IC Documentation 4
advertisement

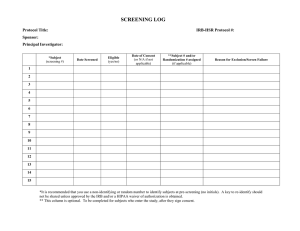
Documentation of the Informed Consent Process USC Office for the Protection of Research Subjects (OPRS) Session Overview Highlights: • Purpose of Informed Consent (IC) • IC Process and Documentation • Witness and Dates on IC • HIPAA Authorization • Significant New Information and Findings (SNIFs) • IC Errors or Omissions • Double-Checking IC Documentation • IC Audit Findings • Resources / Contacts Purpose of Informed Consent Consent (“autonomy” from the Belmont Report) • Protects human subjects • Ensures subject understand the study and are informed about its risks, benefits and procedures • Provides subject an opportunity to ask questions • Allows subjects to voluntary decide whether or not to participate in research Informed Consent is a Process This presentation is focused on IC documentation, however: • Remember that Informed Consent is not just a form…it’s a process that involves ongoing exchange of information • Subjects must be informed about changes or new information about the study that may affect their willingness to participate Informed Consent Process • Use the current IRB-approved, stamped consent for the study • Provide subject or Legally Authorized Representative (LAR) a consent Form in his/her language (or use Short Form Process) • Ensure subjects/LARs have sufficient time to consider participation, free of coercion or undue influence • Provide subject/LAR an opportunity to ask questions about the study Informed Consent Documentation • Subject/LAR must sign and date the form • Person Obtaining Consent must sign and date the form • Provide a copy of the signed consent to the subject/LAR • Document in the subject’s chart or medical record that consent was obtained and file the Consent Form in subject’s records • Document use of a translator on subject’s chart, if applicable Short Form Process • When non-English speaking subjects are anticipated in a study, the consent form should be translated in the subjects’ language • Use the Short Form Process for the unexpected enrollment of subjects when a consent is not available in the subject’s language • A witness and translator must be present during the consent process (translator may serve as witness) • CA Subject Bill of Rights in the subject /LAR’s language (if applicable) *Tip: see pg 1 of consent • Short Form and Subject Bill of Rights templates are available in thirteen languages on the HSIRB website at: http://www.usc.edu/admin/oprs/hsirb/forms Short Form Process • Subject /LAR is presented with a copy of the Short Form and Bill of Rights (if applicable) in a language he/she understands • Translator orally translates the current, IRB approved study consent in the subject’s/LAR’s language in the presence of a witness • Ensure subjects/LARs have sufficient time to consider participation, free of coercion or undue influence • Provide subject/LAR an opportunity to ask questions about the study Short Form Process Documentation • Subject/LAR dates and signs the Short Form and Subject Bill of Rights, if applicable • Witness dates and signs the Short Form and Consent • Person Obtaining Consent dates and signs the Consent • Subject /LAR receives a copy of the signed Short Form, Bill of Rights (if applicable) and Consent • Document that consent was obtained from the subject/LAR in the subject’s chart or medical record and file Short Form, Bill of Rights (if applicable) and Consent in subject’s chart Conditional IC Process • Certain conditions (e.g., illiteracy, blindness) may impede documentation of subject consent • Conditional consent process can be utilized • A witness must be present during the consent process • Ensure subjects/LARs have sufficient time to consider participation, free of coercion or undue influence • Provide subject/LAR an opportunity to ask questions about the study Conditional IC Process Documentation • Subject makes a “mark” on the consent form, if possible • Witness signs and dates consent form • Person Obtaining Consent signs and dates consent form • On consent form, note the method used for communicating with subject and the means by which subject communicated agreement • Subject receives a copy of the signed consent • Document that consent was obtained from the subject in the subject’s chart or medical record and file Consent Consent Witness • Not required unless using the Short Form or the Conditional Process • Additional considerations may be imposed by: • FDA and ICH GCP: “impartial witness” when the subject or LAR is illiterate • Study sponsor • Institutional • Refer to the study protocol, investigator, sponsor or IRB to determine requirements for your study IC Documentation *if consent includes California Subject Bill of Rights, subject must sign Bill of Rights (1st page) and consent (last page) ** Bill of Rights, if applicable (check if English version of consent includes Bill of Rights on 1st page) Tip sheet available at: http://www.usc.edu/admin/oprs/private/docs/hsirb/forms/Consent_and_Short_Forms_Final.pdf Dates on Informed Consent • Signature dates of person obtaining consent and subject or LAR do not have to match (e.g., investigator may sign and date consent during process and subject may sign and date consent after discussion with relatives) • Subject or LAR must sign and date consent before any study procedures are conducted (FDAregulated studies: if subject signs consent on the day study procedures begin, subject chart should document that consent was obtained prior to study procedures) • Check sponsor guidelines • Do not “back date” consent! HIPAA – Privacy Rule • Protected Health Information (PHI) is any identifiable health information relating to a subject’s physical or mental condition or payment for health care (18 elements) • If your study accesses (or creates) PHI, subjects (or LARs) must sign a HIPAA form in addition to informed consent • Changes to the HIPAA form cannot be made unless the Office of Compliance has approved these changes HIPAA Waivers The IRB may grant the following waivers: • Partial HIPAA waiver - for screening, recruiting and identifying participants (very common) • Full HIPAA waiver – if use or disclosure of PHI involves no more than minimal risk to subject, the research could not practicably be conducted without the waiver and the research could not practicably be conducted without access to and use of PHI (rare) Remember: without a HIPAA authorization or waiver, researchers cannot utilize PHI data! Significant New Findings/Information (SNIFs) • Except when necessary to eliminate apparent immediate hazards to subjects, the IRB must review and approve SNIF • Subjects must be informed about SNIFs that may affect their willingness to continue participation • SNIF must be presented to subject in his/her language • Don’t forget to make arrangements for non-English speaking subjects (e.g., originally consented with a translated consent or short form) • HSIRB can provide Spanish translation of SNIF IC Errors or Omissions • If an error is made on the consent: • Strikethrough the mistake with a single line, write the correct information next to it and initial and date the correction (i.e., original entry must be visible) • If an entry was inadvertently omitted: • Initial and date any entry made after the consent process (should be done by person making entry) • Include explanation in the subject’s record or Note to File IC Version vs. Approval / Expiration Dates IC Approval Date and Expiration Date • Located on right margin of each consent form page. Includes IRB study number and valid date range. Ensure that subjects are provided a current, IRB-approved consent. IC Version (HSC) or Date of Preparation (UPC) • Located on the footer of the consent form. This reflects the date the consent was last updated, NOT the approval or expiration dates. Double-Check IC Documentation Remember to check: • • • • • • • Consent expiration date Consent version date Fill-in sections of consent Names, dates and signatures HIPAA Authorization Copies of consent/HIPAA provided to subject/LAR Copies of consent, Short Forms, Bill of Rights and HIPAA were filed in subject’s medical record, as applicable • Documentation that subject/LAR agreed to participate in study in subject’s chart or medical record Approved Documents in iStar To access Approved Documents (consent forms, HIPAA forms, recruitment materials, etc) • Click on “Approved Documents” link or “Documents” tab Additional Considerations • Study personnel must complete educational requirements based on study (e.g. Human Subjects Training, HIPAA, GCP) • New study personnel must be trained on study procedures including the consent process • Regular communication ensures study team is aware of changes in the study and consent documents • If there is a lapse in IRB approval for the study, the study team cannot proceed with study procedures (unless IRB has authorized) IC Audit Findings Most common: • • • • Use of expired consent Use of older version of consent Missing entries on consent Signature date errors Other: • Study staff fill-in subject or LAR sections of consent • Consents are not handwritten (e.g., dates stamped) • Use of one consent for multiple subjects Resources Informed Consent templates and Short Forms: http://www.usc.edu/admin/oprs/hsirb/forms/ OPRS Informed Consent in Human Subjects Brochure: http://www.usc.edu/admin/oprs/private/docs/oprs/broc hures/IFC_Booklet.pdf HSIRB Website: http://www.usc.edu/admin/oprs/hsirb/w.usc.edu/admin/ provost/oprs/training/videos.html Contacts http://www.usc.edu/admin/provost/oprs Health Sciences Campus General Hospital, Suite 4700 1200 North State Street Los Angeles, CA 90033 Tel: (323)223.2340 Fax: (323)224.8389 E-mail: irb@usc.edu Office for the Protection of Research Subjects 3720 South Flower, Third Floor Los Angeles, CA 90089-0706 Tel: (213)821.1154 Fax: (213)740.9299 E-mail: oprs@usc.edu http://www.usc.edu/admin/provost/oprs/ http://www.usc.edu/admin/provost/oprs/hsirb/ University Park Campus 837 Downey Way Stonier Hall, Room 224a Los Angeles, CA 90089-1146 Tel: (213)821.5272 Fax: (213)821.5276 E-mail: upirb@usc.edu http://www.usc.edu/admin/provost/oprs/upirb/ Office of Compliance 3500 Figueroa St. University Gardens Building, Room 105 Los Angeles, CA 90007 Tel: (213)740.8258 Fax: (213)740.9657 E-mail: complian@usc.edu http://www.usc.edu/admin/compliance/ Jennifer Hagemann, MS Office for the Protection of Research Subjects Program started on May 2008 Human Subjects Protection Program Accreditation (AAHRPP) Not-for-cause audits Criteria: random but… High volume of studies Vulnerable population New investigators to USC Format: 2-3 hours, review 2-6 studies, focus: study documentation Consent 72% IRB Application Discrepancies 39% Problem Areas Lack of Documentation 30% HIPPA Form 20% Miscellaneous 13% Lack of Communication with FDA 11% Lack of Communication with IRB 11% Personnel-Related Issues 9% Protocol Non-Compliance 7% 0% 10% 20% 30% 40% 50% 60% 70% 80% Findings by Percentage Consent + HIPAA form Issues: no documentation of consent; use of unapproved consent; missing subject name, signature, or signature date; missing PI signature; use of wrong HIPAA form; HIPAA form not signed by subjects; required fields not completed in HIPAA form IRB Application Discrepancies: discrepancies between IRB application and study procedures; unable to locate approved documents in iStar; study personnel different from those in application; personnel obtaining consent is different from that in application Lack of Documentation: no documentation of subjects meeting inclusion/exclusion criteria; no regulatory binder or substantial documentation missing Personnel-Related Issues: lack of GCP training; lack of personnel; lack of personnel oversight Lack of Communication with FDA: personnel listed on Form 1572 form differs from IRB application; missing information in Form 1572; lack of annual progress report for investigatorinitiated studies Lack of Communication with IRB: done in untimely manner; study closure report not submitted; protocol deviations not reported to IRB Protocol Non-Compliance: differences between protocol and study procedures; inclusion/exclusion violations Miscellaneous: potential for subject coercion; funding not distributed to proper channel, investigator unaware of consent requirement for all subjects and study closure responsibilities FDA: FDA-regulated research (drugs, biologics, devices) http://www.fda.gov/ICECI/EnforcementActions/Bioresearch Monitoring/default.htm OHRP: human subjects research, normally those funded by Health and Human Services (HHS) http://www.hhs.gov/ohrp/compliance/index.html Study Sponsor: for-cause, non-compliance IRB for-cause: non-compliance, whistleblower, deficiencies in IRB submissions, lapses in IRB approval Socio-Behavioral vs. Biomedical Research Templates* (http://www.usc.edu/admin/oprs/research/rc) Study / Regulatory Binder* Participant files ▪ Source Documentation (e.g., physical exam, survey, ECG) ▪ Case Report Forms ▪ Notes to file ▪ Calendar / Subject Visit log* ▪ Consent documentation Logs: Enrollment*, Screening*, Training Train staff: initial and ongoing; maintain log Meet regularly: discuss new developments, Maintain open communication lines: ensure procedures, revised consents team members know whom to contact when unexpected or adverse events occur Standardize procedures: study procedures should be consistent and systematic for all participants (e.g., assessments, recruitment, consent) Participate in educational meetings: specific to field (e.g., symposia) and institution (e.g., IRB training) Form Templates USC http://www.usc.edu/admin/oprs/research/rc Partners UCSF http://www.partners.org/phsqi/vrb/files/index.htm http://hub.ucsf.edu/regulatory-binder USC IRB and OPRS website http://www.usc.edu/admin/oprs/ Investigator Tips – HSC IRB • USC Institutional Review Board (IRB) • Sandy Jean, MS Overview • • • • Recruitment of Participants Retention of Research Records Confidentiality and Security of Research Records What Happens After Your Study is Approved? • Amendments • Continuing Review • Reportable Events Recruitment • • • • Recruitment is the first step in consent process Respect privacy during recruitment IRB reviews and approves recruitment materials Tips for recruitment advertisements • DO: – State that it is research – State what is involved (very brief) – Add department name, USC name or approved logo, IRB number, version date Recruitment • DON’T: – Overstate benefits of participation – Emphasize payment for participation or free services – Use the word “treatment” if your study involves experimental procedures Recruitment • Cannot pay a bonus or finder’s fee for referrals to your study (USC policy) • Cannot coerce students or employees into participating • Avoid appearance of coercion: • Post recruitment flyers in public areas rather than directly approaching students or employees • Have another investigator obtain consent from participants who are your students or employees Confidentiality • Collect the minimum amount of personal info you need to achieve your study objectives • If possible, record data anonymously • If not, record and label data with a random code instead of an identifier • The master list matching up code numbers with names (or other identifiers) must be stored in a secure place, separate from the coded data Confidentiality • Can data be shared with others? • Only as described in the IRB application and as disclosed to participants in the informed consent • Handle your participants’ data the way you want your own sensitive info handled • HIPAA Privacy Rule • Violation of HIPAA rules can lead to fines and imprisonment Security of Records Paper: • Store in locked file drawers, locked office/storage area • Restrict access to research staff (as identified in the IRB application) • Restrict copying of study documents and data Photos and Recordings: • Alter identifying features as early as possible • Transcribe and destroy recordings Security of Records Electronic: • • • • User name and password required to access data files Restrict access to research staff Restrict copying of electronic files Mobile storage devices (laptops, stick drives) must be password protected and encrypted “USC requires all laptops and mobile storage devices that are paid for with university funds and/or used for USC business purposes to be encrypted. We strongly encourage you to avoid storing any sensitive data on such equipment altogether.” - USC Policy Memo dated April 22, 2009 Record Retention How long should you keep research records? • USC policy = 3 years after research is completed • FDA-regulated products (drugs/devices) = 2 years after product is approved / sponsor stops testing • Sponsor may have additional requirements • HIPAA forms = 6 years after research is completed IRB Review after Approval Reminder - Principal Investigator and Faculty Advisor Responsibilities • • • • All staff are properly trained and licensed Won’t change protocol without IRB approval first Will use only current, stamped consent for enrollment Faculty Advisors: • Meet with student regularly to monitor study progress • Arrange for another faculty member to accept responsibility if unable to supervise the student personally IRB Review after Approval Now what? Ongoing responsibilities to IRB: • Amendments – whenever you want to make changes to the study • Continuing Review – annually • Reportable Events – as needed IRB Review after Approval Amendments • Submit amendment for IRB approval BEFORE * implementing changes (add/change procedures, eligibility criteria, informed consent or recruitment materials; or sponsor requires changes) • Open an amendment application in iStar: – Describe changes in amendment application – Edit study application – Wait for IRB approval * Unless change is needed to avoid immediate harm to participants IRB Review after Approval Significant New Information • • • • • If you learn new info that could affect participants’ willingness to continue in the study, you must tell them (as promised in the informed consent) Usually involves new risks or new procedures Prepare “Significant New Information/Findings” form (template available) Submit an amendment to IRB After IRB approval, provide form and discuss with participant IRB Review after Approval Continuing Review (CR) Unless your research qualifies as “exempt” your IRB approval will expire every year. You must submit an annual CR to keep the study open. CR is a review of the research activities over the past year. • You will receive reminders about study expiration • Open a CR application in iStar: – Provide info requested (enrollment to date, participant complaints or withdrawals, study progress) – Submit to IRB at least 1 month before study expires • If study expires, ALL research activities must stop IRB Review after Approval Study Closure When all research activities done (including all data analysis), submit “Final Report” to close study • Open a CR application • Select the “Final Report” option • Provide info requested • Study will be archived in iStar IRB Review after Approval Reportable Events What problems must be reported to the IRB? • Adverse Events • Participant experiences a side effect that is unexpected, serious, and related to the research • Unanticipated Problems (place participants, research staff, or others at greater risk of harm than was previously known) • Laptop containing data is stolen or lost • Files with signed informed consents are lost during a move IRB Review after Approval • Protocol Deviations • Enrollment of a participant who was ineligible • Procedures missed or performed outside of window • Expired or wrong consent form used to enroll participant • Procedure: • • • • Open a Reportable Event application in iStar Select type of event Provide info requested IRB will either acknowledge or request more info (including a corrective action plan) Questions? training/videos.html