The Hematologist January-February 2016
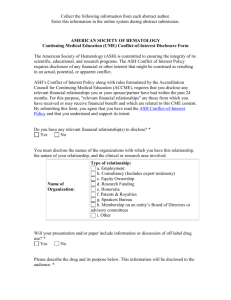
advertisement

ASH NEWS AND REPORTS® JANUARY/FEBRUARY 2016 VOLUME 13 ISSUE 1 What We Carried on Christmas Fiction for the Year’s Best in Hematology JASON GOTLIB, MD, MS, Editor-in-Chief Editor’s Note: The characters in the following story are fictionalized versions of patients we have managed on the hematology service. The title “What We Carried on Christmas” is a tribute to “The Things They Carried,” Tim O’Brien’s critically acclaimed short story from 1987 that uses the list as a writing form to tell a powerful story of a platoon in Vietnam. The commentary following this piece provides my perspective on how hematology advances, including 2015 Year’s Best selections, weave together with the compelling narratives of our patients’ lives. My Christmas morning commute to Stanford Hospital felt like a post-apocalyptic odyssey. I didn’t spot a single car or human being on the eight-mile stretch of Interstate 280. However, shortly after taking the off-ramp to Sand Hill Road, I came upon a freshly struck deer lying in the left lane. I slowed down and surveyed the carnage. Its warm entrails formed an accidental palette with the shoulder’s yellow border. Along this corridor of venture capital firms, a Tesla sped off from the scene. It carried dollops of the deer on its front grille, while leaving an electric hum in its wake. The driver would hide this accident from his family so it couldn’t taint the splendor of the holiday. I drove away, carrying the vicissitudes of this deer’s life with me to inpatient hematology rounds, along with my stethoscope and iPhone. On Christmas morning, Paul carried an extra 5 kg of fluid from his AML induction. The edema made little difference on the 6’6”, 120-kg frame that he sculpted during Army Special Forces training in the early 1990s. His physique blended a perfect combination of slow-twitch and fast-twitch muscle memory that made it easy to double-tap a target while hanging upside down in the dark. Paul carried the tip of the spear as a member of Delta Force during two Gulf wars and numerous clandestine ops around the globe. The team stared at his massive figure when he lapped around the hematology unit with his diminutive IV pole; the nurses and other patients gawked, too, like rubberneckers transfixed by that swirl-cake of a deer. When United Airlines flight 77 tore into the Pentagon, Paul had scooped up workers and carried them to safety before the ceiling of their office collapsed. For a few hours, he inhaled a plume of super-heated dust consisting of incinerated concrete, fuselage, and parts of people’s souls. His lungs carry the scars of that day. A few months after 9/11, he developed pneumonitis and lost a quarter of his pulmonary function. It’s possible the toxic brew also corrupted his bone marrow. During morning rounds, Paul shared tidbits from some of his Delta Force missions, including Operation Gothic Serpent in Mogadishu and Operation Enduring Freedom against the Taliban. During treatment, his waning appetite made him think of meals at home and abroad. He joked about the similar textures and tastes of combat MREs and our cafeteria’s selections. He reminisced about toppings that presaged the dinner menu at his base in Kabul: horseradish on the tables was followed by prime rib, and applesauce heralded pork chops. For worsening trismus related to mucositis, ENT had him bite down on a stack of tongue blades to exercise his jaw. This wasn’t very difficult for him. Muscle memory. I imagined a celluloid version of Paul clenching the blade of a knife between his teeth while scaling a wall just before snatching a high-value target. Paul’s three children and wife spent Christmas day with him in his room. He hopes that his illness will bring them closer together. In two weeks, he’ll leave the hospital. When I have the results of his remission marrow, he’ll be (Cont. on page 6) Advances in aplastic anemia LEUKEMIA 2 PRESIDENT’S COLUMN – ASH President Dr. Charles S. Abrams highlights how ASH will continue to grow in 2016. 3 PET-directed therapy in lymphoma Boosting HSC engraftment Reversal agents for DOACs Clonal Hematopoiesis Hope Myeloma antibodies NEWS AND REPORTS – Meet the four contributing editors that joined The Hematologist’s Editorial Board in 2016. New frontiers in sickle cell disease 6 57th ASH Annual Meeting Wrap-Up: Hematology’s Own Cambrian Explosion LAURA C. MICHAELIS, MD Associate Professor of Medicine, Division of Hematology and Oncology, Medical College of Wisconsin, Milwaukee, WI; ASH News Daily Editor, 2015 Harvard paleontologist Dr. Stephen Jay Gould was best known for his theory of “punctuated equilibrium,” which, as a neophyte like me understands it, argues that evolution is not the smooth upward trajectory envisioned by Charles Darwin. Instead, the fossil record shows evolution to be a bumpy road characterized by very long periods of developmental stasis followed by stretches of remarkably rapid changes as natural selection gallops forward. As I look back on another year of results and ideas presented at the 2015 ASH Annual Meeting, I wonder if our profession’s accomplishments are showing a similar pattern. If so, it seems that we are in the midst of one of those epochs of rapid change. Take lymphoma treatment, for example. For decades, tumor growth rate was the sole target with which to approach therapy — the clearest way to leverage the difference between normal cells and the cancer cell. In 1997, after decades of improvements in the tools and trade of molecular biology, better understanding of cellular processes led to the approval of rituximab, one of the initial landmark “targeted” agents in cancer care. Less than 20 years have passed since that approval, and now most of the treatments that are being tested in lymphoma capitalize on our growing understanding of the molecular behavior of the cancer cell. Translational research, for example, is responsible for remarkable gains in the treatment of chronic lymphocytic leukemia (CLL). This year, the Late-Breaking Abstracts (LBA) session included results from two studies of novel agents for relapsed/refractory CLL. One study presented YEAR’S BEST – The Hematologist lists rankings from the 2015 Year’s Best in Hematology reader survey. (Cont. on page 4) 14 IN MEMORIAM – Colleagues reflect on the life and professional accomplishments of the late Dr. Zucker-Franklin. President’s Column Hematologist THE ASH NEWS AND REPORTS® ISSN 1551-8779 PUBLISHED BIMONTHLY Editor-in-Chief: A New Year Full of Promise for ASH Jason Gotlib, MD, MS Stanford Cancer Institute Stanford, CA A s we enter into the New Year, I would like to acknowledge the support and leadership that Dr. David Williams has provided ASH and its members throughout 2015. Contributing Editors: In the past several years, the January/February issue of The Hematologist has looked back at the previous year’s achievements and has celebrated the way in which ASH’s annual meeting convenes the best minds in the discipline. This year in Orlando, I was impressed with the rapid rate of progress and discovery that the field of hematology is currently enjoying and the unique and enticing opportunities where ASH could play a leading role. Pamela S. Becker, MD, PhD University of Washington Seattle, WA Theresa Coetzer, PhD University of the Witwatersrand Johannesburg, South Africa Some of the most meaningful ways ASH can lead is by steadily growing, and refining, the Society’s content offerings. With each issue of Blood, there continues to be a drive toward high-quality, cutting-edge research, resulting in novel therapies across a wide variety of subspecialties. Additionally, in 2016, these efforts will continue with the launch of a new journal from ASH, designed to keep both researchers and clinicians abreast of topics in emerging areas, including, but not exclusive to, immunotherapies and gene editing. Adam Cuker, MD, MS University of Pennsylvania Philadelphia, PA David Garcia, MD University of Washington Seattle, WA In addition to publications, ASH will launch new educational offerings in 2016 that are in line with the explosive breakthroughs in hematology. To shed continued light on the latest advances in basic and translational lymphoma research, the second Meeting on Lymphoma Biology will take place in June in Colorado Springs, Colorado, while the second ASH Meeting on Hematologic Malignancies in September will feature clinical breakthroughs and cutting-edge treatment approaches to lymphomas, leukemias, and other malignant conditions. Furthermore, because training is so pivotal to our ongoing progress and mission, ASH will launch the Medical Educator’s Institute, which will equip medical educators with a “boot camp” that will cover teaching techniques, as well as proper evaluation of trainees and programs. Tracy I. George, MD University of New Mexico Albuquerque, NM Jonathan Hoggatt, PhD MGH/Harvard University Cambridge, MA It is impossible to discuss the influx of innovation without also mentioning new drugs and precision medicine. At the 2015 Annual Meeting, there were two sessions (one delivered in partnership with the U.S. Food and Drug Administration) devoted to the recent introduction of exciting new drugs available in benign and malignant hematology. With regard to precision medicine, ASH’s newly defined Agenda for Hematology Research has prioritized the areas of genomic profiling and chemical biology and has also created a task force on precision medicine to identify and capitalize on the opportunities in hematology. Building on the research that has been conducted by our members, 2016 is gearing up to be an exciting year in which developments in new drugs and novel treatments based on the human genome will continue on the path to becoming clinically meaningful. Peter Johnson, MD Southampton General Hospital Southampton, United Kingdom Mark J. Koury, MD Vanderbilt University Nashville, TN Impressive momentum abounded all throughout hematology last year, and sickle cell disease (SCD) was no exception. From promising improvements in gene therapy, to new approaches for vaso-occlusion, SCD researchers saw some incredible advancements. To strengthen the pace of innovation, ASH announced a new “Call to Action” for SCD during an April 2015 Summit, and in 2016, the Society will expand on the strategies identified, to create new work groups focused on access to care, research, and global outreach. Ann LaCasce, MD, MSc Dana-Farber Cancer Institute Boston, MA Charles T. Quinn, MD, MS Cincinnati Children’s Hospital Medical Center Cincinnati, OH Finally, 2016 will be another year in which ASH continues to expand outreach and growth on a global scale. To begin with, we were excited to announce, after the close of the 2015 annual meeting, a newly approved category of membership that gives International members the right to vote, and that gives the Nominating Committee the flexibility to nominate international candidates to run for a Councillor position, as appropriate for the needs of the Society, at any given time. Another bylaws amendment has created a membership category for International Associate members, which allows trainees outside of North America to join and enjoy a member benefits package similar to that of Associate members in North America. Elizabeth Raetz, MD University of Utah Salt Lake City, UT Noopur Raje, MD Massachusetts General Hospital Boston, MA I am incredibly proud to help realize the promise of the new year as president of ASH, as our Society continues to demonstrate its leadership in some of the most thrilling areas of scientific and clinical exploration. Managing Editor Juana Llorens, MS Editorial Associate Laura M. Santini Graphic Designer grayHouse design Charles Abrams, MD American Society of Hematology 2021 L Street, NW, Suite 900 Washington, DC 20036 jllorens@hematology.org I N ©2016 by the American Society of Hematology. Contributing authors have declared any financial interest in a product or in potentially competing products, regardless of the dollar amount. Any such financial interest is noted at the bottom of the article. Dr. Gotlib has no relevant conflicts of interest to disclose. The material published in The Hematologist is for informational purposes only. The opinions of the authors and editors of The Hematologist are their own and do not necessarily represent official policy of the American Society of Hematology. ASH does not recommend or endorse any specific tests, physicians, products, procedures, or opinions, and disclaims any representation, warranty, or guaranty as to the same. Reliance on any information provided in this publication is solely at your own risk. Bernard G. Forget, MD (1939-2015) PHOTO BY JOHN CURTIS, YALE MEDICINE All materials contained in this newsletter are protected by copyright laws and may not be used, reproduced, or otherwise exploited in any manner without the express prior written permission of The Hematologist: ASH News and Reports. Any thirdparty materials communicated to The Hematologist become its copyrighted property and may be used, reproduced, or otherwise exploited by The Hematologist. Dr. Bernard G. Forget died on November 6, 2015, at the age of 76, after a threeyear battle with cancer. The hematology community has lost one of its most beloved and esteemed colleagues. Bernie was born in Fall River, Massachusetts, where his French Canadian father served as a dedicated general practitioner. After undergraduate training at the University of Montreal, Bernie received an MD in 1963 from McGill University where he was class valedictorian. Following a medical internship and residency at Massachusetts General Hospital, he received training in hematology at the National Institutes of Health (NIH) and at Children’s Hospital in Boston. His early scientific development was fostered by the mentoring of Drs. Roger Monier, Sherman Weissman, and David Nathan. In 1976, Bernie joined the Departments of Medicine and Human Genetics at Yale University where he devoted the remainder of his career. He was chief of Yale’s Section of Hematology from 1976 to 1987, and again from 1993 to 2005. During this 30-year span, he made landmark research contributions and oversaw the training and mentoring of a generation of students, residents, and fellows, many of whom have become leaders in hematology research and clinical practice. Bernie and his research team pioneered studies of molecular pathogenesis of congenital red cell disorders. He was the first to use specific ribonucleases to prepare two-dimensional maps of globin mRNA that enabled sequence information to be generated on both coding and noncoding segments. This early work was critically important 2 M E M O R I A M in facilitating the cloning of globin genes. His studies of the flanking regions of the human γ-genes provided insight into the physiologically and clinically important switch from γ- to β-gene expression. Subsequently, Bernie’s lab focused on the molecular genetics of red blood cell (RBC) membrane proteins. His lab was the first to clone and sequence genes encoding α- and β-spectrins, the major proteins of the RBC cytoskeleton. These studies paved the way toward a molecular understanding of the assembly of red cell membrane proteins. Bernie’s work on the globin genes and on those encoding RBC membranes have clear-cut relevance to important blood disorders such as thalassemia, sickle cell disease, and congenital hemolytic anemias due to mutations in red cell membrane proteins. During his long and remarkably productive career, Bernie received many honors, including membership in the American Society for Clinical Investigation, the Association of American Physicians, and the American Academy of Arts and Sciences. He was awarded the Henry M. Stratton Medal from ASH in 1996 and was the recipient of the Yale Cancer Center Lifetime Achievement Award in 2013. A happy and fulfilling family life was a huge contributor to Bernie’s remarkable record of leadership and discovery. During their time together in New Haven, his wife Bernadette held a position of comparable responsibility in nursing at the Yale-New Haven Hospital. She and Bernie were blessed with three children and three grandchildren. The Forget family cherished time together at their seaside home in Rhode Island as well as frequent trips to France, which helped sustain Bernie’s Gallic pride and temperament. –H. Franklin Bunn, MD, Hematology Division, Brigham and Women’s Hospital, Harvard Medical School The Hematologist: ASH NEWS AND REPORTS President’s Column N E W S A N D R E P O R T S Register for the First-Ever ASH Workshop on Genome Editing The Hematologist Board of Contributing Editors Maintains the Cycle of Excellence in 2016 The ASH Workshop on Genome Editing will take place July 14-15, 2016, at the Omni Shoreham Hotel in Washington, DC. This workshop was created to provide a forum that focuses on the mechanistic aspects, and possible clinical implications of genome editing for blood disorders. Academic researchers, industry scientists, regulators involved in the clinical application of the technology, and other interested individuals are encouraged to attend. Learn about the basic science of genome editing, its application in clinic, current scientific challenges in using this tool for research purposes, application of the technology to hematologic disorders, as well as regulatory issues. There will also be ample opportunities to network with colleagues and world-class experts, and to explore possible collaborations. For a list of speakers and additional information, and to register online, visit www.hematology.org/genome-editing. The yearly convening of The Hematologist Editorial Board at the ASH annual meeting always marks a time of transition. In December 2015 in Orlando, we expressed our gratitude to four outgoing Contributing Editors: Drs. Mark Koury, Peter Johnson, Pamela Becker, and Charles Quinn. Both Drs. Koury and Johnson served for consecutive terms. Since first joining the editorial board in 2012, Mark, with his wealth of expertise in erythropoiesis along with 30 years of experience in research and clinical practice at Vanderbilt University, has endowed this publication with dozens of challenging, thought-provoking contributions. We will greatly miss the enthusiasm of Southampton General Hospital’s Peter Johnson, whose thoughtful Diffusion selections brought us the most significant developments in topics from lymphoma, to molecular diagnostics, to emerging antibody therapeutics. We also had the benefit of working with Pamela Becker of the University of Washington. Pam’s incredible expertise in a wide range of areas across malignant and nonmalignant hematology, particularly in acute myeloid leukemia and stem cell and regenerative medicine, filled a great need and served our readership well. Finally, we owe a great debt to Charles Quinn of Cincinnati Children’s Hospital Medical Center. With his deep knowledge of sickle cell disease and thalassemia, Charles provided ASH and its members with precise and steadfast coverage of these increasingly vital topics. Four new contributing editors have been appointed to fill the vacancies left by the departures of Drs. Koury, Johnson, Becker, and Quinn. Register for the 2016 ASH Meeting on Lymphoma Biology The ASH Meeting on Lymphoma Biology will take place June 18-21 at The Broadmoor in Colorado Springs, Colorado. This meeting will bring together experts from around the world to discuss the latest breakthroughs in basic and translational lymphoma research, address current challenges in the field and steps to address them, and promote efforts to accelerate the development of new therapeutic strategies. The event spans four days and features didactic sessions, abstract presentations, interactive workshops, and panel discussions. For registration fees, speaker information, and more, please visit www.hematology.org/lymphoma-biology. Remember to register online by the advance registration deadline of May 27. Learn More about the New ASH Medical Educators Institute This new program provides hematologists who are new to medical education with a “boot camp” for teaching techniques, medical education scholarship, and trainee and program evaluation. Topics that will be discussed include educational research design in hematology, use of technology in medical education, adding value to your institution as a hematology educator, small group instruction, and the ins and outs of promotion and tenure. ASH will subsidize participation in the program by covering costs of travel, lodging, and meals. For additional information, visit www.hematology.org/ educators/4692.aspx. Dr. Omar Abdel-Wahab is an assistant attending physician on the leukemia service at Memorial Sloan-Kettering Cancer Center and a member of the Human Oncology and Pathogenesis Program. His laboratory is focused on the functional understanding of genetic alterations in patients with chronic myeloid and lymphoid leukemias. One of his main areas of interest is in understanding the biological and therapeutic significance of epigenetic and transcriptional alterations in patients with leukemia. He also serves on the editorial board of Blood. Dr. Michael DeBaun is professor of pediatrics and medicine, JC Peterson Endowed Chair in Pediatrics, vice chair of clinical and translational research in pediatrics, and the founder and director of the Vanderbilt-Meharry Center for Excellence in Sickle Cell Disease at Vanderbilt University School of Medicine. He is an internationally recognized physician-scientist whose research has resulted in fundamental advances in the genetics of cancer predisposition syndromes and the epidemiology and optimal treatments of stroke and lung disease in sickle cell disease. Dr. DeBaun has mentored numerous medical and graduate students and postdoctoral fellows, several of whom have gone on to receive multiple investigator-initiated federal grants and foundation awards. Dr. DeBaun is an elected member of the American Society for Clinical Dr. Michael R. DeBaun Investigation, the Association of American Physicians, the Institute of Medicine of the National Academy of Sciences, and the American Association for the Advancement of Science. In 2014 he was honored by ASH with the Ernest Beutler Lecture and Prize in Clinical Science. Dr. Paul Moss is professor of hematology and director of medical research at the University of Birmingham, UK. He is also chair of the Infections & Immunity Board at the Medical Research Council, and previously served as Chair of the Cancer Research UK Clinical and Translational Research Committee. Professor Moss has a clinical interest in lymphoproliferative and immunological disorders. His research program focuses on translational immunology within cancer, transplant, and viral disorders. He is author of Essential Haematology, one of the most popular international textbooks on hematology. Dr. Sioban Keel Speakers for the 2016 Meeting on Hematologic Malignancies Have Been Announced The 2016 ASH Meeting on Hematologic Malignancies will take place September 15-17 at the Fairmont Chicago, Millennium Park, in Chicago, Illinois. Hear the top experts in hematologic malignancies discuss the latest developments in clinical care and answer some of your most challenging patient care questions. There will be lectures on topics including leukemia, lymphoma, myelodysplastic syndromes, myeloma, and myeloproliferative neoplasms. For more information about the meeting and to see the full list of sessions and speakers, visit www.hematology.org/malignancies. Follow Blood on Twitter! Stay up to date with Blood, the official journal of ASH, and the most cited peer-reviewed publication in the field of hematology. Follow the journal on Twitter through the handle @BloodJournal. The Hematologist: ASH NEWS AND REPORTS Dr. Omar Abdel-Wahab Dr. Sioban Keel is a clinician-scientist at the University of Washington in Seattle. Her research centers on defining the Dr. Paul Moss phenotypic spectrum and genetic and molecular mechanisms regulating hematopoiesis and marrow failure in inherited bone marrow failure syndromes and inherited predisposition to leukemia and myelodysplastic syndromes. She brings research expertise in the molecular and cellular events that control red blood cell development, which synergizes with her active clinical practice. Dr. Keel cares for adult patients with inherited and acquired marrow failure, intrinsic red blood cell disorders, and unexplained cytopenias at the Seattle Cancer Care Alliance, and both directs and attends on the inpatient hematology consult service at the University of Washington. We look forward to having Omar, Michael, Paul, and Sioban lend their unique viewpoints regarding the molecular underpinnings of leukemia, hemoglobinopathies, immunotherapeutics, and marrow failure states, respectively. The benchtop, clinical, and translational interests of The Hematologist board of Contributing Editors mirror the education, research, and patient care missions of ASH — malignant and non-malignant hematology, pediatric disease, genomic/precision medicine, stem cell biology, hematopathology, and global health. Through our popular Diffusion articles, Ask the Hematologist, and Mini Review pieces, as well as multimedia platforms such as podcasts, our goal is share the dynamic developments in our field while speaking to the broad demographics of our Society. We are always interested in readers’ ideas so that our content can best serve the voices and passions of ASH’s membership. — Jason Gotlib, MD, MS, Editor-in-Chief Save the Date for the 2016 International Highlights of ASH Highlights of ASH provides a summary of the top hematology research presented at the 57th annual meeting in Orlando, to help improve patient management and care strategies. Look out for this year’s International Highlights of ASH: • Latin America: April 29-30 – Natal, Brazil • Asia-Pacific: March 5-6 – Brisbane, Australia For more information, visit www.hematology.org/highlights. 3 57th ASH Annual Meeting Wrap-Up (Cont. from page 1) by Dr. Andrew Zelenetz demonstrated what happens when an inhibitor of the PI3 Kinase pathway, idelalisib, is added to bendamustine and rituximab (BR). In a randomized, double-blind, placebo-controlled phase III study, the threedrug combination showed an impressive improvement in progression-free and overall survival over BR alone. In that same session, Dr. Stephen Stilgenbauer presented results from a phase II study, which used a BCL-2 inhibitor (venetoclax; ABT-199), in patients with del(17p) relapsed or refractory CLL, also with impressive results in this notoriously challenging subset. Multiple myeloma (MM), which was long known as a specialty of therapeutic nihilism, has become a poster child for rapid translation of molecular discoveries into the clinic. In 2015, the FDA approved four agents for the disease, panobinostat, ixazomib, daratumumab, and elotuzumab, each of which takes advantage of a different mechanistic vulnerability of the myeloma cell. At this year’s meeting, attendees were presented with numerous new studies that incorporated these agents either alone or in combination with established therapies. For example, Dr. Saad Usmani presented combined results of two studies that treated a total of 148 patients with late-stage MM with daratumumab, a monoclonal antibody to CD138, for an overall response rate of 31 percent. In the LBA session, the first in-human results using chimeric-antigen receptor (CAR) T-cells that target the B-cell maturation antigen in patients with advanced MM were presented. Dr. Syed Abbas Ali led the study, which showed similar types of toxicities that have been observed with anti-CD19 CAR T-cells (e.g., cytokine release syndrome) and impressive antimyeloma activity, including clearance of bone marrow plasma cells, and a stringent complete remission at the highest dose level. Targeted therapy is beginning to reach the myeloid world as well. Long held out as “too heterogeneous” for a targeted approach, the last two ASH annual meetings have demonstrated the important role that inhibitors of the constitutively activated FLT3 receptor play in the treatment of acute myeloid leukemia (AML). During the Plenary Scientific Session, Dr. Richard Stone revealed the important findings of the RATIFY study, a CALGB/Alliance effort that took years of work in accrual and logistical management. This study randomly assigned patients (ages 18 to 60 years) with newly diagnosed, FLT3-mutated (ITD or TKD) AML to 7+3 alone or in conjunction with the FLT3/multikinase inhibitor, midostaurin. The study showed that addition of midostaurin improved the event-free and overall survival of patients (whether censored or uncensored for transplantation), with this genetically defined subgroup of AML. These data pave the way for drug approval, and may herald an end to the four-decade period of relative stasis in the field of AML therapeutics. The momentum is not limited to areas of malignant disease. Since the discovery of thrombopoietin (TPO) more than 20 years ago, numerous biologic insights have been made regarding its interaction with its receptor c-mpl. This signaling pathway’s role in megakaryocyte production and regulation of platelet mass has been therapeutically exploited, leading to drug approvals of the TPO mimetics romiplostim and eltrombopag in patients with idiopathic thrombocytopenic purpura. TPO also has an established role in regulating hematopoietic stem cells, which led Drs. Cynthia Dunbar and Neal Young of the National Institutes of Health (NIH) to first evaluate its efficacy in patients with refractory severe aplastic anemia (SAA). This year, presenting results of a NIH–led phase II study, Dr. Danielle Townsley outlined the benefits of the TPO agonist eltrombopag on count recovery and response rates when added to up-front immunosuppressive therapy for patients with SAA (see Dr. Tracy George’s Year’s Best article for a more in-depth review of this subject). of therapies. Researchers elegantly demonstrated how control over the gene for fetal hemoglobin is exerted by the transcription factor leukemia/lymphoma–related factor (LRF)/ZBTB7A. The next step is to determine whether one can safely modulate LRF’s usual suppression of fetal hemoglobin to mitigate the clinical consequences of sickle cell disease. Similarly, the first in vitro evidence on how to modulate the spliceosome in myeloid malignancies was presented by Dr. Stanley ChunWei Lee on behalf of the laboratory of Dr. Omar Abdel-Wahab at Memorial Sloan Kettering Cancer Center. For the myriad blood cancers with driver mutations in the spliceosome, such progress bodes well for future therapies. Recognizing the challenges of keeping up with changes in the diseases we treat, in the last several years ASH has added several additional in-depth sessions that cut across diseases. This year, there were two well-attended Friday scientific workshops: one on myeloid diseases and the other on hematology and aging. On Saturday, there was a special interest session on newly approved drugs, shedding light on the right time and place to utilize drugs like blinotumumab, panobinostat, and idarucizumab. Attendees even had an hour-long educational session on social media and Twitter, and the many ways these ubiquitous technologies might be productively used by physicians and patients. We will never know, limited in perspective as we are by time, just what these past few years mean in the whole of our profession’s trajectory. However, I’m sure that I’m not alone in being grateful to have the opportunity to treat patients during a period “punctuated” by a breakneck pace of approvals of rationally designed therapeutics borne from the knowledge and tools of precision medicine. Thank You for Participating in the 2015 ASH Foundation Run/Walk! The 2015 ASH Foundation Run/Walk, which took place during the 57th ASH Annual Meeting, marked another big sprint toward success! For the third consecutive year, a wave of support from corporate sponsors as well as the dedication and enthusiasm of meeting attendees helped ASH reach 1,200 registered run/walk participants, while the foundation raised more than $90,000 to help fund programs in research, career development, and quality care and education. The final race results were as follows: Dr. Jordan Zwick, Top Male 5K Dr. Kinjal Parikh, Top Female 5K Dr. Chris Gregory, Top Male 3K Dr. Molly Hein, Top Female 3K Team Janssen Oncology had the highest number of participants as well as the highest team fundraising total, while Dr. Linda Burns achieved the highest fundraising total among individual donors. To see all results and to view the leaderboard, visit www.hematology.org/runwalk. ASH appreciates the generosity of all participants and donors and looks forward to next year’s Run/Walk, taking place December 4, 2016, in San Diego, California. The ASH Foundation thanks the 2015 Run/Walk Sponsors Seattle Genetics, Gilead Sciences, Incyte Corporation, and Freeman. To learn more and to donate to the ASH Foundation, visit www.hematology.org/Foundation. The Plenary Scientific Session also highlighted biologic and molecular discoveries that may pave the way for the next wave 4 The Hematologist: ASH NEWS AND REPORTS T H E H E A D L I N E S F R O M H E M A T O L O G I S T A D V O C A T E Washington End of 2015 Sees Research Advocacy Victory: Congress Provides $2 Billion Increase for NIH ASH Continues Advocacy to Ensure Patient Access to Safe and Effective Hematologic Drugs After partisan disputes about “policy riders,” ranging from the defunding of Planned Parenthood to changes to the President’s refugee resettlement program due to the current situation with ISIS/L and Syria, Congress finally reached an agreement in mid-December to fund federal programs and agencies, including the National Institutes of Health (NIH), through the remainder of fiscal year (FY) 2016. While oral and patient self-administered forms of chemotherapy have become more prevalent, and represent the standard of care for many types of cancers, they are covered differently than intravenous drugs, leaving many patients responsible for unsustainable, high monthly co-payments. The final funding bill, known as an “omnibus,” avoided a government shutdown and contained very good news for NIH: Advocacy efforts by ASH and the biomedical research community were successful in gaining a significant increase in funding for the agency. Under the terms of the agreement, NIH will receive $32.084 billion in FY 2016, an increase of approximately $2 billion (6.6%) over FY 2015 levels. The agreement also fully funds the Obama Administration’s Precision Medicine Initiative at $200 million. Additionally, the bill maintains FY 2015 funding levels for the numerous blood programs within the National Center on Birth Defects and Developmental Disabilities (NCBDDD) at the Center for Disease Control and Prevention’s (CDC’s) Division of Blood Disorders, which had seen drastic cuts in recent years. With 2015 now behind us, it’s time to take a look at some of the advocacy and policy initiatives that were important to hematology and to the ASH membership throughout the year. In addition to advocating for raising NIH funding levels, ASH also advocated for expanding access to safe and effective hematologic drugs and supporting physician payment. 2015 was also a time of heightened attention to patients with sickle cell disease and sickle cell trait. For additional information about these initiatives and all of ASH’s 2015 advocacy highlights, visit the Policy News section of the ASH website at www.hematology. org/Advocacy/Policy-News. ASH will continue its advocacy efforts on issues of importance to hematology research and practice throughout 2016. The Society needs the help of all ASH members to bring these issues to the attention of the U.S. Congress and other U.S. governmental agencies. Members of the ASH Grassroots Network receive action alerts and information about issues in which they indicate interest. At times, Grassroots Network members are also invited to represent hematology in activities such as visits to Capitol Hill, with NIH leadership, and with other regulatory agencies. To learn more about how you can participate in ASH’s advocacy efforts, visit the ASH website at www.hematology.org/ Advocacy, or contact ASH Legislative Advocacy Manager Tracy Roades at troades@ hematology.org. ASH Submits Comments in Response to Proposed Rulemaking on the “Common Rule” The Obama Administration released a Notice of Proposed Rulemaking (NPRM) to modernize, and strengthen the Federal Policy for the Protection of Human Subjects, otherwise known as the “Common Rule.” By way of background, in 2011, the Obama administration published an Advance Notice of Proposed Rulemaking (ANPRM), “Human Subjects Research Protections: Enhancing Protections for Research Subjects and Reducing Burden, Delay, and Ambiguity for Investigators,” to seek more information on how the Common Rule might be improved and revised to be more effective. The current NPRM proposal, which was published in the Federal Register on September 8, 2015, incorporates the feedback received from the ANPRM. The proposed rule is designed to streamline federal oversight of human subjects protections while reducing administrative burden, delay, and confusion for researchers. Once promulgated, the regulations would impact every research discipline funded by every federal agency, as well as clinical trials, regardless of funding source. As part of the Patients Equal Access Coalition (PEAC), ASH has advocated for legislation in the U.S. House of Representatives and the U.S. Senate (H.R. 2739/S. 1566, the Cancer Drug Coverage Parity Act) to ensure that cancer patients have equality of access (and equality of insurance coverage) to all approved anticancer regimens including, but not limited to, oral and intravenous drugs. Several ASH committees, as well as members of the ASH Advocacy Leadership Institute, advocated for the legislation throughout 2015 and secured the support of a number of members of Congress. The sponsors of the legislation in both the House and Senate remain committed to the issue and are working to urge committees in both houses to hold hearings, with the ultimate goal of passing the bills before the conclusion of the 114th Congress in December 2016. Visit the ASH Advocacy Center at www.hematology.org/TakeAction to send an email to your Senators and Representative urging them to support the Cancer Drug Coverage Parity Act. Although only federal legislation will ensure coverage for all cancer patients, 40 states plus the District of Columbia have passed legislation to limit patient out-of-pocket costs for oral anticancer medications. ASH has supported legislative efforts at the state level as well, and will continue to work with stakeholders and advocacy groups to support ongoing legislative efforts in a number of additional states in 2016, including Michigan, Tennessee, Alabama, North Carolina, and Pennsylvania. If you live in one of these states and are interested in working with ASH to help ensure your patients have affordable access to oral chemotherapy drugs, please contact ASH Legislative Advocacy Manager Tracy Roades at troades@hematology.org. NIH Unveils FY 2016-2020 Strategic Plan In mid-December 2015, NIH released the NIH-Wide Strategic Plan, Fiscal Years 2016–2020: Turning Discovery Into Health, a detailed plan that seeks to ensure the agency remains well positioned to capitalize on new opportunities for scientific exploration and address new challenges for human health. Developed after hearing from hundreds of stakeholders and scientific advisers, and in collaboration with leadership and staff of NIH’s Institutes, Centers, and Offices (ICOs), the plan is designed to complement the ICOs’ individual strategic plans that are aligned with their congressionally mandated missions. The plan focuses on four essential, interdependent objectives that will help guide NIH’s priorities over the next five years as it pursues its mission of seeking fundamental knowledge about the nature and behavior of living systems and applying that knowledge to enhance health, lengthen life, and reduce illness and disability. Over the next five years, NIH leadership will evaluate the agency’s progress in meeting the objectives laid out in the strategic plan, which will be a living document that will be open to refinements throughout its life cycle. The complete strategic plan can be found on the NIH website at www.nih.gov/sites/default/ files/about-nih/strategic-plan-fy2016-2020-508.pdf. One of the most fundamental changes in the Common Rule as proposed in the NPRM is the inclusion of biospecimens in the definition of human subjects research. The focus of the NPRM is to require informed consent for research involving biospecimens in all but a limited number of circumstances. The consent would not need to be obtained for each specific study using the biospecimen, but instead would be obtained through broad consent for future unspecified research. ASH solicited feedback on the NPRM from the ASH Committee on Government Affairs and the Committee on Scientific Affairs, and submitted final comments to the government on January 6, 2016. The Society’s complete comments may be found on the ASH website at www.hematology.org/Advocacy/Testimony. At the time of publication, it is unclear when a final rule will be published. The Hematologist: ASH NEWS AND REPORTS 5 What We Carried on Christmas (Cont. from page 1) studying my face for clues about good or bad news. Reading microexpressions is part of his training. Paul carries the unflinching faith that he’ll dodge another bullet. He visualizes a military retirement, lounging at his beachside home, out from the shadows and cured of AML. In this future, he’ll make the choice to sport a buzz cut, despite it occasionally reminding him of the time when nurses carried away clumps of his hair. Olivia is a 32-year-old blonde with television good looks who came in carrying a new quilt of bruises. She and her husband, owner of a private equity firm, live in an 8,000-square-foot home in Atherton. They are warm and soft-spoken. Their two girls, ages three and six, are angelic clones of their mother. Photos of the kids and their crayon drawings blanket the walls of her hospital room. When the resident and first-year fellow first spied her D-dimer of >20,000 ng/mL, fibrinogen of 42 mg/dL, platelet count of 19 × 109/L, and white blood cell count of 77 × 109/L, they understandably carried apprehension and urgency. I felt the same. They heard of the head bleeds; I managed them; our APL patients died of them. We started ATRA and successfully FISHed for t(15;17). Olivia steadied her shaky voice; she carried guilt, fear, and many questions about things she was afraid to ask since she first heard the word “leukemia.” “I dyed my hair,” she said. “Did this cause my leukemia?” “No,” I firmly replied. “Six months ago I went vegan.” I almost cut her off. “No connection,” I replied. She inspected her bruises. She was unconvinced that she wasn’t to blame. Tears welled in her eyes. “Am I going to give this to my kids?” she asked. “No. None of this is your fault. This is an acquired blood cancer. You can’t pass this on to your children,” I comforted her. We commenced a protocol for high-risk APL and reassured her that she has an excellent chance of being cured. However, we all knew that she wasn’t out of the woods. A year ago, I lost a mother of three young kids to relapsed acute lymphocytic leukemia. Soon after, her husband reconnected with me. While he was thankful and trying to move on, Olivia’s case reminded me that I hadn’t. I still carried an insidious melancholy that bubbled to the surface. It hung on to my conscience the way dried silicone gel sticks to jeans despite repeated washings. I felt that this was a good time for bargaining. I rationalized that if all creatures are equal in God’s eyes, maybe he would agree to a zero-sum arrangement: Olivia for the deer. I turned to her husband to make sure there would be no last-minute hiccups: “Do you drive a Tesla?” Commentary: Our patients remind us daily of what we are fighting for. While there may be “eight million stories in the naked city,”1 we are privileged to be witnesses to a few thousand of them during our careers. In some cases, we can extend patients’ quantity and quality of life so that new epilogues and second chances can be written. 2015’s Year’s Best in Hematology is a subjective list that highlights the achievements of our profession. Our choices mark time and allow different arcs of progress to reveal themselves. However, these choices are most relatable and personal when we can identify specific patients who are beneficiaries of these breakthroughs. Olivia’s promising outlook reflects a narrative of incremental progress in APL throughout the past 30 years. I remain hopeful for Paul. Genomic studies are helping to inform druggable pathways for different subsets of patients with AML. Separately, a day before Christmas, a man with a white blood cell count greater than 100 × 109/L walked into our emergency department. He left a day later with a diagnosis of chronic phase CML, a TKI prescription, and unexpected hope. The transformative success of CML therapy could not have been fleshed out nor appreciated in a single Year’s Best article. I am curious to see how studies of clonal hematopoiesis, myeloma antibodies/immunotherapy, techniques to enhance stem cell engraftment, and the other Year’s Best selections featured herein pay dividends for our patients over the long haul. I will let you know when I am on service again during Christmas 2025. From Jules Dassin’s “The Naked City” 1 6 RAN KI NG S FROM TH E H E MATOLOGI ST R EAD E R SU RVEY 1) Anti-CD19 CAR T-cells for refractory DLBCL 2) Antibodies and immunotherapy for multiple myeloma 3) Reversal agents for direct oral anticoagulants 4) Age-related clonal hematopoiesis in normal individuals 5) Reprogramming of Ph+ ALL cells into nonleukemic macrophages 6) PET-directed therapy for early Hodgkin lymphoma 7) Novel mechanisms of regulation of blood production 8) Boosting hematopoietic stem cell engraftment 9) Perioperative bridging anticoagulation and atrial fibrillation 10) Mutation order and myeloproliferative neoplasms 11) Biologic insights into malaria infection and resistance 12) Practice-defining trials: fresher blood and IVC filters 13) New therapeutic frontiers in sickle cell disease 14) Optimizing maintenance therapy in ALL 15) Somatic mutations in aplastic anemia Reprinted with permission from Nat Rev Drug Discov. 2013;12:229-243. This ranking reflects the results of a survey in which readers of The Hematologist scored several topics from “most influential” to “least influential.” The following articles reflect the top choices of the Editor-in-Chief and individual Contributing Editors. The Hematologist: ASH NEWS AND REPORTS Clonal Hematopoiesis: The Seeds of Leukemia or Innocuous Bystander? PAMELA S. BECKER, MD, PhD Professor of Medicine, Division of Hematology, Institute for Stem Cell and Regenerative Medicine and Center for Cancer Innovation, University of Washington, Seattle, WA The topic of age-related clonal hematopoiesis in normal individuals emerged as a compelling story in late 2014 and dominated 2015 as a subject hematologists are still grappling to understand. It has become clear that in some individuals, these somatic clones might not always remain quiescent or harmless. Instead, they may contribute to clonal expansion and overt development of myeloid neoplasms with the acquisition of additional cooperating mutations. One year ago, in the January/February 2015 Year’s Best issue of The Hematologist, Dr. Ravi Majeti authored the article titled “Pre-Leukemic Hematopoietic Stem Cells in Human Acute Myeloid Leukemia.” He highlighted the seminal findings, published concurrently by three groups,1-3 that some of the typical recurrent mutations found in acute myeloid leukemia (AML) could also be found in the peripheral blood of patients without a prior diagnosis of hematologic disease. Dr. Majeti raised the question of whether these individuals could be followed with the goal of detecting overt disease earlier, allowing for early treatment and/or prevention. The studies by Dr. Siddhartha Jaiswal,1 Dr. Giulio Genovese,2 and Dr. Mingchao Xie3 and their respective colleagues established that these acquired mutations occurred with normal aging and were akin to precursor conditions such as monoclonal gammopathy of undetermined significance (MGUS) or monoclonal Figure B-cell lymphocytosis (MBL). A Analysis of mutations in 12,380 individuals in a Swedish study2 revealed that 10 percent of those older than 65 years had such mutations, compared with 1 percent younger than 50 years. The most frequent mutations in this study and in a similar study of 17,182 individuals in the United States and abroad1 were in the DNMT3A, ASXL1, and TET2 genes. Mutations in the genes JAK2, TP53, SF3B1, CBL, and SRSF2 were less common. Longitudinal follow-up of several cohorts revealed that individuals with clonal hematopoiesis exhibited an increased risk for development of hematologic cancers and all-cause mortality. In 2015, we saw that these “seeds” could remain dormant, in a state of “clonal hematopoiesis of indeterminate potential (CHIP).”4 CHIP is defined as at least 2 percent variant allele frequency (VAF) of somatic mutations known to be associated with hematopoietic neoplasms, but without fulfilling diagnostic criteria for the malignancy (e.g., MDS or AML).4 There is a 0.5 to 1 percent risk of progression to overt malignancy per year (Figure), with increased rates in patients with a higher VAF of the somatic mutation. Instead of remaining dormant, such clones may demonstrate opportunistic tendencies. In patients undergoing chemotherapy, clones may The Hematologist: ASH NEWS AND REPORTS expand under the selective pressure of treatment and contribute to the development of therapy-related MDS or AML (t-MDS/t-AML).5 Historically, it was believed that chemotherapy and radiation led to therapy-related hematologic cancers because of increased numbers of mutations induced by treatment. However, contrary to this dogma, Dr. Terrence Wong and colleagues’ analysis5 of t-AML patient samples showed that there was not an increased number of mutations compared with de novo AML. Moreover, the same AML-associated mutations could be detected long before the diagnosis of cancer, and resistant clones simply expanded after treatment of the cancer.5 For example, in one patient with Hodgkin lymphoma, two TP53 mutations were detected in leukapheresis samples at a VAF of 0.5 percent six years prior to development of t-AML, and both TET2 and NUP98 mutations subsequently arose as potential driver mutations, only detectable later at the time when the leukemia was diagnosed. (ICUS or IDUS, respectively) who do not meet diagnostic criteria for MDS. And what do we tell the otherwise normal individual who is referred to our clinic with one or more “hits” uncovered on a myeloid gene panel that should not have been ordered in the first place? We have much to learn ourselves before we can confidently guide patients through this maze of genetic complexity. Notably, two of the three most commonly observed mutated genes in normal individuals, DNMT3A and TET2, were also found to be the most frequent mutations that failed to clear by day 30 after induction chemotherapy for AML. Patients in whom these mutations persist exhibit a worse outcome, even in complete remission.6 Clearly, these mutations are not always innocuous. It will be our task as hematologists to contextualize the prognostic importance of these molecular abnormalities, not only patients with MDS or AML, but also in individuals with mild cytopenias or dysplasia of unknown significance 4. Steensma DP, Bejar R, Jaiswal S, et al. Clonal hematopoiesis of indeterminate potential and distinction from myelodysplastic syndromes. Blood. 2015;126:9-16. Dr. Becker indicated no relevant conflicts of interest. 1. Jaiswal S, Fontanillas P, Flannick J, et al. Age-related clonal hematopoiesis associated with adverse outcomes. New Engl J Med. 2014;371:2488-2498. 2. Genovese G, Kähler A, Handsaker RE, et al. Clonal hematopoiesis and blood-cancer risk inferred from Blood DNA sequence. New Engl J Med. 2014;371:2477-2487. 3. Xie M, Lu C, Wang J, et al. Age-related mutations associated with clonal hematopoietic expansion and malignancies. Nat Med. 2014;20:1472-1478. 5. Wong TN, Ramsingh G, Young AL, et al. Role of TP53 mutations in the origin and evolution of therapy-related acute myeloid leukaemia. Nature. 2015;518:552-555. 6. Klco JM, Miller CA, Griffith M, et al. Association between mutation clearance after induction therapy and outcomes in acute myeloid leukemia. JAMA. 2015;314:811-822. Model of Clonal Expansion and Clonal Evolution from Normal Hematopoeisis to Myelodysplasia and Myeloid Leukemia Clonal hematopoiesis of indeterminate potential (CHIP) as a precursor state for hematologic neoplasms. The figure depicts a model for evolution from normal hematopoiesis to CHIP and then, in some cases, to myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML). Hematopoietic progenitor cells or stem cells commonly acquire mutations throughout the human lifespan; most of these are passenger mutations that have no consequence for hematopoiesis. Certain mutations, however, confer a survival advantage to the mutated cell and its progeny and allow clonal expansion. Serial acquisition of mutations in an expanded clone can lead to a disease phenotype and ultimately, morbidity and mortality. CHIP can also directly progress to AML without an intervening MDS stage, and CHIP can progress to other conditions such as myeloproliferative neoplasms or lymphoid neoplasms. The majority of patients with CHIP will never develop an overt neoplasm, and patients will eventually die of unrelated causes. From Steensma et al. Blood. 2015;126:9-16, with permission. 7 or double refractory multiple myeloma (MM): 54767414MMY2002 (Sirius). J Clin Oncol. 2015;33:LBA8512. Novel Drugs Push the Envelope in Multiple Myeloma ANDREW J. YEE, MD, 1 ELIZABETH O’DONNELL, MD, 2 AND NOOPUR S. RAJE, MD 3 1. Instructor in Medicine, Harvard Medical School, Center for Multiple Myeloma, Massachusetts General Hospital Cancer Center, Boston, MA 2. Instructor, Massachusetts General Hospital Cancer Center, Harvard Medical School, Boston, MA 3. Associate Professor of Medicine, Harvard Medical School; Director of the Multiple Myeloma Center at Massachusetts General Hospital Cancer Center, Boston, MA The year 2015 has been truly remarkable for the treatment of multiple myeloma (MM). The first oral proteasome inhibitor, ixazomib, is now approved for the treatment of MM. Data from the Tourmaline-MM1 study presented at the 57th ASH Annual Meeting demonstrated the benefit of ixazomib when combined with lenalidomide and dexamethasone in relapsed and/or refractory MM, with improvement in progression-free survival (20.6 months vs. 14.7 months for patients receiving lenalidomide and dexamethasone) and without significant toxicity.1 While there have been continued advances in novel drugs for MM, this has easily been the year where immuno-oncology and monoclonal antibodies (MoABs) have stolen the spotlight. A few days prior to and after ixazomib approval, two new MoABs were approved by the U.S. Food and Drug Administration (FDA): daratumumab and elotuzumab. Daratumumab, a MoAB directed against CD38, was approved for the treatment of MM patients who have received at least three prior lines of therapy including a proteasome inhibitor and an immunomodulatory agent, or those who are refractory to both these classes of drugs (i.e., double-refractory). In a pivotal phase I/II study, daratumumab demonstrated striking effectiveness as a single agent in heavily pretreated patients including doublerefractory patients.2 The overall response rate in this group was 36 percent, including two patients who had a complete response and two patients with a very good partial response. Furthermore, responses were durable, and 65 percent of patients who had a response were free of progression at one year. These observations were corroborated by the Sirius study, in a similar refractory MM population.3 At the 2015 ASH Annual Meeting, we heard about early-stage trials combining daratumumab with lenalidomide4 or pomalidomide,5 with encouraging data demonstrating deeper responses. These studies will inform use of daratumumab as a partnering agent in the evolving MM treatment landscape. Elotuzumab is a humanized recombinant IgG1 MoAB that targets signaling lymphocyte activation molecule (SLAMF7), also known as CS1 (CD2-subset-1). In a phase III study, ELOQUENT-2, the combination of elotuzumab, lenalidomide, and dexamethasone was compared with lenalidomide and dexamethasone in patients with relapsed disease.6 Patients with one to three prior lines of therapy were eligible to participate. This trial enrolled 646 patients with a median of two prior lines of therapy. A significant proportion had highrisk cytogenetics (32% with del[17p] and 9% with t[4;14]). The elotuzumab-containing arm had superior progressionfree survival (19.4 months vs. 14.9 months in the control group; p<0.001), and the overall response rate was also higher (79% vs. 66%; p<0.001). Based on these findings, elotuzumab was approved in combination with lenalidomide and dexamethasone in patients with one to three prior lines of treatment. These studies with elotuzumab and daratumumab are among the first to show promising activity for MoAB therapy in MM, and they will be practice-changing additions to our arsenal against MM. Cellular therapies such as chimeric antigen receptor-T (CAR-T) cell therapy are now being actively studied in MM. Although still in the early days of development, the promising data presented this year with the use of CD19-directed CAR-T cells in a heavily pretreated MM patient with nine prior lines of therapy provide proof of concept for the promise of this strategy.7 During the Late-Breaking Abstracts session at the 2015 ASH Annual Meeting, early data on a series of MM patients undergoing CAR-T cell therapy directed against a different target, B-cell maturation antigen, may translate into the use of personalized cellular therapy with the potential for long-term disease control.8 Continuing the theme of immuno-oncology, data from solid tumors highlight the successful paradigm of using checkpoint inhibitors to target inhibitory mechanisms of the immune system. Nivolumab and pembrolizumab, MoABs targeting the programmed death 1 checkpoint, have shown activity in melanoma and lung cancer and were recently approved by the FDA. In relapsed MM, trials studying the use of immune checkpoint blockade with MoABs such as pembrolizumab are showing promise when the drug is combined with lenalidomide9 or pomalidomide.10 Exploring the full potential of MoABs in the treatment of myeloma is an area of great interest for 2016. 8 Drs. Yee, O'Donnell, and Raje indicated no relevant conflicts of interest. 1. Moreau P, Masszi T, Grzasko N, et al. Ixazomib, an investigational oral proteasome inhibitor (PI), in combination with lenalidomide and dexamethasone (IRd), significantly extends progression-free survival (PFS) for patients (Pts) with relapsed and/or refractory multiple myeloma (RRMM): the phase 3 tourmaline-MM1 study (NCT01564537). Blood. 2015;126:727. 2. Lokhorst HM, Plesner T, Laubach JP, et al. Targeting CD38 with daratumumab monotherapy in multiple myeloma. N Engl J Med. 2015;373:1207-1219. 3. Lonial S, Weiss BM, Usmani SZ, et al. Phase II study of daratumumab (DARA) monotherapy in patients with ≥ 3 lines of prior therapy 4. Plesner T, Arkenau HT, Gimsing P, et al. Daratumumab in combination with lenalidomide and dexamethasone in patients with relapsed or relapsed and refractory multiple myeloma: updated results of a phase 1/2 study (GEN503). Blood. 2015;126:507. 5. Chari A, Lonial S, Suvannasankha A, et al. Open-label, multicenter, phase 1b study of daratumumab in combination with pomalidomide and dexamethasone in patients with at least 2 lines of prior therapy and relapsed or relapsed and refractory multiple myeloma. Blood. 2015;126:508. 6. Lonial S, Dimopoulos M, Palumbo A, et al. Elotuzumab therapy for relapsed or refractory multiple myeloma. N Engl J Med. 2015;373:621-631. 7. Garfall AL, Maus MV, Hwang WT, et al. Chimeric antigen receptor T cells against CD19 for multiple myeloma. N Engl J Med. 2015;373:1040-1047. 8. Ali SA, Shi V, Wang M, et al. Remissions of multiple myeloma during a first-in-humans clinical trial of T cells expressing an anti-B-cell maturation antigen chimeric antigen receptor. Blood. 2015;126:LBA-1. 9. San Miguel J, Mateos MV, Shah JJ, et al. Pembrolizumab in combination with lenalidomide and low-dose dexamethasone for relapsed/refractory multiple myeloma (RRMM): keynote-023. Blood. 2015;126:505. 10. Badros AZ, Kocoglu MH, Ma N, et al. A phase II study of anti PD-1 antibody pembrolizumab, pomalidomide and dexamethasone in patients with relapsed/refractory multiple myeloma (RRMM). Blood. 2015;126:506. Flipping a Switch: Advances in DOAC Reversal in 2015 ADAM CUKER, MD, MS Assistant Professor of Medicine, Assistant Professor of Pathology & Laboratory Medicine, Director, Penn Comprehensive Hemophilia and Thrombosis Program; Clinical Director, Penn Blood Disorders Center; Associate Director, Penn-CHOP Blood Center for Patient Care and Discovery, University of Pennsylvania, Philadelphia, PA The direct oral anticoagulants (DOACs) dabigatran, rivaroxaban, apixaban, and edoxaban, are associated with reduced major bleeding, intracranial hemorrhage, and fatal bleeding compared with warfarin.1 Nevertheless, reversal of these agents may be warranted in patients who have serious bleeding or who require an emergent procedure. At this time last year, there was no standard of care for emergent DOAC reversal. Hospital committees grappled with low-quality evidence to define institutional protocols for reversal. Clinicians lacked guidance on how to manage patients. The best available options, prothrombin complex concentrate and activated prothrombin complex concentrate, were supported primarily by data from animal and healthy volunteer studies, and raised concerns about thrombotic risk. No data were available on the efficacy and safety of these agents in DOAC-treated patients with a clinical indication for emergent reversal.2 2015 was a year of great forward momentum on the reversal front. In the RE-VERSE AD study, dabigatran-treated patients who have serious bleeding or who require an emergent procedure are treated with idarucizumab, a monoclonal antibody fragment that binds and neutralizes dabigatran. An interim analysis of the first 90 patients (51 with bleeding, 39 requiring a procedure) showed normalization of coagulation tests within minutes of infusion. Among patients requiring an emergent procedure, 92 percent were judged to have normal surgical hemostasis. Clinical outcomes, including cessation of bleeding, were more difficult to assess in the group with serious hemorrhage. Idarucizumab was well tolerated. Only one patient had a thrombotic event within 72 hours of administration.3 Based on the favorable results of RE-VERSE AD, idarucizumab was approved in the United States and Europe in autumn of 2015 and is now the standard of care for emergent dabigatran reversal in jurisdictions where it is available. Not far behind idarucizumab in development is andexanet alfa, a modified recombinant factor Xa molecule that lacks catalytic and membrane-binding activity but retains the ability to bind and neutralize factor Xa inhibitors. In the recently published ANNEXA-A and ANNEXA-R trials, healthy volunteers taking apixaban and rivaroxaban, respectively, were randomized to receive andexanet or placebo. Rapid and profound reduction in anti-Xa activity was observed within minutes of bolus administration of andexanet. A continuous infusion following the bolus was necessary to sustain the reversal effect. Andexanet was well tolerated. Plasma samples from some subjects showed increased D-dimer and prothrombin 1+2 fragments.4 The clinical relevance of this observation is unknown. ANNEXA-4 (ClinicalTrials.gov Identifier: NCT02329327), an ongoing phase IIIb-IV study, will provide data on the efficacy and safety of andexanet in patients taking a factor Xa inhibitor who have serious bleeding. Other DOAC-reversal agents are in earlier stages of development. Ciraparantag is a small, positively-charged molecule that binds to, and neutralizes factor Xa inhibitors through noncovalent interactions. It corrected coagulation tests in healthy edoxaban-treated volunteers within minutes of administration.5 Factor XaI16L, a zymogen-like variant of factor Xa, and superFVa, a variant of factor Va engineered to resist inactivation by activated protein C, both rapidly reversed the anticoagulant effect of rivaroxaban in vitro and in animal studies.6,7 A remarkable feature of DOAC reversal agents is the rapidity with which they normalize coagulation parameters. Hours are required for full reversal of the anticoagulant effect of warfarin by vitamin K or plasma. Correction is achieved more quickly with prothrombin complex concentrate, but 40 percent of patients have a persistently elevated INR (≥ 1.4) 30 minutes after infusion.8 In contrast, DOAC-reversal agents correct coagulation tests within minutes of administration, suggesting their potential to turn off anticoagulation almost instantly, like flipping a light switch. Whether the effect of DOAC reversal agents on laboratory endpoints leads to improved clinical outcomes remains to be proven. Continued progress in the field of DOAC reversal in 2016 and beyond is expected to shed light on this and other crucial questions. Clinical observations from RE-VERSE AD and ANNEXA-4 will teach us more about the efficacy and safety of idarucizumab and andexanet alfa, respectively, in patients with DOAC-associated bleeding. Real world data on idarucizumab will be reported and recommendations for its use will be incorporated into clinical practice guidelines and institutional protocols. Dr. Cuker indicated no relevant conflicts of interest. 1. Chai-Adisaksopha C, Crowther M, Isayama T, et al. The impact of bleeding complications in patients receiving target-specific oral anticoagulants: a systematic review and meta-analysis. Blood. 2014;124:2450-2458. 2. Siegal DM, Cuker A. Reversal of target-specific oral anticoagulants. Drug Discov Today. 2014;19:1465-1470. 3. Pollack CV Jr, Reilly PA, Eikelboom J, et al. Idarucizumab for Dabigatran Reversal. N Engl J Med. 2015;373:511-520. 4. Siegal DM, Curnutte JT, Connolly SJ, et al. Andexanet alfa for the reversal of factor Xa inhibitor activity. N Engl J Med. 2015. DOI: 10.1056/NEJMoa1510991. [Epub ahead of print]. 5. Ansell JE, Bakhru SH, Laulicht BE, et al. Use of PER977 to reverse the anticoagulant effect of edoxaban. N Engl J Med. 2014;371:2141-2142. 6. Thalji NK, Ivanciu L, Jasuja R, et al. Zymogen-like FXa is a potent bypassing agent for reversal of direct FXa inhibitors in vivo. Blood. 2014;124:582. 7. Bhat V, Gale AJ, Griffin JH, et al. Reversal of novel oral anticoagulant (NOAC)-induced bleeding in mice by engineered superfactor Va. Blood. 2014;124:695. 8. Sarode R, Milling TJ Jr, Refaai MA, et al. Efficacy and safety of a 4-factor prothrombin complex concentrate in patients on vitamin K antagonists presenting with major bleeding: a randomized, plasmacontrolled, phase IIIb study. Circulation. 2013;128:1234-1243. The Hematologist: ASH NEWS AND REPORTS Using Interim PET to Direct Therapy for Early Hodgkin Lymphoma: Results from the Trials ANN LACASCE, MD, 1 AND PETER JOHNSON, MD 2 1. Program Director, Fellowship in Hematology/Oncology; Assistant Professor of Medicine, Lymphoma Program, Dana-Farber Cancer Institute, Boston, MA 2. Professor of Medical Oncology, Cancer Research UK Centre, University of Southampton, UK In 2015, the vast majority of patients with Hodgkin lymphoma (HL) will be cured of their disease using standard treatments. Despite high rates of long-term disease control, late therapy-related toxicities (most importantly, secondary malignancies and cardiovascular disease) remain a source of significant morbidity and mortality among survivors. In 2015, results from a trio of important risk-adapted trials in early-stage HL were reported on, designed to maintain efficacy while reducing the risk of late effects. All three trials took the approach of using interim positron emission tomography (PET) scanning to determine how well treatment was working, allowing escalation of therapy for individuals in whom the initial response appeared poor, or reduction of therapy for those with an early metabolic response. In the RAPID trial from the United Kingdom (Figure 1), patients with newly diagnosed stage IA and IIA nonbulky HL underwent PET imaging after three cycles of ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine).1 PET-positive patients received an additional cycle of ABVD followed by IFRT. Patients who were PET-negative, defined by a Deauville score of 1 or 2 (fluorodeoxyglucose [FDG] uptake was less than the mediastinal blood pool) were randomized to no further therapy versus involved-field radiation therapy (IFRT) to 30Gy. The randomization was designed to exclude a 7 percent or greater difference in three-year progression-free survival (PFS) between the two arms. After two cycles of ABVD, 75 percent of patients were PET-negative, and 420 patients were ultimately randomized. Although the 95 percent CI for the difference in risk crossed 7 percent (−8.8% to +1.3%), the outcome in both arms was excellent, with a three-year PFS of 94.6 percent in the radiotherapy (RT) arm versus 90.8 percent in the observation arm. There was no difference in overall survival.1 RAPID trial schema ELIGIBILITY Histologically confirmed classic HL Stage IA/IIA by CT scan No mediastinal bulk or B symptoms No prior treatment PET +ve ABVD x 3 cycles Response PET scan R PET –ve CALGB/Alliance 50604 trial schema ELIGIBILITY Histologically confirmed classic HL Stage I/II, A or B No mediastinal bulk No prior treatment PET +ve ABVD x 2 cycles Response PET scan PET –ve Preliminary results of EORTC/LYSA/FIL H10 trial schema the U.S. Intergroup study Figure 3 (Figure 2) of risk-adapted therapy in patients H10 with nonbulky stage I 2 ABVD PET 1 ABVD + INRT 30 Gy (+ 6 Gy) F and II classical HL were presented at the 57th ASH Annual Meeting – 2 ABVD in December.2 In this 2 ABVD PET study, Deauville scores + 2 escBEACOPP + INRT 30 Gy (+ 6 Gy) of 1 to 3 (FDG uptake less than liver) were considered negative. Patients who were PETH10 2 ABVD PET 2 ABVD + INRT 30 Gy (+ 6 Gy) negative after two cycles U of ABVD received two more cycles without RT. Individuals who – 4 ABVD were PET-positive were 2 ABVD PET treated with two cycles + 2 escBEACOPP + INRT 30 Gy (+ 6 Gy) of escalated BEACOPP (doxorubicin, bleomycin, vinblastine, and dacarbazine) followed by of interim PET imaging as a biomarker in patients with IFRT to 30Gy. The group treated 164 patients, 91 percent of early-stage HL. Overall, they suggest that escalation of whom were interim PET-negative. With a median follow-up chemotherapy for PET-positive patients is effective, and of two years, the estimated 3-year PFS was 92 percent they provide evidence to support the idea of omitting RT in the PET-negative arm. In the PET-positive group, the for those with an early metabolic response. This does not estimated three-year PFS was 66 percent.2 This figure may seem to compromise overall survival, though there is a seem lower than in the PET-positive arm of RAPID, where small increase in the risk of recurrence. It is notable that in one further cycle of ABVD followed by 30Gy IFRT yielded all three studies the proportion of patients dying from HL 87 percent PFS at five years, but it is important to note that was less than 3 percent overall, emphasizing the need to the “PET-positive” group in that trial contained 90 patients take a holistic view of the data and not focus exclusively on with a Deauville score of 3, from a total of 145, which is disease control. likely to have increased the PFS substantially. R R During the 13th International Conference on Malignant Lymphoma in June 2015, results from the H10 study by the European Intergroup (EORTC/LYSA/FIL; Figure 3) were presented.3 Patients with stage I and II disease were randomized between PET-adapted therapy and standard treatment with ABVD for three cycles (favorable patients per the EORTC Figure 1 criteria: age 50 years or older, large mediastinal mass, B symptoms and erythrocyte sedimentation rate [ESR] > 30, ESR > 50 without B symptoms, > 2 nodal sites of involvement) 4th cycle ABVD or four cycles (unfavorable then IFRT patients) plus involved-node RT (INRT) to 30Gy. In the PETadapted arm, PET-negative patients (Deauville score of IFRT 30 Gy 1-3) received a total of four cycles (favorable) or six cycles (unfavorable) of ABVD. Interim PET-positive patients No further received intensified therapy treatment (NFT) with escalated BEACOPP for two cycles followed by INRT to 30Gy. In total, 1,950 patients were enrolled, and interim PET was positive in 11 percent and 22 percent for Figure 2 the favorable and unfavorable groups, respectively. With a median follow-up of 4.5 years, among 361 patients who were PET-positive, the 5-year PFS was 91 percent 2 escBEACOPP in those on the PET-adapted then IFRT arm who received BEACOPP, compared with 77 percent in the standard ABVD group. There was also a trend toward improved overall survival in the PET-adapted arm: 96 percent compared with 89 percent (p=0.062).3 ABVD x 2 cycles No RT The Hematologist: ASH NEWS AND REPORTS Many hematologists/oncologists and patients alike are willing to accept a small increased likelihood of disease recurrence to avoid the risk of secondary cancers and cardiovascular disease associated with RT. To identify patients who may benefit from intensified or novel approaches, interim PET, and possibly molecular predictors, such as the recently described gene expression signature, may be useful tools.4 Additionally, with the availability of novel agents with impressive activity, such as brentuximab vedotin and nivolumab, therapeutic options for high-risk patients will continue to evolve, and trials of these approaches are already underway. Drs. LaCasce and Johnson indicated no relevant conflicts of interest. 1. Radford J, Illidge T, Counsell N, et al. Results of a trial of PETdirected therapy for early-stage Hodgkin’s lymphoma. N Engl J Med. 2015;372:1598-1607. 2. Straus D, Pitcher B, Kostakoglu L, et al. Initial results of US Intergroup trial of response-adapted chemotherapy or chemotherapy/radiation therapy based on PET for non-bulky stage I and II Hodgkin lymphoma (HL) (CALGB/Alliance 50604). Blood. 2015;126:578. 3. Raemaekers J. Early FDG-PET adapted treatment improved the outcome of early FDG-PET positive patients with stages I/ II Hodgkin lymphoma (HL): final results of the randomized Intergroup EORTC/LYSA/FIL H10 trial. Presented at the 13th International Conference on Malignant Lymphoma, June 17-20, 2015, Lugano, Switzerland. 4. Scott DW, Chan FC, Hong F, et al. Gene expression-based model using formalin-fixed paraffin-embedded biopsies predicts overall survival in advanced-stage classical Hodgkin lymphoma. J Clin Oncol. 2013;31:692-700. These three studies demonstrate the utility 9 Acquired Aplastic Anemia: Somatic Mutations and Eltrombopag Take the Spotlight MELODY K. HARRISON, MD, 1 AND TRACY I. GEORGE, MD 2 1. Hematopathology Fellow, University of New Mexico School of Medicine, Albuquerque, NM 2. Associate Professor of Pathology; Hematopathology Division Chief and Hematopathology Fellowship Director, University of New Mexico and TriCore Reference Laboratories, Albuquerque, NM Acquired aplastic anemia (AA) results from autoimmune destruction of hematopoietic progenitor cells, and a significant proportion of these patients develop a myelodysplastic syndrome (MDS) and/or acute myeloid leukemia (AML) as a late complication of their disease.1,2 Recent studies have demonstrated clonal hematopoiesis (CH) in the majority of cases of AA, including pediatric patients and those in whom MDS and AML do not ultimately develop, and these clones are generally detectable early in the course of the disease.1,2 The distribution and types of mutations (frame-shift, nonsense, and splice site changes) identified in AA show significant overlap with those observed in association with MDS and AML but with a much lower allelic burden in the former.1,2,3 Comparison of diagnostic samples with those obtained after six months of immunosuppressive therapy shows no significant difference in the numbers of different mutations present; the levels, however, are significantly increased after treatment.1 The specific genes involved in AA show significant differences from, but also a good deal of overlap with, MDS and AML. Alterations of BCOR, BCORL1, and PIGA are more prevalent in AA, while JAK2, RUNX1, TET2, and TP53 are less so. Mutations of DNMT3A and ASXL1 are noted in both.1,2 Dr. Tetsuichi Yoshizato and colleagues2 suggest discrete mechanisms of clonal selection at play in these processes. In other words, CH in general seems to originate from a small clone present early in the disease course, and its evolution is dependent on the progressive accumulation of additional mutations and subsequent clonal selection.1-4 Thus, CH appears to signify leukemogenesis at a very early stage. It is generally accepted that stem cells in all tissues, including the bone marrow, tend to accumulate somatic mutations throughout life, most of which are of no clinical significance. Occasionally though, a disease-initiating alteration occurs.4-6 Recent studies suggest that clones with mutations in certain genes seem to have a survival advantage in bone marrow failure.1,2 This seems to occur through either escape from immune-mediated destruction, as with loss-of-function mutations in HLA class I genes, from a relative increase in proliferation, or both.1 Neal Young, and colleagues from the National Institutes of Health (NIH) showed that eltrombopag elicited a 44 percent response rate, including multilineage responses, in patients with severe AA (sAA) refractory to immunosuppression.8 This led to U.S. Food and Drug Administration approval of eltrombopag in this patient population. In the Late-Breaking Abstracts session, Dr. Danielle Townsley, on behalf of colleagues from the same NIH group, presented data that extended these initial results. She presented data from a phase II trial of 88 treatment-naïve sAA patients, where eltrombopag was added to horse antithymocyte globulin (ATG) and cyclosporine (CSA). Eltrombopag was administered starting at day 14 (due to potential concerns for liver toxicity) for six months (cohort 1) or three months (cohort 2), or from day 1 for six months (cohort 3). The combination was well tolerated, and no increased marrow fibrosis was observed. Among the three treatment cohorts, the combination of eltrombopag with ATG + CSA yielded overall response rates at three and six months of 80 percent and 85 percent, respectively; complete response rates were 28 percent and 34 percent at these time points. The addition of eltrombopag yields response rates that are 20 percent to 30 percent higher than historical rates with ATG + CSA alone in sAA (p < 0.001). Clonal cytogenetic evolution occurred in seven of 88 patients, similar to prior rates observed with standard immunosuppression. No baseline factors were predictive of outcome. 2015 was a breakthrough year for AA. The marriage of clinical breakthroughs with a more sophisticated understanding of the mutational landscape of AA is certain to catalyze robust translational research opportunities moving forward. Additional investigation is needed to correlate both baseline mutation status and temporal Drs. Harrison and George indicated no relevant conflicts of interest. 1. Babushok DV, Perdigones N, Perin JC, et al. Emergence of clonal hematopoiesis in the majority of patients with acquired aplastic anemia. Cancer Genet. 2015;208:115-128. 2. Yoshizato T, Dumitriu B, Hosokawa K, et al. Somatic mutations and clonal hematopoiesis in aplastic anemia. N Engl J Med. 2015;373:35-47. 3. Genovese G, Kähler AK, Handsaker RE, et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N Engl J Med. 2014;371:2477-2487. 4. Xie M, Lu C, Wang J, et al. Age-related mutations associated with clonal hematopoietic expansion and malignancies. Nat Med. 2014;20:1472-1478. 5. Jaiswal S, Fontanillas P, Flannick J, et al. Age-related clonal hematopoiesis associated with adverse outcomes. N Engl J Med. 2014;371:2488-2498. 6. Steensma DP, Bejar R, Jaiswal S, et al. Clonal hematopoiesis of indeterminate potential and its distinction from myelodysplastic syndromes. Blood. 2015;126:9-16. 7. Zeigler FC, de Sauvage F, Widmer HR, et al. In vitro megakaryocytopoietic and thrombopoietic activity of c-mpl ligand (TPO) on purified murine hematopoietic stem cells. Blood. 1994;84:4045-4052. 8. Olnes MJ, Scheinberg P, Calvo KR, et al. Eltrombopag and improved hematopoiesis in refractory aplastic anemia. New Engl J Med. 2012;367:11-19. 9. Townsley DM, Dumitriu B, Scheinberg P, et al. Eltrombopag added to standard immunosuppression for aplastic anemia accelerates count recovery and increases response rates. Blood. 2015;126:LBA-2. Progression of Disease, Patient NIH075 Figure Progression of Disease, Patient NIH075 Immune-mediated destruction of HSCs An understanding of the genes involved can provide some insight into the mechanism of disease. For instance, the most commonly detected mutation in these series results in a loss of function of DNMT3A, which appears to impede stem cell differentiation and results in accumulation of the abnormal cells within the bone marrow. TET2 mutations (also one of the most frequently identified) facilitate selfrenewal and give rise to a competitive growth advantage. It is worth noting that candidate driver mutations, alterations that occur in a subset of genes known to be drivers of hematopoietic neoplasms, are relatively rare among young patients with AA and seem to be enriched in older individuals.3,5 The differences in involved genes are not only of interest for understanding the evolution of disease, but some have also been shown to have prognostic implications. For instance, BCOR, BCORL1, and PIGA mutations generally portend a better response to immunosuppressive therapy and improved overall survival, while abnormalities of ASXL1, CSMD1, DNMT3A, RUNX1, and TP53 tend to herald inferior treatment response and shortened survival. In a similar vein, clones with aberrancies in the former (good prognostic) group of genes tend to remain small or diminish in size over time, whereas clones involving mutations of the latter (poor prognostic) group are more likely to grow in size and progress to MDS and/or AML. changes in clonal architecture (Figure) with disease natural history and response to immunosuppression and hematopoietic stem cell transplantation. Recovery ASXL1 TSC22D1 YTHDF2 FZD8 OR51A4 TET2 BCOR COG1 SETBP1 EHD2 Onset of Aplastic Anemia Base- 1 line 2 3 4 5 6 7 8 9 10 11 12 Years Chronologic history of clonal evolution from the onset of disease to the last follow-up in Patient NIH075. Each mutated gene is depicted in the representative cells. The vertical axis indicates the absolute volume of the clones. Representative mutations in each clone are also shown. From Yoshizato T, Dumitriu B, Hosokawa K, et al. Somatic mutations and clonal hematopoiesis in aplastic anemia. N Engl J Med. 2015;373:35-47. On the clinical front, data presented at the 57th ASH Annual Meeting continue to highlight the promise of the eltrombopag in patients with severe AA. The rationale for using such agents is based on the expression of c-mpl, the receptor for thrombopoietin, on hematopoietic stem and progenitor cells, and the finding that the addition of recombinant thrombopoietin expands the pool of these cells in culture.7 In 2012, Drs. Cynthia Dunbar and 10 The Hematologist: ASH NEWS AND REPORTS Practice-Defining Clinical Trials in Nonmalignant Hematology DAVID GARCIA, MD Professor of Medicine, Division of Hematology, University of Washington, Seattle, WA During 2015, two important myths from the nonmalignant hematology world were busted (to use a verb from the title of a recently popular television series, “Myth Busters”). In both cases, the myth was based on biological theory and observational data from uncontrolled studies, while the definitive evidence emerged from one or more prospective, randomized controlled trials. The first myth consists of the idea that patients who are anticoagulated for so-called high-risk (but hemodynamically stable) pulmonary embolism (PE) might benefit from the placement of a retrievable inferior vena cava (IVC) filter. Indeed, the general notion that more aggressive interventions (over and above anticoagulant therapy) might benefit high-risk PE patients is not new. For example, more than one randomized controlled trial of thrombolysis plus anticoagulation versus anticoagulation alone has been conducted in this population. For some clinicians, the retrievable IVC filter, an intervention with no bleeding risk that theoretically could protect an already tenuous right ventricle from the next embolism, seemed even more attractive, especially after an observational study in PE patients documented an association between IVC filter placement and improved survival.1 Thankfully, a group of investigators was able to carry out a prospective, randomized controlled trial in which patients with highrisk PE were randomly assigned to have (or not have) a retrievable IVC filter placed; all participants received anticoagulation.2 The patients who received a filter had no improvement on any of the efficacy outcomes, and a handful experienced some of the complications known to occur after IVC filter placement such as access site hematoma, filter thrombosis, and retrieval failure. This study, by Dr. Patrick Mismetti and colleagues, should serve as a reminder to all hematologists that, when administered with careful monitoring at a high-quality center, anticoagulation therapy is as effective as more expensive and potentially hazardous treatment options, sometimes considered for patients with high-risk pulmonary embolism. I suspect that Drs. D.W. Barritt and Stanley C. Jordan, the authors who performed the landmark randomized trial of heparin vs. no heparin in patients with PE more than 50 years ago,3 would be pleased to learn that the therapy they tested remains the gold standard in 2015. The second myth to be challenged was that, among patients who require red cell transfusions, those who receive “fresher” units of packed red blood cells (RBCs) fare better than patients who receive RBC units of “standard” age. This idea that fresher blood might be better has a basis in biology4 and observational data.5 However, in 2015, two randomized trials involving a cumulative total of more than 3,500 patients6,7 failed to demonstrate any evidence of a mortality (or other clinical) benefit among those who received “fresher” RBCs. In one study, the mean ages of RBCs were six versus 22 days, and in the other, the median ages were seven versus 28 days. The studies involved critically ill adult patients and patients (12 years or older) undergoing complex cardiac surgery; all RBCs administered were leukoreduced. Like any data from a clinical trial, the evidence provided by these large trials can certainly be criticized: What if more RBC units older than 35 days had been tested? Should the variable of interest (age of RBCs) have been treated as continuous rather than categorical (dichotomous)? Those reservations notwithstanding, the sheer size of these trials, along with the degree to which the findings agree with previous controlled studies, indicates that if there is any benefit from RBCs with storage time longer than 28 days, it is small, and the additional costs of providing “fresher” blood to all patients would be very difficult to justify. Dr. Garcia indicated no relevant conflicts of interest. 1. Kucher N, Rossi E, De Rosa M, et al. Massive pulmonary embolism. Circulation. 2006;113:577-582. 2. Mismetti P, Laporte S, Pellerin O, et al. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism: a randomized clinical trial. JAMA. 2015;313:1627-1635. 3. Barritt DW, Jordan SC. Anticoagulant drugs in the treatment of pulmonary embolism. A controlled clinical trial. Lancet. 1960;1:1309-1312. 4. Zimring JC. Established and theoretical factors to consider in assessing the red cell storage lesion. Blood. 2015;125:2185-2190. 5. Wang D, Sun J, Solomon SB, et al. Transfusion of older stored blood and risk of death: a meta-analysis. Transfusion. 2012;52:1184-1195. 6. Lacroix J, Hébert PC, Fergusson DA, et al. Age of transfused blood in critically ill adults. N Engl J Med. 2015;372:1410-1418. 7. Steiner ME, Ness PM, Assmann SF, et al. Effects of red-cell storage duration on patients undergoing cardiac surgery. N Engl J Med. 2015;372:1419-1429. New Therapeutic Frontiers in Sickle Cell Disease CHARLES T. QUINN, MD, MS Associate Professor of Clinical Pediatrics, University of Cincinnati College of Medicine and Cincinnati Children’s Hospital Medical Center, Cincinnati, OH A panoply of potential new therapies for sickle cell disease (SCD) has emerged in just the past five years. Pharmaceutical companies are now actually interested in SCD. Many sickle cell centers now run more than one clinical trial at the same time, and even decline participation in others because of limited resources and competing enrollment. While this may be unsurprising to many readers of The Hematologist, especially those who treat patients with hematologic malignancies, this is a strange, new world for the sickle cell community. This column highlights three publications from 2015 that reported new therapeutic frontiers in different stages of development: gene therapy, antiadhesive therapy, and modulation of coagulation. Gene therapy for SCD has always been ‘just around the corner.’ Now it is actually here for humans, albeit in an extremely limited and experimental basis. Five individuals with SCD have undergone some form of gene transfer therapy to date, but the durability of clinical benefit of the current generation of gene therapy methods remains to be demonstrated. Even so, next-generation gene therapy techniques are already being studied in preclinical models. An ideal gene therapy for SCD would avoid the problems of insertional mutagenesis and difficulty achieving proper spatiotemporal expression of a transgene by permanently correcting the sickle mutation in situ. In an effort to achieve this goal, Dr. Megan Hoban and colleagues used specifically engineered zinc-finger nucleases and a donor nucleotide template to effect cleavage of the β-globin locus and homology-directed repair of the sickle mutation in hematopoietic stem and progenitor cells (HSPCs).1 These modified HSPCs could engraft in immunodeficient mice and produce cells from multiple lineages. Moreover, gene-corrected CD34+ cells from the bone marrow of individuals with SCD could produce wild-type hemoglobin tetramers. Clearly, more work needs to be done until this gene correction technique is ready for studies in humans, including elimination of off-target cleavage and nonhomologous end joining. Different gene editing techniques (e.g., TALEN- and CRISPR-based systems) are The Hematologist: ASH NEWS AND REPORTS also being actively studied. So, while gene therapy for SCD is “already here,” even better gene therapy is “just around the corner.” prothrombin is a modifier of end-organ damage in SCD in mice and support the study of dabigitran and other direct thrombin inhibitors for the treatment of SCD. Until gene therapy delivers a universal cure, the painful vaso-occlusive episode (VOE) will remain a vexing therapeutic challenge. A number of studies have demonstrated a key role for intercellular adhesive interactions in the pathophysiology of vaso-occlusion, and several antiadhesive therapies are being tested for VOE. Among these is the pan-selectin inhibitor, GMI-1070, now known as rivipansel. Dr. Marilyn Telen and colleagues reported the results of a prospective, multicenter, randomized, placebo-controlled, double-blind, phase II study of 76 patients with VOE.2 Although the time to resolution of VOE was not statistically different between the groups, the medication appeared to be safe, and a secondary analysis showed a significant reduction in opioid usage in the GMI-1070 group. These results provided support for a phase III study of GMI-1070 that is currently recruiting (NCT02187003). GMI-1070 exemplifies the renewed optimism that exists for alternative therapeutic options beyond hydration, analgesics, and supportive care for VOE and related complications of SCD. While promising new therapies and cures for SCD such as these are hotly pursued and eagerly anticipated, we must not forget what we can do for our patients now: Prescribe hydroxyurea.4 Hydroxyurea decreases SCD-related morbidity and mortality and improves quality of life. It is effective and has very few serious side effects. Sadly, it is still not prescribed as broadly as it should be. Looking forward to 2016, we will certainly see expanded indications for hydroxyurea. In particular, the results of the TWiTCH Trial were presented at the Plenary Scientific Session of the 2015 ASH Annual Meeting but not published in time for this Year’s Best in Hematology.5,6 The TWiTCH trial demonstrated that hydroxyurea was not inferior to chronic transfusions for primary stroke prevention in select children with SCD. I predict that these practice-changing findings will top next year’s list. SCD is characterized by activation of the coagulation system and chronic inflammation. This knowledge has prompted a handful of trials of anticoagulant and anti-inflammatory therapies. None had resounding success, perhaps because these agents (e.g., heparins, corticosteroids) have targets that are too broad. As a specific therapeutic target for SCD, thrombin is attractive because it is both a central effector and regulator of coagulation and a key modifier of inflammation. Dr. Paritha Arumugam and colleagues demonstrated that targeted reduction of prothrombin levels, using both antisense oligonucleotides and genetic diminution techniques, significantly ameliorated vasoocclusion, vasculopathy, and inflammation in sickle cell mice.3 Importantly, these benefits were achieved with only a modest increase in the prothrombin time and without hemorrhagic complications. These findings indicate that 1. Hoban MD, Cost GJ, Mendel MC, et al. Correction of the sickle cell disease mutation in human hematopoietic stem/progenitor cells. Blood. 2015;125:2597-2604. Dr. Quinn indicated no relevant conflicts of interest. 2. Telen MJ, Wun T, McCavit TL, et al. Randomized phase 2 study of GMI-1070 in SCD: reduction in time to resolution of vaso-occlusive events and decreased opioid use. Blood. 2015;125:2656-2664. 3. Arumugam PI, Mullins ES, Shanmukhappa SK, et al. Genetic diminution of circulating prothrombin ameliorates multiorgan pathologies in sickle cell disease mice. Blood. 2015;126:1844-1855. 4. Quinn CT. Do not leave for tomorrow what you can do today. Pediatr Blood Cancer. 2015;62:1879-1880. 5. Quinn CT. TWiTCH: itching to find an alternative to transfusions for prevention of stroke in sickle cell anemia. The Hematologist. 2013;6:13. 6. Ware RE, Davis BR, Schultz WH, et al. TCD with transfusions changing to hydroxyurea (TWiTCH): hydroxyurea therapy as an alternative to transfusions for primary stroke prevention in children with sickle cell anemia. Blood. 2015;126:3. 11 Therapeutically Enhancing Stem Cell Engraftment JONATHAN HOGGATT, PhD Assistant Professor, Cancer Center and Center for Transplantation Sciences, Massachusetts General Hospital/Harvard Medical School, Boston, MA Hematopoietic stem cell transplantation is often the only curative treatment modality for a number of hematologic diseases. There are more than 50,000 bone marrow transplants performed each year worldwide. Despite this fact, there are virtually no therapies in clinic today to support or enhance the engraftment of transplanted stem and progenitor cells. In 2015, several high-profile studies were published, which have begun adding to the toolkit of potential therapies to enhance stem cell engraftment. One therapeutic option that is currently being explored is treating the stem cell graft ex vivo with 16,16-dimethyl prostaglandin E2 (dmPGE2)1 — a long-acting analogue of the naturally occurring prostaglandin, which is derived from arachidonic acid via the cyclooxygenase enzymes, COX1 and COX2 (Figure). Two articles in 2015 have now expanded the realm of manipulating arachidonic acid-derived eicosanoids to enhance stem cell engraftment. Work published from the laboratory of Dr. Leonard Zon utilized a novel competitive transplantation system in transparent zebrafish, allowing for direct visualization of stem cell engraftment.2 They screened 480 chemicals with known biologic activity for the ability to alter hematopoietic stem cells, and several hits targeted eicosanoids, including 11,12 epoxyeicosatrienoic acid (11,12EET) and 14,15-EET, which are derived from arachidonic acid via cytochrome P450 epoxygenases (Figure). Mouse bone marrow was treated ex vivo with 11,12-EET for four hours and then washed away (similar to the dmPGE2 protocol), prior to transplantation into lethally irradiated recipients. This short pulse with 11,12-EET resulted in enhanced homing and in increases in both short and long-term hematopoietic reconstitution. These studies highlight the broad role of eicosanoids in regulating stem and progenitor function, and they suggest yet another potential therapeutic strategy utilizing short, ex vivo pulses with small molecules to enhance engraftment. In the future it may be possible to treat a hematopoietic graft with a cocktail of various factors targeting multiple pathways leading to super enhancements. While the 11,12-EET strategy followed the aforementioned concept of an ex vivo pulse, a team of collaborators at Case Western and UT Southwestern utilized an approach of altering the environment within the recipient of a transplant.3 Many therapeutics that we have today, most notably nonsteroidal anti-inflammatory drugs (NSAIDs), focus on inhibiting COX enzyme activity to decrease PGE2 levels. However, as PGE2 enhances stem cell function, the authors evaluated methods to increase the natural levels of PGE2. They accomplished this enhancement with the small molecule SW033291, which inhibits 15-hydroxyprostaglandin dehydrogenase (15-PGDH), a key enzymatic step in the breakdown of PGE2 (Figure). When mice were treated with SW033291 prior to transplantation, there were enhancements to the microenvironment, including elevated stromal derived factor-1 (SDF-1), a chemoattractant and supportive molecule for stem cells, and the growth factor c-kit ligand (stem cell factor [SCF]). Additionally, there was improvement in stem and progenitor cell homing to the bone marrow niche, accelerated recovery of neutrophils and platelets, and enhanced survival in a limited cell transplantation assay. These studies outline a potential therapeutic strategy to augment engraftment by altering the recipient environment those cells are entering, rather than altering the stem cell graft itself. Figure Arachidonic Acid Cascade Arachidonic Acid NSAIDs Cyclooxygenases Lipoxygenases Cytochrome P450 epoxygenases Prostaglandin E2 Leukotrienes EETs 15-PGDH SW033291 Shown is a simplified version of the arachidonic acid cascade. After arachidonic acid is released by phospholipase A2, it can then be converted to numerous other eicosanoid molecules by a variety of enzymatic reactions. Cyclooxygenase enzymes convert arachidonic acid into thromboxanes, prostacyclins, and prostaglandins, notably Prostaglandin E2. These enzymes are the target of many nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen. Prostaglandin E2 is then rapidly degraded by 15-hydroxyprostaglandin dehydrogenase (15-PGDH), which is the target of the small molecule inhibitor SW033291. Arachidonic acid can also be converted into leukotrienes, many of which are mediators of allergy, and into the epoxyeicosatrienoic acids (EETs) by the cytochrome P450 epoxygenases. This past year has not only brought exciting new studies showing that stem cell engraftment can be enhanced by ex vivo manipulation of the hematopoietic graft, or by in vivo enhancement of the recipient environment, but also by simply harvesting the graft with enhancing protocols. Earlier this year in The Hematologist,4 we highlighted work from the Broxmeyer lab that demonstrated exposure to ambient air could lead to a phenomenon they termed “extraphysiologic oxygen shock/stress” or EPHOSS, which led to reductions in stem cell function.5 When bone marrow was harvested in the continuous presence of Cyclosporin A, there was a reversal of the deleterious effects of ambient air exposure, with significant increases in stem cell number and competitive transplantation. These results also extended to human cord blood samples harvested in Cyclosporin A. Given the recurring interest in stem cell expansion and ex vivo manipulation (i.e. gene therapy), the discovery of EPHOSS effects, and more importantly, strategies to mitigate the negative effects on stem cells, represented important contributions to therapeutic enhancement of stem cell engraftment in 2015. Dr. Hoggatt indicated no relevant conflicts of interest. 1. Cutler C, Multani P, Robbins D, et al. Prostaglandin-modulated umbilical cord blood hematopoietic stem cell transplantation. Blood. 2013;122:3074-3081. 2. Li P, Lahvic JL, Binder V, et al. Epoxyeicosatrienoic acids enhance embryonic haematopoiesis and adult marrow engraftment. Nature. 2015;523:468-471. 3. Zhang Y, Desai A, Yang SY, et al. Tissue regeneration: inhibition of the prostaglandin-degrading enzyme 15-PGDH potentiates tissue regeneration. Science. 2015;348:aaa2340. 4. Rasmussen HK, Hoggatt J. Hematopoietic stem cells should hold their breath. The Hematologist. 2015;12(5):9. 5. Mantel CR, O’Leary HA, Chitteti BR, et al. Enhancing hematopoietic stem cell transplantation efficacy by mitigating oxygen shock. Cell. 2015;161:1553-1565. Malaria: Progress in the Host-Pathogen Arms Race THERESA COETZER, PhD Co-Director of Wits Research Institute for Malaria; Associate Professor, University of the Witwatersrand, Johannesburg, South Africa The 2015 Nobel Prize in Physiology or Medicine was awarded to three scientists for their discoveries on novel therapies against parasitic infections. Youyou Tu from China was honored for isolating artemisinin, the active ingredient from the Chinese herb Artemesia annua, which rapidly kills malaria parasites. Artemisinin combination therapy is the current gold standard treatment for malaria, and it has had a major impact on diminishing the burden of the disease. Malaria parasites are transmitted to humans by female Anopheles mosquitoes, and, after initial replication in the liver, they invade and subsequently destroy red blood cells (RBCs), which triggers the clinical symptoms of the disease. The complex parasite lifecycle in both the human host and the mosquito vector has necessitated a multipronged approach in global efforts to eliminate this remarkably successful pathogen. Preventive measures, including the use of insecticide-treated bed nets and indoor residual spraying with insecticides, have been combined with rapid diagnostic test kits in order to detect malaria as early as possible. These interventions, followed by immediate and appropriate treatment of the patient, have contributed to a dramatic global decline in malaria since 2000 and to achievement of the United Nations’ Millennium Development Goal by 2015.1 12 Despite this progress, 3.2 billion people remain at risk of contracting malaria. According to the latest World Health Organization report,2 an estimated 214 million new cases and approximately 438,000 deaths were reported in 2015. SubSaharan Africa continues to bear the brunt of the disease, accounting for 88 percent of the morbidity and 90 percent of the mortality, mainly in children younger than five years. The gains that have been achieved are threatened by the development of insecticide resistance in African vector species and by the alarmingly rapid development and spread of drug-resistant parasites, which have rendered several antimalarial drugs useless. Resistance to artemisinin by Plasmodium falciparum, the most deadly of the five species of Plasmodium parasites that infect humans, has recently been detected in five countries in the Greater Mekong region. This threat has accelerated research into the biology of P. falciparum and its interaction with the human host, and has fueled efforts to develop new drugs and a vaccine. Several major advances have been reported this year, and results from four studies are highlighted here. In a multi-institutional collaboration3 led by Dr. Kasturi Haldar, the specific molecular target of artemisinin in early ring-stage P. falciparum was identified as phosphatidylinositol-3-kinase (PfPI3K). However, PfPI3K polymorphisms were not detected in all resistant strains, and previous genome-wide association studies (GWAS) revealed selective pressure on chromosome 13, in particular on the pfkelch13 gene. The mammalian orthologue is a substrate adaptor for an E3 ubiquitin ligase; the putative substrate binding domain of the parasite PfKelch13 protein has a characteristic kelch propeller domain, and mutations in this region correlated with artemisinin resistance. In an elegant series of biochemical and cell biology experiments, the researchers demonstrated that one of the most prevalent mutations, C580Y, inhibited the binding of PfKelch13 to PfPI3K, which decreased ubiquitination of the enzyme and limited subsequent proteasomal degradation, resulting in increased amounts of enzyme and its lipid product, phosphatidylinositol-3-phosphate (PI3P). It is hypothesized that artemisinin resistance is mediated by PIP3-induced amplification of downstream targets that are currently unknown. This study is important since it provides a tool to screen and monitor clinical parasite isolates for the presence of artemisinin resistance, and it identifies a target that can be exploited for novel drug development. The invasion of RBCs by P. falciparum is a complex process, and interactions between host receptors and parasite ligands The Hematologist: ASH NEWS AND REPORTS millenniumgoals/ne are not fully understood. Genetic manipulation experiments to identify host factors influencing susceptibility to infection have been hampered by the absence of a nucleus in mature erythrocytes. To overcome this challenge, Dr. Elizabeth Egan and colleagues4 exploited two recent technological advances of RNA interference and ex vivo production of RBCs to design a forward hematopoietic stem cell-based genetic screen. They identified CD55 or decay-accelerating factor (DAF) as an essential host receptor and verified their laboratory findings by demonstrating that RBCs from a patient lacking CD55 were refractory to invasion by P. falciparum. CD55 is a membrane-bound glycoprotein that regulates the complement system, and these findings suggest that the role of complement in parasite invasion and pathogenesis should be re-examined. The study also identifies CD55 as a potential target for the development of novel antimalaria therapeutics. P. falciparum is a highly virulent parasite that can cause severe disease, including cerebral malaria. Features that contribute to virulence include binding of infected RBCs to the microvasculature and also to other RBCs to form rosettes. These host-pathogen interactions are poorly understood. Dr. Mats Wahlgren and colleagues5 used molecular and cell biology approaches to demonstrate that P. falciparum expressed repetitive interspersed families of polypeptides (RIFINs) on the surface of infected RBCs and formed rosettes by preferentially binding to blood group A erythrocytes. RIFINs also mediated microvasculature sequestration by interacting with A antigens on endothelial cells. These findings indicate that RIFINs play a major role in the pathogenesis of severe malaria and that blood group A predisposes to the development of severe disease, which correlates with previous clinical studies on African children. This study highlights the impact of malaria on the human genome and suggests that RIFINs contributed to the evolutionary pressure that led to the emergence of the protective blood group O and the variable global distribution of human ABO blood groups. The development of a malaria vaccine has been actively pursued for several decades but has been an elusive and frustrating target. The RTS,S Clinical Trials Partnership published the final results6 of an individually randomized, controlled phase III trial on the most advanced malaria vaccine candidate RTS,S/AS01. More than 15,000 participants, including young children (ages 5 to 17 months) and infants (ages 6 to 12 weeks) were enrolled in seven sub-Saharan African countries representing different levels of malaria transmission. The vaccine was administered at months 0, 1, and 2, with a booster at 20 months. The results showed modest protection against clinical P. falciparum malaria throughout 48 months, with a vaccine efficacy of 36.3 percent in young children and 25.9 percent in infants, and illustrated the importance of the booster to sustain the protective effect. Recent recommendations from international expert committees who evaluated the trial are to conduct three to five real-world demonstration pilot studies with 200,000 African children each time over the next few years to assess the impact and feasibility of implementing the four-dose vaccine strategy. In conclusion, despite the major advances reported in these four studies, they have highlighted our lack of in-depth understanding of the complex interplay between the malaria parasite and its human host. Numerous challenges remain and it will require an enhanced effort not only by researchers, but also by political leaders and funders, to ensure that the current momentum is not lost in the battle against this formidable pathogen. Dr. Coetzer indicated no relevant conflicts of interest. 1. The Millennium Development Goals Report 2015. United Nations. Available at www.un.org/millenniumgoals/news.shtml. Accessed January 3, 2016. 2. Malaria World Report. World Health Organization. Available at www.who.int/malaria/publications/world_malaria_report/en/. Accessed December 22, 2015. 3. Mbengue A, Bhattacharjee S, Pandharkar T, et al. A molecular mechanism of artemisinin resistance in Plasmodium falciparum malaria. Nature. 2015;520:683-687. 4. Egan ES, Jiang RHY, Moechtar MA, et al. Malaria. A forward genetic screen identifies erythrocyte CD55 as essential for Plasmodium falciparum invasion. Science. 2015;348:711-714. 5. Goel S, Palmkvist M, Moll K, et al. RIFINs are adhesins implicated in severe Plasmodium falciparum malaria. Nat Med. 2015;21:314-317. 6. RTS,S Clinical Trials Partnership. Efficacy and safety of RTS,S/ AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet. 2015;386:31-45. A New Roadmap for Optimizing Thiopurine Therapy in Acute Lymphocytic Leukemia ELIZABETH RAETZ, MD, 1 AND JULIA MEYER, PhD 2 1. P rofessor in the Division of Pediatric Hematology/Oncology; Director of High-Risk Leukemia and Lymphoma Program, University of Utah/Huntsman Cancer Institute, Salt Lake City, UT 2. Postdoctoral Fellow, University of Utah School of Medicine, Salt Lake City, UT The treatment of childhood acute lymphocytic leukemia (ALL) has been a success story, with the majority of patients now achieving cure; however, there is still a steep learning curve with regard to our understanding of how to most effectively and safely deliver conventional chemotherapeutic drugs. The bulk of childhood ALL therapy is the approximately two-year maintenance phase, the backbone of which is daily administration of 6-mercaptopurine (6MP). Questions still remain regarding how best to fine tune dosing of 6MP in individual patients and how to enhance compliance with daily oral 6MP during the several-year trajectory of an ALL treatment course. Further, despite overall high cure rates for childhood ALL, some patients develop resistance to 6MP; efforts at early detection of resistance are underway, so preemptive changes can be made to avert relapse. 6MP has been a mainstay of ALL therapy for the past six decades; however, three seminal articles published in 2015 lent critical insights into why optimal delivery of this drug is critical to the success of patient outcomes. Expanding on prior studies, which have demonstrated that nonadherence to 6MP increases relapse risk,1 Dr. Smita Bhatia and colleagues reported their results from a large prospective multiyear study examining the effects of high intra-individual variability of 6MP exposure on the risk of relapse.2 The authors assessed adherence in 742 children throughout a six-month period during the maintenance phase of therapy on Children’s Oncology Group (COG) treatment regimens. The authors observed that patients with a mean 6MP adherence rate of less than 95 percent were at a 2.7-fold increased risk of relapse compared with those having 95 percent or greater adherence. Adherence was measured in this study using a special bottle cap with an electronic monitoring device to record the date and time of bottle opening for medication administration. The authors examined several other variables related to mediation adherence to determine their impact on relapse risk, including erythrocyte thioguanine (TGN) levels, 6MP dose intensity (number of prescribed 6MP doses divided by the number of planned protocol doses), thiopurine methyltransferase (TPMT) genotype, and absolute neutrophil count (ANC). Interestingly, dose intensity and TGN levels were not associated with the risk of relapse. Notably, however, among adherent patients, high intraindividual variability in TGN levels increased relapse risk by 4.4 fold. This variability in TGN levels was the result of varying 6MP dose intensity and drug treatment interruptions. in COG protocols, 6MP dose adjustments are made in an effort to target an ANC range of 1 to 1.5 × 109/L, and 6MP is held when the ANC and/or platelet count are lower than 0.5 × 109/L and 50 × 109/L, respectively. Once blood counts recover, 6MP is reintroduced at a reduced dose with incremental dose increases, as tolerated. Patients tend to experience fluctuations in their blood counts that require 6MP dosing modifications, and given the association of TGN variability and relapse, this raises the question of whether modifications to current dosing guidelines should be considered in an effort to reduce drug interruptions and maintain more consistency in TGN levels. The work by Dr. Bhatia and colleagues also ties in well with other influential reports this year describing a new host polymorphism impacting tolerance of 6MP and new discoveries on mechanisms of thiopurine resistance. While adherence to 6MP is key to minimizing relapse risk, understanding how inherited variants contribute to 6MP intolerance is also important so that consistent exposure can be maintained and excessive toxicity can be avoided. In early 2015, Dr. Jun Yang and colleagues identified a novel germline variant in the gene NUDT15, which was strongly associated with 6MP intolerance and which was most frequently found in patients of East Asian and Hispanic descent.3 The newly identified variant is hypothesized to lead to a loss-of-function phenotype for NUDT15, causing extensive DNA damage and cytotoxicity. Patients that were homozygous for the TT genotype only tolerated 8.3 percent of planned 6MP doses. This discovery, coupled with existing data on the role that TPMT variant alleles also play in 6MP intolerance,4 will help to identify a significant number of children spanning different racial and ethnic groups for individualized 6MP dosing. Since the first reports that relapse-specific acquired mutations in the gene NT5C2 cause overt resistance to 6MP,5,6 two new studies published in 2015 have helped to expand our knowledge of genes contributing to maintenance therapy resistance. Dr. Xiaotu Ma and colleagues showed that the prevalence of mutations in NT5C2 may be as high as 45 percent in patients with early ALL relapses, and further, that these mutations were often acquired in the founding relapse clone.7 They also observed that patients can acquire multiple mutations in NT5C2, albeit in different subclones, demonstrating the selective pressure on leukemia cells to evade 6MP cytotoxicity. Additionally, Dr. Benshang Li and colleagues reported that another mechanism of thiopurine resistance can occur through the acquisition of relapsespecific mutations in the gene PRPS1.8 PRPS1 is an enzyme involved in the de novo purine biosynthesis pathway, and These findings raise important questions about how best to the acquired mutations were shown to reduce nucleotide administer 6MP during ALL maintenance therapy. Presently, feedback inhibition, causing a reduction in the conversion of 6MP into its active metabolite. Mutations were found in 6.7 percent of the B-lineage Figure ALL samples examined and were mutually Strategies for optimizing the delivery exclusive of NT5C2 mutations. Taken of thiopurine therapy together, these studies suggest that resistance to 6MP is a commonly observed mechanism of ALL relapse. While continued advances in the field of pediatric ALL are envisioned with precision medicine initiatives and the development of new targeted agents, the improved utilization of conventional chemotherapy drugs also falls within the spirit of these efforts. The report by Dr. Bhatia and colleagues and the aforementioned studies published in 2015 converge on a central theme of employing different approaches to optimize 6MP delivery during ALL maintenance therapy (Figure). These studies raise important considerations for the development of future prospective ALL trials and suggest that measures to enhance adherence and reduce treatment interruptions will need to be carefully considered. In concert, prospective assessment for TPMT and NUDT15 variants to identify individuals at risk for 6MP (Cont. on next page) The Hematologist: ASH NEWS AND REPORTS millenniumgoals/news.shtml. Accessed January 3, 2016. 13 Clinical Implications of Novel Regulatory Mechanisms for Production of Platelets, Neutrophils, and Erythrocytes MARK J. KOURY, MD Professor of Medicine, Vanderbilt University, Nashville, TN Several 2015 publications involving mouse models that examined blood counts and underlying hematopoietic events have advanced our understanding of both steadystate and emergency production rates for platelets, neutrophils, and erythrocytes. These studies provided insights that were specific to each of the three bone marrow lineages. These newly identified regulatory mechanisms suggest potential new approaches for treating diseases that result in abnormal numbers of platelets, neutrophils, or erythrocytes. A newly described mechanism for rapid platelet production, which occurs in emergency situations such as low circulating platelet levels due to enhanced destruction or increased platelet numbers from intense inflammation or infection, is megakaryocytic rupture induced by interleukin-1α (IL1α).1 Sudden IL-1α–mediated release of larger-than-normal platelets increases production rates by more than an order of magnitude over the pro-platelet shearing mechanism of steady-state platelet production.1 Both of these release mechanisms require development of mature megakaryocytes located adjacent to the vascular sinuses of the marrow, a process regulated by thrombopoietin (TPO), the principal growth factor for megakaryocytes that is produced mainly by the liver. Aging of circulating platelets has been associated with desialylation of surface glycoproteins, which in turn leads to platelet removal from the circulation after binding by asialoglycoprotein receptors on hepatocytes.2 The bound asialoglycoprotein receptors in turn signal through the JAK2-STAT3 pathway inducing TPO transcription, thereby completing a feedback loop that maintains steadystate platelet numbers.2 Megakaryocyte rupture provides explanations for increased platelet size and rapid recovery, with potential overshoot thrombocytosis following correction of platelet destruction processes. The asialoglycoproteinmediated removal of aged platelets and JAK2-STAT3-linked production of TPO help explain thrombocytopenia associated with JAK inhibitor therapy and rapid normalization of platelet numbers after overshoot thrombocytosis. Both of these newly described mechanisms may allow for future approaches to treating thrombocytopenia with sequential TPO mimetics and inducers of megakaryocytic rupture. Despite brief intravascular life spans, neutrophils were found to age in the circulation in response to products of the gut microbiota that signal through Toll-like receptors and myeloid differentiation factor-88.3 The more aged neutrophils had increased tissue adhesiveness and proinflammatory activity, and their expanded population in the chronic inflammation of a murine model of sickle cell disease was reversed by antibiotic treatment of microbiome organisms.3 During acute inflammation or infection, the myeloid progenitor cell pool was shown to expand in response to interstitial reactive oxygen species (ROS) generated by phagocytic NADPH oxidase activity emanating from adjacent mature myeloid cells in the marrow.4 This ROS-mediated emergency granulopoiesis is related to PTEN oxidation/inactivation and does not involve granulocyte colony-stimulating factor (G-CSF).4 Therefore, it has therapeutic potential beyond that provided by G-CSF and granulocyte macrophage colony-stimulating factor (GM-CSF) to raise neutrophil counts in acute situations of increased demand such as sepsis. These new insights provide an opportunity to test two hypotheses: 1) whether antibioticmediated suppression of gut microbiota can improve chronic inflammatory states, and 2) whether pharmacologic manipulation of the ROS-PTEN pathway can improve emergency granulopoiesis in chronic granulomatous disease, in which defective myeloid NADPH oxidase activity increases susceptibility to bacterial infections. Transferrin receptor-2 (TFR2) plays a role in hepcidin transcription in liver when iron saturation of transferrin is increased. TFR2’s function in erythroid cells, where it had been shown to associate with erythropoietin (EPO) receptors, was not known. However, CBCs of mice with TFR2-deficient erythroid cells showed increased hemoglobin owing to increased numbers of RBCs that had decreased MCHs and MCVs, indicating that TFR2 restricts steady-state erythropoiesis and maintains normal RBC size during iron sufficiency, presumably by decreasing EPO responsiveness.5 In iron sufficiency therefore, TFR2 restricts both erythropoietic iron supply via hepcidin-mediated control of iron flux and erythropoietic use of iron. Conversely, in iron deficiency, instability of unbound TFR2 leads to increased iron absorption and flux via decreased hepcidin and increased EPO responsiveness of erythroid cells. The method by which increased EPO responsiveness coordinates with other regulators of erythropoiesis in iron deficiency (such as iron regulatory protein-1 (IRP-1) limiting EPO production and heme-regulated inhibitor (HRI) limiting hemoglobin synthesis) is unknown, but multiple levels of control are present in the erythropoietic response to this common cause of anemia. The emergency situation in anemia is tissue hypoxia, and the erythropoietic response to anemia is termed “stress erythropoiesis.” Renal EPO production has been extensively studied in stress erythropoiesis. However, beginning at the burst-forming unit-erythroid (BFU-E) stage and extending to the proerythroblast stage of differentiation, non-EPO mediators such as glucocorticoid hormones, stem cell factor, and bone morphogenetic protein-4, can expand erythroid progenitor cell populations without inducing differentiation. Glucocorticoid-induced expansion of BFU-Es was shown to involve a direct synergistic interaction between dexamethasone and peroxisome proliferator-activated receptor-α (PPAR-α),6 whereas expansion of EPO-dependent erythroid progenitors, colony-forming units-erythroid (CFU-Es) and proerythroblasts, did not involve PPAR-α, suggesting that other mechanisms are involved in glucocorticoid-mediated expansion of these later differentiation stages. From the clinical standpoint, enhancement of glucocorticoid-mediated erythropoietic activity by PPAR-α agonists6 indicates that, when steroidal side effects become problematic, PPAR-α agonists may allow reduced doses of glucocorticoids. Such agonists could be particularly useful in bone marrow failure syndromes such as Diamond-Blackfan anemia, in which glucocorticoids are the mainstay of treatment. Dr. Koury indicated no relevant conflicts of interest. 1. Nishimura S, Nagasaki M, Kunishima S, et al. IL-1α induces thrombopoiesis through megakaryocyte rupture in response to acute platelet needs. J Cell Biol. 2015;209:453-466. 2. Grozovsky R, Begonja AJ, Liu K, et al. The Ashwell-Morell receptor regulates hepatic thrombopoietin production via JAK2-STAT3 signaling. Nat Med. 2015;21:47-54. 3. Zhang D, Chen G, Manwani D, et al. Neutrophil ageing is regulated by the microbiome. Nature. 2015;525:528-532. 4. Kwak HJ, Liu P, Bajrami B, et al., Myeloid cell-derived reactive oxygen species externally regulate the proliferation of myeloid progenitors in emergency granulopoiesis. Immunity. 2015;42:159-171. 5. Nai A, Lidonnici MR, Rausa M, et al. The second transferrin receptor regulates red blood cell production in mice. Blood. 2015;125:1170-1179. 6. Lee HY, Gao X, Barrasa MI, et al. PPAR-α and glucocorticoid receptor synergize to promote erythroid progenitor self-renewal. Nature. 2015;522:474-477. I N (Cont. from previous page) intolerance so that their dosing can be refined, and periodic monitoring for the emergence of acquired resistance so that regimens could be modified to avert relapse, may be additional beneficial strategies. Dr. Raetz and Dr. Meyer indicated no relevant conflicts of interest. 1. Bhatia S, Landier W, Hageman L, et al. 6MP adherence in a multiracial cohort of children with acute lymphoblastic leukemia: a Children’s Oncology Group study. Blood. 2014;124:2345-2353. 2. Bhatia S, Landier W, Hageman L, et al. Systemic exposure to thiopurines and risk of relapse in children with acute lymphoblastic leukemia: a Children’s Oncology Group study. JAMA Oncol. 2015;1:287-295. 3. Yang JJ, Landier W, Yang W, et al. Inherited NUDT15 variant is a genetic determinant of mercaptopurine intolerance in children with acute lymphoblastic leukemia. J Clin Oncol. 2015;33:1235-1242. 4. Relling MV, Hancock ML, Rivera GK, et al. Mercaptopurine therapy intolerance and heterozygosity at the thiopurine S-methyltransferase gene locus. J Natl Cancer Inst. 1999;91:2001-2008. M E M O R I A M Dorothea Zucker-Franklin, MD (1929 – 2015) Dr. Dorothea Zucker-Franklin, National Academy of Medicine member, pioneer in electron microscopy of blood cells at New York University School of Medicine, and third female president of ASH (1995), passed away November 24, 2015, at the age of 86. Dottie was born in Berlin, Germany, but fled to the Netherlands with her family in 1936 to escape Nazism. There she attended the same school as Anne Frank and was forced into hiding in 1943. Arriving destitute in New York in 1948, Dottie graduated from Hunter College as class valedictorian and proceeded to attend New York Medical College on a scholarship. Dottie and her husband, immunologist Dr. Edward Franklin, who was a childhood neighbor from Berlin, enjoyed a close professional partnership until his death in 1982. The Franklins required separate home offices since, when together, their constant conversation precluded working effectively. However, together Dottie and Ed were able to accomplish a great deal. Aside from their professional accomplishments, they raised their daughter Deborah, cared for their much loved farm in the Berkshires, travelled internationally, and collected pre-Columbian sculptures. When visiting fellow Dr. Mordechai Pras showed Dottie amyloid tissue, her fascination with amyloid’s birefringence convinced Ed that it would be fun to learn more about this substance together. They jointly penned more than 20 articles on amyloid, identified its fibrillary nature, and showed that precursor serum amyloid A was cleaved by monocyte proteases, introducing the concept that cellular proteases modify amyloid in disease. Dr. Steven D. Douglas of the University of Pennsylvania praised Dottie’s goal of juxtaposing numerous techniques to achieve “molecular morphology,” as stated in her book, Atlas of Blood Cells. He noted that, “Dottie’s microscopy not only captured spectacular events in the cell, but was a magnificent form of medical and biologic creative art. Her innovative observations spanned cell biology, hematology, and immunology. With James Hirsch, she published the first evidence that neutrophil and eosinophil granules released their contents into the phagocytic vacuole. This remarkable discovery ushered in modern understanding of phagocyte function.” Her later studies explored electron microscopy of blood cells responding to cytokines, thrombopoietin, and HIV. 7. Ma X, Edmonson M, Yergeau D, et al. Rise and fall of subclones from diagnosis to relapse in pediatric B-acute lymphoblastic leukaemia. Nat Commun. 2015;6:6604. Dr. Barry Coller, ASH president in 1998, wrote, “I was very fortunate to have Dr. Zucker-Franklin as my professor when I was a medical student, my ward attending when I was a resident, and later (as “Dottie”) as my colleague and friend sharing a love for hematology. She was an ideal role model as a physician-scientist, devoted to both her elegant electron microscopic studies and to her patients. Megakaryocytes held a special place in her heart, as in mine! She set and met the highest standards for both research and clinical activities.” Dr. Ralph Nachman commented that “Dottie was a dedicated perfectionist who took great pride in the clarity of her data, particularly the impressive electron micrographs of platelets. She combined old fashioned morphology and molecular physiology.” Dr. Kenneth Kaushansky, ASH President in 2008 added, “Dottie was a passionate hematologist, devoted to understanding the structure and function of blood cells. Our scientific collaboration taught me a great deal about what many consider the most complicated and beautiful cell in all of biology, the megakaryocyte.” 8. Li B, Li H, Bai Y, et al. Negative feedback-defective PRPS1 mutants drive thiopurine resistance in relapsed childhood ALL. Nat Med. 2015;21:563-571. –Barry Coller, MD, Vice-President for Research, Rockefeller University –Steven D. Douglas, MD, Professor of Pediatrics, University of Pennsylvania –Babette Weksler, MD, Professor Emerita of Medicine, Weill Cornell Medicine 5. Meyer JA, Wang J, Hogan LE, et al. Relapse-specific mutations in NT5C2 in childhood acute lymphoblastic leukemia. Nat Genet. 2013;45:290-294. 6. Tzoneva G, Perez-Garcia A, Carpenter Z, et al. Activating mutations in the NT5C2 nucleotidase gene drive chemotherapy resistance in relapsed ALL. Nat Med. 2013;19:368-371. 14 The Hematologist: ASH NEWS AND REPORTS Editors’ Choice SEPTEMBER 24, 2015 NOVE M B E R 5, 2015 Kassim AA, Payne AB, Rodeghier M, et al. Low forced expiratory volume is associated with earlier death in sickle cell anemia. Blood. 2015;126:1544-1550. Kiyasu J, Miyoshi H, Hirata A, et al. Expression of programmed cell death ligand 1 is associated with poor overall survival in patients with diffuse large B-cell lymphoma. Blood. 2015;126:2193-2201. Pulmonary complications are a known contributor to mortality in adults with sickle cell disease (SCD). In this article, Dr. Adetola Kassim and colleagues present data examining the prognostic significance of decreased pulmonary function in a large prospective cohort of SCD patients in the Cooperative Study for Sickle Cell Disease. They confirm that a decreased forced expiratory volume in 1 second percent (FEV1%) predicts for earlier death in patients with SCD. Surprisingly, however, obstructive or restrictive pulmonary function test abnormalities are not predictive of earlier death. Further study is needed to better understand the pathophysiology and negative impact of decreased FEV1% in SCD patients. Dr. Bob Löwenberg (Editor-in-Chief) and Dr. Nancy Berliner (Deputy Editor-in-Chief) have combined efforts to identify some of the most outstanding Blood articles that have appeared either in print or online during the two-month interval between issues of The Hematologist. The goal is to underscore the remarkable research that is published in Blood and to highlight the exciting progress that is being made in the field. SEPTEMBER 10, 2015 Rapetti-Mauss R, Lacoste C, Picard V, et al. A mutation in the Gardos channel is associated with hereditary xerocytosis. Blood. 2015;126:1273-1280. Glogowska E, Lezon-Geyda K, Maksimova Y, et al. Mutations in the Gardos channel (KCNN4) are associated with hereditary xerocytosis. Blood. 2015;126:1281-1284. The Gardos channel is a Ca2+-sensitive potassium channel that is widely expressed in tissues and cells, including erythrocytes. It has been widely studied as a potential regulator of cell volume that may be important in hemoglobinopathies. In this week’s plenary papers, Dr. Raphael Rapetti-Mauss and colleagues and Dr. Edyta Glogowska and colleagues identify mutations in the KCNN4 gene, which encodes the Gardos channel, as the molecular basis for a subset of hereditary xerocytosis and chronic hemolytic anemia associated with dehydrated cells. These studies confirm the importance of the Gardos channel in maintaining erythrocyte hydration, and they offer a potential clinical entry point for treatment of this rare syndrome. S E P T E M B E R 1 7, 2 0 1 5 Donadieu J, Bernard F, Noesel Mv, et al. Cladribine and cytarabine in refractory multisystem Langerhans cell histiocytosis: results of an international phase 2 study. Blood. 2015;126:1415-1423. Dr. Jean Donadieu and colleagues present the most promising treatment data to date in a group of patients with Langerhans cell histiocytosis (LCH) who historically have had a notoriously unfavorable survival. The investigators applied a standardized disease activity score to follow and evaluate these patients on therapy. They report their encouraging results of an intensive chemotherapy regimen of cladribine and cytarabine in a multicenter trial in children with disease of the bone marrow, liver, or spleen who were refractory to standard therapy. Zhu S, Travers RJ, Morrissey JH, et al. FXIa and platelet polyphosphate as therapeutic targets during human blood clotting on collagen/tissue factor surfaces under flow. Blood. 2015;126:1494-1502. Factor XIIa (FXIIa) and FXIa contribute to thrombosis in animal models, while platelet-derived polyphosphate (polyP) may potentiate contact or thrombin-feedback pathways. Dr. Shu Zhu and colleagues discovered that platelet-derived polyP plays a significant role in human whole blood that is distinct from FXIIa activation and thrombin generation through feedback activation of FXI. polyP directly interacts with fibrin in a way that makes the thrombus less susceptible to lysis by fibrinolytic agents. The way in which FXIa and polyP contribute to thrombus formation in human blood and the fact that blocking polyP reduces thrombus stability and increases lysis of the fibrin clot suggest that polyphosphate inhibitors are among the most interesting candidate antithrombotic therapeutic agents. The Hematologist: ASH NEWS AND REPORTS OCTOB E R 1, 2015 Bernard S, Goldwirt L, Amorim S, et al. Activity of ibrutinib in mantle cell lymphoma patients with central nervous system relapse. Blood. 2015;126:1695-1698. A substantial proportion of patients with aggressive forms of mantle cell lymphoma develop central nervous system (CNS) metastasis, which is notoriously difficult to treat. In their article, Dr. Sophie Bernard and colleagues provide evidence that ibrutinib, an orally administered inhibitor of Bruton tyrosine kinase, crosses the blood-brain barrier and has significant therapeutic activity in CNS disease of mantle cell lymphoma. OCTOB E R 22, 2015 Gill JC, Castaman G, Windyga J, et al. Hemostatic efficacy, safety, and pharmacokinetics of a recombinant von Willebrand factor in severe von Willebrand disease. Blood. 2015;126:2038-2046. Dr. Joan Gill and colleagues present the results of a phase III trial of recombinant von Willebrand factor (rVWF) for treatment of bleeds in patients with severe von Willebrand disease (vWD). Their results confirm that rVWF is safe and highly effective for the control of bleeding. Since patients with severe vWD are initially factor VIII (FVIII) deficient as well because VWF stabilizes FVIII, the first dose of rVWF was administered with FVIII. Later FVIII dosing proved to be unnecessary, as endogenous stores recovered upon administration of rVWF. Bleeding control was achieved in 97 percent of bleeds, and only one infusion was required in more than 80 percent of bleeding episodes. These encouraging results represent a major breakthrough in the treatment of vWD. Moretti D, Goede JS, Zeder C, et al. Oral iron supplements increase hepcidin and decrease iron absorption from daily or twice-daily doses in iron-depleted young women. 2015;126:1981-1989. The appropriate oral treatment of iron deficiency is codified and rarely questioned, but perhaps it should be. In this article, Dr. Diego Moretti and colleagues report on a study of iron administration that is based on the current understanding of iron metabolism and may be practice-changing. Since serum iron levels are one factor regulating hepcidin, they postulate that absorption of iron supplements could paradoxically induce hepcidin and inhibit further iron absorption. Using a clever strategy of differing iron doses labeled with different Fe isotopes, they document that this is in fact the case. They demonstrate that iron supplements of 60 mg of iron or more increase hepcidin for up to 24 hours, impairing subsequent iron absorption. They suggest that alternate-day single doses of iron could improve the efficacy of oral iron therapy, allowing a welcome reduction in gastrointestinal side effects; confirmation awaits an appropriate clinical trial. The PD-1/PD-L1 pathway inhibits host antitumor responses in a wide variety of malignancies. However, since PD-1 is normally expressed on lymphocytes within the lymph node, the potential role of this pathway in lymphoma is complex. Dr. Junichi Kiyasu and colleagues report an in-depth study of the expression of PD-1 and PD-L1 in diffuse large B-cell lymphoma (DLBCL) cells and the surrounding microenvironment. They demonstrate that 11 percent of DLBCLs manifest PD-L1 expression on the tumor cells and that this has a negative impact on overall survival. In contrast, expression of PD-L1 by infiltrating lymphocytes within the microenvironment does not affect survival. This suggests that targeting this pathway with checkpoint inhibitors may be a therapeutic option in this subset of DLBCL patients. Sun C, Tian X, Lee YS, et al. Partial reconstitution of humoral immunity and fewer infections in patients with chronic lymphocytic leukemia treated with ibrutinib. Blood. 2015;126:2213-2219. Chronic lymphocytic leukemia (CLL) is associated with hypogammaglobulinemia and immune dysregulation, which contribute to increased infections. The Bruton tyrosine kinase (BTK) inhibitor ibrutinib is a recently approved novel agent that induces a high rate of response in CLL. However, congenital loss of BTK results in Bruton agammaglobulinemia, a severe B-cell defect, suggesting that BTK is also critical to normal B-cell function. In this article, Dr. Clare Sun and colleagues assess the impact of ibrutinib on normal B-cell function in patients with CLL, and demonstrate that the BTK inhibitor allows partial reconstitution of normal B cells and humoral immunity at 12 months. Since patients are treated with ibrutinib longterm, further follow-up is needed to assess the full extent of immune reconstitution and its impact on infectious outcomes. NOVE M B E R 12, 2015 Hur WS, Mazinani N, Lu XJD, et al. Coagulation factor XIIIa is inactivated by plasmin. Blood. 2015;126:2329-2337. This article resolves years of conflicting results regarding the inactivation of factor XIIIa (FXIIIa) by plasmin. Dr. Woosuk Hur and colleagues demonstrate that plasmin inactivates activated blood coagulation factor XIIIa, but not zymogen factor XIII (FXIII). They also show that FXIIIa is inactivated during clot lysis but not during clot formation. NOVE M B E R 19, 2015 Kwok B, Hall JM, Witte JS, et al. MDS-associated somatic mutations and clonal hematopoiesis are common in idiopathic cytopenias of undetermined significance. Blood. 2015;126:2355-2361. Cargo CA, Rowbotham N, Evans PA, et al. Targeted sequencing identifies patients with preclinical MDS at high risk of disease progression. Blood. 2015;126:2362-2365. Increasingly, clinicians are obtaining molecular genetic tests when evaluating patients with unexplained cytopenias. How is one to interpret the detection of clonal hematopoiesis in the absence of dysplastic changes in the bone marrow? If a clonal mutation is discovered, yet diagnostic criteria for a hematological neoplasm are not met, what is the diagnosis? Dr. Brian Kwok et al and Dr. Catherine Cargo and colleagues report results of mutation testing in two series of patients with cytopenia and nondiagnostic marrows. These two plenary papers demonstrate that the answer is challenging and that the appropriate interpretation of positive mutation testing in patients without evidence of dysplasia is not straightforward. 15 W H A T ’ S O N T H E MARK YOUR CALENDAR W E B As technology and the Web have evolved, so too have ASH’s online offerings. Now, beyond the ASH website, you can download ASH apps for your smartphone or tablet, follow ASH on Twitter (www.twitter.com/ASH_hematology), and find ASH videos on YouTube (www.youtube.com/user/ASHWebmaster). Plan to attend The only official H S A f o s t h g li h ig H 2016 in North America ® r internationally in North America to hea Attend Highlights of ASH rts analyze the latest updates expe ogy atol hem ed gniz reco can translate . Learn how this research in hematology research care strategies. and t men age man ent into improved pati ighlights www.hematology.org/h WA | Toronto, Canada • Seattle, January 15-16, 2016 York, NY New • TX as, Dall | 6 201 January 22-23, CA | Atlanta, GA • San Diego, January 29-30, 2016 1/6/15 12:09 PM HOA NA 2016 postcard REV.indd 1 January 22-23Highlights of ASH® in North America Dallas, TX www.hematology.org/highlights 29-30Highlights of ASH in North America San Diego, CA www.hematology.org/highlights February 182016 Clinical Research Training Institute in Latin America application due Washington, DC www.hematology.org/awards 192016 HONORS Award applications due Washington, DC Just Released: The New ASH Pocket Guides App ASH Pocket Guides, quick references covering nine key patient-care topics, are now available in a new mobile app! The ASH Pocket Guides app includes interactive versions of all the Society’s clinical quick-reference guides. In addition to the pocket guide contents, the app includes tools to aid in clinical decision making, including bleeding score and 4Ts calculators, calculators for initial and chronic warfarin dosing, and interactive algorithms for the diagnosis and management of heparin-induced thrombocytopenia and von Willebrand disease. The app is free to download and is available for iOS and Android devices. Visit www.hematology.org/pocketguidesapp for more information. *Please be sure to download the new app, as this version completely replaces the previous ASH Guides app, and the older version will not automatically update to include the new content. www.hematology.org/awards March 5-6Highlights of ASH in Asia-Pacific Brisbane, Australia www.hematology.org/highlights 72016 Minority Medical Student Award Program applications due Washington, DC www.hematology.org/awards 18Latin American Training Program applications due Washington, DC www.hematology.org/awards 252016 Clinical Research Training Institute applications due Washington, DC www.hematology.org/awards 31Visitor Training Program applications due Washington, DC www.hematology.org/awards April 29-30Highlights of ASH in Latin America Natal, Brazil Read The Hematologist online at www.hematology.org/thehematologist, and catch up on the latest news in the field of hematology right on your desktop, mobile phone, or tablet. www.hematology.org/highlights