A t d M ti ti i A t d M ti ti i Assessment and Motivation in Young People
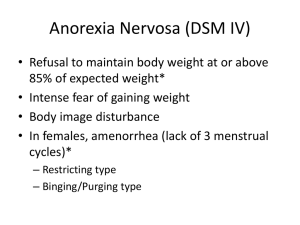
advertisement

A Assessment t and dM Motivation ti ti iin Young People with Eating Disorders Rachel Lawson Senior Clinical Psychologist South Island Eating Disorders Service A quick introduction introduction… South Island Eating Disorders Service Accept p referrals from 13 yyears of age g Twenty five percent of clients aged 1313-17 Treatment offered is mostly outpatient Six inpatient beds Medical admissions Weight Recovery Programme Overview Assessment What are the eating g disorders in yyouth? ED specific questions Physical Risk Motivation An ego syntonic problem Rates of Eating Disorders P Prevalence l ((over a lif lifetime) ti ) Anorexia Nervosa: Bulimia Nervosa: 0.3% 1-2% Incidence (new cases) A i N 000 Anorexia Nervosa: 8 per 100 100,000 Highest for females 1515-19 Bulimia Nervosa: 11 per 100,000 The Eating Disorders Anorexia Nervosa Bulimia Nervosa EDNOS Anorexia Nervosa Diagnostic Criteria Refusal to maintain body weight at or above a minimally normal weight for age and height I t Intense fear f off gaining i i weight i ht or becoming b i ffat, t even though underweight Disturbance in the way in which ones body weight or shape is experienced. Undue influence of body weight on se self e evaluation or de denial of the seriousness of the o a ua o o a o e se ous ess o e current low body weight. Amenorrhea ((absence of at least 3 consecutive menstrual cycles) Anorexia nervosa is divided into two subtypes: restricting type and bingeeating/purging type type. Anorexia Nervosa Diagnostic Criteria Child Children and d Ad Adolescents l t Failure to make expected weight gains (i.e. while growing in height) instead of weight loss No menstruation by age 15 despite other pubertal changes (primary amenorrhea) Bulimia Nervosa Diagnostic Criteria R Recurrent t episodes i d off bi binge eating ti Eating, in a discrete period of time an amount of food that is definitely larger than most people would eat during a similar period of time and under similar episodes A sense of lack of control over eating during the episode Recurrent inappropriate compensatory behaviour in order d tto preventt weight i ht gain i Bulimia Nervosa Diagnostic Criteria Both B th behaviours b h i mustt occur att lleastt ttwice i a week for three months Self-evaluation is unduly influenced by body Selfshape and weight The disturbance does not occur exclusively during episodes of anorexia nervosa Bulimia nervosa is divided into two subtypes: non--purging and purging subtype non Eating Disorder Not Otherwise Specified (EDNOS) Failure to meet the full criteria for either anorexia nervosa or bulimia nervosa Individuals receive the diagnosis of the disorder their symptoms appear to match to the closest Binge eating disorder (BED) Recurrent episodes of binge eating in the absence of the regular use of inappropriate compensatory behaviors characteristic of bulimia nervosa Others types of clinical eating disturbance Pervasive refusal syndrome Food avoidance emotional disorder Functional dysphagia /food phobia Selective eating/extreme faddiness Restrictive eating/poor appetite Lask,B & Bryant Bryant--Waugh, R (2007) Eating Disorders in childhood and adolescence adolescence, Hove Hove, East Sussex:Routledge. Assessment Eating Behaviors Understand eating patterns What she would eat on a typical yp dayy and at different times of the day? E.g., are they restrictive, chaotic, governed by rules about time Fluid intake Physical health problems secondary to dehydration ((especially p y in the case of frequent q vomiting g and laxative use) or excessive fluid intake Eating Behaviors Foods that are specifically avoided, and the reasons for this avoidance Rituals E E.g., eating ti ffood d iin a particular ti l order d Bingeing Frequency of bingeing over a week The types of food she binges on The amount of food eaten in these episodes i d Does she of co control” oes s e feel ee “out out o t o while e bingeing? Bingeing What about Wh b other h times i when h you eat what h seems lik like a llot? ? How much is that? Can you give me an example of a typical binge? How often does it happen? How long has it been happening? When does it happen? Where does it happen? Wh t’ usually ll going i on? ? What’s How fast do you eat? How in control of your eating do you feel? Could you stop once you started? How do you feel before/during/after? What do you think afterwards? Then what happens?… Purging V iti Vomiting For how long? How often? Only after binges? Other times? Are there any rules around vomiting? Laxatives, diuretics, diet pills type and dose Any y other p purging g g behaviours? Excessive Exercise Ai T Aim: To establish t bli h th the diff difference b between t h healthy lth and d excessive exercise Excessive exercise - four or more hours per week undertaken solely or primarily to influence weight or shape Postponement is accompanied by intense guilt (Mond et al al, (2006) Int J Eat Disord Disord, 39:2 147147-153) Does she exercise? How much exercise does she take? Wh type off exercise? i ? Wh h purpose off the h exercise? i ? If What What iis the she could not exercise how would she feel? Compulsive exercise Is there a rigid number of sitsit-ups that must be completed? Triggers To Behaviours Triggers to the bingeing and purging behaviours To get a sense of the function the behaviour is serving, e.g. affect regulation as well as a response to starvation Behaviour Hunger/fullness (tick (t c if reported) epo ted) Social (tick (t c if reported) epo ted) Emotional states? ((indicate d cate which c apply) app y) * * * * * * * * Bingeing Anger ; anxiety ; depression ; shame ; * * boredom ; loneliness Purging Anger ; anxiety ; depression ; shame ; * * boredom ; loneliness Psychosexual functioning Current and past menstrual function current frequency and nature of her periods her age at menarche and her reaction to the onset of her periods history of absence of periods is linked to her weight history Central Cognitive Elements Di t b Disturbance off Body B d Concept C t How she feels about her body? If she likes/dislikes it? Do D her h feelings f li diff for differ f different diff t parts t off her h body? Body checking practices, practices including weighing Disturbance of Body Percept (sees self as too fat/thin) How she sees herself when she looks in the mirror? Do other people agree with what she sees? Body percept exercise Central Cognitive Elements F Fear off fatness f t How would you feel if you gained a kilo? Wh t might What i ht you d do about b t th that? t? Self--Evaluation Self I am now going i to t askk you a rather th hard h d question ti – you may not have thought about this before. Over the past four weeks has your weight/shape been important in influencing how you feel about think yourself as a person? F example, For l ffriend i d who h plays l th the piano i Self--Evaluation Self Cli t' Current Client's C t Self-Evaluation S lf E l ti Pie Chart Relationship Family Friends School Weight and Shape Client's Ideal Self-evaluation Pie Ch t Chart Familyy Friends Relationship School Wgt/Shape Hobbies Weight History History Plunket books Natural Body Weight Set Point theory Family tree for weight and height Ri k tto Physical Ph i l H lth Risk Health What has been happening to your weight over the past 88-12 weeks? k ? Presenting History When did you first start having concerns g p g about yyour weight/shape/eating? Teasing/bullying around weight and shape Wh t was/is What /i your ffamily’s il ’ attitude ttit d tto eating/shape/weight? Who in your family dieted/struggled with weight control? Psychometrics B d Ch Body Checking ki Q Questionnaire ti i (BCQ) 23 items looking at checking related to overall appearance, specific body parts and idiosyncratic checking rituals Eating Disorders Examination Examination--Q4 (EDE(EDE-Q) Focuses on p past 28 days y and asks for frequencies of eating disorder behaviours Subscales – dietaryy restraint,, eating g concerns, concerns about weight and shape, and a global score Physical Risk Physical Risk All clients with eating disorders are at medical risk to some degree g Weight or BMI is only one aspect of this e.g, A patient ti t with ith a BMI off 15 but b t who h is i losing weight at a kilo a week is likely to be i k than th someone who h h more att risk has kkeptt a stable BMI of 14 over many years Frequent use of purging (vomiting, diuretics, laxatives) greatly increases physical risk, especially if patient underweight Urgent Medical Review The client should have a review by a physician p y as a matter of urgency g y if any y of the following apply: BMI is 13 or below There is recent rapid weight loss (more than a kilo per week) over several pe ee ) o e se e a weeks ee s The patient reports fainting, dizziness or blackouts. Evidence of ketoacidosis (e.g., breath has a distinctive sweet smell, similar to nail varnish remover or pear drops) Urgent Medical Review Children and Adolescents Rapid p weight g loss Rapid dehydration Less reserves including body fat South Island Eating Disorders Service Physical Assessment Weight W i ht and dH Height i ht “% weight for height scales” Bloods Urea and Electrolytes: To assess for electrolyte imbalance, dehydration, kidney function Li Liver F Function ti ttests: t To T assess for f damage d to t liver li secondary d to t low weight/ and or alcohol misuse Full Blood Count: To assess for bone marrow suppression secondary to low weight Thyroid stimulating hormone (TSH): To exclude thyroid g loss ((NB thyroid y levels may y be reduced abnormalities for weight in low weight individuals or in people on very restrictive diets) South Island Eating Disorders Service Physical Assessment ECG To assess effect of extreme state of starvation on the heart Squat Test To assess proximal muscle weakness and whether extensive muscle failure has occurred Pulse and blood pressure (lying and standing) To assess stress on cardiac systems and the effects of dehydration Bone Scan May be arranged following assessment Risk factors: Low weight and amenorrhea for more than six months Appendix ppe d Physical Assessment General Health Diabetes and an ED can coco-occur as a devastating combination P Poor di diabetes b t control t l Withhold insulin to provoke hyperglycaemia and weight loss Repeated p ketoacidosis and coma Rapid onset of severe diabetic complications Motivation Developmental Tasks Adjust to new physical sense of self Establish intimacy Develop autonomy Develop new intellectual abilities self-esteem Develop competencies and selfEstablish a unique identity Functions of an Eating Disorder Task: T k New N Ph i l self Physical lf Rapid gains in weight and height Development of secondary sexual characteristics Starvation helps avoid adjusting to a new physical sense of self Task: Establish Intimacy P Peer groups Social withdrawal associated with eating disorders can provide protection from the lack of peer group/ issues within a peer group Anorexia becomes a friend Functions of an Eating Disorder T k Development Task: D l t off Autonomy A t To think, feel, make decisions and act on his or her own Anorexia can reduce the complexities of life to a list of rules about food Filters decisions to the level of “will this make me fat?” Task: Development of competencies and selfself-esteem Achievement preferences and areas where adolescents are willing to strive for success A time to try a variety of activities Anorexia can provide a sense of success “I am good at losing weight” Functions of an Eating Disorder Task: Development of Identity Knowing g where yyou fit,, or your y place p in the world Anorexia can provide an identity Maintaining Factors Key’s Study Preoccupation p with food Social withdrawal Biological Effects g Gastric emptying slows Metabolic rate slows Psychometrics Pros and Cons of Anorexia Scale (P(P-Can) 50 items “I see my anorexia as being dependable and consistent’ “Anorexia is something I am good at” Serpell et al. (2004) The development of the PP-CAN, a measure to operationalize the pros and cons of anorexia nervosa, International Journal of Eating Disorders, 36, 416416-433 Motivation Clinician Stance (Geller et al) St t i Strategies for f assessing i and d enhancing motivation: P Pros and d cons Friend or foe letters Pie charts Life Plans Miracle question Problems and goals Model Stages of change (Procheska & DiClemente) Appendix Medical indicators for hospital admission – Dr Geoff Buckett Rapid wt loss (>4kg in a month) BMI<13 Inability to eat/retain food Confusion, organic brain syndrome, ophthalmoplegia, hth l l i ataxia, t i syncope, LOC LOC, seizures, tetany Dysrhythmia, angina, chest pain, SOB, y p , variable HR ((<60 and bradycardia<40bpm, >150, HR >25 lying vs standing Raised creatinine, oliguria (<400ml/day) Rapidly diminishing exercise tolerance Marked lab abnormalities: K<2.5, PO4<0.3, glucose<2.5 Severe neutropenia <0 <0.6 6 ECG abnormalities – QTc >500, ventricular arrhythmia Medical Risk Information “A guide to medical risk assessment for eating g disorders” Maudsley Hospital, London www.eatingresearch.com