Pain 104 (2003) 509–517
www.elsevier.com/locate/pain
Sensory hypersensitivity occurs soon after whiplash injury and is
associated with poor recovery
Michele Sterlinga,*, Gwendolen Julla, Bill Vicenzinoa, Justin Kenardyb
a
The Whiplash Research Unit, Department of Physiotherapy, The University of Queensland, Brisbane 4072, Australia
b
Department of Psychology, The University of Queensland, Brisbane 4072, Australia
Received 25 November 2002; received in revised form 11 February 2003; accepted 19 February 2003
Abstract
Hypersensitivity to a variety of sensory stimuli is a feature of persistent whiplash associated disorders (WAD). However, little is known
about sensory disturbances from the time of injury until transition to either recovery or symptom persistence. Quantitative sensory testing
(pressure and thermal pain thresholds, the brachial plexus provocation test), the sympathetic vasoconstrictor reflex and psychological distress
(GHQ-28) were prospectively measured in 76 whiplash subjects within 1 month of injury and then 2, 3 and 6 months post-injury. Subjects
were classified at 6 months post-injury using scores on the Neck Disability Index: recovered (, 8), mild pain and disability (10– 28) or
moderate/severe pain and disability (.30). Sensory and sympathetic nervous system tests were also measured in 20 control subjects. All
whiplash groups demonstrated local mechanical hyperalgesia in the cervical spine at 1 month post-injury. This hyperalgesia persisted in
those with moderate/severe symptoms at 6 months but resolved by 2 months in those who had recovered or reported persistent mild
symptoms. Only those with persistent moderate/severe symptoms at 6 months demonstrated generalised hypersensitivity to all sensory tests.
These changes occurred within 1 month of injury and remained unchanged throughout the study period. Whilst no significant group
differences were evident for the sympathetic vasoconstrictor response, the moderate/severe group showed a tendency for diminished
sympathetic reactivity. GHQ-28 scores of the moderate/severe group were higher than those of the other two groups. The differences in
GHQ-28 did not impact on any of the sensory measures. These findings suggest that those with persistent moderate/severe symptoms at
6 months display, soon after injury, generalised hypersensitivity suggestive of changes in central pain processing mechanisms. This
phenomenon did not occur in those who recover or those with persistent mild symptoms.
q 2003 International Association for the Study of Pain. Published by Elsevier Science B.V. All rights reserved.
Keywords: Whiplash; Quantitative sensory testing; Hypersensitivity
1. Introduction
Chronic whiplash associated disorders (WAD) have been
shown to be associated with sensory and motor hypersensitivity that likely reflects underlying changes in neurobiological processing of pain mechanisms. Sensory changes
include hypersensitivity to a variety of stimuli including
mechanical and electrocutaneous stimulation and induced
muscle pain (Koelbaek-Johansen et al., 1999; Curatolo et al.,
2001; Moog et al., 2002; Sterling et al., 2002a). In addition,
there is evidence of increased sensitivity of the flexor withdrawal response in patients with chronic WAD (Curatolo
et al., 2002). This is supported to some extent by findings of
* Corresponding author. Tel.: þ 61-7-3365-4568; fax: þ61-7-3365-2775.
E-mail address: m.sterling@shrs.uq.edu.au (M. Sterling).
hypersensitive motor responses to a clinical test of flexor
withdrawal (Sterling et al., 2002b).
In contrast to the expanding knowledge of mechanisms
involved in chronic WAD, the acute phase of injury and the
processes involved in the transition to either recovery or
symptom persistence have been largely unexplored. A
greater knowledge of these phases of the condition may help
with early identification and management of those at risk of
developing persistent pain – estimated at up to 40% of those
experiencing whiplash injury (Barnsley et al., 1994). Kasch
et al. (2001a,b) demonstrated mechanical hyperalgesia
locally within the cervical spine of acutely injured WAD
subjects but failed to identify any such effects at remote
uninjured sites (as occurs in subjects with chronic WAD).
However, these authors did not explore the possibility that
such changes may occur only in some patients, a likely
0304-3959/03/$20.00 q 2003 International Association for the Study of Pain. Published by Elsevier Science B.V. All rights reserved.
doi:10.1016/S0304-3959(03)00078-2
510
M. Sterling et al. / Pain 104 (2003) 509–517
important factor supported by Yerner et al. (2001) who
showed that altered sensory responses in cutaneous areas
supplied by the trigeminal nerve occurred only in a subgroup of WAD patients. Furthermore, higher levels of pain
and disability in acute WAD have been accepted as a sign
of poor outcome (Cote et al., 2001; Radanov et al., 1995),
suggesting the importance of differentiation between those
with higher pain and disability levels from those with lesser
symptoms.
Involvement of sympathetic nervous system (SNS)
activity as contributing to symptoms of WAD is yet to be
pursued, although suggestions to its presence have been
made (Adeboye et al., 2000; Munglani, 2000). Using the
sympathetic vasoconstrictor reflex (SVR), changes in SNS
activity have been shown to occur in chronic musculoskeletal pain syndromes such as frozen shoulder and lateral
epicondylalgia (Mani et al., 1989; Smith et al., 1994) and
complex regional pain syndrome type 1 (Schurmann et al.,
1999). As some symptoms of WAD such as vasomotor
disturbances, burning pain and cold intolerance mimic those
of complex regional pain syndrome, investigation of SNS
activity may provide further information of the underlying
processes of this condition.
Those with chronic WAD show evidence of psychological distress (Peebles et al., 2001; Radanov et al., 1995),
which is probably not surprising in view of persisting
symptoms. Psychological factors such as anxiety and fear
have been shown to affect measures of both pain threshold
and pain tolerance (Rhudy and Meagher, 2000). For this
reason, it is important that psychological factors are taken
into account when measuring pain responses.
Our study addressed the lack of information of changes
in sensory and SNS function soon after injury and the time
course of such changes to 6 months post-injury (a time
frame after which symptoms change little; Mayou and
Radanov, 1996). The aims of the study were threefold: to
investigate the differences in sensory and SNS function
between those who recover and those who report persistent
symptoms based on their status at 6 months; to investigate
the prospective longitudinal development of such changes
following whiplash injury and to determine the effect of
psychological distress on sensory measures.
2. Methods
2.1. Study design
A prospective longitudinal design was used to study
persons who sustained a whiplash injury from within
1 month of injury to 6 months post-injury. They were
assessed on four occasions – within 1 month of injury, 2, 3
and 6 months post-injury. An asymptomatic control group
was assessed three times, each 1 month apart.
2.2. Subjects
Eighty volunteers (24 males, 56 females, mean age
36.27 ^ 12.69 years) reporting neck pain as a result of a
motor vehicle crash and 20 asymptomatic volunteers
(8 males, 12 females, mean age 40.1 ^ 13.6 years)
participated in the study. The whiplash subjects were
recruited via hospital accident and emergency departments,
primary care practices (medical and physiotherapy) and
from advertisement within radio and print media. They were
eligible if they met the Quebec Task Force Classification of
WAD II or III (Spitzer et al., 1995). Subjects were excluded
if they were WAD IV, experienced concussion, loss of
consciousness or head injury as a result of the accident and
if they reported a previous history of whiplash, neck pain
or headaches that required treatment. The asymptomatic
control group was recruited from the general community
from print media advertisement and were included provided
they had never experienced any prior pain or trauma to the
cervical spine, head or upper quadrant.
Ethical clearance for this study was granted by the
Medical Research Ethics Committee of The University of
Queensland.
2.3. Pressure pain thresholds (PPTs)
PPTs were measured using a pressure algometer with
a probe size of 1 cm2 and application rate of 40 kPa/s
(Somedic AB, Farsta, Sweden). PPTs were measured at two
bilateral cervical spine sites (over the articular pillars of
C2/3 and C5/6), at three bilateral upper limb sites (over the
three main peripheral nerve trunks) and at a bilateral remote
site (tibialis anterior). These sites have been previously used
in investigation of chronic WAD (Sterling et al., 2002b).
The subjects were requested to push a button when the
sensation changed from one of pressure alone to one of
pressure and pain (Brennum et al., 1989). Triplicate
recordings were taken at each site and the mean values
used for analysis.
2.4. Thermal (hot, cold) pain thresholds
Thermal pain thresholds were measured bilaterally over
the cervical spine using the Thermotest system (Somedic
AB, Farsta, Sweden). The thermode was placed over the
skin of the mid-cervical region and preset to 308C with the
rate of temperature change being 18C/s. To identify cold
pain thresholds (CPTs) and heat pain thresholds (HPTs),
subjects were asked to push a patient-controlled switch
when the cold or warm sensation first became painful
(Hurtig et al., 2001). Triplicate recordings were taken at
each site and the mean values used for analysis.
2.5. Brachial plexus provocation test (BPPT)
The BPPT was performed as described previously and in
M. Sterling et al. / Pain 104 (2003) 509–517
the following sequence: gentle shoulder girdle depression,
glenohumeral abduction and external rotation in the coronal
plane, wrist and finger extension and elbow extension
(Elvey, 1979; Selvaratnam et al., 1994). The range of elbow
extension was measured at the subjects’ pain threshold
using a standard goniometer aligned along the mid-humeral
shaft, medial epicondyle and ulnar styloid (Balster and Jull,
1997; Clarkson and Gilewich, 1989). If the subject did not
experience pain, the test was continued until the end of
available range. At the completion of this test, the subjects
were asked to record their pain on a 10 cm visual analogue
scale (VAS).
2.6. Sympathetic vasoconstrictor reflex
The SVR was used as an indication of SNS activity
(Mani et al., 1989; Schurmann et al., 1999). Using laser
Doppler flowmetry (floLAB Monitor, Moor Instruments,
Devon, UK), the skin blood flow in the fingertips of both
hands was measured. Data were sampled at 20 Hz. A
provocation manoeuvre (inspiratory gasp), which is known
to cause a short sympathetic reaction and cutaneous
vasoconstriction, was performed (Schurmann et al., 1999).
A program using Labview software was written which
calculated two quotients that represented the change in
blood flow following the inspiratory gasp. These were taken
after Schurmann et al. (1999) and included the SRF parameter (sympathetic reflex) that represents the relative drop
in the curve after provocation and the quotient of integrals
(QI) that also takes into account the duration of perfusion
decrease. A high QI and low SRF are indicative of an
impaired vasoconstrictor response.
2.7. Questionnaires
Self-reported pain and disability was measured in all
whiplash subjects using the Neck Disability Index (NDI)
(Vernon and Mior, 1991). They also completed the GHQ-28
(Goldberg, 1978) as an indicator of the general psychological well being. Subjects’ pain intensity was measured using
a 10 cm VAS scale.
2.8. Procedure
The following measures were undertaken at each of the
four time points. The whiplash subjects first completed the
NDI and GHQ-28 questionnaires. VAS measures of resting
pain were recorded. Testing of both whiplash and asymptomatic subjects was performed in the following sequence:
SVR, BPPT, PPTs, HPTs and CPTs. The same examiner
performed all tests. This examiner remained blind to the
subjects’ responses on the NDI and GHQ-28 questionnaires.
For all tests, no verbal cues/feedback were given to the
subjects about their performance.
After completion of the questionnaires, the subjects lay
supine and the laser Doppler blood flow sensors were
511
attached to the tips of the middle fingers using double-sided
adhesive discs. Subjects rested their hands on their abdomen
and an electric heating pad was placed over the hands in
order to obtain a uniform increase in blood flow of the
fingertips. Subjects rested in this position for 10 – 15 min.
After this time and as soon as a stable blood flow baseline
was obtained for at least 30 s, the provocation manoeuvre of
inspiratory gasp was performed. Subjects were requested to
inspire as deeply as possible and then to expire with a deep
sigh. The moment of full inspiration was marked with an
electronic footswitch. Recording of blood flow continued
for another 30 s. The SVR testing was performed in a
temperature-controlled laboratory. The temperature was set
at 208C, lights were dimmed and ambient noise was kept
low.
Further testing was completed in a standard laboratory.
The BPPT was then performed, followed by PPTs measures
in the following order: tibialis anterior, median, radial and
ulnar nerves, C5/6 and C2/3. After this, thermal pain
thresholds were measured over the cervical spine; CPTs
followed by HPTs. For BPPT, PPTs and thermal pain
thresholds, the left side was tested first followed by the right
side.
2.9. Statistical analysis
The whiplash subjects were classified into one of three
groups based on results of the NDI at 6 months post-injury.
The groups were recovered (, 8 NDI), mild pain and
disability (10 – 28 NDI) and moderate/severe pain and
disability (. 30 NDI) (Vernon, 1996). This grouping was
validated by a cluster analysis (K-means algorithm), which
showed no significant difference between the analytical
clustering and the NDI groups as proposed by Vernon
(1996).
A repeated measures mixed model analysis of variance
(ANOVA) with a between subjects factor of Group (four
levels: asymptomatic, recovered, mild, moderate/severe)
and a within subjects factor of Time (four levels: , 1 month,
2, 3 and 6 months post-injury) was performed. Age and
gender were used as covariates in this analysis. Differences
between the groups were analysed with a priori contrasts.
A repeated measures mixed model ANOVA with a timechanging covariate of GHQ-28 total scores was used to
assess the effect of psychological distress on the sensory
measures of the whiplash groups. Significance was set at
P , 0:01.
3. Results
3.1. Subject classification at 6 months post-injury
Of the 80 subjects who entered the study, four withdrew
during the study period, all after the initial assessment point.
The reasons given for withdrawal included relocation to
512
M. Sterling et al. / Pain 104 (2003) 509–517
Table 1
The age, gender and classification of subject groups at 6 months according to the NDI scores (Vernon, 1996)
Group
Number
Age (years) (mean ^ SD)
Gender (% female)
NDI classification
NDI (mean ^ SD)
Recovered group
Mild pain and disability group
Moderate/severe pain and disability group
Control group
29
30
17
20
29.3 ^ 11.72
34.3 ^ 12.5
43.7 ^ 14.5
40.1 ^ 13.6
50
77
94
60
,8
10– 28
.30
–
2.9 ^ 2.9
16.5 ^ 5.6
42.8 ^ 12.2
–
another city (two subjects), a head injury several weeks
following the whiplash injury (one subject) and no reason
given (one subject). The remaining 76 subjects formed the
6 month classification. The NDI of the recovered group was
3 ^ 2.9 (mean ^ SD), the mild group 16.5 ^ 5.6 and the
moderate/severe group 42.8 ^ 12.2. Thirty-eight percent of
the whiplash subjects reported recovery by 6 months postinjury, 39.6% reported persistent mild pain and disability
and 22.4% persistent moderate/severe pain and disability
based on NDI scores at 6 months. Age and gender distribution of the four groups is illustrated in Table 1. There was
an uneven distribution of males and females and differences
in ages between the groups approached significance
ðP ¼ 0:03Þ. As a consequence, age and gender were
included as covariates in the initial analysis. NDI scores
and VAS scores of pain intensity at each time point are
shown in Table 2.
After the accident, the onset of pain was immediate in
34% of subjects, occurred within 24 h in 46% and after 24 h
in 20%. Forty-six percent of collisions were rear impact,
22% were front on impact, 21% were combined rear and
front on collisions and 11% were side impact. Sixty-one
percent of subjects filed a compensation claim. This study
did not aim to investigate the effect of treatment. Subjects
were free to pursue any form of treatment. The types and
numbers of treatments received (including medication) were
similar between the three whiplash groups (Table 3).
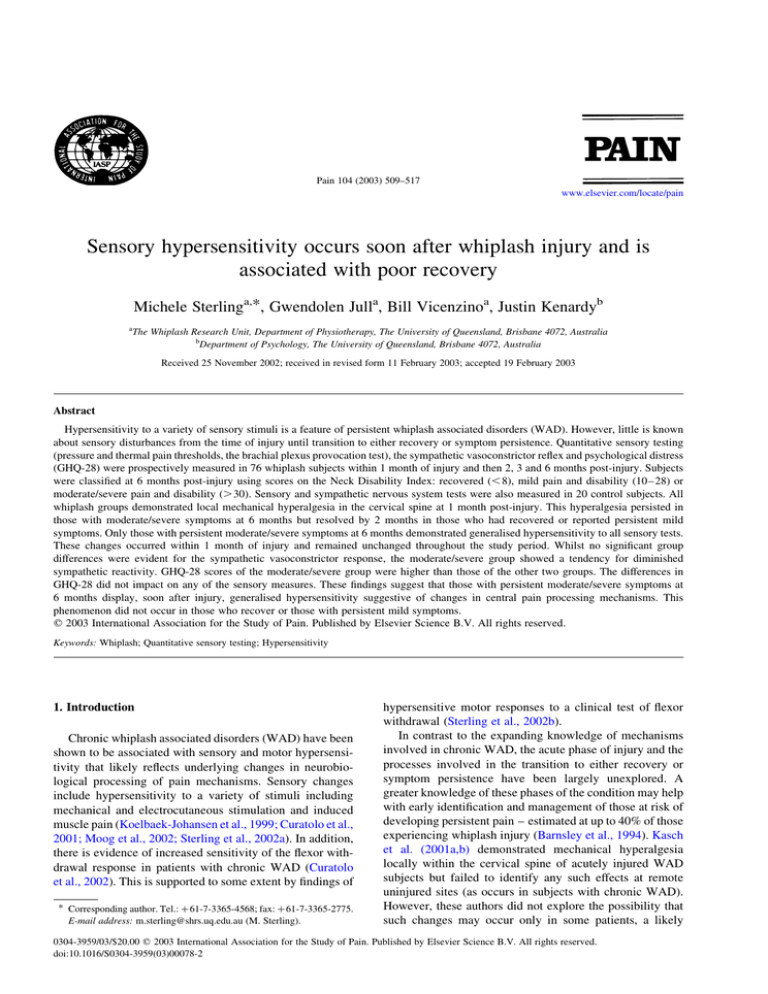
3.2. Pressure pain thresholds
The marginal means (^ SEM) of the four groups for
measures of PPT at cervical spine, median nerve and tibialis
anterior sites, are presented in Fig. 1.
There was a significant main effect for Group ðP , 0:01Þ
for all test sites. There was a significant interaction effect
between Group and Time for both cervical spine sites (C2/3,
C5/6) ðP , 0:01Þ.
The group with moderate/severe symptoms at 6 months
showed lower PPTs at all sites when compared with controls
and the other two whiplash groups ðP , 0:01Þ. PPTs of this
group did not significantly change over the study period and
remained less than all other groups at 6 months post-injury
ðP , 0:01Þ. The recovered and mild pain groups showed
lower PPTs at both cervical spine sites (C2/3, C5/6)
than control subjects ðP , 0:01Þ at entry into the study
(, 1 month). However, both these groups improved over
time ðP , 0:01Þ and by 2 months post-injury were no longer
different from control subjects. There was no effect of age
on PPTs ðP . 0:2Þ but there was an effect of gender at all
sites ðP , 0:01Þ with females having lower PPTs than
males.
3.3. Thermal pain thresholds
There was a significant group difference for both heat
and CPTs ðP , 0:01Þ but there was no interaction effect
between Group and Time for either measure of thermal pain
threshold ðP . 0:09Þ indicating that thermal pain thresholds
remained stable in all groups over the study period (Fig. 2).
HPT of the moderate/severe group was 39.5 ^ 0.48, which
was significantly lower than that of the control group
(43.2 ^ 0.48), the recovered whiplash group (42.6 ^ 0.38)
and those with mild symptoms (43.1 ^ 0.38) (all P , 0:01).
CPT of the moderate/severe group was 19.19 ^ 1.58, which
was significantly higher than that of the control group
(9.66 ^ 1.48), the recovered whiplash group (11.57 ^ 1.18)
Table 2
Mean (SD) NDI and VAS scores for each whiplash group (recovered, mild pain and disability and moderate pain and disability) at each time point
NDI
Recovered
Mild pain and disability
Moderate/severe pain and disability
VAS
Recovered
Mild pain and disability
Moderate/severe pain and disability
,1 month
2 months
3 months
6 months
19.14 (12.7)
36.1 (19.4)
55.6 (13.4)
8 (8.2)
25.6 (10.8)
49.1 (15.1)
5.4 (6.8)
21.45 (12.6)
47.4 (15.4)
2.9 (2.9)
16.3 (5.6)
42.8 (12.2)
2.3 (0.9)
3.2 (1.2)
3.2 (1.3)
1.5 (0.8)
2.6 (0.9)
3.8 (1.3)
0.6 (0.1)
0.9 (0.2)
1.3 (0.3)
0.3 (0.1)
2.0 (0.7)
3.4 (1.0)
M. Sterling et al. / Pain 104 (2003) 509–517
513
Table 3
The numbers and types of treatment and medication received by the three whiplash groups
Group
N (%) who
received
treatment
No. of
treatments
(average/study
period)
Treatment type N (%)
Recovered (n ¼ 29)
14 (48.3%)
10.6
Physiotherapy 29 (100%)
7 (24%)
Mild symptoms (n ¼ 30)
19 (63%)
14.4
Physiotherapy 14 (46.7%),
chiropractic 4 (13.3%),
acupuncture 1 (3.3%)
13 (43.3%)
18.4
Physiotherapy 8 (47.1%),
chiropractic 1 (5.8%)
12 (70.5%)
Moderate/severe symptoms (n ¼ 17)
9 (52.9%)
and the group with mild symptoms (11.39 ^ 1.18). There
was no effect of age on either measure ðP . 0:13Þ but a
significant effect of gender on both measures ðP , 0:001Þ
with females having lower CPTs and lower HPTs than
males.
3.4. Brachial plexus test
There was a significant Group effect for both elbow
N (%) on
medication
Medication type
Simple analgesics (3),
NSAIDS (4), codeine (1),
anti-depressants (0),
steroids (1), opioids (0)
Simple analgesics (2),
NSAIDS (10), codeine (2),
Anti-depressants (1),
steroids (0), opioids (1)
Simple analgesics (2),
NSAIDS (7), codeine (2),
anti-depressants (2),
steroids (0), opioids (1)
extension and pain scores with the BPPT ðP , 0:01Þ and a
significant interaction effect between Group and Time
for both measures ðP , 0:01Þ. Both the groups with
moderate/severe and mild symptoms at 6 months postinjury showed less range of elbow extension
(2 34.27 ^ 3.48, 2 33.97 ^ 2.6, respectively), and higher
VAS scores (4.1 ^ 0.5, 3.2 ^ 0.5) at entry into the study
(, 1 month) than both the control group (2 20.67 ^ 3.128,
1.8 ^ 0.4) and the whiplash group who recovered at
Fig. 1. PPTs at cervical spine, median nerve and tibialis anterior sites (means and SEM) for all groups (control, recovered, mild pain and moderate/severe pain)
over time (1, 2, 3 and 6 months post-injury).
514
M. Sterling et al. / Pain 104 (2003) 509–517
Fig. 2. HPTs and CPTs (means and SEM) for all groups (control, recovered, mild pain and moderate/severe pain) over time (1, 2, 3 and 6 months post-injury).
6 months (2 23.95 ^ 2.48, 1.8 ^ 0.4) ðP , 0:01Þ (Fig. 3).
The group with mild symptoms improved over time ðP ¼
0:004Þ and were no different from controls by the 2 month
assessment point. However, the group with moderate/severe
symptoms showed no change over time ðP . 0:09Þ and
continued to demonstrate less elbow extension and higher
VAS scores than controls at 6 months post-injury
ðP ¼ 0:002Þ. There was no effect of age or gender on either
measure of the BPPT ðP . 0:4Þ.
significant for all measures ðP , 0:01Þ. There was no
interaction between Group and GHQ-28 total score for any
measure, suggesting the effect of psychological distress (as
measured by the GHQ-28) is similar irrespective of group
allocation. The effect size for GHQ-28 (total) on the
measures of sensory function and SNS activity was small
(h2 ranged from 0.027 to 0.147).
4. Discussion
3.5. Sympathetic vasoconstrictor reflex
There was no significant effect for Group on both
quotients of the SVR (QI and SRF) ðP . 0:07Þ nor was there
any interaction effect between Time and Group for either
measure ðP . 0:98Þ (Table 4). However, the moderate/
severe group tended to show higher QI and lower SRF
values than the other two whiplash groups.
3.6. Psychological distress (GHQ-28)
There was a significant main effect for Group for
GHQ-28 total score ðP , 0:01Þ and a significant interaction
between Group and Time ðP , 0:001Þ. As can be seen in
Fig. 4, the groups with moderate/severe (41 ^ 3) or mild
symptoms (33 ^ 3) both had a total GHQ-28 score above
the threshold of 23/24 at entry into the study (, 1 month).
Both groups significantly improved over the 6 month study
period but the moderate/severe group (33.5 ^ 3) continued
to show a GHQ-28 total score above the threshold at
6 months post-injury, whereas the mild group returned to
below threshold levels (21.3 ^ 2).
When GHQ-28 total scores were included in the analysis
of the three whiplash groups, group differences remained
Table 4
Estimated marginal means (SEM) of the sympathetic vasoconstrictor reflex
parameters (QI and SRF) after inspiratory gasp in all groups (all P . 0:07)
Group
QI
SRF
Recovered
Mild pain and disability
Moderate/severe pain and disability
Controls
54 ^ 17.2
53.1 ^ 16.9
64.8 ^ 18.2
52.4 ^ 18.4
0.79 ^ 0.17
0.79 ^ 0.18
0.69 ^ 0.15
0.71 ^ 0.18
Little is known about the continuum of WAD from the
time of injury through transition to either recovery or
chronicity. The results of this study provide the first
evidence that the presence of generalised sensory hypersensitivity can differentiate those with persistent moderate/severe symptoms at 6 months following whiplash injury
from those who have largely recovered. These sensory
disturbances occurred independently of psychological
distress, within a month of injury and persisted unchanged
to 6 months post-injury. It is likely that such changes in
sensory function reflect altered nociception within the
central nervous system. Supporting previous longitudinal
studies (Gargan et al., 1997; Radanov et al., 1995), 61% of
our whiplash subjects reported ongoing pain and disability
of varying degrees at 6 months post-injury. Interestingly, of
this group with persistent symptoms, there exists a subgroup
of subjects (22% of the total cohort) in which there was
evidence of altered nociception and it is this subgroup who
reported more disabling pain levels. This may reflect
different underlying mechanisms between those with higher
pain levels and those with lesser symptoms.
All whiplash injured subjects, irrespective of the level of
reported symptoms, demonstrated early local mechanical
hyperalgesia within the cervical spine possibly reflecting
sensitisation of peripheral nociceptors resulting from
injured neck structures as proposed in previous studies of
acute whiplash (Kasch et al., 2001a; Yerner et al., 2001).
Local mechanical hyperalgesia had resolved by 2 months
post-injury in recovered whiplash subjects and those with
lesser symptoms whereas it persisted in those with ongoing
moderate/severe symptoms. This may reflect healing of the
underlying soft tissue injury in recovered subjects.
Generalised hypersensitivity including widespread
M. Sterling et al. / Pain 104 (2003) 509–517
515
Fig. 3. Range of elbow extension at pain threshold and VAS scores of pain (means and SEM) with the BPPT for all groups (control, recovered, mild pain and
moderate/severe pain) over time (1, 2, 3 and 6 months post-injury).
mechanical and thermal hyperalgesia and heightened
responses to the BPPT was the differentiating feature of
those with persistent moderate/severe symptoms. Widespread hypersensitivity to blunt pressure has been proposed
to occur as a result of sensitisation of central nervous system
nociceptive pathways or changes in endogenous descending
pain modulation mechanisms (Koelbaek-Johansen et al.,
1999; Ren et al., 2000; Treede et al., 2002). This phenomenon has been demonstrated in subjects with chronic WAD
(Koelbaek-Johansen et al., 1999; Sterling et al., 2002a) but
its existence in the earlier stages of the condition has been
disputed (Kasch et al., 2001b). However, past investigation
of such changes have not differentiated whiplash subjects on
the basis of levels of pain and disability and as such may
have overlooked identification of important sub-groups
within this condition. The results of our study emphasise
that whiplash injury is not a homogenous condition.
Heightened responses to the BPPT and thermal (heat and
cold) hyperalgesia were seen soon after injury in the group
with persistent moderate/severe symptoms. Bilateral loss
of elbow extension and higher pain levels with the BPPT
in chronic WAD have been interpreted as reflecting both
hyperalgesic motor and sensory responses as a consequence
of central sensitisation (Quintner, 1989; Sterling et al.,
2002b). Reduced HPT was only present in the more severe
group and may be a feature of nociceptor sensitisation (Kilo
et al., 1994). Enhanced sensitivity to innocuous heat has also
Fig. 4. GHQ-28 total scores (mean and SEM) for all groups (control,
recovered, mild pain and moderate/severe pain) over time (1, 2, 3 and
6 months post-injury).
been proposed to occur due to convergence of fibres
activated by noxious stimuli and heat upon sensitised dorsal
horn neurons (Kosek and Ordeberg, 2000). As such the
reduced HPT seen in the moderate/severe group may be
another reflection of this group’s general hypersensitive
state.
Cold hyperalgesia may be due to changes in the central
mediation of pain (Berglund et al., 2002) but has also been
shown to be a feature of pain due to peripheral nerve injury
(de Medinaceli et al., 1997) and disturbances of SNS
activity (Frost et al., 1988). The possibility of nerve injury
as a contributor to symptoms of those with persistent
moderate/severe symptoms cannot be discounted. Cold
hyperalgesia, together with heightened responses to the
BPPT and mechanical hyperalgesia over peripheral nerve
trunk sites may be indicative of such injury. Injury to nerve
tissue such as nerve roots and dorsal root ganglia has been
demonstrated in cadaveric studies following severe whiplash injury (Taylor and Taylor, 1996) and in clinical studies
where evidence of nerve tissue irritation and ensuing
mechanosensitivity has been shown to be present in chronic
WAD (Ide et al., 2001; Sterling et al., 2002b).
Disturbances in SNS function are not a feature of WAD
as shown on SVR testing. However, there was a tendency
for higher QI and lower SRF quotients in the whiplash group
with moderate/severe symptoms at 6 months post-injury. A
closer inspection of the SVR data in this group revealed that
seven of the 17 subjects showed values for both the QI and
SRF quotients outside approximated normal physiological
ranges (mean values ^ 2 SD) (Schurmann et al., 1996) and
similar to those of patients with complex regional pain
syndrome type 1 (Schurmann et al., 1999). This may suggest
that SNS dysfunction could exist in some whiplash patients
and further investigation involving larger subject numbers is
indicated.
All whiplash subjects in our study were psychologically
distressed to some degree. Both groups with persistent
moderate/severe or mild pain and disability had GHQ-28
total scores above the threshold at entry into the study
(, 1 month post-injury) with the recovered group also
approaching this threshold. All three groups improved over
time until at 6 months post-injury, only the moderate/severe
516
M. Sterling et al. / Pain 104 (2003) 509–517
group continued to score above the threshold. This is
consistent with previous studies showing elevated psychological distress in chronic WAD, likely as a result of their
ongoing pain and disability (Peebles et al., 2001; Radanov
et al., 1996). The presence of hypersensitivity in WAD has
been suggested as being due to the patient’s psychological
distress (Ferrari, 2001). However, when GHQ-28 total
scores were included in the analysis of our data, group
differences on the quantitative sensory tests remained
significant and effect sizes of the GHQ-28 scores on sensory
variables was small. Furthermore, whilst the GHQ-28 scores
of the moderate/severe group significantly decreased over
the study period, all hypersensitive responses remained
unchanged. If the hypersensitivity of the moderate/severe
group seen in this study was merely as a consequence of
psychological distress, a similar pattern of change would be
expected for both psychological and sensory variables.
An alternative explanation for the hypersensitive responses
in the moderate/severe group is disturbances in central pain
processing mechanisms.
The results of this study have implications for the early
management of WAD. Acute WAD is not a homogenous
condition and identification of those with early sensory
disturbances may be important. It has been argued that
appropriate expeditious treatment may help to prevent
transition from acute pain into persistent pain (Cousins,
2002). In the case of the ‘at risk’ patients identified in this
study, this may involve appropriate early pharmaceutical
pain management.
Acknowledgements
This work was supported by Suncorp Metway Insurance,
Queensland and Centre of National Research on Disability
and Rehabilitation Medicine (CONROD).
References
Adeboye K, Emerton D, Hughes T. Cervical sympathetic chain dysfunction
after whiplash injury. J R Soc Med 2000;93:378.
Balster S, Jull G. Upper trapezius activity during the brachial plexus tension
test in asymptomatic subjects. Man Ther 1997;2:144– 9.
Barnsley L, Lord S, Bogduk N. Clinical review. Whiplash injury. Pain
1994;58:283–307.
Berglund B, Harju E-L, Kosek E, Lindblom U. Quantitative and qualitative
perceptual analysis of cold dysesthesia and hyperalgesia in fibromyalgia. Pain 2002;96:177–87.
Brennum J, Kjeldsen M, Jensen K, Jensen K. Measurements of human
pressure pain thresholds of fingers and toes. Pain 1989;38:211–7.
Clarkson H, Gilewich G. Musculoskeletal assessment: joint range of
motion and manual muscle strength. Baltimore, MD: Williams and
Wilkins; 1989.
Cote P, Cassidy D, Carroll L, Frank J, Bombardier C. A systematic review
of the prognosis of acute whiplash and a new conceptual framework to
synthesize the literature. Spine 2001;26:E445–58.
Cousins M. Evidence for persisting pain as a disease entity: clinical
implications. Australian Pain Society, 23rd Annual Scientific Meeting,
Sydney, Australia, 2002
Curatolo M, Petersen-Felix S, Arendt-Nielsen L, Giani C, Zbinden A,
Radanov B. Central hypersensitivity in chronic pain after whiplash
injury. Clin J Pain 2001;17:306–15.
Curatolo M, Banic B, Petersen-Felix S, Andersen O, Radanov B, Villeger P,
Arendt-Nielsen L. Preliminary electrophysiological evidence for
central hypersensitivity in whiplash pain and fibromyalgia. 10th
World Congress on Pain, San Diego, CA: IASP; 2002.
Elvey RL. Brachial plexus tension test and the pathoanatomical origin of
arm pain. In: Glasgow E, Twomey L, editors. Aspects of manipulative
therapy. Melbourne: Lincoln Institute of Health Sciences; 1979.
p. 105–10.
Ferrari R. Whiplash and symptom amplification. Pain 2001;89:203–302.
Frost S, Raja S, Cambell J, Meyer R, Khan A. Does hyperalgesia to cooling
stimuli characterise patients with sympathetically maintained pain? In:
Dubner R, Gebhart G, Bond M, editors. 8th World Congress on Pain.
Amsterdam: Elsevier; 1988. p. 151–6.
Gargan M, Bannister G, Main C, Hollis S. The behavioural response to
whiplash injury. J Bone Joint Surg 1997;79-B:523–6.
Goldberg D. Manual of the general health questionnaire. Windsor: NFERNelson; 1978.
Hurtig I, Raak R, Kendall S, Gerdle B, Wahren L. Quantitative sensory
testing in fibromyalgia patients and in healthy subjects: identification of
subgroups. Clin J Pain 2001;17:316–22.
Ide M, Ide J, Yamaga M, Takagi K. Symptoms and signs of irritation of the
brachial plexus in whiplash injuries. J Bone Joint Surg Br 2001;83:
226 –9.
Kasch H, Stengaard-Pedersen K, Arendt-Nielsen L, Jensen T. Headache,
neck pain and neck mobility after acute whiplash injury. Spine 2001a;
26:1246– 51.
Kasch H, Stengaard-Pedersen K, Arendt-Nielsen L, Staehelin Jensen T.
Pain thresholds and tenderness in neck and head following acute
whiplash injury: a prospective study. Cephalalgia 2001b;21:189–97.
Kilo S, Schmelz M, Koltzenburg M, Handwerker H. Different patterns of
hyperalgesia induced by experimental inflammation in human skin.
Brain 1994;117:385 –96.
Koelbaek-Johansen M, Graven-Nielsen T, Schou-Olesen A, ArendtNielsen L. Muscular hyperalgesia and referred pain in chronic whiplash
syndrome. Pain 1999;83:229 –34.
Kosek E, Ordeberg G. Abnormalities of somatosensory perception in
patients with painful osteoarthritis normalize following successful
treatment. Eur J Pain 2000;4:228– 38.
Mani R, Cooper C, Kidd B, Cole J, Cawley M. Use of laser doppler
flowmetry and transcutaneous oxygen tension electrodes to assess local
autonomic dysfunction in patients with frozen shoulder. J R Soc Med
1989;82:536–8.
Mayou R, Radanov B. Whiplash neck injury. J Psychosom Res 1996;40:
461 –74.
de Medinaceli L, Hurpeau J-C, Merle M, Begorre H. Cold and posttraumatic pain: modeling of the peripheral nerve message. BioSystems
1997;43:145–67.
Moog M, Quintner J, Hall T, Zusman M. The late whiplash syndrome: a
psychophysical study. Eur J Pain 2002;6:283–94.
Munglani R. Neurobiological mechanisms underlying chronic whiplash
associated pain. J Musculoskelet Pain 2000;8:169– 78.
Peebles J, McWilliams L, MacLennan R. A comparison of symptom
checklist 90-revised profiles from patients with chronic pain from
whiplash and patients with other musculoskeletal injuries. Spine 2001;
26:766–70.
Quintner J. A study of upper limb pain and paraesthesiae following neck
injury in motor vehicle accidents: assessment of the brachial plexus
tension test of Elvey. Br J Rheumatol 1989;28:528–33.
Radanov B, Begre S, Sturzenegger M, Augustiny K. Course of
psychological variables in whiplash injury – a 2-year follow-up with
age, gender and education pair-matched patients. Pain 1996;64:
429 –34.
M. Sterling et al. / Pain 104 (2003) 509–517
Radanov B, Sturzenegger M, Di Stefano G. Long-term outcome after
whiplash injury. A 2-year follow-up considering features of injury
mechanism and somatic, radiologic, and psychological findings.
Medicine 1995;74:281–97.
Ren K, Zhuo M, Willis W. Multiplicity and plasticity of descending
modulation of nociception: implications for persistent pain. In: Devor
M, Rowbotham M, Wiesnfeld-Hallin Z, editors. IXth World Congress
on Pain, Vol. 16. Vienna: IASP; 2000. p. 387 –400.
Rhudy J, Meagher M. Fear and anxiety: divergent effects on human pain
thresholds. Pain 2000;84:65– 75.
Schurmann M, Gradl G, Furst H. A standardized bedside test for assessment
of peripheral sympathetic nervous function using laser doppler
flowmetry. Microvasc Res 1996;52:157–70.
Schurmann M, Gradl G, Andress H, Furst H, Schildberg F. Assessment of
peripheral sympathetic nervous system function for diagnosing early
post-traumatic complex regional pain syndrome type I. Pain 1999;80:
149–59.
Selvaratnam P, Matyas T, Glasgow E. Noninvasive discrimination of
brachial plexus involvement in upper limb pain. Spine 1994;19:26–33.
Smith R, Papadopolous E, Mani R, Cawley I. Abnormal microvascular
responses in lateral epicondylitis. Br J Rheumatol 1994;33:1166 –8.
Spitzer W, Skovron M, Salmi L, Cassidy J, Duranceau J, Suissa S, Zeiss E.
517
Scientific monograph of Quebec Task Force on whiplash associated
disorders: redefining ‘Whiplash’ and its management. Spine 1995;20:
1–73.
Sterling M, Treleaven J, Edwards S, Jull G. Pressure pain thresholds in
chronic whiplash associated disorder: further evidence of altered central
pain processing. J Musculoskelet Pain 2002a;10:69–81.
Sterling M, Treleaven J, Jull G. Responses to a clinical test of mechanical
provocation of nerve tissue in whiplash associated disorders. Man Ther
2002b;7:89–94.
Taylor J, Taylor M. Cervical spinal injuries: an autopsy study of 109 blunt
injuries. J Musculoskelet Pain 1996;4:61–79.
Treede R-D, Rolke R, Andrews K, Magerl W. Pain elicited by blunt
pressure: neurobiological basis and clinical relevance. Pain 2002;98:
235– 40.
Vernon H. The neck disability index: patient assessment and outcome
monitoring in whiplash. J Musculoskelet Pain 1996;4:95–104.
Vernon H, Mior S. The Neck Disability Index: a study of reliability and
validity. J Manipulative Physiol Ther 1991;14:409– 15.
Yerner S, Toolanen G, Knibestol M, Gerdle B, Hildingsson C. Prospective
study of trigeminal sensibility after whiplash trauma. J Spinal Disord
2001;14:479–86.