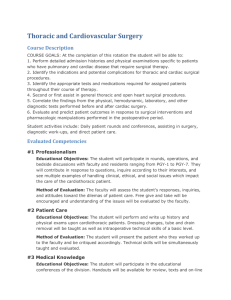
EACTS Daily News
The official newspaper of the European Association for the Cardio-Thoracic Surgery Annual Meeting 2008
SUNDAY
Postgraduate
Course at
EACTS 2008
Welcome to the Postgraduate Course at this year’s EACTS Annual
Meeting. The course has been separated into six full day courses,
which cover the entire spectrum of the cardio-thoracic field. The
courses have been designed to encourage debate and allow delegates to develop their opinions on a variety of topical issues that
are at the very forefront of cardio-thoracic surgery. As well as covering all the relevant surgical and endovascular topics right through
to the latest techniques, clinical results and device updates.
This year’s Postgraduate Course will focus
on the following key areas:
Adult Cardiac
The year’s programme will be split into
three sessions and will examine the latest
developments and topics in coronary intervention with specific discussions concerning the SYNTAX Trial (drug-eluting stents
vs. cardiac artery bypass graft). In addition,
the programme will include a session basic
mechanisms, imaging techniques, stem
cell therapy and surgical treatments
regarding heart failure.
This year’s meeting will also witness a
unique Joint Session between EACTS and
the European Society of Cardiology during
which the latest developments in transcatheter valve intervention will be examined including: a joint position of surgeons
and cardiologists, a critical analysis of the
results for both mitral valve and aortic
valve, the clinical impact of transcatheter
valve intervention and how to provide the
appropriate training and environment.
The Cardiac Surgery programme will
finish with an assessment of arrhythmias
including: an update on maze (necessary
or unnecessary?), intra- and post-operative
pacing, the cardiac surgeon as specialist
for epicardial approach and troubleshooting only? and new devices to be surgically
implanted – perspectives for the cardiac
surgeon.
Thoracic Surgery
This year’s Thoracic Postgraduate Course
will focus on the thoracic patient in the
intensive care unit (ICU). The session will
begin with an examination of ventilation
strategies and the circumstances for their
use. Next, there will be an assessment of
when and how to perform a tracheostomy, followed by a presentation of reducing
intrathoracic sepsis in the ICU patients.
The subsequent session will look at how
a surgeon can help with airleaks in the
ICU, as well as the indications and management strategies for re-operations on
ICU patients. The session will end with
how to increase the chances of recovery to
good quality of life.
This year’s Evidence Lecture will be
delivered by Erico A Rendina (Rome, Italy),
who will present a systematic evidence
review of resection for patients who have
been initially diagnosed with N3 lung cancer after response to induction
chemotherapy.
The final session, which will focus on
pulmonary metastasectomy and will examine the clinical evidence for pulmonary
metastasectomy, current beliefs and practice in Europe, ask whether thoracic sur-
Visit the EACTS stand
geons should follow in the footsteps of
liver surgeons and how to square current
evidence and current practice.
Congenital
The first session in the Congenital Course
will focus on the management of aortic
arch obstruction specifically, morphology,
advanced imaging technologies and techniques, approaches/techniques for coarctation repair (+/-concomittant cardiac
lesions) and approaches/techniques for
hypoplastic arch/interrupted arch repair
(+/-concomittant cardiac lesions). In addi-
tion, there will be an examine of evidencebased medicine and whether there is a
superior approach/technique, as well as
the cardiologic management of late complications (recoarctation, arterial hypertension) and the surgical management of
complex/recurrent obstruction in adult
patients.
The second session will discuss paediatric perfusion and the rationale, strategies
and results normothermic vs. hypothermic
cardiopulmonary bypass, and look at the
strategies to minimise systemic inflammaContinued on page 2
Critical analysis of transcatheter mitral valve repair
Professor Ottavio Alfieri
Division of Cardiac Surgery,
Ospedale San Raffaele, Via
Olgettina 60, Milan 20132, Italy
P
ercutaneous mitral valve
repair (PMVR) is emerging as
a possible alternative to surgical reconstruction in selected
patients. However, while transcatheter aortic valve implantation
(TAVI) for inoperable or high-risk
patients with severe aortic stenosis
is already generally accepted by
the medical community, PMVR is
associated with more scepticism.
There are a number of reasons for
such a different attitude.
First of all, the beneficial impact
on survival of valve replacement in
symptomatic patients with severe
aortic stenosis is out of question
even in the very old population and
in presence of left ventricular dysfunction. On the contrary, there are
no solid data showing increased
survival following surgical correction of mitral regurgitation (MR) in
elderly patients, particularly when
the ventricular function is poor.
Secondly, TAVI is closely replicating what is carried out in the operating room, the final result being a
biological prosthesis in orthotopic
position with a minimal gradient
and a satisfactory orifice area. In
regard to mitral valve repair, a great
variety of surgical techniques are
available to the surgeon to obtain a
competent valve while the percutaneous methods can only reproduce
the edge to edge repair and the
annuloplasty, at present not even in
combination. As a consequence of
these limitations, the applicability of
the percutaneous procedures has to
be restricted only to a minority of
patients with hemodynamically relevant MR. On the contrary, a biological prosthesis can be effectively
implanted in the great majority of
patients affected by severe aortic
stenosis using either a transfemoral
or a transapical approach.
Furthermore, while TAVI is relatively simple and reproducible,
PMVR remains a complex proce-
dure associated with results which
do not appear to be comparable
to those obtained with surgery.
Finally, TAVI is commonly used
as a life-saving procedure for
patients with a letal disease which
is not treatable otherwise, whereas
PMVR is mainly offered as an alternative to patients who can be optimally treated surgically.
The reduction/remodeling of the
mitral annulus with devices implanted in the coronary sinus has been
reserved to patients with functional
MR. The experience accumulated in
the clinical trials (EVOLUTION,
AMADEUS and PTOLEMY) reveals a
low rate of responders and a limited
reduction of MR. In addition, the
occurrence of adverse events (death,
myocardial infarction, tamponade)
was not negligible. Precise patient
selection criteria for each device
have to be developed. The largest
clinical experience with PMVR has
been accumulated with the MITRA
clip (evalve), reproducing the surgical double orifice repair. The results
obtained in the patients enrolled in
the EVEREST I and II registry have
been analyzed and repeatedly presented. Selected patients with
degenerative and functional MR
have been treated with a very low
rate of major adverse events. In the
group of patients in whom a procedural success was achieved, freedom from death, reoperation or
Ottavio Alfieri
MR>2+ was 67% at 3 years.
In conclusion, PMVR is feasible
but its role in the clinical practice
has still to be defined. Certainly
only a small proportion of the current surgical candidates can benefit from PMVR.
Introducing KIMBERLY-CLARK* INTEGUSEAL *
Microbial Sealant.
Join our symposium on "new non pharmaceutical way to
reduce SSI" at the EACTS congress this Monday
15th September 2008 at 12:45 pm.
www.HAIwatch.com
www.Integuseal.com
Contents 1 Welcome to EACTS 2 Adult Cardiac 4 Thoracic 6 Perfusion 6 Techno-College 2008 winner 8 Endovascular Intervention 10 Congenital 12 Basic Science
16 Perfusion 18 Things to do in Lisbon 20 Exhibitors list 21 Floorplan 22 Product listings 22 Calendar of events
2 September 08 EACTS Daily News
Adult Cardiac
Adult Cardic Surgery
timetable
Organisers
M Antunes, Coimbra;
A P Kappetein, Rotterdam;
P Kolh, Liège; B Osswald, Essen
Session 1 Coronary intervention
Moderators M Antunes, Coimbra; A P Kappetein,
Rotterdam
09:00 Coronary artery bypass graft concomitant with
M J Antunes, Coimbra
valve surgery
09:20 The value of a hybrid approach for coronary
revascularisation
A Repossini, Brescia
09:40 Coronary artery bypass grafting in patients with
severe left ventricular dysfunction
A P Kappetein, Rotterdam
10:00 Coffee
Session 2 Heart failure
Moderator P Kolh, Liège
10:30 Basic mechanisms
S Heymans, Maastricht
10:50 Imaging techniques
L Pierard, Liège
11:10 Stem cell therapy: hype or hope?
P Menasché, Paris
11:30 Surgical treatment
G Dreyfus, London
12:00 Lunch
13.00 EACTS/ESC Joint Session
Transcatheter valve intervention
Moderators P Sergeant, Leuven; A Vahanian, Paris
13.00 Joint position of surgeons and cardiologists
A Vahanian, Paris
13.15 Critical analysis of the results:
O Alfieri, Milan
mitral valve
aortic valve
F Mohr, Leipzig
13.30 Clinical impact
P Tornos, Barcelona
13:45 Appropriate training and environment
F Maisano, Milan
14.00 Discussion
Session 3 Arrhythmias
Moderators K Khargi, The Hague;
B Osswald, Essen
14:30 Update on Maze – necessary or unnecessary?
K Khargi, The Hague
14:50 Intra- and post-operative pacing
J G Maessen, Maastricht
15:10 The cardiac surgeon as specialist for epicardial
approach and troubleshooting only?
A Laczkovics, Bochum
15:30 New devices to be surgically implanted –
perspectives for the cardiac surgeon
B Osswald, Essen
16.00 Adjourn
Update on Maze –
necessary or unnecessary
Krishna Khargi, MD PhD
Consultant Cardiothoracic Surgeon
Cardiac Center The Hague-Delft, Haga teaching
Hospital Leyenburg
Leyweg 275, 2545 CH
The Hague, the Netherlands
E
ven within the cardiothoracic surgical community, the necessity of a concomitant anti-arrhythmic procedure to treat atrial fibrillation (AF) is
surprisingly still disputed. Despite emerging evidence
revealing the beneficial effects of a surgical AF treatment, only 38% of all eligible surgical AF patients in
the USA, between 2004 and 2006, received this
therapy.
What are the reasons for denying a potential profitable treatment in so many AF surgical patients?
Several subjective and in part biased explanations can
be distinguished;
Correcting the primary valve or coronary pathology will result in “spontaneously” extinguishing of
AF?!
A concomitant AF procedure extends the surgical
procedure adding to additional morbidity and
mortality?!
Patients are too sick (e.g. enlarged atria, long
duration of AF, poor LVEF) to benefit anyhow from
such a procedure?!
The efficacy of the ablation technique is too low,
since most of the surgical patients postoperatively
reveal to be in AF, at discharge from the hospital?!
The long- term sinus rhythm stability of a successful treatment is too low?!
Patients don’t show any long-term quality of life
or survival benefits?!
During the postgraduate course at the EACTS 2008
in Lisbon, each of these skewed statements will be
addressed, in relationship to the current available
international peer- reviewed literature. The most
recent patients’ selection, indication and postoperative results, including the improvement of the quality
of life- and survival rates for specific subsets of
patients, will be discussed and presented. A more
comprehensive evaluation of these results will, hopefully, pave the way to integrate AF arrhythmia surgery as a standard treatment in each and every cardiothoracic surgical practice.
Postgraduate
Course at
EACTS 2008
Continued from page1
tory response syndrome (coated circuits,
prime issues, pharmacological interventions, perfusion techniques). The session will end with a state of the art
examination of deep hypothermic circulatory arrest (techniques, monitoring,
long-term outcome).
The final session will be an interactive
video session focusing on aortic valve
repair in congenital heart surgery and
will include commissurotomy and leaflet
thinning in a critical neonatal aortic
valve stenosis, the repair of the leaking
bicuspid aortic valve in a child, a repair
of the unicuspid aortic valve and the
repair of a subaortic ventricular septal
defect with aortic valve prolapsus.
Endovascular Intervention
Retrograde endovascular techniques
will be the main focus of discussion in
the Postgraduate Endovascular
Intervention Course. The first talk will
look at surgical training programmes
for endovascular aortic stenting, followed by a look at the indications and
contraindications for endovascular
treatment of abdominal aortic
aneurysms and thoracic aortic
aneurysms. The session will close with
a look at whether overstenting of the
left subclavian artery is without risk.
Continuing the theme of retrograde endovascular techniques will
examine how to prevent complications after overstenting of the left
subclavian artery. The next session
will then look at hybrid approach for
thoracoabdominal EVAR, the development of branched or fenestrated aortic stents, as well as the indications
and contra-indications for endovascular aneurysm repair.
The final session will discuss antegrade endovascular techniques and
begin with an assessment of the
frozen elephant trunk technigue, as
well as the two-stage hybrid approach
for total arch replacement and onestage hybrid approach for total arch
replacement. There will then be three
presentations discussing trans-apical
aortic valve replacement with a specific
focus on angiographic assessment,
intra-cardiac ultrasound and 3-D
echocardiography.
Perfusion
The first session in the Perfusion Course
will look at current controversies in minimized cardiopulmonary bypass and will
begin with asking whether there is a
difference between OPCAB vs MECC.
The session will then move onto complex surgery using minimized extracorporeal circulation and the pros and cons
in the use of cell saver.
The next session entitled, Basic
Science in Perfusion, will start with an
examination of augmenting venous
return in minimal invasive heart surgery, followed by the complications of
vacuum assisted drainage, portable
CPS during normothermic cardiac
arrest and hypothermic Preservation for
Traumatic Cardiac Arrest.
The Cardiopulmonary Bypass in
Non-Cardiac Surgery session will
examine the perfusion strategies in
thoracoabdominal aneurysm surgery,
Hancock® II: Setting the
Gold Standard for 25 years
S
ince the first implant in Hancock II valve.
1982, the Hancock® II
We have been following
valve has provided
our patients pretty much
more than 20 years excelfrom the beginning.
lent hemodynamic performActually, we have over
ance and durability
2,000 patients who have a
Dr Tirone E. David, MD,
Hancock II valve, well docuworld-renowned
mented, not only
Tirone E. David
“You don’t see
cardiac surgeon
with clinical foland the first sur- papers on the
low-up, but with
aortic position, as far as
geon to implant pericardial valve
echocardiogram
durability is concerned. We
the Hancock II
so we have
have no failures at 15 years
showing 20 years objective evivalve 26 years
(determined) by echocardiooutcome from an dence of the
ago shares his
graphy data.
experience and
valve performinstitution”
explains why it
ance on the long
Clinical studies
remains his valve of choice.
term, particularly after the
It is important to remember
“As our experience accufirst decade.
that there are very few
mulated, we learned that
Durability in the aortic
papers on bioprostheses
it’s an extremely durable
position is
performance at
valve. Now we have 26
nothing short
“Hancock II really is 20 years. The
years documented experiof excellent. It the gold standard of Hancock II is one
ence with this valve, and
is very difficult
of the very few
bioprosthetic heart
there are patients out there,
to beat this
ever published at
valves now”
25 years later, with a
valve in the
20 years. We
Jos Maessen and Mark LaMeir –
Academic Hospital Maastricht,
The Netherlands
F
Jos Maessen and Mark LaMeir
An unexpected additional advantage of
being in the atrium at both sides of the
atrial wall became immediately apparent in our first patient, says Mark
LaMeir who pioneered the single sided
minimal invasive thoracosopic, surgical
Basic Science
This year’s course will examine endogenous cell defence: organ protection of
the future. The first presentation will
ask why endogenous cell defence, preand post-conditioning is interesting in
cardiothoracic surgery. Followed by presentations discussing which organs can
be protected, the mechanisms for early
and delayed preconditioning, and postconditioning.
The subsequent presentations will
look at the similarities and differences
in mechanisms of pre- and post-conditioning, alternative methods and
mechanisms of increasing the endogenous cell defence, the present status
of clinical studies in cardiac surgery
and possible ways to exploit the
endogenous cell defence in surgery.
tion of the design of the
have clinical reports from
valve to make them durable.
(the) manufacturer, but not
We have seen over the
from surgeons that follow
past 25 years, several
the patients and obtain
valves that came and
echo every year
went. And some
I continue to
“Durability in the remain. Hancock II is
use the
Hancock II
aortic position is one that, although
valve mostly
nothing short of it’s a 26-year-old
design, still is a very
because of our
good valve.
experience but excellent”
And to be quite
the Patients’
honest, most of my
main concern is durability.
younger partners don’t
I think this valve is diffibother even trying to
cult to beat.
implant the newer ones
There are many new bioand they’re very comfortprosthetic valves that are
able using the Hancock II.
wonderful hemodynamicalI continue testing new
ly; but no data on durability.
ones – mostly for academic
So if durability is the issue,
purposes or scientific
Hancock II is tough
“We have
curiosity – to see if
to beat.
there are valves that
You don’t see
no failures
can be better than
papers on the peri- at 15 years”
the gold standard. I
cardial valve showthink Hancock II really is the
ing 20 years outcome from
gold standard of bioprosan institution. The problem
thetic heart valves now.
with pericardial is largely
Whatever we do has to
the design. The manufacturbe better than Hancock II.”
er has to pay a lot of atten-
Excitement in Maastricht for
hybrid AF ablation procedures
or the departments of cardiothoracic surgery and cardiology of the
university medical centre in
Maastricht, the Netherlands, together
with their colleagues in Namur, Belgium,
the ideal approach in the invasive treatment of AF, is no longer wishful thinking. After years of discussion, writing
protocols and making small steps in
gaining each other’s confidence, electrophysiologists and surgeons as a single
team, now perform hybrid AF ablation
procedures on a routine base.
AF ablation is no longer either a surgeons’ or an electrophysiologists’ business. The best parts of the surgical and
percutaneous approach are brought
together in a single intervention to
offer the patient the most complete
and fastest procedure. The surgeon is
able to create epicardially continuous
ablation lines of centimetres at a
stretch with a single shot, saving time
and radiation.
The electrophysiologist working from
endocardial can check the results of the
ablation and add the ablation of certain
spots to fine tune the procedure and
prevent the need for reinterventions.
pulmonary endarterectomy and selective cerebral perfusion in aortic surgery. The final session of the day, Left
Heart Assist, is scheduled to assess
short-term heart assist with impeller
pumps, Levosimendan in reduced left
ventricular function and long term
heart assist with impeller pumps.
approach. The surgeons radiopaque
ablation catheter, epicardially wrapped
around the pulmonary veins, turned out
to be a perfect landmark for the electrophysiologist looking at his fluoroscopy screen to find his way with a
catheter inside the atrium.
At present the procedure is performed either in the cathlab or in the
OR depending on what kind of ablation
the patient needs. Within months a
dedicated Hybrid-room should become
available combining an OR setting with
advanced fluoroscopy and a electrophysiological navigation system.
Here, the Hybrid development will
not come to an end. A month ago,
approval was obtained to build a new
cardiovascular centre in the near future,
hosting the cardiovascular and related
departments of both the Maastricht
and Aachen medical centres. ‘Hybrid’
should be the standard approach for all
cardiovascular interventions in this centre, Jos Maessen, head of the department of cardiothoracic surgery, says.
We really feel privileged to get the
opportunity to design the outline of a
hybrid cardiovascular centre right from
the beginning.
In general, the results of AF ablation
are considered quite acceptable.
However, the goal of ‘curing’ the disease, is still ahead of us. We need to
make progress in understanding AF
mechanisms and adapt accordingly the
ablation strategy in various patient categories. We strongly believe that the
Hybrid concept offers new conditions
to make this progress. From the tool
development perspective, lesion quality
control comes first. In the mean time,
the surgeon will continue to minimize
the invasiveness of his approach. The
subxyphoidal route may eventually
appear the way to go.
Artis zeego is the newest generation of interventional imaging systems from
SIEMENS Healthcare. Its flexibility makes it the ideal solution for hybrid rooms.
PERFORMER® CPB from MEDTRONIC. The compact Heart Lung Machine for
flexibility and efficiency in your hybrid OR: SAFETY, PERFORMANCE, INNOVATION
At EACTS, Medtronic and Siemens Medical Solutions are introducing
solutions for the Hybrid Suite on their joint booth (nb 2.33). The
Hybrid Suite features the Artis zeego and the Performer® CPB:
The Performer® CPB from Medtronic is a compact Heart Lung
Machine offering all the functionality of existing systems, it occupies
only a 500 cm by 560 cm space responding to the spatial demands
in hybrid operating rooms and providing convenient access for
perfusionists.
“In comparison to traditional stented valves, the stentless ones offer many
advantages for the patients suffering from both aortic valve and root disease.
In general, the current percentages of stentless do not reflect
this. Hence, I would like to share with you our 1800 stentlessimplant experience gained while we tripled of our aortic valve
procedures in the last twelve years.”
Dr. J. Ennker
“I look forward to sharing some of the insights our team
gained while applying multiple techniques for the surgical
therapy of aortic disease including MICS, aortic stenting and
transcatheter valve replacement“
The industrial robot technology integrated in the Artis zeego from
Siemens Healthcare allows the physician to move the C-arm to
almost any position around the patient. If the system is not used, it
can be stowed in a park position to require minimal space. This is a
highly significant feature in hybrid operating rooms.
Prof. R. S. Lange
“Most surgeons recognize the need to evolve into practicing
endovascular techniques. The question is how do you do this?
At this meeting I hope to share some of my knowledge on
catheter skills, training and operating room imaging”
Medtronic and Siemens are hosting a lunch satellite symposium on
Tuesday, September 16 (room 3C) with a view to helping you expand
your practice using open and minimally invasive approaches.
Dr. H. Shennib
© Medtronic, Inc. 2008 UC200901718 EE
A
S E R V I C E
O F
M E D T R O N I C
A C A D E M I A
Expand your skills. Control your future.
4 September 08 EACTS Daily News
Thoracic
Thoracic timetable
Organisers
Thoracic Committee members
Session 1
The thoracic patient in the
intensive care unit
Moderators K Athanassiadi, Athens; W Klepetko,
Vienna
09:00 Ventilation strategies: circumstances for using
them
M Antonelli, Rome
09:20 Tracheostomy - when and how
S Elia, Rome
09:40 Reducing intrathoracic sepsis in intensive care
unit patients
S Halezeroglu, Istanbul
10:00 Chaired Panel Discussion
10:30 Coffee
Session 2
Moderators M Antonelli, Rome; R Schmid, Bern
11:00 How a surgeon can help with airleaks in the
D Subotic, Belgrade
intensive care unit
11:20 Reoperations on intensive care unit patients:
indications and management strategies
L Lang-Lazdunski, London
11:40 How to increase the chances of recovery to
good quality of life
A Brunelli, Ancona
12:00 Chaired Panel Discussion
12:30 Lunch: The Evidence Lecture
Moderator: T Treasure, London
13:30 Resection for patients initially diagnosed
with N3 lung cancer after response to induction
chemotherapy: the evidence
E Rendina, Rome
on systematic review
Session 3 Pulmonary metastasectomy
Moderators D Van Raemdonck, Leuven; J-M
Wihlm, Strasbourg
14:15 The clinical evidence for pulmonary
J Pfannschmidt, Heidelberg
metastasectomy
14:35 Beliefs and practice in Europe
E Internullo, Parma
14:55 Should we follow in the footsteps of liver
surgeons?
J Northover, London
15:15 How do we square evidence and practice?
T Treasure, London
15:35 Panel discussion
16:00 Adjourn
How to increase the chances of The Evidence
recovery to good quality of life Lecture
Dr Alessandro Brunelli,
Umberto I Regional Hospital,
Ancona, Italy
T
he outcome of intensive care
is most frequently measured
as ICU or hospital mortality
rates. Mortality rates however may
be poor estimates of prognosis
because of differing discharge criteria and often permanent restrictions in daily activities.
Therefore assessment of residual
quality of life and function should
be increasingly used in the critical
care setting and is becoming an
accepted relevant measure of ICU
outcome.
Thoracic surgery is one of the
specialties using ICU resources
more frequently either electively for
monitoring of high risk patients
and emergently for major cardiopulmonary complications requiring active life support treatment.
It has been reported that
approximately 5-10% of all ICU
beds are occupied by thoracic surgery patients and that from 5 to
10% of patients submitted to
major thoracic procedures would
require a prolonged and
unplanned ICU admission.
There is scant data about quality
of life and residual physical and
emotional status of thoracic
patients admitted to ICU, therefore
Alessandro Brunelli
inferences need to be drawn from
several studies addressing this subject for the entire cohort of patients
requiring a prolonged ICU stay.
ICU stay determines a number
of important physical and psychological effects. In general after a
prolonged stay in ICU patients will
experience serious neuromuscular
problems with polyneuropathy and
muscle wasting that influence their
mobility. It has been shown that at
8 weeks after ICU discharge 51%
of patients are unable to climb
stairs and 38% use a wheelchair
to go outside. Another major issue
which is still often overlooked is
the presence of important psychological problems such as amnesia
of factual events of ICU, anxiety,
panic attacks, post-traumatic stress
disorder symptoms. It has been
reported that 88% of patients
with an ICU stay longer than 4
days experience some delusional
memories or vivid hallucinations
that may predispose to more serious chronic PTSD symptoms.
All these problems warrant the
institution of a close follow-up
program including early ward visits
by ICU team for providing continuity of care and repeated follow-up
outpatients clinics. This program
may allow the early recognition of
physical and psychological problem and the institution of rehabilitation programs.
Patient directed rehabilitation
through the use of ICU recovery
manual and graded exercise programme have been shown to
improve physical recovery at 6
weeks and 8 months after ICU
and to reduce symptoms of
depression and PTSD at 8 weeks in
a randomized controlled trial
(Jones C et al, Crit Care Med
2003). Other trials are currently
underway to confirm these results.
In conclusion, it would be valuable for each ICU to have instruments to assess the long term survival and quality of life of discharged patients in order to optimize the use of resources and
implement those physical and psychological support programs that
may help to achieve the primary
health care goals.
The clinical evidence for pulmonary metastasectomy
Prognostic indicators –
Cui bono?
Dr Joachim Pfannschmidt
Oberarzt Thoraxchirurgie,
Thoraxklinik am
Universitätsklinikum, Germany
A large volume of the literature on
lung metastasectomy is focused on
prognostic parameters, which may help
to identify patients benefiting the most
from pulmonary metastasectomy.
Complete surgical resection stands
out as the most important prognostic
indicator, and even in recurrent disease,
complete surgical resection of pulmonary metastases may be impacting
on long-term survival. Several prognostic factors are discussed, for instance:
“How many is too many?” , in patients
with multiple pulmonary metastases;
and what is the role of the disease-free
interval in patient selection?
In practice, rendering the patient
free of tumor continues to be the
major objective (as far as the functional
reserve ca be preserved), and this may
help us to decide who should be
offered an operation with curative
intent.
Finally, indication for surgery has to
be discussed in a multi-disciplinary
tumor board, where there is plenty of
opportunity for judgment and individualization of decision-making.
S
ince the first pulmonary metastasectomy by Josef Weinlechner, over
125 years ago, the interest in pulmonary metastasectomy heightened
and gained acceptance. However, there
are still physicians who are considering
pulmonary metastastic disease as an
incurable disease, so where do we stand
in 2008: Can pulmonary metastasectomy be curative and prolong survival?
Many studies on pulmonary metastasectomy were discontinued, because
patients, so far, do not accept randomized trails to reassess evidence levels in
this field. Thus, the clinical evidence for
pulmonary metastasectomy relays on
data, chiefly deriving from retrospective
trials and case series.
Indication for pulmonary
metastasectomy
The most important factor influencing
the use of surgical resection as the pri-
Joachim Pfannschmidt
mary treatment for pulmonary metastases is, how effective chemotherapy is
for a particular type of cancer, and
whether the natural history is to metastasisze predominantly to the lung or to
disseminate wildly.
For different tumors, not susceptible
to systemic therapy, pulmonary metastasectomy is recommended. For a subset of highly selected patients with colorectal cancer, the overall results of a
5-year actuarial survival rate ranged
between 38.3% and 63.7%, as being
reported in the literature. These outcomes exceed those normally associated with metastatic colorectal cancer
The Cold, Bright Future
Capturing the enormous unmet need with cryoablation
A
ccording to estimates
from the European
Commission, by 2050
the number of people over 60
in Europe will have doubled to
40% of the total population.
This trend corresponds to an
expected increase in the incidence of structural heart disease and delivery of procedures conducted by cardiac
surgeons. More specifically, the
treatment of atrial fibrillation
with device procedures is
increasing in Europe at a rate
of 12%, growing to an estimated 102,000 procedures by
2012. Of these, an estimated
17% will be performed by surgical ablation.
These projections include
those expected to be treated,
but do not address the number of patients with atrial fibrillation left untreated. For example, in the U.S. there are an
estimated 3,000,000 individuals with atrial fibrillation and
only 1% are currently treated
with surgery and catheter
ablation. Similarly, there are
approximately 5,000,000 more
with heart failure. In other
words, there are 3,000,000
people with AF and 5,000,000
more with heart failure and
99% of them are treated with
drugs that are famously suboptimal.
If satisfactory surgical therapies were developed, patient
care would be enhanced significantly. The development of
effective stand-alone or sole
and are well comparable with surgical
resection for colorectal liver metastases.
Pulmonary resection also remains the
only effective treatment for pulmonary
metastases from soft tissue sarcomas.
Five-year survival rates are reported
between 25% and 37.6%, since 1990.
For pulmonary metastatic disease in
renal cell carcinoma, several studies
have been published and the overall 5year survival figures reported range
from 21% to 60%.
Dramatic improvements in the
chemotherapy of breast cancer made
pulmonary metastasectomy an uncommon form of therapy. Outside of the
unusual circumstance of a solitary nodule or a limited disease confined to one
lobe, most patients would now be
treated nonsurgically. Advances in the
systemic therapy of osteogenic sarcomas influenced indication for surgery in
a multi-disciplinary approach. Also
metastatic germ cell cancer is today primarily treated with systemic therapy.
The role of pulmonary resection is now
to remove residual tumor and to determine residual tumor cells.
therapy procedures in the
treatment of AF would meet
enormous unmet patient
needs. Only innovation and
new ideas can create the basis
for these surgical therapies.
Fortunately the potential for
innovation in cardiac surgery is
unusually strong at this time in
our history.
Innovation for a less
invasive future.
Advancements in cryoablation
technology by ATS Medical
provides best-in-class alternatives for an envisioned less
invasive reality. As mentioned
above, despite almost a
decade of experience, only 1%
of all patients in the U.S. with
atrial fibrillation are currently
treated by catheter ablation
and surgery combined. This
lack of growth speaks to the
persistently high failure rate
ATS CryoMaze™ Probe
and questionable safety of
catheter ablation techniques
and to the unacceptable
degree of invasiveness of socalled “minimally invasive” surgery for atrial fibrillation.
The original cut-and-sew
Maze procedure was capable
of curing over 90% of all
patients with AF when performed correctly. Because
cryosurgery has been shown to
achieve similar success rates, it
is encouraging to attest to the
ongoing trials using the ATS
CryoMaze™ Surgical Ablation
System in a truly minimally
invasive approach, the ease
with which it can be adopted
by surgeons and the potential
it holds for treating the significant patient population currently under-treated for atrial
fibrillation.
ATS Medical will present a
symposium titled “Frontiers in
Cryoablation: The Rationale for
Lesion Patterns and
Cryosurgery” on Monday, 15
September from 12:24 – 14:00
in Room 5C of the Lisbon
Congress Centre. Open to all
registered attendees, the program will include presentations
of cryoablation experiences by
Pia Mykén, MD, PhD, Sweden
and Michael Andrew Borger,
Germany as well as a presentation from James L. Cox, MD,
United States on “Surgery for
Atrial Fibrillation Physiologic
Basis and Future Approaches.”
Resection for patients initially
diagnosed with N3 lung cancer
after response to induction therapy
Professor Erino Rendina, Professor and Chief of
Thoracic Surgery, University La Sapienza,
Ospedale Sant’Andrea, Roma, Italy
L
ung cancer is classified as N3 when metastases to the contralateral mediastinal and
hilar lymph nodes, the supraclavicular
nodes, and the scalene nodes are present at the
time of diagnosis. N3 lung tumors have been
included in stage IIIB since 1986, when it
appeared clear that such locally advanced disease need to be grouped in a separate stage III
category because of
the extremely poor
prognosis. In the
large series reported
by Mountain, 5-year
survival for N3
patients was 3%.
These tumors have
always been considered inoperable due
to the difficulties in
eradicating all the
detectable disease
Erino Rendina
that markedly limits
the applicability of primary surgery in this setting. Attempts to approach N3 lung cancer
aggressively with surgery including bilateral
lymphadenectomy as first line treatment, have
offered limited survival benefit discouraging the
choice of primary operation.
Bimodality protocols of chemotherapy combined with definitive thoracic irradiation represents, at the moment, the standard treatment of
care for N3 and all stage IIIB patients. With this
combined modality therapy the expected 5-year
survival ranges between 10% and 15%.
However, this treatment achieves tumor sterilization in only 5% to 20% of the patients and
locoregional failure is almost the rule with a
local control of 17% at 1 year in randomized
studies.
Basing on the evidence of the prognostic
advantage achieved by the use of neoadjuvant
therapy in surgically treated IIIA-N2 patients, in
the last two decades, carefully selected IIIB
patients including N3 cases have been enrolled
in a small number of phase II trials exploring the
potential benefits of surgery after aggressive
chemotherapic or radiochemotherapic treatment.
Worldwide published experiences in this field
generally differ for restaging methods
employed, because pathological re-evaluation of
lymph nodal status is performed only in a few
series, and for heterogeneity of surgical technique, because the exploration of the contralateral mediastinum is only rarely carried out.
Moreover, separate analysis for the survival of
N3 and T4 patients is not systematically reported.
Although including limited number of N3
patients, these studies report interesting results
with complete resection rates ranging between
25% and 77% and 5-year survival up to 28% for
the entire IIIB group. In the few studies reporting separate results for the N3 patients, the 5year survival of this group ranges between 17%
and 28%. Patients undergoing complete resection have shown a definetly better prognosis (up
to 43% 5-year survival). Significant improvement
in survival rates (20-30% increase at 5 years) has
been observed in patients experiencing lymph
nodal downstaging to N0-1 status after induction therapy.
However, the strong impact on toxicity and
surgical complications of the aggressive currently employed multi-modality treatments has indicated that enrolment in these protocols should
be strictly limited to patients with good performance status.
These results suggest that therapeutic nihilism
in the face of N3 patients may partially be overcome, since in carefully selected series, surgery
associated with currently available chemo-radiotherapy may prove able to cure a meaningful
rate of patients, which is a better rate than that
obtained without surgery. Since the long term
survival improvement may average about 10%
when compared with historical controls without
surgery, future comparative analyses are awaited to assess whether this advantage could be
confirmed in randomized studies.
Focused exclusively on cardiac
surgery, ATS Medical is dedicated to
developing and delivering innovation
that advances the standard by
fundamentally re-thinking the
way cardiothoracic products and
technologies are designed.
The events on our agenda provide an
ideal opportunity to get a detailed look
at the innovation taking cardiothoracic
surgery to the next level. Welcome.
: Frontiers in Cryoablation:
The Rationale for Lesion Patterns and Cryosurgery
ATS CryoMaze™ Symposium
Presenters: Niv Ad, MD t Pia Mykén, MD, PhD
Michael Andrew Borger, MD, PhD t James L. Cox, MD
Monday, 15 September 2008 t 12:45 –14:00
Lisbon Congress Centre t Room 5B
: Anticoagulation of Mechanical Valves and
Our ATS Open Pivot ® Experience
Presenter: Guido J. Van Nooten, Prof. MD, PhD
Tuesday, 16 September 2008 t 10:45 t Booth 2.24 – 2.25
: ATS 3f ® Revolution Symposium
Presenters: James L. Cox, MD t Ravi Pillai, MD, FRCSED, FRCS
Xu Yu Jin, MD, PhD, FACC, FRCS
Sven Martens, MD, PhD
Tuesday, 16 September 2008 t 12:45 –14:00
Lisbon Congress Centre t Room 5C
ATS Medical—Booth 2.24 – 2.25
Providing life-sustaining solutions for your patients: ATS Open Pivot® Heart Valves t ATS 3f® Aortic Bioprosthesis
ATS Simulus® Annuloplasty Repair Rings and Bands t ATS CryoMaze™ Surgical Ablation System
ATS 3f® Aortic Bioprosthesis is not available for sale in the United States.
www.atsmedical.com
6 September 08 EACTS Daily News
Perfusion
The use of cell saver
Perfusion timetable
Organiser
A Wahba, Trondheim
Session 1
Minimised cardiopulmonary
bypass
Moderators A Wahba, Trondheim;
S Tisherman, Pittsburgh
09:00 Off-pump coronary artery bypass vs. Miniextracorporeal circulation – is there a
V Mazzei, Messina
difference?
09:20 Complex surgery using minimised
A Liebold, Rostock
extracorporeal circulation
09:40 Use of cell saver: pros and cons
G Asimakopoulos, Bristol
10:00 Coffee
Session 2 Basic science in perfusion
Moderators M Karck, Heidelberg;
A Liebold, Rostock
10:30 Augmenting venous return in minimally invasive
heart surgery
L von Segesser, Lausanne
10:50 Complications of vacuum-assisted drainage
J Horisberger, Lausanne
11.20 Portable cardiopulmonary support during
normothermic cardiac arrest
S Tisherman, Pittsburgh
11.40 Hypothermic preservation for traumatic cardiac
S Tisherman, Pittsburgh
arrest
12:00 Lunch
Cardiopulmonary bypass in
noncardiac surgery
Moderators J Horisberger, Lausanne;
D Birnbaum, Regensburg
13:00 Perfusion strategies in thoracoabdominal
aneurysm surgery
M A Schepens, Nieuwegein
13:30 Perfusion strategies in pulmonary
D Jenkins, Papworth
endarterectomy
14:00 Selective cerebral perfusion in aortic surgery
M Karck, Heidelberg
Dr George Asimakopoulos
Consultant Cardiac Surgeon, Bristol
Royal Infirmary, UK
C
ell salvage with a cell saver and
autotransfusion is a method
used in situations characterised
by the loss of one or more units of
blood. Cardiac surgery accounts for
approximately 10% of all homologous
blood transfusions by the National
Blood Service in the UK. In the present
era of declining blood donation and
concern regarding the use of homologous blood, alternative methods are
becoming imperative.
Cell salvage may be used intra-operatively or post-operatively and can involve
washed or unwashed blood. The
Cochrane review on cell salvage recognis-
es that washed cell saver blood is superior to unwashed blood. In the washed
version, blood is collected with a double
lumen suction tubing and is mixed with
anticoagulant solution. Collected blood is
washed with saline while red cells are
separated with centrifugation prior to
autotransfusion. Cell salvage can be
achieved via continuous or intermittent
flow centrifugation. Furthermore, some
modern autotransfusion systems are able
to provide separation of red cells and
platelets. Platelet rich plasma can then be
used as a haemostatic aid.
Advantages of autotransfusion are
related to the reduction of homologous
transfusion and risk for infection and,
also, cost. Potential concerns include
inflammatory response in the salvaged
blood, fat embolism affecting neu-
rocognitive function, haemolysis and
depletion of clotting factors.
In the Society of Thoracic Surgeons
and Society of Cardiovascular
Anesthesiologists Guideline on blood
conservation and transfusion, published
in 2007, the ‘routine use of red cell saving’ is recommended as it is ‘helpful for
blood conservation in cardiac operations using CPB, except in patients with
infection or malignancy’ (Class I, Level
of evidence A).
Blood cell activation is a potential risk
of cell salvage. Expression of inflammatory mediators, such as IL-6 and IL-10 in
plasma, and also CD-11b and TLR-2
and -4 on neutrophils and monocytes,
increases within cell saver blood after
aspiration. Most plasma cytokines are
removed by centrifugation while no systemic inflammatory effects can be
attributed to autotransfusion. Most of
the relevant studies though include
patient receiving small volumes of autotransfused blood.
Two recent Canadian studies aimed to
address the issue of neurocognitive dysfunction after cardiac surgery in relation
with the use of cell salvage. Interestingly,
the use of continuous cell salvage in one
study was associated with reduced rates
of dysfunction post-operatively.
The STS/SCA guideline mentioned
above recognises that excessive of cell
saving may lead to loss of coagulation
factors and platelets resulting in haemorrhagic diathesis. Furthermore, the use
of a cell saving device may not be cost
effective in low risk patients with small
amount of intra-operative blood loss.
Despite the advantages of cell saving,
the perfect system is still eluding us.
Further research and development of
modern cell saver systems aims to alleviate the potential avers effects of the
technique.
Historical review of cerebral protection in aortic arch surgery
and the perspective of antegrade selective cerebral perfusion
Session 3
Session 4 Left heart assist
Moderators A Fiane,Oslo; D Jenkins, Papworth
14:30 Short-term heart assist with impeller pumps
H Granfeldt, Linköping
14:50 Levosimendan in reduced left ventricular
D Nordhaug, Trondheim
function
15:10 Long-term heart assist with impeller pumps
A Fiane, Oslo
15:30 Adjourn
Matthias Karck and Hiroyuki
Kamiya, Department of
Cardiac Surgery, University
of Heidelberg, Germany
T
he treatment of aortic
arch aneurysms by aortic
replacement was first
attempted in the 1950s utilizing temporary shunts or selective perfusion of the
supraaortic vessels to maintain cerebral circulation.
However, results in the following years were disappointing and the repair of these
lesions was essentially abandoned until 1975, when
Griepp et al. showed that aortic arch repair is possible using
HCA alone. In the 1980s, most
surgeons used hypothermic
circulatory arrest (HCA) only,
and reproducible operations
on the aortic arch became feasible. It became clear, however,
that hypothermia alone does
not provide unlimited cerebral
protection.
In the late 1980´s, Bachet
and Kazui presented their clinical series with antegrade selective cerebral perfusion (SCP)
and Ueda reported his initial
experience with retrograde
cerebral perfusion (RCP), both
Techno-College 2008…and the winner is…
C
ongratulations go to JeanMarie Vogel who received
the 2008 Techno-College
Award for the LeGooTM Internal
Vessel Occluder (Pluromed, Inc.).
According to Vogel, the device is
the only true atraumatic device
for temporary occlusion of blood
vessels during vascular surgery
procedures.
LeGoo is made of a biocompatible, aqueous, reverse thermosensitive polymer. At lower tempera-
tures, LeGoo exists as a liquid. At
body temperature, LeGoo rapidly
changes to a viscous gel in a
reversible phase change. When
injected into a blood vessel,
LeGoo forms an occluding plug at
the injection site. The occlusion is
designed to last for the duration
of an average anastomosis,
though a subsequent injection
can prolong the duration of occlusion if needed, and flow can be
fully restored instantly by cooling
the vessel and dissolving the gel.
Once dissolved, it can never resolidify and there has been no
evidence in clinical or preclinical
experience of any tissue damage
related to a LeGoo plug. LeGoo
has been extensively studied for
microvascular reactivity and its
inability to cause micro-infarcts.
LeGoo is neither absorbed nor
metabolized: it passes through
the microcirculation and is excreted in urine.
Hiroyuki Kamiya
as an adjunct to hypothermic
circulatory arrest for the repair
of aortic arch pathologies.
Following Ueda´s report, RCP
Because LeGoo conforms to
any vascular geometry, the surgeon can ‘clamp’ without clamping and achieve a completely
bloodless surgical field without
fear of damaging fragile or calcified blood vessels. LeGoo also
prevents back bleeding from sidebranches or collaterals. Because
LeGoo temporarily stents the vessel and allows for suturing directly through the gel, it facilitates
construction of the anastomosis.
LeGoo does not need to be
removed before completing the
Matthias Karck
became popular and routine in
many institutions in the 1990´s
because of technical simplicity
despite a lack of adequate
anastomosis; upon completion,
LeGoo is dissolved by applying
ice directly to the vessel.
LeGoo is CE-Marked and is
already in clinical use in 2008 in
France, Germany, The
Netherlands, Spain, and
Switzerland. The first clinical
applications of LeGoo, at that
time, include off-pump and onpump coronary artery bypass surgery, femoral bypass, arteriovenous fistula for hemodialysis
patients, and temporary occlusion of the iliac artery.
Surgeons at SIS-E Symposium call for action on surgical site infections
S
urgical Site Infection (SSI) causes considerable
patient mortality and morbidity and has major
economic consequences. That was a key finding
of surgeons who met at the 2nd EMEA Symposium
on ‘New non-pharmaceutical ways to reduce surgical
site infection’ held in Turkey recently.
Surgeons from across Europe shared experiences
on how Kimberly-Clark’s InteguSeal* microbial
sealant (www.integuseal.com), a new, innovative
solution, helps to reduce SSI. Data from two studies
presented at the symposium demonstrated the clinical efficacy of InteguSeal* in reducing wound contamination and infection.
SSI most important problem facing
surgeons
The symposium, part of the 21st Surgical Infection
Society of Europe meeting, was opened by keynote
speaker Professor Miguel Cainzos, Professor of
Surgery and General Surgeon in Santiago de
Compostela in Spain. He said: “Surgical Site Infection
is today the most important problem facing surgeons.
Post operative infections not only destroy the surgeon’s technical work but they also increase postoperative morbidity and mortality whilst reducing the
quality of surgery and hampering the daily running of
surgical departments.”
The presentation from Professor Cainzos was one
of seven made at the Symposium.
He went on to outline to delegates how more
patients suffer from surgical site infections (SSI) than
previously thought with infection rates ranging from
1.4% up to 22%1 depending on the procedure, contamination and physical status of the patient.
Presenters at the 2nd EMEA Symposium on ‘New non-pharmaceutical ways of controlling surgical site infection.
From left to right: Professor Per-Olof NystrÖm – general surgeon from the Karolinska Hospital in Stockholm, Dr. Privat-Dozent
Pascal Dohmen – cardiac surgeon in the Department of Cardiovascular Surgery at the Charité University Hospital in Berlin,
Dionysios Voros – Professor of General Surgery at the University of Athens Medical School and a founding member of the
Surgical Infection Society of Europe, Professor Metin Çakmakçi – currently President of the Surgical Infection Society of
Europe, is Medical Director of the Anadolu Medical Centre in Istanbul, Samuel E. Wilson MD – Professor of Surgery at the
University of California, Irvine, Steve Bell – independent consultant from the Agent for Medics Group, Dr Lynne Kelley – a
general and vascular surgeon and former Assistant Professor of Vascular Surgery at Yale University, is Global Medical Director
Vice President for Kimberly-Clark Healthcare, Miguel Cainzos – Professor of Surgery and General Surgeon in Santiago de
Compostela is a former President of the Surgical Infection Society of Europe and currently Chairman of their Education
Committee. He is one of the foremost authorities on surgical infection.
Procedures to prevent SSI frequently
neglected
In his presentation, Professor Metin Çakmakçi, currently President of the Surgical Infection Society of
Europe and Medical Director of the Anadolu Medical
Centre in Istanbul, referred to US studies that show
that basic procedures to prevent SSI are neglected in
around 50% of patients2.
Further information from the US was presented by
Professor Samuel Wilson, Professor of Surgery at the
University of California, Irvine. He explained that if
experimental data.
However, the “main stream”
of cerebral protection in surgery on the aortic arch has
shifted from RCP to SCP, with
recognition that RCP does not
provide enough manipulation
time for the repair of extended
aortic arch pathologies.
Nowadays, SCP is used by
about 80% of surgeons.
However, aortic arch surgery is still a high risk procedure even with SCP, and there
remains controversy and space
for improvement of this technique, including temperature
management, and surgical
technique. Here detailed evidence, perspectives, and
future directions for improvement are discussed.
only 2% of patients undergoing joint prosthesis surgery in the US have a surgical site infection that adds
up to 12,000 a year at an average additional cost of
$30,0003. “The cost to health services around the
world adds up to billions of dollars”, he said.
InteguSeal* Cuts Infection Rates
It was Dr. Privat-Dozent Pascal Dohmen, a cardiac
surgeon in the Department of Cardiovascular Surgery
at the Charité University Hospital in Berlin, the largest
university hospital in Europe, that presented his per-
Jean-Marie Vogel
suasive new data about the use of InteguSeal* microbial sealant as a means of further minimizing SSI.
With the migration of normal skin flora into surgical
incisions recognised as the major source of wound
contamination, InteguSeal* works by reducing this
contamination by locking down bacteria to the skin
and thus helping to prevent infection. The microbial
barrier is made by a film-forming cyanoacrylate liquid
that dries within a few minutes of application to the
skin. Dr Dohmen data on 910 patients suggests that
using InteguSeal* microbial sealant cuts infection
rates in bypass surgery patients from 4.6% to 1.1%4.
“I was convinced of the benefits of the product and
we have seen a dramatic fall in the rate of surgical
site infection since we began using InteguSeal* in my
patient population”, he explained.
In conclusion the meeting agreed that surgical site
infection is a complex problem and will not have a
simple solution. There is a need for further research, a
clearer understanding of what is, and is not, an infection and unequivocal data on the clinical efficacy of
new measures to reduce SSI. The speakers and participants commented that InteguSeal* is a valuable new
non-pharmaceutical tool for protecting patients from
postoperative infection.
Dr. Privat-Dozent Pascal Dohmen will be presenting
his latest study findings about InteguSeal* at EACTS
on 15th September at 12.45pm.
References
1) NNIS System report for 1992 – 2001. Surgical site infection risk stratification by type of surgery. Issued August 2001. Am J Infect Control
2001; 29(6): 404 – 421
2) Bratzler DW, Houck PM, Richards C et al. Use of antimicrobial prophylaxis for major surgery. Arch Surg 2005; 140: 174 – 182
3) Darouiche RO. Clinical and economic consequences of surgical
implant infection. N Engl J Med 2004; 350: 1422 – 1429
4) A preliminary study of InteguSeal* use in patients undergoing cardiac surgery to prevent surgical site infections. Clinical abstract,
European Society for Cardiovascular Surgery, 57th ESCVS
International Congress, Barcelona, Spain, April 24-27, 2008
Join our symposium on “new non pharmaceutical ways to reduce SSI” at the EACTS
congress this Monday 15th September 2008 at 12:45pm to hear Dr. Privat-Dozent
Pascal Dohmen, cardio-vascular surgeon at the Charite Hospital in Berlin. He will reveal
how he has achieved a dramatic fall in the rate of SSI (with statistical significance) since
he began using InteguSeal* and how it leads to a reduction of secondary cost.
8 September 08 EACTS Daily News
Endovascular Intervention
Endovascular intervention
timetable
Organisers
F Beyersdorf, Freiburg, L K von
Segesser, Lausanne
Session 1
Retrograde endovascular
techniques
Moderators J Bachet, France,
L K von Segesser, Lausanne
09:00 Surgical training programs for endovascular
H-G Wollert, Karlsburg
aortic stenting
09:20 Indications and contraindications for
endovascular treatment of abdominal aortic
P Tozzi, Lausanne
aneurysms
09:40 Indications and contraindications for
endovascular treatment of thoracic aortic
aneurysms
J Kobba, Freiburg
10:00 Overstenting of the left subclavian artery is
without risk
K B Zipfel, Berlin
10:30 Coffee
Session 2
11:00
11:20
11:40
12:00
12:30
Retrograde endovascular
techniques (continued)
How to prevent complications after overstenting
of the left subclavian artery
F Beyersdorf, Freiburg
Hybrid approach for thoracoabdominal
endovascular aneurysm repair E Weigang, Mainz
Development of branched or fenestrated aortic
stents
G Torsello, Münster
Indications and contraindications for
endovascular aneurysm repair
E Diethrich, Phoenix
Lunch
Session 3
Antegrade endovascular
techniques
Moderators F Beyersdorf, Freiburg;
C Mestres, Barcelona
13:30 The frozen elephant trunk A Haverich, Hannover
13:50 Two-stage hybrid approach for total arch
M Czerny, Vienna
replacement
14:10 One-stage hybrid approach for total arch
M Siegenthaler, Pittsburgh
replacement
14:30 Trans-apical aortic valve replacement with
angiographic assessment
A P Kappetein, Rotterdam
14:50 Trans-apical aortic valve replacement with
intra-cardiac ultrasound
L K von Segesser, Lausanne
15:10 Trans-apical aortic valve replacement with
3-D echocardiography
T Walther, Leipzig
15.30 Adjourn
Indications and
contraindications
for EVAR of AAA
Piergiorgio Tozzi
Center Hospitalier
Universitaire Vaudois,
Department of
Cardiovascular Surgery, Rue
du Bugnon, Lausanne
46/1011, Switzerland
C
urrent evidence on the
efficacy and short-term
safety of stent-graft
placement in abdominal aortic
aneurysm appears adequate
to support the use of this procedure not only in patients
who would normally be considered unfit for open surgery
because of high operative risk,
but also in active patients that
ask for all the advantages of a
minimally invasive procedure
such as short hospital stay and
no sexual dysfunction, and
understand the long-term
uncertainties and potential
long-term complications associated with the endovascular
repair. AAA anatomy still
drives the choice of the
endovascular approach and is
the main determinant of successful EVAR.
With the existing devices,
the EVAR is indicated when
the neck has a cylindrical
shape with a maximal diameter below 30mm, a landing
zone longer than 15mm and
an angle below 60°; the angle
between the two iliac axes is
below 100°; at least one of
the distal common iliac artery
is free from disease so that
the occlusion of both
hypogastric arteries is not necessary; both iliac and femoral
axes allow the passage of at
least 20 F catheters. However,
the design of endoprostheses
and their delivery system is
constantly improved leading
to consequent change in the
anatomic criteria for endovascular repair. New generation
of fenestrated and branched
endoprostheses allow the
repair of AAA with virtually no
neck.
Reasons for unsuitability for
EVAR are mainly anatomic
and have considerably
changed over the time.
Specifically, inadequateness of
arterial access, presence of
extensive iliac artery aneurysm
and/or inadequateness of
proximal neck considerably
decreased in the last 5 years.
This is mainly due to the
improvement of the surgical
and endovascular technique
and to the evolution of the
stent design.
Contraindications to the
EVAR that are not linked to
anatomic constrains are few.
An inflammatory aneurysm
used to be an absolute contraindication to EVAR till the
results from the EUROSTAR
registry suggested the opposite, but this issue is still open.
Social and/or personal factors
that prevent the patient to be
enrolled in the follow-up program and allergy to nickel
should be considered absolute
contraindications to EVAR.
How to prevent complications
after overstenting of the left
subclavian artery
Professor Friedhelm
Beyersdorf
University Medical Center
Freiburg, Dept. of
Cardiovascular Surgery,
Hugstetter Strasse 55, 79106
Freiburg, Germany
ndovascular stent-graft
implantation (ESI)
requires suitable proximal and distal “landing
zones” for stent-graft fixation. If the distal aortic arch
is affected, overstenting of
the left subclavian artery
(LSA) can be performed to
elongate the proximal “landing zone”. Few cases have
been published reporting
adverse neurological events
after overstenting of the left
subclavian artery
(Tiesenhausen et al., Journal
of Cardiac Surgery
2003;18:429-35.) Our group
has evaluated (Weigang et
al., EJCTS,31;2007:628-36)
E
whether overstenting of the
LSA is associated with a
higher rate of neurological
complications and peripheral
symptoms by focusing on
management of supra-aortic
vessels.
Twenty patients suffering
from aortic arch aneurysms
(n=3), descending aortic
aneurysms (n=7), acute
(n=6) and chronic (n=4)
type-B aortic dissections
underwent stent-graft
repair with complete (n=14)
or partial (n=6) overstenting of the left subclavian
artery. Three patients
underwent overstenting of
the entire aortic arch with
ascending aortic-bi-carotid
bypass grafting. One
patient with right carotid
and vertebral artery occlusion underwent initial
carotid-to-subclavian
bypass. All patients subse-
Optimal organ protection for the treatment
of complex thoracic aortic aneurysms using
the frozen Elephant trunk technique
Professor Axel Haverich, Hannover , Germany
T
he ‘frozen’ elephant’ trunk technique allows for
single stage repair of combined aortic arch and
descending aortic aneurysms using a
‘hybrid’prosthesis with a stented and a non-stented
end. The combination with improved protection
strategies such as selective antegrade cerebral perfusion as well as lower body perfusion allows approaching even complex pathologies. The newly designed
introduction device for the stented part of the prosthesis has further improved the feasibility of the
device. This report summarizes the operative- and fol-
low-up data (mean follow-up: 20. months) with this
new treatment.
Between 09/01 and 7/08, 54 patients (61 years; 19
female) with different aortic pathologies (27
aneurysms, 27 aortic dissections) were operated on
after approval by the local institutional review board.
The stented end of the hybridprosthesis was placed
through the openend aortic arch under fluoroscopic
control using hypothermic circulatory arrest (28°C) and
selective antegrade cerebral perfusion (14°C). In cases
with anticipated HCA times of more than 40 minutes,
a lower body perfusion was initiated to reduce spinal
and other end organ ischemia. This approach allows to
Axel Haverich with Hybrid prosthesis
perform complex procedures such as the use of
brached grafts or extraanatomical repairs.
All patients survived the procedure. 7 pts (13%) died
early postoperatively, with 2 fatalities directly procedure
related in the early experience. Eleven percent (6pts)
showed new postoperative neurological deficits, in two
of them symptoms resolved completely before discharge.
In one of them, the descending aorta was perforated
due to misplacement of the stented end of the hybrid-
Friedhelm Beyersdorf
quently underwent neurological examination and
Doppler ultrasound for
detection of neurological
and peripheral vascular
complications.
Our results show that
overstenting of the LSA as
treatment of aortic pathologies in high-risk patients is
feasible but associated with
the risk of neurological complications and peripheral
symptoms. Detailed preoperative exploration of vascular anatomy and pathology
via Doppler ultrasound, CTor MRI Scan is mandatory to
avoid adverse neurological
events. Prior surgical revascularization of the left subclavian artery is essential in
patients with high-grade
stenoses, occlusions, or
anatomic variants of the
supra-aortic branches.
prosthesis. In 32/35 pts (91.4%) with postoperative CTimaging (> 6 months post op) complete thrombus formation around the frozen elephant trunk was observed.
This procedure is performed via a median sternotomy and combines the concepts of the elephant trunk
principle and endovascular stenting of descending aortic aneurysms. In conjunction with special techniques
to avoid ischemia of the brain and other organs even
complex pathologies can be repaired. Due to sophisticated selective perfusion techniques deep hypothermia
and therefore prolonged CPB times can be avoided.
Favourable intraoperative and postoperative results in
the follow up with regard to thrombus formation
around the stented descending aortic segment encourage us to evaluate all patients with thoracic aneurysms
extending proximal and distal of the left subclavian
artery for this treatment. Furthermore it seems feasible
that the majority of patients presenting with AADA
may be treated with this approach in the future.
Perfusion
Perfusion strategies in pulmonary endarterectomy
Mr David P Jenkins
Papworth Hospital, Cambridge, UK
n today’s postgraduate course,
David Jenkins will discuss perfusion
strategies in pulmonary thromboendarterectomy (PTE) surgery. The principle of this procedure is a full
endarterectomy into subsegmental
pulmonary artery branches to restore
blood flow and reduce pulmonary
hypertension. Even on cardiopulmonary bypass, there is often substantial collateral flow from the bronchial
circulation and therefore perfusion
strategies have been developed to
allow a clear field for dissection.
Pulmonary endarterectomy, as practiced today, was mainly developed at
the University of California in San
Diego. Over the last 20 years further
centres have initiated programmes
with significant experience now present in France, Germany, Italy and the
UK. It is the treatment of choice for
I
patients with chronic thromboembolic
pulmonary hypertension with the
expectation of substantial symptomatic and prognostic improvement.
Many of these patients have class III
to IV symptoms of breathlessness and
a life expectancy of less than 5 years
without surgery. Although it retains
the aura of high risk, complex,
demanding surgery, the actual hospital mortality for most patients is currently <5% in experienced institutions.
The standard technique involves
core cooling on cardiopulmonary
bypass to 20°C, with periods of up to
20 minutes of circulatory arrest during
which one side of the endarterectomy
can be performed. This allows optimum operating conditions and usually
only two arrest periods are necessary.
Unlike circulatory arrest in aortic and
congenital surgery, reperfusion can be
initiated at any stage so the arrest
period can be controlled.
David Jenkins and PTE specimen
As hospital survival has improved,
more attention has been turned to
morbidity and prognosis following PTE
surgery. Although the neurological
outcome with the standard technique
is subjectively good in most patients
with extubation on the first post operative day and the absence of delerium
the expectation, full neuropsychological testing has not been reported.
Following a similar trend in aortic surgery, a number of European centres
have investigated performing PTE with
less profound cooling and/or maintenance of cerebral perfusion. Whilst the
modern trend is in favour of less invasive surgery some have argued that
for complete PTE, core cooling and circulatory arrest remain essential.
It is therefore important that these
apparent advances are compared with
the established technique and the
effectiveness of the surgical clearance
(reduction in pulmonary hypertension
achieved) and neuropschological outcome carefully evaluated.
At Papworth hospital we believe systemic hypothermia is required for safe
PTE. However, we do not think that
complete circulatory arrest is necessary
in all patients. We have developed a
technique to allow continued cerebral
perfusion by cross clamping the aortic
arch distal to the left carotid artery. The
patient is not exanguinated, but there
is a significant reduction of the circulation to the remainder of the body apart
from the right arm and head.
This situation limits blood flow in
the bronchial and coronary arteries
and provides a relatively bloodless
field to allow thorough endarterectomy in the majority of patients.
If further visualization is required it
is safe and easy to resort to conventional circulatory arrest to complete
the dissection. We now have an institutional experience of well over 400
endarterectomy procedures, and we
are currently investigating whether
avoidance of circulatory arrest has any
advantage for patients undergoing
PTE. We are half way through a randomized controlled trial to compare
conventional circulatory arrest and our
cerebral perfusion technique with full
neuropsychological assessment, pulmonary hypertension evaluation and
extended follow up. This pulmonary
endarterectomy cognitive function
(PEACOG) trial is funded by an independent grant from the Moulton
Foundation UK. We hope that this
study will answer some of the present
controversies in perfusion strategies
for PTE surgery.
EACTS Daily News September 08 9
Maquet Cardiovascular launches
HEARTSTRING III proximal seal system
for coronary artery bypass graft surgery
Innovative technology eliminates the need for an aortic
clamp reducing the risk for cerebral emboli and potentially
improving patient neurocognitive outcomes
S
an Jose, CA – April 14, 2008 MAQUET Cardiovascular LLC today
announced the launch of HEARTSTRING III Proximal Seal System for coronary artery bypass surgery procedures. This
latest version of MAQUET’s innovative
HEARTSTRING proximal seal technology
allows surgeons to perform coronary
artery bypass grafts without the use of a
partial occlusion clamp during beating
heart surgery.
“We firmly believe that off-pump beating heart surgery results in better patient
outcomes. The HEARTSTRING device provides a means to reduce aortic manipula-
tion, a well-appreciated risk factor for
adverse neurologic complications in coronary artery bypass,” said John D. Puskas
M.D., Chief of Cardiac Surgery at Emory
Crawford Long Hospital and Professor of
Surgery. “With its unique features and
improved delivery system, the new HEARTSTRING III system makes it easier for the
cardiac surgeon to perform a clampless
proximal anastomosis for either saphenous
vein or radial artery conduits.”
The HEARTSTRING III system features an
improved seal loader and delivery device
for fast, easy placement. Once deployed, it
maintains a low compliant profile for opti-
mal hemostasis at the anastomotic site.
The HEARTSTRING III system enables surgeons to use their own hand-suturing
technique for creating a proximal anastomosis with either venous or arterial grafts.
With its elegant design and small operational footprint, there is no foreign material left inside the vessel after completion of
the anastomosis. The Aortic Cutter makes
a single, clean hole in the aorta for graft
placement. The HEARTSTRING III system
allows for maximum surgical flexibility.
Surgeons have the option to perform distal or proximal grafts first and to use
grafts of varying lengths, hooded grafts,
and angled take-offs.
Mark W. Connolly, M.D., Director of
Cardiovascular and Thoracic Surgery at
Saint Michael's Medical Center University
Heights stated, “St. Michael's is a busy,
high-volume institution that performs
almost exclusively off-pump, beating
heart CABG procedures. The HEARTSTRING III system provides an easy, reliable, and safe means of constructing
proximal anastomoses with significantly
reduced aortic manipulation. The new
seal loader takes HEARTSTRING’s userfriendliness to a new level.”
“The advancement of our HEARTSTRING product line represents yet
another development in our integrated
approach to providing innovative surgical
solutions for cardiac and vascular surgeons, perfusionists and their teams in
order to help patients live better and
longer lives,” said Patrick Walsh,
President of MAQUET Cardiovascular
LLC. “As a market leader, MAQUET continues to make significant investment
into the field of cardiovascular medicine
and we believe the benefits of clampless
beating heart surgery are very compelling for the future.”
The benefits of clampless beating heart
surgery, also known as off-pump coronary
artery bypass (OPCAB), include a quicker
recovery time, decreased length of hospital
HEARTSTRING III Proximal
Seal System for CABG
stay, less trauma due to the elimination of
the heart-lung machine and fewer cognitive and neurological consequences. This is
especially important for higher risk individuals who have medical conditions such as
diabetes, a history of stroke, or poor physical health.
Hybrid approach
for TAAA EVAR
MAQUET CARDIOVASCULAR GOES
CLAMPLESS WITH THE NEW
HEARTSTRING™ III PROXIMAL SEAL SYSTEM
Ernst Weigang
Ernst Weigang MD
Head of Endovascular Surgery
Department of Cardiothoracic and Vascular
Surgery, University Hospital Mainz,
Langenbeckstraße 1, 55131 Mainz, Germany
O
Optimizing the benefits of beating heart
surgery with the new HEARTSTRING III: This
latest generation HEARTSTRING III device from
MAQUET provides a simple option for CABG proximal anastomoses. It allows the hand-suturing
technique without either the cross clamp or the
side-biting clamp. The HEARTSTRING Proximal
Seal System is an easy-to-use advance in patient
care and helps reduce the release of emboli that
can potentially have neurocognitive consequences
for patients post-surgery.
Flexibility: Performs proximal and distal
anastomoses in any order
Versatility: Uses arteries or veins for grafts
of any size, length, or diameter
Adaptability: Allows for takeoffs at any angle
Safety: Designed to help reduce aortic
manipulation and embolic release
MAQUET – The Gold Standard.
MAQUET Cardiopulmonary AG
Hechinger Straße 38
D-72145 Hirrlingen, Germany
Phone: +49 (0) 7478 921-0
Fax:
+49 (0) 7478 921-100
info@maquet-cp.com
www.maquet.com
MEMBER OF THE GETINGE GROUP
pen surgical thoracoabdominal replacement remains complex and is associated
with significant morbidity and mortality
due to severe cardiac stress and organ
ischemia, with postoperative paraplegia and
renal dysfunction particular complications.
Complex aortic disorders such as extended thoracoabdominal aortic aneurysms (TAAA) are
often deemed unsuitable for EVAR alone
because of the proximal supraaortic vessels and
distal visceral branches.
Recent innovations in endovascular stentgraft technology have made endovascular
treatment in anatomically-challenging TAAAs
feasible and an alternative to open surgical
TAAA replacement. There has been an increasing number of reports on hybrid thoracoabdominal EVAR procedures with adjunctive open
surgical visceral artery revascularisation in the
international literature over the past 9 years.
Their results confirm the successful combination of open surgical visceral artery revascularisation and endovascular treatment for complex
TAAA pathology as a therapeutic alternative.
This innovative combination of simultaneous
conventional vascular surgery and thoracoabdominal EVAR thus reduces the operative risk
in treating TAAA patients with severe comorbidities. The procedure’s less invasive character
without thoracoabdomonal incision and extensive tissue dissection, avoidance of thoracotomy, single-lung ventilation, aortic cross clamping, abdominal organ ischemia, cardiopulmonary bypass, deep hypothermia and circulatory arrest are clear advantages of this method
over open TAAA replacement.
The hybrid approach for repairing TAAA is an
effective treatment for high-risk patients, and it
has the potential to reduce morbidity and mortality. These hybrid procedures can only be performed by surgeons in the operating room.
Mid-term therapeutic results are encouraging,
but long-term results remain to be seen.
Further studies with larger cohorts are mandatory to establish this alternative therapeutic
option for complex TAAA patients.
10 September 08 EACTS Daily News
Congenital timetable
Congenital Heart Disease
Organisers
Congenital Heart Disease
Committee Members
Session 1
Management of aortic arch
obstruction
Moderators B Maruszewski, Warsaw;
V Tsang, London
09:00 Aortic arch obstruction:
Morphology
A Cook, London
Advanced imaging
A Taylor, London
09:20 Approaches/techniques for coarctation repair (±
concomitant cardiac lesions)
A Wood, Dublin
09:40 Approaches/techniques for hypoplastic
arch/interrupted arch repair (± concomitant
F Lacour-Gayet, Denver
cardiac lesions)
10:00 Evidence-based medicine: Is there a superior
approach/technique?
M de Leval, London
10:20 Cardiologic management of late complications
(recoarctation, arterial hypertension)
J Hess, Munich
10:40 Surgical management of complex/recurrent
obstruction in adult patients G Stellin, Padova
11:00 Coffee
Session 2 Paediatric perfusion
Moderators G Sarris, Athens; C Schreiber,
Munich
11:30 Normothermic vs. hypothermic
cardiopulmonary bypass: rationale, strategies,
results.
11:30 Hypothermia is better
G Ziemer, Tuebingen
11.50 Normothermia is better
J Rubay, Brussels
12:10 Strategies to minimise systemic inflammatory
response syndrome (coated circuits, prime
issues, pharmacological interventions,
P Pouard, Paris
perfusion techniques)
12:30 State-of-the-art in deep hypothermic circulatory
arrest (techniques, monitoring, long-term
T Spray, Philadelphia
outcome)
13:00 Lunch
Interactive video session:
Aortic valve repair in congenital
heart surgery
Moderators J Comas, Madrid; R Prêtre, Zurich
14:00 Commissurotomy and leaflet thinning in a
critical neonatal aortic valve stenosis
V Hraska, Sankt Augustin
14:30 Repair of a leaking bicuspid aortic valve
G El Khoury, Brussels
in a child
15:00 Repair of the unicuspid aortic valve
H J Schäfers, Homburg
15:30 Repair of a subaortic ventricular septal defect
with aortic valve prolapse C Brizard, Melbourne
Invited discussants A Cook, London,
J Hess, Munich, D Cameron, Baltimore
16:00 Adjourn
Congenital
Early transatrial repair of tetralogy of
Fallot leads to a good late functional
outcome and normal life
Dr Giovanni Stellin
University of Padova Medical School,
Department of Cardiac, Thoracic,
and Vascular Sciences
Padova 35128, Italy
T
ransatrial repair of tetralogy of Fallot
(TOF) is proposed to avoid the deleterious effects of right ventriculotomy, chronic cyanosis and spells, systemicto pulmonary artery shunts, chronic right
ventricular hypertension, myocardial compensatory hypertrophy, and preserve right
ventricular function in the long term. Since
1990, in Padua, we employed early surgical repair in children of tetralogy of Fallot,
regardless the presence of symptoms.
We have retrospectively reviewed our
15 years experience, with 187 consecutive patients with “classic” TOF. Repair
was achieved in all by means of a
transatrial-transpulmonary approach,
including myotomy and myectomy of
the right ventricular outflow tract. The
ventricular septal defect was closed routinely through the right atrium. The right
ventriculotomy (if any) was confined to
the distal part of the infundibulum,
avoiding involvement of the body of the
right ventricle. The pulmonary valve was
preserved whenever pulmonary annulus
was adequate (Z-score > -2). Median
age at operation was about 3 months.
A systemic-to-pulmonary artery shunt
was performed only in 15 patients (8%)
with very low body weight or in critical
preoperative conditions. The right ventricular outflow tract (RVOT) was reconstructed by means of a transannular
patch in 72.8%. Hospital mortality
accounted for 7 patients (3.7%), with no
death in the last 5 years. At a mean follow up of 8 years (1-15 years, 82% completeness), there was one non-cardiac
related late death. All survivors are in
NYHA class 1, on sinus rhythm except for
1 patient with iatrogenic AV block. Late
reoperation was necessary in 12 pts (6.5
%) for residual pulmonary branch stenosis (6), and residual RVOT obstruction (6).
No patient required so far pulmonary
valve replacement. Freedom from any
reoperation or catheter intervention is
70% at 15 years. (main procedure
included pulmonary artery branches
dilatation). Echocardiographic assessment showed pulmonary regurgitation
more than mild in 4 patients, with global satisfactory right ventricular function.
Stress test (Bruce protocol) performed in
20 patients was within range of normality in 90%.
These encouraging results have led
us to routinely perform transatrial repair
within 3 months of age, regardless
presence of symptoms. In our experience, it has been feasible at any age,
with low operative risk, good hemodynamic result and a low incidence of
residual lesions. Late functional outcome appear satisfactory and a normal
life can be expected for these patients.
Session 3
Sorin Group announces
the publication of superior
21 year durability data
follow up with the
Mitroflow valve in the
Journal of Thoracic and
Cardiovascular Surgery
AUTOSUTURE™
ENDO GIA™ Universal Stapling System
t7FSTBMJUZUIBU4BWFT
t4VQFSJPS4UBQMF-JOF4FDVSJUZ
t/FX,OJGF#MBEFXJUI&WFSZ'JSJOH
S
orin Group, the largest European cardiovascular
company and world leader in medical technologies for cardiac surgery, announced today the
publication of 21 year durability with its Mitroflow
Aortic Pericardial Heart Valve.
The 21 year data represents the longest patient follow up ever published in the history of pericardial
valves. Biological valves have become an increasingly
viable option to replace native diseased valves since
they are designed to improve patient quality of life by
negating the need for lifelong anticoagulation therapy.
“To date, the Mitroflow pericardial bioprosthesis
has demonstrated excellent durability at 21 years”
said Prof. Charles Yankah, Associate Professor of
Surgery, Charité Medical University, Berlin, Germany
and Consultant CardioThoracic and Vascular
Surgeon, Berlin Herzzentrum, Berlin, Germany.
The Mitroflow Aortic Pericardial Heart Valve was
introduced in Europe in 1982. In over 20 years of clinical use it has demonstrated superior hemodynamic
performance and proven long term durability in a
design recognized by surgeons worldwide for its ease
of implant in even the most challenging anatomies.
COVIDIEN, COVIDIEN with logo, “positive results for life“
and ™ marked brands are trademarks of Covidien AG or its affiliate.
© 2008 Covidien AG or its affiliate. All rigths reserved.
S-LA-EGiaU/GB - 07/2008
12 September 08 EACTS Daily News
Basic Science
Basic Science timetable
The endogenous cell defence: organ
protection of the future
Organiser: J Vaage, Oslo
Session 1
Moderators: J Vaage Oslo; F Beyersdorf, Freiburg
09:00 Why is the endogenous cell defence, pre- and
post-conditioning, interesting in cardiothoracic
surgery?
F Beyersdorf, Freiburg
09:20 Which organs can be protected? J Vaage, Oslo
09:40 Early and delayed preconditioning –
mechanisms
D Yellon, London
10:30 Coffee
Session 2
Moderator D Yellon, London
11:00 Post-conditioning – mechanisms
J Vinten Johansen, Atlanta
11:50 Lunch
Session 3
Moderators G Valen, Olso; J Vinten-Johansen,
Atlanta
13:00 Similarities and differences in mechanisms of
pre- and post-conditioning D Hausenloy, London
13:30 Alternative methods and mechanisms of
increasing the endogenous cell defence
G Valen, Oslo
14.10 Coffee
Session 4
Moderators F Beyersdorf, Freiburg; J VintenJohansen, Atlanta
14:30 Clinical studies in cardiac surgery – present
status
M Tarkka, Tampere
15:00 Possible ways to exploit the endogenous cell
defence in surgery
J Vaage, Oslo
15.30 Adjourn
Would you give your right arm
to protect your heart?
Derek J Hausenloy & Derek M Yellon
The Hatter Institute and Centre for Cardiology,
University College London Hospitals and Medical
school, Grafton Way, London WC1E 6DB, UK.
E
very year in the UK, nearly 29,000 patients with
coronary heart disease are treated with coronary
artery bypass graft (CABG) surgery. For adult
patients undergoing elective low-risk surgery the operative mortality rate is about 1-2%. However, given the
recent advances in interventional cardiology, the aging
population, the prevalence of co-morbidities such as
diabetes and obesity, increasingly higher-risk and more
complicated patients are being operated on resulting
in mortality rates of up to 15-20% and even higher
rates of morbidity from CABG surgery. About 20% of
patients undergoing CABG surgery experience a perioperative myocardial infarction (PMI), an event which
is indicated by a rise in serum cardiac enzymes and
ECG changes and is associated with worse clinical
outcomes. Even in the absence of a PMI, significant
myocardial damage can occur during surgery in
response to acute myocardial ischaemia-reperfusion
injury, direct myocardial handling and coronary
microembolisation, resulting in poorer clinical outcomes. Therefore, to improve clinical outcomes in
these patients, new treatment strategies are required
to mitigate the myocardial injury sustained during
CABG surgery.
In this regard, ‘conditioning’ the heart, a process
which renders the myocardium more resistant to the
Derek Hausenloy
Derek Yellon
detrimental effects of acute ischaemia-reperfusion
injury, may offer an innovative interventional strategy
for reducing myocardial injury during cardiac surgery.
This cardioprotective effect appears to be mediated
through the up-regulation of endogenous pro-survival
pathways within the cardiomyocyte. The general principle underlying ‘conditioning’ of the heart is to apply
brief episodes of ischaemia and reperfusion either
prior to the index ischaemic event (ischaemic preconditioning) or at the end of the index ischaemic episode
(ischaemic postconditioning). The ‘conditioning’
ischaemia-reperfusion protocol can either be applied
directly to the heart or more intriguingly it can be
applied to an organ or tissue remote from the heart- a
phenomenon termed remote ischaemic preconditioning (RIPC).
Clinical studies from our group and others have
demonstrated that both ischaemic preconditioning
(IPC) and postconditioning (IPost) can reduce the
amount of myocardial injury encountered during
CABG surgery. However, this approach requires an
invasive protocol of intermittent clamping and
declamping of the aorta for brief episodes (lasting 5
min), instituted either prior to clamping of the aorta
(IPC) or at the time of aortic declamping (IPost). A less
invasive approach is to apply the preconditioning protocol to an organ or tissue remote from the heart a
phenomenon which has been termed remote
ischaemic preconditioning (RIPC). In this respect, we
have recently demonstrated that applying three-5 min
episodes of ischaemia and reperfusion to the right
arm of patients undergoing elective CABG surgery
reduced the peri-operative 72 hour troponin-T release
by 43%. The preconditioning arm ischaemia and
reperfusion was implemented after the induction of
anaesthesia and was achieved by inflating a blood
pressure cuff applied to the upper arm to 200 mmHg
for 5 minutes and deflating the cuff for 5 minutes, a
process which was repeated three times. Other clinical
studies have reported beneficial effects using a similar
RIPC protocol in children undergoing corrective cardiac
surgery for congenital heart disease and in adult
patients being operated on for elective repair of an
abdominal aortic aneurysm. Whether this simple noninvasive cost-free intervention impacts on clinical outcomes following CABG surgery remains to be determined by large multi-centred clinical studies.
Furthermore, the preconditioning limb ischaemia has
the potential to offer widespread systemic protection
against ischaemia-reperfusion injury sustained by
other organs such as the kidney, liver and brain during
CABG surgery. Based on these recent findings, would
you give your right arm to protect your heart?
Transcatheter aortic valve replacement: a reality today
Jacques Seguin, M.D., Ph.D.
Professor of Cardiac Surgery
Chairman, CoreValve Inc.
R
eplacing heart valves without
opening the chest and the
heart were little known concepts until Philipp Bonhoeffer and
Alain Cribier’s groundbreaking pulmonary and aortic transcatheter
procedures were performed in
2000 and 2002 respectively. Today,
numerous development programs
for less invasive treatment of the
aortic, mitral and pulmonary valves
are in progress and the advent of
transcatheter heart valve therapies
heralds a period of great transfor-
mation in cardiac surgery. One of
the most important aspects of this
process will be the need to reengineer the relationship between
surgeons and interventional cardiologists in our common goal to
bring optimal therapy to patients
with heart valve disease.
The primary mission of
CoreValve® Inc. is to reduce the
trauma associated with traditional
open heart valve replacement surgery and to offer definitive transcatheter aortic valve replacement
(tAVR) therapies to patients less suitable or ineligible for surgery. The
Company has developed a selfexpanding technology for perform-
ing tAVR on a beating heart in normal sinus rhythm. Programs for percutaneous retrograde transfemoral,
minimally invasive retrograde subclavian, and antegrade transapical aortic valve replacement systems are in
various stages of clinical realization.
Design concepting and iterative
prototyping took place during
1997–2002 and first generation
pre-clinical, animal, and cadaver
work was completed by early
2004. A First-In-Man feasibility
study enrolled 14 patients with a
first generation 25 French (8mm)
device between July 12, 2004 (first
human implant) and July 2005. A
first safety and efficacy study
enrolled 65 patients with a second
generation 21 French (7mm) device
between August 2005 and August
2006 at seven sites in Belgium,
Canada, Germany, and The
Netherlands. A safety and efficacy
study that enrolled 112 patients
with a third generation 18 French
(6mm) device was conducted
between May 2006 and June 2007
at nine sites in Canada, Germany,
The Netherlands, and UK. Today,
physicians at more than 70 centers
in 19 countries around the world
have implanted over 1,500 valves.
The dramatic size reduction of
the Percutaneous Aortic Valve
Replacement (PAVR) ReValving®
delivery catheter to 18 French size
means that most procedures can
be performed under local anesthesia, without the use of surgical
cut-down/repair (with pre-closing),
without hemodynamic support,
and without artificially accelerating
the heart rate during valve placement. These technique improvements have resulted in a procedure
that has been performed jointly
and independently by both cardiac
surgeons and interventional cardiologists in the hybrid room or in
the cath lab.
CoreValve invites EACTS participants to learn more about the latest CoreValve technological and
clinical developments at the
Transcatheter Aortic Valve
Replacement Lunch Symposium in
room 1.07 on Tuesday, 16
September at 12.45 hrs.
Congenital
Commissurotomy and leaflet thinning in a critical neonatal
aortic valve stenosis: Revitalizing of surgically driven protocol
Viktor Hras̆ka, Department of Pediatric Cardiac Surgery, German
Pediatric Heart Centre, Asklepios Clinic, Sankt Augustin, Germany
N
ewborns and infants with
critical aortic stenosis represent a distinct and challenging group of patients with
severe obstruction at valvular
level and ductus dependent systemic circulation. The most
appropriate management strategy remains controversial. Both
balloon and surgical valvotomy
are firmly established as effective initial treatments with
encouraging survival rates even
in the troublesome neonatal
group. Improved early results
are based rather on the better
understanding of the limits of a
Viktor Hras̆ka
biventricular repair than on the
method of treatment. Valvotomy
of any kind is a palliative procedure and reintervention remains
frequent. Predominant post-valvotomy pathology is an important
predictor of the long-term outcome. The patients undergoing surgical valvotomy are more likely to have residual stenosis, which is
usually very well tolerated and patients have normal exercise tolerance. In contrast, those patients undergoing ballooning are
more likely to develop significant insufficiency, with a detrimental
effect on ventricular performance.
To achieve the optimal results, surgically driven protocol for critical aortic stenosis was adopted in German Pediatric Heart Centre,
Sankt Augustin. If the function of the left ventricle is depressed,
so-called “gentle” ballooning is done as an intermittent step to
stabilize the patient before surgery. Not larger than 5mm in ø bal-
Figure 1. AoS – aortic stenosis; LV – left ventricle; EFE – endocardial
fibroelastosis; BV – balloon valvotomy; OV – open valvotomy.
loon is used to slightly increase the effective orifice area of the
aortic valve with no risk of creating regurgitation. If left ventricle
function is not severely depressed and there is no hypoplastic
annulus of the aortic valve, surgical valvotomy is the method of
choice. In the case of a hypoplastic aortic annulus and developed,
but resectable endocardial fibroelastosis, a Ross-Konno operation
is considered. The Ross option is considered if there is failure of
the ballooning or surgical volvotomy as well (Fig. 1).
Open surgical valvotomy, allows more accurate fashioning of
commissurotomies, with the attempted construction of leaflet
anatomy as close to normal as possible. Shaving of thickened
leaflets, excision of obstructive myxomatous nodularities, and
mobilization of leaflets effectively increase the orifice area of the
valve with minimal risk of creating regurgitation (Fig. 2). This is
not achievable with the ‘blind’ ballooning, where cusps are likely
to get torn or perforated while trying to relieve the obstruction.
The overall 10-year survival rate is close to 90%. There is a late
death-hazard with a 70 % survival rate for neonates and infants
with other severe associated lesions. The 10-year freedom from
Figure 2. Shaving of thickened leaflets of the aortic valve and excision of
obstructive myxomatous nodularities.
recurrent aortic stenosis is approximately 80%. Development of
severe aortic regurgitation after open valvotomy is unlikely with
10 years freedom from severe aortic regurgitation up to 90%.
Direct surgical intervention, where exact splitting of fused commissures and shaving off of obstructing nodules can produce a
better valve with maximum valve orifice without causing regurgitation, might offer superior longer-lasting results in comparison
with blind ballooning.
Reference
1. Hras̆ka V, Photiadis J, Arenz C. Open valvotomy for aortic valve stenosis in newborns and
infants. Multimedia Manual of Cardiothoracic Surgery; http://mmcts.ctsnetjournals.org/cgi/collection/left_heart_lesions.
EACTS Daily News September 08 13
Evaluation of a novel sealant film
(TissuePatch3) for sealing air leaks
during lung surgery
Ideas have
come to life
T
T
he Vivostat® idea was conceived in 1992 by a
group of Danish researchers searching for a simple and fully automated way of preparing fibrin
sealant, onsite and from the patient’s own blood.
Following the initial development phase, the idea
was further matured in co-operation with specialists
from across the world, and in 2001, the first generation of the Vivostat® Fibrin Sealant product was
launched by the Danish company Vivolution A/S
(now known as Vivostat A/S).
Today, the Vivostat® technology comprises more
than autologous fibrin sealant. The advanced blood
processing technology has been further developed
and now a wide range of Vivostat® products are
used on a daily basis in a large number of surgical
departments and wound care centres across Europe
and Asia. The idea has come to life!
his paper presents the findings of a twenty
patient, two centre post market surveillance
study involving TissuePatch3, a novel synthetic surgical sealant film as an adjunct for the
prevention of air leaks in patients undergoing
elective lung resection by open thoracotomy.
Background
Air leaks in lung surgery are a perioperative hazard for thoracic surgeons and can lead to a variety of complications, not least including extended
insertion of chest drain and patient stay. This
study was designed to investigate the intraoperative and post-operative performance of a new
synthetic sealant film, TissuePatch3 (Tissuemed
Ltd). The product is designed to offer the surgeon
effective sealing of air leaks in a user-friendly
presentation with clinically advantageous characteristics including low material bulk, rapid delivery to the target tissues, zero preparation time
and very short application time.
Vivostat® Fibrin Sealant
Results
This two-centre post market study involved the
use of TissuePatch3 as an adjunct in the prevention of air leaks during thoracic surgery. The
study has revealed that in this patient population
the product:
eliminated air leaks at the point of chest closure;
reduced the time to the last recorded air leak
when compared to control patients*
(Statistically significant for patients treated at
one of the two centres).
resulted in 12 out of the 15 subjects (80%)
being air leak free at the end of the surgical
procedure;
provided a high degree of surgeon satisfaction;
was associated with no device related adverse
events.
* Clinicians at both centres provided retrospective control data from a
comparable patient population. These patients received equivalent
surgery to the subjects involved in the study with the exception that
no patch was applied.
TissuePatch3
Conclusions
This study supports the use of TissuePatch3 as an
adjunct in the resolution of air leaks encountered
in elective lung surgery. Due to the low patient
numbers and the range of data presented, data
analysis reveals that while time to last recorded
air leak is shorter with the use of the product,
against some criteria there is no statistical difference (p=0.05) between control and TissuePatch3
treated cases. However there are clear indications
that the product can provide a rapid and effective
solution, and the potential to review the post
operative patient treatment algorithm with a
view to effecting earlier drain removal and
patient discharge.
Visit Tissuemed at Booth 101-102 for a copy of this
White Paper and read more at http://www.tissuepatch3.com/clinical
Vivostat® Fibrin Sealant offers a safe and effective
alternative to conventional fibrin sealants. The fully
automated system prepares approximately 5-6 ml of
autologous fibrin sealant from 120 ml of the
patient’s own blood in just 23 minutes. The autologous nature of the product efficiently eliminates the
risks of viral infection and unlike conventional fibrin
sealants, Vivostat® Fibrin Sealant does not contain
any exogenous thrombin or bovine components.
The unique application devices (e.g. the Spraypen®)
offer the surgeon unparalleled freedom to apply
Vivostat® Fibrin Sealant intermittently throughout
the entire surgical procedure without experiencing
the blockage that is common in conventional systems. Furthermore, Vivostat® Fibrin Sealant can be
applied at very close range for pinpoint application,
and rapid polymerisation ensures that the fibrin
sealant remains where it is applied.
The entire Vivostat® process takes place in a closed
sterile disposable Preparation Unit of highly innovative
design
sealant, growth factors are efficiently protected
from proteolytic degradation and slowly released
over time.
From 120ml blood, approximately 5.5ml of
Vivostat® PRF® can be prepared, with 7 times the
platelet level of the donor’s blood – corresponding
to a platelet level above 1 million platelets/Ìl. Unlike
conventional PRP systems, the instant polymerisation
of the fibrin ensures that the growth factors remain
precisely where they are applied.
For more information about the Vivostat® product
line, please visit www.vivostat.com or stop by our
booth (2.35) at EACTS for an introduction to the
Vivostat® system.
Vivostat® PRF®
Vivostat® PRF® (Platelet Rich Fibrin) solves the problems of conventional PRP systems (platelet rich plasma) by leveraging the revolutionary Vivostat® Fibrin
Sealant blood processing technology. By combining
an autologous platelet concentrate with a fibrin
Vivostat® Fibrin Sealant is easily applied to the surgical
site using the unique Spraypen®
14 September 08 EACTS Daily News
Transforming patient care through innovation
I
n the last years of the 19th century two
brothers formed a new company around
the manufacture of sterile surgical dressings. The idea that doctors and nurses
should use only sterile devices to treat peoples’ wounds was revolutionary at that time.
The company founded by James Wood
and Edward Mead Johnson is today’s internationally renowned Johnson & Johnson.
It has developed to comprise over 250
operating companies, employing a total of
119,200 people around the world.
That early spirit of revolutionary innovation remains at the heart of the Johnson &
Johnson family’s healthcare work.
In 1992, Ethicon Endo-Surgery was created as a separate Johnson & Johnson
company to support the ground-breaking
minimally invasive surgery market. One
year later,
Ethicon Endo-Surgery produced the first
ENDOPATH Surgical Stapler and Linear
Cutter, used for a range of minimally invasive procedures including thoracic surgery.
The company continues to produce
minimally invasive surgical instruments.
Their focus is to design devices for interventional diagnosis and the treatment of
various diseases and conditions.
Ethicon Endo-Surgery is now the global
market leader and innovator for both minimally invasive and traditional mechanical
devices. Its core markets include surgical
cutting and stapling devices, laparoscopic
surgical instruments, access devices and
the use of advanced energy technologies
in surgery.
Ethicon Endo-Surgery´s mission is to
transform patient care through innovation.
The company continually strives for new
ways to ensure that developments in surgical instrumentation and expertise translate into patient benefits.
The company develops innovative surgical solutions that contribute to patient
recovery and wellbeing through earlier
detection and treatment, efficient surgical
solutions and faster recovery.
Our partnership with the thoracic discipline has led to the development of trocars, staplers and other devices essential
for minimally invasive chest surgery.
Ethicon Endo-Surgery is committed to
ensure that surgeons are familiar with
these new and innovative products. In
1991, the opening of the European
Surgical Institute (ESI) in Norderstedt near
Hamburg (Germany) took place, one of
ten Ethicon Endo-Surgery educational
institutes around the globe.
ESI is now one of the leading European
centres for continuing medical education
in minimally invasive and other areas of
surgery. The ESI offers unique learning
and teaching environments and teaches
surgeons and other allied healthcare pro-
fessionals about the latest advances in
their field.
Expert teachers, state of the art simulation technology, and the latest minimally
invasive surgery skills have attracted thousands of healthcare professionals through
the ESI doors. More than 110,000 medical
professionals have completed training at
the institute until now.
Products developed by Ethicon EndoSurgery, together with techniques pioneered at the ESI, have supported the successful establishment of minimally invasive
surgery in 21st century medical practices.
The 122 years since the Johnson brothers produced their first surgical dressings
have seen incredible progress in healthcare.
Tomorrow’s article will introduce the
newest innovation from Ethicon
Endo-Surgery and continues Ethicon
Endo-Surgery´s long-standing commitment to educating the customers
we serve.
Mechanical
heart valves –
A future without
warfarin?
Raul Garcia Rinaldi, MD
Director, Cardiovascular Surgery
Advanced Cardiology Center,
Mayagıez, Puerto Rico
Precise – Customized – Predictable
Innovations for Mitral Valve Repair
C
hronic anticoagulation remains the major
cause of valve related events (VRE) in
patients with mechanical prosthesis. The
most critical VRE’s, thromboembolism and anticoagulation hemorrhage, account for nearly
75% of valve related events.2 These events occur
“despite significant improvements in mechanical
heart valve design and composition.”3
“The thrombogenicity of mechanical heart
valves in the aortic position is due to activation
of platelets generated by high shear stress, turbulent fluctuations and regions of recirculation
of blood. This results in platelet activation,
aggregation and deposition”, and according to
Becker and colleagues, “the contribution of
coagulation factors to overall thrombotic potential is a secondary phenomenon.” 4 High shear
states can damage erythrocyte membranes
(lysis), causing the release of ADP. 5
I believe that the role of antiplatelet therapy in
patients treated with mechanical aortic prostheses may be a significant factor in reducing valve
related events.
My colleagues and I are currently conducting a
physician sponsored feasibility study of clopidogrel and aspirin in combination, as the sole anticoagulant for patients with St. Jude Mechanical
aortic prostheses. The study, currently in its sixth
year, provides an anticoagulation protocol of
clopidogrel 300mg and aspirin 325mg, during
the day of surgery, followed by clopidogrel
75mg and aspirin 325mg daily. No heparin or
warfarin is given at any time after discontinuation of cardiopulmonary bypass.
We have now enrolled 136 patients followed
for 3,891 months, with a mean follow-up period
of 32.4 months.
In the past few years, the degree of platelet
reactivity and percent inhibition has been studied
with the Accumetrics Verify Now assay and with
Thromboelastography (TEG). This testing has
provided important information regarding
patient response to this antiplatelet combination
and its effect on outcomes. The results will be
submitted for publication later this year.
We continue to be very enthusiastic with the
use of antiplatelet agents for patients with the
St. Jude Medical mechanical aortic prosthesis.
The Adjustable Annuloplasty Ring from
MitralSolutions is fully adjustable Off-Pump
Ring is implanted On-Pump using standard
techniques and can then be adjusted under
direct visualization.
allowing optimization of the repair to the
patient’s physiology and hemodynamics.
Precise, controlled adjustments allow both
reduction and enlargement of the mitral
valve with no compromise of key
performance parameters.
Residual regurgitation and length of leaflet
coaptation can be optimized while Off-Pump.
Valve dimensions may be reduced or enlarged
to minimize residual MR or SAM while leaving
the largest valve possible.
References
1. R.W. Emery, C.C. Krogh and K.V. Arom et al., The St. Jude
Medical Cardiac Valve Prosthesis: A 25-Year Experience with
Single Valve Replacement, Ann Thorac Surg 79:776-783
2. H. Koertke, R. Koertke, International Standardized Ratio SelfManagement After Mechanical Valve Replacement: Is an Early
Start Advantageous? Ann Thorac Surg 72:44-48
3. S.E Height, M.P Smith, Strategems for Anticoagulant Therapy
Following Mechanical Heart Valve Replacement, J Heart Valve
Dis 1999; 8: 662-4
4. R.C. Becker, et al., Pathobiologic Features and Prevention of
Thrombotic Complications Associated with Prosthetic Heart
Valves Fundamental Principles and the Contribution of
Platelets and Thrombin, Am Heart J 2001; 141:1025-37.
5. Becker, et al.
To Learn More about the Mitral Adjustable Annuloplasty Ring Feasibility
and Safety Study (MAARS) go to www.clinicaltrials.gov Identifier: NCT00554151
Not approved in the United States. This device is currently in clinical investigations.
www.mitralsolutions.com
16 September 08 EACTS Daily News
Perfusion
Median sternotomy, sternal dehiscence and mediastinitis:
the mechanical factor and the Ley prosthesis™
O
verweight and chronic obstructive pulmonary disease are
probably the most important
risk factors for sternotomy related
complications after cardiac surgery,
these factors may increase the risk for
sternal dehiscence and mediastinitis.
The Ley prosthesis has been developed
for the prevention and treatment of sternal dehiscence and mediastinitis after
median sternotomy. It can be used in
cases with multiple fractures and after
aggressive debridement with removal of
necrotic parts of the sternum.
It is a malleable, 0, 6 mm thick titanium alloy implant. It has a stepladder
shape and is evenly perforated along
its edges. The multiple perforations
allow selection for the best possible
positioning of the sternal wires, hence
achieving an adequate sternal stabilisation. The prosthesis will act as a pled-
get-reinforced, handsewn mattress
wire to the sternum and is easy to
implant.
Healing of the median sternotomy
requires a proper fixation. Since sternal
instability is a major cause for both to
start and to maintain infection after
sternotomy, we assume that achieving
sternal stability even in infected
patients may have advantages overshadowing the theoretical drawbacks.
The Ley prostheses can be used for
the prophylaxis and for the treatment of
closure of the sternum at risk for dehiscence and mediastinitis.
References:
1. Fewer reoperations and shorter stay in the cardiac
surgical ward when stabilising the sternum with
the Ley prosthesis in postoperative mediastinitis.
Astudillo et al;Eur J Cardiothorac Surg.2001
Jul;20(1):133-9
2. Reconstruction of the chronic aseptic sternal
pseudoarthrosis after median sternotomy: initial
experience with the Ley prosthesis. Astudillo et
al; Heart Surg Forum. 2008;11(1):E46-9
Ley prosthesis and devices™ available from GEISTER Medizintechnik
GmbH, Foehrenstrasse 2, D-78532
Tuttlingen/ Germany.
Tel: +49-7461-966240
Fax: +49-7461-9662422
E-mail: carsten.geister@geister.com
ECATS booth 2.40
Edwards Lifesciences – an update
on transcatheter heart valves
R
eflecting on Edwards Lifesciences’ 50-year history of innovation in the treatment of valvular
heart disease, it is rewarding to see how the
surgical community has transformed surgical aortic
valve replacement (AVR), a once high risk procedure,
into one that now has a post-op mortality rate of 23%1. Surgical AVR remains the procedure of choice
and is further strengthened by the use of high caliber
products that offer excellent durability and hemodynamics. More than 1 million patients worldwide
have been treated with Edwards’ heart valve repair
and replacement technologies2.
Looking into the future, even with the availability
of advanced technologies, there remains a significant
population with untreated severe aortic stenosis (AS).
Studies have shown that > 30% of patients with
severe AS are not treated.3 Many are unaware that
surgical replacement of the diseased valve can
improve their health and quality of life.
Innovation allows for the creation of new frontiers,
through continuous product improvements and
breakthrough technologies and procedures. As the
world leader in the science of heart valves, Edwards
is committed to exploring these new horizons and
strives to collaborate with physicians through all
phases of the innovation process: R&D, extensive
clinical research, hands-on training, patient education
and procedural support.
Transcatheter aortic heart valve replacement is one
option that may offer hope to patients who have few
or no treatment alternatives. Transcatheter valve
replacement with both transfemoral and transapical
delivery options continues to gain momentum, as
multi-disciplinary teams focus on optimal patient
treatment strategies.
To date, more than 1,500 patients worldwide have
received the Cribier-Edwards™/ Edwards SAPIEN™
valve through a series of extensive clinical trials and
feasibility studies, as well as European commercial sales
during the last year. It is indicated for high risk
patients with severe AS (EuroSCORE >20%, STS Score
>10%). This month, one 88 year old French patient is
celebrating five years with the Cribier-Edwards™ bioprosthesis. Her valve continues to function well and
she walks, paints and even swims. At the time of her
procedure, she was deemed inoperable.
The Edwards SAPIEN™ THV has incorporated
expertise from Edwards’ continuous advancement in
heart valve technology. This includes special bovine
pericardial tissue processing, ThermaFix™ anti-calcification treatment and leaflet matching for both thickness and deflection, which have been proven to
enhance durability and hemodynamic performance in
Edwards’ surgical valves.
Clinical education and in-depth training are at the
forefront of Edwards’ focus in centers initiating a
THV program. This new technology platform must
be introduced responsibly with long-term outcomes
in mind. Training for centers wishing to utilize the
transcatheter valve technology includes didactic presentations, case reviews, hands-on simulator programs and proctoring. A multi-disciplinary team is
required, and an Edwards clinical specialist is present
at every case.
Please visit the Edwards booth to learn more about
our comprehensive treatment options for heart valve
disease. Edwards looks forward to continuing this
valuable collaboration with both cardiac surgeons
and interventional cardiologists to help shape the
emerging minimally-invasive surgery and transcatheter practices, and develop additional transformational therapies for patients.
Reference sources
1. Society of Thoracic Surgeons, STS Adult CV Surgery National
Database Spring 2005 Report: Executive Summary. 2005:1-5
2. Edwards Press Release, May 8, 2008
3 . Iung B et al. The Euro Heart Survey on Valvular Heart Disease. Eur.
Ht Jour 2003;24:1231-1243
4. Prof. Alain Cribier, latest data (July 2008) on file at Charles Nicolle
Hospital Rouen, France
Edwards SAPIEN™ Transcatheter Heart Valve Bovine Pericardial Tissue with ThermaFix™ Tissue Treatment
Levosimendan: Improved
treatment for failing hearts?
Dag Nordhaug
Dept. of Cardiothoracic Surgery
St. Olavs University Hospital
and Norwegian University of Science and
Technology, Trondheim, Norway
L
ow-output heart failure remains a major problem
after cardiac surgery. Despite recent advances in
mechanical circulatory support, pharmacological
support will remain the first treatment option in postoperative heart failure. The last decade the calcium
sensitizer Levosimendan has proved its efficacy in the
treatment of decompensated chronic heart failure but
is also often used in a surgical setting.
“Levosimendan is a fairly new drug that affects
many aspects of cardiovascular function, and we may
not always know exactly what we do when we use this
remedy,” says Dag Nordhaug, cardiothoracic surgeon
from Trondheim, Norway. He has a Ph.D. in cardiac
mechanics and acute heart failure, and is currently
working with both clinical- and laboratory research
with Levosimendan.
Levosimendan is still surrounded by many myths.
There is good evidence for its calcium sensitizing properties, but the drug also works as a phospodiesterase
inhibitor. The effect on contractility, diastolic properties
and oxygen consumption is still debated.
There is also good evidence for preconditioning properties of Levosimendan. “This aspect is particularly interesting in a surgical setting,” says Nordhaug. “However,
when it comes to hard end-points in cardiac surgery, we
do need to see some more clinical studies before anything
can be concluded,” Nordhaug underlines.
“In my talk Sunday September 14, I will try to give
an overview of the literature concerning
Levosimendan, and in particular go through the scientific foundation for the use of this drug in a cardiac
surgical setting.” He underlines the importance of having a sound scientific approach whenever new treatment options are introduced to cardiac surgeons.
Postoperative heart failure is still a major cause of mortality after cardiac surgery, and our patients deserve the
best treatment available. Whether Levosimendan is the
best treatment option in postoperative low output syndrome remains to be seen, but the drug has many attractive properties. “However, more scientific work needs to
be done,” Nordhaug rounds off.
Portable CPS during
normothermic cardiac arrest
Dr Samuel A Tisherman
Departments of Critical Care Medicine and
Surgery, University of Pittsburgh, Pennsylvania,
USA
N
ormothermic cardiac arrest is a common cause
of death. Resuscitation with Cardiopulmonary
Resuscitation (CPR) and Advanced Cardiac Life
Support (ACLS) has saved many lives. Although
changes have been made to the recommendations for
ACLS, these have had little clinical impact and cardiac
arrest frequently remains refractory and overall success
of resuscitation attempts remains poor.
Extracorporeal cardiopulmonary support (CPS) can
restore normal hemodynamics and tissue oxygenation.
Laboratory studies have demonstrated efficacy in cardiac arrest models. The clinical challenges for using
CPS for management of prolonged refractory cardiac
arrest include the time required for initiation, vascular
complications, and bleeding. Improved CPS systems,
cannulae, and heparin-bonded circuits have made initiation of CPS potentially easier and safer.
Clinical studies of emergency CPS for refractory cardiac arrest have included case reports and small series.
Survival seems to depend upon the cause of the arrest.
The studies suggest that CPS is most appropriately
applied for patients with underlying conditions that are
reversible with appropriate therapy. These include complications during cardiac catheterization, pulmonary
embolism, overdose with hemodynamically active drugs,
and accidental hypothermia.
In children, extracorporeal membrane oxygenation
(ECMO) has been used successfully for a number of
diseases that result in respiratory failure, leading to
development of ECMO teams. These teams have also
applied ECMO for cardiac arrest with a suggestion of
good results, particularly if the underlying indication
was cardiac disease or neonatal respiratory disease
and if the patient did not already have a severe metabolic acidosis.
Ethical issues arise when one considers that CPS
could also be used to support a donor for solid organ
transplantation. When does the resuscitation of the
patient end and support of the organ donor begin?
The answer is not clear, but the question is critically
important.
Raising standards through education and training
SU
R
G
ER
EU
Y
R
O
P
EA
founded in 1986
IA
-T
HO
ASSOC
RACIC
N
I
O
T
IO
N
FOR
CA
RD
23rd EACTS
ANNUAL MEETING
17-21 October 2009
Vienna, Austria
Saturday 17 October 2009
Techno - College
Sunday 18 October 2009
Postgraduate Courses: Surgery for Congenital,
Acquired Heart Disease,Thoracic Surgery,
Perfusion, Basic Science and Endovascular
Intervention
For information please contact:
EACTS Executive Secretariat
3 Park Street,Windsor, Berkshire SL4 1LU, UK
Telephone: +44 (0) 1753 832166
Fax: +44 (0)1753 620407
Email: info@eacts.org
Website: www.eacts.org
18 September 08 EACTS Daily News
What to do and see in Lisbon
Sightseeing
Eating out
Carmo Convent
Built in the 15th century, today the Carmo Convent ruins in
the Chiado district stand as a poignant reminder of the
1755 earthquake. As well as contemplating the ruins, make
time for its compact archaeological collection which
includes Egyptian pieces.
Opening Hours: Mon-Sat 10am-6pm
Address: 4 Largo do Carmo 1200-092
How to get there: Baixa-Chiado or Rossio Metro; elevator
Santa Justa
Belém Tower
Built to guard Lisbon in the 16th century, Belém Tower is
now a UNESCO World Heritage Site. Jutting into the Tagus
River in Belém, the exterior features ornate Manueline religious and maritime carvings. Climb to the top for city
views.
Lisbon's Torre de Belém
was completed in 1520 during Portugal's Golden Age of
Discovery. In the centuries
that followed it became a
customs post, telegraph
office, lighthouse and political prison.
Opening Hours: May-Sep Tue-Sun 10am-6.30pm
Address: Avenida de Brasília 1400-038
How to get there: Tram 15 to Belém
Eleven
Located in São Sebastião, Eleven is Lisbon's only
Michelin-starred restaurant. Admire the contemporary Portuguese art on display while enjoying
panoramic city views. Chef Joachim Koerper creates modern Mediterranean dishes, such as partridge ravioli and red mullet with chorizo. The
five-course set menu accompanied by local wine
is a popular choice.
Opening Hours: Mon-Sat 12.30pm-3pm &
7.30pm-11pm
Address: Rua Marquês de Fronteira, Jardim
Amália Rodrígues 1070
How to get there: São Sebastião or Parque
Metro
Olivier
Owned by celebrity chef Olivier Costa and run by
his sister Nathalie, Olivier in Bairro Alto is popular
with famous faces. Innovative creations include
octopus carpaccio and grilled black pork with
mango chutney. Dark wooden panels contrast
with white linen tablecloths while shelves of vintage Portuguese wine add a traditional touch.
Opening Hours: Mon-Sat 8pm-1am
Address: 35 Rua do Teixeira 1200-459
How to get there: Restauradores metro; then
funicular Elevador da Glória
Nune's Real Marisqueira
Renowned as one of Lisbon's best fish and
seafood restaurants, Nune's Real Marisqueira is
located in historic Belém. Book a table here for a
business lunch or evening out. This simple and
clean restaurant displays fresh fish and tanks of
live seafood. There's also a good selection of
meat dishes on offer.
Opening Hours: Thu-Tue 12pm-12am
Address: Nune's Real Marisqueira, 120 Rua
Bartolomeu Dias 1300-031
Jerónimos Monastery
UNESCO World Heritage Site and national icon, the
Jerónimos Monastery in Belém is a masterpiece of early
16th-century Portuguese Manueline architecture. Highlights
include elaborately carved interior features, peaceful cloisters, explorer Vasco da Gama's tomb and the refectory.
A vast homage to the seafaring men who made
Portugal's name, the Jeronimos Monastery was established
in 1496, when the king petitioned to set up a monastery
devoted to the protection of Portugal's sailors and explorers. Building work took up the most part of the 16th century. The Manueline style of architecture, particular to
Portugal, is an ornate blend of late Gothic and
Renaissance, with signs of seafaring, nature and the
monarchy (rope, flora, fauna and coats of arms) sculpted
into the columns.
The monastery housed monks of the Order of Saint
Jerome, whose prayers were intended to safeguard the seafaring Portuguese on their expeditions. A pilgrimage to visit
the resting place of the ultimate traveller and the expanses
of Manueline architecture are reason enough to visit this
Lisbon landmark, while the Naval Museum is also housed in
the monastery complex.
Opening Hours: Tue-Sun 10am-6pm
Address: Praça do Império 1400-206
How to get there: Tram 15 to Belém
Cervejaria da Trindade
Housed in a former monastery refectory in the
Chiado district, the Cervejaria da Trindade is a
relaxed beer hall lined with 19th- and 20th-century azulejos (tiles). Classic Portuguese meat and
seafood dishes are served in the main dining
room. Sample Portuguese beers and wines in the
front bar area.
Opening Hours: Daily 9am-2am
Address: 20C Rua Nova da Trindade 1200-303
How to get there: Restauradores metro; then
funicular Elevador da Glória.
Culture
National Museum of
Ancient Art
The National Museum of
Ancient Art (Museu
Nacional de Arte Antiga),
also known as the Green
Shutter Museum (Museu
das Janelas Verdes), is
located in a 17th-century
palace in the Chiado district of Lisbon. The
museusm houses
Portuguese sculptures and
paintings from the 13th19th centuries, as well as
European paintings and art
treasures.
The paintings include works by Portuguese masters such as S Vicente de Fora,
Gregório Lopes, Josefa de Óbidos, Lusitano, Pedro Alexandrino and Domingos
António Sequeira. A collection of decorative arts includes nearly 3200 pieces of
goldsmith work; 1200 pieces of jewellery; 1700 pieces of furniture; 7500 ceramic
pieces, including a diverse range of fine porcelain from around the world and 4500
textile works.
In addition to the permanent collection, there are also temporary exhibitions.
Opening Hours: Tue 2pm-6pm; Wed-Sun 10am-6pm
Address: Rua das Janelas Verdes 1249-017 (Chiado district.)
How to get there: Tram 15 or 25 to Santos or by Metro – Chiado.
National Tile Museum
Housed in a former convent in São
João, the National Tile Museum is
home to a vast collection of valuable
azulejos, traditional Portuguese tiles.
Gems include 15th-century Moorish
tiles and large wall panels dating back
to the 18th century.
Over the past 100 years or so tile
designs have reflected various art
movements, from Modernist and Art
Deco to the more eclectic influences
seen today. Some of the later styles are
more elaborate, with entire walls
depicting famous historical scenes and
daily life.
Opening Hours: Tue 2pm-6pm; WedSun 10am-6pm
Address: 4 Rua da Madre de Deus
1900-312
How to get there: Bus 18, 42, 49,
59, 104 or 105
Nation’s Park
Originally built for Expo '98, Nations' Park is a modern architectural showpiece spread
along a three-mile stretch of the Tagus river in north-east Lisbon.
It boasts the vast Vasco da Gama shopping centre and cinema, an Oceanarium, the
Living Science Centre, the Atlantic Pavilion (concert and sports venue), the Lisbon
International Exhibition Centre (FIL), the Camões Theatre, Lisbon Casino and dozens of
bars, restaurants and late-night venues.
Enjoy the view from the cable car along the riverfront, hop on the tourist "mini"
train, or hire a bicycle to get around at your leisure. You can't miss the 17km-long
Vasco da Gama Bridge, 12km of which snake across the Tagus. Look out for the
Portuguese Pavilion, recognisable for its curved roof, designed by Portugal's most
renowned architect, Alvaro Siza, and considered an architectural wonder.
Opening Hours: Daily
Address: Nations' Park, Lisbon, Portugal
How to get there: Comboio and intercity trains arrive at Oriente Station, where
there's also a metro line and plenty of buses to the airport and city centre.
17th Annual
Meeting of Asian
Society for
Cardiovascular
and Thoracic
Surgery (ASCVTS)
T
he 17th Annual Meeting of Asian
Society for Cardiovascular and
Thoracic Surgery (ASCVTS) will be
held in Taipei International Convention
Center (TICC), from 5th March to 8th
March, 2009!
The ASCVTS is a rapid developing and
most attractive society in Asia and the
Annual Meeting has been held every year
since 1993. Participants of 2008 Singapore
Meeting had reached more than 800. The
ASCVTS has become one of the world top
four thoracic and cardiovascular surgery
societies in CTS net.
There have been many new devices and
new concepts developed in the field of
Cardiovascular & Thoracic Society since
2000. After a decade of revolution, we are
entering an Era of Modern Technology.
Thus the main theme: “Formulating a new
Era of Cardiovascular and Thoracic
Surgery in Asia” suits best as we comb
new grounds and face new challenges.
The 2009 annual meeting of ASCVTS will
bring together prolific results for greater
advancements in the field.
During this meeting, the American
Association for Thoracic Surgery (AATS)
will conduct a one-day postgraduate
course. All Asian cardiovascular and thoracic surgeons will not miss this 2nd
AATS/ASCVTS postgraduate course.
Speakers in this postgraduate course will
be: Thoralf M. Sundt, M.D. (Mayo Clinic),
Kit V. Arom, M.D. (Bangkok Heart
Hospital), Joseph E. Bavaria, M.D.
(Hospital of the University of
Pennsylvania) and Lars G. Svensson, M.D.,
Ph.D. (The Cleveland Clinic) and more
speakers are now under invitation.
Concomitantly, there will be a 2009 CrossStrait Cardiovascular and Thoracic Surgery
Symposium. We are expecting totally
more than 1,200 participants, majority
coming from the Mainland China and
Japan to join us in this event.
Together with the Meeting, we also
arrange exhibition during the dates. The
exhibition will showcase professionals,
equipment, methods, and others associated with the fields. Through this exhibition, participants will be able to interact
with the exhibitors for the most updated
information.
As for the speakers, we now confirmed
to have Thomas L. Spray, M.D. (President,
American Association for Thoracic
Surgery, USA), Craig R. Smith, M.D.
(Professor, Columbia Presbyterian Medical
Center, USA), Roland Hetzer, M.D.
(Professor, German Heart Institute Berlin,
Germany), Carl Lewis Backer, M.D.
(Professor, Northwestern University),
Claude Deschamps, M.D. (Division of
General Thoracic Surgery, Mayo Clinic,
USA), Alain F. Carpentier, M.D. (Professor,
Hopital Europeen Georges Pompidou,
Paris), and Hiromi Kurosawa, M.D.
(Professor, Tokyo Women's Medical
University, Japan) joining us. With their
wonderful speeches, the meeting will
surly be a worthy event for all of you to
attend!
It is our great honor that the Taiwan
Association of Thoracic & Cardiovascular
Surgery to host the 17th ASCVTS at 2009.
It is believed to be THE EVENT of Taiwan
Association of Thoracic & Cardiovascular
Surgery and also for all our colleagues
and friends in Cardiovascular and Thoracic
Surgery.
Taking this wonderful opportunity of a
world union, we sincerely invite you to
join us at the Congress. With your support and participating, we will make this
Congress ever more successful! For more
detailed information about the Congress,
please visit our website at
http://www.ascvts2009.org. We hope to
see your attendance at then.
EACTS Daily News September 08 19
Congenital
Normothermic vs Hypothermic
Cardiopulmonary bypass: rationale,
strategies, results. Normothermia is better
Dr Jean-Etienne Rubay
Service de Chirurgie Cardiaque
Avenue Hippocrate 10
Brussel 1200
Belgium
Rationale
Hypothermic cardiopulmonary bypass
(CPB) associated with cold crystalloid
or blood cardioplegia remains the standard method to perform paediatric
cardiac surgery.
The major reasons to maintain such
strategy are three fold : to preserve the
brain in case of inadequate oxygen
delivery, to reduce the inflammatory
response and to maintain a low metabolic state. There are major disadvantages to hypothermia, including its
effects on enzyme function, membrane
stability, calcium sequestration, glucose
utilization, adenosine triphosphate
(ATP) production and consumption, tissue oxygen uptake as well as on Ph
and osmotic homeostasis1 which may
culminate in organ dysfunctions including kidneys, liver, lung and even
myocardium.
The advantages of warm cardioplegia were demonstrated as early as
1989 by the Toronto Group2 and normothermic CPB widely developed in
adult cardiac surgery.
Strategy
Since the beginning of the 2nd millenium, major teams in Paris (Lecompte
and Durandy, Vouhé, Serraf and
Planché) followed by us in Brussels
have initiated a program of normothermic CPB associated with intermittent
warm blood cardioplegia (IWBC) in
neonatal and paediatric cardiac surgery
with the view of assessing its safety,
effectiveness and reproducibility
Results
In a very large study reporting over
1.400 patients including various complex and early repairs, Durandy et al3
concluded on the efficiency of the
warm strategy as a valid alternative to
cold cardioplegia in term of mortality
and other parameters such as rhythm
disturbances, time to extubation and
ICU stays, time of CPB and level of troponin.
In a major study on neonatal arterial
switch operation, Pouard and Vouhé4
have confirmed its the feasibility, most
of the operative data being similar to
hypothermia with improvement in
extubation time, myocardial protection,
length of stay and cost of surgery.
Our unpublished data (5) focused
on cellular metabolism (ATP) and neuropsychological outcome comparing
the two methods.
Normothermia CPB was initiated in
our centre in early 2000 and IWBC end
of the same year. Between 2004 and
2006, 48 patients with equivalent clinical conditions were randomly assigned
in a prospective study. Troponin and
lactate dosage, ATP, length of ventilation and intensive care unit stays, mortality, status at 1 year and late neurodevelopmental studies were considered.
Epicardic and endocardic myocardial
biopsies were collected on CPB before
aortic cross clamping, immediately
before the second cardioplegic infusion
and after release of cross clamp. None
of the analysed data were statistically
different between the two groups.
Meanwhile the ATP dosage showed
significant modification between the
twoo groups, demonstrating a clearly
different physiological status in favour
of the normothermic IWBC situation.
Late neuropsychological outcome
has been assessed by I.Q. measurement.
Excluding Down’s syndrome and
other genetic anomalies, 10 out of
each group could be evaluated by language, visual and manual tests. No
statistical difference could be demonstrated between the 2 groups.
Conclusions
Based on major published studies3,4
and confirmed by our own
experience5, we can conclude that normothermia and IWBC can be applied
in children and complex neonatal congenital repairs with safety, effectiveness and reproducibility with good
early and late results.
References
1. Lichtenstein SV, Ashe KA, el Dalati H, Cusimano
RJ, Panos A, Slutsky AS. Warm heart surgery. J
Thorac Cardiovasc Surg. 1991;101:269-74.
2. Lichtenstein SV, el Dalati H, Panos A, Slutsky AS.
Long cross-clamp time with warm heart surgery.
Lancet. 1989;1:1443.
3. Durandy Y, Hulin S. Intermittent warm blood cardioplegia in the surgical treatment of congenital
heart disease: clinical experience with 1400 cases.
J Thorac Cardiovasc Surg. 2007;133:241-6.
4. Pouard P, Mauriat P, Ek F, Haydar A, Gioanni S,
Laquay N, Vaccaroni L, Vouhé PR. Normothermic
cardiopulmonary bypass and myocardial cardioplegic protection for neonatal arterial switch
operation. Eur J Cardiothorac Surg.
2006;30:695-9.
5. Poncelet A, Barrea C, Anslot C, Hue L, Rennotte
M-Th, Nassogne M-C, Sluysmans Th, Rubay J.
Normothermia and warm blood cardioplegia versus hypothermia and cold crystalloid cardioplegia
in pediatric cardiac surgery. Comparative results
with reference to cellular metabolism and late
neurodevelopmental assesment. Submitted for
publication.
Annual Meeting of the
Society for
Cardiothoracic Surgery
in Great Britain and Ireland
22nd to 24th March 2009
Bournemouth Conference Centre
Society for
Cardiothoracic
Surgery
in Great Britain
and Ireland
Call for abstracts
Submission on-line
www.scts.org
from 1st September 2008
Submission deadline
Further information
5th November 2008
sctsadmin@scts.org
20 September 08 EACTS Daily News
Streamlined process for
EACTS members to
become members of STS
Dear EACTS Member:
The Society of Thoracic Surgeons (STS), in collaboration with the
European Association for Cardio-Thoracic Surgeons (EACTS), has
streamlined the application process for EACTS members interested
in becoming members of STS. STS membership is made up of
cardiothoracic surgeons and allied health care providers from
throughout the world who practice in the adult cardiac, general
thoracic and congenital arenas. Membership in STS has many
benefits including a subscription to The Annals of Thoracic Surgery,
STS News, discounted registration fees for educational offerings,
and opportunities to join leadership in developing and
implementing new programs and activities to advance the interests
of the specialty. Please note, the annual dues for international
members of STS are actually less than the subscription price for The
Annals of Thoracic Surgery!
To join STS, any current EACTS member simply needs to complete
and submit an STS membership application, along with his or her
current CV. There is no need for EACTS members to submit letters
of sponsorship. The application deadline is October 15, 2008, and
the STS Membership will vote to admit new members at the 45th
STS Annual Meeting in January 2009 in San Francisco, California.
Once approved through this arrangement, the STS initiation fee will
be waived, at a savings of $250.
I would like to invite EACTS members to join the Society.
Cardiothoracic surgery is a small specialty that can only benefit from
more international collaboration. For additional information, go to
www.sts.org/membership and click on International Membership in
the right navigation bar or contact Sonia Armendariz, STS Manager
of Member Services at sarmendariz@sts.com. You can also stop by
the STS booth in the Exhibit Hall during the EACTS Annual Meeting
to speak to a representative of STS and to complete your
application on-site.
I look forward to welcoming you as a new member of STS in
January.
Sincerely,
Douglas E. Wood, MD
STS Secretary
Perfusion
Hypothermic Preservation for
Traumatic Cardiac Arrest
Dr Samuel A Tisherman
Departments of Critical Care Medicine
and Surgery, University of Pittsburgh
Pennsylvania, USA
C
ardiopulmonary resuscitation
(CPR) has been utilized to save
many victims of normovolemic
cardiac arrest, e.g., ventricular fibrillation. During exsanguination cardiac
arrest from trauma, however, external
chest compressions are not physiologically effective. Therefore, standard
resuscitation of trauma victims who
become pulseless includes an emergency department (ED) thoracotomy
with open chest CPR and clamping the
descending aorta to maximize blood
flow to the most vulnerable organs,
heart and brain. The hope is to find an
intra-thoracic injury that can be quickly
repaired. Unfortunately, these efforts
are almost always unsuccessful.
Emergency Preservation and
Resuscitation (EPR) was developed to
rapidly preserve the viability of the
entire organism during ischemia, using
hypothermia, drugs, and fluids, to “buy
time” for transport and damage control
surgery, to be followed by resuscitation
using cardiopulmonary bypass (CPB).
Induction of EPR has been with either a
rapid aortic flush of ice-cold fluid or CPB.
Large animal studies have demonstrated the feasibility of good outcomes
after rapid exsanguination, cooling to
<10oC, and 2 hours of circulatory arrest.
Even if the period of circulatory arrest
was preceded by 2 hours of progressive
hemorrhagic shock, 1 hour of EPR
allowed good outcomes while attempted standard therapy (CPR and fluid
resuscitation) yielded no survivors. This
flush approach required enormous
amounts of fluid. So far, studies of
adjunctive pharmacologic strategies and
specific fluids have not yielded impressive benefit, however. In contrast, a
strategy aimed at maintaining cellular
energy during the cooling process and 3
hours of circulatory arrest could provide
good outcomes in some experiments.
Mechanistic studies are now underway
in a rodent model.
A different approach to EPR has been
induction of profound hypothermia
with CPB and prolonged low-flow CPB.
Laboratory studies have demonstrated
the feasibility of this approach, including the ability to repair multiple simulated injuries.
Given this extensive pre-clinical background in clinically relevant large animal research in multiple laboratories,
the first multi-center clinical feasibility
trial of EPR in humans is being planned.
Exhibitors
Company
A&E MEDICAL CORPORATION
ACORN CARDIOVASCULAR INC
AMERICAN ASSOCIATION FOR THORACIC SURGERY
ASANUS MEDIZINTECHNIK & SOFTWARE
ASIAN CARDIOVASUCLAR & THORACIC ANNALS
ATMOS MEDIZINTECHNIK GMBH & CO KG
ATRICURE EUROPE BV
ATRIUM EUROPE BV
ATS MEDICAL INC
AUSTROPA INTERCONVENTION
B BRAUN AESCULAP
BAXTER HEALTHCARE S A
BEMEDTEC MEDICAL SYSTEM
BERLIN HEART
BIOMET
BIORING SA
CALIFORNIA MEDICAL LABORATORIES INC
CARDIA INNOVATION AB
CARDIAMED BV
CARDIO VISION (JOINT BOOTH WITH WELCH ALLYN)
CARIOVASCULAR NEWS/BIBA MEDICAL LTD
CEREMED INC
COREVALVE
CORONEO INC
COVIDIEN
CRYOLIFE EUROPA LTD
CTSNET
DATASCOPE
DELACROIX-CHEVALIER
DENDRITE CLINICAL SYSTEMS LTD
EACTS-CONGENITAL DATABASE
EACTS-THE EUROPEAN ASSOCIATION FOR CARDIO-THORACIC SURGERY
EDWARDS LIFESCIENCES
ELSEVIER HEALTH SCIENCES
ESTECH INC
EUROSETS SRL
FEHLING INSTRUMENTS GMBH & CO KG
FUMEDICA AG
GAMPT MBH
GEISTER MEDIZINTECHNIK GMBH & CO.
GENESEE BIOMEDICAL INC
GEOMED® MEDIZIN-TECHNIK GMBH
GORE & ASSOCIATES
HAMAMATSU PHOTONICS DEUTSCHLAND GMBH
HEART HUGGER - GENERAL CARDIAC TECH
HEARTWARE INC
INTEGRA SURGICAL
INTUITIVE SURGICAL
JARVIK HEART INC
JOHNSON & JOHNSON (ETHICON ENDO-SURGERY & ETHICON)
JOTEC GMBH
KIMBERLY-CLARK HEALTH CARE
KLS MARTIN GROUP
LABCOR LABORATORIOS
LABORATOIRES PEROUSE/FLASH MED
LEVITRONIX
LIFEBRIDGE MEDIZINTECHNIK AG
MAQUET CARDIOPULMONARY AG
MAQUET CARDIOPULMONARY AG
MEDELA AG MEDICAL TECHNOLOGY
MEDI-STIM ASA
MEDOS MEDIZINTECHNIK AG
MEDTRONIC INTERNATIONAL TRADING SÁRL
MEDXPERT GMBH
MICROMED CARDIOVASCULAR EUROPE GMBH
MMCTS/ICVTS EDITORIAL OFFICE
NYCOMED
ON-X LIFE TECHNOLOGIES INC™
PETERS SURGICAL
PLUROMED INC
QUALITEAM SRL
REDAX SRL
SCANLAN INTERNATIONAL INC
SIEMENS AG HEALTHCARE SECTOR (Joint booth with Medtronic)
SMARTCANULA LLC
SORIN GROUP
ST JUDE MEDICAL
STORZ, KARL GMBH & CO KG
SYMETIS SA
SYNCARDIA SYSTEMS INC
SYNTHEMED INC
SYNTHES GMBH
TELEFLEX MEDICAL GMBH
TERUMO EUROPE CARDIOVASCULAR SYSTEMS
THE SOCIETY OF THORACIC SURGEONS (STS)
THORATEC CORPORATION
TISSUEMED LIMITED
VENTRACOR
VITALITEC INTERNATIONAL
VIVOSTAT A/S
WELCH ALLYN
WEXLER SURGICAL SUPPLIES
WISEPRESS ONLINE BOOKSHOP
Stand number
2.52
1.30
3.2
1.56
1.44
1.29
1.33+1.34+1.40+1.41
1.20+1.10
2.25 + 2.24
1.64
2.01A
1.14+1.13+1.12
2.17
2.44
2.37
2.04
2.15
1.51
1.06
2.11
1.63
1.52
1.11
2.06
1.24+1.25
2.43A+2.43B
3.4
2.45
1.59+1.58
1.37
3.1
3.1
2.27
1.43
2.41
2.21+2.22
2.10+2.09
2.18
2.05
2.40
1.42
1.53
1.21
2.16
1.07
1.04
1.61
2.42
2.51
2.19+2.20
2.46+2.47
1.22+1.08
2.48+2.47
2.08+2.07
2.34
2.36
1.49
2.30
2.49
2.13+2.14
1.35+1.36+1.38+1.39
2.38
2.32
1.46
2.01B
3.1
1.17+1.18+1.19
2.23
1.62+1.55
2.01C
2.02
2.03
1.16+1.15
2.33
2.12
2.28
2.31
1.23
1.09
1.32
2.50
1.60+1.57
2.39
2.26
3.3
2.29
1.01+1.02
1.67+1.50
1.28
2.35
2.11
1.31
1.66+1.65
Location
Hall 2
Hall 1
II/Foyer Hall 2
Hall 1
Hall 1
Hall 1
Hall 1
Hall 1
Hall 2
Hall 2
Hall 2
Hall 1
Foyer Hall 1
Hall 2
Hall 2
Hall 2
Hall 2
Hall 1
Hall 1
Hall 2
Hall 1
Hall 1
Hall 1
Hall 2
Hall 1
Hall 2
II/Foyer Hall 2
Hall 2
Hall 1
Hall 1
I/Foyer Hall 2
I/Foyer Hall 2
Hall 2
Hall 1
Hall 2
Hall 2
Hall 2
Foyer Hall 1
Hall 2
Hall 2
Hall 1
Hall 1
Hall 1
Hall 2
Hall 1
Hall 1
Hall 1
Hall 2
Hall 2
Foyer Hall 1
Hall 2
Hall 1
Hall 2
Hall 2
Hall 2
Hall 2
Hall 1
Hall 2
Hall 2
Hall 2
Hall 1
Hall 2
Hall 2
Hall 1
Hall 2
I/Foyer Hall 2
Hall 1
Hall 2
Hall 1
Hall 2
Hall 2
Hall 2
Hall 1
Hall 2
Hall 2
Hall 2
Hall 2
Hall 1
Hall 1
Hall 1
Hall 2
Hall 1
Hall 2
Hall 2
II/Foyer Hall 2
Hall 2
Hall 1
Hall 1
Hall 1
Hall 2
Hall 2
Hall 1
Hall 1
EACTS Daily News September 08 21
Floorplan
HALL 1
BEMEDTEC MEDICAL SYSTEM (2.17)
FUMEDICA AG (2.18)
JOHNSON & JOHNSON (ETHICON ENDO-SURGERY &
ETHICON) (2.19+2.20)
Have been relocated from Hall 2 to the Foyer of Hall 1
Sala
0.05
Cargas e descargas
Sala
0.03
Sala
0.04
gás
1.25 1.05
Catering
1.24 1.06
1.04
1.68 1.49
1.46 1.28
1.23 1.07
1.03
1.67 1.50
1.45 1.29
1.22 1.08
1.02
1.01
arrumos
Cargas e
descargas
1.66 1.51
1.44 1.30
1.21 1.09
1.65 1.52
1.43 1.31
1.20 1.10
1.64 1.53
1.42 1.32
1.19 1.11
1.63 1.54
1.41 1.33
1.18
1.62 1.55
1.40 1.34
1.17
1.61 1.56
1.39 1.35
1.16
1.60 1.57
1.38 1.36
1.15
1.59 1.58
1.37
1.14 1.13 1.12
W.C.
2.17 2.18 2.19 2.20
BAR
Colunas de 0,60mx0,60m
Colunas de 0,45mx0,45m
2.16 2.15 2.14 2.13 2.12
2.24
2.22
Sala
0.01
3,0x3,0m
W.C.
HALL 2
Sala
0.02
2.25
2.11
2.26
2.10 2.09 2.08 2.07 2.06 2.05 2.04 2.03 2.02
2.27
2.28
2.23
2.50 2.51 2.52
2.01a
2.21
2.37 2.34
2.38
2.01c
2.33
2.32
2.31
2.36 2.35
2.39
2.30
2.40
2.41
2.01b
2.42
2.43a
2.43b
2.44
2.45
2.46 2.47 2.48 2.49
2.29
22 September 08 EACTS Daily News
Product listing
Biological Heart Valves
Oxygenators
ATS Medical Inc.
Cryolife
Edwards Lifesciences
Fumedica Ag
Geister Medizintechnik Gmbh
Labcor Laboratórios
Medtronic International Trading Sàrl
Sorin Group
St. Jude Medical
Vascutek Ltd
Eurosets S.R.L.
Sorin Group
California Medical Laboratories, Inc.
Eurosets S.R.L.
Medela Ag
Peters Surgical
Redax S.R.L.
Terumo Europe Cardiovascular Systems
Chest Drainage Systems
Blood Conservation and Delivery
Systems
Eurosets S.R.L.
Fumedica Ag
Medtronic International Trading Sàrl
Quest Medical, Inc.
Redax S.R.L.
Sorin Group
Atrium
California Medical Laboratories, Inc.
Eurosets S.R.L.
Medela Ag
Peters Surgical
Redax S.R.L.
Electrosurgical Units and
Accessories
Cardiopulmonary Bypass
Systems
Cannulae
California Medical Laboratories, Inc.
Edwards Lifesciences
Estech Inc.
Eurosets S.R.L.
Fumedica Ag
Maquet Cardiopulmonary Ag
Medos Medizintechnik Ag
Medtronic International Trading Sàrl
Quest Medical, Inc.
Smartcanula Llc
Sorin Group
Terumo Europe Cardiovascular Systems
Catheters and other Perfusion
Products
California Medical Laboratories, Inc.
Cardia Innovation Ab
Edwards Lifesciences
Estech Inc.
Eurosets S.R.L.
Fumedica Ag
Gampt Mbh
Maquet Cardiopulmonary Ag
Medos Medizintechnik Ag
Medtronic International Trading Sàrl
Quest Medical, Inc.
Sorin Group
Terumo Europe Cardiovascular Systems
Atmos Medizintechnik Gmbh & Co. Kg
Estech Inc.
Fehling Instruments Gmbh & Co. Kg
Geister Medizintechnik Gmbh
Scanlan International, Inc.
Headlight Systems
Cardio Vision
Cardiomedical Gmbh
Geister Medizintechnik Gmbh
Integra Surgical
Welch Allyn
Heart Assist Devices and Laser
Systems
Acorn Cardiovascular Inc
Berlin Heart
Cardio Vision
Cardiomedical Gmbh
Datascope
Hamamatsu Photonics
Heartware, Inc.
Jarvik Heart Inc.
Levitronix
Maquet Cardiopulmonary Ag
Medos Medizintechnik Ag
Micromed Cardiovascular Europe Gmbh
Syncardia Systems, Inc.
Terumo Heart Inc.
Thoratec Europe Ltd
Ventracor
Imaging Equipment
Operating Room Equipment
Ultrasound - Monitoring and
Equipment
Medi-Stim Asa
Siemens Ag Healthcare Sector
Ultrasound - Surgical Instruments
Medi-Stim Asa
Geister Medizintechnik Gmbh
Medi-Stim Asa
Quest Medical, Inc.
Siemens Ag Healthcare Sector
Minimally Invasive Cardiac
Surgery
Endoscopic Instruments and Systems
Atricure Europe Bv
Cardio Vision
Cardiomedical Gmbh
Datascope
Delacroix-Chevalier
Edwards Lifesciences
Estech Inc.
Geister Medizintechnik Gmbh
Maquet Cardiopulmonary Ag
Medtronic International Trading Sàrl
Vascutek Ltd
Vitalitec International
Patches and Membranes
Biomaterials
Fumedica Ag
Labcor Laboratórios
Nycomed Eacts
St. Jude Medical
Synthemed, Inc.
Tissuemed Limited
Vascutek Ltd
Synthetic and Biological Grafts
Datascope
Fumedica Ag
Labcor Laboratórios
Maquet Cardiopulmonary Ag
St. Jude Medical
Tissuemed Limited
Vascutek Ltd
Robotic Surgical Systems
Cardio Vision
Cardiomedical Gmbh
Post-Op Infusion Devices
Thorocoscopy Systems and
Instruments
Professional Services, Database
Software and Services
Atricure Europe Bv
Cardio Vision
Cardiomedical Gmbh
Coroneo Inc.
Delacroix-Chevalier
Estech Inc.
Fehling Instruments Gmbh & Co. Kg
Geister Medizintechnik Gmbh
Genesee Biomedical, Inc.
Medtronic International Trading Sàrl
Scanlan International, Inc.
Wexler Surgical
American Association For Thoracic Surgery
CTSnet
Dendrite Clinical Systems
Eacts Congenital Database
Maquet Cardiopulmonary Ag
Medos Medizintechnik Ag
Siemens Ag Healthcare Sector
Mitral and Tricuspid
Annuloplasty Rings
ATS Medical, Inc.
Bioring Eacts
Cardio Vision
Cardiomedical Gmbh
Coroneo Inc.
Edwards Lifesciences
Genesee Biomedical, Inc.
Labcor Laboratórios
Maquet Cardiopulmonary Ag
Medtronic International Trading Sàrl
Peters Surgical
Sorin Group
St. Jude Medical
Eurosets S.R.L.
9th International Conference of
the International Mesothelioma
Interest Group
Congress Centre de
Meervaart, Amsterdam, The
Netherlands
For information, contact:
International Mesothelioma
Interest Group
Email: j.remmelzwaal@nki.nl
Additional information:
http://www.imig-online.com
/congres/
13–18 October 2008
EACTS Academy: European
School for Cardio-Thoracic
Surgery , Thoracic Course
(level C)
Bergamo, Italy
Villa Elios
Baxter
Biomet
Medxpert Gmbh
Qualiteam S.R.L.
For information, contact:
EACTS Executive Secretariat
3 Park Street, Windsor,
Berkshire SL4 1LU, UK
Phone: +44 1753 832166
Fax:
+44 1753 620407
Email: info@eacts.co.uk
Additional information:
http://school.eacts.org
EACTS
Daily News
12–13 December 2008
17–21 October 2009
EACTS Academy: Focus on
Thymic Tumours
23rd EACTS Annual Meeting
Antwerp, Belgium
Krakow, Poland
For information, contact:
For information, contact:
For information, contact:
European School of
Radiotherapy and Oncology
Guy Pedro Vieira
Centro de Radioterapia e
Medicina Nuclear
Praceta Assis Esperança, PT8000-176 Faro, Portugal
EACTS Executive Secretariat
3 Park Street, Windsor,
Berkshire SL4 1LU, UK
EACTS Executive Secretariat
3 Park Street, Windsor,
Berkshire SL4 1LU, UK
Phone: +32.2.7759342
Email: stine.bomholt@
estro.be
http://courses.eacts.org/sections/Cardiac/AdvTechCar/
index.html
EACTS Academy:
European School for
Cardio-Thoracic Surgery ,
Cardiac Course (level C)
Bergamo, Italy
Villa Elios
For information, contact:
EACTS Executive Secretariat
3 Park Street, Windsor,
Berkshire SL4 1LU, UK
Phone: +44 1753 832166
Fax:
+44 1753 620407
Email: info@eacts.co.uk
Additional information:
http://school.eacts.org
Sutures and Anastomotic
Devices
Other Categories
EACTS Academy: Advanced
Techniques in Adult Cardiac
Surgery
10–15 November 2008
Atricure Europe Bv
Ats Medical, Inc.
Cardio Vision
Cardiomedical Gmbh
Coroneo Inc.
Delacroix-Chevalier
Edwards Lifesciences
Estech Inc.
Ethicon Endo Surgery & Ethicon Products
(Johnson & Johnson)
Fehling Instruments Gmbh & Co. Kg
Geister Medizintechnik Gmbh
Genesee Biomedical, Inc.
Geomed Medizin-Technik Gmbh & Co.
Integra Surgical
Pluromed, Inc
Quest Medical, Inc.
Scanlan International, Inc.
St. Jude Medical
Vitalitec International
Vivostat A/S
Wexler Surgical
Synthetic and Tissue Grafts
Atrium
Datascope
Jotec Gmbh
Laboratoires Perouse / Flashmed
Maquet Cardiopulmonary Ag
Medtronic International Trading Sàrl
20–22 November 2008
http://courses.eacts.org/sections/Thoracic/MCLCMtg/index
.html
Surgical Instruments
Prosthetic Vascular Grafts
Multidisciplinary Care of Lung
Cancer
Additional information:
Cardiovascular News
Ctsnet
Dendrite Clinical Systems
Elsevier
Wisepress Ltd
Mechanical and Tissue Valves
Ats Medical, Inc.
Corevalve Europe Bv
Cryolife
Edwards Lifesciences
Fumedica Ag
Medtronic International Trading Sàrl
On-X Life Technologies, Inc.
Sorin Group
St. Jude Medical
6–8 November 2008
The Lake Resort, Vilamoura,
Portugal
Publishing Companies
A&E Medical Corporation
Ats Medical, Inc.
California Medical Laboratories, Inc.
Cryolife
Ethicon Endo Surgery & Ethicon Products
(Johnson & Johnson)
Fumedica Ag
Maquet Cardiopulmonary Ag
Medtronic International Trading Sàrl
Peters Surgical
Pluromed, Inc
Tissuemed Limited
Prosthetic Heart Valves
Forthcoming Events in 2008
25–27 September
2008
Sorin Group
Symetis S.A.
Vascutek Ltd
Phone: +44 1753 832166
Fax:
+44 1753 620407
Email: info@eacts.co.uk
Additional information:
28–29 November 2008
EACTS Academy: CardioThoracic Surgery and
Regenerative Medicine
Bern, Switzerland
Bellvue Palace Hotel
For information, contact:
Phone: +44 1753 832166
Fax:
+44 1753 620407
Email: info@eacts.co.uk
Additional information:
http://courses.eacts.org/sections/Thoracic/FocusTT/index.
html
4–7 February 2009
EACTS Academy: Cardiac and
Thoracic Robotic Surgery
Strasbourg,. France
For information, contact:
EACTS Executive Secretariat
3 Park Street, Windsor,
Berkshire SL4 1LU, UK
EACTS Executive Secretariat
3 Park Street
Windsor, Berkshire SL4 1LU,
UK
Phone: +44 1753 832166
Fax:
+44 1753 620407
Email: info@eacts.co.uk
Phone: +44 1753 832166
Fax: +44 1753 620407
Email: info@eacts.co.uk
http://courses.eacts.org/sections/CT/RobSurg/index.html
Additional information:
http://courses.eacts.org/sections/CT/CTRegen/index.html
Additional information:
Vienna, Austria
Austria Centre
Abstract submission deadline:
1 April 2009
For information, contact:
EACTS Executive Secretariat
3 Park Street
Windsor, Berkshire SL4 1LU,
UK
Phone: +44 1753 832166
Fax: +44 1753 620407
Email: info@eacts.co.uk
Additional information:
http://www.eacts.org
Publisher
Dendrite Clinical Systems Ltd
Editor in Chief
Pieter Kappetein
Managing Editor
Owen Haskins:
owen.haskins@e-dendrite.com
Advertising:
Mary Kennedy:
mary.kennedy@e-dendrite.com
Published
EACTS Daily News is published
by Dendrite Clinical Systems
Managing Director
Peter K H Walton
peter.walton@e-dendrite.com
Head Office
59A Bell Street,
Henley-on-Thames
Tel: +44 (0) 1491 411 288
Fax:+44 (0) 1491 411 399
Wesite: www.e-dendrite.com
Copyright ©: Dendrite Clinical
Systems Ltd and the European
Association for Cardio-Thoracic
Surgery. All rights reserved. No part
of this publication may be
reproduced, stored in a retrieval
system, transmitted in any form or
by any other means, electronic,
mechanical, photocopying,
recording or otherwise without prior
permission in writing of the editor.
Do your High Risk AS patients fall on the survival curve?
• Leadership in heart valve solutions
• Partnership in education and training
• It’s what you leave behind that matters
Carpentier-Edwards
PERIMOUNT Magna Ease
valve
Edwards SAPIEN
valve
Edwards Lifesciences LLC · One Edwards Way · Irvine, CA 92614 USA · 949.250.2500 · www.edwards.com
Edwards Lifesciences Europe · Ch. du Glapin 6 · 1162 Saint-Prex · Switzerland · 41.21.823.4300
REFERENCES 1. Ross J. Jr, Braunwald E. Aortic stenosis. Circulation. 1968;38 (Suppl 1):61-7.
2. S.J. Lester et al., “The Natural History and Rate of Progression of Aortic Stenosis,” Chest 1998.
Edwards Lifesciences devices placed on the European market meeting the essential requirements referred to in Article 3 of the Medical Device Directive 93/42/EEC bear the CE marking of
conformity. Edwards and Magna Ease are trademarks of Edwards Lifesciences Corporation. Edwards Lifesciences, the stylized E logo, Edwards SAPIEN, Carpentier-Edwards and PERIMOUNT
are trademarks of Edwards Lifesciences Corporation and are registered in the United States Patent and Trademark Offi ce. © 2008 Edwards Lifesciences LLC. All rights reserved. E977/08-08/THV