Circ J 2008; 72: 1481 – 1486
Metabolic Syndrome Predicts 10-Year Mortality
in Non-Diabetic Patients Following
Coronary Artery Bypass Surgery
Kan Kajimoto, MD; Takatoshi Kasai, MD*; Katsumi Miyauchi, MD*;
Hitoshi Hirose, MD; Naotake Yanagisawa, MB*; Taira Yamamoto, MD;
Kenji Takazawa, MD**; Hiroshi Niinami, MD; Yasuyuki Hosoda, MD†;
Hiroyuki Daida, MD*; Atsushi Amano, MD
Background Metabolic syndrome (MetS) is a risk factor for cardiovascular disease and mortality, but, the
relationship between MetS and survival after coronary artery bypass grafting (CABG) remains unclear.
Methods and Results The outcomes of patients with and without MetS were analyzed. Patients who had undergone CABG at Juntendo University Hospital between January 1984 and December 1992 were enrolled. The
survival search was performed by the end of 2000. The patients were categorized by the existence of preoperative
MetS using the modified American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI)
definition with body mass index instead of waist circumference. MetS was present in 551 (46.6%) patients and
absent in 632 (53.4%). Preoperative MetS was associated with long-term poor prognosis in terms of all-cause
death (hazard ratio (HR) 1.34; 95% confidence interval (CI) 1.03–1.74; p=0.028) and cardiac death (HR 2.31;
95% CI 1.36–3.92; p=0.002) in non-diabetic patients. These differences in the mortality of the 2 groups were
more obvious after 10 years. However, among the patients with diabetes, the presence of MetS was not related to
long-term mortality.
Conclusions Preoperative MetS predicted increased all-cause and cardiac mortality, especially after 10 years,
in non-diabetic patients undergoing CABG. (Circ J 2008; 72: 1481 – 1486)
Key Words: Coronary artery bypass grafting; Diabetes mellitus; Long-term outcomes; Metabolic syndrome
R
esearch into metabolic syndrome (MetS) and cardiovascular outcomes has been mostly focused on
primary prevention of coronary artery disease
(CAD).1–3 There are few studies investigating MetS in
patients with CAD4–6 and the relationship between MetS
and outcome following coronary artery bypass grafting
(CABG) has not been studied to our knowledge. Therefore,
the goal of this study was to investigate whether the preoperative existence of MetS is associated with long-term
mortality in patients following CABG.
Methods
Patients
Preoperative data of the patients who had undergone
(Received December 10, 2007; revised manuscript received April 28,
2008; accepted May 1, 2008)
Department of Cardiovascular Surgery, *Department of Cardiology,
Juntendo University School of Medicine, **Department of Cardiovascular Surgery, Social Insurance Chuo General Hospital, Tokyo and
†Department of Cardiovascular Surgery, Kawasaki Saiwai Hospital,
Kawasaki, Japan
There are no any conflicts of interest in this manuscript.
The abstract was presented at the 55th Annual Scientific Session
American College of Cardiology, Atlanta, Georgia, March 11-14,
2006.
Mailing address: Katsumi Miyauchi, MD, Department of Cardiology,
Juntendo University School of Medicine, 2-1-1 Hongo, Bunkyo-ku,
Tokyo 113-8421, Japan. E-mail: ktmmy@med.juntendo.ac.jp
All rights are reserved to the Japanese Circulation Society. For permissions, please e-mail: cj@j-circ.or.jp
Circulation Journal Vol.72, September 2008
isolated CABG at Juntendo University Hospital between
January 1984 and December 1992 were entered into a
structured database. This study was performed according to
the ethics policies of the institution, and was approved by
internal review board. All CABG was performed under
conventional cardiopulmonary bypass, moderate systemic
hypothermia (28–32°C), topical cardiac cooling, and cardioplegic arrest. Demographic data (including age, gender,
and body mass index (BMI)), coronary risk factors (blood
pressure (BP) on admission, fasting total cholesterol, lowdensity lipoprotein-cholesterol, high-density lipoproteincholesterol (HDL-C), triglycerides, fasting plasma glucose,
smoking history, and family history of CAD), medication
use, and operative parameters were prospectively recorded.
MetS was defined as 3 or more of the following 5 criteria
based on the modified American Heart Association/National
Heart, Lung, and Blood Institute (AHA/NHLBI) definition7
(obesity was defined as BMI ≥25 kg/m2 according to the
established Japanese criteria for obesity, rather than waist
circumference as in the AHA/NHLBI definition),15 triglycerides ≥150 mg/dl; HDL-C <40 mg/dl for men, <50 mg/dl for
women; BP ≥130/85 mmHg or treatment with antihypertensive medication; and fasting blood glucose ≥100 mg/dl
or treatment with oral hypoglycemic drugs or insulin injection. Each patient was further categorized according to
coronary risk factors. Diabetes mellitus (DM) was defined
as a fasting plasma glucose level ≥126 mg/dl or requiring
treatment with oral hypoglycemic medication or insulin
use. Hypertension was defined as systolic BP ≥140 mmHg
or diastolic BP ≥90 mmHg, or requiring treatment with spe-
KAJIMOTO K et al.
1482
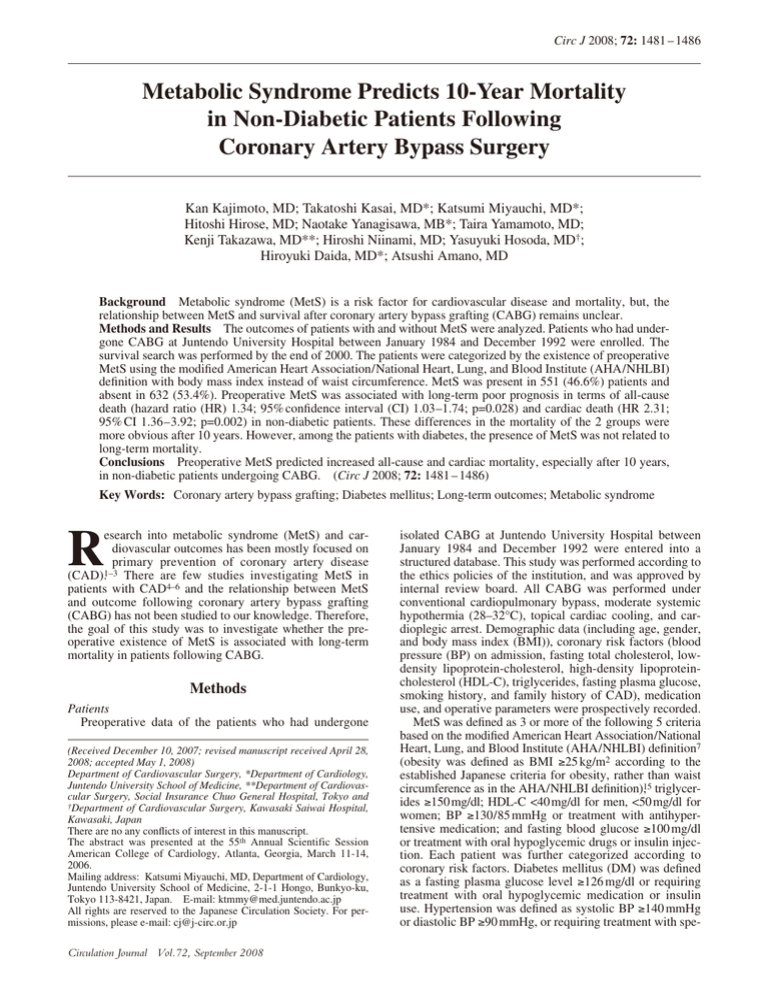
Table 1 Comparison of Patients’ Characteristics Based on the Presence or Absence of MetS
Age (years), mean±SD
Male (%)
3-vessel disease, n (%)
Left main coronary stenosis ≥50%, n (%)
UA, n (%)
Previous MI, n (%)
Previous cardiac operation, n (%)
CCS class 3 or 4, n (%)
Emergency surgery, n (%)
PTCA 0–72 h before surgery, n (%)
LVEF >50%, n (%)
Congestive heart failure, n (%)
BMI, kg/m2, mean±SD
Diabetes mellitus, n (%)
Fasting blood sugar, mmol/L, mean±SD
Hypertension, n (%)
Systolic BP, mmHg, mean±SD
Diastolic BP, mmHg, mean±SD
COPD, n (%)
Peripheral vascular disease, n (%)
Cerebral vascular disease, n (%)
Chronic kidney disease, n (%)
Preoperative dialysis, n (%)
Preoperative IABP, n (%)
LDL-cholesterol, mmol/L, mean±SD
HDL-cholesterol, mmol/L, mean±SD
Triglyceride, g/L, mean±SD
Calcified aorta, n (%)
Current smoker, n (%)
Family history of CAD, n (%)
Preoperative medications
Nitrates, n (%)
ACEI, n (%)
β-blockers, n (%)
Calcium antagonists, n (%)
Aspirin, n (%)
Total bypass time (min), mean±SD
Use of LITA, n (%)
Distal anastomoses, mean±SD
No MetS (n=632)
MetS (n=551)
p value
59±9
535 (85)
427 (68)
81 (13)
101 (16)
245 (39)
2 (0.3)
232 (37)
18 (2.8)
1 (13)
501 (79)
4 (0.6)
22.7±2.3
95 (15)
5.7±1.7
176 (28)
127±17
74±12
5 (0.8)
24 (3.8)
34 (5.4)
227 (36)
7 (1.1)
7 (1.1)
3.9±1.3
1.2±0.3
1.6±1.1
8 (1.3)
453 (72)
180 (29)
59±8
460 (84)
381 (69)
60 (11)
85 (15)
201 (37)
5 (0.9)
186 (34)
13 (2.3)
3 (11)
456 (83)
3 (0.5)
24.4±2.5
179 (33)
6.4±1.9
210 (38)
132±18
77±12
1 (0.2)
24 (4.5)
35 (6.4)
170 (31)
12 (2.2)
5 (0.9)
3.8±1.2
0.9±0.3
2.4±1.2
13 (2.4)
398 (72)
170 (31)
0.36
0.63
0.57
0.32
0.81
0.44
0.26
0.30
0.60
0.32
0.14
1.00
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
0.22
0.66
0.54
0.07
0.17
0.78
0.101
<0.0001
<0.0001
0.19
0.84
0.41
581 (92)
15 (2.4)
222 (35)
200 (32)
264 (42)
159±57
311 (52)
2.4±0.8
510 (93)
21 (3.8)
242 (44)
296 (54)
214 (39)
158±84
285 (54)
2.5±0.8
0.82
0.002
0.02
<0.0001
0.31
0.92
0.54
0.50
MetS, metabolic syndrome; SD, standard deviation; UA, unstable angina; MI, myocardial infarction; CCS, Canadian Cardiovascular Society; PTCA, percutaneous transluminal coronary angioplasty; LVEF, left ventricular ejection fraction; BMI, body mass index;
BP, blood pressure; COPD, chronic obstructive pulmonary disease; IABP, intra-aortic balloon pump; LDL, low-density lipoprotein;
HDL, high-density lipoprotein; CAD, coronary artery disease; ACEI, angiotensin II converting enzyme inhibitors; LITA, left internal
thoracic artery.
cific antihypertensive medications. Chronic kidney disease
(CKD) was defined as glomerular filtration rate <60 ml·
min–1 ·1.73 m–2, calculated by the Cockcroft-Gault equation,
or a requirement for dialysis treatment. A current smoker
was defined as one who smoked at the time of CABG or
had quit smoking within 1 year prior to the procedure.
Outcomes
Survival data were collected by serial contact with the
patients or their families by either telephone interview or
letter with questioners sent every 5 years. The details of
cause of death were obtained from the medical records of
hospitals or by direct contact with private physicians. A
survival search was performed by the end of 2000, and a
common closing day of September 30, 2000 was used for
analysis. Death from myocardial infarction (MI), arrhythmia, congestive heart failure or sudden death was defined
as cardiac death.
Risk Variables
Twenty preoperative risk factors were chosen for analysis:
MetS, age, gender, 3-vessel disease, left main coronary
artery stenosis, percutaneous transluminal coronary angioplasty 0–72 h before operation, unstable angina (UA), previous MI, previous cardiac operation, Canadian Cardiovascular Society angina class 3 or 4, surgical priority, preoperative
intra-aortic balloon pumping, left ventricular ejection fraction (LVEF) <40%, hypertension, CKD, chronic obstructive
pulmonary disease, aortic calcification, smoker, cerebral and
peripheral vascular diseases.
Statistical Analysis
In the comparison of the patients’ characteristics, categorical data are tabulated as frequencies and percentages,
and continuous variables are expressed as mean ± SD. These
data were analyzed using chi-square tests or Student’s t-tests.
Survival curves of both the MetS and Non-MetS groups
were constructed by Kaplan-Meier method and compared
by log-rank test. The effect of MetS on long-term mortality
after CABG was determined using multivariate Cox proportional-hazard regression analysis. From among the 21
risk factors, covariates with a p-value less than 0.10 were
selected for the multivariate analyses. The model was constructed by backward stepwise method first and then by
Circulation Journal Vol.72, September 2008
MetS in Post-CABG Patients
1483
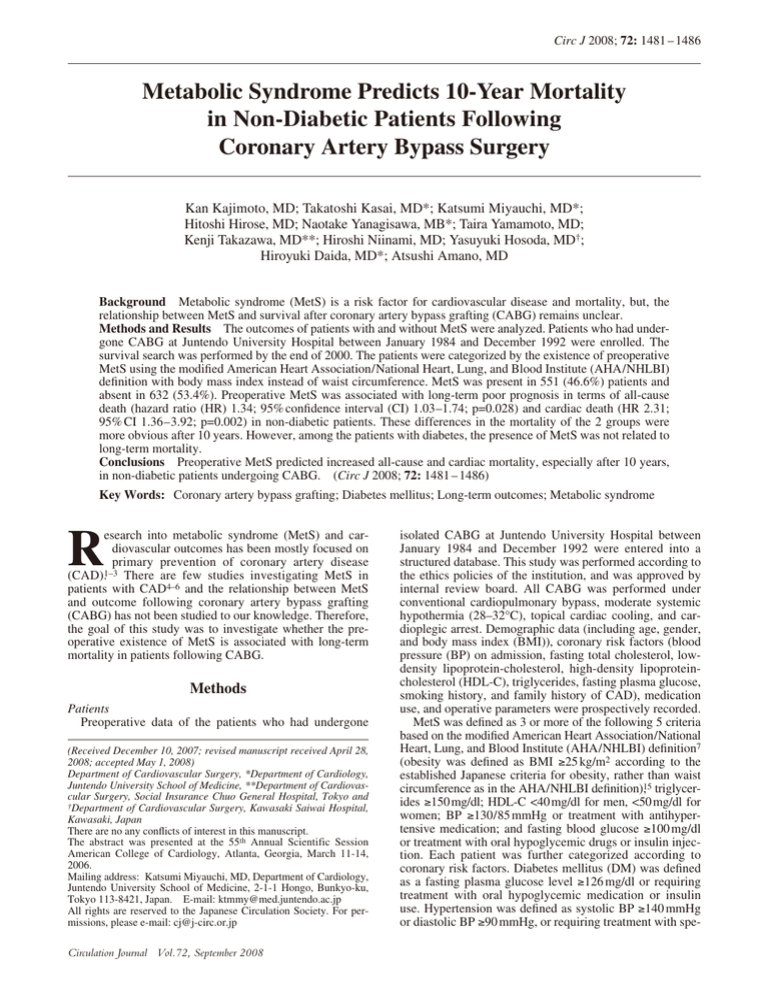
Fig 1. (a) Cumulative survival curves for all-cause death based on the presence or absence of metabolic syndrome.
(b) Cumulative survival curves for cardiac death based on the presence of absence of metabolic syndrome. CABG, coronary artery bypass grafting.
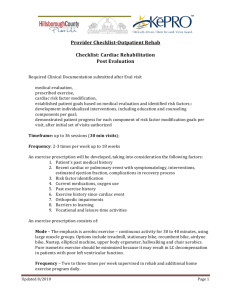
Fig 2. (a) Cumulative survival curves for all-cause death based on the presence of absence of metabolic syndrome in patients without diabetes. (b) Cumulative survival curves for all-cause death based on the presence of absence of metabolic
syndrome in patients with diabetes. (c) Cumulative survival curves for cardiac death based on the presence of absence of
metabolic syndrome in patients without diabetes. (d) Cumulative survival curves for cardiac death based on the presence
of absence of metabolic syndrome in patients with diabetes. CABG, coronary artery bypass grafting.
forward stepwise method. The proportional hazard assumption was checked by including the interaction term between
MetS and other covariates in this model. Presence of MetS
was forced to remain in the multivariate model, and hazard
ratios (HRs) and confidence intervals (CIs) were calculated.
A p-value <0.05 was considered significant. All statistical
analyses were performed using SAS software (SAS Institute,
Circulation Journal Vol.72, September 2008
Cary, NC, USA).
Results
All 1,183 consecutive patients who had isolated CABG
during the study period completed the follow-up. Among
them, 551 (46.6%) met the MetS criteria at the time of
KAJIMOTO K et al.
1484
Table 2 Results of Cox Proportional Hazard Models
Non-diabetes
All-cause death
MetS
Age ≥70 years
Gender, male
CCS angina class 3 or 4
Surgical priority
LVEF ≤40%
Hypertension
Chronic kidney disease
Cerebral vascular disease
Peripheral vascular disease
Cardiac death
MetS
Age ≥70 years
Gender, male
UA
LVEF ≤40%
Hypertension
Chronic kidney disease
Diabetes
HR (95%CI)
p value
HR (95%CI)
p value
1.34 (1.03–1.74)
2.25 (1.59–3.18)
1.93 (1.24–3.01)
1.53 (1.16–2.01)
2.18 (1.05–4.51)
2.16 (1.41–3.30)
1.40 (1.06–1.83)
2.41 (1.76–3.30)
2.26 (1.46–3.51)
2.71 (1.61–4.56)
0.028
<0.0001
0.003
0.002
0.036
<0.0001
0.016
<0.0001
<0.0001
<0.0001
0.84 (0.56–1.27)
1.93 (1.12–3.30)
2.25 (1.27–3.99)
0.86 (0.56–1.34)
1.49 (0.58–3.85)
3.23 (1.82–5.74)
1.43 (0.96–2.15)
4.35 (2.69–7.05)
2.43 (1.28–4.59)
2.52 (1.24–5.14)
0.40
0.017
0.005
0.52
0.41
<0.0001
0.081
<0.0001
0.007
0.011
2.31 (1.36–3.92)
2.25 (1.09–4.63)
3.45 (1.22–9.75)
2.56 (1.41–4.66)
5.03 (2.51–10.1)
2.11 (1.25–3.56)
2.44 (1.31–4.55)
0.002
0.028
0.019
0.002
<0.0001
0.005
0.005
0.75 (0.41–1.36)
1.81 (0.78–4.22)
1.75 (0.78–3.91)
0.86 (0.56–1.34)
2.63 (1.00–6.88)
1.24 (0.68–2.26)
3.86 (1.88–7.92)
0.34
0.17
0.17
0.056
0.049
0.48
<0.0001
HR, hazard ratio; CI, confidence interval. Other abbreviations as in Table 1.
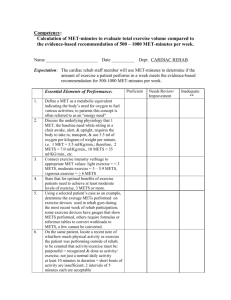
Fig 3. (a) Cumulative survival curves for all-cause death based on
the presence of absence of diabetes. (b) Cumulative survival curves
for cardiac death based on the presence of absence of diabetes.
CABG, coronary artery bypass grafting.
CABG, while 632 (53.4%) did not. The comparisons of the
baseline characteristics and operative variables of the 2
groups are shown in Table 1.
During a mean follow-up period of 10.5±3.6 years, there
were 343 (29%) deaths including 106 (9.0%) cardiac
deaths. The cumulative survival curves for all-cause mortality grouped by the presence of MetS are shown in Fig 1a:
the 12-year survival rate was 68.5% in the MetS group and
74.0% in the non-MetS group. The log-rank test showed
that preoperative MetS was associated with a lower survival rate (p=0.006). The cumulative survival curves from
cardiac mortality are shown in Fig 1b: the 12-year cardiac
death-free rate was 87.7% in the MetS group and 92% in
the non-MetS group (p=0.001).
The other causes of death were neoplasm [40 (6.3%) in
non-MetS vs 35 (6.4%) in MetS, p=0.726], cerebrovascular
disease [24 (3.8%) vs 23 (4.2%), p=0.591], infection [18
(2.8%) vs 20 (3.6%), p=0.278], renal failure [11 (1.7%) vs
5 (0.9%), p=0.271], hepatic failure [4 (0.6%) vs 3 (0.5%),
p=0.913], respiratory failure [3 (0.5%) vs 2 (0.4%), p=
0.851], and others [22 (3.5%) vs 27 (4.9%), p=0.124.
In the risk analyses using the Cox proportional-hazard
models, a significant interaction was found between MetS
and DM. Therefore, further analysis was performed separately for the presence or absence of DM. Among the 909
non-diabetic patients, 537 had MetS and 372 did not. The
results of survival analysis of the patients with or without
DM are shown in Fig 2. Among the non-diabetic patients,
the survival of those with MetS was significantly lower than
those without MetS (p=0.036). However, among the diabetic patients, there was no difference between the survival
outcomes of the patients with or without MetS (p=0.86).
The result from the Cox proportional hazard model for allcause death is shown in Table 2. All 10 risk variables had an
association with long-term death by model selection. MetS
at the time of CABG was a risk factor (HR 1.34, 95% CI
1.03–1.74, p=0.028) in the non-diabetic patients; however,
among the diabetic patients, the presence of MetS was not
associated with long-term outcome.
In the survival analysis for cardiac mortality, the survival of the patients without DM was significantly superior
in those without MetS than in those with MetS (Fig 2c;
p=0.002). In contrast, survival was similar for patients with
DM regardless of MetS (Fig 2d; p=0.60). The result from
the Cox proportional hazard model for cardiac death is
shown in Table 2. A total of 7 risk variables (MetS, older
age, male gender, UA, LVEF <40%, hypertension, and
CKD) had an association with long-term death by model
selection. MetS was identified as a predictor of cardiac
death (HR 2.31, 95% CI 1.36–3.92, p=0.002) among patients without DM, but not among patients with DM
(Table 2).
In addition, patients with DM had higher all-cause mortality when compared with patients without DM (Fig 3a).
With respect to cardiac death, the Kaplan-Meier curve
Circulation Journal Vol.72, September 2008
MetS in Post-CABG Patients
1485
demonstrated that patients with DM had higher mortality
than patients without DM (Fig 3b).
saphenous vein disease most likely has an impact on cardiac
death.
Discussion
Study Limitations
Firstly, this was a post hoc investigation. In addition,
there are some differences in treatment between this study
and the current surgical era; for instance, cardiopulmonary
bypass is now used for all CABG, the use of arterial grafts
has reduced, and perioperative medications and eligibility
for surgical revascularization have changed over time.
Another limitation is that the present study identified obesity on the basis of BMI, as waist circumference measurements were not available; however, studies have demonstrated a concordance between a diagnosis of MetS based
on BMI and that based on waist circumference.17,18 A BMI
≥25 kg/m2 was selected as the cut-off point for obesity
based on the result of a previous study of the relationship
between BMI visceral fat area or waist circumference and
obesity in a Japanese population.8 In contrast, if waist
circumstance had been used as a definition of obesity for
the detection of MetS, more specific results might have been
obtained. This study is also limited by a lack of data on the
progression of each risk factor in MetS, including new
onset of overt DM, hypertension, and dyslipidemia. Furthermore, this study is limited by the homogeneous patient
population (almost all were Asian) and the fact that the
patients were all treated in the same institution.
MetS is a known risk factor for CAD in the general population,1–3 and is a known risk factor for cardiovascular events
and non-cardiovascular-related mortalities in patients with
CAD.4–6 However, MetS was previously unknown in patients with CABG. Although the risk factors of 10-year
death have been identified in multiple studies of patients
with previous CABG,6–9 we are the first to include MetS.
The present study demonstrated that preoperative MetS,
together with the other classic risk factors, is an independent predictor of poor long-term outcome after CABG.
Furthermore, in comparison with the non-MetS group, the
MetS group had more patients with DM, hypertension, and
obesity, which were previously considered independent risk
factors after CABG.9–13 The impact of preoperative MetS in
post-CABG patients has not been documented.
It has been shown that MetS is associated with other
atherosclerotic diseases, including cerebral stroke and renal
dysfunction,6 but we were unable to find significant differences in the cause of death, other than cardiac death,
between patients with and without MetS. The higher total
death rate in the MetS group compared with the non-MetS
group was related to the higher cardiac mortality in MetS
patients than in non-MetS patients.
Risk factors for the development of saphenous vein graft
disease include the presence of DM, hyper low-density
lipoproteinemia, and hypertension,14 which in the present
study were more frequently observed in patients with
MetS. Yilmaz et al reported that MetS increased the risk of
saphenous vein graft disease,15 and may contribute to the
progression of saphenous vein graft disease, possibly
affecting long-term survival.
Increases in both all-cause and cardiac death became
apparent by approximately 10 years after surgery and this
effect of MetS on survival after CABG was stronger in nonDM patients than in DM patients. Patients without DM, but
with MetS at the time of surgery, are more likely to have
late-onset DM. This phenomenon may be appreciated from
our finding that the proportions of deaths in patients with
and without MetS were similar until approximately 9 years
of follow-up, at which time the reduced survival in patients
with MetS became apparent (10 years after CABG). Similarly, the higher 12-year survival observed in patients without DM, but with MetS (92%), than in patients with DM,
but without MetS (76%), became similar at 15 years (76%
and 74%, respectively). The underlying mechanism of MetS
is related to insulin resistance,16 and MetS is a pre-diabetic
status. Therefore, it is possible that some non-DM, but
MetS, patients developed DM during the follow-up period,
because MetS is associated with new onset of DM.11 These
pre-diabetic patients or possible late-developing DM patients may have had further progression of CAD and therefore poor long-term outcomes. In fact, our analysis also
showed that the presence of DM was a strong risk factor
after CABG, so the prevention of DM is important for
improving the long-term prognosis after CABG.
Saphenous vein grafts were frequently used during this
study. MetS may contribute to the progression of saphenous
vein graft disease, which may also affect long-term survival,
as demonstrated by Yilmaz et al who reported that MetS increased the risk of saphenous vein graft disease.15 Increased
Circulation Journal Vol.72, September 2008
Conclusions
This study is the first large observational report to evaluate the relationship between MetS and outcomes 10 years
after cardiac revascularization surgery. It demonstrated that
preoperative MetS predicted increased all-cause death and
cardiac mortality in non-diabetic, but not diabetic, individuals. Our findings suggest that MetS plays important role
with regard to secondary prevention after CABG. Thus,
components of MetS should continue to be monitored and
treated aggressively even after CABG.
References
1. Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissén M, et al.
Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001; 24: 683 – 689.
2. Malik S, Wong ND, Franklin SS, Kamath TV, L’Italien GJ, Pio JR,
et al. Impact of the metabolic syndrome on mortality from coronary
heart disease, cardiovascular disease, and all causes in United States
adults. Circulation 2004; 110: 1245 – 1250.
3. Langenberg C, Bergstrom J, Scheidt-Nave C, Pfeilschifter J, BarrettConnor E. Cardiovascular death and the metabolic syndrome: Role of
adiposity-signaling hormones and inflammatory markers. Diabetes
Care 2006; 29: 1363 – 1369.
4. Levantesi G, Macchia A, Marfisi R, Franzosi MG, Maggioni AP,
Nicolosi GL, et al. Metabolic syndrome and risk of cardiovascular
events after myocardial infarction. J Am Coll Cardiol 2005; 46:
277 – 283.
5. Rana JS, Monraats PS, Zwinderman AH, de Maat MP, Kastelein JJ,
Doevendans PA, et al. Metabolic syndrome and risk of restenosis in
patients undergoing percutaneous coronary intervention. Diabetes
Care 2005; 28: 873 – 877.
6. Nigam A, Bourassa MG, Fortier A, Guertin MC, Tardif JC. The
metabolic syndrome and its components and the long-term risk of
death in patients with coronary heart disease. Am Heart J 2006; 151:
514 – 521.
7. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH,
Franklin BA, et al; American Heart Association; National Heart,
Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart,
Lung, and Blood Institute Scientific Statement. Circulation 2005;
112: 2735 – 2752.
KAJIMOTO K et al.
1486
8. Examination Committee of Criteria for ‘Obesity Disease’ in Japan;
Japan Society for the Study of Obesity. New criteria for ‘obesity
disease’ in Japan. Circ J 2002; 66: 987 – 992.
9. Rajakaruna C, Rogers CA, Suranimala C, Angelini GD, Ascione R.
The effect of diabetes mellitus on patients undergoing coronary
surgery: A risk-adjusted analysis. J Thorac Cardiovasc Surg 2006;
132: 802 – 810.
10. Gao D, Grunwald GK, Rumsfeld JS, Schooley L, MacKenzie T,
Shroyer AL. Time-varying risk factors for long-term mortality after
coronary artery bypass graft surgery. Ann Thorac Surg 2006; 81:
793 – 799.
11. van de Wal RM, van Brussel BL, Voors AA, Smilde TD, Kelder JC,
van Swieten HA, et al. Mild preoperative renal dysfunction as a predictor of long-term clinical outcome after coronary bypass surgery.
J Thorac Cardiovasc Surg 2005; 129: 330 – 335.
12. Pan W, Hindler K, Lee VV, Vaughn WK, Collard CD. Obesity in
diabetic patients undergoing coronary artery bypass graft surgery is
associated with increased postoperative morbidity. Anesthesiology
2006; 104: 441 – 447.
13. Sabik JF 3rd, Blackstone EH, Gillinov AM, Banbury MK, Smedira
NG, Lytle BW. Influence of patient characteristics and arterial grafts
14.
15.
16.
17.
18.
on freedom from coronary reoperation. J Thorac Cardiovasc Surg
2006; 131: 90 – 98.
Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease:
Pathogenesis, predisposition, and prevention. Circulation 1998; 97:
916 – 931.
Yilmaz MB, Guray Y, Guray U, Biyikoglu SF, Tandogan I, Korkmaz
S. Metabolic syndrome negatively impacts early patency of saphenous
vein grafts. Coron Artery Dis 2006; 17: 41 – 44.
Bonora E, Targher G, Formentini G, Calcaterra F, Lombardi S,
Marini F, et al. HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects:
Prospective data from the Verona Diabetes Complications Study.
Diabetes Care 2002; 25: 1135 – 1141.
Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR,
Heymsfield SB. The metabolic syndrome: Prevalence and associated
risk factor findings in the US population from the Third National
Health and Nutrition Examination Survey, 1988 – 1994. Arch Intern
Med 2003; 163: 427 – 436.
Ingelsson E, Arnlov J, Lind L, Sundstrom J. Metabolic syndrome
and risk for heart failure in middle-aged men. Heart 2006; 92: 1409 –
1413.
Circulation Journal Vol.72, September 2008