Section VIII - Quality Assurance - Providers
advertisement

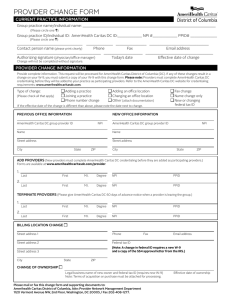
QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT Section VIII Quality Assurance, Performance Improvement, Credentialing, and Utilization Management Quality Management, Credentialing and Utilization Management | 166 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT Quality Assurance and Performance Improvement Quality Assurance and Performance Improvement (QAPI) is an integrative process that links together the knowledge, structure and processes throughout a Managed Care Organization to assess and improve quality. This process also assesses and improves the level of performance of key processes and outcomes within an organization. Opportunities to improve care and service are found primarily by examining the systems and processes by which care and services are provided. Purpose and Scope The purpose of the QAPI Program is to provide the infrastructure for the continuous monitoring, evaluation, and improvement in care and service. The QAPI Program is broad in scope and encompasses the range of clinical and service issues relevant to Members. The scope includes quality of clinical care, quality of service, and preventive health services. The QAPI Program continually monitors and reports analysis of aggregate data, intervention studies and measurement activities, programs for populations with Special Needs and surveys to fulfill the activities under its scope. The QAPI Program centralizes and uses performance monitoring information from all areas of the organization and coordinates quality improvement activities with other departments. Objectives The objectives of the QAPI program are to systematically develop, monitor and assess the following activities: o Maximize utilization of collected information about the quality of clinical care and service and to identify clinical and service improvement initiatives for targeted interventions o Ensure adequate Health Care Provider availability and accessibility to effectively serve the membership o Maintain credentialing/recredentialing processes to assure that AmeriHealth Caritas PA’s network is comprised only of qualified Health Care Providers o Oversee the functions of delegated activities o Continue to enhance physician profiling process and optimize enhanced systems to communicate performance to participating practitioners o Coordinate services between various levels of care, Network Providers, and community resources to assure continuity of care o Optimize Utilization Management to assure that care rendered is based on established clinical criteria, clinical practice guidelines, and complies with regulatory and accrediting agency standards o To ensure that Member benefits and services are not underutilized and that assessment and appropriate interventions are taken to identify inappropriate over utilization o Utilize Member and Network Provider satisfaction when implementing quality activities o Implement and evaluate Disease Management programs to effectively address chronic illnesses affecting the membership o Maintain compliance with evolving National Committee for Quality Assurance (NCQA)and URAC accreditation standards Quality Management, Credentialing and Utilization Management | 167 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT o Communicate results of our clinical and service measures to practitioners, Network Providers, and Members o Identify, enhance and develop activities that promote Member safety o Document and report all monitoring activities to appropriate committees • An annual QI work plan is derived from the QI Program goals and objectives. The work plan provides a roadmap for achievement of program goals and objectives, and is also used by the QM Department as well as the various quality committees as a method of tracking progress toward achievement of goals and objectives • QI Program effectiveness is evaluated on an annual basis. This assessment allows AmeriHealth Caritas PA to determine how well it has deployed its resources in the recent past to improve the quality of care and service provided to AmeriHealth Caritas PA membership. When the program has not met its goals, barriers to improvement are identified and appropriate changes are incorporated into the subsequent annual QI work plan. Feedback and recommendations from various committees are incorporated into the evaluation Quality Assurance and Performance Improvement Program Authority and Structure AmeriHealth Caritas PA's Quality Assurance and Performance Improvement Committee (QAPIC) provides leadership in AmeriHealth Caritas PA's efforts to measure, manage and improve quality of care and services delivered to Members and to evaluate the effectiveness of AmeriHealth Caritas PA's QAPI Program through measurable indicators. All other qualityrelated committees report to the QAPIC. Other quality-related committees include the following: Credentialing Committee The Credentialing Committee is a peer review committee whose purpose is to review Provider's credentialing/recredentialing application information in order to render a decision regarding qualification for membership to AmeriHealth Caritas PA's Network. Health Education Advisory Committee The Health Education Advisory Committee is responsible for advising on the health education needs of AmeriHealth Caritas PA, specifically as they relate to public health priorities and population-based initiatives. The Health Education & Outreach Advisory Committee is also responsible for ensuring coordination of health education activities with DPW for the benefit of the entire HealthChoices population or populations with Special Needs. Quality Management, Credentialing and Utilization Management | 168 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT Pharmacy and Therapeutics (P&T) Subcommittee The P&T Subcommittee is responsible for evaluating the clinical efficacy, safety, and costeffectiveness of medications in the treatment of disease states through product evaluation and drug Formulary recommendations. The Subcommittee also uses drug prescription patterns to develop Network Provider educational programs. Quality Assurance and Performance Improvement I Committee (QAPIC) The Quality Assurance and Performance Improvement Committee (QAPIC) coordinates the AmeriHealth Caritas PA’s efforts to measure, manage and improve quality of care and services delivered to AmeriHealth Caritas PA Members and evaluate the effectiveness of the QAPI Program. It is responsible for directing the activities of all clinical care delivered to Members. Quality of Service Committee (QSC) The QSC is responsible for measuring and improving services rendered to Members and Network Providers in the Member Services, Claims, Provider Services, and Provider Contracting Management Departments. Recipient Restriction Subcommittee The Recipient Restriction Subcommittee is responsible for identifying, evaluating, monitoring, and tracking potential misutilization, Fraud and abuse by Members. Operational Compliance Committee The purpose of the Operational Compliance Committee (OCC) is to assist the Chief Compliance Officer and the Privacy Officer with the implementation and maintenance of the Corporate Compliance and Privacy Programs. Southwest and Lehigh/Capital Behavioral Health/Physical Health MCO Pharmacy & Therapeutics Committee The Southwest and Lehigh/Capital Behavioral Health/Physical Health MCO Pharmacy & Therapeutics Committee reviews behavioral health medication policies and concerns and provides input to the Pharmacy and Therapeutics Subcommittee. The SW BH MCO P&T committee acts as a consultant to the Pharmacy and Therapeutics Subcommittee and meets quarterly. Confidentiality Documents related to the investigation and resolution of specific occurrences involving complaints or quality of care issues are maintained in a confidential and secure manner. Specifically, Members' and Health Care Providers' right to confidentiality are maintained in accordance with applicable laws. Records of quality improvement and associated committee meetings are maintained in a confidential and secure manner. Credentialing/Recredentialing Requirements Quality Management, Credentialing and Utilization Management | 169 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT Provider Requirements (Other than Facilities) AmeriHealth Caritas PA maintains and adheres to all applicable State and federal laws and regulations, DPW requirements, and accreditation requirements governing credentialing and recredentialing functions. The following types of practitioners require initial credentialing and recredentialing(every 36 months): Audiologists Certified Nurse Midwife Chiropractors Physical Therapists* Language Pathologists* CRNPs Dentists Oral Surgeons Occupational Therapists* Registered Dieticians Physicians (DO's and MD's) Podiatrists Therapeutic Optometrists Speech Therapists* *Only private practice occupational, physical and speech therapists require credentialing. The following criteria must be met as applicable, in order to evaluate a qualified Health Care Provider: • A current unrestricted state license, not subject to probation, proctoring requirements or disciplinary action to specialty. A copy of the license must be submitted along with the application • A valid DEA or CDS certificate, if applicable • Education and training that supports the requested specialty or service, as well as the degree credential of the Health Care Provider • Foreign trained Health Care Providers must submit an Education Commission for Foreign Medical Graduates (ECFMG) certificate or number with the application • Board certification is required for all Health Care Providers who apply as a specialist. AmeriHealth Caritas PA requires that all specialists be board-certified or meet one (1) of the following exceptions: o Documented plan to take board exam o An associate within the group practice that the Health Care Provider is joining is board-certified in the requested specialty o Demonstrated network need as determined by AmeriHealth Caritas PA • The following board organizations are recognized by AmeriHealth Caritas PA for purposes of verifying specialty board certification: o American Board of Medical Specialties - ABMS o American Osteopathic Association - AOA o American Board of Podiatric Surgeons - ABPS o American Board of Podiatric Orthopedics and Primary Podiatric Medicine (ABPOPPM) o Royal College of Physicians and Surgeons • Work history containing current employment, as well as explanation of any gaps within the last (5) years • History of professional liability claims resulting in settlements or judgments paid by or on behalf of the Health Care Provider • A current copy of the professional liability insurance face sheet (evidencing coverage) Quality Management, Credentialing and Utilization Management | 170 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT • • Health Care Providers who require hospital privileges as part of their practice must have a hospital affiliation with an institution participating with AmeriHealth Caritas PA. PCPs must have the ability to admit as part of their hospital privileges. As an alternative, those Health Care Providers who do not have hospital privileges, but require them, may enter into a collaboration agreement with a Network provider(s) who is able to admit. CRNP's and CNM's must have agreements with the covering physician Adherence to the Principles of Ethics of the American Medicare Association, The American Osteopathic Association or other appropriate professional organization Provider Application (other than Facilities) AmeriHealth Caritas PA Health Plan offers practitioners the Universal Provider Datasource through an agreement with The Council for Affordable Quality Healthcare (CAQH) that simplifies and streamlines the data collection process for credentialing and recredentialing. Through CAQH, credentialing information is provided to a single repository, via a secure internet site, to fulfill the credentialing requirements of all health plans that participate with CAQH. There is no charge to providers to participate in CAQH or to submit applications. AmeriHealth Caritas PA encourages all providers to utilize this service. Submit your application to participate with AmeriHealth Caritas PA via CAQH (www.caqh.org): • Register for CAQH • Grant authorization for AmeriHealth Caritas PA to view your information in the CAQH database • Send your CAQH ID number to AmeriHealth Caritas PA (credentialing@amerihealth caritaspa.com) • Submit the following documents to AmeriHealth Caritas PA via secure e-mail (credentialing@amerihealthcaritaspa.com) with electronic signature or by fax to 215-8635627: o Credentialing Warranty Attestation o W-9 AmeriHealth Caritas PA Paper Process • Complete a Pennsylvania Standard Application that includes signature and current date • Sign and date the attestation form as certification of the accuracy and completeness of the application information • Sign and date a release of information form that grants permission to contact outside agencies to verify or supply information submitted on the applications • Submit all License, DEA, Board Certification, Education and Training, Hospital Affiliation and other required information with the application, which will be verified directly through the issuing agency prior to the credentialing/recredentialing decision • Submit a PROMISe™/Medicaid number issued by DPW. As part of the application process, AmeriHealth Caritas PA will: Quality Management, Credentialing and Utilization Management | 171 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT • • • • • Conduct a site visit and medical record keeping review upon initial credentialing for all PCP, and OB/GYNs. Scores for these reviews must be 85% or greater. Request information on Health Care Provider sanctions prior to making a credentialing or recredentialing decision. Information from the National Provider Data Bank (NPDB), Health Integrity and Provider Data Bank (HIPDB), Federation of State Medical Board (FSMB), Medicheck (Medicaid exclusions), and HHS Office of Inspector General (Medicare exclusions), Federation of Chiropractic Licensing Boards (CIN-BAD), Excluded Parties List System (EPLS) and Pennsylvania State Disciplinary Action report will be reviewed as applicable Performance review of complaints, quality of care issues and utilization issues will be included in practitioner recredentialing Maintain confidentiality of the information received for the purpose of credentialing and recredentialing Safeguard all credentialing and recredentialing documents, by storing them in a secure location, only accessed by authorized plan employees After the submission of the application, Health Care Practitioners: • Have the right to review the credentialing information with the exception of references, recommendations, and peer protected information obtained by AmeriHealth Caritas PA. When a discrepancy is identified the Credentialing Department will notify the Health Care Provider for correction • Have the right to appeal any credentialing/recredentialing denial within 30 days of receiving written notification of the decision This information should be sent to AmeriHealth Caritas PA's Provider Contracting Department at the following address: Attn: Provider Contracting AmeriHealth Caritas PA 8040 Carlson Road, Suite 500 Harrisburg, PA 17112 Phone: 1-800-642-3510 or Fax: 1-717-651-1673 Facility Requirements Facility Providers must meet the following criteria: • AmeriHealth Caritas PA will confirm that the facility is in good standing with all state and regulatory bodies, and has been reviewed by an accredited body as applicable • If there is no accreditation status results, the State licensure or Medicare/Medicaid Survey will be accepted • Recredentialing of facilities must occur every (3) years • The following types of facilities are credentialed and recredentialed o Hospitals (acute care and acute rehabilitation) o Skilled Nursing Facilities o Nursing Homes (intermediate) Quality Management, Credentialing and Utilization Management | 172 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT • • • • o Sub- Acute Facilities o Home Health Agency o Hospice o Ambulatory Surgical Center A current copy of the facility's unrestricted license not subject to probation, suspension, or other disciplinary action limits Facility malpractice coverage and history of liability A current copy of the accreditation certificate or letter if applicable The facility must submit a PROMISe™/Medicaid number issued by DPW under which service will be rendered Facility Application Facilities must: • Complete the facility application with signature and current date from the appropriate facility officer • Attest to the accuracy and completeness of the information submitted to AmeriHealth Caritas PA AmeriHealth Caritas PA will: • Verify the facility’s status with state regulatory agencies through the State Department of Health • AmeriHealth Caritas PA will accept satisfactory CMS site visit results or satisfactory survey results from the last licensure survey in place of a site visit by AmeriHealth Caritas PA. A site visit will be conducted for facilities that do not have either of these. • Request information on facility sanctions prior to rendering a credentialing or recredentialing decision by obtaining information from the Health Integrity and Protection Data Bank (HIPDB) Medicheck (Medicaid exclusions) and HHS Office of Inspector General (Medicare exclusions) • Performance reviews may include a site visit from AmeriHealth Caritas PA, review of complaints and quality of care issues as a requirement of recredentialing • Maintain confidentiality of the information received for the purpose of credentialing and recredentialing • Safeguard all credentialing and recredentialing documents, by storing them in a secure location, only accessed by authorized plan employees After the submission of the application, Facilities: • Have the right to correct any discrepancies identified as erroneous information* • Have the right to appeal any credentialing/recredentialing denial within 30 days of receiving written notification of the decision *This information should be sent to AmeriHealth Caritas PA's Provider Contracting Department at the following address: Quality Management, Credentialing and Utilization Management | 173 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT Attn: Provider Contracting AmeriHealth Caritas PA 8040 Carlson Road, Suite 500 Harrisburg, PA 17112 Phone: 1-800-642-3510 or Fax: 1-717-651-1673 Member Access to Physician Information Members can call Member Services to request information about their Network Providers, such as where they went to medical school, where they performed their residency, and if the Network Provider is board-certified. Provider Sanctioning Policy It is the goal of AmeriHealth Caritas PA to assure Members receive quality health care services. In the event that health care services rendered to a Member by a Network Provider represent a serious deviation from, or repeated non-compliance with, AmeriHealth Caritas PA’s quality standards, and/or recognized treatment patterns of the organized medical community, the Network Provider may be subject to AmeriHealth Caritas PA’s formal sanctioning process. Prohibition on Payments to Excluded/Sanctioned Persons In addition, pursuant to section 1128A of the Social Security Act and 42 CFR 1001.1901, AmeriHealth Caritas PA may not make payment to any person or an affiliate of a person who is debarred, suspended or otherwise excluded from participating in the Medicare, Medicaid or other Federal health care programs. A Sanctioned Person is defined as any person or affiliate of a person who is (i) debarred, suspended or excluded from participation in Medicare, Medicaid, the State Children’s Health Insurance Program (SCHIP) or any other Federal health care program; (ii) convicted of a criminal offense related to the delivery of items or services under the Medicare or Medicaid program; or (iii) had any disciplinary action taken against any professional license or certification held in any state or U.S. territory, including disciplinary action, board consent order, suspension, revocation, or voluntary surrender of a license or certification. Upon request of AmeriHealth Caritas PA, a Provider will be required to furnish a written certification to AmeriHealth Caritas PA that it does not have a prohibited relationship with an individual or entity that is known or should be known to be a Sanctioned Person. Quality Management, Credentialing and Utilization Management | 174 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT A Provider is required to immediately notify AmeriHealth Caritas PA upon knowledge that any of its contractors, employees, directors, officers or owners has become a Sanctioned Person, or is under any type of investigation which may result in their becoming a Sanctioned Person. In the event that a Provider cannot provide reasonably satisfactory assurance to AmeriHealth Caritas PA that a Sanctioned Person will not receive payment from AmeriHealth Caritas PA under the Provider Agreement, AmeriHealth Caritas PA may immediately terminate the Provider Agreement. AmeriHealth Caritas PA reserves the right to recover all amounts paid by AmeriHealth Caritas PA for items or services furnished by a Sanctioned Person. All Sanctioning activity is strictly confidential. Informal Resolution of Quality of Care Concerns When an AmeriHealth Caritas PA Quality Review Committee (Quality Improvement Committee, Medical Management Committee or Credentialing Committee) determines that follow-up action is necessary in response to the care and/or services begin delivered by a Network Provider, the Committee may first attempt to address and resolve the concern informally, depending on the nature and seriousness of the concern. • The Chairperson of the reviewing Committee will send a letter of notification to the Network Provider. The letter will describe the quality concerns of the Committee, and what actions are recommended for correction of the problem. The Network Provider is afforded a specified, reasonable period of time appropriate to the nature of the problem. The letter will recommend an appropriate period of time within which the Network Provider must correct the problem The letter is to be clearly marked: Confidential: Product of Peer Review • Repeated non-conforming behavior will subject the Network Provider to a second warning letter. In addition, the Network Provider’s Member panel (if applicable) and referrals and/or admissions are frozen while the issue is investigated and monitored • Failure to conform thereafter is considered grounds for initiation of the formal sanctioning process. Formal Sanctioning Process In the event of a serious deviation from, or repeated non-compliance with, AmeriHealth Caritas PA's quality standards, and/or recognized treatment patterns of the organized medical community, the AmeriHealth Caritas PA Quality Improvement Committee or the Chief Medical Officer (CMO) may immediately initiate the formal sanctioning process o The Network Provider will receive a certified letter (return receipt requested) informing him/her of the decision to initiate the formal sanctioning process. The letter will inform the Network Provider of his/her right to a hearing before a hearing panel. Quality Management, Credentialing and Utilization Management | 175 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT o The Network Provider's current Member panel (if applicable) and referrals and/or admissions are frozen immediately during the sanctioning process. Notice of Proposed Action to Sanction The Network Provider will receive written notification by certified mail stating: • That a professional review action has been proposed to be taken • Reason(s) for proposed action • That the Network Provider has the right to request a hearing on the proposed action • That the Network Provider has 30 days within which to submit a written request for a hearing, otherwise the right to a hearing is forfeited. The Network Provider must submit the hearing request by certified mail, and must state what section(s) of the proposed action s/he wishes to contest • Summary of rights in the hearing • The Network Provider may waive his/her right to a hearing Notice of Hearing If the Network Provider requests a hearing in a timely manner, the Network Provider will be given a notice stating: • The place, date and time of the hearing, which date shall not be less than thirty (30) days after the date of the notice • That the Network Provider has the right to request postponement of the hearing, which may be granted for good cause as determined by the CMO of AmeriHealth Caritas PA and/or upon the advice of AmeriHealth Caritas PA’s Legal Department • A list of witnesses (if any) expected to testify at the hearing on behalf of AmeriHealth Caritas PA Conduct of the Hearing and Notice • • • • The hearing shall be held before a panel of individuals appointed by AmeriHealth Caritas PA Individuals on the panel will not be in direct economic competition with the Network Provider involved, nor will they have participated in the initial decision to propose Sanctions The panel will be composed of physician members of the AmeriHealth Caritas PA's Quality Committee structure, the CMO of AmeriHealth Caritas PA, and other physicians and administrative persons affiliated with AmeriHealth Caritas PA as deemed appropriate by the CMO of AmeriHealth Caritas PA. The AmeriHealth Caritas PA CMO or his/her designee serves as the hearing officer The right to the hearing will be forfeited if the Network Provider fails, without good cause, to appear Provider's Rights at the Hearing The Network Provider has the right: • To representation by an attorney or other person of the Network Provider's choice • To have a record made of the proceedings (copies of which may be obtained by the Network Provider upon payment of reasonable charges) • To call, examine, and cross-examine witnesses Quality Management, Credentialing and Utilization Management | 176 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT • • • • To present evidence determined to be relevant by the hearing officer, regardless of its admissibility in a court of law To submit a written statement at the close of the hearing To receive the written recommendation(s) of the hearing panel within 15 working days of completion of the hearing, including statement of the basis for the recommendation(s) To receive the Plan’s written decision within 60 days of the hearing, including the basis for the hearing panel’s recommendation Appeal of the Decision of the AmeriHealth Caritas PA Peer Review Committee The Network Provider may request an appeal after the final decision of the Panel • The AmeriHealth Caritas PA Quality Improvement Committee must receive the appeal by certified mail within 30 days of the Network Provider's receipt of the Committee's decision; otherwise the right to appeal is forfeited • Written appeal will be reviewed and a decision rendered by the AmeriHealth Caritas PA Quality Improvement Committee (QIC) within 45 days of receipt of the notice of the appeal Summary Actions Permitted The CEO, President of PA Managed Care, General Manager of AmeriHealth Caritas PA, and/or the CMO, can take the following summary actions without a hearing: • Suspension or restriction of clinical privileges for up to 14 days, pending an investigation to determine the need for professional review action • Immediate revocation, in whole or in part, of panel membership or Network Provider status subject to subsequent notice and hearing when failure to take such action may result in imminent danger to the health and/or safety of any individual. A hearing will be held within 30 days of this action to review the basis for continuation or termination of this action External Reporting The CMO will direct the Credentialing Department to prepare an adverse action report for submission to the National Provider Data Bank (NPDB), the Healthcare Integrity and Protection Data Bank (HIPDB), and State Board of Medical or Dental Examiners if formal Sanctions are imposed for quality of care deviations and if the Sanction is to last more than 30 days. (NOTE: NPDB reporting is applicable only if the Sanction is for quality of care concerns.) If Sanctions against the Network Provider will materially affect AmeriHealth Caritas PA's ability to make available all capitated services in a timely manner, AmeriHealth Caritas PA will notify DPW of this issue for reporting/follow-up purposes. Utilization Management Program The Utilization Management (UM) program description summarizes the structure, processes and resources used to implement AmeriHealth Caritas PA's programs, which were created in consideration of the unique needs of its Enrollees and the local delivery system. All departmental policies and procedures, guidelines and UM criteria are written consistent with DPW requirements, the National Committee for Quality Assurance (NCQA), Pennsylvania's Act 68 and accompanying regulations, and other applicable State and federal laws and regulations. Quality Management, Credentialing and Utilization Management | 177 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT Where these standards conflict, AmeriHealth Caritas PA adopts the most rigorous of the standards. Annual Review Annually, AmeriHealth Caritas PA reviews and updates it’s UM policies and procedures as applicable. These modifications, which are approved by the AmeriHealth Caritas PA Quality Medical Management Committee, are based on, among other things, changes in laws, regulations, DPW requirements, accreditation requirements, industry standards and feedback from Health Care Providers, Members and others. Mission and Values The AmeriHealth Caritas PA UM Program provides an interactive process for AmeriHealth Caritas PA Members that generally assesses whether the physical health care services they receive are Medically Necessary and delivered in a quality manner. Behavioral health services are provided through a separate arrangement between DPW and Behavioral Health Managed Care Organizations. The AmeriHealth Caritas PA UM Program promotes the continuing education of, and understanding amongst, Members, participating physicians and other healthcare professionals. UM Program techniques that are used to evaluate Medical necessity, access to care, appropriateness and efficiency of services include, but are not limited to, the following programmatic components: intake, Prior Authorization, Concurrent Review, discharge planning and alternate service review, durable medical equipment (DME) review. The UM Program also generally seeks to coordinate, when possible, emergent, urgent and elective health care services. Members are assisted by the UM Program in obtaining transitional care benefits such as transitional care for new Members/covered persons and continuity of coverage for Members/covered persons whose Health Care Providers are no longer participating with AmeriHealth Caritas PA. The UM Program also outlines the responsibility for oversight of entities to whom AmeriHealth Caritas PA delegates Utilization Management functions. Quality Management, Credentialing and Utilization Management | 178 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT Criteria Availability AmeriHealth Caritas PA has adopted clinical practice guidelines for use in guiding the treatment of Members, with the goal of reducing unnecessary variations in care. The clinical practice guidelines represent current professional standards, supported by scientific evidence and research. These guidelines are intended to inform, not replace, the physician's clinical judgment. The physician remains responsible for ultimately determining the applicable treatment for each individual. The following complete clinical guidelines are available in the Provider Center of our website, www.amerihealthcaritaspa.com: Acute Pharyngitis in Children Asthma Chlamydia Cholesterol Chronic Obstructive Pulmonary Disease Diabetes Heart Failure Hemophilia HIV Hypertension Immunization and Screenings Preventive Health Guidelines Maternity Sickle Cell AmeriHealth Caritas PA will provide its Utilization Management (UM) criteria to Network Providers upon request. To obtain a copy of the AmeriHealth Caritas PA UM criteria: • Call the UM Department at 1-800-521-6622 • Identify the specific criteria you are requesting • Provide a fax number or mailing address You will receive a faxed copy of the requested criteria within 24 hours or written copy by mail within 5 business days of your request. Please remember that AmeriHealth Caritas PA has Medical Directors and Physician Advisors who are available to address UM issues or answer your questions regarding decisions relating to Prior Authorization, DME, Home Health Care and Concurrent Review. Call the Medical Director Hotline at: 1-877-693-8271, option #4. Additionally, AmeriHealth Caritas PA would like to remind Health Care Providers of our affirmation statement regarding incentives: • UM decision-making is based only on appropriateness of care and the service being provided • AmeriHealth Caritas PA does not reward Health Care Providers or other individuals for issuing denials of coverage or service • There are no financial incentives for UM decision makers to encourage underutilization Hours of Operation The Plan provides and maintains a toll free number for Health Care Providers and Members to contact the Plan's UM staff. The toll free number is 1-800-521-6622. The Plan's UM Department Quality Management, Credentialing and Utilization Management | 179 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT is available to answer calls from Health Care Providers, practitioners and Members during normal business hours, 8:30 a.m.-5:00 p.m. Translation services are available as needed. After business hours and on weekends and holidays, Health Care Providers and Members are instructed to contact the On-Call Nurse through the AmeriHealth Caritas PA Member Services number 1-888-991-7200. After obtaining key contact and Member information, the Member Service Representative pages the on-call Nurse. The on-call Nurse contacts the Health Care Provider or Member, as needed, to acquire the information necessary to process the request. The on-call Nurse will call the on-call Physician Reviewer to review the request, if necessary. The on-call Nurse is responsible to contact the requesting Health Care Provider or Member with the outcome of their request. Timeliness of UM decisions Several external standards guide AmeriHealth Caritas PA's timeline standards. These include NCQA, DPW HealthChoices standards, and Pennsylvania's Act 68 and accompanying regulations, and other applicable state and federal laws and regulations. Where these standards conflict, AmeriHealth Caritas PA adopts the more rigorous of the standards. Table 1 identifies AmeriHealth Caritas PA’s timeliness standards. Table 1: Timeliness Of UM Decisions – Excludes Pharmacy Case Type Urgent Precertification (including Home Health Care) Non-Urgent Precertification (excluding Home Health Care) Concurrent Review Decision Initial Notification Written Confirmation* 24 hours from receipt of request** 24 hours from receipt of request 24 hours from initial notification 2 business days from receipt of the request ** 2 business days from receipt of the request 2 business days from initial notification 24 hours from receipt of the request 24 hours of the initial notification 24 hours from receipt of the request** Retrospective Review 30 calendar days from receipt of the records 30 calendar days from receipt of the records The earlier of 15 business days or 30 calendar days from the receipt of records Home Health Care Non-Urgent Pre-certification 48 hours from receipt of request** 48 hours from receipt of request 48 hours from initial notification * Written confirmation is provided for all cases where coverage for the requested service is partially or completely denied. ** The timeframes for decisions and notification may be extended if additional information is needed to process the request. In these instances, the member and requesting Health Quality Management, Credentialing and Utilization Management | 180 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT Care Provider are notified of the required information in writing (not applicable to retrospective review). Denial and Appeal Process Medical necessity denial decisions made by a Medical Director, or other physician designee, are based on the DPW definition of Medical necessity, in conjunction with the Member's benefits, applicable MA laws and regulations, the Medical Director’s medical expertise, Medical necessity criteria, as referenced above, and/or published peer-review literature. At the discretion of the Medical Director, in accordance with applicable laws, regulations or other regulatory and accreditation requirements, input to the decision may be obtained from board-certified physicians from an appropriate specialty. The Medical Director or physician designee makes the final decision. AmeriHealth Caritas PA will not retroactively deny reimbursement for a covered service provided to an eligible Member by a Health Care Provider who relied on written or oral authorization from AmeriHealth Caritas PA or an agent of AmeriHealth Caritas PA, unless there was material misrepresentation or Fraud in obtaining the authorization. Upon request of a Member or Network Provider, the criteria used for making Medically Necessary decisions is provided, in writing, by the Medical Director or physician designee. Physician Reviewer Availability to Discuss Decision If a practitioner wishes to discuss a medical necessity decision, AmeriHealth Caritas PA's physician reviewers are available to discuss the decision with the Practitioner. A call to discuss the determination is accepted from the Practitioner: • At any time while the Member is an inpatient • Up to 2 business days after the Member’s discharge date, whichever is later • Up to 2 business days after a determination for a Prior Authorization (Pre-Service) request has been rendered • Up to 2 business days after a determination of a Retrospective Review has been rendered, whichever is later. A dedicated reconsideration line with a toll-free number has been established for practitioners to call at 1-877-693-8271 option 4. A physician reviewer is available at any time during the business day to interface with practitioners. If a practitioner is not satisfied with the outcome of the discussion with the physician reviewer, then the practitioner may file a Formal Provider Appeal. For information on the types of issues that may be the subject of a Formal Provider Appeal, please see Section VII. Denial Reasons All denial letters include specific reasons for the denial, the rationale for the denial and a summary of the UM criteria. In addition, if a different level of care is approved, the clinical rationale is also provided. These letters incorporate a combination of NCQA standards, DPW requirements and Department of Health requirements. Denial letters are available in six languages for Members with Limited English Proficiency. Letters are translated into other languages upon request. This service is available through the cooperation of Member Services and Utilization Management. Quality Management, Credentialing and Utilization Management | 181 QUALITY MANAGEMENT, CREDENTIALING AND UTILIZATION MANAGEMENT Appeal Process All denial letters include an explanation of the Member's rights to appeal and the processes for filing appeals through the AmeriHealth Caritas PA Complaint and Grievance Process and the DPW Fair Hearing Process. Members contact the Member Service Unit to file Complaint and Grievance appeals where a Member advocate is available to assist Members as needed. Evaluation of New Technology When AmeriHealth Caritas PA receives a request for new or emerging technology, it compiles clinical information related to the request and reviews available evidence-based research and/or DPW technology assessment group guidelines. AmeriHealth Caritas PA Medical Directors make the final determination on coverage. Evaluation of Member & Provider Satisfaction and Program Effectiveness Not less than every two years, the UM department completes an analysis of Member and Network Provider satisfaction with the UM program. At a minimum, the sources of data used in the evaluation include the annual Member satisfaction survey, Member Complaints, Grievances and Fair Hearings, Network Provider surveys and complaints. To support its objective to create partnerships with physicians, AmeriHealth Caritas PA actively seeks information about Network Provider satisfaction with its programs on an ongoing basis. In addition to monitoring Health Care Provider complaints, AmeriHealth Caritas PA holds meetings with Network Providers to understand ways to improve the program. Monthly, the department reports telephone answering response, abandonment rates and decision time frames. Quality Management, Credentialing and Utilization Management | 182