwerte korrelierte in 28,7 % mit einer Leberverfettung. Bei 9,4 % der Kohorte lag jedoch auch ohne erh#hte Leberwerte eine relevante Leberverfettung vor. Fibroscan-Untersuchungen zeigten bei 13 von 78 (17%) Patienten eine erh#hte Lebersteifigkeit (> 6kPA). Schlussfolgerung: Die erhobenen Daten zeigen eine unerwartet hohe Pr"valenz von Leberwerterh#hungen und begleitenden Lebererkrankungen bei CED-Patienten, die teilweise auch bereits zu Ver"nderungen der Lebersteifigkeit gef!hrt haben. Ungekl"rt ist die Ursache der geh"uften Assoziation von Leberverfettung und CED. Korrespondierender Autor: Streetz, Konrad L. E-Mail: kstreetz@gmail.com 2.14 Improvement of Depressive Symptoms upon Correction of Vitamin D Deficiency in Women with Chronic Liver Disease Stokes CS1, Gruenhage F1, Baus C2, Riemenschneider M2, Lammert F1 1 Saarland University Medical Center, Department of Medicine II, Homburg, Germany; 2Saarland University Medical Center, Department of Psychiatry and Psychotherapy, Homburg, Germany Introduction: Patients with chronic liver diseases (CLD) frequently suffer from both vitamin D deficiency and depression. A recent meta-analysis reported an inverse correlation between depression and vitamin D levels. Indeed, vitamin D receptor (VDR) is present and genomic and nongenomic VDR-mediated signalling has been identified in brain. As depression is known to occur more frequently in women than in men, this intervention study investigates the differential effects of vitamin D substitution on depressive symptoms in patients with CLD and depression. Methods: Vitamin D insufficiency (as defined by serum concentrations < 30 ng/ml) was present in 77 (79%) of patients with CLD recruited in the overall study. From these, 31% had depressive symptoms as assessed using the BDI-II instrument (score ‡ 14 indicating depression) and were included in the sensitivity analyses herein. Serum 25-hydroxyvitamin D concentrations were determined by chemiluminescence immunoassays. All patients received 20,000 IU vitamin D/week for 6 months. We assessed liver function tests (LFT), vitamin D status and depression after 3, 6, and 12 months during follow-up. Results: The median age of the patients with CLD and depressive symptoms was 56 years, 60% were women, and 42 % had chronic hepatitis C virus (HCV) infection. Men and women with depression and vitamin D insufficiency did not differ (all P > 0.05) with respect to age, body mass index, LFT, 25-hydroxyvitamin D levels (14 vs.17 ng/ml) and BDI-II scores (18 vs. 21 points) at baseline. A significant inverse linear correlation between vitamin D level and depression severity existed in women only (rs=-0.55, P= 0.026). Vitamin D levels significantly (P < 0.001) increased to normal after 3 and 6 months of supplementation in all CLD patients, but higher median 25hydroxyvitamin D levels were consistently displayed in women. Interestingly, during the intervention period, a distinct response was observed in women with BDI-II scores returning to normal levels at 3 and 6 months (13 and 11 points, respectively; both P= 0.002), whereas no change in depression scores was observed in men (18 and 19 points, respectively). LFT remained unchanged with vitamin D supplementation. Conclusions: In patients with CLD, marked gender disparities are observed with regards the association between vitamin D and depressive symptoms herein, with only women showing an inverse relationship between vitamin D levels and depressive symptoms. Moreover, vitamin D therapy signifi- 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen cantly improved depressive symptoms to normal levels in women as compared to men with CLD and vitamin D insufficiency. The functional mechanisms underlying these gender disparities in response to vitamin D substitution in CLD warrant further investigation. Corresponding author: Stokes, Caroline S E-Mail: caroline.stokes@uks.eu 2.15 Investigations on acetaminophen-induced liver injury using an ex-vivo perfusion model with human liver sections Schreiter T1, Sowa JP1, Sydor S1, Treckmann J2, Kaiser G2, Strucksberg KH3, Baba HA4, Gieseler RK5, Gerken G1, Canbay A1 1 University of Duisburg-Essen, Gastroenterology and Hepatology, Essen, Germany; 2University of Duisburg-Essen, Department of General, Visceral and Transplant Surgery, Essen, Germany; 3University of Duisburg-Essen, Endocrinology, Clinical Chemistry and Laboratory Medicine, Essen, Germany; 4University of Duisburg-Essen, Institute of Pathology and Neuropathology, Essen, Germany; 5Medical Park Hannover, Rodos Biotarget GmbH, Hannover, Germany Introduction: A perfusion system for human liver sections able to keep hepatic functionality for up to 30 hours was applied to study liver damage mediated by acetaminophen (APAP) in a human tissue based model. Methods: Perfusions were performed for 30 hours and hourly taken samples from the perfusate were analyzed for markers of general metabolism, hepatic synthesis capacity and liver cell damage. APAP was added after 8 h with amounts relative to the liver weight (6.5 mg/g). NAcetylcysteine was added after 20 h to reduce liver damage in the course of perfusion. Liver function was determined by clearance of indocyanine green (ICG) after 4, 20 and 28 h and normalized to the value at 4 h. Results: ICG clearance in three liver sections perfused without APAP to obtain reference values was 98 € 12% after 20 h and 77 € 18% after 28 h. Liver function in two smaller liver sections (38 g) incubated with APAP was reduced to 41 and 71% after 20 h and 22 % after 28 h, respectively. Liver function in two larger liver pieces (57 g) was dropped to 25 and 36 % after 20 h and to 18 and 10 % after 28 h, respectively, exhibiting nearly complete cell death at the end of experiment. Conclusion: The hepatotoxic sensitivity of the model with patient-relevant amounts of APAP was shown within the perfusion period. Further studies are required to investigate the optimal conditions to gain damaged, but not deceased tissue after 30 h for subsequent analysis. Thus, this model is useful as human-based artificial liver system for the study of new drug candidates and pathologies of the liver. Corresponding author: Canbay, Ali E-Mail: ali.canbay@uni-due.de 2.16 Late onset of disease is associated with poor outcome in patients with primary sclerosing cholangitis Rupp C1, R"ssler A1, Friedrich K1, Wannhoff A1, Weiss KH1, Sauer P1, Stremmel W1, Gotthardt DN1 1 University Hospital Heidelberg, Internal Medicine IV, Heidelberg, Germany Background & Aims: Primary sclerosing cholangitis (PSC) is a chronic cholestatic liver disease, characterized by sclerosis and destruction of the biliary system. The median onset of PSC varies in different populations, but reaches a climax around the age between thirty and forty. We aimed to analyze disease progression and liver-dependent survival in patients with first diagnosis of PSC after the age of fifty years. Methods: Patients who were admitted to our Department during the time period of 1987 and 2012 with well-defined diagnosis of PSC were analyzed in regard to the onset of the disease. Patients with first diagnosis of PSC after the age of fifty were considered as late-onset group and compared to patients with early onset disease. Comparison between frequencies was done using Chi-Square-test or Fisher’s exact test where appropriate. Continuous data were compared with the nonparametric Wilcoxon rank-sum test. Actuarial transplantation-free survival was estimated using Kaplan-Meier product limit estimator. Differences between the actuarial estimates were tested with the log rank test. Fisher test Results: A total of 29/ 210 (13.8 %) patients had an onset of PSC after the age of fifty. There was no difference in baseline clinical and/or laboratory characteristics. The proportion of females was significantly higher in patients with late-onset PSC (50.0 % vs. 28.3 %; p = 0.02). Frequency of dominant stenosis was not different between the two groups, although late-onset patients developed more often re-stenosis, requiring repeated endoscopic treatment (50.5 % vs. 77.8 %; p = 0.04) and suffered more often from recurrent cholangitis (48.3 % vs. 21.0%; p = 0.003). Patients with late-onset PSC had a reduced transplantation-free survival (20.8 % € 1.7 vs. 10.5 % € 0.6 years p < 0.0001) with progredient liver failure and cholangicarcinoma (CC) as leading cause of death. Multivariate Cox regression analysis confirmed late-onset of disease as an independent risk factor for reduced transplantation-free survival. Conclusion: Patients with late-onset PSC display an altered gender-ratio and are at increased risk to suffer from progredient liver failure and hepatobiliary malignancies. Corresponding author: Rupp, Christian E-Mail: christian.rupp@med.uni-heidelberg.de 2.17 Metformin Treatment Ameliorates Liver Injury Indicating Fatty Liver Polycystic Ovary Syndrome Tan S1, Vollmar N1, Benson S2, Bechmann LP3, Gerken G3, F!hrer D1, Canbay A3 1 University of Duisburg-Essen, Endocrinology and Metabolic Diseases, Essen, Germany; 2University of Duisburg-Essen, Medical Psychology and Behavioral Immunology, Essen, Germany; 3University of Duisburg-Essen, Gastroenterology and Hepatology, Essen, Germany Background: Polycystic ovary syndrome (PCOS) is associated with obesity and insulin resistance (IR), two key features of the metabolic syndrome. Non-alcoholic fatty liver disease (NAFLD) is the liver manifestation of the metabolic syndrome, with its progressive form, non-alcoholic steatohepatitis (NASH), comprising a major health risk for affected patients. Metformin (MF) as insulin sensitizing agent leads to a decrease of hepatic IR and could thus possibly ameliorate NASH. The caspase 3cleaved fragment of cytokeratin 18 (CK18), termed M30, has been established as a serum marker for NASH. This study was conducted to evaluate the influence of MF on serologic NASH in PCOS patients. Methods: In 89 PCOS patients (age: 28.2 € 5.2 yrs., BMI: 32.1 € 8.8 kg/m2), metabolic parameters, liver enzymes, and M30 were assessed at baseline and after six months MF treatment. Patients with IR at baseline were subdivided in one group with dissolved IR (PCOS-exIR) and persistent IR (PCOS-PIR) after treatment and compared to an initially insulin sensitive PCOS-group (PCOS-C). Results: Reduction of liver enzymes by MF treatment was observed independently from achieved body weight loss in the PCOS-C and PCOS-exIR in comparison to the PCOS-PIR group. This was associated with decreasing prevalence of liver injury indicating fatty liver (-19.4 resp. )12.0 % vs. 7.2 %, Chi2= 29.5, p < 0.001). No change in mean M30 levels and NASH-prevalence was observed. In PCOS-PIR, ALT levels increased significantly accompanied by a nominal, not significant M30 increase. Conclusion: MF improves liver enzymes in subgroups of PCOS patients without lowering hepatic apoptosis markers. Though, individuals with no improvement of IR exhibited a non-significant increase of liver enzymes and M30. This might a stabilizing effect of MF on NAFLD, inhibiting progression of the disease. Further studies with more participants and a longer follow up period (> 1year) are needed to elucidate the impact of MF on NAFLD in PCOS patients. Corresponding author: Canbay, Ali E-Mail: ali.canbay@uni-due.de 2.18 Microbial translocation in liver fibrosis induces chronic IFNAR signaling that directly affects innate immune responses to systemic bacterial infection Abdullah Z1, Hackstein P1, Trebicka J2, Beyer M3, Schultze JL3, Kastenm!ller W1, Sauerbruch T2, Spengler U4, Kurts C5, Knolle PA1,6 1 University of Bonn, Institute of Molecular Medicine, Bonn, Germany; 2University of Bonn, Department of Internal Medicine I, Bonn, Germany; 3University of Bonn, Genomics and Immunoregulation, Life and Medical Sciences Institute (LIMES), Bonn, Germany; 4University of Bonn, Department of General Internal Medicine, Bonn, Germany; 5University of Bonn, Institute of Experimental Immunology, Bonn, Germany; 6Technische Universit$t M!nchen, Institute of Molecular Immunology (IMI), Munich, Germany A common clinical complication in patients with liver fibrosis or cirrhosis is exacerbations of bacterial infections, which often persist in these Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A23 A24 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen patients. In order to study the underlying pathophysiological cellular and molecular mechanisms in mice, we investigated the immune responses to Listeria infections in the context of liver fibrosis. Using the bile-duct ligation model for the induction of liver fibrosis in mice we found an enhanced susceptibility to Listeria infections leading to persistence of infection, recapitulating clinical situations in humans. While the innate clearance of Listeria in the spleen of those mice was unaltered, bactericidal activity of intrahepatic macrophages and bacterial clearance in the liver were strongly impaired. This reduced local clearance of Listeria was correlated to impaired IFNg, IL-12 and ROS production by the myeloid cells in the liver. Mechanistically, we identified IFNAR signaling in the myeloid cells as the basis for impaired anti-bacterial immune responses in mice with liver fibrosis. Using germ free mice we could show that IFNAR signaling is induced by translocated gut microbiota during liver fibrosis. This chronic Type I IFN signals on myeloid cells in turn lead to IL-10 release, which directly inhibited IFNg, IL-12 and ROS production. Strikingly, we could rescue mice form chronic infection by either blocking IFN signaling in myeloid cells or systemic blockade of IL10 signaling, opening an exciting new therapeutic avenue for bacterial infections in patients suffering from liver fibrosis or cirrhosis. Corresponding author: Abdullah, Zeinab E-Mail: zeinab.abdullah@ukb.uni-bonn.de 2.19 NAFLD linked hepatic iron stores and impact of fat reducing agents on males and females Rattus norveicus Abbas AS1, Sheikh N1, Batool S1 University of the Punjab, Department of Zooloy, Lahore, Pakistan 1 Dietary obesity leading to non alcoholic fatty liver disease (NAFLD) is also linked with hepatic iron overburden. This is the most prevalent hepatic disorder of developed countries. The current project was designed to observe the effect of the fat plummeting agents on NAFLD linked iron stores of body on the basis of gender. Males (M) and females (F) Rattus norveicus (n= 40) were further divided into four groups (n= 10) designated as 0, I, II and III. Group 0 served as negative control and was fed on 100 % rat chow. Group I served as positive control and consumed HFD, group II and III were experimental groups and consumed HFD supplemented with 50 g Nigella sativa seeds or Plantago ovata husks respectively. The histological examination exhibited that elevated iron stores were present in livers of M-I, M-II, F-I and F-II groups while lower iron stores were present in the groups M-III and FIII. Taking together these findings it can be inferred that HFD causes the iron burden in both genders of Rattus norvegicus and P. ovata husk is potent to reduce the NAFLD linked hepatic iron stores. Corresponding author: Abbas, Afshan S E-Mail: asyedasad@gmail.com 2.20 Next generation sequencing analysis of cholestatic patients reveals high impact variation in common and rare candidate genes: Deconstructing the genetic architecture of cholestasis Liebe R1, Christmann A2, Gr!nhage F3, J!ngst C3, Lammert F3 1 University of Heidelberg, Department of Medicine II, Medical Faculty Mannheim, Mannheim, Germany; 2Zentrum f!r Innovative Genetische Diagnostik, Homburg, Germany; 3 Saarland University Hospital, Department of Medicine II, Homburg, Germany Background: Cholestasis indicates bile secretory failure, which might be caused by environmental factors and gene variants, or combination of both. Although there is variability in underlying causes of hepatocellular cholestasis, many patients develop cholestasis of unknown etiology and gene mutations of critical hepatobiliary transporters or their regulators may be suspected. Our aim now was to employ next generation sequencing (NGS) to dissect genetic risk factors in adult patients with cholestatic liver injury of unknown etiology. Methods: The full length coding sequences of 24 genes known to be involved in regulation and transport of drugs and metabolites into bile (Table) were determined by NGS sequencing in selected patients with unexplained cholestatic liver injury, as defined by an at least two-fold increase of serum alkaline phosphatase (AP) activities and ALT/AP ratio £ 2. Population frequency and Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York biochemical impact of all detected variants were analysed; rare, highimpact variants were also considered. ABCB4 ABCB11 ABCC2 ABCG5 ABCG8 ATP8B1 CIRH1A CLDN1 JAG1 NOTCH2 NR1 H4 NR1I2 UGT1A1 – 10 VIPAR VPS 33B Results: Sequence analysis of 24 genes in 22 patients with cholestatic liver disease revealed heterozygosity for several high-impact variants that have previously been associated with cholestatic liver disease such as ABCB11 p.G982R (PFIC2), ABCB11 p.D 482G (PFIC2), ATP8B1 p.I661T (PFIC 1/BRIC), ATP8B1 p.D 70N (BRIC/ICP) and VPS 33B c.177+1G>A (ARC). New high-impact variants that are highly likely to result in nonfunctional protein (complete loss of splice site, frameshift deletion) were detected in ABCB4 (MDR3), NR1I2 (PXR) and UGT1A7. None of these variants were found among 6.500 individual sequences in the NHLBI exome database. Rare, non-conservative variants of yet unknown biochemical impact were also detected in ABCC 2 (MRP2), NOTCH2 and NR1H4 (FXR). Conclusions: Next generation sequencing permits rapid and comprehensive analysis of a large panel of cholestasis-associated transcripts. Peculiar phenotypes appear to be more likely to result in the detection of pathogenic or novel mutations. Correlating the results with systematic clinical phenotyping will result in improved genotypephenotype correlations. Comprehensive genotyping might also permit targeted intervention if the respective mutations are amendable to chemical intervention such as chaperone-therapy. Corresponding author: Liebe, Roman E-Mail: Roman.Liebe@medma.uni-heidelberg.de 2.21 Nicht-alkoholische Fettleberentz"ndung (NASH) – doch nur ein Problem der Energiezufuhr? Jagemann B1, Zyriax B2, Windler E2, Hartig U3, Lohse AW1, Kluwe J1 1 University Hospital Hamburg-Eppendorf, Internal Medicine I, Hamburg, Germany; 2University Hospital HamburgEppendorf, Preventive Medicine, Department of General and Interventional Cardiology, University Heart Center, Hamburg, Germany; 3German Institute of Human Nutrition Potsdam-Rehbruecke, Department of Epidemiology, Nuthetal, Germany Einleitung: Fehlern"hrung und das in der Folge oft entstehende &bergewicht sind als Risikofaktoren f!r die Entwicklung der Nicht-alkoholischen Fettlebererkrankung (NAFLD) bekannt. Die Basis der aktuell empfohlenen Therapie sind Lebensstilver"nderungen mit mehr Bewegung und ausgewogener, kalorienreduzierter Kost. Da die Ern"hrungsempfehlungen sehr allgemein gehalten sind, war das Ziel unserer Studie die Pr!fung der Wirksamkeit dieser Empfehlungen bei sonographisch gesicherten NAFLD -Patienten mit erh#hten ALT Spiegeln. Methodik: Es wurden 20 m"nnliche Patienten im Alter von 18 bis 54 Jahren mit Erstdiagnose NAFLD !ber einen Zeitraum von 6 Monaten beobachtet, die in der I. Med. Klinik der Universit"tsklinik HH in medizinischer und ern"hrungstherapeutischer Behandlung waren. Neben anthropometrischen Daten und Laborparametern konnten mittels eines validierten Food-Frequency-Questionnaires (FFQ) Energieaufnahme, Aktivit"t und N"hrstoffzufuhr zu 2 Zeitpunkten erhoben werden. Gleichzeitig wurden die Patientenparameter zu Beginn der Therapie denen eines gesunden geschlechts- und altersadjustierten Kontrollkollektivs gegen!ber gestellt (n= 40). Ergebnisse: Erwartungsgem"ß unterschieden sich NAFLD-Patienten von den Kontrollen zu Beginn signifikant in den Parametern BMI (27.77 kg € 0.72 vs. 23.42 kg € 0.45), Taillenumfang (98.61 cm € 1.97 vs. 80.00 cm € 1.43), ALT (95.21 U/l € 13.72 vs. 19.03 U/l € 0.91) und gGT (111.5 U/l € 12.81 vs. 16.35 U/l € 1.42) von der gesunden Kontrollgruppe. Die mittels BIA bestimmte Fettmasse zeigte keine signifikanten Unterschiede. Die NAFLD-Patienten nahmen signifikant mehr Kalorien zu sich als die Kontrollen (3161 kcal € 205.9 vs. 2123 kcal € 84.62). Nach 6 Monaten erreichten die Patienten im Rahmen einer 5-maligen Ern"hrungstherapie folgende Ver"nderungen: Gewicht [kg]: – 3, 83 kg (+ 2,2 bis -10,8); Taille [cm]: – 3,04 cm (- 0,5 bis – 7,4); Fettmasse [%]: – 2,25 % (+ 1 bis – 8,0). 10 von 20 Patienten erreichten die empfohlene Reduktion der ALT Werte um 1/ 3 bzw. in den Normbereich, Die ALT fiel im Durchschnitt: um 33,9 U/l (+ 1 bis – 157) p = 0,0448. Die gGT reduzierte sich um 17,85 U/l (+ 111 bis -75). Die gleichzeitig empfohlene Reduktion des Ausgangsgewichtes um mind. 5% wurde von 9 Patienten erreicht. Nach 6 Monaten Therapie reduzierten die Patienten Ihre Kalorienzufuhr deutlich (p = 0,018), unterschieden sich im Mittelwert aber noch immer signifikant vom Kontrollkollektiv (2490 € 142.6 vs. 2123 € 84.62; p = 0,023). Bezogen auf 1000 kcal/d ließen sich zu keinem Zeitpunkt Unterschiede in der Zusammensetzung der Makro- und Mikron"hrstoffe messen. 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen Schlussfolgerung: Anhand des FFQ ließ sich kein charakteristisches Ern"hrungsmuster der NAFLD-Patienten erkennen. Die derzeitige Therapie bei NAFLD f!hrt in diesem nicht adip#sen Kollektiv zu einer Reduktion des Gewichtes und der ALT, wobei aber nur bei einem Teil der Patienten die empfohlenen Ziele erreicht werden. Weiterf!hrende Erhebungen des Lebensstils sind notwendig, um individuelle Risikofaktoren spezifischer erfassen zu k#nnen. Korrespondierender Autor: Jagemann, Bettina E-Mail: b.jagemann@uke.de 2.22 Pr!diktoren f"r splanchnische Thrombosen bei Patienten mit myeloproliferativen Neoplasien G"rtzen J1, Hunka L1, Jansen C1, Vonnahme M1, Lehmann J1, Brossart P2, Strassburg CP1, Wolf D2, Trebicka J1 1 University of Bonn, Medizinische Klinik und Poliklinik I, Bonn, Deutschland; 2University of Bonn, Medizinische Klinik und Poliklinik III, Bonn, Deutschland Einleitung: Das Vorliegen einer Myeloproliferativen Neoplasie (MPN) ist ein Risikofaktor f!r die Entwicklung einer splanchnischer Thrombose. Solche splanchnischen Thrombosen k#nnen unerkannt bleiben, bis Komplikationen durch die portale Hypertension, wie Varizenblutungen, auftreten. In diesem Stadium wird die Behandlung der Patienten schwierig, da die Antikoagulation bei einer drohenden oder vorliegenden Blutung nicht ohne weiteres m#glich ist. Daher ist die fr!he Erkennung und entsprechende Antikoagulation f!r die Patienten außerordentlich wichtig. Wir haben Pr"diktoren f!r splanchnische Thrombosen bei Patienten mit myeloproliferativen Neoplasien ermittelt. Methoden: Es wurden Daten von 126 Patienten analysiert: 81 Patienten mit myeloproliferativen Neoplasien wurden mit 45 Patienten mit splanchnischen Thrombosen anderer Genese verglichen. Klinische und laborchemische Daten der Patienten wurden zum Zeitpunkt der Erstvorstellung und bei der letzten dokumentierten Visite erfasst. Diese Daten wurden dann mithilfe Wilcoxon-Tests, Mann-Whitney-U-Tests und Regressionsanalysen auf m#gliche Pr"diktoren analysiert. Ergebnisse: Von 81 Patienten mit myeloproliferativer Neoplasie litten 18 Patienten unter Polycythaemia vera, 16 Patienten unter essentieller Thrombozyth"mie und 40 Patienten unter Osteomyelofibrose. 12 Patienten konnten keiner dieser Krankheiten zugeordnet werden. Bereits zum Zeitpunkt der Erstvorstellung lag bei 15 Patienten mit MPN eine splanchnische Thrombose vor. Weitere 10 Patienten entwickelten im weiteren Verlauf eine splanchnische Thrombose. Von 45 Patienten mit splanchnischen Thrombosen anderer Genese zeigten 32 Patienten bereits bei Erstvorstellung eine splanchnische Thrombose und 13 Patienten entwickelten eine Thrombose im weiteren Verlauf. Patienten, die bei der Erstvorstellung erh#hte Werte f!r AST, ALT und g-GT aufwiesen, entwickelten im Verlauf h"ufiger splanchnische Thrombosen (p < 0.05). Beim Vorliegen von splanchnischen Thrombosen hatten Patienten mit MPN eine signifikant h#here LDH (p < 0.05). Bei diesen Patienten war die LDH außerdem ein pr"diktiver Faktor f!r das Vorliegen einer MPN (p < 0.05). Die H#he der LDH war ein pr"diktiver Faktor f!r das Gesamt!berleben bei Patienten mit einer MPN (p < 0.05). Diskussion: Erh#hte AST, ALT und g-GT k#nnten Pr"diktoren f!r die Entwicklung von splanchnischen Thrombosen bei Patienten mit einer MPN sein. Ferner kann eine erh#hte LDH bei Patienten mit splanchnische Thrombosen das Vorliegen einer MPN voraussagen. Sie ist außerdem ein pr"diktiver Faktor f!r das Gesamt!berleben bei Patienten mit einer MPN. Korrespondierender Autor: G#rtzen, Jan E-Mail: jan.goertzen@ukb.uni-bonn.de 2.23 Prevalence of hepatic steatosis in healthy health care workers as quantified by controlled attenuation parameter (CAP) Arslanow A1, Lammert F1, Stokes CS1 1 Saarland University Hospital, Department of Medicine II, Homburg, Germany Background: Hepatic fat accumulation is the hallmark of non-alcoholic fatty liver (NAFL), for which prevalence estimates range widely from 5 to 50 % in the population due to differences of screening and detection strategies. Since up to 25% of patients with NAFLD might develop advanced liver fibrosis and cirrhosis, which increase the risk of liver-associated mortality, better NAFL screening is needed. Our aim was to assess the frequency of hepatic steatosis in participants without a history of chronic liver disease who were recruited from the Occupational Health Department at Saarland University Medical Center. Methods: For this prospective study, 81 participants volunteered (80 % women, median age 29 years, range 21 – 63 years). Hepatic steatosis was assessed using controlled attenuation parameter (CAP), which quantifies the degree of ultrasound attenuation based on vibration- controlled transient elastography (VCTE; FibroScan!, Echosens). Body composition was determined using an eight electrode bioelectrical impedance analyzer (BIA; TANITA BC-418 MA). Liver function tests (LFT) and serum lipids were measured from plasma samples with standardized clinical assays. Results: The median CAP score was 226 dB/m (range 100 – 400 dB/m). In total, 33 participants (41 %) presented with hepatic steatosis, when using 238 dB/m as cut-off for liver fat accumulation (Sasso Ultrasound Med Biol 2010). The median body mass index was significantly (P < 0.001) higher in participants with than without liver steatosis (26 vs. 22 kg/m2, respectively) and accordingly, the majority of NAFL patients were overweight (42%) or obese (15%). In contrast, only 15 % of participants without hepatic steatosis were overweight, and none were obese (P < 0.0001). In line with these associations, body fat mass as determined by BIA was elevated in 48% of participants with hepatic steatosis, as compared to only 6 % in those with low liver fat contents. In contrast, LFT and serum lipid parameters did not differ significantly between the two groups. Conclusions: Presence of hepatic steatosis was documented in almost half of the cohort of perceived healthy individuals. Whereas serum surrogate markers did not differentiate the individuals, body composition reflected the differences in liver fat contents among the two groups. CAP (and BIA) represent rapid non-invasive methods that facilitate the identification of fatty liver. Broad NAFL screening in the workplace might be encouraged, since it may allow timely detection of at risk individuals and early implementation of lifestyle changes. Corresponding author: Arslanow, Anita E-Mail: anita.arslanow@uks.eu 2.24 Upregulation of Kr"ppel-Like Factor 6 is associated with acute liver injury in mice and humans Sydor S1, Best J1, Manka P1, Schlattjan M1, Schreiter T1, Vetter D2, Paul A3, Friedman SL4, Gerken G1, Canbay A1, Bechmann LP1 1 University of Duisburg-Essen, Gastroenterology and Hepatology, Essen, Germany; 2University Hospital Z!rich, Visceral and Transplant Surgery, Zurich, Switzerland; 3 University of Duisburg-Essen, General, Visceral and Transplant Surgery, Essen, Germany; 4Mount Sinai School of Medicine, Division of Liver Disease, New York, NY, USA Background: Kr!ppel-like factor 6 (KLF6) is a ubiquitously expressed, multifunctional transcription factor and tumor suppressor gene. In previous studies, we identified KLF6 as an important transcription factor in hepatocyte glucose and lipid homeostasis, and downregulation of KLF6 was associated with accelerated tumor-growth of hepatocellular cancer. So far, no data is available on the role of KLF6 in acute liver injury and regeneration. Here, we aimed to investigate the expression pattern of hepatocyte KLF6 in patients with acute liver failure (ALF), in a human ex-vivo perfusion model of acetaminophen induced liver injury and to study the effects of hepatocyte specific KLF6 depletion in mice undergoing partial hepatectomy (PHx). Methods: Liver samples from 10 patients with drug-induced ALF were obtained (either liver biopsy or explanted liver in patients who underwent liver transplantation) and KLF6 expression was quantified via immunohistochemistry (IHC) and compared to liver samples from 10 non-cirrhotic NAFLD patients with simple steatosis as controls. In another setting, non-cirrhotic liver tissue was obtained from partial liver resection for metastatic surgery in 8 patients. In an established ex-vivo perfusion model, these samples were treated with acetaminophen (APAP) up to 30 hours. KLF6 and HGF (hepatocyte growth factor) mRNA expression was quantified before and after APAP treatment. In a murine model of PHx (n= 6 mice/group), we assessed KLF6 expression before and at different timepoints after PHx. Also, hepatocyte specific KLF6 knockout mice underwent PHx and we performed PCNA staining at different timepoints to assess hepatocyte proliferation, compared to controls (n= 6 mice/group). Results: IHC in ALF patients revealed significant upregulation of KLF6 protein within hepatocytes compared to controls. APAP perfusion of non-cirrhotic liver tissue significantly induced the expression of KLF6 (4.7-fold, p = 0.003) as well as the regeneration-associated molecule HGF (3.9-fold, p = 0.02). In mice, PHx also led to significant induction of KLF6 expression at different timepoints (3.8-fold, p = 0.03). In hepatocyte specific KLF6 knockouts, hepatocyte proliferation, as assessed with PCNA staining was significantly induced at early timepoints (p < 0.05). Conclusion: Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A25 A26 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen Here, we were the first to study KLF6 expression in ALF. Our findings suggest an important role for KLF6 in liver regeneration, as KLF6 expression is upregulated in different models of acute liver injury and ALF patients. Hepatocyte proliferation following PHx was induced in mice with KLF6 knockdown, compared to wildtype controls, suggesting a role for KLF6 in hepatic regeneration. Further studies and data analysis will be needed to identify the individual mechanisms for KLF6 mediated effects in acute liver injury. Corresponding author: Bechmann, Lars P. E-Mail: lars.bechmann@uk-essen.de 2.25 Use of beta-blockers is associated with improved 30 day survival in patients with spontaneous bacterial peritonitis Lutz P1, Nischalke HD1, Kr$mer B1, Langhans B1, Schlabe S1, Nattermann J1, Hoerauf A2, Strassburg CP1, Spengler U1 1 Bonn, Department of Internal Medicine I, Bonn, Germany; 2 Bonn, Institute for Medical Microbiology, Immunology and Parasitology, Bonn, Germany; 3Bonn, German Center for Infection Research, Bonn, Germany Introduction: Use of beta-blockers after spontaneous bacterial peritonitis (SBP) leads to increased long-term mortality. However, the effect on survival of the infection is unclear. In a murine peritonitis model, inhibition of the neuroadrenergic system even increased survival. Thus, we studied the role of beta-blockers for short-term survival in patients with SBP. Methods: We determined transplant-free 30-day survival in cirrhotic patients who developed SBP between March 2012 and April 2014 in our department. Interleukin 8 (IL-8) was measured in in ascites supernatant by ELISA. Ascites cells were stimulated in vitro with 100 ng/ ml Lipopolysacchairde (LPS) with or without pre-treatment with 5 mg/ml propranolol and IL-8 production was assessed by ELISA. Results: The study population comprised 55 patients with SBP (32 (58%) male, median age 59 years). Cirrhosis was due to alcohol in 36 (66%) patients, to viral hepatitis in 11 (20 %) patients. Seven (13%) patients had hepatocellular carcinoma (HCC). Median MELD score was 21, and 42 (76%) patients were classified as Child-Pugh stage C. SBP was nosocomial in 35 (64%) patients. 34 (62 %) and 21 (38%) patients were without and with beta-blockers at time of SBP, respectively: 14 (67%) with propranolol, the rest with metoprolol, bisoprolol or nebivolol. Clinical and laboratory data did not differ between patients with and without beta-blockers. 30day survival was 58% (n= 32): 16/ 21 (76%) in patients on beta-blockers versus 16/ 34 (41%) in patients without (p = 0.049). Poor survival was associated with the presence of HCC (1 / 7 (14%) versus 31/ 48 (65%); p = 0.017) and MELD score > 22 (6 / 25 (24%) versus 26/ 30 (87%), p < 0.001) A forward conditional Cox logistic regression analysis confirmed MELD score £ 22 (p < 0.001) and use of beta-blockers (p = 0.049) as prognostic factors of 30-day survival. During SBP, patients on beta-blockers had higher fractions of mononuclear cells among ascites leucocytes than patients without (median 31% versus 19%; p = 0.036). IL-8 levels in the ascites were lower in patients without (1289 pg/ml) than with beta-blockers (470 pg/ml; p = 0.29) in a subgroup of 19 patients were ascites was available. In-vitro, an increase in IL-8 production after stimulation of ascites cells with LPS could be attenuated by pre-treatment with propranolol (n= 7; p = 0.033). Conclusion: Intake of beta-blockers in patients with SBP was associated with a slightly better 30-day survival, which might be due to attenuated IL-8 secretion and a more balanced peritoneal inflammation. Increased mortality reported for beta-blockers after SBP is probably not related to the infection itself. Corresponding author: Lutz, Philipp E-Mail: philipp.lutz@ukb.uni-bonn.de 2.26 Verbesserte Fr"herkennung der Leberbeteiligung bei Mukoviszidose Radke C1, Siemers E1, Roderfeld M1, Rath T1, Roeb E1 1 Justus-Liebig-Universit$t Gießen, Gastroenterology (AG Roeb), Gießen, Deutschland Einleitung: Die Mukoviszidose (CF) ist mit einer Inzidenz von ca. 1:2.500 die h"ufigste autosomal- rezessiv vererbte Stoffwechselerkrankung in der kaukasischen Bev#lkerung. Bis zu 30% der CF-Patienten entwickeln im Verlauf eine mit der Erkrankung assoziierte Leberbeteiligung. Ziel der Studie ist die Erarbeitung neuer und einfacher Kriterien f!r die fr!hzeitige Erkennung einer CF-assoziierten Lebererkrankung (CFLD) sowie die Integration der transienten hepatischen Elastografie als pr"diktives diag- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York nostisches Werkzeug. Dazu werden in der vorliegenden Arbeit bestehende Richtlinien mit der Diagnostik mittels transienter hepatischer Elastografie verglichen. Methoden: Aus einer Kohorte von 176 CF-Patienten im Alter von 3 – 52 Jahren wurden nach bestehenden Richtlinien (Debray) [1] (sonographischer Befund, klinische Untersuchung, Laborparameter) Patienten mit einer CF-assoziierten Leberbeteiligung ermittelt. Die entsprechenden Befunde aus diesen Untersuchungen wurden mit den Ergebnissen der transienten hepatischen Elastografie (Fibroscan!) verglichen, bei der ein Cut-off Wert von ‡6,3 kPa [2] zugrunde gelegt wurde. Ergebnisse: Nur 10 der 176 Patienten erf!llten die Einordnungskriterien der CFLD nach Debray [1] und zeigten bereits klinisch Zeichen einer Leberzirrhose. Mit Hilfe der transienten hepatischen Elastografie zeigten 71 der 176 CF- Patienten eine erh#hte Lebersteifigkeit, Median 8,0 (range 6,3 – 75). Die Patienten zeigten keine oder nur teilweise klinische, sonographische oder laborchemische Auff"lligkeiten im Hinblick auf eine CFLD. Zudem wurden signifikante erh#hte Verlaufsdaten der Lebersteifigkeit !ber 4 Jahre ermittelt. Schlussfolgerung: Die bisher genutzten Richtlinien zur Erkennung einer CF-assoziierten Leberbeteiligung weisen Defizite in der fr!hzeitigen Diagnostik auf. Aufgrund der umfangreichen Parameter und der strikten Kriterien k#nnen nicht alle Patienten mit einer CF-assoziierten Leberbeteiligung identifiziert werden. Im Vergleich zur herk#mmlichen Erfassung der CFLD nach Debray stellt die transiente hepatische Elastografie (Fibroscan!) eine nicht invasive Methode mit hoher Spezifit"t zur fr!hzeitigen Detektion einer CF-assoziierten Leberbeteiligung dar. Die Elastografie kann zur Verlaufskontrolle einfach und sicher eingesetzt werden. References: 1. Debray D, Kelly D, Houwen R, Strandvik B, Colombo C (2011) Best practice guidance for the diagnosis and management of cystic fibrosis-associated liver disease. J Cyst Fibros 10 Suppl 2: S 29-S 36. 2. Rath T, Hage L, Kugler M, Menendez MK, Zachoval R, Naehrlich L, Schulz R, Roderfeld M, Roeb E (2013) Serum proteome profiling identifies novel and powerful markers of cystic fibrosis liver disease. PLoS One 8: e58955. Korrespondierender Autor: Radke, Caroline E-Mail: carolineradke@icloud.com 2.27 Visceral Adipose Tissue in NAFLD and NASH Patients is Closely Associated with Liver Injury Schlattjan M1, Wree A1, Sydor S1, Bechmann LP1, Gerken G1, Canbay A1 1 University of Duisburg-Essen, Gastroenterology and Hepatology, Essen, Germany Background and aims: Non-alcoholic fatty liver disease (NAFLD) and the more severe form non-alcoholic steatohepatitis (NASH) is the most common liver disease in western countries. Our aim was to investigate the interaction between adipose tissue and liver in NAFLD and NASH at the time of bariatric surgery. Methods: Visceral adipose tissue, liver tissue and blood samples were obtained from 112 (age median= 45 € 10.4y; 85w/ 27 m) morbidly obese patients undergoing bariatric surgery. Biopsies were scored with NAFLD activity score (NAS) and patients were grouped as NAFL (NAS £ 4) or NASH (NAS > 4). Blood samples taken before surgery were analyzed for parameters of liver injury, M30 (Apoptosis) and M65 (Overall cell death). Visceral adipose tissue and hepatic mRNA levels of genes for inflammasome activity were assessed by qRT PCR. Apoptosis in adipose tissue was quantified via TUNEL staining. Results: NASH patients showed a significant higher concentration of markers for apoptosis and necrosis (M30, M65) in serum. Visceral adipose tissue and hepatic mRNA levels of MCP-1 and IL-18 were both significantly upregulated compared to healthy controls. TUNEL-positive cells in adipose tissue showed a strong correlation with mRNA levels of MCP-1 and IL-18. Conclusions: These results suggest that inflammation in adipose tissue is closely associated with hepatic inflammation and liver injury. These findings help to understand the interaction of adipose tissue in liver injury and may establish future therapies. Corresponding author: Canbay, Ali E-Mail: ali.canbay@uni-due.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 3. Metabolism/Transport 3.1 Identification of eQTLs for hepatic Xbp1 s and Socs3 gene expression in mice fed a high-fat, high caloric diet Sarina P2, Kristy A2, Hall RA1, Lammert F1, Green RM2 1 Saarland University, Department of Medicine II, Homburg, Germany; 2Northwestern University, Department of Medicine II, Chicago, USA Non-alcoholic fatty liver disease (NAFLD) is a highly prevalent form of hepatic disease and feeding mice a High-Fat, High-Caloric (HFHC) diet is a standard model of NAFLD. In order to better understand the genetic basis of NAFLD, we conducted an expression quantitative trait locus (eQTL) analysis of mice fed a HFHC diet. 265 (A/Jx C 57BL/ 6 J) F2 male mice were fed a HFHC diet for 8 weeks. QTL analysis was utilized to identify genomic regions that regulate hepatic gene expression of Xbp1 s and Socs3. We identified two overlapping loci for Xbp1 and Socs3 on Chr 1 (164.0 – 185.4 Mb and 174.4 – 190.5 Mb, respectively) and Chr 11 (41.1 – 73.1 Mb and 44.0 – 68.6 Mb, respectively), and an additional locus for Socs3 on Chr 12 (109.9 – 117.4 Mb). C 57BL/ 6 J-Chr 11A/J/NaJ mice fed a HFHC diet manifested the A/J phenotype of increased Xbp1 s and Socs3 gene expression (p < 0.05), while C 57BL/ 6 J-Chr 1A/J/NaJ mice retained the C 57BL/ 6 phenotype. In addition, we replicated the eQTLs on Chr 1 and 12 (LOD scores ‡ 3.5) using mice from the BXD murine reference panel challenged with CCl4 to induce chronic liver injury and fibrosis. We have identified overlapping eQTLs for Xbp1 and Socs3 on Chr 1 and 11, and consomic mice confirmed that replacing the C 57BL/ 6 with the A/ J Chr 11 resulted in an A/J phenotype for Xbp1 and Socs3 gene expression. Identification of the genes for these eQTLs will lead to a better understanding of the genetic factors responsible for NAFLD and potentially other hepatic diseases. Corresponding author: Lammert, Frank E-Mail: frank.lammert@uks.eu 3.2 Lack of hepatic keap-1 ameliorates steatosis through a negative LXR modulation without altering the innate immune response in a diet-induced model of nonalcoholic steato-hepatitis Ramadori P1, Drescher H1, Schumacher F1, Erschfeld S1, Fragoulis A2, Wruck C2, Trautwein C1, Kroy D1, Streetz K1 1 RWTH University Hospital Aachen, Department of Internal Medicine III, Aachen, Germany; 2RWTH University Hospital Aachen, Institute of Anatomy and Cell Biology, Aachen, Germany Background: Although the generation of reactive oxygen species (ROS) in response to triglyceride accumulation has been classically proposed as a possible “second hit” enabling the progression from simple steatosis to NASH, so far, functional studies failed to demonstrate an indispensable role for oxidative stress in this process. Methods: Hepatocyte-specific keap-1 knockout mice (Keap1Dhepa), over expressing the antioxidant regulator Nrf2, were generated and fed a Methionine-Choline-Deficient (MCD) diet for 4 weeks in order to investigate the influence of Nrf2 activation on hepatic lipid metabolism, liver injury and inflammation as well as fibrosis initiation. Serum and liver samples were collected for biochemical, gene and protein expression analyses. Results: After 4 weeks of MCD treatment the liver/body weight ratio of Keap1Dhepa mice was significantly higher compared to controls with no differences in total body weight. Interestingly, liver histology (HE and ORO) revealed a dramatic reduction of lipid droplets in number and size confirmed by a decreased content of intra-hepatic triglycerides (TG) in Keap1Dhepa. Accordingly, expression of the fatty acids transporter FABP1 and of the lipid droplets-associated proteins, G0S2 and PLIN2, was down-regulated. Whereas total protein levels of the transcription factor PPAR-¡ were unchanged, the expression of Liver X Receptor (LXR-a) was significantly decreased in Keap1Dhepa mice compared to controls. In line with these findings, Cyp7a1 gene expression was dramatically reduced and total circulating and hepatic levels of cholesterol were significantly increased in the same group. TUNEL assay showed a reduced number of apoptotic cells without differences in proliferation (Ki67). Interestingly, protein expression analysis showed an increased phosphorylation of the prosurvival signaling protein Akt and of its downstream target GSK3b. Surprisingly, no difference in inflammatory F4/ 80- and CD 11b-positive cells was detected between the two groups as well as in the expression of two important pro-inflammatory mediators, TNF-a and MCP-1. More- over, pro-fibrogenic expression of a-SMA and col1a1 gene was also not decreased in keap1Dhepa mice. Conclusion: In a diet-induced NASH model, hepatocyte specific keap-1 deletion revealed a beneficial effect on hepatic steatosis through a mechanism possibly involving a negative regulation of the lipogenic transcription factor LXR. On the other hand, constitutive hepatic activation of Nrf2 failed to dampen the inflammatory response induced by administration of MCD diet. Corresponding author: Ramadori, Pierluigi E-Mail: pramadori@ukaachen.de 3.3 Leberspezifischer Glutaminsynthetase-Knockout induziert Hyperammon!mie und oxidativen Stress im Maushirn Qvartskhava N1, Lang P1, Pozdeev V1, G"rg B1, H$ussinger D1 1 Heinrich Heine University Hospital, Department of Gastroenterology, Hepatology and Infectiology, Duesseldorf, Germany Einleitung: Ammoniak spielt eine Schl!sselrolle in der Pathogenese der hepatischen Enzephalopathie (HE). In der Leber wird Ammoniak !berwiegend im Harnstoffzyklus metabolisiert. Residualer, nicht im Harnstoffzyklus entgifteter Ammoniak, wird von einer nachfolgenden periven#s-lokalisierten Hepatozytensubpopulation, den sogenannten „Scavenger Zellen“, mit hoher Affinit"t aufgenommen und von der dort exklusiv exprimierten Glutaminsynthetase f!r die Glutaminsynthese genutzt (H"ussinger 1983, Eur J Biochem; H"ussinger & Gerok 1984, Chem Biol Interact; H"ussinger 1985, J Hepatol; H"ussinger 1990, Biochem J). In der vorliegenden Arbeit wurde die Bedeutung der in der Leber exprimierten Glutaminsynthetase f!r die systemische Ammoniakhom#ostase mit Hilfe einer eigens erstellten leberspezifischen Glutaminsynthetase-Knockout Mauslinie untersucht. Methoden: F!r die Generierung einer leberspezifischen GS-Knockout Mauslinie (AlbCre/GS-LoxP) wurde das Glutaminsynthetase-Gen mit LoxP-Sequenzen im Genom flankiert und die erhaltene Mauslinie mit einer Mauslinie verpaart, die eine Cre-Rekombinase unter Albuminpromoterkontrolle exprimiert. Ergebnisse: Ein leberspezifischer Knockout der Glutaminsynthetase wurde durch Western-Blot- und Immunfluoreszenz-Analysen validiert. Leberspezifische Glutaminsynthetase Knockout-M"use zeigten gegen!ber Wildtyp-M"usen signifikant erh#hte Blutammoniakwerte, aber keine Anzeichen f!r das Vorliegen eine Lebersch"digung, gemessen an der makroskopischen Leberarchitektur und der Aspartataminotransferase- und Alaninaminotransferase-Serumspiegel. Sowohl die Harnstoffkonzentration im Urin und Blut, als auch die Expression der Harnstoffzyklusenzyme OrnithinTranscarbamylase, Argininosuccinat-Lyase und CarbamoylphosphatSynthetase waren in den leberspezifischen GS-Knockout gegen!ber dem Wildtyp unver"ndert. Gegen!ber dem Wildtyp war der leberspezifische Glutaminsynthetase Knockout mit einer verst"rkte zerebrale Oxidation von RNA (8-OHG) und Proteintyrosinnitrierung im Hippocampus, Zerebellum und im somatosensorischen Kortex und eine Beeintr"chtigung von Lokomotion und Verhalten assoziiert. Diskussion: Die vorliegende Untersuchung weist der in den Scavenger-Zellen der Leber exprimierten Glutaminsynthetase eine essentielle Funktion f!r die systemische Ammoniakhom#ostase zu. Die aus dem leberspezifischen Knockout resultierende chronische Hyperammon"mie ist mit der Entstehung von zerebralem oxidativem Stress und einer Beeintr"chtigung von Lokomotion und Verhalten assoziiert. Korrespondierender Autor: Qvartskhava, Natalia E-Mail: natalia.qvartskhava@med.uni-duesseldorf.de 3.4 Expression von Seneszenzbiomarker in mit Ammoniak behandelten kultivierten Astrozyten und in post mortem Hirngewebe von Leberzirrhosepatienten mit hepatischer Enzephalopathie Karababa A1, G"rg B1, H$ussinger D1 1 Heinrich Heine Universit$t, Klinik f!r Gastroentrologie, Hepataologie und Infektiologie, D!sseldorf, Deutschland Einleitung: Die hepatische Enzephalopathie (HE) ist ein im Gefolge eines akuten oder chronischen Leberversagens auftretendes neuropsychiatrisches Syndrom. Sie ist Folge einer astroglialen Hydratationsst#rung und der Ausbildung eines geringgradigen zerebralen *dems, welches eng assoziiert ist mit der zerebralen Bildung von oxidativem und nitrosativem Stress. Astrozyten spielen eine Schl!sselrolle in der Pathogenese der HE und neuere Arbeiten lassen vermuten, dass die Beeintr"chtigung Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A27 A28 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen kognitiver Funktionen bei Zirrhosepatienten nach Aufl#sung einer manifesten HE nicht vollst"ndig reversibel sein k#nnen. Da Astrozytenseneszenz neuronale Funktionen dauerhaft beeintr"chtigen kann, haben wir in mit Ammoniumchlorid stimulierten Astrozytenzellkulturen und in post mortem Hirnbiopsien von Kontrollpatienten und Leberzirrhosepatienten mit und ohne HE etablierte Seneszenzbiomarker analysiert. Ergebnisse: Verglichen mit unbehandelten Kontrollen inhibierte NH4Cl die Proliferation kultivierter Rattenastrozyten zeit- und konzentrationsabh"ngig um bis zu 45 % (5 mmol/l, 72 h) und steigerte gleichzeitig die Aktivit"t der mit Seneszenz-assoziierten b-Galaktosidase, gemessen anhand der Umwandlung der b-Galaktosidase Substrate X-Gal und C 12FDG. Die durch Ammoniak vermittelte Astrozytenproliferationshemmung war assoziiert mit einer verst"rkten Bildung reaktiver Sauerstoffspezies, der Phosphorylierung und nukle"ren Akkumulation des Tumorsuppressorproteins p53 und einer verst"rkten Transkription der zellzyklusinhibitorischen Gene GADD 45a und p21 sowie einer Expressionssteigerung und nukle"ren Akkumulation des p21 Proteins. Die durch Ammoniak-vermittelte p53 Aktivierung, die mRNA Expressionssteigerung von GADD 45a und p21 wie auch die Astrozytenproliferationshemmung waren sensitiv gegen!ber einer Hemmung der Glutaminsynthetase, NADPH-Oxidase und p38MAP Kinase. Die Behandlung kultivierter Astrozyten mit NH4Cl (5 mmol/l, 72 h) verringerte die Expression des EGF-Rezeptors, inhibierte die N-Glykosylierung des BDNF-Rezeptors und hemmte gleichzeitig die durch EGF- und BDNF in unbehandelten Astrozyten induzierbare Proliferation vollst"ndig. Erh#hte mRNA Expressionslevel der Seneszenz-assoziierten Gene GADD 45a, p21 und p53 wurden auch in post mortem Hirnbiopsien von Leberzirrhosepatienten mit HE aber nicht in Zirrhosepatienten ohne HE gefunden. Diskussion: Die vorliegenden Daten zeigen, dass die hepatische Enzephalopathie assoziiert ist mit Astrozytenseneszenz. Korrespondierender Autor: Karababa, Ayse E-Mail: ayse.karababa@hhu.de 3.5 A new modelling approach for Gli transcription factor network in hepatocytes Matz-Soja M1, Schmidt-Heck W2, Guthke R2, Gebhardt R1 1 University Leipzig, Medical Faculty, Biochemistry, Leipzig, Germany; 2Hans Knoell Institute, Leibniz Institute for Natural Product Research and Infection Biology, Jena, Germany Morphogenetic pathways, like the Wnt and Hedgehog are complex systems which organize important processes during development and adulthood. In most of these pathways, positive and negative feedback loops are of considerable importance, because they influence and/or modulate the dynamic behaviour of these pathways. Usually, feedback loops are part of the signalling pathway itself based on the interaction of downstream components (e.g. target gene products) with upstream components in circuits of variable length. In the case of vertebrate Hh signalling the 3 Gli proteins Gli1, Gli1 and Gli3 act as transcriptional activators or, in truncated form, as repressors (Gli2, Gli3) of signalling target genes when Hh is present or absent, respectively. To get more insight into the activity of Hh signalling in the adult liver we performed RNA interference experiments to knock-down the expression of Gli1, Gli2 and Gli3 in cultured hepatocytes. Each Gli siRNA significantly depleted its respective mRNA. Surprisingly, Gli1 siRNA also caused an increase in Gli2 and Gli3 mRNAs, suggesting a negative feedback loop in the regulation of Gli factors in hepatocytes. Gli3 siRNA caused a decrease in Gli1 reflecting a target response rather than an off-target effect. This was also found by Dai et al. 1999, who described that in response to Shh, Gli3 can directly bind to the Gli1 promoter and induce Gli1 mRNA transcription. Thus, the Gli factors seem to form a self-stabilizing network in adult hepatocytes. In order to verify this hypothesis a fuzzy logic based gene regulatory network was created. The network model was represented as a system of difference equations, whereby the time dependent changes of the system are calculated by fuzzy inference systems (FIS). The FIS is a modelling approach mapping the input space of a system (current state) to the output space (alteration of the system in the next time step) using the fuzzy set theory. The FIS uses membership functions of the state variables and rules in order to perform the mapping from input to output variables. The number of membership functions per state variable is present to 3 (low, medium, high). The location of the maximum and the spread of the membership functions were calculated using fuzzy-c-means clustering. The rules describing the input-output behavior were learned with the fuzzy a-priori algorithm. A minimal set of rules with a preset maximum number is chosen under the following criteria that most of the data of training samples could be simulated by Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York the FIS. A total of 11 siRNA knockdown experiments were used to infer the gene regulatory network of the Gli factors in hepatocytes. The inferred gene regulatory network contains a negative feedback regulation between Gli1 and Gli3 and, thus, can confirm the experimental finding by Dai et al. 1999, that Gli3 induce the Gli1 transcription. Furthermore, evidence has been found that a similar network motif also exists between Gli2 and Gli3. A further result of this study indicates slight evidence that there is double positive feedback loop between Gli1 and Gli2. Corresponding author: Matz-Soja, Madlen E-Mail: madlen.matz@medizin.uni-leipzig.de 3.6 A novel function of necroptosis in Non-Alcoholic Steatohepatitis Gautheron J1, Vucur M1, Reisinger F2, Canbay A3, Tacke F1, Trautwein C1, Heikenw$lder M2, Luedde T1 1 RWTH University Hospital Aachen, Department of Gastroenterology, Digestive Diseases and Intensive Care Medicine (Department of Medicine III), Aachen, Germany; 2 Technische Universit$t M!nchen, Institute of Virology and Helmholtz Zentrum M!nchen (HMGU), Munich, Germany; 3 University Duisburg-Essen, Department of Gastroenterology and Hepatology, Essen, Germany Non-alcoholic fatty liver disease represents the most common liver disease in Western countries and often progresses to non-alcoholic steatohepatitis (NASH) leading ultimately to liver fibrosis and hepatocellular carcinoma. The occurrence of hepatocyte cell death – so far characterized as hepatocyte apoptosis – represents a fundamental difference between benign steatosis and progressive steatohepatitis. Recently, it was discovered that RIP3-dependent “necroptosis” represents a novel programmed cell-death-pathway activated in chronically inflamed tissues. This novel pathway is counterbalancing the function of Caspase-8 and apoptosis. Given previous studies suggesting a potential function of apoptosis in NASH, we investigated if necroptosis might play a role in murine and human NASH. Using liver biopsies from well-characterized NASH cohorts from Germany and the UK, we show here that RIP3 is upregulated in human NASH, while – surprisingly – apoptosis of hepatocytes was detected on a very low level in human NASH livers. In the mouse dietary NASH model of Methionin-Cholin-Deficient (MCD) Diet (which was previously used to examine the role of apoptosis in NASH fibrosis), activation of RIP3 promotes liver injury, inflammation, induction of hepatic progenitor cells and ultimately liver fibrosis. Importantly, this deleterious pathway is suppressed by Caspase-8, since mice with deletion of Caspase-8 in parenchymal liver cells showed a massive increase of liver injury and fibrosis, which was mediated through RIP3hyperactivation. This novel function of RIP3 is mediated by activation of Jun-(N)-terminal Kinase (JNK). Inhibition of JNK reduces intra-hepatic level of RIP3 and subsequently liver fibrosis, providing evidence that a positive feedback-loop exists in liver cells between RIP3 and JNK. Moreover, JNK-activation promotes the release of pro-inflammatory mediators like MCP-1 (CCL-2), thereby attracting macrophages to the injured liver and further augmenting RIP3-dependent signaling leading to cell death and subsequently liver fibrosis. Previous studies on the role of apoptosis in the MCD NASH model led to clinical trials on apoptosis inhibitors in human NASH. Our present data provide evidence that necroptosis, a pathway counterbalancing apoptosis, and RIP3 as its master regulator promote NASH-induced liver fibrosis in the well-established MCD model and are upregulated in human NASH patients. This pathway might represent a novel and specific target for pharmacological strategies in the context of fatty liver disease. Moreover, our data provide evidence that targeting Caspase-8 in this context might aggravate liver damage and fibrogenesis since its main function is to counterbalance activation of necroptosis. Corresponding author: Luedde, Tom E-Mail: tluedde@ukaachen.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 3.7 A quantitative metabolomic profiling and corresponding modeling approach of hepatocytes with activated Wnt/ß-Catenin signaling B"ttger J1, Schmidt-Heck W2, Matz-Soja M1, Thiel C1, Hofmann U3, Vlaic S2, Guthke R2, Gebhardt R1 1 University Leipzig, Institute of Biochemistry, Faculty of Medicine, Leipzig, Germany; 2Leibniz Institute for Natural Product Research and Infection Biology, Hans Kn"ll Institute, Jena, Germany; 3Dr. Margarete Fischer-Bosch-Institut f!r Klinische Pharmakologie, Stuttgart, Germany The maintenance of liver homeostasis relies on the metabolic zonation, where pericentral (pc) and periportal (pp) zones differ in their enzyme composition, content and activity. To carry out a metabolic fingerprint along the porto-central axis of the sinusoid is of high relevance for establishing a suitable systems biology approach aiding a better mechanistic understanding of hepatocytes heterogeneity with their different cellular functions. Here, we present a metabolic modeling approach for mouse hepatocytes based on metabolite profiles in the cell and cell culture medium of of APCloxPneo mice, with an over-activated Wnt/bCatenin signaling and control mice, with normal Wnt/b-Catenin activity. The pathway has been shown to play a key role in the functional heterogeneity of hepatocytes and fundamentally influence the metabolic zonation in adult liver. APCloxPneo mice develop an expanded zone of hepatocytes with pericentral functions, due to the partial reduction in the Adenomatous Polyposis Coli protein (APC) expression in hepatocytes. Therefore it is well suited for evaluation of the model. Hepatocytes were isolated and cultivated for up to 48 hours and medium was collected at different time points. The culture medium was analyzed with GC-MS and LC-MS methods for quantitative analyses of the compound classes’ amino acids, bile acids and organic acids. A metabolic model consisting of 42 species and 67 interspecies interactions has been established to analyze the flux distribution patterns in different hepatocyte populations. The software system VANTED (Visualization and Analysis of Networks containing Experimental Data) has been used to interpret the different patterns of metabolites, occurring in various hepatocyte populations. To characterize the functional specialization of hepatocytes clustering with self-organizing maps (SOM) was performed. The flux balance analysis (FBA) was carried out to get a general idea of the metabolic capabilities of different hepatocyte populations. The model has been validated by comparison to published data of pp/pc and APCloxPneo hepatocytes. Conclusion: The model offers a valuable tool for understanding the role of hepatocyte heterogeneity in liver homeostasis under normal conditions and possibly also in diseased states. Further, it could serve as an important sub-module for a multi-scale liver model of the cellular metabolism bridging single-cell metabolism to the tissue and the whole-organ level. Corresponding author: B#ttger, Jan E-Mail: jan.boettger@medizin.uni-leipzig.de 3.8 Bcl-3 reguliert die hepatische Lipo- und Gluconeogenese in einem murinen, hochkalorischen F"tterungsmodell der nicht-alkoholischen Fettlebererkrankung (NAFLD) Gehrke N1, Mann A1, Alt Y1, Schad A2, Waisman A3, H"velmeyer N3, Galle PR1, W"rns MA1, Schattenberg JM1 1 Johannes Gutenberg University, I. Department of Medicine, Mainz, Germany; 2Johannes Gutenberg University, Institute of Pathology, Mainz, Germany; 3Johannes Gutenberg University, Department of Immunology, Mainz, Germany Einleitung: B cell leukemia-3 (Bcl-3) – urspr!nglich als Produkt des bcl-3 Protoonkogens identifiziert – ist ein nukle"res und zytoplasmatisch exprimiertes Protein der IkappaB-Familie, das Gewebe- und Modellabh"ngig als Co-Aktivator oder Repressor der NF-kappaB Untereinheiten p50 oder p52 wirkt. Die Rolle von Bcl-3 in der NAFLD sowie der damit assoziierte metabolische Ph"notyp sind bislang v#llig unklar. Daher haben wir die Regulation der hepatischen Lipo- und Gluconeogenese durch Bcl-3 und deren molekulare Mechanismen in einem murinen, hochkalorischen F!tterungsmodell der NAFLD untersucht. Methoden: M"nnliche M"use, die bcl-3 unter Kontrolle der Cre-Rekombinase Leberspezifisch !berexprimieren (alfp-Cre x bcl-3, Bcl-3hepar), und entsprechende Wildtyp-Kontrollen im Alter von 8 – 12 Wochen wurden !ber 12 Wochen mit einer Hochfett- (HFD; 35,5% Fett) oder einer angepassten Kontroll-Di"t (KD; 5,4 % Fett) gef!ttert. Zus"tzlich wurde das Trinkwas- ser der M"use auf HFD mit Fructose (55 %) und Glucose (45%) angereichert. In den experimentellen Gruppen wurden w#chentlich biometrische Daten (K#rpergewicht, Futter- und Trinkmengenverbrauch) gemessen. Nach Abschluss der F!tterung erfolgten Blut- und Gewebeentnahmen f!r serologische, histologische, qRT-PCR-, Western Blot- und FACSAnalysen. Ergebnisse: Nach 12-w#chiger F!tterung der HFD entwickelten die M"use &bergewicht, das durch die &berexpression von Bcl-3 in der Leber verst"rkt wurde. Dar!ber hinaus f!hrte die HFD zu signifikant erh#hten Werten der Alanin-Aminotransferase (ALAT), der Triglyceride, des Gesamt-Cholesterins, der N!chternglucose sowie des N!chterninsulins, begleitet von einer Zunahme des relativen Lebergewichts sowie hepatischer Steatose. In Bcl-3hepar M"usen auf HFD waren ALAT und N!chterninsulin allerdings signifikant h#her als im Wildtyp. Gleichzeitg war die Expression des Insulinrezeptors sowie der Insulinrezeptorsubstrate (IRS)-3 und -4 im Lebergewebe von Bcl-3hepar M"usen herabreguliert, wohingegen IRS-1 und -2 in beiden Genotypen gleichermaßen durch die HFD reguliert wurden. Die Phosphorylierung der Serin-Threonin-Kinase Akt war hingegen verst"rkt. Bei der Untersuchung von Schl!sselregulatoren der hepatischen Lipo- und Gluconeogenese zeigte sich eine signifikante Herabregulation der Phosphoenolpyruvat-Carboxykinase (PEPCK), der Fructose-1,6-bisphosphatase (FBP1) und der Glucose-6-Phosphatase (G6P) in Bcl-3hepar M"usen auf HFD im Vergleich zum Wildtyp. Gleichzeitig war die Expression von Regulatoren der hepatischen de novo-Lipidsynthese, darunter ACC, FAS und SREBP-1, hochreguliert, wohingegen Aktivatoren der beta-Oxidation wie CPT1, PPARalpha und -gamma sowie dessen Regulator PGC-1alpha herabreguliert waren. Zusammenfassung: Der Regulator zellul"ren &berlebens und hepatischer Inflammation Bcl-3 verst"rkt direkt den metabolischen und inflammatorischen Ph"notyp einer NAFLD unter Ausbildung einer Insulinresistenz und k#nnte folglich ein wichtiges Zielprotein f!r die Entwicklung neuer Therapieans"tze sein. Korrespondierender Autor: Gehrke, Nadine E-Mail: NadineGehrke@gmx.net 3.9 Cooperation of Hedgehog and Wnt/b-Catenin signalling in regulation of steroidogenesis in the liver Rennert C1, Aleithe S1, B"ttger J1, Matz-Soja M1, Gebhardt R1 1 Leipzig University, Faculty of Medicine, Institute of Biochemistry, Leipzig, Germany The idea of personalised medicine was focused over the last years, which lead to a growing interest in sex-specific research. Thereby regulation of steroidogenesis is a central aspect. The liver has multiple functions, which can be realised simultaneously only by zonation. Recent studies showed that Hedgehog (Hh) and Wnt/b-Catenin (Wnt) signalling, two morphogenic pathways commonly associated with embryogenesis, development and cancer are active in adult hepatocytes and act as master regulators of zonation in the adult liver [1]. We investigate the specific role of those pathways in two transgenic mouse models. One of them has an inactivated Hh signalling by a hepatocyte-specific knockout (KO) of Smoothened, a key protein of the pathway [2]. The second model, APCloxPneo, has an over-activated Wnt pathway due to partial reduced protein expression of its major repressing element APC, which leads to an extended pericentral zone [1]. Surprisingly we observed alterations in steroidogenesis gene expression in the transgenic mice; yet it was assumed that steroidogenesis occurs in the liver only during embryogenesis and is down-regulated afterwards. To verify which components of the signalling cascades are involved in regulation of steroidogenesis, we performed different RNA interference (KD) experiments in cultivated hepatocytes of C 57BL/ 6N mice and quantified expression levels by qRT-PCR. So far we examined the expression of estrogen receptor (Esr1) and a couple of steroidogenesis associated genes. The varying expression of Cyp17a1, a central regulator of steroidogenesis, is conspicuous. Cyp17a1 expression is activated by estradiol incubation and significantly correlates with Esr1 expression. In the APCloxPneo mouse model Cyp17a1 is significantly down-regulated. However, no changes in steroidogenesis gene expression are observed due to siRNA mediated Apc KD. In contrast, the Hh KO in hepatocytes results in increasing Cyp17a1 expression, which is supported by equal results, provided by an in vitro KD of Gli3, one of the transcription factors of active Hh signalling. These results clearly demonstrate that Cyp17a1 expression in liver is controlled by estradiol level and modulated by aberrant Wnt and Hh signalling. Thereby Hh pathway seems to be the primary effector, while regulation by Wnt signalling may be indirectly through altered Hh signalling. This is supported by further studies, showing that Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A29 A30 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen modulation of one of the signalling pathways causes a time-delayed change in the other one and vice versa. Thus, under pathological conditions the liver may acquire an important role in altering systemic levels of steroid hormones, in particular since we found no changes of Cyp17a1 expression in both, ovaries and kidney cortex of the Hh KO mice. Further studies will focus on additional mechanistic details of the altered regulation of steroidogenesis and are directed to reveal possible physiological consequences of these unexpected changes. References: [1] Gebhardt & Matz-Soja, WJG, 2014 [2] Matz-Soja et al., CCS, 2014 Corresponding author: Rennert, Christiane E-Mail: christiane.rennert2@medizin.uni-leipzig.de Cytotoxicity of anisidine in hepatic cell lines 3.10 3.12 Caliskan S1, Wewering F1, Gerding B1, Luch A1, Zellmer S1 1 German Federal Institute for Risk Assessment (BfR), Department of Chemicals and Product Safety, Berlin, Germany Humans are exposed to azo dyes and its degradation products like aromatic amines through different consumer product. The ECHA classified the aromatic amine o-anisidine as carcinogen (Carc. 1B) and mutagen (Muta 2) due to increased rates of bladder and kidney tumors in mice and rats. In contrast, p-anisidine was classified with specific organ toxicity (STOT RE 2) only. Hepatotoxic effects of o- and p-anisidine were studied using HepG2 and Huh-7 cells. Cells were grown in DMEM (Huh7) or RPMI medium (HepG2), supplemented with 10 % FCS, 5 mM Lglutamine, 100 U/ml penicillin and 0.1 mg/ml streptomycin. EC50 values were determined using the MTT assay, reactive oxygen species (ROS) were detected using 2’,7’-dichlorodihydrofluorescein diacetate (H2DCFDA), and changes in the gene expression were quantified using PCR. In HepG2 cells the EC50 values were 16 € 1 mM and 18 € 1 mM for o- and p-anisidine, respectively. However, in Huh 7 cells EC50 values were 11 € 1 mM and 16 € 1 mM for o- and p-anisidine, respectively. At 1 mM both anisidine isomers induced the generation of ROS in either cell line, which could be suppressed by adding N-acetylcysteine. Moreover, the carcinogenic o-anisidine upregulated the expression of CYP1A1 and NQO1 in both cell lines and TNFa in HepG2 cells. While tumors mainly occur in kidney and bladder tissues, our study shows that human hepatic cells are as well significantly affected by o-anisidine with regard to ROS induction and altered gene expression and – to a lesser extent – also by p-anisidine. Corresponding author: Zellmer, Sebastian E-Mail: sebastian.zellmer@bfr.bund.de 3.11 fore substantially differs from ligand-mediated endocytosis. The in vivo relevance of this novel regulatory mechanism to fine-tune IL-6 responses is currently been analyzed in newly generated endocytosis-deficient gp130 knock-in mice. Conclusion: Our data imply differential routing of gp130 depending on the individual stimulus and cell type which might have far reaching consequences for the control of the cytokine signalling strength during inflammatory processes. Corresponding author: Hermanns, Heike M E-Mail: Hermanns_H@ukw.de Endocytosis of the signal transducing receptor gp130 as mechanism to fine-tune IL-6 responses Hermanns HM1, Mais C2, Walter S2, Geier A1 1 University Hospital W!rzburg, Depatment of Hepatology, W!rzburg, Germany; 2University of W!rzburg, Rudolf Virchow Center, W!rzburg, Germany Background and aims: The restriction of cytokine signalling in strength and duration is of fundamental importance to limit inflammation. We identified a cross-talk mediated endocytosis by which pro-inflammatory stimuli can influence the responsiveness of liver cells for cytokines of the IL-6 family. Methods: HepG2 hepatoma cells were treated with the pro-inflammatory cytokine IL-1b for different periods of time. IL-1bmediated signalling was characterized by Western blotting. Cell surface expression of gp130 was analyzed by flow cytometry and live cell imaging. To identify the signalling pathway responsible for the IL-1bmediated endocytosis of gp130 site-directed mutagenesis and siRNA technology were used. The impact of reduced cell surface expression of gp130 on acute-phase protein expression was determined by reporter gene assay and qPCR. The in vivo relevance of this cross-talk mediated endocytosis of gp130 was addressed by the generation of a gp130 knockin mouse line carrying a point mutation in the gp130 di-leucine internalization motif. Results: IL-1b pretreatment of HepG2 hepatoma cells impaired IL-6-induced JAK/STAT signaling through serine phosphorylation of the common cytokine receptor subunit gp130 and its subsequent internalization and degradation. Investigation of the underlying molecular mechanism identified the activation of the p38/MK2 kinase axis as crucial step. Consequently, inhibition of p38 or MK2, deletion of MK2 or mutation of crucial amino acids within the MK2 target site or the dileucine internalization motif blocked receptor depletion and restored IL6-dependent STAT activation as well as acute phase gene induction. The endocytosis process is mediated via clathrin-coated vesicles and there- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York Enhanced Phenobarbital-induced Thyroid Hormone Breakdown in Hepatocytes by Benzo[a]pyren-dependent Induction of the Constitutive Androstane Receptor Schraplau A1, Schewe B1, Neusch$fer-Rube F1, Ringel S1, Neuber C2, Kleuser B2, P!schel GP1 1 University of Potsdam, Institute of Nutritional Science, Nutritional Biochemistry, Nuthetal, Germany; 2University of Potsdam, Institute of Nutritional Science, Nutritional Toxicology, Nuthetal, Germany Introduction: Xenobiotic exposure has been discussed as a possible contributor to the obesity epidemic. Amongst others, xenobiotics may reduce the metabolic rate because they interfere with the hypothalamicpituitary-thyroid endocrine axis by inducing enzymes that inactivate thyroid hormones. This induction results from an activation of xenosensing nuclear receptors in the liver. The Constitutive Androstane Receptor (CAR, NR1I3) is a xenobiotic-responsive nuclear receptor, which is also involved in the energy homeostasis regulation. The activation of CAR and its target genes leads to an enhanced hepatic thyroid hormone degradation. A possible interaction of CAR with another nuclear receptor, the Aryl hydrocarbon Receptor (AhR) and the resulting effects on the thyroid hormone turnover were investigated. Methods: Primary rat hepatocytes were incubated with the CAR activator Phenobarbital and the AhR ligand Benzo[a]pyrene. After 48 h, the gene expression of CAR and its target genes was measured by RT-qPCR. The CAR promoter activation was studied by luciferase reporter gene assay. After xenobiotic-pretreatment, the hepatocytes were incubated with T3 or T4 and thyroid hormone-degradation and thyroid hormone-glucuronide formation were analyzed by LC-MS/MS. Results: The induction of the nuclear receptor CAR by the polycyclic aromatic hydrocarbon Benzo[a]pyrene, a frequent contaminant of processed food, enhanced the Phenobarbitaldependent induction of phase I and II enzymes and as a consequence thyroid hormone inactivation. Benzo[a]pyrene activated the promoter and induced the expression of CAR in rat hepatocytes dose-dependently. It thereby enhanced the Phenobarbital-dependent induction of the prototypic CAR target gene Cyp2b1 as well as the Phenobarbital-dependent induction of the UDP-glucuronosyltransferases Ugt1a6, Ugt1a8 and Ugt1a10. The induction by the combination of both xenobiotics was more than additive. By inducing CAR, Benzo[a]pyrene enhanced the Phenobarbital-dependent reduction of thyroid hormone half-life and the Phenobarbital-dependent increase in the rate of thyroid hormone glucuronide formation in hepatocyte cultures. Discussion: Aryl-hydrocarbon receptor ligands might thus augment the endocrine disrupting potential of CAR activators by an induction of CAR and by enhancing the CAR activator-dependent increase in hepatic thyroid hormone inactivation. A combination of AhR and CAR activators could result in a larger decrease in energy turnover than single exposure. Hence, exposure to xenobiotic mixes might contribute more to the development of obesity and metabolic diseases than would be deduced from the isolated impact of their individual components. Corresponding author: Schraplau, Anne E-Mail: anne.schraplau@uni-potsdam.de 3.13 ERK and p38 activation are central mediators of irinotecan-induced steatohepatitis Mahli A1, Saugspier M1, Thasler WE2, M!ller M1, Hellerbrand C1 1 University Hospital Regensburg, Department of Internal Medicine I, Regensburg, Germany; 2Ludwig Maximilians University, Department of Surgery, Großhadern Hospital, Munich, Germany Preoperative chemotherapy for hepatic resection of colorectal liver metastases is associated with the development of chemotherapy-associated steatohepatitis (CASH) which increases the risk of perioperative morbid- 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen ity and mortality. The aim of this study was to unravel the molecular mechanisms of this phenomenon. Methods and Results: Initially, we determined the dose-range in which irinotecan treatment did not affect the viability of hepatoma cells and primary human hepatocytes. In this dose-range (up to 50 mM), irinotecan dose-dependently induced lipid accumulation and pro-inflammatory gene expression. Furthermore, irinotecan induced the accumulation of free fatty acids, the formation of reactive oxygen species (ROS) and ERK-activation. Pre-incubation with ROS-scavengers or ERK-inhibitor almost completely inhibited irinotecan-induced inflammatory gene expression but had only a slight effect on lipid accumulation. Moreover and surprisingly, we observed a significant inhibition of ATG7 and VSP34 expression accompanied by lower LC 3II/I ratio and increased p62 protein levels indicative of reduced autophagy, a cellular mechanism known to affect cellular lipid homeostasis. MAPK p38 is a known inhibitor of autophagy and we found that irinotecan induced p38 activation while pretreatment with a p38 inhibitor diminished irinotecan effects on autophagy. To establish an in vivo CASH model, we injected mice with irinotecan (50 mg/kg all 3 days) for 2 weeks, leading to significant hepatic steatosis, ROS-formation and inflammation. Also in this in vivo model as well as in liver tissue samples of irinotecan-treated patients we observed a significant induction of ERK- and p38-activation and a marked reduction of markers of autophagy in comparison to normal liver tissue. Conclusion: ERK and p38 activation are critical mediators of irinotecan-induced steatohepatitis which suggests inhibition of these pathways as promosing therapeutic regime for prevention of CASH. Corresponding author: Mahli, Abdo E-Mail: abdo.mahli@ukr.de 3.14 Experimental validation of the predicted TGR5 binding mode model Spomer L1, Gertzen CGW2, H$ussinger D1, Gohlke H2, Keitel V1 1 Heinrich Heine University, Department of Gastroenterology, Hepatology and Infectiology, Duesseldorf, Germany; 2 Heinrich Heine University, Institute of Pharmaceutical and Medical Chemistry, Duesseldorf, Germany Introduction: TGR5 (Gpbar-1) is a G-protein coupled, membrane-bound bile acid receptor, which is expressed in many human tissues. In the liver TGR5 mediated anti-inflammatory, choleretic and anti-apoptotic effects. Furthermore, the receptor has been linked to bile acid and glucose homeostasis, energy expenditure and inflammatory pathways. Thus, it is conceivable that TGR5 agonists can mediate protective effects in various liver and metabolic diseases. Aim of the present study is the development of a TGR5 structure-function model and a computational and experimental characterization of the ligand binding pocket allow the search for new, specific TGR5 agonists and antagonists. Methods: 3D structure predictions of the TGR5 receptor were made using homology modelling, furthermore the binding mode of the most potent bile acid ligand, taurolithocholat TLC, was analyzed by molecular docking (Gertzen/Gohlke). This binding mode could be confirmed with a 3D structure-activity relationship analysis (3D-QSAR) with 67 TGR5 ligands (Gertzen/Gohlke). The experimental validation was carried out with the help of TGR5 mutations at positions that show significant interactions with TLC in the predicted binding model. TGR5 variations were introduced into TGR5-cDNA constructs by site-directed mutagenesis. TGR5 function was analyzed through co-transfection of HEK293 cells with TGR5 and a cAMP-sensitive luciferase reporter gene construct. Impact on receptor localization was determined by immunofluorescence microscopy and FACS analysis. Results: The structure-based model of the TGR5 binding mode, predicted reduced affinity when residues Arg79, Tyr89, Glu169 and Leu244 where mutated, while variation of Tyr240 showed complete loss of function. This was confirmed in mutagenesis studies in transfected HEK293 cells. The model demonstrates no necessary interaction of Ser21 with TLC, which could also be confirmed experimentally. All mutations are correctly localized in the plasma membrane of transfected cells. Discussion: Mutation of essential residues for TGR5 ligand binding as predicted by a structure-based binding model showed reduced functional activity, which provides strong support for the suggested binding mode of TGR5 agonists. This offers new possibilities to identify not only novel TGR5 agonists but also potential TGR5 antagonists. Corresponding author: Spomer, Lina E-Mail: lina.spomer@hhu.de 3.15 Expression des Multidrug Resistance Protein 4 in mit Ammoniak behandelten kultivierten Rattenastrozyten und in post mortem Hirnproben von Leberzirrhosepatienten mit HE J"rdens M1, G"rg B1, Keitel V1, H$ussinger D1 1 Heinrich Heine University, Department of Gastroenterology, Hepatology and Infectiology, Duesseldorf, Germany Einleitung: Das Multidrug Resistance Protein 4 (Mrp4) ist ein Mitglied der ATP-binding cassette (ABC) Transporter Familie. Es wird insbesondere in Organen mit Barrierefunktion exprimiert und wird im menschlichen Gehirn von Endothelzellen, Neuronen, Mikroglia und Astrozyten exprimiert. Der Mrp4 transportiert unterschiedliche Substrate wie z.B. die in die Pathogenese der hepatischen Enzephalopathie (HE) involvierten zyklischen Nukleotide. Wir haben daher das Expressionsniveau des Mrp4 in mit Ammoniak behandelten kultivierten Rattenastrozyten und in humanen post mortem Hirnproben von Leberzirrhosepatienten mit und ohne HE untersucht. Ergebnisse: Die Behandlung kultivierter Rattenastrozyten mit NH4Cl steigerte zeit- und konzentrationsabh"ngig das Expressionsniveau und inhibierte gleichzeitig die N-Glykosylierung des Mrp4 Proteins. W"hrend sowohl die Expressionssteigerung wie auch die Glykosylierungsst#rung des Mrp4 in mit NH4Cl (5 mmol/l)-behandelten Rattenastrozyten durch den Glutaminsynthetasehemmstoff MethioninSulfoximin (MSO) verhindert werden konnten, blockierte die Hemmung des Transkriptionsfaktors PPARa mit GW6471 lediglich die durch Ammoniak induzierbare Expressionssteigerung des Mrp4 Proteins. Die Heraufregulation und Glykosylierungsst#rung des Mrp4 Proteins wurde begleitet von einer gegen!ber MSO sensitiven Expressionssteigerung von BiP, einem Surrogatmarker f!r Stress im endplasmatischem Retikulum (ER). In humanen post mortem Hirnproben wurden sowohl gesteigerte mRNA- wie auch Proteinexpressionslevel des Mrp4 bei Leberzirrhosepatienten mit HE aber nicht bei Leberzirrhosepatienten ohne HE gegen!ber der Kontrollgruppe nachgewiesen. Diskussion: Unsere Untersuchungen zeigen, dass Ammoniak in kultivierten Rattenastrozyten PPARa-vermittelt und glutaminsyntheseabh"ngig die Expression des Mrp4 Proteins steigert. Gleichzeitig induziert Ammoniak glutaminsyntheseabh"ngig ER-Stress, welcher assoziiert ist mit einer Hemmung der N-Glykosylierung des Mrp4 Proteins. Die in post mortem Hirnproben von Leberzirrhosepatienten mit HE aber nicht ohne HE gefundene Expressionssteigerung der Mrp4 mRNA und des Proteins weisen auf eine Beteiligung des Mrp4 in der Pathogenese der HE. Korrespondierender Autor: J#rdens, Markus E-Mail: markus.joerdens@med.uni-duesseldorf.de 3.16 Identification and proteomic profiling of biliary exosomes Rupp C1, Rupp AK2, Sauer P1, Bode KA3, Leopold Y1, Kloeters-Plachky P1, Weiss KH1, Altevogt P2, Stremmel W1, Gotthardt DN1 1 University Hospital Heidelberg, Internal Medicine IV, Heidelberg, Germany; 2German Cancer Research Center, Tumor Immunology Program, D015, Heidelberg, Germany; 3 University of Heidelberg, Department of Infectious Diseases, Medical Microbiology and Hygiene, Heidelberg, Germany Background & Aims: In previous studies the biliary proteome has been analyzed, showing a distinct set of proteins to be abundantly present in the bile fluid. Within these proteins there was a considerable amount of membranous and cytosolic proteins indicating a vesicular form of protein excretion within the biliary tract. We aimed to identify the possible secretion of exosomes into the bile fluid and characterize their biochemical and proteomic constitution. Methods: Bile fluid of patients admitted to ERC due to the presence of choledocholithiasis in absent of clinical and laboratory signs of cholangitis were collected during routine ERC. We isolated microvesicles by using gradual centrifugation and further purification by floating onto a sucrose gradient. Isolated vesicles were further characterized by Western Blotting, Electron microscopy, Nanoparticle Tracking Analysis and mass spectrometry. Results: In bile fluid of microvesicles with a size of 50 – 90 nm could be regularly detected. In these vesicles exosomal markers like CD9, ADAM10 and HSP70 could be detected. Furthermore electron microscopy revealed cup shaped vesicles indicating the presence of exosomes in human bile fluid. The proteomic analysis of biliary exosomes showed more than 400 nonredundant proteins, of which more than 100 have not been detected in exosomes before as listed by the exosome database ExoCarta. Among these proteins are e.g. Annexin 10, CEACAM6, CEACAM7, as well as tet- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A31 A32 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen raspanins and mucins. Conclusion: Microvesicles isolated from human bile fluid display any characteristics of exosomes. Their hepatobiliary origin afford them as a new diagnostic tool to gain further insight into the pathogenesis of biliary and cholestatic diseases. Corresponding author: Rupp, Christian E-Mail: christian.rupp@med.uni-heidelberg.de 3.17 Identification of cytochrome CYP2E1 as critical mediator of alcohol effects on steatotic hepatocytes Mahli A1, Thasler WE2, M!ller M1, Seitz HK3, Cederbaum AI4, Hellerbrand C1 1 University Hospital Regensburg, Internal Medicine I, Regensburg, Germany; 2Ludwig-Maximilians-University, Grosshadern Tissue Bank and Center for Liver Cell Research, Munich, Germany; 3Heidelberg, Medicine (Gastroenterogy), Salem Medical Centre, Heidelberg, Germany; 4Icahn School of Medicine at Mount Sinai, Pharmacology and Systems Therapeutics, New York, USA Background & Aims: Several clinical studies proposed a strong causative link between the consumption of alcohol and progressive liver disease in obese individuals. However, it is incompletely understood how alcohol and obesity interact and whether the combined pathological effects are additive or synergistic. Here, we aimed to establish an in vitro model for joint effects of alcohol and steatosis in hepatocytes. Methods and Results: Lipid accumulation in primary human hepatocytes was induced by incubation with the fatty acid oleate. Subsequently, steatotic and control hepatocytes were incubated with up to 50 mM alcohol. In this dose range alcohol alone had only a minimal effect but significantly enhanced oleate induced lipogenesis and cellular triglyceride content, as well as lipid peroxidation, oxidative stress and NFkappaB-mediated pro-inflammatory gene expression. CYP2E1 inhibition or reactive oxygen species scavengers blunted these synergistic pathological effects of alcohol and steatosis. Moreover, under the experimental conditions used, alcohol induced autophagy in steatotic but not in control hepatocytes, and also this synergistic effect was mediated via CYP2E1. Further induction of autophagy ameliorated the joint effect of alcohol and oleate stimulation on cellular lipid accumulation and inflammatory gene expression while inhibition of autophagy further enhanced the dual pathological effects. Conclusion: Our model indicates that alcohol and steatosis synergistically induce pathological as well as protective mechanisms in hepatocytes via CYP2E1. These findings may have important implications for the prognosis and treatment of alcoholic liver disease particularly in obese individuals. Corresponding author: Mahli, Abdo E-Mail: abdo.mahli@ukr.de 3.18 Inhibition of the transcriptional regulation of CDCA-induced BSEP expression by IL-1b involves the IL-1b triggered activation of autocrine chemokine circuits Missing L1, H$ussinger D1, Bode JG1* 1 Heinrich-Heine University Hospital, Department of Gastroenterology, Hepatology and Infectiology, Duesseldorf, Germany * corresponding author Introduction: The liver as central regulator of multiple metabolic processes is indispensable for proper systemic function and survival. One important function is the synthesis and transport of bile acids for lipid digestion and adsorption. The malfunction of this machinery leads to accumulation of cytotoxic bile acids in hepatocytes and a subsequent severe damage of the liver. Modulation of transcriptional programs for bile acid homeostasis is achieved by activation of nuclear receptors such as the farnesoid X receptor (FXR), which plays a key role in bile synthesis, secretion, and detoxification by regulation of transporter expression levels in the polarized hepatocytes. Thereby the bile salt export pump BSEP is critical for the transport of bile salts from the hepatocyte into the canaliculus. Its expression is mainly controlled by CDCA stimulated activation of FXR. The inhibition of the expression of BSEP by inflammatory cytokines such as IL-1b has been identified as a critical factor for the development of cholestasis under septic conditions or LPS-inducible inflammation. The molecular mechanisms, which are responsible for down-regulation of BSEP expression by inflammatory factors, are incompletely understood. Objectives – The present study analysis the role of chemokine circuits and its intra-cellular signal- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York transduction for the inhibition of the transcriptional regulation of CDCA induced BSEP expression in primary murine hepatocytes and the human hepatoma cell line HepaRG which displays several characteristics of polarized hepatocytes. Materials and Methods: The study involves transcriptional analysis of BSEP expression in primary hepatocytes from 8 – 12 week old C 57 /BL 6 J male mice and the well-established human hepatoma cell line HepaRG. The cells were grown in Sandwich or Monolayer culture and treated with IL 1b, CDCA and the CXCR2 Inhibitor SB225002 in a cell culture based stimulation assay for defined periods of time. Results – The time resolved analysis of the concentration dependent effects of IL-1b on CDCA-inducible expression of the BSEP gene indicates that even concentrations of less than 0.1 ng/ml of IL-1b efficiently suppress expression of the BSEP gene. The inhibitory effect of IL1b on BSEP gene expression can be partially resolved by inhibition of the CXCR2 receptor. These data suggest that inhibition of CDCA-inducible BSEP expression by IL-1b involves an autocrine circuit mediated via production of CXCR2 ligands. Indeed the analysis of the expression of the CXCR2 ligands CXCL1, 2 and 3 indicates that IL-1b induces the expression of these ligands in hepatocytes. Conclusion: In summary the data suggest that the inhibitory effects of IL 1b on BSEP gene expression are at least part due to autocrine effects of CXCR2 ligands released from hepatocytes upon exposure to IL-1b. Corresponding author: Bode, Johannes G. E-Mail: johannes.bode@med.uni-duesseldorf.de 3.19 Laser ablation inductively coupled plasma mass spectrometry (LA-ICP-MS) in trace metal imaging of experimental and clinical metal disorders Uerlings R1, Boaru SG1, Weiskirchen S1, Zimmermann A2, Matusch A3, Merle U4, Stremmel W4, Weiskirchen R1 1 RWTH University Hospital Aachen, Institute of Molecular Pathobiochemistry, Experimental Gene Therapy and Clinical Chemistry, Aachen, Germany; 2Forschungszentrum J!lich (FZJ), Zentralinstitut f!r Engineering, Elektronik und Analytik, Analytik (ZEA-3), J!lich, Germany; 3 Forschungszentrum J!lich (FZJ), Institute for Neuroscience and Medicine (INM-2), J!lich, Germany; 4University Clinics of Heidelberg, Department of Internal Medicine IV, Heidelberg, Germany Background: The liver is sensitively prone to alterations in metal content and homeostasis. Most of its metabolic and catabolic functions depend on trace elements. Metals are either integral part of enzymes, cofactors, or directly serve as chemical catalysts. Therefore, a lack of trace elements can lead to organ failure or systemic illness. Conversely, excessive hepatic trace element deposition resulting from genetic disorders, intoxication, extensive dietary supply, or long-term parenteral nutrition cause hepatic inflammation, fibrosis, cirrhosis, and hepatocellular carcinoma. Material and Methods: We have recently established novel LA-ICP-MS-based protocols allowing quantitative biometal imaging in human and murine livers or other specimens [1 – 4]. We now extended these studies and provide a multitude of other examples in which these protocols were applied for metal quantification in liver sections taken from clinical cases and experimental models of hepatic metal disorders. Results: Sample preparation and quantification strategies were optimized for application of LA-ICP-MS in daily routine. To evaluate these protocols we have measured clinical samples taken from patients suffering from various metal disorders (e.g. hemochromatosis and Wilson’s disease). In addition, we demonstrate that LA-ICP-MS is an effective tool to image the dynamic changes of various metals and metalloids and their mutual influence on each other during initiation of acute phase response in the liver. Conclusions: In summary, we demonstrate that LA-ICP-MS is an innovative technique that allows accurate biometal imaging with high sensitivity, spatial resolution, specificity, and quantification ability in diagnostic and hepatology research. References cited: [1] M-M P et al. PLoS One 2013;8(3):e58702. [2] M-M P et al. Int J Mass Spectrom. 2013;354 – 355: 281 – 287. [3] Boaru SG et al. BMC Neurosci. 2014;15(1):98. [4] Boaru SG et al. J. Cell. Mol. Med., in press. Corresponding author: Weiskirchen, Ralf E-Mail: rweiskirchen@ukaachen.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 3.20 Lysophosphatidylcholine (LPC) as central player for hepatic fat accumulation and inflammation: implication for the pathogenesis of NASH Stremmel WR1, Staffer S1, Wannhoff A1, Pathil-Warth A1, Chamulitrat W1 1 University Clinics of Heidelberg, Dept. of Internal Medicine, Department IV, Heidelberg, Germany Background: In NASH the intracellular ratio of phosphatidylcholine (PC): lysophosphatidylcholine (LPC) is decreased due to activation of the membrane localized phospholipase A2 (iPLA2ß). Aim: Evaluation of LPC levels in development and reversal of hepatic fat accumulation and inflammation. Methods: In HepG2 cells the bile acid-phospholipid conjugate ursodeoxycholate-lysophosphatidylethanolamide (UDCA-LPE) as iPLA2ß inhibitor was used to modify intracellular LPC levels. We examined the impact of LPC on JNK1-p and transcription of the heterotetrameric fatty acid transport complex constituted of CD36, FABPPM, caveolin1 and iPLA2ß. A NASH phenotype was generated by exposure of HepG2 cells with high concentrations of oleate bound to albumin (4:1) for 3 h. Results: Addition of 1 – 10 mM LPC to delipidated cytosolic extracts revealed a dose dependent increase of JNK1-p as key promoter of fatty acid metabolism and lipoapoptosis. In vitro transcription with native HepG2 nuclear extracts exposed to these LPC conditioned cytosolic samples resulted in synthesis stimulation of all members of the fatty acid uptake complex. In contrast, the NASH phenotype was reversed or prevented by incubation with the iPLA2ß inhibitor UDCA-LPE (1 h, 100 mM) suppressing cytosolic LPC levels. Accordingly JNK1-p and transcription of fatty acid transporter biosynthesis were reduced, concomitantly with disappearance of lipid droplets, triglyceride accumulation and LDH release in the medium. Conclusion: iPLA2ß mediated generation of LPC represents a central regulator for hepatic steatosis and inflammation via JNK1-p. Inhibition of iPLA2ß by the nontoxic UDCA-LPE could be an ideal therapeutic strategy against NASH. Corresponding author: Stremmel, Wolfgang R. E-Mail: wolfgang.stremmel@med.uni-heidelberg.de 3.21 Neue Aspekte der Regulation des Lipidmetabolismus w!hrend der Entstehung von NAFDL Arnold K1, Thiel C1, Marbach E1, B"ttger J1, Matz-Soja M1, Sales S2, Shevchenko A2, Gebhardt R1 1 Universit$t Leipzig, Institut f!r Biochemie, Medizinische Fakult$t, Leipzig, Deutschland; 2Max-Planck-Institut f!r molekulare Zellbiologie und Genetik, Dresden, Deutschland In der westlichen &berflussgesellschaft, die h"ufig von falschen Ern"hrungsgewohnheiten und mangelnder Bewegung gepr"gt ist, tritt die nicht alkoholinduzierte Fettlebererkrankung (NAFLD) immer h"ufiger als Diagnose in den Patientenakten auf, wobei deren Entstehung noch nicht im Detail charakterisiert ist. Sie betrifft in verschiedenen Schweregraden sch"tzungsweise 30 % der Bev#lkerung, wobei das initiale Stadium der geringgradigen Steatose noch reversibel ist und als benigne angesehen wird. Allgemein wird die Dysbalance zwischen Kalorienzufuhr und -Verbrauch, die zu einer positiven Energiebilanz f!hrt, als die entscheidende Ursache f!r die Entstehung der NAFLD betrachtet. Jedoch ist bisher wenig !ber die konkreten molekularen Mechanismen bekannt, wobei auch der genaue Einfluss von nutritiven Faktoren, und deren Auswirkung auf den gesamten Lebermetabolismus weiterer Charakterisierung bed!rfen. Mit diesem Ziel vor Augen, wurde innerhalb des Virtuelle Leber Netzwerks eine Studie gestartet, die am murinen Model durch eine hyperkalorische (fettreiche) Di"t die Entstehung einer reversiblen Lebersteatose gleichzeitig auf Transkriptom-, Proteom-, Metabolom- und vor allem Lipidom-Ebene charakterisieren soll. Besonders und neuartig im Vergleich zu bisher bekannten Studien ist, dass die o.g. Untersuchungen unter dem Aspekt der circadianen Regulation des Lebermetabolismus vergleichend f!r beide Geschlechter vorgenommen wurden. Zu diesem Zwecke wurde C 57BL/6-N M"usen beider Geschlechter !ber einen Zeitraum von 4 bzw. 10 Wochen eine sog. Hochfett-Di"t (HFD) mit einem Rohfettanteil von ca. 42 % verabreicht. Die Kontrolldi"t (KD) enthielt dagegen einen Rohfettanteil von ca. 6%. Nach Beendigung der entsprechenden Di"t-Periode wurden die murinen Hepatozyten zu zwei verschieden Tageszeitpunkten (zeitgeber time ZT3 und ZT15) isoliert und der Analyse hinsichtlich der o.g. Parameter unterzogen. Die hier pr"sentierten Daten befassen sich v.a. mit den Ergebnissen auf der Ebene des Lipidoms, die mittels Q ExactiveTM Massenspektrometrie gewonnen wurden. W"hrend die tageszeitlichen Unterschiede im Lipidgehalt bei der KD kaum Unterschiede zwischen den Geschlechtern zeigten, wurden nach Gabe der HFD f!r 4 Wochen deutliche geschlechter-spezifische Unterschiede in der circadianen Lipideinlagerung festgestellt. Insbesondere die Di"t-abh"ngige Zunahme der Triglyceride und Cholesterinester zeigte eine ausgepr"gte, signifikante Tagesrhythmik, die bei M"nnchen invers zu der bei Weibchen verlief. Nach 10 Wochen HFD ver"nderte sich dieses Muster bei Weibchen nur leicht quantitativ, w"hrend bei den M"nnchen eine Umkehrung, d. h. Angleichung des Rhythmus an den der Weibchen erfolgte. Durch Analyse der parallel erhobenen zus"tzlichen Omics-Daten wird derzeit untersucht, ob dieses Ph"nomen als Folge einer fortscheitenden „Femininisierung“ der M"nnchen unter dem Einfluss der HFD gedeutet werden kann. Unter der gleichzeitigen Ber!cksichtigung der Bedeutung des Geschlechts und eines intakten circadianen Rhythmus’ f!r die Hom#ostase des Leber-Lipidmetabolismus bef"higen die in dieser Studie erlangten Erkenntnisse zu neuen Denkanst#ßen bez!glich der Entstehung von NAFLD und einer m#glichen Progression zu risikoreicheren Erkrankungsformen. Korrespondierender Autor: Arnold, Katrin E-Mail: Katrin.Arnold@medizin.uni-leipzig.de Phenprocoumon-induced liver injury 3.22 Straub BK1, Dries V2, Kasper HU3, Sch"mig E4, Drebber U3, Langner C5, Dienes HP6, Schirmacher P1 1 Ruprecht-Karls-University Heidelberg, Institute of Pathology, University Clinic, Heidelberg, Germany; 2synlab MVZ Pathologie Mannheim GmbH, Institute of Pathology, Mannheim, Germany; 3University of Cologne, Institute of Pathology, Cologne, Germany; 4University of Cologne, Institute of Pharmacology, Cologne, Germany; 5Medical University of Graz, Institute of Pathology, Graz, Austria; 6 University Vienna, Institute of Clinical Pathology, Vienna, Germany Introduction: Phenprocoumon (Marcumar!), a derivative of 4-hydroxycoumarin with similarity to warfarin, is the most frequently used oral anticoagulant drug in continental europe. Apart from bleeding disorders, other adverse reactions are rare due to its mechanism of action. In the last years, hepatotoxicity has been observed and several case reports have been published. Yet, so far, no systematic analyses of this potentially life-threatening complication have been performed. Material & Methods: We analysed the clinical presentation and the liver histology of 53 patients with hepatic disease of unknown origin, who were on medication with phenprocoumon. Results: In 38 cases, the data were highly suggestive of phenprocoumon-induced liver injury, 6 cases were doubtful due to intake of several drugs described to potentially cause similar histologic findings and 9 cases could be ruled out with high probability. Histologically, in all 38 positive cases, acute or subacute hepatitis with a uniform picture of centrolobular/zone 3 necrosis with bridging necrosis was found which lead to the diagnosis. The clinical presentation of these patients ranged from elevated aminotransferases alone up to severe liver disease and acute liver failure in five patients (representing 13% of cases). Hepatic disease occurred in general 4 to 9 months after the first application of phenprocoumon, yet in 4 patients who were reexposed with phenprocoumon, relapse occurred earlier, i.e. after 1 to 6 weeks following renewed phenprocoumon-therapy. Four patients needed liver transplantation, complete recovery was eventually seen in all other patients after drug omission. Summary: Phenprocoumon-induced liver injury is a potentially life-threatening adverse reaction with characteristic histology (centrolobular/zone 3 necroses), occurring after a latency of 4 – 9 months following onset of therapy so that often phenprocoumon is frequently not the suspected cause of the liver injury. The mechanism of action is most likely an idiosyncratic hepatic injury; yet, the mode of action is so far unknown, e.g. polymorphisms for the CYP2C9 gene have been only found in 1 (heterozygous) of 7 cases. In case of phenprocoumon-induced liver injury, complete omission of the drug is mandatory to prevent progression of liver injury, and reexposure should be strictly avoided as relapse will occur faster and more severe. Corresponding author: Straub, Beate K. E-Mail: beate.straub@med.uni-heidelberg.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A33 A34 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 3.23 Reduced HNF3b (FOXA2) levels in steatosis leads to diminished expression of anti-lipoapoptotic protein ALR Dayoub R1, Lupke M1, Hofmann U2, Melter M1, Weiss TS1 1 University of Regensburg Childrens Hospital, Regensburg, Germany; 2Dr. Margarete Fischer-Bosch Institute of Clinical Pharmacology, Stuttgart, Germany Non-alcoholic fatty liver disease (NAFLD) encompasses a spectrum of hepatic pathologies, ranging from steatosis in its most benign form to cirrhosis in its most advanced form with non-alcoholic steatohepatitis (NASH) in an intermediate level. NASH has been thought to be a liver disease triggered by various factors such as triglyceride accumulation in hepatocytes and followed by oxidant stress and lipid peroxidation causing inflammation and fibrosis. The progression of Steatosis to NASH is facilitated when adaptive mechanisms to protect hepatocytes from fatty acid-mediated lipotoxicity are failing. The winged Helix Forkhead Box A2, FOXA2 (HNF3b) transcription factor plays an important role in controlling both metabolism and homeostasis of lipids through regulation of multiple target genes in the liver. ALR (augmenter of liver regeneration), a protein known to augment liver regeneration was further shown to reveal hepatoprotective properties against liver toxins. We have previously shown that gene expression of ALR is regulated by FOXA2 in liver cells. In addition, we have demonstrated that ALR attenuates the ER stress-mediated apoptosis induced by palmitic acid in hepatic cells. The aim of our study was to analyze the expression of FOXA2 and ALR and to investigate the potential protective role of ALR under conditions of NASH/steatosis. Steatotic liver tissues obtained from high fat diet (HFD) mouse model (n= 6) and patients with NAFLD (n= 27) were analyzed to determine the expression of both FOXA2 and ALR demonstrating reduced FOXA2 and ALR levels compared to control groups. Furthermore we cultured HepG2 cells treated with palmitic pcid (PA) followed by FOXA2 immunofluorescence staining. PA-treated cells revealed significant translocation of FOXA2 from nucleus into cytosol compared to non-treated cells. In addition, we found diminished ALR mRNA expression levels in PA-loaded cells compared to non-treated cells. To overcome the functional redundancy, we aimed to investigate the role of ALR in PA treated hepatoma cells by gain-of-function experiments. Therefore, we generated stable-transfected HepG2 cells expressing human 15 kDa (short form) ALR protein (HepG2-ALR). Interestingly, culturing HepG2 and HepG2-ALR cells treated with increasing concentrations of PA showed a significant lower lipotoxicity for HepG2-ALR cells accompanied by reduced triglycerides storage compared to mock HepG2 cells. This study provides evidence that ALR, mediated Foxa2 (HNF3b), plays an important role in NAFLD by alleviating the lipid-mediated ER stress and reducing lipid accumulation in liver cells. Corresponding author: Dayoub, Rania E-Mail: rania.dayoub@ukr.de 3.24 Regulation of energy metabolism in hepatocytes with induced steatosis Sch"nefeld K1, Matz-Soja M1, B"ttger J1, Seibel P2, Gebhardt R1 1 University of Leipzig, Institute of Biochemistry, Faculty of Medicine, Leipzig, Germany; 2University of Leipzig, Molecular Cell Therapy, Center for Biotechnology and Biomedicine (BBZ), Leipzig, Germany Mitochondria are cellular organelles involved in variety of metabolic pathways and important for ATP production. Based on our new findings the Hedgehog (Hh) signaling pathway is an active pathway in healthy mature hepatocytes with relevant impact on endocrine liver function and is involved in lipid metabolism [1,2]. In this study we explored the effects of nutritive induced steatosis in combination with hepatocytespecific deletion of Hh signaling transcription factor Gli3 on the regulation of energy metabolism in mitochondria. For this analysis we used a transgenic mouse model with deletion of Gli3 (KO) and fed mice for four and ten weeks with control (CD) and high fat diet (HFD). To explore the endogenous respiration a Clark type oxygen electrode was used and the oxygen consumption was monitored. The ATP-level was determined by the CellTiter-Glo! Luminescent Cell Viability Assay. Furthermore, the activity of mitochondrial enzymes of respiratory chain complexes was assessed by photometric assays. The mRNA expression levels of selected complex subunits and genes encoded mitochondrial proteins were analysed by qrt-PCR. In general we could observe that hepatocytes from control mice fed with HFD show higher oxygen consumption than control mice fed with CD after ten weeks. Compared with wild type mice, Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York hepatocytes from Gli3-KO mice fed with CD showed increased oxygen consumption after four and ten weeks, which is also true for Gli3-KO mice fed with HFD. Considering the ATP-level the results show that hepatocytes from control mice fed with HFD have decreased amount compared to control mice fed with CD. Referring Gli3-KO mice fed with CD we measured reduced ATP-amount compared to wild type mice after four and ten weeks. The same was true for Gli3-KO mice fed with HFD for four weeks. Interestingly, ATP-level in Gli3-KO mice fed with HFD for ten weeks was slightly increased compared to control mice. We could show that mice fed with HFD have altered mitochondrial functions characterized by higher oxygen consumption and lower ATP-level. The same was true for Gli3-KO mice fed with CD and become more pronounced when feeding Gli3-KO mice with HFD. These results suggest that interrupting the transcriptional output of Hh signaling in the liver at the level of the transcription factor Gli3 causes changes in mitochondrial function which resemble those seen after feeding HFD. However, it remains to be explored whether the low ATP-levels (in spite of an increased oxygen consumption) are due to a partial uncoupling of the mitochondria or whether they reflect simply a low steady state level resulting from an unusually high energy demand. [1] Matz-Soja et al., Hepatic Hedgehog signaling contributes to the regulation of IGF1 and IGFBP1 serum levels. Cell Commun Signal. 2014, 18;12:11. [2] Pospisilik JA et al., Drosophila genome-wide obesity screen reveals hedgehog as a determinant of brown versus white adipose cell fate. Cell. 2010, 8;140(1):148 – 60 Corresponding author: Sch#nefeld, Kristin E-Mail: kristin.schoenefeld@medizin.uni-leipzig.de 3.25 Representation of human non-alcoholic fatty liver disease in murine models Teufel A1, Itzel T1, Erhart W2, Brosch M3, Kim YO4, Sch"nfels W von5, Herrmann A2, Br!ckner S3, Stickel F6, Chavakis T7, Hellerbrand C1, Becker T5, Schreiber S2, Schuppan D4, Schafmeier C5, Hampe J1 1 University of Regensburg, Department of Medicine I, Regensburg, Germany; 2University of Kiel, Department of Internal Medicine I, Kiel, Germany; 3Technical Unversity Dresden, Medical Department I, Dresden, Germany; 4 University of Mainz, Department of Medicine I, Mainz, Germany; 5University of Kiel, Department Visceral and Thoracic Surgery, Kiel, Germany; 6University of Berne, Department of Clinical Research, Berne, Switzerland; 7 Technical University Dresden, Department of Pathobiochemistry, Dresden, Germany Non-alcoholic fatty liver disease (NAFLD) is the most common chronic liver disorder in industrialized countries. Murine models are the key mechanistic platform for the disease. We systematically evaluated genome-wide mRNA expression data from five commonly used murine models of NAFLD (high-fat diet, MCD diet, streptozotocin diet, PTEN (Fox) KO) in comparison to human data from 39 controls and 77 NAFLD samples spanning the range of the phenotype. First, profound differences between human and murine expression patterns exist, that override any disease or phenotype signature. In fact, from the significantly regulated human genes in NASH/NAFLD only between 1 and 16 are significantly and concordantly regulated in mice. The dataset, depending on mouse model and human phenotype, shows correct reflection of key pathways, lack of regulation, or reverse effects thereby providing a guide for murine model selection in future experiments to improve applicability to human NAFLD. Corresponding author: Teufel, Andreas E-Mail: andreas.teufel@ukr.de 3.26 Retinoic acid amplifies the FXR-dependent FGF19 gene expression in human enterocyte-like HT-29 cells by a bi-phasic mechanism Jahn D1, Sutor D1, Hermanns HM1, Schmitt J1, Geier A1 1 University Hospital W!rzburg (UKW), Division of Hepatology, W!rzburg, Germany Background and aims: The intestine-derived hormone Fibroblast Growth Factor 19 (FGF19) and its mouse ortholog Ffg15 are key regulators of bile acid synthesis and energy metabolism. FGF15/ 19 expression is induced by bile acid-mediated activation of FXR. Moreover, vitamin A (VA) has been shown to activate Fgf15 in an RXR/FXR-dependent manner in mice. Whether VA derivatives regulate FGF19 in human entero- 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen cytes and which nuclear receptors contribute to this regulation is currently unknown. Methods: HT-29 cells were treated with VA derivatives with distinct selectivity for different nuclear receptors including 9-cis retinoic acid (9cisRA, RXR/RAR agonist), methoprene acid (MA, RXR agonist) and TTNPB (RAR agonist) alone or in combination with chenodeoxycholic acid (CDCA, FXR agonist). Induction of FGF19, FXR and RXR/ RAR mRNA expression was measured by qPCR. Changes in FXR protein levels were determined by Western blotting. To analyse the contribution of FXR signalling to VA-mediated FGF19 induction, the intracellular localisation of FXR protein was assessed by immunofluorescence microscopy. Results: Expression of FGF19 was strongly induced by 9cisRA (activates RAR and RXR) while CDCA had a minor effect. Moreover, 9cisRA induced FXR expression on mRNA and protein level and amplified the CDCA-mediated induction of FGF19 in a time dependent manner at 8 – 24 h. Interestingly, treatment with TTNPB (RAR-selective) but not MA (RXR-selective) resulted in a strong activation of FGF19 expression. In contrast, selective activation of RXR but not RAR induced FXR expression. Additionally, in contrast to CDCA, treatment with 9cisRA did not result in significant nuclear accumulation of FXR protein suggesting an FXR-independent effect of 9cisRA in human enterocytes. Conclusions: These findings suggest that VA derivatives modulate intestinal FGF19 production in human cells via direct RAR-dependent (early FXR-independent) and indirect FXR-dependent (late transcriptional amplification loop) mechanisms. Our results warrant further studies on the therapeutic usefulness of VA to treat bile acid-associated and metabolic disorders. Corresponding author: Jahn, Daniel E-Mail: jahn_d@ukw.de 3.27 Serum sterol levels indicate distorted cholesterol homeostasis in cirrhotic patients with primary biliary cirrhosis Krawczyk M1, Wunsch E2, L!tjohann D3, Lammert F1, Milkiewicz P4 1 Saarland University Hospital, Department of Medicine II, Homburg, Germany; 2Pomeranian Medical University, Liver Research Laboratories, Szczecin, Poland; 3University Clinics of Bonn, Institute for Clinical Chemistry and Clinical Pharmacology, Bonn, Germany; 4Medical University of Warsaw, Liver and Internal Medicine Unit, Department of General, Transplant and Liver Surgery, Warsaw, Poland Background: In humans new cholesterol derives from de novo synthesis and intestinal absorption. Serum cholesterol precursor (e.g., lathosterol, desmosterol) and plant sterol levels (e.g., sitosterol, campesterol) represent valid surrogate marker for cholesterol biosynthesis and intestinal absorption, respectively. Since chronic liver diseases modulate cholesterol homeostasis, we systematically investigated sterol serum levels in patients with primary biliary cirrhosis (PBC) with and without liver cirrhosis. Patients and methods: Overall, we recruited 111 non-transplanted PBC patients (age 22 – 83 years, 101 females). In this cohort, a total of 30 individuals presented with liver cirrhosis at diagnosis. Serum concentrations of plant sterols, cholesterol and its precursors were measured by gas chromatography/mass spectrometry (GC/MS). Individuals with results suggesting familial hypercholesterolaemia or phytosterolemia were excluded. Serum sterols were compared between cirrhotic and non-cirrhotic patients using non-parametric tests. Results: PBC patients with liver cirrhosis demonstrated significantly higher serum sitosterol and campesterol concentrations than non-cirrhotic individuals. (P= 0.0002 and P= 0.007, respectively). Serum levels of lathosterol and desmosterol were lower in these patients (P= 0.0001 and P= 0.01, respectively), who also displayed a trend to lower serum cholesterol (P= 0.06). In cirrhotic patients we identified increased sitosterol:cholesterol and campesterol:cholesterol but decreased lathosterol:cholesterol ratios (all P < 0.0001). Overall, the ratios of phytosterols to cholesterol precursors were significantly (all P > 0.0001) increased in patients with liver cirrhosis as compared to non-cirrhotic patients. Discussion: PBC patients with liver cirrhosis are characterized by decreased cholesterol synthesis and increased sterol absorption as compared to non-cirrhotic individuals. The determination of serum sterols may improve the clinical assessment and stratification of patients with PBC. Corresponding author: Krawczyk, Marcin E-Mail: marcin.krawczyk@uks.eu 3.28 The effect of extended transportation time on the quality of freshly isolated human liver cells Lee SML1, Demmel M1,2, Hauner M2, Schiergens T1, Werner J1, Thasler WE1 1 Ludwig Maximilians University, Department of General, Visceral, Transplantation, Vascular and Thoracic Surgery, Grosshadern Hospital, Munich, Germany; 2Hepacult GmbH, Regensburg, Germany Introduction: Given that the liver carries out a wide range of functions, such as detoxification, metabolism and homeostasis, isolated hepatocytes are important in vitro models for research questions to do with pharmacokinetics, toxicology etc. In particular, the use of human hepatocytes is important for the validation of studies done with animal models and for translational research. However, generally speaking, it is difficult for an individual researcher to isolate hepatocytes himself for experimentation due to the large amount of manpower required. This manpower is required to collect the donated remnant livers with informed consent according to ethical regulations, carry out serological tests and to isolate liver cells when tissue is made available by surgeries. Thus, core facilities that isolate human liver cells for provision to research groups are essential. Since liver cell quality is paramount for relevant results, this study aims to examine if extended transportation time affects the quality of isolated human liver cells. Methods: Human hepatocytes were isolated by a modified two-step collagenase perfusion technique with modifications. The viability of the isolated hepatocytes (N= 60) was assessed immediately after isolation and after being stored for 17 h in Cold Storage Solution (CSS) on ice. These results were compared to counts from actual shipments of hepatocytes (N= 111) overnight on ice to collaborators. For a number of isolations, adherence to cell culture plates and confluence of hepatocytes was also assessed after storage on ice for 18 h. Results: After 17 h storage on ice, viability dropped significantly from 78 € 0.9 % to 66 € 1.7 %. For the shipped samples, viability dropped significantly from 79 € 0.5% to 67 € 1.9 %. Thus, for both scenarios, hepatocytes dropped approximately 12% in viability. Although, there is a drop in viability, the hepatocytes were able to adhere to cell culture plates with good confluence up to 3 days when a similar number of viable cells were plated. Discussion: In conclusion, there was a small drop in hepatocyte viability when cells were stored overnight on ice in CSS. After the drop in viability, the cells still had an average viability of 66%, which is high enough for downstream experiments. These cells were still able to adhere well to culture plates with a good confluence for further experiments. Thus, these results indicate that hepatocytes can indeed be successfully transported overnight and shows that a distribution system using core facilities to support a large number of research laboratories functions well. Corresponding author: Lee, Serene M. L. E-Mail: serene.lee@med.uni-muenchen.de 3.29 Vitamin D3 acts on the gut-liver-adipose tissue axis to modulate obesity and associated metabolic and inflammatory changes in diet-induced obese mice Jahn D1, Gildein L1, Fleet JC2, Schmitt J1, Hermanns HM1, Geier A1 1 University Hospital W!rzburg (UKW), Division of Hepatology, W!rzburg, Germany; 2Purdue University, Department of Nutrition Science, West Lafayette, Indiana, USA Background: Obesity and associated metabolic complications are increasing problems in industrialized countries. Serum 25-OH Vitamin D 3 (VD3) levels negatively correlate with body mass index, insulin resistance and non-alcoholic fatty liver disease (NAFLD) in humans. The causal relation between VD3 status and NAFLD as well as the potential underlying mechanisms are, however, not fully understood. Methods: To explore the relevance of VD3 for obesity and NAFLD, C 57BL/ 6 mice were fed high-fat diets (HFD) with different levels of VD3. Liver histology and hepatic fat content were analyzed. The expression of metabolic and inflammatory target genes in liver and adipose tissue (AT) was measured by qPCR. Serum parameters were determined by ELISA. Moreover, intestinal effects of VD3 were investigated in Vitamin D receptor (VDR)-deficient mice (VDR-KO) and VDR-KO mice with an intestinespecific human VDR transgene (VDR-KO hTg). Results: High dietary VD3 enhanced HFD-induced weight gain and increased fat mass. This was associated with up-regulation of chemokine signaling in AT and a shift towards pro-inflammatory M1-macrophages. In line, fasting glu- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A35 A36 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen cose and serum insulin were elevated in HFD mice with high VD3 intake. These AT-specific changes coincided with trends towards increased immune activation and ER stress in the liver. Interestingly, analysis of VDRKO hTg mice revealed increased body weight and fat mass compared to VDR-KO in response to HFD-feeding. This was accompanied by differential expression of metabolic and inflammatory target genes in the liver. Conclusions: Together, our data reveal a potential pro-adipogenic effect of VD3 in the applied HFD-feeding model that could possibly be driven by an unanticipated role of VDR in the regulation of intestinal lipid metabolism. This pro-adipogenic effect could, in turn, promote certain unfavorable metabolic and inflammatory effects in the liver highlighting the pathophysiological importance of the gut-liver-adipose tissue axis in the development of obesity and NAFLD. Corresponding author: Jahn, Daniel E-Mail: jahn_d@ukw.de 3.30 Xenobiotic-dependent induction of the tricarboxylate carrier Slc13a5 in primary cultures of rat hepatocytes Neusch$fer-Rube F1, Lieske S1, Birkenfeld AL2, P!schel GP1 1 University of Potsdam, Nutritional Science, Nutritional Biochemistry, Potsdam, Germany; 2Charit#, Department of Endocrinology, Diabetes and Nutrition, Berlin, Germany Background: The tricarboxylate carrier Slc13a5 (mINDY) is an active transporter that mediates concentrative uptake of citrate in symport with sodium ions across the plasma membrane of cells. In mammals, it is expressed predominantly in hepatocytes and appears to contribute to the cytosolic citrate homeostasis. Citrate is an important intermediate and regulator of fatty acid synthesis. Accordingly, knock down of the Slc13a5 gene in mice was associated with reduced liver fat content and consequently improved insulin sensitivity under a high fat diet. Exposure to xenobiotics often results in hepatic lipid accumulation. The study thus aimed at elucidating the impact of xenobiotics on Slc13a5 expression. Methods: Primary cultures of rat hepatocytes were exposed to two xenobiotics, the constitutive androstane receptor (CAR)activator phenobarbital (PB) and the aryl-hydrocarbon receptor (AhR) activator beno[a]pyrene (BaP) alone or in combination for 48 h. AhR, CAR and Slc13a5 gene expression, activity and activity were determined by qPCR, reporter gene assay and radioactive citrate uptake assay, respectively. Results: Exposure of hepatocytes to PB, BaP or a combination of both induced Slc13a5 mRNA 2-fold, 5-fold and 32-fold, respectively. The more than additive induction by the combination of both xenobiotics resulted from a mutual induction of the respective nuclear receptors: CAR was induced 10-fold by BaP while the AhR was induced 6-fold by PB. A combination of PB and BaP induced the expression of a reporter gene under the control of a 1,8 kb Slc13a5 promoter fragment about 3fold. This induction was abrogated by elimination of a putative AhR binding site at -770. Induction of Slc13a5 by a combination of PB and BaP resulted in an about 50 % increase in citrate uptake. Conclusion: Xenobiotic exposure, in particular simultaneous activation of the two nuclear receptors CAR and AhR may increase Slc13a5 expression and thereby might contribute to xenobitoic-induced citrate uptake and hence lipid accumulation in hepatocytes. Corresponding author: P!schel, Gerhard P. E-Mail: gpuesche@uni-potsdam.de 3.31 Zerebrale miRNA-Expressions!nderungen bei hepatischer Enzephalopathie Oenarto J1, G"rg B1, Castoldi M1, H$ussinger D1 1 Heinrich Heine Universit$t, Klinik f!r Gastroenterologie, Hepatologie und Infektiologie, D!sseldorf, Deutschland Einleitung: MicroRNAs (miRNAs) sind kurze, einzelstr"ngige RNA Molek!le, welche die Expression und Translation von Genen posttranskriptionell regulieren k#nnen. Literaturbefunde weisen auf spezifische Expressions"nderungen individueller Gene im Transkriptom in post mortem Hirnproben von Leberzirrhosepatienten mit hepatischer Enzephalopathie (G#rg et al. 2013, Hepatology). Unklar ist gegenw"rtig, ob die beschriebenen Genexpressionsunterschiede Folge einer ver"nderten zerebralen Expression von microRNAs sind. In der vorliegenden Arbeit wurde daher untersucht, ob zerebrale Genexpressions"nderungen in post mortem Hirnproben von Leberzirrhosepatienten mit und ohne hepatische Enzephalopathie assoziiert sind mit miRNA Expressions"nderungen. Methoden: miRNA- und Genexpressionslevel wurden in humanen post mortem Hirnproben aus dem zerebralen Kortex (Gyrus fusifor- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York mis) von 4 Kontrollpatienten und je 4 Patienten mit Leberzirrhose mit und ohne HE mittels mRNA oder miRNA spezifischen Agilent Microarrays gemessen und miRNA Expressionsunterschiede mit einem Realtime-PCR Ansatz (miQPCR) validiert. Potentielle miRNA Zielgene wurden mit Hilfe von Web-basierten Datenbanken ermittelt (Targetscan (MIT, USA), Microcosm (EMBL, Heidelberg), miRDB (MirTarget2, USA), Diana Tools (microT,Athen)). Mit Hilfe bioinformatischer Tools wurden bei Zirrhosepatienten mit HE vermindert exprimierte Gene identifiziert, deren Expressions"nderung einhergeht mit einer gesteigerten Expression von miRNAs, welche die Expression dieser Gene regulieren k#nnen. Ergebnisse: Durch Transkriptomanalyse wurde eine gegen!ber den Kontrollen bei Leberzirrhosepatienten mit HE ver"nderte Expression von 1547 Genen gefunden. 945 Gene zeigten dabei eine erh#hte und 602 Gene eine verringerte Expression. Mittels miRNA Array Analyse konnten 25 miRNAs in post mortem Hirnproben von Zirrhosepatienten mit HE identifiziert werden, die gegen!ber den Kontrollpatienten signifikant erh#ht exprimiert waren. 23 von den 25 in Leberzirrhosepatienten mit HE identifizierten miRNAs mit ver"nderter Expression waren nicht ver"ndert bei Leberzirrhosepatienten ohne HE. Die bioinformatische Analyse zeigte, dass eine Vielzahl der in post mortem Hirnproben von Leberzirrhosepatienten mit HE vermindert exprimierten Gene potentielle Zielgene von gleichzeitg verst"rkt exprimierten miRNAs darstellen. Diese bei Leberzirrhosepatienten mit HE ver"ndert exprimierten Zielgene sind involviert in synaptische Plastizit"t und Verhalten. Diskussion: Unsere Befunde zeigen spezifische zerebrale Gen- und miRNA-Expressions"nderungen im Gehirn von Zirrhosepatienten mit hepatischer Enzephalopathie und lassen vermuten, dass microRNA Expressions"nderungen einen Einfluss auf die zerebrale Genexpression bei hepatischer Enzephalopathie haben k#nnen. Korrespondierender Autor: Oenarto, Jessica E-Mail: Jessica.Oenarto@hhu.de 4. Tumors/Liver Surgery 4.1 Comprehensive analysis of informative target disease relevant nuclear genes and the whole mitochondrial genome in hepatocellular carcinoma by Multiplex PCR and Ultra-Deep Sequencing Amer W1, Quaas A1, Eischeid H1, Vollbrecht C1, Koitzsch U1, B!ttner R1, Drebber U1, Odenthal M1 1 University of Cologne, Institute for Pathology, Cologne, Germany Hepatocellular carcinoma (HCC) are highly malignant tumors triggered by a wide variety of genetic alterations. Importantly, they show multicentric occurrence characterized by a nodule-in-nodule pattern. In the present study, we investigate the occurrence of disease related nuclear mutations and whole mitochondrial genomic variants by a comprehensive ultra-deep sequencing approach as a novel tool for hepatocellular cancer follow-up and prognosis. Macrodissected 48 HCC nodules, representing different tumor grades, and adjacent non-cancerous tissues from HCC patients were studied. Hot spot mutation screening of nuclear DNA (nDNA) was performed using a multiplex PCR approach covering 40 disease relevant gene regions by a total of 394 amplicons. The mitochondrial (mt) genome is highly susceptible to DNA alterations due to the lack of protective histones and a limited repair system. Therefore, we were using mt-variations as a way of focal cancer barcoding and tracking. Thus, 108 primer sets spanning the whole mtDNA were designed and automatic single PCR set-up was established using the Biomek robotic system. Target enriched libraries of mtDNA and nDNA were sequenced by means of the MiSeq platform and data analysis was performed by the CLC Cancer Research Workbench. Whole mt-genome analysis revealed high frequency of variants in the D-Loop region and the MT-CYB gene. In particular, in HCC nodules of non-cirrhotic origin a wide spectrum of mt-variants with high frequency were identified. However, highly frequent mt-variants occur not only in HCC nodules but also in peri-tumorous parenchymal foci raising the possibility that mtDNA mutations might precede nuclear alterations and play a role in the pre-tumor machinery. Furthermore, the occurrence of identical mtvariants in different nodules of one liver sample indicates the monoclonal HCC origin. Most notably, the increasing numbers of mt-variants as well as the increasing frequency of a particular mt-hot-spot mutation refer to the progression of the HCC dedifferentiation. This accumulation of mt-hot-spot variants in highly dedifferentiated nodules was associated with an enrichment of nuclear mutations as shown in the RPS 6KA3, TP53, ARID2, ARID 1A or the ATM gene. In conclusion, screen- 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen ing of mitochondrial genome by ultra-deep sequencing is a reliable and useful molecular tool to identify pre-tumorous nodules with high transformation potential and to illustrate tumor clonality and history. Early appearance and high frequency of mt-hot spot mutations associated with HCC development and nuclear genomic alterations provide novel insights in cancer diagnostics and therapeutic approaches. Corresponding author: Odenthal, Margarete E-Mail: m.odenthal@uni-koeln.de 4.2 4.3 Brunner SM1, Rubner C1, Kesselring R1, Martin M1, Ruemmele P2, Stempfl T5, Teufel A4, Schlitt HJ1, FichtnerFeigl S3 1 University Medical Center Regensburg, Surgery, Regensburg, Germany; 2University Medical Center Regensburg, Pathology, Regensburg, Germany; 3University Medical Center Regensburg, Surgery and Regensburg Center of Interventional Immunology, Regensburg, Germany; 4 University Medical Center Regensburg, Internal Medicine I, Regensburg, Germany; 5University of Regensburg, Center of Excellence for Fluorescent Bioanalytics (KFB), Regensburg, Germany Identification of potential driver genes involved in chromosomal instability and tumor cell migration in hepatocarcinogenesis Meyer ASK1, Wan S1, Weiler S1, Roessler S1, Pinna F1, Marquardt J1, Schirmacher P1, Breuhahn K1 1 University Hospital Heidelberg, Institute of Pathology, Heidelberg, Germany; 2University Hospital Mainz, I Medical Department, Mainz, Germany Background: The genetic heterogeneity of hepatocellular carcinoma (HCC) limits our understanding of the underlying molecular mechanisms and the development of targeted therapies. In the last years, molecular classification of human HCCs revealed that chromosomal instability (CIN) and the existence of a metastatic signature correlate with a poor patients’ prognosis. Based on comprehensive expression profiling data we aim to identify factors involved in the development of a CIN phenotype and tumor cell dissemination in HCC. Methods: Transcriptomic data of 240 primary human HCCs and matched non-neoplastic liver tissues were grouped according to the following selection criteria (Roessler et al., 2010 Cancer Res.): a) > 2-fold induction of mRNA in HCCs, b) significant impact on patient survival. Candidates, which have not been described in the context of liver cancer but which were associated with CIN and migratory phenotypes in other carcinomas were further analyzed. Comparative genomic hybridization (CGH; Roessler et al., 2012 Gastroenterology) data were checked as cause for mRNA induction. Induction of cDNA and protein expression of candidate genes was confirmed in 8 HCC cell lines and an independent HCC cohort.The impact on cell migration after siRNA-mediated silencing was examined for selected genes using time-lapse microscopy. Results: From overall 13,100 detectable transcripts, 347 mRNA were upregulated by a factor > 2-fold in HCCs. Among these, the expression of 122 genes significantly correlated with worse patient survival. Database survey led to the identification of four candidates which fulfill all selection criteria: EB1 / MAPRE1 (microtubule-associated protein-1), SCRIB (Scribbled homolog), TTK (TTK protein kinase), and ZWINT (ZW10-interacting kinetochore protein). For SCRIB, a significant correlation between mRNA levels and genomic gains on chromosome 8q24.3 was observed (p < 0.001). We confirmed that EB1 and ZWINT had higher transcript levels in HCCs than in concordant non-neoplastic tissues (pEB1 = 0.046; pZWINT= 0.018; n= 20). At the protein level all candidate genes were detectable in a subset of HCC cell lines. First functional analyses revealed that silencing of candidate factors impaired the migratory potential of HCC cells. Conclusion/Outlook: Applying specific selection criteria we identified four genes, EB1 /MAPRE1, SCRIB, TTK, and ZWINT, which are candidates linking CIN and migratory phenotypes in hepatocarcinogenesis. Functional analyses of such candidates are aimed at altered pathways or specific points of interference to block metastasis in early and late stage HCC. References: [1] Roessler S et al., Cancer Res. 2010, 70(24):10202 – 12. [2] Roessler S et al., Gastroenterology 2012, 142(4):957 – 966. Corresponding author: Meyer, Anne-Sophie K E-Mail: anne-sophie.meyer@med.uni-heidelberg.de Tumor infiltrating IL-33 producing effector-memory CD 8+ T cells in resected hepatocellular carcinoma prolong patient survival Background: IL-33, a cytokine with pleiotropic functions, is elevated in serum of patients with hepatocellular carcinoma (HCC). This study investigated effects of local IL-33 expression in resected HCC on patient survival and on immunological and molecular tumor microenvironment. Methods: Tissue of resected HCCs was stained for H&E, masson trichrome, alpha smooth muscle actin, IL-33, CD8 and IL-13 and analysed by flow cytometry. Besides histomorphologic evaluation, the immunohistochemical stainings were analysed for the respective cell numbers separately for tumor area, infiltrative margin and distant liver stroma. These findings were correlated with clinical data and patient outcome. Further, gene and microRNA expression of different HCC risk groups was compared using Micro Arrays and PCR Arrays. Results: In multivariable analysis, infiltration of HCCs by IL-33+ cells (P= 0.032) and CD 8+ cells (P= 0.014) both independently were associated with prolonged patient survival. Flow cytometry demonstrated that cytotoxically active CD 8+CD 62L-KLRG1+CD 107a+ effectory-memory cells are the main producers of IL-33 in these HCC patients. Using infiltration by IL-33+ and CD 8+ cells as two separate factors, a HCC immune score (HCCIS) was designed and evaluated that stratified patient survival (P= 0.0004). This HCCIS identified high and low risk patients who differ in gene and microRNA expression profiles (P < 0.001). Conclusion: Infiltration of HCCs by IL-33+ and CD 8+ cells is independently associated with prolonged patient survival. We suggest that this is due to an induction of highly effective cytotoxically active CD 8+CD 62L-KLRG1+CD 107a+ effector-memory cells producing IL-33. Based on these two independent factors we established a HCC immune score that provides risk stratification for HCC patients and can be used in the clinical setting. Corresponding author: Brunner, Stefan M. E-Mail: stefan.brunner@ukr.de 4.4 4EBP1/eIF4E and p70S 6K/RPS6 axes play critical and distinct roles in hepatocarcinogenesis driven by AKT and N-Ras protooncogenes in mice Calvisi DF1, Cigliano A1, Wang C2, Pilo MG1, Sini M1, Dombrowski F1, Chen X1, Evert M3 1 University Medicine of Greifswald, Institute of Pathology, Greifswald, Germany; 2University of California, Department of Bioengineering and Therapeutic Sciences, San Francisco, USA; 3University of Regensburg, Institute of Pathology, Regensburg, Germany Concomitant expression of activated forms of AKT and Ras in the mouse liver (AKT/Ras) leads to rapid tumor development via strong activation of the mTORC1 pathway. mTORC1 functions via regulating p70S 6K/RPS6 and 4EBP1 /eIF4E cascades. How these cascades contribute to hepatocarcinogenesis remains unknown. Here, we show that inhibition of RPS6 pathway via Rapamycin effectively suppressed, whereas blockade of the 4EBP1 /eIF4E cascade by 4EBP1A4, an unphosphorylatable form of 4EBP1, significantly delayed, AKT/Ras induced hepatocarcinogenesis. Combined treatment with Rapamycin and 4EBP1A4 completely inhibited AKT/Ras hepatocarcinogenesis. This strong anti-neoplastic effect was successfully recapitulated by ablating Raptor, the major subunit of mTORC1, in AKT/Ras-overexpressing livers. Furthermore, we demonstrate that overexpression of eIF4E, the protooncogene whose activity is specifically inhibited by 4EBP1, resulted in HCC development in cooperation with activated Ras. Mechanistically, we identified the ENTPD 5/AK1 /CMPK1 axis and the mitochondrial biogenesis pathway as targets of the 4EBP1 /eIF4E cascade in AKT/Ras and Ras/eIF4E livers as well as in human HCC cell lines and tissues. Conclusions: Complete inhibition of mTORC1 is required to suppress liver cancer development Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A37 A38 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen induced by AKT and Ras protooncogenes in mice. The mTORC1 effectors, RPS6 and eIF4E, play distinct roles and are both necessary for AKT/Ras hepatocarcinogenesis. These new findings might open the way for innovative therapies against human hepatocellular carcinoma. Corresponding author: Evert, Matthias E-Mail: matthias.evert@uni-greifswald.de 4.5 A20(TNFAIP3) as modulator of TNFa-induced responses in mouse hepatoma cell lines and primary mouse hepatocytes Pinna F1, Bissinger M1, Schirmacher P1, Breuhahn K1 University of Heidelberg, University Hospital, Institute of Pathology, Heidelberg, Germany 1 Backround/Aims: The tumor necrosis factor-a (TNFa)/NF-kB pathway is known to be involved in several cell responses depending on the nature of its stimulation. In liver, specific macrophage- or endothelial cellsderived TNFa defines very different cellular behaviors in hepatocytes (apoptosis, survival, proliferation). Different in vivo and in vitro models show that TNFa stimulation combined with simultaneous perturbation of NF-kB signalling is leading to apoptosis. Input signals from TNFa require processing from a protein complex system downstream of the TNFa receptor (TNFRI), referred as signalosome. However, molecular mechanisms involved in TNFa/NF-kB-mediated the decision making process are not completely understood, so far. In this work we therefore aim to analyze the role of signalosome-associated TNFa-induced protein 3 (TNFAIP3, synonym: A20) as a critical rheostat factor involved in the specific input/output processing after TNFa stimulation in mouse hepatocytes and hepatoma cell lines. Methods: The time-resolved response of NF-kB and JNK/p38 pathway constituents and target genes (e.g., p65, p-p65, IkB-a, p-IkB-a, A20, JNK, pJNK, p38, pp38) were quantitatively defined using western immunoblotting and real-time PCR (12 time points). Different modes of TNFa stimulation (pulses experiment: 1 ng, 2.5 ng, 5 ng, 10 ng TNFa) were performed in primary mouse hepatocytes and hepatoma cells lines in order to determine specific outputs (NF-kB and JNK/p38 pathway activation). Modulation and activity of downstream signaling (NF-kB, JNK/p38) was measured after knockdown of A20 (siRNA) in a mouse HCC cell line (Hepa1 – 6). Results: We demonstrated that single TNFa treatment in Hepa1 – 6 or primary mouse hepatocytes defines specific response from NF-kB and JNK/p38 (Pinna et. al.Front Physiol. 2012Dec 31;3:466.).After initial activation of signalling (5’ to 20’) the responses (p-p65, p-JNK and p-p38) decreased until the end of our time detection window (240’). The response amplitudes correlated with the respective input of TNFa. Sequential stimulation with TNFaafter the first pulse (t= 0) a second (t = 1 h) or third pulse (t = 2 h) was not able to elicit any additional response from NF-kB signaling (pp65). In contrast, an induction of JNK phosphorylation was observed (t = 1:05 h, t = 1:10 h). SiRNA-mediated suppression of A20 about 70% was able to modulate JNK but not NF-kB signaling after TNFaadministration indicating different inhibitory activities from A20 toward the two pathways. Conclusion/Outlook: NF-kB and JNK signaling respond differently to varying modes of TNFa stimulation. Because input signals are processed by signalosome, it is likely that this protein complexes capable of interpreting and initiating respective output signals. A20 plays a role in decision making process discriminating between TNFa-induced NF-kB and JNK signaling. Current work is focusing on the molecular mechanisms of A20-dependent pathway modulation and its functional relevance with regard to cell proliferation and apoptosis. Current work is focusing on the molecular mechanisms of A20-dependent pathway modulation and its functional relevance with regard to cell proliferation and apoptosis. Corresponding author: Pinna, Federico E-Mail: federico.pinna@med.uni-heidelberg.de 4.6 Activation of PP2A as possible mechanism in HCC therapy Curth HM1, Bowe A1, Hoffmann V1, Goeser T1, Nierhoff D1 University Hospital of Cologne, Department of Gastroenterology and Hepatology, Cologne, Germany 1 Background: Hepatocellular carcinoma (HCC) is one of the most common solid tumor entities worldwide and the third leading cause of cancer related death. For advanced stage disease, systemic pharmacotherapy is the only established therapy, targeting the oncogenic protein kinases pathways. However, chemotherapy still yields poor response rates and survival in those patients. Recently, it could be demon- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York strated, that activating the protein phosphatase pathways may have a therapeutic impact on various types of cancer. Methods: The murine and human HCC cell lines Hepa 1 – 6, Hepa 129, HuH7, HepG2 and Hep3B were used for in vitro studies. Cells were treated with either direct (N-hexanoyl-D-sphingosine) or indirect (N,N-dimethylsphingosine, COG449) protein phosphatase 2A (PP2A) activators and cell proliferation, apoptosis and necroptosis were assessed by neutral red staining. PP2A activity was assessed by coimmunoprecipitation and consecutive activity assay. Regulation of the PP2A inhibitory proteins I1PP2A, I2PP2A and CIP2A, as well as signal transduction pathways, were analysed by Western Blot and qRT-PCR. Human HCC tissue samples, obtained from surgical resection were tested for the above mentioned proteins (n= 22) in relation to tumor-free surrounding liver tissue and correlated with their Ki67 expression. Results: The activity of the PP2A inhibitory proteins was markedly up-regulated in mouse and human HCC cell lines. Furthermore, pharmacologic inactivation of I2PP2A, as well as direct or indirect activation of PP2A, led to an AKT mediated growth suppression of HCC cells in vitro, which was at least partly dependent on necroptosis induction. In human HCC, increased levels of I1PP2A, I2PP2A and CIP2A were furthermore significantly correlated to cell proliferation. Conclusions: Our data demonstrate that the protein phosphatase pathway is a potential novel treatment target in HCC and PP2A activators represent possible agents in the future therapy of this malignancy. Corresponding author: Curth, Harald M E-Mail: Harald-Morten.Curth@uk-koeln.de 4.7 Application of mathematical modelling to assess the functional importance of HIF1A for hepatoma biology Kettelhake A1, Berndt N3, Vvedenskaya O4, Mastrobuoni G4, Bielow C4, Kempa S4, Holzh!tter HG3, Cramer T1 1 RWTH Aachen, Surgery/Molecular Tumor Biology, Aachen, Germany; 2Charit#, Hepatology & Gastroenterology, Berlin, Germany; 3Charit#, Biochemistry, Berlin, Germany; 4MDC, BIMSB, Berlin, Germany Liver cancer is becoming a major health problem in western societies due to constantly rising incidence and loss of effective long-term treatment options. HIF1A is frequently overexpressed in human cancers as well as murine tumor models and considered to be an attractive target for innovative cancer therapy. While hepatoma shows evidence for an activated hypoxic response, the functional importance of HIF1A for hepatoma biology remains largely elusive. Using mass spectrometry we have performed a detailed analysis of the tumor-specific proteome during hepatoma development in a murine model system (ASV-B). Protein abundance values were incorporated into a mathematical model of the central carbon metabolism (CCM) of primary hepatocytes that had been established earlier by the Holzh!tter group. This model comprises detailed kinetics of all CCM enzymes based on published kinetic rate constant and enables computational modelling of product generation dependent on substrate concentration of various metabolic pathways. By applying this model, we were able to show that hepatoma-specific knock-out of HIF1A (via albumin-cre) substantially affects various important CCM pathways. For example, KO tumors displayed a mitochondrial membrane potential significantly closer to the values of primary hepatocytes than WT tumors. This was paralleled by a higher consumption of oxygen of the KO hepatomas. In addition, urea cycle activity, which was shown to be significantly inhibited in WT tumors, was unchanged in KO samples, argueing for a central role of HIF1A for the loss of urea cycle activity during hepatoma development. Taken together, we present the applicability of mathematical modelling of dynamic metabolic pathways important for tumor biology. Our aim is to model the metabolic response to specific perturbations (e.g. chemotherapy) in order to identify new therapy targets and possibilities for effective combination therapies. Corresponding author: Cramer, Thorsten E-Mail: tcramer@ukaachen.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 4.8 Array-based gene expression analysis of M1/ M2-polarized macrophages during treatment with multi-kinase inhibitor Sorafenib Sprinzl MF1, Marquardt J1, Brigitte B1, Weinmann A1, Lang H2, Galle PR1 1 Universit$tsmedizin Mainz, I. Medizinische Klinik, Mainz, Germany; 2Universit$tsmedizin Mainz, Chirurgische Klink, Mainz, Germany Background: Multi-kinase inhibitor Sorafenib is the only approved systemic treatment for hepatocellular carcinoma (HCC) and also exerts modulation of tumor-associated macrophages (TAM), enhancing tumor-directed immune responses. Aiming for a better understanding of these effects we searched for gene expression signatures following Sorafenib treatment of cultured macrophages with a classical (M1) or an alternative TAM-like (M2) polarization state. Methods: Monocyte-derived macrophages either polarized in presence of GM-CSF (M1) or CSF-1 (M2) for 7 days were cultured with Sorafenib (2.5 mg/ml) for 3 hours, followed by stimulation with LPS for additional 3 hours. Macrophage activation was monitored by IL-6 and CD163 release assays via ELISA. Illumina gene arrays of total cRNA preparations were performed in triplicates following the different treatments. Non-treated or resting M1 /M2-macrophages served as controls, respectively. Results: M1- and M2- macrophages developed the typical polarization-related phenotype and showed different IL-6 (M1) and CD 163 (M2) release upon LPS-stimulation. Treatment with Sorafenib induced IL-6 secretion and reduced CD163 shedding in M2-polarized macrophages, suggesting immune priming and reversion of alternative polarization in these cells. Array analysis revealed distinct transcription patterns in stimulated M1- and M2-macrophages. Hereby a higher expression of alternative polarization markers, such as IL-10, TGF-beta and CD163, was confirmed in M2compared to M1- macrophages. Array analysis identified 20 genes significantly affected by Sorafenib treatment (p < 0.001) with impact on apoptosis, immune cell differentiation and IL-10 related signaling pathways, suggesting an immunomodulatory effect. CD163 reduction by Sorafenib, as observed by ELISA, was reproducible in array analysis but did not reach the significance level. Conclusion: Preliminary expression analysis identified distinct features of M1- and M2-polarized macrophages in vitro and confirmed their known functional and phenotypic pattern. Treatment with the multi-kinase inhibitor Sorafenib affected expression signatures involved in M2-macrophage driven immunosuppression, which provides deeper insight into the action of current treatment for HCC. Corresponding author: Sprinzl, Martin F E-Mail: martin.sprinzl@unimedizin-mainz.de 4.9 Comprehensive profiling and predictive molecular marker identification for hepatocellular carcinoma Waldburger N1, Endris V1, Penzel R1, Schemmer P2, Weiss KH3, Straub B1, Longerich T1, Schirmacher P1, R"ssler S1 1 Heidelberg University, Institute of Pathology, University Hospital Heidelberg, Heidelberg, Germany; 2Heidelberg University, Department of General and Transplant Surgery, University Hospital Heidelberg, Heidelberg, Germany; 3 Heidelberg University, Department of Internal Medicine IV, University Hospital Heidelberg, Heidelberg, Germany Background: Hepatocellular carcinoma (HCC) is mostly diagnosed in advanced clinical stages with limited therapeutic options and poor prognosis. Predictive biomarkers and corresponding targeted therapy is still missing for HCC. The only approved systemic drug on the market is the multi-kinase inhibitor Sorafenib, but the results are modest with an additional overall survival of 2 – 3 months. Nevertheless, there are many clinical trials ongoing; however, many fail due to the empiric design. Unlike other tumor entities, no predictive biomarkers with corresponding targeted therapy have so far been established for HCC, although existing molecular studies could identify different genetic alterations, e.g. somatic mutation and amplification of potential target genes. Methods: To establish predictive therapeutic biomarkers for HCC we performed comprehensive molecular profiling of HCC focusing on biomarkers already established for other tumor entities (EGFR, BRAF, KRAS, ALK, cMET, FGF19) and HCC gene alterations frequently found in other studies (CTNNB1, AXIN1, TP53). We tested a well characterized HCC cohort consisting of 127 human HCCs with comprehensive pathological and clinical, including survival data. To unravel genetic changes, we designed a gene panel for next generation sequencing using the Ion Torrent Personal Genome Machine (PGM). To detect alterations on protein level and gene copy number alterations, immunohistochemistry and chromogenic in situ hybridization (CISH) of the same cohort on a tissue microarray (TMA) was used. Results: We detected somatic mutations in different genes, mostly in which well-known HCC-alterations have been described (in decreasing order of frequency: CTNNB1, TP53, AXIN1, CDKN2A, ARID2, SMAD4, PIK3CA, ARID 1A, HNF1A, SMAD2, NFE2L2, PTEN) and additionally 8 cMET mutations that have not been described in HCC before (cosmic database). On protein level, 16% cases showed cMET overexpression (MET-high) and 8% nuclear p53 overexpression. In addition, 3% of the HCCs exhibited an amplification of CCND 1 (cyclin D1), which is a close neighbor of FGF19 on the 11q13.3 amplicon and therefore suggest that CCND1 and FGF19, which are frequently co-amplified, may be potential drug targets in HCC. Conclusion: In this comprehensive HCC profiling study, we could confirm existing gene alterations and the so far proposed molecular classification of HCC. In addition, for the first time, we detected 8 cMET mutations in liver carcinoma and thus identified cMET as well as CCND1 and FGF19 as interesting novel therapeutic targets. Corresponding author: Waldburger, Nina E-Mail: Nina.Waldburger@med.uni-heidelberg.de 4.10 Cooperative function of YAP and TAZ in hepatocytes and hepatocarcinogenesis Lutz T1, Weiler S1, Pinna F1, Wan S1, Marquardt J2, Lang H3, Schirmacher P1, Breuhahn K1 1 Ruprecht-Karls-University, Institute of Pathology, Heidelberg, Germany; 2Johannes Gutenberg-University, Department of Internal Medicine I, Mainz, Germany; 3 Johannes Gutenberg-University, Department of General, Visceral and Transplant Surgery, Mainz, Germany Background: The Hippo pathway with its two downstream effectors, the transcriptional co-activators YAP (yes-associated protein) and TAZ (WW Domain Containing Transcription Regulator 1), is a central regulator of organ size. Inactivation of this pathway or overexpression of YAP has been demonstrated to induce hepatomegaly and liver cancer in mice. TAZ has been implicated in the regulation of epithelial-mesenchymal transition (EMT) and invasiveness of breast cancer cells. However, comparative analyses on the expression and cooperative function of YAP and TAZ under physiological conditions (e.g. liver regeneration) and during hepatocarcinogenesis are missing. Methods: Expression levels and subcellular localization of YAP and TAZ in murine livers after partial hepatectomy (PHx) were analysed at the mRNA and protein levels. Cell viability and apoptosis as well as the expression of YAP and TAZ target genes of hepatocellular carcinoma (HCC) cells were analysed after siRNA-mediated knockdown of YAP and TAZ alone and in combination. Expression of both factors was defined in primary human HCCs (n = 20). Results: In liver regeneration, YAP and TAZ were differentially regulated: while the YAP transcript level did not change, a twofold induction was observed for TAZ in the proliferative phase of liver regeneration (after 8 – 24 hours). However, both transcriptional co-activators exhibited similar dynamics during that time span on protein level. YAP as well as TAZ siRNA-mediated silencing led to significant changes in cell viability and apoptosis, which is amplified after combined inhibition of the two proteins. Target gene analysis revealed the presence of common and exclusive downstream effectors for YAP and TAZ. Interestingly, YAP positively regulated TAZ expression in livers of Yap transgenic animals and in HCC cells. Expression of YAP and TAZ significantly correlated in human HCCs and surrounding normal liver tissue. Summary and Conclusion: Although regulated by common upstream mechanisms, YAP and TAZ facilitate distinct and common biological functions in physiological processes (e.g., liver regeneration) and in liver cancer cells. This is supported by the fact that YAP- and TAZ-deficient mice exhibit distinct phenotypes: YAP-null mice die during embryogenesis with defects in body axis elongation, while TAZ-null mice are viable. Their dynamic expression during liver regeneration and the mutual regulation strongly indicate that both factors are necessary to facilitate the mechanosensor function of the Hippo pathway. Corresponding author: Lutz, Teresa E-Mail: Teresa.Lutz@med.uni-heidelberg.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A39 A40 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 4.11 Cyclin E1 expression level determines the anti-proliferative response of the pharmacological Cdk2 inhibitor Roscovitine in hepatoma cells and in the liver Nevzorova YA1, Hu W1, Haas U1, Hoeltke N1, Trautwein C1, Liedtke C1 1 RWTH University Hospital Aachen, Department of Internal Medicine III, Aachen, Germany Background & Aims: The cyclin-dependent kinase inhibitor Roscovitine (Rosc) has been regarded as a promising anti-cancer agent. However, the anti-proliferative effects of Rosc in hepatoma cells and in the liver are currently unknown and were investigated in the present study to elucidate if Rosc could be a therapeutic option for the treatment of HCC. Methods: The anti-proliferative and pro-apoptotic properties of Rosc were analyzed in murine hepatoma cells and primary hepatocytes in vitro and in mice following partial hepatectomy (PH) in vivo. Potential off-target effects of Rosc were investigated in mice with ubiquitous deletion of Cyclin E1 (CcnE1-/-), Cyclin E2 (CcnE2-/-) or hepatocytespecific inactivation of Cdk2 (Cdk2Dhepa), respectively. Results: In vitro, cell cycle activity and cell viability were dramatically reduced by Rosc in Hepa1 – 6 hepatoma cells and in primary hepatocytes. In vivo, we subjected wildtype (WT) mice to PH and applied Rosc 28 and 40 hours (h) after surgery. Rosc treatment significantly diminished DNA-synthesis and completely blocked both Cdk2 and Cdk1 kinase activities in liver, 48 h after PH. However, this inhibition was transient; delayed DNAsynthesis, full restoration of Cdk1 kinase activity and slight activation of Cdk2 occurred in Rosc-treated mice 72 h post-surgery. We previously demonstrated that genetic deletion of Cdk2 had no effect on liver regeneration. Intriguingly, Rosc application after PH inhibited DNA-synthesis in WT and Cdk2Dhepa livers to the same extend. Thus, the inhibitory effect of Rosc in liver is not mediated via Cdk2 but most likely through inhibition on both Cdk2 and Cdk1. To further evaluate the role of ECyclins for the inhibitory effect of Rosc, we applied this drug to CcnE2-/and CcnE1-/- mice after PH. Ablation of Cyclin E1 accentuated the inhibitory effects of Rosc. In contrast, Rosc treatment induced only a slight reduction of DNA-synthesis in CcnE2-/- mice after PH. Since genetic inactivation of Cyclin E2 results in over-expression of CcnE1, we hypothesized that cell cycle inhibition by Rosc can be in part rescued by high expression level of Cyclin E1. We therefore investigated the antiproliferative effects of Rosc in hepatoma cells with different Cyclin E1 expression levels due to adenoviral over expression or conditional gene ablation. Interestingly, we found a strong synergistic cell cycle inhibition by Cyclin E1 ablation and Rosc treatment in vitro. In contrast, adenovirus-mediated Cyclin E1 over-expression partially rescued the cell cycle arrest by Rosc. Conclusion: Rosc can inhibit proliferation of healthy regenerating hepatocytes and immortalized hepatoma cells most likely through blocking of Cdk1 and Cdk2, as initially suggested. The inhibitory effect of Rosc inversely correlates with endogenous levels of Cyclin E1 expression. This suggests that only HCC patients with moderate hepatic Cyclin E1 expression may benefit from a potential Rosc therapy. Corresponding author: Nevzorova, Yulia A. E-Mail: ynevzorova@ukaachen.de 4.12 Deficiency of calcium-independent phospholipase A2 beta in vivo causes systematic inflammation and hepatocellular carcinoma Wei W1, Inhoffen J1, Straub B2, Tuma S1, Stremmel W1, Chamulitrat W1 1 Heidelberg University Hospital, Internal Medicine IV (Gastroenterology and Hepatology), Heidelberg, Germany; 2 Heidelberg University Hospital, Pathology Institute, Heidelberg, Germany Introduction: Calcium-independent phospholipaseA2beta (iPLA2beta), which is one of the patatin-like phospholipase domain-containing genes, catalyzes the hydrolysis of phospholipids for cell membrane remodeling. It is known that iPLA2beta produces lysophosphatidylcholine as a ’find me signal’ for phagocytes to remove apoptotic cells. We hypothesize that deficiency of iPLA2beta leads an accumulation of apoptotic cells, and that the subsequent inflammatory pressure induces the generation of proliferative hepatocytes which further leads to hepatocellular carcinoma (HCC). Methods: Whole body iPLA2beta-/- (with the deletion of the catalytic domain exon 9) and wild-type (WT) male mice were allowed to age to 20 months old. Histology and immunohistochemistry of livers, spleen and mesenteric lymph nodes were per- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York formed. Results: Compared with WT, iPLA2beta-/- mice exhibited reduced body, liver and visceral fat weight, and showed increased serum transaminases. Hepatic steatosis was observed in aged WT, but not in mutant livers. Not seen in WT livers, livers of mutant mice exhibited periportal inflammation, cholangitis, and necrosis with a 50 %, 11%, 20 % incidence rate, respectively. The mutant livers showed significant fibrosis as seen by Sirius red and a-smooth muscle actin staining. Mutant mice also had significantly decreased cellularity of B cells in the cortex of mesenteric lymph nodes concomitant with increased apoptosis in spleen. Among 34 aged mutant mice, 24% of them had large and dark reddish nodular HCC which showed portal vein obliteration and an invasion front together with decreased epithelial marker E-cadherin, and increased proliferation marker Ki67. The observed loss of cytokeratin 19 in mutant nodular HCC indicated the destruction of bile duct architecture. We also observed small and light color nodules of adenoma or HCC in 10 % of 28 aged WT commonly seen in C 57 /BL6 mice. In another mouse line, the mutation in exon 7 of iPLA2beta gene did not produce any fibrosis nor HCC. Finally, iPLA2beta was expressed in normal human livers with or without steatosis, while being completely absent in human HCC livers without steatosis. Conclusions: In an absence of steatosis, the deficiency of exon 9 in iPLA2beta gene caused systemic inflammation which led to chronic aggressive hepatitis, fibrosis and HCC. Thus, iPLA2beta regulation on apoptosis in liver and immune organs may exacerbate in the development of HCC during aging. Corresponding author: Chamulitrat, Walee E-Mail: Walee.Chamulitrat@med.uni-heidelberg.de 4.13 Development of delivery, targeting, and imaging strategies to improve oncolytic vesicular stomatitis virus therapy for hepatocellular carcinoma Altomonte J1, R"der R2, Mu&oz 'lvarez KA3, Grunert D1, Wagner E2, Ebert O1 1 Klinikum rechts der Isar, Technische Universit$t M!nchen, Department of Medicine II, Munich, Germany; 2Ludwig Maximilian University of Munich, Department of Pharmaceutical Biotechnology, Munich, Germany; 3 Klinikum rechts der Isar, Technische Universit$t M!nchen, Department of Diagnostic and Interventional Radiology, Munich, Germany Hepatocellular carcinoma (HCC) is a disease with rising incidence, limited treatment options and poor prognosis, representing a major worldwide health concern. Due to the vast deficit of viable treatment options, oncolytic viruses have emerged as promising alternative therapies to specifically target and lyse tumor cells. We have previously demonstrated the safety and efficacy of oncolytic vesicular stomatitis virus (VSV) applied via hepatic arterial infusion to treat orthotopic HCC in immune-competent rats, and based on encouraging data such as these, a recombinant VSV vector has recently entered the clinic in phase I trials for HCC in patients. Although systemic administration of oncolytic viral therapies is ideal for targeting metastatic disease, the efficacy of such an approach is extremely compromised due to rapid clearance from circulation as a result of neutralizing blood components and non-specific uptake by liver and spleen. Furthermore, the complex microenvironment in the liver poses a unique set of challenges to the fate of oncolytic viral therapies directed at hepatic tumors. Although attempts to shield viruses from adverse interactions have led to increased circulation times in vivo, they are also associated with decreased infectivity of the target cells. We have therefore developed several strategies, including novel cell carrier and synthetic shielding approaches, to simultaneously protect VSV from nonspecific interactions and deliver it specifically to the tumor target, where it can exert its oncolytic effect. Because a variety of immune cells possess the inherent ability to take up oncolytic virus and subsequently home to tumor beds, they offer the unique dual benefit of delivering viruses in stealth, while contributing to antitumor immune responses. Alternatively, synthetic polymers can provide highly effective shielding through surface modification of oncolytic viruses and have the advantage of being adaptable to optimize the shielding effect. Through the incorporation of targeting ligands or selectively cleavable linkers, the ability of the virus to infect is then rescued locally and specifically at the tumor site. Furthermore, advancement of imaging technologies allows us the possibility to monitor the biodistribution of these shielded viruses to observe the circulation time and replication kinetics noninvasively and in real-time, which will further facilitate the clinical translation of oncolytic virus therapies. A summary of these novel approaches to enhance oncolytic VSV accumulation within orthotopic HCC tumors 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen and improve the therapy outcome, as well as virus imaging strategies, will be presented. Corresponding author: Altomonte, Jennifer E-Mail: jennifer.altomonte@lrz.tum.de 4.14 Die Kostimulation mit CD 40Ligand steigert die Immunantwort von Tumorantigen gepulsten humanen dendritischen Zellen gegen"ber humanen hepatozellul!ren Karzinom- (HCC) und Cholangiozellul!ren Karzinom- (CCC) Zellen Vogt A1, Hillebrand RM2, Raskopf E1, Schmidt-Wolf I2, Strassburg CP1, Gonzalez-Carmona MA1 1 University Hospital of Bonn, Medical Clinic and Polyclinic I, Bonn, Germany; 2University Hospital of Bonn, Center for Integrated Oncology (CIO), Bonn, Germany Einleitung: Dendritische Zellen (DC), als professionelle antigenpr"sentierende Zellen, k#nnen antigenspezifische T-Zellen stimulieren. Um eine effektive Immunatwort zu initiieren, ist die Interaktion von CD 40 /CD 40Ligand (CD 40L) auf DC und T-Zellen von großer Bedeutung. In eigenen Vorarbeiten konnte bereits gezeigt werden, dass die Verwendung des kostimulatorischen Molek!ls CD 40L die DC-vermittelte Immunantwort gegen das HCC im Mausmodell verst"rken kann. Ziel dieses Projektes war zu untersuchen, ob CD 40L die Immunantwort humaner dendritischer Zellen (DC) gegen!ber humanen HCC und CCC Zellen verst"rkt. Methodik: Adenovirale Vektoren kodierend f!r das humane CD 40L wurden nach dem AdenoEasy-System hergestellt. Humane DC aus gesunden Probanden wurden mit Tumorlysat am Tag 5 beladen und adenoviral mit Ad-hCD 40L am Tag 6 transduziert. An Tag 8 wurden diese mittels Durchflusszytometrie ph"notypisiert und die Zytokinexpression im &berstand der Zellen mittels Elisa quantifiziert. An Tag 8 wurden die transduzierten DC mit autologen Zytokin-induzierten Effektorzellen ko-kultiviert. Anschließend wurde die Proliferation der ZIK-Zellen mittels MTT-Test und ihre Zytotoxizit"t gegen!ber humanen HCC(HepG2, Huh7 und CCL13) bzw. CCC-Zellen (EGI-1 und Mz-ChA-2) untersucht. Die Apoptoserate wurde durch Bestimmung der Sub-G1-Fraktion nach Inkubation der HCC- und CCC-Zellen mit &berstand von AdhCD 40L-transduzierten DC untersucht. Ergebnisse: Die Transduktion von DC mit Ad-hCD 40L f!hrte zu einer starken CD 40L-Expression in 35% der Zellen. Zudem zeigten Ad-hCD 40L-transduzierte DC einer signifikante Steigerung der CD83- (90 %) und CCR7-Expression (60 %) im Vergleich zu den Kontrollen. Im Zellkultur!berstand Ad-hCD 40L-transduzierter DC konnte eine signifikant h#here Produktion von Th 1-Zytokine (IL-12, IFNgamma) nachgewiesen werden. Ad-hCD 40L-transduzierte DC konnten die ZIK-Zellen signifikant st"rker stimulieren, was sich in einer h#heren Proliferationsrate zeigte im Vergleich zu den ZIK-Zellen, die mit Ad-Mock-transduzierten DC oder mit untransduzierten DC kokultiviert wurden. Funktionelle Untersuchungen zeigten zudem eine signifikant st"rkere Zytotoxizit"t gegen!ber den humanen HCC- und der CCC-Zellen, wenn diese zuvor mit Ad-hCD 40L-transduzierten DC ko-kultiviert wurden. Interessanterweise, konnte eine signifikant erh#hte Apoptoserate nach der Inkubation mit &berstand von den AdhCD 40L- tranduzierten DC in Huh-7, HepG2- sowie Mz-ChA-2-Zellen ermittelt werden, hingegen nicht in CCL13 und EGI-1 Zellen. Diskussion: Unsere Daten zeigen, dass die adenoviral vermittelte Expression von hCD 40L zu einer deutlich st"rkeren Immunstimulation humaner DC f!hrt, einhergehend mit einer vermehrten Expression ko-stimulatorischer Molek!le, Chemokine sowie Th1 Zytokine. Weiterhin konnten hCD 40L-exprimierende DC tumor-spezifische Effektorzellen stark stimulieren, um so eine effektive Immunantwort gegen!ber humane HCC und CCC Zellen, sowie eine gesteigerte Apoptoserate der Tumorzellen zu induzieren. Diese Resultate zeigen, dass CD 40L ein vielversprechender Ansatz zur Optimierung einer DC-basierten Immuntherapie des HCC und CCC darstellt. Korrespondierender Autor: Vogt, Annabelle E-Mail: Annabelle.Vogt@ukb.uni-bonn.de 4.15 Eine Sequenzvariation in der Bindungsstelle des Transkriptionsfaktors GATA ist verantwortlich f"r eine verminderte TRAIL Regulation beim humanen HCC Piras-Straub K2, Khairzada K1, Paul A2, Canbay A1, Gerken G1, Herzer K1 1 University Hospital of Essen, Gastroenterology and Hepatology, Essen, Germany; 2University Hospital of Essen, Department of General Surgery, Essen, Germany Hintergrund: Das hepatozellul"re Karzinom (HCC) ist einer der h"ufigsten malignen Tumore weltweit. Es ist therapeutisch schwer zug"nglich, was eine schlechte Prognose und hohe Mortalit"t zur Folge hat. Die Entstehungsmechanismen des molekular sehr heterogenen Tumors sind bislang unzureichend verstanden. Das proapoptotische Molek!l TRAIL (Tumor Necrosis Factor Related Apoptosis Inducing Ligand) hat auf Grund seiner Eigenschaft Aufmerksamkeit erregt, in Lebertumorzellen Apoptose auszul#sen, aber nicht in gesundem Lebergewebe. Somit w"re zu vermuten, dass eine verminderte Expression von TRAIL z.B. durch einen Defekt in regulatorischen Elementen des Promoters, einen Wachstumsvorteil f!r ein HCC darstellt. Methoden: Hierf!r wurde Tumorgewebe und tumorumgebendes Lebergewebe von HCC Patienten, die sich einer Leberresektion oder -transplantation unterziehen mussten, hinsichtlich der TRAIL mRNA-Expression mittels qrt-PCR analysiert. Weiterhin wurde die Promoterregion des TRAIL-Gens sequenziert und mittels in silico Analysen auf Variationen in Transkriptionsfaktorbindungsstellen untersucht. Der Einfluss dieser Transkriptionsfaktorbindungsstellen auf die Induzierbarkeit des TRAIL-Promoters wurde mit Hilfe von Reportergenkonstrukten mit intakter oder defekter GATA-1 Bindungsstelle untersucht. Ergebnisse: Die Expression von TRAIL ist im HCC Gewebe, verglichen mit der umgebenen nicht tumor#sen Leber, signifikant (P £ 0,012) verringert. Dar!ber hinaus ergibt sich f!r Tumoren mit zunehmendem Tumorstadium eine verminderte TRAIL-Expression. Die Sequenzanalyse der TRAIL-Promoterregion ergab, dass mehr als 30 % der HCC Patienten eine Variation an Position -1482 des TRAIL Promoters aufwiesen, die laut in silico Untersuchungen zu einem Verlust der Bindungsstelle des Transkriptionsfaktors GATA-1 f!hrte. Die in situ Korrelation dieser Ergebnisse zeigte, dass die Expression von TRAIL in Patienten mit defekter GATA-1 Bindungsstelle signifikant (P £ 0.046) niedriger ist als in Patienten mit intakter GATA-1 Bindungsstelle. Die Reportergenassays der TRAIL Promoterkonstrukte zeigten, dass die Funktionalit"t des TRAIL Promoters bei Mutation der GATA-1 Bindungsstelle zwar weiterhin gegeben ist, die Behandlung mit bekannten, TRAIL induzierenden Substanzen (IFN-a, IFN-g, TGF-b, SAHA, etc.) jedoch zu einer signifikant verringerten Induzierbarkeit des TRAIL Promoters f!hrt. Schlussfolgerungen: Eine verminderte TRAIL Expression scheint einen Wachstumsvorteil f!r das HCC zu bedeuten. Die GATA-1 Bindungsstelle an Position -1482 des TRAIL-Promoters ist maßgeblich bei der Regulation der TRAILExpression involviert. Ein Defekt dieses responsiven Elementes f!hrt zu einer Reduktion der TRAIL-Expression, mit entscheidenden Konsequenzen f!r die Entstehung und das Wachstum eines HCC. Korrespondierender Autor: Piras-Straub, Katja E-Mail: katja.straub@uk-essen.de 4.16 Einfluss metabolischer Faktoren auf die Prognose von Patienten mit fortgeschrittenem hepatozellul!rem Karzinom unter Sorafenib Therapie Koch S1, Presonil V1, Marquardt J1, Galle PR1, Weinmann A1, W"rns MA1 1 Universit$tsmedizin der Johannes Gutenberg-Universit$t Mainz, I. Medizinische Klinik und Poliklinik, Mainz, Deutschland Einleitung: Das Vorhandensein eines Diabetes mellitus bzw. einer Adipositas ist bei Patienten mit hepatozellul"rem Karzinom (HCC) mit einer schlechten Prognose assoziiert, insbesondere was die Rezidivrate nach chirurgischer Therapie, aber auch den Verlauf unter transarterieller Chemoembolisation angeht. Der Einfluss metabolischer Faktoren auf die Prognose von Patienten mit fortgeschrittenem HCC unter Sorafenib Therapie ist nicht bekannt. Methoden: Retrospektive Analyse an 152 Patienten mit fortgeschrittenem HCC, die von Januar 2007 bis Dezember 2013 an der Universit"tsmedizin Mainz mit Sorafenib therapiert wurden. Das Gesamt!berleben der Gruppen wurde mithilfe der Kaplan Meier Methode analysiert; getrennt nach dem Vorliegen eines Diabetes mellitus (DM), von &bergewicht/Adipositas (&A) bzw. eines metabolischen Syndroms (MS; definiert durch das Vorhandensein von mind. 2 Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A41 A42 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen von 4 Risikofaktoren: Diabetes mellitus, Arterielle Hypertonie, &bergewicht/Adipositas, Hyperlipoprotein"mie). Ergebnisse: Ein DM, &A bzw. MS lag bei 55 (36 %), 85 (56%) bzw. 78 (51 %) der Patienten vor. Abgesehen von metabolischen Faktoren (Nicht-alkoholische Fettlebererkrankung, Vorhandensein von DM, &A, MS, h#herer Body Mass Index; p < 0.05) unterschieden sich die drei Gruppen nicht signifikant vom jeweiligen Kontrollkollektiv hinsichtlich Geschlecht, Alter, (tiologie der Lebererkrankung, Leberfunktion (Zirrhose, Child-Pugh Status, Vorliegen von Ascites), Tumorstadium [BCLC, Vorliegen einer Pfortaderthrombose], ECOG PS, Dauer der Sorafenib-Therapie, Rate an Zweitlinien-Therapie bzw. Begleiterkrankungen (p > 0.05). Das mediane &berleben mit oder ohne Vorliegen eines DM lag bei 7.15 bzw. 6.72 Monaten (p = 0.291), das mediane &berleben mit oder ohne Vorliegen eines &A lag bei 7.15 bzw. 6.16 Monaten (p = 0.117) und das mediane &berleben mit oder ohne Vorliegen eines MS lag bei 7.61 bzw. 6.07 Monaten (p = 0.327). Patienten mit einem DM bzw. einem MS nahmen signifikant h"ufiger Metformin ein (p < 0.001 bzw. p = 0.001). Schlussfolgerung: Das Vorliegen eines DM, von &A oder eines MS hat keinen erkennbar negativen Einfluss auf die Prognose von Patienten mit fortgeschrittenem HCC unter Sorafenib Therapie. Korrespondierender Autor: W#rns, Marcus-Alexander E-Mail: Marcus-Alexander.Woerns@unimedizin-mainz.de 4.17 Engraftment and transdifferentiation of ectopic transplanted mature hepatocytes in a liver environment with ongoing biliary fibrosis Yovchev M1, Locker J1, Oertel M2 1 University of Pittsburgh, Pathology, Pittsburgh, USA; 2 University of Pittsburgh, Pathology, McGowan Institute for Regenerative Medicine, Pittsburgh, USA Our current studies are aimed to determine whether ectopic transplanted hepatic epithelial cells can migrate, engraft and repopulate a liver environment with ongoing biliary fibrosis. Biliary fibrosis was induced by common bile duct ligation (BDL) in DPPIV) F344 rats. Using Masson’s trichrome/Sirius red staining and immunohistochemistry for a-SMA, CK-19 and laminin, as well as qRT-PCR analysis of laser-microdissected liver tissues of fibrotic portal areas compared to surrounding parenchyma, we observed characteristic morphological changes in the liver and vigorous expression of fibrogenesis- and biliary epithelial cellspecific genes. Highly purified DPPIV+/GFP+ hepatocytes (HCs) were intrasplenically infused at 2 or 4 weeks after BDL. Although, substantial numbers of infused HCs engrafted in the injection site of the spleen, groups of donor-derived HCs were observed in central portal areas of the recipient liver at day 1. Within one week, transplanted HCs were mainly detected at the periphery of expanding portal areas and formed hepatocytic cell clusters of different size up to 2 months. Engrafted HCs formed also DPPIV+ bile duct structures (CK-19+/claudin-7+). Moreover, transdifferentiation was observed in the majority of intrasplenically engrafted HCs but not in recipient rats without BDL. PCR array analysis demonstrated significant up-regulation of several growth factors in fibrotic portal regions compared to surrounding parenchyma and agematched controls. However, no changes in gene expression profiles were detected in the spleen of BDL rats vs. control spleen, suggesting biliary obstruction induces soluble liver-derived factors that induce transdifferentiation of transplanted hepatocytes. Conclusion: Progressive biliary fibrosis stimulates liver repopulation by ectopic transplanted mature HCs, as well as their transdifferentiation into bile duct structures after engraftment. Corresponding author: Oertel, Michael E-Mail: mio19@pitt.edu 4.18 Entwicklung eines in vivo Transfektionsmodels zur induzierbaren Genexpression in murinen Hepatozyten Hubner EK1, Lechler C1, Kohnke-Ertel B1, Sage J2, Schmid RM1, Ehmer U1 1 Klinikum rechts der Isar, Technische Universit$t M!nchen, II. Medical Clinic and Polyclinic, Munich, Germany; 2 Stanford University, Department of Pediatrics and Genetics, Stanford, CA, USA Einleitung: Studien !ber Signalwege und Tumorentwicklung in der Leber setzen zuverl"ssige Methoden der exogenen Genexpression und des Gen-Knock-downs in der Leber voraus. Wir haben daf!r bereits ein System der stabilen, konstitutiven Genexpression in vivo etabliert, das die Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York Technik der hydrodynamischen Schwanzveneninjektion zusammen mit dem Sleeping Beauty Transposon-System verwendet. Hier stellen wir ein neues System vor, das die Expression eines konstitutiv aktiven Genes mit der Expression eines Doxycyclin-induzierbaren Genes oder einer shRNA mit Hilfe des Tet-On Systems kombiniert. Dieses erlaubt die schnelle, induzierbare und zuverl"ssige Transgenexpression oder den Gen-Knock-down in vivo. Methoden: Die Plasmide wurden mittels hydrodynamischer Schwanzveneninjektion in murine Hepatozyten von Rosa26-mTmG-Reporterm"usen in vivo transfiziert. Das hierf!r verwendetet Vektor-System besteht aus zwei Teilen. Der konstitutiv aktive Teil besteht aus einer Tamoxifen-induzierbaren Cre-Rekombinase, der induzierbare Teil exprimiert !ber das Tet-On System exogene Transgene oder shRNAs in Anwesenheit von Doxycyclin. Die Verwendung eines EntryVektorsystems erlaubt hierbei eine einfache Klonierung der Expressions- und shRNA-Konstrukte. Nach genomischer Integration erfolgte eine Aktivierung der Cre-Rekombinase durch Tamoxifen. Die induzierbare Genexpression wurde durch eine orale Gabe von Doxycyclin ausgel#st. Die Visualisierung der Cre-Aktivierung und der Transgenexpression erfolgte mittels Immunfluoreszenz. Ergebnisse: Nach hydrodynamischer Schwanzveneninjektion wird durch Tamoxifen eine Cre-Aktivierung in transfizierten Hepatozyten erreicht. Diese induziert eine membrangebundene GFP-Expression in bis zu 17% der Hepatozyten in Rosa26-mTmG-Reporterm"usen. Die Aktivierung der induzierbaren Genexpression mittels Doxycyclin f!hrt zu einem zuverl"ssigen Nachweis der Expressionsproteine in den transfizierten Zellen. Die Expression ist hierbei von dem f!r das Tet-On-System verwendeten Promotor abh"ngig. In keinem Fall ließ sich eine Expression des induzierbaren Genes in nicht-transfizierten Hepatozyten oder in Doxycyclin-naiven Tieren nachweisen. Diskussion: Das hier vorgestellte System erlaubt erstmalig die Kombination einer Cre-Lox-vermittelten Genmutation mit einer induzierbaren Genexpression bzw. induzierbarem Gen-Knockdown in vivo. Das System bietet die M#glichkeit zur gezielten Genmutation in der Leber von konditionellen Knock-out-M"usen durch Aktivierung der CreRekombinase in Hepatozyten. In den mutierten Zellen kann mit dem vorgestellten Konstrukt die Relevanz von Zielgenen durch Knock-down oder &berexpression in einem schnellen und einfachen System getestet werden. Dies erlaubt die Analyse komplexer molekularer Zusammenh"nge in unterschiedlichen Systemen und bietet eine vielversprechende Alternative zur zeitaufwendigen und kostenintensiven Generierung von Mauslinien mit den entsprechenden konstitutiven oder konditionellen Keimbahnmutationen. Korrespondierender Autor: Ehmer, Ursula E-Mail: ursula.ehmer@tum.de 4.19 Gene signatures define chromosomal instability (CIN) and poor survival in HCC patients Weiler S1, Wolf T1, Pinna F1, R"ssler S1, Lutz T1, Wan S1, Marquardt J3, Lang H4, Schirmacher P1, Breuhahn K1 1 Ruprecht-Karls-Universit$t, Institute of Pathology, Heidelberg, Germany; 2Ruprecht-Karls-Universit$t, Hartmut Hoffmann-Berling International Graduate School of Molecular and Cellular Biology, Heidelberg, Germany; 3 Johannes-Gutenberg-Universit$t, Department of Medicine I, Mainz, Germany; 4Johannes-Gutenberg-Universit$t, Klinik f!r Allgemein-, Viszeral- und Transplantationschirurgie, Mainz, Germany Background: Chromosomal instability (CIN) is a main characteristic of aggressive tumors and is associated with poor patient prognosis. For different tumor entities such as breast and lung cancer, Carter et al. (2006) defined gene expression signatures which correlate with CIN and poor overall survival of cancer patients. In this study we investigated if HCC patients show elevated expression levels of CIN signature genes and how the overall survival of the patients is affected. Moreover, we addressed whether the presence of the CIN signature is associated with increased chromosomal aberrations. Methods: Gene expression data from 247 HCC patients were clustered hierarchically, plotted in a heatmap and Kaplan-Meier survival analysis was performed (Roessler et al., 2010, 2012). Classification tree (Ctree) analysis was used to determine the most important genes for patient subgroup clustering. Comparative genomic hybridization (CGH) array data were used to asses total chromosomal aberrations by quantifying losses and gains of chromosomal regions. Statistical significance was assessed by Mann-Whitney-U-test. Results were confirmed in an independent cohort using realtime PCR to measure CIN gene mRNA expression levels. Results: Gene expression analysis of HCC patients revealed the presence of the CIN signatures. Patients could be clustered into three different groups with 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen low (26 %), moderate (43 %) and high (31%) expression levels of the CIN signature genes. Survival data analysis showed that patients with high expression levels had the worst overall survival in comparison to patients with moderate or low expression levels. Patients with low CIN gene expression had the best survival prognosis. Classification tree analysis was used to define genes whose expression level classified the patients into the three clusters. PTTG1, CDC20, MAD 2L1 have thus been identified to be possible classifiers of HCC patients. Moreover, CGH data confirmed that elevated expression of CIN signature genes significantly correlated with total genomic aberrations in terms of chromosome losses or gains. In an independent cohort of 20 HCC patients the expression levels of selected CIN genes (n= 9) were measured and revealed significant upregulation in 57 – 82 % of HCC patients. Conclusion: These data demonstrate that the presence of CIN signatures correlate with poor prognosis in HCC patients and could be used to predict overall survival. Genes that classify patients into subgroups according to the expression level of the CIN signature may be used as biomarkers. References: Carter SL, et al., Nat Genet. 2006 Sep;38(9):1043 – 8. Roessler S, et al., Cancer Res. 2010 Dec 15;70(24):10202 – 12. Roessler S, et al., Gastroenterology. 2012 Apr;142(4):957 – 966.e12. Corresponding author: Weiler, Sofia E-Mail: sofia.weiler@med.uni-heidelberg.de 4.20 Hand-foot-syndrome is associated with improved survival in patients treated with sorafenib for hepatocellular carcinoma Pfeiffenberger J1, Gotthardt D1, Unger D1, Radeleff B2, Springfeld C3, Schirmacher P4, Schemmer P5, Stremmel W1, Weiss KH1 1 University Hospital Heidelberg, Department of Gastroenterology and Hepatology, Heidelberg, Germany; 2 University Hospital Heidelberg, Department of diagnostic and interventional Radiology, Heidelberg, Germany; 3 University Hospital Heidelberg, National center for tumor diseases, Heidelberg, Germany; 4University Hospital Heidelberg, Department of Pathology, Heidelberg, Germany; 5 University Hospital Heidelberg, Department of Visceral and Transplant surgery, Heidelberg, Germany Introduction: Hepatocellular carcinoma (HCC) is a frequent complication of chronic liver diseases and a leading cause of cancer related deaths. Systemic treatments for HCC like sorafenib might be limited by toxicity and impaired liver function. Clear parameters predicting to the response to sorafenib therapy are sparse. Patients and methods: Single center cohort study of patients suffering from advanced HCC treated with sorafenib at the university hospital Heidelberg, Germany. Data on adverse events, liver function, remission state and survival were recorded. Influence of adverse events on survival was evaluated in univariate and multivariate analysis. Results: 92 patients could be analyzed. At initiation of systemic treatment with sorafenib 76 patients (83%) presented with Child-Pugh-Score A, 14 patients (15%) presented with Child-Pugh-Score B and 2 patients (2 %) presented with Child-PughScore C. Median overall survival for all patients was 15.9 months. Patients with Child-Score A lived significantly longer than patients with Child-Score B (16.6 vs. 6.9 months). Adverse events were the reason for discontinuation of sorafenib in 26 patients (28%). Overall survival was reduced in patients who showed decreased liver function during sorafenib therapy in comparison to patients with preserved liver function (7.5 vs. 15.7 months). In univariate and multivariate analysis patients suffering from hand-foot-syndrome showed a significantly improved survival (20.3 vs. 11.7 months), while occurrence of diarrhea was not associated with increased survival. Discussion: Systemic treatment in hepatocellular carcinoma is often limited by adverse events and impaired liver function. Our study confirmed cutaneous adverse events as a predictor of improved overall survival. This findings emphasizes the importance of preemptive actions of ensure treatment adherence. Corresponding author: Pfeiffenberger, Jan E-Mail: jan.pfeiffenberger@med.uni-heidelberg.de 4.21 Hepatic steatosis promotes growth and invasiveness of hepatocellular carcinoma cells in vitro and in vivo Koch A1, Thasler WE2, Hellerbrand C1 1 University Hospital Regensburg, Department of Internal Medicine I, Regensburg, Germany; 2Ludwig-MaximiliansUniversity Munich, Grosshadern Tissue Bank and Center for Liver Cell Research, Department of Surgery, Munich, Germany Nonalcoholic fatty liver disease (NAFLD) is associated with increased risk of development of end stage liver disease and cirrhosis, and can be complicated by hepatocellular carcinoma (HCC). Moreover, the metabolic syndrome and hepatic steatosis are independent risk factors for HCC progression also in other types of chronic liver disease. Still, it is incompletely understood how steatosis promotes HCC development and progression. The aim of this study was to analyze the influence of hepatic steatosis on HCC cells in vitro and in vivo. Methods and Results: We applied a syngeneic, orthotopic HCC model, in which we implanted murine Hepa129 HCC cells into the liver of (i) C 3 H/He control mice or (ii) mice fed with a high-fat diet (HFD) causing significant hepatic steatosis. After 14 days, tumors grown in steatotic environment were significantly larger and showed increased expression of mitotic activity. Furthermore, tumors formed in steatotic livers revealed an invasive growth and higher mRNA expression of matrix metalloproteases (MMPs) compared to tumors formed in normal liver tissue, which showed no infiltration in the surrounding liver parenchyma. It has to be noted that under the feeding conditions used the HFD did not cause activation of hepatic stellate cells (HSC) in the non-tumorous liver parenchyme, as evidenced by analysis of a-SMA mRNA expression, a specific and sensitive marker for HSC-activation. However, there was a significant increase of HSC activation in tumors grown in steatotic livers compared to tumors of the control group as shown by a-SMA mRNA and immunohistochemical analysis. This is critical because we and others have shown before that activated HSC promote tumorigenicity of HCC cells. In search for further mechanisms responsible for the enhanced tumorigenicity of HCC cells in fatty liver tissue, we applied different in vitro models. Once, we incubated HCC cells with conditioned medium (CM) of steatotic primary human hepatocytes (PHH) which caused a significant increase of proliferation as compared to HCC cells treated with CM from control PHHs. Furthermore, we observed that addition of FFA to the cell culture medium of HCC cells caused a dose dependent induction of cellular lipid accumulation, which was in line with the observation that also in vivo HCCs grown in mice fed with the HFD revealed higher triglyceride levels compared to HCCs in control livers. Noteworthy, steatotic HCC cells showed enhanced migratory activity in Boyden Chamber assays and higher mRNA expression of MMPs compared to HCC control cells. Conclusions: It appears that there are different mechanisms which are promoting HCC growth in steatotic livers. Once, lipid accumulation in hepatocytes causes secretion of factors promoting tumor growth. In addition, desmoplastic reaction is enhanced in HCC in steatotic tissues and also systemic metabolic changes associated with the metabolic syndrome such as dyslipidemia seem to directly affect HCC cells offering a further option for HCC prevention and treatment. Corresponding author: Koch, Andreas E-Mail: andreas.koch@ukr.de 4.22 Human adult liver stem cells generated from patient samples Gutierrez Jauregui R1, Fekete-Drimusz N1, Manns MP1, Vondran FWR2, Bock M3 1 Hannover Medical School (MHH), Clinic of Gastroenterology, Hepatology und Endocrinology, MHH; REBIRTH-AG “Hepatic Cell Therapy – Patient Liver Stem Cells”, Hannover, Germany; 2Hannover Medical School (MHH), Clinic of General, Visceral and Transplantation Surgery, MHH, Hannover, Germany; 3Hannover Medical School (MHH), German Center for Infection Research (DZIF), TTU Hepatitis, Hannover, Germany Background and Aims: Basic and translational research on primary human hepatocytes is currently hindered by the limited availability of functional human hepatocytes. Moreover, once isolated from tissue samples, they rapidly loose their function and do not proliferate when cultured in vitro. This problem could be overcome by using human liver stem cells, propagated in vitro and subsequently differentiated into cells Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A43 A44 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen of the different liver cell types, ideally reaching full maturation comparable to native cells in vivo. Methods: Based on the culture of primary hepatocyte cell suspensions obtained from patient resectates, we established a specific tissue culture protocol for the generation and enrichment of adult liver stem cells from within these samples, finally leading to stably proliferating pure stem cell populations. Adult liver stem cell cultures and their differentiation potential were then characterized and compared to standard hepatoma cell lines (Huh7, HepG2, HepaRG) and freshly isolated primary human hepatocytes by immunofluorescence microscopy and RT-qPCR gene expression analyses employing an extensive panel of cellular markers. Results: High nucleus-to-cytoplasm ratio and sensitivity to the slightest modifications of culture conditions hint towards the differentiation potential of these cell populations. Cell characteristics are the presence of markers for EMT and for progenitor cells (TERT, EpCAM, A6 and PK M2). Even under maintenance conditions without any rematuration occuring, stable signatures of both the hepatocytic and cholangiocytic phenotypes (Albumin, TDO, CFTR and AE2, amongst others), and interestingly of liver sinusoidal endothelial cells (VEGFR2, ENG, CD 32b, etc), are detected by immunofluorescence and RT-qPCR. Furthermore, stable expression of a wide variety of receptors and/or ligands of the significant signalling pathways known to be involved in endodermal tissue development or liver regeneration also is a characteristic feature and points towards the cells flexible abilities to communicate via all these signalling pathways (Wnt, Notch, Hedgehog, and c-Met amongst others). Conclusions: A method was developed to generate adult liver stem cell populations from patient liver samples. Upon characterisation and comprehensive evaluation of the cells differentiation potential, a plethora of possible uses, ranging from basic research to clinical applications are within reach in the not-so-far future. Corresponding author: Gutierrez Jauregui, Rodrigo E-Mail: gutierrez.rodrigo@mh-hannover.de 4.23 Inactivation of Cyclin E1 acts pro-apoptotic and anti-proliferative in primary hepatoma cells and protects from hepatocarcinogenesis in mice Moro N7, Sonntag R1, Nevzorova YA1, Bangen JM1, Fahrenkamp D2, Lambertz D1, Hu W1, Gassler N3, M!llerNewen G2, Weiskirchen R4, Barbacid M5, Sicinski P6, Trautwein C1, Liedtke C1 1 RWTH University Hospital Aachen, Department of Internal Medicine III, Aachen, Germany; 2RWTH University Hospital Aachen, Institute of Biochemistry and Molecular Biology, Aachen, Germany; 3RWTH University Hospital Aachen, Institute of Pathology, Aachen, Germany; 4RWTH University Hospital Aachen, Institute of Molecular Pathobiochemisty, Experimental Gene Therapy and Clinical Chemistry, Aachen, Germany; 5Centro Nacional de Investigaciones Oncol(gicas (CNIO), Madrid, Spain; 6Dana-Farber Cancer Institute and Department of Genetics, Harvard Medical School, Department of Cancer Biology, Boston, MA, USA; 7University of Cologne, Department of Dermatology, Cologne, Germany Background & Aims: E-type cyclins (CcnE1, CcnE2) are regulatory subunits of Cyclin-dependent kinase 2 (Cdk2). There is evidence that CcnE/ Cdk2 complexes control the transition of quiescent cells into the cell cycle. Surprisingly, genetic deletion of CcnE1, CcnE2 or Cdk2 does not inhibit cell proliferation during embryonic development or liver regeneration. The aim of the present study was to evaluate if E-type cyclins or Cdk2 may have a specific role for hepatocarcinogenesis. Methods: We used genetically modified mice with constitutive deletion of Cyclin E1 (CcnE1-/-) or Cyclin E2 (CcnE2-/-) and conditional knockout mice with hepatocyte-specific inactivation of Cdk2 (Cdk2Dhepa), respectively. To induce hepatocellular carcinoma (HCC), mice were treated with a single dose of Diethylnitrosamine (DEN) at the age of two weeks and analysed for tumor initiation and progression after 24 and 40 weeks. For in vitro studies, we generated immortalized Cyclin E1-floxed hepatoma cells from DEN-treated CcnE1f/f mice. In these cells, acute CcnE1 deletion was performed and visualized by infection with a cre/EGFP expressing adenovirus. Results: Twenty-four weeks after DEN treatment 40 % of wildtyp (WT) and CcnE2-/- mice developed few small tumor nodules, whereas all CcnE1-deficient animals revealed normal liver morphology lacking visible tumor nodules. At the age of 40 weeks, 100 % of DENtreated WT and CcnE2-/- mice developed HCC with an average of 35 – 40 nodules per liver. In sharp contrast, HCC incidence in CcnE1-/- animals was only 50 %, and the overall number of tumor nodules was tenfold reduced in comparison to WT and CcnE2-/- mice. Interestingly, Cdk2Dhepa mice and Cdk2DhepaCcnE2-/- double mutants were also Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York strongly protected from DEN-mediated hepatocarcinogenesis suggesting that the oncogenic potential of CcnE1 is Cdk2-dependent. A similar antitumorigenic effect of CcnE1 ablation was observed in a second HCC model using mice with concomitant hepatic over-expression of the proto-oncogene c-myc indicating that the observed effects are model-independent. Finally, we isolated primary, CcnE1-floxed hepatoma cells from DEN-treated CcnE1f/f mice and inactivated CcnE1 in vitro using EGFPlabeled, cre-expressing adenoviruses. Confocal live cell imaging revealed that acute CcnE1 inhibition in transformed hepatoma cells effectively results in apoptosis within 72 hours. In addition, CcnE1-depleted hepatoma cells showed strong activation of caspase-3, and de-regulation of S-phase and cytokinesis related genes and proteins, respectively. Conclusion: Our data demonstrate that CcnE1-but not its homologue CcnE2, is essential for proliferation and survival of immortalized hepatoma cells in vivo and in vitro. This requirement of CcnE1 seems to be dependent on the availability of Cdk2. We hypothesize that hepatoma cells get addicted to high CcnE1 expression levels during the transformation process. Thus, acute inhibition of CcnE1 during HCC progression could be a novel therapeutic option. Corresponding author: Liedtke, Christian E-Mail: cliedtke@ukaachen.de 4.24 Increased serum levels of regenerative miRNAs in patients with spontaneous recovery from acute liver failure John K1, Hadem J1, Dooley S2, Manns M1, Thum T3, SchulzeOsthoff K4, Bantel H1 1 Hannover Medical School, Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany; 2 Medical Faculty Mannheim, Department of Medicine II, Mannheim, Germany; 3Hannover Medical School, Institute for Translational and Therapeutic Strategies, Hannover, Germany; 4University of T!bingen, Interfaculty Institute for Biochemistry, T!bingen, Germany Introduction: Acute liver failure (ALF) represents a life-threatening situation characterized by sudden and massive liver cell death in the absence of preexisting liver disease. Although most patients require liver transplantation to prevent mortality, some recover spontaneously and show complete liver regeneration. The molecular mechanisms of spontaneous recovery from ALF and the role of miRNAs are largely unknown. We therefore investigated miRNAs such as miR-21 and miR-221, which have been implicated to play a role in liver regeneration, in sera of ALF patients with or without spontaneous recovery. In addition, we analyzed growth-inhibitory target genes of those miRNAs as well as hepatocyte proliferation in liver tissues of spontaneously recovered and non-recovered ALF patients. Results: Patients with spontaneous recovery showed significantly higher serum levels of miR-21 and miR-221 compared to non-spontaneously recovered patients. As compared to non-recovered patients, liver tissue of spontaneous survivors revealed not only increased hepatocyte proliferation, but also a strong down-regulation of miRNA target genes that impair liver regeneration, including the cyclindependent kinase inhibitors p21, p27 and p57. Conclusion: Our data suggest that miR-21 and miR-221 are involved in liver regeneration and might contribute to spontaneous recovery from ALF. Corresponding author: Bantel, Heike E-Mail: Bantel.Heike@mh-hannover.de 4.25 Indirekte Wechselwirkungen zwischen HCC (Hep3B) und humanen mesenchymalen Stammzellen in vitro und in vivo Winkler S1, Schmidt L1, Leibiger K1, Hempel M1, Ditze M2, B"hmer F3, M!ller J3, Kaufmann R2, Christ B1 1 Universit$t Leipzig, Klinik und Poliklinik f!r Viszeral-, Transplantations-, Thorax- und Gef$ßchirurgie, Angewandte Molekulare Hepatologie, Leipzig, Deutschland; 2 Universit$t Jena, Klinik f!r Allgemein-, Viszeral- und Gef$ßchirurgie, Jena, Deutschland; 3Universit$t Jena, Institut f!r Molekulare Zellbiologie, Jena, Deutschland; 4 Universit$t Leipzig, Translationales Zentrum f!r Regenerative Medizin Leipzig (TRM Leipzig), Leipzig, Deutschland Hintergrund: Die Therapie der Wahl des hepatozellul"ren Karzinoms (HCC) ist meist die Leberresektion bzw. -transplantation. Mesenchymale Stammzellen (MSC) besitzen ein hohes regeneratives Potential, so dass 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen sie insbesondere nach Leberresektion bei der Behandlung des HCC unterst!tzend wirken k#nnten. Allerdings gibt es eine kontroverse Datenlage zur Tumorprogression durch MSC. Ein m#glicher Zusammenhang sollte hier untersucht werden. Methoden: Die humane Tumorzelllinie Hep3B und GFP-markierte MSC wurden in vitro in Mono-, Co- und Transwell-Kulturen bez!glich ihres Wachstums qualitativ und quantitativ mittels Durchflusszytometrie analysiert. In vivo wurden subkutane Tumore in der immundefizienten Pfp/Rag2-/- Maus durch einmalige Injektion von 1 x 107 Hep3B mit einer Wachstumszeit von 15 Tagen induziert. MSC wurden entweder co-injiziert (2,25 x 106) oder in ein- bzw. mehrmaliger Dosis nach 3, 8, oder 13 d (0,75 x 106/Injektion) i.v. systemisch gegeben. Ergebnisse: In den Co-Kulturen wuchsen Hep3B und MSC unabh"ngig voneinander und ohne Kontakt zueinander. Zwar wuchsen Hep3B nach 11 Tagen Kultur schneller als MSC, welche das Wachstum aber nicht stimulierten. In vivo stimulierten MSC nach CoInjektion mit Hep3B das Tumorwachstum signifikant (401,7 g € 148 vs. 118,9 g € 44). (hnliches Tumorwachstum wurde auch nach dreimaliger MSC-Injektion erreicht. Einmalige bzw. zweimalige MSC-Injektion an 3 d bzw. 3 d und 8 d f!hrte zur kleinen Tumoren (40,8 g € 28,3 und 42,9 g € 15,8). Eine einmalige Gabe von MSC nach 13 d f!hrte ebenfalls zur Stimulation des Tumorwachstums. Im Tumor konnten nur vereinzelt MSC nachgewiesen werden. Schlussfolgerung: In vitro gibt es keinen f#rdernden oder hemmenden Einfluss von MSC auf das Wachstumsverhalten der Hep3B. In vivo scheint es zeit- und dosisabh"ngig Wechselwirkungen zu geben. MSC tragen nicht direkt sondern vermutlich !ber parakrine Faktoren zur Stimulation des Tumorwachstums bei. Korrespondierender Autor: Winkler, Sandra E-Mail: sandra.pelz@medizin.uni-leipzig.de 4.26 Inducing active demethylation through 5-Azacytidine open a new aspect for treatment of Hepatocellular Carcinoma Sajadian SO1, Ehnert S1, Bachmann A1, Sipos B2, Nuessler AK1 1 Eberhard Karls University T!bingen, BG Trauma Center, Institute for Trauma Research, T!bingen, Germany; 2 University Hospital T!bingen, Institute of Pathology and Neuropathology, T!bingen, Germany Background: Hepatocellular carcinoma (HCC) is the fifth deadliest cancer worldwide. Global deregulation of the methylation status is one of the main causes of HCC. The oxidation of 5-methylcytosine (5mC) triggers the formation of 5-hydroxymethylcytosine (5hmC). 5hmC can be depleted from the genome through down-regulation of the TET proteins leading to the demethylation of previously silenced genes. It has been reported that the anti-cancer drug 5-Azacytidine (5-Aza) mediates the activation of tumor suppressor genes through passive demethylation by inhibiting DNMT1. Our aim was to ascertain, if 5-Aza also induces an active demethylation by increasing the expression of 5hmC mediated by the proteins TET2 and TET3, which may lead to new approaches in cancer therapy. Methods and Results: The expression of 5mC and 5hmC in primary human hepatocytes (hHeps), HCC cells (Huh-7, HLE, HLF) and tissue sections from healthy and HCC patient cohorts (55 patients) was studied by immunofluorescence (IF) staining and immunohistochemistry: The expression of 5hmC was lower in HCC tissue than in healthy tissue samples. This finding was confirmed by comparing HCC cells to hHeps. The expression of TET2 and TET3 was lower in HCC tissues and cell lines than in non-tumor liver tissues and hHeps. In order to evaluate, if the expressions of TETs and 5hmC are inducible by 5-Aza, HCC cell lines were treated with different concentrations of 5-Aza (0 – 20 mM). Even at the highest concentration, no LDH release and toxic effect were registered after 48 hours of incubation. Interestingly, the expressions of TETs and of 5hmC-5mC were increased, while the proliferation marker PCNA indicated an inhibition of cell proliferation. Conclusion: Our data exhibit a decrease of 5hmC and an increase of 5mC in HCCs through down-regulation of the TETs. However, the expression levels of 5hmC and the TETs can be re-induced by 5-Aza through active demethylation, which is a novel function of the drug. We suggest that the loss of 5-hmC expression is an additional marker for hepatocellular carcinoma diagnosis. This would open up new avenues in the therapy of HCC. Corresponding author: Nuessler, Andreas K E-Mail: andreas.nuessler@med.uni-tuebingen.de 4.27 Inhibition of canonical IKK/NF-kB signaling in Hepatitis B Virus surface antigen transgenic mice drastically increases HCC development due to dysregulated Unfolded Protein Response control Sunami Y1,2, Ringelhan M3,4,5, Lu M1, H!ser N1, Kokai E2, Leith$user F6, Kleeff J1, Gul S2, Wissel S2, Hartmann D1, Schmid RM5, Friess H1, Brunner C2, Riedl P7, Schirmbeck R7, Strnad P8, Heikenw$lder M3,4, Wirth T2 1 Klinikum rechts der Isar, Technische Universit$t M!nchen, Surgical Clinic and Polyclinic, Munich, Germany; 2University of Ulm, Institute of Physiological Chemistry, Ulm, Germany; 3 Technische Universit$t M!nchen, Institute of Virology, Munich, Germany; 4Helmholtz Zentrum M!nchen, Institute of Virology, Munich, Germany; 5Klinikum rechts der Isar, Technische Universit$t M!nchen, II. Medical Clinic and Polyclinic, Munich, Germany; 6University Hospital of Ulm, Institute of Pathology, Ulm, Germany; 7University Hospital of Ulm, Internal Medicine I, Ulm, Germany; 8University Hospital of Aachen, Medical Clinic III and IZKF, Aachen, Germany Background and Aims: Hepatitis B Virus (HBV) remains the most common risk factor for hepatocellular carcinoma (HCC). It has been suggested that, in addition to chronic inflammation, HBV viral products directly contribute in HBV-driven hepatocellular carcinogenesis. In patients with low HBV replication, it is proposed that accumulation of HBV surface antigen (HBsAg) in the endoplasmic reticulum (ER) of hepatocytes (referred to as “ground glass hepatocytes”) activates ER stress, directly driving carcinogenesis. In the ER stress response, NF-kB is known to be important for the control of the Unfolded Protein Response (UPR). The role of NF-kB signaling in HCC development has been reported to be on the one hand anti-tumorigenic, due to activation of critical survival signals in hepatocytes. On the other hand, NF-kB has also been identified as a tumor promoter due to its pro-inflammatory function. In this study, we investigate the role of hepatic NF-kB signaling in directly HBV-driven HCC development using mice overexpressing hepatitis B virus surface antigen (HBsAg). Methods: HBsAg transgenic mice were crossed with animals expressing a dominant-negative mutant of IKK2 (an upstream kinase in canonical NF-kB signaling) under the control of tetracycline-inducible LAP-promoter to achieve inhibition of hepatocellular canonical NF-kB signaling. Results: The incidence of HBsAg-driven hepatocellular carcinogenesis was dramatically increased at the age of 18 months, when canonical NF-kB signaling was inhibited. However, there was no significant change in inflammatory response such as T-lymphocyte or macrophage infiltration. In addition, MyD88 deficiency did not inhibit HBsAg-induced tumor development in mice. Our data suggest that the role of canonical NF-kB signaling in this model does not rely on changes in the inflammatory response, but disrupts UPR control in HBsAg-driven hepatocellular carcinogenesis. Consistently, in HBsAg mice, a critical UPR regulator BiP/GRP78 was not upregulated when canonical NF-kB system was blocked. Furthermore, ER stress-associated cell death factor CHOP was strongly expressed, pointing to a failure of UPR control. In addition, a massive oval cell reaction (ductular reaction) was induced in HBsAg transgenic mice upon inhibition of canonical NF-kB signaling, indicating extensive liver damage and lost capacity of hepatocytes to contribute to compensatory proliferation. Conclusion: The role of canonical NF-kB signaling in hepatocellular carcinogenesis depends on the mode of liver damage. In the case of an HBsAgdriven HCC model simulating a direct carcinogenic effect of HBV, NF-kB plays a critical role in controlling the ER stress response. This implies an indispensable role for NF-kB in the control of the UPR and an antitumorigenic role in ER stress-related hepatocarcinogenesis. Corresponding author: Sunami, Yoshiaki E-Mail: yoshiaki.sunami@tum.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A45 A46 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 4.28 Integration of exome sequencing and in vivo RNAi screening identifies new cancer genes in hepatocellular carcinoma Neumann O1, W!stefeld T2, Pellegrino R1, Geffers R3, Schirmacher P1, Zender L1, Longerich T1 1 University of Heidelberg, Institute of Pathology, Heidelberg, Germany; 2University of T!bingen, Department of internal medicine I, T!bingen, Germany; 3Helmholtz Center for Infection Research, Genome Analytics, Braunschweig, Germany The recent improvements in the field of sequencing technologies facilitated profiling of whole (tumor) genomes, while in vivo RNAi screening allows for the detection and validation of new cancer genes in an unbiased fashion. Here we combined whole exomic next generation sequencing (NGS) of a single case of human hepatocellular carcinoma with in vivo RNAi screening to identify new protumorigenic driver genes of hepatocarcinogenesis. The selected case was characterized by a highly differentiated hepatocellular carcinoma (HCC) that manifested as a nodule in a premalignant Dysplastic Nodule (DN) in a cirrhotic patient. We used Illumina’s HiSeq platform to identify genetic variations in gallbladder, cirrhotic liver, DN, and HCC. After normalization against gallbladder tissue we identified 59.723 sequence variations in cirrhotic liver tissue, 59.706 in DN, and 61.652 in the HCC compartment of the nodules. Using the “AnnoVar tool” we identified clonally expanded sequence variations that were predicted to be damaging (Polyphen-2). This algorithm revealed eleven mutations that were present both in the DN and the HCC nodules, while six more alterations were exclusively found in the HCC component. All 17 mutations could be validated by Sanger sequencing. To identify the protumorigenic driver genes among these candidates we compiled a focused shRNA library consisting of 3 independent shRNAs against each gene. We took advantage of a recently described transposon-based delivery system to stably express individual shRNAs in murine hepatocytes after hydrodynamic tail vein injection of the focused library and the transposase vector into p19-/- mice. Mice were monitored for liver tumor development and DNA was isolated form 30 individual tumor nodules. The shRNA(s) that were enriched in each tumor nodule were determined using NGS. These analyses revealed four potential protumorigenic drivers, which are currently validated using a single gene knockdown. In summary, the integration of the NGS technology and in vivo RNAi screening allows for the identification of new protumorigenic drivers of hepatocarcinogenesis in a time-efficient manner. In addition, our integrative analysis is a proof-of-concept for a personalized oncological approach. Corresponding author: Neumann, Olaf E-Mail: olaf.neumann@med.uni-heidelberg.de 4.29 Kombinationstherapie mit dem spezifischen Foxp3-Inhibitor P60 und einer Vakzinierung mit AdmAFP-transduzierten dendritischen Zellen im subkutanen und orthotopen murinen HCC-Tumormodell Waysczak J1, Vogt A1, Schmidt-Wolf I2, Strassburg CP1, Gonzalez-Carmona MA1 1 Universit$tsklinikum Bonn, Medizinische Klinik und Poliklinik I, Bonn, Deutschland; 2Universit$tsklinikum Bonn, Zentrum f!r integrierte Onkologie (CIO), Bonn, Deutschland Einleitung: Immuntherapeutische Ans"tze mit dendritischen Zellen (DC) sind eine aussichtsreiche Strategie zur Behandlung des hepatozellul"ren Karzinoms (HCC). In Vorarbeiten konnten wir mit alpha-Fetoprotein(AFP)-beladenen DC eine spezifische T-Zell-vermittelte Immunantwort gegen AFP-positive HCC-Zellen induzieren. Ziel ist es, diese AFPspezifischen Immunantwort durch eine zus"tzliche spezifische Funktionshemmung regulatorischer T-Zellen (Treg) durch den Foxp3-Inhibitor P60 zu optimieren. Methodik: Die verwendeten adenoviralen Vektoren wurden nach dem AdenoEasy-System hergestellt. DC wurden aus dem Knochenmark von C 3 H-M"usen gewonnen und an Tag 6 mit AdmAFP bzw. AdMock transduziert. Zur Tumorinduktion wurden C 3 H-M"usen subkutan in die rechte Flanke oder orthotop in den linken Leberlappen 106 bzw. 105 mAFP-positive Hepa129-Zellen injiziert. An Tag 9 und 15 nach subkutan. bzw. an Tag 3 und 6 nach orthotoper Tumorinduktion wurden je 106 transduzierte DC subkutan injiziert. Ab dem Tag der ersten DC-Vakzinierung wurden t"glich 50 bzw. 100 mg P60 intraperitoneal injiziert. Das Tumorwachstum wurde durch Messungen mit einer Schieblehre bzw. Wiegen der Tiere kontrolliert. Die M"use wurden geopfert, wenn das Tumorvolumen 1500 – 2000 mm3 erreichte Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York bzw. ein klinisch relevanter Aszites auftrat. Ergebnisse: Sowohl im subkutanen als auch im orthotopen HCC-Modell zeigte eine Monotherapie mit P60 keinen antitumoralen Effekt im Vergleich zu den Kontroll-behandelten M"use (p > 0.05). Allerdings f!hrte die spezifische Hemmung der Treg mit P60 in Kombination mit der Vakzinierung mit AdmAFPtransduzierten DC zu einem signifikant verl"ngerten &berleben gegen!ber der nicht therapierten Kontrollgruppe sowohl im subkutanen als auch im orthotopen Tumormodell. Interessanterweise war der synergistische antitumorale Effekt im orthotopen Tumormodell st"rker ausgepr"gt (p = 0,0056). Diskussion: Schlussfolgernd zeigen unsere Daten, dass eine alleinige funktionelle Inhibition der Treg mit dem spezifischen Foxp3-Inhibitor, P60, keinen Effekt auf das Tumorwachstum von HCC in vivo hat. &berraschenderweise f!hrt P60 dagegen in Kombination mit einer Vakzinierung mit AdmAFP-transduzierten DC zu einem signifikanten zum Teil synergistischen antitumoralen Effekt bei M"usen mit subkutanen oder orthotopen HCC. Diese Resultate lassen das Potential von P60 zur Verbesserung einer DC-basierten Immuntherapie des HCC erahnen und werden derzeit im Hinblick auf die immunologische Grundlage hin untersucht. Korrespondierender Autor: Vogt, Annabelle E-Mail: Annabelle.Vogt@ukb.uni-bonn.de 4.30 Lack of gp130 expression in hepatocytes attenuates tumor progression in the DEN model Cubero FJ1, Hatting M1, Spannbauer M1, Peng J1, Hu W1, Al Masaoudi M1, Sellge G1, Gassler N2, Liedtke C1, Trautwein C1 1 RWTH University Hospital Aachen, Medical Clinic IIII, Aachen, Germany; 2RWTH University Hospital Aachen, Institute of Pathology, Aachen, Germany Background & Aim: Chronic liver inflammation is a crucial event in the development and growth of hepatocellular carcinoma (HCC). Compelling evidence has shown that IL-6 /gp130-dependent signaling plays a fundamental role in liver carcinogenesis. Thus, in the present study we aimed to investigate the role of gp130 in hepatocytes for the initiation and progression of HCC. Methods: Hepatocyte-specific gp130 knockout mice (gp130Dhepa) and control animals (gp130f/f) were treated with diethylnitrosamine (DEN). The role of gp130 for acute injury (0 – 5 days), tumor initiation (24 weeks) and progression (40 weeks) was analyzed. Results: After acute DEN-induced liver injury we observed a reduction in the inflammatory response as reflected by decreased IL-6 and oncostatin M (OSM) levels in gp130Dhepa animals. Loss of gp130 slightly attenuated the initiation of HCC 24 weeks after DEN-induced tumor initiation. In contrast, 40 weeks after DEN treatment, gp130Dhepa livers displayed smaller tumors and reduced tumor burden, indicating a role for hepatocyte-specific gp130 expression during HCC progression. We found increased oxidative stress and substantial DNA damage in animals after DEN injection, but no significant difference between gp130f/f and gp130Dhepa animals. However, while STAT3 phosphorylation was absent in gp130Dhepa hepatocytes we found STAT5 activation and decreased TGFb-dependent activity in these livers. Conclusion: Our results indicate that gp130 deletion in hepatocytes reduces progression, but not HCC initiation in the DEN model. Gp130 deletion resulted in STAT3 inhibition but increased STAT5 activation and diminished TGFb-dependent signaling. Hence, blocking gp130 in hepatocytes is an interesting therapeutic target to inhibit the growth of HCC. Corresponding author: Cubero, Francisco Javier E-Mail: fcubero@ukaachen.de 4.31 Loss of cell polarity defines a cancer-prone phenotype in liver epithelial cells Wan S1, Meyer AS1, Weiler S1, Lutz T1, R"ssler S1, Rupp C2, Schirmacher P1, Pinna F1, Breuhahn K1 1 University of Heidelberg, University Hospital, Institute of Pathology, Heidelberg, Germany; 2University of Heidelberg, University Hospital, Department of Gastroenterology, Heidelberg, Germany Background/Aims: Loss of cell polarity has been shown to play an essential role in the cause and progression of carcinogenesis in cells of epithelial origin. Three polarity protein systems (PPS) are involved in the acquisition and maintenance of cell polarity: the apical Crumbs complex(Crumbs, Pals1,PatJ), the subapical Par complex(Par6, Par3,aPKC), and the basolateral Scribble complex(Lgl1 / 2, Dlg1, Scribble). It is now well accepted that the Hippo pathway and its transcriptional co-activa- 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen tors yes-associated protein (YAP)/TAZ (WWTR1) are well connected to PPS via partly unknown mechanisms. In this project we aim to define the crosstalk between PPS complexes formation and activity of the Hippo/YAP pathway. Methods: We compared immunofluorescence stains of cell junction markers such as tight junction (ZO1) and adherens junction (E-cadherin) in primary hepatocytes and HCC cells with a high (HepG2) and low (HLE, HLF) degree of cell polarity in 2D monolayer cultures and 3D collagen sandwich cultures. The expression and localization of characteristic PPS markers (Scribble, CRB3) were compared. We also analyzed the activity (phosphorylation and localization) of Hippo pathway constituents (YAP/TAZ) and compared their expression with PPS deregulation and mislocalization. Moreover, we analyzed the expression of selected factors (e.g., scribble) in primary human HCC samples. Results: Polarized HCC cells show a clear membrane localization of the wellknown markers for polarity (ZO1, E-Cadherin) and also Scribble and CRB3, whereas in non-polarized HCC cells, these markers are mislocalized in the cytoplasm. In addition, a significant nuclear localization of YAP and TAZ was detectable in non-polarized cells, whereas the nuclear enrichment of YAP/TAZ is lower in polarized HCC cells. YAP nuclear enrichment can be inhibited by cell-cell contact in non-malignantly transformed epithelial cells but not in HCC cells. Surprisingly, high expression of Scribble significantly correlates with poor survival of HCC patients. In contrast, disruption of polarity in polarized HCC cells after silencing of Scribble using gene-specific siRNAs stimulated a significant nuclear translocation of YAP, dephosphorylation of AKT, and induction of a mesenchymal phenotype. Conclusion/Outlook: We demonstrate that the loss of cell polarity correlates with activation of the transcriptional co-activators of the Hippo pathway in HCC cells. First data indicate that the basolateral PPS protein Scribble is an important regulator for YAP/TAZ localization and that the loss of Scribble drives oncogenic YAP/TAZ activity. Because Scribble is highly expressed in human HCCs, we hypothesize that differential subcellular localization of Scribble may affect different signaling pathways: while membranous Scribble may bind and inhibit YAP, cytoplasmic Scribble might promote the PI3K/ AKT pathway. Corresponding author: Wan, Shan E-Mail: Shan.Wan@med.uni-heidelberg.de 4.32 Metastasis development in a novel mouse model of advanced liver cancer Lechler C1, Hubner EK1, Kohnke-Ertel B1, Sage J2, Schmid RM1, Ehmer U1 1 Klinikum rechts der Isar, Technische Universit$t M!nchen, II. Medical Clinic and Polyclinic, Munich, Germany; 2 Stanford University, Department of Pediatrics and Genetics, Stanford, CA, USA Introduction: Liver cancer is one of the leading causes of cancer related mortality worldwide. It is often diagnosed in advanced stages when treatment options remain limited. Novel diagnostic markers and therapies are therefore urgently needed. The absence of reliable mouse models has been a major limitation in the study of advanced, metastatic liver cancer in the past. Here, we present a novel genetically engineered mouse model of primary liver cancer. In this model, activation of oncogenic Kras together with functional inactivation of the tumor suppressor proteins RB and p53 mimics molecular events that occur in the majority of human liver cancer and leads to rapid formation of hepatic tumors with extrahepatic metastases. Methods: Adult Rblox/lox;p53lox/lox;KrasLSL-G12D/+ mice were injected intravenously with a liver specific AAV-Cre. Upon liver tumor formation individual lesions were microdissected and tissue was analyzed for RNA and protein expression. Microarray analysis was performed on an Affymetrix platform (Mouse Genome 430 2.0 Array) and mRNA expression was validated using qPCR. Protein expression was visualized by immunohistochemistry and SDS page gel electrophoresis. Results: The RPK mouse model combines liver specific inactivation of RB and p53 with activation of Ras signaling. After gene recombination, RPK mice rapidly develop hepatic tumors within 3 to 4 months. Cancer lesions in this mouse model express hepatocytic (AFP+ and/or ALB+) as well as biliary (CK19+) differentiation markers. Comparison of gene expression microarrays from RPK tumors with data from human liver cancer samples confirmed clustering with human undifferentiated hepatocellular carcinomas and cholangiocarcinoma. Strikingly, selective targeting of hepatocytes in RPK mice showed that liver tumors of mixed or even biliary differentiation arise from mature hepatocytes. Analysis for activation of oncogenic pathways revealed activated ERK and AKT signaling downstream of Kras in RPK liver tumors. Additionally, numerous genes related to metastasis development were highly expressed in RPK cancer lesions. In line with these findings we detected extrahepatic metastases in the majority of mice with advanced tumor lesions. Summary: The RPK mouse model presents a novel platform to study key molecular mechanisms in liver tumor initiation and development. Importantly, the highly consistent occurrence of metastatic lesion allows for the investigation of molecular drivers of metastasis development in liver cancer. Preliminary data from our mouse model indicate for an important role of Ras signaling in the metastatic process. The underlying molecular mechanisms are currently under investigation. The RPK model will help to answer important question in tumor biology of hepatic malignancies and aims to identify novel therapeutic targets for the treatment of human liver cancer. Corresponding author: Ehmer, Ursula E-Mail: ursula.ehmer@tum.de 4.33 Methylome screen identifies epigenetically deregulated microRNAs in cholangiocarcinoma Goeppert B1, Ernst C2, Baer C2, Mehrabi A3, Hafezi M3, Renner M1, Warth A1, Stenzinger A1, Weichert W1, Schirmacher P1, Plass C2, Weichenhan D2 1 Heidelberg University Hospital, Institute of Pathology, Heidelberg, Germany; 2German Cancer Research Center (DKFZ), Division of Epigenomics and Cancer Risk Factors, Heidelberg, Germany; 3Heidelberg University Hospital, Department of General, Visceral, and Transplantation Surgery, Heidelberg, Germany Background & Aims: The molecular mechanisms, in particular epigenetic alterations, underlying the genesis of cholangiocarcinomas (CC) are poorly understood. We have previously shown data of global methylation changes in CC. Here, we focus on specific microRNAs (miRNAs) that showed drastic methylation alterations in our methylome screen. Methods: Data of a previously presented genome-wide analysis that identified differentially methylated regions (DMRs) in 18 human CCs were used. Candidate miRNAs were selected by a previously described in silico analysis and technically confirmed by quantitative MassARRAY! analysis. MiRNA expression was examined in formalin-fixed-paraffinembedded material of tumor specimen (n= 20) and normal biliary epithelium (n= 20) and functional experiments were performed in vitro using two CC cell lines (TFK-1 and EGI-1). Results: In silico analysis of global methylation data in CC identified large numbers of CC-related hypermethylated and hypomethylated miRNA promoters which were exemplarily confirmed in a second patient cohort. Inverse correlation between promoter methylation and expression suggests miR-129 – 2 and members of the miR-200 family, miR-200a, miR-200b and miR429, as novel tumor suppressors and oncomiRs in CC, respectively. Reporter assays revealed the tumor suppressive genes DLC 1 (deleted in liver cancer 1), FBXW7 (F-box/WD-repeat-containing protein 7) and CDH6 (cadherin-6) as presumed targets in CC. Conclusions: Data of the genome-wide methylation landscape of CC revealed specific changes in the methylation pattern of miRNAs. Herein, we could present specific miRNAs as putative novel tumor suppressors and oncomiRs in CC. Furthermore we offer a valuable repository enabling to study the role of epigenetically altered miRNAs in the onset and progression of CC. Corresponding author: Goeppert, Benjamin E-Mail: benjamin.goeppert@med.uni-heidelberg.de 4.34 Mouse models of colorectal and mammary cancer liver metastases and microenvironmental interplay with tumor-associated macrophages (TAMs) Bocuk D1, Krause P1, Niebert S1, Pukrop T2, Beissbarth T3, Ghadimi M1, Koenig S1 1 University Medical Center, Goettingen, Department of General, Visceral, and Pediatric Surgery, Goettingen, Germany; 2University Medical Center, Goettingen, Department of Hematology and Oncology, Goettingen, Germany; 3University Medical Center, Goettingen, Department of Medical Statistics, Goettingen, Germany Introduction: Colorectal cancer (CRC) and breast cancer (BC) rank as two of the most common tumors in developed countries. Given the relatively frequent formation of liver metastases, investigation of the hepatic microenvironment is crucial. Here we present two new immunocompetent mouse models of liver metastases and the microenvironmental interplay of tumor cells with TAMs. Methods: The cancer cell Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A47 A48 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen lines 410.4 (mammary gland) and CMT-93 (colorectal) were implanted locally into the liver or via the portal vein of syngeneic mice to monitor the time-dependent progression into metastases. Immunostaining demonstrated the growth pattern of metastases and the heterogeneity of TAMs in different tumor compartments. Results: Local implantation of tumor cells resulted in circumscribed tumor masses while the intraportal implantation induced diffuse hepatic infiltration. CRC-derived metastases demonstrated differentiated (glandular: CD 49f, beta-catenin) as well as undifferentiated areas (mesenchymal: vimentin and CD44), whereas BC metastases were mostly undifferentiated. Both tumor entities exhibited a tumor/liver interface marked by an increased density of inflammatory cells. M1 macrophages (tumoricidal activity) were mostly located within the liver metastases (CD 11b+) as well as in the hepatic microenvironment (F4 / 80+ and CD 68+). M2 macrophages (propagation of tumor progression) were mainly detectable in the hepatic microenvironment (CD 163+). Conclusion: The presented animal models allow the investigation of the interaction of liver metastases with TAMs. In further studies, we will use these mouse models and compare the growth patterns and association of TAMs following genetic modification of the cancer cell lines with respect to the Wnt and EGFR signaling pathways. Funded by the German Federal Ministry of Education and Research (Bundesministerium f!r Bildung und Forschung, BMBF) e:Bio project MetastaSys Corresponding author: Bocuk, Derya E-Mail: derya.bocuk@med.uni-goettingen.de 4.35 Novel tumor suppressor genes SORBS3 and SH2D 4A repress IL-6 signaling in hepatocellular carcinoma Pl"ger C1, Fraas A1, Schirmacher P1, R"ssler S1 1 Heidelberg University Hospital, Institute of Pathology, Heidelberg, Germany Background: Different inflammatory states, e.g. chronic hepatitis B or C viral infection, have been shown to contribute to the development of hepatocellular carcinoma (HCC). In patients with chronic liver disease the serum levels of interleukin 6 (IL-6) are elevated and increase even more when HCC develops. However, there is still not much known about the regulation of IL-6 signaling during hepatocarcinogenesis. Recently, we applied an integrative genomic and transcriptomic approach which revealed that loss of chromosome 8 p is associated with poor prognosis. In addition, we showed that the two chromosome 8 p genes SORBS3 and SH2D 4A are functional tumor suppressor genes in vitro and in vivo. The goal of this study is to dissect the molecular mechanisms of SORBS3 and SH2D 4A mediated tumor suppression. Methods: Gene expression analysis was performed to identify chromosome 8 p associated signaling pathways. Furthermore, Tetracycline-inducible SORBS3 or SH2D 4A expressing HCC cell lines were generated to identify potential binding partners by mass spectrometry, co-immunoprecipitation and Western blotting. The expression of target genes was measured by quantitative real time PCR. To examine whether SORBS3 and SH2D 4A are able to suppress IL-6 induced STAT3 transcriptional activity, STAT3 phosphorylation status was measured and STAT3 luciferase reporter assay were performed. Results: We found that SORBS3 and SH2D 4A function in a convergent manner to inhibit IL-6 signaling. Overexpression of SORBS3 and SH2D 4A leads to a decrease of IL-6 target genes Bcl-2, SPINK1 and Bcl-xL and consistently, knockdown to an increase. In addition, loss of SORBS3 mediates a decrease in SH2D 4A suggesting an amplifying mechanism. Luciferase assays revealed that both, SH2D 4A and SORBS3 inhibit STAT3 transcriptional activity possibly via blocking the phosphorylation of Y705 but not S727. A direct interaction could be observed between STAT3 and SORBS 3. Conclusion: Thus, the chromosome 8 p tumor suppressor genes SORBS3 and SH2D 4A are physically and functionally linked and provide a molecular mechanism of inhibition of STAT3-mediated IL-6 signaling in HCC. Corresponding author: R#ssler, Stephanie E-Mail: Stephanie.Roessler@med.uni-heidelberg.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York 4.36 Nuclear CYLD expression plays a role in HCC therapy response in vitro Elssner C1, Welte S1, Scherr AL1, Koehler BC1, SchulzeBergkamen H2 1 National Center for Tumor Diseases, Division of Medical Oncology, Heidelberg, Germany; 2Marien-Hospital Wesel, Gastroenterology, Wesel, Germany The deubiquitinase CYLD removes K63-linked ubiquitin chains from molecules involved, e.g., in NF-kB, Wnt/ß-catenin and BCL-3 signaling pathways. CYLD is dysregulated in different cancers, including hepatocellular carcinoma (HCC). Loss of CYLD is characterized by enhanced NFkB-signaling and increased cell survival. In previous studies, we demonstrated decreased levels of CYLD expression in human HCC. In recent analysis of CYLD expression in tissue microarrays, survival analysis of HCC patients after resection revealed a more favorable outcome of patients with positive nuclear CYLD expression. We hypothesize that reconstitution of CYLD is a promising approach for the treatment of liver diseases and the sensitization of HCC cells towards therapy-induced cell death. To assess the regulation of CYLD by different treatment strategies, HCC cell lines will be treated with chemotherapeutic agents and targeted agents. After treatment, CYLD expression levels including subcellular localization will be measured and cell death induction will be assessed by different analysis. Those targeted agents, which result in a decrease or no alteration of CYLD levels will be used for treatment of HCC cells, previously transfected with CYLD expression plasmids. Cell death induction will be assessed to test, whether CYLD upregulation sensitizes HCC cells to the respective targeted therapy. Another subproject intends to investigate the influence of CYLD on the migration and invasive potential of HCC cell lines in vitro. After CYLD downregulation, cells will be grown in 3D polystyrene scaffolds, which provide a suitable surrounding for long time cell growth. Scaffolds will be further processed for cryosectioning followed by immunostaining to investigate the expression levels of CYLD, Bcl-2 proteins and markers for EMT, migration and proliferation. The invasion depth will be assessed as well. Corresponding author: Elssner, Christin E-Mail: christin.elssner@nct-heidelberg.de 4.37 Nup155 is involved in the posttranscriptional regulation of p53 target genes in HCC Holzer K1, Ori A2, Winkler J1, Cooke A2, Eiteneuer EM1, Schirmacher P1, Beck M2, Singer S1 1 Heidelberg University Hospital, Institute of Pathology, Heidelberg, Germany; 2European Molecular Biology Laboratory, Heidelberg, Germany The nuclear pore complex (NPC) consists of different subunits (nuclear basket and ring, spoke and cytoplasmic rings and the cytoplasmic filaments) the components of which are 30 specialized proteins called the nucleoporins (Nups). The NPC is embedded in the nuclear envelope and represents the only transport gate between the cytoplasm and the nucleoplasm. Therefore, it obtains a central role with almost all oncogenic and tumorsuppressive signal transduction cascades passing through it. An increasing body of evidence suggests that in addition to their role in transport some Nups can also modulate cancer-relevant pathways on different levels (e.g. transport of transcriptions factors or the export/ stability of gene products). In this context we could recently show that Nup98 stabilizes the mRNA of a subset of p53 target genes such as CDKN1A/p21 and thereby shapes the p53-response. A previously performed RNAi screen suggested that also other Nups are linked to the p53 pathway. In HepG2 cells (p53 wild-type) we investigated the impact of Nup155 knockdown on p53 target gene induction upon drug treatment by using quantitative mass spectrometry (qMS). The depletion of Nup155 resulted in a significantly reduced p21 protein accumulation while the induction of other p53 targets such as bax and 14 – 3-3 sigma remained unaffected. A selective impact of Nup155 knockdown on p21 induction was also observed in Hep3B-4Bv cells and in a cell line expressing p21 from a tet-sensitive cDNA construct (“tet off”) by westernblot analysis. Interestingly, p21 mRNA levels were not significantly affected in the aforementioned cell lines. In addition, cycloheximide chase experiments did not point towards a role of Nup155 in p21 protein stability neither was the p21 mRNA transport affected by Nup155 depletion (tested by subcellular fractionationation followed by qRT-PCR). We hypothesized that Nup155 may play a role in p21 mRNA translation and performed polysome fractionation experiments. The resulting data, indeed, indicate an increased subpolysome/polysome p21 mRNA-ratio in the absence of Nup155. We are currently testing proteins involved in 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen mRNA translation and altered in the above mentioned qMS data set that may mediate the observed effect. We conclude that Nup155 regulates p21 on a post-transcriptional level. The underlying regulatory mechanism most likely involves mRNA translation and may represent a novel aspect in p53 target gene regulation by NPC components. Since p21 is a key mediator of several p53 responses such as cell cycle arrest and senescence it will also be of considerable interest to investigate how Nup155-dependent p21 regulation affects these outcomes. References: [1] Singer, S., Zhao, R. et al. Mol Cell (2012) Corresponding author: Holzer, Kerstin E-Mail: Kerstin.Holzer@med.uni-heidelberg.de 4.38 OPI ist zur Vorhersage der Mortalit!t und Morbidit!t nach Lebertransplantation geeigneter als BAR, MELD, D-MELD und DRI B$uerlein FJB1, Guba M2, Frey L3, Andrassy J2, Angele M2, Denk G1, Gr!ner N1, Kaspar M3, Pratschke S2, Rentsch M2, Stangl M2, Vogeser M4, Gerbes AL1, Zachoval R1 1 Ludwig-Maximilians Universit$t, II. Medical Clinic, Munich, Germany; 2Ludwig-Maximilians Universit$t, Surgical Clinic, Munich, Germany; 3Ludwig-Maximilians Universit$t, Anesthesiology, Munich, Germany; 4Ludwig-Maximilians Universit$t, Institute of Laboratory Medicine, Munich, Germany Einleitung: Die Allokation bei Lebertransplantation (LTx) in der UNOS und EUROTRANSPLANT Region basiert auf dem Model for End-Stage Liver Disease (MELD) Score. Der MELD-Score wurde entwickelt, um die 3-Monats-Mortalit"t auf der Warteliste vorherzusagen – scheint jedoch suboptimal zur Vorhersage des &berlebens nach LTx. Der Wert anderer Scores: Donor-Risk-Index (DRI), Organ-Patient-Index (OPI) und der Balance-Of-Risk (BAR) Score – zur besseren Pr"diktion des Outcomes muss noch evaluiert werden. Methoden: Wir analysierten 533 Lebertransplantationen (einschließlich 73 Retransplantationen und 82 high-urgency Transplantationen) an unserem Zentrum von 01/ 1997 bis 12/ 2011 und verglichen die F"higkeit, die post-LTx Mortalit"t und Morbidit"t zwischen BAR-, MELD-, D-MELD-, DRI- und OPI-Score vorherzusagen. Die Morbidit"t wurde gemessen an der L"nge des ICU-Aufenthaltes und am gesamten Krankenhausaufenthalt in den ersten 12 Monaten nach LTx. Ergebnisse: 67% m"nnlich, mittleres Alter bei LTx 50 Jahre (15 – 67), Indikation zur LTx Alkohol 25%, HCV 18%, HCC 12%, akutes Leberversagen 11%, cholestatische Lebererkrankungen 11%, HBV 7%, Andere 14%. Mortalit"t: Alle Score-Cutoffs konnten das 1 J-Transplantat&berleben diskriminieren: BAR (< 16 /‡ 16) 76.1 % – 63.3% (p = 0.015), MELD (< 30 /‡ 30) 82.3 % – 73.5 % (p = 0.030), D-MELD (< 1600 /‡ 1600) 76.0 % – 61.7% (p = 0.004), DRI (< 1.4 / 1.4 – 1.6 /‡ 1.6) 84.4% – 75.0 % – 66.9 % (p< .001), OPI (< 2.0 / 2.0 – 2.5 /‡ 2.5) 86.5 % – 76.8 % – 64.4 % (p< .001). Der OPI konnte am Besten Patienten mit fr!hem Tod nach LTx identifizieren. Die F"higkeit, Patienten mit hohem Mortalit"tsrisiko zu identifizieren, schwindet w"hrend des 10 J-Followups f!r den MELD und BAR-Score, bleibt allerdings signifikant f!r den D-MELD (< 800 / 800 – 1600/‡ 1600) 60.8% – 44.4 % – 31.1% (p< .001), DRI (< 1.4/ 1.4 – 1.6 /‡ 1.6) 65.9% – 49.0 % – 38.2 % (p< .001) und OPI (< 2.0 /2.0 – 2.5 /‡ 2.5) 66.5 % – 50.3 % – 37.1% (p< .001). Morbidit"t: Kaplan Meier Analysen zeigten eine Korrelation zwischen dem Krankenhausaufenthalt auf ICU und der Score-H#he f!r den BAR, MELD, D-MELD und OPI (alle: p< .001), nicht aber f!r den DRI. Der mediane Aufenthalt auf ICU und die [AUROC f!r ICU> 21 d] waren: BAR(< 16 /‡ 16) 7 d – 15 d [.67], MELD(< 30 /‡ 30) 7 d – 12 d [.65], D-MELD(< 1600 /‡ 1600) 7 d – 12 d [.64], OPI(< 2.0 /‡ 2.0) 6 d -10 d [.64]. Der mediane Krankenhausaufenthalt in den ersten 12 Monaten nach LTx war nur mit dem OPI (< 2.0 /2.0 – 2.5 /‡ 2.5) 50 d – 67 d – 76 d (p< .001) signifikant assoziiert. Zusammenfassung: In einer Zeit des extremen Organmangels m!ssen zwei Aspekte der Leber-Allokation ber!cksichtigt werden – die Schwere der Erkrankung, wiedergespiegelt durch den MELD-Score und das Patienten-&berleben nach Transplantation, f!r welches ein idealer Score noch gefunden werden muss. Unsere Ergebnisse zeigen, dass der OPI am Besten die 12-Monats Morbidit"t vorhersagt und noch viel wichtiger das 1/ 10-Jahres &berleben. Korrespondierender Autor: B"uerlein, Felix JB E-Mail: Felix@Baeuerlein.com 4.39 p53 /telomerase-dependent oncolytic adenoviruses harboring a p53-dependent feed forward loop results in reduced viral liver burden Schirmer P1, G!rlevik E1, Saborowski M1, Manns MP1, Kubicka S1, K!hnel F1 1 Hannover Medical School, Clinic for Gastroenterology, Hepatology, and Endocrinology, Hannover, Germany Broad applicable vectors with highly selectivity and efficient lytic capabilities in tumors are essential for oncolytic virotherapy. Therefore, we developed selectively-replicating oncolytic viruses, which simultaneously target tumor cell-specific telomerase reexpression and p53transcriptional deficiency, two molecular alterations which play a fundamental role in carcinogenesis and can therefore be frequently found in human tumors including hepatocellular carcinoma. The generated oncolytic viruses contained a modified Gal4-binding hTert core promoter for the viral E1A locus to achieve telomerase-dependent replication. Additionally viruses were equipped with an additional p53-responsive expression cassette for the transcriptional repressor Gal4-KRAB to block E1A locus and thus viral replication in normal cells. To maintain p53selectivity in face of constant inactivation of p53 by residual levels of viral early gene products, expression of Gal4-KRAB was linked to exogenous p53 via a 2A motif resulting in a self-propelling p53-dependent feed forward loop for maintained or even amplified levels of Gal4-KRAB. According to this concept we constructed two double-controlled oncolytic viruses using either p53wt-driven feed forward loop (Ad-FF p53) or the C-terminally deleted variant p53D30, which showed an increased transactivation of the hTert core promotor, for a p53D30-driven feed forward loop (Ad-FF p53D30). As shown by p53 and Gal4 western blot analysis in cells with different p53 status we could demonstrate p53selective activation of the feed forward mechanism and significant repressor levels. Accordingly, these viruses showed efficient oncolytic and replicative properties in p53-dysfunctional cells but enhanced p53-selectivity in normal cells in vitro when compared to a control virus expressing GFP instead of exogenous p53. In vivo, we could demonstrate viral replication is completely inhibited in the liver of Ad-FF p53 and AdFF p53D30 infected mice due to the p53-feed forward loop. Infection in C 57BL/ 6 mice showed that Ad-FF p53 and Ad-FF p53D30 significantly triggered innate immune receptors in comparison to the GFP control suggesting that p53-loop containing viruses might be a promising tool to augment antitumoral immune response. In summary, Ad-FF p53 and Ad-FF p53D30 effectively regulate their own replication in response to p53-dependent onset of the feed forward loop in vitro and in vivo. We developed a promising strategy to enhance p53-selectivity with possible implications in immune stimulatory activity of these oncolytic viruses. Corresponding author: Schirmer, Paul E-Mail: Schirmer.Paul@mh-hannover.de 4.40 Primary hepatic malignant epitheloid Hemangioendothelioma represent a genetically homogenous tumor entity Mogler C1, Schlitter AM2, Endris V1, Penzel R1, Schirmacher P1, Pfarr N1 1 Ruprecht-Karls-Universit$t, Institute of Pathology, Heidelberg, Germany; 2Technische Universit$t M!nchen, Institute of Pathology, Munich, Germany Aims: Epitheloid Hemangioendothelioma (EHE) is a rare malignant vascular tumors of unknown etiology and molecular pathogenesis. It may arise at many different sites, but liver is among the more frequent manifestations. Course of the disease is highly variable and so far only limited therapeutic options are available such as resection and liver transplantation. Our aim is to molecularly characterize this tumor entity in order to find new potential therapeutical targets. Methods: EHEs were histologically classified by two expert liver pathologists and further characterized by immunohistology. Fifteen formaline fixed and paraffin embedded primary hepatic EHE were immunohistochemically stained for potential predictive markers (KIT, HER2, Estrogen- and Prrogesterone Receptors). To test for genetic alterations, four samples were Sanger sequenced for c-kit, epidermal growth factor receptor (EGFR) and braf. Eleven samples were analyzed by next generation sequencing using the Ion Personal Genome Machine System and the AmpliSeq Cancer Hotspot Panel v2 comprising 207 amplicons from frequently mutated genomic "hot spot" regions of 50 known human cancer genes. Results: All EHEs were negative for the markers tested by immunohistochemistry and wildtype for EGFR, c-kit and braf. Interestingly, all NGS-sequences EHEs showed genetic polymorphisms either in the p53 gene locus or in the Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A49 A50 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen KIT gene locus. One sample showed a mutation in the platelet derived growth factor receptor (PDGFR) alpha gene locus and one sample in the p53 gene locus. For all other tested genes wildtype sequences were found. Conclusion: Hepatic EHEs seem to represent a genetically homogenous group of malignant vascular tumors with only few mutations of potential therapeutical relevance. Corresponding author: Mogler, Carolin E-Mail: carolin.mogler@med.uni-heidelberg.de 4.41 Progranulin autoantibodies and genetic variation in patients with cholangiocarcinoma Zimmer V1, Thurner L2, Acalovschi M3, Pfreundschuh M2, Lammert F1 1 Saarland University Hospital, Department of Medicine II, Homburg, Germany; 2Saarland University Hospital, Department of Medicine I, Homburg, Germany; 3University Iuliu Hatieganu, Department of Medicine III, Cluj-Napoca, Romania Background: Recently, the novel growth factor and TNF signalling adaptor progranulin (PGRN) has been implicated in the inflammation-driven pathogenesis of cholangiocarcinoma (CCA).(1,2) Neutralizing PGRN autoantibodies have been described in autoimmune diseases, including inflammatory bowel disease (IBD).(3,4) Therefore, our aim now was to assess PGRN autoantibody incidence and potential effects of the common PGRN gene variant rs5848 (known to be associated with reduced PGRN serum concentrations) on susceptibility and PGRN autoantibody formation in a large European CCA population.(5) Patients & Methods: Overall, 221 individuals with CCA (males n= 131, age 66 € 11 years) originating from Germany (n= 164) and Romania (n= 57) and 295 CCA-free control individuals were genotyped. The common non-synonymous single nucleotide polymorphism (SNP) rs5846 was genotyped by PCRbased assays with 5’-nuclease and fluorescence detection (TaqMan). PGRN autoantibodies were determined by ELISA.(4) Results: rs5848 genotype frequencies in the control group were consistent with the Hardy-Weinberg equilibrium (HWE), with a call rate > 99% indicating robust genotyping. The association tests did not provide evidence for genetic CCA risk modulation by the PGRN variant (Odds ratio= 0.92; 95 % confidence interval= 0.71 – 1.19; P> 0.05). Seven of 61 patients (11.5%) tested positive for PGRN autoantibodies, with no significant sex differences (3/ 32 males, 4 /29 females). Considering rs5848 variation in the subgroup with available PGRN autoantibody status, no significant differences in allele and genotype distribution were observed. Conclusions: Our preliminary data indicate PGRN autoantibodies as a novel potential tumor antigen in a defined subset of CCA patients. Extension of the current study in larger sample sizes and delineation of potential implications in terms of CCA subtypes and prognostic relevance of PGRN autoimmunity is warranted. References: [1] Frampton et al. Gut 2012 [2] Frampton et al. Am J Physiol Gastrointest Liver Physiol 2012 [3] Thurner et al. J Autoimmun 2013 [4] Thurner et al. Dig Dis Sci 2014 [5] Hsiung et al. J Neurol Sci 2011 Corresponding author: Zimmer, Vincent E-Mail: vincent.zimmer@uks.eu 4.42 Quantitative Analyse der Tumor-Vaskularisation mittels Mikro-CT in ApoE/LDLR Doppel-Knockout M!usen unter Western-Di!t Roderfeld M1, Kampschulte M2, Churin Y1, Roeb E1 1 Justus-Liebig Universit$t Gießen, Gastroenterologie, Gießen, Germany; 2Justus-Liebig Universit$t Gießen, Radiologie, Gießen, Germany Einleitung: Die nicht-alkoholische Fettlebererkrankung (NAFLD) und die daraus entstehende Hepatitis (NASH) sind zunehmend verantwortlich f!r die Entwicklung chronischer Lebererkrankungen bei westlicher Lebensweise (1). Die als Atherosklerose-Modell etablierte ApoE1 /LDLR Doppelknockout Maus (AL-Maus) wurde unter zus"tzlicher Western Di"t als verl"ssliches NASH Modell etabliert. Das Ziel der vorliegenden Studie war die quantitative Erfassung der Tumor-Vaskularisation in ALM"usen unter Western-Di"t mittels Mikro-CT. Methoden: 10AL-M"use und 5 Wildtyp Kontrollm"use wurden 30 Wochen mit einer Cholesterinund Fett-reichen Di"t (Western Di"t) gef!ttert. In entstehenden Tumorenwurde die Vaskularisation per Mikro-CTquantitativ analysiert. Dazu wurden 55 kubische Volumina untersucht (36 Bereiche ausLebergewebe und 19 Bereiche aus Tumoren). Ergebnisse:In 30 % der AL M"use auf Western Di"t wurde histologisch und immunhistochemischdie Entste- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York hung vonTumoren mit HCC-Charakteristika beobachtet. Per quantitativem Mikro-CT-Imaging wurde ein geringeres vaskul"res Volumen im Tumor festgestellt (2,1% € 0,14 vs. 3,59 % € 0,27; p < 0,001). Dar!ber hinaus war das vaskul"re Volumen von Gef"ßen < 0,14 mm im Tumor signifikant erh#ht, w"hrend das vaskul"re Volumen gr#ßerer Gef"ße > 0,14 mm im Vergleich zum umliegenden Lebergewebe signifikant verringert war. Schlussfolgerung:Mikro CT bietet die M#glichkeit, die neoplastische Vaskularisation in Nagern zu visualisieren. Damit ist die M#glichkeit gegeben, Tumor-Gewebe von umgebendem Leber-Gewebe qualitativ zu unterscheiden. Mit Hilfe der 3D Miko CT ist durch die Analyse des vaskul"ren Volumens kleiner Gef"ße < 0,14 mm auch die quantitative Unterscheidung von benignem und von neoplastischem Gewebem#glich. References: [1] Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther 2011;34:274 – 285. Korrespondierender Autor: Roeb, Elke E-Mail: elke.roeb@innere.med.uni-giessen.de 4.43 Relevance of organic cation transporter OCT1 (SLC 22A1) in Diethylnitrosamine-initiated and Phenobarbital-promoted hepatocellular carcinoma in OCT3- knockout mice Knapstein J1, Fuchs P1, Daniel G1, Darstein F1, Marquardt J1, Sprinzl M1, Schattenberg J1, W"rns MA1, Lautem A2, HoppeLotichius M2, Lang H2, Galle PR1, Zimmermann T1 1 Johannes Gutenberg-University, 1st Department of Internal Medicine, Mainz, Germany; 2Johannes GutenbergUniversity, Department of Hepatoboliary and Transplantation Surgery, Mainz, Germany Background: Organic cation transporters (OCT) are responsible for the uptake and intracellular inactivation of a broad spectrum of endogenous substrates. OCTs became pharmaceutically interesting, because they are determinants of the cytotoxicity of platin derivates and the transport activity has been shown to correlate with the sensitivity of tumors towards tyrosine kinase inhibitors. Recent data have shown a down-regulation of OCT1 (SLC 22A1) and OCT3 (SLC 22A3) in human hepatocellular carcinoma (HCC) and human cholangiocarcinoma (CCC), associated with tumor progression and a worse patient survival. The OCT1 downregulation in HCC may affect the ability of sorafenib and platin derivates to reach active intracellular concentrations in these tumors. Methods: HCCs were induced in OCT3-knockout (OCT3-/-) and wildtype (WT) mice with Diethylnitrosamine (DEN) and Phenobarbital. Tumor characteristics were assembled after 10 months. Fibrosis and inflammation were quantified by Sirius Red staining and leukocyte infiltration (Hematoxylin and Eosin, H&E) respectively. Steatosis was measured by quantification of lipid stain (Oil Red O). For proliferation and apoptosis analysis, Ki67- and Caspase 3- staining were assessed immunohistochemically. SLC 22A1 mRNA expression was measured in HCC and corresponding non-neoplastic tumor surrounding tissue (TST) by real time PCR in OCT3-/- and WT mice. Protein expression was determined by western blot analysis. Finally mRNA expression of potential regulatory factors (HNF4a, PPAR-a and c-Myc) were investigated by real time PCR. Results: Tumor size (p < 0.01) and quantity (p = 0.001) were enhanced in OCT3-/-mice in comparison to WT mice after 10 months of DEN/Phenobarbital treatment. Tumors in OCT3-/-mice showed significant higher steatosis than their WT littermates (p < 0.001). Immunohistochemistry showed significantly increased Ki67- (p £0.01) and Caspase 3(p = 0.002) staining in HCCs in OCT3-/- vs. WT mice, suggesting enhanced proliferation and apoptosis. Tumors in OCT3-/- mice showed more fibrosis (p = 0.004) and more inflammation (p = 0.047) than HCCs in WT mice. Real time PCR indicated an up-regulation of SLC 22A1 in untreated OCT3-/- mice (p = 0.002). SLC 22A1 mRNA and OCT1 protein expression were down-regulated in HCC compared to TST in OCT3-/mice (p = 0.001) after 10 months. HNF4a and PPAR-a mRNA expression were up-regulated in untreated OCT3-/- mice compared to their WT littermates and down-regulated in HCC vs. TST in OCT3-/- mice. No significant changes could be found in c-Myc mRNA expression. Conclusion: OCT1 is up-regulated OCT3-/- mice. The down-regulation of OCT1 in HCC in OCT3-/- mice is associated with tumor progression. The expression of OCT1 might be regulated via HNF4a and PPAR-a in OCT3-/mice. Corresponding author: Knapstein, Johanna E-Mail: johanna.knapstein@unimedizin-mainz.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 4.44 Risikofaktoren f"r metabolische St#rungen nach Lebertransplantation: Analyse von Daten n"chterner Patienten Gebhardt S1, Jara M1, Malinowski M1, Seehofer D1, Puhl G1, Pratschke J1, Stockmann M1 1 Charit# – Universit$tsmedizin Berlin, Klinik f!r Allgemein-, Visceral- und Transplantationschirurgie, Berlin, Germany Hintergrund: Metabolische St#rungen wie Diabetes mellitus (DM), Dyslipid"mie und exzessive Gewichtszunahme geh#ren zu den h"ufigen Komplikationen nach orthotoper Lebertransplantation (OLT) und k#nnen zu erh#hter Morbidit"t und Mortalit"t beitragen. Die Identifikation von Risikofaktoren ist nach wie vor eine wichtige Thematik im Hinblick auf das Langzeit!berleben von Transplantationspatienten. Methoden: Glucose- und Lipidmetabolismus sowie das K#rpergewicht von 81 OLTPatienten wurden analysiert. Die prospektive Datenerhebung erfolgte pr"operativ, am 1., 3., 5., 10., 14. und 28. postoperativen Tag sowie 6 und 12 Monate nach Transplantation. Metabolische Daten von nicht n!chternen Patienten wurden von der Analyse ausgeschlossen. Zur Definition und Klassifikation von DM, body mass index (BMI) und Dyslipid"mie verwendeten wir offizielle und standardisierte Kriterien. Unabh"ngige Risikofaktoren f!r das Auftreten der metabolischen St#rungen ein Jahr nach Transplantation wurden ermittelt. Ergebnisse: Die Pr"valenz eines neuaufgetretenen Diabetes nach Transplantation (new-onset diabetes after transplantation; NODAT) betrug 9,3 %, wof!r sich pr"operative Adipositas als einziger Risikofaktor zeigte (odds ratio [OR]: 16,5). Eine gest#rte Glucosehom#ostase vor OLT (OR: 10,8) sowie eine initial schlechte Transplantatfunktion (OR: 6.89) waren unabh"ngige Risikofaktoren eines postoperativen DM. Die maximalen Pr"valenzen von Hypertriglycerid"mie (HTG) und Hypercholestein"mie (HC) wurden am 10. POD bzw. 6 Monate nach OLT beobachtet. Als Risikofaktoren f!r HC ein Jahr nach OLT identifizierten wir Alter (OR: 1,17) und postoperative Niereninsuffizienz (OR: 16,33). Ein h#herer pr"operativer BMI ergab sich als Risikofaktor f!r postoperative HTG (OR: 1,17). K#rpergewicht und BMI der Studienpopulation nahmen !ber 12 Monate signifikant ab (P< 0,05). Die Pr"valenz von Adipositas lag pr"operativ bei 22,2 % und postoperativ bei 20,9 %. Schlussfolgerung: Zum ersten Mal gelang es, eine initial schlechte Transplantatfunktion als Risikofaktor f!r DM nach Transplantation zu identifizieren. Durch eine strikte Definition des N!chtern-Status und den Ausschluss jeglicher exogener Faktoren, die den Metabolismus der Patienten beeinflussen, konnten die wahren Pr"valenzen der metabolischen St#rungen ermittelt werden. Wir glauben, dass wir somit einen wertvollen Beitrag zur Identifikation von Risikofaktoren leisten konnten. Korrespondierender Autor: Gebhardt, Sabine E-Mail: sabine.gebhardt@charite.de 4.45 Role of RAGE and its ligands S 100A8/A9 in hepatocellular carcinoma onset and development De Ponti AM1, Schneller D1, Pusterla T1, Wiechert L1, Longerich T2, Marhenke S3, Schirmacher P2, Vogel A3, Pikarsky E4, Hess J6, Angel P1 1 Division of Signal Transduction and Growth Control, DKFZZMBH Alliance, German Cancer Research Center (DKFZ), Heidelberg, Germany; 2Institute of Pathology, University Hospital Heidelberg, Heidelberg, Germany; 3Department of Hepatology, Medical School Hannover, Hannover, Germany; 4 Lautenberg Center for Immunology and Department of Pathology, IMRIC, Hebrew University-Hadassah Medical School, Jerusalem, Israel; 5Junior Group Molecular Mechanisms of Head and Neck Tumors, DKFZ-ZMBH Alliance, German Cancer Research Center (DKFZ), Heidelberg, Germany; 6Department of Otolaryngology, Head and Neck Surgery, University Hospital Heidelberg, Heidelberg, Germany mouse shows chronic hepatitis, liver damage and fibrosis followed by HCC development. On the other side, DEN is an alkylating agent that promotes DNA-strand breaks, thus leading to HCC formation in a cirrhosis-free context. Regarding HCC onset, we will investigate the role of RAGE and S 100A8 /A9 in HCC progenitor cells (HcPCs). It was already shown that HcPCs can be isolated from different mouse models, and that cells resembling HcPCs reside within dysplastic lesions that appear several months before HCC nodules. Regarding HCC development, we demonstrated that Rage ablation impaired tumor development only in the Mdr2-/- model, where it reduced number and size of tumors and limited liver damage and oval cell activation. On the contrary, absence of S 100a9 in the Mdr2-/- model did not affect HCC development nor liver damage, but lack of this protein significantly reduced the size of tumors in the DEN model. These unexpected results underline the complexity of the cross-talk between RAGE and its ligands, which orchestrate neoplastic transformation and malignant progression. They also highlight the necessity of using more sophisticated genetic models in order to decipher the contribution of each ligand and receptor involved in HCC development. Corresponding author: De Ponti, Aurora Maria E-Mail: a.deponti@dkfz.de 4.46 Serum Reponse Factor (SRF) is a transcriptional activator of Mouse Double Minute 4 (MDM4) in hepatocellular carcinoma Pellegrino R1, Thavamani A2, Geffers R3, Schirmacher P1, Nordheim A2, Longerich T1 1 University Hospital Heidelberg, Institute of Pathology, Heidelberg, Germany; 2University of T!bingen, Department for Molecular Biology, Interfaculty Institute of Cell Biology, T!bingen, Germany; 3Helmholtz Center for Infection Research, Genome Analytics, Braunschweig, Germany The Mouse Double Minute 4 (MDM4) represents a p53-binding protein acting as a transcriptional repressor. We have previously demonstrated that both MDM4 mRNA and protein levels are upregulated in about 50 % of human hepatocellular carcinomas (HCC). Although we identified 1q32 gains as a mechanism leading to MDM4 overexpression in human HCC, many liver tumors show a balanced MDM4 gene locus, but high MDM4 mRNA levels. Thus, we hypothesized that dysregulated transcription may account for the high MDM4 expression observed in human liver tumors. Here, we show that overexpression of the Serum Reponse Factor (SRF) is involved in the transcriptional upregulation of MDM4 in HCC, thereby supporting its protumorigenic function. Overexpression of SRF mRNA compared to normal liver tissue was observed in a collection of human HCCs. In addition, a strong association between MDM4 and SRF expression was found in these samples, which was paralleled by overexpression of the transcriptional co-activators ELK1 and MKL1 / 2 known to form complexes with SRF. Using in silico analysis we identified a putative SRF binding site in the MDM4 promoter region. SRF knockdown by gene-specific siRNAs resulted in a strong downregulation of MDM4 mRNA and protein levels in HCC cell lines, which was associated with a significant reduction of cell viability. The vice versa effect was recorded after ectopic SRF overexpression in vitro. Furthermore, SRF depletion decreased the luciferase activity of a MDM4 promoter reporter and ChIP experiments confirmed that SRF was able to bind the MDM4 promoter in human HCC cell lines. Finally, upregulation of MDM4 was observed in liver neoplastic lesions developed in SRF-VP16 transgenic mice. Taken together, our data demonstrate a crucial role for SRF in the transcriptional activation of MDM4 expression, thereby supporting the oncogenic activity of MDM4 in HCC in vitro and in vivo. Corresponding author: Pellegrino, Rossella E-Mail: Rossella.Pellegrino@med.uni-heidelberg.de The Receptor for Advanced Glycation-End products (RAGE) is a multiligand receptor, mainly involved in tissue damage and inflammatory disorders. RAGE and its ligands S 100A8 and S 100A9 have been shown to be overexpressed in tumors, including hepatocellular carcinoma (HCC), enhancing cancer progression and metastasis by still unknown mechanisms. To address the role played by RAGE and S 100A8 /A9 in HCC onset and development, we took advantage of two mouse models: (i) the multidrug resistance 2 knock-out (Mdr2-/-) mouse and (ii) treatment with the procarcinogen diethylnitrosamine (DEN). The Mdr2-/- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A51 A52 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 4.47 SKP2 cooperates with N-Ras or AKT to induce liver tumor development in the mouse 1 1 1 2 1 Calvisi DF , Delogu S , Cigliano A , Utpatel K , Sini M , Longerich T3, Waldburger N3, Ribback S1, Dombrowski F1, Chen X4, Evert M2 1 University Medicine of Greifswald, Institute of Pathology, Greifswald, Germany; 2University of Regensburg, Institute of Pathology, Regensburg, Germany; 3Ruprecht-KarlsUniversit$t of Heidelberg, Institute of Pathology, Heidelberg, Germany; 4University of California, Department of Bioengineering and Therapeutic Sciences, San Francisco, USA Mounting evidence indicates that S-Phase Kinase-Associated Protein 2 (SKP2) is overexpressed in human hepatocellular carcinoma (HCC). However, the role of SKP2 in hepatocarcinogenesis remains poorly delineated. To elucidate the function(s) of SKP2 in HCC, we stably overexpressed the SKP2 gene in the mouse liver, either alone or in combination with activated forms of N-Ras (N-RasV12), AKT1 (myr-AKT1), or b-catenin (DN90-b-catenin) protooncogenes, via hydrodynamic gene delivery. We found that forced overexpression of SKP2, N-RasV12 or DN90-bcatenin alone as well as co-expression of SKP2 and DN90-b-catenin did not induce hepatic histological alterations. Overexpression of myr-AKT1 alone led to HCC development after long latency. In contrast, co-expression of SKP2 with N-RasV12 or myr-AKT1 resulted in early development of multiple hepatocellular tumors in all SKP2 /N-RasV12 and SKP2 /myrAKT1 mice. At the molecular level, preneoplastic and neoplastic liver lesions from SKP2 /N-RasV12 and SKP2/myr-AKT1 mice exhibited a strong induction of AKT/mTOR and Ras/MAPK pathways. Noticeably, the tumor suppressor proteins whose levels have been shown to be downregulated by SKP2-dependent degradation in various tumor types, including p27, p57, DUSP1, and Rassf1A were not decreased in liver lesions from SKP2/N-RasV12 and SKP2 /myr-AKT1 mice. In human HCC specimens, nuclear translocation of SKP2 was associated with activation of the AKT/mTOR and Ras/MAPK pathways, but not with b-catenin mutations. In hepatoma cell lines, suppression of SKP2 activity by MLN4924 synergized with AKT and MAPK inhibitors to induce growth restraint. Altogether, the present data indicate that SKP2 cooperates with N-Ras or Akt proto-oncogenes to promote hepatocarcinogenesis in vivo. Corresponding author: Evert, Matthias E-Mail: matthias.evert@uni-greifswald.de 4.49 Chinatalpati C1, W"hler C1, Ehlting C1, Bode J1, H$ussinger D1, Keitel V1 1 Heinrich Heine University Hospital, Department of Gastroenterology, Hepatology and Infectiology, Duesseldorf, Germany TGR5 (Gpbar-1) is a G-protein coupled bile acid receptor, which is highly expressed in cholangiocytes, liver sinusoidal endothelial cells, liver macrophages and CD14 positive monocytes of peripheral blood. TGR5-/- mice show impaired liver regeneration after partial hepatectomy and the increased inflammation in liver disease models, thus emphasizing a protective role of TGR5 in liver. While TGR5 functions are being studied extensively, little is known about the transcriptional regulation of this receptor. Aim: To investigate the mechanism and transcriptional regulation of TGR5. Methods: The potential TGR5 promoter (-154 /-79) was cloned into a pGL3 Luciferase expression vector. Luciferase gene expression was used to evaluate the effect of specificity protein 1 (Sp1) and Kr!ppel like factor 5 (KLF5) on TGR5 expression by cotransfection. Binding of the two transcription factors to the promoter was verified by Chromatin Immunoprecipitation (ChIP). Phosphorylation of Sp1 was shown by immunoprecipitation. Results: KLF5 increased the luciferase gene expression in a concentration dependent manner. The effect was lost when the binding site for KLF5 was mutated. High expression of Sp1 mediated a downregulation of luciferase activity, which was absent when mutated Sp1 with no DNA binding activity was cotransfected. KLF5 enhanced the phosphorylation of Sp1. ChIP analysis confirmed the binding of both transcription factors to the promoter region. Conclusion: This study demonstrates that the transcription factor Sp1 downregulates whereas KLF5 upregulates the gene expression of TGR5 in vitro. KLF5 increases the transcription of TGR5 either directly through interaction with the promoter and/or by decreasing the DNA binding activity of Sp1 via increased Sp1 phosphorylation. Corresponding author: Chinatalpati, Chakravarthi E-Mail: chintalapaticv@gmail.com 4.50 4.48 Smad7 suppresses HCC development in a DEN induced mouse model Feng T1, Dzieran J1, Maass T2, Teufel A2, Dooley S1, MeindlBeinker NM1 1 Heidelberg University, Department of Medicine II, Section Molecular Hepatology, Mannheim, Germany; 2University Hospital Regensburg, Department of Internal Medicine I, Regensburg, Germany Introduction: Hepatocellular carcinoma (HCC) is the most frequent primary liver tumor. The transforming growth factor-b (TGF-b) signaling pathway plays a critical role in cancer progression. Smad7, a TGF-b target gene, acts as physiological feedback inhibitor of TGF-b and has been found tumorigenic in several tumors. Knowledge about the role of Smad7 in HCC is limited so far. This study investigated the potential effects of Smad7 in a DEN induced HCC mouse model. Methods: Hepatocyte specific Smad7 transgenic mice were generated by crossing TTRCre mice with Alb-Smad7 transgenic mice. For the induction of HCC, two weeks old mice were injected intraperitoneally (i.p.) with 25 mg/kg DEN (Sigma). At 9 months of age, mice were sacrificed and livers were processed for further analysis. To induce Smad7 expression, 4 weeks old mice were injected with 1 mg/mice/day Tamoxifen (Sigma, T5648) for 5 days. Tamoxifen was dissolved in a pH neutral medium chain triglyceride (Neutral#l, Euro OTC Pharma) at a final concentration of 10 mg/ml. Results: Expression of transgenic Smad7 was confirmed with RT-PCR and by immunohistochemistry. Compared to wild type, Smad7 transgenic mice showed a significantly lower tumor number. Discussion/ Conclusion: The results suggest that Smad7 plays an inhibitory role in the development of DEN induced HCC in mice. We currently use hepatocyte specific inducible Smad7 knock out animals to confirm our findings. Since Smad7 has both TGF-b dependent and independent functions, the detailed molecular mechanism how Smad7 affects the TGF-b or other pathways in this process needs to be further investigated. Corresponding author: Meindl-Beinker, Nadja M E-Mail: Nadja.Meindl-Beinker@medma.uni-heidelberg.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York Sp1 dependent transcriptional regulation of G-protein coupled bile acid receptor Gpbar-1: role of Kr"ppel like factor 5 The hepatic tumor microenvironment is important for the CSC phenotype and progression of liver cancer Fischer M1, Heinrich S2, Andersen JB4, Castven D1, Sprinzl M1, Gockel I2, W"rns MA1, Thorgeirsson S3, Galle PR1, Lang H2, Marquardt JU1 1 University of Mainz, Department of Medicine I, Mainz, Germany; 2University of Mainz, Department of Surgery, Mainz, Germany; 3CCR/NCI/NIH, Laboratory of Experimental Carcinogenesis, Bethesda, USA; 4University of Copenhagen, Biotech Research and Innovation Centre, Copenhagen, Denmark Background: The cancer stem cell (CSC) hypothesis is an emerging concept in cancer research that provides a plausible explanation for the observed phenotypic heterogeneity of many cancers, including hepatocellular carcinoma (HCC). Despite profound therapeutic implications, the prognostic relevance of CSCs and their cellular localization within the tumor formation remain controversial. Methods: Localization and expression levels of selected CSC marker were assessed in 30 HCCs using qRT-PCR, imunohistochemistry and Western-Blotting. Whole transcriptome analysis of the central tumor, invasive tumor margin (TM) as well as surrounding liver (SL) were performed and associated signaling pathways were investigated. Results were integrated with our existing database of 53 HCC. Results: Established HCC markers were gradually induced in the tumor tissue. Activation of CSC and pluripotency markers EpCAM, CD133 and NANOG were predominantly observed in SL and their levels decreased towards the tumor core. Consistently, transcriptomics between SL, tumor tissue and the TM showed a distinct expression profile. The established gene signature showed activation of pathways related to proliferation and apoptosis in the tumor tissue while the TM was characterized by inflammatory, EMT-related gene sets and activation of pro-survival signaling networks such as ERK and FOS. Significantly, integration of the signatures with 53 wellcharacterized HCC cases revealed a strong association of the TM with survival of HCC patients. Conclusion: The CSC phenotype is predominantly determined by a permissive tumor microenvironment. We found, that pro-oncogenic properties originate in the TM. The activation of key oncogenic features and immune response signaling indicates that the 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen cross-talk between tumor and microenvironment might be a promising therapeutic and/or preventive target. Corresponding author: Marquardt, Jens U. E-Mail: marquarj@uni-mainz.de 4.51 Virotherapy overcomes tumor resistance to PD-1-immunotherapy by broad mutanome-directed T cell responses in mice Woller N1, G!rlevik E1, Fleischmann-Mundt B1, Knocke S1, Geffers R2, Manns MP1, Kubicka S1, K!hnel F1 1 Hannover Medical School, Clinic for Gastroenterology, Hepatology, and Endocrinology, Hannover, Germany; 2 Helmholtz-Center for Infection Research, Genome Analytics, Braunschweig, Germany Recently, immune checkpoint blockade has been established as a novel generic immunotherapy of solid tumors. Since pre-existing antitumoral T-cell responses appear to be a precondition for the success of PD-1immunotherapy, concomitant cancer vaccinations have been investigated but did not affect the clinical outcome. Therefore, we investigated whether localized oncolytic virotherapy is capable to overcome resistance to PD-1-immunotherapy. First, we analysed putative neoantigens in selected cell lines. The PD-1 sensitive cell line Hepa1 – 6 revealed 1741 non-synonymous single nucleotide variants suggesting a hypermutated phenotype which can explain the high immunogenicity of this cell line. The anti-PD-1 resistant lung adenocarcinoma cell line CMT64 showed 274 SNVs which is in line with mutation frequency in human patients. Investigations on a selection of 44 putative neoepitope-specific CD8 T cell responses in tumor bearing mice showed that PD-1 immunotherapy was only capable of inducing a single neoepitope-specific response without therapeutic efficacy whereas viral oncolysis by intratumoral application of the oncolytic adenovirus hTert-Ad elicited CD8 T-cell responses to a panel of neoepitopes that also showed cytotoxic activity in an in-vivo CTL-assay. Unexpectedly, virotherapy-induced antitumoral immune responses were not additionally enhanced by concomitant PD-1 blockade. Instead, we observed a strong and irregular spreading of T-cell responses which was correlated to improved elimination of disseminated lung colonies. Next, we investigated the efficacy of adenoviral oncolysis and PD 1-checkpoint inhibition in a transgenic model of electroporation-induced cholangiocarcinoma model which disseminates to the lung. Here, we demonstrated that antitumoral immune responses, raised by adenoviral oncolysis and concomitant PD-1 inhibition, but not single treatments, completely inhibited the growth of lung metastases in a CD 8-dependent manner. In summary, our results show that intratumoral oncolysis breaks tumor resistance to PD-1 immunotherapy and strongly recommend this promising therapeutic combination for further evaluation in clinical studies. Corresponding author: K!hnel, Florian E-Mail: kuehnel.florian@mh-hannover.de 4.52 Volumen-Funktionsplanung in der Leberchirurgie: Was kann man von der Kombination aus 3D- CT- Volumetrie mit dem LiMAx-Test erwarten? Kirchstein A1, Stockmann M1, Malinowski M1, Jara M1, Seehofer D1, Schmidt SC1, Pratschke J1 1 Charit#, Department of General, Visceral and Transplant Surgery, Berlin, Germany Hintergrund und Ziel: Gerade nach ausgedehnten Leberteilresektionen oder bei vorgesch"digtem Lebergewebe bleibt die postoperative Leberinsuffizienz eine gef!rchtete Komplikation. Exakte Volumen- Funktionsplanung k#nnte helfen gef"hrdete Patienten zu identifizieren und ad"quat auf das Risiko zu reagieren. Bislang konnte kein klinisch routinem"ßig anwendbarer Leberfunktionstest verl"ssliche Ergebnisse zur Funktionsplanung liefern. Die Lebervolumetrie und Kalkulation des verbleibenden Leberrestvolumens (future liver remnant, FLR) allein l"sst ebenso keine Aussage auf die tats"chliche Funktionsreserve nach der Operation zu, da f!r jeden Patienten ein individuelles Verh"ltnis aus Lebervolumen und – Funktionskapazit"t anzunehmen ist. Wir postulieren, dass mit dem neuartigen 13C-Methacetin-Atemtest (LiMAx-Test) in Kombination mit virtueller Resektionsplanung anhand einer 3D-CT-Volumetrie der Leber eine zuverl"ssige Vorhersage der postoperativ verbleibenden funktionellen Residualkapazit"t der Leber (future liver remnant function, FLRF) zu treffen ist. Methoden: In dieser durch die Ethikkommission der Charit' – Universit"tsmedizin Berlin und das Bundes- amt f!r Strahlenschutz zugelassenen, kontrollierten prospektiven Single-Center-Studie wurden Patienten vor onkologischen Leberresektion eingeschlossen und pr"operativ einer Volumen-Funktionsplanung mittels 3D-CT-Volumetrie (MeVis Medical Solutions AG, Bremen) und dem LiMAx-Test (Humedics, Berlin) unterzogen. Die FLRF ergab sich aus dem Verh"ltnis von FLR und pr"operativem funktionellem Lebervolumen bezogen auf die maximale pr"operative Funktionskapazit"t (LiMAx-Wert in mg/h/kg). Eine weitere 3D-CT-Volumetrie auf der Basis einer direkt postoperativen CT und die Ermittlung der LiMAx-Werte 6 h postoperativ und am 1. postoperativen Tag dienten der &berpr!fung der Planungsergebnisse. Der postoperative Verlauf wurde !ber 3 Monate verfolgt. Ergebnisse: Von 68 Patienten durchliefen bisher 28 tats"chlich eine Leberresektion und das gesamte Studienprotokoll. Mit im Mittel )28,8 ml untersch"tzt das FLR der virtuellen Resektionsplanung das postoperativ gemessenen Leberresidualvolumen nur leicht. Hier existiert eine starke Korrelation von r = 0.936 (p < 0,001). Auf FLR basierend zeigte die FLRF eine mittlere Abweichung von 15,8 mg/h/kg vom 6 h postoperativ erhobenen LiMAx-Wert und es ergibt sich ebenfalls eine starke Korrelation von r = 0,844 (p < 0,001). Zusammenfassung: Unsere Untersuchungen zeigen, dass eine Volumen-Funktionsplanung mithilfe des LiMAx-Tests und virtueller Resektionsplanung anhand einer 3D-CT-Volumetrie zuverl"ssig die postoperative Leberfunktionskapazit"t prognostizieren kann. Mithilfe dieser Methode lassen sich somit Risikopatienten f!r postoperative Leberinsuffizienz sicher identifizieren, f!r welche alternative Behandlungskonzepte infrage k"men. Im Rahmen eines individuellen Patientenmanagements k#nnte dies helfen die Patientensicherheit zu erh#hen. Korrespondierender Autor: Kirchstein, Antje E-Mail: antje.kirchstein@charite.de 5. Virus Immunology 5.1 Human liver chimeric mice as a new model of Hepatitis E Virus infection and preclinical drug evaluation Gass S1, Volz T1, Giersch K1, Allweiss L1, Lohse A1, Petersen J3, Polywka S4, Pischke S5, Dandri M1, L!tgehetmann M4 1 University Hospital Hamburg-Eppendorf, I. Department of Internal Medicine, Hamburg, Germany; 2German Center for Infection Research (DZIF), Hamburg-L!beck-Borstel Partner Site, L!beck, Germany; 3Asklepios Klinik St. Georg, Hamburg, Germany; 4University Hospital Hamburg-Eppendorf, Institute of Microbiology, Virology and Hygiene, Hamburg, Germany; 5University Hospital Hamburg-Eppendorf, Health Care Center, Outpatient Clinic of Liver Transplantation, Hamburg, Germany Objective: Hepatitis E Virus (HEV) is recognized as important pathogen in developing and industrialized countries leading to acute and chronic infections with considerable morbidity and mortality. Since our knowledge about the molecular biology and pathogenicity of HEV is still rudimental, we employed humanized uPA/SCID/beige (USB) mice to establish a new small animal model of HEV infection. Methods: Homozygous USB mice repopulated with primary human hepatocytes were inoculated with either patient-derived HEV-positive serum or stool suspensions from genotype 1 or 3. Virological parameters were determined at serological and intrahepatic levels with quantitative real-time PCR as well as immunofluorescence staining. Sucrose gradients were performed with HEV from faeces and serum in order to characterize the virions. Results: HEV infection in humanized mice was successful only after intravenous (i.v.) injection of stool-derived virions (1 x 105 IU/mouse; n= 3 /3 genotype 1 and genotype 3, respectively), but not after i.v. injection of serum derived virions (n= 13) obtained from 3 acutely HEV infected patients. Notably, i.v. HEV genotype 1 inoculated mice developed viremia with up to 1 x 106 IU/ml within 4 weeks and remained stable for up to 20 weeks. HEV-infected human hepatocytes could be visualized by immunofluorescence using HEV orf2 and orf3 specific antibodies. Kinetics of infection with HEV genotype 3 were slower and resulted in up to 2.5 x 104 IU/ml viremia within 8 – 11 weeks of infection. Comparable to the situation found in human samples and regardless of the genotype used, HEV concentrations in faeces were higher (1 – 2 log) than in the corresponding serum samples. Sucrose gradient analyses also revealed that HEV virions retrieved either from mouse or human serum displayed a significantly lower density than virions obtained from faeces, which indicates that serum virions are possibly associated with lipids. Notably, HEV infection could be passaged by cohousing HEV Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A53 A54 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen chronically infected with uninfected humanized mice, thus demonstrating the establishment of de novo HEV infection through the faecal-oral route in humanized mice. Finally, six-weeks of treatment with ribavirin (50 mg/kg/daily) led to a 2log reduction of HEV viremia and intrahepatic HEV-RNA/GAPDH as well as loss of orf2-positive hepatocytes. Conclusion: We established an efficient model of HEV infection closely resembling the human infection with respect to viral replication, viral morphogenesis and routes of infection. We could demonstrate successful infection with HEV genotype 1 and 3 and assess the strong antiviral effect of ribavirin in this model. This new infection system offers new possibilities to test the efficacy of established and new antiviral therapeutic concepts, as well as to exploit mechanisms of viral interference in human hepatocytes in vivo. Corresponding author: Gass, Sofia E-Mail: sofi_gass@yahoo.de 5.2 Microbial translocation in liver fibrosis induces chronic IFNAR signaling that directly affects innate immune responses to systemic bacterial infection Abdullah Z1, Hackstein P1, Trebicka J2, Beyer M3, Schultze JL3, Kastenm!ller W1, Sauerbruch T2, Spengler U4, Kurts C5, Knolle PA1,6 1 Institute of Molecular Medicine, University of Bonn, Germany; 2Department of Internal Medicine I, University of Bonn, Germany; 3Genomics and Immunoregulation, Life and Medical Sciences Institute (LIMES), University of Bonn, Germany; 4Department of General Internal Medicine, University of Bonn, Germany; 5Institute of Experimental Immunology, University of Bonn, Germany; 6Institute of Molecular Immunology (IMI), Technische Universit$t M!nchen, Munich, Germany A common clinical complication in patients with liver fibrosis or cirrhosis is exacerbations of bacterial infections, which often persist in these patients. In order to study the underlying pathophysiological cellular and molecular mechanisms in mice, we investigated the immune responses to Listeria infections in the context of liver fibrosis. Using the bile-duct ligation model for the induction of liver fibrosis in mice we found an enhanced susceptibility to Listeria infections leading to persistence of infection, recapitulating clinical situations in humans. While the innate clearance of Listeria in the spleen of those mice was unaltered, bactericidal activity of intrahepatic macrophages and bacterial clearance in the liver were strongly impaired. This reduced local clearance of Listeria was correlated to impaired IFNg, IL-12 and ROS production by the myeloid cells in the liver. Mechanistically, we identified IFNAR signaling in the myeloid cells as the basis for impaired anti-bacterial immune responses in mice with liver fibrosis. Using germ free mice we could show that IFNAR signaling is induced by translocated gut microbiota during liver fibrosis. This chronic Type I IFN signals on myeloid cells in turn lead to IL-10 release, which directly inhibited IFNg, IL-12 and ROS production. Strikingly, we could rescue mice form chronic infection by either blocking IFN signaling in myeloid cells or systemic blockade of IL10 signaling, opening an exciting new therapeutic avenue for bacterial infections in patients suffering from liver fibrosis or cirrhosis. Corresponding author: Abdullah, Zeinab; Knolle, Percy E-Mail: zeinab.abdullah@ukb.uni-bonn.de, percy.knolle@tum.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York 5.3 Nanoparticle-based autoantigen delivery to Treg-inducing liver sinusoidal endothelial cells enables control of autoimmunity in mice Carambia A1, Freund B2, Schwinge D1, Bruns OT3, Salmen SC4, Ittrich H5, Reimer R3, Heine M2, Huber S1, Waurisch C6, Eychm!ller A6, Wraith DC7, Korn T8, Nielsen P2, Weller H4, Schramm C1, L!th S1, Lohse AW1, Heeren J2, Herkel J1 1 University Hospital Hamburg-Eppendorf, Department of Medicine I, Hamburg, Germany; 2University Hospital Hamburg-Eppendorf, Department of Biochemistry and Molecular Cell Biology, Hamburg, Germany; 3Heinrich-Pette Institute, Hamburg, Germany; 4Universit$t Hamburg, Institute of Physical Chemistry, Hamburg, Germany; 5 University Hospital Hamburg-Eppendorf, Department of Diagnostic and Interventional Radiology, Hamburg, Germany; 6Technische Universit$t Dresden, Physical Chemistry, Dresden, Germany; 7University of Bristol, Cellular and Molecular Medicine, Bristol, UK; 8Technische Universit$t M!nchen, Department of Neurology, Munich, Germany Background/Aims: Previously, we have shown that ectopic expression of a neural autoantigen in the liver induced the generation of autoantigen-specific CD 4+ Foxp3+ regulatory T cells (Tregs) that could suppress experimental autoimmune neuroinflammation (L!th S et al., J Clin Invest. 2008). Moreover, we identified liver sinusoidal endothelial cells (LSECs) as the major antigen-presenting cell type responsible for hepatic Treg induction (Carambia A et al., J Hepatol. 2014). Here we aimed to explore whether targeted delivery of autoantigen-peptides to LSECs could be harnessed for the induction of autoantigen-specific Tregs in vivo and the treatment of autoimmune disease. Methods: We engineered a polymeric nanoparticle carrier (NP) that facilitates efficient delivery of autoantigen peptides to LSECs in vivo. In the well-characterized autoimmune disease model of experimental autoimmune encephalomyelitis (EAE), we investigated whether administration of LSEC-targeting autoantigen peptide-loaded NPs could protect mice from autoimmune disease. Results: In two independent disease models, we studied whether treatment with LSEC-targeting myelin-peptide-loaded nanoparticles could protect mice from Myelin Basic Protein (MBP)-induced EAE in B10.PL mice or from Myelin Oligodendrocyte Glycoprotein (MOG)-induced EAE in C 57Bl/ 6 mice. Intriguingly, in both disease models, a single intravenous injection of MBP or MOG peptide-loaded nanoparticles one day after EAE-induction provoked a lasting and complete protection from clinical EAE; in contrast, control mice treated with PBS or with unloaded nanoparticles developed clinical EAE symptoms, including hind-limb paralysis. Even more importantly, the mean clinical score of mice with already established EAE (mean score of 1.6) improved rapidly and substantially following administration of a single dose of MOG-loaded nanoparticles (mean change in EAE score -0.6), whereas the control group deteriorated (mean change in EAE score +1.0; P= 0.0002). Treatment efficacy depended on Tregs since the Treg frequencies in the spleens of mice treated with MOG peptide loaded nanoparticles were significantly higher than those in PBS-treated mice (12.0 % vs. 6.8 % Foxp3+ of CD 4+; P= 0.001). Moreover, nanoparticle-mediated disease control was abrogated after Treg-depletion by repeated administration of the Treg-depleting PC61 antibody (mean score at disease maximum: 0.6 vs. 2.3; P= 0.0027). Mechanistically, NP-induced Tregs seemed to prevent the egress of inflammatory effector cells from the spleens of MOG-NP recipients, as indicated by increased splenocyte numbers and down-regulation of CXCR4 and Syndecan-4 compared to PBS-treated control mice. Conclusion: Our findings provide proof-ofprinciple that the selective delivery of autoantigen peptides to LSECs by nanoparticles can induce antigen-specific Tregs and enable effective treatment of autoimmune disease. Corresponding author: Carambia, Antonella E-Mail: a.carambia@uke.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 5.4 Breadth of the HCV-specific CD 4+ T cell response in spontaneous resolvers is independent from the IL-28 haplotype Scheurich C1, Lewis-Ximenez L2, Lohse AW1, Chung RT2, Kim AY2, Lauer GM2, Schulze zur Wiesch J1 1 University Hospital Hamburg-Eppendorf, I. Department of Internal Medicine, Hamburg, Germany; 2Massachusetts General Hospital, 2. GI Unit, Boston, MA, USA A minority of patients is able to spontaneously clear an acute hepatitis C virus (HCV) infection. A strong, broad and lasting HCV-specific Th cell response is regarded as a hallmark and best correlate of immunologic control of HCV viremia. On the other hand, it was recently determined that certain polymorphisms (eg. SNP rs12979860) in the region of IL-28B highly correlate with spontaneous resolution of viremia. The aim of this study was to test the hypothesis whether the breadth and priming of HCV CD 4+ T cell response is linked to the IL-28 polymorphism. We compare the breadth of the HCV-specific CD 4+ T cell response of two combined cohorts from Hamburg (Germany) and Boston (MA, USA) with a total of 66 patients with spontaneously resolved HCV and different IL28 haplotype by the use of in vitro HCV specific ELISPOT assays and intracellular cytokine staining (ICS) following in vitro stimulation of T cell short term lines with a panel of 24 frequently recognized HCV peptides. We find that while there were few resolver patients with the unfavorable T/T haplotype in our cohort, the responses were comparable in all groups and each patient showed an average of nearly 6 / 24 different HCV CD 4+ epitopes regardless of the IL-28 haplotype (P> 0.70). Our data indicate that Il28 and T cell responses are independent correlates of spontaneous viral clearance in HCV. Corresponding author: Schulze zur Wiesch, Julian E-Mail: julianszw@googlemail.com 5.5 An additional heme oxygenase-1 knockout increases maturation of dendritic cells and liver inflammation in mdr2 knockout mice Barikbin R1, Sandmann M2, Quaas A2, Karimi K1, Sass G1, Tiegs G1 1 University Medical Center Hamburg, Institute of Experimental Immunology and Hepatology, Hamburg, Germany; 2University Medical Center Hamburg, Institute of Pathology, Hamburg, Germany Background: Deletion of the multi drug resistance protein 2 (Mdr2) in mice causes hepatic inflammation and fibrosis with progression to hepatocellular carcinoma (HCC) at about 12 month of age (Mdr2 knockout mouse; Mdr2ko; FVB.129P2-Abcb4tm1Bor). We have recently shown that induction of heme oxygenase-1 (HO-1) in Mdr2ko mice interferes with liver inflammation, fibrosis formation and proliferation. We established a double knockout mouse for Mdr2 and HO-1 (Mdr2 /HO-1ko) to further investigate effects of HO-1 on chronic liver inflammation and its consequences. Methods: Liver damage was monitored by alanine aminotranferase (ALT) levels. Liver hydroxyproline content was measured as a fibrosis marker. Spleen weight was measured as a marker of inflammation. Leukocyte infiltration and neoductuli formation was visualized by H&E staining of liver slices. Flow cytometry was used to analyze liver immune cell populations. Bone marrow derived dendritic cells (BM-DCs) were analyzed for cytokine production and expression of maturation markers. Female and male (F/M) FVB/N background control (wt), Mdr2ko, and Mdr2/HO-1ko mice were analyzed at the age of 12 weeks. Results: ALT levels were significantly up-regulated in Mdr2ko (F/M), and male Mdr2 /HO-1ko mice compared to wt, while female Mdr2 /HO-1ko display even higher ALT levels. Liver hydroxyproline levels were significantly higher in Mdr2 /HO-1ko mice (F/M) compared to Mdr2ko mice (F/ M). Spleen weight was doubled in Mdr2ko (F/M) mice compared to wt, while Mdr2 /HO-1ko (F/M) mice showed a 5 fold elevated spleen weight. In histological stainings, Mdr2ko, and Mdr2 /HO-1ko mice (F/M) showed similar levels of leukocyte infiltration and neoductuli formation and were significantly up-regulated compared to wt mice. Flow cytometry data showed increased frequencies of T-cells and NKT-cells as well as CD 11c+ dendritic cells (DCs) in Mdr2 /HO-1ko mice compared to Mdr2ko mice. In addition DCs showed increased surface expression of CD86. BM-DCs from Mdr2/HO-1ko showed a 5 fold increase in MHCII-, and CD86- expression as well as a 5 fold increase in IL-12 production even without LPS restimulation compared to Mdr2ko. Conclusion: Mdr2 /HO-1ko mice have a stronger fibrotic and inflammatory phenotype compared to the single Mdr2ko. The stronger inflammation can be explained by higher frequencies of CD 3+ T-cells, NKT-cells and mature DCs. High production of IL-12 in BM-DCs indicate a stronger Th1 response in Mdr2 /HO-1ko mice compared to Mdr2ko. Corresponding author: Barikbin, Roja E-Mail: r.barikbin@uke.de 5.6 Assoziation von Autoantik#rpern und Symptomen bei der Prim!r Bili!ren Zirrhose (PBC) Weiler-Normann C1, Voigt L1, Lohse AW1, Schramm C1 1 University Hospital Hamburg-Eppendorf, Medical and Polyclinic I, Hamburg, Germany Hintergrund: In der Literatur finden sich Hinweise auf eine Assoziation von &berleben und der Pr"senz von nukle"ren Antik#rpern bei der Prim"r bili"ren Zirrhose (PBC), insbesondere gp210 Autoantik#rper und Zentromer-Antik#rper scheinen mit einer schlechteren Prognose vergesellschaftet zu sein. Fragestellung: In der vorliegenden Arbeit soll die Assoziation von Autoantik#rpern und Symptomen sowie Erkrankungsstadium bei der PBC untersucht werden. Methodik: Die Akten von 280 Patienten mit der wahrscheinlichen oder gesicherten Diagnose einer PBC wurden retrospektiv analysiert. Alle Patienten wurden an der I. Medizinischen Klinik und Poliklinik des Universit"tsklinikums Hamburg-Eppendorf behandelt. Ergebnisse: Von den 280 Patienten (89,3 % weiblich, medianes Alter 60,7 Jahre) zeigten insgesamt 226 anti-mitochondriale Antik#rper (80,7%). 34 wiesen gp210 Antik#per auf (12%), 62 (22%) sp100 Antik#rper und 32 (11,4 %) anti-Zentromer-Antik#rper. 22 Patienten hatten nur gp210 oder SP100 Antik#rper bei negativem Befund f!r AMA. Der mittlere Beobachtungszeitraum ab Diagnosezeitpunkt war 60 Monate. Das Therapieansprechen gem"ß der Paris-Kriterien unterschied sich nicht zwischen den verschiedenen Gruppen. W"hrend keine Assoziation von Autoantik#rpern mit dem Verlauf der Erkrankung gefunden wurde, hatten Patienten mit sp100-Autoantik#rpern sowie mit Zentromer-Antik#rpern signifikant h"ufiger eine FatigueSymptomatik sowie eine Sicca-Symptomatik. Diskussion: Patienten mit einer sp100- oder zentromer-positiven PBC haben signifikant h"ufiger eine Fatigue-Symptomatik sowie eine Sicca-Symtpomatik. Daher sollten Patienten mit einem solchen Autoantik#rper-Muster gezielt diesbez!glich beraten und ggf. auch therapiert werden. Korrespondierender Autor: Weiler-Normann, Christina E-Mail: cweiler@uke.de 5.7 Baseline gamma-GT levels within the normal range predict high virologic response rates in treatment-na%ve patients undergoing boceprevir triple therapy for HCV genotype 1 (G1) infection Buggisch P1, L"hr HF2, Teuber G3, Steffens H4, Kraus MR5, John C6, Geyer PR7, Weber B8, Witth"ft T9, Herrmann A10, Hoesl M11, Naumann U12, Zehnter E13, Hartmann D14, Dreher B14, Bilzer M14 1 IFI Institute, Hamburg, Germany; 2Gastroenterological Practice, Wiesbaden, Germany; 3Gastroenterological Practice, Frankfurt, Germany; 4Practice of internal Medicine, Berlin, Germany; 5Klinium Burghausen, Medical Department II, Burghausen, Germany; 6Practice of Internal Medicine, Berlin, Germany; 7Gastroenterological Practice, Fulda, Germany; 8Competence Center Addiction, Kassel, Germany; 9Gastroenterological Practice, Stade, Germany; 10 Friedrich-Schiller-University, Jena, Germany; 11 Gastroenterological Practice, Nuremberg, Germany; 12 Center of Medicine, Berlin, Germany; 13Gastroenterological Practice, Dortmund, Germany; 14MSD Pharma GmbH, Haar, Germany Background: A considerable number of patients (pts) with chronic HCV G1 infection will present with elevated serum gamma-GT levels. However, the impact of gamma-GT elevation on virologic response to boceprevir triple therapy has not been investigated until yet and was therefore the aim of the present interim analysis of the German NOVUS observational study. Methods: From April 2012 until January 2014, 536 pts with G1 infection were recruited in the ongoing NOVUS study by 97 practices and hospitals in Germany. Pts were treated with pegylated interferons (PegIFN) and ribavirin (RBV) together with BOC for 24 to 44 weeks after a 4 weeks lead-in period with PegIFN/RBV. The present interim analysis was restricted to 257 previously untreated patients with documented gamma-GT levels at baseline. Results: Overall, 122 of 257 patients (47.5%) had elevated gamma-GT levels at baseline Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A55 A56 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen (66.4 % male, 41.0% > 50 years, 74.6 % with baseline viral load > 400.000 IU/mL) while 135 pts (52.5 %) had gamma-GT levels within the normal range (48.9 % male, 34.1% > 50 years, 62.2 % with baseline viral load > 400.000 IU/mL). Pts with baseline gamma-GT values in the normal range showed a better virologic response to PegIFN/RBV lead-in at the end of treatment week (TW) 4 as demonstrated by a higher proportion of pts with a HCV-RNA decline > 1log10 in comparison to pts with elevated gamma-GT levels (86.8 % vs. 69.0 %, p = 0.0008). In line with this observation a higher proportion of pts with normal gamma-GT values achieved an early virologic response (EVR) at TW8 (83.1% vs. 58.7 %, p < 0.0001) as well as a better virologic response at TW12 (93.4 % vs. 84.5 %, p = 0.0425) and at the end of treatment (EOT) (93.8 % vs. 83.1%, p = 0.0216) when compared with pts with elevated gamma-GT levels. Documented follow-up data were available from 133 pts. Until now, 51 of 61 pts (83.6%) with normal gamma-GT levels achieved a sustained virologic response (SVR) in contrast to 41 of 62 pts (66.1%) with elevated gamma-GT levels (p = 0.0256). Conclusions: Baseline gamma-GT levels within the normal range in more than 50 % of pts with HCV G1 infection are associated with a better response to BOC triple therapy. In particular the high proportion of pts who achieve an EVR (83%) may profit from a shortage of treatment duration. The stronger HCV-RNA decline at the end of lead-in suggests a higher sensitivity to PegIFN/RBV backbone in pts with normal gamma-GT values at baseline. Corresponding author: Bilzer, Manfred E-Mail: manfred.bilzer@bilzer-consulting.de 5.8 Baseline predictors of an early virologic response (EVR) in previously untreated patients undergoing boceprevir (BOC) triple therapy for HCV genotype 1 infection in German real-life Buggisch P1, L"hr H2, Teuber G3, Steffens H4, Kraus M5, John C6, Geyer P7, Weber B8, Witth"ft T9, Herrmann A10, Hoesl M11, Naumann U12, Zehnter E13, Hartmann D14, Dreher B14, Bilzer M14 1 IFI Institute, Hamburg, Germany; 2Gastroenterological Practice, Wiesbaden, Germany; 3Gastroenterological Practice, Frankfurt, Germany; 4Practice of internal Medicine, Berlin, Germany; 5Klinium Burghausen, Burghausen, Germany; 6Practice of Internal Medicine, Berlin, Germany; 7 Gastroenterological Practice, Fulda, Germany; 8Competence Center Addiction, Kassel, Germany; 9Gastroenterological Practice, Stade, Germany; 10Friedrich-Schiller-University, Jena, Germany; 11Gastroenterological Practice, Nuremberg, Germany; 12Center of Medicine, Berlin, Germany; 13 Gastroenterological Practice, Dortmund, Germany; 14MSD Pharma GmbH, Haar, Germany Background: The achievement of EVR during triple therapy of chronic HCV genotype 1 (G1) infection with BOC has been identified as predictor of high SVR rates of up to 90 % as well as a predictor to shorten triple therapy to 24 weeks. The present interim analysis of the NOVUS observational study was aimed to investigate EVR during BOC triple therapy in German real-life and to identify baseline predictors of EVR. Methods: From April 2012 until January 2014, 536 patients with G1 infection were recruited in the ongoing NOVUS study by 97 practices and hospitals in Germany. Patients were treated with pegylated interferons (PegIFN) and ribavirin (RBV) together with BOC for 24 to 44 weeks after a 4 weeks lead-in period with PegIFN/RBV. The present interim analysis was restricted to 222 previously untreated patients with documented HCVRNA levels at treatment week (TW) 8. Results: The frequency of EVR was 71% (158 / 222). Achievement of EVR was significantly associated with the following baseline factors: age < 50 years (vs. > 50 years): 76.3 % vs. 62.7%, p = 0.0303; low viral load (LVL) < 400.000 IU/mL (vs. > 400.000 IU/mL): 84.5% vs. 64.7%, p = 0.0024; gamma-GT levels within the normal range (vs. elevated): 82.0 % vs. 57.4 %, p < 0.0001; ferritin levels < 300 mg/L (vs. > 300 mg/L): 71.6 % vs. 41.6%, p = 0.0088; glomerular filtration rate (eGFR) > 90 mL/min per 1.73 m2 (vs. eGFR 60 – 90): 73.2 % vs. 57.4 %, p = 0.0416. In contrast, no association with the achievement of EVR was found for gender (male vs. female), ALT and glucose levels (normal range vs. elevated), genotype 1 subtypes (1a vs. 1b) or APRI score (< vs. > 0.7). When a multivariate logistic regression model was used, viral load and gamma-GT levels at baseline were identified as independent predictors of EVR: baseline viral load (< vs > 400.000 IU/ mL): OR 2.87 (CI 1.04 – 5.70; p = 0.040); gamma-GT (normal vs elevated): OR 2.87 (CI 1.37 – 6.02; p = 0.0053). In line with this observation an EVR rate of 93% was achieved in patients with LVL < 400.000 IU/mL together with normal gamma-GT levels at baseline. Conclusions: In German real- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York life 71% of previously untreated patients undergoing BOC triple therapy for HCV G1 infection achieve a prognostic favorable EVR. LVL < 400.000 IU/mL and normal gamma-GT levels are independent baseline predictors of high EVR rates > 80 % or EVR rates up to 93 % when combined. The advantage to identify patients with high virologic response rates to BOC triple therapy by standard laboratory parameters in real-life may be helpful for patients and physicians and in addition, appears to be costeffective. Corresponding author: Bilzer, Manfred E-Mail: manfred.bilzer@bilzer-consulting.de 5.9 Biomarkers to predict the clinical outcome of hepatitis delta Wranke A1, Serrano BC1, Ernst S2, Heidrich B1, Kirschner J1, Bremer B1, Hardtke S3, Cornberg M1, Koch A2, Manns MP1, Falk CS4, Wedemeyer H1 1 Hannover Medical School, Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany; 2 Hannover Medical School, Institute for Biometry, Hannover, Germany; 3HepNet Study-House, Hannover, Germany; 4 Hannover Medical School, Institute of Transplant Immunology, IFB-Tx, Hannover, Germany Background: Hepatitis delta is the most severe form of viral hepatitis. Pegylated interferon alpha is effective in only 25 – 30 % of patients and associated with frequent side effects. Thus, it is crucial to identify patients with benign courses of liver disease who may not require treatment. We recently introduced a baseline-event-anticipation (BEA)-Score for hepatitis delta considering thrombocytes, bilirubin, INR, age, sex and country of origin as factors being associated with the development of clinical endpoints. The aim of this study was to improve the BEA-Score with easy to measure biomarkers. Methods: We selected 75 consecutive hepatitis delta patients with retrospective serum samples available and tested 50 cytokines, chemokines and angiogenic factors using multiplex technology (Bio-Plex System). The cohort included 29 female patients (37%); the mean age was 39.5 years. Most of the patients were born in Eastern Mediterranean countries (36%) or the former Soviet Union (39%). 33 patients had already liver cirrhosis at first presentation. The mean time of follow-up was 4.3 years (range 0.5 – 14.2). Clinical endpoints occurred in 27 patients (35 %) and were defined as hepatic decompensation (ascites, encephalopathy, variceal bleeding), hepatocellular carcinoma, orthotropic liver transplantation or death. Results: Most factors included in the previously published BEA-Score were confirmed. Regarding serum markers TNF-a (p = 0.04, HR= 0.97) and VCAM-1 (p = 0.02, HR= 3.1) were associated with the development of endpoints. According to hazard ratios we considered in addition clinical parameters: age (p = 0.03, HR = 1.1), gGt (p = 0.02, HR= 4.6), INR ‡ 1.2 (p < 0.01, HR= 6.6), and albumin (p = 0.02, HR= 0.9). Based on YoudenIndex derived cutoffs a formula was developed for the new BEA 2.0Score: albumin (£35 g/l) + 0.5*INR (‡1.2) + gGt (‡35 U/l) + 2*age (‡40 years) + 2*TNF-a (£35 pg/ml) + VCAM-1 (‡65500 pg/ml). This score determined the clinical outcome of hepatitis delta with high sensitivity (100 %) and specificity (96%) as well as high positive (61 %) and negative (100 %) predictive values. The initial BEA score showed an ROC-AUC of 0.83 in this independent cohort whereas the newly BEA 2.0- Score proved an ROC-AUC of 0.93. Conclusions: The clinical long-term outcome of hepatitis delta can be reliably predicted by a combination of clinical parameters and distinct cytokines and angiogenic factors. These data can have clinical implications for selection of patients at most urgent need for antiviral therapy. The role of TNF-a and VCAM-1 in the pathogenesis of chronic hepatitis delta required further investigation. Corresponding author: Wranke, Anika E-Mail: awranke@freenet.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 5.10 Bispecific antibody constructs mediate immunotherapeutic retargeting of effector cells towards HBV infected target cells Bohne F1, Hasreiter J1, Quitt O1, Bruss V3, Moldenhauer G2, Momburg F2, Protzer U1 1 Technische Universit$t M!nchen/Helmholtz Zentrum M!nchen, Institute of Virology, Munich, Germany; 2German Cancer Research Center (DKFZ), National Centre for Tumor Diseases, Heidelberg, Germany; 3Helmholtz Zentrum M!nchen, Institute of Virology, Neuherberg, Germany Retargeting of effector cells is a promising immune-therapeutic approach to circumvent the immunotolerant state found in malignancies and chronic viral infections. Effector cells are supplied with designed specificities allowing redirection, and can be further equipped with costimulatory signals, together reverting the immunocompromised situation. To achieve retargeting against HBV-infected cells, we constructed tetravalent bispecific antibody constructs harboring two different binding domains of immunoglobulins. The first binding site was designed to target HBV-infected cells by binding the S domain of HBV envelope proteins on the plasma membrane of infected hepatocytes. The second binding motif engages immune effector cells using specificities for T cells (CD 3-T cell receptor and CD28 for co-stimulatory signals). These binding sites are connected via an Fc-linker, also providing for dimerization. We furthermore generated variants of bispecific antibody constructs containing mutations in the Fc-spacer, abrogating Fc-receptor binding, to control for unwanted activation through antibody-dependent cell-mediated cytotoxicity. Confocal microscopy showed that all bispecific constructs bound specifically to the surface of HBV-producing cell lines. Through the engagement of HBV-positive target and immune effector cells, the bispecific constructs induced a specific activation of effector cells, which secreted high amounts of IFNg, IL-2 and TNFa. In deep multispectral flow cytometry was used to measure phenotypic changes of retargeted effector cells by intracellular cytokine staining. This showed, that up to 50 % of effector cells were polyfunctionally activated by the bispecific antibody constructs upon coculture with HBV positive target cells. Co-administration of CD3- and CD 28-specific constructs had a synergistic effect and mediated up to 98.5 % specific cytotoxic elimination of HBV S-protein positive cells in co-cultures with PBMC. MACS sorted CD4 and CD8 positive cells could also individually be retargeted to specifically kill target cells. Importantly, bispecific antibody constructs were also able to redirect effector cells to HBV-infected HepaRG cell resulting in specific killing of HBV-infected cells. Furthermore, immobilized HBsAg was sufficient for immunotherapeutic retargeting, while soluble HBsAg, mimicking the high viral loads in patient serum failed to induce effector cell activation. First preliminary in vivo experiments with transplanted HBV-positive tumors showed a merked decrease in tumor size upon treatment with bispecific constructs. Thus, retargeting of immune effector cells towards HBV-infected cells using bispecific constructs is a promising new immune-therapeutic approach against chronic Hepatitis B. Corresponding author: Bohne, Felix E-Mail: felix.bohne@tum.de 5.11 Broad and cross-genotype-specific T cell responses during acute hepatitis E virus infection Gisa A1, Ventaka SP1, Behrendt P1, Pischke S2, Bremer B1, Manns MP1, Cornberg M1, Wedemeyer H1, Kraft A1 1 Hannover Medical School, Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany; 2 University Hospital Hamburg Eppendorf, MVZ Liver Transplantation, Germany Background and aims: Hepatitis E is an inflammatory liver disease caused by infection with the hepatitis E virus (HEV). In tropical regions HEV is epidemic and predominantly mediated by HEV genotype 1 and 2 with > 3 million symptomatic cases per year and around 70,000 deaths. In Europe and America the zoonotic HEV genotype 3 and 4 have been predominantly reported. Whereas only 500 cases have been registered at the Robert-Koch-Institute in 2013, it has been estimated that approximately 17% of the population in Germany were exposed to HEV. Little is known about T cell responses during acute HEV infection. Therefore, we investigated HEV-specific CD4 and CD8 T cell responses in acute HEV infected individuals. Methods: Peripheral blood mononuclear cells (PBMCs) were incubated with six HEV-specific overlapping peptide pools spanning ORF2 and ORF3 of the HEV genome of genotype 1 and 3. HEV-specific T cell responses were determined by CFSE proliferation assay and intracellular cytokine staining in 12 acute HEV infected patients. All patients were HEV-RNA positive in the blood at their first visit. In 4 of these patients a longitudinal study (1 – 2 month and > 1 year post the first visit) was performed. Results: Broad functional HEVspecific CD4 and CD8 T cell responses were detectable in all 12 HEV infected patients targeting both ORF2 and ORF3 peptides. Importantly, cross-genotype HEV-specific T cell responses were measurable in these patients. Whereas the HEV-specific CD4 T cell response was mainly IFNg/ TNFa double positive, the specific CD8 T cell response predominantly expressed only IFNg. In 4 patients T cell responses were determined in follow up visits and HEV-specific T cell responses were still be detectable. Interestingly, in all 4 follow-ups the proliferative capacity of the HEV-specific CD4 T cell responses decreased early after HEV clearance, but increased to similar proliferative capacity 1 year later. Conclusions: In conclusion, we could show strong functional and cross-genotype HEV-specific T cell responses in acute hepatitis E virus infected individuals. HEV-specific T cell responses against both genotype 1 and 3 suggest potential cross-genotype memory responses. This may have clinical implications for both protection from HEV infection after vaccination (the only licensed Chinese HEV vaccine is based on HEV genotype 1) but also when travelling to HEV-1 endemic countries. Corresponding author: Gisa, Anett E-Mail: gisa.anett@mh-hannover.de 5.12 CEACAM1 deficiency exacerbates acute liver injury in a mouse model of immune-mediated hepatitis Wegscheid C1*, Horst AK1*, Tiegs G1 1 University Medical Center Hamburg-Eppendorf, Experimental Immunology and Hepatology (Center of Experimental Medicine), Hamburg, Germany * equal contribution Introduction: Injection of a sublethal dose of the T cell mitogenic plant lectin concanavalin A (ConA) induces acute immune-mediated liver injury. Hallmarks of liver injury are increased plasma transaminase activities and the release of pro-inflammatory cytokines. CEACAM1 is a cellular adhesion molecule that is expressed on epithelia, endothelia, and leukocytes. Originally, CEACAM1 has been identified as an intercellular homophilic adhesion molecule on hepatocytes. The CEACAM1 isoform with a long cytoplasmic domain contains an immune receptor tyrosine-based inhibition motif (ITIM) that is pivotal in for its negative regulation of leukocyte activation. Methods: C 57BL/ 6 wt and Ceacam1-/- mice were injected with a sublethal dose of ConA (5 mg/kg) or saline, respectively. Mice were sacrificed at different time points after ConA challenge, and plasma transaminase activities and expression of cytokines were determined. FACS analyses were performed to characterize the intrahepatic immune cell composition in wt and Ceacam1-/- mice in comparison to spleen before and after challenge with ConA. Results: In Ceacam1-/- mice, exacerbation of liver damage was observed in contrast to wt mice, evident by significant elevation of plasma transaminase activities. FACS analyses showed a marked increase of CEACAM1-expression on CD 4+ T cells and CD 4+Foxp3+ regulatory T cells (Tregs) after ConA-challenge. Although IL-10 levels were lower in plasma from Ceacam1-/- compared to wt mice, Tregs from na+ve Ceacam1-/- mice showed no impairment of suppressive activity towards responder CD 4+ T cells in vitro in contrast to wt Tregs. Interestingly, overall numbers of Tregs in Ceacam1-/- mice were diminished in thymus, spleen and liver before and after ConA challenge. Furthermore, hepatic neutrophilia and eosinophilia were found in Ceacam1-/- mice. Conclusion: Based on the observation that liver injury is aggravated in Ceacam1-/- mice, we suggest an involvement of CEACAM1 in T cell and myeloid cell-mediated attenuation of liver damage in immune liver diseases. In the ConA model, CEACAM1 exerts immune modulatory functions by regulating hepatic and splenic CD 4+ T cell and myeloid cell abundance and differentiation. Further studies are under way to characterize the role of CEACAM1 for migration or differentiation of Tregs in ConA mediated liver injury. Also, the impact of CEACAM1-negative myeloid cells on acute liver injury needs to be defined. Herein, we demonstrate that CEACAM1+ Tregs yield liver protection following a TH1-polarized immune response. Future studies will have to show whether this phenomenon relies on the qualitative or quantitative regulation of hepatic T cell and myeloid cell recruitment and function. Corresponding author: Wegscheid, Claudia E-Mail: c.wegscheid@uke.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A57 A58 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 5.13 Clinical immune monitoring: Impact of in vitro PBMC expansion on quantity and quality of HBV-specific CD4 and CD8 T cells Russo C1, Dembek C1, Geisler F2, Ringelhan M2, Michler T1, Sprinzl M4, Umgelter A2, Draenert R3, Bauer T1, Protzer U1 1 Technische Universit$t M!nchen/Helmholtz Zentrum M!nchen, Institute of Virology, Munich, Germany; 2 Technische Universit$t M!nchen, II. Medical Department, Munich, Germany; 3Ludwig Maximilian Universit$t, IV. Medical Department, Munich, Germany; 4Johannes Gutenberg-Universit$t, I. Medical Department, Mainz, Germany In vitro expansion of PBMC is commonly used prior to a T-cell monitoring to increase low number of peripheral HBV-specific T cells. However, whether in vitro expansion changes functional composition of T-cell responses detectable directly ex vivo has not yet been investigated in detail. We compared quantity and functionality of HBV surface- (HBs) and core- (HBc) specific CD 4/CD8 T cells ex vivo and after 10-days in vitro expansion in 41 individuals with different HBV status (acute selflimiting, chronic or resolved infection). T-cell reactivity was analyzed by intracellular cytokine staining (IL-2, IFN-g, TNF-a) using multiparametric flow cytometry. The 10-day in vitro expansion significantly increased number of total HBc-specific CD4 and CD8 T cells (median increase factor 12.8 and 7.0, respectively) and HBs-specific CD4 T cells (median increase factor 4.3), but not HBs-specific CD8 T cells. Proliferative capacity of HBV-specific T cells was independent of the detected ex vivo frequency and the donor’s HBV status. However proliferative capacity of HBc-specific CD4 T cells negatively correlated with serum HBs antigen (HBsAg) and alanine transferase (ALT) levels in patients with acute selflimiting hepatitis B (r=-0.9 and r=-0.79, respectively). Unexpectedly, in about 20 % of the donors a HBs-specific T-cell response was detected ex vivo, which was lost after in vitro expansion (CD4: 8/ 41; CD8: 9/ 41). In contrast in vitro expansion increased sensitivity to monitor HBc-specific T-cell responses. Functional composition of ex vivo HBV-specific T-cell responses also differed significantly compared to expanded HBV-specific T cells. Ex vivo, but not any more after expansion detectable HBV-specific T cells were predominantly monofunctional. In summary our data show that in vitro expansion significantly alters number and functionality of HBV-specific T cells compared to an analysis directly ex vivo. No general increase of assay sensitivity was observed after in vitro expansion. From our results, we conclude that ex vivo monitoring of HBVspecific T cells better reflects the in vivo situation, and should thus be considered for future clinical immune monitoring. Corresponding author: Russo, Carolina E-Mail: carolina.russo@helmholtz-muenchen.de 5.14 Clinical significance of drug-drug interactions during HCV therapy with sofosbuvir and simeprevir in comparison to first wave protease inhibitors H"ner zu Siederdissen C1, Maasoumy B1, Deterding K1, Port K1, Manns MP1, Wedemeyer H1, Cornberg M1 1 Hannover Medical School (MHH), Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany Background: Recently, it has been shown that considerable drug-drug interactions (DDI) between a first wave protease inhibitor (PI, boceprevir or telaprevir) and the regular outpatient medication affect up to 50 % of hepatitis C virus (HCV) infected patients. The lately approved second wave direct-acting antiviral agents (DAA) sofosbuvir (SOF) and simeprevir (SMV) are supposed to be involved in less DDI. However, so far, no data is available regarding the potential benefit in the real-world. We here aimed to evaluate the risk for DDI with the regular outpatient medication during therapy with SOF and SMV in comparison to first wave PIs. Methods: A cohort of 115 patients has been assessed for their concomitant outpatient medication, which importantly also included over-the-counter medicine and herbals. DDI with SMV and SOF have been assessed using different DDI websites and the prescribing information of all analyzed drugs. DDI were assigned to 4 different categories (0 = Classification not possible due to lack of information, 1 = no clinically significant interactions expected, 2 = interaction possible, may need dose adjustment/monitoring, 3 = co-administration not recommended). DDI were also compared to DDI with first-wave PI, which have been previously described in the same cohort (Maasoumy et al. AP&T, 2013). Results: 115 patients took 116 different drugs with mean 2.7 drugs per Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York patient (range 0 – 11). Importantly, category 3 DDI did not occur in any of the patients with either SOF or SMV. This is in contrast to the first wave of PIs, in which 10 % of these patients were affected by category 3 DDI (p < 0.0001 for both, SOF and SMV). 3% of the drugs had category 2 DDI with SOF, affecting 3% of the patients. On the contrary, 21% of the drugs had category 2 DDI with SMV, affecting 39 % of patients. In comparison, SOF had significantly lower category 2 DDI than first wave PIs and SMV (p < 0.0001). SMV showed a trend to a lower rate of DDIs in comparison to first wave PIs (p = 0,13). In both, SOF and SMV, DDIs could not be assessed for 4% of the concomitant drugs due to lack of information in all of the above mentioned databases, affecting 7% of patients (category 0). This was caused by certain supplements and herbal medications. Conclusion: Treatment with SOF and SMV is associated with a lower potential for DDI in comparison with first-wave PI, especially for category 3 DDI. However, the risk for DDI must not be neglected, as it still affects a significant number of patients, in particular, if SMV is used as part of the therapeutic regimen. Corresponding author: H#ner zu Siederdissen, Christoph E-Mail: hoenerzusiederdissen.christoph@mh-hannover.de 5.15 Current clinical evaluation of the patient with HCV genotype 1 infection before antiviral treatment in German routine clinical practice Buggisch P1, L"hr H2, Teuber G3, Steffens H4, Kraus M5, John C6, Geyer P7, Weber B8, Witth"ft T9, Herrmann A10, Hoesl M11, Naumann U12, Zehnter E13, Hartmann D14, Dreher B14, Bilzer M14 1 IFI Institute, Hamburg, Germany; 2Gastroenterological Practice, Wiesbaden, Germany; 3Gastroenterological Practice, Frankfurt, Germany; 4Practice of Internal Medicine, Berlin, Germany; 5Klinium Burghausen, Burghausen, Germany; 6Practice of Internal Medicine, Berlin, Germany; 7 Gastroenterological Practice, Fulda, Germany; 8Competence Center Addiction, Kassel, Germany; 9Gastroenterological Practice, Stade, Germany; 10Friedrich-Schiller-University, Jena, Germany; 11Gastroenterological Practice, Nuremberg, Germany; 12Center of Medicine, Berlin, Germany; 13 Gastroenterological Practice, Dortmund, Germany; 14MSD Pharma GmbH, Haar, Germany Background: Invasive and noninvasive tests in patients (pts) with chronic HCV genotype 1 (G1) infection are aimed to assess the severity of liver disease, in particular the stage of fibrosis, and to detect other potential coexisting liver diseases such as hemochromatosis or diseases which can be aggravated by antiviral treatment such as thyroid dysfunctions. The aim of the present interim analysis of the German NOVUS observational study was to investigate the current clinical evaluation of the patient with chronic HCV G1 infection in German routine clinical practice before antiviral treatment with boceprevir. Methods: From April 2012 until January 2014, 536 pts with G1 infection were recruited in the ongoing NOVUS study by 97 practices and hospitals in Germany. Until now, diagnostic tests and imaging techniques performed before triple therapy of HCV G1 infection with boceprevir were documented for 497 pts (treatment-na+ve N= 329, pretreated N = 168). Results: HCV G1 subtypes and HCV-RNA levels were reported for all pts. Serum ALT, AST and gamma-GT levels as well as complete blood cell counts including hemoglobin values were obtained with a frequency of 90 %-95 %. Baseline levels of bilirubin and creatinine were determined in 85% while thyroid function was tested by TSH measurement in 75%. In contrast, metabolic parameters such as triglycerides, cholesterol and glucose were tested with a frequency of 43 %-58 %. IL 28B genotype was determined in only 22% and HCC screening by alpha-fetoprotein was documented for 32 % of pts. Serum ferritin levels were obtained in 37%. Of these 27% and 3% had pathological high/low ferritin levels > 300 and < 15 mg/dL. Abdominal ultrasound was performed in 77% and liver elastography in only 13 %. Liver biopsy findings were documented for only 19 % of pts and 50 % of liver biopsy specimens were obtained within the last 24 weeks. Conclusions: In routine clinical practice standard laboratory test such as determination of HCV-RNA levels, liver enzymes and blood cell counts are performed with a high frequency. However, there is only scarce information about the stage of liver fibrosis or coexisting liver diseases such as hemochromatosis or nonalcoholic steatohepatitis. This is mainly related to a low frequency of liver biopsies and liver elastografies in the daily routine. Corresponding author: Bilzer, Manfred E-Mail: manfred.bilzer@bilzer-consulting.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 5.16 Delayed early HCV RNA response during IFN-free therapy with sofosbuvir in interferon-ineligible patients with advanced cirrhosis Deterding K1, H"ner zu Siederdissen C1, Port K1, Kirschner J1, Sollik L1, Mix C1, Manns MP1, Cornberg M1, Wedemeyer H1 1 Hannover Medical School, Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany Sofosbuvir has been approved for the treatment of patients with chronic hepatitis C in Europe in January 2014. Phase 3 trials suggested lower response rates to sofosbuvir treatment in patients with liver cirrhosis. However, there is limited information on the efficacy and safety of interferon-free sofosbuvir + ribavirin therapy in interferon-ineligible patients with advanced cirrhosis. Sofosbuvir and weight-based ribavirin therapy was initiated in 59 patients with liver cirrhosis who could not be treated with interferon. Simeprevir was not available at that time. All patients had transient elastography values of > 14.5 kPa (41 patients with values > 20kPa) and 15 patients had Child B or C cirrhosis. 64% had received an interferon-based treatment before. HCV genotypes 1, 2, 3 and 4 were present in 29, 3, 25 and 2 patients, respectively. HCV RNA was determined with the Ampliprep-CobasTaqMan Assay (LLoQ of 15 IU/ml) at treatment weeks 1, 2, 4 and 8. Results: All patients had HCV RNA values of < 15 IU/ml at week 8 of therapy, however, 13% of patients showed still positive but unquantifiable HCV RNA results. HCV RNA was undetectable in genotype 1 patients in 4%, 10 % and 31% at weeks 1, 2 and 4 while this was less frequently the case for genotype 3-infected patients (0 %, 0 % and 17%, respectively). Still, a similar proportion of genotype 1 and 3 patients reached HCV results of < 15 IU/ml by week 4 (79% vs. 87%). At this time point, 17 patients were completely negative for HCV RNA, 30 patients were positive but < 15 IU/ml and 9 patients had still HCV RNA values > 15 IU/ml. The week 4 HCV RNA response was associated and lower bilirubin levels (p = 0.002) and higher pre-treatment albumin (p = 0,09). ALT values normalized in most patients before HCV RNA was negative. Albumin levels significantly increased during the first 2 months of therapy (34 g/l € 6 before therapy vs. 36 g/l € 5 after 2 months; p = 0,016). Levels of creatinine and lipase were stable in both groups during therapy. Fatigue (53 %), sleep disorder (25%) and muscle pain (20 %) were the most reported adverse events. Conclusions: Early HCV RNA kinetics in patients with advanced liver cirrhosis differ during sofosbuvir + ribavirin therapy between HCV genotypes and are associated with pre-treatment liver function. Treatment will be continued for 24 weeks and the possible impact of early treatment response for posttreatment relapse will be reported at the meeting. Corresponding author: Deterding, Katja E-Mail: Deterding.Katja@mh-hannover.de 5.17 Die HIV Infektion ist mit einer verminderten anti-HCV Aktivit!t von CD 3+CD 56+ NK-like T Zellen assoziiert Kokordelis P1, Kr$mer B1, Boesecke C1, Gl$ssner A1, Wolter F1, Kaczmarek D1, Voigt E2, Ingiliz P3, Strassburg CP1, Rockstroh JK1, Spengler U1, Nattermann J1 1 University Hospital of Bonn, Department of Internal Medicine I, Bonn, Germany; 2Praxis am Ebertplatz, Cologne, Germany; 3Medical Center for Infectious Diseases (MID), Berlin, Germany Hintergrund: Bei HIV(+) Patienten ist die Ko-Infektion mit dem Hepatitis C Virus die Hauptursache f!r Morbidit"t und Mortalit"t. Es ist gezeigt worden, dass CD 3+CD 56+ NK-like T Zellen, eine Subpopulation von Lymphozyten, in der akuten HCV Monoinfektion eine wichtige Rolle hinsichtlich der spontanen Ausheilung spielen. Dagegen blieb bislang unklar, ob NK-like T Zellen eine direkte anti-HCV Aktivit"t aufweisen und inwieweit die Ko-Infektion mit dem HI-Virus die Funktion dieser Zellen beeintr"chtigt. In dieser Arbeit zeigen wir, dass CD 3+CD 56+ NKlike T Zellen die HCV Replikation effektiv hemmen k#nnen, es jedoch bei HIV(+) Patienten zu funktionellen Ver"nderungen kommt. Methoden: Acht HIV monoinfizierte Patienten, zw#lf HIV(+) Patienten mit chronischer Hepatitis C, acht HIV(-) Patienten mit chronischer HCV Infektion sowie zw#lf gesunde Probanden wurden im Rahmen der Studie untersucht. Periphere NK-like T Zellen (CD 3+CD 56+) wurden ph"notypisch mittels Durchflusszytometrie und die IFN-g Sekretion sowie die antiHCV Aktivit"t der NK-like T Zellen mithilfe des HuH7 Replikon Systems analysiert. Ergebnisse: Nur unstimulierte CD 3+CD 56+ NK-like T Zellen von gesunden Probanden zeigten eine mittelm"ßige anti-HCV Aktivit"t, jedoch erh#hte die Stimulation mit IL-12/IL-15 signifikant deren Kapazit"t die HCV Replikation zu hemmen. Die Tatsache, dass &berst"nde von IL-12/IL-15 stimulierten CD 3+CD 56+ NK-like T Zellen ebenfalls die HCV Replikation in vitro blockieren konnten, lassen vermuten das nicht zytolitische Mechanismen eine Hauptrolle spielen. Dementsprechend konnten wir nur ein geringes Abt#ten von HuH7 HCV Replikon Zellen durch spezifische Lyse von CD 3+CD 56+ NK-like T Zellen nachweisen. Dar!berhinaus stellten wir fest, dass die Stimulation mit IL-12/IL-15 die Produktion von IFN-g signifikant erh#hte und die Blockierung von IFN-g mit einem spezifischen Antik#rper die anti-virale Aktivit"t der CD 3+CD 56+ NK-like T Zellen signifikant reduzierte. Interessanterweise fand sich bei den HIV(+) Patienten, dass die HIV Infektion unabh"ngig von einer HCV Ko-Infektion, mit einer signifikant reduzierten IFN-g Produktion CD 3+CD 56+ NK-like T Zellen assoziiert ist. In &bereinstimmung hiermit zeigten CD 3+CD 56+ NK-like T Zellen von HIV(+) Patienten eine signifikant niedriger anti-HCV-Aktivit"t im Vergleich zu Zellen gesunder Probanden. Eine wichtige Rolle scheinen hierbei CD 161+CD 3+CD 56+ NK-like T Zellen zu spielen, da sich bei HIV(+) Patienten verglichen mit den Kontrollen eine signifikant niedrigere Frequenz dieser Zellen fand und die Frequenz CD161 positiver NK-like T Zellen positiv mit der Produktion von IFN-g korrelierte. Schlussfolgerung: Unsere Daten zeigen, dass die HIV Infektion mit einer verminderten anti-HCV Aktivit"t von CD 3+CD 56+ NK-like T Zellen assoziiert ist. Dies stellt m#glicherweise einen Mechanismus einer dysregulierten Immunantwort bei HIV/HCV Koinfizierten Patienten dar. Korrespondierender Autor: Kokordelis, Pavlos E-Mail: pavlos.kokordelis@ukb.uni-bonn.de 5.18 Differential regulation of TNF receptor signaling during viral infection of hepatocytes determines cell death Janas M3, Heikenw$lder M2, Knolle P1, Wohlleber D1 1 Technische Universit$t M!nchen, Institute of Molecular Immunology, Munich, Germany; 2Technische Universit$t M!nchen, Institute of Virology, Munich, Germany; 3 University of Bonn, Institutes of Molecular Medicine and Experimental Immunology, Bonn, Germany Viral infections are detected by the innate immune system via pattern recognition receptors or by the adaptive immune system via (cross-)presentation of viral antigens. Many viruses have developed mechanism to escape such immune recognition. We identified a new CD8 T Cell effector function against hepatotropic infections that overcomes immune escape by modulating MHC I presentation and conventional innate immune recognition. CD8 T effector cells (CTLs) secrete TNF upon recognition of viral antigens on cross-presenting liver sinusoidal endothelial cells which selectively kills infected hepatocyte. Here we investigated the underlying mechanisms that render infected hepatocytes susceptible to TNF induced cell death. We infected mice with a hepatotropic adenovirus and challenged these mice by injecting TNF. Using knockout mice, as well as biochemical and multiparametric histological methods we demonstrate that viral infection is not recognized by classical pattern recognition receptors. Rather, in hepatocytes viral infection modulates metabolic processes, leads to increased levels of the pro-apoptotic BCL-2 family members Bax and Bad and inflicts damage to mitochondria. This leads to a downregulation of the anti-apoptotic protein XIAP (X-chromosome linked inhibiting of apoptosis protein). Downregulation of XIAP facilitates TNF-induced activation of the initiator caspase 8 that together with increased mitochondrial sensitivity to activated caspase 8 is responsible for TNF-induced cell death in virus-infected hepatocytes. The mechanisms unraveled here demonstrate the existence of a so far unappreciated link between effector functions of adaptive immunity that deploys innate immune sensing mechanisms in virus-infected hepatocytes for control of viral infection in the liver. Corresponding author: Wohlleber, Dirk E-Mail: dirk.wohlleber@tum.de 5.19 Dominance of HLA-B restricted virus-specific CD 8+ T cell epitopes in chronic HBV infection Lang J1, Kiraithe M1, Thimme R1, Neumann-Haefelin C1 1 University Hospital of Freiburg, Department of Medicine II, Freiburg, Germany Background and Aims: HBV-specific CD 8+ T cells are essential for HBV clearance and are an attractive target for immunotherapeutic intervention. However, the HBV-specific CD 8+ T-cell repertoire is poorly characterized. Indeed, < 10 HLA-B restricted HBV-specific CD 8+ T cell epitopes are described to date, although recent findings in the field of HIV and Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A59 A60 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen HCV infection clearly demonstrate a dominant role of these epitopes. We therefore aimed to identify novel CD 8+ T-cell epitopes in HBV-infection and also address the relative contribution of HLA-A versus HLA-B restricted epitopes. Methods: 30 patients with chronic HBV (genotype D) and low viremia were screened for HBV-specific CD 8+ T-cell responses using overlapping peptides spanning all HBV proteins in a matrix setup in an elispot assay. Positive responses were confirmed by intracellular interferon gamma staining, optimal epitopes were finemapped and HLA restriction was determined. In addition, the autologous viral sequences corresponding to the identified epitopes were analyzed in the patients. Results: 10 out of 30 patients targeted at least one CD 8+ T cell epitope (range: 1 – 10). In total, we identified 27 CD 8+ T cell responses. None of these responses targeted previously described HBVspecific CD 8+ T cell epitopes. To date, we were able to fine-map 9 novel CD 8+ T cell epitopes. Importantly, all but one of these epitopes were restricted by HLA-B alleles (4 x HLA-B*35; 2 x HLA-B*7; 1 x HLA-B*15; 1 x HLA-B*51). In one epitope restricted by HLA-B*35:02 we found strong evidence for the selection of viral escape mutations. Conclusion: In our cohort, HBV-specific CD 8+ T cell responses are dominantly restricted by HLA-B alleles. These findings indicate that previous studies on HBVspecific immunity that mainly focused e.g. on HLA-A*02 restricted CD 8+ T cell epitopes may not necessarily be conferrable to the complete CD 8+ T cell repertoire. They also suggest that HLA-B restricted CD 8+ T cell epitopes may be important targets for immunotherapy. Corresponding author: Neumann-Haefelin, Christoph E-Mail: christoph.neumann-haefelin@uniklinik-freiburg.de 5.20 Duration of remission and interpretation of biochemical markers within the normal range help to identify patients with high chance for sustained remission after treatment withdrawal in autoimmune hepatitis Hartl J1, Sebode M1, Weiler-Normann C1, Ehlken H1, Kreuels B1, Zenouzi R1, Pannicke N1, Peiseler M1, Lohse AW1, Schramm C1 1 University Hospital Hamburg-Eppendorf (UKE), First Medical Center, Hamburg, Germany Aims: In autoimmune hepatitis (AIH), relapse rates as high as 95 % have been reported after treatment withdrawal. We therefore investigated, whether longer duration of treatment and proper patient selection could increase the long-term success rates of treatment withdrawal. Methods: Following our previously published experience, treatment withdrawal was considered when biochemical remission was maintained under immunosuppressive monotherapy for at least 2 years. Remission was defined as repeatedly normal serum aminotransferase levels as well as normal IgG levels. Statistical analysis was performed by using cox regression models to assess predictors for relapse. Results: Out of 288 patients with well-defined AIH, 28 patients were included. Median duration of treatment was 48.5 months (range 35 – 179) and a sustained remission was observed for 45 months (range 24 – 111). All patients were in remission on immunosuppressive monotherapy for a minimum of 2 years before treatment was withdrawn. Using this strict approach, 15 patients (54%) remained in long-term remission after a median of 28 months follow-up (range 17 – 57) and 13 patients (46%) required reinstitution of treatment. Higher ALT and IgG levels – although within the normal range in all patients – were associated with the time to relapse. All patients who remained in remission had ALT levels less than half the ULN and IgG levels not higher than 12 g/l at the time of treatment withdrawal. Conclusion: Proper patient selection including a sustained complete biochemical remission on immunosuppressive monotherapy for a minimum of 2 years can markedly improve the success rates of treatment withdrawal. The interpretation of aminotransferase and IgG levels within the normal range could aid in predicting the risk of relapse. Corresponding author: Hartl, Johannes E-Mail: j.hartl@uke.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York 5.21 Dysregulierte Interaktion zwischen CD 4+ T Zellen und NK Zellen in der HIV/HCV Koinfektion Kr$mer B1, Gl$ssner A1, Zwank C1, Goeser F1, Ingeliz P2, Boesecke C1, Strassburg CP1, Spengler U1, Rockstroh J1, Nattermann J1 1 University Hospital of Bonn, Department of Internal Medicine I, Bonn, Germany; 2Medical Center for Infectious Diseases (MID), Berlin, Germany Hintergrund: Die HCV/HIV Koinfektion ist im Vergleich zur HCV Monoinfektion mit einer schnelleren Progression einer Lebererkrankung assoziiert. Nat!rliche Killer (NK) Zellen haben auf die Viruseliminierung bei Hepatitis C einen enormen Einfluss. Bei der Aktivierung von NK Zellen sind nach bisheriger Erkenntnis CD 4+ T Zellen involviert. Allerdings ist eine HIV Infektion insbesondere durch dysfunktionelle CD 4+ T Zellen gekennzeichnet. Aus diesem Grunde vermuten wir bei der Immunpathogense der HIV/HCV Koinfektion eine gest#rte Interaktion zwischen CD 4+ T Zellen und NK Zellen. Material und Methoden: In diese Studie wurden 40 HIV Patienten, davon 21 HIV RNA(-) Patienten mit HAART und 19 HIV RNA(+) Patienten ohne Therapie, und 20 gesunde HIV(-)/HCV(-)Probanden eingeschlossen. Die IL 2-Produktion CD 4+ T Zellen wurde nach CD 3/CD28 Stimulation mittels Durchflusszytometrie getestet. Die antiHCV Aktivit"t von PBMC wurde mit Hilfe des HCV-Replikon-Systems untersucht. Die AnaIyse der IFN-g Produktion isolierter NK Zellen und der anti-HCV Aktivit"t erfolgte nach Koinkubation mit HCV-Replikonzellen in Kokultur mit bzw. ohne aktivierten CD 4+ T Zellen. Ergebnisse: Die Hemmung der HCV Replikation war bei PBMC von HIV Infizierten signifikant niedriger als bei gesunden Probanden (p < 0.001). Passend dazu war bei HIV Infizierten die IFN-g Produktion der NK Zellen signifikant gehemmt (p < 0.001). Interessanterweise korrelierte bei Therapienaiven HIV RNA(+) Patienten die CD 4+ T Zellzahl positiv mit der antiHCV Aktivit"t und IFN-g Produktion von NK Zellen, allerdings nicht bei HIV RNA(-) Patienten unter HAART (p < 0.5). Zudem war die vir"mische HIV Infektion im Vergleich zu gesunden Kontrollen und HIV RNA(-) Patienten mit einer verminderten IL2 Sezernierung von CD 4+ T Zellen assoziiert. In &bereinstimmung mit bisher von uns ver#ffentlichten Arbeiten induzieren aktivierte CD 4+ T Zellen effektiv die IFN-g Produktion von gesunden NK Zellen. Allerdings gab es zwischen CD 4+ T Zellen von HIV Patienten und Gesunden keine Unterschiede in der Stimulierbarkeit der NK Zellen gesunder Probanden. &berraschenderweise ließen sich NK Zellen von vir"mischen HIV Patienten weder durch autologe CD 4+ T Zellen noch von gesunden Kontrollen stimulieren. Das l"sst einen intrinsischen Defekt der NK Zellen vermuten. Diese dysregulierte Funktion wurde auch bei NK Zellen von therapierten HIV RNA(-) Patienten beobachtet. Diskussion: Unsere Daten deuten auf eine gest#rte Interaktion zwischen CD 4+ T Zellen und NK Zellen bei der HIV Infektion hin. Dies hat einen negativen Einfluss auf die anti-HCV Aktivit"t von NK Zellen und f!hrt m#glicherweise zur schnelleren Progression einer HCV assoziierten Lebererkrankung in der HIV Koinfektion. Korrespondierender Autor: Kr"mer, Benjamin E-Mail: m.benjamin.kraemer@gmail.com 5.22 Everolimus beeinflusst die HCV-Replikationsaktivit!t Frey A1, Ecker EM1, Piras-Straub K2, Walker A3, Hofmann T4, Gerken G1, Herzer K1 1 University Hospital of Essen, Department of Gastroenterology and Hepatology, Essen, Germany; 2 University Hospital of Essen, Department of General Surgery, Essen, Germany; 3Heinrich-Heine University Hospital, Institute of Virology, D!sseldorf, Germany; 4 German Cancer Research Center (DKFZ), Research Group Cellular Senescence, Heidelberg, Germany Hintergrund: Ein schwerwiegendes, medizinisches Problem nach erfolgreicher Hepatitis C (HCV) bedingter Lebertransplantation (LT) ist die HCV-Reinfektion des Transplantates. Neue antivirale Behandlungsm#glichkeiten geben Hoffnung auf Verbesserung von Verlauf und Prognose. Allerdings ist der Einfluss verschiedener Immunsuppressiva, insbesondere von mTor-Inhibitoren, auf die Virusreplikation noch nicht gekl"rt. Vorarbeiten legen eine Interferenz viraler Proteine mit dem Tumorsupressor PML nahe, dar!ber hinaus ist ein Zusammenhang des Kernproteins PML mit der mTor-Inhibitor-assoziierten Signaltransduktion beschrieben. Somit war der Einfluss des Immunsuppressivums Everolimus auf die HCV-Replikationsaktivit"t in vitro mit Fokus auf die Rolle von PML Gegenstand unserer Untersuchungen. Methoden: Verschiedene HCV-Replikon-Konstrukte wurden mit unterschiedlichen Immunsup- 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen pressiva (Tacrolimus, Everolimus) behandelt. Ein Einfluss der Therapeutika auf die Zellproliferation wurde sowohl mittels FACS-basierte CFSEZellproliferationsanalysen als auch MTT-Zellvitalit"tsanalysen ausgeschlossen. Um den Einfluss von PML auf die HCV-Replikationsaktivit"t zu untersuchen, wurden shRNA-Kontrukte zum Gene-Silencing von PML verwendet. Der Einfluss von Everolimus auf die PML-Expression wurde mittels qrt-PCR und Western Blot untersucht. Ergebnisse: mTor- bzw. Calcineurin-Inhibitoren wirken sich unterschiedlich auf die HCV-Replikationsaktivit"t aus. Bereits therapeutische Dosen des mTor-Inhibitors Everolimus vermindern die Replikationsaktivit"t des Genotypes 2a um 50 % (P £ 0,001), wohingegen die Replikationsaktivit"t des Genotypes 1b um mehr als 50 % gesteigert wird (P £ 0,001). Interessanterweise ist der Einfluss von Everolimus in PML-defizienten Replikon-Zellen deutlich weniger ausgepr"gt. Zudem ist die HCV-Replikationsaktivit"t genotypunabh"ngig in PML-defizienten Zellen bereits ohne Everolimus-Behandlung signifikant reduziert und kann durch Sublementierung der Zellen mit allen PML Splicevarianten wiederhergestellt werden. Gleichzeitig wird die PML-Expression durch Everolimus in Genotyp 2a, aber nicht in Genotyp 1b-Zellen reduziert. Schlussfolgerungen: Unsere Untersuchungen ergeben einen Zusammenhang zwischen der PML-Expression mit der mTor-basierten Reduktion der Replikationsaktivit"t, welche allerdings vom jeweiligen Genotyp abh"ngig ist. PML hat also m#glicherweise einen entscheideneden Einfluss auf die Virusreplikation. Dar!ber hinaus l"sst sich aus den Ergebnissen ableiten, dass die Wahl der immunsuppressiven Therapie nach HCV bedingter Lebertransplantation einen maßgeblichen Einfluss auf den Verlauf der HCV-Reinfektion haben kann. Korrespondierender Autor: Frey, Alexandra E-Mail: alexandra.frey@uk-essen.de 5.23 Female gender, age elder than 50 years and a reduced glomerular filtration rate (eGFR) at baseline strongly predict the frequency of anemia in patients undergoing boceprevir triple therapy in German real-life Teuber G1, Buggisch P2, L"hr H3, Steffens H4, Kraus M5, John C4, Geyer P7, Weber B8, Witth"ft T9, Herrmann A10, Hoesl M11, Naumann U12, Zehnter E13, Hartmann D14, Dreher B14, Bilzer M14 1 Gastroenterological Practice, Frankfurt, Germany; 2IFI Institute, Hamburg, Germany; 3Gastroenterological Practice, Wiesbaden, Germany; 4Practice of Internal Medicine, Berlin, Germany; 5Klinikum Burghausen, Burghausen, Germany; 6 Practice of Internal Medicine, Berlin, Germany; 7 Gastroenterological Practice, Fulda, Germany; 8Competence Center Addiction, Kassel, Germany; 9Gastroenterological Practice, Stade, Germany; 10Friedrich-Schiller-University, Jena, Germany; 11Gastroenterological Practice, Nuremberg, Germany; 12Center of Medicine, Berlin, Germany; 13 Gastroenterological Practice, Dortmund, Germany; 14MSD Pharma GmbH, Haar, Germany Background: Renal impairment together with a more pronounced anemia has recently been reported in about 5% of patients (pts) under triple therapy with boceprevir (BOC) or telaprevir (S Mauss et al., Hepatology 2014; 59:46 – 48). In the present interim analysis of the NOVUS observational study we investigated whether renal impairment at baseline or during treatment determines the frequency of anemia in patients undergoing BOC triple therapy. Methods: From April 2012 until January 2014, 536 pts with HCV G1 infection were recruited in the ongoing NOVUS study by 97 practices and hospitals in Germany. Pts were treated with pegylated interferons (PegIFN) and ribavirin (RBV) together with BOC for 24 to 44 weeks after a 4 weeks lead-in period with PegIFN/RBV. The present interim analysis was restricted to 292 pts with documented hemoglobin (Hb) and eGFR data from baseline until treatment week (TW) 12. eGFR (mL/min per 1.73 m2) was calculated with the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula. Anemia was defined as Hb < 10 g/dL. Results: The frequency of anemia at TW 12 was significantly higher in females (40.2 %, p < 0.0001) and pts elder than 50 years (34.9 %, p = 0.0107) when compared with males (17.6 %) and pts < 50 years (21.5 %). In addition, a baseline eGFR of 60 – 90, corresponding to renal insufficiency stage 2, was associated with a higher frequency of anemia. At TW12 46.2% of pts with baseline eGFR of 60 – 90 experienced anemia in contrast to only 20.3 % with baseline eGFR > 90 (p < 0.0001). Regarding baseline eGFR in more detail, 73% (212/ 292) of pts had an eGFR > 90, while 27% (80 / 292) showed an eGFR of 60 – 90. The latter occurred more frequent in female patients (33.6% vs. 23.6 %, p = 0.041) and elder patients > 50 years (46.2 % vs. 12.4 %, p < 0.0001). When eGFR remained > 90 from baseline until TW12 the frequency of anemia was 17.4 % while an eGFR decline from > 90 to < 90 until TW12 was associated with a trend towards a higher rate of anemia (27.1%), but the difference did not reach significance (p = 0.116). No influence on the frequency of anemia was observed in pts who had an eGFR decline from 60 – 90 to < 60 (53.8 %) in comparison to pts with stable eGFR of 60 – 90 from baseline until TW12 (53.3 %, p = 0.973). Conclusions: The present interim analysis of the NOVUS study demonstrates a higher frequency of anemia in female pts as well as in pts elder than 50 years. Furthermore, there is a strong association between renal function at baseline and the frequency of anemia caused by BOC triple therapy. As a consequence RBV dose reductions should be considered in pts with impaired renal function. Corresponding author: Bilzer, Manfred E-Mail: manfred.bilzer@bilzer-consulting.de 5.24 HBsAg-specific humoral and cellular immune memory after hepatitis B booster vaccination in adolescents 10 – 15 years after immunization in infancy Brunskole Hummel I1, Zitzmann A1, Wenzel JJ1, Jilg W1 Universit$t Regensburg, Institute of Medical Microbiology and Hygiene, Regensburg, Germany 1 Up to 50 % of individuals lose protecting antibodies within 10 to 15 years after primary vaccination against hepatitis B. However, the presence of immune memory should protect these individuals against hepatitis B disease. To analyze the quality of HBsAg-specific immune memory we studied the kinetics of humoral and cellular immune responses after a booster dose of hepatitis B vaccine in adolescents with anti-HBs below 10 IU/l. Adolescents 14 to 18 years old were tested for anti-HBs 10 to 15 years after infant immunization. Individuals with anti-HBs concentrations below 10 IU/l were offered a booster dose and the analysis of humoral and cellular responses followed at day 0, 3, 7, 14 and 28 after revaccination. Of the 77 study participants, 67,5% showed anti-HBs levels ‡ 10 IU/l and 32,5 % had anti-HBs < 10 IU/l. 23 of the latter were revaccinated. Cellular immune responses were analyzed by measuring the HBsAg-specific IL5- and IFNg-secreting cells in enriched CD 4+ peripheral blood mononuclear cells. Considering both, anti-HBs and cellular responses, four booster patterns have been observed: no or extremely week anti-HBs and cellular response (3 out of 19 subjects), only anti-HBs response (10 subjects), strong anti-HBs and cellular response (4 subjects) and high intrinsic production of IL5 (2 subjects). In conclusion, our data indicate that with the available techniques humoral response is the dominant immune response after hepatitis B revaccination in adolescents. Corresponding author: Brunskole Hummel, Irena E-Mail: irena.hummel@ukr.de 5.25 Hepatitis C Virus activates auto- and paracrine circuits to modify surface expression of growth factor receptors of the Erb family Eisenb!rger S1, Bartenschlager R2, H$ussinger D1, Bode JG1 1 Heinrich Heine University D!sseldorf, Gastroenterology, Hepatology and Infectious Diseases, Duesseldorf, Germany; 2 University Hospital of Heidelberg, Department of Infectious Diseases, Molecular Virology, Heidelberg, Germany Background: To establish a persistent infection HCV must have evolved strategies allowing high viral replication without induction of effective antiviral immunity and without affecting viability of its host cell. Recently, the EGF receptor and EGFR dependent signalling have been identified as co-factor for HCV entry and replication. In how far HCV interferes with the expression of the EGF receptor family is unknown and has been investigated in the present study. Methods: Huh7 cells either infected with the HCVcc strain JC1 or harbouring the HCV subgenomic replicon were used and analysed employing targeted gene knockdown by siRNA, RT-PCR, Immunoblot- and FACS-analysis. Results: The present study demonstrates that HCV causes an NRG1- and Akt-dependent down-regulation of the ErbB3 receptor, while NRG1 expression is enhanced by HCV in a Sp1- and probably also p38MAPK-dependent manner. Decreased ErbB3 surface expression is accompanied by an enhanced expression of other EGFR family members at the cell surface. Knockdown experiments provide evidence that decreased ErbB3 surface expression by HCV is responsible for observed up-regulation of the EGFR Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A61 A62 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen and ErbB2 surface expression in cells that harbour HCV. First experiments provide further evidence that enhanced EGFR expression at the cell surface results in an improved viral replication. Discussion: The data presented suggest that, apart from utilizing EGFR and EGFR-dependent signal-transduction, HCV substantially influences surface expression of EGF receptor family members on the infected cell. This involves down-regulation of ErbB3 expression via an Nrg1-mediated auto- or paracrine loop. The subsequent up-regulation of EGFR and ErbB2 is paralleled by an increased viral replication suggesting that the HCV-induced alterations of the surface expression of the different EGFR family members and improved replication are functionally linked. Corresponding author: Bode, Johannes G. E-Mail: Johannes.Bode@med.uni-duesseldorf.de 5.26 Hepatitis Delta Virus can persist and propagate through human cell division both in vitro and in vivo Bhadra OD1, Giersch K1, Volz T1, Allweiss L1, Lohse AW1, Sureau C3, Petersen J4, Dandri M1, L!tgehetmann M5 1 University Hospital Hamburg-Eppendorf, I. Department of Internal Medicine, Hamburg, Germany; 2German Center for Infection Research (DZIF), Hamburg-L!beck-Borstel Partner Site, Hamburg-L!beck, Germany; 3INTS, Centre National de la Recherche Scientifique, Laboratoire de Virologie Moleculaire, Paris, France; 4Asklepios Klinik St. Georg, Hamburg, Germany; 5University Hospital HamburgEppendorf, Institute of Microbiology, Virology and Hygiene, Hamburg, Germany Intrahepatic latency of the Delta antigen (HDAg) has been determined even months after liver transplantation and we recently showed that a latent HDV mono-infection can persist in humanized mice for at least 6 weeks in the absence of HBV before being converted to a productive HBV/HDV infection (Giersch et al. J. Hepatology 2014). Although these studies highlight the ability of HDV to persist in quiescent hepatocytes, little is known about the impact of cell proliferation on HDV persistence. Aim of the study was to evaluate the ability of HDV to survive human hepatocyte proliferation in vivo using HBV/HDV infected human liver chimeric uPA/SCID/beige mice and in vitro using NTCP-transduced hepatoma cell lines infected with HDV virions. Methods: In vivo proliferation of primary human hepatocytes (PHHs) was triggered by serially transplanting PHHs isolated from HBV/HDV infected humanized mice into na+ve recipient mice. NTCP-transduced HepG2 cells, infected with either mouse-derived or cell culture-derived HDV, were passaged (1:2 dilutions) and analysed every 5 days for a period of 40 days. Virological parameters were determined by qRT-PCR. Presence of HDAg, HBcAg and cell proliferation (Ki67) was determined in vivo and in vitro by immunofluorescence. Results: In vivo expansion of PHHs isolated from HBV/ HDV infected humanized mice was confirmed 2, 4 and 8 weeks after transplantation by human CK18 and Ki67 staining. Similarly to results obtained with HBV mono-infected proliferating PHHs, HBcAg-pos. cell amounts and HBV viremia rapidly dropped in proliferating HBV/HDV coinfected PHHs. However, despite the absence of detectable HDV viremia at week 4 and 8 after transplantation, HDAg-positive PHHs were detected at each observation time point and often formed clusters of adjacent HDAg-positive PHHs, suggesting maintenance of HDV infection among the dividing human hepatocytes. Presence of Ki67-HDAg costaining and appearance of clusters of HDV-positive cells were also observed in vitro after 7 serial cell passages (1:128 total cell dilutions). Notably, comparable amounts of HDAg-positive cells were detected at the beginning and the end of the study (ca. 3%/plate). Conclusions: Our in vitro and in vivo findings suggest that by surviving hepatocyte proliferation, HDV may not only persist but even be able to propagate, at least to some extent, among daughter cells, despite the absence of HBV. Corresponding author: Bhadra, Oliver D. E-Mail: oliver.bhadra@live.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York Histopathology of chronic Hepatitis E 5.27 Beer A1, Holzmann H2, Pischke S3, Behrendt P4, Wrba F1, Schlue J4, Drebber U5, Halilbasic E6, Kreipe H4, Lohse A3, Sterneck M3, Wedemeyer H4, Manns M4, Dienes HP1 1 University of Vienna, Institute of Pathology, Vienna, Austria; 2Medical University of Vienna, Institute of Virology, Vienna, Austria; 3University Hospital Hamburg-Eppendorf, Hamburg, Germany; 4Hannover Medical School (MHH), Hannover, Germany; 5University of Cologne, Institute of Pathology, Cologne, Germany; 6Medical University of Vienna, Department of Gastroenterology, Vienna, Austria Background and aims: Sporadic hepatitis E is an emerging indigenous disease in Europe induced by the genotype 3 of the virus. Whereas in immunocompetent individuals it takes an acute self-limited course, under immunocompromised conditions the majority of cases develop chronic hepatitis. Histopathology of acute hepatitis has been published whereas histology of chronic hepatitis has noit been described so far. Methods: We collected liver biopsies from 19 patients (17 male, 2 female; age 10 – 66 years)who had undergone solid organ transplantation (5 liver, 6 kidney, 4 lungs, 4 heart). One HIV-negative patient had CD4 lymphocyte impairment. Biopsies were stained with H&E,van Gieson, Prussian Blue and PASD. Evaluation of histologic activity and fibrosis was performed by applying the Ishak score. Results: Biochemical data showed a considerable increase with ALT mean levels 479 U/L (25 – 2574), AST mean 244 U/L (35 – 1211), gGT 152 (26 – 362), bilirubin 5 mg/dl(06 – 31). Histopathology displayed typical features of chronic hepatitis of mild to moderate activity (HAI of 9 and mild fibrosis stage 2). In 2 biopsies a conspicuous central vein sclerosis and perisinusoidal fibrosis was present that first mislead to the diagnosis of chronic NASH. The number of PMN leukocytes was considerably increased and all patients had a florid cholangitis that showed a destructive form in 8. Conclusions: Chronic hepatitis E runs a similar course as hepatitis B and C and shows a similar histopathology. However the presence of a sometimes destructive cholangitis and the considerably increased number of PMN leukocytes is markedly different from chronic hepatitis B and C. Corresponding author: Beer, Andrea E-Mail: hp.dienes@gmail.com 5.28 Identification of CD 8+ T-cell epitopes specific for hepatitis C virus genotype 4 Luxenburger H1, Graß F1, B$rmann J1, Nitschke K1, Thimme R1, Neumann-Haefelin C1 1 University Hospital of Freiburg, Department of Medicine II, Freiburg, Germany Virus-specific CD 8+ T-cell responses play an important role in the outcome of hepatitis C virus (HCV) infection. Thus, the identification of CD 8+ T-cell epitopes is essential for the development of successful vaccination strategies against HCV. To date, most HCV-specific CD 8+ T-cell epitopes have been defined in HCV genotype 1 infection. However, in the countries with the highest prevalence of HCV infection, such as Egypt, most patients are infected with HCV genotype 4. Currently, no HCV genotype 4 specific CD 8+ T-cell epitopes have been identified. In this study, we analyzed patients chronically infected with genotype 4 (17 patients) or genotype 1 (20 patients) using a set of 93 well described genotype 1 specific epitope peptides. We were able to detect CD 8+ T-cell responses in the majority of genotype 1 infected patients. However, no CD 8+ T-cell responses were observed in patients infected with genotype 4. Next, we analyzed genotype 4 infected patients using overlapping peptides spanning the whole HCV genotype 4 proteome as well as epitope candidates predicted using an in silico approach. By this method, we were able to identify six novel CD 8+ T-cell epitopes in genotype 4 infection. In conclusion, we were able to identify the six first HCV genotype 4 specific CD 8+ T-cell epitopes. In contrast, epitopes previously identified in HCV genotype 1 infection were not targeted in patients infected by HCV genotype 4. These results further indicate that despite the similarity of HCV genotypes 1 and 4 in antiviral therapy, T-cell based vaccines need to be adapted to the respective genotype. Corresponding author: Nitschke, Katja E-Mail: katja.nitschke@uniklinik-freiburg.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 5.29 Identification of critical intersections points for M1 and M2 differentiation of macrophages by a systems biology approach Albrecht U1, Sanwald J2, Thomas M3, Sawodny O2, Zanger U3, Ederer M2, Feuer R2, H$ussinger D1, Bode JG1 1 Heinrich Heine Heinrich-Heine University Hospital, Clinic for Gastroenterology, Hepatology and Infectious Diseases, Duesseldorf, Germany; 2Universit$t Stuttgart, Institute for System Dynamics, Stuttgart, Germany; 3Universit$t Stuttgart, Dr. Margarete Fischer-Bosch Institute of Clinical Pharmacology, Stuttgart, Germany Objectives: Macrophages are cells with remarkable plasticity. They are able to integrate signals from their microenvironment leading to context dependent differentiation into classically activated macrophages (M1) or alternatively activated macrophages (M2). Within the liver, macrophages are known to mediate important hepatoprotective and pro-regenerative effects but may also be responsible for impaired hepatocyte function and liver injury in response to microbial pathogens. The mechanisms responsible for this controversial role of liver macrophages are still incompletely understood. Methods and Results: Within the Virtual Liver Network (VLN), we applied a systems biology approach for the identification of the differentiation specific, macrophage derived key mediator pattern that may cause these distinct effects. Therefore, a comprehensive literature-based Boolean model was developed in order to describe the activation of macrophages into the M1 phenotype following stimulation with LPS (lipopolysaccharide) and into the M2 phenotype in response to stimulation with the interleukins IL-4 and IL-13. This logical model is validated and refined using high-throughput transcript expression data from bone marrow derived macrophages (BMDM) and suggests that the PI3K and the NFkB pathway may play a critical role as a switch regulating differentiation into the M1 or M2 direction. Conclusion: A Boolean model of the regulatory pathways controlling macrophage differentiation into the M1 or the M2 direction has been established and validated to identify critical intersections points that act as a molecular switch between M1 and M2 differentiation. First simulations suggest that the NFkB and the PI3K pathway may play a role as a molecular switch. This observation may be important for an in depth understanding of processes that drive the hepatic acute phase response or liver regeneration. Corresponding author: Albrecht, Ute E-Mail: Ute.Albrecht@hhu.de 5.30 Impact of genetic polymorphisms in the SCARB1 gene on hepatitis C virus Deest M1, Westhaus S1, Stanke F3, Manns MP1, Berg T4, Sarrazin C2, Ciesek S1, Hahn T von1 1 Hannover Medical School (MHH), Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany; 2Goethe University Hospital, Internal Medicine I, Frankfurt am Main, Germany; 3Hannover Medical School (MHH), Department of Pediatric Pneumology and Neonatology, Hannover, Germany; 4University Hospital of Leipzig, Department of Hepatology, Leipzig, Germany Background: The scavenger receptor type B class I (SR-BI) is the physiological receptor for high density lipoproteins (HDL) on hepatocytes and the primary specific attachment receptor for hepatitis C virus (HCV). Numerous single-nucleotide polymorphisms (SNPs) have been described in the SCARB1 gene encoding SR-BI. Some of these are known to have a phenotype in the form of altered serum lipids, but their impact on HCV infection is unknown. Methods: We aimed to investigate SCARB1 SNPs with a high likelihood to affect HCV biology. All known SNPs that result in an amino acid exchange in the SR-BI protein (5 SNPs) were subjected to in vitro assays testing their ability to function as HCV receptors in SR-BI knockdown cell lines and the capability of binding soluble E2. Another four non-coding SNPs that have an allele minor frequency of > 10 % and had been reported to be associated with a phenotype in humans were investigated in genetic association studies performing single marker and haplotype analyses in a cohort of (n= 262) chronically HCV infected patients of the INDIV-2 study. Results: In the genetic association part of the study we found the A allele of the rs3782287 variant to be associated with higher HCV RNA levels in chronically HCV individuals. Moreover we found an association of the G allele of the rs1084674 variant with higher response rates to dual therapy with interferon and ribavirin. These results have been confirmed by haplotype analysis and we were able to identify haplotype blocks which could predict treatment outcome and viral load. Among the five coding SNPs, we observed comparable infectivity to human SR-BI in SRBI knockdown cells and NIH3T3 cells expressing the non-synonymous SNPs G2S, V135I or P297S but not S 112F or T175A. Soluble E2 binding is detectable in cells expression human SR-BI as well as SR-BI SNPs G2S, V135I and P297S but not mouse SR-BI and SR-BI S 112F or T175A. Currently we are evaluating our results in cell lines lacking SR-BI expression by knockdown due to a CRISPR/Cas system. Conclusion: Host genetic variation in SCARB1 may affect HCV replication in several ways: noncoding variants seem to modulate the clinical course of HCV infection by affecting the viral load and treatment response. The rare coding variants S 112F or T175A result in decreased HCV cell entry. Corresponding author: Deest, Maximilian E-Mail: mail@deest.net 5.31 Increased expression of CD39 on natural killer cells in patients with chronic hepatitis C is associated with an immature phenotype Dierks P1, Eberhard JM1, Schulze zur Wiesch J1 1 University Hospital Hamburg-Eppendorf, I. Department of Internal Medicine, Hamburg, Germany Natural killer (NK) cell function has been shown to be crucial in the innate immune response against chronic viral infections such as hepatitis C (HCV) and HIV. The Regulation of NK cells is not dominated by a single receptor as in B or T cells, but the result of an orchestrated interplay of a variety of activating and inhibitory molecules such as C-type lectin and killer cell immunoglobulin receptors. CD39 is an ectonucleotidase which is known for its ability to degrade ATP to AMP and in connection with CD73 to adenosine. Recent findings in chronic viral infections and especially in the liver revealed the importance of this modulatory pathway for dysfunctional CD 8+ and regulatory T cell responses. The aim of this study is to investigate the distribution and expression level of CD39 on different NK cell populations derived from peripheral blood. To furthermore reveal its role in chronic infections such as HIV and HCV, we compared PBMC samples from HCV monoinfected, HCV/HIV co-infected and HIV mono-infected patients to healthy controls. In a multicolor flow cytometry panel NK cell subsets were characterized by their expression of CD56 and CD 16 (otherwise lineage negative) and were analyzed for expression of KIR2D, KIR3DL 1/ DL2 and CD57 as well as the ectonucleotidases CD39 and CD 73. Overall, the frequency of CD 39-positive CD 3-CD 56+ NK cells was significantly increased in patients with HCV (Mean 8.86 % € 6.43), HCV/HIV (Mean 14.63 % € 10.51) and HIV infection (Mean 23.39 % € 12.22) compared to healthy controls (Mean HC 4.35% € 3.67, HC vs. HCV p = 0.0097; HC vs. HCV/HIV p = 0.0076; HC vs. HIV p = 0.0041). Furthermore, the CD 3CD 56brightCD 16 € NK cell subset shows a relatively higher frequency of CD 39-positive cells compared to the CD 3-CD 56dimCD 16 € NK cell subset within all groups (e.g. HCV Mean: 24.95% € 11.43 (CD 56bright NK) vs. 5.73 % € 5.65 (CD 56dim NK), p < 0.0001). Next, we hypothesized that expression of CD39 might be associated with NK cell differentiation. We compared its expression on CD 56bright, CD 56dimpanKIR-CD57and CD 56dimpanKIR+CD 57+ NK cells subsets representative for a previously described maturation pathway. We observed the highest frequency of CD 39-positive cells in CD 56bright NK cells, followed by a stepwise decline in frequency from CD 56dim panKIR-CD57- NK cells to CD 56dimpanKIR+CD 57+ NK cells within all groups (e.g. HCV Mean: From 26.33% € 11.85 over 14.22 % € 8.09 to 2.20 % € 3.26; CD 56bright vs. CD 56dimpanKIR-CD57- p = 0.01; CD 56bright vs. CD 56dimpanKIR+CD 57+ p < 0.0001). Our data provides evidence that the frequency of CD 39-positive NK cells is increased in chronic viral infections like HCV and HIV. The distribution of CD 39-positive NK cells shows an association with NK cell maturation. Taken together these results indicate a differentiation-associated skewing of the modulatory function of NK cells mediated via CD39 expression in HCV and HIV compared to healthy controls. Corresponding author: Dierks, Patrick E-Mail: pdierks@pdierks.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A63 A64 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 5.32 Infizierbarkeit der Hepatom-Zelllinie HepaRG durch HBV+ Seren mit niedrigem bis hohem Virustiter K!hne C1, Dammermann W1, Heinzel K1, Schulze zur Wiesch J1, L!th S1 1 University Hospital Hamburg-Eppendorf, I. Department of Internal Medicine, Hamburg, Germany Hintergr!nde und Ziele: Die humane Hepatom-Zelllinie HepaRG wurde von der Gruppe um Gripon et al. 2002 erfolgreich als erste mit Hepatitis B-Viren (HBV) in vitro infizierbare Zelllinie eingef!hrt. Bis dahin dienten stabil mit HBV-&berl"ngengenomen transfizierte Hepatom-Zelllinien wie HepG2.2.15 als Werkzeug zur Untersuchung der HBV-Replikation. Eine Untersuchung der Infizierbarkeit dieser Zelllinie mit HBV+ humanen Patientenseren in Abh"ngigkeit vom z.B. HBV-Titer fehlt jedoch bis heute. Das Ziel dieser Studie war es daher, die technischen Spezifikationen dieses infekti#sen Zellkultursystems in Abh"ngigkeit unterschiedlicher HBV+ Patientenseren zu untersuchen. Methoden: HepaRG-Zellen wurden mit HBV+ Seren chronischer Hepatitis B-Patienten infiziert, deren Virustiter zwischen 1*104 und 1*1011 U/l lag. Hierf!r diente das Protokoll von Gripon et al. als Goldstandard. Parallel wurden unterschiedliche technische Spezifikationen des Protokolls variiert, u.a. f!r die Reagenzien Polyethylenglycol 8000 (PEG8000) oder Dimethylsulfoxid (DMSO). Zur &berpr!fung einer erfolgreichen HBV-Infektion dienten PCR, quantitative RTD-PCR sowie ein quantitativer HBsAg-ELISA. Ergebnisse: Humane Seren mit hohem HBV-Titer (> 1*109 U/l) waren am besten geeignet f!r eine stabile Infektion der HepaRG-Zellen. Seren mit mittlerem Titer (1*105 U/l – 1*109 U/l) ben#tigten PEG8000 f!r eine erfolgreiche Infektion. Somit war PEG anders als von Gripon et al. beschrieben nicht immer notwendig f!r die Infizierbarkeit der HepaRGZellen. Im Falle hochtitriger Seren erh#hte es aber den Anteil infizierter Zellen deutlich, was sich in einem u.a. dreimal h#heren HBsAg-Titer im Zellkultur!berstand niederschlug. Niedrigtitrige Seren (< 1*105 U/l) eigneten sich nicht f!r eine Infektion. Es erwies sich auch DMSO in der von Gripon et al. empfohlenen Konzentration von 2% (v/v) im Zellkulturmedium in Langzeitversuchen > 48 h als toxisch f!r HepaRG-Zellen. Zusammenfassung: Die HepaRG-Zelllinie stellt ein ausgezeichnetes Mittel zur Untersuchung der HBV-Replikation in vitro dar. Gleichzeitig ist beim Einsatz HBV+ Patientenseren mit variablem Virustiter als Inokulum im Gegensatz zu hochtitrigen HBV+ Zellkultur!berst"nden eine genaue Kenntnis der Wirksamkeit einzelner Reagenzien des Gripon et al.-Protokolls von Vorteil f!r den Endanwender. Korrespondierender Autor: Dammermann, Werner E-Mail: w.dammermann@uke.de 5.33 Influence of HCV on CREB gene expression and functional relevance Rohr M1, Eisenb!rger S1, Bartenschlager R2, H$ussinger D1, Bode JG1 1 Heinrich Heine University D!sseldorf, Department of Gastroenterology, Hepatology and Infectious Diseases, Duesseldorf, Germany; 2University of Heidelberg, Department of Infectious Diseases, Molecular Virology, Heidelberg, Germany The Hepatitis C Virus is one of the leading causes of chronic liver diseases. In more than 70% HCV establishes a persistent infection. The high rate of persistency as well as the creeping course of disease, taking decades until development of overt disease, indicates that the virus must have evolved mechanisms to circumvent the antiviral host response and to modify inflammation. Moreover persistent viral replication requires the ability to utilize the infrastructure of the host cell for viral life cycle without significantly influencing its viability. The present project aims to investigate molecular mechanisms by which HCV interferes with the regulation of cellular apoptosis and proliferation. Evidence is provided that in the presence of the sub-genomic HCV replicon expression of ATF2 is increased at the level of mRNA and protein. Correspondingly, increased transcript expression of ATF2 was also observable in liver tissue derived from patients chronically infected with HCV. Knockdown of ATF2 using specific siRNA results in an increased induction of Poly(ADP-ribose)-Polymerase (PARP) cleavage upon treatment with Actinomycin D/TNF alpha suggesting that ATF2 prevents HCV-infected cells from undergoing apoptosis upon exposure to respective challenges. Consistently ATF2 down-regulates the HCV-induced expression of pro-apoptotic genes, such as p53 up-regulated modulator of apoptosis (Puma) or Peroxisome proliferator-activated receptor gamma (PPARg). The inhibition of the expression of these genes may contribute Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York to transform infected cells in a stage which is less susceptible to proapoptotic stimuli. In summary these data suggest that HCV up-regulates ATF2 expression to counteract pro-apoptotic signals thereby balancing the increased vulnerability of the infected cell towards pro-apoptotic challenges which results from on-going viral replication. Corresponding author: Bode, Johannes Georg E-Mail: Johannes.Bode@med.uni-duesseldorf.de 5.34 Interruption of nucleos(t)ide analogue therapy in HBeAg negative chronic hepatitis B – A new concept to achieve HBsAg decline? H"ner zu Siederdissen C1, Deterding K1, Port K1, Maasoumy B1, Markova AA1, Michael MP1, Wedemeyer H1, Cornberg M1 1 Hannover Medical School (MHH), Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany Background: Effective suppression of HBV DNA with nucleoside or nucleotide analogues (NA) has shown to delay disease progression in patients with chronic hepatitis B. However, HBsAg loss during NA treatment is a rare event. Thus, treatment duration with NA is not finite and stopping rules before HBsAg loss are not clearly defined, especially in HBeAg negative patients. Methods: We prospectively stopped NA treatment in patients with HBeAg negative chronic hepatitis B. Inclusion criteria were ongoing antiviral treatment with NA and suppressed HBV DNA < 20 IU/ml for at least 3 years as well as HBsAg < 3500 IU/ml. Patients with co-infection, other concomitant liver disease, liver cirrhosis and immunosuppressive therapy were excluded. All patients had a treatment indication for antiviral treatment at the time point of NA initiation. Study visits were scheduled at baseline and at week 4,8,12 and every 12 weeks thereafter. On every visit the patients were assessed for virological relapse, defined by HBV-DNA > 2000 IU/ml. Quantitative HBsAg levels one year before and after treatment cessation were compared to assess differences in HBsAg levels. Results: Data are available for 13 patients with one year follow-up. Virological relapse after treatment cessation was detected in 4 patients (31%) at week 4, in 7 patients (54%) at week 8 and in 1 patient at week 24. No virological relapse occurred in 1 patient. Two patients developed an ALT flare > 5 ULN. No patient experienced signs of liver failure or significant increase of bilirubin. In 11/ 12 patients with virological relapse treatment was re-initiated with either entecavir or tenofovir and HBV-DNA was successfully suppressed at week 48 follow-up. HBsAg levels showed no significant decline in the year before cessation of NA treatment (1206 € 1123 IU/ml vs 1232 € 999 IU/ml, p = 0.86). However, treatment cessation resulted in a significant decline in mean HBsAg levels from baseline to 48 week follow-up (1232 € 999 IU/ml vs 760 € 709 IU/ml, p = 0.0012). Interestingly, both patients with ALT flares > 5 ULN showed a decline of HBsAg levels > 2 log from baseline to week 48 follow-up. Conclusion: Treatment cessation in HBeAg negative chronic hepatitis B is safe but leads to virological relapse in > 90 % of patients until week 24. However, treatment cessation led to a significant decline in HBsAg levels with the strongest decline observed in patients with ALT flare > 5 ULN. Thus interrupting NA treatment and inducing ALT flares should be further investigated as an option to facilitate HBsAg loss. Corresponding author: H#ner zu Siederdissen, Christoph E-Mail: HoenerzuSiederdissen.Christoph@mh-hannover.de 5.35 Kinetic of Hepatitis B core-related antigen (HBcrAg) levels in chronic hepatitis B during NUC therapy Maasoumy B1, Jaroszewicz J2, Deterding K1, Lehmann P1, Bremer B1, Manns MP1, Wedemeyer H1, Cornberg M1 1 Hannover Medical School (MHH), Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany; 2Medical University of Bialystok, Department of Infectious Diseases and Hepatology, Bialystok, Poland Introduction: Hepatitis B core-related antigen (HBcrAg) combines the antigenic reactivity of denatured HBeAg, HBcAg and the core-related protein p22cr. HBcrAg has been introduced as additional marker of HBV infection. High levels of HBcrAg were an independent risk factor for HCC in a large Japanese cohort, while low levels may indicate inactive carrier status. We here aimed to analyze HBcrAg levels during treatment with nucleos(t)ide analogues (NIC) in a European cohort. Methods: We included 57 patients with chronic Hepatitis B that were pre- 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen viously either untreated or treated ineffectively. All patients started a new NUC therapy at the beginning of our observation period. Majority of patients received either entecavir (43%) or tenofovir (23 %). We measured various markers of HBV infection (including HBsAg, HBV DNA and HBcrAg) at baseline, 6, 12, 24, 36, 48, 60 and 72 months (m) after treatment initiation (median follow-up 60 m). Results: There was a rapid decline in HBV DNA levels from median 5.4 log10 IU/ml at baseline to 1.36 log10 IU/ml after only 6 m of treatment and < 1.3 log10 IU/ml (below the limit of quantification) after 12 m. In contrast, HBcrAg levels showed a slower but continuous decline starting from a median level of 2.26 to 1.98, 1.04, 0.57 and -0.12 log10 kU/ml after 6, 12, 48 and 72 m, respectively. There was only a minimal decline in HBsAg levels (median 3.77, 3.52 and 3.18 log10 IU/ml at baseline, 12 m and 72 m, respectively). At the end of follow up 44% of patients were HBV DNA negative, while 89 % still had detectable HBcrAg levels. We documented a high correlation between HBcrAg levels and HBV DNA (Spearman correlation: r= 0.78; p < 0.0001) at baseline, which decreased at later stages of therapy (correlation at last follow-up: r= 0.37; p = 0.035). In contrast, there was a consistent moderate correlation between HBcrAg and HBsAg levels at baseline (r= 0.47; p = 0.0003) as well as at the last follow-up (r= 0.53; p < 0.0001). We found an association of baseline HBcrAg levels with clinical endpoints. Patients with a baseline HBcrAg level < 100 kU/ ml experienced HBsAg loss or at least a decline to < 100 IU/ml in 19 % of cases (n= 5/ 27), while this occurred in none of the 30 patients with a HBcrAg level ‡100 kU/ml. Similarly, all 3 HBeAg positive patients with a baseline HBcrAg level < 2000 kU/ml achieved HBeAg seroconversion, while this only happened in 20 % (n= 3/ 15) of patients with levels ‡2000 kU/ml. Conclusion: HBcrAg shows different kinetics than HBV DNA and HBsAg during antiviral therapy with nucleotide analogues. Low HBcrAg may help to identify patients with a higher chance of HBeAg and HBsAg clearance. Thus HBcrAg should be further investigated, as it may be an interesting marker in patients undergoing NUC therapy. Corresponding author: Maasoumy, Benjamin E-Mail: maasoumy.benjamin@mh-hannover.de 5.36 Large scale biomarker profiling reveals distinct cytokine and chemokine signatures distinguishing different acute and chronic hepatitis virus infections Hardtke S1, Hengst J1, Deterding K1, Falk C2, Manns MP1, Cornberg M1, Wedemeyer H1, Schlaphoff V1 1 Hannover Medical School (MHH), Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany; 2Hannover Medical School (MHH), Institute of Transplant Immunology, IFB-Tx, Hannover, Germany Infections with hepatotropic viruses can cause acute and chronic hepatitis. The detailed immuno-pathophysiological events leading to inflammation and fibrosis progression are not well understood. In order to investigate the effects of different hepatitis viruses on systemic cytokine and chemokine expression, we performed a large scale multianalyte profiling of samples from 163 individuals with acute hepatitis (12 acute HAV, 5 acute HBV, 21 acute HCV) or chronic viral hepatitis (12 HBV, 14 HBV/HDV coinfection, 51 HCV). In addition, 25 subjects who had recovered from acute hepatitis C and 22 healthy controls were studied. 50 serum cytokine, chemokines and angiogenic factors were studied using multiplex technology (Bio-Plex System). Moreover, various clinical parameters were included in the statistical analysis including viral load, ALT,AST, gamma GT and blood counts. Principal component analysis (PCA) was performed by ANOVA/t-test testing using Qlucore Omics Explorer software(Qlucore Lund, Sweden). Results: Profiling revealed distinct signatures by of 31 markers differentiating acute hepatitis from healthy controls as well as chronic hepatitis patients from controls (32 parameters). Similarly, acute and chronic infections could be separated by biomarkers (9 parameters). Interestingly, signatures differed for distinct viruses as HAV infections caused a much more upregulation of various pro-inflammatory cytokines as compared to acute hepatitis C. In contrast, chronic hepatitis C was associated with a broad upregulation of various cytokines and chemokines including IP-10, IL-18, IL12, SDF-1a, and VCAM-1 compared to chronic hepatitis B patients while RANTES (CCL5) appears as the only cytokine/chemokine upregulated in HBV and HBV/HDV. No significant markers could be identified to differentiate between HBV monoinfection and hepatitis delta. Interestingly both groups showed a cluster of markers which are clearly less expressed compared to controls including IL-2RA,IL-3,IL-5, IL-15, IL-17 and G-CFS. Discussion: Acute and chronic liver inflammation is characterized by distinct cytokine signatures which differ between different hepatitis viruses. This large-scale profiling reveals novel insights in the immunopathogenesis and host pathogen interactions. Corresponding author: Hardtke, Svenja E-Mail: hardtke.svenja@mh-hannover.de 5.37 Liver inflammation abrogates T cell mediated tolerance against particulate antigens induced by liver Kupffer cells Heymann F1, Peusquens J1, Ludwig-Portugall I2, Kohlhepp M1, Ergen C1, Niemietz P1, Martin C3, van Roojen N4, Ochando J5, Randolph G6, Luedde T1, Ginhoux F7, Kurts C2, Trautwein C1, Tacke F1 1 University Hospital of Aachen, Medical Clinic III, Aachen, Germany; 2University Hospital of Bonn, Institute for Experimental Immunology, Bonn, Germany; 3University Hospital of Aachen, Department of Pharmacology, Aachen, Germany; 4Universiteit van Amsterdam, Department of Molecular Cell Biology, Amsterdam, Netherlands; 5Mt. Sinai School of Medicine, Department of Nephrology, New York, USA; 6University of St.Louis, Division of Immunobiology, St. Louis, USA; 7SIgN, A*Star, Singapore, Singapore Background and Aims: Liver Kupffer cells are key players in the upkeep of body homeostasis, ingesting apoptotic material, gut derived microbiota and particulate antigens from the circulation. We investigated the immunoregulatory capacities of liver phagocytes in healthy and inflamed conditions against particle bound antigens addressing T cell mediated immune tolerance. Methods: 0.5 mm fluorescent latex (Lx) particles were covalently linked to ovalbumin (OVA) and injected i.v. into recipient mice. Particle distribution was investigated in CX3CR1.eGFP and wildtype animals by flow cytometry and multiphoton microscopy (TPLSM). Tolerance induction was measured by activation of regulatory T cells (Treg) and inhibition of OVA-specific CTL mediated target cell lysis. Interactions between Lx+ phagocytes and T cells were followed using intravital TPLSM in liver. To investigate the role of the liver micromilieu, mice were chronically injured with carbon tetrachloride (CCl4) i.p. or methionine choline-deficient (MCD) diet prior to tolerance induction for several weeks to induce liver injury and inflammation. Results: Peptide antigens associated with particles were phagocytized and processed by Kupffer cells, leading to interactions of Kupffer cells with circulating T cells in liver, expansion and functional activation of natural occurring Foxp3+CD 25+ IL 10-producing regulatory T cells (Treg). Particle-associated antigen delivery to Kupffer cells protected mice from kidney inflammation in a model of T cell-mediated glomerulonephritis. On the contrary, tolerogenic immune responses could not be established, if particulate antigens were encountered within inflamed liver induced by toxic or metabolic liver injury. Upon hepatic inflammation, monocyte-derived macrophages largely augmented the hepatic phagocyte compartment and antigens redistributed between myeloid cell populations. Conclusions: Kupffer cells are the main cell population responsible for induction and maintenance of immunological tolerance against particle-associated antigens under homeostatic conditions in vivo. However, tolerance could not be established under inflammatory conditions, showing that liver injury severely imbalances the body-wide mechanisms for tolerance induction and upkeep. Corresponding author: Heymann, Felix E-Mail: fheymann@ukaachen.de 5.38 Liver sinusoidal endothelial cells and Kupffer cells contribute to HCV innate immune response via TLR3 Cheng X1, Boxtermann M1, H"chst B2, Bockmann JH1, Bester R1, Holzmann B3, Knolle P2, H!ser N3, Hartmann D3, Esser K1, Protzer U1 1 Technische Universit$t M!nchen/Helmholtz Zentrum M!nchen, Institute of Virology, Munich, Germany; 2 Klinikum rechts der Isar, Technische Universit$t M!nchen, Institute of Molecular Immunology, Munich, Germany; 3 Klinikum rechts der Isar, Technische Universit$t M!nchen, Department of Surgery, Munich, Germany; 4German Center for Infection Research (DZIF), Munich and Hamburg sites, Munich, Germany Hepatitis C virus (HCV) infection is a major cause of liver cirrhosis and hepatocellular carcinoma. Within days post infection, innate immunity Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A65 A66 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen is activated by HCV reflected by an induction of IFN-stimulated genes (ISGs). The precise cell type and cellular pathogen pattern recognition receptors (PRRs) involved in innate immune sensing of HCV, however, still remain unknown. To study this as close as possible to the physiological situation, we utilized ex vivo perfused human liver tissue. By pulse perfusing the liver with HCV for 1 h and chase perfusing the liver with HCV free media for 23 h, we found the virus after 1 h predominantly in sinusoidal endothelial cells and kupffer cells(KC). After 23 h chase perfusion, HCV could be found in hepatocytes. When hepatic RNA was extracted after 48 h perfusion, induction of IFN was detected by real time RT-PCR. To investigate if TLRs are involved in HCV recognition, we isolated LSEC, KC and hepatocytes from human liver tissue resections, and compared the TLRs expression levels to circulating immune cells by real time RT-PCR. TLR3 was found to be highly expressed in LSEC, KC and hepatocytes. Cytokine secretion after poly (I:C) stimulation confirmed functionality of TLR3 in KC and LSEC, but revealed that TLR3 has lower functionality in hepatocytes. This could be explained by low expression levels of central adaptors TRIF, RIP1 and RIP3 in the TLR3 signaling cascade in hepatocytes. Thus, we hypothesized that TLR3 might mediate activation of innate immunity against HCV. Since TLR3 is highly conserved from mouse to human and shares structural and functional similarities, we utilized mouse models to verify our hypothesis. Using purified mouse LSEC in vitro, we detected mouse IFN-beta induction by real-time RT-PCR 6 h after HCV stimulation. When we perfused mouse liver with HCV we found that – as in human tissue – the virus predominantly localized in mouse LSECs after 1 h. When comparing wild type to TLR3-/- CH57Bl/ 6 mice, perfusion with HCV induced IFN only in wild type mice but not in knock out mice. From these data we conclude that HCV particles entering the liver are largely endocytosed by LSECs and KCs. In the liver sinusoid, TLR3 senses HCV in LSECs and KCs and induces IFN expression contributing to early immune activation. Corresponding author: Protzer, Ulrike E-Mail: Ulrike.Protzer@tum.de 5.39 Mechanisms of osteopontin-mediated effects on chronic hepatic inflammation and cancer Loscher C1, Keller DA1, W!stenberg A1, Lohmann V2, Barthenschlager R2, Sass G1, Tiegs G1, Barikbin R1 1 University Hospital Hamburg-Eppendorf, Institute of Experimental Immunology and Hepatology, Hamburg, Germany; 2University of Heidelberg, Department of Infectious Diseases, Molecular Virology, Heidelberg, Germany Background and Aims: Osteopontin (OPN) is a ubiquitously expressed protein, which is involved in bone remodeling and immune cell migration and activation. It has been linked to muscle injuries, autoimmune diseases, and cancer. OPN has been found over-expressed in patients with HCV infection and in patients with hepatocellular carcinoma (HCC). Hepatitis virus infection often persist, leading to chronic hepatitis with progression to cirrhosis and HCC. The wnt pathway is associated with higher HCV replication and it is known to be involved in tumor development. In our study we investigated mechanisms and pathways which are involved in effects of OPN, to identify OPN regulated targets to improve HCC therapy. Methods: For in vitro experiments human hepatoma cell lines HepG2 and Huh7 were used and cells expressing HCV genes NS3 to NS 5B alone (Huh5 – 15) or in combination with firefly luciferase (LucUbiNeo-ET). Knock down of OPN expression was achieved by transfection of siRNA, up-regulation was achieved by transfection of an OPN coding plasmid. Gene expression was measured by real time RTPCR and Western Blot analysis. To promote wnt pathway activity the glycogen synthase kinase 3 beta (GSK3b) inhibitors Kenpaullone or SB216763 were used. Inhibition of the wnt pathway was achieved by use of 4,5,6,7-tetrabromo-2-azabenzimidazole (TBB), an inhibitor of beta-catenin stabilizing kinase CK2. Wnt pathway activity was measured by a reporter assay for beta catenin related transcription (CRT) and by real time RT-PCR. Results: OPN was found to be highly expressed in HCV replicon cell lines and this up-regulation was mediated by HCV. However, vice versa OPN was not regulating HCV replication. In addition, OPN is known to be up-regulated in highly proliferating cells like hepatoma cells, but it had no direct effect on cell proliferation. Up-regulation of OPN led to a higher wnt pathway activity whereas downregulation decreased wnt pathway activity which in turn was regulating HCV replication. Conclusions: OPN is regulating the activity of the wnt pathway which in turn promotes HCV replication and tumor cell growth. Therefore, down regulation of OPN or one of its effector molecules in the wnt signaling pathway might not only represent a target to interfere Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York with tumor growth but might also become a novel approach for HCV therapy. Corresponding author: Loscher, Christine E-Mail: christine@familie-loscher.de 5.40 Mechanistic dynamics of Hepatitis C virus replication in single liver cells Knodel MM1, N$gel A1, Reiter S1, Rupp M1, Vogel A1, Targett-Adams P3, Herrmann E2, Wittum G1 1 Goethe University Frankfurt am Main, Goethe Center for Scientific Computing, Frankfurt am Main, Germany; 2Goethe University Hospital, Institute of Biostatistics and Mathematic Modelling, Frankfurt am Main, Germany; 3 Medivir AB, Huddinge, Sweden Infection with hepatitis C virus (HCV) causes chronic liver diseases. HCV-related liver damage is the main reason for liver transplantations in the western world. Spatial resolution is an aspect that has not yet been appreciated in current modeling simulations despite strong biological evidence that suggests intracellular spatial dependence is a crucial factor in the process the virus uses to replicate its RNA genome. HCV replication is believed to occur in specialized compartments within virus-infected cells, termed replication complexes, which are derived from altered regions (called the membranous web) of the endoplasmic reticulum (ER – the ER is a central structure of each cell). Trafficking of both replication complexes, and their components, is likely a dynamic process occurring in three dimensions that is both difficult to capture experimentally and conceptually visualize. Therefore, we are developing a spatially- resolved biophysical model of HCV replication dynamics in single liver cells. We used data derived from 3D confocal microscopy of HCV-infected human hepatoma cells labeled for the ER membrane in order to reconstruct 3D geometries of single hepatocytes using NeuRA2. On top of these geometries, we developed a model using (surface) partial differential equation of viral RNA replication dynamics with particular emphasis upon RNA movement, viral protein production, cleavage and movement, and viral RNA replication within the membranous web. The arising (s)pde s on the ER surface are solved using the simulation platform UG4 within a Finite Volume framework combined with multigrid techniques. Our approach is based on two columns which are intended to grow together in the middle run: On the one hand side, we are doing parameter estimations of single components of viral replication based on the Gauss-Newton algorithm in order for extracting e.g. the diffusion constant of basic viral proteins on the surface of the ER using experimental FRAP time series. On the other hand side, we are developing the model which mimics the interplay of all important component of virus replication, e.g. viral RNA and various states of viral proteins. The estimated parameters are entering the model step by step. Therefore, the presented work is a practical application of the powerful modeling/ simulation tool UG4 and its multigrid techiques for the case of a huge number of degrees of freedom (DoFs) already and demonstrates the excellent usability (and scalability) of UG4 in the context of modern biophysical research. Corresponding author: Knodel, Markus M. E-Mail: markus.knodel@gcsc.uni-frankfurt.de 5.41 Modulation of HCV reinfection by fibroblast growth factor-2 and other non-interferon mediators Dinh NV1, Falk CS4, Vondran FWR5, Helfritz F5, Wedemeyer H1, Manns MP1, Ciesek S1, Hahn T von1 1 Hannover Medical School (MHH), Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany; 2German Center for Infection Research (DZIF) (DZIF), Braunschweig-Hannover site, Germany; 3Hannover Medical School (MHH), Institute for Molecular Biology, Hannover, Germany; 4Hannover Medical School (MHH), Institute of Transplant Immunology, IFB-Tx, Hannover, Germany; 5Hannover Medical School (MHH), Department of General, Visceral and Transplantation Surgery, Hannover, Germany Objective: We aimed to describe the composition of the inflammatory response at the time of hepatitis C virus (HCV) graft reinfection following orthotopic liver transplantation (OLT), assess its impact of the HCV replication cycle and identify individual pro- and antiviral inflammatory mediators. Design: We used a Luminex assay to quantify 50 inflamma- 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen tory mediators in sera before and shortly after OLT. In vitro grown HCV based on the JFH-1 isolate were used to characterize the effects of patient sera and individual mediators on the viral replication cycle. Results: Although the mediator composition is highly variable between individuals, sera drawn in the immediate post-OLT period significantly enhance HCV infectivity compared to control sera from before OLT. Among 27 non-interferon inflammatory mediators that we evaluated for their impact on the HCV replication cycle fibroblast growth factor(FGF-) 2 stood out as it enhanced both HCV RNA replication and release of infectious particles. The effect was concentration-dependent and detectable in dividing and non-dividing cells. Moreover, pharmacological inhibition of FGF-2 receptor signaling abrogated the enhancing effect of FGF-2 and inhibited HCV replication in the absence of serum FGF-2 suggesting that HCV replication is dependent on basal activation of the FGF-2 triggered signaling pathway. Finally, in chronically HCV infected individuals with high viral load serum FGF-2 was significantly higher compared to those with low viral load. Conclusion: Although no single mediator may account for this effect serum shortly post-OLT enhances HCV infection. FGF-2 is a novel endogenous driver of HCV replication and potential therapeutic target. Corresponding author: Nguyen, Van Dinh E-Mail: nguyendinh.van@mh-hannover.de 5.42 Non-responsiveness to therapeutic tumor vaccination is overcome by functional modulation of myeloid derived suppressor cells Heine A1, Llanto C2, Gevensleben H5, Diehl L3, Garbi N2, Brossert P1, Knolle PA4, Kurts C2, H"chst B4 1 University of Bonn, Medical Clinic III for Oncology, Hematology and Rheumatology, Bonn, Germany; 2University of Bonn, Institute of Experimental Immunology, Bonn, Germany; 3University of Bonn, Institute of Molecular Medicine, Bonn, Germany; 4Technische Universit$t M!nchen, Institute of Molecular Immunology, Munich, Germany; 5University of Bonn, Institute for Pathology, Bonn, Germany Therapeutic tumor vaccination represents a promising strategy to induce anti-tumor activity in cancer patients. However, usually only a subpopulation of patients benefits from tumor vaccines, whereas others display continuous tumor growth and metastatic spreading. Here we report a similar observation in a B16 melanoma model. Vaccinating these mice with a model tumor antigen and a combination of adjuvants, i.e. TLR-9-ligand CpG and NKT-cell ligand a-galactosylceramide, controlled the tumor in most animals (High-Responders), whereas others showed no clear benefit from the treatment (Non-Responders). No differences in numbers of B, NK or T cells were detected between both groups. However, Non-Responders showed significantly increased numbers of CD 11b+Gr-1+myeloid-derived-suppressor-cells (MDSCs). Treatment with all-trans-retinoic-acid (atRA), which has been described to modulate MDSCs, effectively restored the tumor control in Non-responders. Frequencies neither of regulatory T cells nor MDSCs differed after treatment with atRA, but those cells from atRA-treated animals with a phenotype of monocytic MDSCs (CD 11b+Ly6ChighLy6G–cells) had lost their suppressive capacity and displayed upregulation of MHC-Class-II, indicating acquisition of immune-stimulatory properties. Concomitantly, IFNg production by CD 8+ T cells was significantly higher in atRA-treated mice. Taken together, we demonstrate that atRA converts Non-Responders to tumor vaccination to responders, offering a novel opportunity for individualized tumor therapy. Corresponding author: H#chst, Bastian E-Mail: Bastian.Hoechst@tum.de 5.43 Oxidiertes Low Density Lipoprotein (oxLDL) – endogener HCV Eintritt Inhibitor und Pr!diktor f"r SVR nach Interferon-basierter Therapie bei chronischer Hepatitis C Solbach P1, Westhaus S2,Deest M3, Herrmann E4, Berg T5, Manns MP1, Ciesek S1, Sarrazin C6, Hahn T von3 1 Hannover Medical School (MHH), Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany; 2German Center for Infection Research (DZIF), Partner site Hannover-Braunschweig, Hannover, Germany; 3 Hannover Medical School (MHH), Institute of Molecular Biology, Hannover, Germany; 4Goethe University Frankfurt am Main, Institute of Biostatistics and Mathematic Modelling, Frankfurt am Main, Germany; 5University Hospital of Leipzig, Department of Hepatology of the Gastroenterology and Rheumatology Clinic, Leipzig, Germany; 6Goethe University Hospital, Medical Clinic I, Center for Internal Medicine, Frankfurt am Main, Germany Hintergrund: Oxidiertes Low Density Lipoprotein (oxLDL) ist ein endogener Ligand des Hepatitis C Virus (HCV) Rezeptors scavenger receptor class B type I (SR-BI) und ein potenter Inhibitor des HCV Zelleintritts. Wir haben die Bedeutung von Serum oxLDL Spiegeln vor Therapie auf das Ansprechen auf eine duale Therapie mit pegyliertem Interferon und Ribavirin bei chronischer Hepatitis C untersucht. Methoden: Baseline Serum oxLDL in n= 398 HCV Genotyp 1 infizierten Patienten der INDIV-2 Studie wurde mittels kommerziellen oxLDL ELISA bestimmt. F!r in vitro flankierende Untersuchungen wurden Huh-7.5 Zellen und Volll"nge sowie subgenomische HCV RNA Genomen benutzt. Ergebnisse: Univariate und multivariate Regressionsanalysen zeigten, dass oxLDL mit der sustained virological response (SVR) nach dualer Therapie aus pegyliertem Interferon und Ribavirin hoch signifikanten assoziiert ist. Die PEG-vermittelte Inhibition der Replikation von Volll"nge HCV (Genotyp 2a – Jc1) sowie HCV Subgenom (Genotyp 1b – Con1) in vitro blieb in Abwesenheit oder Anwesenheit von oxLDL unver"ndert (50 % inhibitorische Konzentration 4.8 und 6.6 mg/ml). Damit scheint oxLDL keinen Effekt auf das zellul"re Interferonansprechen zu haben. Ebenfalls konnte keine Ver"nderung der Serum oxLDL Spiegel unter Interferon Behandlung beobachtet werden womit die Regulation von oxLDL durch Interferon selbst unwahrscheinlich ist. Weitere in vitro Untersuchungen zeigten, dass oxLDL als potenter Inhibitor des cell-to-cell spread zwischen benachbarten Zellen fungiert, eine dominante Verbreitungsroute in infizierten Lebergewebe w"hrend einer chronischen HCV Infektion. Außerdem war Serum oxLDL signifikant mit der Verlustrate infizierter Zellen unter Therapie assoziiert. Zusammenfassung: oxLDL ist ein neuer Pr"diktor f!r SVR unter dualer Therapie. W"hrend der Effekt nicht auf der Aktivierung der antiviralen Abwehr oder der (nderung der zellul"ren Interferon Sensitivit"t beruht, scheint die Hemmung der viralen Verbreitung durch direkten cell-to-cell spread die Chancen zum Erreichen einer SVR zu verbessern. Corresponding author: Westhaus, Sandra E-Mail: westhaus.sandra@mh-hannover.de 5.44 Presence of naive-like HBV-specific CD 8+ T cells in chronically infected patients despite ongoing viral replication Schuch A1, Neumann-Haefelin C1, Thimme R1 1 University Hospital of Freiburg, Department of Medicine II, Freiburg, Germany In chronically HBV-infected patients, virus-specific CD 8+ T cell responses are rarely detectable ex vivo by conventional tetramer staining. This lack of HBV-specific CD 8+ T cell responses may be explained by insufficient priming, T cell exhustion and/or deletion. Here, we set out to address this issue by using new techniques for enumerating virus-specific T cells from human peripheral blood based on the combination of tetramer staining, magnetic-bead enrichment, and multiparametric flow cytometry. Indeed, we were able to detect and characterize CD 8+ T cell populations specific for 4 well-described HLA-A0201-restricted HBV epitopes (core18 – 27, env183 – 191, env335 – 343 and pol455 – 463) in 24 chronically HBV-infected patients suggesting that these cells are not completely deleted. CD 8+ T cells specific for core18 – 27, env335 – 343 and pol455 – 463 were detectable in the majority of analyzed patients (79%, 75 % and 100 % respectively) while env183 – 191-specific CD 8+ T cells were found less frequently (54%). Interestingly, about 20 % of analyzed CD 8+ T cells had a naive-like phenotype with high expression of CD 45RA, CCR7 and CD27 and low expression of CD 11a. By contrast 39% Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A67 A68 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen of HBV-specific CD 8+ T cells showed an effector-memory phenotype characterized by the absence of CD 45RA, CCR7 and high expression of CD27 and CD 11a indicating viral recognition. Of note, HBV-specific CD 8+ T cell populations with naive-like and effector-memory phenotype were detected in parallel for different epitopes within the same patients (9 of 24). Importantly, the observed phenotype did not correlate with any clinical parameter such as HBeAg status, viral load or transaminases and was independent of antiviral treatment. Furthermore, viral sequence analysis revealed the presence of wild-type sequences in patients with naive-like HBV-specific CD 8+ T cells indicating that the observed lack of priming is not due to infection with a variant HBV containing mismatched epitopes. Our results indicate that HBV-specific CD 8+ T cells are not completely deleted in chronically infected patients, but rather maintained at a very low frequency. Furthermore, a substantial fraction of these cells display a naive-like phenotype despite ongoing viral replication. This suggests, that in addition to T cell exhaustion insufficient priming may also contribute to HBV-specific CD 8+ T cell failure in chronically infected patients. Corresponding author: Schuch, Anita E-Mail: anita.schuch@uniklinik-freiburg.de 5.45 Proteasome subunit alpha type-6 regulates the expression of proviral host genes in hepatitis C virus infection Broering R1, Trippler M1, Lutterbeck M1, Real CI1, Megger DA2, Bracht T2, Schweinsberg V2, Sitek B2, Eisenacher M2, Meyer HE3, Baba HA4, Hoffmann AC6, Weber F5, Gerken G1, Schlaak JF1 1 University of Duisburg-Essen, University Hospital, Department of Gastroenterology and Hepatology, Essen, Germany; 2Ruhr-Universit$t Bochum, Medizinisches Proteom-Center, Bochum, Germany; 3Leibniz Institute for Analytical Sciences, ISAS, Dortmund, Germany; 4University of Duisburg-Essen, University Hospital, Department of Pathology and Neuropathology, Essen, Germany; 5University of Duisburg-Essen, University Hospital, Department of General, Visceral and Transplantation Surgery, Essen, Germany; 6University of Duisburg-Essen, University Hospital, Department of Medicine, Molecular Oncology RiskProfile Evaluation, Essen, Germany Objective: The interferon stimulated gene 15 (ISG15) plays an important role in the pathogenesis of hepatitis C virus (HCV) infection. ISG15regulated proteins have previously been identified that putatively affect this proviral interaction. The present observational study aimed to elucidate the relation between ISG15 and these host factors during HCV infection. Design: Transcriptomic and proteomic analyses were performed using liver samples of HCV-infected (n= 54), HBV-infected patients (n= 23) and uninfected controls (n= 10). Primary human hepatocytes (PHH) were treated with toll-like receptor ligands, interferons and kinase inhibitors. Expression of ISG15 and proteasome subunit alpha type-6 (PSMA6) was suppressed in subgenomic HCV replicon cell lines using specific siRNAs. Results: Comparison of hepatic expression patterns revealed significantly increased signals for ISG15, IFIT1 (interferoninduced protein with tetratricopeptide repeats 1), HNRNPK (Heterogeneous nuclear ribonucleoprotein K) and PSMA6 on the protein level as well as ISGs and PSMA6 on the mRNA level in HCV-infected patients. In contrast to ISGs, PSMA6 expression occurred independent of HCV load and genotype. Expression of ISG15 and PSMA6 was induced by poly(I:C), depending on interferon regulatory factor 3 activation and phosphoinositide 3-kinase/AKT signalling, respectively. Suppression of PSMA6 led to significant induction of ISG15 expression, thus combined knockdown of both genes abrogated the antiviral effect induced by the separate suppression of ISG15. Conclusions: PSMA6 is up-regulated during viral hepatitis and functions as a negative regulator for ISG15, a proviral factor in the pathogenesis of HCV infection. These findings suggest that the proteasome might affect the enigmatic interaction between ISG15 and HCV. Corresponding author: Broering, Ruth E-Mail: ruth.broering@uni-due.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York 5.46 Protektiver HBsAg-Expressionsverlust bei HBV-transgenen M!usen durch Methylierungen der DNA Graumann F1, Churin Y1, Roderfeld M1, Schr"der D1, Glebe D2, Roeb E1 1 Justus-Liebig-Universit$t, Gastroenterology, Medical Clinic II, Gießen, Germany; 2Justus-Liebig-Universit$t, Institute of Medical Virology, Gießen, Germany Einleitung: Zu den wichtigsten Ursachen f!r Morbidit"t und Mortalit"t bei Hepatitis B (HBV) Infektionen z"hlen die Leberzirrhose und das hepatozellul"re Karzinom. Die immunvermittelte Sch"digung HBV-Infizierter Leberzellen ist bereits gut erforscht. &ber die direkten pathogenen Effekte des HBV Oberfl"chenproteins ist nur sehr wenig bekannt [1]. Die vorliegende Studie untersucht den Mechanismus des altersabh"ngigen Transgenexpressionsverlustes sowie deren positive Effekte auf die Leber HBV- transgener M"use. Methoden: Es wurden Serum-Analysen, Western Blots und immunhistochemische F"rbungen an Leberproben HBV-Oberfl"chenprotein-transgener M"use (pAlb-PSX [2]) auf dem genetischen Hintergrund BALB/c durchgef!hrt. Außerdem wurden RT-PCRs aus Leberproben analysiert. Ergebnisse: Ab einem Alter von 4 Monaten verlieren die Tiere die Expression des HBV-Oberfl"chenproteins partiell bzw. komplett. Es l"sst sich ein Zusammenhang zwischen dem Verlust der Antigenexpression und verbesserten Serum-Leberparametern nachweisen. Der Verlust der Antigenexpression korreliert außerdem mit vermindertem ER-Stress, wie sich in den Western Blots mit ER-Stressmarkern nachweisen l"sst. Der Expressionsverlust findet auf transkriptioneller Ebene statt und wird durch Methylierungen im Genom der Versuchstiere reguliert. Die Menge der HBsAg-Expression korreliert in diesem Fall negativ mit der Anzahl der Methylierungen. Schlussfolgerung: 1. Der Expressionsverslust des großen Oberfl"chenproteins bei HBVtransgenen M"usen findet auf transkriptioneller Ebene statt und wird durch Methylierungen des Genoms reguliert. 2. Der spontane Verlust der Expression des HBV H!llproteins ist protektiv. 3. Eine therapeutische Anwendbarkeit des Effektes sollte evaluiert werden. Literatur: [1] Churin Y et al., Pathological Impact of Hepatitis B Virus Surface Proteins on the Liver Is Associated with the Host Genetic Background, PLoS one, 2014. 4;9(3):e90608. [2] Chisari FV et al., Expression of hepatitis B virus large envelope polypeptide inhibits hepatitis B surface antigen secretion in transgenic mice, J Virol. 1986;60(3):880 – 887. Korrespondierender Autor: Graumann, Franziska E-Mail: graumannfranziska@gmail.com 5.47 PSC-Patienten weisen eine verminderte Apoptosesensitivit!t von CD 4+ T-Zellen im peripheren Blut auf Schoknecht T1, Schwinge D1, Herkel J1, Lohse AW1, Schramm C1 1 University Hospital Hamburg-Eppendorf, I. Medical Clinic and Polyclinic, Hamburg, Germany Hintergrund und Ziele: Die Prim"r Sklerosierende Cholangitis (PSC) ist eine autoimmune Gallengangserkrankung, deren Immunpathogenese bisher weitgehend unklar ist. Genomweite Assoziationsstudien weisen auf Grund von Polymorphismen im Locus des pro-apoptotischen Bim auf eine defekte Apoptose von T-Zellen als m#glichen pathogenetischen Mechanismus der PSC hin. Bim scheint eine Schl!sselrolle beim extrinsischen Restimulierungs-induzierten Zelltod (RICD) und beim intrinsischen Zytokinentzug-induzierten Zelltod (CWID) von T-Zellen zu haben. Ziel dieser Arbeit war die Untersuchung der Apoptosesensitivit"t von T-Zellen und die Expressionsanalyse der pro-apoptotischen Molek!le Bim, Fas-Ligand und Bak und des anti-apoptotischen Bcl-2 nach RICD und CWID im peripheren Blut von PSC-Patienten und Vergleichsgruppen. Methoden: Es wurden 34 PSC-Patienten, 26 PBC-Patienten und 32 gesunde Kontrollprobanden in die Studie eingeschlossen. Die Apoptoseinduktion humaner T-Lymphozyten erfolgte durch Restimulierung mit anti-CD3 in Anwesenheit von IL-2 (RICD) bzw. durch Deprivation von IL-2 (CWID) in aktivierten Effektor-T-Zellen. Die Apoptosesensitivit"t wurde durchflusszytometrisch mittels Annexin V F"rbung bestimmt. Die Expressionsanalyse pro- bzw. anti-apoptotischer Proteine nach RICD- bzw. CWID-Apoptoseinduktion erfolgte mittels qRT-PCR, wobei GAPDH als Haushaltsgen diente. Die Ergebnisse wurden zwischen PSCund PBC-Patienten und Gesunden verglichen. Als Kontrolle dienten T-Zellen ohne Apoptoseinduktion. Ergebnisse: Die Untersuchung der Apoptosesensitivit"t zeigte bei den CD 4+ T-Zellen aus PSC-Patienten 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen sowohl nach RICD (PSC= 20,9 % vs Gesund= 30,1% vs PBC= 33,6%, p = 0,0002) als auch nach CWID (PSC= 7,1% vs Gesund= 12,1% vs PBC= 12,3 %, p = 0,003) signifikant reduzierte Apoptoseraten im Vergleich zu den Kontrollgruppen. Der prozentuale Zellverlust der CD 8+ T-Zellen wies hingegen weder nach RICD (PSC= 25% vs Gesund= 29,3 % vs PBC= 30,5 %, p > 0,05) noch nach CWID (PSC= 12,6 % vs Gesund= 15,5 % vs PBC= 14,3 %, p > 0,05) signifikante Unterschiede zwischen PSC-Patienten und den anderen Kohorten auf. Desweiteren zeigten T-Zellen von PSC-Patienten nach RICD eine signifikant verminderte Expression des pro-apoptotischen Bim im Vergleich zu den Kontrollgruppen (relative Expression zu T-Zellen ohne Apoptoseinduktion: PSC= 6,8 vs Gesund= 12,9 vs PBC= 12,8, p = 0,0098). Das Expressionsprofil von Fas-Ligand, Bak und Bcl-2 wies keine signifikanten Unterschiede zwischen den untersuchten Gruppen auf. Schlussfolgerung: In dieser Studie konnte gezeigt werden, dass CD 4+ T-Zellen aus PSC-Patienten eine signifikant verminderte Apoptoserate aufweisen. Desweiteren korreliert der verminderte CD 4+ T-Zellverlust nach RICD mit einer signifikant reduzierten Induktion des pro-apoptotischen Bim. Somit ist eine dysfunktionelle Apoptose von CD 4+ T-Zellen ein weiterer Baustein der Immunpathogenese der PSC. Der Einfluss des beschriebenen Bim-Polymorphismus auf die Apoptose von Lymphozyten muss in weiteren Untersuchungen gekl"rt werden. Korrespondierender Autor: Schoknecht, Tanja E-Mail: t.schoknecht@uke.de 5.48 Renal impairment under triple therapy with boceprevir in German real-life: evidence for a pivotal role for peginterferon/ribavirin backbone, female gender and age elder than 50 years Buggisch P1, L"hr H2, Teuber G3, Steffens H4, Kraus M5, John C6, Geyer P7, Weber B8, Witth"ft T9, Herrmann A10, Hoesl M11, Naumann U12, Zehnter E13, Hartmann D14, Dreher B14, Bilzer M14 1 IFI Institute, Hamburg, Germany; 2Gastroenterological Practice, Wiesbaden, Germany; 3Gastroenterological Practice, Frankfurt, Germany; 4Practice of Internal Medicine,Berlin, Germany; 5Klinikum Burghausen, Burghausen, Germany; 6Practice of Internal Medicine, Berlin, Germany; 7Gastroenterological Practice, Fulda, Germany; 8Competence Center Addiction, Kassel, Germany; 9 Gastroenterological Practice, Stade, Germany; 10FriedrichSchiller-University, Jena, Germany; 11Gastroenterological Practice, Nuremberg, Germany; 12Center of Medicine, Berlin, Germany; 13Gastroenterological Practice, Dortmund, Germany; 14MSD Pharma GmbH, Haar, Germany Background: Recently, renal impairment corresponding to renal insufficiency stage 3 has been reported in about 5 % of patients treated for HCV genotype 1 infection with telaprevir or boceprevir (S Mauss et al., Hepatology 2014; 59:46 – 48). The present interim analysis of the NOVUS observational study was conducted to determine the frequency of stage 2 and stage 3 renal insufficiencies and to elucidate associated risk factors and mechanisms in patients (pts) undergoing boceprevir triple therapy in German real-life. Methods: From April 2012 until January 2014, 536 pts with HCV G1 infection were recruited in the ongoing NOVUS study by 97 practices and hospitals in Germany. Pts were treated with pegylated interferons (PegIFN) and ribavirin (RBV) together with boceprevir for 24 to 44 weeks after a 4 weeks lead-in period with PegIFN/RBV. The present interim analysis was restricted to 353 pts having documented data for the calculation of estimated glomerular filtration rate (eGFR) from baseline until treatment week (TW) 24. eGFR (mL/min per 1.73 m2) was calculated with the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula (Levey AS et al., Ann Intern Med 2009; 150:604 – 612). Results: At baseline, 72% (254/ 353) had an eGFR > 90, while 28% (99 / 353) showed an eGFR of 60 – 90, corresponding to renal insufficiency stage 2. Until TW24, 71 of 254 pts (28 %) experienced a decline in eGFR from > 90 to 60 – 90. Interestingly, in 28 of 71 pts (39 %) this decline was observed at the end of the 4 week lead-in period, suggesting a pivotal role for PegIFN/RBV in the mechanism of eGFR decline. Regarding eGFR declines to < 60, corresponding to renal insufficiency grade 3, only 2 pts (0.8 %) had a baseline eGFR > 90, in contrast to 19 pts (19.2 %) with baseline eGFR of 60 – 90. Considering all pts who experienced an eGFR decline to < 60 until TW24 (21/ 353, 5.9 %), 71.4% were females and 90.5 % were elder than 50 years. In 95 % of pts the eGFR decline to < 60 occurred within the first 12 treatment weeks and was reversible until TW24 in 11 of 21 pts (52.4 %). Until now, no patient discontinued BOC triple therapy because of renal impairment. Conclusions: This interim analysis of the NOVUS study demonstrates an unexpected high frequency (28 %) of eGFR declines from > 90 to 60 – 90 which seem to be in part related to PegIFN/RBV backbone therapy. eGFR declines to < 60 occur with a frequency of 5.9 % predominantly until TW12 in elder female pts with reduced eGFR of 60 – 90 at baseline and seem to be reversible despite continuation of triple therapy in more than 58 % of pts. These findings suggest the need of drug dose adjustments in a considerable number of pts undergoing dual therapy with PegIFN/RBV or triple therapy with boceprevir. Corresponding author: Bilzer, Manfred E-Mail: manfred.bilzer@bilzer-consulting.de 5.49 Serum biomarker profile can predict the outcome of acute HCV infection Schlaphoff V1, Deterding K1, Hardtke S1, Hengst J1, Falk C2, Bremer B1, Manns MP1, Cornberg M1, Wedemeyer H1 1 Hannover Medical School (MHH), Department of Gastroenterology, Hepatology and Endocrinology, Hannover, Germany; 2Hannover Medical School (MHH), IFB-Tx, Hannover, Germany Introduction: The natural course of acute hepatitis C virus infection is highly diverse varying between spontaneous clearance of the virus to evolution of chronic hepatitis C (HCV) virus infection. The aim of this study was to identify parameters during early time points of infection predicting the natural course of the infection by analysis of serum IP-10 levels and other cytokines and chemokines thus enabling identification of patients not achieving spontaneous viral clearance who might require antiviral treatment. We performed multianalyte profiling of 50 cytokines and chemokines in the serum using the BioPlex method. Serum samples from 26 patients with acute symptomatic HCV infection recruited within the German Hep-Net-acute HCV-III cohort were analyzed together with ten clinical parameters at the time of diagnosis of infection. To identify profiles characterizing spontaneous sustained viral resolvers we performed principal component analysis (PCA) using Qlucore Omics Explorer Software (Qlucore, Lund, Sweden). Results: Half of the patients were male (50 %), most of them were older than 30 years (77%) and they were mainly genotype 1-infected (70%). First, we performed analyses of serum IP-10 levels alone to evaluate the possibility of predicting the natural outcome of infection as described previously. However, no correlation of IP-10 levels with natural outcome could be observed. Also inclusion of IL 28b polymorphisms did not correlate with spontaneous clearance. We then analyzed whether profiles of all 50 serum cytokines/chemokines would allow a prediction of the natural outcome. Using PCA three cytokines could be identified that significantly differed between patients achieving spontaneous sustained viral clearance (n= 8) from those patients who were still HCV-RNA positive 12 weeks or more after the first diagnose of acute HCV infection. (n= 18). Here, a spontaneous clearance of the virus was associated with lower levels of ICAM-1, SCGF-b and VCAM-1 in the serum as compared to patients who did not achieve a sustained spontaneous viral clearance. Furthermore, serum ALT levels or viral load did not correlate with cytokine levels. Conclusion: In conclusion, the sustained spontaneous viral clearance of acute HCV infection could be reliably predicted by concordantly decreased levels of the serum cytokines and chemokines ICAM-1, SCGF-b and VCAM-1. These parameters might be helpful for the decision whether antiviral treatment of acute HCV infection is required. Corresponding author: Schlaphoff, Verena E-Mail: schlaphoff.verena@mh-hannover.de 5.50 The differential phenotype and functionality of CMV- and EBV-specific CD8 T cells in patients with chronic hepatitis C is associated with an altered plasma cytokine milieu Owusu SS1, Venkata PS1, Hengst J1, Falk C2, Hardtke S1, Manns MP1, Cornberg M1, Wedemeyer H1, Schlaphoff V1 1 Hannover Medical School (MHH), Department of Gastoenterology, Hepatology and Endocrinology, Hannover, Germany; 2Hannover Medical School (MHH), IFB-Tx, Hannover, Germany Persistent infections such as chronic hepatitis C (CHC) are often characterized by an ongoing inflammation and thus altered cytokine milieu due to the constant antigen stimulation. It is still under debate whether such persistent infections may also affect immune responses towards Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A69 A70 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen other pathogens. We therefore investigated the phenotype and function of CD8 T cells specific for common pathogens like CMV and EBV using PBMC from HLA-A2+ CHC patients (n= 37) and healthy blood donors (n= 31). Total and CMV/EBV-specific CD8 T cells were assessed for expression of PD-1, Tim-3 and 2B4 ex vivo and after in vitro stimulation with cognate peptides as well as their functionality investigated. We further comprehensively analysed serum profiles of 50 cytokines/chemokines in these CHC patients and in further healthy individuals (n= 35). We demonstrate here that ex vivo expression of PD-1, Tim-3 and 2B4 on total CD8 T cells were 1.6-, 1.5- and 1.5-fold higher in patients with CHC compared to healthy individuals, respectively. Similarly, expression of PD-1, Tim-3 and 2B4 were likewise increased on the CMV/ EBV-specific CD8 T cells in CHC patients (CMV: 1.2 fold, 3.2 fold 1.1 fold, EBV: 1.2 fold, 2.0 fold, 1.1 fold, respectively) compared to healthy humans despite their ex vivo frequencies being similar. Importantly, this increased expression culminated in a yet even stronger proliferation and cytokine production by CMV/EBV-specific CD8 T cells in patients with CHC upon peptide stimulation. In order to investigate which role cytokines/chemokines might play in this altered phenotype and activation status during CHC, we compared the plasma cytokine/chemokine levels between healthy individuals and CHC patients using ONE-WAY ANOVA and Principal Component Analysis. Here, IFN-a2, SDF-1a, HGF, MIG, SCF, SCGF-b, CTACK, ICAM-1, VCAM-1, and IP-10 were present at significantly higher levels, while PDGF-bb, G-CSF and GRO-a were lower in CHC patients. We then correlated the levels of these cytokines to the ex vivo expression of PD-1, 2B4 and Tim-3 on both bulk and CMV/EBV-specific CD8 T cells in these CHC patients. Here, levels of IP-10, ICAM-1, VCAM-1, LIF and GRO-a showed to be positively correlating with PD-1 and 2B4 expression on both cell populations. Importantly, the impact on Tim-3 expression differed with plasma levels of SDF-1, INF-a2, PDGF-bb and GCSF positively correlating while VCAM-1, ICAM-1 and CTACK were a negatively associated on both cell populations. In conclusion, our results suggest an important influence of the cytokine microenvironment in shaping the phenotype and function of antiviral CD8 T cells possibly by affecting the expression of co-regulatory molecules. Corresponding author: Schlaphoff, Verena E-Mail: schlaphoff.verena@mh-hannover.de 5.51 The interaction of the Hepatitis C Virus with intra-cellular signaling converts EGF into a potent inducer of the production of CXCR2-ligands by the infected host cell Gr"pper C1, Triller N1, Bartenschlager R1, H$ussinger D1, Bode JG1 1 Heinrich Heine Universit$t D!sseldorf, I. Department of Gastroenterology, Hepatology and Infectious Diseases, Duesseldorf, Germany Introduction: To establish persistent infection the hepatitis C virus (HCV) must have evolved strategies to escape antiviral and innate immunity and to influence the inflammatory response. Migration of the different cell types of adaptive and innate immunity is largely controlled by chemokines. Hence chemokines are decisive for the local composition of the different types of immune- or inflammatory cells and therefore play a major role for the formation of the local inflammatory- or immune-milieu. It is therefore not surprising that HCV has evolved strategies to gain influence on the expression of chemokines. The molecular mechanisms, which are employed by HCV to modify the expression of these factors, are incompletely understood. Likewise the influence of HCV on the regulation of chemokine expression in response to different stimuli is not clear. The present study investigates the impact of HCV on the production of the major chemo-attractants of neutrophils, the CXCR2 ligands CXCL1, 2, 3 and 8, in its host cell upon stimulation with the growth factor EGF. Methods: Huh-7 cells either infected with the HCV cc strain JC1 or harbouring the HCV subgenomic replicon were used and the impact of HCV on cellular signalling and gene expression was analysed employing targeted gene knockdown by siRNA, inhibitor-studies, rtPCR and Immunoblot-analysis. Results: Expression of the CXCR2 ligands in the hepatoma cell lines Huh-7 or Huh-7.5 is not or only weakly influenced upon stimulation with EGF. Therefore, the observation was surprising, that in the presence of either the sub-genomic or the full-length HCV replicon or upon infection of Huh-7.5 cells with the HCVcc strain JC1 EGF is converted in to a potent inducer of the different CXCR2 ligands. The further analysis of the molecular mechanism involved in this phenomenon revealed that with respect to the regulation of CXCL8 the NS 3/ 4A mediated down-regulation of the endogenous feedback inhibitor of the EGF receptor (EGFR), the ubiquitously ex- Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York pressed T cell protein-tyrosine phosphatase (TC-PTP) and subsequent sensitization of the EGFR is important. Furthermore inhibitor studies and studies using targeted gene knockdown by specific siRNA suggest that downstream of the EGFR activation of the mitogen activated protein kinase (MAPK) activating protein kinase (MEK)1 and of its down-stream effector kinases the extracellular signal stimulated kinase (Erk)1 and 2 play a role for EGF inducible expression of CXCL8 in the presence of HCV. Interestingly this mechanism is not responsible for the EGFR-dependent up-regulation of the other CXCR2 ligands CXCL-1, 2 and 3 in HCV infected cells upon stimulation with EGF. Conclusion: The study provide evidence that HCV utilizes EGFR and EGFR-dependent signalling not only as cofactors for viral entry and replication but also interferes with EGF-dependent signalling thereby modifying the inter-cellular communication of the infected host cell. Corresponding author: Bode, Johannes G. E-Mail: johannes.bode@med.uni-duesseldorf.de 5.52 Treatment of previously untreated patients with chronic HCV genotype 1 infection with boceprevir in German real-life: high end of treatment response of 95 % in patients with early virologic response Buggisch P1, L"hr H2, Teuber G3, Steffens H4, Kraus M5, John C6, Geyer P7, Weber B8, Witth"ft T9, Herrmann A10, Hoesl M11, Naumann U12, Zehnter E13, Hartmann D14, Dreher B14, Bilzer M14 1 IFI Institute, Hamburg, Germany; 2Gastroenterological Practice, Wiesbaden, Germany; 3Gastroenterological Practice, Frankfurt, Germany; 4Practice of Internal Medicine, Berlin, Germany; 5Klinikum Burghausen, Burghausen, Germany; 6Practice of Internal Medicine, Berlin, Germany; 7 Gastroenterological Practice, Fulda, Germany; 8Competence Center Addiction, Kassel, Germany; 9Gastroenterological Practice, Stade, Germany; 10Friedrich-Schiller-University, Jena, Germany; 11Gastroenterological Practice, Nuremberg, Germany; 12Center of Medicine, Berlin, Germany; 13 Gastroenterological Practice, Dortmund, Germany; 14MSD Pharma GmbH, Haar, Germany Background: The achievement of early virologic response (EVR) during triple therapy of chronic HCV genotype 1 infection with the HCV protease inhibitor boceprevir has been identified as predictor to shorten treatment to 24 weeks. The present interim analysis of the NOVUS observational study was aimed to determine the frequency of EVR during boceprevir triple therapy in German real-life and to determine the virologic outcome of patients with and without EVR. Methods: From April 2012 until January 2014, 536 patients (pts) with genotype 1 infection were recruited in the ongoing NOVUS study by 97 practices and hospitals in Germany. Patients were treated with pegylated interferons (PegIFN) and ribavirin (RBV) together with BOC for 24 to 44 weeks after a 4 weeks lead-in period with PegIFN/RBV. The present interim analysis was restricted to 222 previously untreated patients with documented HCVRNA at treatment week (TW) 8. Results: Overall, 158 of 222 pts (71.2 %) undergoing boceprevir triple therapy achieved an EVR (59.5 % male, 32.9 % > 50 years, 61.8 % with baseline viral load > 400.000 IU/mL) while 64 pts (28.8 %) did not (48.4 % male, 48.4 % > 50 years, 82.8% with baseline viral load > 400.000 IU/mL). Pts who achieved EVR showed more frequent a HCV-RNA decline > 1log10 to PegIFN/RBV lead-in at the end of TW4 (89.3% vs. 54.1%, p < 0.0001). In addition there was a significant higher virologic response at TW12 in pts with EVR (90.9 % vs. 67.8 %, p< .0001). Only 1 patient (0.8 %) with EVR had HCV-RNA levels > 100 IU/mL thereby fulfilling TW12 stopping rules in contrast to 9 pts (9.2 %) without EVR. Furthermore, a better virologic response was found at TW24 (87.2 % vs. 64.9 %, p = 0.0006) and at the end of treatment (EOT) with EOT response rates of 94.9 % and 65.9% (p < 0.0001) in pts with and without EVR. Follow-up data were available from 123 pts with EOT documentation: Until now, 78 of 89 pts with EVR (87.6 %) achieved SVR in contrast to only 14 of 34 (41.2%) in the subgroup of pts without EVR. Conclusions: Approximately 70% of treatment-na+ve pts with HCV G1 infection undergoing triple therapy with boceprevir in German reallife experience an EVR which allows shortage of triple therapy to 24 weeks. In addition, achieving EVR is associated with high EOT response rates as well as high SVR rates of 95 % and 88%. The more rapid HCVRNA decline at the end of lead-in suggests a higher sensitivity to PegIFN/ RBV backbone in pts who achieve EVR. Corresponding author: Bilzer, Manfred E-Mail: manfred.bilzer@bilzer-consulting.de 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 5.53 Treg impairment is not a sufficient cause of autoimmune liver inflammation 1 1 1 1 Laschtowitz A , Carambia A , Lohse AW , Schramm C , Herkel J1 1 University Hospital Hamburg-Eppendorf, Department of Medicine I, Hamburg, Germany Background: The role of Foxp3+ regulatory T cells (Tregs) in autoimmune hepatitis is controversial. Whereas some reports suggested that autoimmune hepatitis is caused by Treg impairment, other reports did not find such link. Here, we directly addressed this issue using a mouse model, in which tolerance to a defined autoantigen is induced in the liver through generation of antigen-specific Tregs. This model is characterised both by ectopic expression of the prototypical autoantigen myelin basic protein (MBP) in the liver and by the presence of autoreactive MBP-specific T cells, due to a transgenic T cell receptor. As a result of MBP expression in the liver, these (CRP-MBP x tg4) mice feature MBPspecific Tregs that can completely suppress MBP-induced inflammation both in the liver and in the CNS (Carambia A, et al., J Hepatol 2014; L!th S, et al., J Clin Invest 2008). Methods: The functionality of Tregs and T effector cells in (CRP-MBP x tg4) mice was confirmed in vivo and in vitro. Treg impairment in these mice was induced either by 1) crossing onto hCD 2-DkTbRII mice, in which T cells feature a dominant-negative TGFb receptor that prevents peripheral Treg induction; or by 2) Treg depletion with the PC61 antibody. Results: (CRP-MBP x tg4) mice feature MBP-responsive T cells; nonetheless, these mice were completely resistant to the induction of autoimmune inflammation in liver and CNS. Tregs of (CRP-MBP x tg4) mice were functional suppressors of MBPspecific effector cells that could effectively suppress inflammatory cytokine secretion of T effector cells upon MBP-stimulation in vitro. However, Treg depletion did not abrogate disease resistance in (CRP-MBP x tg4) mice. Moreover, although hepatic Treg generation was impaired in (CRP-MBP x tg4 x hCD 2-DkTbRII) mice displaying a dominant-negative TGFb receptor on T cells, these mice were still completely disease resistant. Conclusion: Our findings confirm that Tregs are instrumental for hepatic tolerance in CRP-MBP mice. Nonetheless, Treg impairment is not a sufficient cause of autoimmune liver inflammation. Corresponding author: Laschtowitz, Alena E-Mail: laschtowitz@gmail.com 5.54 Type III interferons induce cccDNA degradation similar to type I interferons in HBV-infected HepaRG cells Bockmann JH1, Xia Y2, Stadler D2, Protzer U2 1 University Hospital Hamburg-Eppendorf, I. Department of Internal Medicine, Hamburg, Germany; 2Technische Universit$t M!nchen, Institute of Virology, Munich, Germany Type III interferons (IFN-lambda 1,2 and 3 or IL-29, IL 28a and IL-28b, respectively) and Type I interferons (IFN-alpha/beta) activate similar signaling cascades although via different receptors. While the IFN-alpha/beta receptor is ubiquitously expressed, the IFN-lambda receptor, which is a heterodimer consisting of IL-10 and IL-28 receptor subunits, is mainly expressed on epithelial cells. Despite the convergence of IFNlambda signaling cascades with that of type I and II IFNs, the cytokine families are known to differ in their antiviral activities. In this study we therefore aimed at dissecting at which step IFN-lambda blocks HBV replication after infection. For this, HepaRG cells differentiated in 1.8% DMSO were treated for different time periods with IFN-lambda1, IFNlambda2 or IFN-alpha and mRNA expression of interferon-stimulated genes (ISG) was analyzed by qRT-PCR. Differentiated HepaRG cells were infected with HBV at an MOI of 200 DNA containing particles/cell for 10 d and treated for another 7 d with 1 – 1000 U IFN-lambda1 or IFNlambda2. CccDNA amounts and secreted HBeAg were measured by qPCR and ELISA, respectively. Hereby, we found that Type III interferons IFNlambda1 and IFN-lambda2 induce interferon-stimulated genes (f.e. Mx1 and OAS) as well as cytidine deaminases (f.e. Apobec3A, Apobec3B and Apobec 3G) in HepaRG cells with a similar efficacy as IFN-alpha but with distinct kinetics. IFN-lambda1 and IFN-lambda2 did not only reduce HBV replication, progeny and HBeAg secretion, but also reduced levels of intracellular cccDNA. Analysis of cccDNA amplicons indicated sequence alterations from GC to AT-rich regions as a consequence of IFNlambda induced deamination of HBV cccDNA. Conclusions: IFN-lambda1 and IFN-lambda2 efficiently suppress HBV replication and reduce intracellular cccDNA similar to IFN-alpha but with distinct kinectics. Thus, both cytokine families seem to operate through a common mole- cular mechanism of cccDNA deamination and subsequent degradation. Corresponding author: Bockmann, Jan-Hendrik E-Mail: j.bockmann@uke.de 5.55 Untersuchung von Resistenzmutationen innerhalb der NS3 Protease zur Vorhersage des Therapieausgangs der HCV Triple-Therapie Dietz J1, Rupp D2, Perner D1, Berkowski C1, R$der M1, Susser S1, Zeuzem S1, Bartenschlager R2, Sarrazin C1 1 Goethe University Hospital, Medical Clinic I, Frankfurt am Main, Germany; 2University of Heidelberg, Molecular Virology, Heidelberg, Germany Einleitung/Ziele: Von 2011 bis 2013 wurden Triple-Therapien mit den NS3 Proteaseinhibitoren (PI) Telaprevir (TVR) und Boceprevir (BOC) h"ufig zur Therapie der chronischen HCV (Hepatitis C Virus) Genotyp (GT) 1 Infektion eingesetzt und dies ist aktuell noch die Standardbehandlung in vielen L"ndern. Das virologische Ansprechen h"ngt dabei von viralen und Wirtsfaktoren ab, wie pr"existente HCV-Resistenzen, der HCV-Viruslast/Subtyp, Zirrhose sowie dem IL 28B Genotyp und IP10-Spiegeln (interferon-gamma inducible protein), welche daher in einer Kohorte von TVR/BOC-behandelten Patienten untersucht wurden. Methodik: Im Rahmen einer prospektiven, multizentrischen Studie wurde von Patienten unter einer Triple-Therapie Blut zu baseline (PIRB) und nach Therapieversagen (PISA) gesammelt. Die NS3 Protease wurde aus Patientenseren amplifiziert und populationsbasiert sequenziert. Es erfolgte eine Auswertung von resistenz-assoziierten Varianten (RAVs) an den Positionen: V36, T54, V55, Q80, R117, R155, D168 und I/V170. Die NS3 Protease Quasispezies wurde von ersten Patienten (n= 22) zu baseline in Replikon-basierte Bibliotheken inkorporiert, um die HCV Resistenzen ph"notypisch zu charakterisieren. Ferner erfolgte die Analyse von bekannten negativen Pr"diktoren f!r das Therapieansprechen, wie IL 28B non-CC, Zirrhose, HCV GT1a, Nicht-Ansprechen auf vorherige Therapien, hohe IP10-Spiegel und RAVs zu baseline. Ergebnis: Es wurden 212 Patienten in die PIRB- und 89 Patienten in die PISA Studie eingeschlossen. Erste Analysen zur Korrelation von baseline RAVs mit den Ph"notypen und weiteren klinischen Parametern wurden in einer Subgruppe von 81 Patienten mit einer SVR (sustained virologic response) und 33 Individuen mit Therapieversagen durchgef!hrt. Zu baseline waren TVR-/BOC-relevante RAVs selten nachweisbar (7 / 81 Patienten mit SVR (9 %) und 1/ 33 (3 %) Individuen mit Therapieversagen) und die Pr"existenz von RAVs korrelierte nicht mit dem sp"teren Therapieansprechen. Hingegen waren bei 50 % der Patienten nach dem virologischen Therapieversagen RAVs (haupts"chlich in Kombination mit R155K) detektierbar. Zu baseline konnten sensitive (n= 13) und resistente (n= 9) Ph"notypen nachgewiesen werden, diese waren nicht mit der Existenz von RAVs assoziiert. Es war jedoch ein Trend zu einer Korrelation von sensitiven Ph"notypen mit einer SVR detektierbar. Dabei waren einzelne bekannte negative Pr"diktoren nur schwach mit dem Therapieansprechen in unserer Kohorte assoziiert. Allerdings war insgesamt die Anzahl von negativen Pr"diktoren bei Patienten mit Therapieversagen h#her im Vergleich zu Individuen mit SVR (2.1 versus 1.3; P < 0.001). Schlussfolgerung: Zu baseline kamen RAVs selten vor und die Sensitivit"t der Ph"notypen korrelierte nicht mit pr"existenten RAVs. Einzelne bekannte Pr"diktoren waren nicht mit dem Therapieansprechen assoziiert, jedoch korrelierte in kombinierten Analysen die Gesamtzahl negativer Pr"diktoren zu baseline signifikant mit dem Therapieansprechen. Korrespondierender Autor: Dietz, Julia E-Mail: julia.dietz@em.uni-frankfurt.de Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A71 A72 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber | 30.–31. Januar 2015, M!nchen 5.56 Viral sequence analysis of the hepatitis B virus core protein reveals CD8 T cell epitopes under reproducible selection pressure Kefalakes H1, Budeus B2, Walker A1, Jochum C3, Hilgard G3, Heinold A4, Heinemann F4, Gerken G3, Hoffmann D2, Timm J5 1 University of Duisburg-Essen, Institute of Virology, Essen, Germany; 2University of Duisburg-Essen, Bioinformatics Department, Centre for Medical Biotechnology, Essen, Germany; 3University of Duisburg-Essen, Department of Gastroenterology and Hepatology, Essen, Germany; 4 University of Duisburg-Essen, Institute of Transfusion Medicine, Essen, Germany; 5Heinrich Heine University D!sseldorf, Institute of Virology, Duesseldorf, Germany Background: Chronic infections with the hepatitis B virus (HBV) are worldwide an enormous public health problem. Effective suppression of viral replication can be achieved with inhibitors of the viral polymerase, however, in most cases lifelong treatment is required to avoid recurrence of viremia. Activation of HBV-specific CD8 T cells by therapeutic vaccination may promote sustained control of viral replication by clearance of cccDNA from infected hepatocytes. Importantly, little is known about the exact targets of the CD8 T cell response and the extent Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York of selection pressure on the virus. Here, it was hypothesized that CD8 T cell responses associated with strong selection pressure on the virus can be identified by viral sequence analysis. Methods: The HBV core gene was amplified and sequenced from 148 patients with chronic HBV infection and the HLA class I genotype (A and B locus) was determined. Residues under selection pressure in the presence of particular HLA class I alleles were identified by a statistical approach utilizing a novel analysis package ’SeqFeatR’. Candidate CD8 T cell epitopes were confirmed by analysis of PBMCs from patients with chronic and acute infection. Results: With a false discovery rate set to 0.2 a total of 9 residues under selection pressure in the presence of 10 different HLA class I alleles were identified. Additional immunological experiments confirmed that 7 of the residues were located inside previously unidentified epitopes targeted in patients with chronic HBV infection carrying the relevant HLA class I allele. Consistent with viral escape some of the selected substitutions impaired recognition by HBV-specific CD8 T cells. Conclusion: Viral sequence analysis allows identification of HLA class I-restricted epitopes under reproducible selection pressure in HBV core. The possibility of viral adaptation to CD8 T cell immune pressure needs attention in the context of therapeutic vaccination. Corresponding author: Kefalakes, Helenie E-Mail: helenie.kefalakes@uk-essen.de Namenverzeichnis | 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber Namenverzeichnis A Abbas AS A7, A24 Abbasi MH A4 Abdullah Z A23, A54 Acalovschi M A50 Ahmad S A8 Akhar T A8 Al Masaoudi M A46 Albrecht U A63 Aleithe S A29 Al-Herwi E A18 Alidousty C A17 Allweiss L A53, A62 Alsamman M A15 Al-Samman M A6 Alt Y A29 Altevogt P A31 Altomonte J A40 Altrock E A10, A11 Amann T A6 Amer W A14, A36 Anadol E A18 Anastasiou O A22 Andersen JB A52 Andrassy J A49 Andruszkow JHK A11 Angel P A51 Angele M A49 Arnold K A33 Arslanow A A25 Asimakopoulou A A11 Augustin HG A2 B Baba HA A23, A68 Bachmann A A45 Baer C A47 Bangen JM A44 Bantel H A44 Barbacid M A44 Barikbin R A55, A66 B"rmann J A62 Bartenschlager R A61, A64, A70, A71 Barthenschlager R A66 Batool S A24 Bauer T A58 B"uerlein FJB A49 Baus C A22 Bechmann LP A22, A23, A25, A26 Beck J A1 Beck M A48 Becker T A34 Beer A A62 Begher-Tibbe B A2 Behrendt P A57, A62 Beisel C A20 Beissbarth T A47 Benson S A23 Benten D A20 Berg T A63, A67 Bergheim I A5 Berkowski C A71 Berndt N A38 Bernhagen J A12 Berres ML A12 Best J A25 Bester R A65 Beyer M A23, A54 Bhadra OD A62 Bias K A21 Bielow C A38 Bilzer M A55, A56, A58, A61, A69, A70 Birkenfeld AL A16, A36 Bissinger M A38 Blessin U A20 Boaru SG A13, A32 Bock M A43 Bockmann JH A65, A71 Bocuk D A47 Bode J A52 Bode JG A8, A12, A32, A61, A63, A64, A70 Bode KA A31 Boesecke C A59, A60 B#hm M A15 B#hmer F A44 B#hmer O A12 Bohne F A57 Boor P A3 Borkham-Kamphorst E A11, A13 Bosserhoff A A6, A7, A9 B#ttger J A29, A33, A34 Bowe A A3, A38 Boxtermann M A65 Bracht T A68 Br"gelmann C A5 Braspenning J A9 Braun S A12 Breitkopf-Heinlein K A9, A12 Bremer B A21, A56, A57, A64, A69 Breuhahn K A37, A38, A39, A42, A46 Breunig I A22 Brigitte B A39 Broering R A3, A68 Brosch M A34 Brossart P A25 Brossert P A67 Br!ckner S A34 Brueckner S A14 Brune M A19 Brunner C A45 Brunner SM A37 Bruns OT A54 Bruns T A18 Brunskole Hummel I A61 Bruss V A57 Budeus B A72 Buggisch P A55, A56, A58, A61, A69, A70 Burgermeister E A16 B!ttner R A14, A16, A36 C Caliskan S A30 Calvisi DF A37, A52 Camargo RG A8, A16 Canbay A A3, A22, A23, A25, A26, A28, A41 Carambia A A54, A71 Castoldi M A36 Castven D A52 Cederbaum AI A32 Chamulitrat W A17, A33, A40 Chavakis T A34 Chen X A37, A52 Cheng X A65 Chinatalpati C A52 Christ B A14, A44 Christmann A A24 Christoph HzS A19 Chung RT A55 Churin Y A17, A50, A68 Ciesek S A63, A66, A67 Cigliano A A37, A52 Coleman D A8 Cooke A A48 Cornberg M A19, A56, A57, A58, A59, A64, A65, A69 Cox A A21 Cramer T A38 Cubero FJ A13, A46 Curth HM A38 Czech B A6, A7, A9 D Dahmen U A14 Dammermann W A64 Dandri M A53, A62 Daniel G A50 Darstein F A50 Dayoub R A7, A34 De Bandt JP A5 de Bruin A A13 De Ponti AM A51 Deest M A63, A67 Degen C A5 Delogu S A52 Dembek C A58 Demmel M A35 Denk G A49 Deterding K A19, A58, A59, A64, A65, A69 Dewidar B A2 Diehl L A67 Dienes HP A14, A16, A33, A62 Dierks P A63 Dietz J A71 Dinh NV A66 Dirsch O A14 Ditze M A44 Dollinger M A2 Dombrowski F A37, A52 Dooley S A2, A10, A12, A15, A16, A44, A52 Draenert R A58 Drasdo D A2 Drebber U A33, A36, A62 Dreher B A55, A56, A58, A61, A69, A70 Drescher H A27 Dries V A33 Driftmann S A3 Dropmann A A15 D!rl S A10 Dzieran J A52 E Eberhard JM A63 Ebert M A9, A12, A16 Ebert O A40 Ecker EM A60 Ederer M A63 Ehlken H A20, A60 Ehlting C A12, A52 Ehmer U A42, A47 Ehnert S A45 Eischeid H A36 Eisenacher M A68 Eisenb!rger S A61, A64 Eiteneuer EM A48 Elssner C A48 Endris V A39, A49 Engstler J A5 Ergen C A65 Erhart W A34 Ernst C A47 Ernst S A21, A56 Erschfeld S A27 Esser K A65 Evert M A37, A52 Eychm!ller A A54 F Fahrenkamp D A44 Falk C A65, A69 Falk CS A56, A66 Fekete-Drimusz N A43 Feng T A2, A52 Ferrer J A10 Feuer R A63 Fichtner-Feigl S A37 Fickert P A3 Finkelmeier F A19 Fischer M A52 Fischer P A12 Flechtenmacher C A19 Fleet JC A35 Namenverzeichnis Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A73 A74 Namenverzeichnis | 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber Fleischmann-Mundt B A53 Floege J A3, A17 Folseraas T A19 Fraas A A48 Fragoulis A A27 Freund B A54 Frey A A60 Frey L A49 Friebel A A2 Friedman SL A25 Friedrich K A19, A20, A23 Friess H A45 Fuchs P A50 F!hrer D A22, A23 G Gaestel M A12 Galle PR A29, A39, A41, A50, A52 Gao B A2 Garbi N A67 Gass S A53 Gassler N A11, A44, A46 Gautheron J A28 Gebhardt R A28, A29, A33, A34 Gebhardt S A51 Geffers R A46, A51, A53 Gehrke N A29 Geier A A30, A34, A35 Geisler F A10, A58 Gekle M A2 Gerbes AL A49 Gerding B A30 Gerken G A3, A9, A22, A23, A25, A26, A41, A60, A68, A72 Gertzen CGW A31 Gevensleben H A67 Geyer P A56, A58, A61, A69, A70 Geyer PR A55 Ghadimi M A47 Ghafoory S A9 Ghallab A A4 Giersch K A53, A62 Gieseler RK A22, A23 Gildein L A35 Ginhoux F A65 Gisa A A57 Gl"ssner A A59, A60 Glebe D A68 Gockel I A52 Goeppert B A47 Goeser F A60 Goeser T A38 Gohlke H A31 Gonzalez-Carmona MA A41, A46 G#rg B A27, A31, A36 G#rtzen J A4, A21, A25 Gotthardt D A43 Gotthardt DN A19, A20, A23, A31 Granzow M A5 Graß F A62 Graumann F A68 Green RM A27 Greinert R A18 Groos S A11 Gr#pper C A70 Gruenhage F A22 Gr!ner N A49 Grunert D A40 Gr!nhage F A6, A10, A24 Guba M A49 Gul S A45 G!rlevik E A49, A53 Guthke R A28, A29 Gutierrez Jauregui R A43 H Haas U A13, A40 Hackstein P A23, A54 Hadem J A44 Hafezi M A47 Hahn T von A63, A66, A67 Hahnel MJ A12 Halilbasic E A62 Hall R A16 Hall RA A15, A27 Hammad S A2, A14 Hammerstingl C A21 Hampe J A34 Hardtke S A21, A56, A65, A69 Hartig U A24 Hartl J A20, A60 Hartmann D A45, A55, A56, A58, A61, A65, A69, A70 Hasreiter J A57 Hassan R A4 Hatting M A46 Hauner M A35 H"ussinger D A8, A12, A27, A31, A32, A36, A52, A61, A63, A64, A70 Heeren J A54 Heidrich B A21, A56 Heikenw"lder M A10, A28, A45, A59 Heine A A67 Heine M A54 Heinemann F A72 Heiner W A19 Heinold A A72 Heinrich S A52 Heinrichs D A12 Heinz S A9 Heinzel K A64 Heinzen J A5 Helfritz F A66 Hellerbrand C A2, A6, A7, A9, A30, A32, A34, A43 Hempel M A44 Hengst J A65, A69 Hengstler JG A2, A4, A14 Henkel J A8, A16 Herkel J A54, A68, A71 Hermanns HM A30, A34, A35 Hermert D A17 Herrmann A A34, A55, A56, A58, A61, A69, A70 Herrmann E A66, A67 Herzer K A41, A60 Hescheler J A16 Hess J A51 Heymann F A65 Hilgard G A72 Hillebrand RM A41 Hippchen T A20 Hiththetiya K A1, A5 H#chst B A65, A67 Hoehme S A2 Hoeltke N A40 Hoerauf A A26 Hoesl M A55, A56, A58, A61, A69, A70 Hoffmann AC A68 Hoffmann D A72 Hoffmann V A3, A38 Hofmann T A60 Hofmann U A29, A34 Hohaus P A18 Hollenbach M A5, A18 Holzer K A48 Holzh!tter HG A38 Holzmann B A65 Holzmann H A62 H#ner zu Siederdissen C A58, A59, A64 Hoppe-Lotichius M A50 Horst AK A57 Hov JR A19 H#velmeyer N A29 Hu J A2 Hu W A40, A44, A46 Huang J A14, A16 Huber S A54 Namenverzeichnis Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York Hubner EK A42, A47 Hunka L A25 H!ser N A45, A65 I Idilman R A21 Ingeliz P A60 Ingiliz P A59 Inhoffen J A40 Ittrich H A54 Itzel T A34 J Jagemann B A24 Jahn D A34, A35 Janas M A59 Janicot M A15 Jansen C A18, A21, A25 Jara M A21, A51, A53 Jaroszewicz J A64 Jaschinski F A15 Jeliazkova P A10 Jilg W A61 Jin C A5 Jochum C A72 Johanen T A2 John C A55, A56, A58, A61, A69, A70 John K A44 J#rdens M A31 J#rs S A10 J!ngst C A24 K Kaczmarek D A59 Kaiser G A3, A23 Kampschulte M A50 Kanwal S A4 Karababa A A27 Karimi K A55 Kaspar M A49 Kasper HU A33 Kastenm!ller W A23, A54 Katsounas A A9, A22 Kaufmann R A44 Kawelke N A10, A11 Kazakov A A15 Kefalakes H A72 Keitel V A31, A52 Keller DA A66 Kempa S A38 Keskin O A21 Kesselring R A37 Kettelhake A A38 Khairzada K A41 Khawar B A4 Kim AY A55 Kim YO A34 Kiraithe M A59 Kirchstein A A53 Kirschner J A56, A59 Klaus C A11 Kleeff J A45 Klein S A1, A4, A5 Kleinehr K A3 Kleuser B A30 Klingm!ller U A12 Kloeters-Plachky P A31 Kluwe J A20, A24 Knapstein J A50 Knauel M A12 Knierim J A19 Knocke S A53 Knodel MM A66 Knoefel WT A12 Knolle P A12, A59, A65 Knolle PA A23, A54, A67 Kn!chel R A11 Koch A A9, A21, A43, A56 Koch S A41 Namenverzeichnis | 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber Koehler BC A48 Koenig S A47 Kohlhepp M A65 Kohnke-Ertel B A42, A47 Koitzsch U A36 Kokai E A45 Kokordelis P A59 K#nig A A10 Korhonen H A15 Korn T A54 Kottilil S A9 Kraft A A57 Kr"mer B A26, A59, A60 Kraus M A56, A58, A61, A69, A70 Kraus MR A55 Krause P A47 Krawczyk M A6, A35 Kreipe H A62 Kreisel W A5 Kreuels B A60 Kristy A A27 Kronenberger B A19 Kroy D A22, A27 Kubicka S A49, A53 K!hne C A64 K!hnel F A49, A53 Kurts C A23, A54, A65, A67 Kuttkat N A13 L Laleman W A4 Lambertz D A44 Lammert F A3, A6, A10, A15, A16, A22, A24, A25, A27, A35, A50 Lang H A39, A42, A50, A52 Lang J A59 Lang P A27 Langhans B A26 Langner C A33 Laschtowitz A A71 Lauer GM A55 Laufs U A15 Lautem A A50 Lechler C A42, A47 Lee SML A35 Lehmann J A21, A25 Lehmann P A64 Leibiger K A44 Leith"user F A45 Leopold Y A31 Lewis-Ximenez L A55 Li Y A2 Liebe R A12, A16, A24 Liebscher T A20 Liedtke C A13, A40, A44, A46 Lieske S A16, A36 Liu Y A2 Llanto C A67 Locker J A42 Lohmann V A66 L#hr H A56, A58, A61, A69, A70 L#hr HF A55 Lohse A A53, A62 Lohse AW A20, A24, A54, A55, A60, A62, A68, A71 Longerich T A39, A46, A51, A52 Loscher C A66 Lu M A45 Luch A A3, A30 Luciano L A11 Ludwig-Portugall I A65 Luedde T A28, A65 Lupke M A34 L!tgehetmann M A53, A62 L!th S A54, A64 L!tjohann D A35 Lutterbeck M A3, A68 Lutz P A26 Lutz T A39, A42, A46 Luxenburger H A62 M Maasoumy B A19, A58, A64 Maass T A52 Macheleidt I A16 Mahli A A30, A32 Mai M A18 Mais C A30 Malinowski M A51, A53 Mandorfer M A18 Manka P A22, A25 Mann A A29 Manns M A44, A62 Manns MP A19, A21, A43, A49, A53, A56, A57, A58, A59, A63, A64, A65, A66, A67, A69 Manowsky J A8 Marbach E A33 Marhenke S A51 Markova AA A64 Marquardt J A37, A39, A41, A42, A50 Marquardt JU A52 Martin C A65 Martin IV A3 Martin M A37 Masing N A1 Mastrobuoni G A38 Math' Z A3 Matusch A A32 Matz-Soja M A28, A29, A33, A34 Megger DA A68 Mehrabi A A47 Meindl-Beinker N A15 Meindl-Beinker NM A52 Meissner EG A9 Melter M A7, A34 Merle U A32 Meurer SK A13 Meyer AS A46 Meyer ASK A37 Meyer HE A68 Michael MP A64 Michler T A58 Milkiewicz P A35 Missing L A32 Mix C A59 Moeller LC A22 Mogler C A49 Mohs A A13 Moldenhauer G A57 Momburg F A57 Moriconi F A8 Moro N A44 Morton CH A3 M!ller J A44 M!ller M A7, A30, A32 M!ller-Newen G A44 Mu,oz -lvarez KA A40 M!nst B A9 M!nzberg C A2 N N"gel A A66 Nakchbandi IA A10, A11 Nattermann J A26, A59, A60 Naumann U A55, A56, A58, A61, A69, A70 Neuber C A30 Neumann O A46 Neumann-Haefelin C A59, A62, A67 Neusch"fer-Rube F A30, A36 Nevzorova YA A40, A44 Nickenig G A21 Niebert S A47 Nielsen P A54 Niemietz P A65 Nierhoff D A3, A38 Nischalke HD A26 Nitschke K A62 Noetel A A16 Nordheim A A51 Nuessler AK A45 O Ochando J A65 Odenthal M A14, A16, A18, A36 Oenarto J A36 Oertel M A42 Ori A A48 Ostendorf T A3, A17 Othman A A2 Owusu SS A69 P Pannicke N A20, A60 Park O A2 Pathe-Neusch"fer-Rube A A8 Pathil A A17 Pathil-Warth A A33 Paul A A3, A25, A41 Peck-Radosavljevic M A18 Peiseler M A20, A60 Pellegrino R A46, A51 Peng J A46 Penzel R A39, A49 Perner D A71 Perrech M A16 Petersen C A11 Petersen J A53, A62 Peusquens J A65 Pfarr N A49 Pfeiffenberger J A43 Pfreundschuh M A50 Piiper A A19 Pikarsky E A51 Pilo MG A37 Pinna F A37, A38, A39, A42, A46 Piras-Straub K A41, A60 Pischke S A53, A57, A62 Plass C A47 Pl#ger C A48 Pohl S A5 Polywka S A53 Port K A19, A58, A59, A64 Pozdeev V A27 Pratschke J A21, A51, A53 Pratschke S A49 Presonil V A41 Protzer U A57, A58, A65, A71 Proudfoot Fichard A A13 Puhl G A51 Pukrop T A47 P!schel GP A8, A16, A30, A36 Pusterla T A51 Q Quaas A A36, A55 Quitt O A57 Qvartskhava N A27 R Radeleff B A20, A43 R"der M A71 Radke C A26 Raffetseder U A17 Ramachandran SD A9 Ramadori P A27 Randolph G A65 Raskopf E A41 Rath T A26 Real CI A68 Reiberger T A18 Reif R A4 Reimer R A54 Reisinger F A28 Reiter S A66 Renner M A47 Rennert C A29 Rentsch M A49 Namenverzeichnis Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A75 A76 Namenverzeichnis | 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber Reuken P A18 Ribback S A52 Richter B A14 Riedl P A45 Riemenschneider M A22 Ringel S A30 Ringelhan M A10, A45, A58 Ripoll C A5, A18 Rockstroh J A18, A60 Rockstroh JK A59 R#der R A40 Roderfeld M A14, A17, A26, A50, A68 Roeb E A14, A17, A26, A50, A68 Roessler S A37 Rohr M A64 Rolle S A21 R#ssler A A23 R#ssler S A39, A42, A46, A48 Rubner C A37 Ruemmele P A37 R!hrup J A22 Rupp AK A31 Rupp C A19, A20, A23, A31, A46 Rupp D A71 Rupp M A66 Russo C A58 S Saborowski M A49 Sage J A42, A47 Sahin A A7 Sajadian SO A45 Sales S A33 Salmen SC A54 Sander M A10 Sandmann M A55 Sanwald J A63 Saric T A16 Sarina P A27 Sarrazin C A63, A67, A71 Sass G A55, A66 Sauer I A16 Sauer P A23, A31 Sauerbruch T A1, A5, A23, A54 Saugspier M A9, A30 Sawodny O A63 Schad A A29 Schafmeier C A34 Schanze N A8, A16 Schattenberg J A50 Schattenberg JM A29 Schemmer P A20, A39, A43 Scherr AL A48 Scheurich C A55 Schewe B A30 Schiergens T A35 Schierwagen R A1, A4, A5, A18 Schildberg F A12 Schirmacher P A19, A33, A37, A38, A39, A42, A43, A46, A47, A48, A49, A51 Schirmbeck R A45 Schirmer K A9 Schirmer P A49 Schlaak JF A3, A9, A68 Schlabe S A26 Schlaphoff V A65, A69 Schlattjan M A25, A26 Schlitt HJ A37 Schlitter AM A49 Schlue J A62 Schmid RM A10, A42, A45, A47 Schmidt L A44 Schmidt SC A53 Schmidt-Heck W A28, A29 Schmidt-Wolf I A41, A46 Schmitt J A34, A35 Schneider U A11 Schneller D A51 Schoknecht T A68 Scholten D A6, A15 Sch#mig E A33 Sch#nefeld K A34 Sch#nfels W von A34 Schott E A21 Schramm C A20, A54, A55, A60, A68, A71 Schraplau A A30 Schreiber S A34 Schreiter T A23, A25 Schr#der D A68 Schuch A A67 Schueler R A21 Schulte am Esch J A12 Schultze JL A23, A54 Schulze zur Wiesch J A55, A63, A64 Schulze-Bergkamen H A48 Schulze-Osthoff K A44 Schumacher F A27 Schuppan D A34 Sch!tz E A1 Schwabl P A18 Schweinsberg V A68 Schwill F A14 Schwinge D A54, A68 Sebode M A20, A60 Seehofer D A51, A53 Seelaender M A8 Seibel P A34 Seitz HK A32 Sellge G A22, A46 Sellmann C A5 Sens C A11 Serrano BC A56 Seufferlein T A2 Sharif Z A4 Sheikh N A4, A7, A8, A24 Shen Z A2 Shevchenko A A33 Sicinski P A44 Siemers E A26 Singer S A48 Sini M A37, A52 Sipos B A45 Sitek B A68 Siveke JT A10 Skibbe K A3 Solbach P A67 Sollik L A59 Sonntag R A44 Sottile J A10 Sowa JP A22, A23 Spannbauer M A46 Spengler U A23, A26, A54, A59, A60 Spomer L A31 Springfeld C A43 Sprinzl M A50, A52, A58 Sprinzl MF A39 Stadler D A71 Staffer S A33 Stallmach A A18 Stangl M A49 Stanke F A63 Steffens H A55, A56, A58, A61, A69, A70 Stempfl T A37 Stengel S A18 Stenzinger A A47 Sterneck M A62 Sterzer V A6, A15 Stickel F A34 Stockmann M A21, A51, A53 Stokes CS A22, A25 Strassburg CP A1, A4, A5, A18, A21, A25, A26, A41, A46, A59, A60 Straub B A39, A40 Straub BK A33 Streetz K A27 Streetz KL A22 Stremmel W A17, A19, A20, A23, A31, A32, A40, A43 Namenverzeichnis Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York Stremmel WR A33 Strnad P A45 Strucksberg KH A23 Su J A17 Sunami Y A45 Sureau C A62 Susser S A71 Sutor D A34 Sydor S A23, A25, A26 Syn WK A22 T Tacke F A28, A65 Tan S A23 Targett-Adams P A66 Tebr!gge I A22 Teuber G A55, A56, A58, A61, A69, A70 Teufel A A34, A37, A52 Tewes B A5 Thalhammer J A10 Thasler W A7 Thasler WE A30, A32, A35, A43 Thavamani A A51 Thiel C A29, A33 Thies SJ A1 Thimme R A59, A62, A67 Thomas M A7, A12, A63 Thonig A A5 Thorgeirsson S A52 Thum T A44 Thurner L A50 Tiegs G A55, A57, A66 Tihaa L A13 Timm J A3, A72 Tischendorf J A22 Tischendorf S A22 Trautwein C A6, A12, A13, A15, A22, A27, A28, A40, A44, A46, A65 Trebicka J A1, A4, A5, A18, A21, A23, A25, A54 Treckmann J A23 Treckmann JW A3 Triller N A70 Trippler M A9, A68 Tschuschner A A14 Tuma S A40 U Uerlings R A32 Umgelter A A58 Unger D A43 Uschner FE A4, A5 Utpatel K A52 V Valletta D A6, A7, A9 Van de Leur E A13 van Roojen N A65 Vartak A A14 Vasel M A10 Venkata PS A69 Ventaka SP A57 Vetter D A25 Vlaic S A29 Vogel A A51, A66 Vogeser M A49 Vogt A A41, A46 Voigt E A59 Voigt L A55 Vollbrecht C A36 Vollmar N A23 Volz T A53, A62 Vondran FWR A43, A66 Vonnahme M A25 Vucur M A28 Vvedenskaya O A38 W Wagner E A40 Waidmann O A19 Namenverzeichnis | 31. Jahrestagung der Deutschen Arbeitsgemeinschaft zum Studium der Leber Waisman A A29 Waldburger N A39, A52 Waldow K A12 Walker A A60, A72 Walter S A30 Wan S A37, A39, A42, A46 Wang C A37 Wannhoff A A19, A20, A23, A33 Warth A A47 Wasmuth HE A12 Wasmuth JC A18 Waurisch C A54 Waysczak J A46 Weber B A55, A56, A58, A61, A69, A70 Weber F A68 Weber SN A3 Wedemeyer H A21, A56, A57, A58, A59, A62, A64, A65, A66, A69 Wegscheid C A57 Wei W A40 Weichenhan D A47 Weichert W A47 Weiler S A37, A39, A42, A46 Weiler-Normann C A20, A55, A60 Weinmann A A39, A41 Weiskirchen R A11, A13, A17, A32, A44 Weiskirchen S A32 Weiss C A20 Weiss KH A19, A20, A23, A31, A39, A43 Weiss TS A7, A34 Weller H A54 Welte S A48 Weng HL A2 Wenzel JJ A61 Werner J A35 Westhaus S A63, A67 Wewering F A3, A30 Wiechert L A51 Windler E A24 Winkler J A48 Winkler S A44 Wirth T A45 Wissel S A45 Witth#ft T A55, A56, A58, A61, A69, A70 Wittum G A66 W#bse M A21 W#hler C A52 Wohlleber D A59 Wolf D A25 Wolf S A8 Wolf T A42 W#lfl S A9 Woller N A53 Wolter F A59 W#rns MA A29, A41, A50, A52 Wraith DC A54 Wranke A A56 Wrba F A62 Wree A A26 Wruck C A27 Wunsch E A35 W!rger T A17 W!stefeld T A46 W!stenberg A A66 X Xia Y A71 Y Yovchev M A42 Yurdaydin C A21 Z Zachoval R A49 Zanger U A7, A12, A63 Zanger UM A12 Zehnter E A55, A56, A58, A61, A69, A70 Zellmer S A3, A30 Zender L A46 Zenouzi R A20, A60 Zeuzem S A19, A71 Zimmer V A50 Zimmermann A A32 Zimmermann T A50 Zipprich A A5, A14, A18 Zitzmann A A61 Zwank C A60 Zyriax B A24 Namenverzeichnis Z Gastroenterol 2015; 53: A1–A77 Georg Thieme Verlag KG Stuttgart · New York A77