Availability of audiological equipment and protocols for paediatric
advertisement
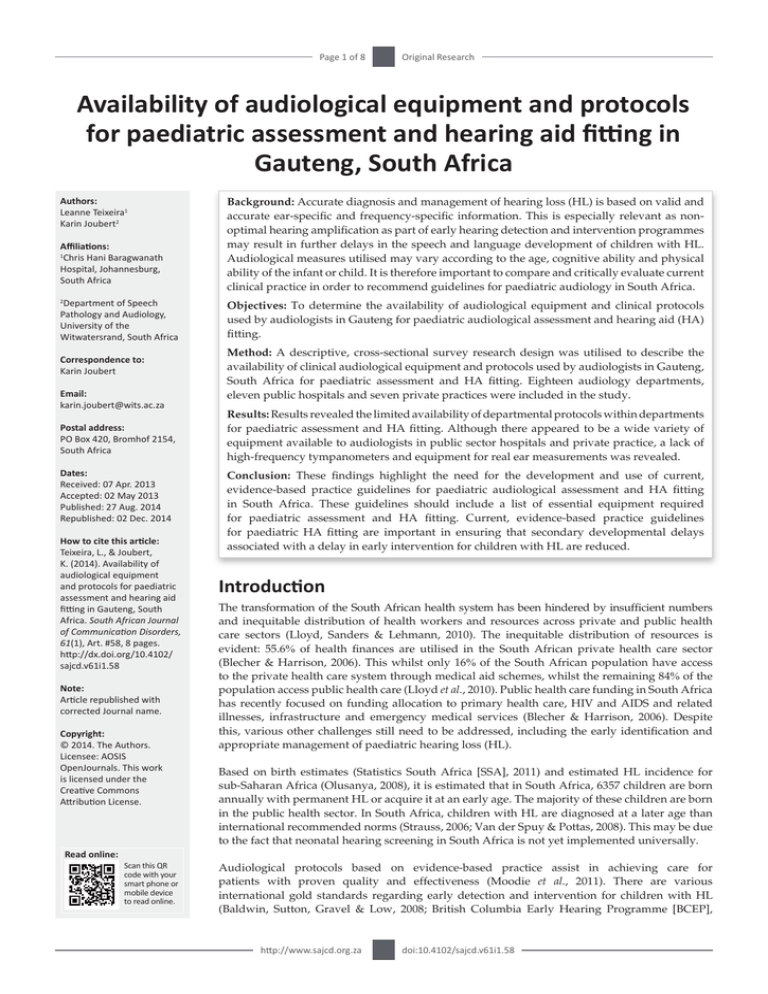
Page 1 of 8 Original Research Availability of audiological equipment and protocols for paediatric assessment and hearing aid fitting in Gauteng, South Africa Authors: Leanne Teixeira1 Karin Joubert2 Affiliations: 1 Chris Hani Baragwanath Hospital, Johannesburg, South Africa Department of Speech Pathology and Audiology, University of the Witwatersrand, South Africa 2 Correspondence to: Karin Joubert Email: karin.joubert@wits.ac.za Postal address: PO Box 420, Bromhof 2154, South Africa Dates: Received: 07 Apr. 2013 Accepted: 02 May 2013 Published: 27 Aug. 2014 Republished: 02 Dec. 2014 How to cite this article: Teixeira, L., & Joubert, K. (2014). Availability of audiological equipment and protocols for paediatric assessment and hearing aid fitting in Gauteng, South Africa. South African Journal of Communication Disorders, 61(1), Art. #58, 8 pages. http://dx.doi.org/10.4102/ sajcd.v61i1.58 Note: Article republished with corrected Journal name. Copyright: © 2014. The Authors. Licensee: AOSIS OpenJournals. This work is licensed under the Creative Commons Attribution License. Background: Accurate diagnosis and management of hearing loss (HL) is based on valid and accurate ear-specific and frequency-specific information. This is especially relevant as nonoptimal hearing amplification as part of early hearing detection and intervention programmes may result in further delays in the speech and language development of children with HL. Audiological measures utilised may vary according to the age, cognitive ability and physical ability of the infant or child. It is therefore important to compare and critically evaluate current clinical practice in order to recommend guidelines for paediatric audiology in South Africa. Objectives: To determine the availability of audiological equipment and clinical protocols used by audiologists in Gauteng for paediatric audiological assessment and hearing aid (HA) fitting. Method: A descriptive, cross-sectional survey research design was utilised to describe the availability of clinical audiological equipment and protocols used by audiologists in Gauteng, South Africa for paediatric assessment and HA fitting. Eighteen audiology departments, eleven public hospitals and seven private practices were included in the study. Results: Results revealed the limited availability of departmental protocols within departments for paediatric assessment and HA fitting. Although there appeared to be a wide variety of equipment available to audiologists in public sector hospitals and private practice, a lack of high-frequency tympanometers and equipment for real ear measurements was revealed. Conclusion: These findings highlight the need for the development and use of current, evidence-based practice guidelines for paediatric audiological assessment and HA fitting in South Africa. These guidelines should include a list of essential equipment required for paediatric assessment and HA fitting. Current, evidence-based practice guidelines for paediatric HA fitting are important in ensuring that secondary developmental delays associated with a delay in early intervention for children with HL are reduced. Introduction The transformation of the South African health system has been hindered by insufficient numbers and inequitable distribution of health workers and resources across private and public health care sectors (Lloyd, Sanders & Lehmann, 2010). The inequitable distribution of resources is evident: 55.6% of health finances are utilised in the South African private health care sector (Blecher & Harrison, 2006). This whilst only 16% of the South African population have access to the private health care system through medical aid schemes, whilst the remaining 84% of the population access public health care (Lloyd et al., 2010). Public health care funding in South Africa has recently focused on funding allocation to primary health care, HIV and AIDS and related illnesses, infrastructure and emergency medical services (Blecher & Harrison, 2006). Despite this, various other challenges still need to be addressed, including the early identification and appropriate management of paediatric hearing loss (HL). Based on birth estimates (Statistics South Africa [SSA], 2011) and estimated HL incidence for sub-Saharan Africa (Olusanya, 2008), it is estimated that in South Africa, 6357 children are born annually with permanent HL or acquire it at an early age. The majority of these children are born in the public health sector. In South Africa, children with HL are diagnosed at a later age than international recommended norms (Strauss, 2006; Van der Spuy & Pottas, 2008). This may be due to the fact that neonatal hearing screening in South Africa is not yet implemented universally. Read online: Scan this QR code with your smart phone or mobile device to read online. Audiological protocols based on evidence-based practice assist in achieving care for patients with proven quality and effectiveness (Moodie et al., 2011). There are various international gold standards regarding early detection and intervention for children with HL (Baldwin, Sutton, Gravel & Low, 2008; British Columbia Early Hearing Programme [BCEP], http://www.sajcd.org.za doi:10.4102/sajcd.v61i1.58 Page 2 of 8 2008; Joint Committee on Infant Hearing [JCIH], 2007). These guidelines highlight the importance of using appropriate audiological equipment and age-appropriate measures during early HL detection and intervention (EHDI), to ensure the appropriate diagnosis and management of paediatric HL. In South Africa, the Health Professions Council of South Africa’s (HPCSA) position statement on EHDI (HPCSA, 2007) describes the age at which intervention should be initiated, as well as what early intervention should involve. The position statement recommends that, in a hospital-based setting, HL should be identified by 3 months of age and intervention provided by 6 months of age, whilst in a clinic-based setting, HL should be identified by 4 months of age and intervention provided by 8 months of age. This guideline, however, only includes limited information on how audiological results should be used for HA fitting. The goal of paediatric audiological assessment is to determine whether permanent HL is present and, if required, to initiate a management plan as directed by the child’s family (BCEP, 2008). This process involves the application of a test-battery approach to determine the exact nature of the HL, as well as evaluating the integrity of the auditory pathway (Diefendorf, 2009). This ensures that an accurate diagnosis is made, based on valid and accurate ear-specific and frequency-specific hearing information (BCEP, 2008). The audiological measures utilised may vary according to the age, cognitive ability and physical ability of the infant or child (Diefendorf, 2009). Case history and clinical observation are important components of the audiological assessment of children of all ages. Both these components provide the clinician with an understanding of a child’s overall development, which will guide audiological procedures used during assessment (Diefendorf, 2009). A test battery for audiological assessment of children from birth to 6 months may, in addition, include a family report and observations; high-frequency (1000 Hz) tympanometry and acoustic reflexes; oto-acoustic emissions (OAEs); auditory brainstem response (ABR) (Gravel, 2000); cochlear microphonic (CM); and auditory steady-state response (ASSR) (Stevens, Sutton, Wood & Mason, 2007). Behavioural testing can usually be included as part of the test battery from 5 to 6 months of age (Madell, 2008), as well as using a low-frequency immittance probe tube from 6 months of age (Baldwin et al., 2008). Research exploring EHDI services in South Africa found that only 2% of the hospitals surveyed conducted universal hearing screening (Theunissen & Swanepoel, 2008). The reasons provided for the lack of universal screening included the lack of staff and equipment. The researchers further reported that only 34% of hospitals had access to screening equipment (such as an OAE screener and/or automated ABR) (Theunissen & Swanepoel, 2008). However, there is limited information on the availability of equipment and protocols used for diagnostic paediatric audiological assessment and http://www.sajcd.org.za Original Research management in South Africa. Together with the necessary resources (equipment and staff), a sustainable programme for EHDI should be based on evidence-based protocols. Hyde (2010) clearly states the importance of clinical protocols: Good protocols are absolutely and unquestionably essential for all major components of a high quality EHDI program. Without them, high effectiveness, equity and efficiency of services are virtually impossible to achieve, sustain or improve. (p. 64) Despite this, Strauss (2006) found that only 35% of individual audiology departments surveyed in South Africa reported following a protocol for EHDI. Without adequate resources (such as equipment and skilled paediatric audiologists) and evidence-based protocols the implementation of a sustainable EHDI programme will remain a challenge in South Africa. It is thus important to compare and critically evaluate current clinical practice in order to recommend guidelines for paediatric audiology in South Africa. This is especially relevant as non-optimal HA fitting as part of EHDI may result in further delays in the speech and language development of children with HL (Yoshinago-Itano, Sedey, Coulter & Mehl, 1998). Due to the dearth of information on the current clinical practice, this study addressed the following question: What is the clinical practice of South African audiologists, with specific reference to the availability of audiological equipment and protocols for paediatric audiological assessment? Method Aim The study aimed to: • determine the availability of clinical audiological equipment used by audiologists in Gauteng for paediatric audiological assessment and HA fitting • determine the availability of clinical protocols used by audiologists in Gauteng for paediatric audiological assessment and HA fitting. Research design A non-experimental, descriptive, cross-sectional survey research design was utilised for the purposes of the study. A questionnaire was developed by consulting current evidence-based practice protocols, and refined after a pilot study was completed. The self-developed questionnaire administered through face-to-face interviews assisted in ensuring high response rates and allowed the researchers to describe the current clinical practice of audiologists employed in Gauteng. Participants Sampling strategy A non-probability, purposive sampling strategy was employed to recruit as many participants as possible who met the participant selection criteria (Cresswell, 2003). Participants in this study were required to be audiologists working in doi:10.4102/sajcd.v61i1.58 Page 3 of 8 departments that render paediatric audiological services in either the private or public health care sector in Gauteng. Participant description Of the 23 potential audiology departments and practices in Gauteng, a total of 18 audiology departments (N = 18) agreed to participate in this study. Participants had to be performing paediatric ABR or ASSR testing and/or be fitting hearing aids to children based on such results. A total of 34 interviews were conducted: 27 within the public health sector and 7 within the private health sector. Public sector audiology departments comprised 61% of the sample (n1 = 11), whilst private audiology practices comprised the remaining 39% (n2 = 7). More than one participant from each department was interviewed if they were willing to participate in the study. This allowed for comparison of participants’ responses to the same questions. In some cases, more than one participant from public health sector departments were interviewed. This was not the case in private audiology practices, where often only one clinician was employed or available due to smaller departmental staff size. If more than one participant was interviewed per department, between two and four participants were interviewed, depending on their availability and departmental staff size. The majority of participants (82%; n = 28) included in the study were qualified as both speech-language pathologists and audiologists, whilst 18% (n = 6) of participants were qualified as audiologists only. Since qualifying, 26% (n = 9) of the dually qualified therapists were now practicing as audiologists only. Participants’ years of experience ranged from < 1 year to > 15 years. The majority of participants (68%; n = 23) had 4 or less years’ experience. Private practice participants had the most years of experience. Fifty-seven percent of the private practice participants had 10 or more years’ experience, whilst only 7% of the public sector participants had 10 or more year’s clinical experience. Materials A self-developed structured questionnaire with predominantly close-ended questions was used during the face-toface interviews. The questionnaire included eight sections, but for the purposes of this article only the sections related to current clinical practice will be reported on. These sections included the availability of audiological equipment and departmental protocols for paediatric assessment and management (see Appendix 1). Procedures Ethical considerations Various ethical considerations were implemented throughout the research study. The researcher obtained ethical clearance from the University of the Witwatersrand Research Ethics Committee and written permission from the Gauteng Department of Health to conduct this study. All participants in the study were fully informed of the nature of the study and were assured of confidentiality. Each participant was http://www.sajcd.org.za Original Research required to sign a consent form, providing proof of their willingness to participate in the study. They further had the right to withdraw from the study at any time, without any negative consequences. Only participants who signed the consent forms were included in the study. Data collection Data was collected during November and December 2010. Once possible participants were identified, they were contacted telephonically, informed of the nature of the study and invited to participate. Appointments were made at times that were convenient for participants. Participants received a written information sheet detailing the information discussed telephonically and once participant consent was obtained the self-developed questionnaire was administered via individual personal interviews. Data was documented on the measuring instrument. Participants were thanked for their participation. Reliability and validity Various measures were adopted to improve the validity and reliability of this study. Content validity was achieved by consulting current literature and experienced professionals in the field whilst developing the questionnaire. In addition, a pilot study was conducted to finalise the measuring instrument and data collection procedures. In an attempt to minimise the Hawthorne effect, it was made clear to participants that there were no correct or incorrect answers to the questions. Interviews were not electronically recorded, but participants were provided opportunity to discuss or elaborate on their responses to questions. Faceto-face interviews assisted in ensuring that participants could not consult one another regarding their responses to questions, improving reliability of responses, as well as allowing for comparison of participants’ responses to the same questions, in order to analyse participants’ awareness of resources such as protocols and equipment. As this study was only conducted in the Gauteng province, generalisation of results to clinical practice and availability of resources across the whole of South Africa could not be assumed (Cresswell, 2003). Data analysis Data was documented on all relevant measuring instruments and encoded for data analysis. All data was computerised for statistical analysis with Microsoft Excel and SigmaXL 6.11 software packages. Results were analysed utilising descriptive statistics (such as measures of central tendency and variability) that assisted in the summary and organisation of the collected data. Results Availability of audiological equipment Participants were provided with a list of audiological equipment and requested to indicate which of these were doi:10.4102/sajcd.v61i1.58 Public % n 27 3 9 1 9 1 18 2 18 2 9 1 9 1 n 1 % 6 - Total Private % n Public % n 64 7 64 7 55 6 9 1 36 4 36.5 4 82 9 45.5 5 36 4 64 7 27 3 Public % n 36 4 36 4 100 11 18 2 82 9 100 11 55 5 45.5 5 100 11 100 11 36.5 4 55 6 36 4 73 8 - % 44 61 100 50 6 72 100 50 50 100 100 11 44 50 39 78 6 ASSR Diagnostic ABR Diagnostic audiometer Diagnostic OAEs ECochG Noisemakers Otoscope Screening ABR Screening audiometer Screening OAE Sound-treated booth Sound level meter HF & LF tympanometry LF tympanometry only REMs VRA VNG (1 specified) Private % n 57 4 100 7 100 7 100 7 14 1 57 4 100 7 43 3 57 4 100 7 100 7 29 2 57 4 43 3 43 3 86 6 14 1 Total n 8 11 18 9 1 13 18 9 9 18 18 2 8 9 7 14 1 Private % n 43 3 43 3 57 4 43 3 71 5 43 3 57 4 57 4 14 1 - Not available Available % 56 39 33 22 44 39 78 44 44 61 22 - Total n 10 7 6 4 8 7 14 8 8 11 4 - Departments Equipment TABLE 1: Equipment available at private and public sector audiology departments (N =18). ASSR, Auditory steady-state response; ABR, auditory brainstem response; OAEs; oto-acoustic emissions; ECochG, electrocochleography; HF, high-frequency; LF, low-frequency; REMs, real ear measures; VRA, visual reinforcement audiometry; VNG, videonystagmography. †Varied responses (that is, participants from the same public audiology department provided differing responses regarding whether equipment was available or not). Varied responses† Public % n 9 1 - Private % n Unsure % 17 6 6 11 11 6 6 - Total n 3 1 1 2 2 1 1 - Page 4 of 8 http://www.sajcd.org.za Original Research available in their department or practice. The results are presented in Table 1. All departments (N = 18) reported having access to soundtreated booths, otoscopes, diagnostic audiometers and screening OAEs. Only 44% (n = 8) of departments had access to ASSR, whilst slightly more departments (61%, n = 11) had access to diagnostic ABR equipment. All private sector departments (n2 = 7) reported having access to diagnostic OAE equipment, whilst only 18% (n1 = 2) of public sector departments reported having access to such equipment. Seventy-two percent (n = 13) of departments had access to noisemakers, of which 82% (n1 = 9) were public sector departments and 57% (n2 = 4) were private sector departments. With regard to other screening equipment, 50% (n = 9) of departments reported having access to both screening ABR and screening audiometers. Only two audiology departments (11%), which were within the private sector, reported having access to sound level meters (SLMs). There was limited availability of real ear measure (REM) equipment for verification of HA fitting, as only 39% (n = 7) of departments reported having access to such equipment. This was for both private and public audiology departments. Availability of REM equipment was similar for both private (43%, n2 = 3) and public (36%, n1 = 4) sector departments. All departments (N = 18) reported having access to some form of tympanometry. Fifty percent (n = 9) of departments reported having access to low-frequency tympanometry, whilst 44% (n = 8) of departments reported having access to high-frequency probe tone tympanometry. The remaining department (6%) was unsure whether their immittance equipment had both high-frequency and low-frequency probe tone options or not. Only 57% (n2 = 4) of the 7 private sector departments reported having high-frequency tympanometry, but all reported seeing babies of less than 6 months of age. All but one public sector department (91%, n1 = 10) reported seeing infants from birth to 6 months of age. Despite this, only 36.5% (n1 = 4) of the 11 public sector departments interviewed reported having access to highfrequency tympanometry. Some public sector departments further reported that certain equipment was not functioning and that their hospital employer had not provided funding for the timely repair of equipment. As seen in Table 1, some public health sector participants from the same department gave varied responses regarding the availability of equipment in their department. Varied responses regarding the presence of equipment per public sector audiology department were given regarding diagnostic OAEs, noisemakers, screening ABR and screening audiometers, SLMs as well as high-frequency and low-frequency probe tone tympanometers. doi:10.4102/sajcd.v61i1.58 Page 5 of 8 Departmental protocols for paediatric assessment and HA fitting It is vital that audiological practice is evidence-based in order to ensure that patients’ audiological needs are appropriately met, whilst being of a high standard, as well as assisting with continuity of care with staff turn-over. The presence of protocols for paediatric assessment (including ABR and ASSR) and HA fitting within departments was probed. Results indicate that only 28% of departments (n = 5) reported having a paediatric HA fitting protocol. In some departments, more than one audiologist was interviewed. Nine percent (n = 3) of the 34 individual participants in the study were unsure whether their department had a paediatric HA fitting protocol or not. Furthermore, although 44% (n = 15) of participants reported having a paediatric HA fitting protocol, when comparing the response to this question across participants at the same department, not all (n = 4) responded with the same answer. Seven public sector departments had more than one participant. Eleven of the 18 participating departments reported that they perform ABR and/or ASSR testing. Only three (27%) of these departments had protocols for paediatric ABR and/ or ASSR assessment. At one public sector department (9%), responses regarding the presence of a protocol varied across participants. Participants were asked for copies of their ABR and/or ASSR assessment protocol, if available. The protocols reviewed appeared to be mainly procedural with limited direct reference to current evidence-based practice or comprehensive reference lists. Discussion Overall, there appeared to be a wide variety of equipment available to both the private and public sector departments included in this study. However, this equipment was not always adequate in terms of meeting the audiological needs of all paediatric patients. Public sector departments were more limited than private sector departments in terms of access to certain types of equipment and experienced particular challenges regarding the timely repair of equipment by hospital management. The lack of functioning, well-maintained audiological equipment may affect a clinician’s ability to undertake appropriate evidence-based audiological practices. The varied responses of some public sector participants regarding the availability of equipment suggest a lack of awareness of resources available. This may be due to high staff turn-over and lack of carry-over, including information regarding availability of equipment. This lack of awareness of available resources results in the underutilisation of equipment as well as delivering services that may not be appropriate or meet a child’s audiological needs. Of particular concern is the limited availability of highfrequency probe tone tympanometry. The importance of using an appropriate immittance probe tone to accurately http://www.sajcd.org.za Original Research determine the middle-ear status of a child cannot be underestimated. Recommended practice stipulates the use of a 1000-Hz rather than a 226-Hz probe tone for immittance assessment of infants less than 6 months corrected age (Baldwin et al., 2008). Appropriate evaluation of middleear status is of particular importance in South Africa, where HIV and AIDS are major health challenges prioritised in the public health care sector (Open Society Foundation for South Africa, 2007). Children with HIV or AIDS may have recurrent bacterial infections, neurologic disease or developmental problems (Muma, Lyons, Borucki & Pollard, 1997). Due to recurrent infections, these children may require more frequent monitoring of their middle-ear status and hearing. It is therefore important to accurately undertake tympanometry measures utilising the appropriate probe tone. According to Valente and Valente (2009, p. 858), ‘[t]he most reliable and efficient method for assessing the performance provided by amplification is real ear measures’. Despite this, the majority of participants indicated that REMs are not routinely conducted to verify paediatric HA fittings. The majority of participants reported lack of equipment as the main reason. Other reasons provided included malfunctioning equipment; unfamiliarity with the equipment; infrequent fittings not justifying the cost of the equipment; and REMs being too time consuming or unreliable. In addition, it was reported that REMs were only completed if the child was making insufficient progress, or if they were older than 6 years. Some participants also reported that they rely on other measures such as aided testing, parental report and checklists. This feedback is disconcerting as objective verification ensures that target gain, compression ratio and threshold as well as output levels are met, resulting in optimal HA fitting (Beauchaine, 2001). The use of current, evidence-based practice for paediatric HA fitting is important in ensuring that secondary developmental delays associated with a delay in early intervention for children with HL are reduced. However, the current study established that departments have limited protocols for paediatric assessment and HA fitting. The lack of departmental protocols is concerning, as it makes meeting the needs of patients and families, development of services, consistent clinical practice, as well as adherence to current, evidence-based practice challenging. The approach to paediatric HA fitting is unique and differs from adult HA fitting due to various factors, such as smaller ear canals and different listening needs. As an infant’s ear canal is smaller, higher sound pressure levels (SPLs) will be produced in the ear canal than in an adult’s (BCEP, 2008). The listening needs of a child also differ from those of an adult. For children, the goal of amplification is to promote oral speech and language development. For adults, however, acquired HL is usually post-lingual. Language, cognitive and world knowledge can thus be utilised to facilitate understanding of acoustic information (Stelmachowicz & Hoover, 2009). For equivalent speech recognition ability, young children require doi:10.4102/sajcd.v61i1.58 Page 6 of 8 Original Research greater SPLs than adults (Stelmachowicz, Hoover, Lewis, Kortekaas & Pittman, 2000). Acknowledgements Protocols should be utilised within all areas of paediatric audiology, including ABR and ASSR assessment and HA fitting. It is vital to ensure that protocols are as focused as possible and encompass all relevant areas to ensure that clinical practice is evidence-based. An evidence-based approach assists in putting research into clinical practice, improves patient care and promotes standardisation of care (Moodie et al., 2011). The authors declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article. Conclusion Despite the fact that this study was limited to the Gauteng province, which restricted the generalisability of the results, it is representative of the typical distribution of audiology departments and private practices in Gauteng. The study provides specific information regarding the availability of clinical audiological equipment and protocols currently used by audiologists in Gauteng. The findings from this study suggest several recommendations for paediatric audiology in South Africa that would promote development of this area in this country. Firstly, it is recommended that national, evidence-based guidelines or standards that include levels of service delivery and the minimum equipment required are developed for both paediatric assessment and HA fitting. In recent years, draft national guidelines have been in circulation for review and development, but these guidelines have yet to be finalised. Once final guidelines have been released, departments should develop their own internal guidelines by referring to national guidelines and provide clinic-specific procedures, if appropriate. This will assist with standardisation of care and sustainability of services. In the interim, it is recommended that departments develop their own guidelines based on evidence-based practice. Secondly, it is imperative that clinicians have access to well-maintained audiological equipment that is relevant for use in the paediatric population. Adequate funding for the procurement and maintenance of equipment should be a priority, as without fully functioning equipment, audiologists cannot effectively meet the needs of children with HL as outlined in the HPCSA (2007) position statement on EHDI. For universal newborn hearing screening to be a viable project, it should be supported by the National Department of Health, with dedicated funding for human and equipment resources. Given the dearth of information regarding the South African audiological clinical practice, this study provided the groundwork for future, more in-depth, research. This may include refinement and expansion of the current study in various ways that would allow for generalisation of results beyond this specific population. It may be useful to replicate the study once appropriate equipment has been procured and protocols have been implemented in order to monitor changes in clinical practice. http://www.sajcd.org.za Competing interests Authors’ contributions L.T. (Chris Hani Baragwanath Hospital) acted as researcher and K.J. (University of the Witwatersrand) as research supervisor; both contributed equally to writing the manuscript. References Baldwin, M., Sutton, G., Gravel, J., & Low, R. (2008). Tympanometry in babies under 6 months. A recommended test protocol version 2.0. Newborn Hearing Screening Programme (England). Retrieved October 13, 2011, from http://hearing. screening.nhs.uk/audiologyprotocols Beauchaine, K.L. (2001). An amplification protocol for infants. In R.C. Seewald & J.S. Gravel (Eds.), A sound foundation through early amplification (pp. 105–112). Warrenville, IL: Phonak Hearing Systems. Blecher, M., & Harrison, S. (2006). Health care financing. In P. Ijumba & A. Padarath (Eds.), South African health review 2006. Durban: Health Systems Trust. Retrieved September 20, 2011, from http://www.hst.org.za/uploads/files/sahr2006.pdf British Columbia Early Hearing Programme (BCEP) (2008). Diagnostic audiology protocol. Retrieved February 14, 2011, from http://www.phsa. ca/AgenciesServices/Services/BCEarlyHearingPrgs/ForProfessionals/ ProtocolsStandards.htm Cresswell, J.W. (2003). Research design: Qualitative, quantitative and mixed methods approaches. (2nd edn). Thousand Oaks, CA: Sage. Diefendorf, A.O. (2009). Assessment of hearing loss in children. In J. Katz (Ed.), Handbook of clinical audiology (6th edn.) (pp. 545–563). Baltimore, MD: Lippincott Williams & Wilkins. Gravel, J.S. (2000). Audiological assessment for the fitting of hearing instruments: Big challenges from tiny ears. In R. Seewald (Ed.), Proceedings of the A Sound Foundation through early amplification conference (pp. 33–46). Zurich: Phonak AG. Health Professions Council of South Africa (HPCSA). (2007). Professional board for speech, language and hearing profession: Early hearing detection and intervention programmes in South Africa, Position statement, Year 2007, 1–42. Retrieved May 10, 2011, from http://www.hpcsa.co.za/downloads/speech_education/early_ hearing_detection_statement.pdf Hyde, M. (2010). Buzz off, I know what I’m doing – Protocols in EHDI. In R.C. Seewald & J.M. Bamford (Eds.), Proceedings of the fifth international A sound foundation through early amplification conference (pp. 49–66). Chicago, IL: Phonak AG. Joint Committee on Infant Hearing (JCIH). (2007). Year 2007 Position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics, 120, 898–921. http://dx.doi.org/10.1542/peds.2007-2333 Lloyd, B., Sanders, D., & Lehmann, U. (2010). Human resource requirements for national health insurance. In A. Padarath & S. Fonn (Eds.), South African Health Review 2010. Durban: Health Systems Trust. Retrieved January 14, 2011, from http://www.hst.org.za/publications/south-african-health-review-2010 Madell, J.R. (2008). Using visual reinforcement audiometry to evaluate hearing in infants from 5–36 months. In J.R. Madell & C. Flexer (Eds.), Pediatric audiology: Diagnosis, technology, and management (pp. 65–75). New York, NY: Thieme Medical Publishers. Moodie, S.T., Kothari, A., Bagatto, M.P., Seewald, R., Miller, L.T., & Scollie, S.D. (2011). Knowledge translation in audiology: Promoting the clinical application of best evidence. Trends in Amplification, 15(1/2), 5–22. http://dx.doi. org/10.1177/1084713811420740 Muma, R.D., Lyons, B.A., Borucki, M.J., & Pollard, R.B. (1997). HIV manual for health care professionals. Stamford, CT: Appleton & Lange. Olusanya, B.O. (2008). Priorities for early hearing detection and intervention in subSaharan Africa. International Journal of Audiology, 47(Suppl. 1), S3–S13. http:// dx.doi.org/10.1080/14992020802287143 Open Society Foundation for South Africa. (2007). South Africa. Effective service delivery in the education and health sectors. A discussion paper. A review by AfriMAP and Open Society Foundation for South Africa. Newlands: Open Society Foundation for South Africa. Retrieved May 11, 2011, from http://afrimap.org/ english/images/report/AfriMAP_SA_PublicServices.pdf Statistics South Africa (SSA) (2011). Statistical release (P0302). Mid-year population estimates 2011. Retrieved November 25, 2011, from http://www.statssa.gov.za/ Stelmachowicz, P., & Hoover, B. (2009). Hearing instrument fitting and verification for children. In J. Katz (Ed.), Handbook of Clinical Audiology (6th edn.) (pp. 827–845). Baltimore, MD: Lippincott Williams & Wilkins. doi:10.4102/sajcd.v61i1.58 Page 7 of 8 Stelmachowicz, P.G., Hoover, B.M., Lewis, D.E., Kortekaas, R.W., & Pittman, A.L. (2000). The relation between stimulus context, speech audibility, and perception for normal-hearing and hearing-impaired children. Journal of Speech, Language and Hearing Research, 43(4), 902–14. Stevens, J.C., Sutton, G.J., Wood, S., & Mason, S. (2007). Guidelines for the early audiological assessment and management of babies referred from the newborn hearing screening programme. Newborn Hearing Screening Programme: London. Retrieved December 16, 2010, from http://hearing.screening.nhs.uk/cms. php?folder=21 Strauss, S. (2006). Early hearing intervention and support services provided to the paediatric population by South African audiologists. Unpublished master’s thesis, University of Pretoria, South Africa. Retrieved January 15, 2011, from http:// explore.up.ac.za/search~S9?/astrauss%2C+susa/astrauss+susa/1,2,3,B/l856~b17 12567&FF=astrauss+susan&2,,2,1,0/indexsort=- Original Research Theunissen, M., & Swanepoel, D. (2008). Early hearing detection and intervention services in the public health sector in South Africa. International Journal of Audiology, 47(Suppl. 1), S23–S29. http://dx.doi.org/10.1080/14992020802294032 Valente, M., & Valente, M. (2009). Hearing aid fitting for adults: Selection, fitting, verification, and validation. In J. Katz (Ed.), Handbook of clinical audiology (6th edn.) (pp. 846–870). Baltimore, MD: Lippincott Williams & Wilkins. Van der Spuy, T., & Pottas, L. (2008). Infant hearing loss in South Africa: Age of intervention and parental needs for support. International Journal of Audiology, 47(Suppl. 1), S30–S35. http://dx.doi.org/10.1080/14992020802286210 Yoshinago-Itano, C., Sedey, A., Coulter, D.K., & Mehl, A.L. (1998). Language of earlyand later-identified children with hearing loss. Pediatrics, 102(5), 1161–1171. http://dx.doi.org/10.1542/peds.102.5.1161 Appendix starts on the next page http://www.sajcd.org.za doi:10.4102/sajcd.v61i1.58 Page 8 of 8 Appendix 1 • Low-frequency probe (226 Hz) only • Visual reinforcement audiometry (VRA) • Other: ______________________________________________________ Protocol or guidelines 1. Does your department have a paediatric hearing aid fitting protocol or guideline (that is, the assessments or techniques that should be undertaken prior and during hearing aid fitting)? If yes, please provide a copy of the protocol or guideline available. _ ____________________________________________________________ _ ____________________________________________________________ 3. Do you complete real ear measures (REMs) with EVERY paediatric fitting to verify the fitting? (Yes, no or sometimes) 4. If NO, please provide a reason for not completing REMs: Availability of equipment 2. What assessment equipment does your hospital, clinic or practice have? • • • • • • • • • • • • • Original Research Auditory steady-state response (ASSR) Diagnostic auditory brainstem response (ABR) Diagnostic audiometer Diagnostic oto-acoustic emissions (OAEs) Noisemakers Otoscope Screening automated auditory brainstem response (AABR) Screening audiometer Screening OAE Sound-treated booth Sound level meter Tympanometry High-frequency (1000-Hz and 678-Hz) and low-frequency (226-Hz) probe http://www.sajcd.org.za • Lack of equipment • I do not see the need for REMs to be completed • I rely on other measures such as____________________________ _ ____________________________________________________________ • Other: ______________________________________________________ _ ____________________________________________________________ _ ____________________________________________________________ 5. If SOMETIMES, please provide a reason for your answer: • Only if there is time • Only if the child is not making as much progress with his or her hearing aids as expected • Only if requested by another professional or family • I rely on other measures such as____________________________ _ ____________________________________________________________ • Other: ______________________________________________________ _ ____________________________________________________________ _ ____________________________________________________________ doi:10.4102/sajcd.v61i1.58