Title Effects of powered toothbrush cleaning on acrylic resin dental
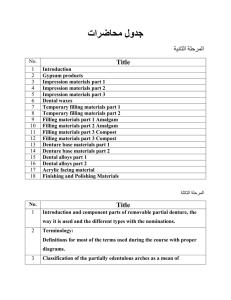
advertisement

Title Author(s) Citation Issued Date URL Rights Effects of powered toothbrush cleaning on acrylic resin dental prostheses Tan, Chow Ming.; 陳昭明. Tan, C. M. [陳昭明]. (2012). Effects of powered toothbrush cleaning on acrylic resin dental prostheses. (Thesis). University of Hong Kong, Pokfulam, Hong Kong SAR. Retrieved from http://dx.doi.org/10.5353/th_b4833471. 2012 http://hdl.handle.net/10722/174262 The author retains all proprietary rights, (such as patent rights) and the right to use in future works. Effects of Powered Toothbrush Cleaning on Acrylic Resin Dental Prostheses by Tan Chow Ming Dental Materials Science Faculty of Dentistry The University of Hong Kong A thesis submitted to The University of Hong Kong for the completion of the Master of Science in Dental Materials Science degree 1st September 2012 Declaration I declare that, with the exception of the assistance acknowledged, all the work described in this report is my own original work and that no part of it has been included in any report, thesis or dissertation submitted to the University of Hong Kong or any other institution for degree, diploma or other qualification. Signed: ………………………………… Tan Chow Ming Acknowledgements I am deeply grateful to my supervisors Dr J.P. Matinlinna, Dr James K.H. Tsoi of Dental Materials Science and Dr C.J. Seneviratne of Oral Biosciences for their guidance and supervision. I wold like thank Dr Christie Y.K. Lung, Dr Alexander T.H. Tang and Dr May C.M. Wong for their generosity in sharing their expert knowledge with me throughout my studies. I would like to extend many thanks to support staff of Dental Material Science Department Mr Tony Yuen, Mr Paul Lee and Mr Bentley Yeung and Mr Simon Lee as well as staff from Oral Biosciences Department for their assistance and help to allow the smooth running of the experiments. My appreciation to Miss. Sarah Wong for patiently guided me through the procedure in microbiology experiment and Ms Regina Chan for her ever ready excellent secretarial assistant offered. I would like to express my hearth felt appreciation to Professor Christopher Boey C.M. from Department of Paediatrics, Faculty of Medicine, University of Malaya for his constant encouragement. Lastly, I thank my colleagues for the many informal chats and suggestions offered and my families who put up with me being at my computers and laboratory late in the evenings and on many weekends. Contents Declaration……………………………………………………………………………..…………i Acknowledgements………………………………………………………………………………ii Table of Contents……………………………………………………………………………….iii Abbreviations……………………………………………………………………………………iv Part I: Literature review 1. Poly(methyl methacrylate) PMMA 1.1 Introduction………………………………………………………………....1 1.2 Chemistry of poly(methyl methacrylate)…………………………………...2 1.3 Properties of poly(methyl methacrylate) 1.3.1 Physical properties 1.3.1.1 Surface of PMMA……………………………………..11 1.3.1.2 Thermal properties…………………..………………...15 1.3.2 Mechanical Properties…………………………………………...17 1.3.2.1 Flexural strength……………………………………….18 1.3.2.2 Fracture toughness……………………………………..22 1.3.2.3 Hardness……………………………………………….23 1.3.3. Biological Properties…………………………………………....24 1.4 Processing of poly(methyl methacrylate) 1.4.1 Heat polymerization……………………………………………..25 1.4.2 Chemical polymerization………………………………………..26 1.4.3 Microwave polymerization……………………………………...28 1.4.4 Light activated polymerization………………………………….30 1.5 Mode of polymerization process and its effects on PMMA 1.5.1 Porosity in PMMA……………………………………………....31 1.5.2 Residual methyl methacrylate (MMA)………………………….33 1.6 Water storage and poly(methyl methacrylate) 1.6.1 Effect of water storage on dimensional stability………………..36 1.6.2 Effect of water storage on surface of PMMA…………………...39 2. Hygiene aspects of prostheses made of poly(methyl methacrylate) 2.1 Biofilm and plaque on dental prostheses………………………….41 2.1.1 Candida albicans biofilm………………………………..42 2.2 Denture hygiene…………………………………………………...45 2.3 Mechanical cleaning method for dental prostheses……………….48 2.3.1 Powered denture brush…………………………………..50 2.3.2 Powered toothbrush……………………………………...51 2.3.3Manual denture brushes and manual toothbrushes………55 2.3.4 Sonic and ultrasonic cleaners............................................56 2.4 Chemical cleaning………..………………………………………..58 2.5 Microwave disinfection…………………………………………....63 3. Conclusion…………………………………………………………………………..66 References.…………………………………………………………………………….67 Part II: Laboratory Report Abstract………………………………………………………………………………..84 1. Introduction………………………………………………………………………....86 2. Materials and methods 2.1 Specimen grouping………………………………………………………...93 2.2 Materials…………………………………………………………………...94 2.3 Specimens fabrication……………………………………………………..95 2.4 Polymerization and post processing……………………………………….99 2.5 Storage condition........................................................................................100 2.6 Powered toothbrush brushing protocol of specimens………………….....101 2.7 Surface roughness test................................................................................105 2.8 Flexural strength test..................................................................................106 2.9 Statistical analysis......................................................................................108 2.10 Microbiology 2.10.1 Materials and methods..............................................................109 2.10.2 Specimen grouping...................................................................111 2.10.3 Candida albicans cultured biofilm growth on specimens........112 2.10.4 Brushing protocol for Candida albicans coated specimens.....114 2.10.5 SEM of Candida albicans coated specimens...........................117 3. Results 3.1 Surface roughness......................................................................................118 3.2 Flexural strength........................................................................................123 3.3 SEM...........................................................................................................128 4. Discussion 4.1 Surface roughness......................................................................................135 4.2 Flexural strength........................................................................................137 4.3 SEM...........................................................................................................139 5. Conclusion...............................................................................................................142 Appendix.....................................................................................................................143 References...................................................................................................................161 Abbreviations PMMA: poly(methyl methacrylate) MMA: methyl methacrylate AFM: Atomic force microscopy SEM: Scanning electron microscope. EPS: Extracellular polymetric substance SFE: Surface free energy Ra: arithmetic average Tg: Glass transition temperature vol: volume ml: millilitres wt: weight kg: kilogram g: grams µg: microgram mm: millimetre μm: micrometer h: hour min: minutes s: second M: Moles PBS: Phosphate buffered saline YNB: yeast nitrogen base SAB: Sabouraud's dextrose psi: pounds per square inch MPa: megapascal rpm: revolutions per minute CAD/CAM: Computer Aided Design/Computer Aided Manufacture °C: degree Celsius W: watts Part I: Literature Review 1. Poly(methyl methacrylate) 1.1 Introduction Poly(methyl methacrylate) (PMMA) was developed 75 years ago in 1937, and is still the major material for fabrication of denture bases due to its aesthetic characteristics, high processing and polishing abilities, relining and rebasing possibility and low cost [1]. The main disadvantages of PMMA are its dimensional changes during polymerization, porosity and allergic or cytotoxic effects from leached and degraded monomers [2]. Prior to the introduction of PMMA as denture base material, vulcanite (vulcanized rubber) was material of choice in 1855 [3]. Due to its poor aesthetic qualities and taste it was replaced. Harold M. Vernon and Lester B. Vernon collaborated with the research and development team of Rohm and Haas Company in the USA and eventually formulated PMMA which is suitable for the use in dentistry and replaced vulcanite [1, 3]. PMMA popularity in use as a material of choice for the construction of dental prostheses continues even until today. The application of PMMA in the fields of medical and dental science has been expanding ever since its inception. For example, in ophthalmology, patients suffer from cataract would need the intraocular lens replacement with an artificial lens that is usually made from PMMA [4]; in orthopaedic, it is used as bone cement to anchor cemented arthroplasties to the contiguous bone [5]. 1 1.2 Chemistry of poly(methyl methacrylate) PMMA polymers are derivatives of ethylene containing a vinyl (─C═C─) group in their structural formula H₂C═CHR, where R is an organic functional group. Methacrylic acid, the precursor of methacrylate with the formula of: CH3 H2C O O OH Methacrylic acid is a polar molecule due to the present of carboxyl group. This polarity absorbs water molecules, which will tend to separate the polymer chains and cause softening and loss of strength of the polymer. The monomer of PMMA, methyl methacrylate (MMA), is the ester of methacrylic acid: CH3 H2C O O Methyl methacrylate CH3 PMMA is formed through a free radical addition polymerization process of MMA monomer. The monomers are added to the living end (with radical) of a growing chain. No change is made to the composition during the addition polymerization reaction; the monomer and polymer have the same empirical formulas. The polymerization of monomeric methyl methacrylate to form polymer of PMMA involves an exothermic reaction.An amount of heat, equivalent to 80 kJ/Mol, is released in reducing the C═C double bond to C─ C single bond. 2 The sequence of conversion from monomer to polymer involves activation, initiation, propagation, chain transfer and termination. The following is a description of the process. The polymerization of polymer PMMA is an addition polymerization process that requires a source of free radicals and the presence of an unsaturated group i.e. a double bond Free radicals are generated through activation of radicalproducing molecules by using another chemical, heat, visible light, ultraviolet light or energy transfer from another compound that acts as a free radical ( R• ). A free radical is an atom or group of atoms possessing an unpaired electron (symbol •). The process of producing free radical is called activation, for example, the decomposition of benzoyl peroxide (Fig. 1.1). The free radical has the ability to withdraw electron from high electron density double bond in monomer due to the present of unpaired electron. When the free radical approaches a double bond, an electron is extracted, and it pairs with the unpaired electron in R• to form a bond between the radical and the monomer molecule, leaving the other electron of the double bond or central carbon unpaired. The original free radical bonds to one end of the monomer molecule and a new free radical site forms at the other end. O O O O 2 O O benzoyl peroxide free radical Fig. 1.1 Activation of benzoyl peroxide to generate free radicals ( • ) 3 Benzoyl peroxide is the most often used initiator which is activated at temperature range of 50 ° C to 100 ° C to form two free radicals. These free radicals react with MMA molecule to initiate polymer chain growth (Fig. 1.2): O CH3 O + Initiation H2C H O C O O CH3 C H O O O CH3 CH3 Initiation of methyl methacrylate O H O H CH3 O C CH3 C O O H C O H O CH3 O CH3 Fig. 1.2 Initiation of methyl methacrylate molecules. An unpaired electron of a free radical attracted to one of the electron in the double bond to form an electron pair and a covalent bond between the free radical and the monomer molecule. The remaining unpaired electron makes the new molecule a free radical. In the propagation stage of the polymerization reaction, the resulting free radical-monomer complex acts as a new free radical centre when it approaches 4 another monomer to become a free radical. Polymerization continues through the propagation of the reactive centre, successively adding reactive species to a large number of methacrylate molecules (Fig. 1.3). In theory, the chain reactions are supposed to continue until all the monomers have been converted to a polymer. However, in reality, the polymerization reaction is never totally completed due to the reaction has passed exotherm and the reaction of polymerization reaches an equilibrium state [6]. The polymer chain stops to grow any longer when the reactive centre is destroyed by the termination reactions. O CH3 CH3 C H2C + O O O O O CH3 CH3 Propagation CH3 H2C O CH3 CH3 O O C O O O O O CH3 + CH3 Chain growth Repeating process. CH3 Fig. 1.3 Propagation and chain growth. When the molecule with a free radical approaches other methyl methacrylate molecules, the free electron interacts with the double bond of the methyl methacrylate molecule forming a longer free radical. 5 During the stage of chain transfer, the active free radical is transferred to a monomer or inactivated polymer chain and a new free radical for growth is created (Fig. 1.4). CH3 CH3 O CH3 C O H2C + O O O O O CH3 CH3 CH3 O chain transfer CH3 O CH3 CH3 O O O CH3 H3C C O O CH3 O + O CH3 Fig. 1.4 Chain transfer occurs when a free radical donates a hydrogen atom to the methyl methacrylate molecule. Resulted in the free radical rearrange to form a double bond and turns nonreactive, and the MMA monomer becomes a free radical. 6 The final stage of polymerization reaction is the termination which can result from chain transfer. Addition polymerization reactions are often terminated by direct coupling of two free radical chain ends or by the exchange of a hydrogen atom from one growing chain to another ( i.e. hydrogen abstraction). In direct coupling, both molecules combine to become deactivated by the formation of a covalent bond (Fig. 1.5). The exchange of a hydrogen atom from one growing chain to another growing chain produces a double bond (Fig. 1.6). O H O CH3 H H O CH3 H H3C H3C C H C + O O O O CH3 CH3 H O O O O H O H H3C H3C Termination O CH3 H3C CH3 O CH3 O O O O O O CH3 CH3 O O O O CH3 CH3 Fig 1.5 Termination of polymerization occurs when free radicals react to form stable molecule as well as a transfer process. 7 O CH3 H O H H CH3 C H O O O O CH3 CH3 H O O O O H C + O O H H H3C H3C H3C H3C Termination after chain transfer H3C O CH3 CH3 O O O CH3 O O O O O CH3 CH3 + O H O O CH3 CH3 Fig 1.6 The transfer of a hydrogen atom from a growing chain to another chain forming a double bond. Addition polymerization reactions are unlikely to completely use up all monomers; in addition, polymers of high molecular weight are not always formed. The reason for this is that the presence of inhibitors in the form of impurities retard the polymerization reaction or react with activated initiator. Inhibitors affect the storage stability and the working time of the acrylic resin. Commercial dental acrylic resins usually contain a trace amount of inhibitor such as the methyl ether of hydroquinone to prevent spontaneous polymerization during storage and the control of working time in the case of a cold-cured acrylic resin. In the three dimensional molecular structures of polymers, conformation relates to the internal movement of molecules and configuration relates to the way in which a chain is built at any asymmetric carbon. Tacticity refers to the ordering 8 of the configuration sequence of a polymer [6]. MMA monomer polymerized in system without complex steric constraints produces atactic polymer. This means the substituents in the polymer chain are randomly arranged along the chain without any regularity. In a polymer where the relative positions of the substituent are always the same along the length of the chain, the polymer is said to be isotactic. In the situation where the substituents are in an alternating configuration it is called syndiotactic. Atactic polymers cannot crystallize; they are amorphous and less brittle than crystallize materials. The constituent of the liquid consists of methacrylate based monomers, such as methyl methacrylate (MMA), hexamethylene glycol dimethacrylate (HDMA), hydroxyl ethyl methacrylate (HEMA), or n-butyl methacrylate, along with a cross-linking agent (e.g. ethylene glycol dimethacrylate, trimethylolpropane trimethacrylate, or 1,6-hexanediol dimethacrylate) [7]. However, the liquid monomer of chemically polymerized PMMA has an additional component of chemically activated accelerator, viz. N, N-dimethyl ptoluidine, which is a tertiary amine to activate the radical formation. Differences in the composition and structure of the component may influence the physical and mechanical properties of a PMMA polymer, such as tensile strength, transverse bend strength, water sorption and solubility. The MMA has a boiling point of 100.8 °C at normal atmospheric pressure and its melting point is -48 °C. This means it is highly volatile and also highly flammable. Extra precautionary measures are necessary when handling a liquid of such nature. The liquid is kept in a dark glass bottle to extend the shelf life of the monomer by preventing spontaneous polymerization from the action of light. The liquid monomer has a density of 0.945 g/mL at 20 °C temperature and the heat of 9 polymerization is 12.9 kcal/mol [8]. Traces of inhibitors such as hydroquinone are added to extend the shelf life of monomer during storage. The use of MMA as an organic solvent is excellent, however, it has proven to be highly toxic [9]. PMMA is a clear and transparent resinous thermoplastic. Thermoplastic resin refer to PMMA can be soften and shaped by heating it above its glass transition temperature (Tg). The Tg of PMMA is about 72 °C [6]. It is stable to heat with a softening temperature at 125 °C. Heat decomposition of PMMA can start to occur at temperature range of 125 ° C and 200 ˚ C, and about 90 % of polymer decompose . PMMA has a Brinell hardness number of 25 to 28 and it may be considered relatively hard. PMMA is extremely stable. It does not discolour in ultraviolet light and it has remarkable aging properties. Its tensile strength is approximately 59 MPa and its specific gravity is 1.19 g/cm³ [8]. 10 1.3 Properties of poly(methyl methacrylate) 1.3.1 Physical properties 1.3.1.1 Surface of PMMA The term surface commonly refers to a boundary define by the outer atomic layer that separate a bulk solid from an adjacent phase. However, another approach is to consider the surface as a region of variable depth and having a degree of flexibility that depends on the nature of the material [10, 11]. Material surfaces are a special state of matter with unique chemistry, organization, dynamics and electrical properties. The surface molecules have the direct access for reaction with adjacent phases and the tendency for surface energy minimization to reach equilibrium with environment. All processes for breakdown of materials are initiated at the surfaces, provided bonds within the bulk material are not disrupted. The polar or non-polar nature, the hydrogen-bonding capacity, and the electron donor or acceptor potential seem to have a controlling influence on the hydrophilic or hydrophobic character and energetic state of the surfaces of materials. The surfaces of PMMA are hydrophilic and exhibit a tendency to absorb water by a process of imbibition sorption that is due to the polar nature of the resin molecules. A positive correlation exists between the recolonization rate of bacteria and the substratum surface free energy (SFE). On surfaces with a low surface free energy the rate of bacterial recolonization is slower and the strength of adhesion on these surfaces is weaker. Low surface free energy bacteria adhere preferentially to low surface free energy surfaces (e.g. poly(tetrafluoroethylene) or 11 Teflon), and bacteria with high surface free energy prefer high surface free energy substrata (e.g. enamel). The rate of bacterial colonization of intraoral hard surfaces is positively correlated with surface roughness (SR). Surface roughness exhibits more influence on plaque accumulation and plaque composition compare to surface free energy [12]. The surface free energy of heat polymerized PMMA is 36.5 ergs/cm2, compared to Teflon which is 24.0 ergs/cm2. Surface roughness is a 2-dimensional parameter of a material surface measured by roughness measuring system such as the so-called Stylus system and is described as arithmetic average roughness (Ra). It is the arithmetic mean of the departures of profile from the mean line. It is a distance measurement between the peak and valley part of a material surface and does not represent the morphological configuration of the surface. The morphology of surface describe the pattern of a material surface such as a porous surface, grid-like surface and texture surface, it is a 3-dimensional parameter. The evaluation of surface morphology is usually carried out under scanning electron microscope (SEM) and atomic force microscopy (AFM) examination [13]. Quantitative study of a surface roughness can be analysed with a surface roughness profilometer with a diamond stylus. The profilometer will give a reading of Ra which is the arithmetic average of the absolute values of the measure profile height of surface irregularities, measured from a mean line within a preset length of specimen. The output measurement in unit µm of can be obtained when the stylus needle passing across a length of 0.8 mm at 1 mm/s. Another output reading from profilometer is root-mean-square roughness (Rrms). It has been known that bacteria react to surface topographical features which are larger than the bacterial cells. Bacteria have shown preferential 12 adherence to the bottom of the crevices rather than the top [14]. A general perception regards that rough surfaces colonize more rapidly than smooth surfaces due to more surface area available for attachment and that the greatest initial accumulation is in the bottoms of roughness elements because of protection from shear. However, it is still uncertain whether this preferential adherence at bottom of pits, in microscopic and nanoscopic scale, is a function of preferential attachment of microorganism or the end result of ineffective cleaning [15]. There are controversies as to the bacterial response to micro-scale surface features. Some studies showed that the lowest Ra value resulted in the most hygienic surfaces [16]. One study [17] recommended searching for optimal surface smoothness for all intraoral hard surfaces for the reduction of bacteria colonization and plaque formation. This was based on the investigation on standard implant abutment and surface roughened titanium implant abutment in patient subjects, which demonstrated that rough surfaces harboured 25 time more bacteria accumulation compared to smooth surface [17]. However other investigators showed that surface roughness had no effect on the number of bacteria adhered [18]. Rough surfaces can be formed through the original surfaces imprint of mould used or created through frictional abrasion using some abrasive. In the latter case, frictional work is defined as the loss of energy that leads to deformation and dissipation within the contacting element and under some circumstances mechanical or chemical damage of the interface zone. This has resulted in significant chemical, morphological, mechanical and topographical modification of the interfacial zone. Heat and debris are always produced in this interaction at the interfacial zone. 13 In the case of brushing a PMMA based dental prosthesis using a powered toothbrush, the spinning of brush head carrying the bristles can cause kinetic energy transformation where the polymer molecules on interface zone can experience bond stretching from heat energy dissipated and may result in plastic strain. Once sufficient amount of plastic strain has accumulated, this will result in the appearance of surface craze and ultimately the cumulative effect of catastrophic fracture of the bulk material under service conditions. The studies of materials revealed that the rougher the surface, the higher the surface free energy count. The more difficult it will be for the denture wearers to thoroughly clean and maintain their prostheses devoid of biofilm and plaque on the denture. The rough surface finish on the fitting surface of denture promotes the retention of Candida albicans [19, 20]. Surface roughness influences the adhesion of micro-organisms to enamel surfaces [21] and tooth surfaces [22], probably because of the greater surface area provided and the provision of protected sites for colonization. In addition, rough surface may aid mechanical retention of microorganism during the early plaque formation in the depth of surface irregularities found on enamel [23]. The valleys on the rough surface provided microorganism shield from shearing force therefore promoting the growth and survival of microorganism in plaque and biofilm on the dental prostheses. When Candida albicans was incubated on the surfaces of acrylic resin specimens, results showed more microorganisms on the rougher surfaces than on the smoother surfaces. Pre-coating denture base materials with saliva reduced Candida albicans adhesion on PMMA specimens [24]. 14 1.3.1.2 Thermal properties. Glass transition temperature of PMMA exhibits a variation of which was observed. A characteristic for all polymeric materials is the glass transition temperature (Tg), which is the temperature at which a transition to a softer and more flexible material occurs. The glass transition temperature is related to the degree of polymerization [25]. The interatomic bonds that hold the different polymer chains together contain valence electrons that continuously move back and forth. These movements of electrons cause a varying electron density that exists along the chain at different times and location. A situation of disequilibrium is created and the adjacent chains adapt their electron densities along the chain to balance these unbalanced charge densities. These interactions cause the development of interatomic induction force which is also known as van der Waals (or London forces) among the chains. These forces together with hydrogen bonding can form polar bonds between the polymer chains. These polar bonds are weaker than the primary bond along the polymer chains. The weaker polar bonds are broken when the polymer is heated to its Tg or higher temperature and this will allow the polymer molecular chains to move more freely relative to each other. The increased mobility can impact on the physical properties which include strength, modulus of elasticity and thermal expansion. At or near the Tg temperature the strength and elastic modulus of PMMA decrease, but the thermal expansion increases. Thermal conductivity of PMMA is around 6 X 10-4 •g-1•cm-2 which is considered low. The significance of this is that when heat is generated during polymerization; it can be difficult for this heat to dissipate away. As a result, temperature within the bulk material can reach above the boiling point and the 15 quality of final denture could be compromised. In the mouth, the insulating effect can lead to under stimulation of the mucosa cover by the denture plate possibly promoting the occurrence of denture stomatitis. Coefficient of thermal expansion for PMMA is high at approximately 80 ppm/°C. The linear coefficient of thermal expansion for PMMA is 76 x 10-6 / g - . Thermal diffusivity of PMMA is 0.124 mm2/sec. Colour and appearance are of considerable importance to dental prostheses end user, especially at the delivery of final finished prostheses. Every patient wants to look as naturally and aesthetically pleasing as possible with their dental prostheses in use. The ability to manipulate colour of PMMA polymeric material is a significant quality well suited for such aesthetic demand in dentistry. Colouring pigments and veins can be incorporated in the powder of PMMA, in order to make the finished product well accepted by clinician and end user. On the other hand, it may be made clear and exceptionally transparent for ophthalmology purpose. 16 1.3.2 Mechanical properties. “Mechanical properties” is a description expressing the response of a material to externally applied force in a scale-independent manner [6]. Strength of a material or a design of dental prosthesis generally refers to the mechanical property that ensures the prosthesis serves its intended function effectively, safely and for a reasonable time period. Effectively speaking, the strength is the ability of the prosthesis to resist induced stress without fracture or permanent deformation. Plastic deformation occurs when the elastic stress limit within the material is exceeded. Deformation may be observed as elastic or reversible when the force applied is within range of proportional limit of a material. Stress and strain are often used as the units of expression about the mechanical properties of a material. Stress is defined as force per unit area acting on a given plane of material. The types of stress in a functional setting for prosthesis include tensile stress, shear stress and compressive stress [8]. The average level of stress at which a material exhibits initial plastic deformation or at which fracture occurs in test specimen of the same shape and size can be defined as the strength of a material [8]. Factors that influence strength include strain rate, the shape of the test specimen, the surface finish which denotes surface flaws and the testing environment. Strain is defined as the change in length per unit original length [6]. It is the relative deformation of an object subjected to a stress. In particular, the tensile strength of PMMA is typically 50 MPa or less. The elastic modulus is low; the flexural modulus is within the range of 2200-2500 MPa [26]. Dental PMMA resins are visco-elastic materials because these materials act as rubbery solids that recover elastic deformation once the stresses induced are 17 removed. When PMMA resins are subjected to a sustained load, the materials exhibit an initial deformation, and additional plastic deformation may occur over time under continuous load. The additional deformation is called creep. 1.3.2.1 Flexural strength. The transverse strength or also known as flexural strength of a material, is a measure of stiffness and resistance to fracture. Flexural strength provides an indication of the material performance under static loading. This property would only be directly correlated for PMMA in which the elastic range extended to the point of fracture and the viscoelastic properties were not strain rate dependant. Flexural strength can be measured and calculated through performing a three-point bending test (Fig. 1.7). Fig.1.7 Schematic of a 3-point bending test. The three points are the two supports at the bottom and the central loading point on the top. 18 Impact strength is another property include in the evaluation of material. Robinson J.G. et al. [27] conducted an investigation into PMMA on these two properties by creating surface defects on specimens. They suggested that the use of small surface defects and high test rate which was 100mm min -¹ crosshead speed, would give useful information on the behaviour of denture base materials under stress. Nevertheless, the outcome of this investigation appeared to suggest that a flexural test alone was not able to fully characterize the mechanical properties of PMMA. This is comprehensible because PMMA is a type of biomaterial that is unique in many of its characteristics. For example, recently it is used in CAD-CAM milling to produce longer term intermediate implant supported prostheses. Thus, there are still potential characteristics to be discovered or to be expanded in its use. Currently, the International Standard Organization (ISO 1567) (1988) and the British Standard specification 1989 (BS 2487) for denture base resins still use the three-point bending test and have specified transverse deformation limits which are from 1 to 2.5 mm for a force of 15–35 N and 2–5 mm for a force of 15–50 N. The minimum average breaking force of acrylic resin is 55 N. PMMA has relatively weak flexural strength, with a typical value of flexural modulus of 2200 – 2500 MPa [26]. Attempts were made to strengthen it by reinforcing PMMA with incorporation of fibres, with some degree of success. The reinforcement resulted in a tougher material with high impact strength and improved fracture resistance. The incorporation of various types of fibres or beads, such as carbon [28, 29], polyethylene [30, 31] , glass [32, 33] , E-glass [34], aramid [35, 36] and poly(methyl methacrylate) [37, 38] into acrylic resin has been an attempt to improve its mechanical properties. These fibres are available in 19 various blends, e.g. continuous, woven and chopped. Metal inserts in the form of wires, meshes and plates have been incorporated into dentures in an attempt to reinforce areas potentially vulnerable to fracture [39, 40] . Flexural strength tests can reflect the loading characteristics of a denture base in a clinical situation [41]. Studies by Regli et al. and Swoope et al. [42, 43] showed that dentures in service undergo only small deformations and Ladizesky et al. [44] reported that flexural modulus should be measured at similar small deformations. The calculated flexural modulus with small deflection may be regarded as Young's (elastic) modulus of the material. Deflection of specimen during the flexural test is dependent on the thickness and type of materials [45, 46]. When comparing the actual flexure strength of various materials these factors need to be taken into account. Three-point bending test can be performed with a universal testing machine to measure the maximum load at fracture of a test material, expressed in the unit MPa. The device consists of a loading wedge and a pair of adjustable supporting wedges placed apart from each other at specified distance. The specimens may be cantered on the device where the loading wedge is set to travel at a crosshead speed of 1 mm/min or at a pre-determined rate, engaged the centre of the upper surface of specimens. Specimens are loaded until fracture occurred. 20 Flexural strength in MPa is calculated using the following formula: where 𝑭 is the maximum load (N) exerted on the specimen, 𝓵 is the distance (mm) between the supports, 𝒃 is the width (mm) of the specimen measured, and 𝒉 is the height (mm) of the specimen measured. Flexural tests can also be conducted through a four-point bending test using the same type of specimens: two loading noses are used at equal spacing from their adjacent support points, with a distance between the load points of onethird or one half of the support span [47]. The major difference between fourpoint and three-point bending test is the location of the maximum bending moment and the maximum axial fiber stress. The maximum axial fiber stress in four-point bending test is uniformly distributed between the loading noses, whereas, the maximum axial fiber stress in three-point bending is located immediately under the loading nose [48]. Comparing the three-point and four-point bending tests in measuring the flexural strength and modulus of denture base polymers, Chitchumnong et al. showed that the three-point test always gave higher values [45]. This suggested that the test method had an influence on the parameter flexural strength. In the four-point bending test, the two loading elements apply a more uniform load to the beam that prevents V-shaped buckling of the beam, and avoids stress concentrations in the midline when a single loading element is used. 21 1.3.2.2 Fracture toughness. The fracture toughness of a material is a measure of the ability of the material to resist propagation of a preformed crack. A fracture on materials always occurs by initiation and propagation of a crack. The inherent resistance against cracks propagation can be measured by introducing a crack of predetermined size and shape notch and then measuring the stress required for this crack to grow. A calculation made on a parameter known as K1c of the test polymeric material. Although determination of fracture toughness is sensitive to the specimen geometry and loading conditions, it provides two mechanical parameters namely “fracture toughness” which relates to the sensitivity of crack initiation, and “work of fracture” which relates to the resistance to crack propagation [12]. The Izod impact test is a popular method to evaluate the fracture resistance of denture base. Results of impact tests have often been used to compare flexural properties with fracture toughness. However, it was found that there are poor correlations between the impact test and flexural strength or flexural modulus results [41, 46]. Zappini et al. demonstrated that results of impact tests showed only moderate correlation with fracture toughness [12]. They suggested that fracture toughness test would be more reliable than impact tests to determine mechanical properties of acrylic denture resins. 22 1.3.2.3 Hardness The hardness test has been considered as a simple and useful method to assess mechanical properties of polymeric materials because it is very sensitive to monomer content of dental polymers [49, 50]. Hardness has been known to correlate with mechanical properties such as tensile strength for many metals [51]. For PMMA base acrylics, Vickers hardness measurement has been used to investigate changes in the surface physical properties after long-term immersion in water or in a disinfection solution [52-54]. The surface hardness was positively correlating with the flexural parameters and negatively correlating with fracture toughness [51]. 23 1.3.3. Biological properties Biocompatibility is defined as the ability of a material to perform with an appropriate host response in a specific application [55]. PMMA based resins are widely used resins in dentistry, especially in fabrication of dentures and orthodontic appliances. Other uses include bone cements, acrylic glass, and artificial fingernails and nail varnish. Literature regarding the biocompatibility of PMMA resins mainly consists of in vitro studies. Various factors in the mouth such as saliva characteristics, chewing, thermal, and chemical dietary changes may influence the biological behaviour of these materials. PMMA is considered to be biocompatible material, and it has been rigorously trialled and tested in the field of biomaterial. However, allergy may occur due to the leachable components mainly attributed to the monomers and benzoic acid [56]. Most allergic reactions are associated with cold-cured acrylic resin due to the presence of high residual monomer or benzoic acid [57]. Investigation and experiments were carried out to minimize the present of residual methyl methacrylate by subjecting the dental prosthesis to additional curing cycles but this can cause dimensional distortion as the internal processing stress are released. Lung et al. [58] investigated the curing conditions and the concentration of residual monomer, and found that the extended time at high temperature employed for polymerization would decrease the residual monomer concentration. This extended time of cure can compensate for lower processing temperature than 100 °C which is recommended by manufacturers [59, 60] . 24 1.4 Processing of poly(methyl methacrylate). 1.4.1 Heat polymerization Heat-polymerized PMMA for dental use is supplied in the form of powder polymer and liquid monomer components. The advantages of powder-liquid formulations are the ability to process by the dough technique and the polymerization shrinkage can also be minimized. The beads or granules in powder are already polymerized. Another noteworthy point for powder-liquid formulation is that the heat from polymerization reaction is reduced because a large proportion of mixture is in the polymeric form, thus preventing the potential overheating. The constituents of the power-liquid formulation are depicted in the Table 1. Table 1 Constituent of heat polymerized PMMA. Adapted from [26]. Power Liquid 1. Beads or granules of PMMA. 1. Methyl methacrylate monomer. 2. Benzoyl peroxide as initiator. 2. Hydroquinone as inhibitor. 3. Pigment and dye for colouring. 3. Ethylene glycol dimethacrylate as 4. Titanium/zinc oxides as opacifiers. cross-linking agent. 5. Dibutyl phthalate as plasticiser. 6. Nylon or acrylic, or other synthetic fibers. The heating process used to control polymerization is called the polymerization cycle or curing cycle. A well-controlled polymerization cycle can prevent the effect of uncontrolled temperature rise, such as boiling of monomers 25 or the material porosity. One technique involves processing the polymer resin at a constant temperature in a bath at 74 ° C for 8 h without terminal boiling. A second technique is processing at 74 ° C in a water bath for 8 h and then increasing the temperature up to 100° C for 1 hour. A third technique involves processing the resin at 74 ° C for approximately 2 h and then increasing the temperature of the water bath to 100 ° C and processing for an additional 1 hour. In literature there were many combinations of processing cycle studies and proposals. The purpose of such extensive investigations was aimed at minimising the presence of residual methyl methacrylate monomer [58]. The denture flask should be cooled slowly to room temperature after the completion of the polymerization cycle. Rapid cooling may result in warping due to the excessive internal stress created because of difference in thermal contraction of resin and investment medium. 1.4.2 Chemical polymerization Many terms are used to assign the same process, these include chemicalcured, cold-cured, self-cured and auto-polymerized. The chemical reaction of the chemical cure is the same as heat polymerization except that the polymerization is initiated by a tertiary amine instead of using heat. Chemically polymerized PMMA materials involve a chemical activator such as N,N-dimethyl-p-toluidine and N,N-dihydroxyethyl-p-toluidine [61]. Benzoyl peroxide is the initiator that generates free radicals. An accelerator, such as a tertiary amine, sulfinic acid, or substituted barbituric acid is required in chemically polymerized process. The most important combination is an amine– 26 peroxide redox system. The amine forms a complex with benzoyl peroxide to reduce the thermal energy required to break the initiator into free radical at room temperature. Polymerization process continues the same as heat-cured PMMA involving four stages: activation, initiation, propagation and termination. The chemical polymerization method is less efficient than the heat polymerization. The amount of uncured residual MMA in post chemical-cured PMMA is high compared to other methods of polymerization [62]. As a result, PMMA produced through chemical polymerization has a lower molecular weight and lower strength properties as well as low colour stability when compared to heat polymerized PMMA. The lower molecular weight might relate to the lowering of glass transition temperature (Tg) 70-80 °C. However, this fact remains debatable [63]. The implication for this is a material with a lower glass transition temperature which could be particularly prone to distortion when exposed to high temperatures, which may happen when hot water is used for cleaning or soaking dental prostheses. Polishing denture creates frictional heat on the surfaces of PMMA made prostheses. Such concentrated heat on the surface can adversely affect the fit of denture as a result of warpage. Dental prostheses made with chemically polymerized resins have poorer mechanical properties, including lower transverse bending strength, impact strength, fatigue resistance and abrasion resistance, than those made with heat polymerized acrylic resins. 27 1.4.3 Microwave polymerization The first report of the use of microwave energy to polymerize denture base materials was by Nishi in 1968 [64]. Kimura et al. [65] reported that it was possible to cure acrylic resin in a very short time using this technique. In some other studies [65, 66], the light fibre-reinforced plastic flask was substituted for the heavy brass flask and compress, and the water-bath curing tank was replaced with a microwave oven. The supply of microwave energy to a liquid monomer, which is polar in its nature, would cause the MMA to be oriented in an electromagnetic field. The rapid flipping of such polarized molecules is supposed to generate heat resulting from molecular friction. Free radicals are initiated and polymerization reactions with monomers may continue. The microwave heating might evenly distribute heat energy within the entire thickness of the bulk material of PMMA. There will be no concerns in regard to the excessive rise of temperature to cause boiling of monomers leading to porosity. Thus, rapid heating cycles can be used to polymerize PMMA in a shorter time compared to water-bath heating. The major advantages of the microwave heating over the water-bath heating are equal heating and rapid temperature rise throughout the bulk of PMMA material. Peyton [67] reviewed the polymerization methods and a careful control of the temperature during processing was the only important factor when all factors were considered for its advantageous use. In terms of the flexural strength, the microwave polymerized, injection-moulded, polyurethane-based polymer offered no advantage over the existing heat polymerized PMMA denture base [12]. 28 Polymerization method determines the mechanical properties of the denture base PMMA. So et al. showed that microwave heat treatment of coldcured acrylic resins with glass fibre reinforcement increased the mechanical property [34]. However, Schlosberg et al. [68] found no statistical difference between the heated water bath polymerized and microwave polymerized PMMA denture base material in term of transverse strength, Knoop hardness, density and residual monomer in test specimens. Thus, the observed beneficial improvement was with post polymerization treatment with microwave of self-curing PMMA resin. Flexural strength of selected chemically polymerized PMMA was shown to be optimised by post-polymerization microwave irradiation [69]. Microwave generated heat polymerization may also affected by, e.g. the volume of the investment gypsum, amount of water contained in the gypsum, powder/liquid ratio of the resin, thermal conductivity of the flask, and microwave translucency of the flask material. A shorter polymerization time, and less residual monomer are considered as two of the advantages of microwave polymerization [49]. 29 1.3.4 Light activated polymerization. Light activated polymerizing PMMA materials are derived partly from PMMA and partly from urethane dimethacrylates (UDMA) [70]. Photons from a light source activate the initiator to generate free radicals which may initiate the polymerization process. A visible light source is the preferred choice nowadays because of the safety concerns compared to ultraviolet light. When visible light of the blue-to-violet region is irradiated towards these materials, camphorquinone and an organic amine will generate free radicals. The supplies of free radicals are limited by such factors as light intensities, angle of illumination and distance of resin from the light source. The monomer-polymer conversion is dependent on the duration of the light irradiation [71]. Machado et al. [72] observed that heat polymerized PMMA showed less porosities in processed specimens compared to light activated polymerized denture base polymer viz. Triad VLC (Dentsply Trubyte, York PA). It has been proposed that internal porosities could concentrate stresses in the matrix and contribute to the formation of microcracks under loading. These air-filled voids presented an air-inhibited layer of incompletely polymerized matrix at the void surface [73]. 30 1.5 Mode of polymerization and its effects on PMMA 1.5.1 Porosity in PMMA. Porosity in the final processed material has a great impact on the properties of dental prostheses constructed. This can made the denture prone to fracture, easy staining with dietary colouring, promote denture plaque accumulation and finally denture cannot be fitted well. It has been proposed that internal porosities my concentrate stresses in the matrix and contribute to the formation of microcracks under loading [74]. Causes of porosity in PMMA base denture base material are attributed to factors such as polymerization shrinkage, volatilization of monomer, incorrect liquid-powder ratio and pressure application during processing, as well as thermal contraction [8]. Polymerization shrinkages or contraction porosity may happen because the density of polymer and monomer differs, and in addition to that, the intermolecular bonds change from van der Waals to covalent after the polymerization reaction. The stronger covalent bond entails a shorter intermolecular distance, hence the closer packing of polymer molecules. The calculated percentage shrinkage was found to be 21 vol.% in one study [75]. Volatilization of monomers also known as gaseous porosity is due to the evaporation of the monomer, which can happen when the temperature of heated water bath reaches temperature above 100 C. The evaporation temperature . C. Within the thicker area of dental prostheses, the added heat release from the resultant exothermic polymerization reaction will cause the temperature rising quickly above the boiling point of the monomer [8]. 31 Granular porosity occurs mainly due to the loss of monomer during mixing of the powder and the liquid monomer. It is advisable to keep the mixture of polymer-monomer dough in a tight-lid cover container before packing it into a mould which might minimise granular porosity in polymerized PMMA [76]. Thermal contraction occurs within the whole bulk PMMA material when the curing temperature changes from 100 °C to post-polymerization bench cooling temperature of C. Voids or air bubbles inclusion during mixing and packing of dough into mold can contribute to porosities in PMMA. When pressure is insufficiently applied to the moulding flask during processing, porosity may occur within cured denture. It was suggested that the screw knob on the press-flask which hold the curing flasks, needs to be tighten to 37 N m throughout the polymerization process to ensure that sufficient pressure be applied to maintain the dimensional stability and prevent porosities within the bulk material of PMMA [77]. The principle is correct; however, the 37 N m is arbitrary and may not be applicable and suitable for all situations. Porosities found on dental prostheses have many negative effects to the denture wearer such as staining, harbouring the growth of microorganisms [78] and compromising the strength of PMMA [26, 79] . A report in literature [80] suggested that porosities on dental prosthesis had favour the retention and subsequent progressive released of allergen persulfate, which is also a chemical usually present in denture cleanser to cause allergic contact chelitis. 32 1.5.2 Residual methyl methacrylate (MMA) The conversion of monomers to a polymer is never complete and some unreacted monomer call residual monomers are left in the PMMA polymer [81]. Residual monomer refers to those substances (monomers, additives, and reaction products) that are not firmly incorporated (whether reacted or unreacted) in the polymer network from which they may leach out. Monomer–polymer conversion and the residual monomer content are two essentially important aspects of leachable substances from processed PMMA. The rate of monomer–polymer conversion indicates the number of unsaturated C=C double bonds converted to saturated single C―C bonds during polymerization. The concentration of residual monomers and elutable additives are dependent on several parameters and interrelated factors such as polymerization method, polymerization cycle and post polymerization treatment [82]. It has been known that leaching of residual methyl methacrylate (MMA) can cause allergic reactions in sensitized subject. On the other hand, residual MMA can have a plasticizing effect on the acrylic resin leading to altered mechanical properties [58]. Residual MMA was found to leach out from bulk material and the amount leached was proportional to the amount of residual MMA present. Cold-cured PMMA resin leached more monomer compare to heat-cured PMMA. The major loss of residual MMA was during the the first few days of immersion but became almost constant after 2 weeks. This diffusive loss of residual MMA was also found to increase with the immersion temperature [58, 83]. 33 The amount of residual monomers in the polymerized resin was dependent on the type of the polymerization process and the amount of the monomer in the mixture ratio and the processing method [70], and especially dependent on the duration of curing [84]. The amount of residual monomers in cold-cured resin is about 10 times that of a heat-cured denture base resin, and the polymer in a cold cured-resin also has a low molecular weight [8]. Baker et al. demonstrated that detectable MMA l lv lv w 8 μg/ L x μg/ L lv y l g , the total MMA l b detected for up to one week after insertion of a cold-cured appliance with the l w l ly b g μg/ L [85]. PMMA base acrylic dentures may release MMA over long periods of time, but the level of leachable substances is difficult to detect. Studies have shown that MMA was not the only substance that was released from acrylic denture bases. Other substances that could be detected included methacrylic acid, benzoic acid, phthalates, dibutylphthalate, dicyclohexyl phthalate, phenyl benzoate, and phenyl salicylate [86], as well as formaldehyde [56]. Even though the amount released for formaldehyde was lower than MMA, its toxicity was higher [87, 88]. These reported leaching of residual MMA have shown mild to strong allergic reactions in skin-patch tests. Besides the allergenic behaviour of MMA, it was also found to be an irritant to skin and oral mucosa [89-91]. T “b g ” syndrome is a symptom related to such irritant and allergic reaction of mucosa in the oral cavity is associated to the eluded residual MMA from dental prostheses made of PMMA [92]. 34 The presence of residual monomer is inevitable. An extensive research and investigation by Lung et al. pointed out that residual monomers are an inevitable consequence of the equilibrium of a chemistry of system. Moreover, they suggested to take an advantage of the relative rates of depolymerisation and diffusive loss of monomers to attain lower values of residual MMA with a suitable choice of the processing conditions, namely time and temperature. The suggestion of a processing temperature of 95 °C and overnight processing was considered appropriate in laboratory conditions. Another suggestion from the same literature review was a processing temperature at 70 C for 7 h with terminal boiling was suggested to give the lowest value of residual monomers [58]. Residual monomers of chemical polymerizing resin decreased when post polymerization treatment with microwave irradiation was conducted [69, 93]. 35 1.6 Water storage and poly(methyl methacrylate) 1.6.1 Effects of water storage on dimension stability The American Dental Association (ADA) Specification No. 12 for denture base polymer recommends that the increase in mass of the polymer should not be more than 0.8 mg/cm2 of surface after immersion in water for seven days at 37±1°C [94]. The order of water sorption is within the range of 1.0-2.0 wt.%. The noncrystalline structure of PMMA possesses a high internal energy. This allows the molecular diffusion to occur in the resin because less activation energy is required when compared to a crystalline structure of a polymer. Polymers with crystalline structure possess a highly ordered short range structure and very strong intermolecular covalent bonds. This makes penetration of water molecules through breaking the strong intermolecular covalent bond in crystalline structure of the polymer quite impossible. Although the exact mechanism through which a PMMA polymer reaches water saturation is unknown, a 2-phase process was proposed base on the results of a study by Takahashi et al. [95]. When a denture polymer is immersed in water, soluble constituents, such as unreacted monomers, plasticizers, and initiators leach out. The resultant microvoids formed are filled with water molecules by inward diffusion. Both the outward leakage of the soluble constituents and the inward diffusion of water are time-dependent processes, and finally may reached an equilibrium state [95]. According to work the done by Braden [96], the kinetics of water sorption for PMMA follows the mathematical law of diffusion and could be described by two physical parameters i.e. the equilibrium water absorption and the diffusion 36 coefficient. The diffusion coefficient of PMMA will determine the time required for saturation in water immersion or drying out in air. Braden also found that the equilibrium value of water sorption for PMMA was independent of temperature, but the temperature has an influence on the diffusion coefficient by an increment of two times factor at the temperature range 22.5 °C to 37 °C. Water molecules may act as plasticizers in a PMMA polymer when subjected to water storage. The water molecules can penetrate into the spaces between the polymer chains and push them farther apart. Thus, the intermolecular distances of polymers increase and the intermolecular bonds, such as van der Waals forces, are weakened. As a result, the weight and volume increase to cause an expansion. The greater absorption of water by the PMMA material, the greater will be the associated dimensional change [97] and decrease in flexural strength [53]. Because the expansion effectively increases the free volume and the chain segments polymer can move about relatively easily followed by the decrease of the elastic modulus of the material. Degradation occurs in a PMMA denture base material under water storage which may be due to leaching of monomer [98]. Factors that may influence water sorption induced dimensional changes include the type of resin, thickness of material and the amount of crosslinking polymer species. For example, a heat polymerized PMMA polymer takes a longer time than a chemically polymerized polymer for water sorption to reach saturation because of the lower diffusion coefficient of water [95]. However, Arima et al. [99] found no significant differences between highly cross-linked chemical polymerizing relining resins and heat polymerizing denture base resins [50]. There seems to be little agreement as to how long PMMA polymers should be immersed prior to their mechanical testing. Although the international standard 37 guidelines [100] points to 50 hours of water immersion, Takahashi et al. [101] suggested that the equilibrium strength of some denture polymers may well exceed 30 days and they recommended a 4-month water immersion protocol whereas, the water sorption mainly occurs during the initial 14 days [95]. In the study by Chow et al. wa w w b y the linear expansion was 0.45 % [102]. 38 1.6.2 Effects of water storage on surface of PMMA Von Fraunhofer et al. [101] demonstrated that at room temperature water could absorb into acrylic denture base material and cause changes in microhardness of the surface. Absorption of water into PMMA resins is facilitated by the polarity of poly(methyl methacrylate) molecules; water molecules penetrate the mass and occupy position between the polymer chains. A craze is a localised region of plastic deformation of polymer which may be filled with small voids. As the voids in the crazed region grow these tiny voids become separated by thin fibrils of polymer, ultimately the fibrils fail and a crack is formed. In fact, the mechanism of crazing found on these surfaces is related to solvent attack and water sorption. PMMA is saturated with water through the process of water sorption, once it is exposed to dry environment, drying will take place progressively from the surface extending into the depth of the full thickness of bulk material. This can result in a water concentration gradient within the bulk material of PMMA. The concurrent effect of drying is the shrinkage of material on the air contacting surfaces. The outward surfaces are dry while the internal section is wet, which fact can lead to build up of tensile stresses on the surface that, on the other hand, can cause surface crazing through action of solvents such as MMA. PMMA processed dental prostheses which are totally well soaked in water or thoroughly dry, will be free from the surface crazing effect. Crazing generally begin at the surface of PMMA resin and is oriented at right angles to tensile forces. Micro cracks formed in this manner will progress internally from the surface into bulk material. Heat generated during polishing of 39 dental prosthesis, different contraction around metals component or attack by solvents such as alcohol may lead to crazing. Zappini et al. [12] reported that the fracture pattern of Lucitone® 199, a denture base through heat polymerized PMMA, exhibited large amounts of permanent deformation and crazing before fracturing. Crazing on surface of PMMA material would promote an ultimate material fracture. Precaution taken to stop crazing can extend the service life of a PMMA made denture. 40 2. Hygiene aspects of prostheses made of poly(methyl methacrylate). 2.1 Biofilm and plaque on dental prostheses In the oral cavity, an acquired pellicle forms rapidly on non-shedding surfaces. This acquired pellicle is composed of primarily host derived salivary substances which include high molecular weight mucins. This is to be followed by a microorganism adhering to a component of the acquired pellicle and thus denture plaque accumulates through continuous adhesion, aggregation, and growth of attached microorganism on the denture surfaces [103]. Biofilms are defined as microbial communities encased in a matrix of extracellular polymeric substance (EPS) and, displaying phenotypic features that differ from their planktonic or free-floating counterparts [104]. The plaque and biofilms on a denture or dental prostheses are composed of a complex mixture of fungi, bacteria and desquamated epithelial cells from the host. This biofilm acts as a protective reservoir for oral microorganisms. Studies have demonstrated that different species of oral and non-oral pathogens are associated with denture plaque. These include Candida spp., Staphylococcus spp., Streptococcus spp., Lactobacillus spp., Pseudomonas spp., Enterobacter spp. and Actinomyces spp.[105, 106]. Mature biofilm on natural and denture teeth may have similar total numbers of bacteria but different species proportions [107]. The continuous swallowing or aspiration of micro-organisms from denture plaque may pose a risk of upper respiratory tract infection in vulnerable group such as immune compromised patients or debilitated elderly people [108]. Nikawa et al. (1998) proposed the term ‘ l q ’ which should be used because the microbiota and its pathogenicity of denture plaque resemble 41 those of dental plaque formed on the tooth surface. Moreover, they suggested that ‘ l ’ w l b red ‘ ’, because the inflammation of (palatal) mucosa is not induced by the denture, but by wearing the denture or by plaque accumulation on the denture [109]. In view of these facts presented, the efficient mechanical plaque removal is one of the important oral health measures to prevent the onset and progression of denture related diseases for individuals. 2.1.1 Candida albicans biofilm The development of a Candida biofilm consists of four steps. The first step is the adhesion of a microorganism onto a surface [110]. The second involves discrete colony formation, and organization of cells. The third step is the secretion of extracellular polymeric substances (EPS) and maturation into a threedimensional structure. The final step is the dissemination of progeny biofilm cells. Some studies have reported that Candida biofilm formation on PMMA occurs in three phases namely an early phase, intermediate phase, and the maturation phase [111]. The early phase was characterized by the presence of adhering and developing blastospores into distinct microcolonies. Intermediate phase can be seen between 18 to 24 h and the Candida biofilm appears as a mixture of yeasts, germ tubes, young hyphae and an extracellular polymeric 42 substance (EPS). The mature Candida biofilm consists of dense network of yeasts, pseudohyphae, and hyphae embedded in a thick EPS layer. Fig. 2.1 Scanning electron micrograph of different morphology of Candida albicans on surface of PMMA specimen. Denture wearers harbour the growth of Candida albicans when the hygiene practices and maintenance standard are poor. The prevalence of Candida albicans present on denture was reported by Meurman et al. at 78.4% of the population [112]. Denture plaque containing Candida may cause denture-induced stomatitis, oral candidiasis, as well as Candida-associated caries, and periodontitis of 43 abutment teeth. However, only limited evidence is available on the cariogenic potential of Candida [113]. The presence or absence of dental prosthesis determines the prevalence and concentration of Candida in different sites of the oral cavity. In healthy denture-wearing carriers Candida is found distributed on the dorsum surface of tongue, fitting surface of the upper denture and in some cases the palate [114]. Evidence from previous studies showed that presence of dental prostheses [78] or removable orthodontic appliances [115] increases the density of Candida colonization in all sites in the oral cavity. A major clinical implication of Candida biofilm is its higher resistance to antifungal agents [116-118]. 44 2.2 Denture hygiene The purpose of denture hygiene practise is to minimize or totally eliminate the fungal and bacterial attachment and activity on dentures, in addition to reducing food-related stains on the denture surfaces. This would prevent the occurrence of denture stomatitis on the oral mucosa covered by the denture [119]. Denture cleaning may be divided into mechanical cleaning method and chemical cleaning methods [120, 121]. A mechanical cleaning method such as brushing or the use of ultrasonic water bath are the most effective means in removing denture-plaque and biofilms from the surfaces of dental prostheses. Qualities of a good denture cleaning agent are: ease of use, effective removal of deposit on surfaces of denture without damage to the denture, bactericidal and fungicidal, non-toxic, non-irritant, chemically defined and stable, regulatoryapproved on a global basis and cost-effective [122]. Chemical cleaning methods using denture cleansers are popular among the denture-wearers for the prevention of colonization by Candida albicans and related Candida species, as well as to impede denture plaque formation. Effective plaque removal from soiled dental prostheses from a period of in-service use requires a degree of manual dexterity that is often lacking especially among elderly patients and those individual who are ill and frail [123]. The value of good dental and denture hygiene, as shown in a systematic review by van der MaarelWierink et al. [124] in the frail older people, could reduce aspiration pneumonia. Another systematic review on the subject of cleaning denture for adults by Souza Raphael et al. pointed out that no evidence conclusively states that any denture cleaning method is more beneficial for the health of denture bearing areas 45 ’ and preference when compared with each other [124, 125]. There is a lack of evidence on this subject of effective denture cleaning method. Professional denture hygiene instruction goes hand in hand with the advanced designs of devices in achieving an optimal effect on denture hygiene practice. The same has been shown in the study on maintaining dental hygiene. When professional instruction was not given, the potential of the electric powered toothbrush was underutilized, compare to the manual toothbrushes [126]. Currently, a plethora of information from various sources contributes to the controversy of the easiest or most effective cleaning method to maintain denture hygiene and much of it can be controversial. There is a need in this field of studies to clear this confusion, and this current investigation at hand may help to advance the understanding on the subject of mechanical cleaning methods one step further. A study conducted by Sumi et al. pointed out that elderly people may have difficulty in mechanically removing dental plaque due to diminished manual dexterity, impaired vision, or ill .T l ’ bl y perform self- care gradually decreases with advancing age, and the role of the caregiver in daily oral care becomes increasingly a necessity. However, optimal oral care by caregivers is not always possible because of the time constraints, difficulties involved in brushing other individuals’ ,l k , and the lack of perceived need. The recognition of this issue faced by the elders and care givers have prompted them to make a device through modification of a powered toothbrush. The results from their investigation were positive and promising, 46 especially in helping those concerned subjects and care givers to achieve good dental plaque control [127]. Briefly, the use of a powered toothbrush is not just an aid to the elderly, it can help the care givers substantially in delivering better services as well. Denture hygiene practise may further improve from the use of powered devices such as powered toothbrushes. No quantitative and qualitative investigation on the positive contribution from such usage is yet reported. 47 2.3 Mechanical cleaning method for dental prostheses Brushes of various designs and made are use in the mechanical cleaning method (Fig. 2.1). Broadly, they can be classified into manual and powered brushes plus the sonic cleaners. The mechanical movement of bristles perpendicular to the surface of dental prostheses creates a scarping motion to get rid of the layer of an attached biofilm. The efficacy of brushing with regard to plaque removal is dictated by three main factors namely the design of the brush, the skill of the individual using the brush and the frequency and duration of use [128]. 48 Varieties in Bristles stiffness, form and arrangement. Size and shape of head & handle design. Manual denture brush Manual toothbrush Brushes for cleaning dental prostheses Powered denture brush Powered toothbrush Direct Replaceable batteries Rechargeable batteries Power source Motion of head Reciprocating Dual motion Arcuate Circular Vibratory Sonic Ultrasonic Fig. 2.1 Diagram showing types of brushes for cleaning dental prostheses. 49 2.3.1 Powered denture brush The powered denture brush is a purpose-designed and manufactured device, commercially marketed in the United States. The designer Jim Harrison found that denture wearers often lacked the ability, knowledge or dexterity to maintain the hygiene of their prostheses. He conceived of the idea for a purposedesigned powered denture brush from a manual denture brush. He and his team members designed and developed the Power Dent Pulse™, the brand name of the powered denture brush. It looked like a manual denture brush except with a large handle to hold batteries. To date, no research has been conducted to investigate efficacy on denture plaque removal and the influences that may impact on the properties of acrylic resin of its usage. This investigation initiated intends to explore the gap in this area of research by means of using the battery powered toothbrush which has a simple rotational movement bristles head. 50 2.3.2 Powered Toothbrush The origin of powered toothbrushes date back to the 18th century. They were originally designed as a mechanical toothbrush [129] by a Swedish l k k D S ’ l b [130], but it was not until the 1960s that electrically powered toothbrushes were introduced [131] and became established as a preferred alternative to manual toothbrushes. These designs ‘b k ’ l l b . Powered toothbrushes have been indicated for young children, handicapped or patients with special needs who lack the dexterity to brush manually. Patients wearing fixed orthodontic appliances and hospitalized or institutionalized patients who need a care worker or nurse to carry out oral hygiene, would benefit from using powered toothbrushes. A powered toothbrush may also be considered for any individual who wish to improve the tooth brushing technique and enhance interest in the oral hygiene practice. It may increase motivation and compliance with oral and denture-hygiene measures. It is desirable to extend these benefits to individuals wearing dental prostheses through the use of powered toothbrush as a mean of mechanical cleaning to remove accumulated plaque and biofilm. Mechanisation of tools, in any form, is certain to produce some form of efficiency in the process application. There is currently a favourable trend in the continuing advancement and improvement of devices of personal hygiene in general, and oral or denture hygiene. The parts of powered toothbrush consist of a head, bristles and a handle which house the batteries. The head which is connected to the shank is detachable from the handle and also replaceable. In general, power toothbrush heads are 51 smaller than manual toothbrush heads. They are available in a full size or a compact size head. The shape of a replaceable head may be circular, rectangular or diamond-like. The bundles of bristles are arranged either in rows (as for a conventional toothbrushes) or in a circular pattern mounted in a rounded head. Bristles are also arranged as more compact single tufts which facilitate interproximal cleaning and brushing in less accessible areas of the mouth. Bristles used in the manufacturing of brushes for personal hygiene maintenance are commonly made of nylon e.g. Tynex® by DuPont. The hardness or stiffness, end-rounding, shape and type of bristles have influences on the efficacy of plaque removal from surfaces. The factors such as the material, length, thickness, compactness and tip geometry of bristles, might affect abrasion by tooth brushing. The same brushing abrasion effect is accurately correlated in tests carried out on PMMA ’ surfaces as well. The motion of the brush head includes a multitude of different movements e.g. reciprocating, circular and sonic vibratory. Some advance models (e.g Vitality™ Dual Clean by Oral-B, Proctor & Gamble) may be a combination of two types of motion. Range of sonic vibration is 18,000 to 32,000 brush strokes per minute. The speeds at which the head or the bristles move differ according to the designs of powered toothbrushes. The number of strokes per minute varies from, for example, as low as 1,000 cycles per minute for a replaceable battery type, to about 3,600 oscillations per minute for an arcuate model. The ultrasonic bristles vibrate at 31,000 brush strokes per minute. 52 The power source that supply direct current to the powered tooth brushes is commonly replaceable batteries or rechargeable batteries. The force applied during the use of power toothbrush for brushing teeth in the mouth is less compare to manual toothbrush [132]. Findings of van der Weijden [132] showed that the force used with an electric powered toothbrush was significantly less than with a manual brush when performing tooth-brushing. They also recorded the forces loads for powered toothbrushes which were in the range of 80-90 g and in the 250 g when manual toothbrushes were used. A contemporary powered toothbrush may feature a pressure sensor to avoid gingival trauma from overzealous brushing. Pressure sensor incorporated into a powered toothbrush enables the user to self-adjust the applied force-pressure when brushing force is over the pre-set limit. The brush head flexes back with an audible warning buzz and light when a predetermined brushing force threshold is breached. A timer is incorporated in some powered brushes to allow the users beware of the time recommended for tooth brushing and not exceed the duration. Many studies [59, 133-135] attributed the harmful and undesirable adverse effects of tooth brushing to prolonging as well as to a longer accumulated total time of brushing. These features can help to minimise the damaging effects of surface abrasion and surface wear of substrate caused by brushing. Tooth brushing abrasion is influence by variables such as the frequency of brushing, the force applied during brushing, the characteristics of bristle, the bristle stiffness and the end-rounding of bristle ends [18]. 53 The subject of abrasion to dental hard tissue and gingiva is an inquiry that challenges many researchers to find a reliable conclusion. The same is true for the effects of denture hygiene practice impact on the surface quality of dental prostheses. There is still some debate about the conclusions made. However, unequivocal consensuses among the investigators have concluded that the brushing of dental prostheses using brush with toothpaste can abrade the surface of acrylic resins [57, 136]. Factors that were attributed to abrasion include frequency of brushing, applied brushing forces, bristles characteristics such as stiffness and end-rounding, and composition of dentifrice used [18]. Brushing PMMA specimens using a powered toothbrush with water alone did not cause increase in surface roughness [136]. The linear motion of bristles caused more wear and abrasion on PMMA specimens compare to rotary motion of bristles [137]. According to a previous study, the occurrence of a polishing effect on resins may be possible when the denture was brushed using a toothbrush with low abrasion toothpaste [138]. Cleaning and brushing teeth using powered toothbrushes have been proven to reduce dental plaque and gingival bleeding score in clinical trials. A powered toothbrush is effective and efficient compared to the use of manual toothbrushes in reducing dental plaque score [139]. However, there were inconclusive findings from other investigators stating that there was no different in efficacy between powered toothbrushes and manual toothbrushes [140]. This may be due to differences in experimental designs and conditions [18]. 54 2.3.3 Manual denture brushes and manual toothbrushes These mainly consist of purpose-designed denture brushes with a large and a small bristles area opposing each other back to back. The longer, circularly arranged tufts of bristle are used to clean the tissue surface or small hard-to-reach surfaces of the denture. The flat rectangular portion is used for cleaning the polished and the occlusal surfaces. A regular toothbrush with regular stiffness of bristles can be used for cleaning dentures as long as its design permits access to all the surfaces of dentures. These toothbrushes are easily and readily available alternative means to clean dental prostheses, as well as conveniently within reach and comparatively cheap for the public. The difficulty to adapt a regular size toothbrush into the recesses and curves of the fitting surface may sometimes result in an inadequately clean denture. The choice of bristles on any toothbrush used for dental prostheses cleaning should neither be too soft nor too hard in stiffness. The use of a toothbrush with hard bristles and excessive pressure during overzealous brushing can result in damaged surfaces of PMMA denture base material to the extent that the fit and aesthetic of the prosthesis may be compromised. The physical and mechanical properties can be adversely affected as a consequence, which may lead to a catastrophic fracture which may happen below a normal load of function. 55 2.3.4 Sonic and ultrasonic cleaners Sonic and ultrasonic devices are mechanical aids generally used by the dental professionals. A chemical solution may be used together with an immersion medium to increase the efficacy. Sonic cleaners operate through the generation of audible sonic energy wave; ultrasonic cleaners operate by means of highfrequency sound waves. The processes are generally known as sonication where particles are dislodged from adhering to surfaces. The sonic type of cleaners are more common among the general population and they produce less mechanical agitation of solution than do the ultrasonic found in most dental operators. It has been reported that ultrasonic sonic cleaning done in the dentist’ office was more efficient in plaque removal than either a commercial chemical immersion cleanser or a sonic cleaner at home [141]. There are two mechanisms of action proposed for ultrasound generated cleaning, the first being the movement of liquid resulting from sound waves transferred to the liquid (vibration), and the second, the cavitation and collapse of bubbles formed by vibration of the unit [142]. Budtz-Jorgensen et al. reported that although ultrasonic treatment by itself did not reduce the number of microorganisms that could be cultured from soiled dentures, it did enhance the effectiveness of disinfecting solutions in which dentures were immersed during the ultrasonic treatment [143]. There is disagreement as to the effectiveness of these mechanical cleaners in reducing plaque on denture. The effectiveness of ultrasound generated cleaning is contradictory; it may be attributed to the mechanical action of the device [144] or to the chemical solutions used [141]. The combination of an ultrasonic cleaning 56 method with brushing or with a chemical immersion method has been suggested as an effective alternative for cleaning complete dentures; however, this effectiveness has not been clinically tested [145]. 57 2.4 Chemical cleaning The use of chemical solutions for soaking dental prostheses is a popular alternative to mechanical cleaning. It requires less effort and compliance from individuals and the solution may reach surfaces on the prostheses that may be inaccessible to denture brush. Commercial denture cleansers are classified into the following groups: neutral peroxides with enzymes, enzymes, acids, hypochlorites, peroxides, crude drugs, and mouth rinses for dentures [121, 146] . Denture cleansers are widely used to prevent colonization by Candida albicans and related Candida species, and to prevent denture plaque formation in addition to the primary function of plaque removal from dentures [147]. Daily use of denture cleansers as proposed by Palenik et al.[141], if inappropriately done by ill-informed individual, can affect the physical and mechanical properties of the PMMA denture base materials. For some individuals or in circumstances that could raise the concern of safety issues, it may be best to avoid any use of such chemicals or microwave irradiation disinfection. A case in point may be the incapacitated seniors with concomitant dementia and frail condition. Simply brushing a dental prosthesis with a suitable powered toothbrush and water could possibly be a more viable and safer choice in such a situation. Sodium hypochlorite is effective as a denture cleanser or disinfection agent because of its ability to dissolve organic material which is made up of accumulated biofilm on the dental prostheses. It is bactericidal and fungicidal which can fulfil the objective of disinfection of dental prostheses. However, it is not suitable for dental prostheses with metal components due to corrosion of these metal parts. Dental prostheses should be soaked in a hypochlorite solution for 58 only 10 to 15 min and not over night because hypochlorite has an unpleasant taste and odour. Bleaching of an acrylic resin denture by sodium hypochlorite has been reported by McNeme et al. [148] and Moore et al [149]. No matter how brief the contact time between the metal components, much as the low concentration of hypochlorite used, the cumulative effect of regular long term use cannot be underestimated. Glutaraldehyde disinfection of acrylic resin denture was investigated by Polyzios et al. [150]. They used a microwave energy polymerized PMMA specimens immersed in a solution of 2% alkaline glutaraldehyde (Cidex-7, Johnson & Johnson. East Windsor, NJ) for 1 h or 12 h. They had compared the chemical method vs. using microwave irradiation disinfection with respect to the dimensional stability, flexural properties and hardness of acrylic resin. Their results showed that flexural properties were not affected by these two methods of disinfection. However, contacting glutaraldehyde on eyes or skin can cause irritation (American Dental Association, 1985). There is also possibility of some residual solution in the acrylic resin because of the porosities found on the surfaces of prostheses. It is important that the selection of the disinfection solutions should be based on its disinfection effectiveness and compatibility with the oral tissues. Shen et al. studied the effect of two glutaraldehyde base disinfectants, namely alkaline and phenol buffered, on flexural strength and rigidity of denture base resins and reported that the flexural strength was not affected by immersion time or the type of disinfectant used [151]. The alkaline and neutral peroxides act through an oxygen-releasing mechanism, which loosens debris and removes light extrinsic stain on surfaces. The effervescent tablets sold over-the-counter belong to this group. When these 59 agents are added to water they produced an alkaline solution of hydrogen peroxide [152]. This peroxide solution subsequently releases oxygen and the oxygen bubbling effect would enable minor mechanical cleaning [143]. The oxidising agents incorporated can remove extrinsic stain and serve as antibacterial agents. A study by Nikawa et al. revealed the ability of the peroxide cleansers to decrease Candida albicans biofilm activity [146]. The use of the peroxide preparation on a regular basis may help to prevent the formation of stain and calculus if accompanied by brushing and rinsing. In some commercial formulations enzymes may be added to ‘enhance’ their antibacterial action. Enzymes are effective in destroying the plaque matrix and allowing the accumulated plaque be easier brushed or rinsed off [153]. This type of chemical cleaning is generally considered as safe and effective for cleaning all type of dental prostheses including those with metal components. However, precaution needs to be taken seriously, not to ingest the tablets by accident. The elderly or visually impaired may mistake the tablets as antacid tablets and small children may be vulnerable as well. The proper care of denture-soaking container is critical in a situation where the critically ill individual is with suppressed immunity. The chemical soaking solutions can serve as growth media for pathogenic microorganisms that are formed on dental prostheses. Well cleaned dental prostheses may be recontaminated when placed in the holding containers with such solutions. The recontaminated dental prostheses may become a source of infection for such patients. The hassle of cleaning the holding container and discarding the soiled solution is a pertinent issue well worth the effort to be carried out conscientiously. 60 Diluted acids are used as aids to clean dental prostheses. They include 3% to 5 % hydrochloric acid with or without phosphoric acid, and clear coloured household vinegar. An acid solution dissolves the inorganic material which accumulated on the dental prostheses and is good for the removal of persistent stains not removed by regular cleaning methods. These acids should be handled with extra care. The ability of acids to corrode metals is a disadvantage that limits their use to prostheses without any metal parts. Chlorhexidine is commonly prepared as the digluconate or acetate salt in suitable concerntrations in aqueous solutions. Chlorhexidine destroys bacteria by breaking their membranes and inducing cytoplasmic precipitation [154]. It is a cationic molecule capable of interacting with inorganic human dentine particles and it also bonds to negatively charged surfaces, such as the bacterial cells wall [155, 156]. Chlorhexidine gluconate is an antiseptic agent with a broad spectrum of antimicrobial activity including Candida albicans and other common nonalbican Candida species [157, 158]. Chlorhexidine gluconate at concentration 0.12% with immersion duration of 15 min and 2.0% with an immersion duration of 5 min have been shown to be effective for denture cleansing in clinical trials, compared to using water as the control [159]. A major drawback with chlorhexidine is extrinsic staining on dental prostheses after a repeated use, making it unsuitable for a daily routine use. As the facts presented demonstrate that chemical method still fall short of ideal cleaning and the inherent shortcomings of chemical contain within these cleansers, therefore, chemical denture cleansers should be used as an adjunct with 61 other methods of cleaning. In vivo studies are lacking the information whether the daily use of a cleanser may cause mucosal irritation and allergy [80]. Comparison on efficacy of the various denture-cleaning products is difficult due to the lack of research studies comparing a variety of products used on dentures in vivo. Available research results are difficult to compare because of the wide variations in materials and methods as well as in the quantification of results. Nikawa et al.[121] had attempted discussion on this subject and suggested a recommendation addressing this issue on comparing efficacy of the denturecleansers. 62 2.5 Microwave disinfection. The use of a standard microwave oven as an efficient method for cleaning and disinfecting denture was first suggested by Rohrer and Bulard [160]. The proposed mechanism for the action of disinfection was the thermal effect and the non-thermal effect. The thermal effect on Candida albicans was studied by Campanha [87] and it led to a suggestion that the direct effect of heat could alter cell structures, modify cell membrane permeability and cause cell death. The effects are the direct causes of heat generated by microwave radiation upon the organic matter. The non-thermal effect involved the destruction of microorganisms at a temperature lower than the thermal destruction point [88]. Microwave irradiation is selectively absorbed by certain biochemical molecules such as proteins, nucleic acids and protein-lipopolysaccharide compounds of cell membranes which can lead to cell destruction [161]. It seems that the microwave disinfection is simple, easy to use, effective, quick and a cheap method for the denture disinfection [162, 163]. The incidence of drug induced resistance for fungi and other microorganism can be eliminated. However, it cannot be used if the dental prostheses contain any metal components. Water and other solution have been used as media during microwave disinfection of prostheses to prevent detrimental dimensional and structural changes [160]. It was suggested that placing the dental prosthesis in a cup of water to obtain an even distribution of heat was more effective for disinfection [164]. Furthermore, the microwave energy might be able to further cure the denture and alter the mechanical and physical properties, such as hardness, flexural strength and colour of the denture [34]. Therefore, many other relevant points are to be considered before embarking on this method of cleaning dentures. 63 Studies suggested that the exposure time required for microwave disinfection ranges from 1 min to 20 min and the power setting varies from the low of 350 W to the high of 800 W [60] and the immersion media used during microwave irradiation disinfection may include water [164] or sodium hypochlorite. A point of concern is that such heated liquid could possibly pose a danger of scalding to an individual especially aged and frail. Controversy and mixed result still appear in reported experiments when dentures have been colonized by microorganism in laboratory compare to when it is taken directly from the patient’s mouth [165, 166]. Both short term and long term effects of microwave use on denture materials are inconsistent and no consensus has been agreed on an acceptable standardised protocol for the microwave oven therapy. There still exist potential risk for causing structural damages to PMMA denture base material on its application [60]. The adverse effects of microwave irradiation on the mechanical properties of PMMA depend on the duration of exposure, the power setting of microwave oven, immersion solution, frequency of use and the polymerization process whether auto or microwave. The efficacy of microwave disinfection of the dental prostheses seems to be temporary, re-infection and re-growth of plaque biofilm can readily occur as the mouth remains contaminated. It seems unreasonable to microwave a dental prosthesis daily or a few times a week as a replacement for regular brushing. When regular cleaning is performed prior to microwave disinfection, the results tend to favour better disinfection and denture related stomatitis control [60]. 64 Residual biofilms remaining on oral mucosa could lead to fungal regrowth and re-colonization, regardless of how thoroughly cleaned the prosthesis is when putting it back in the mouth. The oral mucosa needs to be swabbed clean as well which implies the prosthesis is off the mouth and cleaning with liquid soap and a powered toothbrush is a logical action step to achieve a better denture plaque removal. The present philosophy of making a killing of microorganism requires a balanced thinking of sustaining a reasonable length of material life span through guarded material deterioration. There is an increasing acceptance of the hypothesis that the microflora should not be eliminated but should instead be prevented from shifting from a favourable ecology to an ecology favouring oral disease [167]. 65 3. Conclusion The use of battery powered toothbrushes as a mean of mechanical cleaning method of PMMA prostheses has a good potential to be promoted as a good and safe device, especially for the elderly patient and their care-takers. The use of such devices requires judicious care and consideration from the dental health care providers and the end users. Both professionals and patients are definitely in need of quality information to assist to make a well informed choice from the great varieties of options on brushing devices available on the market. 66 References 1. Murray, M.D. and B.W. Darvell, The evolution of the complete denture base. Theories of complete denture retention — A review. Part 1. Australian Dental Journal, 1993. 38(3): p. 216-219. 2. Polyzois, G.L., In vitro evaluation of dental materials. Clinical Materials, 1994. 16(1): p. 21-60. 3. Rueggeberg, F.A., From vulcanite to vinyl, a history of resins in restorative dentistry. The Journal of Prosthetic Dentistry, 2002. 87(4): p. 364-379. 4. Werner, L., Biocompatibility of intraocular lens materials. Current opinion in ophthalmology, 2008. 19(1): p. 41-49. 5. Charnley, J., Anchorage of the femoral head prosthesis to the shaft of the femur. Journal of Bone & Joint Surgery, British Volume, 1960. 42-B(1): p. 28-30. 6. Darvell, B.W., Materials Science For Dentistry. 8th ed2006, Hong Kong: B W Darvell. 7. Hong, G., H. Murata, Y. Li, S. Sadamori, and T. Hamada, Influence of denture cleansers on the color stability of three types of denture base acrylic resin. The Journal of Prosthetic Dentistry, 2009. 101(3): p. 205-213. 8. Anusavice, Phillips' Science of Dental Materials Elevents Edition ed2003, St. Louis: Saunders. 9. Dahl, O.E., L.J. Garvik, and T. Lyberg, Toxic effects of methylmethacrylate monomer on leukocytes and endothelial cells in vitro. Acta Orthopaedica, 1994. 65(2): p. 147-153. 10. Klauber, C. and R.S.C. Smart, Solid system: Their structure and composition, in Surface Analysis Methods in Material Science, S.B. O'Connor DI, Smart R St C, Editor 1992, Springer-Verlag: Berlin. p. 3-65. 11. Faot, F., M.A. Costa, A.A. Del Bel Cury, and R.C.M. Rodrigues Garcia, Impact strength and fracture morphology of denture acrylic resins. The Journal of Prosthetic Dentistry, 2006. 96(5): p. 367-373. 67 12. Zappini, G., A. Kammann, and W. Wachter, Comparison of fracture tests of denture base materials. The Journal of Prosthetic Dentistry, 2003. 90(6): p. 578585. 13. Kakaboura, A., M. Fragouli, C. Rahiotis, and N. Silikas, Evaluation of surface characteristics of dental composites using profilometry, scanning electron, atomic force microscopy and gloss-meter. Journal of Materials Science: Materials in Medicine, 2007. 18(1): p. 155-163. 14. Characklis, W.G., Bioengineering report: Fouling biofilm development: A process analysis. Biotechnology and Bioengineering, 1981. 23(9): p. 1923-1960. 15. Scheuerman, T.R., A.K. Camper, and M.A. Hamilton, Effects of Substratum Topography on Bacterial Adhesion. Journal of Colloid and Interface Science, 1998. 208(1): p. 23-33. 16. Whitehead, K.A., J. Colligon, and J. Verran, Retention of microbial cells in substratum surface features of micrometer and sub-micrometer dimensions. Colloids and Surfaces B: Biointerfaces, 2005. 41(2–3): p. 129-138. 17. Quirynen, M., H.C. Van Der Mei, C.M.L. Bollen, A. Schotte, M. Marechal, G.I. Doornbusch, I. Naert, H.J. Busscher, and D. Van Steenberghe, An in vivo Study of the Influence of the Surface Roughness of Implants on the Microbiology of Supraand Subgingival Plaque. Journal of Dental Research, 1993. 72(9): p. 1304-1309. 18. Heasman, P.A. and G.I. McCracken, Powered toothbrushes: a review of clinical trials. Journal of Clinical Periodontology, 1999. 26(7): p. 407-420. 19. Samaranayake, L.P., J. McCourtie, and T.W. MacFarlane, Factors affecting the invitro adherence of Candida albicans to acrylic surfaces. Archives of Oral Biology, 1980. 25(8–9): p. 611-615. 20. Verran, J. and C.J. Maryan, Retention of Candida albicans on acrylic resin and silicone of different surface topography. The Journal of Prosthetic Dentistry, 1997. 77(5): p. 535-539. 21. Gurgan, S., S. Bolay, and R. Alacam, In vitro adherence of bacteria to bleached or unbleached enamel surfaces. Journal of Oral Rehabilitation, 1997. 24(8): p. 624627. 68 22. Bollen, C.M.L., W. Papaioanno, J. Van Eldere, E. Schepers, M. Quirynen, and D. Van Steenberghe, The influence of abutment surface roughness on plaque accumulation and peri-implant mucositis. Clinical Oral Implants Research, 1996. 7(3): p. 201-211. 23. Lie, T., Morphologic studies on dental plaque-formation-summry. Acta Odontologica Scandinavica, 1979. 37(2): p. 73-85. 24. Radford, D.R., S.P. Sweet, S.J. Challacombe, and J.D. Walter, Adherence of Candida albicans to denture-base materials with different surface finishes. Journal of Dentistry, 1998. 26(7): p. 577-583. 25. Jerolimov, V., R.G. Jagger, and P.J. Milward, Effect of the curing cycle on acrylic denture base glass transition temperatures. Journal of Dentistry, 1991. 19(4): p. 245-248. 26. Noort, R.v., Introduction to Dental Materials. 3rd ed2007, London: Mosby Elsevier. 27. Robinson, J.G. and J.F. McCabe, Impact strength of acrylic resin denture base materials with surface defects. Dental Materials, 1993. 9(6): p. 355-360. 28. Bowman, A.J. and T.R. Manley, The elimination of breakage in upper dentures by reinforcement with carbon-fiber. British Dental Journal, 1984. 156(3): p. 87-89. 29. Ekstrand, K., I.E. Ruyter, and H. Wellendorf, Carbon/graphite fiber reinforced poly(methyl methacrylate): Properties under dry and wet conditions. Journal of Biomedical Materials Research, 1987. 21(9): p. 1065-1080. 30. Clarke, D.A., N.H. Ladizesky, and T.W. Chow, Acrylic resins reinforced with highly drawn linear polyethylene woven fibres. 1. Construction of upper denture bases. Australian Dental Journal, 1992. 37(5): p. 394-399. 31. Ladizesky, N.H., T.W. Chow, and Y.Y. Cheng, Denture base reinforcement using woven polyethylene fiber. Int J Prosthodont, 1994. 7(4): p. 307-14. 32. Solnit, G.S., The effect of methyl-methacrylate reinforcement with silanetreatedand untreated glass-fibers. Journal of Prosthetic Dentistry, 1991. 66(3): p. 310-314. 69 33. Vallittu, P.K., Comparison of the In Vitro Fatigue Resistance of an Acrylic Resin Removable Partial Denture Reinforced With Continuous Glass Fibers or Metal Wires. Journal of Prosthodontics, 1996. 5(2): p. 115-121. 34. So, Y., J. Tsoi, and J. Matinlinna, A New Approach to Cure and Reinforce ColdCured Acrylics. SILICON, 2012: p. 1-12. 35. Grave, A.M.H., H.D. Chandler, and J.F. Wolfaardt, Denture base acrylic reinforced with high modulus fibre. Dental Materials, 1985. 1(5): p. 185-187. 36. Berrong, J.M., R.M. Weed, and J.M. Young, Fracture resistance of Kevlarreinforced poly(methyl methacrylate) resin: a preliminary study. Int J Prosthodont, 1990. 3(4): p. 391-5. 37. Jagger, D.C. and A. Harrison, The effect of chopped poly(methyl methacrylate) fibers on some properties of acrylic resin denture base material. International journal of Prosthodontics, 1999. 12(6): p. 542-546. 38. Jagger, D.C., A. Harrison, and K. Al-Marzoug, Effect of the addition of poly(methyl methacrylate) beads on some properties of acrylic resin. International journal of Prosthodontics, 2000. 13(5): p. 378-382. 39. Vallittu, P.K. and V.P. Lassila, Effect of metal strengthener's surface roughness on fracture resistance of acrylic denture base material. Journal of Oral Rehabilitation, 1992. 19(4): p. 385-391. 40. Polyzois, G.L., Reinforcement of denture acrylic resin: the effect of metal inserts and denture resin type on fracture resistance. Eur J Prosthodont Restor Dent, 1995. 3(6): p. 275-8. 41. Jagger, D.C., R.G. Jagger, S.M. Allen, and A. Harrison, An investigation into the transverse and impact strength of `high strength' denture base acrylic resins. Journal of Oral Rehabilitation, 2002. 29(3): p. 263-267. 42. Swoope Jr, C.C. and W.L. Kydd, The effect of cusp form and occlusal surface area on denture base deformation. The Journal of Prosthetic Dentistry, 1966. 16(1): p. 34-43. 43. Regli, C.P. and W.L. Kydd, A preliminary study of the lateral deformation of metal base dentures in relation to plastic base dentures. The Journal of Prosthetic Dentistry, 1953. 3(3): p. 326-330. 70 44. Ladizesky, N.H., Y.Y. Cheng, T.W. Chow, and I.M. Ward, Acrylic resin reinforced with chopped high-performance polyethylene fiber-properties and denture construction. Dental Materials, 1993. 9(2): p. 128-135. 45. Chitchumnong, P., S.C. Brooks, and G.D. Stafford, Comparison of three- and fourpoint flexural strength testing of denture-base polymers. Dental Materials, 1989. 5(1): p. 2-5. 46. Uzun, G. and N. Hersek, Comparison of the Fracture Resistance of Six Denture Base Acrylic Resins. Journal of Biomaterials Applications, 2002. 17(1): p. 19-28. 47. ASTM and International, ASTM D6272-02, in Standard Test Method for Flexural Properties of Unreinforced and Reinforced Plastics and Electrical Insulating Materials by Four-Point Bending2008. 48. Polyzois, G.L., P.E. Lagouvardos, and M.J. Frangou, Flexural and bond strengths of relined denture polymers assessed by four-point bending tests and Weibull analysis. Gerodontology, 2012. 29(2): p. e543-e552. 49. Azevedo, A., A.L. Machado, C.E. Vergani, E.T. Giampaolo, and A.C. Pavarina, Hardness of denture base and hard chair-side reline acrylic resins. Journal of Applied Oral Science, 2005. 13: p. 291-295. 50. Rueggeberg, F.A. and R.G. Craig, Correlation of Parameters used to Estimate Monomer Conversion in a Light-cured Composite. Journal of Dental Research, 1988. 67(6): p. 932-937. 51. Lee, H.-H., C.-J. Lee, and K. Asaoka, Correlation in the mechanical properties of acrylic denture base resins. Dental Materials Journal, 2012. 31(1): p. 157-164. 52. Neppelenbroek, K.H., A.C. Pavarina, C.E. Vergani, and E.T. Giampaolo, Hardness of heat-polymerized acrylic resins after disinfection and long-term water immersion. The Journal of Prosthetic Dentistry, 2005. 93(2): p. 171-176. 53. Machado, A.L., L.C. Breeding, C.E. Vergani, and L.E. da Cruz Perez, Hardness and surface roughness of reline and denture base acrylic resins after repeated disinfection procedures. The Journal of Prosthetic Dentistry, 2009. 102(2): p. 115-122. 71 54. Regis, R.R., N.C. Soriani, A.M. Azevedo, C.H. Silva-Lovato, H.F. Oliveira Paranhos, and R.F. De Souza, Effects of Ethanol on the Surface and Bulk Properties of a Microwave-Processed PMMA Denture Base Resin. Journal of Prosthodontics, 2009. 18(6): p. 489-495. 55. Williams, D., Revisiting the Definition of Biocompatibility. Medical Device Technology, 2003. 14(8): p. 10. 56. Tsuchiya, H., Y. Hoshino, K. Tajima, and N. Takagi, Leaching and cytotoxicity of formaldehyde and methyl methacrylate from acrylic resin denture base materials. The Journal of Prosthetic Dentistry, 1994. 71(6): p. 618-624. 57. Richmond, R., T.V. Macfarlane, and J.F. McCord, An evaluation of the surface changes in PMMA biomaterial formulations as a result of toothbrush/dentifrice abrasion. Dental Materials, 2004. 20(2): p. 124-132. 58. Lung, C.Y.K. and B.W. Darvell, Minimization of the inevitable residual monomer in denture base acrylic. Dental Materials, 2005. 21(12): p. 1119-1128. 59. Wiegand, A., F. Lemmrich, and T. Attin, Influence of rotating–oscillating, sonic and ultrasonic action of power toothbrushes on abrasion of sound and eroded dentine. Journal of Periodontal Research, 2006. 41(3): p. 221-227. 60. Wiegand, A., M. Begic, and T. Attin, In vitro Evaluation of Abrasion of Eroded Enamel by Different Manual, Power and Sonic Toothbrushes. Caries Research, 2006. 40(1): p. 60-65. 61. Braden, M., Some Aspects of the Chemistry and Physics of Dental Resins. Advances in Dental Research, 1988. 2(1): p. 93-97. 62. Vallittu, P.K., V. Miettinen, and P. Alakuijala, Residual monomer content and its release into water from denture base materials. Dental Materials, 1995. 11(5–6): p. 338-342. 63. Agapov, A.L. and A.P. Sokolov, Does the Molecular Weight Dependence of Tg Correlate to Me? Macromolecules, 2009. 42(7): p. 2877-2878. 64. Nishii, M., Curing of denture base resins with microwave irradiation: with particular reference to heat-curing resins. Journal of Osaka Dental University, 1968. 2(1): p. 23-40. 72 65. Kimura, H., F. Teraoka, H. Ohnishi, T. Saito, and M. Yato, Applications of microwave for dental technique (part 1). Dough-forming and curing of acrylic resins. The Journal of Osaka University Dental School, 1983. 23: p. 43-49. 66. Reitz, P.V., J.L. Sanders, and B. Levin, The curing of denture acrylic resins by microwave energy. Physical properties. Quintessence international, 1985. 16(8): p. 547-551. 67. Peyton, F.A., Packing and processing denture base resins. Journal of American Dental Association, 1950. 40: p. 521-526. 68. Shlosberg, S.R., C.J. Goodacre, C.A. Munoz, B.K. Moore, and R.J. Schnell, Microwave energy polymerization of poly(methyl methacrylate) denture base resin. The International Journal of Prosthodontics, 1989. 2(5): p. 453-458. 69. Vergani, C.E., R.S. Seo, A.C. Pavarina, and J.M. dos Santos Nunes Reis, Flexural strength of autopolymerizing denture reline resins with microwave postpolymerization treatment. The Journal of Prosthetic Dentistry, 2005. 93(6): p. 577-583. 70. Çelebi, N., B. Yüzügüllü, Ş. Canay, and Ü. Yücel, Effect of polymerization methods on the residual monomer level of acrylic resin denture base polymers. Polymers for Advanced Technologies, 2008. 19(3): p. 201-206. 71. Ogle, R.E., S.E. Sorensen, and E.A. Lewis, A new visible light-cured resin system applied to removable prosthodontics. The Journal of Prosthetic Dentistry, 1986. 56(4): p. 497-506. 72. Machado, C., E. Sanchez, S.S. Azer, and J.M. Uribe, Comparative study of the transverse strength of three denture base materials. Journal of Dentistry, 2007. 35(12): p. 930-933. 73. William J. O’Brien, Dental Materials and Their Selection. 3rd ed2002, Chicago: Quintessence Publishing Co, Inc. 74. O'Brien, Dental Materials and Their Selection. 4 ed, ed. P.F. William J. O'Brien2008, Hanover Park, IL: Quintessence Publishing Co, Inc. 75. Shalaby, S.W. and K.J.L. Burg, Polymers for Dental and Orthopedic Applications2006, Boca Raton, FL, USA: CRC Press. 73 76. Seneviratne, C.J., L.J. Jin, Y.H. Samaranayake, and L.P. Samaranayake, Cell Density and Cell Aging as Factors Modulating Antifungal Resistance of Candida albicans Biofilms. Antimicrobial Agents and Chemotherapy, 2008. 52(9): p. 32593266. 77. Yau, W.F.E., Y.Y. Cheng, R.K.F. Clark, and T.W. Chow, Pressure and temperature changes in heat-cured acrylic resin during processing. Dental Materials, 2002. 18(8): p. 622-629. 78. Budtz-Jörgensen, E., A. Stenderup, and M. Grabowski, An epidemiologic study of yeasts in elderly denture wearers. Community Dentistry and Oral Epidemiology, 1975. 3(3): p. 115-119. 79. Wolfaardt, J.F., P. Cleaton-Jones, and P. Fatti, The occurrence of porosity in a heat-cured poly (methyl methacrylate) denture base resin. The Journal of Prosthetic Dentistry, 1986. 55(3): p. 393-400. 80. Le Coz, C.J. and M. Bezard, Allergic contact cheilitis due to effervescent dental cleanser: combined responsibilities of the allergen persulfate and prosthesis porosity. Contact Dermatitis, 1999. 41(5): p. 268-271. 81. Ruyter, I.E. and H. Øysaed, Conversion in denture base polymers. Journal of Biomedical Materials Research, 1982. 16(5): p. 741-754. 82. Gautam, R., R.D. Singh, V.P. Sharma, R. Siddhartha, P. Chand, and R. Kumar, Biocompatibility of polymethylmethacrylate resins used in dentistry. Journal of Biomedical Materials Research Part B: Applied Biomaterials, 2012. 100B(5): p. 1444-1450. 83. Vallittu, P.K., I.E. Ruyter, and S. Buykuilmaz, Effect of polymerization temperature and time on the residual monomer content of denture base polymers. European Journal of Oral Sciences, 1998. 106(1): p. 588-593. 84. Kedjarune, U., N. Charoenworaluk, and S. Koontongkaew, Release of methyl methacrylate from heat-curved and autopolymerized resins: Cytotoxicity testing related to residual monomer. Australian Dental Journal, 1999. 44(1): p. 25-30. 85. Baker, S., S.C. Brooks, and D.M. Walker, The Release of Residual Monomeric Methyl Methacrylate from Acrylic Appliances in the Human Mouth: An Assay for Monomer in Saliva. Journal of Dental Research, 1988. 67(10): p. 1295-1299. 74 86. Dyer, D., M. Addy, and R.G. Newcombe, Studies in vitro of abrasion by different manual toothbrush heads and a standard toothpaste. Journal of Clinical Periodontology, 2000. 27(2): p. 99-103. 87. Campanha, N.H., A.C. Pavarina, I.L. Brunetti, C.E. Vergani, A.L. Machado, and D.M.P. Spolidorio, Candida albicans inactivation and cell membrane integrity damage by microwave irradiation. Mycoses, 2007. 50(2): p. 140-147. 88. Baysan, A., R. Whiley, and P.S. Wright, Use of microwave energy to disinfect a long-term soft lining material contaminated with Candida albicans or Staphylococcus aureus. The Journal of Prosthetic Dentistry, 1998. 79(4): p. 454458. 89. Fisher, A.A., Allergic sensitization of the skin and oral mucosa to acrylic resin denture materials. The Journal of Prosthetic Dentistry, 1956. 6(5): p. 593-602. 90. Giunta, J.L., I. Grauer, and N. Zablotsky, Allergic contact stomatitis caused by acrylic resin. The Journal of Prosthetic Dentistry, 1979. 42(2): p. 188-190. 91. McCabe, J.F. and R.M. Basker, Tissue sensitivity to acrylic resin. A method of measuring the residual monomer content and its clinical application. British Dental Journal, 1976. 140(10): p. 347-350. 92. Ali, A., J F Bates, A.J. Reynolds, and D.M. Walker, The burning mouth sensation related to wearing of acrylic dentures: an investigation. British Dental Journal, 1986. 161(12): p. 444-447. 93. Bural, C., E. Aktaş, G. Deniz, Y. Ünlüçerçi, N. Kızılcan, and G. Bayraktar, Effect of post-polymerization heat-treatments on degree of conversion, leaching residual MMA and in vitro cytotoxicity of autopolymerizing acrylic repair resin. Dental Materials, 2011. 27(11): p. 1135-1143. 94. Swaney, A., G. Paffenbarger, H. Carl, and W. Sweeny, ADA Specification No. 12 for Denture Resin, ed. 2. Journal of American Dental Association, 1953. 46(1): p. 54-66. 95. Bevan, E.M. and R. Earnshaw, The role of water sorption in the solvent crazing of acrylic resins: Part I. Australian Dental Journal, 1968. 13(4): p. 265-273. 96. Braden, M., The absorption of water by acrylic resins and other materials. The Journal of Prosthetic Dentistry, 1964. 14(2): p. 307-316. 75 97. Anusavice, K.J., Phillip's Science of Dental Materials. 11th ed2003, St Louis: Elsevier Science. 98. Musanje, L. and B.W. Darvell, Aspects of water sorption from the air, water and artificial saliva in resin composite restorative materials. Dental Materials, 2003. 19(5): p. 414-422. 99. Devlin, H. and P. Kaushik, The Effect of Water Absorption on Acrylic Surface Properties. Journal of Prosthodontics, 2005. 14(4): p. 233-238. 100. Association, A.N.S.A.D., ANSI/ADA Standard No. 12—Denture Base Polymers: 2002 (Reaffirmed 2008), 2002. 101. von Fraunhofer, J.A. and C. Suchatlampong, The surface characteristics of denture base polymers. Journal of Dentistry, 1975. 3(3): p. 105-109. 102. Chow, T.W., Y.Y. Cheng, and N.H. Ladizesky, Polyethylene fibre reinforced poly(methylmethacrylate)—water sorption and dimensional changes during immersion. Journal of Dentistry, 1993. 21(6): p. 367-372. 103. Theilade, E., E. Budtz-Jørgensen, and J. Theilade, Predominant cultivable microflora of plaque on removable dentures in patients with healthy oral mucosa. Archives of Oral Biology, 1983. 28(8): p. 675-680. 104. Costerton JW, L.-S.H., Introduction to microbial biofilms, in Microbial Biofilms, L.S.H. Costerton JW, Editor 1995, Cambridge University Press: Cambridge. p. 1-11. 105. Glass, R.T., J.W. Bullard, C.S. Hadley, E.W. Mix, and R.S. Conrad, Partial spectrum of microorganisms found in dentures and possible disease implications. Journal of the American Osteopathic Association, 2001. 101(2): p. 92-94. 106. Pavarina, A.C., A.C. Pizzolitto, A.L. Machado, C.E. Vergani, and E.T. Giampaolo, An infection control protocol: Effectiveness of immersion solutions to reduce the microbial growth on dental prostheses. Journal of Oral Rehabilitation, 2003. 30(5): p. 532-536. 107. Teles, F., R. Teles, A. Sachdeo, N. Uzel, X. Song, G. Torresyap, M. Singh, A. Papas, A. Haffajee, and S. Socransky, Comparison of Microbial Changes in Early ReDeveloping Biofilms on Natural Teeth. Journal of Periodontology 2012(19433670 (Electronic)): p. T - ahead of print. 76 108. Ishikawa, A., T. Yoneyama, K. Hirota, Y. Miyake, and K. Miyatake, Professional care reduces the number of oropharyngeal bacteria. Journal of Dental Research, 2008. 87(6): p. 594-8. 109. Nikawa, H., T. Hamada, and T. Yamamoto, Denture plaque — past and recent concerns. Journal of Dentistry, 1998. 26(4): p. 299-304. 110. Seneviratne, C.J., L. Jin, and L.P. Samaranayake, Biofilm lifestyle of Candida: a mini review. Oral Diseases, 2008. 14(7): p. 582-590. 111. Chandra, J., D.M. Kuhn, P.K. Mukherjee, L.L. Hoyer, T. McCormick, and M.A. Ghannoum, Biofilm Formation by the Fungal PathogenCandida albicans: Development, Architecture, and Drug Resistance. Journal of Bacteriology, 2001. 183(18): p. 5385-5394. 112. Meurman, J.H., P. Pärnänen, C.J. Seneviratne, L.P. Samaranayake, A.M.J. Saarinen, and K. Kari, Prevalence and antifungal drug sensitivity of non-albicans Candida in oral rinse samples of self-caring elderly. Gerodontology, 2011. 28(4): p. 246-252. 113. Samaranayake, L.P., W. Keung Leung, and L. Jin, Oral mucosal fungal infections. Periodontology 2000, 2009. 49(1): p. 39-59. 114. Arendorf, T.M. and D.M. Walker, The prevalence and intra-oral distribution of Candida albicans in man. Archives of Oral Biology, 1980. 25(1): p. 1-10. 115. Addy, M., W.C. Shaw, P. Hansford, and M. Hopkins, The effect of orthodontic appliances on the distribution of Candida and plaque in adolescents. Journal of Orthodontics, 1982. 9(3): p. 158-63. 116. Coulthwaite, L. and J. Verran, Potential pathogenic aspects of denture plaque. British Journal of Biomedical Science, 2007. 64(4): p. 180-189. 117. Chandra, J., P.K. Mukherjee, S.D. Leidich, F.F. Faddoul, L.L. Hoyer, L.J. Douglas, and M.A. Ghannoum, Antifungal Resistance of Candidal Biofilms Formed on Denture Acrylic in vitro. Journal of Dental Research, 2001. 80(3): p. 903-908. 118. Hawser, S.P. and L.J. Douglas, Resistance of Candida albicans biofilms to antifungal agents in vitro. Antimicrobial Agents and Chemotherapy, 1995. 39(9): p. 2128-31. 77 119. Wilson, J., The aetiology, diagnosis and management of denture stomatitis. Br Dent J, 1998. 185(8): p. 380-384. 120. Abelson, D.C., Denture plaque and denture cleansers. The Journal of Prosthetic Dentistry, 1981. 45(4): p. 376-379. 121. Nikawa, H., T. Hamada, H. Yamashiro, and H. Kumagai, A Review of in Vitro and in Vivo Methods to Evaluate the Efficacy of Denture Cleansers. International journal of Prosthodontics, 1999. 12(2): p. 153-159. 122. Morgan, T.D. and M. Wilson, Anti-adhesive and antibacterial properties of a proprietary denture cleanser. Journal of Applied Microbiology, 2000. 89(4): p. 617-623. 123. Pietrokovski, J., J. Azuelos, S. Tau, and R. Mostavoy, Oral findings in elderly nursing home residents in selected countries: Oral hygiene conditions and plaque accumulation on denture surfaces. The Journal of Prosthetic Dentistry, 1995. 73(2): p. 136-141. 124. Barrett, D., Interventions for cleaning dentures in adults. International Journal of Evidence-Based Healthcare, 2010. 8(4): p. 286-287. 125. de Souza Raphael, F., H. de Freitas Oliveira Paranhos, H. Lovato da Silva Claudia, L. Abu-Naba'a, Z. Fedorowicz, and A. Gurgan Cem Interventions for cleaning dentures in adults. Cochrane Database of Systematic Reviews, 2009. DOI: 10.1002/14651858.CD007395.pub2. 126. Stoltze, K. and L. Bay, Comparison of a manual and a new electric toothbrush for controlling plaque and gingivitis. Journal of Clinical Periodontology, 1994. 21(2): p. 86-90. 127. Sumi, Y., K. Nakajima, T. Tamura, M. Nagaya, and Y. Michiwaki, Developing an instrument to support oral care in the elderly. Gerodontology, 2003. 20(1): p. 3-8. 128. Frandsen, A., Dental Plaque Control Measures and Oral Hygiene Practice. Practices: State-of-the-science review., ed. L. J. and D.V. Kleinmann1985, Oxford: Oxford: IRL Press Ltd. 129. Scutt, J.S. and C.J. Swann, The first mechanical toothbrush? Br Dent J., 1975. 139(4): p. 152. 78 130. Rosa, M.D.l., J.Z. Guerra, D.A. Johnston, and A.W. Radike, Plaque growth and removal with daily toothbrushing. Journal of Periodontology, 1979. 50(12): p. 661-664. 131. Chilton, N., A.Didio, and J. Rothner, Comparison of the clinical effectiveness of an electric and a standard toothbrush. Journal of American Dental Association, 1962. 64: p. 777-782. 132. van der Weijden, G.A., M.F. Timmerman, E. Reijerse, C.M. Snoek, and U. van der Velden, Toothbrushing force in relation to plaque removal. Journal of Clinical Periodontology, 1996. 23(8): p. 724-729. 133. Addy, M. and M.L. Hunter, Can tooth brushing damage your health? Effects on oral and dental tissues. International Dental Journal, 2003. 53(S3): p. 177-186. 134. Lee, A., L.H. He, K. Lyons, and M.V. Swain, Tooth wear and wear investigations in dentistry. Journal of Oral Rehabilitation, 2012. 39(3): p. 217-225. 135. Brandini, D.A., A.L.B. de Sousa, C.L. Trevisan, L.A.P. Pinelli, S.C.d.C. Santos, D. Pedrini, and S.R. Panzarini, Noncarious Cervical Lesions and Their Association With Toothbrushing Practices: In Vivo Evaluation. Operative Dentistry, 2011. 36(6): p. 581-589. 136. Harrison, Z., A. Johnson, and C.W.I. Douglas, An in vitro study into the effect of a limited range of denture cleansers on surface roughness and removal of Candida albicans from conventional heat-cured acrylic denture base material. Journal of Oral Rehabilitation, 2004. 31: p. 460-467. 137. Dyer, D., E. MacDonald, R.G. Newcombe, C. Scratcher, F. Ley, and M. Addy, Abrasion and stain removal by different manual toothbrushes and brush actions: studies in vitro. Journal of Clinical Periodontology, 2001. 28(2): p. 121-127. 138. Tarbet, W.J., S. Axelrod, S. Minkoff, and P.A. Fratarcangelo, Denture cleansing: A comparison of two methods. The Journal of Prosthetic Dentistry, 1984. 51(3): p. 322-325. 139. Van der Weijden, G.A., M.F. Timmerman, A. Nijboer, M.A. Lie, and U. Van der Velden, A comparative study of electric toothbrushes for the effectiveness of plaque removal in relation to toothbrushing duration. Journal of Clinical Periodontology, 1993. 20(7): p. 476-481. 79 140. Trimpeneers, L.M., I.A. Wijgaerts, N.A. Grognard, L.R. Dermaut, and P.A. Adriaens, Effect of electric toothbrushes versus manual toothbrushes on removal of plaque and periodontal status during orthodontic treatment. American Journal of Orthodontics and Dentofacial Orthopedics, 1997. 111(5): p. 492-497. 141. Palenik, C.J. and C.H. Miller, In vitro testing of three denture-cleaning systems. The Journal of Prosthetic Dentistry, 1984. 51(6): p. 751-754. 142. Pitt, W.G. and S.A. Ross, Ultrasound Increases the Rate of Bacterial Cell Growth. Biotechnology Progress, 2003. 19(3): p. 1038-1044. 143. Budtz-Jørgensen, E., Materials and methods for cleaning dentures. The Journal of Prosthetic Dentistry, 1979. 42(6): p. 619-623. 144. Raab, F.J., C.A. Taylor, J.A. Bucher, and B.L. Mann, Scanning electron microscopic examination of ultrasonic and effervescent methods of surface contaminant removal from complete dentures. The Journal of Prosthetic Dentistry, 1991. 65(2): p. 255-258. 145. Cruz, P.C., I.M. de Andrade, A. Peracini, M.C.M. de Souza-Gugelmin, C.H. SilvaLovato, R.F. de Souza, and H.F.O. Paranhos, The effectiveness of chemical denture cleansers and ultrasonic device in bio film removal from complete dentures. Journal of Applied Oral Science, 2011. 19(6): p. 668-673. 146. Nikawa, H., H. Iwanaga, T. Hamada, and S. Yuhta, Effects of denture cleansers on direct soft denture lining materials. The Journal of Prosthetic Dentistry, 1994. 72(6): p. 657-662. 147. Nikawa, H., T. Hamada, T. Yamamoto, and H. Kumagai, Effects of salivary or serum pellicles on the Candida albicans growth and biofilm formation on soft lining materials in vitro. Journal of Oral Rehabilitation, 1997. 24(8): p. 594-604. 148. McNeme, S.J., A.S. von Gonten, and G.D. Woolsey, Effects of laboratory disinfecting agents on color stability of denture acrylic resins. The Journal of Prosthetic Dentistry, 1991. 66(1): p. 132-136. 149. Moore, T.C., D.E. Smith, and G.E. Kenny, Sanitization of dentures by several denture hygiene methods. The Journal of Prosthetic Dentistry, 1984. 52(2): p. 158-163. 80 150. Polyzios, G.L., A J Zissis, and S.A. Yannikakis, The effect of glutaraldehyde and microwave disinfection on some properties of acrylic denture resin. International Journal of Prosthodontics, 1995. 8(2): p. 150-154. 151. Shen, C., N.S. Javid, and F.A. Colaizzi, The effect of glutaraldehyde base disinfectants on denture base resins. The Journal of Prosthetic Dentistry, 1989. 61(5): p. 583-589. 152. Backenstose, W.M. and J.G. Wells, Side effects of immersion-type cleansers on the metal components of dentures. The Journal of Prosthetic Dentistry, 1977. 37(6): p. 615-621. 153. Ramage, G., K. Tomsett, B.L. Wickes, J.L. López-Ribot, and S.W. Redding, Denture stomatitis: a role for Candida biofilms. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 2004. 98(1): p. 53-59. 154. Gomes, B.P.F.d.A., M.E. Vianna, C.U. Matsumoto, V. de Paula e Silva Rossi, A.A. Zaia, C.C.R. Ferraz, and F.J. de Souza Filho, Disinfection of gutta-percha cones with chlorhexidine and sodium hypochlorite. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 2005. 100(4): p. 512-517. 155. Montagner, H., F. Montagner, K.O. Braun, P.E.C. Peres, and B.P.F.d.A. Gomes, In vitro antifungal action of different substances over microwaved-cured acrylic resins. Journal of Applied Oral Science, 2009. 17: p. 432-435. 156. Mohammadi, Z. and P.V. Abbott, The properties and applications of chlorhexidine in endodontics. International Endodontic Journal, 2009. 42(4): p. 288-302. 157. Ellepola, A.N.B. and L.P. Samaranayake, Oral Candidal Infections and Antimycotics. Critical Reviews in Oral Biology & Medicine, 2000. 11(2): p. 172198. 158. Ellepola, A.N.B. and L.P. Samaranayake, Adjunctive use of chlorhexidine in oral candidoses: a review. Oral Diseases, 2001. 7(1): p. 11-17. 159. Machado de Andrade, I., P.C. Cruz, C.H. Silva-Lovato, R.F. de Souza, M. Cristina Monteiro Souza-Gugelmin, and H. de Freitas Oliveira Paranhos, Effect of Chlorhexidine on Denture Biofilm Accumulation. Journal of Prosthodontics, 2012. 21(1): p. 2-6. 81 160. Rohrer, M. and R. Bulard, Microwave sterilization. The Journal of the American Dental Association, 1985. 110(2): p. 194-198. 161. Watanabe, K., Y. Kakita, N. Kashige, F. Miake, and T. Tsukiji, Effect of ionic strength on the inactivation of micro-organisms by microwave irradiation. Letters in Applied Microbiology, 2000. 31(1): p. 52-56. 162. Banting, D.W. and S.A. Hill, Microwave disinfection of dentures for the treatment of oral candidiasis. Special Care in Dentistry, 2001. 21(1): p. 4-8. 163. Webb, Thomas, Harty, and Willcox, Effectiveness of two methods of denture sterilization. Journal of Oral Rehabilitation, 1998. 25(6): p. 416-423. 164. Burns, D.R., A. Kazanoglu, and P.C. Moon, Dimensional stability of acrylic resin materials after microwave sterilization. International Journal of Prosthodontics, 1990. 3(5): p. 489-493. 165. Mima, E.G., A.C. Pavarina, K.H. Neppelenbroek, C.E. Vergani, D.M.P. Spolidorio, and A.L. Machado, Effect of Different Exposure Times on Microwave Irradiation on the Disinfection of a Hard Chairside Reline Resin. Journal of Prosthodontics, 2008. 17(4): p. 312-317. 166. Sanitá, P.V., C.E. Vergani, E.T. Giampaolo, A.C. Pavarina, and A.L. Machado, Growth of Candida species on complete dentures: effect of microwave disinfection. Mycoses, 2009. 52(2): p. 154-160. 167. Roberts, F.A. and R.P. Darveau, Beneficial bacteria of the periodontium. Periodontology 2000, 2002. 30(1): p. 40-50. 82 Part II: Laboratory Report This part has been submitted as the manuscript with title “Effect of powered toothbrush cleaning on acrylic resin dental prostheses” to the journal, Gerodontology. Effects of Powered Toothbrush Cleaning on Acrylic Resin Dental Prostheses Abstract Introduction Optimal denture hygiene maintenance requires brushing and other supplementary methods to effectively remove plaque and biofilm build-up on surfaces of dental prostheses. Brushing denture using manual brushes is the most common practise among denture wearers. Evaluation on the effects of mechanical cleaning using a powered toothbrush on poly(methyl methacrylate) (PMMA) denture base material was performed. Materials and methods Heat polymerized PMMA specimen beams with the dimension of 45.0 x 6.5 x 4.5 mm were fabricated in stainless steel moulds. PMMA of the brand Trevalon C (Dentsply Ltd. De Tray Division Weybridge, UK) was mixed at the powder to liquid ratio of 2.4 : 1 and processed according to manufacturer’s instruction. Specimens were kept in water storage for 0, 1, 7, 15, 30 and 60 days was assigned to control and then tested at random. Test specimens underwent a focal area of brushing action using battery powered toothbrush at 2 N applied force for 22 min with water as the medium. Observations were made on the surface roughness measurement (Ra) and flexural strength computed through performing 3-point bending test. Specimens had Candida albicans biofilm coated and efficacy of powered toothbrush removing the biofilm was investigated. The 84 results of mean surface roughness value and flexural strength were analysed by using 2-way ANOVA and Tukey post hoc test at 5% significance level. Results The mean ± standard deviation of the Ra value of surfaces of PMMA specimens before and after brushed for 22 min with water were 0.29 ± 0.06 μm and 0.27 ± 0.06 μm respectively. The lowest mean flexural strength of 87.37 ± 9.23 MPa was recorded for specimen group after brushing plus water storage for 7 days. The highest mean flexural strength was 103.72 ± 8.52 MPa for specimens without water storage after brushed. The experiment showed that PMMA specimens recorded decrease surface roughness value and no observable significant changes on flexural strength after brushing with power toothbrush. However, flexural strength and surface roughness value were significantly lower in specimens group after 7 days in water storage compared to control with no storage. Mean flexural strength for 15, 30 and 60 days storage reached a plateau thereafter. SEM micrographs of post-brushed specimens revealed satisfactory removal of Candida albicans biofilm. Conclusion: Power toothbrush seemed a suitable device for cleaning dental prostheses made of poly(methyl methacrylate) when brushing was performed with liquid medium added. 85 1. Introduction Poly(methyl methacrylate) (PMMA) base dental prostheses deteriorate over the useful time span of dental prosthesis. The deterioration is related to its inherent properties as a polymer, the physical wear and tear in the oral environment during function as well as methods of denture hygiene practised. When the dentures are inappropriately cleaned, which lead to surface and bulk material flaw, this can contribute to the material deterioration within PMMA and give way to ultimate failure. It is of interest to investigate the influence and the effect of using powered toothbrush denture cleaning protocol on PMMA denture base material. The oral cavity is a unique environment that promotes formation, accumulation and deposition of biofilm on the surfaces of natural tissue and artificial prostheses. Microbial biofilms form on the teeth is known as dental plaque whereas the biofilm on dentures are termed denture plaque [1]. Matured biofilm on natural and denture teeth may have similar total numbers of bacteria but proportion of sepsis may differ [2]. Persistent long term accumulation of denture plaque can cause denture related stomatitis [3] in denture wearer and aspiration pneumonia in frail elderly through continuous swallowing or aspiration of microorganism present on denture [4]. In particular, the old and frail elderly people have unique requirement in their need to maintain denture hygiene. Their frail conditions have made the task of personal hygiene and dental hygiene very challenging for themselves and for their caregivers [5]. They require some form of efficiency enhancement design incorporated in denture brushes so as to help them cope with brushing denture. 86 The simple, compact designed, highly versatile and affordable generic brand battery powered toothbrush suggested here, may be suitable for the old frail as well as their caregivers to help with better daily oral and denture hygiene maintenance. A study conducted by Sumi et al. pointed out that elderly people may have difficulty in mechanically removing dental plaque due to diminished manual dexterity, impaired vision, or chronic illness [5, 6]. The older person’s ability to perform self-care gradually decrease with advancing age, and the role of the caregiver in daily oral care becomes increasingly a necessity. However, optimal oral care by caregivers is not always possible because of time constraints, difficulty involved in brushing other individuals’ teeth, lack of cooperation, and the lack of perceived need. The recognition of this issue faced by the elders and care givers prompted them to make a device through modification of a powered toothbrush. The results from their investigation were positive and promising, especially in helping those concerned subjects and care givers to achieve good dental plaque control [6]. The presence of distressing oral malodour is of great concerned to denture wearer which is the direct consequence of inefficient cleaning of denture [7]. There is a need to consistently perform good standard of denture hygiene and oral hygiene practice in order to prevent the development of pathology affecting general health and oral health [1, 8]. An early study described the methods of cleaning dental prosthesis as two broad category of mechanical and chemical means [7]. The addition to these groups which can be considered new are ultrasonic solution or water-bath cleaning and microwave generated denture sterilization in microwave oven [9]. 87 A mechanical cleaning method such as brushing or use of ultrasonic water bath are the most effective in removing denture-plaque and biofilm from surfaces of dental prostheses according to previous studies [10, 11]. Qualities of a good denture cleaning agent are, but not limited to: the ease of use, effective removal of deposit on surfaces of denture without damage to the denture, bactericidal and fungicidal, non-toxic, non-irritant, chemically defined and stable, regulatoryapproved on a global basis and cost-effective [12]. Battery operated powered toothbrush can satisfy most of the required qualities, except bactericidal and fungicidal. The mechanical cleaning method with brushes involves mechanically moving bristles across the surfaces of denture. Toothpaste or powder cleanser can be added together during brushing, in order to increase cleaning efficiency [13]. The use of toothpaste carries within it the risk of abrasion created on denture surfaces, due mainly to its abrasive nature of the filler particles. Tap water is used as rinsing medium during and after cleaning with brushes. The cleaned dental prostheses will either be worn in the mouth or stored in a container filled with an immersion medium. The types of immersion media use may contain any combination or single constituent of antiseptic chemical, or antifungal and antimicrobial substances plus chemical solvent for example alcohol. From the denture wearer’s perspective and the manufacturer’s interest, colouring dye and flavouring chemical are a must-have formulated addition into these over-thecounter personal hygiene consumer products sold in a great number of conveniently located retailing business outlets. The efficacy of using such solution to clean and to “kill” bacteria in denture plaque still remains an elusive pursuit to most denture wearers and an inconclusive confusion to the dental profession. 88 During the physiologic function of the denture in the mouth and throughout the useful life span of the dental prosthesis, it is constantly subjected to physical load as well as chemical interaction with the immersion media. When the denture is left outside the mouth and kept in an immersion solution, surfaces of denture may be influenced by the immersion medium. The dentist often advices the denture wearer to meticulously clean the denture daily. However, when such measures are being over zealously under taken by the patient, the longevity of the prosthesis would be compromised [13, 14]. The brushes, cleaning pastes, denture-soaks and other liquid chemicals that can have long duration contact with the surfaces of the PMMA denture base material will certainly speed up the process of deterioration of PMMA made dental prostheses. Adding to this list are the chemical substances that denture wearer might consume in the diet, the PMMA is constantly subject to chemical challenges at the molecular level. The qualities of the physical and surface properties of PMMA denture base material are certainly affected. Cracks, craze lines and voids or surface irregularities buildup on the surfaces of denture will cause stress fatigue during normal functional load and lead to may result in the eventual denture breakage [14]. Factors that could affect the surface properties and the mechanical properties of PMMA include the magnitude of force applied during brushing, the stiffness of the bristles, the type of brushing media used concurrently, the total duration of brushing, the type of cure of PMMA used and the temperature setting of the brushing performed whether under cold or hot water condition. The resultant observable increase in surface roughness was reported when brushing was performed using a type of toothpaste [15]. 89 Previous researches emphasized cleaning the denture to remove denture plaque biofilm and the efficiency and efficacy were the main primary target outcomes [15, 16]. There is a lack of information and research carried out on the subject of parallel damage affecting the surfaces of dental prosthesis made of PMMA that contribute to material substance deterioration which cause the ultimate failure of prosthesis. The research paper by Harrison et al. [15] was referred to for the experimental protocol and the design of current study. The current study follows the same applied for brushing. Some variations were made to suit the current laboratory condition. The force applied on the brush head was set at 204 g equivalent to 2 N of the normal brushing force. Denture wearers have very limited choice of suitable brushes to choose from the available consumer market, especially in this region. The brushes are either with brush head too large in size or too soft in bristles which are unsuitable for brushing and cleaning dentures. Dentures soaking effervescent tablets seem the only choice left and using these alone has been proven to be inconclusive in its efficiency to totally remove denture plaque and Candida biofilm [16-18]. These tablets are meant for adjunctive use with mechanical brushing [10, 19-21]. The purpose of this experiment at hand is intended to fill the current gap in researches on mechanical cleaning method of dental prostheses. The null hypothesis for this study was set that the use of powered toothbrush to clean dental prosthesis has no impact on the mean flexural strength and mean surface roughness value of poly(methyl methacrylate) denture base specimens. These two parameters of investigation formed the first and second part of a three-part research experiment, microbiology constituted the third part. 90 The aim of the microbiological experiment was to qualitatively evaluate the efficacy of battery powered toothbrush for the in vitro removal of Candida albicans biofilm formed on denture acrylic surfaces. In principle, Candida albicans can adhere and colonise PMMA surfaces to form biofilms [22, 23]. Mature biofilms are recognized as matrix-enclosed microbial population adhering to each other and they characteristically display a phenotype that is different from planktonic cells, such as increase resistance to antimicrobial agents and protection from host defences [24]. The purpose of denture hygiene practice is to reduce and to eliminate microbial biofilm formation. Mechanical cleaning and chemical disinfection have been recommended for effective removal of denture plaque and Candida biofilms [19, 25]. The structure of Candida albicans and other yeasts as observed by scanning electron microscopy (SEM) has been described earlier by Barnes et al. [26]. SEM micrographs were used to evaluate the effectiveness of denture cleaning using ultrasonic device compared to effervescent tablets immersion method [27]. It has been established that it is feasible to use SEM in determining the morphologic type and distribution of surface coating and microorganisms on the surface of dentures [28]. SEM images a sample by scanning it with a high-energy beam of electrons, and it is capable of imaging at a significantly higher resolution than light microscopes. SEM allows the evaluation of detailed surface topography and morphology of Candida albicans biofilm at high magnification but involves 91 degradation of the hydrated structural features (e.g. matrix) due to the fixation and dehydration steps performed during sample preparation [29]. The advantages of SEM examination include a deeper depth of field, which allows more of a specimen to be in focus at one time compare to light microscope that only manage relative shallow depth of field. Besides, the SEM has much higher resolution and higher level of magnification level at thousands of times. The images produce are strikingly clear which makes SEM most useful for the examination of Candida biofilm architecture and surface topography in greater detail. In the current experiment, the absent of Candida cells and biofilm in SEM micrographs would confirm their thorough and complete removal effected through the experimental brushing protocol [27]. In recent years, there has been an increase in the preference of atomic force microscopy (AFM) in biomaterial imaging due to its advantages over the other types of spectroscopy such as fluorescence microscopy and confocal scanning laser microscopy (CSLM). AFM provides not only a three-dimensional image of a sample but also a three-dimensional surface profile. In the AFM imaging, the samples do not require any special treatment such as coatings with metal or carbon, and no drying is required. Additionally, the images can be obtained in the ambient air or even in a liquid environment [30]. 92 2. Materials and methods 2.1 Specimen groups A total of 244 pieces of PMMA specimens beam were required for this experiment. Specimens were kept in water storage for 0, 1, 7, 15, 30 and 60 days. 12 PMMA specimens from each test group were subjected to brushing protocol and 12 specimens from control group were not. Surface roughness value (Ra) of 12 specimens for all groups was analysed before brushed and after brushed. Specimens for this test were from the test group of flexural strength test prior to loading into universal testing machine. Table 1 showed the specimen allocation for this study. Table 1 Specimen allocation Day(s) in Water Storage Testing Parameter 0, 1, 7, 15, 30, 60 Surface Roughness value Ra (μm) Flexural strength (MPa) Before brushing S p e c i m e n Test n=12 After brushing Control n=12 After brushing No brushing 93 2.2 Materials Poly(methyl methacrylate) of the brand Trevalon C (DENTSPLY Ltd. De Tray Division Weybridge, UK) in liquid monomer and powder polymer forms and of the heat polymerized type was used for fabrication of PMMA specimens beam. Stainless steel moulds which can be assemble and disassemble with 6 compartments for specimens were used. (Fig. 2.1 (a) & (b)) (a) (b) Fig.2. 1(a) and (b) Stainless steel mould for specimens fabrication. 94 2.3 Specimens fabrication Heat cured PMMA specimens beam with the dimensions of 45.0 x 6.5 x 4.5 mm were fabricated in a stainless steel mould. The PMMA was mixed at the powder to liquid ratio of 2.4 : 1.0 and process according to manufacturer’s instruction and Prince Philip Dental Hospital, Dental Technology Laboratory heat-cured poly(methyl methacrylate) processing protocol. Firstly, the stainless steel (SS) moulds were pre-coated with a thin layer of petroleum jelly (Vaseline®, USA) for easy detachment of the cured specimens. A small portion of dough was placed on the SS mould and firmly pressed with fingers at the beginning which showed uneven distribution of pressure and dough material into mould spaces (Fig. 2.2). Then, incremental packing pressure was applied to stainless steel moulds range from 1500-4500 psi (105-316 kg·cm-2). The fastening screws of moulds were progressively tightened at successive trial packing while the flash of excess dough was squeezed out (Fig. 2.3). This progressive screw tightening step was to facilitate the pressure release and prevent a back pressure build-up which could cause porosity due to extreme air-traps while packing the dough into SS mould. The excess PMMA dough that flowed out of the mould as flash during pressing was folded back overlay the dough in the mould after the hydraulic press was released and the cover plate of the mould uncovered (Fig. 2.4). This step was repeated twice and the fastening screws were tightened in each successive step. The layers of overlay became thinner with each successive pressing and compacting which facilitated fabricating more compact dough specimens (Fig. 2.5). 95 Fig. 2.2 A lumpy dough placed on mould caused uneven pressure distribution. Fig.2.3 Pressed and tightened fastening screw through sequential steps. Fig.2.4 Flash folded back overlay mould followed by pressing. Fig.2.5 Further compaction of thinner fold-over flash and dough. 96 At final pressing, the pressure was maintained for 10 minutes. Each folding back and overlay of mould with flash of PMMA dough followed by pressure application would make the dough stage PMMA specimens more compact where air bubbles included during mixing and packing could be compressed and expelled. An example of insufficiently compacted dough in specimens is showed with large quantity of visible air bubbles (Fig. 2.6). Fig. 2.6 Close up view of specimens removed from mould at 1st press-packing to show air bubbles at base which appeared as white spots in specimens at dough stage packing. The SS moulds were transferred to a spring flask clamp (Ash™, England). The tightening screw on the clamp was tightened to a torque of 36 N m [31], this is to ensure sufficient pressure applied to minimized porosities in PMMA specimens. 97 Fabricated specimens were not subject to surface finish polishing protocol. Specimens were group assigned to control and test at random selection. Specimens with excessive porosity throughout or polymerization shrinkage concentrated on one surface were excluded (Fig. 2.7). The inclusion of these porous specimens could result in extreme data to be generated from experiment which would make subsequent erroneous interpretation inevitable. Specimens that were included in experiment had minimal porosity (Fig. 2.8). Fig. 2.7 Specimen excluded due to excessive porosities. Fig. 2.8 An example of specimens without porosity included in experiment. 98 2.4 Polymerization and post processing Heat curing of PMMA was carried out in a polymerization hot-water bath (Model 1491, Loborwelt Leleux Gmbh, Germany). The stainless steel moulds with packed PMMA dough were secured in a spring clamp and placed into the water bath at room temperature thereafter heated to 100 °C and maintained at this temperature for 40 minutes. At the end of polymerization, the stainless steel moulds in clamp were removed from hot-water bath and left on bench to cool overnight at room temperature. The moulds were removed from the clamp the following day and disassembled to retrieve the polymerized specimen beams. Flash and fins of excess PMMA on specimens were trimmed and removed using sharp blades and fine silicon carbide paper No. 500 (Struers, Denmark) to render the edges of specimens even and smooth. This was to ensure a more uniform and homogeneous measurement of all dimensions. Each specimen was labelled accordingly to indicate the date of fabrication, the specimen group and the specimen number. 99 2.5 Storage condition Specimens were totally immersed in a plastic container filled with deionized water covered with plastic wrap (Parafilm®), and stored in a waterjacket incubator (Model 3157, Forma Scientific, Ohio, USA) at a constant temperature of 37 ⁰C with a 99 % relative humidity. The duration of storage in deionized water (Milli-Q® RG Ultra-pure water system, Millipore, Massachusetts, USA) in an incubator before other testing was 1 day, 7 days, 15 days, 30 days and 60 days. Specimens with no water storage conducted were assigned as the control group for comparison to test groups and it was kept in water storage. Specimens were tested dry at room temperature after immediate removal from container filled with deionized water. 100 2.6 Powered toothbrush brushing protocol of specimens The powered toothbrush used was a generic brand battery powered with rotating brush head obtained off-the-shelf from a local supermarket, at the purchased price of USD 5.00. The rotating head measured 13.5 mm in diameter, with a total of 28 turfs of Tynex®(DuPont, USA) nylon bristles, arranged in circular pattern of 2 distinct height where the groups centrally placed is slightly shorter than the peripheral flank. The peripheral group was longer and only lined in single circular row. Each bristle was approximately 150 µm in diameter and end-rounded (Fig. 2.9). The peripheral turfs of bristles were trimmed down to make all bristles same level (Fig. 2.9). This was done carefully using a pair of sharp scissor under a microscope magnification (20x) (Fig. 2.9). Fig. 2.9 Arrow points to periphery bristles trimmed even to central tufts (20x). This was to ensure more even distribution of applied on surface of specimen during brushing. The head of the powered brush rotated at a rotational 101 speed of 2540 (±5) rpm measured with a stroboscope (Gr 1538-A, Strobotac, General Radio, MA., USA). Test specimens underwent a single focal area of brushing action using battery powered toothbrush with a rotating brush head at a vertically applied force of 2 N (equivalent to 204 g) [15], measured at the bristles-specimen interface. The applied force was in the form of weight placed over the handle of powered toothbrush, perpendicularly to the surface of the specimen beam to be brushed. The duration of the brushing was 22 min continuous with 5 ml of deionized water as the medium. Brushing station which housed the experimental powered toothbrush and force gauge was originally conceived, designed and constructed in laboratory (Fig. 2.10). The toothbrush was fixed in the holder of the brushing station, allowing an alignment of the refillable brush head parallel to the surface of the samples. Weight placed over the handle of powered toothbrush would register a reading of applied brushing force of 2 N in force gauge (Model NK-10, AIGU® GTGY Group Co. Ltd., Hong Kong). The applied force on PMMA specimens was a constant at 2 N throughout, a screw at the bottom of toothbrush support frame allowed such a fine control (Fig.2.10). The specimen holder was designed to hold two specimens at one time and the brush head was centred on the midpoint of two specimens in line with the push lever of the force gauge. Thus, the central portion of specimens were brushed leaving the two tail ends unbrushed (Fig. 2.11). The central area of a specimen was the point of application of the crosshead of universal testing machine and the stylus of profilometer used. 102 Fig.2.10 The brushing station, a PMMA beam specimen holder and a force gauge with weight distributed to maintain stability of the station. 103 Fig. 2.11 Two pieces of specimens fitted into holder with centring marks clearly mark out for brushing target. Deionized water (5 ml for each 22 min session) was contained within the specimens’ holder stage. Each brush head was used for a cumulative time of 66 min before replacing with another. The purpose was to reduce excessive bristles wear of any one particular brush head refill. New brush heads refill unpacked from packaging were subjected to pre-conditioning which involved a single session of 22 min brushing with water as the medium. This was to age the brand new nylon bristles, making them less stiff compared to those used brush head refills. 104 2.7 Surface roughness test The profilometer consists of a stylus that traverses across the surface, and an amplified trace of the profile is provided in surface roughness value Ra. The Ra value is the arithmetical average of all deflection of the profile through the mean sample length, measured in micrometres (µm). A set of mould was randomly picked up for an analysis of surface roughness on the surfaces of stainless steel component plates with profilometer (Surtronic3+, Taylor-Hudson Limited, Leicester, England). This served as reference to the Ra surface roughness of the specimens. The surface analysis was set with a cut-off length (or sampling length) of 0.8 mm, and evaluation length of 4.0 mm. Evaluation length is the length over which the values of surface analysis parameters are assessed. Cut-off length is the length of the reference line used for identifying the irregularities characterizing the surface. Measurements were taken for specimens before and after brushing. Three measurement readings from 3 parallel locations, 1 mm apart were taken on target spot. The quadrant at 9-12 o’clock position within the semi-circular brushed area was earmarked for surface roughness evaluation (see: Fig. 2.12). Fig. 2.12 Schematic illustration of surface roughness value Ra measurement. 105 2.8 Flexural strength test The dimensions of specimens were measured using a scientific calliper (± 0.02 mm) with analogue output (Model No. 1143M, Moore & Wright, Sheffield, England). Three measurement readings were taken for each dimension of length, width and height prior to the start of 3-point bending test. An average measurement calculated to be applied for flexural strength calculation. A universal testing machine (ElectroPuls™ E3000, Instron Industrial Products, Grove City, PA, USA) was use to performed the 3-point bending test on the specimens (Fig. 2.13). The span length between 2 supports was 20.0 mm and the crosshead speed was set at 1.0 mm/min during loading. The load was applied to fracture specimens into two. Load and deflection were recorded with Console software (Instron Industrial Products) and the load and deflection curves were plotted. The maximum load to fracture was applied to formula (1) to calculate the flexural strength of these PMMA specimens beam: (1) Where σ: Flexural strength in 3-point bending test 𝑭: Maximum load on the load-deflection curve (N) 𝓵: Span length between the supports (mm) 𝒃: Width of the specimen measured (mm) 𝒉: Height of the specimen measured (mm) 106 Fig. 2.13 A PMMA specimen for 3-point bending test set up with a loading wedge above and two support wedges below. The loading wedge crosshead speed was set at 1 mm/min and span length between supports was 20.0 mm. 107 2.9 Statistical analysis Data collected on the mean value and the standard deviation of the flexural strength and surface roughness value (Ra) were calculated and statistically analysed using software Predictive Analytics Software (PASW) Statistic 18.0 (Statistical Package for Statistical Science Inc., Chicago, IL, USA). The level of significant α was set at 0.05. Analysis of data was perform with 2 –way ANOVA and the Tukey multiple comparison post hoc analysis were perform (p<0.05) to compare the testing in different water storage days. 108 2.10 Microbiology 2.10.1 Materials and methods The work scheme of the microbiology experiment was represented in an illustration (Fig. 2.14). PMMA specimens of the control group for the flexural strength test which were tested and fractured into two parts were used for this part of the investigation. The specimens with the dimension 22.0 x 6.5 x 4.5 mm were trimmed, fitted and arranged into a 6-well polystyrene tissue culture plate (Iwaki™, Tokyo, Japan) (Fig. 2.15 ). Each well could fit 4 specimen beams, and they required immobilization to prevent specimens from floating in culture medium. Fig. 2.14 Schematic illustration of PMMA specimens cultured with Candida albicans biofilm experiment. 109 Fig. 2.15 PMMA specimens in 6-well tissue culture plate. 110 2.10.2 Specimen grouping Specimens for the microbiology experiment were grouped as shown in Table 2. Table 2 Specimens allocation for microbiology experiment. Brushing performed with moistened bristles S p e c i m e n Brushed Duration (second) 10 20 30 30 with 0.5 g toothpaste Test n=2 2 2 2 2 Control n=2 No brushing performed Specimens were kept in water-jacket incubator with total immersion in deionized water at constant temperature of 37 ºC for 30 days before brushing test conducted. This step was to simulate PMMA in oral environment under constant contact with saliva in the mouth. 111 2.10.3 Candida albicans cultured biofilm growth on specimens Sterilization of PMMA specimens was necessary to ensure the uninterrupted growth of Candida albicans biofilm. For this purpose specimens were immersed in 0.05 % sodium hypochlorite for three minutes with ultrasonic agitation. This was followed by washing and rinsing of the specimens with sterile distilled water for 10 min in ultrasonic water bath. This step was repeated three times to ensure the total removal of residual sodium hypochlorite on the surfaces of PMMA specimens. Standard inoculum for Candida biofilm formation was prepared as previously described [32]. Subculture of Candida albicans was incubated on Sabouraud dextrose agar (SDA) (Gibco, Paisley,UK) at 37 ºC overnight. The Candida albicans subculture was used for the subsequent broth culture. The broth culture was prepared by inoculate a large loopful (3-5 colonies) of Candida strain using a sterile wire loop and dissolved in 20 ml liquid medium of yeast nitrogen base (YNB) ( Difco Laboratory Inc., USA) with 50mM glucose. The broth culture was kept in a temperature control shaker (Stuart SI500, Bibly Scientific Limited, Staffordshire, UK) set at 80 rpm and incubated at 37 ˚C for 24 hour. At the end of 24h, the broth culture was then centrifuged at 3500 rpm for 10 min at 37 ºC and resultant cells pellets were washed twice with phosphate-buffer saline (PBS) solution. The cells pellets were resuspended in 15 ml of a medium containing YNB with 100mM glucose. A final suspension of approximately 107 cells/ml of Candida albicans was prepared through dilution. The PMMA specimens in the tissue culture plate were immersed in this final suspension. The plate was placed in a temperature control shaker rotating at 112 80 rpm and incubated for 90 min at 37 ºC, to allow Candida albicans to adhere onto the PMMA specimens. Subsequently, the specimens were washed with PBS twice to remove nonadherent cells. Culture medium containing YNB with 100 mM glucose was added to cover specimens in plate and continued biofilm development in a temperature control shaker at 80 rpm with incubation temperature at 37 ºC for 48 hours. At the completion of biofilm development after 48 hours, the culture medium was poured away and the specimens were washed lightly with PBS solution twice to remove non-adherent cells. 113 2.10.4 Brushing protocol for Candida albicans coated specimens The specimens were carefully removed from the culture plate and secured in the holder of the brushing station, prepared for the brushing test. A clean new brush head was used for each brushing test. It was necessary to disinfect the bristles before the test to ensure that the brushed surfaces on specimens were free from any contamination with microorganisms. The procedure to disinfect the bristles of brush heads involved immersion into a sodium hypochlorite solution 6.25 % (Clorox®) and placement in a ultrasonic bath (BioSonic UC100, Whaledent, West Sussex, UK) for 5 minutes (Fig. 2.16) This was followed by rinsing the brush heads in sterile distilled water for 15 minutes in a ultrasonic bath, and this step was repeated three times to ensure a complete rinse off residual sodium hypochlorite from within bristles in the brush heads. Fig. 2.16 Disinfection of brush heads and bristles of powered toothbrush. 114 Specimens from the test group were subjected to brushing whereas the control group was spared intact. Brushing force applied on test specimens was set at 2 N but the length of time varied. Two pieces of securely positioned specimens were subjected to brushing at one time (Fig. 2.17). Fig. 2.17 A close-up view of specimens in a holder with a brush head aligned to the top surface of two pieces of specimens. The same holder in previous experiment was modified to accommodate shorter specimens. The green material is silicone impression material (Genie™, Sultan Healthcare Inc. USA) to hold specimens in place, the rest is cold-cured acrylic resin. Tightened metal screw fastened the specimens to provide additional stability. 115 The brushing protocol proposed was set for 10 s, 20 s, 30 s and 30 s with toothpaste as depicted in Table 3. The control group was not brushed, thus the biofilm was intact. Table 3 Brushing protocol Test Group. Brushing with moistened bristles brushes. 10 s Control group. 20 s No brushing 30 s 30 s with 0.5g toothpaste During the brushing procedure, the PMMA specimens with Candida biofilm and the heads of the powered toothbrush were enclosed within a layer of cling-wrap to prevent the sputter of microorganism, which could lead to contamination of surrounding environment. The specimens and the wrap were later discarded as bio-hazard waste. The used brush heads were then sterilised in sodium hypochlorite at a concentration of 6.25 % with ultrasonic agitation. . 116 2.10.5 SEM of Candida albicans coated specimens Specimens with the attached biofilm from brushed and non-brushed groups were prepared for scanning electron microscopy (SEM) by fixing them for 2 hours in a 2.5% glutaldehyde (v/v) (BDH Lab. Supplies, UK) and then dehydrated for 15 minutes at each concentration in a graded ethanol series (70, 85, 95 and absolute alcohol). The dry specimens were mounted on aluminium stubs and sputter coated with gold in an ion sputter coater (JFC-1100 JEOL, Tokyo, Japan) and each sample was examined with a Hitachi S-3400N (VP-SEM) scanning electron microscope at Electron Microscope Unit, Faculty of Medicine, The University of Hong Kong. Observation was made in high-vacuum mode at 15 kV. Images of high magnification were taken on the specimens from control (non-brushed) group and tested (brushed) groups. For the brushed specimens, the zooming target under the scanning electron microscope was the brushed areas that need to be scanned and evaluated. 117 3. Results 3.1 Surface roughness The mean ± standard deviation of the Ra value of surfaces of PMMA specimens before brushing was 0.29 ± 0.06 μm. The mean of the Ra values after brushing for 22 min with water was 0.27 ± 0.06 μm (Fig. 3.1), which were significantly smaller than that of before brushing (p = 0.022). Among the groups of specimen, the number of days in water storage affect the Ra before and after brushing differently (p = 0.006) with lowest Ra recorded from specimen groups after 7 days in water storage compared to no storage. A 2-way ANOVA (Table 4) was conducted to examine the effect of before-after brushed factor and the duration of water storage factor on the surface roughness value mean. There did not appear to be any interaction between the factors of duration in water storage and before-after brushing (p = 0.826). Tukey analysis revealed that the surface roughness value of 7 days water storage was significantly different from 0, 15, 30 and 60 days water storage (Table 5, Fig. 3.2). 118 Fig.3.1 Boxplot of mean surface roughness value Ra (µm) for specimen before and after brushed (p<0.05). 119 Table 4 Result of 2-way ANOVA of surface roughness value of before and after brushed specimens in different days of water storage. Dependent Variable: Surface roughness Type III Sum of Source Squares df Mean Square F Sig. a 11 .008 2.219 .014 20.230 1 20.230 5.812E3 .000 Storage .059 5 .012 3.386 .006 Brushed .019 1 .019 5.319 .022 Storage * Brushing .008 5 .002 .432 .826 Error .835 240 .003 Total 21.150 252 .920 251 Corrected Model Intercept Corrected Total .085 a. R Squared = .092 (Adjusted R Squared = .051) 120 Table 5 Result of Tukey post hoc multiple comparison of surface roughness value Ra with various duration in water storage 121 Mean surface roughness Value Rₐ (µm) 0.4 0.35 Mean Rₐ (µm) 0.3 0.25 0.2 Before Brushing After Brushing 0.15 0.1 0.05 0 0 day 1 day 7 days 15 days 30days 60 days No. of days in water storage at 37 ° C Fig. 3.2 Bar chart of mean surface roughness value Ra (µm) in various duration of water storage with error bars denoting standard deviation. 122 3.2 Flexural strength. Table 6 and Fig. 3.3 showed the mean flexural strength of specimen with varying the water storage condition. The mean from the group of brushed specimen and underwent 7 day in water storage recorded the lowest value of 87.37 ± 9.23 MPa. The highest recorded value of 103.72 ± 8.52 MPa was from the brushed specimen group without water storage. The mean value of specimens from non-brushed specimen in 15 days water storage group was relatively higher than other storage day groups. Table 6 Mean flexural strength results (Test: brushed; Control: non-brushed) Day(s) in Water Storage Specimen 1 2 3 4 5 6 7 8 9 10 11 12 0 day 1 day 7 days 15 days Control 112.82 128.56 87.53 120.92 120.86 84.66 96.04 86.52 115.20 99.85 103.22 71.71 30 days 60 days Test 114.68 97.75 91.59 96.77 102.39 97.41 108.08 117.8 97.68 106.1 115.02 99.36 Control 82.78 98.59 110.65 108.62 108.15 99.52 96.18 88.16 81.67 100.8 103.6 94.2 Test 103.54 111.52 88.99 88.18 81.98 104.85 102.87 112.73 119.32 101.55 89.32 93.03 Control 100.29 111.26 105.41 96.79 91.88 68.31 81.33 97.73 80.60 87.07 104.44 83.69 Test 111.03 92.62 88.11 86.48 81.52 86.64 94.10 87.55 74.24 79.33 84.47 82.39 Control 84.38 86.94 80.45 106.48 107.82 95.12 86.61 80.18 97.44 88.45 96.72 74.78 Test 84.78 101.46 83.93 101.33 85.66 87.60 64.36 88.76 84.32 86.91 95.06 91.35 Test 81.22 89.77 105.74 89.69 105.05 104.68 84.93 99.40 109.54 78.50 99.45 103.97 Control 86.90 70.30 80.72 83.81 98.22 92.52 93.67 88.65 88.07 87.68 95.87 74.46 Test 95.72 100.88 89.52 96.44 92.10 97.52 85.48 100.41 98.13 85.92 89.68 92.97 Control 75.80 107.43 87.68 73.51 82.10 82.57 102.23 111.41 89.87 112.04 83.03 80.12 Mean 103.72 Standard deviation 8.52 97.74 9.68 99.82 11.53 92.40 12.25 87.37 9.23 90.44 10.39 87.96 102.32 95.99 9.66 17.62 10.62 86.74 8.36 93.73 5.28 90.65 13.93 123 Mean flexural strength of PMMA specimens 140 * ** Flexural Strength (MPa) 120 100 80 Test 60 Control 40 20 0 0 day 1 day 7 days 15 days 30 days No. of days in water storage at 37 °C 60 days Fig. 3.3 Bar chart of mean flexural strength with error bars represents standard deviation. Horizontal lines denoting significant difference in means from Tukey post hoc multiple comparison of days in water storage (p<0.05) (Test=brushed, Control=non- brushed) A 2-way ANOVA (Table 7) was conducted to examine the effect of brushing and water storage on the flexural strength. There was a significant interaction between the effect of brushing and the factor on number of days in water storage (p = 0.003). There was no significant difference in flexural strength between before and after brushing the specimens (p = 0.452). There was a significant difference in the flexural strength among groups of specimens in different days in water storage (p = 0.006). Therefore, Tukey HSD’s test was performed to compare all conditions including duration of days in water storage. The flexural strengths of various days in water storage conditions are summarized in Table 8 and Fig.3.4. 124 Table 7 Result of 2-way ANOVA of flexural strength between before-after brushing and duration in water storage. Type III Sum of Source Squares df Mean Square F Sig. a 11 409.819 3.369 .000 1274482.945 1 1274482.945 1.048E4 .000 Storage 2095.628 5 419.126 3.446 .006 Brushed 69.278 1 69.278 .570 .452 2343.099 5 468.620 3.853 .003 Error 16055.440 132 121.632 Total 1295046.390 144 20563.445 143 Corrected Model Intercept Storage * Brushed Corrected Total 4508.005 a. R Squared = .219 (Adjusted R Squared = .154) 125 Table 8 Result of Tukey post hoc multiple comparison for flexural strength under the factor duration of water storage 126 Fig. 3.4 Estimated marginal mean of flexural strength. 127 3.3 SEM Observations under SEM revealed presence of Candida albicans biofilms on the surfaces of specimens. Specimen without brushing showed presence of thick biofilm layer consisted of dense network of yeasts, pseudohyphae and hyphae embedded in a thick EPS layer (Fig. 3.5). Fig. 3.5 SEM micrograph on a specimen with no brushing, an intact biofilm showed intricate network of yeast cells and hyphae (x3700). 128 Specimens with surface irregularities and porosities demonstrated the ingrowth of Candida albicans into micro crevices (Fig. 3.6 & Fig. 3.7). These Candida albicans cells and hyphae were inaccessible to the rotating brush bristles. Fig. 3.6 Porosities (red arrows) on a PMMA specimen (x500). Fig. 3.7 Candida albicans cells grew into porosities on a PMMA specimen (x1000). 129 A distinct brushed area on specimens was visible (Fig. 3.7) compared to non-brushed specimens (Fig. 3.8) after fixation and dehydration. SEM micrograph at lower magnification showed the same distinct brushed area (Fig.3.9). Fig. 3.7 Mark out dash line area brushed for 20 s. Fig. 3.8 Control group non-brushed with intact biofilm. Fig. 3.9 The semi-circle dash line area was brushed for 20 s (x32). 130 Candida albicans cells were evident on surface of PMMA specimens after brushing with powered toothbrush for 10 s under the SEM evaluation (Fig.3.9). Fig. 3.9 A specimen from test group after 10 s of brushing performed, cells and hyphae were found (x500). The micrographs of specimens after 20 s and 30 s brushing showed present of scanty number of Candida albicans cells and some crushed cell debris (Fig. 3.11 and Fig. 3.12) compared to 10 s brushing. Less cells debris was observed on specimen surface after 30 s brushing protocol compare to 20 s brushing (Fig 3.12). 131 Fig. 3.11 A specimen after 20 s of brushing showed the presence of Candida cells and some crushed cell debris (x1000). Fig.3.12 A test specimen after 30 s of brushing performed (x500). 132 Fig. 3.11 illustrated the SEM micrograph taken of specimen after 30 s brushing with toothpaste. It revealed the total absent of yeast cell and present of filler particles from toothpaste which were evenly distributed. The present of filler particles were due to no rinsing procedure in the brushing protocol. Fig.3.13 A specimen was brushed for 30 s with toothpaste showed presence of well scattered filler particles (red arrows) and absence of Candida cell (x2000). Evaluation of the clean PMMA surface of specimen without Candida albicans growth revealed the topography of PMMA surfaces were even and uniform with linear layers stacking pattern. Some layers appeared more extruded (Fig.3.13 and Fig. 3.15). This was a contrast to the polished surface of PMMA with fine silicon carbide paper No. 500 (Struers, Denmark) as shown in Fig.3.14 which appeared relatively rough surface topography with innumerable overt scored lines. 133 Fig. 3.14 Contrast between polished and unpolished surface. Area below red dotted line was polished with No. 500 silicon carbide paper, area immediately above red dotted line was manifestation of surface shrinkage of PMMA which was indented and preclude polishing. Fig. 3.15 Clean surface of PMMA specimen without Candida albicans biofilm. 134 4. Discussion 4.1 Surface roughness Surface roughness is associated with the surface finishing of a dental prosthesis. The highly polished surface of PMMA dental prosthesis has a low surface roughness value Ra compared to a coarse finish surface. In this experiment the specimens of PMMA were not subjected to post fabrication finishing and polishing. Thus, there was an observation of surfaces of PMMA specimens after brushing protocol that showed a decrease in the surface roughness value Ra. This might have been due to the polishing phenomena of the nylon bristles on the surfaces of polymer. The same observation was reported by Harrison et al.[15]. This would suggest that the rotating motion of nylon bristles of the experimental powered toothbrush on the surface of PMMA, did not pose an increased risk of abrading the surface during brushing action, when water was used as medium. However, the favourable effect may be lost in a situation where surface of PMMA deteriorates in service condition and abrasion effect would be probable. When toothpaste was used during brushing, the surface roughness of PMMA acrylic resin increased due to the abrasive action of filler particles in a toothpaste [33]. The experiment with Candida albican showed that the removal of Candida biofilm was more thorough when some toothpaste was added during brushing. It is noteworthy that toothpastes may not be suitable in daily denture cleaning routine with a powered toothbrush. Brushing with a non-abrasive liquid medium such as soap and mouth rinses would avoid the risk of abrasion, but the Candida biofilm would not be thoroughly removed. The supplementary chemical cleaning method such as hypochlorite and chlorhexidine immersion might be necessary in order to totally eliminate Candida biofilms [16]. 135 The force of 2 N equivalents to a load of 204 g applied on the brushed area throughout the experiment appeared sufficient to remove biofilm and did not cause visible damage to the PMMA surfaces. Previous research has demonstrated that the force applied with powered toothbrush in dental hygiene practise was lower compared to using manual tooth brushing [34]. The forces recorded for powered toothbrushes were in the range of 80-190 g (as load) and in the 250 g range when manual toothbrushes were used [34]. The actual force applied in individual varies greatly during the cleaning process, correlation between cleaning forces applied intraorally and extraorally may be an overinterpretation. However, it was reasonable not to go far beyond these ranges of force indicated in previous researches [35-37]. It would be of interest to research into the forces applied by individual when performing denture brushing with a powered toothbrush. The specimens were not subjected to polish finishing, this might have contributed to a higher surface roughness value before brushing. However, a report stated that surface roughness was influenced to the greatest extent by finishing and polishing procedure and to a lesser extent by acrylic resin material itself [38]. The SEM evaluation of a PMMA specimen in present study confirmed this, as shown in Fig. 3.14 and Fig. 3.15. Therefore, it was reasonable to avoid adding this variable into the current experiment by not polishing finished PMMA specimen beams. It was interesting to note that current study with unpolished finish specimens showed a reduction in surface roughness value after brushing whereas others studies reported no change [15, 39, 40] with polished finish PMMA specimens, when brushing was carried out with water only. This phenomena appeared to be worthy of further examination. 136 4.2 Flexural strength The data from this experiment showed that the PMMA beams after 7 days in water storage would experience a decline in flexural strength compared to no water storage. Specimens in 15, 30 and 60 days of water storage produced relatively constant mean flexural strength. This may be attributed to the plasticiser effect of water molecules acting on PMMA polymer molecules creating a change in strength of the bulk material. This plasticiser influence started from the beginning until it reached a plateau at about the day 15 in water storage. There seemed to be little agreement as to how long PMMA polymers should be immersed prior to their mechanical testing. Despite the international standard guidelines points to 50 hours of water immersion [41], Takahashi et al. [42] suggested that the equilibrium strength of some denture polymers may well exceed 30 days. Although they recommend a 4-month water immersion protocol, the water sorption mainly occurs during the initial 14 days [43]. In the study by Chow et al. water sorption saturation was attained about 30 days after immersion in water at a constant temperature of 37 °C and the linear expansion was 0.45 % [44]. The factor on effect of temperature between control group and test group was not convincingly accounted for in the present experiment. The specimens from control group which had not undergone storage in water were kept exposed to room temperature whereas the test groups were kept at 37 °C. An assumption was made that the influence of the difference would be negligible; on the other hand, this significance might have been overlooked. 137 The effect and influence of brushing using a powered toothbrush on PMMA specimens beam seemed inconclusive from the findings gathered in the current experiment. There was uncertainty appeared during the data analysis (Fig. 3.4) where the lines plot exhibited confusing pattern of intersection, making meaningful interpretation of interaction among factors impossible. The hypothesis accounted for this uncertainty might be due to other confounding factors which failed to be recognized. Another possibility might be the experimental set-up was not sensitive enough to detect minor differences in mean flexural strength. The parameter of surface microhardness might seem to be a viable alternative to be investigated [45] after having subjected the polymer surface to powered toothbrush brushing. Although the same material was used, separate batches of specimens were fabricated. This might account for some differences between these sample groups during testing for flexural strength as well as surface roughness value. 138 4.3 SEM SEM examination of specimens revealed the presence of thick layers of matured Candida albicans biofilm on surfaces of PMMA for non-brushed specimens. The biofilm consisted of intricate networks of yeast cells and hyphae deeply embedded into porosities, cracks, and crevices of the PMMA specimens. Brushing with a powered toothbrush for 10 s, 20 s, 30 s and 30 s plus using some toothpaste could not remove the Candida from the porosities. However, on more even surfaces where irregularities were absent, all protocols of brushing showed the thick layer of Candida albicans biofilm was cleanly brushed away. The result of the present study was consistent with Harrison et al. [15]. They demonstrated that powered toothbrush cleaning could remove Candida biofilm when observed under SEM evaluation. SEM micrographs showed that Candida albicans biofilm was removed from PMMA specimen surfaces with different brushing duration experimented. More efficient removal was seen with 30 s compared to 10 s brushing duration. The removal was not totally complete for brushing time especially in 10 s and 20 s, since some cells and cell fragments remained attached on the surface irregularities of specimens. The reason for this might be that the Candida albicans cells were shielded away from the movement of bristles during brushing due to the uneven surface topography in microscopic scale. Another reason postulated could be the bristles maintained no contact with the surface of PMMA specimens during brushing. This condition of non-contact exited because assumption was made that when the 2 N forces was applied to the powered toothbrush, the pressure was equally loaded and evenly distributed to all bristles in the brush head onto the target brushed area. This was certainly not the case in such an experiment 139 set-up. Human error might have contributed to this, where the seating of specimens into the holder and lowering the brush head was performed without any aid of precision control and monitoring, it was entirely carried out under human visual judgement that was prone to error [46, 47]. There was uncertainty concerned the re-deposition of Candida albicans cells and cell debris back to surface irregularities during brushing after their removal. This could contribute to erroneous interpretation of result in current study. A constant supply of running stream of water to rinse off dislodged cells and debris might have allayed this concern. Brushing with some added toothpaste seemed to produce a more favourable result as shown in the scanning electron micrographs (Fig. 3.13) when compared to brushing alone (Fig.3.12). No remains of Candida cell were found during SEM observation base on this brushing protocol. However, previous studies have confirmed that the surfaces of PMMA specimens were abraded leading to increased surface roughness especially when toothpaste was added and the brushing time was extended [33, 36, 48]. Thus, increased surface roughness would lead to increased denture plaque retention and microorganism accumulation on the denture surfaces [49], as well as to promote the initial adhesion of microorganism [50]. In view of the facts presented, the mechanical cleaning method using powered toothbrush requires supplementary chemical or other cleaning methods in order to achieve optimal level of denture hygiene [10, 20]. Powered toothbrush offers the advantages of an increased ease and efficiency, especially for the frail elderly who may have lost some degree of manual dexterity [5, 6, 51]. A powered toothbrush is intended as one device for 140 two purposes; cleaning dentures extraorally and brushing the teeth intraorally. Other methods of cleaning dental prostheses, such as chemical soaking, could not measure up to powered toothbrush in this unique characteristic of both intra- and extraoral applications. However, extrapolating findings from current laboratory investigations to clinical outcome is always difficult and must be exercised with caution. Evaluation on biofilm removal may be expected to show differences in results from clinical use. 141 5. Conclusion Within the limit of these experiments the following conclusion may be made: 1. A battery powered toothbrush with a simple mono direction rotational movement could be a suitable device for hygiene maintenance of acrylic resin dental prostheses. 2. The results suggested that surfaces of PMMA specimens after brushing with a powered toothbrush demonstrated no adverse effect in flexural strength and no increase in surface roughness value (Ra) when water was used as medium. 3. In vitro Candida albicans biofilm cultured on surfaces of PMMA specimens can be removed by brushing with powered toothbrush. 4. Further research is required to expand and redefine the experiments. 142 Appendix 1. Surface Roughness Test Table 9 Raw data of surface roughness value Ra for PMMA specimens Water storage Brushed 0 day 1 day 7 days 15 days 30 days 60 days No. Before After Before After Before After Before After Before After Before After 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 0.22 0.26 0.28 0.38 0.26 0.22 0.26 0.30 0.30 0.32 0.34 0.38 0.32 0.38 0.26 0.26 0.24 0.20 0.36 0.36 0.24 0.26 0.24 0.32 0.28 0.34 0.32 0.24 0.34 0.30 0.28 0.30 0.28 0.38 0.32 0.36 0.30 0.20 0.22 0.28 0.26 0.34 0.22 0.30 0.34 0.32 0.32 0.18 0.36 0.28 0.20 0.40 0.38 0.26 0.26 0.24 0.36 0.20 0.32 0.24 0.36 0.26 0.18 0.40 0.28 0.16 0.32 0.32 0.24 0.30 0.32 0.16 0.26 0.26 0.20 0.26 0.24 0.42 0.38 0.32 0.30 0.26 0.24 0.20 0.26 0.24 0.26 0.28 0.20 0.20 0.28 0.22 0.28 0.34 0.30 0.18 0.28 0.26 0.20 0.30 0.34 0.32 0.28 0.18 0.34 0.22 0.24 0.30 0.18 0.22 0.22 0.24 0.24 0.24 0.22 0.20 0.18 0.30 0.26 0.20 0.22 0.30 0.24 0.24 0.20 0.32 0.32 0.28 0.24 0.30 0.24 0.34 0.32 0.30 0.30 0.22 0.28 0.32 0.22 0.38 0.32 0.36 0.26 0.30 0.36 0.24 0.34 0.22 0.34 0.24 0.26 0.26 0.28 0.34 0.26 0.26 0.22 0.32 0.36 0.22 0.24 0.24 0.34 0.26 0.32 0.28 0.30 0.32 0.26 0.30 0.34 0.22 0.34 0.20 0.32 0.32 0.30 0.38 0.28 0.34 0.24 0.32 0.30 0.32 0.36 0.34 0.32 0.32 0.32 0.24 0.22 0.28 0.20 0.32 0.26 0.22 0.24 0.28 0.24 0.36 0.28 0.26 0.38 0.36 0.30 0.32 0.34 0.36 0.26 0.20 0.30 0.26 0.42 0.38 0.42 0.24 0.14 0.20 0.16 0.32 0.36 0.32 0.26 0.32 0.22 0.24 0.40 0.38 0.42 0.38 0.30 0.16 0.22 0.24 0.36 0.30 0.16 0.14 0.32 0.24 0.30 0.38 0.26 0.24 0.30 0.26 0.28 0.42 0.30 0.40 0.32 0.24 Mean 0.29 0.29 0.28 0.28 0.26 0.24 0.30 0.28 0.31 0.28 0.31 0.28 Standard Deviation 0.06 0.05 0.07 0.07 0.05 0.04 0.05 0.04 0.04 0.06 0.09 0.08 R a ( µ m ) 1.1 Surface roughness statistical output Between-Subjects Factors Days in Water Storage Before and After Brushed Value Label N 0 0 day 42 1 1 day 42 2 7 days 42 3 15 days 42 4 30 days 42 5 60 days 42 0 Before Brushed 126 1 After Brushed 126 143 Before and After Brushed Surface roughness Before Brushed Statistic Mean .2919 95% Confidence Interval for Lower Bound .2811 Mean Upper Bound .2923 Median .3000 .004 Std. Deviation After Brushed .00548 .3027 5% Trimmed Mean Variance Std. Error .06146 Minimum .14 Maximum .42 Range .28 Interquartile Range .10 Skewness -.110 .216 Kurtosis -.585 .428 Mean .2748 .00522 95% Confidence Interval for Lower Bound .2644 Mean Upper Bound .2851 5% Trimmed Mean .2742 Median .2600 Variance Std. Deviation .003 .05863 Minimum .14 Maximum .42 Range .28 Interquartile Range .08 Skewness Kurtosis .224 .216 -.262 .428 144 Descriptive Statistics Dependent Variable:Surface roughness Days in Water Before and After Storage Brushed Mean Std. Deviation N 0 day Before Brushed .2924 .05744 21 After Brushed .2933 .04662 21 Total .2929 .05167 42 Before Brushed .2848 .06809 21 After Brushed .2781 .07040 21 Total .2814 .06849 42 Before Brushed .2638 .05162 21 After Brushed .2371 .03964 21 Total .2505 .04742 42 Before Brushed .2971 .04703 21 After Brushed .2800 .04472 21 Total .2886 .04615 42 Before Brushed .3067 .04487 21 After Brushed .2819 .05582 21 Total .2943 .05157 42 Before Brushed .3067 .08610 21 After Brushed .2781 .07561 21 Total .2924 .08132 42 Before Brushed .2919 .06146 126 After Brushed .2748 .05863 126 Total .2833 .06056 252 1 day 7 days 15 days 30 days 60 days Total Levene's Test of Equality of Error Variances a Dependent Variable:Surface roughness F df1 3.016 df2 11 Sig. 240 .001 Tests the null hypothesis that the error variance of the dependent variable is equal across groups. a. Design: Intercept + Storage + Brushed + Storage * Brushed 145 Estimated Marginal Means 1. Days in Water Storage Dependent Variable:Surface roughness Days in 95% Confidence Interval Water Storage Mean Std. Error Lower Bound Upper Bound 0 day .293 .009 .275 .311 1 day .281 .009 .263 .299 7 days .250 .009 .233 .268 15 days .289 .009 .271 .307 30 days .294 .009 .276 .312 60 days .292 .009 .274 .310 2. Before and After Brushed Dependent Variable:Surface roughness 95% Confidence Interval Before and After Brushed Mean Std. Error Lower Bound Upper Bound Before Brushed .292 .005 .282 .302 After Brushed .275 .005 .264 .285 146 3. Days in Water Storage * Before and After Brushed Dependent Variable:Surface roughness Days in 95% Confidence Interval Water Before and After Storage Brushed 0 day Before Brushed .292 .013 .267 .318 After Brushed .293 .013 .268 .319 Before Brushed .285 .013 .259 .310 After Brushed .278 .013 .253 .303 Before Brushed .264 .013 .238 .289 After Brushed .237 .013 .212 .263 Before Brushed .297 .013 .272 .323 After Brushed .280 .013 .255 .305 Before Brushed .307 .013 .281 .332 After Brushed .282 .013 .257 .307 Before Brushed .307 .013 .281 .332 After Brushed .278 .013 .253 .303 1 day 7 days 15 days 30 days 60 days Mean Std. Error Lower Bound Upper Bound Tests of Normality a Before and After Brushed Surface Before roughness Brushed After Brushed Kolmogorov-Smirnov Statistic df Sig. Shapiro-Wilk Statistic df Sig. .105 126 .002 .981 126 .071 .115 126 .000 .980 126 .064 a. Lilliefors Significance Correction 147 Homogeneous Subsets Surface roughness Tukey HSD Days in Subset Water Storage N 1 2 7 days 42 .2505 1 day 42 .2814 15 days 42 .2886 60 days 42 .2924 0 day 42 .2929 30 days 42 .2943 Sig. .159 .2814 .918 Means for groups in homogeneous subsets are displayed. Based on observed means. The error term is Mean Square(Error) = .003. Profile Plots Fig. 6.1 Line graph of estimated marginal mean in various days of water storage 148 2. Flexural Strength Test statistical output Between-Subjects Factors Days in water storage Before and After Brushed Value Label N 0 0 day 24 1 1 day 24 2 7 days 24 3 15 days 24 4 30 days 24 5 60 days 24 0 Before brush 72 1 After Brushed 72 Tests of Normality a Days in water storage Flexural strength Kolmogorov-Smirnov Statistic df Shapiro-Wilk Sig. Statistic df Sig. 0 day .106 24 .200 * .972 24 .726 1 day .091 24 .200 * .980 24 .903 7 days .186 24 .032 .933 24 .112 15 days .158 24 .127 .943 24 .190 30 days .102 24 .200 * .976 24 .821 60 days .088 24 .200 * .979 24 .876 a. Lilliefors Significance Correction *. This is a lower bound of the true significance. 149 Test of Homogeneity of Variance Levene Statistic Flexural strength df1 df2 Sig. Based on Mean 2.004 5 138 .082 Based on Median 1.604 5 138 .163 1.604 5 104.878 .166 2.005 5 138 .082 Based on Median and with adjusted df Based on trimmed mean 150 Descriptive Statistics Dependent Variable:Flexural strength Days in water Before and After storage Brushed Mean 0 day Before brush 97.7433 9.67561 12 After Brushed 1.0374E2 8.55863 12 Total 1.0074E2 9.44458 24 Before brush 92.4000 12.52819 12 After Brushed 99.8233 11.53115 12 Total 96.1117 12.37070 24 Before brush 90.4475 10.39052 12 After Brushed 87.3733 9.23938 12 Total 88.9104 9.74305 24 1.0232E2 17.62734 12 After Brushed 87.9600 9.66076 12 Total 95.1421 15.71840 24 Before brush 86.7392 8.36010 12 After Brushed 95.9950 10.65278 12 Total 91.3671 10.49042 24 Before brush 90.6492 13.93243 12 After Brushed 93.7308 5.28456 12 Total 92.1900 10.42450 24 Before brush 93.3839 13.10185 72 After Brushed 94.7711 10.81627 72 Total 94.0775 11.99168 144 1 day 7 days 15 days 30 days 60 days Total Before brush Std. Deviation N 151 Levene's Test of Equality of Error Variances a Dependent Variable:Flexural strength F df1 2.729 df2 11 Sig. 132 .003 Tests the null hypothesis that the error variance of the dependent variable is equal across groups. a. Design: Intercept + Storage + Brushed + Storage * Brushed Tests of Between-Subjects Effects Dependent Variable:Flexural strength Type III Sum of Source Squares df Mean Square F Sig. a 11 409.819 3.369 .000 1274482.945 1 1274482.945 1.048E4 .000 Storage 2095.628 5 419.126 3.446 .006 Brushed 69.278 1 69.278 .570 .452 2343.099 5 468.620 3.853 .003 Error 16055.440 132 121.632 Total 1295046.390 144 20563.445 143 Corrected Model Intercept Storage * Brushed Corrected Total 4508.005 a. R Squared = .219 (Adjusted R Squared = .154) 152 Estimated Marginal Means 1. Days in water storage Dependent Variable:Flexural strength Days in 95% Confidence Interval water storage Mean Std. Error Lower Bound Upper Bound 0 day 100.744 2.251 96.291 105.197 1 day 96.112 2.251 91.659 100.565 7 days 88.910 2.251 84.457 93.364 15 days 95.142 2.251 90.689 99.595 30 days 91.367 2.251 86.914 95.820 60 days 92.190 2.251 87.737 96.643 2. Before and After Brushed Dependent Variable:Flexural strength 95% Confidence Interval Before and After Brushed Mean Std. Error Lower Bound Upper Bound Before brush 93.384 1.300 90.813 95.955 After Brushed 94.771 1.300 92.200 97.342 3. Days in water storage * Before and After Brushed Dependent Variable:Flexural strength Days in 95% Confidence Interval water Before and After storage Brushed 0 day Before brush 97.743 3.184 91.446 104.041 After Brushed 103.744 3.184 97.446 110.042 Before brush 92.400 3.184 86.102 98.698 After Brushed 99.823 3.184 93.526 106.121 Before brush 90.447 3.184 84.150 96.745 After Brushed 87.373 3.184 81.076 93.671 Before brush 102.324 3.184 96.026 108.622 After Brushed 87.960 3.184 81.662 94.258 Before brush 86.739 3.184 80.441 93.037 After Brushed 95.995 3.184 89.697 102.293 1 day 7 days 15 days 30 days Mean Std. Error Lower Bound Upper Bound 153 60 days Before brush 90.649 3.184 84.351 96.947 After Brushed 93.731 3.184 87.433 100.029 Multiple Comparisons Flexural strength Tukey HSD 95% Confidence Interval (I) Days in water (J) Days in water storage storage 0 day 1 day 7 days 15 days 30 days Std. (I-J) Error Sig. Upper Bound Bound 13.8395 3.18371 .004 2.6260 21.0407 15 days 5.6017 3.18371 .495 -3.6057 14.8090 30 days 9.3767 3.18371 .043 .1693 18.5840 60 days 8.5538 3.18371 .085 -.6536 17.7611 0 day -4.6321 3.18371 .693 -13.8395 4.5753 7 days 7.2012 3.18371 .217 -2.0061 16.4086 15 days .9696 3.18371 1.000 -8.2378 10.1770 30 days 4.7446 3.18371 .671 -4.4628 13.9520 60 days 3.9217 3.18371 .821 -5.2857 13.1290 3.18371 .004 -21.0407 -2.6260 1 day -7.2012 3.18371 .217 -16.4086 2.0061 15 days -6.2317 3.18371 .372 -15.4390 2.9757 30 days -2.4567 3.18371 .972 -11.6640 6.7507 60 days -3.2796 3.18371 .907 -12.4870 5.9278 0 day -5.6017 3.18371 .495 -14.8090 3.6057 1 day -.9696 3.18371 1.000 -10.1770 8.2378 7 days 6.2317 3.18371 .372 -2.9757 15.4390 30 days 3.7750 3.18371 .843 -5.4324 12.9824 60 days 2.9521 3.18371 .939 -6.2553 12.1595 0 day 4.6321 3.18371 .693 Lower -4.5753 7 days 1 day Mean Difference 11.8333 -11.8333 * * * * 0 day -9.3767 3.18371 .043 -18.5840 -.1693 1 day -4.7446 3.18371 .671 -13.9520 4.4628 7 days 2.4567 3.18371 .972 -6.7507 11.6640 15 days -3.7750 3.18371 .843 -12.9824 5.4324 60 days -.8229 3.18371 1.000 -10.0303 8.3845 154 60 days 0 day -8.5538 3.18371 .085 -17.7611 .6536 1 day -3.9217 3.18371 .821 -13.1290 5.2857 7 days 3.2796 3.18371 .907 -5.9278 12.4870 15 days -2.9521 3.18371 .939 -12.1595 6.2553 30 days .8229 3.18371 1.000 -8.3845 10.0303 Based on observed means. The error term is Mean Square(Error) = 121.632. *. The mean difference is significant at the .05 level. Homogeneous Subsets Flexural strength Tukey HSD Subset Days in water storage N 7 days 24 88.9104 30 days 24 91.3671 60 days 24 92.1900 92.1900 15 days 24 95.1421 95.1421 1 day 24 96.1117 96.1117 0 day 24 Sig. 1 2 1.0074E2 .217 .085 Means for groups in homogeneous subsets are displayed. Based on observed means. The error term is Mean Square(Error) = 121.632. 155 Fig 6.2 Box plot of flexural strength in various days in water storage 156 Table 10 Surface roughness value of SS mould-plates Mean Ra (µm) on surfaces of SS mould Plate label Side A Side B B3 0.30 0.40 B5 0.29 0.30 B7 0.26 0.35 B9 0.24 0.23 B11 0.18 0.28 3. Images from experiment Fig. 6.3 Disassembled stainless steel mould with fasten screw shown 157 Fig. 6.4 Fracture surfaces of specimen, solid black arrows denote tension areas, red arrows point to compression area (x10) Fig. 6.5 Black arrow points to area brushed for 22 min with brand new brush head showing noticeable scratch marks, blue arrow points to target area (dash line) brushed for 22 min with aged bristles, no scratches observed. 158 Fig. 6.6 Processed specimen beams after removal from mould shows surface porosities on top side (vertically displayed) and the underside of specimens had no porosity (horizontally arranged) Fig. 6.7 Hydraulic press and spring clamp with screw knob 159 Fig. 6.8 Generic brand battery powered toothbrush used in current experiment Fig. 6.9 Candida albicans of matured biofilm (x7000) 160 References 1. Coulthwaite, L. and J. Verran, Potential pathogenic aspects of denture plaque. British Journal of Biomedical Science, 2007. 64(4): p. 180-189. 2. Teles, F.R., R.P. Teles, A. Sachdeo, N.G. Uzel, X.Q. Song, G. Torresyap, M. Singh, A. Papas, A.D. Haffajee, and S.S. Socransky, Comparison of Microbial Changes in Early Re-Developing Biofilms on Natural Teeth and Dentures. Journal of Periodontology, 2012: p. 1-13. 3. Wilson, J., The aetiology, diagnosis and management of denture stomatitis. Br Dent J, 1998. 185(8): p. 380-384. 4. Barrett, D., Interventions for cleaning dentures in adults. International Journal of Evidence-Based Healthcare, 2010. 8(4): p. 286-287. 5. Padilha, D.M.P., F.N. Hugo, J.B. Hilgert, and R.G. Dal Moro, Hand Function and Oral Hygiene in Older Institutionalized Brazilians. Journal of the American Geriatrics Society, 2007. 55(9): p. 1333-1338. 6. Sumi, Y., K. Nakajima, T. Tamura, M. Nagaya, and Y. Michiwaki, Developing an instrument to support oral care in the elderly. Gerodontology, 2003. 20(1): p. 3-8. 7. Neill, D., A study of Materials and methods Employed in cleaning dentures. British Dental Journal, 1968. 124(3): p. 107-115. 8. Ellepola, A.N.B. and L.P. Samaranayake, Adhesion of oral Candida albicans isolates to denture acrylic following limited exposure to antifungal agents. Archives of Oral Biology, 1998. 43(12): p. 999-1007. 9. Rohrer, M. and R. Bulard, Microwave sterilization. Journal of American Dental Association, 1985. 110(2): p. 194-198. 10. Nikawa, H., T. Hamada, H. Yamashiro, and H. Kumagai, A Review of in Vitro and in Vivo Methods to Evaluate the Efficacy of Denture Cleansers. International journal of Prosthodontics, 1999. 12(2): p. 153-159. 11. Abelson, D.C., Denture plaque and denture cleansers. The Journal of Prosthetic Dentistry, 1981. 45(4): p. 376-379. 12. Morgan, T.D. and M. Wilson, Anti-adhesive and antibacterial properties of a proprietary denture cleanser. Journal of Applied Microbiology, 2000. 89(4): p. 617-623. 161 13. Budtz-Jørgensen, E., Materials and methods for cleaning dentures. The Journal of Prosthetic Dentistry, 1979. 42(6): p. 619-623. 14. Wiskott, H.W., J.I. Nicholls, and U.C. Belser, Stress fatigue: basic principles and prosthodontic implications. The International Journal of Prosthodontics, 1995. 8(2): p. 105-116. 15. Harrison, Z., A. Johnson, and C.W.I. Douglas, An in vitro study into the effect of a limited range of denture cleansers on surface roughness and removal of Candida albicans from conventional heat-cured acrylic denture base material. Journal of Oral Rehabilitation, 2004. 31: p. 460-467. 16. Nikawa H, H.T., Yamashiro H, Kumagai H. , A review of in vitro and in vivo methods to evaluate the efficacy of denture cleansers. The International Journal of Prosthodontics, 1999. 12(2): p. 153–9. 17. Felton, D., L. Cooper, I. Duqum, G. Minsley, A. Guckes, S. Haug, P. Meredith, C. Solie, D. Avery, and N. Deal Chandler, Evidence-Based Guidelines for the Care and Maintenance of Complete Dentures: A Publication of the American College of Prosthodontists. Journal of Prosthodontics, 2011. 20(SUPPL. 1): p. S1-S12. 18. de Souza Raphael, F., H. de Freitas Oliveira Paranhos, H. Lovato da Silva Claudia, L. Abu-Naba'a, Z. Fedorowicz, and A. Gurgan Cem Interventions for cleaning dentures in adults. Cochrane Database of Systematic Reviews, 2009. DOI: 10.1002/14651858.CD007395.pub2. 19. Paranhos, H.F.O., C.H. Silva-Lovato, R.F. Souza, P.C. Cruz, K.M. Freitas, and A. Peracini, Effects of mechanical and chemical methods on denture biofilm accumulation. Journal of Oral Rehabilitation, 2007. 34(8): p. 606-612. 20. Shay, K., Denture hygiene: A review and update. Journal of Contemporary Dental Practice, 2000. 1(2): p. 15-22. 21. Jose, A., B.J. Coco, S. Milligan, B. Young, D.F. Lappin, J. Bagg, C. Murray, and G. Ramage, Reducing the Incidence of Denture Stomatitis: Are Denture Cleansers Sufficient? Journal of Prosthodontics, 2010. 19(4): p. 252-257. 22. McCourtie, J., T.W. MacFarlane, and L.P. Samaranayake, A comparison of the effects of chlorhexidine gluconate, amphotericin B and nystatin on the adherence of Candida species to denture acrylic. Journal of Antimicrobial Chemotherapy, 1986. 17(5): p. 575-583. 162 23. Radford, D.R., S. Challacombe, and J.D. Walter, Denture Plaque and Adherence of Candida Albicans To Denture-Base Materials in Vivo and in Vitro. Critical Reviews in Oral Biology & Medicine, 1999. 10(1): p. 99-116. 24. Blankenship, J.R. and A.P. Mitchell, How to build a biofilm: a fungal perspective. Current Opinion in Microbiology, 2006. 9(6): p. 588-594. 25. Oliveira Paranhos, H.F., C.H. Silva-Lovato, R.F. De Souza, P.C. Cruz, K.M. De Freitas-Pontes, E. Watanabe, and I.Y. Ito, Effect of Three Methods for Cleaning Dentures on Biofilms Formed In Vitro on Acrylic Resin. Journal of Prosthodontics, 2009. 18(5): p. 427-431. 26. Barnes, W.G., A. Flesher, A.E. Berger, and J.D. Arnold, Scanning Electron Microscopic Studies of Candida albicans. Journal of Bacteriology, 1971. 106(1): p. 276-280. 27. Raab, F.J., C.A. Taylor, J.A. Bucher, and B.L. Mann, Scanning electron microscopic examination of ultrasonic and effervescent methods of surface contaminant removal from complete dentures. The Journal of Prosthetic Dentistry, 1991. 65(2): p. 255-258. 28. Gwinnett, A.J. and L. Caputo, The effectiveness of ultrasonic denture cleaning: A scanning electron microscope study. The Journal of Prosthetic Dentistry, 1983. 50(1): p. 20-25. 29. Chandra, J., P.K. Mukherjee, and M.A. Ghannoum, In vitro growth and analysis of Candida biofilms. Nat. Protocols, 2008. 3(12): p. 1909-1924. 30. Kim, K., Y. Kim, I. Han, M. Kim, M. Jung, and H. Park, Quantitative and qualitative analyses of the cell death process in Candida. PLoS One, 2011. 6(12): p. 1932-6203 (Electronic). 31. Yau, W.F.E., Y.Y. Cheng, R.K.F. Clark, and T.W. Chow, Pressure and temperature changes in heat-cured acrylic resin during processing. Dental Materials, 2002. 18(8): p. 622-629. 32. Seneviratne, C.J., L.J. Jin, Y.H. Samaranayake, and L.P. Samaranayake, Cell Density and Cell Aging as Factors Modulating Antifungal Resistance of Candida albicans Biofilms. Antimicrobial Agents and Chemotherapy, 2008. 52(9): p. 3259-3266. 33. Richmond, R., T.V. Macfarlane, and J.F. McCord, An evaluation of the surface changes in PMMA biomaterial formulations as a result of toothbrush/dentifrice abrasion. Dental Materials, 2004. 20(2): p. 124-132. 163 34. van der Weijden, G.A., M.F. Timmerman, E. Reijerse, C.M. Snoek, and U. van der Velden, Toothbrushing force in relation to plaque removal. Journal of Clinical Periodontology, 1996. 23(8): p. 724-729. 35. Panzeri, H., E.H.G. Lara, H. De Freitas Oliveira Paranhos, C.H. Lovato Da Silva, R.F. De Souza, M.C.M. De Souza Gugelmin, C. Tirapelli, P.C. Cruz, and I.M. De Andrade, In vitro and clinical evaluation of specific dentifrices for complete denture hygiene. Gerodontology, 2009. 26(1): p. 26-33. 36. Lira, A.F., R.L.X. Consani, M.F. Mesquita, M.A.A. Nóbilo, and G.E.P. Henriques, Effect of toothbrushing, chemical disinfection and thermocycling procedures on the surface microroughness of denture base acrylic resins. Gerodontology, 2012. 29(2): p. e891-e897. 37. Machado, A.L., E.T. Giampaolo, C.E. Vergani, A.C. Pavarina, D. da Silva Lopes Salles, and J.H. Jorge, Weight loss and changes in surface roughness of denture base and reline materials after simulated toothbrushing in vitro. Gerodontology, 2012. 29(2): p. e121-e127. 38. Kuhar, M. and N. Funduk, Effects of polishing techniques on the surface roughness of acrylic denture base resins. The Journal of Prosthetic Dentistry, 2005. 93(1): p. 76-85. 39. Haselden, Hobkirk, Pearson, and Davies, A comparison between the wear resistance of three typesof denture resin to three different dentifrices. Journal of Oral Rehabilitation, 1998. 25(5): p. 335-339. 40. Heath, J.R., J.C. Davenport, and P.A. Jones, The abrasion of acrylic resin by cleaning pastes. Journal of Oral Rehabilitation, 1983. 10(2): p. 159-175. 41. Associasion, A.D., ANSI/ADA Standard No. 12—Denture Base Polymers: 2002 (Reaffirmed 2008), in Denture base polymers2008. 42. von Fraunhofer, J.A. and C. Suchatlampong, The surface characteristics of denture base polymers. Journal of Dentistry, 1975. 3(3): p. 105-109. 43. Braden, M., The absorption of water by acrylic resins and other materials. The Journal of Prosthetic Dentistry, 1964. 14(2): p. 307-316. 44. Chow, T.W., Y.Y. Cheng, and N.H. Ladizesky, Polyethylene fibre reinforced poly(methylmethacrylate)—water sorption and dimensional changes during immersion. Journal of Dentistry, 1993. 21(6): p. 367-372. 164 45. Neppelenbroek, K.H., A.C. Pavarina, C.E. Vergani, and E.T. Giampaolo, Hardness of heat-polymerized acrylic resins after disinfection and long-term water immersion. The Journal of Prosthetic Dentistry, 2005. 93(2): p. 171-176. 46. Hollingworth, H.L., The Central Tendency of Judgment. The Journal of Philosophy, Psychology and Scientific Methods, 1910. 7(17): p. 461-469. 47. Brenner, E. and W.J.M. van Damme, Perceived distance, shape and size. Vision Research, 1999. 39(5): p. 975-986. 48. Morgan, T.D. and M. Wilson, The effects of surface roughness and type of denture acrylic on biofilm formation by Streptococcus oralis in a constant depth film fermentor. Journal of Applied Microbiology, 2001. 91(1): p. 47-53. 49. Quirynen, M. and C.M.L. Bollen, The influence of surface roughness and surface-free energy on supra- and subgingival plaque formation in man. Journal of Clinical Periodontology, 1995. 22(1): p. 1-14. 50. Morris, I.J., W.G. Wade, M.J. Aldred, and D.M. Walker, The early bacterial colonization of acrylic palates in man. Journal of Oral Rehabilitation, 1987. 14(1): p. 13-21. 51. Schimmel, M., P. Schoeni, G.B. Zulian, and F. Müller, Utilisation of dental services in a university hospital palliative and long-term care unit in Geneva. Gerodontology, 2008. 25(2): p. 107-112. 165