Proposed USP Chapter <797>
Changes are coming!
Published Sept 25, 2015
Presented by Eric S. Kastango, MBA, RPh, FASHP
Copyright © 2008-2016
1999 -2016CriticalPoint,
2008-2014
ClinicalIQ,
Clinical IQ,LLC®
LLC®
LLC®
- -All
All
- All
Rights
Rights
Rights
Reserved
Reserved
Reserved
I am speaking in my individual capacity and
not as a representative of any organization or committee regardless
of my status, membership or affiliations with any entity.
The views and opinions presented are entirely my own.
They do not necessarily reflect the views of any other organization I
may be associated with, nor should they be construed as an
“official” explanation or interpretation of any USP chapter or any
State Board of Pharmacy rule/law.
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Scope of USP <797>
Compounded sterile preparations affected are:
• Injections
• Aqueous bronchial inhalations
• Baths and soaks for live organs and tissues
• Irrigation solutions for internal body cavities*
• Nasal/Sinus solutions does not have to be sterile, just clean (USP 795)
• Ophthalmics
• Implants
– Pellets
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
3
Who does the chapter apply to?
• Applies to
– all persons who prepare CSPs
– all places where CSPs are prepared
– pre-administration manipulations of CSPs including
storage, compounding, and transport
• Does not apply to administration!
• Specific chapter language:
– “shall” is a requirement (must)
– “should” is a recommendation
• Note: 503b outsourcing sterile compounding
facilities will be expected to comply with FDA cGMP
regulations
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Mission of Chapter: To Prevent Harm
• Microbial contamination
• Excessive bacterial endotoxins
• Variability in intended strength that
exceed monograph limits
• Use of ingredients of inappropriate quality
• Unintended physical and chemical
contaminants
Courtesy CBS News
This is a image of the fungus growing from a
sample taken from a patient’s spinal fluid.
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
USP Chapter <797>
• Enforceable by the FDA and 28 State
Boards of Pharmacy (more or less)
• Based on current scientific information
and best sterile compounding practices
• Recognized as the national standard of
• Included in TJC and other accreditation
organization requirements only if their
standards address sterile compounding
• Minimum practice and quality standards
for compounding sterile preparations
practice
Published
11/2003
Official
1/2004
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Revision
released
12/2007
Official
6/2008
Out for Public
Comment
9/2015
Proposed USP <797>
Summary of Major Changes:
3 risk levels changed to 2 categories distinguished
by conditions under which they are made and time
within which used
Removal of HD handling section and cross-referenced
to USP 800
Quarterly requirement for Personnel Monitoring
(visual observation of hand hygiene and garbing,
MFT and ongoing GFS)
Monthly requirement for Viable Air sampling and
Surface sampling
BUD and Storage times changed with a maximum
BUD of 45 days regardless of sterility testing
Introduction of “In-Use time” (time before which
conventionally manufactured product or compounded
dilution bag must be used after it is punctured)
Master formulation and compounding records will
be required for all batch and non-sterile
compounding
New guidance for sterility testing of CSP prepared in
batch sizes of less than 40. (10% rule)
New placement requirements on use of isolators
Requirement for sterile gloves and sterile sleeves,
sterile wipers and cleaning tools that need to be resterilized but not sterile disinfectants
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Definitions and Practice Issues
• Current USP Chapter <797> rejects this statement
“Compounding does not include mixing, reconstituting, or similar acts that are
performed in accordance with the directions contained in approved labeling
provided by the product's manufacturer and other manufacturer directions
consistent with that labeling” [21 USC 321 (k) and (m)].
• For one patient for immediate administration a function of medication
administration
– This is fundamentally low-risk compounding
• Batching <797> applies
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Briefing of Proposed Changes
• Reorganized, redundancies eliminated, and requirements clarified
• Minor editorial changes have been made to update the chapter to current
USP style.
• Organized in a similar manner as 21 CFR Part 211 – US FDA CGMPs
• Key procedures placed in boxes for reference
• All sample documents and media procedures removed
• Hazardous Drug requirements referred to USP <800>
• Allergen extracts no longer given a carve-out
• Radiopharmaceuticals still need to comply with USP 797
• Administration is still out of scope – defer to CDC guidance
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Current BUD Paradigm
• Applied only to pre-administration activities (handling, compounding and
storage)
– Once CSP was administered, then USP 797 was no longer applicable
• Chemical Stability must be assured during the use of the CSP
• Not capped: USP 71 Sterility Test passed has allowed BUD to chemical
stability of the drug.
– Not Closure-Container Integrity Test required
• Current USP 797 is silent on the requirements for compounding multi-dose
vials/containers
– USP <51> Antimicrobial Effectiveness Test
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
New Proposed BUD Paradigm
• NEW DEFINITION: The date or time after which a CSP cannot be used and
must be discarded.
• The BUD is determined from the time the CSP is compounded.
– One day is equivalent to 24 hours.
• BUDs is capped to 42 days refrigerated
• Closure-Container Integrity Test required for frozen CSPs
• CSPs that are made as a MDV must undergo USP <51> Antimicrobial
Effectiveness Testing
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
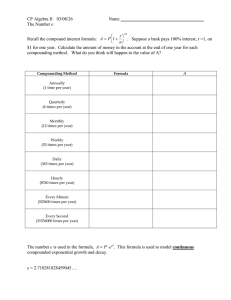
Flowchart of BUDs
1.
2.
3.
4.
5.
Aseptically-prepared or terminally-sterilized?
Sterility test performed?
Preservative added?
Only sterile components or any nonsterile component?
Storage temperature
A. Controlled Room Temperature
B. Refrigerator
C. Freezer
Changes in BUDs are based on increasing the frequency
of monitoring personnel and the environment
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Proposed USP 797: Category 1 CSPs
PEC placement
Not in ISO classified air
Sterility Testing
Not required
Endotoxin Testing
Not required
BUD
≤ 12 hours room temperature or ≤ 24 hours
refrigerated
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Proposed USP 797: Storage for Category 2 CSPs
PEC placement
Placed in ISO classified air
Sterility Testing
Based on BUD Assignment below
Endotoxin Testing Not required if sterile components
Storage
Method
Terminally
Sterilized CSPs
Aseptically
Prepared CSPs
BUD Assignment
> 12 hour room temperature or > than 24 hours refrigerated
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Sterility Testing
Preservative
Added
No
No
Controlled
Room
Refrigerated
Frozen
Made from 1 or more non sterile components
4 days
7 days
45 days
Made with only sterile components
Yes
No
Yes
6 days
9 days
Yes (USP 51)
28 days
42 days
No
28 days
42 days
Yes (USP 51)
42 days
42 days
No
14 days
28 days
Yes (USP 51)
28 days
42 days
No
28 days
42 days
Yes (USP 51)
42 days
45 days
45 days
45 days
In-Use Time
The time before which a conventionally manufactured
product used to make a CSP must be used after it has
been opened or punctured, or a CSP must be used after
it has been opened or punctured.
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
In-Use Times
Conventionally Manufactured Products Opened, Stored, and Used for Sterile Compounding
in ISO Class 5 or Better Air Quality
Components
In-Use Time
Ampuls
Use immediately after opening and passing through a
sterile particulate filter
Pharmacy Bulk Package
As specified by the manufacturer
Single-dose container (e.g., bag, bottle,
syringe, or vial)
6 hours
Multiple-dose container
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
28 days, unless otherwise specified by the
manufacturer
In-Use Times
CSPs Opened, Stored, and Used for Sterile Compounding in ISO Class 5 or Better Air Quality
Components
In-Use Time
Compounded Single-Dose Container
Use for single patient immediately; discard remainder
Compounded Stock Solutions
6 hours
Compounded Multiple Dose Containers1
28 hours, unless otherwise specified by the original
compounder
1The particular
CSP formulation must pass antimicrobial effectiveness testing in accordance with (51) at the
completion of the sterility test (if conducted) or at the time of preparation (if sterility testing is not
performed). The test must be completed and the results obtained on the specific formulation before any of
the CSP is released or dispensed. The test needs to be conducted only once on each formulation in the
particular container–closure system in which it will be stored or released/dispensed.
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Preparation of Dilutions: BUD Decision Tree*
General Example
*This example uses pooling however pooling is not always necessary.
OR
Step 1
Combine Single Dose
Vials
Copyright © 2008-2016 CriticalPoint, LLC® - All Rights Reserved
Step 2
SDVs combined to make Medium Risk CSP
This is source vial/bag for additional doses
Make it the right size so that it will be used up < 8 days
Step 3
Final CSP to Patient
Use within 24 hours and
do NOT recycle
Core Personnel Competencies
Training to establish the following competencies must be completed before
compounding:
• Hand hygiene and garbing
• Cleaning and disinfection
• Measuring and mixing
• Aseptic manipulation
• Proper clean room behavior
• Methods of sterilization and depyrogenation
• Use of compounding equipment
• Documentation
• Understanding air flow patterns
• Proper use of primary engineering controls
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
19
Personnel Garbing for Compounding
CSP Category
PEC type
Category 1
Any
Minimum Requirement
Non-cotton, low-lint, disposable gown or coveralls
Low-lint, disposable covers for shoes
Low-lint, disposable covers for head and facial hair that cover
the ears and forehead
Sterile gloves and sterile sleeves1
Laminar airflow
Non-cotton, low-lint, disposable gowns or coveralls
Category 2
system (LAFS) and
Low-lint, disposable covers for shoes
biological safety cabinet
Low-lint, disposable covers for head and
(BSC)
facial hair that cover the ears and forehead
Mask
Sterile gloves and sterile sleeves1
Eye shield is optional
RABS (CAI or CACI) or
Category 2
Non-cotton, low-lint, disposable gowns or coveralls
isolator
Low-lint, disposable covers for shoes and hair
Sterile gloves
1 Compounding or repackaging must not occur in worse than ISO Class 5 air.
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Garbing changes/clarifications
• Remove all cosmetics because they shed flakes and particles
• Remove all hand, wrist, and other exposed jewelry or piercings (e.g., rings,
watches, bracelets, earrings, and lip or eyebrow rings) that can interfere with
the effectiveness of PPE (e.g., fit of gloves, cuffs of sleeves, and eye
protection)
• Cover any jewelry that cannot be removed (e.g., surgically implanted jewelry)
must be covered
• Ear buds, headphones, and cell phones, or other similar devices are not
permitted in the cleanroom
• Dry hands and forearms with either low-lint disposable towels or wipes. No
hand dryers mentioned
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Environmental Monitoring – Facility Related Metrics
Test
Current
Proposed
Non-viable air sampling
Every six months
Every six months
Viable air sampling
Every six months
Quarterly
Periodic
Monthly
Surface sampling
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Personnel Monitoring
Test
Media fill
Current
• Annually if only low/medium risk
compounded
• Semiannually if high risk
compounded
Failed test
• Requalification
Gloved fingertip test • Annually if only low/medium risk
(following initial
compounded
test)
• Semiannually if high risk
compounded
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Proposed
Quarterly
Any failed competency must
be repeated 3 times prior to
restarting
Quarterly
Primary Engineering Controls
• Laminar Air Flow Systems (LAFS)
– Laminar Air Flow Workbenches
– Laminar Air Flow zones
– Biological Safety Cabinets (BSC)
• Restricted Access Barrier System(RABS)
– Compounding aseptic isolator (CAI)
– Compounding aseptic containment isolator (CACI)
• Isolators
– Transfer ports
– Use sporicidal chemical decontamination
– Constant overpressure requirement
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Sterile gloves are
required when working
in a RAB or isolator!
Secondary Engineering Controls
• Segregated Compounding Area
• Category 1 CSPs
(SCA)
• Positive pressure buffer room with
access through a positive pressure
anteroom
• Category 2 CSPs
To meet Category 2, any PEC must be located in an ISO Class 7 area
The use of displacement airflow is NOT permitted
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Facility Design Requirements
• The surfaces of ceilings, walls, floors, fixtures, shelving, counters, and
cabinets in a classified area or in a segregated compounding area must be
smooth, impervious, free from cracks and crevices, and non-shedding,
thereby promoting cleanability and minimizing spaces in which
microorganisms and other contaminants can accumulate.
• The buffer area or area inside the perimeter of a segregated compounding
area cannot contain water sources (e.g., sinks) or floor drains.
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Facility Design Requirements
• The room temperature must be maintained at 20° or
cooler and a humidity below 60% at all times.
– Temperature and humidity must be controlled
through an efficient heating, ventilation, and air
conditioning (HVAC) system rather than through
use of humidifiers and dehumidifiers, which can
contain standing water that can contribute to
microbial contamination
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Storage conditions
• Storage under frozen conditions places the container–closure under physical
stress, and the degree of stress may depend on the formulation and other
factors.
• Therefore, if a Category 2 CSP is to be stored in a freezer, the integrity of the
CSP in the particular container–closure system in which it will be stored must
have been demonstrated for 45 days at frozen storage.
• A container–closure integrity test needs to be conducted only once on each
formulation and fill volume in the particular container–closure system in
which it will be stored or released/dispensed.
• Once the CSP is thawed, the CSP must not be re-frozen.
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
SOPS and Master Formulation and Compounding Records
• A Master Formulation Record is required
when CSPs are prepared in a batch for
multiple patients or when CSPs are
prepared from nonsterile ingredients.
• Compounding Record is required for every
CSP prepared and requires documentation
by all individuals involved in the actual
preparation of the CSP.
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Urgent-Use CSPs (replaces Immediate-Use)
• A CSP may be prepared in worse than ISO Class 5 air quality (see 4.1
Protection from Airborne Contaminants) in rare circumstances when a CSP is
needed urgently (e.g., cardiopulmonary resuscitation) for a single patient,
and preparation of the CSP under conditions described for Category 1 or
Category 2 would subject the patient to additional risk due to delays in
therapy.
• In these circumstances, the compounding procedure must be a continuous
process not to exceed 1 hour, and administration of the CSP must begin
immediately upon completion of preparation of the CSP.
• Aseptic technique must be followed during preparation, and procedures
must be in place to minimize the potential for contact with nonsterile
surfaces, introduction of particulate matter or biological fluids, and mix-ups
with other CSPs.
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Technology advances
• The statement in the current chapter has
been removed:
– “The use of technologies, techniques,
materials, and procedures other than
those described in this chapter is not
prohibited so long as they have been
proven to be equivalent or superior with
statistical significance to those described
herein.”
• No reference to Rapid Microbiological
Methods as an alternative to USP Chapter
<71>
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
How to Provide Comments to USP
• Go to www.USP.org and search for USP <797>
• Download the proposed revisions
• Comments must be submitted on Comment Submission Template by email to
compoundingsl@usp.org by January 31, 2016
– Be sure to include line numbers for your comments
• If you have any questions, contact the Healthcare Quality Standards team
at CompoundingSL@usp.org
Copyright © 1999 -2016 Clinical IQ, LLC® - All Rights Reserved
Revisions to USP <797> Pharmaceutical
Compounding – Sterile Preparations
Tony Cundell
Consulting Microbiologist,
Scarsdale, NY
Copyright
© 2008-2014
CriticalPoint, LLC®
- All Rights
Reserved
Copyright
© 2008-2016
Tony
Cundell
- All Rights
Reserved
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
Disclaimer
The opinions expressed in this presentation are
solely my own and are not representative of the
USP Microbiology Expert Committee, of which I
am a member, or my consulting clients.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
Revisions to USP <797>
• Members of the USP Microbiology and Sterile Compounding Expert Committees in
collaboration with the FDA, after numerous meetings, have published the long-awaited
revisions to USP <797> Pharmaceutical Compounding – Sterile Preparations online at the
USP website September 25, 2015 with a 90-day comment period ending January 31, 2016.
• Eric Kastango and I strongly recommend, as stakeholders, you review and comment on the
revision.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
Scope of the Chapter
• This chapter describes the minimum practices and quality standards to be followed when
preparing compounded sterile human and animal drugs CSPs.
• These practices and standards must be used to prevent harm, including death, to human
and animal patients that could result from:
1.
microbial contamination (non-sterility)
2.
excessive bacterial endotoxins
3.
variability from the intended strength of correct ingredients
4.
chemical and physical contaminants, and/or
5.
use of ingredients of inappropriate quality.
• Note: 503b outsourcing sterile compounding facilities will be expected to comply with FDA
cGMP regulations.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
USP <797> Revision
As a microbiologist I will discuss the following sections of the proposed revision:
• Competency Testing in Garbing and Hand Hygiene
• Environmental Monitoring
• Sterilization and Depyrogenation
• Release Testing
• Establishing Beyond-use Dating and In-use Times
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
Presentation Structure
I will structure my commentary as follows:
• Summary of the requirements in the 2015 USP <797> revision
• Comparison to the 2008 USP <797> chapter
• Expert analysis of the intent and limitations of the USP <797> revisions
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
Microbial Risk Analysis
Firstly, what are the major risks for CSP microbial and endotoxin contamination?
Personnel and Compounding Environment:
• Gloved Hands > Surfaces (Working) > Airborne > Surfaces (Non-working)
Compounding Operation:
• Non-sterile-to-sterile >> Sterile -to-sterile compounding
• Ingredient water > Compounding ingredients > Packaging materials
Sterilization Processes
• Sterile Filtration > Dry heat sterilization > Steam sterilization
• Aseptic compounding >> Terminal sterilization
• Multiple manipulations >> Single manipulations
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
39
Microbial Risk Analysis (continued)
What are the major risks for CSP microbial and endotoxin contamination?
Storage Temperature:
• Room temperature > Refrigeration >> Frozen
Storage Time:
• Short time > Longer time
Administration route:
• Intrathecal > Intravenal > Intramuscular
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
40
Hospital Usage of CSPs
Based on a 2012 FDA survey of acute-care hospitals that participated in Medicare the
following was found:
• 92% of the hospitals used CSPs
• Of those hospitals, 92% used sterile-to-sterile products and only 25% used higher risk nonsterile-to-sterile products.
• Non-sterile-to-sterile products composed less than 1% of the CSPs used.
• Of the hospital that used non-sterile-to-sterile CSPs, 85% outsourced at least some of
these products
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
41
Personnel Qualification
Revised USP <797>:
• Compounding personnel must gown and don gloves and have zero CFU on finger/thumb
sampling of both hands in an ISO 5 area, no fewer than three consecutive times, before
being allowed to compound.
• During quarterly sampling no more a total of 3 CFU from both gloved hands would be
acceptable.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
42
Fingertip Monitoring
• Gloved hand fingertip monitoring with a contact plate containing TSA plus lecithin and
Tween 20
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
43
Comparison of Personnel Testing Requirements
Personnel Qualification
Current
Proposed
Visual observation of
hand hygiene and
garbing
Finger-tip monitoring
Prior to compounding
and during media fill
testing
Quarterly
(category 1 & 2 CSPs)
Media Fill Testing
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
Annually (low and
medium risk level)
Semi-annually
(high risk level)
Quarterly
(category 1 & 2 CSPs)
Personnel Qualification Analysis
Analysis of the proposed changes:
• The current chapter is more nuanced with the minimum requirements more closely
matching the risk level.
• As microbial contamination of the gloved fingertips is the greatest risk to CSP safety, glove
monitoring should be incorporated into environmental monitoring conducted monthly and
the technician removed from the compounding area, released CSPs evaluated, requalified, prior to returning to their duties, if they fail.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
45
Personnel Qualification: Analysis (continued)
Analysis of the proposed changes:
• Personnel qualification should be reduced to annually for sterile-to-sterile compounding
and semi-annually for non-sterile-to-sterile compounding.
• More emphasis should be given to the definition, observation and qualification of aseptic
technique in the USP <797> revision.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
46
Airborne Non-viable Particulate Monitoring
Revised USP <797>:
• For ISO 5 areas, the action level is ≥ 3,520
particles per m3 (1000 L) under typical
operating conditions (Semi-annually)
• Compounding will cease if the
requirements are not met.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
47
Airborne Non-viable Particulate Monitoring: Analysis
Analysis of proposed changes:
• What does typical operating conditions mean in practice?
• Does particulate monitoring distort the air flow patterns in a laminar
flow hood?
• Does semi-annual facility certification meet this requirement or not?
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
48
Viable Airborne Particle Monitoring
Revised USP <797>:
• For ISO 5 areas, the action level is ≥ 1 cfu/m3 (1000 L) during compounding operations
(monthly)
• If the action level is exceeded, investigate and take corrective action
• Trend below action levels for ISO 7 and 8 areas
• Identify action level isolates to species or at least genus and give greater emphasis to the
presence of pathogens in compounding areas
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
49
Active Viable Particulate Air Samplers
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
50
Viable Airborne Particle Monitoring
Action Levels for Viable Air Sampling
Air Cleanliness
Classification
Current
cfu/m3
Proposed
cfu/m3
ISO Class 5
>1
≥1
ISO Class 7
> 10
≥ 10
ISO Class 8
> 100
≥ 100
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
51
Viable Airborne Particle Monitoring: Analysis
Analysis of the proposed changes:
• Frequency from semi-annually to monthly which will allow for trending.
• Lower level of response, i.e. investigate and corrective actions, compared to non-viable
airborne particle monitoring.
• The action level in the revised USP <797> would be any isolation of microorganisms in the
ISO 5 area.
• Response related to pathogenicity of the isolated microorganisms.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
52
Viable Surface Monitoring
Revised USP <797>:
• For ISO 5 areas work surfaces, action level > 3 CFU/plate or 25 cm2 (monthly)
• Exceeding action levels requires an investigation and corrective actions but not ceasing
compounding.
• Reduce CSP beyond-use dating from Category 1 to 2
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
53
Viable Surface Monitoring
Action Levels for Viable Surface Sampling
Air Cleanliness
Classification
ISO Class 5
ISO Class 7
ISO Class 8
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
Current
cfu/m3
Proposed
cfu/m3
>3
> 3 working
N/A non-working
>5
> 100
> 5 working
> 10 non-working
> 25 working
> 50 non-working
54
Viable Surface Monitoring: Analysis
Analysis of the proposed changes:
• Is the distinction between working and non-working surfaces useful?
• Given the analytical capability of the microbial method is there a real difference between 3
and 4 CFU/cm2 , i.e., a passing or failing result?
• Should compounding cease if the ISO 5 working surface action level is exceeded?
• Is the more stringent ISO class 8 action levels, i.e., 25 versus 100 CFU, justified?
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
55
Sterilization and Depyrogenation
• USP <797> references USP
<1229.4> Sterilizing Filtration
of Liquids, USP <1229.1> Steam
Sterilization by Direct Contact,
USP <1229.8> Dry Heat
Sterilization.
• Biological indicators are
included in routine steam and
dry heat sterilization cycles.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
56
Release Sterility Testing
Revised USP <797>:
• With aseptically prepared CSPs from non-sterile starting materials, the beyond-use dating
is extended from 4 to 28 days, if a USP <71> sterility test is performed.
• With aseptically prepared CSPs from only sterile starting materials, the beyond-use dating
is extended from 6 to 28 days, if a sterility test is performed.
• Storing the CSP at refrigerated temperature adds an extra 3 and 14 days to the beyond-use
dating respectively.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
57
Release Sterility Test: Analysis
Analysis of the proposed chapter <797>:
• The proposed revision to USP <797> should allow the use of
alternative methods to the USP <71> sterility test to reduce the
time to complete the test from 14 days to 7 day or within one
working shift using more rapid sterility testing methods.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
58
Release Endotoxin Testing
Revised <797> chapter:
• All category 2 CSPs made from one or more non-sterile ingredients, except those for
inhalation and topical ophthalmic, must be tested for bacterial endotoxin.
• Exceptions are when the certificates of analysis list the endotoxin level or the
compounding facility has a history of ingredient testing.
• In the absence of endotoxin limits in official USP monographs, the CSP must exceed the
limits calculated as described in USP <85>.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
59
Bacterial Endotoxin Requirements
Current
All high-risk CSPs, except for those
for inhalation and ophthalmic
administration, prepared in groups
of more than 25 SDPs or in MDVs or
that are exposed longer than 12
hours at 2 to 8˚ C or longer than 6
hours at room temperature before
they are sterilized shall be tested.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
Proposed
All Cat 2 made from 1 or more non
sterile ingredients EXCEPT those for
inhalation or topical administration
must be tested.
Exception are if the non-sterile
ingredients have a COA listing
endotoxin bioburden or the
compounder has a testing history.
60
Release Endotoxin Testing: Analysis
Analysis of the proposed changes:
• A distinction is made between topical and intraocular ophthalmic administration in the
revised chapter.
• The testing is still directed towards high-risk CSPs
• The stated policy of the USP is to remove proscribed endotoxin limits for USP monographs.
• The clinician must communicate the patient dosage to the compounding pharmacy so they
can calculate the endotoxin limit.
• The small batch sizes, i.e. <25 SUVs are not exempt.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
Comparison of Beyond-Use Dating
Proposed
Category
1
12 hours
Storage
Conditions
Current
Risk Levels
Room
48 hours (low)
30 hours (medium)
24 hours (high)
24 hours
Refrigerated
14 days (low)
9 days (medium)
3 days (high)
7 days (non-sterile to sterile)
9 days (sterile to sterile)
42 days (sterility tested)
Frozen
45 days
All risk levels
N/A
45 days
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
Proposed
Category 2
4 days (non-sterile to sterile)
6 days (sterile to sterile)
28 days (sterility tested)
Beyond-use Dating: Analysis
Analysis of proposed changes:
• The preparation of Category 1 CSPs is actively discouraged by the short beyond-use dating,
i.e. 24 hours for RT storage.
• Release sterility testing gains an extra 8 and 21 days for room temperature and
refrigerated CSPs respectively.
• The beyond-use dating of sterile-to-sterile CSPs is extended from 48 hours to 6 days
(without sterility testing) and 28 days (with sterility testing) in the proposed USP <797>
revision.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
Beyond-Use Dating: Analysis (continued)
Analysis of proposed changes
• Preservatives are not typically included in IV drug products due to toxicity issues. However,
they may be included in pharmaceutical manufactured multiple-use products used as
starting materials in sterile compounding.
• Frozen storage is not commonly used in acute-cure facilities.
• Terminal sterilization is not a common practice in sterile compounding due to a lack of
steam sterilization capabilities. BUDs for terminally sterilized CSPs is limited to 45 days
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
64
In-Use Times
Revised USP <797>:
• USP <797> defines this new concept, the in-use time as the time before a manufactured
sterile product or CSP must be used after it is opened or needle-punctured.
• The in-use time assigned cannot exceed the expiration dating of the manufactured product
or BUD of the CSP.
• The regulators believe that the in-use time will depend on the type of product or CSP and
the environment where the manipulations occur, i.e. ISO 5 or worse.
• For manufactured products, the in-use times assigned for ampules, single-use container
and multi-dose containers manipulated in ISO 5 areas are use immediately, 6 hours and 28
days respectively.
• For CSPs, the in-use times assigned for compounded single-dose containers, compounded
stock solutions and compounded multi-dose containers that pass the Antimicrobial
Effectiveness Test manipulated in ISO 5 areas are 6 hours, 6 hours, and 28 days.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
65
In-Use Times: Analysis
Analysis of the proposed changes:
• The question must be asked where these in-use times came from and are they
scientifically justified?
• In-use time recommendations based on microbiological and physicochemical stability are
found in the package inserts of manufactured products. This labeling material is approved
by the FDA for each manufactured drug product using stability data submitted by the
manufacturer. They are not found in any GMP regulation or guidance document.
• It is presumed that the 28 days is derived by the longest time interval in the USP <51>
chapter.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
66
In-Use Times: Analysis (continued)
Analysis of the proposed changes:
• It is assumed that the administration time,
e.g. hang time for a IV bag, is not included
in the in-use time.
• Guidance for administration time would be
obtained from CDC recommendations and
ASHP guidelines
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
67
Conclusions
• Overall the changes to chapter <797> can be supported.
• There are opportunities for improvements especially if there is detailed and constructive
comments from stakeholders.
• Thanks for your attention. We will take questions as time permits.
Copyright © 2008-2016 Tony Cundell - All Rights Reserved
68