ATVB in Focus
Smooth Muscle Cells
Series Editor:
Giulio Gabbiani
Previous Brief Reviews in this Series:
• Hillebrands J-L, Klatter FA, Rozing J. Origin of vascular smooth muscle cells and the role of circulating stem cells
in transplant arteriosclerosis. 2003;23:380 –387.
• Iso T, Hamamori Y, Kedes L. Notch signaling in vascular development. 2003;23:543–553.
• Kumar MS, Owens GK. Combinatorial control of smooth muscle-specific gene expression. 2003;23:737–747.
• Schaper W, Scholz D. Factors regulating arteriogenesis. 2003;23:1143–1151.
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
Arterial Smooth Muscle Cell Heterogeneity
Implications for Atherosclerosis and Restenosis Development
Hiroyuki Hao, Giulio Gabbiani, Marie-Luce Bochaton-Piallat
Abstract—During atheromatous plaque formation or restenosis after angioplasty, smooth muscle cells (SMCs) migrate
from the media toward the intima, where they proliferate and undergo phenotypic changes. The mechanisms that
regulate these phenomena and, in particular, the phenotypic modulation of intimal SMCs have been the subject of
numerous studies and much debate during recent years. One view is that any SMCs present in the media could undergo
phenotypic modulation. Alternatively, the seminal observation of Benditt and Benditt that human atheromatous plaques
have the features of a monoclonal or an oligoclonal lesion has led to the hypothesis that a predisposed, medial SMC
subpopulation could play a crucial role in the production of intimal thickening. The presence of a distinct SMC
population in the arterial wall implies that under normal conditions, SMCs are phenotypically heterogeneous. The
concept of SMC heterogeneity is gaining wider acceptance, as shown by the increasing number of publications on this
subject. In this review, we discuss the in vitro studies that demonstrate the presence of distinct SMC subpopulations in
arteries of various species, including humans. Their specific features and their regulation will be highlighted. Finally,
the relevance of an atheroma-prone phenotype to intimal thickening formation will be discussed. (Arterioscler Thromb
Vasc Biol. 2003;23:1510-1520.)
Key Words: smooth muscle cell 䡲 heterogeneity
S
pothesis that all SMCs of the media can undergo phenotypic
modulation1 is the concept that a predisposed SMC subpopulation is responsible for the production of intimal thickening
(IT). This possibility has been raised on the basis of original
work by Benditt and Benditt,4 who reported that human
atheromatous plaques have the features of a monoclonal
lesion, an observation that has been confirmed by several
laboratories.5–7 More recently, with use of in situ microdissection techniques, it has been demonstrated that human
plaques are at least oligoclonal.8 These findings support the
suggestion that SMCs of the arterial wall are biologically
mooth muscle cells (SMCs) are important actors in the
pathogenesis of atherosclerosis and of restenosis after
angioplasty or stent application. In both phenomena, one of
the characteristic changes is the accumulation of SMCs
within the intima. The contemporary paradigm is that the
combined action of growth factors, proteolytic agents, and
extracellular matrix proteins, produced by a dysfunctional
endothelium and/or inflammatory cells, induces migration of
SMCs from the media and their proliferation.1 Moreover,
during these processes, SMCs switch from a contractile to a
synthetic phenotype.2,3 Alternative to the predominant hy-
Received May 14, 2003; revision accepted June 16, 2003.
From the Department of Pathology, University of Geneva–CMU, Geneva, Switzerland.
Correspondence to Dr Marie-Luce Bochaton-Piallat, University of Geneva–CMU, Department of Pathology, 1 rue Michel-Servet, 1211 Geneva 4,
Switzerland. E-mail Marie-Luce.Piallat@medecine.unige.ch
© 2003 American Heart Association, Inc.
Arterioscler Thromb Vasc Biol. is available at http://www.atvbaha.org
1510
DOI: 10.1161/01.ATV.0000090130.85752.ED
Hao et al
heterogeneous, and thus, attempts have been made to isolate
distinct SMC phenotypes from arterial vessels. Intimal SMCs
have been proposed to originate from diverse sources, including fibroblasts of the adventitia during restenosis,9 endothelial
cells,10 and/or circulating bone marrow– derived cells.11 Although the existence of these possibilities is gaining acceptance, the role of each of them is subject to much debate.
These possibilities, including the SMC origin of IT, are not
mutually exclusive. The ultimate aim of these studies, including those that have investigated SMC heterogeneity, the focus
of this review, is to define an atheroma-prone phenotype
(APP) involved in atheroma and restenosis formation.
Establishment of Distinct SMC Populations
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
The concept of SMC heterogeneity has been established by
the description of contractile and synthetic phenotypes in
vivo and in vitro.2,3 The contractile phenotype is typical of the
differentiated artery, and the synthetic one is typical of
developing and pathologic arteries. A further step was the
characterization in vitro of morphologically distinct SMC
populations, which has been observed in many species,
including humans (Table 1). Until now, the most-studied
species has been the rat. The initial description of SMC
heterogeneity was made in the rat carotid artery injury model,
wherein 2 SMC populations were identified: (1) a spindleshaped phenotype, with the classic “hill-and-valley” growth
pattern, obtained from the normal media (NM), and (2) an
epithelioid phenotype, in which cells grow as a monolayer
and exhibit a cobblestone morphology at confluence, isolated
from the IT 15 days after endothelial injury.12 This has been
confirmed by many laboratories (Figure 1; eg, see Orlandi et
al,13 Bochaton-Piallat et al,14 and Yan and Hansson15).
The last 2 decades have seen several advances in the
understanding of SMC heterogeneity, including the identification of (1) distinct phenotypes in healthy arteries of the rat
at different ages16 –23; (2) SMC subpopulations from particular compartments within the NM of the rat aorta24; (3) clonal
populations from the NM and IT of the rat aorta14,15,25,26; and
(4) distinct phenotypes in arteries of various species, such as
the dog,27 cow,28 pig,29 and human.30 –32
SMC populations with either spindle-shaped or epithelioid
phenotypes were isolated from the healthy rat aorta at
different ages.18,19,21,22 In particular, spindle-shaped SMCs
were predominant in fetuses at different developmental stages,22 as well as in newborn (4 to 5 days)19,21,33 and adult (6
weeks to 3 months) rats,13,21,34,35 whereas epithelioid SMCs
were prevalent in old rats (⬎18 months).18,21 This suggests
that the population of SMCs that exhibit an epithelioid
phenotype in vitro increases in rat aortic NM with age. In this
respect, several studies have shown that greater IT in response to injury is produced in old rats compared with adult
rats.36 –38 It is, however, noteworthy that a predominant
population of epithelioid SMCs was recovered from the NM
of 12-day-old newborn rats,16,17,20,23 an age when sexual
maturation occurs. These results suggest that a proportion of
SMCs that exhibit an epithelioid phenotype in vitro exists
within the media throughout the whole life span and that its
size can be influenced by circulating or microenvironmental
factors.
Smooth Muscle Cell Heterogeneity
1511
Villaschi et al,24 using tissue explantation, isolated epithelioid SMCs from the luminal part of the rat aorta NM. Our
group has produced clones from the NM and IT and has
demonstrated that spindle-shaped and epithelioid clones can
be recovered from both locations. However, the proportion of
clones that exhibit these phenotypes differed according to
their origin, the NM predominantly yielding spindle-shaped
clones and the IT yielding a majority of epithelioid clones.14
Several groups have confirmed the production of SMC clones
that exhibit spindle-shaped or epithelioid phenotypes from
the NM of rats15,25,26 and mice.39 Taken together, these
studies support the possibility that IT develops essentially
from a distinct, medial subpopulation that exhibits an epithelioid phenotype when placed in culture. It should be noted
that an SMC population that displays an epithelioid phenotype has been obtained from the NM of the spontaneously
hypertensive rat aorta,40 extending the role of this subpopulation in arterial diseases other than atherosclerosis and
demonstrating that SMCs with a propensity to produce an
epithelioid population in culture can increase within the
media subjected to pathologic stimuli.
Some experimental data indicate that rodent, including rat,
SMCs are not ideal models for human SMCs (vide infra
“Mechanisms of SMC Phenotypic Modulation”); hence, attempts have been made to culture SMCs from larger animals.
Frid et al28,41 have performed extensive studies of bovine
pulmonary artery and aorta. They first characterized the
morphologically distinct compartments within the NM41 and
then isolated from these compartments, by means of tissue
explantation, SMC subpopulations that exhibited spindleshaped, rhomboid, and epithelioid morphologies, the last 2
being similar to rat epithelioid SMCs.28 However, they did
not study arterial lesions. In the canine carotid artery,
Holifield et al27 have shown by sequential enzymatic digestion that spherical SMCs, similar to rat epithelioid cells, arise
from the abluminal part of the NM and are predominant in the
IT produced 14 days after endothelial injury. Our group has
recently isolated 2 distinct SMC subpopulations from the
porcine coronary artery.29 SMCs isolated by enzymatic digestion from the NM exhibit a spindle-shaped phenotype and
grow in a hill-and-valley configuration,29,42 similar to SMCs
derived from the porcine aortic NM.43,44 In contrast, SMCs
obtained by tissue explantation are either spindle-shaped or
rhomboid (flat, but more elongated than epithelioid rat
SMCs); the luminal side of the media yields equal proportions of spindle-shaped and rhomboid SMCs, whereas the
abluminal side yields a high proportion of rhomboid SMCs
(Figure 1).29 With these same techniques, IT induced 15 days
after stent implantation gives rise to a high proportion of
rhomboid SMCs. Hence, these cells represent good candidates for the formation of IT in the porcine coronary artery.
Identification of particular SMC subpopulations in human
arteries represents a difficult challenge for understandable
reasons, such as material availability and experiment standardization. Nevertheless, distinct SMC subpopulations have
been isolated from various human healthy and pathologic
arteries.30,32,45–51 In the 1980s, Orekhov et al45,46 characterized the morphological polymorphism of SMCs isolated from
arterial intima. Among the distinct shapes observed, elon-
1512
Arterioscler Thromb Vasc Biol.
September 2003
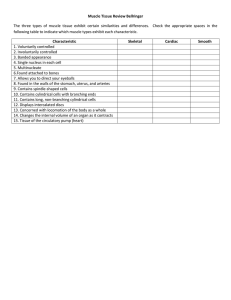
TABLE 1.
Description of Smooth Muscle Cell Subpopulations
Species
Vessel
Age
Location
Method
Morphology
Rat
Aorta
Embryo
NM
Explant
Spindle
References
22
Aorta
Newborn, 4–5
days
NM
Digestion
Spindle
19, 33
Aorta
Newborn, 12–19
days
NM
Digestion
Spindle and cobblestone
17
Aorta
Newborn, 12
days
NM
Cloning from passage 14
Spindle and cobblestone
23
Aorta
Adult
NM
Digestion, Explant
Spindle
13, 21, 34, 35
14
Aorta
Adult
NM
Cloning from primary culture
Spindle and epithelioid
Aorta
Adult
Luminal portion of NM
Explant
Epithelioid
24
Aorta
Adult
Abluminal portion of NM
Explant
Spindle
24
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
Aorta
Adult
IT 15 days after injury
Digestion
Epithelioid
13,14
Aorta
Adult
IT 15 days after injury
Cloning from primary culture
Spindle and epithelioid
14
Aorta
Adult
IT 60 days after injury
Digestion
Spindle
13
Aorta
Adult
Media underneath
15-day-old IT
Digestion
Spindle
13
18, 21
Aorta
Old
NM
Digestion
Epithelioid
Carotid artery
Adult
NM
Digestion
Spindle
12, 20
Carotid artery
Adult
IT 15 days after injury
Digestion
Epithelioid
12, 20
40
SHR
Aorta
Adult
NM
Cloning from primary culture
Spindle and monolayer
Chick
Abdominal aorta
Embryo
NM
Digestion
Spindle
56
Aortic arch
Embryo
NM
Digestion
Epithelioid
56
Aorta
Newborn, 7
days
NM
Cloning from primary culture
Spindle and epithelioid
39
Aorta
Adult
NM
Cloning from primary culture
Spindle
39
Carotid artery
Adult
NM
Digestion
Bipolar and spherical
27
Mouse*
Dog
Cow
Pig
Human
Carotid artery
Adult
IT 14 days after injury
Digestion
Spherical
27
Aorta and
pulmonary artery
Adult
Luminal portion of NM
Explant
Rhomboid
28
Aorta and
pulmonary artery
Adult
Middle portion of NM
Explant
Spindle
28
Aorta and
pulmonary artery
Adult
Abluminal portion of NM
Explant
Spindle and epithelioid
28
Aorta
Adult
NM
Digestion
Spindle
43, 44
Coronary artery
Adult
NM
Digestion
Spindle
42
Coronary artery
Adult
Luminal portion of NM
Explant
Spindle and rhomboid
29
Coronary artery
Adult
Abluminal portion of NM
Explant
Rhomboid
29
Coronary artery
Adult
IT 15 days after injury
Explant
Rhomboid
29
Aorta and renal
artery
Not described
Luminal portion of media
with IT
Explant
Multilayer and monolayer
48
Aorta
25–60 y
Unaffected and
atherosclerotic intima
Dissociation of prefixed
artery
Elongated and stellate
45, 46
Aorta
25–60 y
Unaffected and
atherosclerotic intima
Digestion
Elongated, asymmetric,
polygonal, and stellate
47
Abdominal aorta
10–45 y
Nonatherosclerotic artery
Cloning from passage 3
Spindle and broad
30
Aorta and carotid
artery
Not described
Atherosclerotic artery
Explant
Spindle and round
49
Pulmonary artery
40–60 y
Nonatherosclerotic artery
Explant
Spindle and polygonal
50
Coronary artery
Adult
Nonatherosclerotic and
atherosclerotic artery
Explant
Spindle and epithelioid
51
Internal thoracic
artery
Adult
Nonatherosclerotic artery
Cloning from passage 6
Spindle and epithelioid
32
SHR indicates spontaneously hypertensive rats.
*H-2Kb-tsA58 transgenic mice.
Hao et al
Smooth Muscle Cell Heterogeneity
1513
subpopulations arise and are maintained because of the
particular environment of cell culture. We have implanted
into the rat carotid artery subjected to endothelial injury 2
SMC subpopulations, ie, spindle-shaped, isolated from newborn rats, and epithelioid, isolated from old rats, that exhibit
distinct differentiation features (defined in addition to morphology by the expression level of ␣-SM actin, SM myosin
heavy chains [MHCs], and cellular retinol binding protein
[CRBP]-1; vide infra “Features of SMC Subpopulations” and
“Markers of Epithelioid and Spindle-Shaped Phenotypes”).52
Once seeded, the 2 SMC populations maintained their distinct
features, indicating that the phenotype of SMCs depends
more on their intrinsic features rather than their environment,
thereby reinforcing the notion of SMC heterogeneity.
Features of SMC Subpopulations
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
Irrespective of the species studied, epithelioid and rhomboid
phenotypes, when compared with spindle-shaped SMCs,
have in common several features, among which the most
relevant are (1) enhanced proliferative activity, including
serum-independent growth in some species; (2) enhanced
migratory activity; (3) increased proteolytic activity; (4) poor
level of differentiation, as defined by cytoskeletal and contractile protein expression (Table 2); and (5) high sensitivity
to apoptotic stimuli.
In all species studied, epithelioid and rhomboid SMCs
show a higher proliferative activity than do spindle-shaped
SMCs; however, contrary to spindle-shaped SMCs, they stop
growing at confluence as a result of cell contact inhibition.12,14,28,29,32 It is notable that rat epithelioid SMCs are able
to grow in the absence of serum.13,14,16,18,20,23,53–55 In addition,
albeit spindle-shaped, SMCs isolated from rat embryos exhibit serum-independent growth capacity.22 Epithelioid
SMCs produce platelet-derived growth factor (PDGF)-BB,
which is a potent SMC mitogen,16,20,23 and fail to respond to
the growth-inhibitory effect of transforming growth factor
(TGF)-.55 However, the factor(s) responsible for serum
independence has never been clearly identified. Autonomous
growth by epithelioid and rhomboid SMCs has been observed
in other species,28,56 with the exception of the pig,29 which in
this respect is similar to humans.32,51
One of the most striking differences between epithelioid or
rhomboid and spindle-shaped SMCs is that the first exhibit a
Figure 1. Morphological features of SMC subpopulations.
Phase-contrast microphotographs show spindle-shaped (a) and
epithelioid (b) phenotypes, respectively, isolated from the NM
and IT of rat aorta and spindle-shaped (c) and rhomboid (b)
phenotypes isolated from the NM of pig coronary artery.
Bar⫽150 m.
gated cells (ie, differentiated SMCs) were predominant in the
unaffected intima, whereas stellate cells (ie, undifferentiated
SMCs) were predominant in the atherosclerotic intima. Such
increase was correlated with collagen deposition and lipid
accumulation in the lesion.46 This cell diversity was partially
retained in primary culture.47 At the same time, Björkerud48
showed that 2 cell types, distinguishable by their shape and
adhesion properties, were present in SMCs cultured from IT.
Taken together, these studies suggest the presence of phenotypically distinct SMC populations in human arteries. More recently, it was shown that SMC subpopulations isolated by tissue
explantation49 –51 or cell cloning30,32 from healthy30,32,49 –51 or
atherosclerotic49,51 arteries display phenotypic features similar to
those observed in the rat and pig. In particular, the finding that
epithelioid SMCs can be cloned from human arterial media32
supports the suggestion that expansion of an SMC subset in
atherosclerotic lesions is conceivable. However, the relevance of
SMC heterogeneity to human disease still remains to be
demonstrated.
The distinct phenotypes of arterial SMCs have been mainly
identified in vitro, suggesting that specific features of SMC
TABLE 2.
Biological and Biochemical features of Smooth Muscle Cell Subpopulations
Species
Phenotype
Rat
Cow
Pig
Human
References
Spindle
Epithelioid
Spindle
Rhomboid
Epithelioid
Spindle
Rhomboid
Spindle
Autonomous growth
No
Yes
No
Yes
Yes
No
No
No
Epithelioid
No
13, 14, 16, 18, 22, 28, 29, 32, 53–55
Migratory activity
Low
High
ND
ND
ND
Low
High
Low*
High*
14, 28, 29, 32, 53, 57
␣-SM actin
⫹⫹
⫹
⫹⫹
⫹/⫺
⫹
⫹⫹⫹
⫹
⫹⫹⫹
⫹⫹
13, 14, 21, 22, 28, 29, 32, 33, 35, 42, 51, 57, 92
Desmin
⫹/⫺
⫺
ND
ND
ND
⫹
⫹/⫺
ND
ND
13, 14, 21, 29, 33, 42, 57
SMMHC
⫹
⫹/⫺
⫹⫹
⫺
⫺
⫹⫹
⫹
⫹⫹⫹
⫹⫹
13, 14, 21, 29, 32, 33, 42, 51, 57, 92
Smoothelin
ND
ND
ND
ND
ND
⫹
⫹/⫺
ND
ND
29, 42
SM22␣
⫹⫹
ND
⫹⫹
⫹/⫺
⫹
ND
ND
ND
ND
28, 49, 70, 92
Differentiation features
SMMHC indicates smooth muscle myosin heavy chain.
*Under PDGF-BB stimulation.
1514
Arterioscler Thromb Vasc Biol.
September 2003
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
high migratory activity, as has been shown in the rat,14,57
pig,29 and humans.32 With the aim of exploring the mechanisms involved in this activity, we have demonstrated that rat
epithelioid SMCs display high tissue plasminogen activator
(tPA) activity58 and that pig rhomboid SMCs display high
urokinase-type PA (uPA) activity.29 Likewise, Lau25 has
shown that rat epithelioid SMCs might produce tPA, uPA,
and metalloproteinase-2 under particular growth conditions.
In this respect, both PAs have been detected in both experimental IT59 – 61 and human atherosclerotic62– 65 lesions.
The study of cytoskeletal proteins, which are accepted as
reliable differentiation markers,66 –70 has allowed characterization of the contractile versus the synthetic phenotype
(Table 2). It should be noted that when placed in culture, all
SMCs tend to show a dedifferentiated phenotype.2,3 With this
limitation, the phenotypic variation of cultured SMCs furnishes
important information concerning the influence of many factors
on their biologic features. ␣-SM actin is expressed in vascular
SMCs,71 even at early stages of development, and thus represents the most general marker of SMC lineage.72 Although
␣-SM actin is permanently expressed in SMCs, it is more
abundant in spindle-shaped SMCs than in epithelioid or rhomboid SMCs.14,21,23,27–29,32,33,57 Desmin, an intermediate filament
protein, and SMMHC are expressed in well-differentiated
SMCs70,72 and are relatively well studied. In cultured rat SMCs,
desmin generally disappears.35 In larger animals, desmin is
maintained at a significant level of expression in spindle-shaped
SMCs, whereas it is hardly detectable in epithelioid and rhomboid SMCs.28,29 SMMHCs are clearly expressed more importantly in spindle-shaped SMCs than in epithelioid and rhomboid
SMCs.14,21,23,28,29,33,57 Other cytoskeletal proteins have been less
extensively studied. In particular, smoothelin, SM22␣, calponin,
h-caldesmon, and metavinculin70 serve as late differentiation
makers and are more abundant in spindle-shaped SMCs than in
epithelioid and rhomboid SMCs.27–29,56 In general, SMCs isolated from larger animals, including humans, are more differentiated than are those isolated from rodents. Porcine spindleshaped SMCs maintain appreciable expression of ␣-SM actin,
SMMHC, desmin, and smoothelin.29,42 SMMHC, calponin,
h-caldesmon, and metavinculin are abundantly expressed in
bovine spindle-shaped SMCs.28 SMCs isolated from human
arteries behave similarly.32 An interesting correlation has been
demonstrated, albeit occasionally, between dedifferentiated
and/or highly proliferating SMC phenotypes and increased LDL
uptake50,73–75 or decreased HDL binding sites.76 The role of LDL
and HDL processes in atheromatous plaque formation with
respect to SMC heterogeneity should be further investigated.
Taken together, the data obtained in different species suggest
that the degree of differentiation of SMCs changes with the
phenotype; this integrates well into a view that reconciles the
heterogeneity of SMCs with the modulation concepts.
An enhanced susceptibility of rat epithelioid SMCs to
apoptosis induced by reactive oxygen species,26 retinoic
acid, and antimitotic drugs77 has been recently described.
Interestingly, SMCs isolated from healthy human coronary
arteries show marked heterogeneity to Fas-induced apoptosis.78 It is noteworthy that apoptosis is an important
phenomenon in the development of experimental IT and
has been detected in SMCs of atherosclerotic and reste-
notic lesions (for a review of different aspects of this
problem, see Kockx and Herman,79 McCarthy and Bennett,80 and Geng and Libby81). Apoptosis could participate
in the regulation of cellularity in restenosis and in the
stability of the plaque; the role of distinct SMC populations in this context remains to be demonstrated.
Markers of Epithelioid and
Spindle-Shaped Phenotypes
Once distinct populations have been defined, the ultimate aim
is to identify genes and/or proteins that are differentially
expressed and to test whether they are involved in the
phenotypic changes that occur in vivo. Using the technique of
2-dimensional polyacrylamide gel electrophoresis, we have
identified several proteins that are differentially expressed in
rat aortic spindle-shaped versus epithelioid SMCs.82,83
Among them, 3 proteins have been sequenced and identified
as markers of the rat epithelioid phenotype in vitro: CRBP-1,
a protein involved in retinoid metabolism, and cytokeratins 8
and 18, intermediate filament proteins.
In vivo, CRBP-1 is constitutively expressed in rare SMCs
of the NM of adult and old rats but not of newborn rats.83
After endothelial injury, CRBP-1 is rapidly activated in a
subset of medial SMCs located toward the lumen and is
expressed in the large majority of SMCs present in the IT;
however, it disappears when reendothelialization is achieved.
Remodeling of IT is associated with SMC apoptosis.84 – 86
CRBP-1, which is present in replicative SMCs during the
initial phase of IT formation, is also detected in apoptotic
cells of IT.83 Altogether, these results suggest that a predisposed subset of medial SMCs becomes rapidly CRBP-1–
positive after injury, undergoes replication during the early
phase of IT development, and then disappears, allegedly
through apoptosis, when reendothelialization takes place.83
Some additional data support this scenario: SMCs cultured
from reendothelialized IT (60 days after injury) are exclusively spindle-shaped, suggesting that potentially epithelioid SMCs have disappeared.13 Moreover, cultured rat
epithelioid SMCs are more sensitive to apoptosis than are
spindle-shaped SMCs.26,77 Taken together, these results indicate that CRBP-1 is a marker of the epithelioid phenotype in
vitro and of SMC activation after endothelial injury in vivo.
Unfortunately, when the analysis of CRBP-1 expression was
extended to pigs and humans in vitro and in vivo, the role of
this protein as a marker was not confirmed (M.-L. BochatonPiallat, P. Neuville, G. Gabbiani, unpublished observations).
This further supports the assumption that rodent SMCs do not
represent a reliable model for human SMCs.
Cytokeratins 8 and 18, intermediate filament proteins, as
well as zonula occludens-2 protein and cingulin, 2 proteins of
tight junctions, were thought to be exclusively expressed in
epithelial or endothelial cells. They have since been identified
as markers of rodent epithelioid SMCs39,83,87 and are expressed in experimental IT87 or human atheromatous
plaque.88 Studies of these proteins could give further insight
into the mechanisms of SMC pathologic modulation.
Several other genes have been discovered, mainly in
rodents, as being specific or at least more abundant in 1
SMC population compared with the other. Epithelioid
Hao et al
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
SMCs express osteopontin,89 –92 tropoelastin,20,23,87 PDGFBB,20,23 cytochrome P450,93 and peroxisome proliferatoractivated receptor-␥,87 whereas spindle-shaped SMCs express procollagen type I and PDGF-␣ receptor.20,23,87 This
pattern of gene expression is broadly observed in cloned
SMCs that exhibit phenotypes similar to their parental
populations, with the exception of procollagen type I,
whose expression appears to be sensitive to cell density
and serum level.23 Although none of these genes has
conclusively been proved to be relevant to the pathogenesis of human lesions, the study of osteopontin, an extracellular matrix protein involved in bone mineralization,
has shed new light on the mechanisms of IT formation.
Osteopontin is associated with SMC proliferation90 and
migration.94,95 In vivo, it is transiently upregulated in
experimental IT91,96 and accumulates in calcified areas of
the atheromatous plaque.91,97–99 Recently, it has been
shown that SMCs lose their lineage markers and acquire an
osteogenic phenotype in vitro under calcifying conditions
and in vivo in transgenic mice whose arteries calcify
spontaneously.100 This suggests that SMCs can play a role
in vascular calcification.
Interestingly, the subtractive hybridization approach with
RNA isolated from rat embryo SMCs with an autonomous
growth property and rat adult SMCs with a nonautonomous
growth property22 allowed identification of several embryonic genes; one of them, ie, embryonic growth-associated
protein, is involved in the serum-independent growth of
embryonic SMCs and is reexpressed in experimentally induced IT.101
Recent studies performed in species other than the rat are
providing novel insight into the understanding of IT formation. Autonomously growing, rhomboid SMCs isolated from
bovine pulmonary artery exhibited constitutively activated
extracellular signal–regulated kinase (ERK-2) and eicosanoid
production.102 Other studies with microarray techniques or
differential-display polymerase chain reaction have been
performed with SMCs in various situations, yielding identification of numerous, differentially expressed genes in monkeys and humans.103–105 They are either unknown or known to
be involved in atherosclerotic processes. A very recent study
with suppressive subtractive hybridization that was performed in the pig has compared the coronary artery, predisposed to atherosclerosis, with the mammary artery, which is
resistant to atherosclerosis.106 Genes that are preferentially
associated with the mammary artery are involved in cell-cell
junction formation, whereas genes that are preferentially
expressed in the coronary artery are implicated in lipid
metabolism, inflammation, and cell proliferation. However,
the presence of distinct SMC populations within the same
vessel has not been taken into account in these studies.
Taken together, the studies performed in a variety of
species, including humans, provide evidence that arterial
SMCs are phenotypically heterogeneous. Moreover, the epithelioid and rhomboid (according to the species) phenotypes
are good candidates for representing the APP for several
reasons: (1) they always exhibit an enhanced capacity for
proliferation and migration that is associated with high
proteolytic activity, features essential for the accumulation of
Smooth Muscle Cell Heterogeneity
1515
SMCs in the IT; (2) they acquire a poorly differentiated
phenotype typical of intimal SMCs in vivo; and (3) they
express specific proteins crucial for their behavior. In this
respect, the most demonstrative example is the identification
of CRBP-1 as a specific marker of intimal SMCs in the rat
model. The discovery of new genes and/or proteins typical of
the APP in other species is still a challenge and, once
possible, should provide new insight into the understanding
of atherosclerosis and restenosis mechanisms.
Origin of Epithelioid and SpindleShaped Phenotypes
During vasculogenesis, SMCs have been proved to originate
from diverse sources depending on the vessel type: mesoderm, neurectoderm (neural crest), epicardium (for coronary
arteries), and, more rarely, endothelium.10 This has led to the
hypothesis that the various SMC phenotypes could arise from
distinct lineages. A study performed in the chick embryo
aorta has shown that spindle-shaped and epithelioid phenotypes can be isolated from 2 distinct regions of the artery,
which differ in their embryologic origin, namely, the mesoderm and neural crest.56 The 2 populations are quite similar in
their cytoskeletal equipment but respond differently to
TGF-. These results suggest that different SMC subpopulations play a role in the formation of the tunica media, at least
in the chick embryo.
The morphological similarity of epithelioid SMCs to endothelial cells has led Kohler et al107 to investigate whether
this SMC subtype exhibits an angiogenic capacity. For this
purpose, they cultured mouse epithelioid SMCs in a collagen
gel and observed that they were capable of forming vessellike structures, and in coculture, that they induced spindleshaped SMCs to participate in this process. Moreover,
Nicosia and Villaschi108 have shown that the luminal part of the
rat aorta, which contains predominantly epithelioid SMCs (vide
supra “Establishment of Distinct SMC Populations”), gives rise
to pericytes when placed in coculture with endothelial cell–
forming microvessels, whereas SMCs from the deeper part of
the aorta (mainly composed of spindle-shaped SMCs) do not.
We have shown that the capacity of porcine rhomboid SMCs to
invade a collagen gel is remarkably higher than that of spindleshaped SMCs.29 These data suggest that epithelioid SMCs could
play a major role in angiogenesis and/or arteriogenesis.109 In
addition, they could be considered a potential source of locally
derived stem cells, ie, cells present in adult tissues that exhibit
pluripotent features.110
Recent studies suggest that endothelial cells could acquire
SMC features, ie, ␣-SM actin expression in vitro111 and in
vivo.10 Moreover, bone marrow– derived cells have been
reported to undergo transdifferentiation toward the SMC
phenotype in transplant arteriopathy,112,113 in IT induced after
arterial injury,113,114 and in hypercholesterolemia-induced
IT.115 Although considered a minor source of SMCs, it would
be of interest to study whether these cells participate in the
emergence of those that exhibit the APP.
Mechanisms of SMC Phenotypic Modulation
Many attempts have been made to modulate the behavior of
distinct SMC subpopulations. The factors tested can be
1516
Arterioscler Thromb Vasc Biol.
September 2003
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
distributed in 4 categories: (1) those described as classic
inhibitors of SMC proliferation and/or increasing SMC differentiation, eg, heparin, TGF-, and retinoic acid; (2) those
known to stimulate SMC proliferation and/or decrease SMC
differentiation, eg, PDGF-BB, fibroblast growth factor
(FGF)-2, and insulin growth factor-I and II; (3) vasoactive
substances, such as endothelin-1, angiotensin II, histamine,
and norepinephrine; and finally (4) vasodilator factors, such
as nitric oxide (NO).
Heparin, which is the most powerful inhibitor of SMC
growth in vitro and in vivo, at least in the rat,116,117 did not
exhibit differences of action on the distinct rat118 or pig29
SMC subpopulations. In the bovine pulmonary artery model,
heparin exerted dramatic growth inhibition on rhomboid
SMCs, whereas it had almost no effect on spindle-shaped
SMCs.28 These results indicate that the action of heparin on
diverse SMC subpopulations depends on the species studied.
In the rat, TGF-118 as well as retinoic acid119 changes the
morphology of epithelioid SMCs; however, these cells do not
achieve a typical spindle-shaped phenotype. In contrast, in
pig coronary artery SMCs, TGF- does not influence SMC
morphology, although it does decrease proliferation and
increase the differentiation level of both SMC subtypes. In
the rat, retinoic acid increases the expression of ␣-SM actin
only in epithelioid but not in spindle-shaped SMCs; however,
in both cell types, retinoic acid decreases proliferation and
increases migration.119 All of the effects of retinoic acid are
mediated by the nuclear receptor RAR-␣. These results
indicate that rat epithelioid SMCs, ie, CRBP-1–positive
SMCs, are more prone to respond to retinoic acid than are
spindle-shaped SMCs, at least so far as their differentiation
state is concerned. In vivo, feeding rats with retinoic acid or
with an RAR-␣ agonist inhibits aortic or carotid artery IT
formation,119 –121 thus functionally confirming that CRBP-1 is
a marker of the APP in the rat model.
Some articles have shown that spindle-shaped SMCs are
more responsive than are epithelioid SMCs to vasoactive
factors such as endothelin-1,24 angiotensin II, histamine, and
norepinephrine,32 either by measuring collagen gel contraction or by evaluating the intracellular calcium concentration.
This is in accordance with the contractile feature of spindleshaped SMCs. Conversely, epithelioid SMCs exhibit increased expression of inducible NO synthase,15,122 which is
correlated with enhanced nuclear factor-B expression when
compared with spindle-shaped SMCs.122 Moreover, these
cells fail to respond to NO15,38 because of the lack of the
-subunit of soluble guanylyl cyclase.38 This suggests that
despite a large production of NO, epithelioid SMCs are less
sensitive than are spindle-shaped SMCs to NO actions.
FGF-2 and PDGF-BB similarly increase the proliferation
and migration of porcine SMC subpopulations.29 Human
epithelioid SMCs migrate more actively than do spindleshaped SMCs in response to PFGF-BB.32 We have shown
that FGF-2 and PDGF-BB induce a switch from the spindleshaped to the rhomboid phenotype in pig SMCs.29 This is
associated with increased proliferation and a decrease in
expression of differentiation markers. A similar effect has
been obtained for spindle-shaped SMC clones. In both
situations, this shape change is reversible when treatment is
ceased. These results indicate that the switch depends on
phenotypic modulation rather than on selection of a given
population. Interestingly, endothelial cells isolated from the
porcine coronary artery and placed in coculture with SMCs
induce a switch from the spindle-shaped to the rhomboid
phenotype.29 In these experiments, endothelial cells did not
exhibit a quiescent state even after confluence, suggesting
that they mimic an injured or dysfunctional endothelium. In
other species, previous studies with endothelial cell/SMC
cocultures have shown that endothelial cells stimulate SMC
proliferation123–125 and decrease the expression of ␣-SM actin
and SMMHC,126 particularly when nonquiescent endothelial
cells are used. It has been suggested that endothelial cells
stimulate the proliferation of SMCs by producing plasminogen activator inhibitor-1, which in turn inhibits TGF-
activation.124,127,128 The mechanisms through which endothelial cells specifically act on porcine spindle-shaped SMCs
remain to be clarified, but these results indicate that spindleshaped SMCs can evolve, at least to some extent, into the
rhomboid phenotype, supporting the view that pig SMCs
display an enhanced phenotypic plasticity compared with rat
SMCs. It will be important to establish whether this plasticity
is present in human SMCs.
Conclusions and Perspectives
The original observation by Benditt and Benditt4 has stimulated a significant number of experiments, which support the
possibility that SMC heterogeneity exists in different species.
Epithelioid and/or rhomboid SMCs appear to be the most
likely candidate to represent the APP by playing an important
role in the formation of IT.
Studies on the possibility that an SMC phenotype can
evolve into another have shown that the results depend on the
species used. This suggests that the mechanisms of IT
formation differ according to the model (Figure 2). Thus, in
the rat, the most studied model, SMCs show 2 phenotypes
that do not appear to be interchangeable, both in vitro and in
vivo. Indeed, the specific phenotype of SMC observed in
vitro is maintained when they are placed back into an in vivo
environment. The evolution of the lesion in vivo appears to
depend on the relative replicative activity and/or susceptibility to apoptosis of these phenotypes. Moreover, in the rat, an
agent that influences the biologic behavior of epithelioid
SMCs, ie, retinoic acid, inhibits IT formation. In the pig, the
situation is different, in that spindle-shaped SMCs can modulate into rhomboid SMCs and, if the stimulus ceases, can
return to their original phenotype, at least in vitro. This
supports the assumption that the evolution of in vivo lesions
is more complex in the pig than in the rat. In this respect,
porcine SMCs appear to behave similarly to human SMCs.
It should be emphasized that at present, the phenotypic
identification of APP SMCs other than in the rat is at a very
early stage. Studies at the genetic and/or proteomic levels
similar to those performed in the rat are needed to achieve
clear identification of the markers of each phenotype in vitro
and in vivo. An extension of these studies to vascular
development in appropriate species will also furnish useful
information on the origin of different SMC phenotypes and
on their localization in arterial vessels. In conclusion, the
Hao et al
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
Figure 2. Schematic hypothetical representation of IT formation
in rat and porcine models. In the rat model, a predisposed SMC
population, ie, atheroma-prone (AP)-SMCs, is localized to the
luminal portion of the media. After endothelial injury, AP-SMCs
either accumulate in the intima and subsequently acquire
CRBP-1 (➀) or first express CRBP-1 in the media before migrating toward the intima (➁). It should be noted that the non–APSMCs (ie, spindle-shaped phenotype) and AP-SMCs (epithelioid
phenotype) are not interchangeable. In the porcine model,
AP-SMCs are located at the abluminal part of the media. The
mechanisms (➀) and (➁) described in the rat model are the
same for the porcine model. In addition to these 2 possibilities,
non–AP-SMCs (ie, spindle-shaped phenotype) can evolve to
AP-SMCs (rhomboid phenotype), which then accumulate within
the intima (➂). For a dynamic view, see video available at
http://atvb.ahajournals.org.
paradigm of SMC heterogeneity has begun to produce experimental information and should be very useful in the future to
characterize precisely the biologic features of arterial SMCs
and to yield a better understanding of the role of different
SMC subpopulations in physiologic and pathologic
situations.
Acknowledgments
The authors acknowledge the support of the Swiss National Science
Foundation (grant Nos. 31.061336.00 and 32– 068034.02). We thank
Pierre-Alain Rüttimann and Jean-Claude Rumbeli for their graphic
work.
References
1. Ross R. Atherosclerosis: an inflammatory disease. N Engl J Med. 1999;
340:115–126.
2. Campbell G, Campbell J. The phenotypes of smooth muscle expressed
in human atheroma. Ann N Y Acad Sci. 1990;598:143–158.
3. Thyberg J, Blomgren K, Hedin U, Dryjski M. Phenotypic modulation of
smooth muscle cells during the formation of neointimal thickenings in
the rat carotid artery after balloon injury: an electron-microscopic and
stereological study. Cell Tissue Res. 1995;281:421– 433.
4. Benditt EP, Benditt JM. Evidence for a monoclonal origin of human
atherosclerotic plaques. Proc Natl Acad Sci U S A. 1973;70:1753–1756.
5. Pearson TA, Dillman JM, Solez K, Heptinstall RH. Clonal characteristics in layers of human atherosclerotic plaques: a study of the selection
hypothesis of monoclonality. Am J Pathol. 1978;93:93–116.
Smooth Muscle Cell Heterogeneity
1517
6. Pearson TA, Dillman JM, Solez K, Heptinstall RH. Clonal markers in
the study of the origin and growth of human atherosclerotic lesions. Circ
Res. 1978;43:10 –18.
7. Thomas WA, Kim DN. Biology of disease: atherosclerosis as a hyperplastic and/or neoplastic process. Lab Invest. 1983;48:245–255.
8. Schwartz SM, Murry CE. Proliferation and the monoclonal origins of
atherosclerotic lesions. Annu Rev Med. 1998;49:437– 460.
9. Zalewski A, Shi Y, Johnson AG. Diverse origin of intimal cells: smooth
muscle cells, myofibroblasts, fibroblasts, and beyond? Circ Res. 2002;
91:652– 655.
10. Gittenberger-de Groot AC, DeRuiter MC, Bergwerff M, Poelmann RE.
Smooth muscle cell origin and its relation to heterogeneity in development and
disease. Arterioscler Thromb Vasc Biol. 1999;19:1589–1594.
11. Hillebrands JL, Klatter FA, Rozing J. Origin of vascular smooth muscle
cells and the role of circulating stem cells in transplant arteriosclerosis.
Arterioscler Thromb Vasc Biol. 2003;23:380 –387.
12. Walker LN, Bowen-Pope DF, Ross R, Reidy MA. Production of platelet-derived growth factor-like molecules by cultured arterial smooth
muscle cells accompanies proliferation after arterial injury. Proc Natl
Acad Sci U S A. 1986;83:7311–7315.
13. Orlandi A, Ehrlich HP, Ropraz P, Spagnoli LG, Gabbiani G. Rat aortic
smooth muscle cells isolated from different layers and at different times
after endothelial denudation show distinct biological features in vitro.
Arterioscler Thromb Vasc Biol. 1994;14:982–989.
14. Bochaton-Piallat ML, Ropraz P, Gabbiani F, Gabbiani G. Phenotypic
heterogeneity of rat arterial smooth muscle cell clones: implications for
the development of experimental intimal thickening. Arterioscler
Thromb Vasc Biol. 1996;16:815– 820.
15. Yan ZQ, Hansson GK. Overexpression of inducible nitric oxide
synthase by neointimal smooth muscle cells. Circ Res. 1998;82:21–29.
16. Seifert RA, Schwartz SM, Bowen-Pope DF. Developmentally regulated
production of platelet-derived growth factor-like molecules. Nature.
1984;311:669 – 671.
17. Gordon D, Mohai LG, Schwartz SM. Induction of polyploidy in cultures
of neonatal rat aortic smooth muscle cells. Circ Res. 1986;59:633– 644.
18. McCaffrey TA, Nicholson AC, Szabo PE, Weksler ME, Weksler BB.
Aging and arteriosclerosis: the increased proliferation of arterial smooth
muscle cells isolated from old rats is associated with increased plateletderived growth factor-like activity. J Exp Med. 1988;167:163–174.
19. Hültgardh-Nilsson A, Krondahl U, Querol-Ferrer V, Ringertz NR. Differences in growth factor response in smooth muscle cells isolated from
adult and neonatal rat arteries. Differentiation. 1991;47:99 –105.
20. Majesky MW, Giachelli CM, Reidy MA, Schwartz SM. Rat carotid
neointimal smooth muscle cells reexpress a developmentally regulated
mRNA phenotype during repair of arterial injury. Circ Res. 1992;71:
759 –768.
21. Bochaton-Piallat ML, Gabbiani F, Ropraz P, Gabbiani G. Age
influences the replicative activity and the differentiation features of
cultured rat aortic smooth muscle cell populations and clones. Arterioscler Thromb Vasc Biol. 1993;13:1449 –1455.
22. Cook CL, Weiser MC, Schwartz PE, Jones CL, Majack RA. Developmentally timed expression of an embryonic growth phenotype in
vascular smooth muscle cells. Circ Res. 1994;74:189 –196.
23. Lemire JM, Covin CW, White S, Giachelli CM, Schwartz SM. Characterization of cloned aortic smooth muscle cells from young rats. Am J
Pathol. 1994;144:1068 –1081.
24. Villaschi S, Nicosia RF, Smith MR. Isolation of a morphologically and
functionally distinct smooth muscle cell type from the intimal aspect of
the normal rat aorta; evidence for smooth muscle cell heterogeneity. In
Vitro Cell Dev Biol Anim. 1994;30A:589 –595.
25. Lau HK. Regulation of proteolytic enzymes and inhibitors in two
smooth muscle cell phenotypes. Cardiovasc Res. 1999;43:1049 –1059.
26. Li WG, Miller FJ Jr, Brown MR, Chatterjee P, Aylsworth GR, Shao J,
Spector AA, Oberley LW, Weintraub NL. Enhanced H2O2-induced cytotoxicity in ‘epithelioid’ smooth muscle cells: implications for neointimal
regression. Arterioscler Thromb Vasc Biol. 2000;20:1473–1479.
27. Holifield B, Helgason T, Jemelka S, Taylor A, Navran S, Allen J, Seidel
C. Differentiated vascular myocytes: are they involved in neointimal
formation? J Clin Invest. 1996;97:814 – 825.
28. Frid MG, Aldashev AA, Dempsey EC, Stenmark KR. Smooth muscle
cells isolated from discrete compartments of the mature vascular media
exhibit unique phenotypes and distinct growth capabilities. Circ Res.
1997;81:940 –952.
29. Hao H, Ropraz P, Verin V, Camenzind E, Geinoz A, Pepper MS,
Gabbiani G, Bochaton-Piallat ML. Heterogeneity of smooth muscle cell
1518
30.
31.
32.
33.
34.
35.
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
Arterioscler Thromb Vasc Biol.
September 2003
populations cultured from pig coronary artery. Arterioscler Thromb
Vasc Biol. 2002;22:1093–1099.
Benzakour O, Kanthou C, Kanse SM, Scully MF, Kakkar VV, Cooper
DN. Evidence for cultured human vascular smooth muscle cell heterogeneity: isolation of clonal cells and study of their growth characteristics. Thromb Haemost. 1996;75:854 – 858.
Li S, Sims S, Jiao Y, Chow LH, Pickering JG. Evidence from a novel
human cell clone that adult vascular smooth muscle cells can convert
reversibly between noncontractile and contractile phenotypes. Circ Res.
1999;85:338 –348.
Li S, Fan YS, Chow LH, Van Den Diepstraten C, van Der Veer E, Sims
SM, Pickering JG. Innate diversity of adult human arterial smooth
muscle cells: cloning of distinct subtypes from the internal thoracic
artery. Circ Res. 2001;89:517–525.
Bochaton-Piallat ML, Gabbiani F, Ropraz P, Gabbiani G. Cultured
aortic smooth muscle cells from newborn and adult rats show distinct
cytoskeletal features. Differentiation. 1992;49:175–185.
Haudenschild CC, Grünwald J. Proliferative heterogeneity of vascular
smooth muscle cells and its alteration by injury. Exp Cell Res. 1985;
157:364 –370.
Skalli O, Bloom WS, Ropraz P, Azzarone B, Gabbiani G. Cytoskeletal
remodeling of rat aortic smooth muscle cells in vitro: relationships to
culture conditions and analogies to in vivo situations. J Submicrosc
Cytol Pathol. 1986;18:481– 493.
Hariri RJ, Alonso DR, Hajjar DP, Coletti D, Weksler ME. Aging and
arteriosclerosis, I: development of myointimal hyperplasia after endothelial injury. J Exp Med. 1986;164:1171–1178.
Stemerman MB, Weinstein R, Rowe JW, Maciag T, Fuhro R, Gardner
R. Vascular smooth muscle cell growth kinetics in vivo in aged rats.
Proc Natl Acad Sci U S A. 1982;79:3863–3866.
Chen L, Daum G, Fischer JW, Hawkins S, Bochaton-Piallat ML, Gabbiani G,
Clowes AW. Loss of expression of the -subunit of soluble guanylyl cyclase
prevents nitric oxide–mediated inhibition of DNA synthesis in smooth muscle
cells of old rats. Circ Res. 2000;86:520–525.
Ehler E, Jat PS, Noble MD, Citi S, Draeger A. Vascular smooth muscle
cells of H-2Kb-tsA58 transgenic mice: characterization of cell lines with
distinct properties. Circulation. 1995;92:3289 –3296.
Hall KL, Harding JW, Hosick HL. Isolation and characterization of clonal
vascular smooth muscle cell lines from spontaneously hypertensive and normotensive rat aortas. In Vitro Cell Dev Biol. 1991;27:791–798.
Frid MG, Moiseeva EP, Stenmark KR. Multiple phenotypically distinct
smooth muscle cell populations exist in the adult and developing bovine
pulmonary arterial media in vivo. Circ Res. 1994;75:669 – 681.
Christen T, Bochaton-Piallat ML, Neuville P, Rensen S, Redard M, van Eys
G, Gabbiani G. Cultured porcine coronary artery smooth muscle cells: a
new model with advanced differentiation. Circ Res. 1999;85:99–107.
Chamley-Campbell JH, Campbell GR, Ross R. Phenotype-dependent
response of cultured aortic smooth muscle to serum mitogens. J Cell
Biol. 1981;89:379 –383.
Patel S, Shi Y, Niculescu R, Chung EH, Martin JL, Zalewski A.
Characteristics of coronary smooth muscle cells and adventitial fibroblasts. Circulation. 2000;101:524 –532.
Orekhov AN, Karpova II, Tertov VV, Rudchenko SA, Andreeva ER,
Krushinsky AV, Smirnov VN. Cellular composition of atherosclerotic
and uninvolved human aortic subendothelial intima: light-microscopic
study of dissociated aortic cells. Am J Pathol. 1984;115:17–24.
Orekhov AN, Andreeva ER, Krushinsky AV, Novikov ID, Tertov VV,
Nestaiko GV, Khashimov KhA, Repin VS, Smirnov VN. Intimal cells
and atherosclerosis: relationship between the number of intimal cells and
major manifestations of atherosclerosis in the human aorta. Am J Pathol.
1986;125:402– 415.
Orekhov AN, Krushinsky AV, Andreeva ER, Repin VS, Smirnov VN.
Adult human aortic cells in primary culture: heterogeneity in shape.
Heart Vessels. 1986;2:193–201.
Björkerud S. Cultivated human arterial smooth muscle displays heterogeneous pattern of growth and phenotypic variation. Lab Invest. 1985;
53:303–310.
Bonin LR, Madden K, Shera K, Ihle J, Matthews C, Aziz S, Perez-Reyes
N, McDougall JK, Conroy SC. Generation and characterization of
human smooth muscle cell lines derived from atherosclerotic plaque.
Arterioscler Thromb Vasc Biol. 1999;19:575–587.
Llorente-Cortes V, Martinez-Gonzalez J, Badimon L. Differential cholesteryl ester accumulation in two human vascular smooth muscle cell
subpopulations exposed to aggregated LDL: effect of PDGF-stimulation
and HMG-CoA reductase inhibition. Atherosclerosis. 1999;144:335–342.
51. Martinez-Gonzalez J, Berrozpe M, Varela O, Badimon L. Heterogeneity
of smooth muscle cells in advanced human atherosclerotic plaques:
intimal smooth muscle cells expressing a fibroblast surface protein are
highly activated by platelet-released products. Eur J Clin Invest. 2001;
31:939 –949.
52. Bochaton-Piallat ML, Clowes AW, Clowes MM, Fischer JW, Redard M,
Gabbiani F, Gabbiani G. Cultured arterial smooth muscle cells maintain
distinct phenotypes when implanted into carotid artery. Arterioscler
Thromb Vasc Biol. 2001;21:949 –954.
53. Grünwald J, Haudenschild CC. Intimal injury in vivo activates vascular
smooth muscle cell migration and explant outgrowth in vitro. Arteriosclerosis. 1984;4:183–188.
54. Schwartz SM, Foy L, Bowen-Pope DF, Ross R. Derivation and properties of platelet-derived growth factor-independent rat smooth muscle
cells. Am J Pathol. 1990;136:1417–1428.
55. McCaffrey TA, Falcone DJ. Evidence for an age-related dysfunction in
the antiproliferative response to transforming growth factor- in
vascular smooth muscle cells. Mol Biol Cell. 1993;4:315–322.
56. Topouzis S, Majesky MW. Smooth muscle lineage diversity in the chick
embryo: two types of aortic smooth muscle cell differ in growth and
receptor-mediated transcriptional responses to transforming growth
factor-. Dev Biol. 1996;178:430 – 445.
57. Li Z, Cheng H, Lederer WJ, Froehlich J, Lakatta EG. Enhanced proliferation and migration and altered cytoskeletal proteins in early passage
smooth muscle cells from young and old rat aortic explants. Exp Mol
Pathol. 1997;64:1–11.
58. Bochaton-Piallat M-L, Gabbiani G, Pepper MS. Plasminogen activator
expression in rat arterial smooth muscle cells depends on their phenotype and is modulated by cytokines. Circ Res. 1998;82:1086 –1093.
59. Clowes AW, Clowes MM, Au YP, Reidy MA, Belin D. Smooth muscle cells
express urokinase during mitogenesis and tissue-type plasminogen activator
during migration in injured rat carotid artery. Circ Res. 1990;67:61–67.
60. Reidy MA, Irvin C, Lindner V. Migration of arterial wall cells:
expression of plasminogen activators and inhibitors in injured rat
arteries. Circ Res. 1996;78:405– 414.
61. Carmeliet P, Moons L, Herbert JM, Crawley J, Lupu F, Lijnen R, Collen
D. Urokinase but not tissue plasminogen activator mediates arterial
neointima formation in mice. Circ Res. 1997;81:829 – 839.
62. Lupu F, Heim DA, Bachmann F, Hurni M, Kakkar VV, Kruithof EK.
Plasminogen activator expression in human atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 1995;15:1444 –1455.
63. Noda-Heiny H, Daugherty A, Sobel BE. Augmented urokinase receptor
expression in atheroma. Arterioscler Thromb Vasc Biol. 1995;15:37– 43.
64. Raghunath PN, Tomaszewski JE, Brady ST, Caron RJ, Okada SS,
Barnathan ES. Plasminogen activator system in human coronary atherosclerosis. Arterioscler Thromb Vasc Biol. 1995;15:1432–1443.
65. Steins MB, Padro T, Li CX, Mesters RM, Ostermann H, Hammel D,
Scheld HH, Berdel WE, Kienast J. Overexpression of tissue-type plasminogen activator in atherosclerotic human coronary arteries. Atherosclerosis. 1999;145:173–180.
66. Kocher O, Gabbiani G. Cytoskeletal features of normal and atheromatous
human arterial smooth muscle cells. Hum Pathol. 1986;17:875–880.
67. Schwartz SM, deBlois D, O’Brien ER. The intima: soil for atherosclerosis and restenosis. Circ Res. 1995;77:445– 465.
68. Shanahan CM, Weissberg PL. Smooth muscle cell heterogeneity:
patterns of gene expression in vascular smooth muscle cells in vitro and
in vivo. Arterioscler Thromb Vasc Biol. 1998;18:333–338.
69. Owens GK. Molecular control of vascular smooth muscle cell differentiation. Acta Physiol Scand. 1998;164:623– 635.
70. Sartore S, Franch R, Roelofs M, Chiavegato A. Molecular and cellular
phenotypes and their regulation in smooth muscle. Rev Physiol Biochem
Pharmacol. 1999;134:235–320.
71. Skalli O, Ropraz P, Trzeciak A, Benzonana G, Gillessen D, Gabbiani G.
A monoclonal antibody against ␣-smooth muscle actin: a new probe for
smooth muscle differentiation. J Cell Biol. 1986;103:2787–2796.
72. Owens GK. Regulation of differentiation of vascular smooth muscle
cells. Physiol Rev. 1995;75:487–517.
73. Campbell JH, Reardon MF, Campbell GR, Nestel PJ. Metabolism of
atherogenic lipoproteins by smooth muscle cells of different phenotype
in culture. Arteriosclerosis. 1985;5:318 –328.
74. Parlavecchia M, Skalli O, Gabbiani G. LDL accumulation in cultured rat
aortic smooth muscle cells with different cytoskeletal phenotypes. J
Vasc Med Biol. 1989;1:308 –313.
75. Thyberg J. Caveolae and cholesterol distribution in vascular smooth muscle
cells of different phenotypes. J Histochem Cytochem. 2002;50:185–195.
Hao et al
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
76. Dusserre E, Bourdillon MC, Pulcini T, Berthezene F. Decrease in high
density lipoprotein binding sites is associated with decrease in intracellular cholesterol efflux in dedifferentiated aortic smooth muscle cells.
Biochim Biophys Acta. 1994;1212:235–244.
77. Orlandi A, Francesconi A, Cocchia D, Corsini A, Spagnoli LG. Phenotypic heterogeneity influences apoptotic susceptibility to retinoic acid
and cis-platinum of rat arterial smooth muscle cells in vitro: implications
for the evolution of experimental intimal thickening. Arterioscler
Thromb Vasc Biol. 2001;21:1118 –1123.
78. Chan SW, Hegyi L, Scott S, Cary NR, Weissberg PL, Bennett MR.
Sensitivity to Fas-mediated apoptosis is determined below receptor level
in human vascular smooth muscle cells. Circ Res. 2000;86:1038 –1046.
79. Kockx MM, Herman AG. Apoptosis in atherosclerosis: beneficial or
detrimental? Cardiovasc Res. 2000;45:736 –746.
80. McCarthy NJ, Bennett MR. The regulation of vascular smooth muscle
cell apoptosis. Cardiovasc Res. 2000;45:747–755.
81. Geng YJ, Libby P. Progression of atheroma: a struggle between death
and procreation. Arterioscler Thromb Vasc Biol. 2002;22:1370 –1380.
82. Cremona O, Muda M, Appel RD, Frutiger S, Hughes GJ, Hochstrasser
DF, Geinoz A, Gabbiani G. Differential protein expression in aortic
smooth muscle cells cultured from newborn and aged rats. Exp Cell Res.
1995;217:280 –287.
83. Neuville P, Geinoz A, Benzonana G, Redard M, Gabbiani F, Ropraz P,
Gabbiani G. Cellular retinol-binding protein-1 is expressed by distinct
subsets of rat arterial smooth muscle cell in vitro and in vivo. Am J
Pathol. 1997;150:509 –521.
84. Bochaton-Piallat ML, Gabbiani F, Redard M, Desmouliere A, Gabbiani
G. Apoptosis participates in cellularity regulation during rat aortic
intimal thickening. Am J Pathol. 1995;146:1059 –1064.
85. Han DK, Haudenschild CC, Hong MK, Tinkle BT, Leon MB, Liau G.
Evidence for apoptosis in human atherogenesis and in a rat vascular
injury model. Am J Pathol. 1995;147:267–277.
86. Perlman H, Maillard L, Krasinski K, Walsh K. Evidence for the rapid
onset of apoptosis in medial smooth muscle cells after balloon injury.
Circulation. 1997;95:981–987.
87. Adams LD, Lemire JM, Schwartz SM. A systematic analysis of 40
random genes in cultured vascular smooth muscle subtypes reveals a
heterogeneity of gene expression and identifies the tight junction gene
zonula occludens 2 as a marker of epithelioid ‘pup’ smooth muscle cells
and a participant in carotid neointimal formation. Arterioscler Thromb
Vasc Biol. 1999;19:2600 –2608.
88. Jahn L, Kreuzer J, von Hodenberg E, Kubler W, Franke WW, Allenberg
J, Izumo S. Cytokeratins 8 and 18 in smooth muscle cells: detection in
human coronary artery, peripheral vascular, and vein graft disease and in
transplantation-associated arteriosclerosis. Arterioscler Thromb. 1993;
13:1631–1639.
89. Giachelli C, Bae N, Lombardi D, Majesky M, Schwartz S. Molecular
cloning and characterization of 2B7, a rat mRNA which distinguishes
smooth muscle cell phenotypes in vitro and is identical to osteopontin
(secreted phosphoprotein I, 2aR). Biochem Biophys Res Commun. 1991;
177:867– 873.
90. Gadeau AP, Campan M, Millet D, Candresse T, Desgranges C.
Osteopontin overexpression is associated with arterial smooth muscle
cell proliferation in vitro. Arterioscler Thromb. 1993;13:120 –125.
91. Giachelli CM, Bae N, Almeida M, Denhardt DT, Alpers CE, Schwartz
SM. Osteopontin is elevated during neointima formation in rat arteries
and is a novel component of human atherosclerotic plaques. J Clin
Invest. 1993;92:1686 –1696.
92. Shanahan CM, Weissberg PL, Metcalfe JC. Isolation of gene markers of
differentiated and proliferating vascular smooth muscle cells. Circ Res.
1993;73:193–204.
93. Giachelli CM, Majesky MW, Schwartz SM. Developmentally regulated
cytochrome P-450IA1 expression in cultured rat vascular smooth muscle
cells. J Biol Chem. 1991;266:3981–3986.
94. Liaw L, Almeida M, Hart CE, Schwartz SM, Giachelli CM. Osteopontin
promotes vascular cell adhesion and spreading and is chemotactic for
smooth muscle cells in vitro. Circ Res. 1994;74:214 –224.
95. Chaulet H, Desgranges C, Renault MA, Dupuch F, Ezan G, Peiretti F,
Loirand G, Pacaud P, Gadeau AP. Extracellular nucleotides induce
arterial smooth muscle cell migration via osteopontin. Circ Res. 2001;
89:772–778.
96. Gadeau AP, Chaulet H, Daret D, Kockx M, Daniel-Lamaziere JM,
Desgranges C. Time course of osteopontin, osteocalcin, and osteonectin
accumulation and calcification after acute vessel wall injury. J Histochem Cytochem. 2001;49:79 – 86.
Smooth Muscle Cell Heterogeneity
1519
97. Hirota S, Imakita M, Kohri K, Ito A, Morii E, Adachi S, Kim HM,
Kitamura Y, Yutani C, Nomura S. Expression of osteopontin messenger
RNA by macrophages in atherosclerotic plaques: a possible association
with calcification. Am J Pathol. 1993;143:1003–1008.
98. Fitzpatrick LA, Severson A, Edwards WD, Ingram RT. Diffuse calcification in human coronary arteries: association of osteopontin with atherosclerosis. J Clin Invest. 1994;94:1597–1604.
99. O’Brien ER, Garvin MR, Stewart DK, Hinohara T, Simpson JB, Schwartz SM,
Giachelli CM. Osteopontin is synthesized by macrophage, smooth muscle, and
endothelial cells in primary and restenotic human coronary atherosclerotic
plaques. Arterioscler Thromb. 1994;14:1648–1656.
100. Steitz SA, Speer MY, Curinga G, Yang HY, Haynes P, Aebersold R, Schinke
T, Karsenty G, Giachelli CM. Smooth muscle cell phenotypic transition associated with calcification: upregulation of Cbfa1 and downregulation of smooth
muscle lineage markers. Circ Res. 2001;89:1147–1154.
101. Weiser-Evans MC, Schwartz PE, Grieshaber NA, Quinn BE, Grieshaber
SS, Belknap JK, Mourani PM, Majack RA, Stenmark KR. Novel
embryonic genes are preferentially expressed by autonomously replicating rat embryonic and neointimal smooth muscle cells. Circ Res.
2000;87:608 – 615.
102. Frid MG, Aldashev AA, Nemenoff RA, Higashito R, Westcott JY,
Stenmark KR. Subendothelial cells from normal bovine arteries exhibit
autonomous growth and constitutively activated intracellular signaling.
Arterioscler Thromb Vasc Biol. 1999;19:2884 –2893.
103. de Vries CJ, van Achterberg TA, Horrevoets AJ, ten Cate JW,
Pannekoek H. Differential display identification of 40 genes with altered
expression in activated human smooth muscle cells: local expression in
atherosclerotic lesions of smags, smooth muscle activation-specific
genes. J Biol Chem. 2000;275:23939 –23947.
104. Blindt R, Vogt F, Lamby D, Zeiffer U, Krott N, Hilger-Eversheim K,
Hanrath P, vom Dahl J, Bosserhoff AK. Characterization of differential
gene expression in quiescent and invasive human arterial smooth muscle
cells. J Vasc Res. 2002;39:340 –352.
105. Geary RL, Wong JM, Rossini A, Schwartz SM, Adams LD. Expression
profiling identifies 147 genes contributing to a unique primate neointimal smooth muscle cell phenotype. Arterioscler Thromb Vasc Biol.
2002;22:2010 –2016.
106. Qin M, Zeng Z, Zheng J, Shah PK, Schwartz SM, Adams LD, Sharifi
BG. Suppression subtractive hybridization identifies distinctive
expression markers for coronary and internal mammary arteries. Arterioscler Thromb Vasc Biol. 2003;23:425– 433.
107. Kohler A, Jostarndt-Fogen K, Rottner K, Alliegro MC, Draeger A.
Intima-like smooth muscle cells: developmental link between endothelium and media? Anat Embryol (Berl). 1999;200:313–323.
108. Nicosia RF, Villaschi S. Rat aortic smooth muscle cells become
pericytes during angiogenesis in vitro. Lab Invest. 1995;73:658 – 666.
109. van Royen N, Piek JJ, Buschmann I, Hoefer I, Voskuil M, Schaper W.
Stimulation of arteriogenesis: a new concept for the treatment of arterial
occlusive disease. Cardiovasc Res. 2001;49:543–553.
110. Verfaillie CM. Adult stem cells: assessing the case for pluripotency.
Trends Cell Biol. 2002;12:502–508.
111. Frid MG, Kale VA, Stenmark KR. Mature vascular endothelium can
give rise to smooth muscle cells via endothelial-mesenchymal transdifferentiation: in vitro analysis. Circ Res. 2002;90:1189 –1196.
112. Shimizu K, Sugiyama S, Aikawa M, Fukumoto Y, Rabkin E, Libby P,
Mitchell RN. Host bone-marrow cells are a source of donor intimal
smooth-muscle-like cells in murine aortic transplant arteriopathy. Nat
Med. 2001;7:738 –741.
113. Religa P, Bojakowski K, Maksymowicz M, Bojakowska M, Sirsjo A,
Gaciong Z, Olszewski W, Hedin U, Thyberg J. Smooth-muscle progenitor cells of bone marrow origin contribute to the development of
neointimal thickenings in rat aortic allografts and injured rat carotid
arteries. Transplantation. 2002;74:1310 –1315.
114. Campbell JH, Han CL, Campbell GR. Neointimal formation by circulating bone marrow cells. Ann N Y Acad Sci. 2001;947:18 –24.
115. Sata M, Saiura A, Kunisato A, Tojo A, Okada S, Tokuhisa T, Hirai H,
Makuuchi M, Hirata Y, Nagai R. Hematopoietic stem cells differentiate
into vascular cells that participate in the pathogenesis of atherosclerosis.
Nat Med. 2002;8:403– 409.
116. Karnovsky MJ, Wright TC Jr, Castellot JJ Jr, Choay J, Lormeau JC,
Petitou M. Heparin, heparan sulfate, smooth muscle cells, and atherosclerosis. Ann N Y Acad Sci. 1989;556:268 –281.
117. Au YP, Kenagy RD, Clowes MM, Clowes AW. Mechanisms of inhibition by heparin of vascular smooth muscle cell proliferation and
migration. Haemostasis. 1993;23(suppl 1):177–182.
1520
Arterioscler Thromb Vasc Biol.
September 2003
118. Orlandi A, Ropraz P, Gabbiani G. Proliferative activity and ␣-smooth
muscle actin expression in cultured rat aortic smooth muscle cells are
differently modulated by transforming growth factor-1 and heparin.
Exp Cell Res. 1994;214:528 –536.
119. Neuville P, Yan Z, Gidlof A, Pepper MS, Hansson GK, Gabbiani G, Sirsjo A.
Retinoic acid regulates arterial smooth muscle cell proliferation and phenotypic
features in vivo and in vitro through an RAR␣-dependent signaling pathway.
Arterioscler Thromb Vasc Biol. 1999;19:1430–1436.
120. Miano JM, Kelly LA, Artacho CA, Nuckolls TA, Piantedosi R, Blaner
WS. All-trans-retinoic acid reduces neointimal formation and promotes
favorable geometric remodeling of the rat carotid artery after balloon
withdrawal injury. Circulation. 1998;98:1219 –1227.
121. DeRose JJ Jr, Madigan J, Umana JP, Prystowsky JH, Nowygrod R,
Oz MC, Todd GJ. Retinoic acid suppresses intimal hyperplasia and
prevents vessel remodeling following arterial injury. Cardiovasc
Surg. 1999;7:633– 639.
122. Yan ZQ, Sirsjo A, Bochaton-Piallat ML, Gabbiani G, Hansson GK.
Augmented expression of inducible NO synthase in vascular smooth
muscle cells during aging is associated with enhanced NF-B activation.
Arterioscler Thromb Vasc Biol. 1999;19:2854 –2862.
123. Peiro C, Redondo J, Rodriguez-Martinez MA, Angulo J, Marin J,
Sanchez-Ferrer CF. Influence of endothelium on cultured vascular
smooth muscle cell proliferation. Hypertension. 1995;25:748 –751.
124. Nackman GB, Bech FR, Fillinger MF, Wagner RJ, Cronenwett JL. Endothelial
cells modulate smooth muscle cell morphology by inhibition of transforming
growth factor-1 activation. Surgery. 1996;120:418–425.
125. Fillinger MF, Sampson LN, Cronenwett JL, Powell RJ, Wagner RJ.
Coculture of endothelial cells and smooth muscle cells in bilayer and
conditioned media models. J Surg Res. 1997;67:169 –178.
126. Vernon SM, Campos MJ, Haystead T, Thompson MM, DiCorleto PE,
Owens GK. Endothelial cell-conditioned medium downregulates
smooth muscle contractile protein expression. Am J Physiol. 1997;272:
C582–C591.
127. Petzelbauer E, Springhorn JP, Tucker AM, Madri JA. Role of plasminogen activator inhibitor in the reciprocal regulation of bovine aortic
endothelial and smooth muscle cell migration by TGF-1. Am J Pathol.
1996;149:923–931.
128. Powell RJ, Bhargava J, Basson MD, Sumpio BE. Coculture conditions
alter endothelial modulation of TGF-1 activation and smooth muscle
growth morphology. Am J Physiol. 1998;274:H642–H649.
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
Downloaded from http://atvb.ahajournals.org/ by guest on October 1, 2016
Arterial Smooth Muscle Cell Heterogeneity: Implications for Atherosclerosis and Restenosis
Development
Hiroyuki Hao, Giulio Gabbiani and Marie-Luce Bochaton-Piallat
Arterioscler Thromb Vasc Biol. 2003;23:1510-1520; originally published online August 7, 2003;
doi: 10.1161/01.ATV.0000090130.85752.ED
Arteriosclerosis, Thrombosis, and Vascular Biology is published by the American Heart Association, 7272 Greenville
Avenue, Dallas, TX 75231
Copyright © 2003 American Heart Association, Inc. All rights reserved.
Print ISSN: 1079-5642. Online ISSN: 1524-4636
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://atvb.ahajournals.org/content/23/9/1510
Data Supplement (unedited) at:
http://atvb.ahajournals.org/content/suppl/2003/09/15/23.9.1510.DC1.html
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in
Arteriosclerosis, Thrombosis, and Vascular Biology can be obtained via RightsLink, a service of the Copyright
Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is
being requested is located, click Request Permissions in the middle column of the Web page under Services.
Further information about this process is available in the Permissions and Rights Question and Answerdocument.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Arteriosclerosis, Thrombosis, and Vascular Biology is online at:
http://atvb.ahajournals.org//subscriptions/