REvIEwS
evolving challenges in hepatic fibrosis
Scott L. Friedman
abstract | Continued elucidation of the mechanisms of hepatic fibrosis has yielded a comprehensive and
nuanced portrait of fibrosis progression and regression. The paradigm of hepatic stellate cell (HSC) activation
remains the foundation for defining events in hepatic fibrosis and has been complemented by progress
in a number of new areas. Cellular sources of extracellular matrix beyond HSCs have been identified. In
addition, the role of chemokine, adipokine, neuroendocrine, angiogenic and NAPDH oxidase signaling in the
pathogenesis of hepatic fibrosis has been uncovered, as has the contribution of extracellular matrix stiffness
to fibrogenesis. There is also increased awareness of the contribution of innate immunity and greater
understanding of the complexity of gene regulation in HSCs and myofibroblasts. Finally, both apoptosis
and senescence have been recognized as orchestrated programs that eliminate fibrogenic cells during
resolution of liver fibrosis. Ironically, the progress that has been made has highlighted the growing disparity
between advances in the experimental setting and their translation into new diagnostic tools and treatments.
As a result, focus is shifting towards overcoming key translational challenges in order to accelerate the
development of new therapies for patients with chronic liver disease.
Friedman, S. L. Nat. Rev. Gastroenterol. Hepatol. 7, 425–436 (2010); published online 29 June 2010; doi:10.1038/nrgastro.2010.97
Introduction
the field of hepatic fibrosis enjoys remarkable vitality—a
Pubmed search with the keywords ‘hepatic fibrosis’ or
‘hepatic stellate cell’ reveals that there were approximately
3,304 publications on the topic in 2009 alone, and 15,377
publications over the past 5 years. a prior review of the
topic in this journal in 20041 emphasized the emerging
mechanisms of the disease and their therapeutic implica­
tions, focusing on the role of the hepatic stellate cell (HsC)
as the key fibrogenic element in response to chronic liver
injury. more recent advances in the cellular and mol­
ecular biology of the fibrotic wound healing response
have moved into surprising new frontiers, including stem
cells, immune and apoptotic signaling, and epigenetics.
Complementing these advances is further proof that the
liver is uniquely resilient, with evidence that cirrhosis
has regressed in a growing number of patients whose
underlying liver disease has been treated effectively.
Progress could not arrive a moment too soon. a
recent institute of medicine report has imparted a sense
of urgency based on the burden of chronic viral hepa­
titis B and C, which are the leading causes of cirrhosis
and hepatocellular carcinoma (HCC) worldwide and
are currently estimated to affect 1–2% of the us popula­
tion.2 the increasing burden of liver disease in the usa
in part reflects a rising prevalence of cirrhosis among
Competing interests
The author declares an association with the following
companies: Abbott, Amgen, Angion Biomedica, Axcan Pharma,
Bayer, Celera, Conatus Pharmaceuticals, Exalenz, Human
Genome Sciences, Intercept Pharmaceuticals, MDRNA, Onyx
Pharmaceuticals, Salix Pharmaceuticals, Sanofi Aventis and
Siemens Diagnostics. See the article online for full details of the
relationships.
those patients with chronic hepatitis C.3 the worldwide
burden is equally compelling, with chronic liver diseases
affecting hundreds of millions of individuals, which is
associated with an accelerated risk of HCC.4 Contributing
to this burden, the explosive growth in obesity worldwide
has led to a dramatic increase in the prevalence of non­
alcoholic steatohepatitis (nasH),5 which also confers a
risk of HCC once cirrhosis develops.6,7 in fact, HCC has
the fastest rising cancer incidence of any neoplasm in the
usa and western europe.8
Despite all this progress, however, no drug has yet
emerged as an effective antifibrotic agent in humans
and, therefore, it is instructive not only to provide an
update on our understanding of the pathways of fibrosis,
but also to acknowledge the evolving challenges that lie
ahead when translating these discoveries into new treat­
ments. Following an update on recent advances in our
understanding of the mechanisms of fibrosis, this review
highlights a few key areas of progress in the past 5 years
and focuses primarily on four persistent challenges. the
first challenge is to find better markers of fibrosis stage
and activity. the second is to be able to predict which
patients with chronic liver disease will progress to cir­
rhosis and which patients will reverse their fibrosis. the
third is predicting which patients with cirrhosis will
develop decompensated disease. Finally, the fourth chal­
lenge is to perform a proof­of­concept clinical trial that
establishes the rationale for targeting fibrosis in patients
with chronic liver disease.
Advances in the mechanisms of fibrosis
in the past few years, several reviews have emphasized
the essential role of HsC activation into myofibroblasts
nature reviews | gastroenterology & hepatology
© 2010 Macmillan Publishers Limited. All rights reserved
Mount Sinai School of
Medicine, Division of
Liver Diseases,
Box 1123, 1425
Madison Avenue,
Room 1170C, New
York, NY 10029, USA.
scott.friedman@
mssm.edu
volume 7 | auGust 2010 | 425
reviews
Key points
■ Progress in defining the cellular and molecular basis of hepatic fibrosis has
brought us to a juncture where translation of these discoveries into diagnostic
tools and treatments is nearing reality
■ Novel therapeutic targets continue to be unearthed by new discoveries,
including the emergence of the hepatic stellate cell (HSC) as an
immunoregulatory cell type
■ HSCs are also now known to participate in adipokine, angiogenic and
neuroendocrine signaling, interact with other resident cell types and be
regulated by epigenetic and transcriptional mediators
■ Finding better noninvasive markers of fibrogenic activity and disease
progression is a high priority in order to accelerate progress in developing
antifibrotic drugs
■ Genetic markers that predict fibrosis progression risk, combined with new
paradigms to stratify the risk of decompensation among patients with cirrhosis,
should improve clinical trial design quality and patient selection for antifibrotic
therapies
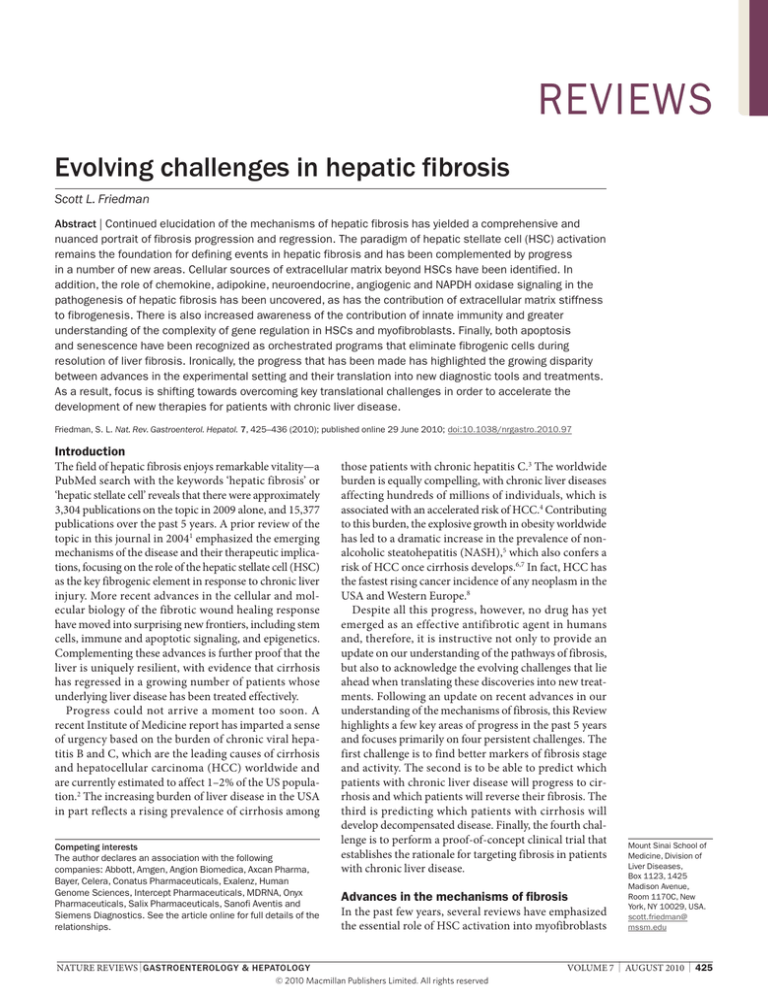
in the pathogenesis of hepatic fibrosis,9–13 and therefore
this concept is not reviewed here in detail, but summa­
rized in Figure 1. instead, several new areas of progress in
our understanding of the mechanisms underlying hepatic
fibrosis are highlighted below. First is the identification of
non­HsC cellular sources of extracellular matrix (eCm).
second is the emerging importance of chemokine, adipo­
kine, neuroendocrine, angiogenic and naPDH oxidase
signaling. third is the role of eCm stiffness in driving
fibrogenesis. Fourth is the contribution of innate immu­
nity involving natural killer (nK) cells, dendritic cells,
and toll­like receptor (tlr) signaling. Fifth is the com­
plexity of gene regulation in HsCs and myofibroblasts,
including control by transcriptional, post­transcriptional,
and epigenetic events, as well as micrornas. sixth is the
recognition that fibrogenic cells can be eliminated during
resolution of liver injury and fibrosis by the orchestrated
programs of apoptosis and senescence.
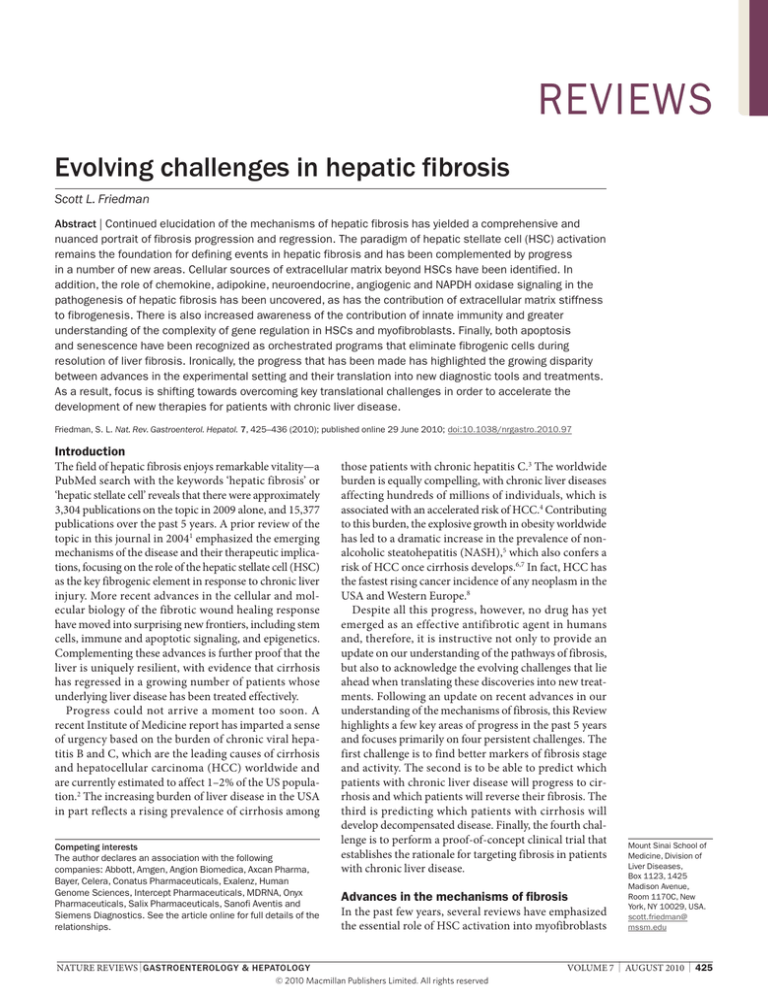
alternative sources of extracellular matrix
several potential non­HsC sources of eCm have been
identified (Figure 2). a number of studies have impli­
cated bone­marrow­derived cells in hepatic fibrogenesis,
both in experimental models and human chronic liver
injury.14–18 these findings parallel those of studies of
fibrogenesis in lung 19 and kidney,20 which have reached
similar conclusions. moreover, circulating fibrocytes,
which are also presumably bone­marrow derived, have
Intitiation
Perpetuation
Injury
Oxidative stress
Apoptotic bodies
LPS
Paracrine stimuli
Contractility
Proliferation
ET1
NO
PDGF
VEGF
FGF
Fibrogenesis
TGFβ1/
CTGF
NOX
Leptin
Reversion
p53
Senescence
Resolution
NFκB
TIMP1 & TIMP2
TRAIL
Fas
Apoptosis
Chemokines
TLR ligands
MMP2 & MMP9
MT1-MMP
TIMP1 & TIMP2
PDGF
Chemokines
Altered matrix
degradation
Adenosine
T cells
B cells
NK cells
NKT cells
Dendritic cells
Mast cells
HSC
chemotaxis
Inflammatory signaling
Figure 1 | HSC activation. The pathways of HSC activation include those that provoke initiation and those that play a part in
perpetuation. Initiation is stimulated by soluble stimuli such as oxidant stress signals (reactive oxygen intermediates),
apoptotic bodies, LPS and paracrine stimuli from neighboring cell types including hepatic macrophages (Kupffer cells),
sinusoidal endothelium and hepatocytes. Initiation is followed by perpetuation. Proliferation, contractility, fibrogenesis,
altered matrix degradation, chemotaxis and inflammatory signaling are specific phenotypic changes characteristic of
perpetuation. Resolution of hepatic fibrosis, which occurs following clearance of the primary liver disease, leads to loss of
activated HSCs, either through apoptosis, senescence or reversion of activated cells to a more quiescent phenotype.
Abbreviations: CTGF, connective tissue growth factor; ET1, endothelin 1; FGF, fibroblast growth factor; HSC, hepatic stellate
cell; LPS, lipopolysaccharide; MMP, matrix metalloproteinase; MT1-MMP, membrane type matrix metalloproteinase; NFκB,
nuclear factor κB; NK, natural killer; NKT, natural killer T cell; NO, nitric oxide; NOX, NAPDH oxidase; PDGF, platelet-derived
growth factor; TGF-β1, transforming growth factor β1; TIMP, tissue inhibitor of metalloproteinase; TLR, Toll-like receptor;
TRAIL, tumor-necrosis-factor-related apoptosis-inducing ligand; vEGF, vascular endothelial growth factor. Permission
obtained from Elsevier Ltd © Friedman, S. L. Gastroenterology 134, 1655–1669 (2008) and the American Society for
Biochemistry and Molecular Biology © Friedman S. L. J. Biol. Chem. 275, 2247–2250 (2000).
426 | AUGUST 2010 | volUme 7
www.nature.com/nrgastro
© 2010 Macmillan Publishers Limited. All rights reserved
reviews
also been implicated in hepatic fibrogenesis.21 However,
not all studies agree with these conclusions.22 indeed, the
overall contribution of fibrocytes to fibrosis is probably
very small. nonetheless, alternative contributions of these
cells to the response to liver injury beyond fibrogenesis
(for example, immunoregulation) merit further study.
although it is not clear how to reconcile these opposing
views on the contribution of bone­marrow­derived cells
to fibrosis, studies of this type differ in several ways—the
models used, duration of injury, markers used to charac­
terize cells, and methods of detection—so their direct
comparison may be difficult.
some evidence also implicates epithelial­to­
mesenchymal transition (emt) as a source of fibrogenic
cells, a pathway that has previously been described in
renal fibrosis.20,23 However, more recent studies refute this
conclusion.24,25 in liver studies, experimental models have
identified both hepatocytes26 and biliary epithelium27 as
potential epithelial origins for emt. Bone morphogenic
protein 7 has specifically been implicated in hepato­
cyte­derived emt,26 whereas the hedgehog pathway
seems dominant in biliary epithelium­derived emt.27,28
moreover, transitions of this type may be bidirectional,
with some epithelium arising from fibrogenic cells (that
is, mesenchymal­to­epithelial transition [met]).29 what
is unclear from these studies, however, is whether cells
simply express mesenchymal markers or contribute sub­
stantively to eCm production. one study indicates that
their actual contribution is minimal in vivo, even though
emt can be documented in cell culture.30,31 in addition,
there is intriguing evidence that either transdifferentia­
tion between HsCs and liver progenitor cells occurs32 or,
alternatively, that HsCs provide a uniquely supportive
environment for progenitor cell survival and expan­
sion.33,34 the implications of these findings for hepatic
regeneration, fibrosis and cancer remain to be clarified.
signaling in hepatic fibrosis
Chemokine signaling
two elegant studies published in 2009 35,36 implicate
chemokine signaling in the pathogenesis of hepatic fibrosis
and complement earlier work that has been summarized
elsewhere.37 in particular, the CC chemokine receptors
CCr1 and CCr5 are both fibrogenic, but they arise from
distinct cellular sources: CCr1 is derived from bone
marrow cells, whereas CCr5 is derived from resident liver
cells.35 interestingly, the site of the CC chemokine receptor
CCr2 expression evolves with progressive liver injury—
CCr2 is initially expressed by bone marrow cells, but later
by resident liver cells.36 By contrast, the activity of CXC
chemokine ligand 9 (CXCl9), through its cognate recep­
tor CXCr3, is antifibrotic, and polymorphisms in the gene
encoding CXCl9 may contribute to fibrosis progression
risk in patients who have chronic liver disease.38
Adipokine signaling
similar to chemokine signaling, signaling by adipo­
kines—polypeptides derived from adipose tissue—has
assumed increasing importance in parallel with rapid
advances in understanding the role of adipokines in
Bone marrow
?
Fibrocytes
Myofibroblasts
Stellate cell
Activated
stellate cell
MET
Portal
fibroblast
EMT:
Hh signaling
BMP7
Hepatocytes and
cholangiocytes
Figure 2 | Sources of fibrogenic cell types in hepatic fibrosis. Upon liver injury
quiescent hepatic stellate cells (HSCs) transition initially into ‘activated’ HSCs and
then further into contractile myofibroblasts. Other cells may also transdifferentiate
into fibrogenic myofibroblasts in liver injury, although their relative contribution to
extracellular matrix (ECM) production and the human diseases in which they
participate are not clear. Some, but not all, studies indicate that these additional
sources of ECM include bone marrow (which probably gives rise to circulating
fibrocytes), portal fibroblasts, and EMT from hepatocytes and cholangiocytes,
driven by Hh signaling and bone morphogenetic protein (BMP). In addition, a MET
may also occur, in which mesenchymal cells give rise to epithelium; here too, the
relative importance of this pathway is uncertain in human diseases. Abbreviations:
EMT, epithelial-to-mesenchymal transition; Hh, hedgehog; MET, mesenchymal-toepithelial transition. Permission obtained from Elsevier Ltd © Friedman, S. L.
Gastroenterology 134, 1655–1669 (2008).
metabolic homeostasis outside the liver.39 whereas some
adipokines are strictly derived from fat, others are also
produced by resident liver cells. For example, leptin and
adiponectin are both derived from HsCs, and their recip­
rocal dysregulation (that is, elevated levels of leptin and
diminished levels of adiponectin) may drive fibrogenesis
primarily through local paracrine signaling.40,41
Neuroendocrine signaling
neuroendocrine activity has also been uncovered in
liver, 42 most prominently in studies of cannabinoid
signaling. interruption of cannabinoid activity is an
appealing therapeutic target. specifically, CB1 receptor
signaling is profibrogenic, and thus efforts to antago­
nize this molecule have met with significant success in
animal models,43 and are being evaluated in human trials.
Conversely, CB2 receptor signaling is antifibrogenic—a
strategy to agonize this receptor also shows promise.44
CB2 agonists may, however, amplify inflammation,45
suggesting that CB1 antagonism may be a more rational
target than CB2. similar to cannabinoids, data now also
implicate neurotrophins,46,47 serotonin and opioids in
local fibrogenic signaling. like cannabinoids, divergent
effects of these compounds in HsCs may be elicited by
different subtypes of their receptors.42
Angiogenic signaling
angiogenic signaling is a key component of the wound
healing response in hepatic fibrosis, contributing not only
nature reviews | gastroenterology & hepatology
© 2010 Macmillan Publishers Limited. All rights reserved
volume 7 | auGust 2010 | 427
reviews
to eCm production, but also to portal hypertension.48
Classic angiogenic mediators, most notably vascular
endothelial growth factor (veGF) and platelet­derived
growth factor (PDGF), drive both the angiogenic and
fibrogenic responses, and may also foster a milieu that
is permissive for the development of HCC (see below).
on the other hand, angiogenesis may also be essential for
regenerative responses to chronic liver injury, and thus
efforts to antagonize angiogenic signaling must be titrated
sufficiently to preserve normal growth responses while
inhibiting neoplasia.
NADPH oxidase signaling
oxidant stress has been implicated in fibrogenic stimula­
tion for many years, and the intracellular pathways medi­
ating its generation have been greatly clarified of late.49,50
among several enzymes that regulate the generation of
oxidant stress, the naDPH oxidase protein complex is
particularly important, and inhibition of naDPH oxidase
is an attractive target for antifibrotic therapy.50 moreover,
the fibrogenic effect of apoptotic body ingestion by HsCs
is also mediated by naDPH oxidase.51
long­term administration of the angiotensin recep­
tor blocker losartan in patients with chronic hepatitis C
significantly decreases the expression of naDPH oxidase,
collagen i, matrix metalloproteinase 2 and urokinase type
plasminogen activator.52 targeting of losartan to the liver
may offer some benefit by possibly reducing its unwanted
activities (for example, lowering of blood pressure),
as demonstrated in an animal study that used a liver­
targeted complex containing losartan.53 the promise of
antioxidant therapy has received an important boost from
a large­scale trial of vitamin e in patients with nasH,54,55
a disease in which oxidant stress has been consistently
implicated. Future efforts with antioxidant therapies will
probably attempt to enhance their potency by more tar­
geted delivery to the liver, or by the use of formulations
that are activated upon reaching the liver.
extracellular matrix stiffness drives fibrogenesis
new diagnostic modalities that correlate the stiffness of
the liver with the fibrosis stage (for example, transient
elastography [see below]) have found a molecular corre­
late in studies demonstrating that the physical proper­
ties of eCm, in addition to their chemical composition,
affect HsC activation.56 moreover, stiffness may actually
precede fibrosis57 as a result of both increased edema and
inflammatory cell infiltration.
the contribution of innate immunity
Growth in our understanding of the contribution of innate
immunity to hepatic fibrosis has been almost explosive.
there has been rapid progress in defining the roles not
only of macrophages and traditional lymphocyte subsets
(for example, t and B cells), but also of nK cells, nKt
cells,13,58–60 B cells, dendritic cells61 and mast cells. there
are also the newly uncovered contributions of tlrs,62–65
nFκB signaling 66 and the inflammasome, a molecular
complex activated upon stress that promotes inflam­
mation.67 moreover, bidirectional interactions between
HsCs and/or myofibroblasts, and immune cell subsets,
elicit specific cellular responses that modulate the com­
position of inflammatory infiltrates and the vigor of fibro­
genesis.68,69 in aggregate, these studies point to the liver
as a major immunoregulatory organ, and underscore the
critical contribution of immune cell subsets in modulating
fibrosis as well as liver injury.
gene regulation in hsCs and myofibroblasts
Progress in understanding gene regulation in HsCs
and myofibroblasts has paralleled the dramatic expan­
sion of knowledge about both traditional mechanisms
of gene regulation, including transcription factor
activity, localization and modification,70 as well as epi­
genetic regulation of gene expression by methylation,71,72
mrna stabilization73 and microrna interactions.72,74,75
elucidating the precise molecular events underlying HsC
activation and fibrogenesis is translating into fruitful new
therapeutic approaches.66
the repertoire of transcription factors known to
cooperatively regulate gene expression through post­
translational modification of regulatory proteins, particu­
larly through phosphorylation, is growing. For example,
HsC activation provokes phosphorylation of the rela
subunit of nFκB at a specific serine residue (ser 536) that
leads to its nuclear import, resulting in increased nFκB
transcriptional activity,76 which increases the survival of
activated HsCs. treatment of rodents with experimental
fibrosis by using an angiotensin­converting­enzyme
inhibitor or humans with hepatitis C by using an angio­
tensin receptor blocker, leads to reduced survival of
activated HsCs and/or myofibroblasts and regression
of fibrosis by inhibiting the phosphorylation of the rela
subunit of nFκB at ser 536.76
in an example of epigenetic regulation, myofibroblast
activity can also be controlled by a microrna, mir132,
that releases a translational block on the methyl­CpG
binding protein, which in turn leads to repression of
the PParγ transcription factor.72 in a final example,
phosphorylation of the transcription factor C/eBPβ by the
ribosomal s­6 kinase (rsK) is critical for HsC activation;
this phosphorylation can be inhibited by cell­permeable
peptides that block rsK and lead to cellular apoptosis.77
apoptosis, senescence and resolution of fibrosis
exciting clinical evidence has demonstrated that cirrhosis
may not only be reversible,78 but that regression of fibro­
sis leads to improved clinical outcomes.79 at what point
cirrhosis becomes irreversible is uncertain, but irreversi­
bility becomes increasingly likely as the scar thickens,
becomes more acellular and is chemically crosslinked.
nonetheless, these successes in demonstrating fibrosis
regression even in patients with advanced fibrosis have
redoubled our efforts to understand the mechanistic basis
for fibrosis regression in the hope of exploiting pathways
that drive the clearance of HsCs in the fibrotic liver.
Complex, but remarkably well­orchestrated intracel­
lular events conspire to sustain HsC survival and growth
during progressive fibrosis, while permitting their regu­
lated clearance during resolution of fibrosis. in support
428 | AUGUST 2010 | volUme 7
www.nature.com/nrgastro
© 2010 Macmillan Publishers Limited. All rights reserved
reviews
a
b
Serum
markers
Liver biopsy
c Ultrasound (ARFI) and MRI
Push pulse
Region of interest
Shear waves
d Metabolic breath tests
f Transient elastography
Transducter
Detection pulse
Ribs
Probe
Labeled
substrate
Vibrator
Pressure (mmHg)
e Hepatic venous pressure gradient (HVPG)
WHVP
FHVP
Time (s)
Figure 3 | Diagnostic approaches to detecting liver fibrosis. A growing number of complementary diagnostic approaches are
emerging to detect and quantify hepatic fibrosis. a | Liver biopsy remains the gold standard for assessing both diseasespecific pathologies and fibrosis stage, but newer approaches provide complementary information. These newer modalities
include: b | serum tests, such as ELF, Fibrotest, Fibrometer and several others; c | imaging modalities such as acoustic
radiation force impulse (ARFI)—an ultrasound-based technique (the principles shown here are for the virtual Touch Tissue
Quantification mode; courtesy of Siemens Medical Solutions)—and MRI-based techniques (not shown here); d | Metabolic
breath tests that assess the functional reserve of the liver rather than structure; e | Hepatic venous pressure gradient
(HvPG), which requires direct catheterization of the hepatic vasculature and of all the methods correlates best with clinical
outcomes; and f | transient elastography (either by bedside probe or using magnetic resonance elastography (MRE; not
shown). Both elastography methods measure liver stiffness, which may reflect fibrosis or edema and inflammation.
Abbreviations: FHvP, free hepatic venous pressure; wHvP, wedge hepatic venous pressure.
of this concept, progression of hepatic fibrosis in patients
with hepatitis C is associated with progressive loss of HsC
apoptosis.80 whereas earlier, groundbreaking studies
highlighted the importance of tissue inhibitor of metallo­
proteinase 1 (timP1) in sustaining HsC survival during
progressive injury, more recent efforts have focused
on intracellular events that are targetable; for example,
interfering with survival signals mediated by the nFκB
cascade and kinase activities (see preceding section).76,81,82
the tumor suppressor protein p53 has entered the field
of hepatic fibrosis through evidence demonstrating that
it drives senescence of activated HsCs during resolution
of experimental fibrosis.83 the functional and regulatory
relationship between apoptosis and senescence of HsCs
remains to be defined.
Challenges to progress
with the astonishing progress in clarifying the pathways
of hepatic fibrosis, the greatest obstacles to translation of
these advances no longer reside in the laboratory but rather
rest firmly in the clinical setting. Four such translational
challenges are highlighted in the following sections.
Markers of fibrosis stage and activity
the first challenge that we face is the need for better
markers of fibrosis stage and activity (Figure 3).
Liver biopsy
the foundations of the discipline of hepatology were built
upon histologic assessment of liver tissue, and thus percu­
taneous biopsy has been a bedrock for the diagnosis and
staging of fibrosis. However, its limitations have become
painfully clear. apart from its invasive nature and thus
the limited number of samples that can be obtained over
time in an individual patient, the modality suffers from
significant sampling variability, owing to the fact that the
tissue obtained represents only ~1/50,000th of the organ.
although most chronic liver diseases are relatively homo­
geneous, the modest variability from region to region
is sufficient to yield discordance in fibrosis staging in
at least one­third of biopsy samples from patients with
hepatitis C84 or nasH.85 indeed, even very large biopsy
samples (>2.5 cm) will be unlikely to exceed 75% accu­
racy in assessing fibrosis in patients with hepatitis C.86
Fibrosis quantification in liver biopsy samples can be
improved by morphometric methods rather than con­
ventional staging,87,88 but this does not overcome the
problem of sampling variability when the tissue sample
is inadequate.
remarkably, only recently has a study explored the
relationship between fibrosis stage and outcome, using
patients enrolled in the niH Halt­C trial of long­term
treatment with interferon α for patients with chronic
nature reviews | gastroenterology & hepatology
© 2010 Macmillan Publishers Limited. All rights reserved
volume 7 | auGust 2010 | 429
reviews
hepatitis C.89 in this trial, which used the six­stage ishak
staging system, there was a clear relationship between
fibrosis stage and both baseline markers of disease sever­
ity as well as clinical events over a 6­year period. However,
among those patients with stage 6 fibrosis (that is, cir­
rhosis) there were no features reported within the biopsy
sample that identified those patients who were more likely
to develop clinical events. in addition, 25% of biopsy
samples were fragmented, which significantly diminished
the ability to establish an association between fibrosis stage
and outcomes. Finally, the use of a discontinuous scoring
system implies that the incremental changes in fibrosis
content between consecutive stages are equal, when in fact
there is far more fibrosis accumulated between the more
advanced stages than between the early stages. this means
that the amount of matrix that must be resorbed if fibrosis
is reversed will be far greater if patients have advanced
fibrosis at the time of treatment with either an antiviral or
antifibrotic drug than if patients have mild fibrosis.
Transient elastography
innovative new methodologies have begun to circum­
vent the need for biopsy samples to be taken in a growing
fraction of patients. the most popular new modality is
transient elastography, which correlates the speed of
transmission of a shear wave through the liver with the
organ’s relative stiffness.90–92 numerous studies have firmly
established the value of transient elastography in distin­
guishing cirrhosis from earlier stages of fibrosis in patients
with chronic hepatitis C, in whom stiffness largely reflects
matrix accumulation. By contrast, stiffness in patients with
acute hepatitis more likely reflects edema and inflam­
mation, and does not correlate with fibrosis.93,94 Post­
transplantation, the measurement of liver stiffness may
enable stratification between a mild or severe recurrence
of hepatitis C.95
a more comprehensive assessment of the entire liver’s
stiffness can be obtained by mr elastography.96 regardless
of which approach is employed (bedside versus mr assess­
ment), elastography is becoming an appealing adjunct to
patient management that is currently approved for use in
western europe and awaiting evaluation by the FDa in the
usa. it remains uncertain, however, whether these tech­
nologies will enable accurate assessment of fibrosis pro­
gression over time in individual patients that is sufficient
to permit their usage in patients without cirrhosis.
Other imaging modalities
other imaging modalities are also gaining momentum
for the assessment of liver fibrosis.97 specialized mri
techniques, including diffusion­weighted imaging,98 per­
fusion imaging 99 and functional imaging 100 are gaining
interest. a newer technology—acoustic radiation force
impulse (arFi)—is an ultrasound­based technology
that seems to be comparable to transient elastography
in its ability to distinguish cirrhosis from earlier stages
of fibrosis in patients with chronic hepatitis C. arFi
utilizes a conventional ultrasound device, which makes
the technology more readily available given the wide use
of ultrasound.101,102
Serum markers
serum markers of fibrosis, measured using combinations
of either common laboratory studies or proprietary matrix
assays, have roughly comparable ranges of accuracies;
some tests are more useful in specific diseases and at dif­
ferent stages than others.103,104–107 the two best­validated
methods, Fibrotest (BioPredictive, Paris, France) and
the enhanced liver Fibrosis (elF ™ ) test (iQur ltd,
southampton, uK), are even more accurate than liver
biopsy in predicting clinical outcomes, whether or
not they directly reflect either fibrosis accumulation
or regression.108,109
serum markers can also distinguish between mild and
progressive hepatitis C recurrence after liver transplanta­
tion, presumably by reflecting increased edema and
inflammation in patients with recurrence.95 like trans­
ient elastography, serum markers enable many patients to
avoid biopsy in cases in which the results clearly indicate
the presence of either minimal or advanced fibrosis, with
up to 50% of biopsies being avoidable based on current
estimates.110 the accuracy of serum tests may be further
increased by combining them with elasto graphy find­
ings.111 Finally, serum assay values are reduced following
successful treatment of hepatitis C,112 further reinforcing
their correlation with fibrogenic activity.
the use of noninvasive markers is especially appealing
in populations in whom percutaneous biopsy is more
challenging, for example children113 and patients co­
infected with Hiv and HCv.114,115 information regarding
fibrosis stage is especially vital in co­infected patients,
as successful therapy for HCv can greatly reduce liver­
related complications.116
Markers of fibrogenesis
Perhaps a more compelling issue is whether the amount
of scar per se is the best indication of prognosis and
response to therapy. as a relatively static consequence
of liver injury, fibrosis content alone does not convey
information about the fibrogenic activity or liver reserve.
accordingly, tests that reflect fibrogenesis (that is, the
activity of scar production) are important complements
to tests that assess only fibrosis content. For example,
immunohistochemical markers of HsC activation in liver
sections, particularly α­smooth muscle actin, are a more
sensitive indicator of the rate of fibrogenesis and risk
of clinical complications, particularly in patients with
hepatitis C following liver transplantation.117
Measures of hepatic reserve
similarly, functional tests of hepatic reserve—once an
appealing but cumbersome diagnostic method used in
specialized centers—are making a comeback. improved
technology now enables bedside assessment of the liver’s
metabolic activity. 118,119 rather than simply correlat­
ing its results to the amount of scar, tests of this type
provide complementary information that ultimately
may be more informative than simple hepatic histologic
features in predicting outcomes. Continued validation
and standardization of tests of functional reserve will be
essential to ensure that their results are reproducible, and
430 | AUGUST 2010 | volUme 7
www.nature.com/nrgastro
© 2010 Macmillan Publishers Limited. All rights reserved
reviews
are not confounded by external factors including diet,
concurrent medications and/or comorbidities.
Hepatic venous pressure gradient assessment
another test of hepatic function, albeit an invasive one,
is the hepatic venous pressure gradient (HvPG) assess­
ment. in fact, the test is remarkably accurate in deter­
mining which patients with cirrhosis are at risk for
decompensation120 (see section below). However, the
utility of assessing the HvPG is confined to patients with
relatively advanced disease who are at risk of, or already
have, portal hypertension.
The future of fibrosis markers
what could ultimately emerge from these broad efforts
across a range of methodologies may be a multimodal
approach to assess both liver structure and function. the
essential advance, not yet realized, will be to define a test,
or series of tests, which reliably predict changes in hepatic
structure, function, fibrogenic activity, and/or prognosis
over time, as well as response to therapy in individual
patients. such an advance will accelerate the ability to
conduct long­term trials of antifibrotic drugs by yielding
unambiguous evidence of efficacy.121
predicting fibrosis progression and reversal
our second challenge is to find a way to predict which
patients with chronic liver disease will progress to
cirrhosis and which patients will reverse their fibrosis.
Fibrosis progression
Fibrosis progression is strongly driven by genetic factors
that can be identified by simple tests already available for
clinical usage. a large number of genetic markers have
been uncovered that reportedly correlate with fibrosis
progression rate, primarily in hepatitis C.38,122–125 among
these, a seven­gene cirrhosis risk score (Crs)—seven
single nucleotide polymorphisms (snPs) combined into
a scoring system—is strongly associated with fibrosis pro­
gression,126,127 and has been validated in a separate large
prospective cohort study.128
in addition to testing genetic markers in multiple popu­
lations, a key to establishing their relevance is to link the
Dna sequence changes to altered pathways of disease
pathogenesis, thereby providing a mechanism to explain
the impact of the snP on fibrosis. at least one of the snPs
within the Crs has been linked to altered HsC activity.64
several other snPs that are not part of the Crs have also
been linked to altered HsC activity.38,124,129–131
what is the utility of determining fibrosis progression
risk in a patient who has chronic liver disease? First, the
knowledge that a patient may progress more rapidly, even
if the liver histology findings are currently at an early
fibrosis stage, may influence the frequency of follow­up
evaluations and the timing of a disease­specific therapy
(for example, antiviral drugs) if one is available. second,
this information is vital to designing clinical trials of
antifibrotic drugs that will produce unambiguous find­
ings (Figure 4). specifically, if the relative distribution of
fibrosis risk is not evenly distributed among placebo and
treatment groups, then interpreting the potential response
to a drug will be confounded by underlying, genetically
determined differences in fibrosis progression rates
independent of the drug’s effect. third, by enrolling only
those patients who have a high risk of fibrosis progression
into antifibrotic trials, clearer results will be obtained in
a shorter study interval, as differences between a placebo
and treatment group would emerge more rapidly if the
drug were effective.
in addition to genetic determinants, the associations
between environmental or behavioral risk factors and
fibrosis progression have also been strengthened. For
example, studies have demonstrated that both coffee132,133
and caffeine134 have a protective effect on fibrosis progres­
sion. the antifibrotic effect may be due to antagonism
of adenosine receptor activity, which in animal models
reduces the fibrogenic activity of HsCs.135 moreover, until
recently there were no data linking specific viral factors
with fibrosis progression, but two studies have now
demonstrated that hepatitis B genotype C,136 and hepa­
titis C genotype 3137 are both associated with more rapid
fibrosis progression. the findings complement the well­
known acceleration of fibrosis progression due to Hiv
and HCv co­infection, as underscored by the findings of
a study based on liver biopsy in co­infected patients.138
Fibrosis regression
similar to factors that drive the rate of fibrosis progres­
sion, there are likely to be factors that determine which
patients will have regression of fibrosis when the primary
disease has been arrested. ample evidence indicates that
cirrhosis may regress to earlier stages in many patients
who have been successfully treated with antiviral therapy,
for example,79,139 yet it is unclear in whom this will occur.
moreover, the determinants of regression might be bio­
chemical rather than genetic, for example based on the
density of chemical cross linking of collagen, or the cell­
ularity of the scar.140 Clarifying the factors that confer
regression of fibrosis will become increasingly possible as a
greater number of patients are successfully treated for their
underlying liver disease because of improved therapies.
predicting decompensation
the third challenge that we face is being able to predict
which patients with cirrhosis will develop decompen­
sated disease. indeed, not all patients with cirrhosis have a
comparable prognosis—some will remain stable for up to
10 years while others are at imminent risk of decompen­
sation.141 these disparate outcomes are not sufficiently
predicted by either histologic staging systems or standard
clinical parameters in patients with either a low melD or
Child–Pugh score, although a large­scale analysis from
the Halt­C trial indicates that common clinical and
laboratory features may be predictive in patients who have
more advanced disease.142 moreover, some, but not, all
studies suggest that Fibroscan® (echosens, Paris, France)
may identify patients who have a higher likelihood of
developing esophageal varices143 or HCC.144
why haven’t better tests been developed before now
to predict the risk of decompensation among patients
nature reviews | gastroenterology & hepatology
© 2010 Macmillan Publishers Limited. All rights reserved
volume 7 | auGust 2010 | 431
reviews
Risk of fibrosis
progression
Placebo group
Treatment group
a
Unequal
stratification
Low
b
Equal
stratification
Medium
HCV patients
c
Inclusion of
high-risk patients
for trials of
antifibrotic agents
High
Figure 4 | Implications of assessing the genetic risk of fibrosis progression for designing an antifibrotic drug trial. Studies
determining the genetic risk of fibrosis progression in patients with chronic liver disease provide new opportunities to
refine disease-specific and generalized antifibrotic therapies. This diagram illustrates the potential implications of genetic
risk information in designing a theoretical antifibrotic drug trial. a | Unequal stratification; the potential outcome of
randomization if genetic data are not considered. In this example, more patients at high risk of fibrosis progression are
inadvertently randomized to the placebo arm, whereas the treatment arm contains more low risk patients. In this situation,
if an antifibrotic drug was ineffective, the placebo group would progress more rapidly owing to the underlying genetic risk of
disease, leading to the false interpretation that the drug was effective. b | Equal stratification. In this situation unequal
stratification is rectified by instead stratifying the genetic risk of disease equally between the treatment and placebo
groups. c | Genetic progression risk data are further exploited by first identifying only high-risk patients, who are then
randomized to both placebo and treatment groups. By restricting the enrollment to only patients with high risk of fibrosis
progression in this example, the number of patients and duration of therapy required to achieve a statistical difference if an
antifibrotic drug is effective should be reduced.
with cirrhosis? the answer, in part, reflects the futility of
managing cirrhosis in earlier eras—with no treatments
available for either the primary disease or the consequent
fibrosis, it hardly seemed critical to refine the classifica­
tion and prognosis of cirrhosis. even now, liver trans­
plantation is only indicated for those patients who have
already developed decompensated disease or who have
developed potentially curable HCC that is not treatable
by liver resection. therefore, more sensitive tests to strat­
ify the risk of decompensation among apparently stable
patients who have cirrhosis are still needed.
among the candidate modalities for predictive tests,
HvPG, although an invasive test requiring techni­
cal expertise, is remarkably accurate in predicting
decompensation. For example, a long­term study of
patients enrolled in a trial of β­blockers to prevent
variceal hemorrhage demonstrated that patients with a
baseline HvPG of <10 mmHg had only an ~15% chance
of decompensation during a follow­up of 8 years, whereas
those patients with a baseline HvPG >10 mmHg had an
~70% risk of decompensation over the same interval.120
remarkably, simple pathologic features seen on liver
biopsy may provide surrogate evidence for these divergent
outcomes—smaller nodule size and thicker septae both
indicate a higher risk of decompensation, presumably
because they reflect a higher HvPG.145 interestingly, these
same features are also characteristic of more advanced
experimental cirrhosis, and when fibrosis regresses in
these experimental models the smaller nodules begin to
expand and thickened septae become thinner.13 although
none are available yet, a noninvasive or minimally invasive
means of assessing HvPG could greatly enable the esti­
mation of decompensation risk, and might even be useful
in determining the response to antifibrotic agents.
as underscored in a review published in early 2010,141
the increasingly refined view of cirrhosis as being more
than one stage demands a reassessment of staging systems
to create better ways of predicting prognosis and antici­
pating complications. with new therapies on the horizon,
newer models of risk stratification will enable more careful
selection of patients and better prediction of outcomes.
a proof-of-concept antifibrotic clinical trial
we are still lacking a proof­of­principle trial that estab­
lishes the value of attacking fibrosis directly despite
ongoing liver disease, and that is our fourth challenge.
with all the tremendous progress that has been made in
unearthing the mechanisms of hepatic fibrosis, it is rea­
sonable to ask why there are no approved drugs for the
treatment of fibrosis in patients with chronic liver disease.
the first point is that animal models, although vital for
creating a path to clinical development, have limitations.
Fibrosis that develops in weeks in rodents does not com­
pletely mimic the slow evolution of fibrosis in humans,
particularly with respect to the amount of eCm crosslink­
ing and loss of cellularity that occurs over longer intervals
432 | AUGUST 2010 | volUme 7
www.nature.com/nrgastro
© 2010 Macmillan Publishers Limited. All rights reserved
reviews
in humans.146 thus, animal studies have variable relevance,
based on the model used, administration schedule and
dosing, and the therapeutic target or targets (Box 1). the
second point is that clinical trials of antifibrotic drugs are
still reliant on liver biopsy as an endpoint, which obligates
the trials to be conducted over lengthy intervals, increas­
ing their cost and limiting the enthusiasm of sponsors.150
moreover, there is growing skepticism about the reli­
ability of liver biopsy in this setting. thus, the third and
most important point is that there is an urgent need for
better noninvasive biomarkers that indicate early, robust
responses to antifibrotic therapies. the field of hepato­
logy has been conditioned by trials of antiviral agents, in
which unequivocal responses to therapy are demonstrable
by serum tests showing the absence of viral replication.
in the fibrosis sphere, however, it is the tissue’s response
to injury, rather than detection of a virus, that is being
assessed. as such, responses are may be more ambiguous
and require longer intervals to be established.
Despite this obstacle, the number of potential anti­
fibrotic therapies is expanding rapidly, and their potential
has been embraced by the pharmaceutical and biotech
sectors, and also by the public. Dozens of antifibrotic
approaches, too numerous to discuss in this article, have
emerged and been reviewed.10,151–153 moreover, exciting
prospects for targeting diagnostic agents or therapies
directly to HsCs may enhance efforts to improve both
the diagnosis and treatment of hepatic fibrosis.53,154–157
Conclusions
in summary, the field of hepatic fibrosis continues to
expand rapidly, and represents a vibrant paradigm of
translational research. the persistent challenges that limit
the development of antifibrotic therapies are rapidly being
offset by tremendous energy, creativity and persistence in
both the laboratory and clinical settings, and are certain
to yield accelerating, tangible progress for patients with
chronic liver diseases.
1.
2.
3.
4.
5.
6.
7.
8.
Friedman, S. L. Mechanisms of hepatic fibrosis
and therapeutic implications. Nat. Clin. Pract.
Gastroenterol. Hepatol. 1, 98–105 (2004).
Mitchell, A. E., Colvin, H. M. & Palmer Beasley, R.
Institute of Medicine recommendations for the
prevention and control of hepatitis B and C.
Hepatology 51, 729–733 (2010).
Davis, G. L., Alter, M. J., El-Serag, H., Poynard, T.
& Jennings, L. w. Aging of hepatitis C virus
(HCv)-infected persons in the United States: a
multiple cohort model of HCv prevalence and
disease progression. Gastroenterology 138,
513–521, 521 e1–6 (2010).
Lim, Y. S. & Kim, w. R. The global impact of
hepatic fibrosis and end-stage liver disease.
Clin. Liver Dis. 12, 733–746 (2008).
Cheung, O. & Sanyal, A. J. Recent advances in
nonalcoholic fatty liver disease. Curr. Opin.
Gastroenterol. 25, 230–237 (2009).
Bugianesi, E. Non-alcoholic steatohepatitis and
cancer. Clin. Liver Dis. 11, 191–207 (2007).
Hashizume, H. et al. Primary liver cancers with
nonalcoholic steatohepatitis. Eur. J.
Gastroenterol. Hepatol. 19, 827–834 (2007).
Jemal, A. et al. Cancer statistics, 2009. CA
Cancer J. Clin. 59, 225–249 (2009).
9.
10.
11.
12.
13.
14.
15.
16.
17.
Box 1 | Determinants of relevance of animal models to human hepatic fibrosis
the model or models used
Typically, the efficacy of an antifibrotic drug should be demonstrated in at least two
mechanistically distinct animal models, e.g. one provoking parenchymal fibrosis
(e.g. carbon tetrachloride or thioacetamide) and another associated with biliary
fibrosis (e.g. bile duct obstruction, Mdr2–/– animals,147 or ANIT administration148).
administration schedule and dosing
The drug should be efficacious in a ‘treatment’ model in which fibrosis is already
present before the agent inducing fibrosis is started. The drug should not interfere
with the toxicity or mechanism of injury of the model itself, but rather block fibrosis
directly.
The dose should achieve a drug level within a range that is comparable to the safe
and effective concentrations used in humans.
target of action
The cellular or molecular target of the therapy, and its role in fibrosis, should be
similar between the animal model and human disease. For example, immune
pathways between animals and humans may differ substantially, and thus immune
targets that are valid in animals may not have an established role in human
disease. Conversely, TGF-β1, e.g. has a well-established role as a fibrogenic
mediator in both humans and animal models, and thus is an appealing target to
test in animal models.
Similarly, the models used must mimic the key features of the human disease. For
example, induction of αvβ6 integrin has been documented in biliary models,149 and
thus its relevance may only extend to human biliary disease but not parenchymal
diseases (e.g. viral hepatitis or NASH).
Review criteria
Articles were selected following a comprehensive review
of English-language, full-text papers listed in PubMed,
based on the impact and novelty of the work, relevance
to the topic and overall quality. Great emphasis was
placed on selecting high quality research and review
articles published primarily within the past 3 years to
ensure that the review was up to date. In addition to the
PubMed search, the reference lists of high-impact papers
and review articles were scrutinized to ensure that no
significant papers were overlooked.
Friedman, S. L. Mechanisms of hepatic
fibrogenesis. Gastroenterology 134, 1655–1669
(2008).
Schuppan, D. & Afdhal, N. H. Liver cirrhosis.
Lancet 371, 838–851 (2008).
Jiao, J., Friedman, S. L. & Aloman, C. Hepatic
fibrosis. Curr. Opin. Gastroenterol. 25, 223–229
(2009).
Parola, M. & Pinzani, M. Hepatic wound repair.
Fibrogenesis Tissue Repair 2, 4 (2009).
Henderson, N. C. & Iredale, J. P. Liver fibrosis:
cellular mechanisms of progression and
resolution. Clin. Sci. (Lond.) 112, 265–280
(2007).
Baertschiger, R. M. et al. Fibrogenic potential
of human multipotent mesenchymal stromal
cells in injured liver. PLoS ONE 4, e6657
(2009).
Miyata, E. et al. Hematopoietic origin of hepatic
stellate cells in the adult liver. Blood 111,
2427–2435 (2008).
Russo, F. P. et al. The bone marrow functionally
contributes to liver fibrosis. Gastroenterology
130, 1807–1821 (2006).
Forbes, S. J. et al. A significant proportion of
myofibroblasts are of bone marrow origin in
nature reviews | gastroenterology & hepatology
© 2010 Macmillan Publishers Limited. All rights reserved
18.
19.
20.
21.
22.
23.
24.
human liver fibrosis. Gastroenterology 126,
955–963 (2004).
Fujimiya, T. et al. Pathological roles of
bone-marrow-derived stellate cells in a mouse
model of alcohol-induced fatty liver. Am. J.
Physiol. Gastrointest. Liver Physiol. 297,
G974–G980 (2009).
Strieter, R. M. & Mehrad, B. New mechanisms
of pulmonary fibrosis. Chest 136, 1364–1370
(2009).
Grande, M. T. & Lopez-Novoa, J. M. Fibroblast
activation and myofibroblast generation in
obstructive nephropathy. Nat. Rev. Nephrol. 5,
319–328 (2009).
Kisseleva, T. et al. Bone marrow-derived
fibrocytes participate in pathogenesis of liver
fibrosis. J. Hepatol. 45, 429–438 (2006).
Higashiyama, R. et al. Negligible contribution of
bone marrow-derived cells to collagen
production during hepatic fibrogenesis in mice.
Gastroenterology 137, 1459–1466 (2009).
Kalluri, R. & Neilson, E. G. Epithelialmesenchymal transition and its implications for
fibrosis. J. Clin. Invest. 112, 1776–1784 (2003).
Lin, S. L., Kisseleva, T., Brenner, D. A. &
Duffield, J. S. Pericytes and perivascular
volume 7 | auGust 2010 | 433
reviews
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
fibroblasts are the primary source of collagenproducing cells in obstructive fibrosis of the
kidney. Am. J. Pathol. 173, 1617–1627 (2008).
Humphreys, B. D. et al. Fate tracing reveals the
pericyte and not epithelial origin of
myofibroblasts in kidney fibrosis. Am. J. Pathol.
176, 85–97 (2010).
Zeisberg, M. et al. Fibroblasts derive from
hepatocytes in liver fibrosis via epithelial to
mesenchymal transition. J. Biol. Chem. 282,
23337–23347 (2007).
Omenetti, A. et al. Hedgehog signaling regulates
epithelial-mesenchymal transition during biliary
fibrosis in rodents and humans. J. Clin. Invest.
118, 3331–3342 (2008).
Omenetti, A. et al. Repair-related activation
of hedgehog signaling promotes cholangiocyte
chemokine production. Hepatology 50,
518–527 (2009).
Choi, S. S. & Diehl, A. M. Epithelial-tomesenchymal transitions in the liver. Hepatology
50, 2007–2013 (2009).
Taura, K. et al. Hepatocytes do not undergo
epithelial-mesenchymal transition in liver
fibrosis in mice. Hepatology 51, 1027–1036
(2010).
wells, R. G. The epithelial-to-mesenchymal
transition in liver fibrosis: here today, gone
tomorrow? Hepatology 51, 737–740 (2010).
Kordes, C. et al. CD133+ hepatic stellate cells
are progenitor cells. Biochem. Biophys. Res.
Commun. 352, 410–417 (2007).
Sawitza, I., Kordes, C., Reister, S. &
Haussinger, D. The niche of stellate cells within
rat liver. Hepatology 50, 1617–1624 (2009).
Roskams, T. Relationships among stellate cell
activation, progenitor cells, and hepatic
regeneration. Clin. Liver Dis. 12, 853–860
(2008).
Seki, E. et al. CCR1 and CCR5 promote hepatic
fibrosis in mice. J. Clin. Invest. 119, 1858–1870
(2009).
Seki, E. et al. CCR2 promotes hepatic fibrosis
in mice. Hepatology 50, 185–197 (2009).
Pinzani, M. & Marra, F. Cytokine receptors and
signaling in hepatic stellate cells. Semin. Liver
Dis. 21, 397–416 (2001).
wasmuth, H. E. et al. Antifibrotic effects of
CXCL9 and its receptor CXCR3 in livers of mice
and humans. Gastroenterology 137, 309–319,
319 e1–3 (2009).
Marra, F. & Bertolani, C. Adipokines in liver
diseases. Hepatology 50, 957–969 (2009).
Ikejima, K., Okumura, K., Kon, K., Takei, Y. &
Sato, N. Role of adipocytokines in hepatic
fibrogenesis. J. Gastroenterol. Hepatol.
22 (Suppl. 1), S87–S92 (2007).
Ding, X. et al. The roles of leptin and
adiponectin: a novel paradigm in adipocytokine
regulation of liver fibrosis and stellate cell
biology. Am. J. Pathol. 166, 1655–1669 (2005).
Ebrahimkhani, M. R., Elsharkawy, A. M. &
Mann, D. A. wound healing and local
neuroendocrine regulation in the injured liver.
Expert Rev. Mol. Med. 10, e11 (2008).
Teixeira-Clerc, F. et al. CB1 cannabinoid receptor
antagonism: a new strategy for the treatment of
liver fibrosis. Nat. Med. 12, 671–676 (2006).
Munoz-Luque, J. et al. Regression of fibrosis
after chronic stimulation of cannabinoid CB2
receptor in cirrhotic rats. J. Pharmacol. Exp. Ther.
324, 475–483 (2008).
Deveaux, v. et al. Cannabinoid CB2 receptor
potentiates obesity-associated inflammation,
insulin resistance and hepatic steatosis. PLoS
ONE 4, e5844 (2009).
Passino, M. A., Adams, R. A., Sikorski, S. L. &
Akassoglou, K. Regulation of hepatic stellate
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
cell differentiation by the neurotrophin receptor
p75NTR. Science 315, 1853–1856 (2007).
Kendall, T. J. et al. p75 Neurotrophin receptor
signaling regulates hepatic myofibroblast
proliferation and apoptosis in recovery from
rodent liver fibrosis. Hepatology 49, 901–910
(2009).
Fernandez, M. et al. Angiogenesis in liver
disease. J. Hepatol. 50, 604–620 (2009).
Novo, E. & Parola, M. Redox mechanisms in
hepatic chronic wound healing and fibrogenesis.
Fibrogenesis Tissue Repair 1, 5 (2008).
De Minicis, S. & Brenner, D. A. NOX in liver
fibrosis. Arch. Biochem. Biophys. 462, 266–272
(2007).
Zhan, S. S. et al. Phagocytosis of apoptotic
bodies by hepatic stellate cells induces NADPH
oxidase and is associated with liver fibrosis
in vivo. Hepatology 43, 435–443 (2006).
Colmenero, J. et al. Effects of losartan on
hepatic expression of non-phagocytic NADPH
oxidase and fibrogenic genes in patients with
chronic hepatitis C. Am. J. Physiol. Gastrointest.
Liver Physiol. 297, G726–G734 (2009).
Moreno, M. et al. Reduction of advanced liver
fibrosis by short-term targeted delivery of an
angiotensin receptor blocker to hepatic stellate
cells in rats. Hepatology 51, 942–952 (2009).
Sanyal, A. J. et al. Pioglitazone, vitamin E, or
placebo for nonalcoholic steatohepatitis.
N. Engl. J. Med. 362, 1–5 (2010).
Sanyal, A. A randomized controlled trial of
pioglitazone or vitamin E for nonalcoholic
steatohepatitis (PIvENS) [abstract]. Hepatology
50, 90A (2009).
wells, R. G. The role of matrix stiffness
in regulating cell behavior. Hepatology 47,
1394–1400 (2008).
Georges, P. C. et al. Increased stiffness of the
rat liver precedes matrix deposition:
implications for fibrosis. Am. J. Physiol.
Gastrointest. Liver Physiol. 293, G1147–G1154
(2007).
Park, O. et al. Diverse roles of invariant natural
killer T cells in liver injury and fibrosis induced
by carbon tetrachloride. Hepatology 49,
1683–1694 (2009).
Gao, B., Radaeva, S. & Park, O. Liver natural
killer and natural killer T cells: immunobiology
and emerging roles in liver diseases. J. Leukoc.
Biol. 86, 513–528 (2009).
Notas, G., Kisseleva, T. & Brenner, D. NK and
NKT cells in liver injury and fibrosis. Clin.
Immunol. 130, 16–26 (2009).
Connolly, M. K. et al. In liver fibrosis, dendritic
cells govern hepatic inflammation in mice via
TNF-alpha. J. Clin. Invest. 119, 3213–3225
(2009).
Seki, E. et al. TLR4 enhances TGF-beta signaling
and hepatic fibrosis. Nat. Med. 13, 1324–1332
(2007).
Seki, E. & Brenner, D. A. Toll-like receptors and
adaptor molecules in liver disease: update.
Hepatology 48, 322–335 (2008).
Guo, J. et al. Functional linkage of cirrhosispredictive single nucleotide polymorphisms of
Toll-like receptor 4 to hepatic stellate cell
responses. Hepatology 49, 960–968 (2009).
Mencin, A., Kluwe, J. & Schwabe, R. F. Toll-like
receptors as targets in chronic liver diseases.
Gut 58, 704–720 (2009).
Chakraborty, J. B. & Mann, D. A. NF-kappaB
signalling: embracing complexity to achieve
translation. J. Hepatol. 52, 285–291 (2010).
watanabe, A. et al. Inflammasome-mediated
regulation of hepatic stellate cells. Am. J. Physiol.
Gastrointest. Liver Physiol. 296, G1248–G1257
(2009).
434 | AUGUST 2010 | volUme 7
68. Muhanna, N. et al. Activation of hepatic stellate
cells after phagocytosis of lymphocytes: a novel
pathway of fibrogenesis. Hepatology 48,
963–977 (2008).
69. Holt, A. P. et al. Liver myofibroblasts regulate
infiltration and positioning of lymphocytes in
human liver. Gastroenterology 136, 705–714
(2009).
70. Mann, J. & Mann, D. A. Transcriptional regulation
of hepatic stellate cells. Adv. Drug Deliv. Rev. 61,
497–512 (2009).
71. Mann, J. et al. Regulation of myofibroblast
transdifferentiation by DNA methylation and
MeCP2: implications for wound healing and
fibrogenesis. Cell Death Differ. 14, 275–285
(2007).
72. Mann, J. et al. MeCP2 controls an epigenetic
pathway that promotes myofibroblast
transdifferentiation and fibrosis.
Gastroenterology 138, 705–714, 714 e1–4
(2010).
73. Fritz, D. & Stefanovic, B. RNA-binding protein
RBMS3 is expressed in activated hepatic
stellate cells and liver fibrosis and increases
expression of transcription factor Prx1. J. Mol.
Biol. 371, 585–595 (2007).
74. Guo, C. J., Pan, Q., Li, D. G., Sun, H. & Liu, B. w.
miR-15b and miR-16 are implicated in activation
of the rat hepatic stellate cell: an essential role
for apoptosis. J. Hepatol. 50, 766–778 (2009).
75. venugopal, S. K. et al. Liver fibrosis causes
down-regulation of miRNA-150 and miRNA-194
in hepatic stellate cells and their over-expression
causes decreased stellate cell activation. Am. J.
Physiol. Gastrointest. Liver Physiol. 298,
G101–G106 (2009).
76. Oakley, F. et al. Angiotensin II activates I kappaB
kinase phosphorylation of RelA at Ser 536 to
promote myofibroblast survival and liver fibrosis.
Gastroenterology 136, 2334–2344 e1 (2009).
77. Buck, M. & Chojkier, M. A ribosomal S-6 kinasemediated signal to C/EBP-beta is critical for the
development of liver fibrosis. PLoS ONE 2,
e1372 (2007).
78. Friedman, S. L. & Bansal, M. B. Reversal of
hepatic fibrosis—fact or fantasy? Hepatology 43,
S82–S88 (2006).
79. Mallet, v. et al. Brief communication: the
relationship of regression of cirrhosis to outcome
in chronic hepatitis C. Ann. Intern. Med. 149,
399–403 (2008).
80. Gonzalez, S. A. et al. Inverse association
between hepatic stellate cell apoptosis and
fibrosis in chronic hepatitis C virus infection.
J. Viral Hepat. 16, 141–148 (2009).
81. Oakley, F. et al. Inhibition of inhibitor of kappaB
kinases stimulates hepatic stellate cell
apoptosis and accelerated recovery from rat liver
fibrosis. Gastroenterology 128, 108–120
(2005).
82. Jiang, J. X., Mikami, K., venugopal, S., Li, Y. &
Torok, N. J. Apoptotic body engulfment by
hepatic stellate cells promotes their survival by
the JAK/STAT and Akt/NF-kappaB-dependent
pathways. J. Hepatol. 51, 139–148 (2009).
83. Krizhanovsky, v. et al. Senescence of activated
stellate cells limits liver fibrosis. Cell 134,
657–667 (2008).
84. Regev, A. et al. Sampling error and intraobserver
variation in liver biopsy in patients with chronic
HCv infection. Am. J. Gastroenterol. 97,
2614–2618 (2002).
85. Ratziu, v. et al. Sampling variability of liver
biopsy in nonalcoholic fatty liver disease.
Gastroenterology 128, 1898–1906 (2005).
86. Bedossa, P., Dargere, D. & Paradis, v. Sampling
variability of liver fibrosis in chronic hepatitis C.
Hepatology 38, 1449–1457 (2003).
www.nature.com/nrgastro
© 2010 Macmillan Publishers Limited. All rights reserved
reviews
87. Goodman, Z. D. et al. Fibrosis progression in
chronic hepatitis C: morphometric image
analysis in the HALT-C trial. Hepatology 50,
1738–1749 (2009).
88. Calvaruso, v. et al. Computer-assisted image
analysis of liver collagen: relationship to Ishak
scoring and hepatic venous pressure gradient.
Hepatology 49, 1236–1244 (2009).
89. Everhart, J. E. et al. Prognostic value of Ishak
fibrosis stage: findings from the hepatitis C
antiviral long-term treatment against cirrhosis
trial. Hepatology 51, 585–594 (2010).
90. Castera, L. Transient elastography and other
noninvasive tests to assess hepatic fibrosis in
patients with viral hepatitis. J. Viral Hepat. 16,
300–314 (2009).
91. vizzutti, F., Arena, U., Marra, F. & Pinzani, M.
Elastography for the non-invasive assessment
of liver disease: limitations and future
developments. Gut 58, 157–160 (2009).
92. Pinzani, M., vizzutti, F., Arena, U. & Marra, F.
Technology Insight: noninvasive assessment
of liver fibrosis by biochemical scores and
elastography. Nat. Clin. Pract. Gastroenterol.
Hepatol. 5, 95–106 (2008).
93. Arena, U. et al. Acute viral hepatitis increases
liver stiffness values measured by transient
elastography. Hepatology 47, 380–384 (2008).
94. vigano, M. et al. Transient elastography
assessment of the liver stiffness dynamics
during acute hepatitis B. Eur. J. Gastroenterol.
Hepatol. 22, 180–184 (2009).
95. Carrion, J. A. et al. Liver stiffness identifies two
different patterns of fibrosis progression in
patients with hepatitis C virus recurrence after
liver transplantation. Hepatology 51, 23–34
(2010).
96. Talwalkar, J. A. et al. Magnetic resonance
imaging of hepatic fibrosis: emerging clinical
applications. Hepatology 47, 332–342 (2008).
97. Bonekamp, S., Kamel, I., Solga, S. & Clark, J.
Can imaging modalities diagnose and stage
hepatic fibrosis and cirrhosis accurately?
J. Hepatol. 50, 17–35 (2009).
98. Taouli, B. et al. Diffusion-weighted MRI for
quantification of liver fibrosis: preliminary
experience. AJR Am. J. Roentgenol. 189,
799–806 (2007).
99. Hagiwara, M. et al. Advanced liver fibrosis:
diagnosis with 3D whole-liver perfusion MR
imaging--initial experience. Radiology 246,
926–934 (2008).
100. Barash, H. et al. Functional magnetic resonance
imaging monitoring of pathological changes in
rodent livers during hyperoxia and hypercapnia.
Hepatology 48, 1232–1241 (2008).
101. Fahey, B. J., Nightingale, K. R., Nelson, R. C.,
Palmeri, M. L. & Trahey, G. E. Acoustic radiation
force impulse imaging of the abdomen:
demonstration of feasibility and utility.
Ultrasound Med. Biol. 31, 1185–1198 (2005).
102. Friedrich-Rust, M. et al. Liver fibrosis in viral
hepatitis: noninvasive assessment with acoustic
radiation force impulse imaging versus transient
elastography. Radiology 252, 595–604 (2009).
103. Smith, J. O. & Sterling, R. K. Systematic review:
Non-invasive methods of fibrosis analysis in
chronic hepatitis C. Aliment. Pharmacol. Ther.
30, 557–576 (2009).
104. Smith, M. w. et al. Gene expression patterns
that correlate with hepatitis C and early
progression to fibrosis in liver transplant
recipients. Gastroenterology 130, 179–187
(2006).
105. Leroy, v. et al. Prospective comparison of six
non-invasive scores for the diagnosis of liver
fibrosis in chronic hepatitis C. J. Hepatol. 46,
775–782 (2007).
106. Gressner, O. A., weiskirchen, R. &
Gressner, A. M. Biomarkers of hepatic fibrosis,
fibrogenesis and genetic pre-disposition
pending between fiction and reality. J. Cell. Mol.
Med. 11, 1031–1051 (2007).
107. Nunes, D. et al. Noninvasive markers of liver
fibrosis are highly predictive of liver-related
death in a cohort of HCv-infected individuals
with and without HIv infection. Am. J.
Gastroenterol. doi:10.1038/ajg.2009.746.
108. Ngo, Y. et al. A prospective analysis of the
prognostic value of biomarkers (FibroTest) in
patients with chronic hepatitis C. Clin. Chem.
52, 1887–1896 (2006).
109. Mayo, M. J. et al. Prediction of clinical outcomes
in primary biliary cirrhosis by serum enhanced
liver fibrosis assay. Hepatology 48, 1549–1557
(2008).
110. Sebastiani, G. et al. SAFE biopsy: a validated
method for large-scale staging of liver fibrosis in
chronic hepatitis C. Hepatology 49, 1821–1827
(2009).
111. Castera, L. et al. Prospective comparison of
transient elastography, Fibrotest, APRI, and liver
biopsy for the assessment of fibrosis in chronic
hepatitis C. Gastroenterology 128, 343–350
(2005).
112. Fontana, R. J. et al. Serum fibrosis marker levels
decrease after successful antiviral treatment
in chronic hepatitis C patients with advanced
fibrosis. Clin. Gastroenterol. Hepatol. 7,
219–226 (2009).
113. Nobili, v. et al. Performance of ELF serum
markers in predicting fibrosis stage in pediatric
non-alcoholic fatty liver disease.
Gastroenterology 136, 160–167 (2009).
114. de Ledinghen, v. et al. Diagnosis of hepatic
fibrosis and cirrhosis by transient elastography
in HIv/hepatitis C virus-coinfected patients.
J. Acquir. Immune Defic. Syndr. 41, 175–179
(2006).
115. Sanchez-Conde, M. et al. Comparison of
transient elastography and liver biopsy for the
assessment of liver fibrosis in HIv/hepatitis C
virus-coinfected patients and correlation with
noninvasive serum markers. J. Viral Hepat. 17,
280–286 (2009).
116. Berenguer, J. et al. Sustained virological response
to interferon plus ribavirin reduces liver-related
complications and mortality in patients
coinfected with human immunodeficiency virus
and hepatitis C virus. Hepatology 50, 407–413
(2009).
117. Russo, M. w. et al. Early hepatic stellate cell
activation is associated with advanced fibrosis
after liver transplantation in recipients with
hepatitis C. Liver Transpl. 11, 1235–1241
(2005).
118. Armuzzi, A. et al. Review article: breath testing
for human liver function assessment. Aliment.
Pharmacol. Ther. 16, 1977–1996 (2002).
119. Petrolati, A. et al. 13C-methacetin breath test
for monitoring hepatic function in cirrhotic
patients before and after liver transplantation.
Aliment. Pharmacol. Ther. 18, 785–790 (2003).
120. Ripoll, C. et al. Hepatic venous pressure
gradient predicts clinical decompensation in
patients with compensated cirrhosis.
Gastroenterology 133, 481–488 (2007).
121. Talwalkar, J. A. Antifibrotic therapies—emerging
biomarkers as treatment end points. Nat. Rev.
Gastroenterol. Hepatol. 7, 59–61 (2010).
122. Hold, G. L., Untiveros, P., Saunders, K. A.
& El-Omar, E. M. Role of host genetics in
fibrosis. Fibrogenesis Tissue Repair 2, 6 (2009).
123. weber, S., Gressner, O. A., Hall, R., Grunhage, F.
& Lammert, F. Genetic determinants in hepatic
fibrosis: from experimental models to fibrogenic
nature reviews | gastroenterology & hepatology
© 2010 Macmillan Publishers Limited. All rights reserved
gene signatures in humans. Clin. Liver Dis. 12,
747–757 (2008).
124. wasmuth, H. E. et al. The Marburg I variant
(G534E) of the factor vII-activating protease
determines liver fibrosis in hepatitis C infection
by reduced proteolysis of platelet-derived growth
factor BB. Hepatology 49, 775–780 (2009).
125. Asselah, T. et al. Genetics, genomics, and
proteomics: implications for the diagnosis and
the treatment of chronic hepatitis C. Semin.
Liver Dis. 27, 13–27 (2007).
126. Huang, H. et al. A 7 gene signature identifies
the risk of developing cirrhosis in patients with
chronic hepatitis C. Hepatology 46, 297–306
(2007).
127. Huang, H. et al. Identification of two gene
variants associated with risk of advanced
fibrosis in patients with chronic hepatitis C.
Gastroenterology 130, 1679–1687 (2006).
128. Marcolongo, M. et al. A seven-gene signature
(cirrhosis risk score) predicts liver fibrosis
progression in patients with initially mild chronic
hepatitis C. Hepatology 50, 1038–1044 (2009).
129. wasmuth, H. E. et al. CC chemokine receptor 5
delta32 polymorphism in two independent
cohorts of hepatitis C virus infected patients
without hemophilia. J. Mol. Med. 82, 64–69
(2004).
130. Hillebrandt, S. et al. Complement factor 5 is a
quantitative trait gene that modifies liver
fibrogenesis in mice and humans. Nat. Genet.
37, 835–843 (2005).
131. Hung, T. M. et al. A novel nonsynonymous variant
of matrix metalloproteinase-7 confers risk of
liver cirrhosis. Hepatology 50, 1184–1193
(2009).
132. Freedman, N. D. et al. Coffee intake is
associated with lower rates of liver disease
progression in chronic hepatitis C. Hepatology
50, 1360–1369 (2009).
133. Ruhl, C. E. & Everhart, J. E. Coffee and tea
consumption are associated with a lower
incidence of chronic liver disease in the United
States. Gastroenterology 129, 1928–1936
(2005).
134. Modi, A. A. et al. Increased caffeine consumption
is associated with reduced hepatic fibrosis.
Hepatology 51, 201–209 (2010).
135. Chan, E. S. et al. Adenosine A(2A) receptors
play a role in the pathogenesis of hepatic
cirrhosis. Br. J. Pharmacol. 148, 1144–1155
(2006).
136. Chan, H. L. et al. Hepatitis B virus genotype C is
associated with more severe liver fibrosis than
genotype B. Clin. Gastroenterol. Hepatol. 7,
1361–1366 (2009).
137. Bochud, P. Y. et al. Genotype 3 is associated with
accelerated fibrosis progression in chronic
hepatitis C. J. Hepatol. 51, 655–666 (2009).
138. Macias, J. et al. Fast fibrosis progression between
repeated liver biopsies in patients coinfected with
human immunodeficiency virus/hepatitis C virus.
Hepatology 50, 1056–1063 (2009).
139. Pinzani, M. & vizzutti, F. Fibrosis and cirrhosis
reversibility: clinical features and implications.
Clin. Liver Dis. 12, 901–913 (2008).
140. Ramachandran, P. & Iredale, J. P. Reversibility of
liver fibrosis. Ann. Hepatol. 8, 283–291 (2009).
141. Garcia-Tsao, G., Friedman, S., Iredale, J. &
Pinzani, M. Now there are many (stages) where
before there was one: In search of a
pathophysiological classification of cirrhosis.
Hepatology 51, 1445–1449 (2010).
142. Ghany, M. G. et al. Predicting clinical and
histologic outcomes based on standard
laboratory tests in advanced chronic
hepatitis C. Gastroenterology 138, 136–146
(2010).
volume 7 | auGust 2010 | 435
reviews
143. Kazemi, F. et al. Liver stiffness measurement
selects patients with cirrhosis at risk of bearing
large oesophageal varices. J. Hepatol. 45,
230–235 (2006).
144. Masuzaki, R. et al. Risk assessment of
hepatocellular carcinoma in chronic hepatitis C
patients by transient elastography. J. Clin.
Gastroenterol. 42, 839–843 (2008).
145. Nagula, S., Jain, D., Groszmann, R. J. &
Garcia-Tsao, G. Histological–hemodynamic
correlation in cirrhosis—a histological
classification of the severity of cirrhosis.
J. Hepatol. 44, 111–117 (2006).
146. Iredale, J. P. Models of liver fibrosis: exploring
the dynamic nature of inflammation and repair
in a solid organ. J. Clin. Invest. 117, 539–548
(2007).
147. Popov, Y., Patsenker, E., Fickert, P., Trauner, M.
& Schuppan, D. Mdr2 (Abcb4)–/– mice
spontaneously develop severe biliary fibrosis via
massive dysregulation of pro- and antifibrogenic
genes. J. Hepatol. 43, 1045–1054 (2005).
148. Lichtman, S. N., wang, J. & Clark, R. L.
A microcholangiographic study of liver disease
models in rats. Acad. Radiol. 2, 515–521 (1995).
149. Popov, Y. et al. Integrin alphavbeta6 is a marker
of the progression of biliary and portal liver
fibrosis and a novel target for antifibrotic
therapies. J. Hepatol. 48, 453–464 (2008).
150. Friedman, S. L. Reversibility of hepatic fibrosis
and cirrhosis--is it all hype? Nat. Clin. Pract.
Gastroenterol. Hepatol. 4, 236–237 (2007).
151. Ghiassi-Nejad, Z. & Friedman, S. L. Advances in
antifibrotic therapy. Expert Rev. Gastroenterol.
Hepatol. 2, 803–816 (2008).
152. Rockey, D. C. Current and future anti-fibrotic
therapies for chronic liver disease. Clin. Liver
Dis. 12, 939–962 (2008).
153. Popov, Y. & Schuppan, D. Targeting liver fibrosis:
strategies for development and validation
of antifibrotic therapies. Hepatology 50,
1294–1306 (2009).
154. Schoemaker, M. H. et al. PDGF-receptor betatargeted adenovirus redirects gene transfer
436 | AUGUST 2010 | volUme 7
from hepatocytes to activated stellate cells.
Mol. Pharm. 5, 399–406 (2008).
155. Gonzalo, T. et al. Local inhibition of liver fibrosis
by specific delivery of a PDGF kinase inhibitor to
hepatic stellate cells. J. Pharmacol. Exp. Ther.
321, 856–865 (2007).
156. Friedman, S. L. Targeting siRNA to arrest
fibrosis. Nat. Biotechnol. 26, 399–400 (2008).
157. Sato, Y. et al. Resolution of liver cirrhosis using
vitamin A-coupled liposomes to deliver siRNA
against a collagen-specific chaperone. Nat.
Biotechnol. 26, 431–442 (2008).
acknowledgments
work in the author’s laboratory is supported by NIH
grants RO1DK37340, RO1DK56621, P20AA017067
and 1K05AA018408-01. This article highlights
primarily recent studies and review articles of general
interest to the readership. As a result many
outstanding publications in the field could not be
cited because of space constraints.
www.nature.com/nrgastro
© 2010 Macmillan Publishers Limited. All rights reserved