GEORGE WASHINGTON UNIVERSITY SPORTS MEDICINE NEW
advertisement

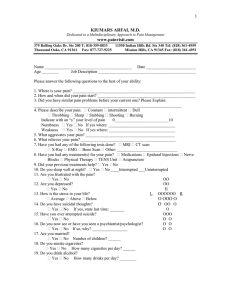
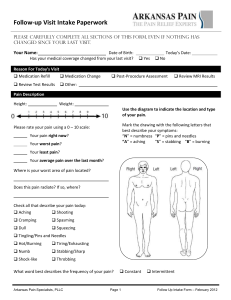
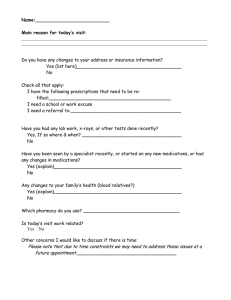
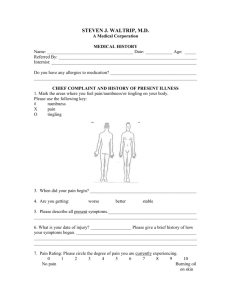
GEORGE WASHINGTON UNIVERSITY SPORTS MEDICINE NEW PATIENT QUESTIONNAIRE RAJEEV PANDARINATH, MD Name: _______________________________ Gender: ____ Male ____ Female Date of Birth: ____/____/____ Telephone Number: Home: _________________ Work: ___________________ Cell Phone: _________________ Primary Care Physician: ______________________________________ Phone Number: ______________________ Address:__________________________________________________________________________________ Referring Physician/ Work Comp Agency/ Nurse/ Trainer/ Therapist (circle one): Name: _______________________________________________ Phone Number: ______________________ Address: _________________________________________________________ Age:______ Height: ____ ft. ____ in. Weight: _______lbs. Heart Rate: ______ Hand Dominance: ___ R ___L Occupation: ___________________________________ Auto/Worker’s Compensation Case: _____ Yes _____ No What leisure activities/sport(s), if any, do you participate in? ___________________________________________ Location of Symptoms: _____ Right _____ Left _____ Both ____ Head ____ Neck ____ Shoulder ____ Arm ____ Elbow ____ Forearm ____ Wrist ____ Hand ____ Mid-Back (thoracic) ____ Low-Back (lumbar) ____ Hip ____ Thigh ____ Knee ____ Shin/Calf ____ Ankle ____ Foot Please Mark Location of Symptoms on Figures(s) Below: Front Back Date of Injury (if known): _____/_____/_____ Duration of Symptoms: _____ Day(s) _____Week(s) _____Month(s) _____ Year(s) How Injured: _____ Trauma _____ Motor vehicle/Motorcycle accident _____ Sports _____ No Injury _____ Fall _____ Other:_______________________ Mechanism of Injury: _____ Chronic overuse _____ Sudden stop _____ Throwing Symptoms: _____ Swelling _____ Locking _____ Catching _____ Clicking _____ Giving way _____ Stiffness _____ Fevers/Chills _____ Twist/Pivot _____ Direct impact _____ Reaching _____ Weakness _____ Numbness _____ Tingling _____ Burning _____ Partial dislocation _____ Dislocation _____ Symptoms in morning Pain Level: __ Mild __ Moderate __ Severe Where injured: _____ Work _____ Sporting event _____ Home _____ Gym _____ Other:____________________________ _____ Lifting _____Fall _____ Running _____ Jumping _____ Bending _____ Don’t recall _____ Other:____________________________________ _____ Symptoms during day _____ Symptoms in evening _____ Symptoms at sleep _____ Symptoms at rest _____ Symptoms with activity _____ Symptoms with reaching _____ Symptoms with stairs _____ Symptoms with squat/kneel _____ Symptoms with sitting _____ Symptoms with walk/run _____ Symptoms with throwing What makes the symptoms worse? ________________________________________________________________ ______________________________________________________________________________________________ What makes the symptoms better? ________________________________________________________________ ______________________________________________________________________________________________ Prior history of surgery or treatment for this specific problem? ____ Yes ____ No If "YES" please check all that apply: ____ Physical/Occupational Therapy (Duration: _____ Weeks _____ Months) Improved condition: _____ Yes _____ No Worsened condition: _____ Yes _____ No ____ Injection(s) Type: _____ Joint _____ Soft tissue _____ Trigger point _____ Epidural Medication used: _____ Steroid _____ Joint fluid (ie. Synvisc, Supartz, Hyalgan, Orthovisc, Euflexxa) Total number of injections given: _________ (Date of most recent injection: ____/_____/_____) Improved condition: _____ Yes _____ No Worsened condition: _____ Yes _____ No ____ Medications used: _____________________________________________________________________ ____ Surgery Procedure: ___________________________________________________ Date: ____/____/____ Surgeon: _________________________________________________________________________ Any complications during or after? _____________________________________________________ Procedure: ___________________________________________________ Date: ____/____/____ Surgeon: _________________________________________________________________________ Any complications during or after? _____________________________________________________ ____ Chiropractic ____ Accupuncture ____ Foot Orthotics ____ Casting (How many weeks were you casted? _______ weeks) ____ Brace (Type: ________________________________________________ ) ____ Other (please specify): _________________________________________ Have you had any studies done to evaluate this problems? _____ Yes _____ No Date(s) Location ____X-rays __________________________ ________________________________________________ ____MRI ____________________________ ________________________________________________ ____Cat Scan ________________________ ________________________________________________ ____Ultrasound _______________________ ________________________________________________ ____ Bone Scan ______________________ ________________________________________________ ____ EMG/NCS ______________________ ________________________________________________ MEDICAL/SURGICAL HISTORY: Medical problems you currently have OR have had in the past (Check all that apply): ____ High blood pressure ____ Asthma ____ Osteoarthritis ____ Kidney disease ____ Heart attack ____ COPD ____ Rheumatoid arthritis ____ Urinary problems ____ Heart failure ____ Sleep Apnea ____ Gout ____ Bleeding disorder ____ High cholesterol ____ Diabetes ____ Systemic lupus ____ Anemia ____ Irregular heart beat ____ Thyroid disease ____ Lyme disease ____ TB ____ Pacemaker/Defib. ____ Osteopenia,-porosis ____ Fibromyalgia ____ HIV ____ Vascular disease ____ Migraines ____ Stress fractures ____ Depression ____ Clots ____ Seizures ____ Hepatitis ____ Glaucoma ____ Aneurysm ____ Concussion ____ Gastric reflux/ulcer ____ Hearing loss ____ Stroke ____ Alzheimers ____ Irritable bowel ____ ADHD ____ Cancer (Type(s): _____________________________________________________________________________ Please list any surgical procedures (for any reason) you have had in the past: Month/Year Surgery Type ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ALLERGIES to any medications? _______ Yes _______ No If "YES", please list: _____________________________________________________________________ MEDICATIONS/VITAMINS/DIETARY SUPPLEMENTS you are currently taking? _____________________________________________________________________________________ _____________________________________________________________________________________ SOCIAL HISTORY: Do you smoke? ____ Yes ____ No If "YES", how many packs per day? ________ Do you drink alcohol? ____ Yes ____ No If “YES”, is you weekly intake: ____ Light ____ Moderate ____ Heavy ____ Social drinker only Are you currently working? ____ Yes ____ No ____ Disabled ____ Student If "YES", what is your current occupation? __________________________________________________ Your current work day is: ____ Full Time ____ Part Time What is your current work status: ____ Full Duty ____ Modified Duty with Restrictions Are you married? ____ Yes ____ No ____ Divorced/Separated How many children do you have? _______ _____ Widowed What leisure activities/sports do you regularly participate in?: _______________________________ FAMILY HISTORY (including parents, grandparents, and siblings): Illness Which Family Member(s)? Cancer ____ Yes ____ No ________________________________________ High blood pressure ____ Yes ____ No ________________________________________ Heart disease ____ Yes ____ No ________________________________________ Asthma/COPD ____ Yes ____ No ________________________________________ Diabetes ____ Yes ____ No ________________________________________ Thyroid disease ____ Yes ____ No ________________________________________ Strokes ____ Yes ____ No ________________________________________ Mental illness ____ Yes ____ No ________________________________________ Bleeding disease ____ Yes ____ No ________________________________________ Rheumatoid arthritis ____ Yes ____ No ________________________________________ Osteoarthritis ____ Yes ____ No ________________________________________ Systemic lupus ____ Yes ____ No ________________________________________ Other: __________________________________________________________________________ REVIEW OF SYSTEMS (Please check all current medical issues): YES NO ____ ____ Decreased hearing ____ ____ Ringing in ear ____ ____ Ear infections ____ ____ Dizzy spells ____ ____ Fainting spells ____ ____ Double vision ____ ____ Blurred vision ____ ____ Nosebleeds ____ ____ Sinus trouble ____ ____ Sore Throats ____ ____ Hay fever/allergies ____ ____ Shortness of breath ____ ____ Chest pain ____ ____ Heart palpitations ____ ____ Leg pain when walking ____ ____ Tremors/ hands shaking ____ ____ Muscle weakness ____ ____ Headaches ____ ____ Foot pain ____ ____ Rash ____ ____ Eczema ____ ____ Insomnia YES ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ NO ____ Loss of appetite ____ Difficulty swallowing ____ Heartburn ____ Nausea/vomiting ____ Chronic abdominal pain ____ Change in bowel habits ____ Constipation/diarrhea ____ Bloody/tarry stools ____ Urinary problems ____ Urethral discharge ____ Chronic fatigue ____ Weight change ____ Gain ____ Loss ____ Numbness/tingling ____ Back pain ____ Cold/numb feet ____ Hives ____ Memory loss ____ Difficulty concentrating ____ Anxiety ____ Nervousness By signing below, I verify that the above information is correct and true to the best of my knowledge. __________________________________ (Patient Name) __________________________________ (Patient Signature) _____________ (Date)