Arterial Blood Pressure Response to Transient Arousals
advertisement

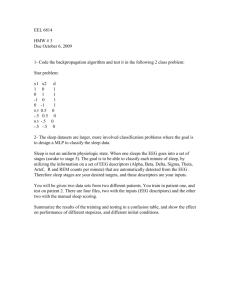
Arterial Blood Pressure Response to Transient Arousals From NREM Sleep in Nonapneic Snorers With Sleep Fragmentation* Frederic Lofaso, MD; Francoise Goldenberg, MD; Marie Pia d'Ortho, MD; Andre Coste, MD; and Alain Harf, MD Study objectives: To assess the hemodynamic effects of graded arousals during nonrapid eye (NREM) sleep in patients with partial upper airway obstruction during sleep without obstructive sleep apnea/hypopnea, overnight beat-to-beat BP was recorded in six patients. Setting: At the end of each nonapneic obstructive event, EEG responses were graded as follows: grade 2, grade 1, and grade 0 were defined as increased high-frequency EEG lasting > 15 s, 3 to 15 s, and no EEG arousals according to the American Sleep Disorders Association, respectively. Measurements and results: The following were observed during grade 0, 1, and 2 EEG patterns (mean±SD): systolic pressure increased by 7.1±1.5, 11.7±1.9, and 14.2±3.4 (p<0.005), respec¬ tively; diastolic pressure increased by 4.6±0.6, 6.7±1.7, and 9.4±3.0 (p<0.005), respectively; heart rate increased by 2.9±0.4, 3.9±2.2, and 8.6±4.6 (p<0.005), respectively. Conclusions: We conclude that nonapneic-nonhypopneic obstructive events are followed by arterial systemic pressure increases whose magnitude varies with the grade of the arousal. movement (CHEST 1998; 113:985-91) Key words: arousal; blood pressure; snoring; upper airway resistance Abbreviations: ASDA=American Sleep Disorders Association; NREM=no rapid eye movement; OSAS=obstructive sleep apnea syndrome; REM rapid eye movement = long been recognized that the obstructive sleep apnea syndrome (OSAS) is associated with acute increases in arterial BP at the termination of respiratory events.1 This phenomenon has been as¬ cribed to hypoxemia,2'3 to the hemodynamic effects of intrathoracic pressure changes,46 to interruptions in respiration,7-9 and to disruption of sleep.10-14 For others, the magnitude of the increase in arterial BP does not vary with the grade of the arousal.15 Recent reports have demonstrated that an abnor¬ mal amount of breathing effort due to partial upper airway obstruction, even in the absence of sleep apnea or oxygen desaturation, can disrupt sleep architecture by causing arousals.1617 The purpose of this study was to examine whether the termination of nonapneic-nonhypopneic obstructive events coin¬ cides with an abrupt increase in arterial BP similar to T t has -*- *From the Service de Physiologie-Explorations Fonctionnelles, Institut National de la Sante et de la Recherche Hopital Henri Mondor, Creteil, France. Medieale, Manuscript received January 28, 1997; revision accepted October requests: F. Lofaso, MD, Service de Physiologie-ExploReprint rations Henri 94010 7, 1997. France Fonctionnelles, Hopital Mondor, Creteil, that seen in OSAS, despite the absence of oxygen desaturation and interruption of ventilation. In addi¬ tion, the relationship between the magnitude of the arterial BP increase and the change in the EEG pattern was examined. We recorded acute increases in systemic arterial BP at the time of the abrupt reduction in upper airway obstruction, and found that this BP rise was primarily due to sleep disrup¬ tion. Materials and Methods Patients Six men were studied. Mean age was 45 ± 11 years (range, 33 to 65 years). Mean body mass index was 27±3 kg/m2. All six subjects had heavy snoring confirmed by a roommate or bed partner and daytime sleepiness with an Epworth sleepiness scale18 >10. Patients were included in the study after a home polysomnog¬ raphy study, including EEG (C4-Al9 C3-A2), electro-oculography, chin electromyography, electromyography of the tibialis anterior muscle of both legs, oronasal airflow recordings, rib cage move¬ ment recordings (Multi-Parameter Analysis recorder 2/Medilog 9200; Oxford Medical Instruments; Abingdon, England), and arterial pulse oximetry (Nellcor BS; Nellcor Inc; Hayward Calif). CHEST/ 113/4 /APRIL, 1998 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 985 To be eligible for the study, subjects had to have an at-home polysomnography study that met the following criteria: apneaindex <5/h of sleep (apnea was defined as cessation of hypopnea airflow lasting ^10 s and hypopnea 2:50% fall in oronasal airflow for 10 s or a fall in oronasal airflow with an oxygen desaturation ^3% of the preceding baseline level); and arousal index >10/h of sleep (arousals were detected on the basis of an abrupt shift in EEG frequency, including alpha and/or frequen¬ cies >16 Hz but not spindles, and were scored according to standard criteria19). To relate clinical complaints and sleep fragmentation to an upper airway obstruction without obstructive sleep apnea/hypopnea, a sleep polygraphic investigation, includ¬ ing respiratory effort evaluation, was performed as recommend¬ ed.20 The study was approved by the Research Ethics Committee of our institution, and each subject gave consent in accordance committee's as a with the requirements. The clinical trial consisted of a repeat polysomnography study, including EEG (C4-Al5 C3-A2), electro-oculography, chin elec¬ tromyography, thoracic and abdominal movement recording, and arterial pulse oximetry (Nellcor BS, Nellcor Inc.). During the study night, oronasal airflow was quantified using a tight-fitting facial mask and a No. 2 pneumotachograph (Fleisch; Lausanne, Switzerland) connected to a differential pressure transducer MP45 ±5 cm H20; Northridge, Calif). frequencies >16 Hz, except spindles; grade 0b, low-frequency EEG changes (K-complexes and/or delta wave burst) without any increase in EEG frequency except spindles; grade 0c, no increase in cortical high frequency and no occurrence of K-complexes or Clinical Trial (Validyne and after the end of respiratory events were looked for. Arousal was performed by one of us (F.G.), who was aware of the time at which respiratory events were terminated, but was not aware of the changes in respiratory effort and in BP at the time ofthe respiratory event. EEG changes were graded as follows: grade 2, shift in EEG frequency lasting >15 s and including alpha activity and/or frequencies >16 Hz, according to the standard criteria of awakening;22 grade 1, shift in EEG frequency lasting from 3 to 15 s and including alpha activity and/or frequencies >16 Hz, except spindles, according to stan¬ dard criteria of arousal;19 grade 0, no EEG changes or minor EEG changes, usually not classified as arousals in the American Sleep Disorders Association (ASDA) criteria.19 Grade 0 EEG changes were further classified as follows: grade 0a, shift in EEG frequency lasting <3 s and including alpha activity and/or scoring analysis In addition, respiratory effort was monitored by measuring esophageal pres¬ sure (Gaeltec; Dunvegan, Isle of Skye, UK), and BP and heart rate were monitored by recording digital arterial beat-to-beat systolic/diastolic pressure at the third finger ofthe left hand using an infrared plethysmographic volume clamp method (Finapres; Ohmeda; Maurepas, France). As previously proposed,1112 the left hand was taped to the epigastric area to avoid artifactual BP modifications caused by changes in hydrostatic pressure associ¬ ated with hand movement. All signals were recorded using a 14-channel paper recorder (Electroencephalograph; Nihon Kohden; Japan) digitized at 128 Hz and sampled using an analogic/ Tokyo, numeric system (MP100; Biopac System; Goleta, Calif) for subsequent analysis. Data Analysis nonapneic-nonhypopneic obstructive event was defined as the occurrence, in the absence of hypopnea (airflow drop <50% of the preceding baseline during 10 s or airflow drop with desaturation <3% of the preceding baseline level), of a progres¬ sive in the of the flow A change shape inspiratory contour charac¬ terized by increasing limitation21 and of a concomitant increase in the esophageal pressure swing, with termination of the vent as abrupt normalization of both the inspiratory flow contour and the esophageal pressure swing. Esophageal pressure swings were calculated as the difference between the maximal expiratory value and the minimal inspiratory value. Esophageal pressure swing decrease was quantified as the decrease in esophageal pressure swing at the termination ofthe respiratory event, ie, the difference between esophageal swings immediately before and after the termination of the respiratory event. BP parameters and heart rate were analyzed over two 10-s periods before and after the termination of the respiratory event. BP parameters were taken into account only during the expiratory phase of the breathing cycle. They corresponded to at least three data points for each 10-s period. Sleep staging was performed according to standard criteria.22 Only respiratory events from nonrapid eye movement (NREM) sleep periods were used. EEG changes during the 10 s before delta wave bursts. Statistical Analysis For each patient and each type of EEG change, the changes in arterial pressure and in esophageal pressure at the end of the nonapneic-nonhypopneic respiratory events were averaged and Friedman's two-way analysis of variance was performed. Where appropriate (p value <0.05), pairwise comparisons were per¬ formed using a Wilcoxon matched paired test. The level of significance was set at 5%. Results Epworth sleepiness scale18 and main sleep and respiratory parameters during the polysomnography with arterial BP measurement are presented in Table 1. A mean (±SD) of 167 (±145) nonapneicevents were observed per nonhypopneic respiratory patient during NREM sleep. Distribution of EEG patterns during these nonapneic-nonhypopneic re¬ spiratory events is presented in Table 2. Systolic and diastolic BPs and heart rate rose after the end of the respiratory events, reaching a peak within 10 s after event termination (Fig 1). BP and heart rate changes in response to different grades of EEG modifications are shown in panels A (top) and B (center) of Figure 2, respectively. The were observed during grade 0, 1, and 2 following EEG patterns (mean±SD): systolic pressure in¬ creased by 7.1 + 1.5, 11.7+1.9, and 14.2+3.4 (p<0.005), respectively; diastolic pressure increased by 4.6+0.6, 6.7±1.7, and 9.4+3.0 (p<0.005), re¬ spectively; heart rate increased by 2.9±0.4, 3.9±2.2, and 8.6±4.6 (p<0.005), respectively. No differences were observed across the three grade 0 subclasses (0a, 0b, and 0c). Systolic and diastolic BP increases were significantly higher for grade 2 and grade 1 than for grade 0. The heart rate increase was significantly higher for grade 2 than for grade 0. Clinical Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 Investigations Table Respiratory Data During Polysomnography With Arterial BP 1.Epworth Sleepiness Score and Sleep andMeasurements* Epworth Sleepiness Patient A B C D E F min %TST %TST %TST 80 112 146 163 160 102 93 72 84 77 65 58 0 17 16 13 25 19 / 59 11 ¦0 10 10 17 22 54 12 14 23 Scale mm 19 21 11 12 11 12 426 398 279 362 360 182 *TST.total sleep time; WASO=wake after sleep onset; swing decreases in response Esophageal pressure different grades of arousals are shown in panel C (bottom) of Figure 2. No differences in esophageal pressure swing changes were observed across grades. The mean fall in arterial oxygen saturation was <0.3% for each grade of arousal, with no significant differences across grades. Discussion airway obstruction without exhibit increased sleep apnea/hypopnea NREM during sleep, often withof respiratory EEG pattern changes. We found that termination these nonapneic-nonhypopneic obstructive events was consistently followed by a rise in BP, and that the magnitude of this rise increased with the inten¬ sity of EEG arousal, although significant but smaller in of efforts rises were detectable EEG arousal. In this study, as the absence REM, apparent previously proposed,1113 BP was analyzed by infrared plethysmography. Because this noninvasive indirect method may overestimate BP,12 we measured only arterial BP changes. However, increased arteriolar vasoconstriction at the periphery could increase systolic BP measured at the finger by a phenomenon of reflectance ofthe pressure wave at the resistance vessels causing amplification and rise systolic BP. However, diastolic BP is virtually by this phenomenon.11 We found that magnitude of diastolic pressure increases also varied with the grade of arousal. This indicates that the BP rises that we observed cannot be due solely to this artifact of pulse wave amplification. Although we analyzed both rapid eye movement (REM) and NREM data, the amount of data was too small to allow comparisons of the different grades of arousal during REM sleep. Only two patients expe¬ rienced nonapneic-nonhypopneic obstructive events both with and without awakening/arousal during REM sleep. This is due in part to the fact that apneas/hypopneas were predominant in REM sleep, whereas nonapneic-nonhypopneic obstructive events were observed less frequently. The age range in our six patients was quite large, but only one patient was >50 years (patient E, 65 he was the patient who had the years). Interestingly, lowest arterial BP response to the different levels of arousal. During grade 2, 1, and 0 EEG patterns, by only 10, 9, and 4 mm systolic pressure increased This result corroborates the study Hg, respectively. of Hajduczok et al23 that demonstrated that sympa¬ thetic activity is impaired with senescence. The cardiovascular consequences of OSAS include a rise in systemic BP after each episode of apnea.1 These postapneic BP elevations contribute signifiin unaffected Table 2.EEG Patterns at the End of Nonapnoeic-Nonhypopnoeic Patients A B C D E F Mean SD Nonapneic-Nonhypopneic Grade 2, 421 137 250 59 73 59 167 145 16 12 8 12 26 2 13 8 Respiratoiy Events Hour of Sleep AHI=apnoea-hypopnoea index; UAR=upper airway resistance. to Patients with upper Nonapneic-Nonhypopneic Respiratory Events per Hour of Sleep Stages 3+4, WASO, obstructive AHI, Events per Stages 1+2, TST, Respiratory Events During NREM Sleep Grade 0, Grade 1, Total Grade 0 % % 66 48 81 27 53 72 57 23 18 40 11 61 21 26 30 18 Grade 0a Grade 0b Grade Oc 12 24 7 49 16 23 21 15 3 14 3 13 2 1 6 6 CHEST/113/4/APRIL, 1998 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 987 Arousal grade 1 ^*^r^W^^ *¦'.»i' j (L/sec) Peso (cmH20) .ji'ifw.4.k><. .0.5 0 -20 s:: siis^^ (mmHg) 100 grade Oh m^fc^^ (L/sec) +0;.5 .0U5 Peso ° Flow (cmHiO) .20 Pressure (mmHg) 100 If^tyj^^ Flow +0.5 (L/sec) Peso _05 ° (cmH20) .20 ,. Arterial J40 Pressure (mmHg) 100 polysomnographic recordings obtained in a patient, showing BP changes in arousals due to nonapneic-nonhypopneic respiratory events. The grades of EEGchin EEG, electro-oculogram (EOG), electromyogram (EMG), air flow (Flow) pneumotachograph recording, esophageal pressure (Peso) recording, and arterial BP recordings are shown. Figure 1. Continuous response to various cantly to the nocturnal hypertension and perhaps also to the diurnal hypertension seen in patients with obstructive sleep apnea. A recent study demon¬ strated that acute increases in systemic arterial BP also occur after each respiratory event in the patients with upper airway obstruction without obstructive sleep apnea/hypopnea.24 We found that the magni¬ tude of these BP increases is related to the intensity of EEG arousal. Both arterial hypoxemia23 and arousal from sleep10-14 have been suggested as the main causes of 988 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 the nocturnal hemodynamic oscillations seen in pa¬ tients with OSAS, although Rees et al15 found no between the rise in BP and the occur¬ relationship rence of EEG change. To evaluate the respective contributions of hypoxia and arousal, investigators have used a variety of approaches to isolate these two factors from each other. To maintain arterial oxygen saturation >90% at the end of apneas, Ringler et al10 and Ali et al12 provided supplementary oxygen to OSAS patients undergoing polysomnography. They found that oxygen supplementation did not alter the Clinical Investigations 20 H" X ISA 10 is © o 0 12 s n-1-r nr J 5 10 also induced arousals by auditory stimulation in normal subjects. In their study, the magnitude ofthe BP increase was proportional to the degree of arousal, as defined by the duration of the increase in high-frequency EEG activity. In our study, in pa¬ tients with upper airway obstruction without ob¬ structive sleep apnea/hypopnea, we also found that the magnitude of the BP rise was closely related to the degree of arousal. These data corroborate the findings from the studies on OSAS, providing addi¬ tional evidence that arousals related to obstructive respiratory events may be accompanied by signifi¬ cant BP rises even in the absence of oxygen desatu¬ ration. Other factors than arousal have been hypoxia for suggested possibly being responsible the BP elevation in OSAS. These factors include reinflation of the lung, which may change cardiovascular per¬ formance via a number of mechanisms,7-9 and ter¬ mination of deep negative pleural pressure dips generated by frustrated inspiratory efforts during obstructive apnea.25 These factors may also be in¬ volved in patients with upper airway obstruction without obstructive sleep apnea/hypopnea, either in combination with arousals or since or as SA 5 10 m s 7.5 «8 « 2.5 W i-1-r 2 Figure 2. Systolic 0a 10 Ob Grade of Arousal From Sleep pressure (squares) 0c and diastolic pressure The left-sided panels show the values observed during 2, 1, and 0 arousals. In the right-sided panels, grade 0 grade arousals are divided into three subgroups (see "Materials and Methods" for definition). No differences were observed across diastolic BP increases were grade 0 subtypes. for Systolic and 2 and grade 1 than for grade 0. significantly higher grade Heart rate increases were significantly higher for grade 2 than for 0. No differences in esophageal pressure swing changes grade were observed across grades. Values are means± SEM. events. BP increase after apnea termination. In et al10 induced during nonapneic-nonhypopneic respiratory events only 100 mL. It can be postulated that such a small increase in end-inspiratory thoracic volume at the end of a respiratory event will result in insignif¬ icant inflation-associated cardiovascular responses. A second factor may be intrathoracic pressure changes, which are known to influence BP. BP decreases from expiration to inspiration, and when pleural pressure becomes more negative during inspiration, such as in with was (diamonds) changes (top, A), heart rate changes (center, B), and esophageal pressure swing decrease (bottom, C) in response to various grades of arousal at the end of nonapneic respiratory Ringler we ob¬ alone, served some increase in BP in the absence of arousals (EEG pattern scored as grades 0). In a discussion of the lung volume changes in patients with upper airway obstruction without obstructive sleep apnea/hypopnea, Stoohs and Guilleminault26 pointed out that the mean decrease in tidal volume addition, nonrespiratory (auditory) arousals in OSAS patients treated by nasal positive airway pressure and observed that the BP increase after auditory arousal was similar to the BP increase after obstructive apnea. Similarly, Ali et al11 demon¬ strated that arousals induced by periodic leg move¬ ments induce an increase of BP in the same order as the rises seen after obstructive apneas. Davies et al13 asthma, inspiratory arterial pressure patients decreases further.5 Because part of the increase in BP occurring at the end of respiratory events may be ascribable to a reduction in the inspiratory decline of arterial BP, we decided to avoid this possible me¬ chanical effect by measuring arterial BP during expiration. However, because mean intrathoracic pressure is more negative during an obstructive respiratory event, left ventricular ejection may de¬ following increases in left ventricular afterload4 and in venous return,6 which increase enddiastolic volume of this cardiac chamber: this increase of end-diastolic volume of right ventricle can also decrease the left ventricular diastolic com¬ therefore the left ventricular preload pliance and the mechanisms of the ventricular interdethrough crease CHEST/ 113/4 /APRIL, 1998 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 pendence.27 Thus, a return to normal intrathoracic pressure after the end of the obstructive respiratory event may increase BP by raising left ventricular ejection. Such a phenomenon may explain the in¬ crease in BP that occurred in our study after the end of nonapneic-nonhypopneic respiratory events, even in the absence of visible EEG changes. However, the putative role of a decrease in intrathoracic pressure in decreasing left ventricular ejection under condi¬ tions appropriate to sleep apnea syndrome has not yet been confirmed by experimental studies.27 In addition, in our study, although esophageal pressure did become more negative during these respiratory events, the mean esophageal pressure swing increase was <10 cm H20, a value much lower than in the sleep apnea syndrome. Since none of these previous hypotheses is satis¬ an increase in BP (during factory,Ocwe suggest thatoccur as a result of brainstem grade arousals) may activation caused by the respiratory event and suffi¬ response produceThisan autonomic has ciently marked toarousal. been but not cortical hypothesis who Davies et observed al,13 suggested previously by that auditory stimuli could also induce BP increases (with magnitudes similar to those in our study during 0 arousals) without causing EEG arousal. grade A recent study investigated a subpopulation of patients with upper airway obstruction without ob¬ structive sleep apnea/hypopnea and without detect¬ able EEG arousals.20 In our study, one third of respiratory events were nonapneic-nonhypopneic not associated with arousals according to AS DA criteria (grades 0), but were associated with abrupt these events with¬ BP increases. out respiratory Among arousal, many (80%) were associated with EEG changes, which were usually of low frequency (grade Ob: K-complexes and/or delta wave bursts). Since it has been demonstrated that a minimal EEG event, such as a K complex, may induce an increase of the sympathetic discharge,28 we checked whether these events with minimal EEG changes (grades 0a and Ob) were associated with larger arterial BP elevations than events with no EEG changes (grade 0c). We found no differences, suggesting that use of arous- ability criteria that are more sensitive than AS DA criteria does not provide any additional clinical in¬ formation on the cardiovascular consequences of upper airway obstruction without obstructive sleep apnea/hypopnea. conclusion, we found that, similar to OSAS patients, snorers with upper airway obstruction with¬ In sleep apnea/hypopnea exhibited transient systemic BP elevations at termina¬ abrupt tion of respiratory events. In addition, the magnitude of the transient BP increases during NREM sleep varied with the grade of the arousal associated with out obstructive 990 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 the nonapneic-nonhypopneic respiratory event. However, BP increases were also seen in the absence of detectable EEG arousal. Because the other factors generally believed to produce postapneic BP eleva¬ tion in OSAS are absent or insignificant in patients with upper airway obstruction without obstructive sleep apnea/hypopnea, we believe that arousal is the main cause of the systemic BP increases seen after termination of nonapneic-nonhypopneic obstructive events. In addition, given that BP increases also oc¬ curred without apparent EEG arousal, beat-to-beat BP evaluation may be a more sensitive means of identifying nonapneic-nonhypopneic respiratory events than con¬ ventional evaluation of EEG changes. ACKNOWLEDGMENT: We are grateful to Djibril Bokar Thire, Nathalie Gadenne, Denise Henry, and Richard Morales for their skillful technical assistance. 1 2 References Coccagna G, Montovani M, Brignani F, et al. Continuous recording of the pulmonary and systemic arterial pressure during sleep in syndromes of hypersomnia with periodic breathing. Bull Eur Physiopathol Respir 1972; 8:1159-72 Shepard JJ. Gas exchange and hemodynamics during sleep. Clin Med North Am 1985; 69:1243-64 3 O'Donnell C, Ayuse T, King E, et al. Air-way obstruction during sleep increases blood pressure without arousal. J Appl Physiol 1996; 80:773-81 4 Buda AJ, Pinsky MR, Ingels NB, et al. Effect of intrathoracic pressure on left ventricular performance. N Engl J Med 1979; 301:453-59 5 Jardin F, Bourdarias JP. Influence of abnormal breathing conditions on right ventricular function. Intensive Care Med 1991; 17:129-35 6 Lloyd T. Effect of inspiration on inferior vena caval blood flow in dogs. J Appl Physiol 1983; 55:1701-08 7 Howell J, Permutt S, Proctor D, et al. Effect of inflation of the lung on different parts on pulmonary vascular bed. J Appl Physiol 1961; 16:71-76 8 Marini JJ, Culver BH, Butler J. Mechanical effects of lung distension with positive pressure on cardiac function. Am Rev Respir Dis 1981; 124:382-86 9 Kaufman M, Iwamoto G, Ashton J, et al. Response to inflation of vagal afferents with endings in the lungs of dogs. Circ Res 1982; 51:525-31 10 Ringler J, Basner R, Shannon R, et al. Hypoxemia alone does not explain blood pressure elevations after obstructive apneas. J Appl Physiol 1990; 69:2143-48 11 Ali NJ, Davies RJ, Fleetham JA, et al. Periodic movements of the legs during sleep associated with rises in systemic blood pressure. Sleep 1991; 14:163-65 12 Ali N, Davies R, Fleetham continuous on J, et al. The acute effects of positive airway pressure on oxygen administration blood pressure during obstructive 1992; 101:1526-32 13 Davies R, Belt P, Roberts S, sleep apnea. Chest et al. Arterial blood pressure responses to graded transient arousal from sleep in normal humans. J Appl Physiol 1993; 74:1123-30 14 Ringler J, Garpestad E, Basner R, et al. Systemic blood pressure elevation after airway occlusion during NREM sleep. Am J Crit Care Med 1994; 150:1062-66 15 Rees K, Spence D, Earis J, et al. Arousal responses from Clinical Investigations 16 apneic events during non-rapid-eye-movement sleep. Am J Respir Crit Care Med 1995; 152:1016-21 Guilleminault C, Stoohs R, Duncan S. Snoring (I): daytime 23 sleepiness in heavy snorers. Chest 1991; 99:40-48 17 Guilleminault C, Stoohs R, Clerk A, et al. A cause of excessive daytime sleepiness: the upper airway resistance syndrome. Chest 1993; 104:781-87 18 Murray W. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991; 14:540-45 19 American Sleep Disorders Association. EEG arousals: scoring rules and examples. Sleep 1992; 15:174-84 20 Guilleminault C, Stoohs R, Clerk A, et al. Excessive daytime 24 25 26 somnolence in women with abnormal respiratory effort dur¬ Respir Physiol 1991; 85:151-67 27 Scharf S. The effect of decreased intrathoracic pressure on ventricular function. J Sleep Res 1995; 4S:53-58 28 Somers V, Dyken M, Mark A, et al. Sympathetic-nerve ing sleep. Sleep 1993; 16:sl37-38 21 Liistro G, Stanescu C, Veriter C, et al. Pattern of snoring in obstructive sleep apnea patients an in heavy snorers. Sleep 1991; 14:517-25 22 Rechtschaffen A, Kales A. A manual of standardized AMERICAN activity during sleep in normal subjects. N Engl J Med 1993; 328:303-07 termi¬ COLLEGE nology, techniques and scoring system for sleep stages of human subjects. Washington, DC: National Institutes of Health 1968; publication No. 204 Hajduczok G, Chapleau MW, Johnson SL, et al. Increase in sympathetic activity with age: I. Role of impairment of arterial baroreflexes. Am J Physiol 1991; 260:H1113-20 Guilleminault C, Stoohs R, Shiomi T, et al. Upper airway resistance syndrome, nocturnal blood pressure monitoring, and borderline hypertension. Chest 1996; 109:901-08 Parish JM, Shepard JW Jr. Cardiovascular effects of sleep disorders. Chest 1990; 97:1220-26 Stoohs R, Guilleminault C. Snoring during NREM sleep: respiratory timing, esophageal pressure and EEG arousal. OF BCHE ST CONTINUING MEDICAL EDUCATION PHYSICIANS SleepforMedicine the Chest Physician May 20-23, 1998 Chicago, Illinois FOR INFORMATION CALL 800*343*2227 OR 847*498*1400 CHEST/113/4/APRIL, 1998 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 991