Repeated Thrombolysis for Chronologically Separated
Ischemic Strokes
A Case Series
Roland Sauer, MD; Hagen B. Huttner, MD; Lorenz Breuer, MD; Tobias Engelhorn, MD;
Peter D. Schellinger, MD; Stefan Schwab, MD; Martin Köhrmann, MD
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Background and Purpose—Recombinant tissue plasminogen activator is used for the treatment of acute myocardial
infarction, pulmonary embolism, and acute ischemic stroke. With many years since approval of the drug and an aging
population, chances increase that patients are treated twice for chronologically separated events.
Methods—We identified patients from the prospective Erlangen Stroke and Thrombolysis Database who received repeated
thrombolysis for acute ischemic stroke. Baseline demographic data and clinical, laboratory, and imaging findings were
analyzed. Functional outcome was assessed after 3 months.
Results—Eight patients treated twice and one patient with 3 treatments were identified. The median time span between first
and second thrombolysis was 10 (3 to 48) months. All patients had a favorable outcome after the first treatment, and
67% of patients had a favorable outcome after the second thrombolysis. Neither allergic reactions nor other
immunoreactive events were observed.
Conclusions—Repeated administration of recombinant tissue plasminogen activator for chronologically separate ischemic
strokes does not appear to be associated with severe immune reactions. Larger case numbers are needed to evaluate
safety and efficacy of repeated systemic thrombolysis. (Stroke. 2010;41:1829-1832.)
Key Words: tissue plasminogen activator 䡲 acute ischemic stroke 䡲 thrombolysis
R
ecombinant tissue plasminogen activator (rt-PA) is used
for treatment of acute myocardial infarction, pulmonary
embolism, and acute ischemic stroke. Development of antibodies against the recombinant protein has been described in
various animal models1,2 and humans.3,4 However, their
relevance for repeated application of the drug is unknown.3,4
Antibodies may influence efficacy of repeated treatment by
neutralizing the active drug and may even harm patients in
case of allergic reactions because of sensitization. With many
years since approval and an aging population, the question of
efficacy and safety of repeated thrombolysis will gain importance. We here report on 8 patients who were treated twice
with rt-PA and one patient with 3 thrombolytic treatments,
the first such case in the literature, for chronologically
separated acute ischemic stroke.
excluded from analysis (n⫽3 with very early retreatment [⬍72
hours] for recurrent thromboembolism).
Demographic and baseline clinical data as well as neuroradiological data, including screening imaging modality, occurrence of
symptomatic intracerebral hemorrhage, and site of infarction, were
analyzed. Treatment and outcome parameters included the choice of
treatment, immunologic complications, and functional outcome data
assessed at 90 days using the modified Rankin Scale. Favorable
outcome was defined as a modified Rankin Scale score 0 to 2 or
recovery to the status before the acute stroke.
Results
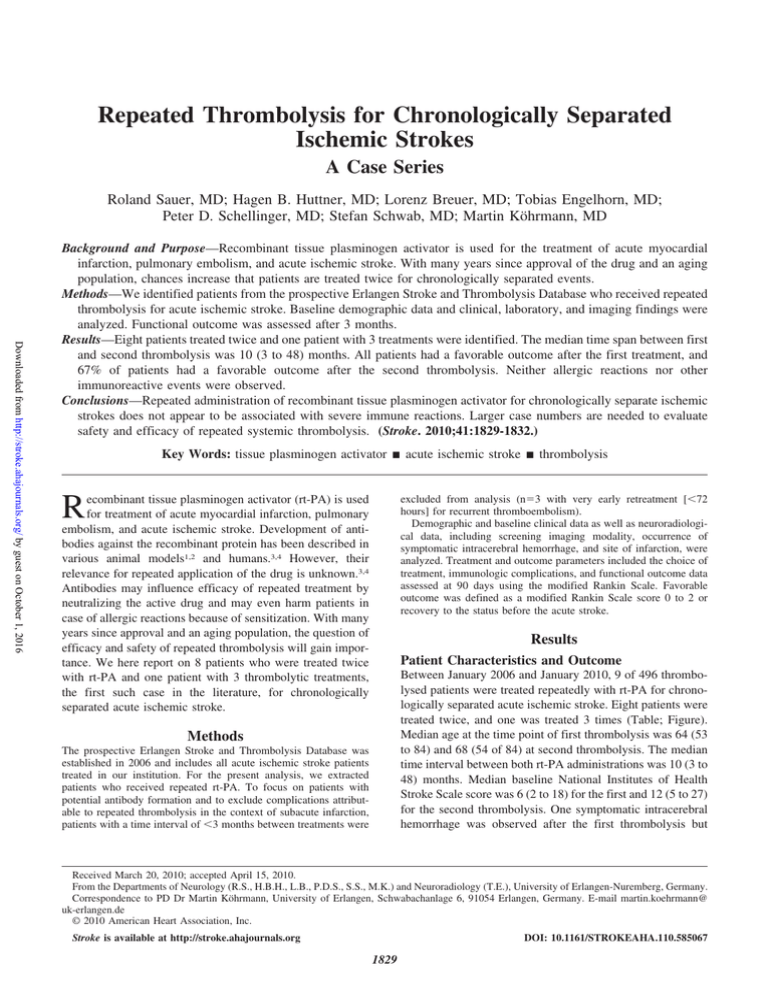
Patient Characteristics and Outcome
Between January 2006 and January 2010, 9 of 496 thrombolysed patients were treated repeatedly with rt-PA for chronologically separated acute ischemic stroke. Eight patients were
treated twice, and one was treated 3 times (Table; Figure).
Median age at the time point of first thrombolysis was 64 (53
to 84) and 68 (54 of 84) at second thrombolysis. The median
time interval between both rt-PA administrations was 10 (3 to
48) months. Median baseline National Institutes of Health
Stroke Scale score was 6 (2 to 18) for the first and 12 (5 to 27)
for the second thrombolysis. One symptomatic intracerebral
hemorrhage was observed after the first thrombolysis but
Methods
The prospective Erlangen Stroke and Thrombolysis Database was
established in 2006 and includes all acute ischemic stroke patients
treated in our institution. For the present analysis, we extracted
patients who received repeated rt-PA. To focus on patients with
potential antibody formation and to exclude complications attributable to repeated thrombolysis in the context of subacute infarction,
patients with a time interval of ⬍3 months between treatments were
Received March 20, 2010; accepted April 15, 2010.
From the Departments of Neurology (R.S., H.B.H., L.B., P.D.S., S.S., M.K.) and Neuroradiology (T.E.), University of Erlangen-Nuremberg, Germany.
Correspondence to PD Dr Martin Köhrmann, University of Erlangen, Schwabachanlage 6, 91054 Erlangen, Germany. E-mail martin.koehrmann@
uk-erlangen.de
© 2010 American Heart Association, Inc.
Stroke is available at http://stroke.ahajournals.org
DOI: 10.1161/STROKEAHA.110.585067
1829
1830
Stroke
August 2010
Table. Demographic, Clinical, and Neuroradiological Parameters As Well As Outcome Measures Before and After First and
Second Thrombolysis
Patient 9 (Three Treatments)
Age (First/Second
Thrombolysis)
Patient 1
62/64
Patient 2
84
Patient 3
76
Patient 4
71/72
Patient 5
81/83
Patient 6
62/64
Patient 7
53/54
Patient 8
64/68
62/63/65
Female
Female
Male
Male
Female
Male
Female
Female
Male
Time window (min)
90
120
125
65
140
150
90
270
60
Imaging (CT/MRI)
CT
CT
CT
CT
MRI
CT
CT
CT
CT
Sex
First thrombolysis
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
NIHSS baseline
4
9
12
2
6
2
18
3
Infarction site
MCA
PCA
MCA
MCA
MCA⫹ACA
18
MCA
MCA
BA
MCA
Thrombolysis
(iv/ia/combined)
iv
iv
iv
iv
Combined
iv
iv
iv
iv
Symptomatic
hemorrhage
No
No
No
No
No
No
No
Yes
No
Outcome day 90
(mRS)
0
1
1
0
2
1
1
2
0
Immune reaction
(yes/no)
No
No
No
No
No
No
No
No
No
Third treatment
Time between
treatments (months)
23
3
7
9
24
18
8
48
10
26 (between second
and third treatment)
0
1
1
0
2
1
1
0
0
Time window (min)
60
120
165
180
200
120
170
60
120
140
Imaging (CT/MRI)
CT
CT
CT
CT
MRI
CT
CT
CT
CT
CT
NIHSS
19
12
6
6
18
7
27 (ventilated)
22
5
7
Second thrombolysis
mRS before
second treatment
Infarction site
MCA
MCA
MCA
MCA
MCA⫹ACA
MCA
BA
MCA
MCA
PCA
Thrombolysis
(iv/ia/combined)
iv
iv
iv
iv
Combined
iv
iv
iv
iv
iv
Symptomatic
hemorrhage (yes/no)
No
No
No
No
No
No
No
No
No
No
Outcome day 90
(mRS)
4
2
1
0
3
2
1
6
0
Immune reaction
(yes/no)
No
No
No
No
No
No
No
No
No
1* (*at hospital
discharge)
No
NIHSS indicates National Institute of Health Stroke Scale; mRS, modified Rankin Scale; iv, intravenous thrombolysis; ia, intraarterial thrombolysis; ACA, anterior
cerebral artery; MCA, middle cerebral artery; PCA, posterior cerebral artery; BA, basilar artery.
none after the second. All patients achieved a favorable
outcome after the first treatment, and 6 of 9 (67%) patients
recovered to a favorable outcome after the second
thrombolysis. No hypersensivity or other immune reactions
were observed after repeated rt-PA administration.
Discussion
Longer time since approval of rt-PA and wider use in clinical
practice combined with an aging population increase the
possibility that the same patient is treated with thrombolysis
more than once. However, there are very little data on
efficacy and safety of repeated treatment with rt-PA.
Because alteplase is a purified human glycoprotein, studies
in various animal models demonstrate antibody formation
inducing altered pharmacokinetic properties as well as sensitization on re-exposure.1,2 Less immunogenicity of the recombinant endogenous protein is expected in humans. However, clinically relevant antibody formation against human
recombinant proteins have been described in the past (eg,
recombinant human insulin).5 Several studies investigated the
development of antibodies against rt-PA after treatment for a
variety of cardiac and noncardiac indications in humans.3,4
Reed et al screened 1.686 patients after rt-PA administration
and identified only 3 patients (⬍0.01%) who developed
significant titers of antibodies.3 Conversely, Cugno et al
showed significantly increased titers in 14% of cardiac
patients after treatment.4 Hence, the overall incidence of
post-treatment antibodies against rt-PA is still unclear. The
highest antibody titer in the series by Cugno et al was found
in a patient after 2 treatments. Thus, the risk appears to
increase with subsequent exposures.4 No immunologic complications were encountered in the patient with a third
exposure in our series, the first such case in the literature.
True anaphylactic reaction is rare in rt-PA–treated patients.
Rudolf et al reported a case in which preexisting IgE
antibodies against rt-PA lead to severe anaphylaxis in a
Sauer et al
Repeated Thrombolysis for Stroke
1831
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Figure. A 65-year-old patient with triple thrombolysis. A, CT before (left) and after (right) thrombolysis for isolated aphasia. Old lesion
(right middle cerebral artery), otherwise normal. Complete recovery. B, CT 10 months later for acute aphasia, rt-PA at 120 minutes. CT
before thrombolysis (left) normal, CT perfusion imaging (time to peak; middle) demonstrates hypoperfusion (left middle cerebral artery).
Complete recovery, no new infarction on follow-up (right). C, CT 26 months after B for acute aphasia and hemianopia. CT before
thrombolysis normal (left), CT perfusion (time to peak; middle) shows hypoperfusion (left posterior cerebral artery). Follow-up with new
left posterior cerebral artery infarction (right).
patient without previous exposure to the drug.6 This has to be
distinguished from anaphylactoid reactions and the development of orolingual angioedema, which is more common and
occurs in up to 2% of patients treated with rt-PA.7 It is caused
by direct activation of the complement system and kinin
cascades, with patients with angiotensin-converting enzyme
inhibitor pretreatment being more susceptible.7
Several smaller case studies reported on patients who received
repeated thrombolysis mainly for early rescue treatment after
failed intervention for myocardial infarction8 or pulmonary
embolism.9 There is only one case of repeated rt-PA treatment
for acute ischemic stroke in the literature.10 However, as in the
above-mentioned nonstroke studies, retreatment in this case was
performed shortly (90 hours) after the first thrombolysis:10 too
early for antibody formation to occur.
There are obvious limitations in our case series, the most
important being the small number of patients presented, which
does not allow firm conclusions on safety and efficacy of
repeated thrombolysis in stroke. However, to our knowledge,
this case series represents the first report on this topic. Thus, it
1832
Stroke
August 2010
may serve as a trigger for future research and gives an overview
of the available literature. Another limitation is that no antibody
titers were analyzed. This should be done in future studies.
Disclosures
H.B.H., P.D.S., and M.K. received travel grants from Boehringer
Ingelheim. P.D.S. and S.S. are members of the advisory board and
received speaker honoraria from Boehringer Ingelheim, the manufacturer of rt-PA. No funding was involved in the present study.
References
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
1. Zwickl CM, Hughes BL, Piroozi KS, Smith HW, Wierda D. Immunogenicity of tissue plasminogen activators in rhesus monkeys: antibody
formation and effects on blood level and enzymatic activity. Fundam
Appl Toxicol. 1996;30:243–254.
2. Katsutani N, Yoshitake S, Takeuchi H, Kelliher JC, Couch RC, Shionoya
H. Immunogenic properties of structurally modified human tissue plasminogen activators in chimpanzees and mice. Fundam Appl Toxicol.
1992;19:555–562.
3. Reed BR, Chen AB, Tanswell P, Prince WS, Wert RM Jr, GlaesleSchwarz L, Grossbard EB. Low incidence of antibodies to recombinant
human tissue-type plasminogen activator in treated patients. Thromb
Haemost. 1990;64:276 –280.
4. Cugno M, Cicardi M, Colucci M, Bisiani G, Merlini PA, Spinola A,
Paonessa R, Agostoni A. Non neutralizing antibodies to tissue type
plasminogen activator in the serum of acute myocardial infarction
patients treated with the recombinant protein. Thromb Haemost. 1996;
76:234 –238.
5. Fineberg SE, Galloway JA, Fineberg NS, Rathbun MJ, Hufferd S. Immunogenicity of recombinant DNA human insulin. Diabetologia. 1983;25:
465– 469.
6. Rudolf J, Grond M, Prince WS, Schmulling S, Heiss WD. Evidence of
anaphylaxy after alteplase infusion. Stroke. 1999;30:1142–1143.
7. Hill MD, Barber PA, Takahashi J, Demchuk AM, Feasby TE, Buchan
AM. Anaphylactoid reactions and angioedema during alteplase treatment
of acute ischemic stroke. CMAJ. 2000;162:1281–1284.
8. Gershlick AH, Stephens-Lloyd A, Hughes S, Abrams KR, Stevens SE,
Uren NG, de Belder A, Davis J, Pitt M, Banning A, Baumbach A, Shiu
MF, Schofield P, Dawkins KD, Henderson RA, Oldroyd KG, Wilcox R.
Rescue angioplasty after failed thrombolytic therapy for acute myocardial
infarction. N Engl J Med. 2005;353:2758 –2768.
9. Meneveau N, Seronde MF, Blonde MC, Legalery P, Didier-Petit K,
Briand F, Caulfield F, Schiele F, Bernard Y, Bassand JP. Management of
unsuccessful thrombolysis in acute massive pulmonary embolism. Chest.
2006;129:1043–1050.
10. Topakian R, Gruber F, Fellner FA, Haring HP, Aichner FT. Thrombolysis
beyond the guidelines: two treatments in one subject within 90 hours
based on a modified magnetic resonance imaging brain clock concept.
Stroke. 2005;36:e162– e164.
Repeated Thrombolysis for Chronologically Separated Ischemic Strokes: A Case Series
Roland Sauer, Hagen B. Huttner, Lorenz Breuer, Tobias Engelhorn, Peter D. Schellinger, Stefan
Schwab and Martin Köhrmann
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Stroke. 2010;41:1829-1832; originally published online July 8, 2010;
doi: 10.1161/STROKEAHA.110.585067
Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2010 American Heart Association, Inc. All rights reserved.
Print ISSN: 0039-2499. Online ISSN: 1524-4628
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://stroke.ahajournals.org/content/41/8/1829
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click
Request Permissions in the middle column of the Web page under Services. Further information about this
process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Stroke is online at:
http://stroke.ahajournals.org//subscriptions/