Intracorneal Hydrogel Lenses and Corneal Aberrations
advertisement

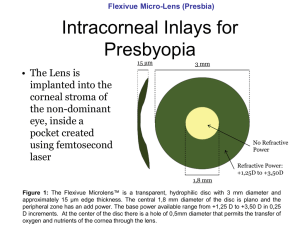
Intracorneal Hydrogel Lenses and Corneal Aberrations Jorge L. Alió, MD, PhD; Mohamed Helmy Shabayek, MD, MSc; Robert Montes-Mico, OD, MPhil; M. Emilia Múlet, MD, PhD; Ahmed Galal Ahmed, MD, MSc; Jesús Merayo, MD, PhD ABSTRACT PURPOSE: To investigate the optical performance of the cornea based on corneal aberrometry following intracorneal hydrogel lens implantation. METHODS: A retrospective, nonconsecutive, observational study of the anterior corneal surface aberration profile of four hyperopic eyes previously implanted with an intracorneal hydrogel lens were studied by videokeratographic elevation maps before and 6 months after surgery. RESULTS: Intracorneal hydrogel lenses reduced the optical performance in all four eyes by increasing the spherical aberrations by a mean factor of 1.87 and 1.95, coma aberrations by a mean factor of 2.98 and 3.01, and total higher order aberrations by a mean factor of 2.6 and 2.17 at 3.0-mm and 6.5-mm pupils, respectively (P⬍.005). CONCLUSIONS: Intracorneal hydrogel lenses decreased the optical performance of the cornea by significantly increasing spherical, coma, and total higher order aberrations. [J Refract Surg. 2005;21:247-252.] S ynthetic intrastromal implants have been investigated as a refractive surgical procedure for the past 40 years. This technology was first suggested by Barraquer in 1949.1 Assessment of the corneal tissue reaction to intracorneal hydrogel lenses was first studied in primates2-4 then in humans to prove the biocompatibility of the lens with the corneal tissue. The implantation of hydrogel intracorneal lenses in human eyes was initially performed by Werblin et al in 1992.5 The hydrogel lenses are biocompatible and implantation does not produce a significant physiological disruption. Therefore such devices can be removed or exchanged with minimal biological consequences. The most important characteristic of the hydrogel intracorneal lens is permeability, which is similar to the corneal stroma, allowing exchange of water and nutrients between the posterior and anterior layers of the cornea to maintain normal corneal physiology.2,4,6 However, despite previous reports on the refractive performance of intracorneal hydrogel lenses,4,5,7 once implanted in the human eye the effects on the finer aspects of optical performance are basically unknown. In this study, the corneal aberration pattern that results following implantation of intracorneal hydrogel lenses was evaluated. PATIENTS AND METHODS This study comprised four eyes of three patients implanted with intracorneal hydrogel lenses between February and April 2002. The criteria for selecting these cases included From the Department of Refractive Surgery, Vissum Instituto Oftalmológico de Alicante and Division of Ophthalmology, Miguel Hernández University, Medical School, Alicante, Spain (Alió, Shabayek, Montes-Mico, Múlet, Ahmed); Research Institute of Ophthalmology, Giza, Egypt (Shabayek, Ahmed); and Instituto de Oftalmobiologia Aplicada, University of Valladolid, Spain (Merayo). This study was supported in part by a grant of the Spanish Ministry of Health, Instituto Carlos III, Red Temática de Investigación en Oftalmología, Subproyecto de Cirugía Refractiva y Calidad Visual (C03/13). The authors have no proprietary interest in the materials presented herein. Correspondence: Jorge L. Alió, MD, PhD, Instituto Oftalmológico de Alicante, Avda. Denia, s/n, (Edificio VISSUM) 03016 Alicante, Spain. Tel: 96 5150025; Fax: 96 5151501; E-mail: jlalio@oftalio.com Received: April 29, 2004 Accepted: October 6, 2004 Journal of Refractive Surgery Volume 21 May/June 2005 JRS0505ALIO.indd 247 247 5/11/2005 8:58:46 AM Intracorneal Hydrogel Lenses and Corneal Aberrations/Alió et al TABLE 1 Preoperative and 6-month Postoperative Visual Acuity and Refraction in Four Eyes With Intracorneal Hydrogel Lenses Eye Parameter 1 2 3 4 Preoperative UCVA 0.4 0.3 0.15 0.2 Sphere (D) ⫹5.50 ⫹5.50 ⫹3.50 ⫹3.50 Cylinder (D) ⫺1.50 ⫺1.00 ⫺1.75 ⫺1.00 Axis (°) 25 155 20 10 SE (D) ⫹4.75 ⫹5.00 ⫹2.75 ⫹3.00 BSCVA 1.0 1.0 0.2 0.6 ⫹6.00 ⫹6.00 ⫹3.00 ⫹4.00 5.00 5.00 5.00 5.00 0.6 0.4 0.15 0.6 Sphere (D) ⫹1.00 ⫹2.00 ⫹3.00 0 Cylinder (D) ⫺1.75 ⫺2.00 ⫺1.00 ⫺1.50 INLAY labeled power (D) INLAY diameter (mm) 6-month Postoperative UCVA Axis (°) 40 130 15 20 SE (D) ⫹0.25 ⫹1.00 ⫹2.50 ⫺0.75 BSCVA 0.9 0.8 0.2 0.8 UCVA = uncorrected visual acuity, SE = spherical equivalent refraction, BSCVA = best spectacle-corrected visual acuity complete normal postoperative clinical outcome, no observable corneal edema or decentration of the intracorneal hydrogel lens, no tear film dysfunction, and no other complication that would lead to postoperative manipulation of the intracorneal hydrogel lens 6 months postoperatively. Mean patient age was 47.5⫾16.1 years (range: 24 to 58 years). All eyes were implanted with PermaVision intracorneal hydrogel lenses (Anamed Inc, Lake Forest, Calif) following the surgical protocol provided by the manufacturer. This hydrogel lens has a water content of ⬎70%, a refractive index of 1.37, and a 5-mm diameter. The intracorneal hydrogel lenses were implanted after creation of an inferior hinged 8.5-mm corneal flap using the 180-µm head of the M2 microkeratome (Moria, Antony, France). The corneal flap was centered with respect to limbus and had a 4-mm hinge. Following the manufacturer’s indications, a “dry technique” was used for implantation of the intracorneal hydrogel 248 JRS0505ALIO.indd 248 lenses. In such a technique, the interface was not irrigated after the microkeratome cut or after lens implantation. The lenses were placed in the pupil zone of the stromal bed by means of a specific manual vacuum device provided with the inlay. The postoperative treatment included 0.3% ofloxacin (Exocin; Allergan, Madrid, Spain) four times/day combined with tobramycin 0.3% and 0.1% dexamethasone (Tobradex; Alcon Cusí, Barcelona, Spain). These three patients (four eyes) were selected from a larger cohort of patients who underwent implantation in 2002 following a strict protocol approved by the ethical board committee at our institute. Preoperative and 6-month postoperative corneal topography maps were obtained using the Orbscan II Slit Scanning Corneal Topography/Pachymetry System, version 3.10.27 (Orbtek, Salt Lake City, Utah). Measurements in each eye were repeated until a well-focused and aligned image was obtained. Corneal videokeratographic data were downloaded onto floppy disks in ASCII files that contained information regarding corneal elevation, curvature, power, and position of the pupil. The aberrometric wavefront data were fit with Zernike polynomials up to the sixth order to determine the aberration coefficients, using CT-View Software (Sarver & Associates, Fla) from which the wavefront aberration function was reconstructed. From the Zernike coefficient, the root-mean-square (RMS) wavefront errors for spherical-like aberrations (fourth-order component Z14 and the sixth-order component Z06) and coma-like aberrations (third-order components Z13 and fifth-order component Z15) were calculated. Because of the linear independence of the Zernike terms, the higher order RMS wavefront error was computed by adding all components (ie, the total RMS error was the square root of the sum of the squares of the RMS values of the components except astigmatism). RESULTS Preoperative and 6-month postoperative visual acuity, refraction, inlay labeled power, and diameter are shown in Table 1. As expected, in all four eyes, the RMS value of the spherical, coma, and total higher order aberrations increased at 3.0-mm and 6.5-mm pupils from before to after implantation of the intracorneal hydrogel lens (Tables 2 and 3). The mean difference between pre- and postoperative RMS spherical aberration was 0.185 µm (P⭐.005) and 0.2140 µm (P⭐.004) for the 3.0-mm and 6.5-mm pupils, respectively. Similarly, the difference in coma aberration was 0.0584 µm (P⭐.000) and 0.5652 µm (P⭐.002) and for total higher order aberrations was journalofrefractivesurgery.com 5/11/2005 8:58:51 AM Intracorneal Hydrogel Lenses and Corneal Aberrations/Alió et al TABLE 2 Change in Corneal Aberrations (µm) After Intracorneal Hydrogel Lens Implantation for a 3.0- and 6.5-mm Pupil 3.0-mm Pupil Eye 1 2 3 4 RMS (Aberration) Preoperative Spherical 0.0227 6.5-mm Pupil Postoperative Increasing Factor (%) Preoperative Postoperative Increasing Factor (%) 0.0381 167 0.2299 0.5187 225 Coma-like 0.0313 0.0861 275 0.3186 0.8338 261 Higher order 0.0531 0.1229 231 0.5472 1.4731 269 Spherical 0.0229 0.0377 164 0.2414 0.4043 167 Coma-like 0.0318 0.0914 287 0.3678 0.8177 222 Higher order 0.0588 0.1244 211 0.5278 1.1285 213 Spherical 0.0212 0.0395 186 0.2016 0.4039 200 Coma-like 0.0207 0.0817 385 0.2011 0.8067 401 Higher order 0.0424 0.1378 325 0.4291 1.2174 283 Spherical 0.0189 0.0444 234 0.2278 0.4297 188 Coma-like 0.0397 0.0978 246 0.3088 0.9988 323 Higher order 0.0618 0.1879 304 0.5379 1.4759 274 RMS = root-mean-square 0.0892 µm (P⭐.008) and 0.8132 µm (P⭐.002) for the 3.0-mm and 6.5-mm pupils, respectively. DISCUSSION Along with refractive outcome, quality of vision is also important after refractive surgery. The introduction of wavefront science in refractive surgery has provided a better understanding of the optical performance of the eye following different procedures. Refractive intracorneal hydrogel lens surgery may be accompanied by different clinical complications that may affect overall clinical outcome.7 However, the optical behavior in terms of aberrometry performance of the intracorneal hydrogel lens once implanted in the human cornea for the correction of hyperopia has never been reported, hence we are unable to compare our results with any previous data. The changes in the pattern of corneal aberrations observed in this study might be caused only by the microkeratome cut or by the presence of the inlay. Porter et al8 and Pallikaris et al9 studied the aberrations induced by the microkeratome cut and reported that the microkeratome cut can generate significant but small increases in higher order aberrations. In relation to the hyperopic patients evaluated, the magnitude of preoperative corneal RMS aberration Journal of Refractive Surgery Volume 21 May/June 2005 JRS0505ALIO.indd 249 appears to lie within normal limits reported for 3.0and 6.0-mm pupil sizes.10 If we consider the results obtained in corneal aberrations after intracorneal hydrogel lens implantation, an increase was found in the total higher order aberration terms. Table 2 shows the change after intracorneal hydrogel lens implantation for all eyes studied. The Figure shows the change for all aberrations at both pupil diameters. According to these data, spherical-like, coma-like, and total higher order aberrations all increased after intracorneal hydrogel lens implantation by a factor of between 1.8 and 3.7 times for both pupil diameters. The results were statistically significant at the 1% level for both pupil diameters (P⬍.001). If we consider the results in more detail, changes in spherical aberration (fourth-order term, Z04) are caused by shifting the thickness distribution within the cornea followed by a change in corneal surface topography. Intracorneal hydrogel lens implantation creates a more prolate cornea, thereby inducing a negative shift in spherical aberration (by mean of ⫻1.87 and ⫻1.94, 3.0- and 6.5-mm pupil, respectively). The total amount of the spherical aberration changes should depend on the thickness of the intracorneal hydrogel lens implanted for a particular diameter. Due to the small sample of cases implanted with intracorneal hydrogel lenses (four 249 5/11/2005 8:58:51 AM Intracorneal Hydrogel Lenses and Corneal Aberrations/Alió et al TABLE 3 Mean Difference of Root-Mean-Square (RMS) Value Preoperatively and Postoperatively for 3.0- and 6.5-mm Pupils Aberration Postoperative Difference Pre- and Postoperative (P value) 0.0214 0.0399 .005 0.0189 to 0.0229 (0.0018) 0.0377 to 0.0444 (0.003) Preoperative Spherical 3.0-mm pupil Range (SD) 6.5-mm pupil Range (SD) Difference 3.0- and 6.5-mm (P value) 0.2252 0.4392 0.201 to 0.241 (0.016) 0.4039 to 0.5187 (.05) .0001 .001 .004 Coma-like 3.0-mm pupil Range (SD) 6.5-mm pupil Range (SD) Difference 3.0- and 6.5-mm (P value) 0.0309 0.0893 0.0207 to 0.0397 (0.007) 0.0817 to 0.0978 (0.006) 0.2991 0.8643 0.201 to 0.367 (0.07) 0.8067 to 0.9988 (0.09) .004 .0003 0.0540 0.1432 0.0424 to 0.0618 (0.08) 0.1229 to 0.1879 (0.03) 0.5105 1.3237 0.429 to 0.547 (0.05) 1.1285 to 1.4759 (0.17) .0003 .001 .000 0.002 Total higher order 3.0-mm pupil Range (SD) 6.5-mm pupil Range (SD) Difference 3.0- and 6.5-mm (P value) eyes), it is not possible to assess a correlation between preoperative spherical error and induced postoperative spherical aberration. However, it would be expected that the increment of spherical aberration would be directly related to the preoperative refraction: the larger the correction, the larger amount of spherical aberration induced by intracorneal hydrogel lens implantation. Comparison of our findings with those reported on corneal aberrometry changes induced by hyperopic laser in situ keratomileusis (LASIK)10 shows that changes in spherical aberration are similar between hyperopic LASIK and intracorneal hydrogel lens implantation for photopic conditions (3.0-mm pupil). However, some discrepancies are found when we compare those results under mesopic conditions (6.5-mm pupil). Wang and Koch10 found a reduction in spherical aberration after hyperopic LASIK in contrast to ours (Table 2), which revealed an increase under photopic conditions. Considering that our results are computed for a 6.5-mm pupil and those of the previous authors10 are for a 6.0-mm pupil, we believe the difference is due to the different paracentral region of the cornea between post-hyper250 JRS0505ALIO.indd 250 .008 .002 opic LASIK and intracorneal hydrogel lens implantation. The first has a 6-mm ablation zone and a 9-mm transition zone, and the intracorneal hydrogel lens has an optical diameter of 5.00. Therefore, a transition zone between the ablated and non-ablated cornea is expected to reduce the change in spherical aberration. If we consider the changes found in coma-like aberration (Table 2), the mean increasing factor ranged from 2.94 to 3.71 (3.0-mm and 6.5-mm pupil, respectively). Although the increase in spherical aberration is systematic, an intereye variability is present in the amount of coma induced by intracorneal hydrogel lens implantation. As mentioned earlier for spherical aberration, we do not have enough data to correlate the change in coma-like aberration with preoperative spherical error. However, in contrast to spherical aberration change, coma-like aberration should not correlate with preoperative error in the same way (eg, eye 3, which required half the correction required for eyes 1 and 2, had a more noticeable increase in coma-like aberration). Compared with hyperopic LASIK, we found large amounts of coma-like change after surgery. For journalofrefractivesurgery.com 5/11/2005 8:58:52 AM Intracorneal Hydrogel Lenses and Corneal Aberrations/Alió et al preoperative postoperative preoperative 0.16 1.4 0.14 1.2 0.12 1 RMS 0.1 RMS postoperative 0.08 0.8 0.6 0.06 0.4 0.04 0.2 0.02 0 Spherical Aberration Coma-like Aberration 0 Higher Order Aberration 3.0-mm Pupil A Spherical Aberration Coma-like Aberration Higher Order Aberration 6.5-mm Pupil B Figure. Mean changes in corneal aberrations (µm) after intracorneal hydrogel lens implantation for a A) 3.0-mm and B) 6.5-mm pupil. example, Wang and Koch10 found an increasing factor between 1.03 and 1.42 after LASIK and our results revealed a factor between 2.22 and 4.01 (photopic and mesopic conditions). They explained the reductions in coma aberration could be expected from lasers with eye tracker systems. In fact, they found lower values in coma using the VISX Star S3 versus the VISX Star S2 (VISX, Santa Clara, Calif) (eye tracker and non-eye tracker systems, respectively). How can we explain our increasing factor in coma aberration after intracorneal hydrogel lens implantation? We believe that centration of the intracorneal hydrogel lens plays a decisive role in this change. Despite this fact, we did not observe any decentration clinically. A slight degree of misalignment with respect to the line of sight, which is used for centration during topography, and the intracorneal hydrogel lens optical axis will provoke an increase in this non-rotationally symmetric aberration. The effect of simulated pupil dilation, from 3.0- to 6.5-mm, is consistent with previous reports on the effect of pupil dilation on corneal aberrations.10-13 Although previous studies reported the effect after photorefractive keratectomy or LASIK procedures, it seems reasonable to attribute the change to the same source when the pupil dilates in intracorneal hydrogel lens implantation. Those changes between the mid-peripheral region of the cornea induced by intracorneal hydrogel lens insertion modify the corneal profile, giving a bifocal effect and consequently an increase of the corneal aberration when large pupils are considered.14 Intracorneal hydrogel lens implantation increases higher order corneal aberrations. In coma-like aberration, improvements in intracorneal hydrogel lens centration could aid postoperative optical quality. The change in spherical aberration, which is greater folJournal of Refractive Surgery Volume 21 May/June 2005 JRS0505ALIO.indd 251 lowing intracorneal hydrogel lens implantation than LASIK surgery, is probably a function of the intended cornea steepening and the flattening of the mid-peripheral region. Modifying the peripheral form of the intracorneal hydrogel lens (eg, choosing an aspheric design), could improve the optical quality of the postoperative surface. REFERENCES 1. Barraquer JI. Modification of refraction by means of intracorneal inclusions. Int Ophthalmol Clin. 1966;6:53-78. 2. McCarey BE, Andrews DM. Refractive keratoplasty with intrastromal hydrogel lenticular implants. Invest Ophthalmol Vis Sci. 1981;21:107-115. 3. McDonald MB, McCarey BE, Storie B, Beuerman RW, Salmeron B, van Rij G, Knight PM. Assessment of long-term corneal response to hydrogel intrastromal lenses implanted in monkey eyes for up to five years. J Cataract Refract Surg. 1993;19:213-222. 4. Barraquer JI, Gomez ML. Permalens hydrogel intracorneal lenses for spherical ametropia. J Refract Surg. 1997;13:342-348. 5. Werblin TP, Patel AS, Barraquer JI. Initial human experience with Permalens myopic hydrogel intracorneal lens implants. Refract Corneal Surg. 1992;8:23-26. 6. Maurice DM. The cornea and sclera. In: Davison H, ed. The Eye. New York, NY: Academic Press; 1984:95. 7. Alió JL, Mulet EM, Zapata LF, Vidal MT, De Rojas V, Javaloy J. Intracorneal INLAY complicated by intrastromal epithelial opacification. Arch Ophthalmol. 2004;122:1441-1446. 8. Porter J, MacRae S, Yoon G, Roberts C, Cox IG, Williams DR. Separate effects of the microkeratome incision and laser ablation on the eye’s wave front aberration. Am J Ophthalmol. 2003;136:327-337. 9. Pallikaris IG, Kymionis GD, Panagopoulou SI, Siganos CS, Theodorakis MA, Pallikaris AI. Induced optical aberrations following formation of a laser in situ keratomileusis flap. J Cataract Refract Surg. 2002;28:1737-1741. 10. Wang L, Koch DD. Anterior corneal optical aberrations induced by laser in situ keratomileusis for hyperopia. J Cataract Refract Surg. 2003;29:1702-1708. 11. Martinez CE, Applegate RA, Klyce SD, McDonald MB, Medina 251 5/11/2005 8:58:52 AM Intracorneal Hydrogel Lenses and Corneal Aberrations/Alió et al JP, Howland HC. Effect of pupillary dilation on corneal optical aberrations after photorefractive keratectomy. Arch Ophthalmol. 1998;116:1053-1062. 12. Marcos S, Barbero S, Llorente L, Merayo-Lloves J. Optical response to LASIK surgery for myopia from total and corneal aberration measurements. Invest Ophthalmol Vis Sci. 2001;42:33493356. 252 JRS0505ALIO.indd 252 13. Oshika T, Miyata K, Tokunaga T, Samejima T, Amano S, Tanaku S, Hirhara Y, Mihashi T, Maeda N, Fujikado T. Higher order wave front aberrations of cornea and magnitude of refractive correction in laser in situ keratomileusis. Ophthalmology. 2002;109:1154-1158. 14. Montes-Mico R, Charman WN. Image quality and visual performance in the peripheral visual field following photorefractive keratectomy. J Refract Surg. 2002;18:14-22. journalofrefractivesurgery.com 5/11/2005 8:58:52 AM