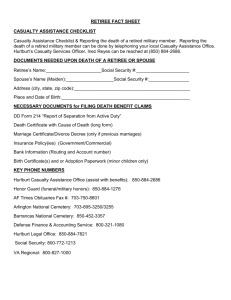
ABC to Advanced
First Aid
Includes...
• Workplace
• Advanced
• Remote
• Oxygen
• Defib
• CPR
• LVR
International
Emergency Numbers
2010 Guidelines
Dr Audrey Sisman
ABC to Advanced First Aid
1st Edition June 2011
Published by: Author:
ISBN: ABC Publications, PO Box 106, Mapleton, Qld 4560, Australia
Dr Audrey Sisman, MBChB
978-0-9806283-2-6
Copyright © 2011 by ABC Publications
All rights reserved. Reproduction of this book, in part or entirely, without written permission is prohibited.
This book has been written based on current guidelines and requirements as defined by:
• Australian, New Zealand and European Resuscitation Councils
• Royal Flying Doctor Service (RFDS)
• National Heart Foundation of Australia
• Australasian Society of Clinical Immunology & Allergy (ASCIA)
• National Asthma Council Australia
• Griffith University, School of Nursing & Midwifery, Prof Jenny Gamble
• Epilepsy Association of Tasmania
• Divers Emergency Service (DES)
For more information about this manual, visit: www.abcpublications.com.au
The information in this book contains, at the time of printing, the most current resuscitation guidelines.
This book is designed to be an information resource and is not a substitute for attending a first aid course
conducted by an approved provider. The author of this book accepts no responsibility for any injury or damage
that may occur as a result of using this book in first aid management.
Introduction
Congratulations on taking positive steps towards learning first aid which is an essential life skill we
should all learn in order to help others and possibly save a life.
The ABC to Advanced First Aid book is written by a medical practitioner with experience in
emergency medicine, hospital medicine, general practice and natural therapies.
The book contains clear, simple first aid advice which will assist you in handling most emergency
situtations.
Keep this book with your first aid kit at home, in your car or when travelling overseas.
How to use this book
ABC to Advanced First Aid is divided into 9 main colour coded sections:
•Essential First Aid •Trauma •Medical Emergencies •Advanced Resuscitation
•Low Voltage Rescue •Advanced First Aid •Workplace First Aid •Remote First Aid
•General First Aid
Each subsection shows you step-by-step how to recognise and deal with an emergency situation.
Emergencies are recognised by SIGNS & SYMPTOMS which are contained in a red box.
Displayed in a green box is the FIRST AID management of an emergency situation.
means dial your country’s emergency number.
A fold out World Map of international emergency numbers at the back of the book identifies
emergency numbers across the world. The Emergency Numbers page is for writing local,
national and international emergency numbers.
Also at the back, there is a First Aid Report Form and Workplace Casualty Report Form which
can be torn out and used in a first aid incident.
☎
Essential First Aid
Unconscious..................................................2
DRSABCD - Basic Life Support......................3
CPR...............................................................4
Choking.........................................................6
Drowning................................................7
Trauma
Soft Tissue Injury & Fracture..........................8
Upper Limb Injury..........................................9
Lower Limb / Pelvic Injury.............................10
Bleeding .......................................................12
Shock ...........................................................14
Crush Injury ................................................14
Burns ...........................................................15
Electric Shock ............................................16
Triage/ Prioritizing .........................................16
Chest ...........................................................17
Abdomen .....................................................18
Eye ..............................................................19
Head Injury ..................................................20
Spinal Injury .................................................21
Medical Emergencies
Heart Conditions ..........................................22
Asthma .........................................................23
Croup/ Epiglottitis .........................................24
Faint .............................................................24
Seizure/ Epilepsy .........................................25
Febrile Convulsion .......................................25
Diabetes .......................................................26
Stroke ..........................................................27
Hyperventilation ...........................................27
Heat Exposure .............................................28
Cold Exposure .............................................29
Bites and Stings .........................................30
Poisons ........................................................32
Allergy/ Anaphylaxis .....................................33
Advanced Resuscitation
Oxygen Equipment .....................................34
Oxygen Therapy .........................................36
Oxygen Resuscitation .................................37
Oropharyngeal Airways ...............................38
Suction .........................................................39
Jaw Thrust ..................................................40
Normal Heart Function ................................40
Abnormal Heart Rhythms ...........................40
Defibrillation & AEDs....................................41
Cardiac Arrest..............................................42
Chain of Survival.........................................42
Advanced Resus Techniques.......................42
.
Low
Voltage Rescue
What is Electric Shock.............................44
What Can Electric Shock Do to Me?..........44
Contents
What Type of Injuries Follow?.....................44
What is Arc Flash?.....................................45
What is Flash Burn?.....................................45
What is Airway Burn?.................................45
What is an Electrical Burn?.........................46
Consequences of Electrical Burns..............46
How Do I Handle Electrical Fires?..............46
Poisonous Gases.........................................47
Low Voltage Rescue Kit.............................47
Performing Low Voltage Rescue.................47
Advanced First Aid
Cervical Collars /Stretchers.........................48
Helmet Removal..........................................50
Harness Suspension...................................51
Scuba Diving................................................52
Childbirth..............................................54
Analgaesia - Penthrox, Entonox, Opiates.....56
Substance Misuse.......................................58
Workplace First Aid
Confined Space...........................................60
Chemical Spills............................................60
Wound Care.................................................61
Wound Infection...........................................62
Infection Control...........................................63
Planning a Workplace First Aid Facility.........64
First Aid Room.............................................65
Remote First Aid
Travelling to a Remote Area........................66
Lost or Injured..............................................67
Survival in Special Circumstances................69
Early Signs of General Unwellness............71
Dehydration............................................71
Altitude Sickness.........................................71
Hygiene ........................................................72
Infection Control in a Remote Area...............72
Moving a Casualty........................................73
Communication ............................................74
Royal Flying Doctor Service (RFDS)............75
Evacuation - Air Rescue................................76
General First Aid
Principles of First Aid ..................................78
Legal Issues ................................................78
Communication/ Reports .............................79
Record Keeping/ Self-Help ..........................79
Safe Manual Handling/ Hygiene .................80
First Aid Kits/Needlestick Injury ..................80
Casualty Assessment ..................................81
Advanced Casualty Assessment ..................82
Narural Medicine in First Aid........................84
Workplace Casualty Report Form
First Aid Report Form
World Map
Emergency Numbers
☎
☎
2 | Essential First Aid
Essential First Aid | 3
Unconsciousness is a state of unresponsiveness, where the casualty is
Basic Life Support & AED
unaware of their surroundings and no purposeful response can be obtained.
NO RESPONSE
NO Breathing or
Follow Basic Life Support Chart
D
Dangers?
Causes of an unresponsive (unconscious), breathing state:
• A - Alcohol (Pg 59)
• T - Trauma (head/ spinal (Pg 20, 21)
Combinations of different
•
E
Epilepsy
(Pg
25)
•
I - Infections (meningitis)
causes may be present in
•
I
Insulin
(Diabetes
Pg
26)
•
P - Pretending
an unconscious casualty eg
• S - Stroke (Pg 27)
• O - Overdose (Pg 32, 58)
head injury and diabetes.
• U - Uraemia (renal failure)
NB.The sense of hearing is usually the last sense to go, so be careful what you say near an unconscious casualty.
R
Response?
All unconscious casualties must be handled gently and every effort made to avoid any twisting
or forward movement of the head and spine.
S
Abnormal Breathing
Breathing Normally
Recovery Position, Call
☎, monitor
(An unconscious, breathing woman in advanced pregnancy should be placed on her left side).
The recovery position:
• Maintains a clear airway - allows the tongue to fall forward.
• Facilitates drainage and lessens the risk of inhaling
foreign material.
• Permits good observation and access to the airway.
• Avoids pressure on the chest which facilitates
breathing.
• Provides a stable position and minimises injury to casuality.
Airway management
takes priority over
spinal injury
© ABC Publications
Response
Obtain history,
Monitor,
Send for help
NO RESPONSE
Send for help. Call
☎
A
Open Airway
B
NO Breathing or
abnormal breathing
Breathing
Normally
Recovery position
& monitor
Send or go for AED
C
Call
☎
Compressions
Shock
Start CPR
30 x Compressions
Step 1
•Raise the casualty’s furthest
arm above the head.
•Place the casualty’s nearest
arm across the body.
•Bend-up the casualty’s nearest
leg.
•With one hand on the shoulder
and the other on the knee, roll
casualty away from you.
Step 2
•Stabilise the casualty by
flexing the bent knee to 90°
when resting on the ground.
•Tuck the casualty’s hand
under their armpit.
•Ensure the casualty’s
head is resting on their
outstretched arm.
CPR
30:2
Step 3
•Carefully tilt the head
slightly backwards
and downwards. This
facilitates drainage of
saliva and/or stomach
contents and reduces
the risk of inhalation
which may cause
pneumonia.
2 x Rescue Breaths
D
Defibrillation
use AED
No
Shock
Advised
Shock
Advised
•Switch on
•Attach pads
•Follow voice
prompts
AED
Analyses
Rhythm
In an EMERGENCY CALL
☎ or
4 | Essential First Aid
Essential First Aid | 5
CPR
HAZARDS!
Dangers
• Biohazards – blood, bodily fluids
• Survey Scene
• Remove or Minimise Hazards
Protect yourself
- use antiseptics
and barrier
protection
(gloves, mask,
goggles).
Response •Talk and touch
Send for help. Call
Airway
☎
•
•
•
•
•
•
•
•
•
•
Chemicals – spills, fumes, fuel
Electricity – powerlines
On coming traffic
Fire, explosion
Unstable structures
Slippery surfaces
Broken glass
Sharp metal edges
Needle stick
Aggressive behaviour
SPEAK LOUDLY – Don’t shout
“Hello, can you hear me”? Are you all right?
“Open your eyes”
“Squeeze my hands”
SQUEEZE SHOULDERS firmly – Don’t shake
NB. When approaching a collapsed casualty with
caution, ascertain a response from a standing position
by tapping casualty’s foot with your foot before kneeling
down.
• Check - for foreign material which could be obstructing the airway.
• Open - use chin lift and backward head tilt to open airway.
Chin lift
Head
tilt
•Use pistol grip to achieve chin
To clear foreign material
lift. Watch that your knuckle doesn’t
compress neck and obstruct airway
and breathing.
•If foreign material is present, roll
casualty into recovery position and
clear using postural drainage and
finger sweep method. Spinal injury and infants(<1yr): Keep head in a
neutral position (i.e. minimise backward head tilt)
• The airway takes precedence over any other injury including a possible spinal injury (Pg 21).
• Check airway and breathing in recovery position if incident involves drowning (Pg 7) or vomiting.
• Look - for rise and fall of lower chest/ upper abdomen
Breathing • Listen - for breath sounds
• Feel - for movement of chest and escape of air from mouth
Abnormal or NO Breathing?
Take 10 seconds
to check for
breathing
• If casualty is unresponsive and not breathing
normally after the airway has been cleared and
opened, the rescuer must immediately commence
chest compressions then rescue breathing (CPR).
• If unwilling or unable to perform rescue breathing,
continue with compression only CPR.
NB. In the first few minutes of a casualty’s cardiac arrest,
sounds of gurgling, sighing or coughing may be present, but
this is ineffective breathing and CPR should be commenced.
Compressions
30 Compressions
CPR
30 Chest Compressions : 2 Rescue Breaths = CPR
• Depth = 1/3 of chest wall (At least 5 cm for adults)
• Rate = 100 per min (almost 2 compressions per sec)
• Place heel of one hand in centre of casualty’s chest
(which is the lower half of the sternum).
• Place other hand on top, arms straight and press down
on sternum at least 5 cm in adults.
• Allow complete recoil of chest after each compression.
• Keep compressions rhythmical at a rate of 100 per min.
• Use 1 or 2 hands in children (Infants 2 fingers)
2 Rescue Breaths
• 2 breaths over 2 secs
•Take a breath.
•Close casualty’s nostrils
(pinch with fingers).
•Mouth to mouth (good seal).
•Blow to inflate lungs.
CPR
30:2
•Turn your head after each RB.
•Listen and feel for air exhaled
from mouth.
•Avoid inhaling re-expired air.
•Inflate until chest starts to
rise.
•Over-inflation forces air
into the stomach causing
regurgitation.
•Infants – perform mouth to
mouth/nose RB and inflate
with puff of air from cheeks.
•Use resuscitation mask or
barrier protection if possible.
•If unwilling or unable
to give RB, do chest
compressions only.
• Cardio Pulmonary Resuscitation • Rate = 5 cycles every 2 mins
• Combines 30 Compressions with 2 Rescue Breaths (30:2) = 1 cycle
Same ratio
for infant,
child, adult
• Change rescuers every 2 mins to reduce fatigue. Stop CPR when:
• Do compression only CPR, if unwilling or unable • Casualty responds or begins breathing normally
• Exhaustion – can’t continue.
to give rescue breaths (RB).
• Health professional arrives and takes over.
• Continue CPR until responsiveness or normal
• Health professional directs that CPR be ceased.
breathing returns.
Defibrillation
An AED (Automated External Defibrillator) delivers electric shock to
reverse abnormal heart rhythms. Not all heart rhythms are reversible.
• When there are 2 rescuers, continue CPR while one
rescuer organises and attaches AED pads (Pg 41):
• Expose chest – cut clothing.
• Remove any medication patch, remove jewelry, wipe
chest dry, remove chest hair with razor.
• Switch on AED & attach pads – peel backing off first.
• Follow voice/ visual prompts of the AED.
• Nobody should touch casualty during analysis or shock
delivery
• DO NOT have casualty in contact with metal
NB.No harm to rescuers has occurred while using an AED in the wet
Chain of survival (Pg 42): is the key to improving the survival rate from cardiac arrest. Time
Early 2) Begin CPR immediately
is the essence. The 4 steps required are: 1) Call
3) Early Defibrillation 4) Advanced cardiac life support by paramedics.
☎
6 | Essential First Aid
Choking
Essential First Aid | 7
Inhalation of a foreign body can cause partial or complete airway obstruction.
Partial Airway Obstruction (Effective cough):
FIRST AID
SIGNS &
SYMPTOMS
• Encourage casualty to keep
coughing
• Reassure
• DO NOT deliver back-blows
if cough is effective.
If blockage doesn’t
• Call
clear
• Coughing
• Wheezing
• Difficulty breathing
• Noisy breathing
• Cyanosis
(blue skin colour)
☎
Complete Airway Obstruction (Ineffective cough):
SIGNS &
SYMPTOMS
• Unable to breathe,
speak or cough
• Agitated/
distressed
• Grips the throat
• Cyanosis (blue)
• Rapid loss of
consciousness
standing or lying using the
heel of the hand between the
shoulder blades.
If after 5 back
blows the
airway is still
obstructed, use chest
thrusts.
Back Blows
Back blows
are delivered
with the
infant lying
face down
across the
lap. Check
airway after
each back
blow.
Drowning or near drowning is the process of experiencing respiratory impairment from
immersion in liquid. Interruption of the oxygen supply to the brain is the most important
consequence of drowning so early rescue and resuscitation are the major factors in survival.
SIGNS & SYMPTOMS
• Coughing • Chest pain • Frothy sputum
• Clenched teeth • Shortness of breath
• Blue lips and tongue • Unconscious
• Irregular or no breathing
A Drowning Victim
FIRST AID
• Deliver up to 5 back-blows.
• Check and clear mouth after each blow.
• Deliver up to 5 chest thrusts.
• Check and clear mouth after each blow.
• Repeat back blows and chest thrusts if
obstruction not relieved.
.
• Call
• If unconscious, commence CPR (Pg 4,5).
DO NOT apply abdominal pressure – may
cause internal injury.
Chest Thrusts
When giving Rescue Breaths in an attempt to blow past the obstruction, there will be resistance. If the
obstruction is blown further down the airways, the obstruction can be removed later by bronchoscope.
• DO NOT attempt to save a
drowning casualty beyond your
swimming ability.
• Remove casualty from water as
soon as possible.
• Only begin Rescue Breathing in
water if trained to do so (requires a
floatation aid) and immediate exit is
impossible.
• Cardiac compressions in water
are both difficult and hazardous and
should not be attempted.
FIRST AID
On land or boat:
• Call
• Roll casualty into recovery position for
assessment of airway and breathing.
• Commence CPR if required (Pg 4,5)
• Roll into recovery position if vomiting
or regurgitation occurs.
• DO NOT attempt to empty distended
stomach by external compression.
• Treat for hypothermia (Pg 29) - often
associated with immersion.
• Give oxygen if trained (Pg 36).
• All immersion casualties must be
assessed in hospital as complications
often follow.
☎
☎
Chest thrusts are delivered standing, sitting
or lying using one or two hands - a
wall or firm surface is required. The
elbow(s) are slightly bent and chest
thrusts are sharper and
slower than chest
compressions (CPR).
Check airway after
each chest thrust.
Back blows are delivered
Drowning
The risk of regurgitation and inhalation is high
following immersion. This is due to distension of
the stomach from swallowing large volumes of
water. The airway and breathing is assessed in
the recovery position to
minimise risk of inhalation.
Rescuing a Drowning Victim
• If conscious: Throw a buoyant aid (life jacket, surf board) or drag from water using an
umbrella, rope, towel, stick.
• If unconscious: Turn casualty face up and remove from water.
• Consider possibility of spinal injury (Pg 21) – remove from water gently, maintaining spinal
alignment as much as possible.
8 |Trauma
Trauma | 9
Soft Tissue Injury & Fracture
Sprain:Over-extension of a joint with stretching and tearing of ligaments.
Strain: Over-stretching of muscles and tendons with tearing of muscle tissue or
tendon fibres.
Slings: Use a triangular
bandage or improvise.
Soft
Tissue
Injury
Improvise:
By using a belt or
buttons on shirt
Dislocation: Displacement of bone ends in a joint.
Fracture: Broken bones can be classified as:
Closed: Fractured bone doesn’t penetrate skin.
Open: Fracture is exposed through open wound or penetrates skin.
Complicated: Vital organ, major nerve or blood vessel is damaged by a broken bone.
The Signs & Symptoms and First Aid for a fracture and soft tissue injury are very similar.
FIRST AID
SIGNS & SYMPTOMS
• Pain • Tenderness
• Snap or pop at time of injury
• Restricted movement
• Discolouration • Swelling
• Deformity*
* Indicative of fracture or dislocation
Fracture Management:
• Control external bleeding or cover wound (Pg 12)
• Remove rings from fingers – swelling likely
• Support or Immobilise +/_ R.I.C.E
• Medical Assistance: X-rays are the only sure
way of diagnosing the type of injury.
if: Deformity as blood vessels
• Call
and nerves can be damaged.
Open Fracture: Risk of blood loss
and infection.
Breathing difficulty
• Monitor Vital Signs (Pg 81)
The radius
always
attaches to
the thumb.
☎
The main aim of fracture treatment is
to support or immobilise an injured
part which: • Minimises pain • Prevents further damage • Minimises bleeding and
• Prevents a closed fracture becoming an open fracture.
Support:
• Leave injured part as found and pack around to give support.
Immobilise:
Elevation Sling
Arm Sling
for 10 - 20mins – do not place ice directly on skin. Ice pack or frozen peas can be placed
over a bandage. Continue to cool injury three times/day for 2-3 days after the injury.
Compression: Apply a firm supporting bandage to injured part. This restricts movement of
injured part and reduces bleeding and swelling.
Elevation: Raise injured area above the level of the heart if possible. This slows the flow of blood and reduces swelling.
Note:
• Degree of pain is not a good indicator of injury type since pain tolerance varies in individuals (Pg 56).
• Never manipulate a dislocation - there may be an associated fracture.
• When in doubt, always treat an injury as a fracture.
• Check circulation (Pg11) after immobilisation ie after bandaging, splinting, sling.
• You may need to slowly adjust position of limb if no circulation is present.
Rigid Splint: Rolled up newspaper,
tied either end with triangular
bandages.
Fractured
humerus:
Notice
deformity
• Use Splint, Sling or bandage to prevent movement.
• Stabilise joint above and below fracture site.
• Apply triangular or broad bandages above and below fracture site.
• Check circulation every 15mins (Pg 11).
• DO NOT elevate a suspected fracture until it has been immobilised.
Soft Tissue Management:
R.I.C.E: Method used to treat soft tissue injuries (sprains/ strains) and fractures.
Rest: Rest casualty and injured part; this prevents further damage and reduces bleeding.
Ice: Reduces pain, fluid and swelling by constricting blood vessels. Apply wrapped ice pack
Upper
Limb Injury
Finger Splints: Immobilisation
reduces pain. After splinting, apply
an elevation sling to minimise
swelling.
Pain in:
Shoulder
Collar
& Cuff Sling
Could be:
•Fractured clavicle •Dislocated shoulder
•Fractured upper humerus •Sprain/ strain
Upper Arm
•Fractured mid-humerus •Sprain/ strain
Fore Arm/
Wrist
•Fractured radius/ ulna •Sprain/ strain
•Fractured carpal bone
Hand
•Fractured/ dislocated metacarpal
•Fractured/ dislocated phalange
•Sprain/ strain
Management:
•Allow casualty to adopt
position of comfort.
•Apply sling which best
suits casualty.
•Keep hand higher than
elbow to reduce swelling
•If unsure whether injury
is a fracture or soft tissue
injury, treat as for fracture
(Pg 8)
10 |Trauma
Trauma | 11
Lower Limb Injury
Pelvic Injury:
SIGNS &
SYMPTOMS
• Pain in hip or
groin region
• Pain worse on
movement
• Inability to walk
• Shock (Pg 14)
Immobilising Lower limb:
FIRST AID
☎
• Call
• Reassure casualty
• Control any external bleeding.
• Lie casualty flat with knees slightly bent and
supported.
• Place padding between legs and on either side
of hips (eg blanket, towel, pillow).
• ‘Figure-of-eight’ bandage around ankles and
feet.
• Apply broad bandage above knees.
• Don’t attempt to move casualty.
• Discourage attempts to urinate.
• Maintain body temperature.
• Monitor vital signs (Pg 81)
Consider internal
bleeding from
bladder, uterus,
bowel damage.
Hip Injury
Left leg appears
shorter and is rotated
outwards.
Notice swelling over
hip due to internal
bleeding. This is the
typical position of the
leg with a fractured
hip (fractured neck of
femur) and is common
in the elderly after a
minor fall.
A 1.5 litre blood loss
can result from a
closed fracture of the
femur. In this case a 3
litre blood loss could
result in shock (Pg 14)
and death.
This type of injury is
common in road traffic
accidents.
Thigh Injury
R.I.C.E (Pg 8)
R.I.C.E (Pg 8)
Ankle Injury
for a sprained ankle:
Rest: Casualty doesn’t
move ankle
Ice: Cool injured area
Compression: Use a
crepe bandage
Elevation: Place foot
higher than hip
for a sprained
knee: Support
knee in position
of comfort. Do not
try to straighten
knee if painful.
Knee Injury
Lower Limb Injury
• A body splint is an effective way
Fracture site
to immobilise lower limb fractures.
• The key to immobilising leg
fractures is a figure of 8 bandage
around the feet.
Use triangular
• Place padding in natural hollows
bandages,
between legs.
broad bandages,
• Stabilise joints above and below
Fracture site
belts, clothing or
fracture site.
sheets to tie legs
• Position all bandages before tying
together. Tie-off on
off.
uninjured leg, above
• Apply broad bandages above and
and below fracture
below injured area.
site.
• Tie bandages off on uninjured
side of body.
Splints can be classified as:
• If using a rigid splint (eg stick)
• Body Splint: Uses uninjured, adjoining body part to ensure splint doesn’t extend
immobilise an injury. Lower limbs, fingers and toes are
commonly strapped together as body splints.
further than length of legs.
• Soft Splint: Folded blankets, towels, pillows.
• Ensure splint stabilises joints
• Rigid Splint: Boards, sticks, metal strips, folded above and below injury.
magazines and newspapers.
• Pad over splint to make more
comfortable.
Checking Circulation:
• Check circulation
• Check skin colour below injury - if pale or discoloured,
there may be impaired circulation.
• Assess skin temperature by gently placing hand below
SIGNS AND SYMPTOMS that
level of injury. Compare to other side. If colder, there
a bandage is too tight:
may be impaired circulation.
• Pain • Numbness • Cold
• Squeeze fingernail until nail turns white. Colour should
to touch • Tingling • Pale or
return within a few seconds.
discoloured • Pulse weak/absent
• Compare pulse below injury with other side - if weaker
below injury.
or absent, circulation may be impaired.
Pain in:
Hip/groin
Could be:
•Fractured Pelvis •Fractured neck of femur
•Dislocated head of femur •Sprain/strain
Thigh
•Fractured femur •Strain: front of thigh
(quadriceps) •Strain: back (hamstrings)
Knee
•Fractured patella •Dislocated patella
•Cartilage tear
•Sprain
Lower Leg/
Ankle
Foot
•Fractured tibia •Fractured fibula
•Dislocation •Sprain/ strain
•Fractured tarsal/metatarsal/phalange
•Dislocation •Sprain/ strain
Management:
• Allow casualty to
adopt position of
comfort.
• If unsure whether
injury is a fracture or
soft tissue injury, treat
as for fracture (Pg 8).
• Elevate a suspected
fracture after it has
been immobilised.
• Minimise movement to
avoid further injury.
• Check circulation after
immobilisation (above).
12 |Trauma
Trauma | 13
Bleeding
Bleeding (haemorrhage) can be external and obvious, or internal (within the body) and often
not seen (Pg 13).
Bleeding is classified according to the type of blood vessel damaged:
Artery - bright red, spurting; Vein - dark red, flowing; Capillary - bright red, oozing.
Types of wounds associated with bleeding are: (See also Pg 62)
• Abrasions • Incisions • Laceration • Puncture • Embedded object • Tear • Amputation.
Major External Bleeding:
The aim is to
reduce blood
loss from the
casualty.
Direct Pressure and Elevation
FIRST AID
• Check for dangers to self, casualty & bystanders.
• Use disposable gloves if available.
• Direct Pressure Method:
• Quickly check for embedded objects (Pg13)
• Apply firm direct pressure until bleeding stops.
• Maintain pressure over the wound using hands or
pad (sterile dressing, tea towel or handkerchief).
• Bandage firmly to hold pressure pad in place.
• If bleeding continues - apply another pad and a
tighter bandage.
• Elevate, immobilise and rest injury.
• Call
• Reassure casualty.
• Assist casualty into position of comfort.
• Monitor vital signs (Pg 81).
• Give oxygen if trained (Pg 36).
• DO NOT give casualty food, alcohol, medication.
• If major bleeding continues - remove all pads to
locate a bleeding point, then apply a more direct
pressure over bleeding point.
• If above methods fail - use a tourniquet.
• Treat for shock (Pg 14) if required.
Direct, sustained pressure is the
fastest, easiest, most effective
way to stop bleeding.
TOURNIQUET: Used to control
life-threating bleeding.
• Use as a LAST RESORT.
• Use a wide bandage (>5cm
wide).
• Apply high above wound.
• Ensure tourniquet is clearly
visible.
• Tighten until bleeding stops.
• Note the time of application;
write time of application on
casualty.
• Continue to maintain direct
pressure over wound.
• DO NOT apply tourniquet over a
joint or wound.
• DO NOT remove tourniquet
until casualty receives specialist
care.
☎
Embedded Object: eg knife, glass, stick or metal.
FIRST AID
• DO NOT remove the object - it could be plugging the wound.
• Build up padding around the object.
• Apply sustained pressure over the pad (indirect pressure).
• Bandage firmly over the pad.
• DO NOT apply pressure over the object.
• DO NOT shorten object unless its size is unmanageable.
• Elevate, immobilise, restrict movment of the limb.
• Advise casualty to remain at rest.
• Call
☎
Internal Bleeding: Signs, symptoms and management as for Shock (Pg 14)
• Suspect internal bleeding if a large blunt force
is involved - eg road traffic accident, fall from
a height; or a history of stomach ulcers, early
pregnancy (ectopic pregnancy) or penetrating
injury.
• Internal bleeding may be concealed or revealed.
• If a casualty is coughing up frothy blood, allow
casualty to adopt position of comfort – normally
half-sitting.
• First aiders can’t control internal bleeding but
can save lives.
early recognition and calling
☎
Concealed: (no bleeding visible)
• Spleen • Liver • Pancreas • Brain
Revealed:
• Lungs – Cough up frothy pink sputum.
• Stomach – Vomit brown coffee grounds
or red blood.
• Kidneys/ Bladder – Blood stained urine.
• Bowels – Rectal bleeding: bright red or
black and “tarry”.
• Uterus - Vaginal bleeding.
Nose bleed
FIRST AID
• Pinch soft part of nose just below the bone.
• Have casualty seated and leaning forward.
• Ask casualty to breathe through their mouth.
• Maintain pressure and posture for at least 10mins (longer may
be required after exercise, hot weather or if casualty has high
blood pressure or takes aspirin or warfarin tablets - maintain
pressure for at least 20 minutes).
• If bleeding continues >20mins - seek medical assistance.
• Apply cold compress to forehead and neck.
• Advise casualty not to blow or pick their nose for a few hours.
Amputation
Tourniquet with time of application noted
Bleeding
Manage amputated limb as for major external bleeding (Pg 12).
Amputation of a limb often requires a tourniquet (Pg12) to control life-threatening bleeding.
• DO NOT wash or soak amputated part in water or any other liquid.
• Wrap the part in gauze or a clean handkerchief and place in watertight plastic bag.
• Place sealed bag or container in cold water which has ice added to it.
• The amputated part should not be in direct contact with ice.
• Send to hospital with the casualty.
14 |Trauma
Trauma | 15
Shock
Shock is a term used to describe an ineffective blood circulation.
CAUSES:
Loss of blood volume: Bleeding or fluid loss
Loss of blood pressure: Heart/ pump failure
or abnormal blood vessel dilatation.
• Internal or external bleeding
bleeding
• Major or multiple fractures
• Severe burns or scalds
• Severe diarrhoea and vomiting
fluid loss
• Heat stroke
The total blood volume in the body is
• Heart attack
- pump failure about 6 litres. Blood loss of >1 litre
• Severe infection
(20%) may result in shock. Rapid
abnormal
• Allergic reactions
blood loss leads to more severe
dilatation of
• Brain/ spinal cord injury
blood vessels shock.
SIGNS & SYMPTOMS
• Pale, cool, clammy skin
• Thirst
• Feeling cold
• Feeling Faint
• Rapid, shallow breathing.
• Nausea/ vomiting
• Confusion
• Reduced level of consciousness.
• Rapid, weak pulse
• Ridged, painful abdomen (from
internal abdominal bleeding).
NOTE: In early stages of blood loss,
children may have a normal pulse
rate, but pallor is the warning sign.
FIRST AID
• DRSABCD - Ensure your own safety
• Call
• If conscious – lie casualty flat
• Control external bleeding (Pg12); stabilise
fractures; treat injuries (use disposable gloves
if available).
• Give oxygen if trained (Pg 36)
• Give nothing by mouth (may cause vomiting
and delay surgery).
• Keep casualty warm but don’t overheat.
• Reassure while monitoring vital signs (Pg 81).
• If casualty becomes unconscious, vomits or
has breathing difficulty, place in recovery position
and monitor.
☎
Crush Injury
A heavy, crushing force to part of the body usually causing extensive tissue damage from
internal bleeding, fractures, ruptured organs, or an impaired blood supply.
FIRST AID
• DRSABCD - Ensure your own safety.
• Call
• If safe - remove crushing force as soon as possible.
• Control external bleeding (Pg12).
• DO NOT use a tourniquet (Pg12) to manage a crush
injury.
• Manage other injuries.
• Give oxygen if trained (Pg 36).
• Reassure while monitoring vital signs (Pg 81)
NB - the casualty’s condition may deteriorate quickly
due to extensive damage.
☎
Crush Injury Syndrome:
•Is a complication of crush injury
usually involving a thigh or pelvis
(ie not a hand or foot).
•Toxins released from damaged
tissue may cause complications but
the risk of sudden death following
removal of a crushing force is
extremely small.
Burns
Burns may result from: • Heat (flame, scald, direct contact) • Cold • Friction
• Chemical (acid, alkali) • Electrical • Radiation (sunburn, welders arc).
• DO NOT apply ice directly to burns.
FIRST AID
• DO NOT break blisters.
• DRSABCD - Ensure your own safety
• DO NOT apply lotions, ointments, creams or
• Cool affected area with water for as long
powders (except hydrogel).
as necessary - usually 20mins.
• DO NOT peel off adherent clothing or other
• Remove rings, watches, jewelry from
substances.
affected area.
• DO NOT use “fluffy” dressings to cover burn
• Cut off contaminated clothing – do not
(towels, tissues, cotton wool).
remove clothing contaminated with
Seek
medical help for:
chemicals over the head or face.
•
Chemical
burns • Electrical burns
• Elevate burnt limb if possible.
•
Inhalation
burns • Full thickness burn
• Cover burnt area with a loose, non-stick
• Infant, child or elderly.
dressing (sterile non-adherent dressing,
• Burns to hands, face, feet, major joints, or plastic cling wrap, wet handkerchief,
genital area.
sheet, pillow case).
•
Burn
size > casualty’s palm.
• DO NOT allow shivering to occur.
•
Burns
encircling limbs or chest.
• Hydrogel products are an alternative if
• Burns associated with trauma.
water is not available.
Extensive burns may result in shock from fluid loss (Pg14).
Full Thickness Burn
Partial Thickness Burn
Superficial Burn
(1st degree)
(2nd degree)
(3rd degree)
Reddening (like sunburn)
Red and Blistering
White or blackened
Painful
Very Painful
Not painful
Flame: • STOP, DROP, COVER, ROLL the casualty to put out flames • Smother flames with a
blanket, coat or rug and force casualty to lie on the ground • Move to safety • Call
☎
Inhalation: (See also Pgs 32, 45, 47) • Inhalation of flames or heated air can cause severe
damage to the airways resulting in swelling and possible airway obstruction • DO NOT enter a
buring or toxic atmosphere without appropriate protection • Remove to a safe, ventilated area
ASAP • Look for evidence of inhalation injury around nose or face • Coughing or hoarseness
may indicate exposure • Give oxygen if trained • Call
Chemical: • Acids and alkalis cause chemical burns • Brush powered chemicals from the
skin before cooling with water • Do not neutralise either acid or alkali burns because this will
increase heat generation and cause more tissue damage • Call
☎
☎
Bitumen: • Bitumen holds heat therefore cool with water for 30mins • DO NOT remove from
skin unless it’s obstructing the airway • If the limb is completely encircled, split the bitumen
lengthwise as it cools • Call
☎
Electrical: • Burns are usually more severe than they appear and often associated with other
injuries (Pg 16, 46) • Call
☎
16 |Trauma
Trauma | 17
Electric Shock
(See also Pg 44)
Electric shock may cause: • Respiratory Arrest • Cardiac Arrest (Pg 42) • Burns (Pgs 15, 46)
FIRST AID
• Ensure safety of yourself and bystanders.
• Call
• If safe to do so switch off power at wall - if necessary
switch off power at fuse box.
• If not possible, use non-conducting material (wooden
stick, dry towel) to move casualty from electrical source.
• Commence CPR if required (Pg 4,5).
• Apply first aid to burns (Pg 15, 46).
SIGNS & SYMPTOMS
Dry towel around casualty’s ankles to
move from electrical source.
DO NOT touch casualty’s skin before electrical source is disconnected.
BEWARE: Water on floor and metal materials can conduct electricity from casualty to you.
• When POWERLINES are in contact with a vehicle or
a person, there should be no attempt at removal or
resuscitation of the casualty until the situation is declared
safe by electrical authorities.
• Remain at least 6m from energized material (car body, pool
of water, cable).
• You can do nothing for a casualty within the danger zone!
Protect yourself and others.
Triage/ Prioritizing
You may be faced with the dilemma of two or more casualties needing your care. In making
a decision who to treat first, remember the goal is for the greatest good for the greatest
number of people. In all cases remember the principles of safety to yourself, bystanders
and casualty.
Prioritize casualties as follows:
Code Red
URGENT - Immediate resuscitation and stabilization eg • Control
severe bleeding • Open & stabilize airway in an unconscious casualty.
Priority 2
HIGH - Treatment but no active resuscitation eg • Burns • Spinal
injury • Open fracture • Crush injury • Head, Chest , Abdominal Injury.
Priority 3
LOW - Walking Wounded
eg • Cuts • Grazes • Sprains • Closed fracture.
Priority 4
NO ACTION - Dead or beyond help
eg • Decapitation • Massive head or torso injuries.
Code yellow
Code Green
Code Black
Major chest injuries include fractured rib, flail chest (multiple rib fractures,
producing a floating segment of ribs), and sucking chest wound. A fractured
rib or penetrating injury may puncture the lung.
Fractured Rib/
Flail Chest:
☎
Priority 1
Chest
Note: A casualty is always in a changing, non static condition. This is especially important in head
(Pg 20) and abdominal injuries (Pg 18) in which deterioration can occur - monitor vital signs (Pg 81).
•Holding chest
•Pain at site
•Pain when breathing
•Rapid, shallow breathing
•Bruising
•Tenderness
•Blue lips (flail chest or
punctured lung)
•Flail Chest –section
of chest wall moves in
opposite direction during
breathing.
•Onset of shock (Pg 14)
FIRST AID
•Position casualty in position of
comfort - half-sitting, leaning
toward injured side, if other
injuries permit.
•Encourage casualty to breathe
with short breaths.
•Place padding over injured area.
•Bandage the upper arm on
injured side to the body.
•If bandages increase discomfort,
loosen or remove them.
•Apply a ’Collar & Cuff’ sling to
arm on injured side (Pg 9).
•Call
•Monitor for internal bleeding/
shock (Pg 13, 14)
•Give oxygen if available (Pg 36).
•If Unconscious: Recovery
position, injured side down.
☎
Sucking Chest Wound:
SIGNS & SYMPTOMS
• Pain
• Breathing difficulty
• Sucking sound over wound
when casualty breathes.
• Bloodstained bubbles
around wound when casualty
breathes.
• Coughing up bloodstained
frothy sputum.
• Onset of shock (Pg 14).
FIRST AID
• Assist casualty into position of comfort - half-sitting,
leaning toward injured side.
• If the object is still in place, stabilise with padding
around the wound.
• If the wound is open, cover with plastic or non-stick
pad taped on 3 sides -this allows air to escape
from pleural cavity and prevents lung collapse
(pneumothorax).
• Call
• Monitor for internal bleeding/ shock (Pg 13, 14).
• Administer oxygen if available (Pg 35).
☎
18 |Trauma
Abdomen
An injury to the abdomen can be an open or closed wound. Even with a closed wound the
rupture of an organ can cause serious internal bleeding (Pgs 13, 14), which results in shock
(Pg 14). With an open injury, abdominal organs sometimes protrude through the wound.
FIRST AID
☎
• Call
• Place casualty on their back with pillow
under head and shoulders and support
under bent knees.
• If unconscious - place in recovery position.
• Cover exposed bowel with moist non-stick
dressing, plastic cling wrap or aluminium
foil.
• Secure with surgical tape or bandage (not
Open Abdominal Injury
tightly).
Plastic cling wrap has been placed over an
• Rest and reassure.
open abdominal wound and secured with
surgical tape.
• Monitor vital signs (Pg 81).
• Administer oxygen if available (Pg 36).
• Elevate legs if shock develops (Pg 14).
• DO NOT push bowel back into abdominal
cavity.
• DO NOT apply direct pressure to the wound.
• DO NOT touch bowel with your fingers (may
cause spasm).
• DO NOT give food or drink (this may delay
surgery for wound repair).
Trauma | 19
Eye
Types of eye injuries: • Burns • Foreign bodies • Penetrating injury • Direct blow
Burns:
FIRST AID
Chemical - acids, caustic soda, lime
UV - Welder’s flash, snow blindness
(the eyes are red and feel gritty hours later)
Heat - flames or radiant heat
Contact Lenses: • DO NOT remove if the
surface of eye is badly damaged • Casualty
should remove own lenses • Lenses may
initially protect the eye but if a chemical or
foreign body tracks under the lens, severe
injury may occur.
• IRRIGATE with cool running water or sterile
eye (saline) solution for 20 -30mins.
• Flush from the inside to the outside of eye.
• Irrigate under the eyelids.
• Lightly pad affected eye(s).
• Seek urgent medical assistance.
• Chemical burn - DO NOT waste time
looking for neutralizing agent - irrigate as
above with water or saline solution.
• NB. Alkaline burn is worse than acid burn.
Foreign body: Grit, dust, metal particles, insects, eyelashes.
FIRST AID
• Gently irrigate eye to wash out object – use sterile eye
(saline) solution or gentle water pressure from hose/ tap.
• If this fails, and the particle is on white of eye or eyelid,
gently lift particle off using a moistened cotton bud or the
corner of a clean handkerchief.
(DO NOT attempt this if particle is on coloured part of eye –
irrigate only)
• If still unsuccessful, cover the eye with a clean pad ensuring
no pressure is placed over injured eye.
• Seek medical aid.
• DO NOT allow casualty to rub eye.
Penetrating Injury:
FIRST AID
• Lay the casualty flat.
• Reassure
• Call
• Place padding around the object.
• Place a paper cup over the object to stabilize it.
• Tape or bandage to hold in place.
• Advise casualty to avoid moving unaffected eye, because
this will cause movement of injured eye.
• Cover the unaffected eye, but remove if casualty becomes
anxious.
• DO NOT remove embedded object.
• DO NOT apply pressure over the object.
☎
Direct Blow: Any direct blow to the eye such as a fist or squash ball can cause fracture
of the eye socket or retinal detachment.
FIRST AID • Rest and Reassure • Place padding over eye • Secure with tape or
bandage • Ask casualty to limit eye movement • Seek urgent medical aid
20 |Trauma
Trauma | 21
Head Injury
Spinal Injury
Blood or fluid from the ear may indicate a
ruptured eardrum (Pg 53) or skull fracture:
• Position casualty injured side down to
allow free drainage of fluid from the ear.
• DO NOT plug or bandage ear.
SIGNS & SYMPTOMS
•Headache or giddiness
•Nausea or vomiting
•Drowsy or irritable
•Slurred speech
•Blurred vision
•Confused or disorientated.
•Loss of memory
•Swelling and bruising around eyes.
•Bleeding into corner of eyes.
•Bruising behind ears.
•Straw coloured fluid or bleeding
from nose or ear.
•Loss of power in limbs.
•Loss of co-ordination.
•Seizure
•Unequal pupils
•Loses consciousness, even briefly.
Concussion: “Brain Shake” is a
temporary loss or altered state of
consciousness followed by complete
recovery. Subsequent decline
(see signs and symptoms above)
suggests a more serious brain injury.
Conscious:
Cervical
SIGNS & SYMPTOMS
Lumbar
Thoracic
Spinal Column
•AIRWAY management takes priority
over any other injuries.
•ALL cases of unconsciousness, even
if casualty was unconscious only
briefly, must be assessed by a doctor.
•If casualty didn’t lose consciousness,
but later develops any of the following
signs and symptoms (below), urgent
medical advice must be sought.
•Monitor all casualties closely for the
first 8 hrs after a head injury.
•All head injuries should be treated as
a suspected spinal injury until proven
otherwise.
(See also Pgs 48, 49)
The key to managing a spinal cord injury: Protect airway & Minimise spinal movement.
FIRST AID
Check DRSABCD (Pg 3)
Conscious:
• Support casualty’s head as best as possible.
• Reassurance, especially if confused.
• If blood or fluid coming from ear or nostril, loosely
cover with a dressing (do not plug).
• Control bleeding and cover wounds (Pg 12).
• DO NOT give anything to eat or drink.
• DO NOT give analgaesia (Pg 56) for headache may cause drowsiness and confuse vital signs.
• Prepare for possible vomit – locate bowl, towel.
• Administer oxygen if available (Pg 36).
• Seek urgent medical aid.
Unconscious:
• Recovery position with head & neck support.
• Call
• Continuously monitor & record vital Signs every
5-10mins (Pg 81).
• Control bleeding and cover wounds.
• Support/stabilize head and neck.
• Keep warm with a blanket.
• Prepare for possible vomit.
☎
Cerebral Compression: Brain swelling or bleeding
within the skull shows deteriorating signs and
symptoms (above). This is a serious brain injury and
could be life threatening.
• Pain in neck or back.
• Pins and needles in any part of
body.
• Numbness or weakness.
• Unable to move legs or arms.
• Uncontrolled penile erection.
• Onset of shock (Pg 14).
FIRST AID
• Prevent further injury by AVOIDING movement
of patient - leave this to the experts.
• Advise casualty to remain still.
• Call
• Support the head and neck.
• Reassure casualty.
• Maintain body temperature with a blanket.
☎
QUICK CHECK
Conscious Casualty:
Support the head and
neck in a conscious
casualty with neck pain.
Do not remove helmet
and ask casualty to
remain still.
Suspect spinal injury with:
Unconscious casualty:
(Log Roll Technique)
Turn casualty onto their side,
maintaining head, neck, and spinal
alignment. Rescuer at head takes
charge. Maintain an open airway.
• Can you wriggle your fingers and toes for
me?
• Can you make a fist?
• Can you shrug your shoulders?
• Can you pull your toes up towards you
and point them away?
• Do you have pins and needles anywhere?
• Can you feel me touch your hands/ feet?
NB. If the casualty has neck or back pain- treat as a spinal injury. The pain may be
due to an unstable vertebral fracture which
may result in spinal cord damage if handled
incorrectly.
Motor vehicle accidents, motor bike and
cyclists, diving, falls from a height, minor
falls in the elderly and sports injuries such
as rugby and horse riding.
Unconscious:
Any person found unconscious is potentially spinal injured until proven otherwise - turn
casualty onto their side and maintain an open airway.
REMEMBER, airway management takes priority over spinal injury.
Helmet Removal: Helmets could be
preventing further spinal or head injuries.
If a full-face (motorcycle) helmet is
impeding proper airway management in
an unconscious casualty and/ or you need
to perform CPR, the helmet needs to be
removed carefully (Pg 50). Otherwise leave
helmet removal to the experts.
FIRST AID
• Recovery position with head & neck support.
• Call
• Continuously monitor & record vital Signs
every 5-10mins (Pg 81).
• Control bleeding and cover wounds.
• Support/ stabilize head and neck.
• Keep warm with a blanket.
• Prepare for possible vomit.
☎
22 | Medical Emergencies
Heart Conditions
Medical Emergencies | 23
Angina is a “cramping” of the heart muscle; relieved by
rest, with no permanent muscle damage.
Heart attack is caused by a blocked coronary artery,
resulting in muscle damage which may lead to
complications such as cardiac arrest.
Cardiac arrest (Pg 42) is a condition in which the heart
stops beating and pumping effectively. The damage
caused by a heart attack may cause abnormal rhythms
(Venticular Fibrillation) which result in cardiac arrest (Pg
40). Some abnormal rhythms can be reversed by an AED.
Cardiac arrest is fatal without basic life support (Pg 3).
“Heart attack” and “Angina” are heart conditions
which present with similar signs and symptoms.
SIGNS & SYMPTOMS – vary greatly, and not all symptoms and signs are present!
• Central chest pain – may be described as •Crushing •Tightness •Heaviness
• Breathlessness or difficulty “catching the breath”
• Indigestion type pain in the upper abdomen (referred pain from the heart)
• Pain radiating to the •Jaw •Neck •Shoulder •Left arm
• Heaviness or weakness in left arm
• Dizzy
• Nauseous
NB. Casualties having a heart attack may present with
• Pale and sweaty
breathlessness alone while others may have heaviness
• Irregular pulse
in the arm or believe they have indigestion.
Asthma
Asthma is spasm and narrowing of the airways with inflammation and
increased mucus production which causes breathing difficulties. Asthma attacks are
triggered in sensitive airways by changes in the weather, exercise, emotional stress, pollen,
dust-mite, food preservatives, smoke, fumes or cold and flu infection.
• Dry cough
• Wheeze – during exhalation
• Breathless but speaks in sentences
Moderate:
• Wheeze - during exhalation and inhalation
• Rapid breathing
• Breathless - speaks in phrases
• Anxious
• Pale and sweaty
• Rapid pulse
Severe:
• Can’t speak (too breathless)
• Wheeze inaudible (no air movement)
• Cyanosis (blue lips)
• Exhaustion
• Distressed
• Altered state of consciousness
• Collapse - Respiratory arrest
FIRST AID
• STOP and REST – in position of comfort (usually sitting).
• Reassure and talk to casualty – Are you on prescribed heart medication?
Do you have angina? Can you take aspirin?
• If casualty has no heart medication and has never been diagnosed with heart problems
’ • Give aspirin if directed • Monitor
– treat as for HEART ATTACK • Call ‘
• Assist casualty to take prescribed heart medication (anginine tabs or GTN spray).
• If after 5 mins symptoms are not relieved, and if directed, give another dose of heart medication.
Warning signs:
DON’T WAIT
Pain lasts > 10 mins
ACT NOW
Pain gets suddenly worse
Aspirin should be given if directed.
DO NOT give aspirin if:
• Casualty takes Warfarin
(blood thinning medication)
• Allergic to aspirin
• History of Asthma or Stomach ulcers
Call
☎
Give Aspirin 300mg
(one chewable tablet)
if directed.
Monitor vital signs
Give Oxygen if trained
(Pg 36)
Vital Signs
(Pg 81)
Prepare for CPR
• Sit casualty comfortably upright.
• Calm and reassure.
• Follow casualty’s Asthma Action Plan or
give:
• Reliever Medication - 1 puff followed by
4 breaths, repeat 4 times (total 4 puffs).
• If no improvement in 4 mins, repeat.
• Call
if no improvement
• Give oxygen if trained (Pg 36).
• Keep giving 4 puffs every 4 mins until
ambulance arrives or casualty improves
significantly.
• Collapse:
• Commence DRSABCD (Pg 3)
☎
Rescue breaths require much greater
force due to narrowed airways. Slowly
inflate with a steady pressure until chest
begins to rise. Allow time for chest to fall
during expiration. It may take longer to
give the two rescue breaths.
Give Reliever Medication
via spacer. Use puffer
on it’s own if spacer not
available.
☎
ANGINA should be relieved by rest and medication (tablets or spray).
• If after 3 doses of medication over 10mins, the pain has not diminished,
then the condition should be considered a HEART ATTACK
FIRST AID
SIGNS & SYMPTOMS
Mild:
Spacer
Reliever Medication:
• Blue - grey coloured
inhalers (puffers) eg
Ventolin, Respolin,
Atrovent, Salbutamol.
•Borrow an inhaler if
necessary.
• No harm is likely to
result from giving a
Reliever to someone who
does not have asthma.
Using Puffer - no spacer
• Shake inhaler (Puffer).
• Place mouthpiece in casualty’s
mouth.
• Administer 1 puff as casualty
inhales slowly and steadily.
• Casualty takes 4 normal
breaths.
• Continue until 4 puffs have
been given.
• Wait 4 mins and repeat if no
improvement.
Using Puffer - with a spacer
• Shake inhaler and place
mouthpiece into spacer.
• Place spacer mouthpiece into
casualty’s mouth.
• Administer 1 puff and ask
casualty to breath in and out for 4
breaths.
• Continue until 4 puffs have been
given.
• Wait 4 mins and repeat if no
improvement.
24 | Medical Emergencies
Medical Emergencies | 25
Croup/ Epiglottitis
Croup and Epiglottitis are infections of the upper airways (larynx, pharynx and trachea) and
occur in young children. Both conditions start with similar signs and symptoms but epiglottitis
progresses to a life-threatening state.
Croup: Viral infection
EPIGLOTTITIS:
• Drools –can’t swallow
• Quiet, doesn’t cough
• Leans forward
• Won’t talk
• High temperature
• Skin flushed
Mild
FIRST AID
Severe
SIGNS & SYMPTOMS
CROUP:
• Cold-like symptoms
• Barking cough
• Noisy breathing
• Slight temperature
• Worse at night
• Breathing difficulties
• Cyanosis (blue lips)
• DO NOT examine child’s
throat – this may cause
complete blockage.
• Calm and Reassure.
• Steamy shower room.
• Paracetamol
• Seek medical aid.
☎
• Call
• Comfort, reassure
• Sit upright on your lap.
• Lots of TLC until
ambulance arrives.
affecting upper airways in
infants and children
< 4yrs. Slow onset,
usually follows a cold or
sore throat and lasts 3 – 4
days.
Epiglottitis: Bacterial
infection of the epiglottis
(flap above the vocal
cords) causing upper
airway obstruction. It
usually occurs in the
4 - 7yr age group and has
a rapid onset over 1-2hrs.
This is an emergency
and requires urgent
ambulance transport to
the hospital.
Steam helps
alleviate symptoms
of Croup but won’t
cure the problem.
Doctors find it
difficult to clinically
differentiate
between Croup and
Epiglottitis - further
tests are usually
required.
A seizure is caused by abnormal electrical activity in
the brain. Seizures vary from the briefest lapses of attention to prolonged convulsions
(tonic-clonic or grand mal seizure). A seizure can occur in a person with • Epilepsy • Head
Injury (Pg 20) • Stroke (Pg 27) • Meningitis • Fever (febrile convulsion) • Hypoglycaemia
(diabetics Pg 26) • Poisoning (Pg 32) • Alcohol and • Drug Withdrawal (Pg 58).
SIGNS & SYMPTOMS
Tonic-Clonic Seizure (Grand Mal)
• Aura (warning sign: eg abnormal
taste, smell, sound or sight).
• Cry out or make moaning sound.
• Collapse and momentary rigidity
(tonic phase – lasts few secs).
• Eyes roll upwards or stare.
• Jerking movements of body (clonic
phase – lasts few mins).
• Blue discolouration of face/ lips
• Excessive salivation
• Tongue biting may result in blood
stained saliva.
• Loss of bladder or bowel control.
• Breathing ceases – resumes once
seizure finishes.
• Drowsiness and lethargy follows.
Febrile Convulsion
FIRST AID
• Protect from harm – remove dangerous objects
or protect head with cushion/ pillow.
• Note the time.
• AVOID restraining unless this is essential to
protect from injury.
• DO NOT put anything into casualty’s mouth.
• Roll into Recovery position as soon as possible.
• Monitor Vital Signs (Pg 81).
• Reassure casualty and allow to sleep under
supervision at end of seizure.
•Call
if:
• Seizure lasts longer than 5mins.
• Another seizure quickly follows.
• Casualty is pregnant or has diabetes.
• Seizure occurred in water.
• This is casualty’s first ever seizure.
• Casualty is injured or you’re in doubt.
☎
A person known to have epilepsy may not require
ambulance care.
(Normal body temperature = 37°C)
Febrile convulsions are associated with a high body temperature (>38°C). It is the rate of rise
in temperature, not how high it gets, which causes the convulsion. They occur in 3% of all
children between the age of 6mths and 6yrs.
Faint
Fainting is a sudden,
brief loss of consciousness
caused by lack of blood flow
to the brain with full recovery.
It often occurs in: • Hot
conditions with long periods
of standing • Sudden postural
changes (eg from sitting to
standing) • Pregnancy (lower
blood pressure) • Pain or
emotional stress (eg sight of
blood).
Seizure/ Epilepsy
SIGNS & SYMPTOMS
• Dizzy or light headed.
• Nausea
• Sweating
• Return of consciousness
within a few seconds of
lying flat.
• Pale and sweaty
• Mild confusion or
embarrassment.
FIRST AID
• Lie casualty flat
• Raise legs
• Pregnant woman turn onto
left side.
• Recovery position if
unconscious for more than a
few seconds.
• DO NOT give food or drink.
• Check for other injuries.
SIGNS & SYMPTOMS
(Similar to epilepsy + fever)
• Fever
• Skin hot, flushed
• Eyes roll up
• Body stiffens
• Back and neck arches
• Protect from harm • Place in • Jerking of face, limbs
recovery position after seizure • Frothing at mouth
• Blue face and lips
stops • Remove excess
• Lethargy follows
clothing
FIRST AID
• Manage as for Seizure/
Epilepsy (above).
PLUS:
• Remove excess clothing
• Apply moist cloth to
forehead (no ice).
• DO NOT allow shivering
to occur
• DO NOT put in cold bath
26| Medical Emergencies
Medical Emergencies | 27
Diabetes
• Diabetes is an imbalance between glucose and insulin levels in the body.
• The imbalance may result in Hypoglycaemia (Low blood sugar) or Hyperglycaemia
(High blood sugar). Both conditions, if left untreated, result in altered states of
consciousness which are medical emergencies.
DIFFERENCES
SIGNS & SYMPTOMS - Both conditions share similar signs and symptoms:
• Appear to be drunk (Dizzy, drowsy, confused, altered level of consciousness) • Rapid breathing • Rapid pulse • Unconscious
HYPOglycaemia (LOW)
• Pale, cold sweaty skin
• Fast progression
• Hunger
• Trembling
• Weakness
• Seizure
HYPERglycaemia (HIGH)
• Warm, dry skin
• Slow progression
• Acetone smell on breath (nail polish remover)
• Thirst
• Passes urine frequently
• Nausea and vomiting
• Abdominal Pain
• The most common type of diabetic emergency is Hypoglycaemia.
• Hyperglycaemia is not common, as its slow onset allows diabetics to take corrective
measures.
FIRST AID
Hypoglycaemia can occur if a
Both conditions (Hypo and Hyperglycaemia) are
person with diabetes:
managed the same way by first aiders:
• Takes too much insulin
Conscious:
• Fails to eat adequately
• Give sweet drink/ food: 5-7 jelly beans, 2-4
• Over-exercises ie burns off sugar
teaspoons of sugar or honey, glass of fruit juice
faster than normal.
(not diet or low sugar type).
• Becomes ill – viral infection
• Repeat if casualty responds
eg diarrhoea and vomiting.
• On recovery assist with high carbohydrate food - • Experiences great emotional
sandwich, few biscuits, pasta or rice meal.
stress.
if no improvement within a few minutes of The reason sugar is given to
• Call
giving sugar (could be hyperglycaemia or another
diabetics with an altered state of
medical condition).
consciousness is that most will be
Unconscious:
hypoglycaemic. The symptoms
• Place in recovery position
of hypoglycaemia progress more
• Call
rapidly and must be addressed
• DO NOT administer insulin – could be fatal
quickly.
• GIVE NOTHING by mouth
If the casualty is hyperglycaemic,
the small amount of sugar given
by a first aider will not significantly
raise blood sugar levels and will do
no harm.
☎
☎
Fruit Juice
Sugar
Jelly Beans
Don’t give diet or diabetic food/
drink which contains artificial
sweetener – this doesn’t correct low
blood sugar.
Stroke
•The blood supply to part of the brain is disrupted, resulting in damage to brain tissue.
•This is caused by either a blood clot blocking an artery (cerebral thrombosis) or a ruptured
artery inside the brain (cerebral haemorrhage).
•The signs and symptoms of a “stroke” vary, depending on which part of the brain is damaged.
SIGNS & SYMPTOMS
• Confusion or dazed state
• Headache
• Unequal-sized pupils
• Blurred vision
• Drooping of one side of face
• Slurred speech
• Difficulty swallowing - drool
• Weakness or paralysis affecting one
side of body.
• Loss of balance
• Incontinence of bladder/ bowel.
• Seizure
• Unconsciousness
FAST is a simple way of
remembering the signs of a
stroke:
• Facial weakness – Can the
casualty smile? Has their mouth or
eye drooped?
• Arm weakness – Can casualty
raise both arms?
• Speech – Can casualty speak
clearly and understand what you
say?
• Time to act fast - Call
☎
Hyperventilation
FIRST AID
• If casualty fails one of the FAST tests, act
fast and Call
• Assist casualty to adopt position of comfort
• Reassure
• Recovery position if unconscious
• Maintain body temperature
• Give oxygen if trained (Pg 36).
• Monitor Vital Signs (Pg 81)
☎
New drugs and medical procedures can limit or
reduce damage caused by a stroke, however, these
drugs are less effective beyond the first couple of
hours after the event.....therefore Call
FAST.
☎
TIA (Transient Ischaemic Attack) is a mini-stroke
with signs and symptoms lasting < 60mins.
The risk of a stroke subsequent to a TIA is high,
therefore early recognition and treatment is vital.
Cerebral haemorrhage
Cerebral thrombosis
Hyperventilation syndrome is the term used to describe the signs and symptoms resulting
from stress-related or deliberate over-breathing.
The increased depth and rate of breathing upsets the balance
SIGNS & SYMPTOMS
of oxygen and carbon dioxide which results in diverse
• Rapid breathing
symptoms and signs.
NB. Other conditions
• Light-headedness
which may present with
• Tingling in fingers and
rapid breathing:
FIRST AID
toes.
• Asthma attack
• Calm and Reassure.
• Blurred vision
• Encourage slow regular breathing • Heart failure
• Spasms in hands and
• Heart attack
- count breaths aloud.
fingers.
• Collapsed lung
• Seek medical aid – exclude other • Embolus (clot) in lung
• Severe Anxiety
medical condition.
• Chest discomfort
• Diabetes
• DO NOT use a bag for rebreathing. • Some poisons
• Rapid pulse
28 | Medical Emergencies
Heat Exposure
Medical Emergencies | 29
Normal body temp = 37°C
Heat Exhaustion: occurs when the body cannot lose heat fast enough. Profuse
sweating occurs in an effort to lower body temperature but this leads to fluid loss and
decreased blood volume (mild shock). If not treated quickly, it can lead to heat-stroke.
Heat Stroke: occurs when the body’s normal cooling system fails and the body
temperature rises to the point where internal organs (eg brain, heart, kidneys) are damaged:
Blood vessels near the skin’s surface dilate in an attempt to release heat, but the body is
so seriously dehydrated that sweating stops (red, hot, dry skin). Consequently, the body
temperature rises rapidly because the body can no longer cool itself.
This is a life-threatening condition.
Heat Exhaustion
Organs cook at 42°C
(Mild – Moderate Hyperthermia)
• Body Temp 37°C – 40°C
Heat Stroke
(Severe hyperthermia)
SIGNS & SYMPTOMS
• Body Temp > 40°C
• Sweating
• Pale, cold, clammy skin
SIGNS & SYMPTOMS
• Headache
• NO Sweating
• Muscle cramps
• Red, hot, dry skin
• Thirst
• Nausea and vomiting
• Fainting
• Visual disturbances
• Nausea
• Irritability/ confusion
• Rapid pulse
• Staggering/ unsteady
(Onset of mild shock due to fluid
loss, Pg 14)
Progresses to
Heat radiates from the
body, especially the head
into the surrounding air
• Seizures
• Unconscious
(Sometimes profuse sweating occurs)
FIRST AID
• Move casualty to cool,
shaded, ventilated area.
• Lie flat with legs elevated.
• Loosen and remove excess
clothing.
• Cool by: •fanning •spraying
with water •applying wrapped
ice packs to neck, groin and
armpits •draping wet sheet
over body and fanning.
• Give cool water to drink if
fully conscious.
• Seek medical help or
if in doubt
• Call
☎
Breeze or fan
During breathing, cold air
is inhaled and warm air is
exhaled
Heat is lost through
evaporation (sweat) on
the skin
Heat is
conducted
from the
warm body to
a cold object
Heat Exhaustion and Heat Stroke are
usually caused by over-exertion in hot,
humid conditions with poor fluid intake.
Heat is lost through
convection ie warm
air around the body is
replaced with cold air
- worse on windy days
Body heat can be lost quickly in high, exposed areas.
Frost bite
Cold Exposure
Exposure to cold conditions can lead to hypothermia (generalised cooling of the body) or
frostbite (localised cold injury).
Hypothermia: is a condition where the body temperature drops below 35°C.
• Hypothermia can be mistaken for drunkenness (Pg 59), stroke (Pg 27) or drug abuse (Pg 58).
• Suspect hypothermia when conditions are cold, wet and windy, especially in the young
and elderly or individuals under the influence of alcohol or drugs.
• As the core body temperature drops, so does the metabolic rate which means the cells
require less oxygen. Hypothermia protects the brain from the effects of hypoxia so
resuscitation should be continued until the casualty can be rewarmed in hospital.
MILD Hypothermia
35°– 34°C
• Maximum shivering
• Pale, cool skin, blue lips
• Poor coordination
• Slurred speech
• Apathy and slow thinking
• Irritable or confused
• Memory loss
MODERATE Hypothermia
33°– 30°C
• Shivering ceases
• Muscle rigidity increases
• Consciousness clouded
• Slow breathing hard to
• Slow pulse
detect
• DO NOT re-warm too quickly - can
cause heart arrhythmias.
• DO NOT use radiant heat (eg fire
or electric heater) - re-heats too
quickly.
• DO NOT rub or massage
extremities - dilates blood vessels in
skin so body heat is lost.
• DO NOT give alcohol – dilates
blood vessels in skin and impairs
shivering.
• DO NOT put casualty in hot bath
as monitoring and resuscitation if
needed may be difficult.
Frostbite: is the freezing of body
tissues and occurs in parts exposed to the
cold.
}
SEVERE Hypothermia
<30°C
• Unconscious
• Cardiac arrhythmias
• Pupils fixed and dilated
• Appears dead
• Cardiac arrest
FIRST AID
☎
• Call
• Seek shelter – protect from wind chill (Pg 67).
• Handle gently to avoid heart arrhythmias.
• Keep horizontal to avoid changes in blood
supply to brain.
• Replace wet clothing with dry.
• Wrap in blankets/ sleeping bag or space
blanket and cover head.
• Give warm, sweet drinks if conscious.
IF NOT SHIVERING and help is delayed:
• Apply heat packs to groins, armpits, trunk
and side of neck.
• Body-to-body contact can be used.
IF UNCONSCIOUS:
• DRSABCD (Pg 3) - Check breathing for
30- 45secs as hypothermia slows down
everything.
• If unresponsive and not breathing normally–
commence CPR while re-warming casualty.
SIGNS & SYMPTOMS • White, waxy skin • Skin feels hard • Pain or numbness
FIRST AID
• Seek shelter (Pg 67) • Treat hypothermia before frostbite • Gently remove clothing from
affected area • Rewarm affected area with body heat - place in armpit (rewarming can
be very painful) • DO NOT rub or massage affected area – tiny ice crystals in tissue
may cause more damage • DO NOT use radiant heat • DO NOT break blisters
• NEVER thaw a part if there is any chance of it being re-frozen. Thawing and refreezing
results in far more tissue damage than leaving tissue frozen for a few hours.
30 | Medical Emergencies
Medical Emergencies | 31
Bites/ Stings
(Found in Tropical waters)
Box Jellyfish
LAND
ANIMALS
TYPE
FIRST AID
FATAL
Snakes
Pressure Immobilisation Technique
(PIT) - Pg 31
Funnel web Spiders
Red back spiders/ others
Bees
COLD COMPRESS/ ICE PACK
(PIT if allergic to bite/ sting)
Wasps
Scorpion
Red Back Spider
Ants
TYPE
FATAL
Sea Snakes
Tropics
SEA
CREATURES
FIRST AID
Blue-Ringed Octopus
Cone Shell
Box Jelly Fish
Irukandji Jelly Fish
Pressure Immobilisation Technique
(PIT) - Pg 31
VINEGAR - If vinegar not available rinse with
seawater (not fresh water).
Bluebottles
Fish Stings : Stingray
: Stonefish
HOT WATER - Use cold compress if no pain relief
with hot water
: Bullrouts
Snakes
Funnel web Spider
Irukandji Jellyfish
SIGNS & SYMPTOMS
• Severe immediate skin pain
• Frosted pattern of skin marks
• Collapse
• Cardiac Arrest
(Anti-venom available)
FIRST AID
Bites/ Stings
SIGNS & SYMPTOMS
• Mild sting followed 5-40mins later by:
• Severe generalised pain
• Nausea, vomiting, sweating
• Collapse /Respiratory arrest
(No anti-venom)
☎
• DRSABCD • Remove casualty from water • Call
•Reassure • AVOID rubbing sting
area • Flood sting with VINEGAR for 30 secs • If no vinegar–pick off remnants of tentacles
and rinse with seawater (NOT freshwater) • If no signs of life, commence CPR (Pgs 3-5)
Fish stings: • Sharp barb • Painful wound • Bleeding
• Place wound in hot water
Red Back Spider: • Intense local pain at bite site • Not life-threatening • Apply cold pack
Bee/Wasp stings: • Scrape sting off sideways • Apply cold pack • PIT if allergic to sting
Ant/ Scorpion: • Painful sting • Not life-threatening • Apply cold pack for pain relief
Pressure Immobilisation Technique (PIT): There are only 5 situations for using
PIT (all potentially fatal): 1. Snake
4. Cone shell
2. Funnel web spider
3. Blue-ringed octopus
5. Bee, wasp and ant bites in allergic individuals.
Cone Shell
Blue-Ringed Octopus
SIGNS & SYMPTOMS: similar for all 4 species with death from Respiratory Arrest
within minutes to hours.
• Painless bite • Droopy eyelids • Blurred vision • Difficulty speaking and swallowing •
Breathing difficulties • Abdominal pain • Nausea and vomiting
• Headache
• Tingling/numbness around mouth • Profuse sweating • Copious salivation • Collapse
FIRST AID
• DRSABCD
• Rest and reassurance.
• Call
• Pressure Immobilisation Technique
• Resuscitation if needed, takes
priority over PIT.
• DO NOT wash bite site (land
animals).
• DO NOT suck venom from a bite.
• DO NOT kill animal – identification
of species is made from venom on
skin.
☎
Snake
BlueRinged
Octopus
Funnel web
Spider
Cone Shell
1.
Apply a pressure
bandage over the bite area
as firmly as a bandage to a
sprain.
• DO NOT wash bite site
• Mark “X” over bite site
(If only one bandage
available: start from
fingers/ toes and wind as
far up limb as possible
covering the bite).
2. Apply a second
3.
Splint the bandaged
limb, including joints either
toes extending upwards
side of bite site.
covering as much of limb as • Rest casualty and limb.
possible.
• Check circulation (Pg 11)
• Bandage over the top of
• DO NOT elevate limb.
jeans/ shirts as undressing • DO NOT remove bandage
causes unnecessary
and splint once it has been
movement.
applied.
• Mark “X” over bite site.
• DO NOT suck venom from
bite site.
bandage from fingers or
PIT - aim of treatment: to slow the lymphatic circulation and spread of venom.
32 | Medical Emergencies
Medical Emergencies | 33
Poisons
A poison is any substance which causes harm to body tissues.
A toxin is a poison made by a living organism (eg animal, plant, micro-organism).
A venom is a toxin which is injected by a fang or sting (eg snake, spider, fish).
13 11 26 - Australian Poisons Information Centre
Free Call, Available 24hrs, Australia wide.
Poisons can be ingested (swallowed), absorbed, inhaled or injected. The effect of a poison
will vary depending on what the substance actually is and how much has been absorbed.
Ingested:
Swallowed substances can be broadly categorised into ‘corrosive’ or ‘non-corrosive’.
Corrosive: Burning substances eg dish washer detergents, caustics, toilet/ bathroom
cleaners and pertoleums.
Non-Corrosive: Non-burning substances eg medications (tablets/ liquids) and some plants.
SIGNS & SYMPTOMS of a corrosive
substance: •pain in the mouth/
abdomen •Burns to lips/ mouth •Nausea/
vomiting •Tight chest •Difficulty breathing
•Sweating •Unconscious
• If rescue breathing is required, wipe away
any contamination from around the mouth.
• Use a resuscitation mask if available.
• DO NOT use Syrup of Ipecec to induce
vomiting unless advised by Poisons
Information Centre.
Absorbed:
Chemical splash from eg pesticide, weed killer.
FIRST AID
• Identify type and quantity of poison
(from container/ bottle).
• Establish the time of poisoning.
• DO NOT induce vomiting.
• DO NOT give anything by mouth.
FOR ALL POISONING:
• DRSABCD
• What? When? How Much?
• Call Poisons Information Centre for advice
or Call
• Monitor Vital Signs (Pg 81)
• Send any containers and/ or suicide notes
with casualty to hospital.
• Send any vomit with casualty to hospital.
☎
FIRST AID
Allergy/ Anaphylaxis Anaphylaxis is a life-threatening allergic reaction
which can be triggered by nuts (especially peanuts), insect stings (bee, wasp, ant),
shellfish, latex products and certain drugs (eg Penicillin).
The airways rapidly swell and constrict, interfering with breathing, and the blood vessels
widen, leading to shock (Pg 14). Casualties need an immediate injection of adrenaline.
People who know they are at risk may wear a medical alert bracelet and carry their own
injectable adrenaline.
FIRST AID
• Assist casualty to position of comfort.
SIGNS & SYMPTOMS
• Call
Mild to moderate Allergic
• If bite/sting is the cause - flick off sting and apply
reaction:
Pressure Immobilization Technique (Pg 31).
• Swelling of lips, face, eyes
• Follow casualty’s Action Plan for Anaphylaxis.
• Hives or rash (red, itchy)
• Give EpiPen/ Anapen.
• Metallic taste in mouth
• Record time EpiPen/ Anapen was given.
• Dizziness and Weakness
• Give another Epipen/Anapen if no response after 5
• Rapid pulse
mins • Administer oxygen if trained (Pg 36).
• Nausea
• Collapse or unconsciousness - DRSABCD (Pg 3).
• Abdominal cramps
NB - Rescue Breaths require more force due to narrowed airways.
☎
Severe Allergic Reaction
(Anaphylaxis):
• Swelling of throat, tongue
• Difficulty swallowing
• Noisy breathing (stridor)
• Wheezing
• Difficulty talking/ hoarseness
• Pale and floppy (young child)
• Collapse or unconsciousness
1.
Use EpiPen or Anapen when symptoms become severe.
EpiPen and Anapen are pre-loaded auto-injecting pens
containing a measured dose of adrenaline (Epinephrine).
It can take 5- 20 mins for a mild allergic reaction to
escalate to anaphylaxis.
Hives
How to Use an Anapen:
(See also Pg 47)
Toxic fumes from gas, burning solids or liquids. Inhaled poisons include: carbon monoxide
(car exhausts); methane (mines, sewers); chlorine (pool chemicals, cleaning products);
fumes from paints, glues, and industrial chemicals. FIRST AID
• Move casualty to fresh air
SIGNS & SYMPTOMS
• Loosen tight clothing
• Breathing problems • Headache
• Give oxygen if trained (Pg 36)
• Nausea • Dizziness • Confusion
• Call
Injected:
As a result of a bite or sting (Pg 30, 31) or may be injected with a needle.
The most common type of drug overdose via injection are narcotics (Pg 58) which cause
respiratory depression (slow breathing), respiratory arrest (no breathing) or unconsciousness.
The most common injection sites are: hands, feet, crease of elbow, between toes and fingers
NB. Narcotic users may be carriers of Hepatitis B, C, and/ or HIV (AIDS).
☎
How to Use an EpiPen:
2.
• DO NOT become contaminated yourself – wear gloves, goggles, protective clothing.
• In a workplace, call 13 11 26 and refer to MSDS (Pg 60) to describe poison.
• Ask casualty to remove all contaminated clothing.
• Flood affected area with running water • Seek medical advice.
Inhaled:
Swelling
1.
Pull off Black needle
shield.
Pull off grey safety cap
from red button.
3.
4.
Place needle end firmly
against outer mid-thigh
(with or without clothing).
Press red button so it
clicks and hold for 10secs.
Remove Anapen and
massage injection site for
10secs.
BEWARE of needle protruding from end after use.
Form fist around
EpiPen and pull off
grey safety cap.
3.
2.
Place black end against
outer mid-thigh. (with or
without clothing).
4.
Push down hard until a click Remove EpiPen and
is heard or felt and hold in
massage injection site
place for 10secs.
for 10secs.
DO NOT remove grey cap until ready to use.
BEWARE of needle protruding from black end after use.
34 | Advanced Resuscitation
Advanced Resuscitation | 35
Oxygen Equipment - Storage & Handling
• Medical oxygen is compressed gas which is stored in a white coloured, metal cylinder.
• Oxygen cylinders should be stored in a cool, ventilated place and secured either standing
or lying flat • Empty cylinders should be stored in a clearly marked place separate from full
ones • DO NOT drag, drop or roll cylinders • Oil or grease (combustible materials) must not
come in contact with oxygen equipment • No smoking or sources of ignition when using
oxygen.
Plastic seal
denotes full cylinder
Cylinder key - turn anticlockwise to
OPEN (on), clockwise to CLOSE (off)
Heat tag - if
distorted do
not use
Outlet valve - face outlet valve away
from people before opening - high
pressure gas can cause injury.
Place hand under plastic tags
when opening (cracking) cylinder.
‘Cracking’ purges dust from outlet
valve before fitting regulator.
‘C’ sized cylinder is 490 litres.
A full ‘C’ sized cylinder lasts
1 hour @ 8lpm flow rate.
Fitting the Regulator:
Oxygen Equipment - Care & Maintenance
•Never use oil or fat-based soaps on any oxygen equipment - grease/ oil is combustible.
•Never seal oxygen cylinder outlet valve with adhesive tape - glue is petroleum based.
•Never allow cylinder to run empty as moisture and contaminants may enter.
•If cylinder is emptied, turn off valve immediately.
•Use reputable gas suppliers for refills.
•Disposable items should be thrown away after use and replaced with new ones.
•Masks and other parts should be checked for wear, cleaned and disinfected and dried
before packing.
•Follow specific cleaning instructions provided with equipment - check which chemicals are
effective and compatible with particular pieces of equipment.
•Any missing items should be noted and replaced.
•Tubing should be coiled to prevent from kinking.
•Soft masks have a tendency to distort if squashed during
storage - pack carefully.
•Check contents of cylinder and functioning of equipment
regularly - eg after each use and/ or at start of each shift.
•Oxygen units should be inspected and serviced by an
appropriate trained technician as specified by manufacturer.
‘Cracking’ Cylinder
• Check hands are clean and free of grease/ oil.
• Ensure area is ventilated and there is no ignition sources.
• Remove plastic seal from cylinder neck.
• Purge outlet valve by quickly opening and closing cylinder (cracking) - see above.
• Check regulator is dust and grease free and that ‘O’ ring is seated and not damaged.
• Place regulator over cylinder neck ensuring index pins and index holes are in place.
• Secure regulator in place by tightening ‘T’ piece - not too tight.
• Set flow meter to low - this reduces pressure in regulator when cylinder is opened.
• OPEN cylinder by turning cylinder key anticlockwise.
• Turn flow meter OFF and listen for leaks.
• Check pressure gauge - 16,000kpa (2300 psi) indicates cylinder full.
• CLOSE cylinder and adjust for leaks if necessary.
• If not using immediately, depressurize system - close valve, open flow meter.
• Leave regulator attached and store ready for use with all valves off.
Pressure Gauge
‘T’ piece
(don’t use if cylinder is less
Regulator
Oxygen nipple
than 1/4 full as flow rate is
(attach tubing)
Safety Pin Index
coupling system for
‘C’ sized cylinder - the
index pins on the
cylinder correspond to
the index pins on the
regulator.
‘T’ piece
Flow meter
Cylinder neck
‘O’ ring (Bodok seal) - if damaged or not seated
properly, may cause leaks - keep spares.
not accurate)
Regulator
(reduces cylinder pressure
to a usable pressure)
When to use Oxygen
Oxygen can be given in high or low
concentration in all conditions associated
with hypoxia (see below). Hypoxia is a lack
of oxygen in the body’s tissues which can be
caused by many conditions - generalized (eg
asthma) or local (eg crushed limb).
Oxygen administration will benefit
the following conditions:
• Respiratory distress/ Asthma (Pg 23)
• Heart attack/ Angina (Pg 22)
• Anaphylaxis (Pg 33)
• Bleeding & shock (Pgs 12,14)
• Drowning & diving emergencies (Pgs 7, 52)
• Head & spinal injury (Pgs 20, 21)
• Crush injury & fractures (Pgs 11, 14)
• Burns (Pg 15)
• Smoke/ fume inhalation (Pg 15, 47)
• Drug overdose/misuse (Pg 58)
• Poisoning (Pg 32)
• Unconsciousness (Pg 2)
• Resuscitation (Pg 37)
NB. There are no absolute contra-indications
to oxygen therapy (Pg 36). However, in COAD
(Chronic Obstructive Airways Disease) low
oxygen concentrations should be used.
RESPIRATORY DISTRESS
SIGNS & SYMPTOMS
Mild:
• Dry cough
• Noisy breathing
• Wheeze – during exhalation
• Breathless but speaks in sentences
Moderate:
• Wheeze - during exhalation and inhalation
• Rapid breathing
• Breathless - speaks in phrases
• Anxious
• Pale and sweaty
• Rapid pulse
Severe:
• Can’t speak (too breathless)
• Wheeze inaudible (no air movement)
• Cyanosis (blue lips)
• Flared nostrils
• Intercostal recession
• Use of accessory muscles
• Exhaustion
• Distressed
• Confusion or aggressive behaviour
• Altered state of consciousness
• Collapse - Respiratory arrest
36 | Advanced Resuscitation
Advanced Resuscitation | 37
Oxygen Therapy
Oxygen administration to a breathing casualty - conscious or unconscious.
A conscious casualty with breathing difficulty (eg asthma or heart attack) usually finds it
easier to breathe while sitting or semi-reclined. However, a casualty with shock (Pg 14) or
decompression illness from scuba diving (Pg 52), is positioned horizontally. Administer oxygen
(O2) to an unconscious, breathing casualty in the recovery position.
Conscious Casualty:
• Reassure • Position casualty appropriately • Explain what
you are doing • Explain that oxygen will help • Turn on
oxygen supply • Select appropriate oxygen delivery device
and follow steps:
Unconscious, Breathing Casualty
Oxygen Delivery Devices:
1) Standard Therapy Mask - Low to Medium % O2
•Connect oxygen tubing to mask and oxygen outlet.
•Open flow meter and check oxygen is flowing.
•Set flow rate to 8lpm - adjust as necessary.
•Position mask over mouth and nose with narrow end
upwards and metal band over bridge of nose.
•Pass elastic strap over casualty’s head & adjust strap.
•Squeeze metal band over nose - this prevents oxygen
blowing into casualty’s eyes.
Some casualties won’t tolerate a mask - allow
•Ask casualty to breath normally and observe.
casualty to hold mask near face.
2) Non-Rebreathing Mask
High % O2
•Similar to standard therapy mask
but has a reservoir bag.
•Set flow rate to 15lpm.
•Ensure reservoir bag is inflated
before fitting mask.
•Fit as standard mask (above).
Oxygen
Delivery Device
Oxygen Resuscitation
Oxygen administration to an unconscious non-breathing casualty.
Rescue breaths can be supplemented with oxygen (O2) during CPR (oxygen resuscitation).
For inexperienced rescuers, mouth to mask rescue breathing is the preferred method. It
delivers 50-70% oxygen and ventilations are performed more effectively than bag-valvemask or manual triggering devices. With all oxygen resuscitation devices, inflate until the
chest begins to rise. Over inflation will cause stomach distension and regurgitation.
Oxygen
Delivery Device
Flow
Rate
% O2
Resuscitation
Mask (no O2)
exp
air
16%
Resuscitation
Mask (with O2)
15
70%
Bag Valve Mask
(no O2)
room
air
21%
Bag Valve Mask
(O2, no resevoir)
15
45%
Bag Valve Mask
(O2 plus resevoir)
15
100%
Manually triggered
Resuscitator
_
100%
Resuscitation (Pocket) Mask:
Mouth to Mask (Pocket)
with O2
•If resuscitation mask is without
an oxygen nipple, place oxygen
tubing under the cuff of the mask.
•Set flow rate: 8-15lpm.
•Press mask firmly to face
forming a good seal while
maintaining head tilt.
•Inflate by blowing through valve
until chest begins to rise.
Flow % O2
Rate
Standard
Therapy Mask
8
50%
Non-Rebreathing
Mask
15
95%
Nasal Cannula
4
30%
Demand Valve
-
100%
4) Demand Valve - 100% O2
•Attach mask to demand
3) Nasal Cannula - Low % O2
valve and test if working.
•Connect oxygen tubing to
•Position mask over mouth
prongs and oxygen outlet valve.
and nose.
•Open and set flow meter at
•Press firmly to get a good
1-4lpm - higher rates dry the
seal.
nostrils.
•Ask casualty to breath
•Insert tips of prongs into nostrils.
deeply and listen for
•Hook tubing around casualty’s
a click as valve is
ears and tighten.
triggered.
•Ask casualty to breath normally.
•Sick,
distressed casualties have difficulty
If oxygen is in short supply and emergency services a long
way off, use a lower flow rate. This does not apply to scuba triggering the valve - use a constant flow
divers suffering from decompression illness (Pg 52).
device instead which offers little resistance.
BVM with O2, plus reservoir,
one operator
Manually Triggered Resuscitator
Manually Triggered Resuscitator:
•Delivers positive pressure by the
touch of a trigger.
•Delivers 100% O2.
•Reduces operator fatigue
•Dependant on an oxygen. supply
and become useless once supply is
depleted.
•The high flow rates can easily
cause stomach inflation and
regurgitation.
•If the safety valve is not functioning
or used on a small person, lung
damage can occur due to overinflation.
BVM with O2, plus reservoir,
two operators
Bag-Valve-Mask (BVM): Where difficulty with BVM
resuscitation is experienced, two trained operators may
be required - the first to manage the airway, the second to
operate the bag.
•Assemble the unit and squeeze the resuscitation bag to
check the function of the valves.
•Ensure oxygen tubing is attached to BVM and outlet
valve on oxygen cylinder.
•Turn on O2 supply • Set flow rate: 8-15l/min
When equipment is ready:
•Position mask over mouth & nose, ensuring a good seal.
•Take a position behind the casualty’s head and open
airway using head tilt and jaw thrust while holding mask to
casualty’s face.
•Deliver oxygenated rescue breaths by squeezing bag
until chest begins to rise
•Monitor casualty • Monitor oxygen supply.
OP airways (Pg 38) can be used with resuscitation masks, bag-valve-masks
and manually triggered devices to assist airway management.
38 | Advanced Resuscitation
Advanced Resuscitation | 39
Oropharyngeal Airways (OPs)
•Oropharyngeal airways (Guedel airways) may be necessary to maintain an open airway
when using mouth to mask or bag-valve-mask ventilation.
•An OP airway DOES NOT remove the need for head tilt or the recovery position.
•It DOES NOT prevent suffocation by fluids or the closing of the glottis. But it does facilitate
CPR by holding the tongue forward in casualties with a thick tongue.
•OP airways must only be used on unconscious casualties who do not have a gag reflex.
The main risks of its use are:
•If the casualty has a gag reflex, they may vomit.
•When it’s too large, it can close the glottis and thus close the airway.
•Improper sizing can cause trauma to the throat and bleeding in the airway.
Flange
Sizing an OP Airway:
Suction Equipment:
Suction units are powered by oxygen, air, battery, hand, foot or electricity.
Yankauer Suction Catheter
Catheter tip
Finger port (air vent)
can be sealed and
unsealed by operators
finger to control suction
Suction catheter
Bite Block
Collection bottle
Squeeze handle
to create vaccum
Ear
Lobe
Hand Operated
Suction Unit
Suction tubing
2 methods for sizing OP airway
Inserting an OP Airway:
•Ensure casualty is unresponsive.
•Clear airway using postural drainage, finger sweep and/ or suction.
•Position casualty on their back.
•Select correct size OP airway (above).
•If lubrication is necessary, use water, casualty’s saliva or KY jelly.
•Open casualty’s mouth using finger and thumb scissor motion.
•Apply head tilt and/or jaw thrust (Pgs 4, 40).
•Insert OP airway by following steps 1, 2, 3:
Scissor motion for opening mouth
2
• Point tip of OP airway toward • When tip reaches back
the roof of casualty’s mouth.
of throat, rotate airway 180
Slide the airway towards back degrees.
of throat.
NB. If casualty starts to regain consciousness, cough,
gag or vomit, remove OP airway immediately.
Removing an OP Airway:
•Suction helps maintain a clear airway by aspirating saliva, blood, mucus and vomit.
•Suction does not remove the need for postural drainage and finger sweep to remove solid
matter or viscous mucus.
•Fluids and solids must be removed before and during resuscitation to maintain a clear airway.
Angle of
Jaw
•OP airways come in different sizes.
•To select the appropriate size, place OP airway
on casualty’s outside cheek and measure from:
•1) Centre of lips to angle of jaw or 2) Corner of
mouth to bottom tip of ear lobe (see diagram).
•The correct size keeps the tongue forward and
maintains an open airway.
1
Suction
Pull out following curvature of the tongue - no rotation necessary.
Dispose of in biohazard bag (Pg 63) as it is a single use item.
3
• Advance the airway until the
flange rests on the casualty’s
lips and the bite block is
between teeth.
• Ensure lower lip is not
pinched between teeth and OP
airway.
• Check breathing - look, listen,
feel.
• Maintain head tilt and jaw
support.
Battery Powered
Suction Unit
Suction Method:
Oxygen Powered
Suction Unit - use sparingly
as depletes oxygen supply
•Position casualty on side if possible, or leave on back and turn casualty’s head to the side.
•Open casualty’s mouth and wipe away any large debris with gloved fingers.
•Measure the suction catheter from corner of casualty’s mouth to earlobe. This gives the
correct depth to insert the end of the suction tip (no further than back teeth).
•Turn on the suction device and place suction tip in lower inside cheek.
•If using a Yankauer suction catheter, generate suction by occluding air vent with finger.
•Sweep catheter across lower cheek and aspirate for a maximum of 5 secs.
•Withdraw catheter slowly from casualty’s mouth while still aspirating.
•Flush line with water (place catheter tip in bowl of water and suck up)
•Ensure suction bottle does not fill beyond 2/3 full. Empty if necessary..
•Turn off immediately after use.
Note:
Failure of Suction Equipment:
•Inserting a suction catheter into
Test suction by placing a finger over the end of tubing
the throat beyond the back teeth
(without catheter attached) and turn on - there should
may cause gagging & vomiting.
be enough suction to hold your finger in place.
•Suction must be timed so it does
not interfere with the casualty’s
If suction is not working check:
spontaneous breathing or
•Suction unit is turned on.
ventilations.
•Lid of collection bottle is tight.
•The seal inside collection bottle is in place and in good condition.
•No cracks in collection bottle or not more that 2/3 full.
•Suction tubing is not blocked or kinked.
•In oxygen powered units check that oxygen supply is not exhausted.
40 | Advanced Resuscitation
Advanced Resuscitation | 41
The jaw thrust method is used to open the airway with minimal neck movement on
casualties with suspected spinal injury. The simplest way of ensuring an open airway in an
unconscious casualty is to use the head tilt, chin lift technique (Pg 4).
REMEMBER: Airway management takes priority over spinal injury.
Jaw Thrust Method:
• Kneel at top of casualty’s head.
• Rest your elbows on the surface where casualty is lying.
• Place one hand on each side of casualty’s
lower jaw, below the ears (angle of jaw).
• Use your index and middle fingers to push
the jaw forward away from chest.
• Use your thumbs to retract lower lip to keep
casualty’s mouth open if necessary.
• Slight head tilt may be necessary to
Opening Airway Using Jaw Thrust Method
maintain airway patency.
Normal Heart Function
Natural
Pacemaker
•Electrical impulses generated
within the heart from a natural
pacemaker, coordinate contraction
and pumping of the heart.
Normal Sinus Rhythm
•These elecrical impulses can be
recorded by an ECG (Electrocardiograph).
•A normal functioning heart shows sinus rhythm on an ECG.
• AEDs (Automated External Defibrillators) have an inbuilt ECG
monitor which analyses the heart rhythm and determines if
shock is required.
Defibrillation & AEDs
Defibrillation consists of delivering a therapeutic dose
of electrical energy to the heart with a device called a
defibrillator.
A defibrillator depolarizes the heart muscle, terminates the
abnormal rhythm, and allows normal sinus rhythm to be reestablished by the heart’s natural pacemaker (Pg 40).
The delay to defibrillate is the most important factor in
determining survival from cardiac arrest. For every minute
without defibrillation, survival declines by 10% ie 50% survival
after 5 mins delay.
% Survival
Jaw Thrust
Time to Defibrillate (mins)
Automated External Defibrillators (AEDs), are simple-to-use units designed to
analyse the heart rhythm and inform the user if a shock is advised.
Preparation of Casualty:
1) Expose chest - cut clothing.
2) Remove any medication patch or jewelry.
3) Wipe chest dry, remove chest hair with razor.
AED
Pad Position
AED Set-Up and Operation:
Left
Atrium
LA
RA
Left
Ventricle
LV
RV
Abnormal Heart Rhythms
Electrical
Impulse
• During cardiac arrest, ECGs will detect abnormal elecrical activity (heart rhythms).
• The following 3 heart rhythms are associated with cardiac arrest:
Ventricular Fibrillation (VF):
• VF is the most common rhythm in cardiac arrest.
• The heart quivers but doesn’t pump.
• VF lasts a few minutes before all electrical activity ceases (asystole).
• VF is a shockable rhythm - asystole is not (see below).
Ventricular Tachycardia (VT):
• The heart beats too fast to pump effectively (pulseless VT).
• VT may progress to VF then asystole.
• VT is a shockable rhythm.
Asystole (flat line):
• Asystole is a non-shockable heart rhythm.
• All electrical activity has ceased and survival is unlikely.
AEDs only shock two rhythms - VF and VT (not asystole)
1) Turn it ON.
2) Attach AED Pads - peel backing off first.
3) Follow voice prompts.
AED Voice Prompts:
•If voice prompt advises ‘check electrodes’ you should check:
1) Pads are sticking properly to chest (wipe chest dry/ remove chest hair).
2) Pad connection cable is plugged in and pads are positioned correctly.
•If voice prompt advises ‘shock now’ ensure nobody is touching the casualty when the
shock is delivered. SHOUT ‘stand clear’, then press shock button.
•If voice prompt says ‘no shock advised’, check responsiveness/ breathing and follow voice prompts.
Children and AEDs:
•Standard adult AEDs and pads are suitable for the use in children older than 8 years.
•Ideally, for children between 1 and 8 years, paediatric pads and an AED with a paediatric
capability should be used.
•Pads should be placed in the same way as an adult (See illustration above, AED Pad Position).
•If an AED does not have a paediatric mode or paediatric pads then the standard adult AED
and pads can be used.
•Ensure the pads do not touch each other on the child’s chest. This may require one pad to be
placed on the centre of the chest and the other on the back of chest between shoulder blades.
Note:
•AEDs should only be used on unresponsive, non-breathing casualties.
•An AED can and should be used on pregnant casualties.
•In large-breasted individuals, place the left electrode pad lateral to or underneath the left breast.
•If the casualty has an artificial, implanted pacemaker, a scar and raised area will be seen just below
the left or right collar bone. Position AED pads 8cms from the pacemaker unit and proceed as usual.
•An AED analyses the heart rhythm every 2 mins and continues for up to 5 hrs or 150 shocks depending on
make, model and battery life of AED. DO NOT bump casualty while AED is analysing rhythm.
•AED batteries and pads have expiry dates.
•AED packs should include: razor, scissors, hand towel, spare pads, gloves and face shield.
•AEDs conduct automatic internal checks and provide visual indicators that the unit is ready and
functioning properly - no need to turn on daily - follow manufacturer guidelines.
42 | Advanced Resuscitation
Cardiac Arrest
Advanced Resuscitation | 43
(See also Pg 22)
• In cardiac arrest the heart stops beating and pumping properly resulting in cessation of
normal blood circulation (no pulse) • Arrested blood circulation prevents delivery of oxygen
to the body • Lack of oxygen to the brain causes unconsciousness and absence of breathing
(respiratory arrest) • This is a medical emergency which if treated early is potentially reversible
• Treatment involves CPR to provide circulatory support, followed by defibrillaton if a shockable
rhythm is present • If a shockable rhythm is not present after CPR and other interventions,
survival is unlikely.
Causes of Cardiac Arrest:
• Heart attack (blocked coronary artery) - 70% of all cardiac arrests.
• Massive blood Loss • Drug overdose • Drowning • Pulmonary embolus (clot in lung).
• Electric shock • Anaphylaxis • Airway obstruction (choking, severe asthma).
Chain of Survival
(See also Pg 5)
Defibrillation is NOT a standalone treatment for
cardiac arrest. All links in the ‘Chain of Survival’
must be in place to increase survival. Time is
the essence. The 4 steps in the chain of survival
are: 1) Early Access 2) Early CPR 3) Early
defibrillation 4) Early advanced life support
Advanced Resuscitation Techniques
Advanced Resuscitation Techniques
Two Operators:
• If two rescuers are available, one rescuer commences CPR while the other:
1) Calls
2) Retrieves the AED.
3) Retrieves oxygen equipment.
• Minimise interruption to CPR (Pg 4,5) while the second person sets up and attaches AED
pads to casualty’s chest.
• While AED analyses the heart rhythm (takes 10-20 secs), CPR is stopped and oxygen
resuscitation equipment is set up (Pg 8,11).
• One rescuer takes up position above the casualty’s head and is responsible for managing
the airway and forming a good seal with the resuscitation mask.
• The second rescuer is positioned at the side of the casualty and performs chest
compressions, rescue breaths (squeezes the bag) and operates the AED.
•Follow AED voice prompts (Pg 41).
•Rescuers swap roles after 5 cycles of CPR (2 mins) to avoid fatigue.
• Continue until:
1) Casualty responds or begins breathing normally.
2) Rescuers become exhausted.
3) Health professional arrives and takes over.
4) Health professional directs that CPR be ceased.
☎
1
Single Operator:
• If there is one rescuer and an AED is immediately available, set up AED (Pg 41) before
commencing CPR (Pg 4,5)
• While waiting for the AED to analyse the heart rhythm, set up oxygen equipment (Pgs 34, 37)
and position yourself above the casualty’s head.
and place on loud speaker.
• If you have a mobile phone, call
• Follow AED voice prompts (Pg 41).
• Perform chest compressions and oxygen resuscitation from above casualty’s head.
• Continue until: 1) Casualty responds or begins breathing normally 2) Rescuer becomes
exhausted 3) Health professional arrives and takes over 4) Health professional directs that
CPR be ceased.
2
3
☎
1
2
3
If casualty regains consciousness:
• Roll casualty into recovery position.
• Administer oxygen via standard face mask.
• Turn off AED.
• Keep AED pads attached to chest in case casualty
relapses into cardiac arrest.
• Monitor and reassure casualty.
Note:
Recovery Position with
Oxygen & AED
•Rescuers must communicate with each other to keep the resuscitation process flowing.
•It is vitally important that CPR is not interrupted while the AED and oxygen is set up.
•Resuers should use the 10-20 sec window while AED analyses heart rhythm to swap roles and
re-organise.
44 | Low Voltage Rescue
Low Voltage Rescue | 45
What is Electric Shock?
What is Arc Flash?
An electric shock can occur upon contact
of a human's body with any source of
voltage high enough to cause sufficient
current through the muscles or hair.
Arc Flash is a short circuit that flashes from one exposed
live conductor to another, or to the ground.
● Death caused by an electric
shock is referred to as electrocution.
● The greater the current, the
greater the shock!
● The severity of electric shock
depends on voltage, amperage, and
resistance.
Always test a circuit to make sure it is
de-energized before working on it.
Power drills use 30 times
more power than will kill!
What can Electric Shock do to me?
LOW VOLTAGE = less than 1000V AC or 1500 V DC
LOW VOLTAGE DOES NOT MEAN LOW HAZARD!
The Arc Flash produces intense:
● Heat (> 5000 degrees causing severe burns)
● Light (The same light radiation as welders)
● Pressure wave (blast) equivalent to several sticks of
dynamite and can break bones and cause internal organ
damage.
● Arc Flash can result from inserting a tool in the wrong place or dropping a tool into a circuit
breaker or service area.
● 80% of all injuries and fatalities caused by electrical incidents are caused by Arc Flash……
not electric shock!
What is Flash Burn?
Flash Burn also known as Arc Flash, Arc Eye or Welder’s Flash, is a burn sustained from an
electric arc either by the extreme heat it produces or through UV radiation.
SIGNS & SYMPTOMS
Effects of Electrical Current on the Body (Less than 600 Volts)
•Minor Flash burn to the eyes becomes painful and ‘gritty’ about
2-3hrs after the event.
Current
Reaction
1 milliamp
Just a faint tingle
FIRST AID
5 milliamps
Slight shock felt. Disturbing, but not painful. Most people can “let go.”
6-25 milliamps (women) Painful shock. Muscular control is lost. This is the range where
9-30 milliamps (men)
“freezing currents” start. It may not be possible to “let go.”
50-150 milliamps
Extremely painful shock, respiratory arrest (breathing stops), severe
muscle contractions. Flexor muscles may cause holding on; extensor
muscles may cause intense pushing away. Death is possible.
1,000-4,300 milliamps
(1-4.3 amps)
Ventricular fibrillation (heart pumping action not rhythmic) occurs.
Muscles contract; nerve damage occurs. Death is likely.
10,000 milliamps
(10 amps)
Cardiac arrest and severe burns occur. Death is probable.
15,000 milliamps
(15 amps)
Lowest overcurrent at which a typical fuse or circuit breaker opens a
circuit!
What type of injuries follow Electrical Accidents?
● Cardiac Arrest ● Respiratory arrest ● Burns/ Tissue damage
Electrical Burns cause Massive Tissue Damage:
This worker fell and grabbed a powerline to catch himself.
The resulting electric shock mummified his first two fingers,
which had to be removed.
The acute angle of the wrist was caused by burning of the
tendons, which contracted, drawing the hand with them.
Generally flash burns resolve within 36 hrs.
Minor Flash Burn to Eyes
Seek urgent medical help if any of the following occurs:
(This is common when welding • Blurred vision • Vision changes • Seeing spots or flashes of light
without protective eyewear). • Pain on moving eyes • Worsening pain • Casualty concerned about eyes
This man was near a
power box when an
electrical explosion
occurred. He did
not touch the box,
but electricity arced
through the air and
entered his body.
The current was
drawn to his armpits
because perspiration
is very conductive.
This is severe flash
burn caused by an Arc
Flash. The explosion
caused airway burns and
embedded molten copper
into the casualty’s eyes,
resulting in permanent
blindness.
FIRST AID
☎
• Apply burns dressing
• Move to safety • Call
• For airway burns - see below
What is Airway Burn?
Smoke, steam, superheated air or toxic fumes
from Arc Flash explosions can cause severe
damage to the airways resulting in swelling and
possible airway obstruction.
•Look for evidence of inhalation injury around
nose or face (see photo above).
•Coughing or hoarseness may indicate exposure.
FIRST AID
•DO NOT enter a burning or toxic
atmosphere without appropriate protection
•Remove to a safe, ventilated area ASAP
•Give oxygen if trained (Pg 36)
•Call
☎
46 | Low Voltage Rescue
Low Voltage Rescue | 47
What is an Electrical Burn?
High resistance of the skin transforms electrical energy into heat energy, producing burns.
Electrical burns are often associated with an entry and exit point and are usually more
severe than they appear due to massive internal tissue damage.
Entry Wound:
The dark dot in the
centre of wound is
a burn at the entry
point.
This man was
lucky - the current
narrowly missed his
spinal cord.
FIRST AID • Move to safety • Call
☎
Exit Wound:
Current flows through the
body from the entry point,
until finally exiting where the
body is closest to the ground.
This foot suffered massive
internal injuries, which weren’t
readily visible, and had to be
amputated a few days later.
• Apply burns dressing
What are the consequences of an Electrical Burn?
This worker was zapped by a
tool he was holding. The entry
wound and thermal burns from the
overheated tool are apparent.
To prevent damage to the nerves and blood vessels,
the pressure was relieved by cutting open the skin
on the arm.
How do I handle Electrical Fires?
To extinguish an electrical fire you can use a fire blanket or two
types of fire extinguisher - carbon dioxide or dry chemical:
☎
•Product of incomplete
combustion.
•Colourless, odourless,
tasteless gas
•Forms an explosive mixture
SIGNS & SYMPTOMS
• Collapse • Drowsiness
• Confusion • Pink lips and
skin • Headache • Dizziness
•Product of burning PVC
•Pungent, acrid gas which
forms hydrochloric acid when
in contact with water
SIGNS & SYMPTOMS
• Burning sensation in
airways • Stinging eyes
• Coughing • Breathing
difficulties
FIRST AID
•Product of burning some
plastics (not PVC), wool and
polyurethane
•May notice an ‘almond’
smell
SIGNS & SYMPTOMS
• Light headed • Dizzy
• Breathing difficulties
• Collapse • Flushed • Blue
extremities • Convulsions
☎
• Move to ventilated area • Get Help - Call
• Administer Oxygen (Pg 36) • Prepare to give CPR (Pgs 2-5)
What is a Low Voltage Rescue Kit?
Same hand a few days
later, when massive
subcutaneous tissue
damage caused severe
swelling (swelling usually
peaks 24-72 hours after
electrical shock).
To use a fire blanket on a burning casualty:
● Pull the tabs to release the blanket from its container.
● Shake it open, hold an edge and cover your hands.
● STOP, DROP, COVER, ROLL
● Wrap blanket around to smother flames.
● Start at the head - work down to the feet.
● BEWARE – of your clothes igniting.
FIRST AID • Move to safety • Call
• Apply burns dressing
What Poisonous Gases are released in electrical fires?
Carbon Monoxide Hydrogen Chloride Hydrogen Cyanide
It’s a kit which contains 6 essential tools to assist in a
Low Voltage Emergency Rescue.
Your life could depend on a complete kit!
● Insulated gloves - test for holes by inflating with air
● Insulated crook - check for cracks or splits
● Non-conductive torch - carry spare batteries
● Fire blanket
● Burns dressing
● Isolation Tag
Check LVR kit before starting a
job and certify every 6 months.
How do I perform Low Voltage Rescue?
1 YELL for Response!
2
Check for DANGER
3
Put on Gloves
4
5
Move to Safety
6
DRSABCD
Carbon Dioxide Dry Chemical
(black band)
(white band)
STOP, DROP, COVER, ROLL
Break Connection
OR
OPEN
ISOLATOR
Crook
48 | Advanced First Aid
Advanced First Aid | 49
Cervical Collars
•A cervical collar helps immobilise the neck when cervical spinal injury is suspected (Pg 21).
•Cervical collars do not provide complete spinal support - head blocks, head straps and/ or
manual handling is required to stabilse casualty on a spinal board.
•It requires two trained first aiders to apply a cervical collar correctly:
Rescuer 1 supports the head and
neck while Rescuer 2 assesses
collar size and adjusts collar
to fit. (Follow manufacture’s
guidelines).
Velcro strap
Rescuer 2 fits the collar by
bending to shape, then sliding the
velcro end behind casualty’s neck.
Position chin piece and faster
velcro strap.
Chin piece
Rescuer 2 secures collar with
velco tab. Ensure collar is firm and
comfortable, adjust if necessary.
Rescuer 1 maintains head and
neck support during all adjustments
Size adjuster
Velcro
strap
Chin piece
Adjustable Cervical Collar
If a casualty with suspected spinal injury must be moved, follow these
guidelines:
•Immobilise the lower limbs by applying a figure of 8 triangular bandage, around the feet (Pg 11).
•Secure casualty’s hands.
•A minimum of 6 people are required to perform the lift where possible.
•The person at the head of the casualty is in control of the lift and must ensure that alignment
of the spine is maintained.
Scoop Stretcher
Clamp
together
Wider head end
•A scoop stretcher splits vertically into two and the sections fit around the casualty lying on the
ground. The sections are reconnected and the casualty is lifted.
•Both sides of the casualty must be accessible to use a scoop stretcher.
•Scoop stretchers are length adjustable to fit the height of the casualty.
•Particular attention must be paid to the closure area beneath the casualty so that clothing or
skin is not pinched or trapped.
•Scoop stretchers can be used as a transport device provided the patient is strapped.
•Scoop Stretchers are uncomfortable for the casualty and transfer to a spinal board or vaccum
mattress is preferable - place the scoop stretcher on top of the transport device and unclamp.
Spinal Board
Head Block
A spinal board (backboard) is designed to provide rigid support during
Strap
transport of a casualty with suspected spinal injury.
•A casualty is transferred onto a spinal board using a scoop stretcher (Pg 48)
or the log roll technique (Pg 21).
•Spinal boards are almost always used in conjunction with the following devices:
• Cervical collar (Pg 48)
• Side head supports to minimise lateral rotation of the head (head blocks or roll blanket).
• Straps to secure casualty’s head and body to the board.
•Spinal boards are usually plastic, light weight and are slightly longer
Spinal
and wider than the average human body to accommodate immobilisation
Board
straps and handles for carrying.
•Most spinal boards are buoyant and are X-ray translucent.
•It is advised that no casualty should spend more than 30 mins on a spinal board to avoid
discomfort and pressure sores.
If casualty becomes unconscious and/or vomits/regurgitates while strapped to a spinal board
or vaccum stretcher (below): • Tilt the stretcher onto it’s side to clear airway (postural drainage)
• Assess casualty’s airway and breathing - DRSABCD (Pgs 2-5)
Vaccum Mattress
•The vaccum mattress is used to immobilise and transport casualties with spinal, pelvic or limb
trauma.
•It can be used as a standalone transportation device or placed on top of a stretcher.
•The vaccum mattress consists of a sealed polymer bag filled with
small polystyrene balls and a valve. The mattress is flexible and
moulds to shape but when air is pumped out through the valve, the
polystyrene balls squeeze together forming a rigid structure.
•The conforming nature means that casualties can be
Handle
kept immobilised on it for longer periods of time.
Strap
•It is washable and x-ray translucent.
Valve
•A sheet is usually placed on the inside of the mattress
Vaccum Mattress
for three reasons:
1) To protect the mattress from puncture - the casualty might be wearing sharp jewellery or
have broken glass on their clothing.
2) To reduce sweating - the polymer material is not breathable.
3) To help transfer casualty in the emergency room.
Basket Stretcher
Basket Stretcher
A rigid basket stretcher can be used to transport a casualty across uneven terrain from a
remote location that is inaccessible by ambulance or other vehicle.
If a spinal injury is suspected, the casualty must first be immobilized on a spinal board
(above) then the spinal board placed into the basket stretcher.
Basket stretchers surround and support the casualty yet their design allows water to drain
through holes in the bottom.
Basket stretchers with special ratings can be used for specialised rescues (eg helicopter,
water and technical rope) but rescuers must have special training.
50 | Advanced First Aid
Advanced First Aid | 51
Helmet Removal (See also Pg 21)
Full face helmets should only be removed if the
casualty is unresponsive and the airway cannot
be maintained or resuscitation is required.
Call
☎
Harness Suspension Trauma
If casualty is conscious, leave
helmet in place. Support head
and neck.
Remove helmet ONLY if
casualty becomes
unresponsive and airway
cannot be maintained.
Removing a helmet requires two people:
1 immobilises
1 Rescuer
casualty’s head and neck.
2 continues supporting
4 Rescuer
head and neck while rescuer 1
removes the helmet.
2 removes
2 Rescuer
obstructions ie opens
viser, removes glasses
and unfastens chin strap.
2 carefully
5a Rescuer
lowers the casualty’s
head and neck into the
neutral position.
2 supports casualty’s
3 Rescuer
head & neck by placing a hand
behind neck and the other
supporting the jaw. Rescuer 1
pulls helmet laterally to clear
ears and rocks helmet back
and forth to clear nose and
back of head.
and neck in
5b Head
neutral position.
Head
tilt
Suspension trauma (orthostatic shock) occurs when the body
is at rest in a vertcal position with the lower body motionless
for a prolonged period of time (5 - 30mins). As a result, blood
pools in the lower extremities, blood pressure drops, the brain
is deprived of oxygen and fainting (Pg 24) occurs. However,
fainting while suspended vertically can lead to death.
Those at Risk:
Anyone immobilised in a vertical position is at risk:
• Rock climbers • Cavers • Circus performers
• Stretcher casualties • Confined space workers.
Factors affecting the degree of risk:
• Dehydration • Hypothermia • Fatigue • Ability of the person to
move their legs.
Prevention:
•Ensure harnessed is person well hydrated, warm and not
fatigued before commencing activity.
•Cease activity if fatigue, dehydration or hypothermia develops.
•Wear a good fitting harness.
•Ensure everyone in the group is trained in single rope rescue
techniques.
•Avoid hanging motionless....keep legs moving.
•Ensure everyone in the group is aware of signs and symptoms
of suspension trauma (below).
•Have a buddy system and communicate continually....don’t
work alone.
•Have a group risk management action plan.
If symptoms occur and casualty is still conscious:
•Alert buddy and activate action plan to get casualty to ground ASAP.
•If casualty is stranded and there is something to kick against or stand on (eg rock ledge or
caving leg-hoops) use leg muscles by pushing against it every so often to keep blood pumping
back to torso.
•If casualty is stranded in mid-air or is exhausted, raise legs to a sitting position which can be
done with a loop of rigging tape behind the knees or specialised rescue equipment.
NB. Pedaling legs should only be used as a last-ditch effort to prolong consciousness, as pedaling quickly
fatigues leg muscles which demand blood. As soon as pedaling stops, loss of consciousness quickly follows.
FIRST AID
SIGNS & SYMPTOMS
1 takes over control of
2 checks airway and
is opened using
6 Rescuer
7 Rescuer
8 Airway
head and neck and maintains head
breathing (Pg 4). If casualty is
head tilt (Pg 4) or jaw
and neck in the neutral position.
not breathing normally, open
airway.
thrust (Pg 40).
NB. Airway management takes priority over spinal injury.
• Faintness
• Dizziness
• Breathlessness
• Nausea
• Sweating
• Paleness
• Unconsciousness
• Low blood pressure
If conscious:
• Call
• Rest in position of comfort - ideally lying flat
• Loosen or remove harness
• Give oxygen if trained (Pg36)
• Look for other injuries
• Monitor vital signs regularly (Pg 81)
If unconscious:
• Call
• DRSABCD - Follow Basic Life Support Chart (Pg 3)
☎
☎
52 | Advanced First Aid
Advanced First Aid | 53
SCUBA Diving
Ruptured Lung (Pulmonary Barotrauma)
SCUBA divers breathe compressed air from cylinders underwater which can lead to unique
problems:
Decompression Illness (DCI)
Also known as the ‘Bends’ is caused by nitrogen bubbles forming in the bloodstream and
body tissues which results from a scuba diver surfacing too quickly. This can lead to serious
complcations (eg neurological damage, chronic joint pain or even death) if not managed properly.
SIGNS & SYMPTOMS
(within an hour of a dive)
•Numbness/ tingling
•Extreme fatigue
•Weakness/ paralysis
•Visual, speech, hearing difficulty
•Headache
•Joint pains
•Rash
•Poor balance or coordination
•Altered consciousness
•Convulsions
•Collapse
Prevention is Best:
•Avoid deep dives.
•Reduce depths during multi-level
dives.
•Do safety stops.
•Ascend slowly - 10 metres/ minute.
•Stay hydrated.
•Stay insulated.
•Don’t dive if feeling unwell.
•Ensure equipment is operational.
•Dive with a buddy.
•DO NOT fly within 24 hrs of a dive.
•DO NOT use Entonox (nitrous oxide)
for pain relief (Pg 56).
FIRST AID
Conscious:
•Lie diver flat (horizontal, no pillow) - this reduces
the likelihood of bubbles travelling to the brain.
•Give 100% oxygen through demand valve or nonregreathing mask (Pg 36). Oxygen reduces the size
and number of nitrogen bubbles.
•Give fluids to drink if conscious (no alcohol) divers are often dehydrated after breathing dry gas
underwater which worsens the effects.
•Keep diver warm and no exertion.
for immediate transfer to recompression
•Call
chamber.
•Seek advice from Divers Emergency Service (DES)
•Record details of recent dives.
Unconscious:
Follow Basic Life Support (Pg 2-5)
☎
Demand valve 100% oxygen
(DES) Divers Emergency Service - 24hr emergency hotline
Japan
+81-3-38124999
Europe
+39-06-42118685
Korea
010-4500-9113
Air under skin
(subsutaneous
emphysema)
SIGNS & SYMPTOMS
(within 5 mins of a dive)
•Breathing difficulty
•Chest pain
•Coughing
•Blood streaked sputum
•Cyanosis (blue lips)
•Swallowing difficulty
•Voice changes
•Air bubbles under skin around neck
and face (subcutaneous emphysema)
•Altered consciousness
Pneumothorax
(collapsed lung)
Barotrauma is damage to body tissues caused
by pressure difference between air spaces within
the body and the surrounding environment.
Barotrauma can affect the lungs, sinuses, ears and
even the eyes behind a diving mask.
FIRST AID
•Remove diver from water immediately.
•If immediate exit is delayed, remove divers weight belt and inflate buoyancy vest.
On land or boat:
•Rest diver in position of comfort - sitting upright or reclined.
•Give 100% Oxygen (Pgs 36, 37).
•Call
•Call DES for advice (Pg 52).
☎
Australia
1800 088 200
+61-8-82129242
New Zealand
0800 4337 111
+64-9-4458454
South Africa
0800 020 111
+27-10-2098112
The Ear
If the pressure difference between the outer and middle
ear is not equalized via the eustachian tube, the diver will
+
experience earache and possible eardrum rupture. This
+
may lead to complications such as vertigo (dizziness),
middle ear infections, and deafness.
Outer ear
Sinus Squeeze (Sinus Barotrauma)
Drink
America
+1-919-6849111
As a diver surfaces, the gas in the lungs expands. If
expanding gas is not adequately exhaled, the diver’s lungs
distend and tear. This may result in a pneumothorax,
subcutaneous emphysema or arterial gas embolism.
Ear Squeeze (Ear Barotrauma)
Horizontal - no
pillow
Call DES to speak to a medic trained in diving medicine.
The medic will assess the situation and advise what
course of action should be taken. The medic will not make
arrangments for evacuation or local transport.
Arterial gas embolism
in the brain - symptoms
similar to a stroke (Pg 27)
Eardrum
+
Middle ear
canal
Sinuses are air spaces within the head which connect to the
nasal cavity. If mucus blocks the sinuses, the pressure difference
causes pain and rupture of the sinus lining which may lead to
sinus infection.
Eustachian
tube to throat
+
FIRST AID
SIGNS & SYMPTOMS
•Pain in ear/ sinuses
•Bleeding from ear/ nose
•Apply clean compress over ear/ nose
•Position casualty injured side down to allow
free drainage of fluid from ear.
•Seek medical advice - antibiotics may be needed
Best treatment is prevention:
•Equalize pressure in ears on descent (Valsalva Manoeuvre).
•DO NOT dive when congested (head cold).
Sinuses
54 | Advanced First Aid
Advanced First Aid | 55
Childbirth
The Mother:
Uterus
Birth is Imminent if:
•Congratulate the mother!
•Observe the mother for bleeding - 300 to 500mls is normal
provided the mother feels well.
•Clean the vaginal opening with a clean moist towel, from
front to back, and place a sanitary pad over vaginal opening
and ask mother to bring legs together.
•10-30mins after the birth of the baby, the placenta
(afterbirth) is delivered.
•Encourage mother to breast feed as this releases a
hormone to contract uterus and expel placenta.
•DO NOT pull on the cord to extract the placenta as this
may cause bleeding.
Placenta
• The woman has had a child before and states the baby is on the way.
• There are strong contractions 2-3 mins apart with a desire to push.
• Waters/ membranes have ruptured.
Blankets
You will need:
Plastic sheet/ bag
Pillows
Newspaper
Cord
Cutting the Cord:
Goggles
3-5cm from
baby’s skin
Sanitary pad
Scissors
Gloves
Hot water or Methylated spirits
Soap
String
Towels
Preparation:
•Call
- keep on loud speaker for assiatance if required.
•Assist the woman to adopt position of comfort (lying, squatting, kneeling).
•Place pillows under head and shoulders if lying on back.
•Place a plastic sheet (bag/ shower curtain) with newspapers and towels on top to absorb fluids.
•Ensure clothing is removed from woman’s lower body.
•Ensure adequate heating and privacy of the area.
•Wash hands thoroughly with soap - wear gloves and protective eye wear if available.
The Birth:
•Reassure & encourage mother to relax between
Normal birth - head
presents first
contractions.
•If mother passes a bowel motion while pushing, fold up
soiled towel and replace with clean towel. This reduces
chance of infection.
•When baby’s head appears, support with both hands.
•Let the mother push out the baby.
•DO NOT pull baby’s head to hurry the birth.
•Baby will be slippery.
•When baby is completely out - Record the time of birth.
☎
The Baby:
NB. If the umbilical cord is looped around baby’s neck, let birth
proceed and once baby is out then unravel cord from around neck.
•Place baby on the mother’s abdomen/chest and allow
mother to hold and handle baby.
•Keep baby warm by placing a blanket over baby and
mother.
•Wipe the baby dry with a warm towel.
•The baby will initially be blue in colour but when
rubbed will cry and start to ‘pink up’.
•DO NOT cut the cord until the placenta has been delivered
and the cord has stopped pulsating - at least 10 mins after
delivery.
•Sterilize string and scissors by placing in metho/ alcohol
spray or boiling water for 5 mins prior to use.
•Tie cord with sterile string in 3 places (see diagram).
•First tie should be 3-5cm from baby’s skin - ensure baby’s
skin is not caught in the tie.
•Cut between the 2nd and 3rd tie using sterile scissors.
•Check cord stump for bleeding after 2mins and 10mins.
•Place placenta in plastic bag for medical inspection.
Complications of Childbirth
Mother bleeds in excess of 500mls:
•Massage the top of the uterus (at the level of the mother’s navel) for about 30 secs or until
it contracts (feels firm).
•Massage in a circular motion with hand at right angles to abdomen.
•Encourage mother to breast feed - this stimulates uterine contraction and stops bleeding.
(see, Shock Pg 14).
•If mother feels, nauseated, faint or unwell, Call
Baby does not start to cry or breathe:
•Towel dry baby immediately after birth which should stimulate baby to cry and breathe.
•If baby does not cry, check mouth and nose and wipe away mucus with soft cloth/ towel.
•If baby still doesn’t cry and is unresponsive, commence CPR (Pg 2-5).
•Call
Breech Birth:
and advise emergency services.
• If the woman knows her baby is breech, Call
•Assist woman to an upright, forward leaning position eg kneeling and leaning on a chair.
•Allow baby to birth - the baby’s buttocks or feet will present first.
•Allow baby’s body to hang vertical.
•DO NOT pull the baby out to hurry the birth.
•If possible, ask the woman to pant while baby’s head comes out.
•When baby is completely out - Record the time of birth.
•Manage baby, mother and cord as per normal birth (see above)
☎
☎
☎
NB. Breech birth babies are more likely to need resuscitation (see above, Baby does not start to
cry or breathe).
56 | Advanced First Aid
Advanced First Aid | 57
Analgaesia - Pain Relief
Principles of pain management:
•The severity of the casualty’s pain response does not indicate the severity of the condition.
•Assess pain in the secondary survey, not the primary survey (Pg 81).
•Look for the cause of pain • DO NOT give analgaesia for headache following head trauma (Pg 20).
•Reassess pain regularly as changing levels of pain may indicate a change in the casualty’s condition.
Pain Management Techniques:
• Reassurance • Position casualty or part of the body to minimise pain.
• Distraction & relaxation techniques to diminish awareness of pain.
• Maintain casualty’s privacy & dignity to minimise discomfort.
• Analgaesia - Assist casualty to self administer own analgaesics when appropriate.
As a general rule, first aiders should not give pain relief medication. First aiders can assist a
casualty with their prescribed medication or medication which the casualty chooses to take
independently.
In the workplace, follow the established guidelines for the use of pain-relieving medication.
Entonox
Contents gauge
Single pin index
connection
•Entonox is an analgaesic gas composed of 50%
nitrous oxide (laughing gas) and 50% oxygen.
Demand valve
•The gas is self administered through a demand valve,
using a mouthpiece, bite block or face mask and is often
used in dental proceedures or childbirth.
•Entonox offers fast acting pain relief (2mins), wears off
quickly and has few adverse effects (drowsiness).
•Entonox is a ‘Prescription Only Medicine (Schedule 4
drug) and authorisation to administer is required from a
medical authority.
•There is no risk of overdose as the casualty’s level of
consciousness governs his/her ability to maintain flow of gas.
Entonox Equipment:
Flexible tubing
•Entonox cylinders are blue with a white quartered shoulder
and have a single pin index mounting on the cylinder neck.
•Store cylinder horizontal and above freezing, if possible.
•If a cylinder is stored below -5ºC, the gases will separate - re-warm
Entonox cylinder
cylinder and invert at least 3 times.
Before Administering:
•Seek permission from a medical authority to administer Entonox.
•Ensure airway is clear (no vomit).
•Ensure casualty can breath deeply enough to operate the demand valve.
•Ensure casualty is fully conscious and compliant with instructions for self administration.
•Advise casualty about the possibility of drowsiness.
•Supervise casualty at all times by a person trained in Entonox administration.
Contraindications to using Entonox:
•Decompession Illness or scuba diving within 24hrs (Pg 52).
•Reduced level of consciousness following head injury (Pg 20).
•Suspected pneumothorax (collapsed lung), (Pgs 17, 52)
•Casualty unable to understand or comply with instructions for self-administration.
•Casualty is delirious or confused.
Penthrox
•Penthrox is a hand-held inhaler device which is used for self-administration of methoxyfluorane
for pain relief.
•This portable, disposable, single use inhaler device along with a single 3ml brown glass vial of
methoxyfluorane is provided in a kit that allows conscious, stable casualties (children over 5yrs) to
self-administer the drug under supervision.
•Penthrox is a ‘Prescription Only Medicine’ (Schedule 4 drug) and authorisation to administer is
required from a medical authority.
•Each 3ml dose of methoxyfluorane lasts approx 30 mins - Max dose of 6ml per day or 15mls per week.
•Pain relief should start after 6-10 breaths - relief continues for 5-10mins after ceasing the use of
Penthrox.
•Penthrox may be administered with or without oxygen added.
Contraindications to using Penthrox:
• Allergic or adverse reaction to general anaesthetic • Renal impairment (Kidney problems)
• Respiratory depression • Cardiovascular instability • Pregnancy • Breast feeding • Casualty
taking tetracycline or gentamycin antibiotics.
1
Mouthpiece
AC Chamber
2
Base of
Inhaler
3ml bottle
Oxygen
port
Dilutor
hole
Attach AC (Activated Charcoal)
chamber onto penthrox inhaler
(optional).
4
Dilutor
hole
Hold Penthrox inhaler at a 45 angle.
Slowly pour contents of 3ml bottle
(methoxyfluorane) into base of
inhaler while rotating inhaler.
5
Finger covering
dilutor hole
3
Wrist-loop
Tilt Penthrox inhaler from
side to side to distribute
methoxyfluorane over the wick.
6
Wrist-loop
Place wrist-loop around casualty’s
wrist. Casualty inhales and exhales
through mouthpiece of inhaler
to obtain relief. First few breaths
should be gentle, followed by
normal breathing.
Opiates
If stronger relief is required,
casualty covers dilutor hole on top
of AC chamber with finger when
inhaling. (If AC chamber is not
attached, dilutor hole on Penthrox
inhaler is covered).
Replace cap on empty
3ml bottle and place used
inhaler and bottle in sealed
plastic bag and dispose of
responsibly after use.
•Opiates (morphine and pethidine) are schedule 8 drugs which are strong, often addictive
analgaesics (Pg 58) prescribed and administered under a doctor’s supervision.
•Opiates must be stored seperately under lock and key, checked daily, recorded in a specified
register, and signed for by two people to ensure correct quantities are stored.
58 | Advanced First Aid
Advanced First Aid | 59
Substance Misuse
Stimulant & Hallucigen Misuse
Substance misuse may be accidental or deliberate. Those most at risk of
accidental misuse are the elderly and children. The elderly may confuse
their medications and young children may mistaken medications for
sugary treats.
Minimise accidental misuse by storing medications out of reach of childern
and by assisting the elderly to organise and label their medications.
A pill box is a great way to organise daily doses.
NB. When handling a drug/alcohol misuse situation:
• DO NOT put yourself at risk.
• DO NOT approach if you feel unsafe.
• DO NOT provoke hostility.
Pill Box
Narcotics (opiates) include heroine, morphine, pethidine, methadone and codeine. Narcotics are
strong pain killers which are addictive and in overdose can result in respiratory arrest and death.
•Drowsiness
•Constricted (pinpoint) pupils
•Blood-shot (red) eyes
•Slow breathing
•Shallow breathing
•Cyanosis (blue lips)
•Slow pulse rate
•Low Blood pressure
FIRST AID
•Ensure area is safe - beware of needles & blood
•Wear gloves if available
•If unresponsive:
•Call
•Commence CPR (Pg 3-5)
•For RB, use resuscitation (pocket) mask (Pg 37)
•Seizure
•Unconsciousness
•Respiratory arrest
•Needle tracks (hands, feet, elbow)
Needle tracks in
elbow crease
☎
Solvent Misuse
Solvent abuse involves inhaling the fumes from domestic and industrial products creating
a strong intoxication. The majority of solvent abusers are males aged 11-16yr. The intoxication
wears off quickly but there is risk of vomiting, choking and unconsciousness.
SIGNS & SYMPTOMS
•Dazed appearance
•Unsteadiness
•Slurred speech
•Unpredictable behaviour
•Headache
•Hallucinating
•Rash around mouth
•Vomiting & Choking
•Unconsciousness
Solvent Inhalants:
• Glues • Lighter fluid • Aerosol
Sprays • Dry cleaning products
• Paint • Petrochemicals
FIRST AID
•Ensure area is safe
•Move casualty to a ventilated area
•Give oxygen if trained (Pg 36)
•Place in recovery postion if
unconscious
•Call
☎
SIGNS & SYMPTOMS
• Dilated pupils • Rapid pulse • Rapid breathing • Flushed appearance • Sweating
• Rambling speech • Headache • Dry mouth • Aggressive • Unpredictable behaviour
FIRST AID
Narcotic Misuse
SIGNS & SYMPTOMS
Stimulant and hallucigenic drugs can be swallowed, sniffed, injected or inhaled. They increase
mental and physical activity leading to a state of euphoria and altered perception followed by a
period of depression or ‘let down’.
Stimulant Drugs: • Amphetamines (Speed, Ice) • Cocaine (coke) • Crack • Ecstasy • Ritalin
Hallucigen Drugs: • LSD (acid) • Phencyclidine (PCP, angel dust) • Mescaline • Marijuana (hashish)
• Ensure area is safe • Wear gloves if available • Speak calmly & reassure
• DO NOT be argumentative • Keep casualty warm • Monitor vital signs regularly (Pg 81)
Alcohol Misuse
SIGNS & SYMPTOMS
•Alcohol on breath
•Slurred words
•Very loud or very
withdrawn behaviour
•Unsteadiness on feet
•Loss of coordination
•Blurred vision
•Slow reaction time
•Confusion
•Memory loss
•Unconsciousness
FIRST AID
•Ensure area is safe
•Wear gloves if available
•Position casualty on their side - likely to
regurgitate or vomit
•Examine for head injury and exclude,
diabetes (Pg 26) and stroke (Pg 27)
•Call
☎
Recognising a Drug/ Alcohol Misuse Problem
If you’re worried that a friend, work colleague or family member might be misusing drugs or
alcohol, look for the following warning signs:
Physical warning signs of drug/alcohol misuse:
•Changes in appetite or sleep patterns.
•Bloodshot (red) eyes.
•Pupils that are larger or smaller than usual.
•Sudden weight loss or weight gain.
•Deterioration of physical appearance and personal grooming.
•Unusual smells on clothing or breath.
•Impaied coordination, tremors or slurred speech.
Behavioral warning signs of drug/alcohol misuse:
•Sudden change in hobbies, friends and favorite hangouts.
•Drop in performance and attendance at school or work.
•Unexplained need for money or financial problems. May borrow or steal to get it.
•Develops secretive or suspicious behaviours.
•Frequently gets into trouble (accidents, fights, illegal activities).
Psychological warning signs of drug/alcohol misuse:
•Appears fearful, anxious, or paranoid, for no reason.
•Unexplained change in attitude or personality.
•Sudden mood swings, irritability, or angry outbursts.
•Periods of unusual hyperactivity, agitation, or giddiness.
•Lack of motivation; appears lethargic or “spaced out.”
60 | Workplace First Aid
Confined Space
A confined space is a partially or fully enclosed space that is at atmospheric pressure during
occupancy, is not designed as a normal workplace and which may have:
•Restricted means of entry and exit.
•An atmosphere that is potentially harmful - eg unsafe oxygen levels, toxic air pollutants,
combustable materials, heat, cold.
•A risk of engulfment - eg grain, sand, wood chip, sawdust, soil.
Obvious confined spaces include:
Tunnels, storage tanks, trenches, boilers, pits, silos, pipes, sewers, manholes, shafts, ducts.
Less obvious confined spaces include:
Rooms that are inadequately ventilated, or rooms that become confined spaces by virtue of the
activities being undertaken eg spray painting.
Hazards Associated with Confined Spaces:
• Oxygen deficiency (asphyxiation) • Oxygen enrichment (risk of combustion) • Presence of gases,
fumes, vapours • Engulfment from sawdust, grain, soil • Explosions, fire or electrocution • Heat, cold
or noise.
Entry Requirements:
Entry into a confined space occurs when a person’s head, breathing zone or upper body is within
the boundary of the confined space.
Before entering a confined space the following may be required:
• Risk assessment to include the following:
- The nature and hazards of the confined space to be entered.
- The work to be done, including the need to enter the confined space.
- The range of methods by which the work can be done.
- The risks associated with the work and equipment.
- Emergency response procedures.
- The training and competencies of the persons undertaking the work.
• Entry permit
• Atmospheric testing - oxygen, carbon monoxide, methane, Hydrogen Sulphide.
• Rescue and first aid personnel - to be on standby at all times.
• Warning signs - to be displayed outside the confined space.
• Appropriate PPE - eg helmet, eye protection, breathing apparatus, hearing protection.
• Communication - eg radio, lifeline, visual.
Confined Space Rescue:
•Plan, prepare and rehearse a rescue for every confined space.
•All rescuers must be trained and competent in confined space rescue.
•Rescue equipment and breathing apparatus must be functional and readily available.
•Safety must be maintained at all times throughout a rescue.
Chemicals Spills
Spill Prevention:
• Ensure appropriate chemical containers are used with seals that are in good condition.
• Ensure all chemicals are stored appropriately • Ensure appropriate equipment and procedures
are in place for decanting chemicals • Ensure employees or contractors have appropriate training
in safe chemical handling.
Spill Management:
• Keep a fully stocked and regularly maintained chemical spill response kit readily available
• Predetermine spill procedures and train relevant employees • Ensure appropriate PPE is
provided and used • Know the location and proper use of cleanup material • Know how to turn
equipment and energy sources off (e.g. air conditioning, gas, electricity) • Maintain and review
the relevant Material Safety Data Sheets (MSDS) to ensure appropriate risk controls are in place
• Refer to MSDS or call 13 11 26 for first aid management (Pg 32) • MSDS must be no more than
five years old from date of issue • Develop and maintain chemical Safe Work Procedures (SWP).
Workplace First Aid | 61
Wound Care
FIRST AID
• STOP BLEEDING (Pg 12) • CLEAN • DRESS with sterile dressing
How to Clean and Dress a Wound:
Step 1 You Will Need
Gauze
Swabs
Soap
Bandage
Antiseptic
Cream
Water
Betadine
Alcohol gel
Step 2
Gloves
Tweezers
Sterile
dressing
Bowl
Infection Control
then
OR
Wash hands thoroughly
Step 3
Saline Soution
Apply alcohol gel
Clean wound
OR
Use gloves if there is a risk of
contamination to the casualty
or first aider. Gloves are only an
adjunct to hand washing/gels.
then
Soak wound for 3-5mins in saline
or water (1 part betadine to 4 parts
water or saline).
Remove residual debris with
Irrigate wound for 3-5mins
with saline or water (1 part
tweezers or gauze swab
betadine to 4 parts water or
- DO NOT use cotton wool.
saline).
Wounds are most likely to become infected if foreign material (debris) remains in the
wound or contaminants are introduced into the wound.
Step 4
Dress wound
•Use a sterile non-stick dressing.
•Use antiseptic cream on grazes (abrasions)
or closed wounds to reduce infection.
•Bandage dressing in place if required.
•A wound should be cleaned before applying
a dressing and everytime a dressing is
changed.
•Seek medical advice if appropriate (Pg 62).
62 | Workplace First Aid
Workplace First Aid | 63
Recognising Wound Infection
A wound becomes infected when germs enter a break in
the skin. Wounds can be punctures (holes), lacerations
(tears), incisions (cuts), blisters or burns.
SIGNS & SYMPTOMS
Red
Hot
Odour
Pus
Pain
Swelling
• Pain • Redness • Swelling • Heat • Pus • Odour
• Red line tracking from wound
• Swollen, tender lymph nodes • Fever
Infected Wound
FIRST AID
• Clean & Dress wound (Pg 61) • Seek medical advice
If fever develops this indicates the
wound infection may have spread
systemically and requires urgent
medical attention.
Wounds - We to Get Help
Deep Incision
The skin is cut through to expose
fat, tendon or muscle or the edges
of the wound remain apart.
Loss of function
eg you can’t bend or
extend an injured finger.
Cut to Face
Puncture Wound
Caused by a rusty nail,
thorn, animal bite, is on
sole of foot or over a joint.
Foreign material
Even a small cut on the
face may require suturing
to prevent scarring.
Wound Infection
eg unable to remove
(see above)
grit from a wound
Treated with antibiotics.
Animal bite
Risk of infection
•A tetanus shot is required if the wound is caused by an animal bite, puncture wound or the
wound is dirty and your last tetanus shot was greater than 5-10yrs ago.
•DO NOT delay suturing - wounds older than 8-12hrs are sutured with a skin drain in place or
cannot be sutured at all as the risk of wound infection becomes too great.
Example of Good Wound Care Management:
Deep
Laceration
1
Bleeding was controlled (Pg12),
wound cleaned (Pg 61), then
checked for damage and
embedded objects.
2
Wound was sutured, cleaned
and dressed daily for two
weeks and antibiotics were
prescribed.
3
1 yr later - no complications
and the scar is bearly visible Great result!
Infection Control (See also Pgs 72 & 80)
Every employer is required under an Occupational
Health and Safety Act to provide a safe workplace
for employees and visitors; including providing
adequate infection control procedures and suitable
training and equipment.
• Infection control is achieved by preventing pathogens being transmitted from one person to another.
• The basis of proper infection control is to assume that all persons are potentially infectious.
• Basic infection control procedures include hand washing and keeping the workplace clean.
Spreading of infection:
Infectious agents (pathogens/ contaminants) can be spread in a number of ways,
including:
• Airborne - coughing or sneezing releases airborne pathogens, which can be inhaled by others.
• Skin-to-skin contact - some pathogens can transfer through touch, or by sharing personal
items such as clothing, helmets, or other objects.
• Contact with body fluids - contaminants in blood, saliva, urine or faeces can be transmitted to
another person via cuts or abrasions, or through the mucus membranes of the mouth and eyes.
• Contaminated objects or food - if hands are not properly washed, contaminants from a
person’s faeces may be spread to food; surfaces, and other objects.
Managing spills of body fluids:
Body fluids include blood, saliva, urine and faeces. When managing
spills of body fluids, the organisation’s infection control procedures
should be followed carefully.
You must:
•Isolate the area by using signage and/or barricades.
•Wear gloves, a plastic apron and eye protection such as goggles.
•Soak up the fluid with disposable paper towels, or cover the spill with
a granular chlorine releasing agent for a minimum of 10 minutes.
•Scoop up granules and waste using a newspaper (or similar) and
place in a plastic bag and dispose of properly.
•Mix one part bleach to 10 parts water and apply to the area for 10
minutes.
•Wash with hot water and detergent.
•Dry the area.
•Dispose of paper towels and gloves properly.
•Wash your hands with an appropriate cleaning agent.
•Rinse contaminated clothing in cold running water; Soak it in
bleach solution/disinfectant for half an hour; Wash separately from
other clothing with hot water and detergent.
Infectious or Biohazard Waste:
When disposing of infectious waste you should:
• Wear heavy duty gloves and other appropriate protective clothing.
• Place waste in plastic bags marked Infectious Waste or Biohazard.
• Dispose of waste in accordance with Enviroment Protection Act (EPA) regulations.
64 | Workplace First Aid
Establishing a Workplace First Aid Plan
Step 1 - Establish your Workplace’s First Aid Needs:
The factors that determine your organisation’s most effective first aid plan depend upon the
specific activities of your workplace and the industry in which you operate. Your workplace
situation can be assessed using the following 3 steps:
1. Hazard Identification - Identify hazards in your workplace. Hazards are things that can
cause harm (e.g. machinery, chemicals, working at heights).
2. Assess Risks - Assess the health and safety problems in the workplace - who is in
danger, what injuries could occur (eg cuts, burns, heat exhaustion), the factors contributing
to the danger and how likely they are to occur.
3. Control or Eliminate Risks - ie make changes to protect people. For example train
employees, develop safety proceedures, replace hazardous chemicals, guard machinery or
as a last resort use personal protective equipment (PPE).
Step 2 - Assess First Aid Requirements:
What type of work is performed? - Restaurant workers will have different first aid
requirements from those working in an oil refinery.
What type of injuries and illnesses are likely? - eg cuts, burns, chemical poisoning or
crush injuries. Also consider common medical problems which may occur amongst employees eg
epilepsy, asthma, diabetes or angina.
Locality and Number of employees - regulations may require a minimum number of trained
first aiders per number of employees, including during shift work and overtime.
Employees with disabilities - consider first aid needs and access issues of employees with
disabilities or special needs.
Workplace layout - first aid facilities must be appropriate for the type of work being performed
in different work areas.
Location of workplace - proximity of the workplace to medical centres, hospitals or ambulance
Step 3 - Develop a Written First Aid Action Plan:
• How many trained first aiders are needed? (Consult with OHS body/industry regulator).
• What are the training and qualification requirements for your first aiders?
• What is your Standard Operating Procedure when an employee requires first aid?
• Is a first aid room required and how should it be managed?
• What are your requirements for first aid kits? - • Contents (this will depend on your
workplace hazards, and the types of injury/illness likely to occur) • Number of kits • Location of
kits • Signs (clearly identified) • Information (contents list, emergency numbers) • Management
(assessing kit requirements, checking & replenishing contents).
• What system do you have in place for managing and maintaining first aid records?
Step 4 - Implement the First Aid Action Plan:
Nominated first aider officers need:
• Wrtten documentation outlining your organisation’s First Aid Plan to ensure they
understand their specific role and responsibilites.
• Ongoing training to maintain and update skills.
• Input towards developing and implementing the organisation’s first aid management plan.
Employees must be provided with:
Information about first aid during induction, and also at formal regular intervals. Language
and literacy needs of all employees must be considered and taken into account.
Workplace First Aid | 65
Employees must know:
• Where to go if first aid assistance is required • Who the first aider officers are in the
workplace • What role they have if a first aid incident occurs (e.g. reporting incidents and
accidents to supervisors).
This information may be communicated by:
• Information sessions • Induction training • Posters or signs in the workplace • Newsletters,
emails or memos.
Step 5 - Evaluate First Aid Action Plan:
• Organise a mock first aid emergency to check that your first aid plan works.
• If an incident requiring first aid does occur, evaluate the effectiveness of the first aid
provided, and make changes to your first aid plan if necessary.
• If new information is obtained about a previously unidentified hazard, review your first aid
system.
Being prepared for an OHS Inspection:
A WorkCover Inspector will most likely ask the following questions about your first aid set-up:
• What have you documented in regard to your first aid procedures?
• What type of injuries or illnesses has the workplace had over the last 5 years?
• What kinds of hazards are there in the workplace and what is the organisation doing to
advise and protect its employees and visitors?
• Is there a qualified and nominated first aid officer(s), trained to administer first aid?
• Show me the first aid kit(s).
• How many people work on this site, and show me how they access first aid?
• Who is responsible for keeping your first aid documentation up to date?
• How do employees and visitors know what to do and where to go if there is an injury or
illness requiring first aid?
First Aid Room
State and industry regulations determines if
your worplace is required to provide a First Aid
room.
Suggested items for a First Aid Room:
Furniture & Fittings:
• Sink with hot and cold water supplies.
• Cupboards for storage of linen and supplies.
• Desk, work bench or dressing trolley.
• Telephone • Electric power points.
• Lockable filing cabinet for record keeping (Pg79)
• Suitable seating • Couch (waterproof surface) with blankets and pillows.
• Moveable screen, suspended curtain, or a door that can close for privacy needs.
Medical Requirements:
• Examination table • Examination lamp • Stretcher, lifting frame or similar device for
transporting patients • Container safe disposal of needles or other sharp implements
• Container fitted with disposable bag or liner for soiled dressings and gloves • First aid kit
appropriate to the workplace • Soap, disposable towels, trays, gloves and bowls.
Documentation and Information:
• First Aid Incident/report form (Pg 79) • Daily Attendance Record Form • Injury/illness
statistic summary form (detects trends and evaluates safety proceedures) • First Aid Action
Plan • Names and contact numbers of first aiders and external emergency organisations.
66 | Remote First Aid
Remote First Aid | 67
Travelling to a Remote Area
A remote area can be defined as one in which medical care is more than one hour away.
Parties travelling to remote areas should be well organised and experienced.
Planning & Preparation:
When preparing for a trip to a remote area, plan for the unexpected:
• Injury/ illness • Getting Lost • Change in weather •Trip takes longer
than predicted.
Your provisions and equipment depends on the number of participants,
duration, and likely conditions. Consider:
• Food • Water (litres per day per person) • Clothing • Shelter • Fire
• First aid kits • Medications and repeat scripts • Communication
devices • Insurances • Vaccinations • Fitness and ability of group
members • Medical history of group members.
If going overseas to a remote area:
•Get a medical and dental checkup prior to your trip.
•Speak to a travel doctor who understands the environment you are travelling to.
•Check medication is not heat or cold sensitive - asthma puffers don’t work in extreme cold.
•Some medications are illegal in certain countries - check with your travel doctor.
•Check your prescribed medication is compatible with medications in your first aid kit.
•Ensure your travel insurance covers emergency evacuation by helicopter. Some countries
require proof of ability to pay. Leave credit card details, insurance cover or cash with travel
agent, embassy and/ or next-of-kin.
Team Leaders:
•Register and de-register your trips - this involves notifying authorities and friends of
your planned route and estimated time of arrival. When you arrive at your destination, notify
friends and authorities immediately.
•Check weather and other pertinent condition reports.
•Talk to members with a chronic medical condition and have them explain how to deal with
any possible emergencies (eg testing a diabetic blood sugar level, dealing with asthma attack).
•Give regular briefings to your group and local staff on what to expect on the next stage of trip.
•Don’t overestimate group abilities.
Buddy System:
•Always allow time for the unexpected.
•Pair up everyone in group with
•Don’t go faster than the slowest member of your group. instructions to keep an eye on
•Use the buddy system to monitor individual progress.
each other.
•If someone is not well, (Pg 71) stop as soon as it’s safe to •Any signs of general unwellness
do so and follow up the problem.
(Pg 71) is reported to group leader
•Don’t leave an injured person alone in the bush
without telling sick buddy (who
Personal Survival Kit:
often plays down early signs).
•Leaders must also have a buddy.
•Radio Distress Beacon (Pg 74)
•Water bottle • Pocket knife • Matches • Flint • Cotton wool - good tinder (Pg 67)
•Small metal pot - for boiling water and cooking
•Poly zip bags - keeps cotton wool & matches dry. Stores water.
•Iodine or chlorine tablets - purifies water (Pg 68).
•Vitamin C tablets - removes iodine and chlorine taste from water. Boosts immune system.
•Salt tablets - replenishes salt after sweating.
•Thermal blanket & black garbage bag - sleeping bag, roof for shelter, collects rain water,
carrys firewood, signaling device, marks trail when torn into strips.
•Wire saw - sawing wood for fire or shelter.
LOST or Injured
1
Sit down, stay put, stay calm.
Think through your situation, take stock - assess resources and needs.
Observe your surroundings.
Plan your survival - in most cases the priority should be:
• Make a SHELTER • Build a FIRE • SIGNAL • Find WATER
2 SURVIVE
•Shelter is the means by which your body is protected
from excess exposure to sun, cold, wind, rain or snow.
•Anything that takes away or adds to your overall body
temperature can be your enemy.
Black Garbage
•Clothing is the first line of shelter protection - have the
Bag
right clothes for the right conditions.
•Wear a hat - protects from the sun and
preserves body heat in the cold.
•Keep the layer closest to your body dry.
•Layers trap air and are warmer than one thick layer.
•Do not expend energy making a shelter if nature
provides one.
•Space (thermal) blanket prevents dampness, insulates your shelter,
collects rain water, makes a solar still (Pg 68), conserves body heat and
makes a good reflective signaling device.
•Black garbage bags make a good alternative to space blankets.
Space /Thermal blanket
SHELTER
FIRE
Fire can purify water, cook food, signal rescuers, provide warmth, light and comfort and help
keep dangerous predators at a distance. The smoke keeps flying insects at bay.
Outdoor adventurers should have a minimum of two ways of starting a fire - eg a flint
striker and waterproof matches on their person, and with their gear.
To make a fire you need to build up gradually beginning with tinder, then kindling, then
small pieces of wood progressing to larger pieces. Tinder is dry material that ignites
easily eg paper, leaves, grass, bark, resin, cotton wool. Kindling is readily combustable
material that is added to burning tinder eg small twigs and pine cones. Dead tree
branches make good fuel wood.
•Collect enough fire wood for the night, then
collect the same again.
•Carefully bank your fire to prevent igniting
surrounding areas.
•Conserve fuel by making a fire where the
ends of large logs meet the fire only - push
inward as more fuel is needed.
•Make a refector from your space blanket on
the back wall of a shelter to reflect the heat
of your fire to your back.
•Sit between fire and back shelter wall.
•Never leave a fire unattended.
•Extinguish fire before leaving camp.
68 | Remote First Aid
Remote First Aid | 69
Survival in Special Circumstances
SIGNAL FOR HELP
If you don’t have a mobile phone, satellite phone, two
way radio, whistle or Radio Distress Beacon (Pg 74) you
will need to use visual signals.
Select a good signal site close to your shelter with good
visibility such as a clearing, hilltop or lakeshore.
A search will probably start from your last known location
and sweep over your proposed route.
Lightning
•If you hear thunder, a storm is within 16km of you.
•Lightning strikes can occur within 10km of a storm.
•The scene is not safe until 30mins after the last thunder.
Whistle
3 short blasts
Fire & smoke, flashing light, bright coloured markers, flags,
flares and reflective devices can be used to create a
visual distress signal. (NB. Using fire & smoke as a
distress signal is potentially dangerous).
•Find shelter in a building or vehicle - tents offer no
protection and small open shelters, very little.
Flare
Torch
Flash 3 times
SOS (Safe Our Souls) is the best known international
distress signal. The SOS signal can be transmitted by
any method, visual or audio - 3 short, 3 long, 3 short.
Pause. Repeat signal.
If difficult to produce long and short signals, any signal
repeated 3 times will serve as a distress signal.
Three fires built in a triangle or straight line is recognised
as a distress signal.
On a sunny day use a mirror or shiny object as a signaling
‘V’ Sheet
EPIRB
device. A canteen cup, belt buckle, thermal blanket or mirror(Pg 74)
signaling-compass flashed 3 times serves as a distress signal.
Construct ‘SOS’ with rocks, logs or clothing as a ground to air signal.
If an aircraft recognises your distress signal, the pilot will respond by:
Rocking the aircraft’s wings (daylight) or flashing the aircraft lights on and off twice (night)
Lack of the above indicates that the message has not been understood.
WATER
Collecting water:
Survival is unlikely if you go:
30 hrs
3 days
30 days
3 mins
without O2 without shelter without water without food
•Never wait until you are out of water before collecting it.
•Select the cleanest water from the best site - running rather than still, and above villages.
•Catch rainwater in your space blanket by laying it out in a trench.
•Use Transpiration Bag, Solar Still or Beach Well method to collect water (see diagrams below).
•Polyzip bags are good for collecting and storing water.
•Contaminated water can cause diarrhoea so purify before drinking (see below).
Transpiration
Bag
plastic
bag
Solar Still
dirt
anchor
green foliage
creates
moisture
Water Purification - 2 Methods:
Beach Well
container
plastic
sheet
rock
weight
container
ocean
hole
dig for
water
saturated sand
1) Boiling - Strain large particals using a shirt or handkerchief before boiling for 10mins.
This is the best method of purification but requires a container and fire.
2) Chemical Tablets - (Iodine or Chlorine). Strain water as above then add tablet and
swirl around. Leave 30mins before drinking. To remove iodine taste, add 1/2 Vitamin C tablet.
•A motor vehicle or caravan with a metal roof
protects but avoid touching the metal sides.
•If no buildings or vehicles, seek shelter in low
areas under a thick growth of small trees or shrubs
or in concave ground ie valleys or dry ravines.
Feet
together
Hands off
ground
Crouch Position
Insulate
•If you are on a boat, get in the cabin and stay away from any metal or electronic components.
•If the boat has no cabin, adopt the crouch position - feet together, hands off floor.
•Avoid open ground, water, tall isolated trees, masts, pylons, summits, wire fences and tent poles.
•Place any metal (eg walking poles, ice axes, umbrellas) well away from you.
•Remove jewelry, hair clips, belt buckles, steel capped boots or other metal objects .
•DO NOT use electronic equipment (eg two-way radio or mobile phone) during a storm.
•If in an open area, assume the crouch position with feet together and hands off the ground.
•If possible, insulate under your feet with eg rain jacket, foam mat, plastic bag.
•If in a group, seperate each member at least 10m apart and all adopt the crouch position.
•Some victims are struck directly by lightning but others electrocuted from ground current.
•DO NOT lie flat on the ground as this increases your chances of ground current
electrocution.
•It is safe to touch and help a lightning victim as they are not ‘electrified’.
•Lightning injuries include cardiac arrest (Pgs 22, 42) and severe burns (Pg 15).
Floods
•Stay alert during stormy weather - heavy rain upstream could send flash floods your way
without you ever feeling a drop of rain.
•Know where streams and rivers run and local safe zones of higher ground.
•Avoid camping at the bottom or gullies and dried river beds during wet season.
•If you see or hear water rising, or notice water turning muddy, climb to the nearest high
point and wait out the flood or call for emergency assistance if necessary.
•Do not cross flood water more than ankle deep especially when an obvious current exists.
•If crossing, beware of objects in the water eg broken glass, torn metal, splintered wood and
electrical wires - wear appropriate foorwear.
•Being a strong swimmer in flood water may not save you as most people are killed from the
impact of objects such as logs or rocks.
•Flood water is often polluted by sewage and if swallowed may cause infection.
•If in a vehicle, avoid driving into flood water more than knee deep.
•If you have a radio or TV, stay tuned to local weather reports, warnings and evacuation
information. Heed warnings and immediately follow all instructions.
70 | Remote First Aid
Remote First Aid | 71
Early Signs of General Unwellness:
Snow
If injured or lost:
• Seek shelter - if snow is deep, build a snow cave on the
leeward side of a hill or under a tree. This is strenuous exercise
which will generate body heat. Pace the exercise to prevent
sweating as this increases cooling.
• Stay warm - Consume calories, rehydrate, keep your
Shelf for
body moving, build a fire (Pg 67), if wet get dry. Ensure
sleeping bag
the layer of clothing next to your skin is dry.
• Rehydrate - Do not eat snow as this chills your
Snow Cave Under a Tree
system. Pack snow into a flask and place under
Wind direction
clothing to melt.
• Make yourself visible - Cross your skis or stomp a
Vent - ski pole
large ‘X’ in the snow. Display bright clothing or use
keeps it open
other visual distress signals (Pg 68).
Shelf for
sleeping bag
• Use your PBL (Pg 74) if you have one.
If your trip is registered (Pg 51), help should not be too
far away - wait for rescuers.
Injury from cold exposure includes hypothermia
and frostbite (Pg 29).
Bushfire
Dehydration:
Dehydration is loss of body fluid resulting from excessing sweating, diarrohoea, vomiting, burns
and/or blood loss. 2-3 litres of water is lost daily through sweating and urination but increases
during exertion, at high altitude and windy conditions.
Drink 2 litres
of water
per hr in hot
strenuous
activities.
Snow block
seals entrance
Snow Cave on a Slope
Bush fires have 3 deadly qualities: 1) Radiant heat so intense as to induce heat stroke (Pg 28)
2) Smoke and hot gases causing asphyxiation (Pg 47) 3) Flames causing direct burns (Pg 15)
If trapped on foot:
•Go to an area that is already burnt or free of fuel.
•DO NOT try to run through a fire front.
•DO NOT try to out run the fire, move to it’s flanks.
•Move downhill to a low fuel area.
•Seek shelter in a large water mass (river, waterhole) on the side furthest from the fire.
•DO NOT climb into water tanks as this water heats rapidly, possibly to boiling point.
•If no water, hide behind a raised object - a log, rock or tree stump in a fuel free clearing.
•Seek shelter away from potential fuel and cover any exposed skin with dirt or clothing.
•In bare areas, find hollows in the ground, eg wheel ruts, which offer some protection.
•If possible lie face down with feet towards the oncoming fire.
•Protect your airway using a damp cloth or clothing.
If trapped in a vehicle:
• Grumble • Mumble • Stumble • Tumble
Heat Exhaustion (Pg 28); Hypothermia (Pg 29); Low blood Sugar from lack of food (Pg26);
Dehydration and Altitude Sickness (refer below) are common in endurance type activities. These
conditions share similar signs & symptoms and may occur together to create general unwellness.
•Stay in the car and do not try to run - the main intensity will pass quickly.
•If you think it’s hot in the car, it will be hotter outside the car.
•DO NOT drive through thick smoke.
•Stop vehicle on bare ground eg on a road.
•Turn off the ignition and switch on headlights and hazard lights.
•Wind up windows and close all vents.
•Stay below the level of the windows.
•Shelter from radiant heat by lying on the floor and covering yourself with woollen
blankets, floor mats or clothing.
•Remain in the car until the fire front has passed - even if the tyres are burning,
the petrol tank is unlikely to explode.
Signs & Symptoms
Mild Dehydration
(2% fluid loss)
•Thirst
•Urine dark, decreased
•Weakness
•Muscle cramps
•Irritability
•Headache
•Dry mouth
•Dry skin
•Dizziness
Sports drinks contain water,
electrolytes and sugar for quick
rehydration.
MAKING A SPORTS DRINK
1 litre water,
1/2 tsp baking soda,
1/2 tsp table salt,
1/4 tsp potassium salt (low salt),
2 tablespoons sugar
Moderate Dehydration
(5% fluid loss)
•Heart rate increases
•Breathing rate increases
•Decreased sweating
•Fever
•Nausea
•Tingling limbs
•Weight Loss
•Tongue coated & thick
Severe Dehydration
(10% fluid loss)
•Muscle spasms
•Vomiting
•Racing pulse
•Dim vision
•Painful urination
•Confusion
•Breathing difficulty
•Seizures
•Chest & Abdo pain
•Unconsciousness
First Aid
•Reduce Fluid Loss: Rest; Keep Cool; Seek Shade & Shelter
•Rehydrate: Drink water, sports drinks, eat food or salt tablet
•DO NOT DRINK: caffeinated drinks or alcohol (body consumes
fluids to digest them).
•Record Fluid Intake/Output (Pg 83)
•Moderate/ Severe Dehydration: Call
(IV fluids needed)
☎
Altitude Sickness
Common above 2400m (8000ft) where air pressure and oxygen concentration drops. Acute
Mountain Sickness (AMS) can progress to High Altitude Pulmonary Edema (HAPE) or High
Altitude Cerebral Edema (HACE), which are potentially fatal.
Signs & Symptoms
Acute Mountain Sickness
(AMS)
Headache
Fatigue
Dizziness
Breathlessness on exertion
Sleep disturbance
Poor appetite, Nausea
Swelling of hands, feet, face
First Aid
• Re-warm
High Altitude Pulmonary
Edema (HAPE)
Fluid on the lungs Persistent dry cough
Breathlessness at rest
Fever
• Re-hydrate
• Re-sugar
High Altitude Cerebral
Edema (HACE)
Swelling of the brain Headache
Unsteady gait
Uncoordinated
Loss of consciousness
• Re-oxygenate
• Descend
72 | Remote First Aid
Hygiene
(See Pgs 63, 80)
Hygiene is the actions or practices of personal cleanliness that protect health.
In a remote situation, without hot and cold running water, proper hygiene requires
more effort and planning.
•Wash hands frequently with soap and water, alcohol wipes or sanitizer gel.
•Place a basin with water, disinfectant and nail brush near toilet area.
•DO NOT share utensils or water bottles .
•Wash and dry your face, underarms, genitalia and feet daily to avoid
chaffing and fungal infections.
Infection Control in a Remote Area
Anyone suffering from diarrhoea, infected eye / wound or influenza should be
isolated as follows:
•The infectious person should sleep in a tent on their own and keep their dishes, cutlery,
soap and towel separate.
Anyone having contact with an infectious person should:
•Use protective/rubber gloves with all cases of infection, especially when cleaning up blood,
vomit, stools (Pg 63), or cleaning an infected wound (Pgs 61, 62).
•Wear goggles or sunglasses when attending to wounds.
•Use face masks in cases of airborne infection such as influenza.
•Wash and dry hands after contact with the infectious person, their clothes or belongings.
Preventing Diarrhoea and Food Poisoning:
•Purify drinking water (Pg 68)
•Avoid touching your mouth with your hands.
•Wash hands frequently and dry using a clean towel or air dry (drying is as important as
washing especially if preparing food).
•An infectious person should not be allowed near food preparation, serving or washing up.
•All kitchen utensils must be kept scrupulously clean.
•Keep flies, cockroaches, and rats off prepared food and preparation surfaces.
•Use two chopping boards (and knives) - one for meat and fish and one for other purposes.
•Chopping board and knife used for meat and fish must be scalded after use.
•Vegetables should be washed, soaked in iodine solution and well cooked.
•Salads may cause diarrhoea even after careful preparation.
•Peel fruit and boil fresh milk.
•All cooked food should be eaten immediately.
•Avoid reheated food or reheat thoroughly to minimize the risk of food poisoning.
Remote First Aid | 73
Moving a Casualty
As a general rule you should avoid moving a casualty unless there is a hazard or situation
you cannot remove eg fire, floods, cold, heat, fumes, rough ground, ants, snakes.
Moving a casualty, especially an unconscious or spinal injured casualty, can be difficult
and should be left to medical personnel who have the training and equipment necessary to
protect themselves and the casualty. If moving the casualty is essential, take extreme care
and use a good lifting technique.
Lifting Technique (see Pg 80):
• Bend your knees • Keep back straight
Before moving a casualty consider:
and head up • Stay balanced • Keep
• Size of casualty in relation to yourself • Number of
a low centre of gravity • Hold weight
people helping • Type and seriousness of injuries
close to your body • Work as a team • Terrain to be crossed • Distance to be covered
someone must take control.
• Neck stabilisation • Travel and motion sickness.
If the decision to move is made, ENSURE:
• Bleeding is controlled • Fractures are immobilised
• Casualty is secure • Aiway is managed (if
unconscious) • Casualty feels safe.
• Conscious casualty
sits forward and
folds arms across
their chest.
• 1st helper bends
down and places
their arms under
casualty’s armpits
and graps wrists.
• 2nd helper bends
down and secures
casualty’s knees.
• Both helpers rise
together & walk forward
Fore & Aft Carry
4 Handed Seat Carry
Improvised Stretchers:
•Before using an improvised stretcher, test it out of casualty’s sight.
•Tent poles or straight branches can be used with jackets, sacks, broad bandages or tarpaulins
to make stretchers.
Preventing wound infection:
•In hot humid environments wounds may easily become infected.
•Clean superficial wounds thoroughly with purified water or saline (salt) solution.
•Apply antiseptic preparation such as iodine, betadine, savlon cream to prevent infection.
•Deep, dirty wounds occurring in remote areas must be cleaned and covered but not
closed, as serious infections such as tetanus and gangrene thrive in dark, moist, low oxygen
environments. Medical attention must be arranged ASAP.
•Recognise signs of wound infection (Pg 62).
• Each helper grasps their
own left wrist with their right
hand.
• Then each helper grasps
the right wrist of the rescuer
opposite with their free hand.
• Both helpers lower
themselves sufficiently for
casualty to sit on 4 handed
seat.
• Casualty places her arms
around helpers’ shoulders
and before helpers rise to an
upright position.
Broad Bandage & Pole
• Tie broad bandages
1) Button 2 or 3 jackets
and turn them inside out,
leaving the sleeves inside
Jacket & Pole
between poles at intervals.
• Place blanket, sleeping
bag or tarpaulin on top.
2) Pass poles
through the sleeves
Sack & Pole
• Use 2 empty heavy-fabric sacks
• Cut holes in the 2 corners of
closed ends • Place sacks with
open ends facing each other
• Slide poles through holes
• Overlap open ends 10 cm to
provide extra strength in the middle
74 | Remote First Aid
Remote First Aid | 75
Communication
Radio: UHF, 27MHz, CB and VHF radios all operate by direct line of sight. UHF and
and 27MHz (Citizen Band & marine) radios only relay short range communications and are not
reliable for emergency transmissions.
VHF Radio:
Repeator stations are
in place to increase
communication range.
Land and marine VHF radios operate
on different frequencies. Channel 16 is
the marine VHF emergency channel in Australia.
Phonetic
Alphabet
UHF handheld two way
radio - range 300m - 5km
27MHz UHF radio:
CB and marine radios use different Ultra High Frequencies.
Using a radio:
Press transmit button. Say call station name 3 times
followed by your call sign 3 times. Say ‘Over’ when
transmission complete then wait for a reply.
HF Radio:
eg. “Coast guard Mooloolaba, coast guard Mooloolaba,
High Frequency radio units
coast guard Mooloolaba this is ABC 1, ABC 1, ABC 1, over”.
transmit over long distances
OVER: Finished and awaiting reply
using the ionosphere.
AFFIRMATIVE: Yes
Communications are affected by NEGATIVE: No
weather conditions. The Royal
SAY AGAIN: Repeat message
I SPELL: Spell word using the phonetic alphabet
Flying Doctor Service (RFDS),
STAND BY: Wait and continue listening
army and commercial marine
RECEIVED: Message was heard and understood
vessels use HF radios of
OUT: Transmission finished and complete
specific frequencies.
A radio licence and annual fees are Distress Call: Mayday, Mayday, Mayday
Urgency Call: Pan, Pan, Pan (requesting urgent assistance)
required to operate an HF radio.
Phone:
Mobile Phone
☎
Call
or ‘112’ or ‘911’.
112 and 911 connects you to the
nearest phone network. If there
is no signal, an emergency call
cannot be made. Try operating
from top of the nearest high
point to get a signal.
Radio Distress Beacons:
A - Alpha
B - Bravo
C - Charlie
D - Delta
E - Echo
F - Foxtrot
G - Golf
H - Hotel
I - India
J - Juliet
K - Kilo
L - Lima
M - Mike
N - November
O - Oscar
P - Papa
Q - Quebec
R - Romeo
S - Sierra
T - Tango
U - Uniform
V - Victor
W - Whisky
X - X-ray
Y - Yankee
Z - Zulu
Call ‘112’ or ‘911’ from sat
phone. Ideal for communicating
over long distances and in
remoteareas where there is no
phone coverage.
Operates by direct line of sight
to a satellite dish and therefore
can’t transmit from inside a car,
forestry, or in cyclonic weather.
Satellite Phone
Also known as EPIRBs (Pg 68), ELTs and PLBs are tracking transmitters which aid in the
detection and location of boats, aircraft and people in distress. A radio beacon transmits a
signal which is detected by an international satellite system designed to calculate
a beacon’s location. If the radio beacon is fitted with a GPS, it’s location can
be tracked to within 5 metres.
EPIRB (Emergency Position-Indicating Radio Beacon) - triggered by submersion and
signals maritime distress.
ELT (Emergency Locator Transmitter) - activated on impact and signals aircraft distress.
PLB (Personal Locator Beacon) - is for personal use and is operated by pushing a button.
Royal
Flying
Doctor
Service
(RFDS)
Queensland Section
Derby
1800 625 800
or
08 9417 6389
sat phone
Mt Isa
Alice Springs
Carnarvon
Western
Section
Cairns
Port Hedland
Meekatharra
Perth
Or call ‘000’
Cairns: 07 4040 0500
Mt Isa:
07 4743 2802
Charleville: 07 4654 1443
Broken Hill
Kalgoorlie
Sydney
Port Augusta
Adelaide
Central Section
Brisbane
Charleville
Canberra
Melbourne
08 8648 9555
Hobart
South
Eastern
Section
08 8088 1188
Or call ‘000’
When calling the RFDS, state the following:
• Date & time of message • Time of incident • Location & description of incident
• Number of casualties • Suspected nature & severity of injuries • Special hazards
• Name and distance from major town, landmark or station
• Location of nearest telephone landline if known
After the RFDS doctor has taken the emergency call, information as to the closest medical
chest may be provided. Doctors will also advise on the best method of evacuation if deemed
appropriate.
RFDS Medical Chest:
RFDS medical chests are registered to specific locations in rural
Australia and are placed in the custodial care of persons on site, who take
full responsibility for the medical chest.
RFDS medical chests provide an extensive range of pharmaceutical
and non pharmaceutical items, enabling treatment of emergency, life
threatening and everyday ailments, for persons living and working in
isolated remote areas. The contents cover a wide range of therapeutic
categories, including analgesics, antibiotics, anaphylactics,
antihistamines, cardiovascular, gastrointestinal, respiratory and
ophthalmic.
Using the RFDS Medical Chest:
RFDS Medical Chest
•Call the RFDS via telephone (HF radio rarely used now).
•Have a pen and paper handy.
•Be ready to answer questions about the casualty’s condition.
•Listen carefully to the doctor’s instructions.
•Repeat the doctor’s instructions and ask any questions if unsure.
•Access the medical chest which must be in the presence of the authorised chest holder.
•Administer any treatment or medication the doctor may order.
76 | Remote First Aid
Evacuation
Remote First Aid | 77
Evacuation
by either Air (fixed wing or helicopter); Water; Road; Foot
AIR RESCUE - Fixed Wing Aircraft:
1.2km
d
in n
W ctio
re
Di
Fixed wing aircraft - After landing:
•Stand well clear of taxiing aircraft and face rear with caution as dust and
debris is driven backwards at high velocity from propellers.
•Do not approach aircraft until propellers have
Rear door
stopped spinning, the flashing beacon turned
off, and cabin door is open.
•Secure all loose items and protect casualty
NO
from windborne debris.
PARKING
•Vehicles may approach aircraft slowly (<10km/
hr) after permission from pilot and park near
rear aircraft door.
•Do not reverse vehicle towards the aircraft.
•At night, vehicle headlights must be switched
DANGER
off so as not to impair pilot’s night vision.
Diagram 3 - After Landing
•NO smoking near aircraft.
Landing
Direction
Small Smoke
Fire
20m
30m
Weighted
Cone
30m
Diagram 4 - Helicopter Day Landing
Helicopter - Night Landing:
At night the LZ can be marked by flares, strobe lights
or two vehicles with headlights crossed at the centre
of the landing zone (Diagram 5).
Hi
gh
Touch
Down
Be Point h B
am
g
Hi
ea
m
Wind
Direction
Fixed wing aircraft - Night Landing
•Pilots never land at night on unlit airstrips.
•Remote properties with airstrips usually have
commercial flares for lighting but 2 litre open tins
Double
Flares
filled with rags soaked in kerosene, or toilet rolls
soaked in diesel will suffice.
18m
Flares evenly
•Flares should line both sides of the airstrip (30m
runway
spaced 90m
apart) and be evenly spaced (90m) with double flares
apart.
30m
at both ends (Diagram 2).
airstrip
•The pilot must be able to see the length of the strip
from the air.
•Air to ground communication via radio or phone
should be available at all times during a night
approach.
•A night landing using car headlights is rarely done
and only in extreme emergencies when the pilot is
Diagram 2 - Fixed Wing Night landing
familiar with the strip.
Helicopter - Safety Guidelines:
•Landing zone (LZ) must be at least 30 sqm of level,
firm surface clear of debris (avoid slopes).
•No powerlines, trees, poles, buildings or other
overhead obstructions near LZ.
•Mark LZ with weighted construction cones, or
smoke canisters during daytime landing.
•Markings such as rope, tape or light weight
materials should not be used for danger of being
sucked into rotor blades.
•Helicopters land into the wind so a wind indicator is
required (eg small smoke fire or windsock).
•Vehicles or people must be 20m away from
perimeter of landing zone.
•Arrange in penguin huddle with backs to helicopter
as it lands.
Wind
Direction
m
2k
1.
Fixed wing aircraft - Safety Guidelines:
•Pilots land fixed wing aircraft on approved airstrips
only.
•The runway must be 18m wide, 1.2km long and the
airstrip 45m wide for daylight landing in almost all
weather conditions (Diagram 1).
Di Win
re d
•The runway must be a smooth, firm surface and
18m
ct
io
n
runway
clear of scrub, rocks, potholes and livestock.
•If the runway is dry and rough, drive a vehicle at
90km/hr - excessive bumping or pulling indicates
45m
the strip is not safe for landing.
airstrip
•If the runway is wet, drive a vehicle at 15km/hr - if
tyre imprints exceed 25mm it is not safe for landing.
•Pilots always land and take off into the wind so a
wind indicator is required - windsock or smoke fire.
•Never encourage a landing if unsure about the
Diagram 1 - Fixed Wing Day Landing
safety of the strip.
AIR RESCUE - Helicopter:
Helicopter - After Landing:
•Do not approach while the blades are turning unless
you get thumbs up from the crew.
Flare
30m
•Approach and depart helicopter within the pilot’s
field of vision -10 to 2 o’clock (Diagram 6).
Diagram 5 - Helicopter Night Landing
•Indicate your intensions to approach by giving a
thumbs up to the pilot.
•Keep head and shoulders bent over - move calmly and swiftly (Diagram 7).
•Secure hats and other loose gear.
•Do not carry anything above your head.
•If blinded by dust, stop, sit down and wait for assistance - do not stumble around blindly.
•On sloping ground approach from the downhill side (Diagram 7).
•No smoking near aircraft.
10 O’Clock
Diagram 6
2 O’Clock
Diagram 7
78 | General First Aid
Principles
of First Aid
General First Aid | 79
Communication
What is First Aid? It’s the immediate care of an injured or
suddenly sick casualty until more advanced care arrives.
The aims of first aid are to:
• Preserve life – This includes the life of rescuer, bystander and casualty.
• Protect from further harm – Ensure the scene is safe and avoid harmful intervention.
• Prevent condition worsening – Provide appropriate treatment.
.
• Promote recovery – Act quickly, provide comfort and reassurance, get help, Call
Helping at an emergency may involve:
• Phoning for help • Comforting casualty or family • Keeping order at an emergency scene
• Administering first aid
There are many ways you can help, but first you must decide to act.
Reasons why people do not help:
•Fear of doing something wrong •Fear of disease transmission •Uncertainty about the
casualty •Nature of injury or illness (blood, vomit, burnt skin can be unpleasant) •Presence
of bystanders (embarrassed to come forward or take responsibility).
You may need to compose yourself before acting. Do not panic – a calm and controlled first
aider gives everyone confidence. If you follow basic first aid procedures, you should deliver
appropriate care, even if you don’t know what the underlying problem is. Remember, at an
emergency scene, your help is needed.
Getting Help:
for ambulance, fire or police. If
from a mobile phone fails, call ‘112’ or ‘911’.
Call
If you ask for ‘ambulance’, a trained communications officer will ask you the following:
• What is the exact location of the incident? • What is the phone number from which you
are calling? • Caller’s name • What has happened? • How many casualties? • Condition of
the casualty(s)
•Stay calm and respond clearly. The communications officer will provide you with first aid
instructions and dispatch the ambulance and paramedics.
•DO NOT hang-up until you are told to do so or the operator hangs up first.
call, ensure they confirm with you that the call has been
•If a bystander is making the
made and that the location is exact.
☎
☎
☎
☎
Legal Issues
No ‘Good Samaritan’ or volunteer in Australia has ever been successfully sued for the
consequences of rendering assistance to a person in need. A ‘Good Samaritan’ is a person
acting in ‘good faith’ without the expectation of financial or other reward.
Duty of care: In a workplace environment there is an automatic duty of care to staff and
customers - a failure to act in a way that is consistent with an obligation to provide reasonable
assistance, to the best of your ability, may result in negligence and possible litigation. In the
community, you are under no legal obligation to provide first aid.
Consent: Before providing first aid, you must first gain consent from the casualty. If the
casualty refuses help, you must respect their decision. If the casualty is unresponsive or of
unsound mind and therefore unable to give consent, it is assumed they would give consent
if they were conscious and/ or orientated. If the casualty is a child, the parent/ guardian
should be asked permission, but if no parent/guardian is present and the injury/illness is lifethreatening, immediate first aid should be given.
Confidentiality: Personal information about the health of a casualty is confidential. This
information includes details of medical conditions, treatment provided and the results of tests.
Disclosure of personal information, without the person’s written consent is unethical and in
some cases may be illegal.
The role of the first aider depends on gaining and honouring the trust of casualties.
Maintaining trust requires attentiveness to body language, quality of listening and finding
culturally appropriate ways of communicating that are courteous and clear. It may
sometimes be necessary to communicate through verbal and non-verbal communication
and you may need to identify issues that may cause conflict or misunderstanding. The first
aider also needs to maintain respect for privacy and dignity and pay careful attention to
client consent and confidentiality.
Reports
While waiting for help and if time permits, make a brief written report to accompany the
casualty to hospital. This will reduce time spent at the scene for ambulance crew and further
assist medical and nursing staff with initial patient management. A report can be written on a
spare piece of paper and should include the following:
• Date, time, location of incident
The back inside page
• Casualty details - Name, DOB, Address.
contains a ‘First Aid Report
Form,’ which can be torn
• Contact person for casualty - Family member, friend.
out and used at a first aid
• What happened - Brief description of injury or illness.
incident.
• First aid action taken – What you did to help the casualty.
• Other health problems – Diabetes, epilepsy, asthma, heart problems, operations.
• Medications/ allergies – Current tablets, medicines.
• When casualty last ate or drank – Tea, coffee, water, food.
• Observations of Vital Signs - Conscious state, pulse, breathing, skin state, pupils.
• First aider’s name/ phone number incase medical staff need any further information.
Record Keeping
• In the workplace, it is important to be aware of the correct documentation and record
keeping used in first aid situations • Every organisation has its own procedures and
documentation so, familiarize yourself with the correct process • All documentation must be
legible and accurate and must contain a description of the illness or injury and any treatment
given • Thorough, accurate medical records are essential in any court case or workers
compensation issue • NEVER record your opinion or judgement • Documents completed in
the course of employment remain the property of the employer • Retain records for 3-7yrs
• Write in pen (not pencil) • Never use correction fluid – cross out and initial any changes
• Sign and date the form • Keep contents strictly confidential • Store in secure location
Self-help/ Evaluation
Each person reacts differently to traumatic events and in some instances strong emotions
may affect wellbeing and work performance. Symptoms may appear immediately or
sometimes months later after an event and may develop into chronic illness.
There is no right or wrong way to feel after an event but what a person experiences is valid
for that person. It is useful to identify and work through these reactions/feelings as early as
possible. Speaking to an understanding friend, counselor or medical professional may be
beneficial in assisting you to cope with the situation.
In addition, seeking feedback from medical personnel about your first aid performance may
assist with self-improvement and prepare you better for any future events.
Some Reactions/ Symptoms • Crying for no apparent reason • Difficulty making decisions
• Difficulty sleeping • Disbelief • Irritability • Disorientation • Apathy • Sadness • Depression
• Excessive drinking or drug use • Extreme hunger or lack of appetite • Fear/anxiety about
the future • Feeling powerless • Flashbacks • Headaches • Stomach problems • Heart
palpitations • Muscle aches • Stiff neck
80 | General First Aid
General First Aid | 81
Safe Manual Handling
When lifting or moving a casualty it’s important the first aider protects him/herself from
injury by using correct lifting techniques - bending the knees and using leg muscles
will help protect against back injury. However, knowing your own limitations and asking
for assistance if required is also important in preventing injury. In addition, learning the
correct procedures for moving a casualty (eg rolling casualty into recovery position) further
minimises injury to the casualty and first aider.
Needle Stick Injury
FIRST AID
The risk of catching a serious infection (Hepatitis B, C • Squeeze blood out of injury site.
• Wipe with alcohol swab.
and HIV) from needle stick injury is very low.
• Wash hands.
Reduce the risk of needle stick injury:
• Place syringe in plastic drink
• Never bend or snap used needles
bottle or sharps container.
• Never re-cap a needle
• Place used needles into a sharps approved container • Take syringe with you to
• Hepatitis B vaccination for workers who regularly
hospital for analysis.
come in contact with blood/ body fluids
NB. Disposable gloves will not protect against needle stick injury.
Hygiene
Prior to treatment:
Minimise the risk of cross infection to yourself, bystanders and casualty
by taking appropriate precautions:
• Wash hands with soap
and water, or rinse with
antiseptic.
• Cover cuts on your hands
with a waterproof dressing
before putting on gloves.
• Wear disposable gloves.
• Do not touch any unclean
object when wearing
gloves .
• Use a plastic apron and
eye protection.
• Cover any adjacent areas
likely to produce infection.
During treatment: After treatment:
• Use a face shield/
mask, if available
when performing
resuscitation.
• DO NOT cough,
sneeze or breath
over a wound.
• Avoid contact with
body fluids.
• DO NOT treat
more than one
casualty without
washing hands
and changing
gloves.
• Clean up the casualty, yourself and
immediate vicinity.
• Safely dispose of used dressings,
bandages and disposable gloves
• Wash hands thoroughly with soap
and water, even if gloves were used.
• Restock first aid room/ first aid kit.
Recommended Contents of
a Personal First Aid Kit
Adhesive Strips (Band Aids)
10
Adhesive Tape
1
Alcohol Swab
3
Combine Dressing - Large
1
Crepe Bandage 5cm
1
Crepe Bandage 7.5cm
1
Eye Pad - Sterile
1
First Aid Booklet/Guide
1
• Keep a first aid kit at home, in your car and at
Gauze Swab
3
work in a clean, dry location.
Gloves
Disposable
2
• Make sure it is kept in easy reach and that all family
Hand Towels
3
members and staff know where the kit is located.
Non-Adhesive Dressing
2
• A regular check of contents is essential to ensure
Plastic Bag for Amputations
1
contents are present, not out of date and are in
Resuscitation Mask
1
good condition.
Safety Pins
5
• First aid kits will vary depending on the number of
Scissors - Blunt/Sharp
1
employees, and even the industry you work in
Splinter Probe
1
(Pg 64). If living in a remote area the contents will
vary from kits kept in urban homes.
Sterile Eye (saline) Solution- 15ml 2
Triangular Bandage
2
• Under State and Territory legislation first aid
kits are required in all workplaces.
Wound Dressing No. 14
1
First Aid Kits
Casualty Assessment When dealing with a person who is ill or injured,
you need a clear Plan of Action:
1.Start with a Primary Survey (DRSABCD), (Pg 3-5)
which enables identification and management of
life-threatening conditions.
2.If there are no life-threatening conditions which
require immediate first aid (severe bleeding, no
response) then proceed to Secondary Survey.
Secondary Survey - is a systematic check of the casualty involving:
• Questions • Examination • Clue Finding to help identify any problems that may have been missed.
• If the casualty is unconscious, the secondary survey is conducted in the recovery
position. You may need to look for external clues and ask bystanders some questions.
• If the casualty is conscious start with questions followed by examination. Remember to
introduce yourself, ask for consent to help and ask their name.
Examination
Questions
•What happened?
Vital Signs: are indicators of body function and provide
•Do you feel pain or numbness
a guide to the casualty’s condition and response to
anywhere?
treatment.
•Can you move your arms and
• Conscious State: There are 3 broad levels –
legs?
•Conscious •Altered consciousness •Unconscious
•Do you have any medical
Altered consciousness = uncooperative, aggressive,
conditions?
confused, drowsy (see also AVPU, Pg 83).
•Do you take any medications?
•Pulse: The carotid pulse in the neck is the best pulse
•Do you have any allergies?
to check. Feel for rate, rhythm, force, irregularities.
•When did you last eat?
Normal pulse rates:
Adults: 60-80 /min
•(Bystanders may be helpful)
Children: 80-100/min
• Breathing: Look, listen and/or feel for breathing rate,
External Clues
depth and other noises eg wheezing, noisy breathing.
Medical Alert: casualties
Normal
breathing rates: Adults 16-20 breaths/min
with medical conditions such
Children: 25-40 breaths/min
as diabetes, epilepsy or severe
(Check pulse/ breathing for 15 secs then x by 4 to
allergy usually have a bracelet,
get rate/min. Use a watch)
pendant or card to alert people of
Skin
State: Look at face and lips.
•
their condition.
Red, hot skin – fever, heat exhaustion, allergy
Medications: People on
Cool, pale, sweaty – shock, faint, pain, anxiety
regular medication usually carry
Blue lips (cyanosis) – airway obstruction, asthma, flail
it with them.
chest, collapsed lung, heart failure, hypothermia
Carotid pulse • Pupils: Equal, reactive to light
Radial pulse
Head to Toe:
• Seek consent from the conscious casualty before you
begin.
• Look and feel for bruises, cuts, deformities and painful
areas.
• Start from the head and work down.
• Explain to casualty what you are about to do at each
stage eg “I’m just going to move your arm”.
• Ask casualty for feedback at each stage eg “Does it
The pulse is not checked during CPR
hurt when I move your arm?”
82 | General First Aid
General First Aid | 83
Advanced Casualty Assessment
Blood Pressure
•Blood pressure (BP) is defined as the force
exerted by circulating blood on the walls of blood
vessels.
•BP is usually taken at the brachial artery with a
sphygmomanometer and stethoscope.
•Two pressure readings are recorded - systolic
(heart contracts) and diastolic (heart relaxes).
•The pressure difference between systolic and
diastolic is normally 40-50 mmHg.
•A normal adult BP is 120/70 but varies with age.
•Blood pressure and pulse are very closely
related and to make an accurate assessment of
the circulatory state both must be compared at
regular intervals.
Pressure
Gauge
Fluid Balance - Intake and Output
Bulb
120 Systolic
Fluid Intake/ Output charts are used to monitor and assess the level of
hydration in a sick casualty eg with diarrhoea and vomiting.
(For signs and symptoms of dehydration see Pg 71).
70 Diastolic
Cuff
Valve
Weight:
Time
Measuring Blood Pressure
Measuring Blood Pressure:
•Explain to casualty what you are doing (if conscious).
•Casualty can be sitting or lying with their arm at heart level (recovery position if unconscious).
•Use the left arm unless injury or position of casualty prevents this.
•Wrap cuff around bare upper arm (remove thick clothing) and secure velcro strip.
•Place stethoscope earpieces in your ears and stethoscope bell in the crease of casualty’s
arm (over brachial artery).
•Close valve on bulb of sphygmomanometer by rotating clockwise between finger and thumb.
•Inflate cuff by squeezing bulb until radial pulse is lost.
•Slowly deflate cuff by rotating valve anticlockwise whilst listening with stethoscope and
looking at pressure gauge.
•When the cuff pressure falls to the point where blood flows through the brachial artery again,
you will hear a ‘hub-dub’ sound. Look at the pressure gauge and read the number at this point.
This is the systolic pressure.
•When the cuff de-pressurises to the point that blood flows freely in the artery, the sound is no
longer heard in the stethoscope. Look at the pressure gauge and read the number at this point.
This is the diastolic pressure.
•Record the systolic and diastolic pressures (eg 120/70) and note the arm used for taking the
measurement.
Low Blood Pressure (Hypotension): Is defined as a systolic pressure below 90 mmHg.
Causes:
•Reduced cardiac output due to a weakened heart (eg heart attack).
•Reduced blood volume due to dehydration or massive blood loss.
•Excessive dilitation of blood vessels (eg anaphylaxis, spinal cord injury).
NB. A rising pulse rate and a dropping BP following trauma is suggestive of internal bleeding
High Blood Pressure (Hypertension):
Is defined as a repeatedly elevated blood pressure exceeding 140 over 90 mmHg ie a
systolic pressure above 140 with a diastolic pressure above 90. Lifestyle is often the cause
of chronic high blood pressure eg smoking, obesity, lack of exercise and diet.
NB. High blood pressure and a rapid pulse is associated with acute pain (adrenaline surge)
1 cup
150ml
1 glass
240ml
1 ounce
You will need:
•One jug marked in milliletres (all volumes recorded in milliletres).
1 tablespoon
•Two large containers (eg buckets) marked with capacity - eg one for
1 teaspoon
vomit, the other for watery stool.
•Fluid intake and output chart to record all measurements and remarks.
30ml
15ml
5ml
Fluid Input/ Output Chart
Date:
Stethoscope
Conversion Table
INTAKE
Oral
* IV
OUTPUT
Urine
Vomit
Stools
NOTES
Blood
7am - 3pm
3pm - 11pm
11pm - 7am
24hr Totals
SUM TOTAL for
24hrs
-ve Fluid Balance:
+ve Fluid Balance:
* IV means intravenous fluid and only applies to casualties on a drip
Fluids In: • Water • Juice • Tea • Soup • Ice cream • Custard • Ice cubes (melt to half their volume)
Fluids Out: • Urine • Watery stools • Vomit • Blood • Excessive sweating
AVPU Scale - a Measure of Responsiveness
•The AVPU scale is a system for measuring a casualty’s state of responsiveness.
•The AVPU system is only used to monitor vital signs in a sick or injured casualty while
awaiting medical assistance (see Workplace Casualty Report at back of book).
•To ascertain a response in a collapsed casualty follow DRSABCD (Pg 4).
ALERT
- Fully awake (may be disorientated). Casualty spontaneously opens eyes and responds to voice (may be confused).
VOICE
- Casualty responds when spoken to - this may be a grunt, moan, slight movement or opening of eyes.
PAIN
- Casualty makes a response to a painful stimulus:
• Pinch casualty’s ear • Press pen (or key) onto casualty’s fingernail.
UNRESPONSIVE - Casualty does not give any eye, voice or motor response to voice or pain.
Core Body Temperature
(See also Pgs 28-29)
Core temperature readings depend on which part of the body is being measured.
The sites used by a first aider to measure core body temperature include: • Under the arm
(36.4 °C) • Under the tongue (36.8 °C) • In the ear (37.6 °C)
A digital thermometer can be used under the tongue or
armpit at any age from birth (ear
thermometers not suitable for babies).
A temperature reading by itself does
not indicate how sick the casualty is but
progressive measurements may assist
medics ascertain a diagnosis/ treatment.
Digital Thermometer
84 | General First Aid
/
Natural Medicine in First Aid
Tea tree
Antiseptic
A few drops of tea tree essential oil mixed with
Papaw ointment makes an effective antiseptic for minor cuts
and grazes (Pg 61).
Topical: Apply to skin
Oral: Homoeopathic and flower remedies are dissolved under the tongue
Phone:
Document Findings!
(Clinical Assessment)
Clean wounds with sterile gauze swabs soaked in warm water
and sea salt (saline solution). DO NOT use cotton wool for
cleaning – cotton fibres stick to wound (Pg 61).
D
Wound
Cleaner
Other Findings:
Sea Salt
L – Laceration
P – Pain
R – Rigidity
S – Swelling
T – Tenderness
W – Wound
Peppermint essential oil rubbed onto soles of feet helps lower
body temperature.
A – Abrasion
B – Burns
C – Contusion
(Bruise)
D – Deformity
H – Haemorrhage
Fever/ Heat
Exhaustion
Last EAT or drink?
Peppermint
E
Homoeopathic Rhus Tox and Ruta Grav taken orally are
effective for ligament and tendon injuries. Combine with
homoeopathic Arnica and Symphytum for fracture and soft
tissue injuries.
□ Diabetes □ Asthma □ Epilespsy □ Heart Problems
□ Cancer □ Operations □ Previous Injuries □ Other
Soft tissue
injury
Medical Conditions?
Rhus Tox
Ruta Grav
M
Bach flower, ’Rescue Remedy’ and Australian Bush Flower,
‘Emergency Essence’ taken orally are effective remedies for
emotional stress.
Medications?
Emotional
stress
M
Rescue
Remedy
Allergies?
Mulla mulla, an Australian Bush Flower Essence, taken orally
helps to lower fevers and heal burns.
A
Burns/ Fever
How do you feel?
(Signs & Symptoms)
Mulla Mulla
H
Remedy for nerve injuries, especially crushed finger and
toenails. Homoeopathic hypericum taken orally helps relieve
pain and assist healing.
What Happened?
Nerve Injury
W
Hypericum
Location:
6% H2O2 kills infection in wounds when applied topically.
Effective for sore throat when gargled –froths in mouth. NOT
poisonous if swallowed.
Time of Incident:
Antiseptic/
Throat Gargle
/
Hydrogen
Peroxide
/
On day 3 or 4 after injury, soak injury for 20mins in bucket
of Epsom salts and warm water to draw inflammation and
swelling.
Date:
Soft Tissue
injury
INCIDENT:
Epsom Salts
Name:
Comfrey
Fractures/ Soft Grind fresh comfrey leaf in a mortar/ pestle to form a rough
(Symphytum) Tissue Injury
paste. Apply paste to a dressing and secure in place over injury.
Homoeopathic comfrey (Symphytum) under tongue also assists
healing.
Contact Person for Casualty (Friend/Relative)
Homoeopathic cantharis dissolved under the tongue assists
healing of all burn types (Pg 15).
Mobile:
Burns
Phone:
Cantharis
Address:
Calendula tincture or ointment can be applied topically to minor
cuts and grazes (Pg 61).
DOB:
Antiseptic
Age:
Calendula
M / F
Arnica ointment or tincture applied topically to a bruised area
assists healing. DO NOT apply to broken skin. Homoeopathic
arnica taken orally is also effective.
Surname:
Bruising
First Name:
Arnica
CONFIDENTIAL ONCE STARTED
Aloe vera gel (a Hydrogel) is very soothing when applied
topically to superficial burns eg sunburn (Pg 15).
□ VISITOR □ WORKER - Work Division:
DESCRIPTION
Burns
Casualty Details:
USE
Aloe Vera
WORKPLACE CASUALTY REPORT
REMEDY
/
Some natural remedies may be of benefit in first aid management.
15
80
Alert
Eg 09.15
Pink, warm
Skin
(Pg 81)
RO LO
RO LO
RO LO
RO LO
RO LO
(Pg 81)
Pupils
37.5
Cap refill 3 s
(Pg 83)
Temp
(Pg 11)
Circulation
120 / 70
Blood
Pressure
Low Priority
(Pg 16)
Triage
Medication:
Medication:
Work Division:
Dose:
Signature:
Dose:
Dose:
Expiry date checked: Y
Expiry date checked: Y
Expiry date checked: Y
Ambulance Arrival:
Referred to:
Departure Time:
Copy of Casualty Report Sent to: □ Ambulance □ GP □ Hospital □ Supervisor □ Safety Officer □ WHS □ Other:
Work Position:
Time:
Medication:
NAME OF FIRST AIDER(s):
Time:
Time:
MEDICATIONS ADMINISTERED: Have you had this medication previously? Y N Have you had any adverse reaction previously? Y N
MANAGEMENT: REFUSED TREATMENT: Y N WITNESS:
(Pg 81)
Breaths
Conscious
Pulse
(Pg 81)
(AVPU) - Pg 83
Time
OBSERVATIONS of Vital Signs:
N
N
N
First Aid Report Form
(Complete this form as best you can and give to ambulance officer/ medical personnel)
Date: /
/
Casualty Details:
Diabetes
Epilepsy
Asthma
Heart problems
Cancer
Operations
Previous injuries
Time:
Name:
Name:
Other health problems:
Location:
Pension No:
DOB:
/
/
M/F
Address:
Postcode:
Contact Person for Casualty (friend/ relative):
Phone:
What Happened (a brief description):
First Aid Action Taken:
Current Medications:
Allergies:
Last ate or drank:
Turn over
Emergency Numbers
Country
Australia
Casualty Examination:
mark location of injuries on diagram and
briefly describe injury eg cut, bruise, pain, swelling, burn.
☎
000
112
13 11 26
Embassy
Travel
Agent
Observations
of Vital Signs:
Dial ‘112’ or ‘911’ from a mobile phone with GSM coverage anywhere in the world and
Time
your call will be automatically translated to that country’s emergency number.
Conscious State
Fully Conscious
Drowsy
Unconscious
Pulse
Local Emergency Numbers
Phone
rate:
description:
DOCTOR
Breathing
rate:
description:
DENTIST
Skin State
PHARMACY
HOSPITAL
Colour:
Temp:
Dry/Clammy:
POLICE
Pupils
TAXI
R
ELECTRICAL
L
GAS
First Aider’s Details:
(Incase the hospital needs to contact you for more information regarding the incident).
Name:__________________________________________________
Phone:
Mobile:
WATER
VEHICLE
BREAKDOWN
Notes
World Map of International Emergency Numbers
© ABC Publications
☎
112
Greenland
Alaska
Iceland
Canada
911
Norway
113
Belarus
St Pierre &
Miquelon
USA
911
Moldova 903
France
112/15
Georgia
022
Bulgaria150
Azores
Gibralta 999
Bermuba
Canary
Islands
Mexico
Cuba
066
26811
060
080 Belize
Bahamas
Guatemala 120
El Salvador
Nicaragua
Costa Rica
Panama
Mauritania
Antigua
Martinique
Venezuela
171
Columbia
Algeria
14
Western Sahara
150
Dominican Republic
Cayman
Jamaica Haiti
Honduras 199
Albania
17
Morocco
Barbados 511
Trinidad 990
Guyana 913
Suriname
Mali
15
French Guiana
Libya
193
Syria
Kuwait
Saudi
Arabia
997
Niger
Iran
115
UG
Ecuador
Oman 9999
Maldives
French Polynesia
(Tahiti)
Bolivia
118
Chile
131
Ascension Island
6000
Thailand
1669
Seychelles
Bots
Papa New Guinea
Indonesia 119
Christmas
Bali 112
Island
Argentina
107
Falkland Islands
911
☎
15
Solomon Islands
Vanuatu
Fiji
Madagacar
Mozambique 117
Cape Town
107
France, Mali, Martinique, Mayotte, Morocco,
St Pierre & Miquelon, Tahiti (French Polynesia)
Niue
Tonga
Norfolk Island
☎
119
Cambodia, Indonesia, Japan,
South Korea, Taiwan
110
Bhutan, Jamaica, Sri Lanka, Syria, Turkey
115
Iran, Pakistan, Suriname, Vietnam
117
Madagasca, Mozambique, Philippines
103
118
Andorra, Angola, Bolivia, Haiti, Nicaragua,
San Marino
03
199
Bangladesh (Dhaka), Nigeria
000
Armenia, Belarus, Kyrgyzstan,
Mongolia
Azerbaijan, Kasakhstan, Russia
(Asian) Tajikstan, Uzbekistan
Australia, Christmas Island,
Norfolk Islands
No National Emergency Number
Cook Islands
998
Samoa
Australia
000
South Africa
10177
Uruguay
Beijing, Burma, Channel
Islands, Falkland Islands,
Ghana, Gibralta, Hong Kong,
Kenya, Malaysia (Singapore
995), Mauritius, Niue, Qatar,
Samoa, Seychelles, Sierra
Leone, Solomon Islands,
Sudan, Tansania, Uganda,
United Arab Emirates (UAE),
United Kingdom (UK),
Zimbabwe
Cambodia
Malaysia
Mauitius
Zimb
Bahamas, Belize, Bermuda,
Botswana, Canada, many
Caribbean Islands, Fiji,
Hawaii, some South America
countries, Tonga, United
States (USA)
Philippines
117
991
Namibia
Paraguay
Malawi 998
Mayotte
Angola
118
Zambia
Vietnam
Bangladesh
Sri Lanka
Singapore
995
Somalia
Kenya
Tanzania
Brazil
192
Hong Kong 999
Burma
Yemen 191
Japan
119
Taiwan
India
102
UAE
Zaire
Peru
116
South
Korea
Pakistan
Ethiopia
92
Ghana
999
China - Beijing
999 for private ambulance
120 for government
Sudan
999
Nigeria
199
Sierra
Leone
Iraq
Egypt
123
Chad
The Gambia
16
Mongolia
103
Kyrgyzstan
Turkey 110
Tunisia 190
Hawaii
Russia
(Asian)
03/112
Russia
(European)
112
UK
999/112
911
Most of Europe, Azores, Bali,
Canary Islands, Columbia,
Cyrus, Kuwait, Malta, Vanuatu
New Zealand
111
112
Dial 112 or 911 from a mobile
phone with GSM coverage
anywhere in the world and
your call will be automatically
translated to that country’s
emergency number.
ABC to Advanced First Aid is
divided up into 9 main
colour coded sections:
1. Essential First Aid
2. Trauma
3. Medical Emergencies
4. Advanced Resuscitation
ABC to
Advanced
First Aid
5. Low Voltage Rescue (LVR)
6. Advanced First Aid
7. Workplace First Aid
8. Remote First Aid
9. General First Aid
Each subsection shows you step-bystep how to recognise and deal with
an emergency situation.
In conjuction with an approved first
aid course, this book will assist you
learn the skills to perform basic to
advanced first aid techniques.
This book incorporates the 2010 Resuscitation
Guidelines and is written for Australian conditions.
For training purposes, this book satisfies the
Australian Health Training Package competency
units:
HLTFA403A: Manage First Aid in the Workplace
HLTFA402B: Apply Advanced First Aid
HLTFA404A: Apply Advanced Resuscitation
Techniques
HLTFA302A: Provide First Aid in Remote
Situation
HLTFA301B: Apply First Aid
HLTFA201A: Provide Basic Emergency Life
Support
HLTCPR201A: Perform CPR
Keep this book with your first aid kit in the workplace, at
home, in your car or when travelling overseas.
This book contains international emergency numbers and
is a useful resource no matter where you are in the world.