Grading of monosodium iodoacetate-induced osteoarthritis reveals
advertisement

Neuroscience Letters 465 (2009) 184–188
Contents lists available at ScienceDirect
Neuroscience Letters
journal homepage: www.elsevier.com/locate/neulet
Grading of monosodium iodoacetate-induced osteoarthritis reveals
a concentration-dependent sensitization of nociceptors in the
knee joint of the rat
Niklas Schuelert, Jason J. McDougall ∗
Department of Physiology & Pharmacology, University of Calgary, 3330, Hospital Drive NW, Calgary, AB, T2N 4N1 Canada
a r t i c l e
i n f o
Article history:
Received 2 July 2009
Received in revised form 14 August 2009
Accepted 24 August 2009
Keywords:
Joint pain
Osteoarthritis
Monosodium iodoacetate
Electrophysiological recordings
Animal model
Joint primary afferents
a b s t r a c t
Osteoarthritis (OA) is a degenerative joint disease characterized by joint pain for which there is currently
no effective treatment. Previous studies have found that intra-articular injection of monosodium iodoacetate (MIA) caused a dose-dependent destruction of rat knees with concomitant increased pain. In this
study, varying degrees of OA were induced by intra-articular injection of 0.1 mg, 0.3 mg and 3 mg MIA.
Electrophysiological recordings were made from knee joint primary afferents in response to rotation of
the joint and firing frequencies were determined and compared to saline-injected control joints. The analgesic effect of local application of the classic non-steroidal anti-inflammatory drug (NSAID) diclofenac
(0.1 mg/0.1 ml bolus) was also determined in each group. Joint afferent firing frequency was significantly
enhanced in OA knees compared to saline injected control joints and the magnitude of this sensitization
showed a direct relationship with increasing dose of MIA. Diclofenac reduced nociception significantly
in the 3 mg MIA treated joint, but had no effect on nerve mechanosensitivity in rats with milder OA.
This study shows for the first time that MIA produces a graded sensitization of joint nociceptors making this a useful model for the study of pain mechanisms in joints with progressive OA severity. The
anti-nociceptive effect of diclofenac further indicates that the MIA model offers an attractive means of
objectively testing potential therapeutic agents.
© 2009 Elsevier Ireland Ltd. All rights reserved.
Osteoarthritis (OA) is the most common form of joint disease
and is widespread in the elderly population [12]. OA primarily
affects the weight bearing joints (e.g. knees, hips) and is associated with degeneration of the articular cartilage and subchondral
bone. Patients with OA have joint pain that typically worsens with
weight bearing and activity. Currently no disease-modifying drugs
are available so the objective of pharmacological treatment has
been aimed at reducing functional impairment and the associated
pain. Studies on new therapeutic drugs for human OA and associated pain have been hampered because of the lack of useful animal
models that closely mimic the human disease. The monosodium
iodoacetate (MIA) model of OA has been well described in the rat
especially in terms of pathological progression of the disease [8],
pain behaviour [5,7,18,32] and peripheral nerve sensitization [30].
Injection of MIA into joints inhibits glyceraldehye-3-phosphate
dehydrogenase activity in chondrocytes, resulting in disruption of
glycolysis and eventual cell death [5,15,31]. The progressive loss of
chondrocytes results in histological and morphological changes to
the articular cartilage, closely resembling those seen in human OA
∗ Corresponding author. Tel.: +1 403 220 4507; fax: +1 403 283 3840.
E-mail address: mcdougaj@ucalgary.ca (J.J. McDougall).
0304-3940/$ – see front matter © 2009 Elsevier Ireland Ltd. All rights reserved.
doi:10.1016/j.neulet.2009.08.063
[13]. One of the main mechanisms responsible for the generation
of joint pain is the activation of nociceptors located on the terminal
branches of joint type III (A␦ fibre) and type IV (C fibre) primary
afferents [14,25,26]. These afferent nerve fibres show increased
activity when a noxious stimulus is applied to the innervated tissue [14,25,26,33]. In animal models of inflammatory joint disease
and OA, it has been shown that these joint primary afferent nerves
become sensitized, causing enhanced mechanosensation in the
affected joint leading to allodynia, hyperalgesia and spontaneous
pain [17,27,28,29]. Classical treatment for OA pain includes nonsteroidal anti-inflammatory drugs (NSAIDS), opioids and steroids.
The limitations of current therapy are such that patients still cite
pain as their worst symptom and current analgesic options have
significant side effects. It is therefore important to try to elucidate
the mechanisms responsible for the induction and maintenance
of these pain states to help in the development of more effective
analgesics for the treatment of OA. The emphasis of this study concerns the relationship between MIA concentration and the degree
of sensitization of afferent nerve fibres. A number of studies have
shown that structural damage and pain increase with higher MIA
concentration; however, the effect of MIA induced OA on peripheral sensory nerve activity is unknown. In this study we have shown
for the first time that there is a direct relationship between MIA
N. Schuelert, J.J. McDougall / Neuroscience Letters 465 (2009) 184–188
induced severity of OA and the mechanosensitivity of afferent nerve
fibres. We were also able to show that local administration of the
NSAID diclofenac can reduce nerve sensitization in the most severe
form of MIA-induced OA.
Experiments were performed on 44 male Wistar rats
(250–450 g) which were housed in cages at room temperature
(22 ◦ C) under a 12:12 h light/dark cycle with free access to water
and food. The animal handling and surgical procedures outlined
in this study all adhered to the Canadian Council for Animal Care
guidelines for the care and use of experimental animals. Fortyfour rats were deeply anaesthetised with 2% isoflurane in 100% O2
(1 l/min) until the flexor withdrawal reflex was abolished. In 21 rats,
OA was induced by an injection of 3 doses of sodium monoiodoacetate (Tocris Bioscience, Missouri USA; 0.1 mg, 0.3 mg and 3 mg;
50 l volume) in 0.9% saline into the joint cavity through the patellar ligament. Animals were allowed to recover for 14 days which
has consistently been shown to cause severe end-stage OA in this
species [2,7,15]. Twenty-three rats received an intra-articular injection of 0.9% saline and served as a control group.
Following OA development, animals were deeply anaesthetized
with urethane (Sigma–Aldrich, Ontario, Canada; 25% stock solution; 2 g/kg, i.p.) and an acceptable depth of anaesthesia was
determined by the absence of the hindpaw withdrawal reflex.
Core body temperature was measured by a rectally inserted thermometer and maintained at 37 ◦ C. The trachea was cannulated and
connected to a Harvard rodent respiratory pump to allow artificial
ventilation with 100% O2 (stroke volume: 2.5 ml breath frequency:
60 breaths/min). The left carotid artery was then exposed and
cannulated with a fine bore catheter (Portex Fine Bore Tubing,
0.5 mm ID, 1.00 mm OD; SIMS Portex Ltd., Kent, England) containing heparinised saline (100 units/ml). The cannula was connected
to a pressure transducer to allow continuous blood pressure measurement as recorded by a blood pressure monitor (BP-1, World
Precision Instruments, Sarasota, FL, USA). A catheter with heparinised saline was placed in the left jugular vein (Portex Fine Bore
Tubing, 0.40 mm ID, 0.80 mm OD; SIMS Portex Ltd., Kent, England)
and a single administration of the muscle relaxant gallamine triethiodide (Sigma–Aldrich, Ontario, Canada; 50 mg/kg) was injected
to eliminate neural interference arising from the hindlimb musculature. The right saphenous artery was cannulated below the knee
joint to permit local close intra-arterial injection of an NSAID to
the knee joint. A specialised clamp was fixed to the mid-shaft of
the isolated right femur and attached to a stereotaxic frame to
prevent movement of the proximal aspect of the rat hindlimb. To
apply rotation torque to the knee joint, the right hindpaw was
placed in a shoe-like holder and the hindlimb rotated to standardized torque levels as measured by a force transducer and a
torque meter (MVD2510; Hottinger-Baldwin Messtechnik, Darmstadt, Germany). Finally, a longitudinal skin incision was made
along the medial aspect of the hindlimb and the skin flaps were
fixed to a metal “O” ring to create a pouch which was filled with
warm paraffin oil to prevent tissue desiccation throughout the
experiment.
The technique used for recording afferent activity from articular nerve fibre from rat knee joints has been described previously
[17]. To prevent input from the foot and ankle region, the saphenous nerve was transected distally to the knee joint. The saphenous
nerve was then isolated in the inguinal region and cut centrally to
prevent the generation of spinally mediated reflexes. The saphenous nerve stump projecting from the knee was placed on a
small, black Perspex stage. Under a dissecting microscope, the perineurium was removed and fine neurofilaments were dissected free
from the nerve using fine watchmaker forceps. The neural strands
were then placed over a platinum electrode to record single afferent
fibre activity. To ensure that recorded fibres originate from the knee
joint, the receptive field of the fibres were identified by the elicita-
185
tion of a response to gentle probing of the knee joint with a glass rod
with a 1 mm tip. The mechanical threshold of each recorded joint
afferent was determined by a gradual increase of the torque applied
to the joint until the fibre started to elicit action potentials. The
mechanosensitivity of articular afferents was measured in response
to rotational torque which was gradually increased in 10 mNm
steps starting from 10 to 40 mNm. Each movement lasted 10 s and
the same level of rotation was repeated 3 times every 20 s. In all MIA
treated groups, recordings were made before (control) and after
close intra-arterial injection of the NSAID diclofenac sodium salt
(Tocris Bioscience; Missouri USA). The dose of diclofenac administered was 0.1 mg in 0.1 ml which has previously been shown
to be effective in attenuating inflammatory and postsurgical pain
[1,6]. Percent changes in nerve firing rate at different torque levels were calculated after NSAID application and compared to the
saline injected control group. Neuronal activity was recorded by
a data acquisition system (CED1401, Cambridge Electronic Design,
Cambridge, UK) and stored on a microcomputer for off-line analysis. The number of action potentials/movement was determined
using Spike 2 software (Cambridge Electronic Design, Cambridge,
UK).
All data were normally distributed and expressed as
means ± SEM for “n” observations. The effect of different doses of
MIA on joint mechanosensitivity was analyzed by two-way ANOVA
while the effect of diclofenac was tested by a paired Student t-test.
Torque-dependency was tested by one-way ANOVA. All differences
were considered statistically significant at a P value less than 0.05.
Between 1 and 3 afferent fibres were examined per animal such
that a total of 59 units were recorded in this study. The conduction
velocities of recorded afferents ranged from 0.47 to 9.29 m/s in the
control group (mean 1.9 ± 0.75; n = 26). In the 0.1 mg MIA group the
conduction velocities ranged from 0.54 to 4.1 m/s (mean 1.8 ± 0.34;
n = 9), in the 0.3 mg MIA group it ranged from 1.0 to 7.3 m/s (mean
3.0 ± 1.1; n = 11) and in the 3 mg MIA group the conduction velocities ranged from 0.98 to 2.84 m/s (mean 2.7 ± 0.94; n = 13). All
recorded fibres were found to be slowly adapting. All four animal groups showed an increase in firing rate with increasing levels
of torque (10 mNm; 20 mNm; 30 mNm; 40 mNm). This torquedependent effect was highly significant in all groups (P < 0.0001;
two-way ANOVA). The effect of different concentrations of MIA
on afferent firing rate at the four applied torque levels was also
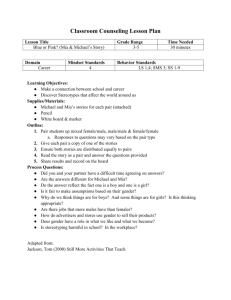
found to be highly significant among groups (P < 0.001). Specimen recordings showing the concentration-dependent increase
in nerve fibre firing rate with MIA is shown in Fig. 1 (40 mNm
torque is shown in each trace). In rats treated with 0.1 mg MIA
the mean afferent firing rate across all four torque levels was
28 ± 12.6 action potentials/movement cycle. This firing frequency
was found to be not significantly different from the saline control
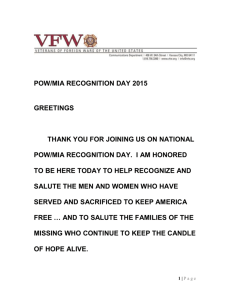
group (32 ± 13.2 action potentials/movement cycle). Treatment
with 0.3 mg MIA (59 ± 21.4 action potentials/movement cycle) and
3 mg MIA (81 ± 22.0 action potentials/movement cycle) induced a
highly significant increase in joint afferent firing rate compared
to control (P < 0.0001; Fig. 2). A significant increase in firing rate
was also observed comparing the 0.3 mg MIA to the 3 mg MIA
group (P < 0.05). The mechanical threshold required to initiate afferent firing in control joints was 15.2 ± 1.5 mNm. In the 0.1 mg MIA
group the mechanical threshold was 17.0 ± 2.3 mNm, in the 0.3 mg
MIA group it was 14.5 ± 2.4 mNm and in the 3 mg MIA group the
mechanical threshold was 12.4 ± 1.5 mNm. Local application of
the classic NSAID diclofenac (100 g) significantly reduced MIAinduced sensitization of nerve fibres in the 3 mg MIA group with
noxious joint rotation (P < 0.001) but had no significant effect in
rats treated with lower MIA concentrations (Fig. 3). Diclofenac had
no effect on mechanosensitivity in control joints (data not shown).
All units tested could be activated by local intra-arterial injection
of KCl (0.4 mM, 0.1 ml) at the end of the experiment confirming
186
N. Schuelert, J.J. McDougall / Neuroscience Letters 465 (2009) 184–188
Fig. 1. Location of the receptive fields of the afferents recorded in this study (top). Exemplar single unit recordings from control and osteoarthritic joint afferents (middle) in
response to noxious (40 mNm) joint rotation (bottom). Graded osteoarthritis was produced by injecting different doses of MIA leading to a dose-dependent sensitization of
afferent fibres. The units shown had a conduction velocity between 1.0 and 1.7 m/s with a mechanical threshold of 22 mNm (control joint fibre), 28 mNm (0.1 mg MIA fibre),
12 mNm (0.3 mg MIA fibre), and 10 mNm (3 mg MIA fibre).
that administered reagents reached mechanosensory nerve endings throughout the experiment.
Intra-articular injection of MIA into rat knee joints induces histological changes and pain related behaviours characteristic of
human OA [2,15,18]. It is possible to vary the degree of joint
pathology by injecting different concentrations of MIA and this
has been shown to correlate with pain intensity [2,5]. Most studies
have focused on MIA-induced histological changes of the joint and
related pain behaviour but not much is known about the concomitant changes in primary afferent discharge properties during the
transmission of nociceptive information from the damaged joint
to the central nervous system. Recent studies showed that MIAinduced OA leads to an increased firing rate and reduced activation
threshold of afferent nerve fibres [29], which consequently leads to
sensitization of spinal neurons in the dorsal horn [10]. The present
study revealed for the first time that there is a direct relationship
between the concentration of intra-articularly injected MIA and
afferent nerve fibre activity. Furthermore, incremental rotational
forces applied to the knee resulted in a rise in afferent discharge
rate in all animal groups. This torque-dependent increase in firing
Fig. 2. Effect of 3 doses (0.1 mg, 0.3 mg, 3 mg) of monosodium iodoacetate (MIA)
injected intra-articular on afferent nerve firing rate in response to different torque
levels (10 mNm, 20 mNm, 30 mNm, 40 mNm) compared to saline injected control
joint. Significance levels refer to the mean firing rate of all torque intensities in
each MIA group to the mean firing rate of all torque intensities in the control group
(* P < 0.05, two-way ANOVA, n = 9–26 fibres; n.s.: not significant). Values are the
mean ± SEM.
frequency corroborates an earlier report which described the same
phenomenon in normal rat knees [14].
Although some clinical studies have shown a correlation
between reported pain and the extent of OA disease [21], many
patients with relatively undamaged joints describe intense pain
while others with severe OA report little or no pain [9]. Thus,
the link between structural tissue damage and joint pain remains
unclear highlighting the necessity for robust and relevant animal
models to explore further this phenomenon. In the Dunkin Hartley
guinea pig model of spontaneous OA, for example, it was found that
the degree of knee joint pathology correlates well with increasing
age; however, there was no statistical correlation between joint
nociception and morphologically determined joint degeneration
[16]. Aged Dunkin Hartley guinea pigs, therefore, are a clinically
relevant model of OA pain although disease severity cannot be easily controlled for between animals. The MIA model of OA on the
other hand offers the ability to control not only disease severity,
but as described here, it is also possible to gradate the magnitude
of nociception incurred. This model therefore, provides a unique
opportunity to evaluate potential analgesics in animals with varying degrees of joint degeneration. One reason why the MIA model
correlates well with disease severity while the guinea pig model of
Fig. 3. Effect of the classic non-steroidal anti-inflammatory drug diclofenac (0.1 mg)
on afferent nerve firing rate during noxious movement (40 mNm) of the joint.
Diclofenac reduced nociception only at the highest dose of MIA by up to 62%
(** P < 0.01, paired Student t-test; n = 7–10 fibres; n.s.: not significant). Values are
the mean ± SEM.
N. Schuelert, J.J. McDougall / Neuroscience Letters 465 (2009) 184–188
OA does not may be related to differences in overall joint pathology.
Aged Dunkin Hartley guinea pig knees possess areas of meniscal ossification, cartilage apposition, contain osteophytes and have
other bony remodelling features not seen in the MIA model. Furthermore, joint degeneration in the MIA model occurs over 14 days
whereas spontaneous OA in the guinea pig develops over months
which likely differentially impacts the sensory properties of joint
nociceptive nerves.
Little is known regarding the exact mechanisms responsible
for MIA-induced joint pain but it may be related to early inflammatory reactions in the joint. Initial inflammation can induce a
sensitization of peripheral receptors which consequently changes
the response characteristics of primary afferent fibres [23] leading
to more chronic pain states. Activation of normally non-nociceptive
fibres by noxious stimuli may then be perceived as painful (for
review see [4,33]). The acute inflammatory response in the MIA
model lasts approximately 3 days during which time trophic factors
are likely released into the joint that upregulate pro-nociceptive
receptor expression leading to a reduction in mechanosensory
threshold [19]. A-fibres may start synthesising receptors that are
normally only found on nociceptive C-fibres, thus signalling a phenotypic shift with some A-fibres adopting C-fibre characteristics
[20]. Inflammation subsequently resolves in the MIA model giving
way to the more prolonged degenerative phase of the disease.
Although human OA is classically defined as a non-inflammatory
disease with limited pain relief by NSAIDs, there are clearly molecular and pathophysiological indices of inflammation in OA that
warrant closer inspection [11,22]. Previous investigations into the
ability of NSAIDs to alleviate joint pain are controversial. Systemic
treatment with diclofenac was found to reduce secondary hyperalgesia during the acute phase of MIA induced OA (day 3 following
MIA injection), but failed to have any analgesic effect at later time
points [5]. In contrast, other studies observed that systemic application of NSAIDs at days 7 and 14 after MIA injection significantly
reduced joint pain [2,3,24]. The present study found that peripheral administration of diclofenac reduced afferent nerve firing rate
in animals treated with the highest dose of MIA only. This finding
suggests that high dose MIA produces an OA joint with ongoing
inflammation that is amenable to local treatment with NSAIDs,
whereas the inflammation produced by low dose MIA is transient
and therefore insensitive to NSAIDs during the latter stages of OA
development. Further studies are necessary, however, to test this
assumption that the inflammatory component of MIA-induced OA
is concentration-dependent.
In summary, this study shows that increasing rotation of rat
knees leads to enhanced firing of joint mechanoreceptors. The magnitude of these discharges is augmented in animals treated with
MIA and this effect was found to be concentration-dependent. Thus,
the MIA model of OA offers an attractive means of evaluating novel
pain therapeutics in animals with various levels of disease severity.
[3]
[4]
[5]
[6]
[7]
[8]
[9]
[10]
[11]
[12]
[13]
[14]
[15]
[16]
[17]
[18]
[19]
[20]
[21]
[22]
Acknowledgements
We thank Dr. Fiona Russell and Dr. Shu Zhan for their technical
assistance and contribution to this paper. This work was supported
by a grant from the Canadian Institutes for Health Research. J.J.Mc.D.
receives salary support from the Alberta Heritage Foundation for
Medical Research (AHFMR) and The Arthritis Society of Canada. N.S.
is AHFMR and Canadian Arthritis Network Postdoctoral Fellow.
[23]
[24]
[25]
[26]
References
[27]
[1] D.P. Alves, M.A. Tatsuo, R. Leite, I.D. Duarte, Diclofenac-induced peripheral
antinociception is associated with ATP-sensitive K+ channels activation, Life
Sci. 74 (2004) 2577–2591.
[2] S.E. Bove, S.L. Calcaterra, R.M. Brooker, C.M. Huber, R.E. Guzman, P.L.
Juneau, D.J. Schrier, K.S. Kilgore, Weight bearing as a measure of disease
[28]
187
progression and efficacy of anti-inflammatory compounds in a model of
monosodium iodoacetate-induced osteoarthritis, Osteoarthritis Cartilage 11
(2003) 821–830.
P. Clark, S.E. Rowland, D. Denis, M.C. Mathieu, R. Stocco, H. Poirier, J. Burch,
Y. Han, L. Audoly, A.G. Therien, D. Xu, MF498 [N-{[4-(5,9-Diethoxy-6-oxo6,8-dihydro-7H-pyrrolo[3,4-g]quinolin-7-yl)-3-m
ethylbenzyl]sulfonyl}-2(2-methoxyphenyl)acetamide], a selective E prostanoid receptor 4 antagonist,
relieves joint inflammation and pain in rodent models of rheumatoid and
osteoarthritis, J. Pharmacol. Exp. Ther. 325 (2008) 425–434.
T.J. Coderre, J. Katz, A.L. Vaccarino, R. Melzack, Contribution of central neuroplasticity to pathological pain: review of clinical and experimental evidence,
Pain 52 (1993) 259–285.
J. Fernihough, C. Gentry, M. Malcangio, A. Fox, J. Rediske, T. Pellas, B. Kidd, S.
Bevan, J. Winter, Pain related behaviour in two models of osteoarthritis in the
rat knee, Pain 112 (2004) 83–93.
R. Furedi, K. Bolcskei, J. Szolcsanyi, G. Petho, Effects of analgesics on the plantar incision-induced drop of the noxious heat threshold measured with an
increasing-temperature water bath in the rat, Eur. J. Pharmacol. 605 (2009)
63–67.
C. Guingamp, P. Gegout-Pottie, L. Philippe, B. Terlain, P. Netter, P. Gillet, Monoiodoacetate-induced experimental osteoarthritis: a dose–response study of
loss of mobility, morphology, and biochemistry, Arthritis Rheum. 40 (1997)
1670–1679.
R.E. Guzman, M.G. Evans, S. Bove, B. Morenko, K. Kilgore, Mono-iodoacetateinduced histologic changes in subchondral bone and articular cartilage of rat
femorotibial joints: an animal model of osteoarthritis, Toxicol. Pathol. 31 (2003)
619–624.
M.T. Hannan, D.T. Felson, T. Pincus, Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee, J. Rheumatol. 27
(2000) 1513–1517.
V.L. Harvey, A.H. Dickenson, Behavioural and electrophysiological characterisation of experimentally induced osteoarthritis and neuropathy in C57Bl/6 mice,
Mol. Pain 5 (2009) 18.
E. Hedbom, H.J. Hauselmann, Molecular aspects of pathogenesis in osteoarthritis: the role of inflammation, Cell Mol. Life Sci. 59 (2002) 45–53.
R. Hinton, R.L. Moody, A.W. Davis, S.F. Thomas, Osteoarthritis: diagnosis and
therapeutic considerations, Am. Fam. Physician 65 (2002) 841–848.
M.J. Janusz, E.B. Hookfin, S.A. Heitmeyer, J.F. Woessner, A.J. Freemont, J.A. Hoyland, K.K. Brown, L.C. Hsieh, N.G. Almstead, B. De, M.G. Natchus, S. Pikul,
Y.O. Taiwo, Moderation of iodoacetate-induced experimental osteoarthritis in
rats by matrix metalloproteinase inhibitors, Osteoarthritis Cartilage 9 (2001)
751–760.
S. Just, M. Pawlak, B. Heppelmann, Responses of fine primary afferent nerve
fibres innervating the rat knee joint to defined torque, J. Neurosci. Methods
103 (2000) 157–162.
D.A. Kalbhen, Chemical model of osteoarthritis—a pharmacological evaluation,
J. Rheumatol. 14 (Spec No.) (1987) 130–131.
J.J. McDougall, B. Andruski, N. Schuelert, B. Hallgrimsson, J.R. Matyas, Unravelling the relationship between age, nociception and joint destruction in
naturally occurring osteoarthritis of Dunkin Hartley guinea pigs, Pain 141
(2009) 222–232.
J.J. McDougall, M. Pawlak, U. Hanesch, R.F. Schmidt, Peripheral modulation of rat
knee joint afferent mechanosensitivity by nociceptin/orphanin FQ, Neurosci.
Lett. 288 (2000) 123–126.
J.J. McDougall, L. Watkins, Z. Li, Vasoactive intestinal peptide (VIP) is a
modulator of joint pain in a rat model of osteoarthritis, Pain 123 (2006)
98–105.
G.J. Michael, J.V. Priestley, Differential expression of the mRNA for the vanilloid
receptor subtype 1 in cells of the adult rat dorsal root and nodose ganglia and
its downregulation by axotomy, J. Neurosci. 19 (1999) 1844–1854.
S. Neumann, T.P. Doubell, T. Leslie, C.J. Woolf, Inflammatory pain hypersensitivity mediated by phenotypic switch in myelinated primary sensory neurons,
Nature 384 (1996) 360–364.
S.C. O’Reilly, A. Jones, K.R. Muir, M. Doherty, Quadriceps weakness in knee
osteoarthritis: the effect on pain and disability, Ann. Rheum. Dis. 57 (1998)
588–594.
J.P. Pelletier, J. Martel-Pelletier, S.B. Abramson, Osteoarthritis, an inflammatory disease: potential implication for the selection of new therapeutic targets,
Arthritis Rheum. 44 (2001) 1237–1247.
S. Petersen-Felix, M. Curatolo, Neuroplasticity—an important factor in acute
and chronic pain, Swiss Med. Wkly. 132 (2002) 273–278.
A.M. Pulichino, S. Rowland, T. Wu, P. Clark, D. Xu, M.C. Mathieu, D. Riendeau,
L.P. Audoly, Prostacyclin antagonism reduces pain and inflammation in rodent
models of hyperalgesia and chronic arthritis, J. Pharmacol. Exp. Ther. 319 (2006)
1043–1050.
H.G. Schaible, B.D. Grubb, Afferent and spinal mechanisms of joint pain, Pain
55 (1993) 5–54.
H.G. Schaible, R.F. Schmidt, Activation of groups III and IV sensory units in
medial articular nerve by local mechanical stimulation of knee joint, J. Neurophysiol. 49 (1983) 35–44.
H.G. Schaible, R.F. Schmidt, Effects of an experimental arthritis on the sensory properties of fine articular afferent units, J. Neurophysiol. 54 (1985)
1109–1122.
H.G. Schaible, R.F. Schmidt, Time course of mechanosensitivity changes in articular afferents during a developing experimental arthritis, J. Neurophysiol. 60
(1988) 2180–2195.
188
N. Schuelert, J.J. McDougall / Neuroscience Letters 465 (2009) 184–188
[29] N. Schuelert, J.J. McDougall, Electrophysiological evidence that the vasoactive
intestinal peptide receptor antagonist VIP6-28 reduces nociception in an animal model of osteoarthritis, Osteoarthritis Cartilage 14 (2006) 1155–1162.
[30] N. Schuelert, J.J. McDougall, Cannabinoid-mediated antinociception is
enhanced in rat osteoarthritic knees, Arthritis Rheum. 58 (2008) 145–153.
[31] P.M. van der Kraan, E.L. Vitters, L.B. van de Putte, W.B. van den
Berg, Development of osteoarthritic lesions in mice by “metabolic” and
“mechanical” alterations in the knee joints, Am. J. Pathol. 135 (1989)
1001–1014.
[32] J.L. Vonsy, J. Ghandehari, A.H. Dickenson, Differential analgesic effects of morphine and gabapentin on behavioural measures of pain and disability in a model
of osteoarthritis pain in rats, Eur. J. Pain (2008).
[33] C.J. Woolf, M.W. Salter, Neuronal plasticity: increasing the gain in pain, Science
288 (2000) 1765–1769.