View Presentation - Society of Actuaries
advertisement

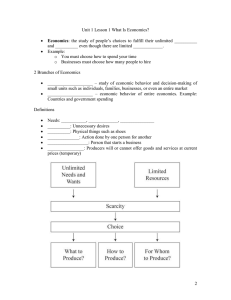
Session 95 PD, Pharmaceutical Manufacturer Perspectives Moderator: Gregory L. Warren, FSA, MAAA, FCA Presenters: Martin Marciniak, Ph.D. Vipan Sood, RPh, MBA, MRPharmS Nicole Yurgin, Ph.D. LINK BETWEEN VALUE, QUALITY AND OUTCOMES Society of Actuaries 2015 Health Meeting June 17, 2015 Martin Marciniak, Ph.D. Vice President, GlaxoSmithKline THIS DISCUSSION REFLECTS MY OPINIONS AND DOES NOT REFLECT THOSE OF GSK OR ANY ASSOCIATED ORGANIZATIONS. SHIFT TO VALUE Today Tomorrow Volume Driven Model Value Driven Model Fee for Service Visits (FFS) Procedures Patients Episodes Fixed costs Variable costs Patient satisfaction Resource/case Outcomes Profit Profit Per Diems Case rates Readmission Bundled Payments Fee for Value (FFV) ACOs – Other Valuebased Delivery Systems The market is shifting to value-based payment models where delivery and payment will be based on the quality of outcomes SHIFT TO VALUE REQUIRES PAYMENT AND DELIVERY REFORM Transparency: Collecting and reporting quality and cost data to consumers enables informed decision-making HIT: Use of HIT tools facilitates care integration, information collection and improves quality and efficiency Delivery System Measurement: Linking payment to quality of care requires improved measurement and evaluation framework HIT / Supports Incentivizes Transparency / System Infrastructure Measurement/ Evidence / Payment Structure Evidence: New evidence from comparative effectiveness research helps define delivery and payment patterns New payment models require a shift in the way providers deliver care: Value-based delivery models create the relationships and structure for sharing payments and coordinating care that will be necessary under the new payment models Presentation title 5 Presentation title 6 HEALTHCARE REFORM PROMOTES THE ADOPTION OF HIGH VALUE CARE, DETERMINED BY ASSESSING BOTH QUALITY AND COST Quality Value Cost • Provisions in the Affordable Care Act place a greater emphasis on the value of care provided • Value incorporates both quality and cost components, with the goal of promoting better care at a lower cost • Several drivers within the Act influencing provider behavior center on this idea of providing high value care 7 Presentation title HOW HEALTH OUTCOMES STUDIES ARE VALUED IN QUALITY MEASURE DEVELOPMENT 8 COMPARISON OF NQF #1799 AND #1800 1799: Medication Management for People with Asthma 1800: Asthma Medication Ratio (AMR) NCQA, NQF endorsed NCQA, NQF endorsed HEDIS, QRS (State Exchange) HEDIS The percentage of patients 5-64 years of age during the measurement year who were identified as having persistent asthma and were dispensed appropriate medications that they remained on during the treatment period. Two rates are reported: (1) The percentage of patients who remained on an asthma controller for at least 50% of their treatment period and (2) The percentage of patients who remained on an asthma controller for at least 75% of their treatment period The percentage of patients 5–64 years of age who were identified as having persistent asthma and had a ratio of controller medications to total asthma medications of 0.50 or greater during the measurement year. Numerator: Medication compliance of 50% and 75% as measured by PDC (proportion of days covered by at least one asthma controller medication prescription, divided by the number of days in the period) Numerator: The number of patients who have a medication ratio of 0.50 or greater during the measurement year. Denominator: Patients 5-64 years of age during the measurement year who were identified as having persistent asthma. Denominator: Patients 5–64 years of age during the measurement year who were identified as having persistent asthma. 1. National Quality Forum. http://www.qualityforum.org/Home.aspx. Accessed October 1, 2014. 9 LITERATURE REVIEWED Broder et. al.5 Schatz et. Description of difference inpatient characteristics and resource use in patients with high ratio (>0.5) versus low ration (<0.5), AMR, 5-56 year olds Mixed (2010) al.1-3 Comparison of asthma quality measures (including AMR and HEDIS Fill) 18-56 year olds Commercial (2005, 2006, 2008) Samnaliev et. al.4 Comparison of AMR and HEDIS adherence measures 18-56 year olds Medicaid (2009) Schatz et. al.6 Comparison of AMR and various HEDIS adherence measures 18-56 year olds Mixed (Kaiser) (2010) Stanford et. al.7 Comparison of AMR in various plan types and by age, 4-17 years old & >18 years old, Medicaid & Commercial (2013) NQF #1799 NQF#1800 Endorsed July 31, 2012 AMR = Asthma Medication Ratio, HEDIS = Health Effectiveness Data and Information Set, NQF = National Quality Forum Engelkes et. al.8 Systematic literature review examining association between asthma controller therapy adherence and serious exacerbations (2015) 1. Schatz, M, et al. Chest 2005;128,1968-1973. 2. Schatz M et al Chest 2006;130:43–50. 3. Schatz M and Stempel D. Ann Allerg Asthma Immunol. 2008;101(3):235-239. 4. Samnaliev M, et al. Chest 2009;135:1193-1196. 5. Broder et al. Am J Manag Care. 2010;16(3):170-178. 6. Schatz, M et al. Am J Manag Care. 2010;16(5):327-333. 7. Stanford, R et al. Am J Manag Care. 2013;19(1):6067. 8. Engelkes M et al. Eur Respir J. 2015 Feb;45(2):396-407. 10 STUDY DESIGN Study Period Enrollment Period 12/01/2009 12/01/20102 1-year pre-index period 12/31/2013 12/31/2011 15 -24 months post-index period Index RX Date 3 -12 months marker definition period •Controller to total asthma medication ratio •Albuterol use ED = Asthma-related Emergency Department visit Data on File 2015N236368_00 ICU = Asthma-related Intensive Care Unit visit 12 months outcomes assessment period Hospitalizations, ED, ICU, OCS OCS = Asthma-related Outpatient visit with Filled Oral corticosteroid prescription 11 RISK OF AN ASTHMA RELATED EVENT OR’s for cutoff >= 0.5 AMR and 50% PDC Asthmarelated Event Any event ED/IP IP ED visit Marker Periods 3-month 6-month 9 month ORs (95% CIs) ORs (95% CIs) ORs (95% CIs) CONTROLLER TO ASTHMA MEDICATION RATIO 0.390 (0.309 – 0.492) 0.403 (0.265 - 0.611) 0.477 (0.281 - 0.811) 0.294 (0.173 – 0.500) 0.393 (0.311 – 0.497) 0.348 (0.228 – 0.531) 0.334 (0.199 – 0.561) 0.374 (0.212 – 0.662) 0.341 (0.268 – 0.433) 0.304 (0.198 – 0.465) 0.290 (0.171 – 0.492) 0.320 (0.181 – 0.567) 12-month ORs (95% CIs) 0.336 (0.264 – 0.427) 0.349 (0.229 – 0.533) 0.338 (0.201 – 0.569) 0.341 (0.194 – 0.601) PROPORTION OF DAYS COVERED Any event ED/IP IP ED visit 1.057 (0.771 – 1.450) 1.361 (0.761 – 2.433) 1.550 (0.745 – 3.226) 1.138 (0.532 – 2.438) 1.201 (0.830 – 1.738) 1.204 (0.612 – 2.366) 1.817 (0.764 – 4.318) 0.940 (0.389 – 2.270) 0.966 (0.683 – 1.365) 1.050 (0.562 – 1.961) 0.950 (0.436 – 2.068) 1.123 (0.491 – 2.568) 1.047 (0.711 – 1.542) 0.874 (0.448 – 1.705) 1.046 (0.453 – 2.411) 0.681 (0.283 – 1.635) – Any event = Combined IP/ED visit/outpatient visit with OCS fill within +/- 7 days – Logistic regression models include baseline demographic characteristics – Age – Gender – Baseline ED event – Baseline hospitalization AMR = Asthma Medication Ratio, PDC=Proportion of Days Covered, ED = Asthma-related Emergency Department visit, IP = Asthma-related Inpatient visit , OR = Odds Ratio, OCS = Oral corticosteroids Data on File 2015N236368_00 12 DISCUSSION POINTS AMR was observed in this population of patients aged 65 years or older to perform in a similar fashion as what has been observed in the original AMR validation studies PDC was not observed to be a significant predictor of asthma related outcomes PDC was calculated as per HEDIS and PQA recommendations The methodology does not match past observational studies that have observed a benefit of PDC on asthma related events. Data on File 2015N236368_00 13 Presentation title HOW HEALTH OUTCOMES STUDIES ARE EVOLVING: THE EMERGENCE OF PRAGMATIC CLINICAL TRIALS 14 “EROOM’S LAW” Source: Scannell et al Nature Reviews Drug Discovery 2012, 11, 191 THE OPPORTUNITY FOR EFFECTIVENESS RESEARCH IN SALFORD AND BEYOND The Salford Lung Study is the world's first pragmatic randomised clinical trial initiated in a pre-licence setting 16 SCALE OF THE PROJECT 88 GP sites 128 community pharmacies 2800 COPD and 1425 asthma subjects recruited Bespoke eCRF and data monitoring system designed, built and working specialist safety team covering 2 hospitals Over 300 study staff Over 3000 GP and pharmacy staff trained in GCP and research-ready 17 ELECTRONIC CLINICAL MONITORING >300 users 54,560 radiology results 51,940 patient visits 15 data feeds per subject 4.97 million medications processed 9072 event alerts in last 12mnths 2 million clinical observations >50 million rows of data 977 SAE reports 2.8 million biochemistry and haematology results 18 SUMMARY The Salford Lung Study is the first of its type in the world Maintains scientific rigour • • • randomised, active control robust primary endpoint It has, and continues to be an enormous logistical effort But..... It will offer important information for clinicians, healthcare decision makers and most especially patients And will provide valuable information about how to conduct real-world effectiveness studies in future 19 WHAT IS THE LINKAGE? The U.S. is shifting to a value driven payment model Increasing importance on quality of care measures – including patient centered outcomes Changing U.S. health care environment is leading to different ways to approaches in study development and increased data Using Health Economics and Outcomes Research to Assess the Value of New Drugs An Example from Hepatitis C Virus Vipan C. Sood RPh, MBA, MRPharmS Vice President HEOR Virology/Endocrinology/Renal AGENDA 1. Overview of Hepatitis C Virus (HCV) 2. Role of Health Economics and Outcomes Research (HEOR) 3. Late Phase HEOR Activities: A Case Study from HCV 1. Overview of Hepatitis C Virus (HCV) Hepatitis C Virus Overview • Hepatitis C is a liver disease resulting from infection with the Hepatitis C virus (HCV)1 • Severity can range from mild illness to a serious, lifelong illness1 • Main routes of transmission2 ~3.2 M infected individuals in the US alone4 – Unsafe injections, inadequate sterilization of medical equipment, blood transfusion, sexual transmission • Long-term complications of HCV include cirrhosis, hepatocellular carcinoma, and death3 – HCV is the leading cause of liver transplantation in the US – Treating 5% of the HCV+ population avoids the need for 600-1,500 liver transplants • Sustained Virologic Response (SVR) following completion of treatment is reflective of a cure3 1. 2. 3. 4. Centers for Disease Control and Prevention. Hepatitis C for the Public. http://www.cdc.gov/hepatitis/C/ Accessed on 5/30/15. U.S. Department of Veterans Affairs. Viral Hepatitis. http://www.hepatitis.va.gov/provider/reviews/transmission.asp Accessed on 5/30/15. Hepatitis C: The Basics. http://www.hepmag.com/articles/2512_18755.shtml. Accessed on 5/30/15. Centers for Disease Control and Prevention. Hepatitis C Information for Health Professionals. http://www.cdc.gov/hepatitis/HCV/HCVfaq.htm#a4. Accessed on 5/30/15 Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 4 HCV Disease Burden and Costs are Rising Prevalence (95% CI) 4.5 US Prevalence (millions) 3.5 $16 $12 3.0 2.5 $8 2.0 1.5 $4 1.0 0.5 0.0 1950 1960 1970 1980 1990 2000 2010 2020 Healthcare Cost ($ billions) 4.0 Health Care Cost (95% CI) $0 2030 US HCV prevalence is in decline, however prevalence of advanced liver disease will continue to increase, as well as corresponding healthcare costs Razavi H, et al. Hepatology. 2013;57:2164-2170. Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 5 History of HCV Therapies Traditional Standard of Care New Direct Acting Antivirals (DAAs) 1st Generation DAA 2nd Generation DAA 1998 2001 2011 2013 2014 IFN + RBV1 PegIFN + RBV2 TVR + PegIFN + RBV3 SMV + PegIFN + RBV5 LDV/SOF7 BOC + PegIFN + RBV4 SOF + PegIFN + RBV6 OBV+PRV/r+DSV8 Three times a week injection Weekly injection Improved efficacy, safety, and tolerability IFN=interferon; RBV=ribavirin; PegIFN=pegylated interferon; TVR=telaprevir; BOC=boceprevir; SMV=simeprevir; SOF=sofosbuvir; LDV=ledipasvir; OBV=ombitasvir; PTV/r=paritaprevir/ritonavir; DSV=dasabuvir 1. 2. 3. 4. 5. 6. 7. 8. Rebetron FDA Approval. https://www.centerwatch.com/drug-information/fda-approved-drugs/drug/442/rebetron-tm-combination-therapy Peg-Intron FDA Approval. https://www.centerwatch.com/drug-information/fda-approved-drugs/drug/697/peg-intron-peginterferon-alfa-2b Incivek FDA Approval. http://investors.vrtx.com/releasedetail.cfm?ReleaseID=580154 Victrelis FDA Approval. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm255390.htm Olysio FDA Approval. http://www.jnj.com/news/all/OLYSIO-simeprevir-Receives-FDA-Approval-for-Combination-Treatment-of-Chronic-Hepatitis-C Sovaldi FDA Approval. http://www.gilead.com/news/press-releases/2013/12/us-food-and-drug-administration-approves-gileads-sovaldi-sofosbuvir-for-the-treatment-ofchronic-hepatitis-c Harvoni FDA Approval. http://www.gilead.com/news/press-releases/2014/10/us-food-and-drug-administration-approves-gileads-harvoni-ledipasvirsofosbuvir-the-firstoncedaily-single-tablet-regimen-for-the-treatment-of-genotype-1-chronic-hepatitis-c Viekira Pak FDA Approval. http://abbvie.mediaroom.com/2014-12-19-AbbVie-Receives-U-S-FDA-Approval-of-VIEKIRA-PAK-Ombitasvir-Paritaprevir-Ritonavir-Tablets-DasabuvirTablets-for-the-Treatment-of-Chronic-Genotype-1-Hepatitis-C Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 6 Higher SVR and Costs with DAAs SVR 100 90.3 96.4 15000 Cost/week, $ SVR, % 92.3 74.5 80 60 Cost/week 49.4 40 12000 9000 3000 0 0 1st generation DAA + PR 12000 6900 6000 20 PR 12200 2nd generation DAA + PR 2300 900 2nd generation DAA + RBV Two 2nd generation DAAs (no PR) PR=pegylated interferon; DAA=direct acting antiviral; RBV=ribavirin Bansal S, et al. World J Hepatol. 2015;7:806-813. Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 7 Controversy Over Costs of HCV Treatment Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 8 Summary • HCV is a disease with significant downstream morbidity and mortality • Due to the availability of new therapies, the cure rate (SVR) has increased significantly • Costs of therapy may seem high, but there is value to the health system and society in the long term • Health Economics and Outcomes Research (HEOR) generates evidence to assess the value of new drugs Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 9 2. The Role of Health Economics and Outcomes Research (HEOR) The Role of HEOR in Assessing a Drugs’ Value Greater Scrutiny of Costs with the Rising Rate of Health Care Expenditures US Health Expenditures by Year National Health Expenditures, Billions ($) $3,500 $3,000 $2,500 $2,000 $1,500 $1,000 $500 $0 1960 1970 1980 1990 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 Centers for Medicare and Medicaid Services. National Health Expenditure Data. Table 01. National Health Expenditures. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-andReports/NationalHealthExpendData/NationalHealthAccountsHistorical.html Accessed 5/30/15. Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 11 If You Can’t Pay for Everything, What Do You Pay For? Vaccination Heart Surgery The Ones That Bring the Most Value! Dialysis Cancer Treatment Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 12 Drug Approval Does Not Guarantee Patient Access and Reimbursement; Value Must Be Demonstrated Marketing Approval Reimbursement Considerations Patient New Drug Drug Approval Requirements All of these components make up a drugs value Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 13 The Role of HEOR in Assessing a Drugs’ Value LoE Product Launch HEOR INPUT L&A/Drug Discovery Clinical Development - Phase I–III Assessing unmet need 1- Incidence/ prevalence 2- Epidemiology 3- Burden of disease Trial Design 4- Patient-reported outcomes Marketed Product Preparing For Launch Real World Effectiveness 8- Medical chart reviews 5- Cost effectiveness 9- Prospective observational studies 6- Budget impact 7- Long-term outcomes 10- Retrospective claims HEOR=health economics and outcomes research; L&A=licensing and acquisition; LoE=loss of exclusivity Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 14 Summary • With rising health care expenditures, there is increased scrutiny on costs • HEOR uses rigorous methodology to establish evidence to demonstrate a drug’s value through • Budget impact models • Cost-effectiveness studies • Modeling long-term outcomes Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 15 3. Late-Phase HEOR Activities: A Case Study from Hepatitis C Virus (HCV) Examining budget impact, cost-effectiveness and long-term health outcomes with new treatments Budget Impact Model Introduction Key Question • What is the incremental impact on health care (and/or pharmacy) budget for patients in a health plan if a new HCV regimen is included? Analytical Approach • Budget impact is the difference between health care spending in world with a new HCV regimen vs. the world without a new HCV regimen Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 17 Example of Budget Impact of New HCV Regimen Without New HCV Regimen $40 Millions ($) With New HCV Regimen $30 $20 $10 $0 Without With Year 1 Without With Year 2 Without With Year 3 Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 18 Cost-Effectiveness Introduction Key Question • Is the value of a treatment worth its cost? Analytical Approach • CEA is an assessment of a therapy’s value-for-money • Compares costs and health effects of an intervention to assess whether it can be regarded as providing value for money Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 19 Cost-Effectiveness Introduction Quality-Adjusted Life Year (QALY) • A standard measure of treatment benefit and consequence that is represented in a common unit that can be compared across disease stages and other interventions • A QALY represents one year of life lived in perfect health (i.e. without illness) Quality of Life 1 0 QALYs without treatment Improvement in quality of life with treatment Length of life (years) HCV=hepatitis C virus; HCC=hepatocellular carcinoma Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 20 Cost-Effectiveness Introduction Incremental Cost-Effectiveness Ratio (ICER) • ICER measures the additional cost needed to achieve one QALY with a treatment vs a comparator • A cost-effectiveness threshold is needed to determine whether a treatment option is cost-effective or not • ICER < threshold suggests therapy is cost effective • Most conservative, $50K/QALY and commonly used in US/UK Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 21 Cost-Effectiveness of All-Oral DAAs Compared to No Treatment ICER threshold of $50,000 $50,000 ICER $40,000 $30,000 $20,000 $10,000 $0 F0 F1 F2 Fibrosis stage F3 F4 Compared to watchful waiting, all-oral DAAs are cost effective based on a threshold of $50,000 per quality-adjusted life-year (QALY) among treatment-naïve genotype 1 patients with any fibrosis stage DAA=direct acting antiviral; F=fibrosis stage (0, none; 4, cirrhosis or advanced scarring of the liver) Johnson S, et al. Poster presented at AMCP annual meeting, April 7-10, 2015, San Diego, CA, USA. Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 22 Modeling Long-Term Outcomes Introduction Key Question • What are the long-term benefits of treatment vs. no treatment? Analytical Approach • Use of modeling techniques to simulate patient progression with and without treatment Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 23 Long-Term Outcomes of Patients Treated With All-Oral DAAs Compared to No Treatment 100 All-oral DAA 80 % No treatment 78.3 60 40 36.7 30.2 16.7 20 6.8 0 Likelihood of cirrhosis Likelihood of liver cancer 1.9 9.2 7.1 Likelihood of liver transplant Likelihood of death Compared to watchful waiting, all-oral DAAs have a lower likelihood of long-term liver morbidity DAA=direct acting antiviral. Johnson S, et al. Poster presented at AMCP annual meeting, April 7-10, 2015, San Diego, CA, USA. Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 24 Long-Term Reduction in Average Annual Lifetime Medical Costs with Treatment of GT1 Patients $10 All-oral DAA Thousands ($) $8 No Treatment $6 $4 $2 $0 F0 F1 F2 F3 F4 Stage of Disease at Treatment In GT1 patients, overall lifetime medical costs associated with all-oral DAAs are significantly lower than those associated with no treatment DAA=direct acting antiviral; F=fibrosis stage (0, none; 4, cirrhosis or advanced scarring of the liver); GT=genotype Johnson S, et al. Poster presented at AMCP annual meeting, April 7-10, 2015, San Diego, CA, USA. Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 25 Summary • Through this case study of HCV, HEOR generated evidence to demonstrate the value of these new all-oral DAAs • Budget-impact model: Higher cost of all-oral DAAs • Cost-effectiveness model: All-oral DAAs are cost-effective based on ICER threshold of $50,000 • Long-term model: All-oral DAAs lead to a reduction in downstream morbidity, mortality, and post-treatment medical costs Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 26 Back Up Looking Back at History to Help Us Look Ahead History of HIV • Human immunodeficiency virus (HIV) was one of the most devastating disease globally • Highly active antiretroviral therapy (HAART) emerged in the mid-1990s revolutionizing care • Protests over the high price of HAART Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 30 HAART Had A Dramatic Impact on Survival Philipson T and Jena AB. Who Benefits from New Medical Technologies? Estimates of Consumer and Producer Surpluses for HIV/AIDS Drugs. Forum for Health Economics and Policy. 2006;9(2). Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 31 Most Of the Benefits of HAART Flowed to Patients $63 Billion 5% of the value creation was returned to innovators $1.4 Trillion Manufacturer revenues Patient health benefit Philipson T and Jena AB. Who Benefits from New Medical Technologies? Estimates of Consumer and Producer Surpluses for HIV/AIDS Drugs. Forum for Health Economics and Policy. 2006;9(2). Using Health Economics and Outcomes Research to Assess the Value of New Drugs | June 2015 | Company Confidential © 2015 32 Actuarial Science and Health Economics Outcomes Research Building Bridges: Common Foundations, Divergent Approaches and Applications June 17, 2015 Atlanta, Georgia Gregory Warren, MAAA Gregory Warren, FSA,FSA, MAAA President, Actuarial Consulting ViceVice President, Actuarial Consulting Englewood, Colorado Englewood, Colorado P: 303-714-1022 P: 303-714-1022 C: 847-942-9159 gregory.warren@optum.com gregory.warren@optum.com Actuarial Science and Health Economics & Outcomes Research Building Bridges: Common Foundations, Divergent Approaches and Applications Common Foundations Calculus-Based Statistical Theory Measuring Results Health Economic Impact Dealing with Uncertainty Divergent Approaches and Applications Law of Large Numbers (minimize statistical variation) Characteristic-Matched Studies (minimize confounding factors) Estimate Confounding Factors Eliminate Confounding Factors Financial Outcomes Clinical & Economic Outcomes Book of Business Focus Disease Focus Identify Correlations Identify Causations Short/Intermediate-Term Horizons Intermediate/Long-Term Horizons Model-Building Experts Proprietary and Confidential. Do not distribute. 2 Evaluation of Innovative Cardiovascular Therapies Nicole Yurgin, PhD Executive Director, Global Health Economics June 17th, 2015 The views expressed herein represent those of the presenter and do not necessarily represent the views or practices of the presenter’s employer or any other party. 2 We want meaningful innovations that lead to better health outcomes 3 But budget constraints force tough choices Scarcity: Healthcare resources are limited and budgets are constrained. Choice: Must decide how best to fund resources to maximize health. Opportunity Cost: Resources deployed in one fashion cannot be used in other ways – i.e. we give something up. …given scarcity, choice and opportunity cost, we increasingly need systematic ways to evaluate alternatives A health economist considers both value-for-money and affordability • Economic evaluation – “the comparative analysis of alternatives in terms of both costs and outcomes.” • “…the basic tasks are to identify, measure, value, and compare costs and outcomes of the alternatives” • Perspective: typically societal and long term • Typical activities for health economist: • • • • • • Evaluate the current burden of disease Describe areas of highest unmet need Quantify potential value of innovative treatment Identify the highest risk patients Estimate value-for-money (cost-effectiveness) Estimate affordability (budgetary impact) Drummond et al. (1997) Methods for the Economic Evaluation of Health Care Programmes. 2nd Ed. Cardiovascular Disease (CVD) has received a lot of media attention lately In The Debate About Cost And Efficacy, PCSK9 Inhibitors May Be The Biggest Challenge Yet CVS Urges Cost Controls for New Cholesterol Drugs CVD impacts many people in the US, therefore both the costs and the benefits for new therapies in this area could be large CVD causes substantial healthcare resource use and costs CVD causes substantial healthcare resource use and costs 6M 1 out of 3 5M In 2010, CVD lead to almost 6M hospitalizations and stroke and heart disease lead to 5M disabilites CVD accounted for 1 out of 3 deaths in the US each year 17 Years Individuals with a fatal heart attack lose an average of 17 years $320B 61% 65% The total cost of CVD is $320B annually 61% of which were direct costs which; the highest of all major diseases 65% of CVD costs were due to heart disease including CHD Mozaffarian, et al. Heart Disease and Stroke Statistics – 2015 Update: A Report from the American Heart Association. Circulation. 2015;131:e29–e322 Patients with low LDL-C have a lower likelihood of having a major CV event Patients with LDL-C levels of >100mg/dL are 4x more likely to have a major cardiac event compared to patients with LDL-C levels of <50 mg/dL Risk Estimates for Cardiovascular Events by Category of Achieved LDL-C Level Chance to experience Major Cardiovascular Event (%) 35% 32.8% 30% 25% 22.0% 20% 44 15% 16.5% 16.5% 75-100 100-125 17.8% 11.4% 10% 5% 4.4% 0% <50 50-75 125-150 150-175 >175 LDL-C Level Boekholdt, et al. Very low levels of atherogenic lipoproteins and the risk for cardiovascular events: a meta-analysis of statin trials. J Am Coll Cardiol. 2014: 64: 485-94. Many patients at high risk for CVD cannot reach target LDL-C levels % Not Achieving LDL-C Treatment Goals Approximately 30% - 87% of patients at high risk* for CVD cannot adequately lower their LDL-C levels with statins and/or other available lipid-lowering agents to achieve therapeutic targets Percent of Patients Not Achieving LDL-C Treatment Goals 100% 89% 87% 90% 78% 80% 77% 74% 73% 70% 59% 60% 56% 53% 50% 40% 39% 37% 33% 30% 36% 30% 20% 10% 0% MI CHD Angina Stroke Patient Type Goal of 100 mg/dL Diabetes Total Secondary Prvention Primary Prevention High-Risk Goal of 70 mg/dL * High-Risk Patients are defined as: Patients with FH receiving background therapy; Patients unable to tolerate an effective dose of statin; Secondary prevention patients receiving background statin therapy; Diabetic patients with high LDL-C levels Muntner, et al. Trends in the prevalence, awareness, treatment and control of high low density lipoprotein-cholesterol among united states adults from 1999–2000 through 2009–2010. Am J of Cardiol. 2013; 112.5: 664-670 Risk segmentation can identify highest risk patients who benefit the most • Each ~40 mg/dL absolute LDL-C reduction reduces the risk of CV death, non-fatal MI or stroke by 22%1 • Suppose a new therapy reduced LDL-C by 60% • 114 mg/dL reduction gives 63% relative risk reduction; 30% X 0.63 = 19% absolute risk reduction 1. Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet. 2010;376:1670–81. Cost effectiveness analysis can also show which patients benefit the most • Cost effectiveness analysis is a technique for comparing the relative value of competing clinical alternatives Costs A Drug A Outcomes A Life Years or Quality Adjusted Life Years (QALY) Choice Costs B Drug B Outcomes B • The ratio of the differences in costs to differences in outcomes is also called an incremental cost effectiveness ratio (ICER) • Higher risk patient groups offer higher value (i.e., lower ICERs) Drummond et al. (1997) Methods for the Economic Evaluation of Health Care Programmes. 2nd Ed. Economic value is increasingly being included in clinical guidelines • American College of Cardiology/American Heart Association (ACC/AHA) will be issuing value guidelines for different therapies based on cost-effectiveness. • This is the ACC/AHA guidance for value: Cost of a quality adjusted life year (ICER) 0 $50K High value $100K Intermediate value $150K Low value Anderson, et al. AHA/ACC statement on cost/value methodology in clinical practice guidelines and performance measures: A report of the American College of Cardiology/American Heart Association task force on performance measures and task force on practice guidelines. J Am Coll Cardiol. 2014; 63(21):2304-22. This type of economic analysis allows us to examine the components of value Illustrative - All costs and values depicted in this graph are hypothetical Net Monetary Benefit $160,000 $140,000 Incremental Monetary Benefit $120,000 Positive net monetary benefit $100,000 $80,000 $60,000 $40,000 $20,000 $0 Lifetime Treatment Cost CV Event Costs Avoided Incremental cost with New Treatment Benefit from Additional Survival Benefit from Additional QoL Incremental value with new treatment A health economist’s approach to affordability • To determine budgetary impact, we must estimate the size of the eligible populations and potential uptake of new therapy • Uptake can easily be overestimated • For example, in 2000 only 20% of adults with high cholesterol in 20001 • After considering any pharmacy cost offsets, we estimate pharmacy budget impact from putting the drug on formulary • Estimate medical cost offsets from reduced events and provide the total budget impact 1. Mann, et al. Trends in Statin Use and Low-Density Lipoprotein Cholesterol Levels Among US Adults: Impact of the 2001 National Cholesterol Education Program Guidelines. Ann Pharmacother 2008; 42:1208-15. Could benefit from partnering to identify high risk CV patients 71M* Pts with high LDL-C 39M* Diagnosed and treated 16M * High risk LDL>70 7M * High risk patients with LDL>100 *Amgen, data on file • Risks with utilization in large populations • Potential for high budget impact • Budget impact much lower with appropriate patient identification • Gains from partnering to find the highest risk patients Ultimately treated by physicians Given the large population, the CV area may be a good candidate for a creative risk share agreement Innovation in CV has the potential to make a big impact on health outcomes • The right disease area - CV is the #1 killer • The right time – we have the methodology to choose the right patients • The right patient – we need work together to target high risk patients and provide access to these patients The goal is to improve patient outcomes and more efficiently allocate resources Questions 17 Back-Up CV events are costly CV Event Direct Costs (SD); First year Subsequent years First year: ACS (UA/MI) $49,764 ($25,211) $16,611 ($13,287) First year: IS $44,007 ($26,274) $16,533 ($20,924) Fatal CHD $55,100 ($71,618) Fatal IS $48,895 ($64,157) Revascularization PCI: $39,421 ($17,930) CABG: $77,695 ($26,581) ACS, acute coronary syndrome; CABG, coronary artery bypass graft; CHD, coronary heart disease; CVD, cardiovascular disease; HF, heart failure; IS, ischemic stroke ; MI, myocardial infarction; PCI, percutaneous coronary intervention; SD, standard deviation; UA, unstable angina. Bonafede et al. Medical costs associated with cardiovascular events among high-risk patients with hyperlipidemia. ClinicoEconomics and Outcomes Research 2015: 7(1-9). The need for innovative therapies in CVD • Hyperlipidemia is a major modifiable risk factor for CHD and ischemic stroke1 • Elevated LDL-C plays a critical role in atherosclerotic plaque formation, and is a principal driver of CV risk in humans2-5 • The main available LDL-C lowering therapies include: statins, ezetimibe, bile acid sequestrants, fibrates, and nicotonic acid. 1. Jacobson T, Ito M, Maki K, et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: part 1 - executive summary. J Clin Lipidol. 2014;8:473-488. 2. Akram, et al. Beyond LDL cholesterol, a new role for PCSK9. Arterioscler Thromb Vasc Biol. 2010;30:1279-1281. 3. Cholesterol Treatment Trialists' (CTT) Collaborators. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581-590. 4. Francis A, & Pierce G. An integrated approach for the mechanisms responsible for atherosclerotic plaque regression. Exp Clin Cardiol. 2011;16:77. 5. Martin S, Blumenthal R, & Miller M. LDL cholesterol: the lower the better. Med Clin N Am. 2012;96:13-26. Better lipid management has the potential to prevent additional MACE events in 2035 for high risk patients Annual Projected Residual Major Adverse Cardiac Events (MACE)* in Treated Adults, LDL>70 2.0 1.47 M 1.5 1.56 M 1.63 M 1.37 M 1.28 M Annual MACE*1.0 (millions) 0.5 0.0 2015 2020 2025 2030 2035 *Myocardial infarction, ischemic stroke, unstable angina, coronary artery bypass graft surgery, percutaneous coronary intervention, congestive heart failure, cardiac death For Internal Use Only. Amgen Confidential. 21 Relationship between events and LDL For Internal Use Only. Amgen Confidential. 22 Every ~40 mg/dL reduction in LDL-C decreases relative risk for events by 20-25% The relationship between LDL-C reduction and CV event reduction is also holds for non-statin therapies Relative Risk in CV Events vs Absolute Risk in LDL-C