Specific overexpression of IL-7 in the intestinal mucosa: the role in
advertisement

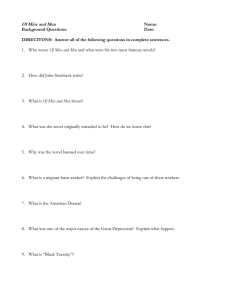
Am J Physiol Gastrointest Liver Physiol 294: G1421–G1430, 2008. First published April 10, 2008; doi:10.1152/ajpgi.00060.2008. Specific overexpression of IL-7 in the intestinal mucosa: the role in intestinal intraepithelial lymphocyte development Hua Yang,1,2 Blair Madison,3 Deborah L. Gumucio,3 and Daniel H. Teitelbaum2 1 Department of General Surgery, Xinqiao Hospital, Chongqing, China; and Departments of 2Surgery and 3Cell and Developmental Biology, the University of Michigan Medical School, Ann Arbor, Michigan Submitted 4 February 2008; accepted in final form 10 April 2008 transgenic; interleukin-7; mouse; epithelial cells IL-7 IS A MEMBER OF THE gamma chain-dependent (␥c) family of cytokines, which share a common receptor ␥c component and include IL-2, IL-7, IL-9, and IL-15. These cytokines strongly influence T cell development and function (12, 38) and signal T cell activation (35). In vivo only IL-7, and not other ␥c family members (e.g., IL-4 or IL-15), has been found to be essential for homeostatic proliferation of naive peripheral T cells (34). IL-7 is produced by thymic and intestinal epithelial cells (EC) (9, 37, 39), and in turn IL-7 receptors (IL-7R) have been detected on the surface of thymocytes and intestinal intraepithelial lymphocytes (IEL) (37, 50). Administration of IL-7 has been demonstrated to enhance both peripheral T cells and IEL numbers and function (9, 49). Kenai et al. (15) found that anti-IL-7 antibody treatment disturbed the induction of Addresses for reprint requests and other correspondence: D. H. Teitelbaum, Section of Pediatric Surgery, Univ. of Michigan Hospitals, Mott F3970, Box 0245, Ann Arbor, MI 48109 (e-mail: dttlbm@umich.edu) or H. Yang, Dept. of General Surgery, Xinqiao Hospital, Third Military Medical Univ., Chongqing 400037, China (e-mail: hwbyang@hotmail.com). http://www.ajpgi.org ␣-T cell receptor (TCR)⫹ T cells after athymic nude mice were implanted with fetal thymocytes. In the absence of IL-7, homeostatic proliferation of naive T cells is almost completely abolished, and the lifespan of naive T cells is greatly reduced (34). In vitro, in the absence of any other stimulus, IL-7 has been shown to induce proliferation of freshly isolated T cells in a dose-dependent fashion (1, 41). It has been shown that systemic overexpression of IL-7R in a transgenic mouse model increased survival of AKR/J early thymocytes and can contribute to thymocyte proliferation (19). Recently, our laboratory has shown that exogenous IL-7 administration significantly affected IEL phenotype and led to an increase in IEL number, as well as changes in IEL function. Cytokine expression changed significantly in both ␣-TCR⫹ IEL and ␥␦-TCR⫹ IEL subtypes. Exogenous IL-7 administration resulted in a significant expansion in the ␣-TCR⫹ IEL subpopulation (49). These studies suggest that IL-7 plays a critical role in regulating T cell homeostasis in peripheral lymphoid tissues. IL-7 is produced by EC in the thymus and intestinal mucosa (8, 9, 37, 39). Recent studies have demonstrated that close interaction between mucosal lymphocytes and intestinal EC are crucial in regulating immune response and EC growth in the intestinal mucosa (37, 45, 49). Several studies have indicated that EC may play an important role in mucosal immune responses by helping to regulate IEL (11, 50). We have also demonstrated that there is a close physical proximity of ECderived IL-7 and the IEL (49). IEL are a distinct population of T lymphocytes that are located at the basolateral side of EC in the epithelial layer of the intestine. It has been shown that IL-7R are expressed on the surface of CD4⫺,CD8⫺, CD4⫹,8⫺, and CD4⫺,8⫹ T cells, but not in CD4⫹,8⫹ double-positive T cells (32). More recently, a study from our group has found that IL-7R were identified on both ␣-TCR⫹ IEL and ␥␦-TCR⫹ IEL subpopulations (50). IL-7 knockout and IL-7 receptor knockout mice show distinct declines in absolute numbers of thymocytes and IEL (24). In an IEL culture model, IL-7 added to media significantly prevented the spontaneous apoptosis of IEL by decreasing caspase activity and preventing the decline in Bcl-2 expression (43). Previous studies have examined IL-7 given either by systemic administration or systemic overexpression of IL-7 or IL-7R (38, 49) (19). Such studies, however, may not permit one to gain a complete understanding of the role that intestinal EC-derived IL-7 has on the local IEL populations and how the IEL might be modulated by local IL-7 production. To better understand the role intestinal EC-derived IL-7 has in directing The costs of publication of this article were defrayed in part by the payment of page charges. The article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. 0193-1857/08 $8.00 Copyright © 2008 the American Physiological Society G1421 Downloaded from ajpgi.physiology.org on June 10, 2008 Yang H, Madison B, Gumucio DL, Teitelbaum DH. Specific overexpression of IL-7 in the intestinal mucosa: the role in intestinal intraepithelial lymphocyte development. Am J Physiol Gastrointest Liver Physiol 294: G1421–G1430, 2008. First published April 10, 2008; doi:10.1152/ajpgi.00060.2008.—IL-7 plays a crucial role in controlling T cell development and homeostasis. Since IL-7 may be derived from extraintestinal sources, and exogenous IL-7 broadly affects lymphoid populations, the actions of epithelial cell (EC)derived IL-7 are not fully understood. The effect of intestinal specific expression of IL-7 on intestinal mucosal lymphocytes was investigated by using an IL-7 transgenic mouse model. We generated an intestinal EC-specific overexpressing IL-7 transgenic mouse model (IL-7vill) and compared their phenotype and function to wild-type C57BL/6J mice. EC-derived IL-7 overexpression was found to be exclusively in the small and large intestine. Numbers and subtypes of mucosal lymphocytes, including intraepithelial lymphocytes (IEL) and lamina propria lymphocytes (LPL), significantly changed in IL-7vill mice. From a functional standpoint, IEL proliferation also significantly increased in IL-7vill mice. IEL cytokine expression significantly changed in both T cell receptor (TCR)-␣⫹ and TCR-␥␦⫹ IEL subpopulations, including a significant increase in IFN-␥ and TNF-␣ as well as an increase in keratinocyte growth factor expression. EC expression of CD103 (integrin ␣E7), the ligand of Ecadherin, markedly upregulated and may account for a mechanism of the massive expansion of IEL in transgenic mice. Systemic lymphoid populations did not change in transgenic mice. IL-7 overexpression by intestinal EC significantly affected IEL phenotype and function. These results offer insight into the role of IL-7 in IEL development and suggest a critical role of EC-derived expression of IL-7 in the phenotype and function of IEL. G1422 INTESTINAL MUCOSA SPECIFIC OVEREXPRESSION OF IL-7 IEL lineage and function, we established an intestinal ECspecific overexpressing IL-7 transgenic mouse model by using a 12.4-kb region from the mouse villin gene to direct intestinal overexpression of IL-7. We hypothesized that intestinal EC specific IL-7 overexpression would significantly affect the neighboring IEL phenotype and function. METHODS Creation of IL-7 Transgenic Mice Sample Harvesting All mice were euthanized at 8 wk of age, and serum and intestine, spleen, kidney, and liver tissues were harvested. IEL and LPL isolation from small intestine. Cells were isolated as previously described (17). Briefly, the small bowel was placed in tissue culture medium (RPMI 1640 with 10% FCS; Life Technologies, Gaithersburg, MD). Mesenteric fat and Peyer’s patches were removed. The intestine was cut into 5-mm pieces, washed three times in an IEL extraction buffer (l mM EDTA, l mM DTT in PBS), and incubated in the same buffer with continuous brisk stirring at 37°C for 20 min. The supernatants containing released sloughed EC and IEL were stored on ice. The remaining tissue pieces were incubated three times for 45 min each with RPMI 1640 containing collagenase (40 U/ml), 5% FBS, glutamine, and an antibiotic mixture at 37°C (20). Fig. 1. P12.4KVill vector was modified by ligation the IL-7 gene in a site beyond the villi promoter region. The 2 sites (Kpn and XhoI) where the IL-7 sequence will be inserted are labeled into P12.4KVill vector. The two sites to be cut by PmeI for release of the entire construct are also labeled. After selection of an appropriately stable clone as determined by size and sequence, the P12.4KVill ⫹ IL-7 construct will be released and injected into pronuclei of fertilized ova to create this IL-7vill transgenic mouse. Reverse Transcriptase-Polymerase Chain Reaction Isolation of total RNA. A guanidinium isothiocyanate-chloroform extraction method was used. Total RNA from isolated EC or IEL, or subtype IEL, LPL, thymocytes, splenocytes, and a piece of liver or kidney tissues were extracted by using Trizol reagent (Life Technologies) according to the manufacturer’s directions. RT-PCR. Poly-A tailed mRNA was reversed transcribed into complementary DNA by adding total cellular RNA to the following reaction mixture: PCR Nucleotide Mix (Invitrogen, Carlsbad, CA), M-MLV Reverse Transcriptase (Invitrogen), oligo(dT)12–18 Primer (Invitrogen), and RNAse Inhibitor (40 U/l, Roche Diagnostics, Mannheim, Germany). DEPC-treated H2O was added to yield the appropriate final concentration. For quantification of the IL-7 mRNA (including transgenic IL-7 mRNA) expression study, IL-7 primers were designed by using sequence from the encodable sequence of mouse IL-7 cDNA: forward primer. TGCCCGAATAATGAACCAA, reverse primer CAACCTCTCCAAGTTATGAACCA GTAG. For transgenic IL-7 gene detection, the forward primer was designed from exon-1, CAACTTCCTAAGATCTCCCAGGTG, and the reverse primer was designed from IL-7 cDNA, GTTCCTGTCATTTTGTCCAATTC. Primers for other cytokines, keratinocyte growth factor (KGF), and ligands were designed by use of proprietary software (Lasergene 6; DNA Star, Madison, WI). Samples were incubated at 40°C for 70 min, and the reaction was then stopped by incubating at 95°C for 3 min. PCR reaction was run. Thermal cycler settings were optimized to insure products were in the logarithmic phase of production. The PCR products were run out on a 2% agarose gel. Quantification of cDNA product was completed using a Kodak 1D image quantification software (Kodak, Rochester, NY), and target PCR products were compared by normalizing each sample to the production of -actin. AJP-Gastrointest Liver Physiol • VOL 294 • JUNE 2008 • www.ajpgi.org Downloaded from ajpgi.physiology.org on June 10, 2008 Development of a p12.4KVill-IL-7 transgene. We utilized a previously characterized 12.4-kb murine villin promoter/enhancer fragment to drive the expression of an IL-7 cDNA exclusively in the epithelium of the large and small intestine (23). Since the 12.4-kb region contains at least a portion of a locus control region, 70 – 80% of founder mice were expected to express the transgene in the small and large intestine. The full-length sequence of mouse IL-7 cDNA (generously donated by Dr. Jay Bream, National Institute of Arthritis and Musculoskeletal and Skin Diseases) was cloned behind the 12.4-kb villin promoter/ enhancer. The final clone used for transgenesis (P12.4KVILL-IL-7) was confirmed by restriction digestion and sequence analysis (across the complete IL-7 and into the villin sequences). Generation of IL-7vill transgenic mice. The transgene, containing villin regulatory sequences linked to IL-7, was prepared by digestion of P12.4KVILL-IL-7 with PmeI (Fig. 1). After purification, transgene DNA was injected into the pronuclei of fertilized ova (C57BL/6J ⫻ SJL/J) by the University of Michigan Transgenic Animal Core. Founders were identified by PCR amplification of tail DNA with primers specific for the transgene (forward primer ACAGGCACTAAGGGAGCCAATG; reverse primer TCCTGTCAT TTTGTC CAATTCA). Founders were then mated to C57BL/6J mice for the creation of F1 hybrids. All mice were bred and housed under clean specific pathogen-free conditions. Transgenic lines were maintained by crossing transgenic mice with C57BL/6J mice; transgenic animals were identified by PCR analysis of their tail DNA. Supernatants containing lamina propria lymphocytes (LPL) from each incubation were pooled on ice. Supernatants containing IEL and EC were then filtered through a glass wool column, and IEL and EC were separated by using magnetic beads conjugated with antibody to CD3 (BioMag SelectaPure antimouse CD3 antibody particles, Polyscience, Warrington, PA). Cells bound to beads were considered purified IEL; the EC remained in the supernatant. Flow cytometry confirmed purity of sorted cells, which was greater than 99%. Supernatant containing LPL (after collagenase incubation) were filtered through a glass wool column. Suspensions were centrifuged, the pellets were resuspended in 40% Percoll (Pharmacia, Piscataway, NJ), and the cell suspensions were overlaid on 75% Percoll. After centrifugation for 20 min at 600 g at 25°C, viable lymphocytes were recovered from the 40%/75% interface and washed in RPMI 1640 with 5% FBS, glutamine, and the antibiotic mixture (20). Purification of IEL subpopulations. Some IEL specimens were further separated between ␣-TCR⫹ and ␥␦-TCR⫹ subpopulations by using biomagnetic beads conjugated to monoclonal antibody as previously described (48). The purity of samples was confirmed by flow cytometry and compared with nonseparated IEL samples. Briefly, IEL were stained either with anti-␣-TCR⫹ antibody conjugated with fluorescein isothiocyanate (FITC) (PharMingen, San Diego, CA) or with anti-␥␦-TCR⫹ antibody conjugated with FITC (PharMingen), followed by incubation with magnetic beads conjugated with antibody to FITC (Polyscience, Warrington, PA). Cells bound to beads were considered purified ␣-TCR⫹IEL or ␥␦-TCR⫹ IEL and were processed for RNA isolation. Isolation of lymphocytes from spleen and thymus. Thymocytes and splenocytes were individually isolated by passage through a stainless steel mesh grid in sterilized RPMI 1640. Red blood cells were lysed with red blood cell lysis buffer for splenocytes, washed twice in 10% FCS/RPMI 1640, and counted. INTESTINAL MUCOSA SPECIFIC OVEREXPRESSION OF IL-7 Immunoblot Analysis for EC-Derived IL-7 Expression Briefly, isolated EC were homogenized on ice in lysis buffer (42). Protein determination was performed by using a Micro BCA Protein Assay Kit (Pierce, Rockford, IL). Approximately 40 g of total protein in loading buffer was loaded per lane in a SDS-polyacrylamide gel (13%) and separated by electrophoresis. Proteins were then transferred to a polyvinylidene difluoride membrane (Bio-Rad Laboratories, Hercules, CA). The membrane was blocked with blocking solution (Zymed Laboratories, South San Francisco, CA) and probed with goat anti-mouse biotinylated-IL-7 antibody (R&D Systems, Minneapolis, MN) (0.15 g/ml in blocking solution) for 1 h. Bound antibodies were exposed to a strepavidin-horseradish peroxidase conjugate (1:10,000, Zymed Laboratories), detected on X-ray film. Blots were then stripped and reprobed with monoclonal mouse anti--actin antibody (1:8,000 in blocking solution; Sigma, St. Louis, MO) to confirm equal loading of protein. The peroxidase-conjugated second antibody was goat anti-mouse IgG (1.8,000 in blocking solution; Invitrogen). Quantification of results was performed using Kodak 1D image quantification software (Kodak). Thus results of immunoblots are expressed as the relative expression of IL-7 to -actin expression. Recombinant mouse IL-7, anti-mouse IL-7 antibody, and biotinylated anti-IL-7 antibody were purchased from R&D Systems. Methods utilized are similar to those previously described (7, 48). Briefly, anti-IL-7 antibody was coated to the ELISA plate, and IL-7 levels were measured by ELISA by use of matched-pair antibodies. Serum IL-7 levels were determined graphically by using standard curves generated with recombinant mouse IL-7. Flow Cytometric Analysis Lymphoid phenotype was studied by fluorescent-labeled antibody staining detected with three-color flow cytometry. Monoclonal antibodies (BD PharMingen, San Diego, CA), consisting of anti-CD4, CD8␣, CD8, ␣-TCR and ␥␦-TCR, CD44, as well as CD69 antibodies, were used to examine the IEL subsets. Acquisition and analysis were performed on a FACSCalibur (Becton-Dickinson, San Jose, CA) using CellQuest software (Becton-Dickinson). The IEL population was gated on the basis of forward- and side-scatter characteristics. Quantification of each subpopulation was based on its percentage of the gated IEL population. In Vivo IEL Proliferation Study BrdU administration. Mice were provided with water ad libitum with 0.6 mg/ml 5-bromo-2-deoxyuridine (BrdU; Sigma) for 7 days as described by Tough and Sprent (36). After this 7-day period of BrdU labeling, mice were given unsupplemented water for an additional 14 days and then analyzed. Intracellular BrdU staining analysis. Cell staining for BrdU utilized a BrdU Flow Kit (BD Pharmingen, CA), as directed by the manufacturer. Briefly, isolated cells were suspended in FACS buffer and cell surface was stained with appropriate phycoerytherin (PE)conjugated antibody at 4°C for 30 min. Cells were then washed twice and resuspended, and Cytofix/Cytoperm (BrdU flow staining kit, BD Pharmingen) was added for 20 min at 4°C. The cells were washed, resuspended with Cytoperm plus buffer, and incubated for 10 min, washed with Perm/Wash buffer, resuspended with Cytofix/Cytoperm, incubated for 5 min, resuspended with diluted DNase buffer (provided with kit), and incubated for 1 h. Cells were washed with Perm/Wash buffer, and PE-conjugated antibody to BrdU was added at 4°C for 30 min. Cells were washed twice and resuspended in staining buffer prior to flow cytometry. Acquisition and analysis were performed on a FACSCalibur (Becton-Dickinson) using CellQuest software (Becton-Dickinson). The IEL population (gated on the basis of forward- and side-scatter characteristics) was quantified for each subpopulation on the basis of its percentage of the gated IEL population. Histological Analysis Segments 0.5 cm long of jejunum and ileum were fixed in 10% formaldehyde for histological sectioning. Tissues were then dehydrated with ethanol and embedded in paraffin. Sections were cut and stained with hematoxylin-eosin. The villus height and width and crypt depth were measured by use of a calibrated micrometer. Each measurement of the crypt and villus dimensions consists of the mean of seven different fields. Data Analysis Data are expressed as means ⫾ SD. Cytokine expression and flow cytometric results were analyzed by paired t-tests, with significance being defined as P ⬍ 0.05. RESULTS Intestinal EC-Derived IL-7 Expression in Transgenic Mice Villin is expressed in all EC of the small and large bowel and along the entire crypt-villus axis, with an increasing gradient from crypt to tip (25). It has been shown that the 12.4-kb fragment of the mouse villin promoter is reliable and reproducible to drive reporter gene expression in the intestine in a pattern that closely resembles that of the endogenous mouse gene (23). This 12.4-kb regulatory promoter is largely specific for the intestinal epithelium (23). RT-PCR showed EC-derived IL-7 expression to be expanded exclusively in the intestine. IL-7 mRNA expression was significantly higher in transgenic mice than wild-type mice (Fig. 2, A and B), and no transgenic expression of IL-7 mRNA was seen in thymus, kidney, spleen, or liver tissues in transgenic IL-7vill mice (data not shown). To clarify whether IL-7 overexpression in the intestinal EC of transgenic mice led to local overproduction of IL-7 protein, Western blot was used to detect EC-derived IL-7 expression in the jejunum and ileum of IL-7vill transgenic mice. IL-7 expression was significantly higher in both jejunum and ileum compared with that of wild-type mice (Fig. 2, C and D). IL-7 expression increased nearly 3-fold in jejunum and 3.3-fold in ileum compared with wild-type mice. Furthermore, this overexpression did not extend beyond the gastrointestinal tract; serum IL-7 levels were undetectable in both IL-7vill mice and wild-type mice by ELISA detection. Effect of EC Specific Overexpression of IL-7 on the IEL Numbers of IEL are increased in transgenic mice. Numbers of IEL in IL-7vill mice were significantly (P ⬍ 0.05) expanded compared with wild-type mice. The number of IEL in transgenic mice increased threefold compared with wild-type mice (Fig. 3A). IEL phenotype significantly changed in IL-7vill mice. To better understand the changes occurring in the IEL in transgenic mice, phenotype analysis was performed with flow cytometry. Several changes were identified in the surface phenotype of IL-7vill mice compared with wild-type mice (Fig. 4). Both CD4⫹,CD8⫺ and CD4⫹,CD8⫹ IEL subpopulations were significantly higher in transgenic mice (Fig. 3B) (P ⬍ 0.05). The CD4⫹,CD8⫺ IEL numbers increased 16.8-fold and CD4⫹,CD8⫹ IEL numbers increased 8.1-fold in IL-7vill mice compared with wild-type mice (Fig. 3B). The number of AJP-Gastrointest Liver Physiol • VOL 294 • JUNE 2008 • www.ajpgi.org Downloaded from ajpgi.physiology.org on June 10, 2008 IL-7 ELISA Detection G1423 G1424 INTESTINAL MUCOSA SPECIFIC OVEREXPRESSION OF IL-7 Fig. 2. Changes in epithelial cell (EC)-derived IL-7 expression in intestinal mucosal EC. A: RT-PCR detection of IL-7 mRNA expression. B: results of RT-PCR are expressed as a ratio of IL-7 to -actin mRNA expression. Expression of IL-7 mRNA was significantly increased in IL-7 transgenic mice (n ⫽ 6) compared with wild-type mice (n ⫽ 6). *P ⬍ 0.05. C: composite Western blot of EC-derived IL-7 expression in an IL-7vill mouse and a wild-type mouse. J, jejunum; I, ileum. D: EC-derived IL-7 expression was significantly higher in transgenic mice (n ⫽ 6) than wild-type mice (n ⫽ 6), P ⬍ 0.05. Results are the relative expression of IL-7 protein normalized to the expression of -actin multiplied by 100; n ⫽6 per group, *P ⬍ 0.05 total parenteral nutrition (TPN) group compared with control group. Fig. 3. Changes in the number of intraepithelial lymphocyte (IEL) in IL-7vill mice. A: the number of IEL significantly increased in IL-7vill mice (n ⫽ 6) compared with wild-type mice (n ⫽ 6) *P ⬍ 0.05. B: changes in the number of IEL phenotype compared with wild-type mice (n ⫽ 6), *P ⬍ 0.05. ␣-TCR⫹ IEL compared with wild-type mice (2.7 ⫾ 0.6 ⫻ 106). The percentage of the ␣-TCR⫹ IEL increased twofold compared with wild-type mice, whereas it was interesting to note that the percentage of ␥␦-TCR⫹ IEL population was significantly lower in IL-7vill mice compared with wild-type Fig. 4. Representative flow cytometry results of gated IEL populations. Cell populations are expressed as the percentage of gated cells with different cell phenotype markers. A: CD4 and CD8 markers. Increased the percentage of CD4⫹CD8⫺ CD4⫹CD8⫹ IEL subpopulations were found in IL-7vill mice compared with wild-type mice. B: CD8␣ and CD8 markers. IL-7vill mice increased the percentage of CD8␣⫹ IEL population IEL. C: ␣-T cell receptor (TCR) and ␥␦-TCR⫹ IEL markers, the percentage of ␣-TCR⫹ IEL subpopulation significantly increase, and percentage of ␥␦-TCR⫹ IEL decreased in IL-7vill mice (n ⫽ 6) compared with wild-type mice (n ⫽ 6). P ⬍ 0.05. AJP-Gastrointest Liver Physiol • VOL 294 • JUNE 2008 • www.ajpgi.org Downloaded from ajpgi.physiology.org on June 10, 2008 CD8␣⫹ IEL (i.e., CD8␣ heterozygote portion of CD8⫹ cells) was also significantly increased in the IL-7vill mice compared with wild-type mice (P ⬍ 0.05; Fig. 3B). TCR subpopulations were also studied. The relative percentage of the ␣-TCR⫹ IEL population significantly increased in IL-7vill mice compared with wild-type mice (Fig. 4C), as well as the absolute number (17.1 ⫾ 2.1 ⫻ 106) of harvested INTESTINAL MUCOSA SPECIFIC OVEREXPRESSION OF IL-7 mice (Fig. 4C); however, this decline was relative in respect to all IEL, and there was no significant difference of the absolute number of isolated ␥␦-TCR⫹ IEL between IL-7vill mice and wild-type mice (4.2 ⫾ 1.1⫻106 vs. 5.4 ⫾ 1.2⫻106 , P ⬎ 0.05). IEL maturation and activation changes in IL-7vill mice. CD44 was used as a marker of IEL maturation (26). CD4⫹,CD44⫹ IEL were significantly increased in IL-7vill mice compared with wild-type mice (38.4 ⫾ 5.9 vs. 6.5 ⫾ 1.7%, respectively) (Fig. 5A); representing a 15.2-fold increase in IL-7vill mice compared with wild-type mice (Fig. 3B). CD8⫹,CD44⫹ IEL also significantly increased (P ⬍ 0.05) in transgenic mice, representing a 1.9-fold increase compared with wild-type mice (Fig. 3B). Surface expression of CD69 was used as a marker of T cell activation (31) and was noted to be significantly altered in IL-7vill compared with wild-type mice (Fig. 5B). The CD4⫹,CD69⫹ IEL number increased nearly G1425 Fig. 6. Changes in IEL IL-7R mRNA expression from IL-7vill mice and a wild-type mice. Results of RT-PCR are expressed as a ratio of IL-7 mRNA to -actin mRNA expression. Expression of IL-7R mRNA was markedly increased in both ␣-TCR⫹IEL and ␥␦-TCR⫹ IEL in IL-7vill mice (n ⫽ 6) compared with control mice (N ⫽ 6), *P ⬍ 0.05. Functional Changes in the IEL Fig. 5. IEL populations are expressed as the percentage of gated cells. A: EC-derived IL-7 overexpression significantly increased the percentage of mature CD4⫹ IEL, as measured by the percent of CD44-positive cells. B: representative flow cytometry dot plots showing that IL-7vill mice have a much higher level of IEL activation, as measured by CD69-positive cells, compared with wild-type mouse. Increased IEL proliferation in transgenic mice. Because of the profound increase in IEL number and phenotypic changes in IL-7vill mice, we next investigated alterations in proliferation in various IEL subtypes. The results in Fig. 7 demonstrate that the IEL from IL-7vill mice have a dramatic increase in the proportion of cells entering the cell cycle compared with IEL from wild-type mice. More specifically, IEL proliferation in the CD4⫹ IEL was 18.5 ⫾ 1.2% in IL-7vill mice compared with 2.1 ⫾ 0.4% in wild-type mice (n ⫽ 6 each group, P ⬍ 0.05) (Fig. 7A). CD8⫹ IEL proliferation was 27.9 ⫾ 6.9% in IL-7vill mice compared with 8.5 ⫾ 0.2% in wild-type mice (P ⬍ 0.05; Fig. 7B). Similarly, the percentage of proliferating ␣-TCR⫹ IEL was significantly higher in transgenic mice (Fig. 7C). Concomitant with the observed decline in the relative number of ␥␦-TCR⫹ IEL; however, no significant difference in ␥␦-TCR⫹ IEL proliferation was noted between transgenic and wild-type mice (Fig. 7D). Changes in cytokine expressions in ␣-TCR⫹ and ␥␦-TCR⫹IEL. A panel of cytokines was selected that could contribute to both T cell activation as well as a downregulation of T cell activity (28, 40). TNF-␣ expression significantly increased in both ␣-TCR⫹ and ␥␦-TCR⫹ IEL populations in IL-7vill mice compared with wild-type mice (P ⬍ 0.05; Fig. 8). Because the AJP-Gastrointest Liver Physiol • VOL 294 • JUNE 2008 • www.ajpgi.org Downloaded from ajpgi.physiology.org on June 10, 2008 19.7-fold in IL-7vill mice (Fig. 3B) whereas CD8⫹,CD69⫹ IEL number actually only increased twofold compared with wildtype mice (Fig. 3B). IEL IL-7 receptor expression. IL-7R expression has been detected on IEL and LPL (37, 50). It has been shown that the IL-7/IL-7R-dependent signaling pathway plays a crucial role in regulating the immune response in the intestinal mucosa (44, 50). To determine whether local overproduction of IL-7 affects the neighboring IEL through the IL-7/IL-7R dependent signaling pathway, IEL IL-7R mRNA expression was studied. IL-7R mRNA expression in both ␣-TCR⫹ IEL and ␥␦-TCR⫹IEL subtypes were significantly increased compared with wild-type mice (Fig. 6). The ␣-TCR⫹ IEL subtype IL-7R mRNA expression increased 92.2%, and the ␥␦-TCR⫹ IEL IL-7R mRNA expression increased 53.4% compared with wild-type mice (Fig. 6). G1426 INTESTINAL MUCOSA SPECIFIC OVEREXPRESSION OF IL-7 pared with wild-type mice. Interestingly, despite a lack of expansion in the ␥␦-TCR⫹ IEL population, IL-7 overexpression led to a 37.3% increase in ␥␦-TCR⫹ IEL-derived KGF mRNA expression compared with wild-type mice (Fig. 9). Histological Morphology in IL-7 Transgenic Mice Fig. 7. Using 5-bromo-2-deoxyuridine (BrdU) incorporation, we measured IEL proliferation via flow cytometry. Cell populations are expressed as the percentage of gated cells. A: the percentage of proliferating CD4⫹ IEL in IL-7vill mice was significantly increased compared with wild-type mice. B: the percentage of proliferating CD8⫹ IEL in IL-7vill mice was significantly increased compared with wild-type mice. C: the percentage of proliferating ␣-TCR⫹ IEL in IL-7vill mice was significantly increased compared with wild-type mice. D: there was no significant difference in the proliferation rates of ␥␦-TCR⫹ IEL between IL-7vill and wild-type mice. PE, phycoerytherin. IEL is a major source of IFN-␥ (16, 46), IEL-derived IFN-␥ mRNA expression was also studied and was noted to be significantly increased in both ␣-TCR⫹ IEL and ␥␦-TCR⫹ IEL populations of IL-7vill mice (Fig. 8). Other cytokines studied, including IL-2 and IL-4, showed little to no change compared with wild-type mice (Fig. 8). Changes in ␥␦-TCR⫹IEL-derived KGF expression. KGF is a known mitogenic growth factor and has been shown to stimulate proliferation in a variety of EC lines (30). KGF has a critical role in intestinal epithelial growth and maintenance (45), and ␥␦-TCR⫹ IEL express KGF within the intestinal mucosa (5, 45). Thus we investigated whether EC overexpression of IL-7 would influence the neighboring ␥␦ TCR⫹ IELderived KGF expression. ␥␦-TCR⫹ IEL-derived KGF was noted to be significantly higher in IL-7 transgenic mice com- IL-7vill mice were noted to have profoundly altered crypt and villus structures (Fig. 10A). Villus height in IL-7vill mice was significantly higher than in wild-type mice. Crypt depth in IL-7vill mice was significantly deeper than in wild-type mice (Fig. 10B). One of the most dramatic changes in our transgenic mice was a significant increase in the width of the villi (Fig. 10B). It appeared that this marked increase in villus width was due to a marked expansion of lymphocytes in the underlying LPL population. We therefore investigated the associated alterations in the LPL of transgenic mice. Fig. 9. Changes in keratinocyte growth factor (KGF) mRNA expression in ␥␦-TCR⫹ IEL. Results of RT-PCR are expressed as a ratio of KGF to -actin mRNA expression. Expression of KGF mRNA was markedly increased in IL-7vill mice (n ⫽ 6) compared with control mice (n ⫽ 6), *P ⬍ 0.05. AJP-Gastrointest Liver Physiol • VOL 294 • JUNE 2008 • www.ajpgi.org Downloaded from ajpgi.physiology.org on June 10, 2008 Fig. 8. ␣-TCR⫹ and ␥␦-TCR⫹ IEL cytokine mRNA expressions. Both ␣-TCR⫹ and ␥␦-TCR⫹ IEL-derived TNF-␣ and IFN-␥ mRNA expression in IL-7vill mice significantly increased compared with wild-type mice, but either ␣-TCR⫹ or ␥␦-TCR⫹ IEL-derived IL-2 and IL-4 mRNA expression did not significantly change in IL-7vill mice (n ⫽ 6) compared with control mice (n ⫽ 6). Values (means ⫾ SD) are expressed as the ratio of target cytokine vs. expression of -actin; *P ⬍ 0.05. INTESTINAL MUCOSA SPECIFIC OVEREXPRESSION OF IL-7 G1427 Lamina Propria Changes in IL-7vill Mice EC-specific overexpression of IL-7 also induced a significant expansion of LPL numbers and suggested that EC-derived IL-7 may influence lymphoid development within the entire crypt-villus structure, and not just the epithelial mucosal lining. The number of LPL increased significantly in IL-7vill mice compared with wild-type mice (P ⬍ 0.05; Fig. 11A). Numbers of LPL increased threefold in IL-7 transgenic mice compared with wild-type mice. B cells (as detected with CD19) were not significantly different between IL-7 transgenic mice and wildtype mice (data not shown). Significant changes were also seen in the LPL phenotype. The percentages of CD3⫹CD4⫹CD8⫹; CD3⫹CD4⫹CD44⫹ and CD3⫹CD4⫹CD69⫹ subtypes significantly increased in transgenic mice compared with wild-type mice (P ⬍ 0.05) (Fig. 11B). Systemic Lymphoid Populations To assess whether local overexpression of IL-7 affected other lymphoid populations, thymocytes and splenocytes were studied. Overexpression of IL-7 did not result in any significant changes in thymocyte or splenocyte phenotype. There was also no significant difference in the number of thymocytes or splenocytes between transgenic and wild-type mice (data not shown). These results indicate that IL-7 overexpression by EC had no effect on systemic lymphoid populations. Thus the changes induced by EC-derived IL-7 were due to the direct effect on the mucosal level and not due to secondary changes in other lymphoid populations that might be a source of some portion of the IEL (i.e., thymic-derived IEL). Mechanisms for IEL Recruitment to the Mucosal Epithelium Although we demonstrated that the IEL are rapidly proliferating in our IL-7vill mice, we also noted a marked increase in TCR-␣⫹ IEL; this cell population could come from extraintestinal sources, such as the thymus (13, 21, 29). Therefore, we wanted to examine whether the expansion of the IEL in these mice might be influenced by changes in the expression of the IEL integrin ␣E7, which is a critical population for homing of lymphocytes to the mucosa. Interestingly, both ␣-TCR⫹ and ␥␦-TCR-⫹ IEL integrin ␣E7 expression increased significantly compared with controls (Table 1). TCR-␣⫹ IEL integrin ␣E7 expression was also noted to be much higher than in the ␥␦⫹ IEL in IL-7vill mice, as well as has previously been observed in wild-type mice. The ligand of CD103 (␣E7) is E-cadherin; therefore, we next investigated whether the marked overexpression of the integrin ␣E7 resulted in any changes to E-cadherin expression. In fact, we noted a 50% increase in E-cadherin expression in our transgenic mice, suggesting that local IL-7 overexpression contributes to IEL expansion not just by increased proliferation, but by the recruitment of lymphocytes to the epithelium. DISCUSSION In this study, we found that EC-specific IL-7 overexpression in our IL-7 transgenic mice significantly affected IEL phenotype and function and resulted in a significant expansion of the IEL population. IEL functional changes included a significant increase in IEL proliferation and alterations in cytokine expression for both ␣-TCR⫹ and ␥␦-TCR⫹ subtypes. In addition to the IEL, the intestinal LPL population was also seen to be significantly expanded, and a significant change in the proportion of LPL subtypes was observed. Finally, systemic lymphoid populations did not change in the IL-7vill transgenic mice, which supported the concept that local overexpression of IL-7 resulted in a restricted area of action to the intestinal mucosa and submucosa. Villin is a cytoskeletal protein that is produced by EC and is expressed along the brush border. Because villin is also expressed in the proliferative stem cells of the intestinal crypts cells, it is believed to be an early marker of EC from the remainder of the digestive tract (27). In the adult, the concentration of villin increases as cells move from the crypt to the tip of the villi (25). The 12.4-kb regulatory fragment of villin we used has been shown to be largely specific for the intestinal epithelium (22, 23). This villin promoter/enhancer has been shown to allow for the creation of a number of transgenic mouse models with robust overexpression of several genes (-galactosidase, Cre recombinase, green fluorescent protein, and Hedgehog interacting protein) (23). In our IL-7vill mice AJP-Gastrointest Liver Physiol • VOL 294 • JUNE 2008 • www.ajpgi.org Downloaded from ajpgi.physiology.org on June 10, 2008 Fig. 10. A: histology of jejunum and ileum from wild-type and IL-7vill mice using hematoxylin and eosin staining. B: histological analysis of sections of small intestine from wild-type mice and IL-7vill mice. *P ⬍ 0.05 compared with IL-7vill mice. Data are expressed as means ⫾ SD. G1428 INTESTINAL MUCOSA SPECIFIC OVEREXPRESSION OF IL-7 this 12.4-kb villin/IL-7 transgene was only detected from small and large intestinal epithelial tissue and was not detected in thymocytes, splenocytes, and kidney and hepatic tissues. Immune blot results showed that IL-7 protein expression in both jejunum and ileum in IL-7vill mice was significantly higher than in wild-type mice. Furthermore, the expression was confined to the local EC expression as, similar to wild-type mice; serum IL-7 from transgenic IL-7 mice was undetectable. The predominant IEL subpopulation is CD8⫹,CD4⫺ (70 – 85% of the total in mice) (10). IEL in mice also comprise a large number of ␥␦-TCR⫹ cells, and ⬃50% of IEL are Table 1. Alteration of CD103 (␣E7mRNA) and E-cadherin in IL-7vill mice Mouse Number ⫻106 (IEL) ␣E7 mRNA (TCR-␣⫹ IEL) ␣E7 mRNA (TCR-␥␦⫹IEL) E-Cadherin mRNA Wild-type IL-7vill 4.8⫾1.2 14.6⫾4.5* 261⫾76 2263⫾446* 61.8⫾15 1134⫾257* 92.9⫾30.5 140.6⫾39.8* Results are means⫾SD. IEL, intraepithelial lymphcytes. *P ⬍ 0.05, using ANOVA compared to wild-type group. AJP-Gastrointest Liver Physiol • VOL 294 • JUNE 2008 • www.ajpgi.org Downloaded from ajpgi.physiology.org on June 10, 2008 Fig. 11. A: changes in the number of lamina propria lymphocytes (LPL) in IL-7vill mice. The number of LPL significantly increased in IL-7vill mice (n ⫽ 6) compared with wild-type mice (n ⫽ 6) *P ⬍ 0.05, B: graphic distribution of the LPL phenotypes. CD3 was used as T cell marker, and CD44 was used as a marker of T maturation. CD69 was used as a T activation marker. CD3⫹CD4⫹CD8⫺ subtype was significantly expended in transgenic mice compared with wild-type mice, P ⬍ 0.05. There is a much higher CD3⫹CD44⫹CD4⫹ LPL population in transgenic mice than wild-type mice. The CD3⫹CD44⫹CD8⫹ LPL subtype decrease in transgenic mice than wild-type mice, P ⬍ 0.05. There is a much higher CD3⫹CD69⫹CD4⫹ LPL subtype in transgenic mice than wild-type mice, *P ⬍ 0.05. ␥␦-TCR⫹, compared with less than 2% of peripheral blood lymphocytes (16). The function of the IEL appears to very important in maintaining the intestinal barrier and gut immunity, as well as regulating intestinal growth (regulating EC proliferation and apoptosis) (45, 46, 48, 51). Alterations in the luminal environment may produce significant changes in the IEL. A previous study from our group has shown that administration of total parenteral nutrition (TPN) in mice (the complete absence of luminal nutrients) led to a significant decline in the CD4⫹,CD8⫺, CD4⫹,CD8⫹, and CD8⫹,CD44⫹ IEL subpopulations, as well as a nearly complete loss of the CD8␣⫹ IEL population. TPN also led to a significant change in the expression of a variety of cytokines (16, 45). This change in IEL function resulted in a loss of epithelial barrier function and intestinal mucosal atrophy (47, 48, 52). The mechanism that caused these IEL changes is unknown. Recent studies have demonstrated that interactions between mucosal lymphocytes and intestinal EC are crucial in regulating the immune response in the intestinal mucosa (33, 37, 45, 46). Several studies have indicated that EC may play an important role in mucosal immune responses by helping to regulate IEL phenotype and function (11, 37). Watanabe et al. (37) demonstrate that intestinal EC express IL-7. IL-7 has been shown to play a crucial role in controlling T cell development and homeostasis (4), and this is supported by the wide range of IEL subpopulations that express IL-7R (18, 37, 44). IL-7 knockout and IL-7R knockout mice show distinct declines in absolute numbers of thymocytes and IEL (including an absence of ␥␦-TCR⫹ IEL) (24). Using the intestinal fatty acid binding protein promoter, Laky et al. (18) were able to reinstate IL-7 expression in IL-7 knockout mice, and this low level of expression was sufficient for the development of the extrathymic IEL. This demonstrates the essential role that the local expression of IL-7 has on the development of the mucosal immune system. Exogenous administration of IL-7 resulted in a significant increase in CD8␣⫹ IEL. Exogenous IL-7 also resulted in a similar stimulation of LPL growth (24, 49). In a more elegant fashion, Watanabe et al. (38) showed that the systemic overexpression of IL-7 with an SR␣ promoter demonstrated an expansion of lymphoid populations and the development of chronic colitis. One particular distinguishing feature of our particular model is that the overexpression of IL-7 is predominantly in the small bowel and progressively decreases in the colon, so that we may not observe the degree of colitic changes that was identified by Watanabe et al. The functional relevance of altered IL-7 expression in the mucosal epithelium is illustrated in a recent study by our laboratory that showed that TPN administration resulted in a significant decrease in EC-derived IL-7 expression (53). Additionally, exogenous IL-7 administration to TPN mice significantly attenuated TPN-associated IEL changes (50). The precise etiology of these TPN-associated changes in IL-7 is uncertain. It is difficult to determine whether the action of the INTESTINAL MUCOSA SPECIFIC OVEREXPRESSION OF IL-7 interesting, in that although IL-7 is critical for the formation of ␥␦-TCR⫹ IEL, IL-7 overexpression had little action on expanding the ␥␦-TCR⫹ IEL population but was able to influence its functional expression of both cytokines and growth factors. We did not find any significant change in IL-2 or IL-4 expression between IL-7vill and wild-type mice. It is possible that exogenous administration of IL-7 may stimulate extramucosal lymphoid populations that may account for the observed increase in IEL-derived IL-2, a finding that did not occur in our IL-7vill transgenic mouse model. A previous study of our laboratory has shown that there is a close physical crosscommunication between EC-derived IL-7 and the neighboring IEL via the IL-7R (49). Taken together, our data suggest that cell-to-cell interactions between EC and IEL, via IL-7/IL-7R, are an important mode of communication for the maintenance and activation of the IEL. In conclusion, this study demonstrated that intestinal specific IL-7 overexpression significantly affected IEL and LPL populations and significantly changed IEL function, resulting in overexpansion of the CD4⫹, CD8␣⫹ IEL, and ␣-TCR⫹ IEL subtypes, as well as an increase CD4⫹ IEL maturation and activation. The results of this study confirm a close physical and functional cross-communication between EC-derived IL-7 and the mucosal lymphoid population. ACKNOWLEDGMENTS This study was presented in part at the Annual Congress of the American Gastroenterology Association, May 14 –19, 2005, Chicago, IL. GRANTS This research was supported by National Institute of Allergy and Infectious Diseases Grant 2R01-AI044076-08 (to D. H. Teitelbaum), National Institute of Diabetes and Digestive and Kidney Diseases Grant 5R01DK065850-02 (to D. L. Gumucio), the ASPEN Rhoads Research Foundation Maurice Shils Grant (to H. Yang), and the University of Michigan DNA Core, University of Michigan Transgenic Core. REFERENCES AJP-Gastrointest Liver Physiol • VOL 1. Armitage RJ, Namen AE, Sassenfeld HM, Grabstein KH. Regulation of human T cell proliferation by IL-7. J Immunol 144: 938 –941, 1990. 2. Barnard JA, Beauchamp RD, Coffey RJ, Moses HL. Regulation of intestinal epithelial cell growth by transforming growth factor type beta. Proc Natl Acad Sci USA 86: 1578 –1582, 1989. 3. Beagley KW, Husband AJ. Intraepithelial lymphocytes: origins, distribution, function. Crit Rev Immunol 18: 237–254, 1998. 4. Bhatia SK, Tygrett LT, Grabstein KH, Waldschmidt TJ. The effect of in vivo IL-7 deprivation on T cell maturation. J Exp Med 181: 1399 –1409, 1995. 5. Boismenu R, Havran WL. Modulation of epithelial cell growth by intraepithelial gamma delta T cells. Science 266: 1253–1255, 1994. 6. Borger P, Kauffman HF, Postma DS, Vellenga E. IL-7 differentially modulates the expression of IFN-gamma and IL-4 in activated human T lymphocytes by transcriptional and post-transcriptional mechanisms. J Immunol 156: 1333–1338, 1996. 7. Eisenbraun MD, Mosley RL, Teitelbaum DH, Miller RA. Altered development of intestinal intraepithelial lymphocytes in P-glycoproteindeficient mice. Dev Comp Immunol 24: 783–795, 2000. 8. Fujihashi K, Kawabata S, Hiroi T, Yamamoto M, McGhee JR, Nishikawa S, Kiyono H. Interleukin 2 (IL-2) and interleukin 7 (IL-7) reciprocally induce IL-7 and IL-2 receptors on gamma delta T cell receptor-positive intraepithelial lymphocytes. Proc Natl Acad Sci USA 93: 3613–3618, 1996. 9. Geiselhart LA, Humphries CA, Gregorio TA, Mou S, Subleski J, Komschlies KL. IL-7 administration alters the CD4:CD8 ratio, increases T cell numbers, and increases T cell function in the absence of activation. J Immunol 166: 3019 –3027, 2001. 294 • JUNE 2008 • www.ajpgi.org Downloaded from ajpgi.physiology.org on June 10, 2008 exogenous IL-7 was due to an effect on the thymus or directly on the intestinal mucosa. Using intestinal specific overexpressing IL-7 transgenic mice has greatly facilitated our understanding of the role of EC-derived IL-7 on the neighboring IEL. This allows one to detect the action of IL-7 in a more local or paracrine fashion, as opposed to systemic (or endocrine) action of this cytokine. In our present study, the IEL population was significantly expanded, consisting of an increase in the CD4⫹ and CD8␣⫹, as well as ␣-TCR⫹ IEL subtypes. The increase in IEL subtypes is disproportionately biased to an expansion of the CD4⫹ IEL population, which increased ninefold, compared with CD8⫹ IEL, which increased fourfold compared with wild-type mice. A bias toward the expansion of the ␣-TCR⫹ IEL over the ␥␦-TCR⫹ IEL subpopulation was also noted. This appears consistent with a greater colocalization of IL-7 expression the ␣-TCR⫹ group of IEL (49). Our observation of an increase in IEL proliferation, as well as a marked increase in CD103 (integrin ␣E7), suggests that the expansion of the IEL population was due to both a local increase in IEL growth as well as a recruitment of extraintestinal lymphocytes to the epithelium. Interestingly, the LPL population was also expanded in our transgenic mice. The fact that we did not find any significant changes in the systemic lymphoid population in our IL-7vill transgenic mice shows that the critical action of this local (paracrine) expression of IL-7 was confined to the formation of the IEL and LPL populations and suggests a potential functional role of EC-derived IL-7 to act on the underlying LPL population. Studies suggest that IEL do not spend their entire cycle in the epithelium but recirculate into the lamina propria after activation, although this movement occurs at a much slower rate than for most T cells (3, 11). Those studies may explain the fact that LPL population was also found to be significantly expanded in our transgenic mice. It is also possible that this expansion of the LPL might be due to a direct effect of the IL-7 acting below the basement membrane of the epithelium on the T cell population of the LPL. Although many of these changes may potentially have been due to increased nutritional intake in the transgenic group, this appears unlikely. In fact, the measured amount of chow consumed was not different between transgenic and wild-type mice. Furthermore, body weights were actually about lower for the IL-7vill transgenic mice, compared with wild-types (20.49 ⫾ 0.81 vs. 22.91 ⫾ 0.87 g, at 8 wk of life for transgenic vs. wild-type, respectively), suggesting that the increase in lymphoid populations was not due to increased food intake. IL-7 has been shown to enhance peripheral T cell expression of IL-4 (2, 6). Jiang and McGee (14) found that EC-derived IL-7 could enhance human peripheral T cell IL-4 secretion but not IFN-␥ in a cell culture model. A recent study from our group showed that exogenous IL-7 administration to wild-type healthy mice can upregulate both ␣-TCR⫹ and ␥␦-TCR⫹ IEL-derived IL-2 and IL-10 expression. As well, IL-7 was also able to increase the expression of ␥␦-TCR⫹ IEL-derived KGF expression. IL-7 had no effect on the expression of IL-4 or IL-6 (49). In this present study, both ␣-TCR⫹ and ␥␦-TCR⫹ IEL-derived cytokine expressions were studied. Both IFN-␥ and TNF-␣ expression were noted to be significantly increased in IL-7vill transgenic mice compared with wild-type mice. Interestingly, ␥␦-TCR⫹ IEL-derived KGF expression was also noted to increase in our transgenic mice. This latter finding is G1429 G1430 INTESTINAL MUCOSA SPECIFIC OVEREXPRESSION OF IL-7 33. Suzuki K, Oida T, Hamada H, Hitotsumatsu O, Watanabe M, Hibi T, Yamamoto H, Kubota E, Kaminogawa S, Ishikawa H. Gut cryptopatches: direct evidence of extrathymic anatomical sites for intestinal T lymphopoiesis. Immunity 13: 691–702, 2000. 34. Tan JT, Dudl E, LeRoy E, Murray R, Sprent J, Weinberg KI, Surh CD. IL-7 is critical for homeostatic proliferation and survival of naive T cells. Proc Natl Acad Sci USA 98: 8732– 8737, 2001. 35. Thomis DC, Gurniak CB, Tivol E, Sharpe AH, Berg LJ. Defects in B lymphocyte maturation and T lymphocyte activation in mice lacking Jak3. Science 270: 794 –797, 1995. 36. Tough DF, Sprent J. Turnover of naive- and memory-phenotype T cells. J Exp Med 179: 1127–1135, 1994. 37. Watanabe M, Ueno Y, Yajima T, Iwao Y, Tsuchiya M, Ishikawa H, Aiso S, Hibi T, Ishii H. Interleukin 7 is produced by human intestinal epithelial cells and regulates the proliferation of intestinal mucosal lymphocytes. J Clin Invest 95: 2945–2953, 1995. 38. Watanabe M, Ueno Y, Yajima T, Okamoto S, Hayashi T, Yamazaki M, Iwao Y, Ishii H, Habu S, Uehira M, Nishimoto H, Ishikawa H, Hata J, Hibi T. Interleukin 7 transgenic mice develop chronic colitis with decreased interleukin 7 protein accumulation in the colonic mucosa. J Exp Med 187: 389 – 402, 1998. 39. Watanabe M, Yamazaki M, Okamoto R, Ohoka S, Araki A, Nakamura T, Kanai T. Therapeutic approaches to chronic intestinal inflammation by specific targeting of mucosal IL-7/IL-7R signal pathway. Curr Drug Targets Inflamm Allergy 2: 119 –123, 2003. 40. Weissenbach M, Clahsen T, Weber C, Spitzer D, Wirth D, Vestweber D, Heinrich PC, Schaper F. Interleukin-6 is a direct mediator of T cell migration. Eur J Immunol 34: 2895–2906, 2004. 41. Welch PA, Namen AE, Goodwin RG, Armitage R, Cooper MD. Human IL-7: a novel T cell growth factor. J Immunol 143: 3562–3567, 1989. 42. Witkowski J, Miller R. Increased function of P-glycoprotein in T lymphocyte subsets of aging mice. J Immunol 150: 1296 –1306, 1993. 43. Yada S, Nukina H, Kishihara K, Takamura N, Yoshida H, InagakiOhara K, Nomoto K, Lin T. IL-7 prevents both caspase-dependent and -independent pathways that lead to the spontaneous apoptosis of i-EIL. Cell Immunol 208: 88 –95, 2001. 44. Yamazaki M, Yajima T, Tanabe M, Fukui K, Okada E, Okamoto R, Oshima S, Nakamura T, Kanai T, Uehira M, Takeuchi T, Ishikawa H, Hibi T, Watanabe M. Mucosal T cells expressing high levels of IL-7 receptor are potential targets for treatment of chronic colitis. J Immunol 171: 1556 –1563, 2003. 45. Yang H, Antony PA, Wildhaber BE, Teitelbaum DH. Intestinal intraepithelial lymphocyte gammadelta-T cell-derived keratinocyte growth factor modulates epithelial growth in the mouse. J Immunol 172: 4151– 4158, 2004. 46. Yang H, Fan Y, Teitelbaum DH. Intraepithelial lymphocyte-derived interferon-gamma evokes enterocyte apoptosis with parenteral nutrition in mice. Am J Physiol Gastrointest Liver Physiol 284: G629 –G637, 2003. 47. Yang H, Finaly R, Teitelbaum DH. Alteration in epithelial permeability and ion transport in a mouse model of total parenteral nutrition. Crit Care Med 31: 1118 –1125, 2003. 48. Yang H, Kiristioglu I, Fan Y, Forbush B, Bishop DK, Antony PA, Zhou H, Teitelbaum DH. Interferon-gamma expression by intraepithelial lymphocytes results in a loss of epithelial barrier function in a mouse model of total parenteral nutrition. Ann Surg 236: 226 –234, 2002. 49. Yang H, Spencer AU, Teitelbaum DH. Interleukin-7 administration alters intestinal intraepithelial lymphocyte phenotype and function in vivo. Cytokine 31: 419 – 428, 2005. 50. Yang H, Sun X, Haxhija EQ, Teitelbaum DH. Intestinal epithelial cell-derived interleukin-7: a mechanism for the alteration of intraepithelial lymphocytes in a mouse model of total parenteral nutrition. Am J Physiol Gastrointest Liver Physiol 292: G84 –G91, 2007. 51. Yang H, Teitelbaum DH. Novel agents in the treatment of intestinal failure: humoral factors. Gastroenterology 130: S117–S121, 2006. 52. Yang H, Wildhaber B, Tazuke Y, Teitelbaum DH. 2002 Harry M. Vars Research Award. Keratinocyte growth factor stimulates the recovery of epithelial structure and function in a mouse model of total parenteral nutrition. JPEN J Parenter Enteral Nutr 26: 333–340; discussion 340 –341, 2002. 53. Yang H, Wildhaber BE, Teitelbaum DH. Decline in intestinal epithelial cell-derived IL-7: a mechanism for the alteration of intraepithelial lymphocytes in a mouse model of total parenteral nutrition (Abstract). Gastroenterology 126: A-126, 2004. AJP-Gastrointest Liver Physiol • VOL 294 • JUNE 2008 • www.ajpgi.org Downloaded from ajpgi.physiology.org on June 10, 2008 10. Guy-Grand D, Vassalli P. Gut intraepithelial T lymphocytes. Curr Opin Immunol 5: 247–252, 1993. 11. Hayday A, Theodoridis E, Ramsburg E, Shires J. Intraepithelial lymphocytes: exploring the Third Way in immunology. Nat Immunol 2: 997–1003, 2001. 12. He YW, Malek TR. The structure and function of gamma c-dependent cytokines and receptors: regulation of T lymphocyte development and homeostasis. Crit Rev Immunol 18: 503–524, 1998. 13. Howie D, Spencer J, Delord D, Pitzalis C, Wathen NC, Dogan A, Akbar A, Macdonald TT. Extrathymic T cell differentiation in the human intestine early in life. J Immunol 161: 5862–5872, 1998. 14. Jiang Y, McGee DW. Regulation of human lymphocyte IL-4 secretion by intestinal epithelial cell-derived interleukin-7 and transforming growth factor-beta. Clin Immunol Immunopathol 88: 287–296, 1998. 15. Kenai H, Matsuzaki G, Nakamura T, Yoshikai Y, Nomoto K. Thymusderived cytokine(s) including interleukin-7 induce increase of T cell receptor ␣⫹ CD4-CD8- T cells which are extrathymically differentiated in athymic nude mice. Eur J Immunol 23: 1818 –1825, 1993. 16. Kiristioglu I, Antony P, Fan Y, Forbush B, Mosley RL, Yang H, Teitelbaum DH. Total parenteral nutrition-associated changes in mouse intestinal intraepithelial lymphocytes. Dig Dis Sci 47: 1147–1157, 2002. 17. Kiristioglu I, Teitelbaum DH. Alteration of the intestinal intraepithelial lymphocytes during total parenteral nutrition. J Surg Res 79: 91–96, 1998. 18. Laky K, Lefrancois L, Lingenheld EG, Puddington L. Enterocyte expression of interleukin 7 induces development of gamma delta T cells and Peyer’s patches. J Exp Med 191: 1569 –1580, 2000. 19. Laouar Y, Crispe IN, Flavell RA. Overexpression of IL-7R alpha provides a competitive advantage during early T-cell development. Blood 103: 1985–1994, 2004. 20. Li J, Kudsk KA, Gocinski B, Dent D, Glezer J, Langkamp-Henken B. Effects of parenteral and enteral nutrition on gut-associated lymphoid tissue. J Trauma 39: 44 –52, 1995. 21. Lin T, Matsuzaki G, Yoshida H, Kenai H, Omoto K, Umesue M, Singaram C, Nomoto K. Thymus ontogeny and the development of TCR alpha beta intestinal intraepithelial lymphocytes. Cell Immunol 171: 132–139, 1996. 22. Madison BB, Braunstein K, Kuizon E, Portman K, Qiao XT, Gumucio DL. Epithelial hedgehog signals pattern the intestinal crypt-villus axis. Development 132: 279 –289, 2005. 23. Madison BB, Dunbar L, Qiao XT, Braunstein K, Braunstein E, Gumucio DL. Cis elements of the villin gene control expression in restricted domains of the vertical (crypt) and horizontal (duodenum, cecum) axes of the intestine. J Biol Chem 277: 33275–33283, 2002. 24. Maki K, Sunaga S, Komagata Y, Kodaira Y, Mabuchi A, Karasuyama H, Yokomuro K, Miyazaki JI, Ikuta K. Interleukin 7 receptor-deficient mice lack gammadelta T cells. Proc Natl Acad Sci USA 93: 7172–7177, 1996. 25. Maunoury R, Robine S, Pringault E, Leonard N, Gaillard JA, Louvard D. Developmental regulation of villin gene expression in the epithelial cell lineages of mouse digestive and urogenital tracts. Development 115: 717–728, 1992. 26. Miller RA. Age-related changes in T cell surface markers: a longitudinal analysis in genetically heterogeneous mice. Mech Ageing Dev 96: 181– 196, 1997. 27. Pinto D, Robine S, Jaisser F, El Marjou FE, Louvard D. Regulatory sequences of the mouse villin gene that efficiently drive transgenic expression in immature and differentiated epithelial cells of small and large intestines. J Biol Chem 274: 6476 – 6482, 1999. 28. Porter BO, Malek TR. Thymic and intestinal intraepithelial T lymphocyte development are each regulated by the gammac-dependent cytokines IL-2, IL-7, and IL-15. Semin Immunol 12: 465– 474, 2000. 29. Rocha B, Vassalli P, Guy-Grand D. Thymic and extrathymic origins of gut intraepithelial lymphocyte populations in mice. J Exp Med 180: 681– 686, 1994. 30. Rubin J, Osada H, Finch P. Purification and characterization of a newly identified growth factor specific for epithelial cells. Proc Natl Acad Sci USA 806: 802–906, 1989. 31. Sillett HK, Southgate J, Howdle PD, Trejdosiewicz LK. Expression of activation and costimulatory elements by human intestinal intraepithelial lymphocytes. Scand J Immunol 50: 52– 60, 1999. 32. Sudo T, Nishikawa S, Ohno N, Akiyama N, Tamakoshi M, Yoshida H. Expression and function of the interleukin 7 receptor in murine lymphocytes. Proc Natl Acad Sci USA 90: 9125–9129, 1993.